Abstract
BACKGROUND AND PURPOSE: There are a few reports regarding the treatment of traumatic vertebral arteriovenous fistulas and pseudoaneurysms. Our aim was to describe the clinical and angiographic results of endovascular therapy for traumatic injuries of the vertebral artery.
MATERIALS AND METHODS: The clinical and angiographic features of 18 traumatic injuries of the vertebral artery during an 8-year period were reviewed. There were 14 male (78%) and 4 female patients (22%). The average age was 28 years (range, 11–49 years). Of the 18 lesions of the vertebral artery, 17 (95%) were the result of penetrating trauma (gunshot or stab wound injury) and 1 (5%) was iatrogenic (jugular vein catheter). In 16 (89%) instances, the injury resulted in an arteriovenous fistula, and in the other 2 (11%), in a pseudoaneurysm. All patients were treated with an endovascular approach by using different techniques (balloon occlusion, coil embolization, and/or stent deployment).
RESULTS: Endovascular therapy resulted in immediate lesion total occlusion in 16 (89%) patients. Delayed total occlusion was demonstrated angiographically during follow-up in the 2 remaining patients. Clinical improvement was documented in all patients, and there were no clinically symptomatic complications.
CONCLUSION: In this small series, endovascular techniques were a safe and effective method of treatment and were not associated with significant morbidity or mortality.
Vertebral artery traumatic lesions can be classified either as dissecting, thrombotic, pseudoaneurysm, or arteriovenous fistula (AVF). AVFs compromising the vertebral artery are rare lesions, defined by the presence of an abnormal shunt between the extracranial vertebral artery or 1 of its muscular or radicular branches and an adjacent vein.1-3 These lesions can be of traumatic or spontaneous origin.1-6 Traumatic fistulas are frequently associated with penetrating neck injuries.7-8 Less frequent causes include puncture of the vertebral artery after gaining jugular vein access for central line placement, neck surgery, dislocations, and fractures of the cervical spine.9-11
Approximately 30% of AVFs can be asymptomatic,12 discovered incidentally after auscultation of a neck bruit. However, these lesions can have ischemic symptoms of vertigo, diplopia, and cephalgia secondary to arterial steal. The presence of myelopathy or cervical neuralgia is rare but can result after arterial blood reflux into spinal pial veins or after root compression by engorged epidural veins.2
Closure of the AVF or pseudoaneurysm with preservation of the parent artery is the main goal of treatment, rarely achieved with surgery but frequently attained with an endovascular approach.12 In this article, our purpose was to review our experience in the management of traumatic injuries of the vertebral artery, to evaluate the morphologic characteristics of this uncommon condition, and to determine the benefits of endovascular treatment on the basis of clinical and angiographic results.
Materials and Methods
The clinical records and imaging studies of patients treated for traumatic vertebral artery injuries between 1997 and 2005 were retrospectively analyzed, and endovascular treatment was performed in 18 patients (Table 1). This series represents all of the patients seen during the interval of our study, because all of the vertebral artery lesions were treated with endovascular techniques. There were 14 male (77.8%) and 4 female patients (22.2%). The average age was 28 years (range, 11–49 years). Pre- and postoperative angiographic images were available for review in all patients. The clinical information was introduced into a data base, including variables referring to topography and morphology of vertebral artery lesions previously established elsewhere.3,12 Information about clinical presentation, endovascular techniques used, and angiographic and clinical outcomes of treatment was registered.
