Highlights
-
•
The classical pattern in HRCT of COVID-19 infected individuals is GGO that progressed into a consolidation with increasing severity of infection.
-
•
The most common distribution pattern of COVID-19 is bilateral involvement of lungs with multiple lesions in peripheral areas of both lungs.
-
•
Typical but less common findings are pleural effusion, reversed halo sign and lymph adenopathy.
Abbreviations: HRCT, High Resolution Computed Tomography; GGO, Ground Glass Opacity; COVID-19, Corona Virus Disease-2019; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2
Keywords: HRCT, CT-scan, COVID-19, SARS-CoV-2, Ground glass opacity, Consolidation
Abstract
Background
Recent studies reported that CT scan findings could be implicated in the diagnosis and evaluation of COVID-19 patients.
Objective
To identify the role of High-Resolution Computed Tomography chest and summarize characteristics of chest CT imaging for the diagnosis and evaluation of SARS-CoV-2 patients.
Methodology
Google Scholar, PubMed, Science Direct, Research Gate and Medscape were searched up to 31 January 2020 to find relevant articles which highlighted the importance of thoracic computed tomography in the diagnosis as well as the assessment of SARS-CoV-2 infected patients. HRCT abnormalities of SARS-CoV-2 patients were extracted from the eligible studies for meta-analysis.
Results
In this review, 28 studies (total 2655 patients) were included. Classical findings were Ground Glass Opacities (GGO) (71.64 %), GGO with consolidation (35.22 %), vascular enlargement (65.41 %), subpleural bands (52.54 %), interlobular septal thickening (43.28 %), pleural thickening (38.25 %), and air bronchograms sign (35.15 %). The common anatomic distribution of infection was bilateral lung infection (71.55 %), peripheral distribution (54.63 %) and multiple lesions (74.67 %). The incidences were higher in in the left lower lobe (75.68 %) and right lower lobe (73.32 %). A significant percentage of patients had over 2 lobes involvement (68.66 %).
Conclusion
Chest CT-scan is a helpful modality in the early detection of COVID-19 pneumonia. The GGO in the peripheral areas of lungs with multiple lesions is the characteristic pattern of COVID-19. The correct interpretation of HRCT features makes it easier to detect COVID-19 even in the early phases and the disease progression can also be accessed with the help of the follow-up chest scans.
1. Introduction
It has been a century since mankind has experienced a globally spreading disease influenza that appeared in 1918. Now in 2019 mankind is again to witness another globally spreading disease COVID-19 [1]. This novel SARS-COV-2 first manifested itself as a strange sort of respiratory disorder with the first reported case in Wuhan, China on 12 December 2019 [2,3]. The novel coronavirus disease that appeared from Wuhan, China has been spread to every country around the globe and has forced the people to modify their lives in new inconvenient ways [4]. It has been found that this coronavirus infection passes through three distinguishable phases, the first stage in which SARS-CoV-2 has not manifested its sign and symptoms in its host, the second stage in which symptoms have developed but they are less intense and in third stage symptoms become intense and COVID-19 virus has reached to its maximum number by multiplication [5]. In the early phases of this epidemic, it was considered that this SARS−COV-2 can only affect the elderly population [6]. As the epidemic spread, it was found that this disease not only affects the elderly population but also virulent in young individuals [7]. Coronavirus possesses a very high ability to transmit as well as very high virulence. The mode of transmission of SARS-CoV-2 is direct touch as well as droplets of cough and sneeze of an infected person [10]. The pathogenesis of SARS−COV-2 lead to the development of clinical manifestations that appear within two days or it may take almost two weeks after getting in contact with the infected person [8]. According to the basic structure of SARS−COV-2, it bears spikes made-up of glycoprotein on its envelope. It is an RNA-containing virus and is very small in size with a diameter of 65−125 nm. The sub-groups of coronaviruses are as follows: alpha (α), beta (β), gamma (γ), and delta (δ) [9]. As an appropriate vaccine has not been developed against this coronavirus so it is very important to early detect, diagnose and isolate the patients from the healthy individuals to protect them from this lethal virus [16]. Researchers give the primary position to real-time polymerase chain reaction (RT-PCR) to label the patient as the victim of COVID-19. But the issue with this testing procedure is the false negative reports because of the decreased number of viruses and technical errors. According to researches it has been found that in the first five days real-time PCR gives a false negative report. But if the clinicians took a modality from radiology to detect these viral infections, then Computed Tomography showed the ability to unveil the infection even in the early phases [11]. Chest computed tomography plays significant role in the detection, evaluation and management of coronavirus infection [12]. Computed tomography has superiority over plain chest imaging because it is very easy to miss GGO by using plain radiography. So, it is recommended to use computed tomography for the early detection of coronavirus infection [13]. The important characteristic of the scanning is to focus the GGO along with or without solid masses near the borders of the inferior and dorsal pulmonary areas [14]. The unusual findings are fluid in the pleural cavity, lymph enlargement, lung cavitation and calcification as well [15]. Thin-section chest computed tomography is effectual in the diagnosis of lung infection caused by a coronavirus and assess the progression of the disease [16]. The severity of lung involvement in coronavirus disease 2019 is assessed by the radiologic features of chest CT scan [17].
2. Materials & methods
This systematic review and meta‐analysis were carried out in agreement with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses guidelines (PRISMA).
