Abstract
BACKGROUND AND PURPOSE: DAVFs (dural arteriovenous fistulas) represent one of the most dangerous types of intracranial AV shunts. Most of them are cured by arterial or venous embolization, but surgery/radiosurgery can be required in case of failure. Our goal was to reconsider the endovascular treatment strategy according to the new possibilities of arterial embolization using non polymerizing liquid embolic agent.
MATERIALS AND METHODS: Thirty patients were included in a prospective study during the interval between July 2003 and November 2006. Ten of these had type II, 8 had type III, and 12 had type IV fistulas. Sixteen presented with hemorrhage. Five had been treated previously with other embolic materials.
RESULTS: Complete angiographic cure was obtained in 24 cases. Of these 24 cures, 20 were achieved after a single procedure. Cures were achieved in 23 of 25 patients who had not been embolized previously and in only 1 of 5 previously embolized patients. Among these 24 patients, 23 underwent a follow-up angiography, which has confirmed the complete cure. Partial occlusion was obtained in 6 patients, 2 were cured after additional surgery, and 2 underwent radiosurgery. Onyx volume injected per procedure ranged from 0.5 to 12.2 mL (mean, 2.45 mL). Rebleeding occurred in 1 completely cured patient at day 2 due to draining vein thrombosis. One patient had cranial nerve palsy that resolved. Two ethmoidal dural arteriovenous fistulas were occluded. All 10 of the patients with sinus and then CVR drainage were cured.
CONCLUSION: Based on this experience, we believe that Onyx may be the treatment of choice for many patients with intracranial dural arteriovenous fistula (ICDAVF) with direct cortical venous reflux (CVR). The applicability of this new embolic agent indicates the need for reconsideration of the global treatment strategy for such fistulas.
Several studies have shown an association between intracranial (IC) dural arteriovenous fistula (DAVF) venous drainage patterns and clinical presentation.1,2 DAVFs draining retrogradely into cortical veins exhibit a much higher incidence of hemorrhage or venous infarction.3,4 The annual mortality rate for cortical venous reflux (CVR) may be as high as 10.4%, whereas the annual risk for hemorrhage or nonhemorrhagic neurologic deficits during follow-up are 8.1% and 6.9%, respectively, resulting in an annual event rate of 15%.4 In subjects presenting with hemorrhage, the risk of rebleeding has been evaluated at 35% in the 2 weeks after the initial hemorrhage.3 Consequently, DAVFs with CVR require treatment aimed at a complete and definitive fistula closure. In general, treatment of such fistulas primarily involves an endovascular approach, and if this fails, surgical or radiosurgical approaches are used. The present prospective study investigated the use of a new nonadhesive liquid embolic agent, Onyx (ev3, Irvine, Calif), in the treatment of DAVF with CVR.
Materials and Methods
Patients
In a prospective study of the use of Onyx in DAVF with CVR during the interval between July 2003 and November 2006, 30 patients underwent endovascular treatment. Inclusion criteria were as follows: every patient presenting with a DAVF with CVR; type IIb to V according to DAVF venous drainage classification1 and for whom the treatment was decided by a multidisciplinary neurovascular team. Exclusion criteria were as follows: DAVF with no CVR (type I and IIa), DAVF draining into a sinus with CVR (type IIb and type IIa+b) with no sinus occlusion or anfractuosities and for which the venous approach was considered the best option, cavernous sinus DAVFs, and patient age less than 18 years. Eighteen patients with a DAVF were excluded from this series: 10 patients with type I or IIa DAVF, 3 patients with a type IIa+b DAVF treated by venous approach and sinus occlusion with coils, 1 patient with type IV DAVF who rebled and died 2 hours after diagnostic angiography, and 4 patients with cavernous sinus DAVF.
There were 18 men and 12 women, ranging from 36 to 76 years of age (mean, 62.4 ± 10.4 years). Patients were questioned about medical history to identify etiologic factors such as thrombophlebitis, otitis or sinusitis, cranial trauma, neurosurgery, or phlebitis of the lower limb. Five patients had thrombophlebitis, and 3 patients reported head trauma a few years before the current presentation. Fistulas were located at the transverse sinus (15 cases), superior sagittal sinus (4 cases), tentorium (5 cases), anterior fossa (2 cases), foramen magnum (1 case), vein of Galen (1 case), sphenoparietal sinus (1 case), and falx cerebri (1 case).
