Abstract
Background
It has long been suspected that Canadian Inuit children suffer from frequent severe lower respiratory tract infections (LRTIs), but the causes and risk factors have not been documented. This study assessed the infectious causes and other epidemiologic factors that may contribute to the severity of LRTI in young Inuit children on Baffin Island.
Methods
A prospective case study was carried out at the Baffin Regional Hospital in Iqaluit, Nunavut, of infants less than 6 months of age, who were admitted to hospital between October 1997 and June 1998 with a diagnosis of LRTI. Immunofluorescent antibody testing was used to identify respiratory viruses, and enzyme immunoassay (EIA) and polymerase chain reaction (PCR) were used to test for Chlamydia trachomatis. Demographic and risk factor data were obtained through a questionnaire.
Results
The annualized incidence rate of admission to hospital for bronchiolitis at Baffin Regional Hospital was 484 per 1000 infants who were less than 6 months of age; 12% of the infants were intubated. Probable pathogens were identified for 18 of the 27 cases considered in our study. A single agent was identified for 14 infants: 8 had respiratory syncytial virus, 2 adenovirus, 1 rhinovirus, 1 influenza A, 1 parainfluenza 3 and 1 had cytomegalovirus. For 4 infants, 2 infectious agents were identified: these were enterovirus and Bordetella pertussis, adenovirus and enterovirus, cytomegalovirus and respiratory syncytial virus, and respiratory syncytial virus and adenovirus. C. trachomatis was not identified by either EIA or PCR. All infants were exposed to maternal smoking in utero, second-hand smoke at home and generally lived in crowded conditions.
Interpretation
Inuit infants in the Baffin Region suffer from an extremely high rate of hospital admissions for LRTI. The high frequency and severity of these infections calls for serious public health attention.
Aboriginal children around the world suffer from more severe lower respiratory tract infections (LRTIs) and have higher rates of admission to hospital and mechanical ventilation than their non-Aboriginal counterparts,1,2,3,4,5 but little is known about the epidemiology of LRTI in Canadian Inuit children.
Clinical experience at the Baffin Regional Hospital in Iqaluit suggests that Inuit children in the Baffin Region suffer high rates of LRTI. This was documented in a retrospective chart review6 of admissions to the Baffin Regional Hospital between March 1995 and February 1996, which revealed a high rate of bronchiolitis among infants under the age of 12 months. There were 94 admissions of infants for bronchiolitis, yielding a rate of 306 admissions to hospital per 1000 infants. Of all the children admitted with bronchiolitis, about 13% required intubation and transfer to a tertiary care centre. This study identified Chlamydia trachomatis as a pathogen in a significant fraction of admissions; the results of testing for respiratory syncytial virus, which is the infectious agent most commonly associated with bronchiolitis, proved to be negative in many cases.
We therefore carried out a prospective study aimed at confirming the high rate of LRTI among Inuit infants on Baffin Island and identifying pathogens and other risk factors.
Methods
The study took place at Baffin Regional Hospital in Iqaluit, which is situated in Nunavut. Baffin Regional Hospital services the town of Iqaluit and about 10 smaller isolated communities on Baffin Island. Baffin Island has a population of about 13 200, of whom about 80% are Inuit (Department of Executive and Intergovernmental affairs, Government of Nunavut: unpublished data based on Statistics Canada Census, 1996). There were about 316 births per year in the Baffin Region between 1992 and 1996 (i.e., in the catchment population for the Baffin Regional Hospital) (NWT Bureau of Statistics, Government of the Northwest Territories: unpublished data, 1996).
Eligible infants were less than 6 months of age and were admitted to Baffin Regional Hospital between Oct. 15, 1997, and June 15, 1998, with a diagnosis of LRTI. A research nurse in Iqaluit was responsible for identifying and enrolling study subjects, obtaining informed consent, and collecting and transporting specimens. Epidemiologic data were collected using a questionnaire regarding medical history, breast-feeding, exposure to cigarette smoke and household information. Information was also collected on length of stay in hospital and the need for intubation and mechanical ventilation. The results of maternal antenatal screening for C. trachomatis were obtained from the infants' charts.