2.1. Search strategy
Google Scholar, PubMed, Science Direct, Research Gate and Medscape were searched to find relevant articles using the keywords or abbreviations: “COVID-19”, “coronavirus disease”, “2019n-CoV”, “SARS-CoV-2”, “Computed Tomography”, “Chest CT-scan”, “CT-imaging in COVID-19”, “GGO”, and “Imaging characteristics in SARS-CoV-2”.
2.2. Selection criteria
The inclusion criterion was as follows: (a) articles contained the information related to adults or children, (b) laboratory‐confirmed RT-PCR positive COVID‐19 pneumonia patients undergoing chest scanning, (c) thoracic computed tomography and pulmonary features of SARS-CoV-2 (d) Positive Computed tomography findings in coronavirus disease patients, (e) studies containing radiological features of SARS-CoV-2 with more than 5 patients (d) all articles which were published in English language.
Case reports, reviews, letters to editorials, comments, studies with less than 5 patients and studies with insufficient data were excluded.
2.3. Data collection
Articles were screened according to above mentioned keywords in their title and abstract. Studies which did not meet pre-defined criteria were excluded. After duplication removal, second screening was performed for finding the relevant full-text articles based on radiological manifestation of chest CT scan.
2.4. Data extraction
Data were extracted from the full journal eligible articles and studies were assessed for applicability and quality. Summary statistics were calculated from the raw data given in the study if they were not reported. Numerical values were taken from graphs or bar-charts if not found in the text of the studies.
2.5. Data synthesis and analysis procedure
The 28 eligible studies were used for the extraction of data. Data was extracted for following characteristics: Author, year of publication, number of patients, research type, country of research, timing of CT scan, ground-glass opacities (GGO), mixed pattern, consolidation, pleural effusion, pleural thickening, lymphadenopathy, nodule, interlobular septal thickening, bronchial wall thickening, subpleural bands, traction bronchiectasis, vascular enlargement, lobe of lung involved, unilateral or bilateral pneumonia, peripheral or central involvement, numbers of lobes involved, reversed halo sign, number of lesion, crazy paving pattern, and air bronchogram.
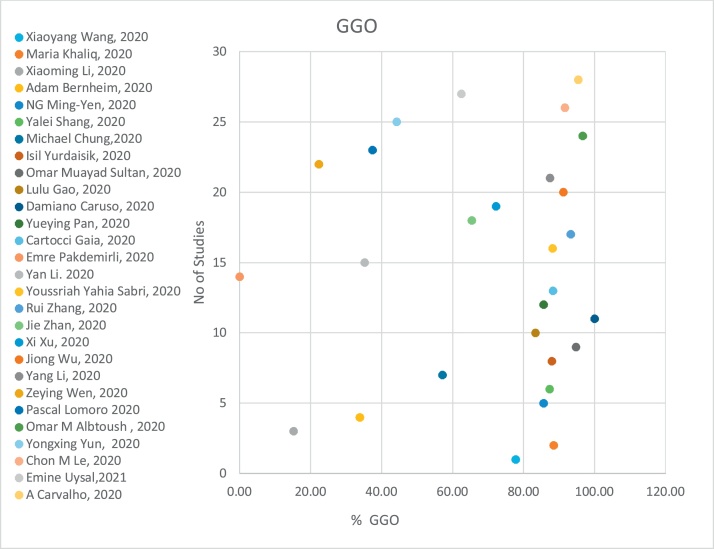
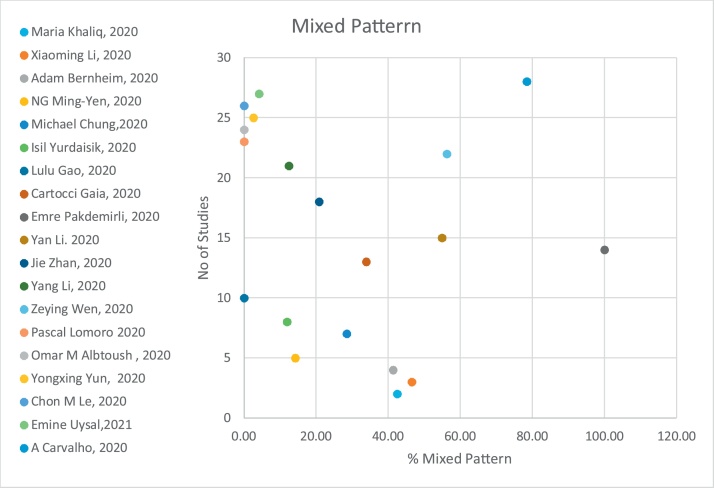
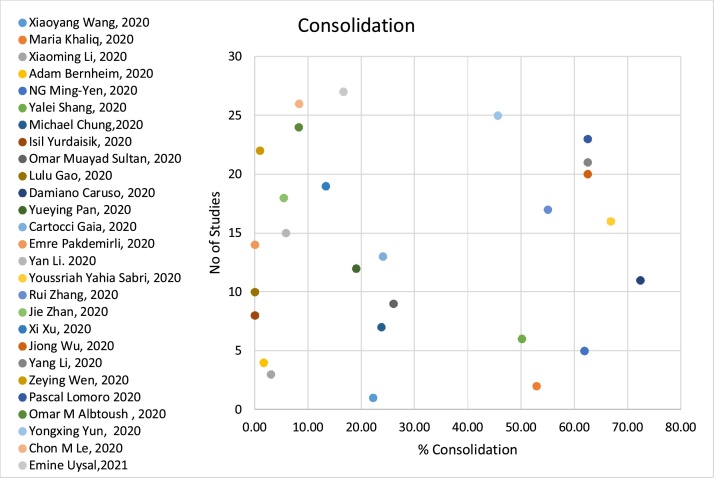
2.6. Statistical analysis
Extracted data from the 28 articles was entered in Microsoft Excel Spread Sheet (V. 2016). Mean age, Gender Ratio, Individual Radiological parameters percentages, overall percentages (Pooled Analysis) were calculated. Scatter plots for GGO, Consolidation, Mixed pattern, Pleural Thickening, Bilateral Pneumonia and peripheral distribution were constructed to have better visualization of results.