According to DAVF venous drainage classification,1 6 cases were type IIb fistulas (drainage into a sinus then reflux into cortical veins only), 4 cases were type IIa+b (drainage into a sinus then reflux into cortical veins and other sinuses), 8 cases were type III (direct drainage into a cortical vein without venous ectasia), and 12 cases were type IV (drainage into a cortical vein with a venous ectasia). The clinical presentations were intracranial hemorrhages (16 cases), subarachnoid hemorrhages (2 cases), and parenchymal hematomas (14 cases). Other presentations were seizures (4 cases), tinnitus (2 cases), venous infarctions (2 cases), incidental (2 cases), intracranial hypertension (1 case), vision loss (1 case), hemianopia due to a mass effect (1 case), and headaches (1 case). Five patients had been embolized previously: 2 patients once, 2 patients twice, and 1 patient 3 times. The technique used previously was arterial embolization with particles in 2 patients, with n-butyl-2-cyanoacrylate n-BCA (histo-acryl or glubran) in 6 patients, and with coils in the feeding artery in 1 patient (in another hospital).
In terms of a high risk of rebleeding, all of the hemorrhage cases were considered emergencies and were treated in the days after the initial bleeding when possible. All of the patients underwent endovascular treatment under general anesthesia. The anticoagulation protocol was 20 IU/kg of bolus heparin at the commencement of the procedure, then continuous infusion to keep the activated clotting time (ACT) at approximately twice the normal value. In all of the cases, including hemorrhage cases, heparinization was maintained for 48 hours aiming an ACT at twice the normal value, after which low molecular weight heparin was administered at a preventive dose for 15–30 days.
Briefly, the procedure is composed of the following steps: a femoral artery 6F sheath; complete selective angiography (internal and external carotid artery and vertebral artery ipsilateral to the fistula) to precisely determine the anatomic characteristics of the shunt; a 6F guiding catheter placed into the parent artery (MPD; Cordis Neurovascular, Miami Lakes, Fla); superselective catheterization of 1 arterial feeder using a microcatheter compatible with Onyx (UltraFlow, Marathon, or Echelon, ev3) on a guidewire (Mirage or X-Pedion, ev3) or GT 12 (Terumo, Tokyo, Japan); positioning of the microcatheter as close as possible to the origin of the draining vein; flushing of the microcatheter with saline (5 mL), filling of the dead space with 0.25 mL of dimethyl-sulfoxide (DMSO), and then slow injection of 0.25 mL of Onyx (over ∼40 seconds) to wash out the DMSO; very slow injection of Onyx under subtraction fluoroscopy; and then removal of the microcatheter by rapid withdrawal. The following parameters were recorded for each procedure: the number and type of every embolized pedicle, the volume of Onyx injected, the duration of the injection, any technical complications, any clinical complications, and the immediate angiographic result.
Follow-up
A follow-up angiography was requested in every case and performed approximately 3 months after the procedure. A neurologist or neurosurgeon performed clinical follow-up during the postoperative period and at the time of the hospitalization for the 3-month follow-up angiography.
Results
Immediate Posttreatment Angiographic Results
Twenty-four of the 30 patients who underwent treatment were found to have complete closure of the shunt (ie, cure). Closures were achieved in 1 procedure for 20 patients, in 2 procedures for 3 patients, and in 3 procedures for 1 patient. Follow-up angiography in 23 of these 24 patients confirmed complete closure. In 6 patients, a partial result was obtained, with a significant reduction of flow. Of these 6 patients, 2 underwent additional surgery that resulted in cure according to follow-up angiography, and 2 patients underwent radiosurgery and will undergo follow-up angiography after 3 years. One patient is scheduled for another embolization, and 1 patient refused radiosurgery. Only 1 of the 5 previously embolized patients was completely cured by the current Onyx embolization. That patient had been embolized previously 3 times (twice with particles and once with n-BCA). In summary, embolization with Onyx resulted in a complete cure in 23 of 25 patients who were not embolized previously and in 1 of 5 patients embolized previously.
Four patients with type II DAVF (2 with type IIb and 2 type with IIa+b) initially underwent venous catheterization for coil occlusion of the sinus. However, that treatment failed, and recanalization of the thrombosed sinuses or navigation through compartments within the sinus was not possible. Thus, arterial Onyx injection was indicated. The 6 other patients with type II DAVF were treated by arterial Onyx injection without initially attempting a venous approach.