Table 1:
Angiographic and clinical results after endovascular treatment of traumatic lesions of the vertebral artery
| Patient No. | Sex/Age (yr) | Clinical Presentation | Cause | Topography | Treatment | Occlusion Grade | Clinical Outcome |
|---|---|---|---|---|---|---|---|
| 1 | M/18 | Neck bruit | Gunshot | Above C2, left | Coiling | Total | Asymptomatic |
| 2 | M/28 | Neck bruit | Gunshot | C5-C2, left | Balloon occlusion (trapping technique) | Total | Asymptomatic |
| 3 | M/18 | Neck bruit, cephalgia | Gunshot | Below C5, left | Balloon occlusion (parent artery sacrifice) | Total | Asymptomatic |
| 4 | M/26 | Spinal cord symptoms | Stab wound | Below C5, right | Stent, coils, n-butyl cyanoacrylate | Partial* | Asymptomatic |
| 5 | M/35 | Neck bruit | Gunshot | Below C5, left | Balloon occlusion (trapping technique) | Total | Asymptomatic |
| 6 | M/27 | Neck bruit | Gunshot | C5-C2, right | Balloon occlusion (trapping technique) | Total | Asymptomatic |
| 7 | M/35 | Neck bruit, cephalgia | Gunshot | Above C2, left | Ballon occlusion and coiling of the AVF | Partial* | Asymptomatic |
| 8 | M/42 | Neck bruit | Gunshot | Above C2, left | Coiling | Total | Asymptomatic |
| 9 | M/26 | Brain infarcts | Stab wound | Below C5, right | Balloon occlusion (parent artery sacrifice) | Total | Partial improvement |
| 10 | M/36 | Neck bruit | Stab wound | C5-C2, left | Balloon occlusion (parent artery sacrifice) | Total | Asymptomatic |
| 11 | F/11 | Radiculopathy | Jugular catheter | C5-C2, right | Balloon occlusion (trapping technique) | Total | Asymptomatic |
| 12 | M/19 | Neck bruit | Gunshot | Below C5, right | Balloon occlusion (trapping technique) | Total | Asymptomatic |
| 13 | F/21 | Neck bruit | Gunshot | Above C2, right | Balloon occlusion (trapping technique) | Total | Asymptomatic |
| 14 | M/25 | Neck bruit | Stab wound | C5-C2, right | Spontaneous occlusion | Total | Asymptomatic |
| 15 | M/23 | Tinnitus | Gunshot | Above C2, left | Balloon occlusion (trapping technique) | Total | Asymptomatic |
| 16 | F/43 | Neck bruit | Stab wound | C5-C2, right | Balloon occlusion (parent artery sacrifice) | Total | Asymptomatic |
| 17 | F/49 | Bruit, arm weakness, SAH | Detonation | C5-C2, left | Balloon occlusion (trapping technique) | Total | Asymptomatic |
| 18 | M/27 | Neck bruit | Gunshot | Above C2, left | Balloon occlusion of the AVF | Total | Asymptomatic |
Note:—SAH indicates subarachnoid hemorrhage; AVF, arteriovenous fistula.
Initially partial angiographic occlusion, total occlusion during follow-up.
All procedures were performed with the patient under moderate conscious sedation with neuroleptanalgesia, allowing regular clinical and neurologic evaluation, except for an 11-year-old patient who required general anesthesia. All patients received 70 U/Kg of heparin after proximal positioning of a 6 or 7F catheter in the compromised vertebral artery. According to the particular requirements of each patient, diverse materials and techniques were used, including parent artery occlusion or fistula trapping with detachable balloons, stent delivery, and embolization with coils or liquid agents like n-butyl cyanoacrylate. When sacrifice of the vertebral artery was unavoidable, a balloon occlusion test was performed for 20 minutes while evaluating for possible neurologic deficits secondary to posterior circulation ischemia. During balloon occlusion, the collateral circulation was evaluated by injecting the contralateral vertebral artery and both carotid arteries. The balloon was detached if there were no neurologic deficits and the collateral circulation was judged adequate. In all patients, comparative pre- and postembolization images were obtained. After the procedure, the patients were taken to the intensive care unit for neurologic and vital sign monitoring during 24 hours.
Results
The causes of the injuries were the following: gunshot wounds in 11 patients (61.1%), stab wounds in 5 patients (27.7%), detonation with explosive-propelled fragments penetrating the neck in 1 patient (5.5%), and an iatrogenic lesion in 1 patient secondary to the puncture of the internal jugular vein during placement of a central line (5.5%).
Patients were most commonly asymptomatic (n = 11; 61.1%) and had their lesion discovered after auscultation of a neck bruit. The rest of the patients had diverse symptoms, including cephalgia, cervical radiculopathy, subarachnoid hemorrhage and stiff neck, tinnitus, spinal cord symptoms, and vascular dementia syndrome (Table 1).
Sixteen patients (88.8%) had vertebral AVFs, of whom 7 (43.7%) had an associated pseudoaneurysm. Two (11.1%) patients had pseudoaneurysms without arteriovenous shunt. These lesions were found on the following portions of the vertebral artery: below C5 in 5 (27.7%), between C5 and C2 in 7 (38.8%), and above C2 in 6 (33.3%). Detailed information about lesion morphology including arterial feeders, presence of pseudoaneurysm, and venous drainage is given in Table 2.