2.7. Ethical considerations
No ethical consideration is required for this systematic review.
3. Results
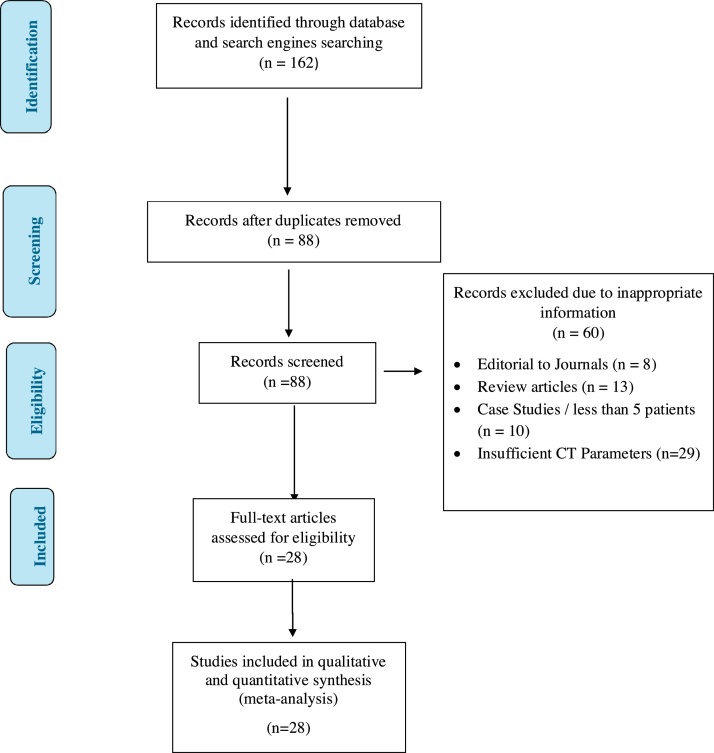
Our Primary literature screening identified one hundred and sixty two (162) articles. Seventy four (74) articles were removed because of duplication. 88 studies were screened for title and abstract. Sixty (60) articles were excluded not containing required information. Twenty eight (28) articles (total of 2655 patients) were included and used for the extraction of data related to CT-scan radiological manifestation of COVID-19 patients. The whole process of searching is depicted in Fig. 1. Table 1 shows the qualitative variables (number of patients, mean age, type of research, and place of research, timing of CT-scan) of 28 screened studies. Table 2 show the number of patients, who presented with radiological features of COVID-19. In this review, the mean age of COVID-19 patients is 48.04 years. The percentages of male and female COVID-19 infected individuals are 54 % and 46 % respectively. Timing of CT-Scan ranges from the onset of symptoms to 21st day of follow up among various studies recruited for this review.
Fig. 1.
PRISMA Flow diagram of literature searched.
Table 1.
Article first authors, Number of patients, Research type, Country of origin & Timing of CT Scan.
| First Author, Year | Number of Patients | Mean Age (Years) | Research Type | Country | Timing of CT Scan |
|---|---|---|---|---|---|
| Xiaoyang Wang, 2020 [18] | 54 (M = NA, F = NA) | 44 | Retrospective | China | 1−11 days (M = 4 days) |
| Maria Khaliq, 2020 [19] | 87 (M = 45, F = 42) | 47.2 | Cross-sectional | Pakistan | NA |
| Xiaoming Li, 2020 [20] | 131 (M = 63, F = 68) | 55 | Retrospective | China | 2−7 days ( = 3.5 days) |
| Adam Bernheim, 2020 [21] | 121 (M = 61, F = 60) | 45 | Retrospective | China | 0−18 days ( = 4.5 days) |
| NG Ming-Yen, 2020 [22] | 21 (M = 13, F = 8) | 56 | Retrospective | Hongkong, China | 1−7 days (M = 3 days) |
| Yalei Shang, 2020 [23] | 307 (M = 164, F = 143) | 46 | Multicenter | China | 1−21 days |
| Michael Chung,2020 [24] | 21 (M = 13, F = 8) | 51 | Retrospective | China | 1−4 days ( = 2.5 days) |
| Isil Yurdaisik, 2020 [25] | 50 (M = 35, F = 15) | 53.8 | Retrospective | Turkey | 1st day of admission |
| Omar M Sultan, 2020 [26] | 96 (M = 61, F = 35) | 49.3 | Retrospective cross-sectional | Iraq | 1−14 days (70 = 1−7 days, 26 = 8−14 days) |
| Lulu Gao, 2020 [27] | 6 (M = 1, F = 5) | 40 | Retrospective | China | 2nd day from the onset of symptoms |
| Damiano Caruso, 2020 [28] | 158 (M = 83, F = 75) | 57 | Prospective | Rome, Italy | NA |
| Yueying Pan, 2020 [29] | 63 (M = 33, F = 30) | 44.9 | Retrospective Cross-sectional | China | 3−14 days |
| Cartocci Gaia, 2020 [30] | 162(M = NA, F = NA) | 59.2 | Retrospective | Rome, Italy | NA |
| Emre Pakdemirli, 2020 [31] | 5 (M = 2, F = 3) | 48.2 | Retrospective | London, UK | NA |
| Yan Li. 2020 [32] | 51 (M = 28, F = 23) | 58 | Retrospective cohort | China | 2−15 days ( = 5 days) |
| Youssriah Sabri, 2020 [33] | 220 (M = 152, F = 68) | 49.2 | Cross-sectional | Egypt | NA |
| Rui Zhang, 2020 [34] | 120 (M = 43, F = 77) | 45.4 | Retrospective | China | NA |
| Jie Zhan, 2020 [35] | 110 (M = 67, F = 43) | 43.8 | Retrospective | China | 2−9 days ( = 5.3 days) |