Forty-three arterial feeders were embolized, with a mean of 2.5 per patient. Embolization of only 1 feeder led to complete obliteration of the fistula in 18 of 24 cured patients. For the other 6 patients, embolization of 2 feeders was required in 4 patients, 3 feeders in 1 patient, and 4 feeders in 1 patient. Of the 18 patients where a single catheterization obtained a complete cure, the pedicle embolized was the middle meningeal artery in 15, ophthalmic artery in 2, and occipital artery in 1 patient.
The duration of the injection per pedicle ranged from 7 to 100 minutes, with a mean of 45.3 minutes (±23.2 minutes). The volume of Onyx injected ranged from 0.35 to 11 mL per pedicle (mean, 1.92 mL), from 0.5 to 12.2 mL per procedure (mean, 2.45 mL), and was a mean 2.53 mL per patient.
Angiographic Results at Follow-up
Follow-up angiography was obtained 3 months after the last treatment (embolization or surgery) in 25 patients showing a complete cure in all of them (in 23 patients after embolization alone and in 2 patients after associated surgery). One patient with partial result is scheduled for another embolization. One patient with partial result refused an associated treatment by radiosurgery, rebled 24 months later, and eventually died. One patient with complete occlusion after embolization was not controlled because of old age and poor clinical status. The 2 patients who underwent radiosurgery will be followed by angiography 3 years later.
Technical Problems
One microcatheter was stretched and broken during retrieval without any clinical complications. No other catheter was glued.
Clinical Complications
Two patients showed clinical complications after treatment. One patient originally presented with a 6-month history of headaches and a hemianopia due to a type IV DAVF of the tentorium with a 25-mm venous ectasia compressing the optic radiations. Three Onyx injections were administered to the middle meningeal artery branches. Reflux of Onyx until the foramen spinosum was accepted during the last injection due to the inability to reach the vein origin. The patient woke up with third and fourth cranial nerve palsies with proptosis and ophthalmoplegia and fifth cranial nerve territory pain. Three months later, the proptosis and facial pain had completely resolved, whereas a slight ophthalmoplegia due to third nerve palsy persisted. The patient refused any additional treatment involving radiosurgery. He presented 24 months later with a large hematoma and eventually died.
The other complication arose in a patient who originally presented with a left cerebellar hematoma (Hunt and Hess grade I) due to a type IV DAVF of the tentorium with a 20-mm venous ectasia. Onyx embolization resulted in a complete cure. Three days after treatment, the patient developed an acute static and dynamic cerebellar syndrome. CT scans showed an extensive thrombosis of the draining vein and venous ectasia, as well as rebleeding with a cerebellar hematoma. Six months later, the patient had recovered, albeit with a slight persistent ataxia, which did not affect independence.
Discussion
DAVF with CVR carries a high risk of intracranial hemorrhage or ischemic venous infarction due to arterialization of the draining veins. Optimal treatment involves complete shunt occlusion as soon as possible. One approach is to use surgery,5–8 and Hoh et al6 described a technique of clipping the draining vein together with extensive cauterization of the surrounding dura. Surgical techniques must be adapted to the type of venous drainage.5,8 In cases of sinus drainage, then CVR (type II), surgical excision of the fistulous sinus segment, or direct surgical sinus packing may represent a definitive treatment option if the sinus is nonfunctional. In cases with a direct CVR (types III, IV, or V), surgical interruption of the draining veins is indicated.7,8 Radiosurgery is inefficient for DAVF, and the time for closure carries a risk of bleeding or rebleeding.9–11 Nevertheless, radiosurgery remains indicated where embolization has failed and surgery appears to carry a high risk.
