Abstract
BACKGROUND AND PURPOSE: The evidence for traumatic brain injury in amateur boxers is controversial. Hypothetically, sudden acceleration of the head due to the impact of the blow during the boxing fight might result in diffuse axonal injury or contusion. We wanted to determine whether cerebral microhemorrhages occur more often in amateur boxers than in nonboxers.
MATERIALS AND METHODS: In 42 male, classical amateur boxers and in 37 healthy, nonboxing male volunteers we performed cranial MR imaging at 3T. The study protocol included a transverse dual spin-echo MR imaging sequence, a 3D sagittal magnetization-prepared rapid acquisition of gradient echo sequence, a coronal T2*-weighted sequence, and an axial time-of-flight MR angiography sequence. MR imaging data were made anonymous before 2 neuroradiologists independently evaluated the images. In addition, the following risk factors were assessed: total numbers of fights and knockouts, weight division, and duration of boxing. We compared the group proportions of microhemorrhages with Fisher test of exact probability.
RESULTS: There was a statistically higher prevalence of cerebral microhemorrhages in the group of boxers (3 of 42; 7.1%) than in nonboxing persons (0 of 37; 0%). This difference was not statistically significant, however (P = .2479; Fisher exact test).
CONCLUSION: Although we detected more microhemorrhages in amateur boxers than in nonboxing persons, this difference did not prove to be significant.
Hypothetically, sudden acceleration of the head because of the impact of a blow during a boxing fight might result in cerebral contusion involving the superficial gray matter, in diffuse axonal injury (DAI) from axonal stretching because of a movement of the overlying cerebral cortex relative to the underlying cerebral white matter, or in subcortical injury. DAI can be detected by MR imaging as multiple round or ovoid lesions of the cerebral white matter, especially at the gray/white matter interface (corticomedullary junction), the corpus callosum, and the upper brain stem, representing multifocal punctate hemorrhages. T2*- and susceptibility-weighted gradient-echo images are very useful tools for detecting small foci of hemorrhage in the brain. An additional increase in the sensitivity for detecting hemorrhagic shear injuries can be achieved using higher MR field strengths, such as 3T.1 Because the evidence concerning traumatic brain injury in amateur boxers is controversial,2–6 the aim of our study was to determine the prevalence of cerebral microhemorrhages in boxers as compared with nonboxers by using 3T MR imaging. Our working hypothesis was that MR imaging would show a higher prevalence of cerebral microhemorrhages in amateur boxers than in nonboxers.
Methods
We studied 42 male, classical amateur boxers ranging in age between 18 and 73 years (mean age, 33 years) and 37 healthy, nonboxing male volunteers ranging in age between 18 and 66 years (mean age, 29 years). The mean duration of boxing was 11 years, ranging between 1 and 25 years. The total number of fights ranged between 1 and 375 (Table). Three of the boxers (subjects 3, 14, and 22) could not specify the exact number of fights; in these boxers, the total number of fights was estimated according to the duration of boxing and the average number of fights per year. Three of the boxers (subjects 10, 15, and 27) had never participated in fights but only in training. The total number of knockouts in each boxer ranged between 0 and 12. Boxers and control persons with neurologic and other diseases involving the central nervous system, such as metabolic disorders, traumatic brain injury, epilepsia, perinatal asphyxia, arterial hypertension, or drug abuse, were generally excluded from this study. Furthermore, American football players, soccer players, participants of other forms of contact sport, and persons who had previously been involved in a car crash were excluded. None of the boxers had participated in fights in which they lost consciousness or were hospitalized. All of these data were acquired using a standardized protocol in the form of a questionnaire and by clinical and neurologic examination of the boxers and the nonboxing persons. The control persons were recruited by asking friends and colleagues to acquire normal MR datasets for this and other MR imaging-based studies. The data from patients and control subjects were accrued during the period from January 2005 to February 2006. All of the MR images were acquired using a 3T unit (TRIO; Siemens, Erlangen, Germany) with an 8-channel head coil. The MR imaging protocol included a transverse dual spin-echo MR imaging sequence (TR/TE, 5850/10,90 ms; section thickness, 6 mm; flip angle, 149°, acquisition matrix, 256 × 256 ms; and FOV, 200 mm), a 3D sagittal magnetization-prepared rapid acquisition of gradient echo (MPRAGE) sequence (TR/TE, 2250/3 ms; section thickness, 1 mm; flip angle, 9°; acquisition matrix, 256 × 256 ms; and FOV, 245 mm), a coronal T2*-weighted sequence (TR/TE, 599/20 ms; section thickness, 6 mm; flip angle, 20°; acquisition matrix, 256 × 256 ms; and FOV, 200 mm), and an axial time-of-flight (TOF) MR angiography sequence (TR/TE, 42/4,67 ms; section thickness, 0.8 mm; flip angle, 25°; acquisition matrix, 512 × 512 ms; and FOV, 200 mm). MR imaging data were made anonymous before evaluation. The study protocol was approved by our institutional review board, and informed consent was obtained from each subject according to the Declaration of Helsinki 2000.