All specimens were refrigerated at 4°C until they were transported by air to Montreal Children's Hospital. Nasopharyngeal aspirate specimens for virologic studies were collected by suction aspiration and were placed in viral transport media. At Montreal Children's Hospital, one aliquot was inoculated into HEp2 and rhesus monkey kidney cells. Cytopathic effect was confirmed by immunofluorescent antibody (IFA) testing on cells scraped from the monolayer. A second aliquot was processed using a pool of monoclonal antibodies (IFA) directed against respiratory syncytial virus, adenovirus, influenza A and B, and parainfluenza 1, 2 and 3 (Bartel Immunodiagnostics, Bellvue, Wash.). Eye and nasopharyngeal aspirate specimens for C. trachomatis enzyme immunoassay (EIA) testing were collected and processed weekly using Chlamydiazyme (Abbott Diagnostics, Chicago). Eye and nasopharyngeal aspirate specimens for C. trachomatis polymerase chain reaction (PCR)7 testing were collected using a calcium alginate swab and placed into Chlamydia medium (2SP). They were kept frozen at –70° C until June 1998 when they were processed with AMPLICOR (Roche Diagnostics Systems, Branchburg, NJ).
Ethics approval for this study was obtained through the ethics committee and institutional review boards of the Montreal Children's Hospital and the Baffin Regional Inuit Health Board. The study was licensed through the Nunavut Research Institute.
Descriptive statistics such as proportions were calculated for categorical variables. The statistical significance of differences in the means of continuous variables was assessed using t-tests.
Results
During the 8-month period between Oct. 15, 1997, and June 15, 1998, there were 51 admissions to hospital for LRTI of 42 infants who were less than 6 months of age. The annualized incidence rate of admission to hospital for LRTI was 484 per 1000 among infants under 6 months of age. The calculation was based on 51 admissions х 1000 divided by a population at risk of 105.3. The population at risk was calculated as follows: 316 (approximate annual birth rate) х 8/12 (8-month study period) х 50% (representing the 50% of the children who were < 6 months of age). Twenty-six infants (27 admissions) were enrolled in our study. Reasons for nonenrollment included unavailability of the guardian (n = 15), declining to participate in the study (n = 7) and immediate transfer to a tertiary hospital (n = 2). The median age of enrolled subjects was 8 weeks (range 4 days to 6 months). Six of the 26 infants (23%) had had previous admissions to Baffin Regional Hospital for LRTI. Four (15%) infants were born preterm (< 37 weeks' gestation).
Admission diagnoses were bronchiolitis (n = 23), apnea (n = 2), bacterial pneumonia (n = 1) and pertussis (n = 1) (Table 1). The mean duration of stay in hospital was 8.5 days per child; 4 infants spent a total of 75 days in tertiary care. Three infants (12%) were intubated and received mechanical ventilation for 4, 17 and 9 days respectively.
Table 1
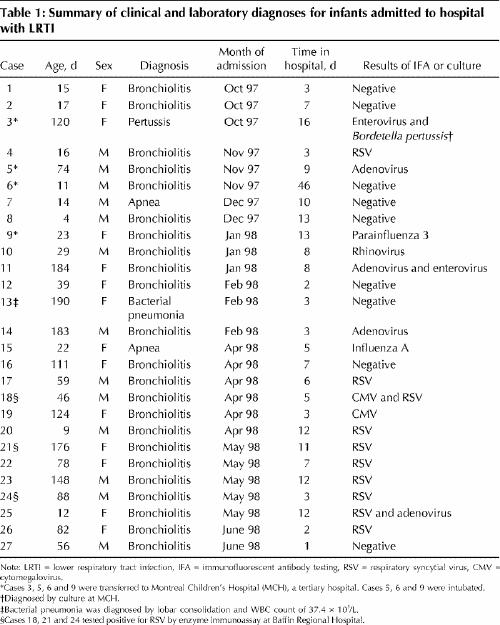
For 18 of the infants, one or more infectious agent was identified (Table 1). In 14 infants, a single agent was identified: respiratory syncytial virus in 8 patients, adenovirus in 2, rhinovirus in 1, influenza A in 1, parainfluenza 3 in 1, and cytomegalovirus in 1. In 4 infants, 2 infectious agents were identified; these were enterovirus and Bordetella pertussis, adenovirus and enterovirus, cytomegalovirus and respiratory syncytial virus, and respiratory syncytial virus and adenovirus. The median time from procurement of the specimen at Baffin Regional Hospital to inoculation into viral culture at Montreal Children's Hospital was 3.0 days (range 1–6 days). All eye and nasopharyngeal aspirate specimens tested for C. trachomatis by PCR or EIA were negative. Antenatal records were available for 24 of the 26 patients, whose mothers were screened for C. trachomatis by ligase chain reaction (LCR) testing of the urine with 5 positive results (21%).
All 26 mothers smoked during pregnancy, with a self-declared mean of 8.7 cigarettes per day. All infants were exposed to second-hand smoke in their homes. On average, there were 2.9 smokers per household (range of 1–7). The average household consisted of 6.4 members (3.4 adults and 3.0 children).