Before the use of surgical or radiosurgical treatments, the present consensus is to first attempt to treat such fistulas by using an endovascular approach. In cases of sinus drainage, CVR (type II), a transvenous approach with coil occlusion of the affected sinus, is the best option.12,13 However, retrograde venous catheterization of the fistulous sinus may be difficult or even impossible. The affected sinus may be stenosed, compartmentalized, or even occluded downstream and/or upstream of the fistula. Recanalization of an occluded sinus is sometimes possible.14–17 In some rare instances, a direct surgical puncture or approach may give access to the sinus and allow coil deposition.18,19 Arterial embolization is usually not considered for this type of fistula due to the multiplicity of arterials feeders, and much better results are obtained by using sinus occlusion. For direct CVR (types III, IV, and V), the optimal technique is arterial embolization with an injection of diluted n-BCA after arterial feeder distal catheterization in a wedge position.20 The goal of embolization is to glue the origin of the draining vein. However, n-BCA injection can be hazardous, and the use of glue generally requires a highly experienced operator with the ability to determine the appropriate glue dilution (depending on the catheter tip positioning and evaluation of the flow). An injection that is too proximal and does not occlude the vein can result in arterial recruitment and a persistent fistula, whereas an injection too distal may lead to migration within the draining veins resulting in an increased risk of infarction or hemorrhage. There have been rare reports of retrograde catheterization of the cortical vein draining the DAVF and coil deposition at the level of the origin of the vein.21 However, such catheterization can be high risk, and it may be difficult to ensure that the coils are introduced precisely at the level of the shunt and not a few millimeters too distal, which can increase the risk of hemorrhage.
The Onyx Liquid Embolic System (ev3) is a new nonadhesive agent containing a mixture of ethylene-vinyl alcohol copolymer and DMSO. The advantages of a nonadhesive liquid are a decreased risk of gluing the catheter and the ability to inject a larger volume of agent per administration. Onyx is now used as an alternative to cyanoacrylates in many brain arteriovenous malformations (AVMs).22,23 There have been a few recent reports describing the use of Onyx for DAVFs.24–26 Our 3 years of experience using Onyx has resulted in a new strategy for treating DAVF with CVR.
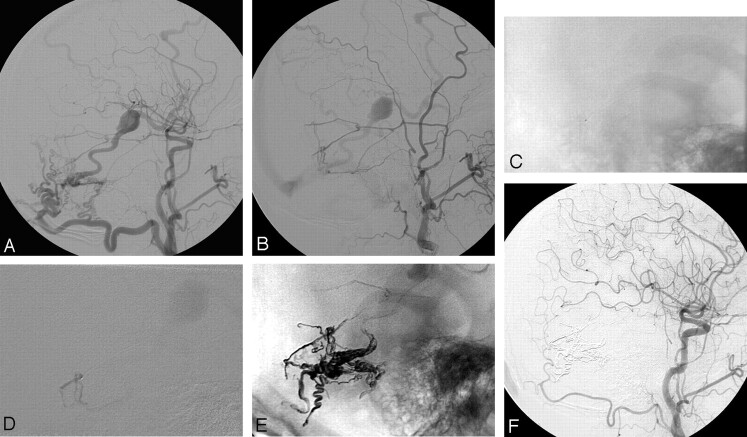
The present study involved 30 patients who underwent endovascular treatment for DAVF with CVR. Sixteen patients had an intracranial hemorrhage. Ten cases involved sinus drainage and then CVR (type II), and 20 cases were direct CVR (types III and IV). Onyx embolization resulted in complete shunt closure in 24 cases. Complete cure was achieved in 23 of 25 patients who were not embolized previously and in only 1 of 5 patients who were embolized previously with n-BCA or coils. These findings indicate that Onyx should be used as the primary treatment and that the rate of success is far lower after a previously failed embolization that has closed the main feeders. The main advantage of Onyx is the ability to administer a large volume via a long-duration injection through 1 pedicle. This results in progressive filling of the arteriovenous network and veins with arterio-arterial retrograde migration of the agent, which avoids the need for multiple catheterizations and embolizations (Fig 1). In 18 cases, complete obliteration of the fistula was achieved after embolization of only 1 feeder in only 1 administration. In 15 of those 18 cases, embolization was performed through the middle meningeal artery. Indeed, we found that it was far more efficient to gain access through the middle meningeal artery, even when the diameter was very small, than through other more dilated feeders (eg, occipital and posterior auricular arteries) due to the superior flow control and Onyx progression (Fig 1). The mean Onyx injection duration achieved was 45 minutes, which compares very favorably to cyanoacrylate administration, which can generally only last a few minutes.
Fig 1.
A 67-year-old man with a left temporal hematoma. A, Type IV DAVF of the transverse sinus draining directly into the vein of Labbe. B, Middle meningeal artery (MMA) was small compared with the occipital artery. C and D, MMA distal catheterization was easily performed. E, Onyx injection allowed arterio-arterial filling of other arterial feeders and occlusion of the draining vein. F, Postoperative 3-month assessment shows complete fistula cure.