History of the boxers
| Case (No.) | Age, y | Weight Division Up To, kg | Duration of Boxing, y | Kind of Boxing |
Total No. of Knockouts | Total No. of Fights | Microhemorrhage Present | ||
|---|---|---|---|---|---|---|---|---|---|
| Classical | Thai | Kick | |||||||
| 1 | 36 | 93 | 11 | Yes | Yes | Yes | 2 | 46 | No |
| 2 | 25 | 60 | 6 | Yes | No | No | 1 | 2 | Yes |
| 3 | 40 | 74 | 25 | No | Yes | Yes | 0 | >50 | Yes |
| 4 | 26 | 72 | 14 | Yes | No | No | 3 | 72 | No |
| 5 | 24 | 57 | 11 | Yes | No | No | 0 | 76 | No |
| 6 | 21 | 62 | 17 | Yes | No | No | 0 | 85 | No |
| 7 | 65 | 97 | 10 | Yes | No | No | 0 | 76 | No |
| 8 | 36 | 67 | 15 | Yes | No | No | 10 | 30 | No |
| 9 | 27 | 76 | 4 | Yes | No | No | 9 | 12 | No |
| 10 | 27 | 69 | 1 | Yes | Yes | No | 0 | 0 | No |
| 11 | 48 | 75 | 25 | Yes | No | No | 3 | 12 | No |
| 12 | 62 | 75 | 10 | Yes | No | No | 3 | 75 | No |
| 13 | 73 | 84 | 12 | Yes | No | No | 1 | 200 | No |
| 14 | 20 | 84 | 4 | Yes | No | No | 0 | >100 | No |
| 15 | 46 | 73 | 3 | Yes | No | No | 0 | 0 | No |
| 16 | 32 | 84 | 13 | Yes | Yes | Yes | 8 | 25 | No |
| 17 | 37 | 85 | 10 | Yes | Yes | Yes | 12 | 10 | No |
| 18 | 28 | 65 | 3 | Yes | No | No | 1 | 13 | No |
| 19 | 21 | 60 | 10 | Yes | No | No | 0 | 110 | No |
| 20 | 24 | 61 | 8 | Yes | No | Yes | 0 | 86 | No |
| 21 | 19 | 90 | 6 | Yes | No | No | 0 | 35 | No |
| 22 | 30 | 57 | 18 | Yes | No | No | 0 | >150 | No |
| 23 | 23 | 60 | 12 | Yes | No | No | 0 | 140 | Yes |
| 24 | 48 | 103 | 16 | Yes | No | No | 2 | 375 | No |
| 25 | 24 | 87 | 5 | Yes | No | No | 1 | 1 | No |
| 26 | 27 | 85 | 6 | Yes | Yes | No | 6 | 10 | No |
| 27 | 38 | 81 | 15 | Yes | No | Yes | 0 | 0 | No |
| 28 | 18 | 50 | 7 | Yes | No | No | 1 | 51 | No |
| 29 | 18 | 55 | 7 | Yes | No | No | 0 | 65 | No |
| 30 | 27 | 91 | 12 | Yes | No | No | 0 | 105 | No |
| 31 | 23 | 77 | 9 | Yes | No | No | 0 | 150 | No |
| 32 | 22 | 64 | 12 | Yes | No | No | 0 | 176 | No |
| 33 | 52 | 77 | 14 | Yes | No | No | 1 | 216 | No |
| 34 | 20 | 58 | 10 | Yes | No | No | 2 | 120 | No |
| 35 | 18 | 77 | 4 | Yes | No | No | 0 | 42 | No |
| 36 | 22 | 67 | 10 | Yes | No | No | 0 | 173 | No |
| 37 | 20 | 76 | 10 | Yes | No | No | 0 | 110 | No |
| 38 | 18 | 57 | 6 | Yes | No | No | 0 | 96 | No |
| 39 | 20 | 82 | 6 | Yes | Yes | No | 1 | 80 | No |
| 40 | 39 | 80 | 8 | Yes | No | No | 0 | 60 | No |
| 42 | 54 | 76 | 26 | Yes | No | No | 1 | 122 | No |
| 41 | 53 | 100 | 22 | Yes | No | No | 2 | 165 | No |
Statistical Analysis
We compared the group proportions of microhemorrhages with Fisher test of exact probability and obtained 95% confidence intervals from statistical tables. The level of significance was set at P < .05.