Table 2:
Angiographic features of traumatic lesions of the vertebral artery
| Patient No. | Type | Arterial feeders | Venous Drainage |
|---|---|---|---|
| 1 | AVF + pseudoaneurysm | Left vertebral, ECA | Vertebral vein, IJV; Asc, Desc |
| 2 | AVF | Left vertebral | Epidural plexus; Asc, Desc |
| 3 | AVF | Left vertebral | Vertebral vein; Desc |
| 4 | AVF + pseudoaneurysm | Right vertebral | Perimedullary plexus; Asc, Desc |
| 5 | AVF + pseudoaneurysm | Left vertebral | IJV; Asc, Desc |
| 6 | AVF | Right vertebral | Vertebral vein, IJV; Desc |
| 7 | AVF + pseudoaneurysm | Left vertebral, ECA | IJV; Asc |
| 8 | AVF + pseudoaneurysm | Left vertebral | Vertebral vein, IJV; Asc, Desc |
| 9 | Pseudoaneurysm | Right vertebral | None |
| 10 | AVF + pseudoaneurysm | Left vertebral, muscular branch | Vertebral vein; Asc |
| 11 | Pseudoaneurysm | Right vertebral | None |
| 12 | AVF | Right vertebral | Vertebral vein, IJV, epidural plexus; Desc |
| 13 | AVF | Right vertebral | IJV, perimedullary plexus; Asc, Desc |
| 14 | AVF | Right vertebral | Vertebral vein; Desc |
| 15 | AVF | Left vertebral | Vertebral vein; Asc, Desc |
| 16 | AVF | Right vertebral, thyrocervical trunk | Perimedullary plexus; Asc, Desc |
| 17 | AVF | Left vertebral | IJV, epidural plexus; Desc |
| 18 | AVF + pseudoaneurysm | Left vertebral | Perimedullary plexus, dural sinus; Asc |
Note:—ECA indicates external carotid artery; IJV, internal jugular vein; Asc, ascending; Desc, Descending; AVF, arteriovenous fistula.
Endovascular treatment was performed by using balloon occlusion of the parent vessel and AVF in 12 patients (66.6%), coil embolization in 2 patients (11.1%), detachable balloon and coil embolization of the AVF in 1 patient (5.5%), balloon occlusion of the AVF in 1 patient (5.5%), stent delivery, and coil and n-butyl cyanoacrylate embolization of the AVF in 1 patient (5.5%) (Table 1). One patient with an AVF diagnosed by CT angiography experienced occlusion of the shunt by spontaneous dissection of the vertebral artery demonstrated during conventional angiography.
Immediate angiographic occlusion after endovascular treatment was documented in 16 patients (88.9%), and partial occlusion, in 2 patients (11.1%). In the 2 patients with only partial endovascular occlusion, complete closure of the fistula was demonstrated at 24-month follow-up. In 17 of the 18 study patients (94.5%), the objective and subjective findings disappeared. Only 1 patient (5.5%) had partial clinical improvement (this individual presented with dementia secondary to emboli from a pseudoaneurysm of the vertebral artery producing cerebellar, occipital, and bithalamic infarcts). There were no clinically symptomatic complications in any of the patients treated.
Discussion
Vertebral arteriovenous fistulas are an uncommon pathology, either spontaneous or traumatic in origin. Our series differs from that of Beaujeux et al12 because most of the arteriovenous fistulas in their patients were spontaneous (59%), whereas all of our patients had traumatic lesions. This difference may be due to the fact that our institution is a regional referral center for trauma patients.
In our series, we also found differences in the location of the lesions compared with other studies.4-7,12 Although the literature reports a preponderance of involvement of the vertebral artery below C5, we found a greater frequency of lesions between C2 and C5 (38.8%). This finding reflects the fact that traumatic lesions tend to occur in zone II of the neck (zone II lies between the cricoid and the angle of the mandible), in concordance with results reported in a study with similar demographic characteristics compared with our patient population.13
Clinical symptoms produced by arteriovenous vertebral fistulas are related to the flow velocity in the shunt, venous drainage pattern, and lesion chronicity. These factors can affect neighboring structures by means of steal phenomenon or venous hypertension.7 Most of our patients were asymptomatic at diagnosis, probably because they presented during the acute phase of the fistula when a neck bruit was found at physical examination in the emergency department. Ischemic injury resulting in dementia syndrome can result after clot embolization from a pseudoaneurysm, as described in 1 of our patients. Symptomatic thromboembolism was seen in only 1 patient in our series, despite the high incidence of pseudoaneurysm (43.7%), probably because of a protecting effect of the shunt into the venous side of the fistula.