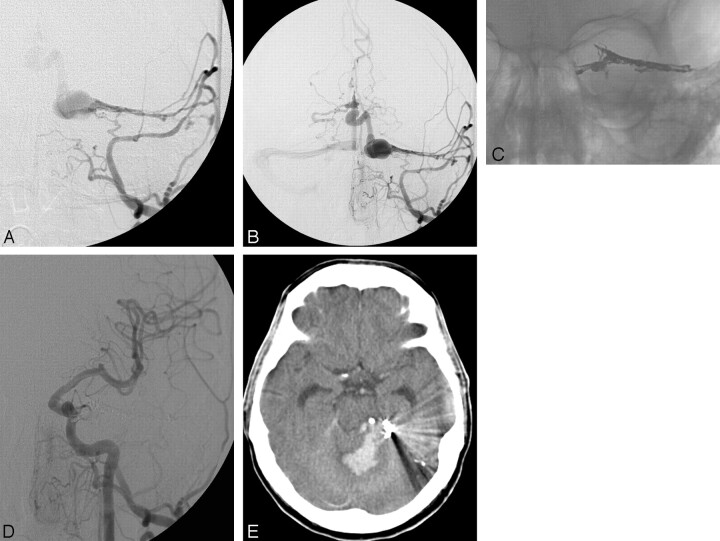
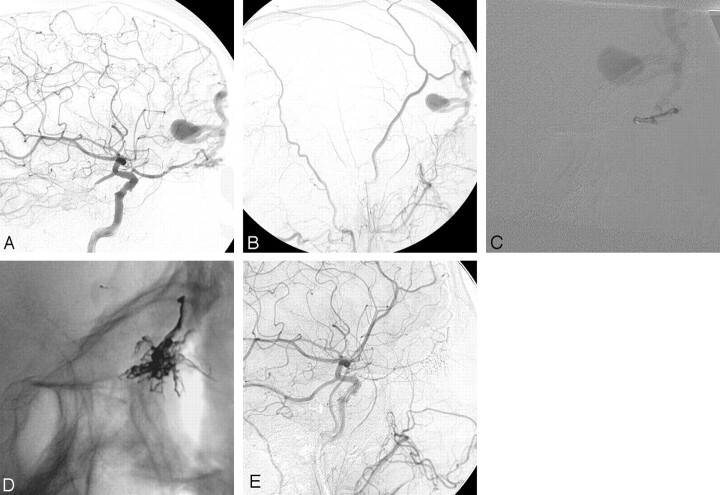
Although there are some potential disadvantages for Onyx use in brain AVMs, these are not relevant for treating DAVFs. Navigation with a guidewire does not carry any risk in meningeal arteries, nor does catheter retrieval. Injection of large volumes (≤11 mL) is less risky than for brain AVM in terms of postembolization hemorrhage. Venous Onyx migration can be controlled by temporarily halting the administration (Figs 2 and 3). There is less risk of inadvertent uncontrolled venous migration with Onyx than with cyanoacrylates that can fly into the draining vein. Indeed, a few minutes after administration, the initially liquid Onyx becomes pasty, and the Onyx column can be pushed progressively from the catheter tip to the vein and from the vein backwards to the distal aspect of other feeders (Fig 3).
Fig 2.
A 62-year-old woman with 1 episode of seizures. A–C, Type IV DAVF of the vein of Galen draining into multiple dilated veins to the superior sagittal sinus. The straight sinus was occluded. D and E, Distal catheterization of the right MMA allowed injection of 11 mL of Onyx in 48 minutes, with retrograde occlusion of other feeders, occlusion of the venous pouch, and no migration into cortical veins. F and G, Postoperative 3-month assessment shows complete fistula cure.