Results
Microhemorrhages were found in 3 (7.1%) of 42 boxers. In subjects 2 and 3, the microhemorrhages were seen as hypointense foci on the T2*-weighted images, hypointense foci on the MPRAGE images with a continuous or discontinuous hyperintense rim because of susceptibility from blood products, and hypointense foci on the axial TOF source images. In subject 23, the microhemorrhages were not visible on the coronal T2*-weighted images because of artifacts from the bone of the skull base, but only on the MPRAGE images and the axial TOF source images. In 1 boxer, 2 separate microhemorrhages were detected (subject 23), whereas in the other boxers, only solitary lesions were visible. In the group of nonboxing persons, microhemorrhages were detected in 0 (0%) of 37. This difference was not statistically significant (P = .2479; Fisher exact test; confidence interval, 95%). The microhemorrhages were exclusively located at the gray/white matter interface (corticomedullary junction) of the frontal or temporal lobes. In detail, the microhemorrhages were located adjacent to the right orbital gyrus (subject 2, Fig 1), adjacent to the left inferior temporal gyrus (subject 3, Fig 2), and adjacent to the left rectal gyrus (subject 23). The magnetic susceptibility artifact because of the hemoglobin products of the microhemorrhages ranged in size between 1 (subjects 2 and 23) and 3 mm (subject 3). No other imaging abnormalities were detected either in the boxers or in the nonboxing persons.
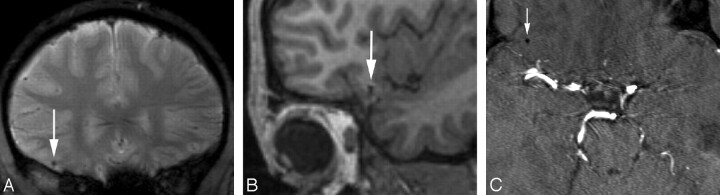
Fig 1.
Case 2. Microhemorrhage adjacent to the right orbital gyrus. A, Coronal T2* weighted image; B, Sagittal T1-weighted image of the 3D sagittal MPRAGE sequence; and C, axial TOF source image showing an hypointense focus with a diameter of approximately 2 mm (arrows).
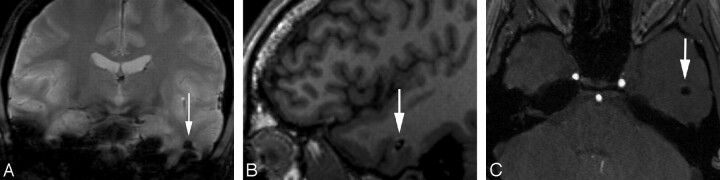
Fig 2.
Case 3. Microhemorrhage adjacent to the left inferior temporal gyrus. A, Coronal T2* weighted image; B, Sagittal T1-weighted image of the 3D sagittal MPRAGE sequence; and C, Axial TOF source image showing an hypointense focus with a diameter of approximately 3 mm (arrows).
Discussion
DAI because of axonal stretching has been described as a major form of primary damage to the brain in blunt head injury. Repetitive exposure to head blows in contact sports, such as boxing and soccer, are supposed to result in chronic traumatic encephalopathy with the consequence of dementia pugilistica.2–6
Pathoanatomic data of boxers mainly result from collections of case reports and from small histopathologic studies.2–6 Although there are many more or less sensational reports of epidural, subdural, intraparenchymal, and subarachnoid hemorrhages in boxers, to our knowledge no systematic neuroanatomic studies have been conducted, let alone case-control studies. Nevertheless, according to the review by Unterharnscheidt,2 clinical and morphologic publications show convincingly that participation in boxing leads to severe permanent brain damage.