CT angiography has a preponderant role in the evaluation of vascular neck trauma.13 However, we think that conventional angiography remains the study of choice for treatment planning because it evaluates collateral circulation and detects venous hypertension. It is also helpful to differentiate between a small hole in the vessel wall or complete transection. It is very important that the examination include catheterization of the external carotid artery and the thyrocervical trunk,4 because 2 of our patients had additional shunt surgery from those vessels.
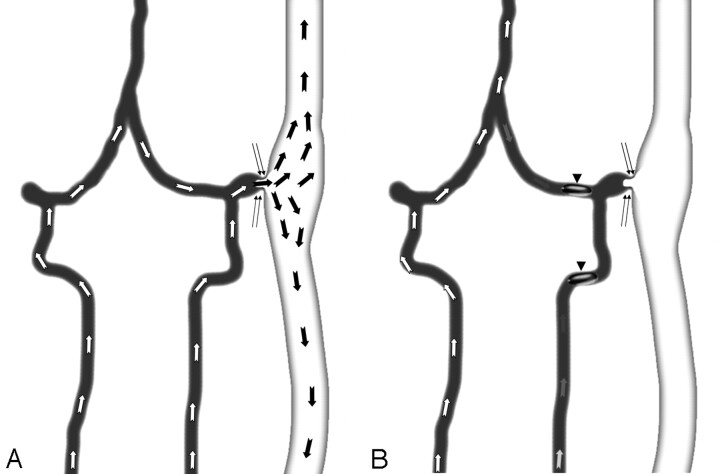
Because in most penetrating injuries of the vertebral artery, there is extensive damage of the vessel wall, possibly with transection, a reconstructive endovascular approach is not possible and vascular sacrifice may be necessary. This technique of treatment is safe whenever the contralateral vessel is adequate to supply both intracranial vertebral circulations. Parent artery occlusion can be performed if posterior inferior cerebellar artery patency is demonstrated and the balloon occlusion test is negative for vertebrobasilar ischemic symptoms. This is supported in our series with the occlusion of the vertebral artery in 13 patients, without any immediate or delayed ischemic complications. Because the possibility of steal phenomena from the contralateral vertebral artery exists, it is important to perform a trapping technique (Figs 1,2), occluding both the proximal and distal aspects of the fistula by using detachable balloons or coils.14
Fig 1.
Schematic representation of a vertebral arteriovenous fistula with steal phenomenon. Arrows represent blood-flow direction. A, Blood flow from both vertebral arteries is directed to the fistula site (double thin arrows). B, Trapping technique with positioning of detachable balloons (arrowheads) proximal and distal to the arteriovenous communication re-establishes normal flow through the basilar artery.
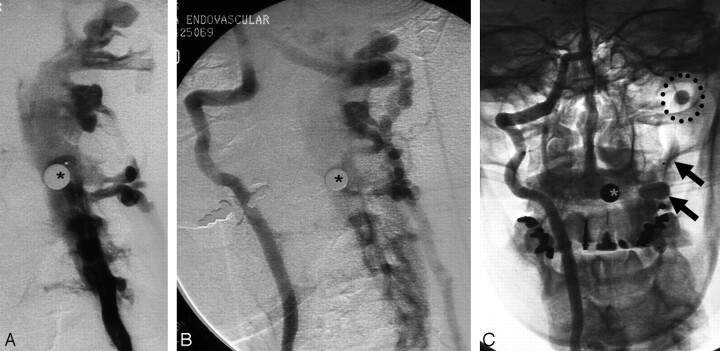
Fig 2.
Traumatic arteriovenous fistula caused by detonation with propelled metal fragments (asterisks) penetrating the neck. A, Left vertebral arteriovenous fistula is identified with both ascending and descending venous drainage. B, There is steal phenomenon represented by filling of the fistula through the right vertebral artery. C, Fistula trapping has been performed with proximal (arrows) and distal (circle) balloon detachment. Note occlusion of the fistula with re-establishment of normal flow in the right vertebral artery.