Eleven (42%) infants were adopted by a relative. The adopted infants stayed in hospital for 12.6 days on average compared with 5.7 days (p = 0.08) for nonadopted infants. Breast-fed infants stayed in hospital for a mean of 6.5 days versus 10.4 in nonbreast-fed infants (p = 0.28).
Interpretation
Our study confirms that Inuit infants suffer from a high rate of LRTI and often require mechanical ventilation. The rates of admission to hospital for LRTI in this population are among the highest in the world.8 Indeed, the Northwest Territories and Nunavut have the highest infant mortality rates in Canada, which are double the Canadian average.9
A recent study8 of acute respiratory tract infections in native children in Alaska demonstrated very high annual rates of admission to hospital for respiratory syncytial virus infections of 53–249 cases per 1000. Respiratory syncytial virus was associated with 46% of all admissions for acute respiratory tract infections. Although respiratory syncytial virus tends to be the major infectious agent of bronchiolitis in most populations, our study found only 10 cases (37%) that were positive for respiratory syncytial virus. Respiratory tract infections with respiratory syncytial virus, other viruses and C. trachomatis in early infancy have been associated with recurrent LRTI and are associated with chronic lung disease.10,11,12,13
The Northwest Territories have reported the highest incidence in Canada of C. trachomatis infections in adults, that is, about 11 times the national average,14 and high rates in infants were found in the chart review, however, C. trachomatis was not detected prospectively in children by EIA or PCR. Antenatal testing for C. trachomatis was performed at Baffin Regional Hospital by EIA on endocervical swabs but, in March 1997, was replaced with testing by LCR on first void urine. This resulted in a substantial increase in the number of positive cases of C. trachomatis. In this interval of time, the treatment for C. trachomatis in pregnancy changed from erythromycin to a single dose of azithromycin. These diagnostic and treatment changes may have affected antenatal and postnatal C. trachomatis rates.
Host and environmental factors have been implicated as contributing to the severity of LRTIs in this population. Preliminary results have shown that Inuit infants on Baffin Island may have defects in cell-mediated immunity.15,16 Environmental factors such as substandard housing and crowding and poor ventilation in the home may play a role. The mean number of members per household was 6.4, which is much higher than the Canadian mean of 2.6 people per household and the Nunavut mean of 3.9. Overcrowded conditions have been implicated previously in LRTIs in Aboriginal children.1,2,3 Similarly, studies have shown that Aboriginal infants who were breast-fed generally had less severe disease and a shorter stay in hospital for LRTI.1,2,3 Another potential environmental factor is adoption, which is an Inuit tradition, but there are no reliable statistics for adoption rates, nor for the effects of adoption on the health of Inuit children.
Smokers comprise 64% of the Nunavut population, but only 27% of the overall Canadian population (NWT Bureau of Statistics, Government of the Northwest Territories. Drug and Alcohol Survey: unpublished data, 1996). In Nunavut, the rate of smoking in the Aboriginal population is nearly twice that in the non-Aboriginal population. All of the patients we studied had had exposure to tobacco in utero and to second-hand smoke at home. Cigarette exposure may be further magnified in the Arctic by increased time spent indoors in relatively airtight housing. Exposure to cigarette smoke in utero is known to be associated with infants who are small for their gestational ages, prematurity, increased risk of LRTI, reactive airway disease and death.17,18,19
The major limiting factor in our research was the small population studied, which limited the potential number of enrolments. A control group was not included, and invasive procedures were limited because of a general apprehension about research in Inuit populations. The viability of infectious agents may have been lost in transportation.
This study suggests that LRTI in Inuit infants is one of the most important health challenges in this population. Host and environmental factors may contribute to the severity of their illness. The infants in this study were exposed to a substantial amount of cigarette smoke in utero and after birth, and they lived in crowded conditions. The reduction of exposure to cigarette smoke is essential for a population that is already compromised due to respiratory illness. It is hoped that larger studies in the future will clarify the roles of smoking, breast-feeding, adoption, overcrowding and other risk factors in LRTI, with the goal of reducing the impact of respiratory disease in the Inuit population.
Footnotes
This article has been peer reviewed.
Acknowledgements: We would like to acknowledge the help of Baffin Regional Hospital; the Sir Mortimer B. Davis Jewish General Hospital, Montreal; Montreal General Hospital laboratories; and especially Diane Newby and her virology staff at the Montreal Children's Hospital, Montreal, Que. Most of all we would like to thank the Inuit people on Baffin Island who participated in this study.
We would like to thank the Medical Research Council of Canada, the Canadian Infectious Disease Society and Bayer Canada for funding a clinical research fellowship position for Dr. Banerji, and we would like to thank the Division of Sexual Health Promotion and STD Prevention and Control of Health Canada and the Montreal Children's Hospital Research Institute for a research grant. We would like to thank Roche Diagnostic Systems, Branchburg, NJ, for donating supplies for the PCR.