| Xi Xu, 2020 [36] | 90 (M = 39, F = 51) | 50 | Retrospective | China | 1−6 days ( = 3.5 days) |
| Jiong Wu, 2020 [37] | 80 (M = 42, F = 38) | 44 | Retrospective | China | 3−11 days ( = 7 days) |
| Yang Li, 2020 [38] | 8 (M = 3, F = 5) | 2.6 | Retrospective | China | NA |
| Zeying Wen, 2020 [39] | 103 (M = 48, F = 55) | 46 | Retrospective | China | NA |
| Pascal Lomoro [40] | 40(M-25, F = 15) | 66.3 | Retrospective | Como, Italy | NA |
| Omar M Albtoush, 2020 [41] | 121 (M = 70, F = 51) | 46.1 | Retrospective | Jordan | NA |
| Yongxing Yun, 2020 [42] | 305(M-149, F = 156) | 49 | Retrospective | China | 3−6 days ( = 5 days) |
| Chon M Le, 2020 [43] | 24(M = 14, F = 10) | 34.4 | Retrospective | Macao | 5.7 days |
| Emine Uysal,2021 [44] | 48(M = 17, F = 31) | 59.4 | Retrospective | Turkey | NA |
| A Carvalho, 2020 [45] | 153 (M = 87, F = 66) | 64.7 | Retrospective | Portugal | 10.9 ± 6.6 days |
(M = Male, F = Female, NA = Not Available, =Mean, M = Median).
Table 2.
CT Findings in COVID-19 patients from included studies.
| First Author, Year | GGO | Mixed Pattern | Consolidation | Pleural Effusion | Pleural Thickening | Pleural Effusion/ thickening | Lymph-adenopathy | Nodule | Interlobular Septal Thickening | Bronchial Wall Thickening | Subpleural bands |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Xiaoyang Wang, 2020 [18] | 42 | NA | 12 | NA | NA | 14 | 2 | NA | 11 | 3 | NA |
| Maria Khaliq, 2020 [19] | 77 | 37 | 46 | 2 | NA | NA | NA | 0 | NA | NA | NA |
| Xiaoming Li, 2020 [20] | 20 | 61 | 4 | NA | 31 | NA | 17 | 7 | 68 | NA | NA |
| Adam Bernheim, 2020 [21] | 41 | 50 | 2 | 1 | NA | NA | 0 | 0 | NA | 14 | NA |
| NG Ming-Yen, 2020 [22] | 18 | 3 | 13 | 0 | NA | NA | NA | 1 | NA | NA | NA |
| Yalei Shang, 2020 [23] | 268 | NA | 154 | 8 | 154 | NA | 8 | NA | 186 | NA | NA |
| Michael Chung,2020 [24] | 12 | 6 | 5 | 0 | NA | NA | 0 | NA | NA | NA | NA |
| Isil Yurdaisik, 2020 [25] | 44 | 6 | 0 | NA | NA | NA | NA | NA | NA | NA | NA |
| Omar M Sultan, 2020 [26] | 91 | NA | 25 | 3 | NA | NA | NA | 4 | NA | 13 | NA |
| Lulu Gao, 2020 [27] | 5 | 0 | 0 | NA | NA | NA | NA | 4 | 1 | 4 | 2 |
| Damiano Caruso, 2020 [28] | 58 | NA | 42 | 2 | NA | NA | 34 | NA | 8 | 1 | NA |
| Yueying Pan, 2020 [29] | 54 | NA | 12 | NA | NA | NA | NA | NA | NA | NA | NA |
| Cartocci Gaia, 2020 [30] | 143 | 55 | 39 | 4 | NA | NA | 24 | NA | 37 | 37 | NA |
| Emre Pakdemirli, 2020 [31] | 0 | 5 | 0 | 1 | 1 | NA | NA | NA | NA | 1 | NA |
| Yan Li. 2020 [32] | 18 | 28 | 3 | 1 | NA | NA | 0 | NA | 37 | NA | NA |
| Youssriah Sabri, 2020 [33] | 194 | NA | 147 | NA | NA | NA | NA | NA | NA | NA | NA |
| Rui Zhang, 2020 [34] | 112 | NA | 66 | 10 | NA | NA | 5 | 65 | NA | NA | NA |
| Jie Zhan, 2020 [35] | 72 | 23 | 6 | 2 | 12 | NA | 0 | 48 | NA | 62 | 65 |
| Xi Xu, 2020 [36] | 65 | NA | 12 | 4 | 50 | NA | 1 | NA | 33 | NA | NA |
| Jiong Wu, 2020 [37] | 73 | NA | 50 | 5 | NA | NA | 3 | NA | 47 | 9 | 42 |
| Yang Li, 2020 [38] | 7 | 1 | 5 | 1 | 1 | NA | 1 | 1 | 4 | 1 | NA |
| Zeying Wen, 2020 [39] | 23 | 58 | 1 | 1 | NA | NA | 0 | NA | NA | NA | NA |
| Pascal Lomoro [40] | 15 | 25 | 0 | 3 | NA | NA | 6 | 1 | NA | NA | 15 |
| Omar M Albtoush, 2020 [41] | 117 | 10 | 0 | 2 | NA | NA | 0 | 13 | NA | NA | NA |
| Yongxing Yun, 2020 [42] | 135 | 139 | 8 | 9 | NA | NA | NA | NA | NA | NA | NA |
| Chon M Le, 2020 [43] | 22 | 2 | 0 | 2 | NA | NA | 1 | 4 | 1 | NA | NA |