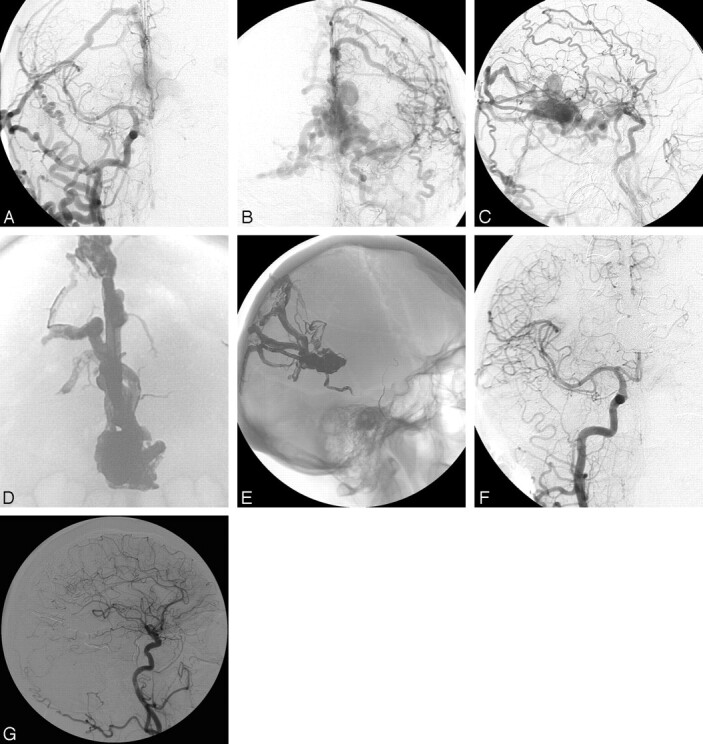
Fig 3.
A 68-year-old man with a left cerebellar hematoma. A and B, Type IV DAVF of the tentorium draining into the lateromesencephalic vein, then through a large venous ectasia into the central vein, then to the basal vein and straight sinus. C and D, Injection of Onyx resulted in occlusion of the origin of the draining vein. E, Extensive thrombosis of the draining vein and ectasia due to shunt occlusion with cerebellar rebleeding.
One of the present cases involved a dangerous type IV DAVF. In our desire to achieve a cure, we administered Onyx for too long; this created reflux to the level of the foramen spinosum, which resulted in cranial nerve palsy. Onyx reflux must be carefully controlled, and administration should be halted to avoid it reaching the base of the skull due to the risk of cranial nerve injury and inadvertent embolization through anastomoses into cerebral arteries. Regardless of the agent used, it is important to consider that a complete fistula cure may produce devastating complications due to extensive thrombosis of the draining veins initially arterialized and a risk of venous infarction or hemorrhage. For this reason, all of the patients were treated with intravenous heparin aimed at achieving an ACT twice the normal value for 48 hours postoperatively and then low molecular weight heparin at a preventive dose for 15–30 days postoperatively. Despite these conditions, 2 days after the procedure, 1 patient presented with parenchymal bleeding in contact with a huge venous ectasia, which rapidly thrombosed after closure of the shunt (Fig 3).
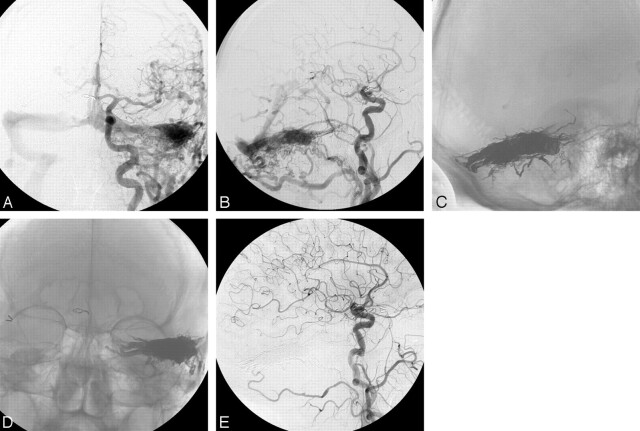
Although DAVFs at the anterior skull base have previously been surgically treated,27 the efficacy of Onyx embolization allowed us to treat 2 such cases in the present study. Catheterization through the ophthalmic artery allowed venous injection of Onyx without any technical or clinical complications and, hence, avoided surgery (Fig 4). One patient with preoperative vision loss showed complete vision recovery very rapidly postoperatively. Nevertheless, Onyx injection through the ophthalmic artery carries the risk of reflux and occlusion of the central retinal artery with consequent vision loss. Surgery should remain a consideration in such cases, because it is relatively simple.
Fig 4.
A 68-year-old man with right vision loss. A, Type IV DAVF fed by the distal ophthalmic artery. B, External carotid feeders. C, Distal ophthalmic artery catheterization. D, Injection of 0.8 mL of Onyx over 43 minutes resulted in occlusion of the draining vein origin. E, Postoperative 3-month assessment shows complete fistula cure.