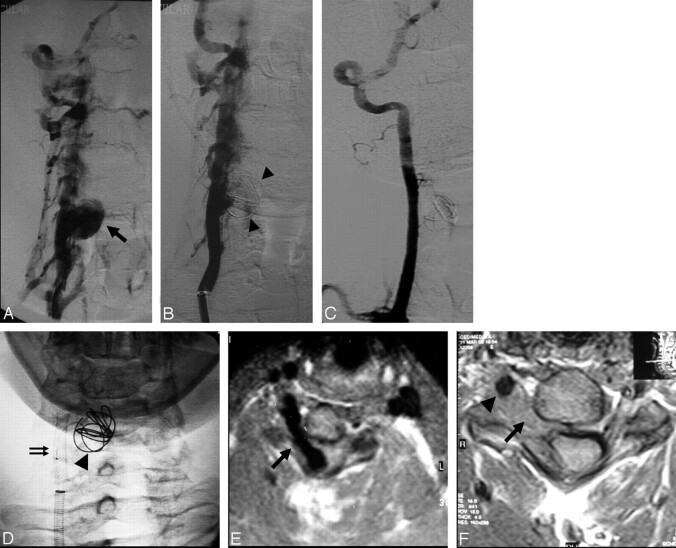
Whenever the dominant vertebral artery was injured, a reconstructive endovascular approach by using a stent and coils was accomplished (Fig 3). However, there are other possible sources of collateral supply in addition to the contralateral vertebral artery, including the posterior communicating arteries or anastomosis between the external carotid and the vertebral artery that could be identified during a balloon test occlusion, allowing parent vessel sacrifice.
Fig 3.
Right vertebral arteriovenous fistula after a stab wound injury of the neck. A, Prominent ascending and descending venous drainage with the presence of pseudoaneurysm (arrow) is noted. B, Uncovered stent deployment with coiling (arrowheads) was performed. There is partial occlusion of the pseudoaneurysm and reduction in venous drainage in the immediate postreatment angiographic images. C, Angiographic control image 18 months after treatment shows normal flow through the right vertebral artery without evidence of fistula or pseudoaneurysm. D, Reconstructive endovascular approach by using a stent (double arrows) and coils (arrowhead) was accomplished. E, Transverse T1-weighted MR image demonstrates the right vertebral AVF compressing the cervical spinal cord (arrow). F, MR control image 18 months after treatment shows AVF thrombosis (arrow) and patency of the right vertebral artery (arrowhead).
Initial total occlusion of the vertebral artery lesions was achieved in 89% of patients; nearly identical with that in the study of Beaujeux et al,12 who reported immediate occlusion in 91% of lesions. In our series, both patients with immediate partial occlusion had delayed total occlusion, during follow-up in 1 patient (Fig 3) and after a new session of treatment in the other. We also observed spontaneous occlusion without treatment of an AVF. This circumstance is similar to the occlusion of the fistula after selective catheterization reported in 1 study12 and the spontaneous closure of the shunt without intervention mentioned by another author.15
Seventeen patients (94.5%) had clinical resolution of symptoms after embolotherapy. One patient who presented with incomplete improvement had dementia syndrome, and though improvement in mentation was difficult to quantify, some objective change was observed.
Although ischemic events, contrast media reactions, and clinical deterioration have been described after treatment of AVFs,3,16-19 the absence of complications in our series and that of Beaujeux et al12 shows that this technique can be a safe method of management for this pathology.