A number of imaging techniques have been used to investigate changes produced in the brain by boxing. The most important brain abnormalities that have been suggested to be associated with boxing are cerebral and cerebellar atrophy, nonspecific white matter changes such as gliosis, and fenestrations of the cavum of the septum pellucidum.2–6 Until now, however, the few existing systematic morphologic studies on boxers have failed to show significant correlations between boxing and putative abnormalities by neuroimaging.5
The violence of a blow to the head in boxing is related to the velocity of the fist and the masses involved. It further depends on the mechanical properties of the colliding bodies, the glove, and the head. On impact, a force is produced on both the gloved fist and the head. The head is accelerated, and the fist is decelerated. Both bodies are deformed by the force of this impact. The compressibility of the glove is so much greater than that of all of the other elastic elements in the system, such as skin and bones, that it can be ignored.7 The influence of the head guard with its rather large elastic constant is small when the glove being used is soft and weighty (higher number of ounces) and, consequently, its elastic constant is small. The effectiveness of the head protection grows in relation to the progressing rigidity of the glove, that is, with the use of lighter gloves (lower number of ounces).7 Although in amateur boxers, gloves of 10 ounces (284 g) are prescribed for all weight classes, in professional boxers gloves of 8 ounces (227 g) are used for the weight classes miniflyweight to welterweight, and gloves of 10 ounces are used for the weight classes cruiserweight to heavyweight. In contrast to amateur boxing, where a head guard is mandatory, a head guard is not permitted in professional boxing. Therefore, the impact forces on the head are higher in professional boxers than in amateur boxers, and it must be expected that microstructural changes in the brain of professional boxers are also more pronounced than in amateurs. In kickboxing, a head guard is prescribed only in boxers younger than 17 years of age; a mouthguard is generally prescribed in kickboxing. In contrast to classical boxing, in kickboxing, not only blows but also kicks to the head of the opponent are allowed.
In our study, there was a statistically higher prevalence of cerebral microhemorrhages in the group of the boxers (3 of 42; 7.1%) than in the nonboxing persons (0 of 37; 0%). However, this difference was not statistically significant (P = .2479; Fisher exact test). Therefore, according to our study in 42 boxers, the working hypothesis that MR imaging will show a higher prevalence of cerebral microhemorrhages in amateur boxers than in nonboxers was not confirmed. Assuming a prevalence of microhemorrhages of 7% in the whole population of amateur boxers, as we found in our small sample of 42 boxers, and one of 0% in age-related, nonboxing persons, the number of boxers that have to be imaged is estimated at 106, when a β-value (risk of type 2 error) of 20% (statistical power = 80%) and an α-value (risk of type 1 error) of 5% are taken as a basis.8
Our study has several limitations. For several reasons, it was not possible to include very many boxers and matching nonboxing persons in our study. In addition to the small sample size, MR imaging was only performed at 1 time point in the boxers, and a baseline MR image had not been acquired before they started their boxing career. However, it is difficult to design such a longitudinal study, and this would haven taken our group more than 20 years. Furthermore, MR imaging technology is evolving very rapidly. The optimal study protocol for the assessment of traumatic brain injury in amateur boxers would include a baseline MR image before the boxers start their career, yearly follow-up MR images after every season, and a final scan after the boxers have finished their boxing career. Therefore it would be difficult to image persons by MR and to reimage them recurrently during a period of 10–25 years using identical scan parameters. In our study, many boxers (n = 22; 52%) had never been knocked out, and only 2 boxers (4.8%) suffered more than 10 knockouts. Therefore, the prevalence of microhemorrhages in the whole population of boxers, and especially in boxers who suffered knockouts, may possibly be higher than the overall prevalence of microhemorrhages in our study. Our study was not designed to compare the sensitivity of 1.5T and 3T regarding cerebral microhemorrhages in boxers, making further comparative studies necessary to confirm the advantages of 3T MR imaging.
Interestingly, the microhemorrhages that we found generally were located at the corticomedullary junction of the frontal and temporal lobes. This location is typical for DAI, when the overlying cortex moves at a different speed in relation to underlying deep brain structures, resulting in axonal stretching.1 Therefore, we believe that, considering size and location (corticomedullary junction), the microhemorrhages that we found are most likely the result of DAI. The most important differential diagnoses of our findings are multifocal hemorrhagic lesions of other origin, such as amyloid angiopathy, hypertensive microhemorrhages, and cavernous vascular malformations (cavernous hemangioma or cavernoma). However, amyloid angiopathy occurs preferentially in elderly, often demented persons. Hypertensive microhemorrhages result from long-standing, chronic arterial hypertension, and cavernous malformations are lobulated vascular masses with blood products at different ages and a “mulberry”-like or “popcorn ball” appearance.