| Emine Uysal,2021 [44] | 30 | 8 | 2 | NA | NA | NA | NA | NA | 8 | NA | NA |
| A Carvalho, 2020 [45] | 146 | NA | 120 | 45 | NA | NA | 32 | 6 | NA | NA | NA |
| First Author, Year | Traction bronchiectasis | Vascular enlargement | RUL | RML | RLL | LUL | LLL | Unilateral pneumonia | Bilateral pneumonia | Peripheral | Central | Mixed (Central + Peripheral) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Xiaoyang Wang, 2020 [18] | NA | NA | NA | NA | NA | NA | NA | NA | NA | 50 | 4 | NA |
| Maria Khaliq, 2020 [19] | 10 | 10 | NA | NA | NA | NA | NA | 21 | 66 | 71 | 26 | 24 |
| Xiaoming Li, 2020 [20] | NA | 84 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Adam Bernheim, 2020 [21] | 1 | NA | 53 | 50 | 79 | 58 | 76 | NA | 73 | 63 | 0 | NA |
| NG Ming-Yen, 2020 [22] | NA | NA | 14 | 10 | 16 | 16 | 17 | NA | NA | 18 | NA | NA |
| Yalei Shang, 2020 [23] | NA | 208 | 201 | 171 | 208 | 209 | 257 | 60 | 253 | 104 | NA | NA |
| Michael Chung,2020 [24] | NA | NA | 14 | 12 | 16 | 14 | 14 | NA | NA | NA | NA | NA |
| Isil Yurdaisik, 2020 [25] | NA | NA | NA | NA | 38 | NA | 36 | 11 | 39 | 18 | 2 | 28 |
| Omar M Sultan, 2020 [26] | 4 | NA | NA | NA | NA | NA | NA | 14 | 82 | 62 | 11 | 23 |
| Lulu Gao, 2020 [27] | NA | NA | 1 | 3 | 1 | 3 | 3 | 4 | 2 | NA | NA | NA |
| Damiano Caruso, 2020 [28] | 24 | NA | 53 | 48 | 54 | 49 | 53 | NA | 53 | NA | NA | NA |
| Yueying Pan, 2020 [29] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cartocci Gaia, 2020 [30] | NA | NA | NA | NA | NA | NA | NA | 55 | 107 | 68 | 21 | 73 |
| Emre Pakdemirli, 2020 [31] | NA | NA | 5 | 5 | 5 | 4 | 5 | 0 | 5 | 4 | 1 | NA |
| Yan Li. 2020 [32] | NA | 44 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Youssriah Sabri, 2020 [33] | 142 | 220 | NA | NA | NA | NA | NA | 52 | 168 | NA | NA | NA |
| Rui Zhang, 2020 [34] | 14 | NA | 54 | 50 | 83 | 48 | 79 | NA | 68 | 109 | 40 | NA |
| Jie Zhan, 2020 [35] | NA | 43 | 68 | 60 | 87 | 64 | 72 | 27 | 68 | NA | NA | NA |
| Xi Xu, 2020 [36] | NA | NA | 48 | 40 | 59 | 48 | 55 | NA | 53 | 46 | NA | NA |
| Jiong Wu, 2020 [37] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Yang Li, 2020 [38] | NA | 5 | NA | NA | NA | NA | NA | 2 | 5 | NA | NA | NA |
| Zeying Wen, 2020 [39] | NA | NA | 14 | 37 | 58 | 17 | 63 | 25 | 57 | 63 | 3 | 16 |
| Pascal Lomoro [40] | NA | 10 | 39 | 35 | 39 | 39 | 39 | NA | 40 | 27 | 1 | 12 |
| Omar M Albtoush, 2020 [41] | NA | NA | 76 | 61 | 90 | 73 | 87 | 31 | 86 | NA | NA | NA |
| Yongxing Yun, 2020 [42] | 10 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Chon M Le, 2020 [43] | NA | NA | 12 | 10 | 18 | 13 | 18 | NA | NA | 24 | NA | NA |
| Emine Uysal,2021 [44] | NA | NA | 26 | 20 | 38 | 27 | 34 | 16 | 32 | 22 | 5 | 21 |
| A Carvalho, 2020 [45] | NA | NA | 136 | 129 | 136 | 138 | 150 | NA | NA | 60 | 5 | 85 |
| First Author, Year | UL | LL | 1 lobe involved | 2 lobes involved | Over 2 lobes involved | Reversed halo sign | Single Lesion | Multiple Lesion | Crazy Paving Pattern | Air Bronchogram |
|---|---|---|---|---|---|---|---|---|---|---|
| Xiaoyang Wang, 2020 [18] | 12 | 42 | NA | NA | NA | 9 | 8 | 46 | NA | 18 |
| Maria Khaliq, 2020 [19] | NA | NA | NA | NA | NA | 0 | NA | NA | 29 | NA |
| Xiaoming Li, 2020 [20] | NA | NA | NA | NA | NA | NA | NA | NA | NA | 75 |
| Adam Bernheim, 2020 [21] | NA | NA | 18 | 14 | 60 | 2 | NA | NA | 6 | NA |