Although arterial embolization with Onyx for direct CVR DAVFs (types III and IV) appears appropriate, treatment of DAVFs with sinus drainage and then CVR (type II) is more controversial. Treatment of such sinus fistulas is usually performed via a venous approach and occlusion with coils. However, in some cases it may be difficult or impossible to access the fistulous sinus, and, thus, surgical puncture of the sinus and coiling or direct surgical treatment may be required. In such cases, arterial Onyx embolization may be an efficient and safe alternative. The present series involved 10 such cases. In 4 such patients with type II DAVF, the initial venous catheterization for coil occlusion of the sinus failed. In those patients, arterial Onyx injection was then chosen, because recanalization of the thrombosed sinuses was not possible. The risk in these sinus-type DAVFs was migration of Onyx from the sinus to the arterialized draining veins, which may cause distal venous occlusion and consequent venous infarction or hemorrhage. In the present cases, Onyx was slowly pushed into the sinus with very efficient progression control. There was no entry into the veins (Fig 5), and complete filling of the sinus was eventually obtained. Due to the ease of sinus filling from the arterial approach in those 4 patients, the other 6 patients with type II DAVF were primarily treated with Onyx arterial embolization without a previous attempt at venous catheterization.
Fig 5.
A 67-year-old woman with seizures. A and B, Type IIa+b DAVF of the left transverse sinus draining into cortical veins and in the straight sinus. C and D, Injection of 9.3 mL of Onyx over 90 minutes through the middle meningeal artery. E, Postoperative 7-month assessment shows complete fistula cure.
Conclusions
The present study examined the use of Onyx for endovascular treatment of ICDAVF with CVR. The study found that Onyx injections were easier to control than n-BCA injections, a much larger volume could be injected over a longer time period, injection in a single feeder allowed obtaining arterio-arterial reflux and avoided embolization of other feeders, and access through the meningeal artery was more efficient even if the size was very small.
It appears that Onyx can be used as a primary treatment option for most cases of ICDAVF with direct CVR. This new agent provides an alternative to surgery for treatment of anterior skull base fistulas. In cases of a DAVF draining into a sinus with secondary CVR, Onyx arterial embolization may be performed as an alternative to retrograde venous catheterization. In conclusion, the technological options provided by this new embolic agent encourage a reconsideration of the global treatment strategy for DAVF with CVR.
References
- 1.Cognard C, Gobin YP, Pierot L, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology 1995;194:671–80 [DOI] [PubMed] [Google Scholar]
- 2.Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg 1995;82:166–79 [DOI] [PubMed] [Google Scholar]
- 3.Duffau H, Lopes M, Janosevic V, et al. Early rebleeding from intracranial dural arteriovenous fistulas: report of 20 cases and review of the literature. J Neurosurg 1999;90:78–84 [DOI] [PubMed] [Google Scholar]
- 4.van Dijk JM, terBrugge KG, Willinsky RA, et al. Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke 2002;33:1233–36 [DOI] [PubMed] [Google Scholar]
- 5.Collice M, D’Aliberti G, Arena O, et al. Surgical treatment of intracranial dural arteriovenous fistulae: role of venous drainage. Neurosurgery 2000;47:56–66 [DOI] [PubMed] [Google Scholar]
- 6.Hoh BL, Choudhri TF, Connolly ES Jr, et al. Surgical management of high-grade intracranial dural arteriovenous fistulas: leptomeningeal venous disruption without nidus excision. Neurosurgery 1998;42:796–804 [DOI] [PubMed] [Google Scholar]
- 7.Perrini P, Di Lorenzo N. Surgical occlusion of the leptomeningeal drainage is a safe and effective treatment for intracranial dural arteriovenous fistulas without dural sinus drainage. Acta Neurochir (Wien) 2004;146:1279–80 [DOI] [PubMed] [Google Scholar]
- 8.Ushikoshi S, Houkin K, Kuroda S, et al. Surgical treatment of intracranial dural arteriovenous fistulas. Surg Neurol 2002;57:253–61 [DOI] [PubMed] [Google Scholar]