The most recent systematic study on structural brain abnormalities in amateur boxers as detected by MR imaging was performed in 1992 by Holzgraefe et al.9 In this study of 13 boxers, no brain abnormalities were found, and the prevalence of cerebral microhemorrhages was 0%.9 However, this study was performed on a 0.5T MR scanner, and only 10-mm-thick images were acquired. Our study was performed on a 3T MR scanner, and thin sections down to 1 mm were analyzed. Therefore, the sensitivity of our MR study concerning microstructural lesions, such as microhemorrhages, is much higher than that of the study of Holzgraefe et al9 at 0.5T and of other past and possible future studies using field strengths lower than 3T.
By the use of diffusion tensor MR imaging, Zhang et al10,11 found higher diffusion constants in the brains of professional boxers than in control subjects. These data suggest that concussion because of professional boxing may lead to microstructural brain damage and subsequent elevation of whole-brain water diffusion. Microhemorrhages are not reported in these studies, however.10,11
Conclusion
Although we found more microhemorrhages in boxers than in nonboxers, our working hypothesis that MR imaging will show a higher prevalence of cerebral microhemorrhages in amateur boxers than in nonboxers was not confirmed. The prevalence of microhemorrhages in amateur and in professional boxers should be assessed in a larger population of boxers. In particular, it would be of interest to track the origin of microhemorrhages associated with repetitive trauma and to identify correlations between these lesions and cognitive function, boxing style, number of knockouts, use of a head guard, and other factors.
References
- 1.Scheid R, Preul C, Gruber O, et al. Diffuse axonal injury associated with chronic traumatic brain injury: evidence from T2*-weighted gradient-echo imaging at 3 T. AJNR Am J Neuroradiol 2003;24:1049–56 [PMC free article] [PubMed] [Google Scholar]
- 2.Unterharnscheidt F. A neurologist's reflections on boxing. V. Conclude remarks. Rev Neurol 1995;23:1027–32 [PubMed] [Google Scholar]
- 3.Tokuda T. Boxer's brain and other types of post-traumatic dementia [in Japanese]. No To Shinkei 1993;45:1109–18 [PubMed] [Google Scholar]
- 4.Blennow K, Popa C, Rasulzada A, et al. There is a strong evidence that professional boxing results in chronic brain damage. The more head punches during a boxer's career, the bigger is the risk [in Swedish]. Lakartidningen 2005;102:2468–70, 2472–75 [PubMed] [Google Scholar]
- 5.Moseley IF. The neuroimaging evidence for chronic brain damage due to boxing. Neuroradiology 2000;42:1–8 [DOI] [PubMed] [Google Scholar]
- 6.Moriarity J, Collie A, Olson D, et al. A prospective controlled study of cognitive function during an amateur boxing tournament. Neurology 2004;62:1497–502 [DOI] [PubMed] [Google Scholar]
- 7.Unterharnscheidt F. A neurologist's reflections on boxing. I: Impact mechanics in boxing and injuries other than central nervous system damage. Rev Neurol 1995;23:661–74 [PubMed] [Google Scholar]
- 8.Livingston EH, Cassidy L. Statistical power and estimation of the number of required subjects for a study based on the t-test: a surgeon's primer. J Surg Res 2005;126:149–59 [DOI] [PubMed] [Google Scholar]
- 9.Holzgraefe M, Lemme W, Funke W, et al. The significance of diagnostic imaging in acute and chronic brain damage in boxing. A prospective study in amateur boxing using magnetic resonance imaging (MRI). Int J Sports Med 1992;13:616–20 [DOI] [PubMed] [Google Scholar]
- 10.Zhang L, Heier LA, Zimmerman RD, et al. Diffusion anisotropy changes in the brains of professional boxers. AJNR Am J Neuroradiol 2006;27:2000–04 [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang L, Ravdin LD, Relkin N, et al. Increased diffusion in the brain of professional boxers: a preclinical sign of traumatic brain injury? AJNR Am J Neuroradiol 2003;24:52–57 [PMC free article] [PubMed] [Google Scholar]