| NG Ming-Yen, 2020 [22] | 3 | 8 | NA | NA | NA | NA | NA | NA | NA | NA |
| Yalei Shang, 2020 [23] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Michael Chung,2020 [24] | NA | NA | 1 | 2 | 15 | NA | NA | NA | 4 | NA |
| Isil Yurdaisik, 2020 [25] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Omar M Sultan, 2020 [26] | 4 | 16 | NA | NA | 67 | NA | NA | NA | 15 | NA |
| Lulu Gao, 2020 [27] | NA | NA | NA | NA | NA | NA | 2 | 4 | 1 | NA |
| Damiano Caruso, 2020 [28] | NA | NA | 4 | 2 | 52 | NA | NA | NA | 26 | 24 |
| Yueying Pan, 2020 [29] | NA | NA | 19 | 5 | 39 | NA | NA | NA | NA | NA |
| Cartocci Gaia, 2020 [30] | NA | NA | NA | NA | NA | NA | NA | NA | NA | 52 |
| Emre Pakdemirli, 2020 [31] | NA | NA | NA | NA | NA | 0 | NA | NA | 0 | 0 |
| Yan Li. 2020 [32] | NA | NA | NA | NA | NA | NA | NA | NA | NA | 36 |
| Youssriah Sabri, 2020 [33] | NA | NA | 34 | NA | 186 | 64 | NA | NA | 82 | NA |
| Rui Zhang, 2020 [34] | NA | NA | 43 | 24 | 56 | NA | NA | NA | 30 | 24 |
| Jie Zhan, 2020 [35] | NA | NA | 21 | 11 | 70 | NA | NA | NA | 37 | 60 |
| Xi Xu, 2020 [36] | 40 | 47 | 12 | 4 | 49 | NA | 7 | 62 | NA | NA |
| Jiong Wu, 2020 [37] | NA | NA | NA | NA | NA | NA | NA | NA | 23 | NA |
| Yang Li, 2020 [38] | NA | NA | NA | NA | NA | NA | NA | NA | 3 | AN |
| Zeying Wen, 2020 [39] | NA | NA | 16 | NA | 65 | NA | NA | NA | NA | NA |
| Pascal Lomoro [40] | NA | NA | 0 | 1 | 39 | NA | NA | NA | 24 | 11 |
| Omar M Albtoush, 2020 [41] | NA | NA | 29 | 13 | 75 | 19 | NA | NA | NA | NA |
| Yongxing Yun, 2020 [42] | NA | NA | NA | NA | NA | NA | NA | NA | NA | 67 |
| Chon M Le, 2020 [43] | NA | NA | 4 | 9 | 11 | NA | NA | NA | 1 | NA |
| Emine Uysal,2021 [44] | NA | NA | 15 | 5 | 28 | NA | NA | NA | 8 | NA |
| A Carvalho, 2020 [45] | NA | NA | 8 | 5 | 141 | 20 | NA | NA | 55 | NA |
(GGO = Ground Glass Opacity, NA = Not Available).
(RUL = Right Upper Lobe, RML = Right Middle Lobe, RLL = Right Lower Lobe, LUL = Left Upper Lobe, LLL = Left Lower Lobe).
(UL = Upper Lobe, LL = Lower Lobe).
According to pooled analysis of this systematic review the clinical features of COVID-19 were found with following percentages: GGO 71.64 %, mixed pattern 35.22 %, consolidation 29.15 %, pleural effusion 5.08 %, pleural thickening 38.25 %, lymphadenopathy 7.64 %, nodules 14.84 %, interlobular septal thickening 43.28 %, bronchial wall thickening 20.71 %, subpleural bands 52.54 %, traction bronchiectasis 20.36 %, vascular enlargement 65.41 %, RUL 60.39 %, RML 54.97 %, RLL 73.32 %, LUL 60.83 %, LLL 75.68 %, unilateral pneumonia 24.04 %, bilateral pneumonia 71.75 %, peripheral involvement 54.63 %, central involvement 11.45 %, mixed involvement 38.16 %, UL 22.60 %, LL 43.29 %, 1 lobe involvement 17.34 %, 2 lobes involvement 9.80 %, over 2 lobes involvement 68.66 %, reversed halo sign 14.98 %, single lesion 11.33 %, multiple lesions 74.67 %, crazy paving pattern 28.74 %, and air bronchogram 35.15 %.
The typical features of COVID-19 are GGO progressed into consolidation in peripheral areas of both lungs with the presentation of multiple lesions. Interlobular septal thickening, bronchial wall thickening, traction bronchiectasis, vascular enlargement, and pleural effusion were possible but atypical features of COVID-19. Lymphadenopathy, pleural effusion, air bronchogram, and reversed halo sign were uncommon.