Conclusions
In this small series, endovascular techniques for occlusion of vertebral artery lesions were safe and effective methods of treatment. They were not associated with significant morbidity or mortality and could be the methods of choice for the treatment of most vertebral artery traumatic lesions, reserving surgery only for patients with severe bleeding or after failed embolization.20
References
- 1.Nagashima C, Iwasaki T, Kawanuma S, et al. Traumatic arteriovenous fistula of the vertebral artery with spinal cord symptoms. J Neurosurg 1977;46:681–87 [DOI] [PubMed] [Google Scholar]
- 2.De Bray JM, Bertrand P, Bertrand F, et al. Spontaneous arteriovenous fistulas of the vertebral artery: apropos of a case—review of the literature [in French]. Rev Med Interne 1986;7:133–39 [DOI] [PubMed] [Google Scholar]
- 3.Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR Am J Roentgenol 1988;150:405–12 [DOI] [PubMed] [Google Scholar]
- 4.Merland JJ, Reizine D, Riche MC, et al. Endovascular treatment of vertebral arteriovenous fistulas in twenty-two patients. Ann Vasc Surg 1986;1:73–78 [DOI] [PubMed] [Google Scholar]
- 5.Hieshima GB, Cahan LD, Mehringer CM, et al. Spontaneous arteriovenous fistulas of cerebral vessels in association with fibromuscular dysplasia. Neurosurgery 1986;18:454–58 [DOI] [PubMed] [Google Scholar]
- 6.Deans WR, Block S, Leibrock L, et al. Arteriovenous fistula in patients with neurofibromatosis. Radiology 1982;144:103–07 [DOI] [PubMed] [Google Scholar]
- 7.Reizine D, Laouiti M, Guimaraens L, et al. Vertebral arteriovenous fistulas: clinical presentation, angiographical appearance and endovascular treatment—a review of twenty-five cases [in English, French]. Ann Radiol (Paris) 1985;28:425–38 [PubMed] [Google Scholar]
- 8.Hayward R, Swanton H, Treasure T. Acquired arteriovenous communication: complication of cannulation of internal jugular vein. Br Med J (Clin Ed) 1984;288:1195–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verrières D, Bernard C, Dacheux J, et al. Cervical arteriovenous fistulas after internal jugular catheterization. Ann Fr Anesth Reanim 1986;5:162–64 [DOI] [PubMed] [Google Scholar]
- 10.Johnson CE, Russell EJ, Huckman MS. Resolution of spinal epidural vascular pseudotumor following balloon occlusion of a postoperative vertebral arteriovenous fistula. Neuroradiology 1990;31:529–32 [DOI] [PubMed] [Google Scholar]
- 11.Olson RW, Baker HL Jr, Svien HJ. Arterio-venous fistula: a complication of vertebral angiography—a report of a case. Neurosurg 1963;20:73–75 [DOI] [PubMed] [Google Scholar]
- 12.Beaujeux RL, Reizine DC, Casasco A, et al. Endovascular treatment of vertebral arteriovenous fistula. Radiology 1992;183:361–67 [DOI] [PubMed] [Google Scholar]
- 13.Múnera F, Soto JA, Palacio DM, et al. Penetrating neck injuries: helical CT angiography for initial evaluation. Radiology 2002;224:366–72 [DOI] [PubMed] [Google Scholar]
- 14.Connors JJ, Wojak JC. Interventional Neuroradiology: Strategies and Techniques. Philadelphia: Saunders;1999
- 15.Kubota M, Watanabe O, Takase M, et al. Spontaneous disappearance of arteriovenous fistula between the vertebral artery and deep cervical vein: case report. Neurol Med Chir (Tokyo) 1992;32:84–87 [DOI] [PubMed] [Google Scholar]
- 16.Halbach VV, Higashida RT, Hieshima GB, et al. Normal perfusion pressure breakthrough occurring during treatment of carotid and vertebral fistulas. AJNR Am J Neuroradiol 1987;8:751–56 [PMC free article] [PubMed] [Google Scholar]
- 17.Higashida RT, Halbach VV, Tsai FY, et al. Interventional neurovascular treatment of traumatic carotid and vertebral artery lesions: results in 234 cases. AJR Am J Roentgenol 1989;153:577–82 [DOI] [PubMed] [Google Scholar]
- 18.Spetzler RF, Wilson CB, Weinstein P, et al. Normal perfusion pressure breakthrough theory. Clin Neurosurg 1978;25:651–72 [DOI] [PubMed] [Google Scholar]
- 19.Kondoh T, Tamaki N, Takeda N, et al. Fatal intracranial hemorrhage after balloon occlusion of an extracranial vertebral arteriovenous fistula. J Neurosurg 1988;69:945–48 [DOI] [PubMed] [Google Scholar]
- 20.Demetriades D, Theodorou D, Asensio J, et al. Management options in vertebral artery injuries. Br J Surg 2005;83:83–86 [DOI] [PubMed] [Google Scholar]