- 9.Friedman JA, Pollock BE, Nichols DA, et al. Results of combined stereotactic radiosurgery and transarterial embolization for dural arteriovenous fistulas of the transverse and sigmoid sinuses. J Neurosurg 2001;94:886–91 [DOI] [PubMed] [Google Scholar]
- 10.Koebbe CJ, Singhal D, Sheehan J, et al. Radiosurgery for dural arteriovenous fistulas. Surg Neurol 2005;64:392–99 [DOI] [PubMed] [Google Scholar]
- 11.Soderman M, Edner G, Ericson K, et al. Gamma knife surgery for dural arteriovenous shunts: 25 years of experience. J Neurosurg 2006;104:867–75 [DOI] [PubMed] [Google Scholar]
- 12.Dawson RC 3rd, Joseph GJ, Owens DS, et al. Transvenous embolization as the primary therapy for arteriovenous fistulas of the lateral and sigmoid sinuses. AJNR Am J Neuroradiol 1998;19:571–76 [PMC free article] [PubMed] [Google Scholar]
- 13.Roy D, Raymond J. The role of transvenous embolization in the treatment of intracranial dural arteriovenous fistulas. Neurosurgery 1997;40:1133–41 [DOI] [PubMed] [Google Scholar]
- 14.Benndorf G, Bender A, Lehmann R, et al. Transvenous occlusion of dural cavernous sinus fistulas through the thrombosed inferior petrosal sinus: report of four cases and review of the literature. Surg Neurol 2000;54:42–54 [DOI] [PubMed] [Google Scholar]
- 15.Biondi A, Milea D, Cognard C, et al. Cavernous sinus dural fistulas treated by transvenous approach through the facial vein: report of seven cases and review of the literature. AJNR Am J Neuroradiol 2003;24:1240–46 [PMC free article] [PubMed] [Google Scholar]
- 16.Gobin YP, Houdart E, Rogopoulos A, et al. Percutaneous transvenous embolization through the thrombosed sinus in transverse sinus dural fistula. AJNR Am J Neuroradiol 1993;14:1102–05 [PMC free article] [PubMed] [Google Scholar]
- 17.Murphy KJ, Gailloud P, Venbrux A, et al. Endovascular treatment of a grade IV transverse sinus dural arteriovenous fistula by sinus recanalization, angioplasty, and stent placement: technical case report. Neurosurgery 2000;46:497–501 [DOI] [PubMed] [Google Scholar]
- 18.Houdart E, Saint-Maurice JP, Chapot R, et al. Transcranial approach for venous embolization of dural arteriovenous fistulas. J Neurosurg 2002;97:280–86 [DOI] [PubMed] [Google Scholar]
- 19.Pierot L, Visot A, Boulin A, et al. Combined neurosurgical and neuroradiological treatment of a complex superior sagittal sinus dural fistula: technical note. Neurosurgery 1998;42:194–97 [DOI] [PubMed] [Google Scholar]
- 20.Nelson PK, Russell SM, Woo HH, et al. Use of a wedged microcatheter for curative transarterial embolization of complex intracranial dural arteriovenous fistulas: indications, endovascular technique, and outcome in 21 patients. J Neurosurg 2003;98:498–506 [DOI] [PubMed] [Google Scholar]
- 21.Defreyne L, Vanlangenhove P, Vandekerckhove T, et al. Transvenous embolization of a dural arteriovenous fistula of the anterior cranial fossa: preliminary results. AJNR Am J Neuroradiol 2000;21:761–65 [PMC free article] [PubMed] [Google Scholar]
- 22.Jahan R, Murayama Y, Gobin YP, et al. Embolization of arteriovenous malformations with Onyx: clinicopathological experience in 23 patients. Neurosurgery 2001;48:984–95 [DOI] [PubMed] [Google Scholar]
- 23.Pierot L. Endovascular treatment of brain arteriovenous malformations using Onyx: preliminary results of a prospective, multicenter study. Intervent Neuroradiol 2005;11:159–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arat A, Inci S. Treatment of a superior sagittal sinus dural arteriovenous fistula with Onyx: technical case report. Neurosurgery 2006;59:ONSE169–70 [DOI] [PubMed] [Google Scholar]
- 25.Rezende MT, Piotin M, Mounayer C, et al. Dural arteriovenous fistula of the lesser sphenoid wing region treated with Onyx: technical note. Neuroradiology 2006;48:130–34 [DOI] [PubMed] [Google Scholar]
- 26.Toulgoat F, Mounayer C, Tulio Salles Rezende M, et al. Transarterial embolisation of intracranial dural arteriovenous malformations with ethylene vinyl alcohol copolymer (Onyx18). J Neuroradiol 2006;33:105–14 [DOI] [PubMed] [Google Scholar]
- 27.Abrahams JM, Bagley LJ, Flamm ES, et al. Alternative management considerations for ethmoidal dural arteriovenous fistulas. Surg Neurol 2002;58:410–16 [DOI] [PubMed] [Google Scholar]