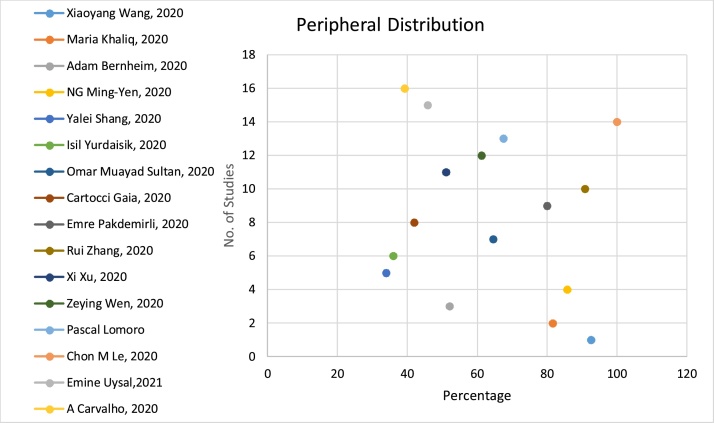
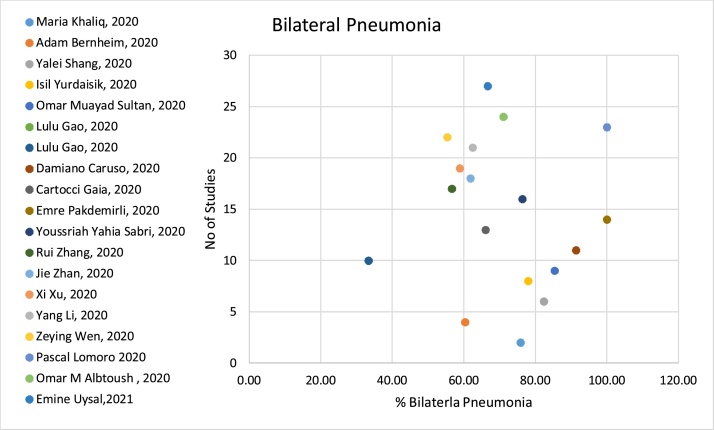
Fig. 2, Fig. 3, Fig. 4 gives a good visual description of the percentages of patients, who presented with GGO, mixed pattern, and consolidation on their CT-scan, respectively. Fig. 5, Fig. 6 present peripheral distribution and bilateral pneumonia, respectively.
Fig. 2.
Ground Glass Opacities.
Fig. 3.
Mixed Pattern.
Fig. 4.
Consolidation.
Fig. 5.
Peripheral Distribution.
Fig. 6.
Bilateral Pneumonia.
4. Discussion
2019-nCoV is a single-stranded RNA virus that has a natural flora in bats and spread to humans from the Seafood market in China [46,47]. Due to the human-to-human transmission through infected sneezing and coughing droplets of this infection infected millions of people around the globe [48]. Due to its rapid spread to different continents, this infection was declared a pandemic by WHO on 30−01-2020 [49]. This deadly coronavirus that showed a very high mortality rate is quite similar to highly virulent SARS as well as MERS coronaviruses as the treatment of this infection has not yet been discovered it is very important to adopt preventive measures to stop the transmission of this deadly virus. Along with the Precautionary measures to prevent the spread of Coronavirus (COVID-19) in people, the early detection is also very important for effective management. RT-PCR and CT-scan play a very crucial role in the detection of infection. The disadvantage of RT-PCR is that it takes several hours to produce the results with a sensitivity of sixty to seventy percent that is dependent on the quality of the sample [50] The COVID-19 has mostly affected middle-aged individuals [51] and the same pattern has been witnessed in our review where the mean age of infected individuals is 48.04 years. But in the early detection of COVID-19 chest computed tomography has proved its efficiency over other diagnostic tools on the basis of early characteristic presentation of novel COVID-19 [52]. As compared to RT-PCR the CT-scan has a sensitivity of 97 %, the specificity of 25 %, and accuracy of 68 % [53]. HR CT-scans help to detect the infection in the early days and provide comprehensive detail of patterns of parenchymal involvement in the lungs. On the follow-up CT-scans the radiologists can find the rapid spread of infection by highly evolving denser patterns of lung damage [54].
This systematic review presented that chest CT-scan is a helpful modality in the evaluation and management of SARS-CoV-2 infected patients. The most important clinical characteristic according to this review is GGO. Other important features in patients infected by SARS-CoV-2 included vascular enlargement, interlobular septal thickening, and air bronchogram. The imaging finding commonly manifested multiple lesions with bilateral involvement in peripheral areas of the lungs.
The most common classical finding in thoracic CT of SARS-CoV-2 infected patients was Ground Glass Opacities [55]. Meta-analysis conducted by Zarifian A. et al. [56], Bao C. et al. [57], Zheng Y. et al. [58], Zhu J. et al. [59], Zhou X. et al. [70], Homsi M. et al. [71], and Yang H. et al. [72] reported GGO to be 77.18 %, 83.31 %, 78 %, 68.1 %, 68 %, 71.70 %,and 79 % respectively. In our review, we also found the higher overall percentage (71.64 %) of GGO. According to included studies of Wang et al., Maria Khaliq. et al., Ming-Yen. et al., Shang. et al., Chung et al., Yudaisik. et al., Sultan. et al., Gao et al., Caruso. et al., Pan. et al., Gaia. et al., Sabri. et al., Zhang. et al., Zhan. et al., Xi Xu. et al., Wu. et al., Li et al., Omar M et al., Chon Le et al., Uysal E et al., and Carvalho A et al., GGO was reported in 77.8 %, 88.5 %, 86 %, 87 %, 57 %, 88 %, 94.3 %, 83.3 %, 100 %, 85.7 %, 88 %, 88.1 %, 93 %,65.4 %, 72 %, 91 %, 87 %, 97 %, 92 % and 62 % of patients respectively. Six studies of our review reported GGO in less than 50 % of patients: Li et al. 15 %, Bernheim et al. 34 %, Yan Li et al. 35.3 %, Wen et al., 28 %, Pascal L et al., 37.50 % and Yun Y et al., 44.30 %.