Competing interests: None declared.
Reprint requests to: Dr. Anna Banerji, BC's Children's Hospital, Emergency Department, 4480 Oak St., Vancouver BC V6A 3V4; fax 604 681-8930; abanerji@sprint.ca
References
- 1.Singleton RJ, Petersen KM, Berner JE, Schulte E, Chiu K, Lilly CM, et al. Hospitalizations for respiratory syncytial virus infection in Alaska native children. Pediatr Infect Dis J 1995;14(1):26-30. [DOI] [PubMed]
- 2.Houston CS, Weiler RL, Habbick BF. Severity of lung disease in Indian children. CMAJ 1979;120(May 5):1116-21. [PMC free article] [PubMed]
- 3.Brody JA. Lower respiratory illness among Alaskan Eskimo children. Arch Environ Health 1965;11:620. [DOI] [PubMed]
- 4.Carson JB, Postl BD, Spady D, Schaefer O. Lower respiratory tract infections among Canadian Inuit children. Int J CircumpolarHealth 1984;84:226-8.
- 5.Fleshman JK, Wilson JF, Cohen JJ. Bronchiectasis in Alaska native children. Arch Environ Health 1986;17:517. [DOI] [PubMed]
- 6.Banerji A. High admission rates for bronchiolitis in Inuit children on Baffin Island. Int J Circumpolar Health. In press. [PubMed]
- 7.Hammerschlag MR, Roblin PM, Gelling M, Tsumura N, Julie JE, Kutlin A. Use of polymerase chain reaction for the detection of C. trachomatis in ocular and nasopharyngeal specimens from infants with conjunctivitis. Pediatr Infect Dis J 1997;16:293-6. [DOI] [PubMed]
- 8.Karron RA, Singleton RJ, Bulkow L, Parkinson A, Kruse D, Irma DeSmet. Severe respiratory syncytial virus disease in Alaska Native children. J Infect Dis 1999;180:41-9. [DOI] [PubMed]
- 9.Infant mortality rate. Ottawa: Statistics Canada; 1996. Cat no 82-221-XDE.
- 10.Gurwitz D, Midorff C, Levison H. Increased incidence of bronchial reactivity in children with a history of bronchiolitis. J Pediatr 1981;98(4):551-5. [DOI] [PubMed]
- 11.Brasfield DM, Stagno S, Whitley RJ. Infant pneumonitis associated with cytomegalovirus, chlamydia, pneumocystis and ureaplasma: followup. Pediatrics 1987;79:76-83. [PubMed]
- 12.Wiess SG, Newcomb MD, Beem MO. Pulmonary assessment of children after chlamydial pneumonia of infancy. J Pediatr 1986;108:659-64. [DOI] [PubMed]
- 13.Harrison RH, Phil D, Taussig LM, Fulginiti VA. Chlamydia trachomatis and chronic respiratory disease in childhood. Pediatr Infect Dis J 1982;1(1):29-33. [DOI] [PubMed]
- 14.Health Canada. Chlamydia trachomatis in Canada: an update. Can Commun Dis Rep 1997;23(15):1-6. [PubMed]
- 15.Culman KN, Ward BJ, Pekeles GS, Aouchiche S, Mills EL, Johns TM. Comparison of immune cell phenotypes in Inuit and non-Inuit Canadian infants [abstract]. Interscience Conference on Antimicrobial Agents and Chemotherapy; 1999 Sept 26-29; San Francisco.
- 16.Pekeles GS, Aouchiche S, Johns TM, Mills EL, Culman KN, Ward BJ. Differences in costimulatory molecules on peripheral blood mononuclear cells in Inuit and non-Inuit Canadian infants [abstract]. Interscience Conference on Antimicrobial Agents and Chemotherapy; 1999 Sept 26-29; San Francisco.
- 17.Health Canada. The effects of tobacco smoke and second-hand smoke in the prenatal & post partum periods: a summary of the literature. Ottawa: Health Canada; 1995.
- 18.Tager IB, Weiss ST, Munoz A, Rosner B, Speizer FE. Longitudinal study of the effects of maternal smoking on pulmonary function in children. N Engl J Med 1983;309:699-703. [DOI] [PubMed]
- 19.Stick SM, Burton PR, Gurrin L, Sly PD, LeSouef PN. Effects of maternal smoking during pregnancy and a family history of asthma on respiratory function in newborn infants. Lancet 1996;348(9034):1060-4. [DOI] [PubMed]