In severe cases of SARS-CoV-2 infections, GGO is accompanied with consolidation i.e., mixed pattern. In meta-analysis conducted by Bao C. et al., [57], Zhou X. et al. [70], Homsi M. et al. [71], and Yang H. et al. [72] the overall percentage of mixed pattern was reported as %, 58.42 %, 48 %, 46.6 % and 46 % respectively while in this review, overall incidence of mixed pattern was found to be 35.22 %.
Consolidation is a common finding in SARS-CoV-2 pneumonia [60,61]. Recent meta-analysis conducted by Zarifian A. et al. [56], Bao C. et al., [57], Zheng Y. et al. [58] and Zhu J. et al. [59] Zhou X. et al. [70], Homsi M. et al. [71], and Yang H. et al. [72] reported consolidation as 35.56 %, 43.97 %, 34 % and 32 %, 18 %,41.20 % and 34 % respectively. The overall percentage of consolidation seen in this review was 29.15 %. The air bronchogram important typical airway abnormality and radiological feature of COVID-19 [62] was found in 35.15 % patients in this meta-analysis. Meta-analysis conducted by Bao C. et al. [57], Zheng Y. et al. [58] and Zhu J. et al. [59] Zhou X. et al. [70], Homsi M. et al. [71], and Yang H. et al. [72] incidence of air bronchogram was 46.46 %,25 %, 44.70 %,39 %,50 %, and 41 % respectively.
In our review, the overall incidence of crazy cave pattern is observed in 24.47 % COVID-19 patients, while the recent meta-analysis conducted by Bao C. et al. [57], Zheng Y. et al. [58] and Zhu J. et al. [59] and Zhou X. et al. [70] showed pooled percentages as 14.81 %, 24 %, 35.6 % and 20 % respectively.
Sub-pleural bands is another typical radiological feature in SARS-CoV-2 infections, and was observed as 55.61 %, in our review while the meta-analysis conducted by Zheng Y. et al. 58 % of the patients developed sub-pleural bands during coronavirus disease [58].
Researchers reported that bilateral lung involvement was most commonly observed in SARS-CoV-2 disease while it mostly affected the peripheral areas of the lungs [63] and the same pattern was found in our study where 54.63 % patients had peripheral parenchyma lungs involved and bilateral pneumonia (71.75 %). Left Lower Lobe (LLL) was more involved as compared to Left Upper Lobe (LUL) [57]. It was found in the study of Pakdemirli et al. with percentage of 100. In some studies, RML was relatively uncommon to be involved [62] but in our review, we found the involvement of RML in (54.97 %) patients. The involvement of the lower lobes is more due to the effect of gravity and the same pattern was found in our studies where in 75.68 % and 73.56 % of patients have LLL and RLL involvement respectively. COVID-19 in significant percentage (68.66 %) infected more than two lobes and showed multiple lesions (74.67 %) in the peripheral areas (54.63 %) of the lungs, according to our review.
Interlobular septal thickening [37], bronchial wall thickening [61], airway dilatation [64], and blood vessels dilatation [65] are some of the prominent features of CT-scan of coronavirus infected patients. In our review, we found the interlobular septal thickening, bronchial wall thickening, airway dilatation, and blood vessels dilatation 43.28 %, 20.71 %, 20.36 %, and 65.41 %., respectively. Pleural effusion is one of the possible but atypical features of COVID-19 [66]. In our review, we found the overall percentage of (5.09 %).
Pleural thickening is more common in comparison to pleural effusion [14]. The overall percentage of pleural thickening is (38.25 %), according to our review. Lymphadenopathy and pleural effusion are an uncommon clinical feature of COVID-19 [67] and in our review, we found the overall percentage as 7.64 % and 5.09 %. Reversed halo sign is a possible but uncommon feature of COVID-19 [68] while in our review this sign was positive in (14.98 %) patients.
A study conducted by Bollineni V.R. et al. correlated the RT-PCR timing with CT-Scan. Out of 96 patients with negative RT-PCR, 69 were presenting with abnormal CT findings depicting viral pneumonia. 33 out of 96 with negative RT-PCR undergone repeat RT-PCR and 7 turned out to be positive and the mean time interval between baseline negative RT-PCR and positive RT-PCR was 3 ± 2 days with a range of 2–4 days. Chest CT is found to have high sensitivity and high negative predictive value as compared RT-PCR and can be used as an alternative tool for primary screening of COVID-19 patients. [69]
In conclusion COVID-19 is a novel disease that has affected millions of people across the country. The early detection of the disease is very important in controlling the spread of the disease and in this regard, the role of the thoracic computed tomography is very important based on the representation of radological features of the infection. Chest CT-scan is a helpful modality in the early detection and assessment of disease severity in COVID-19 patients. The GGO in the peripheral areas of lungs with multiple lesions is the characteristic pattern of COVID-19. The progression of the disease can also be assessed based on follow-up chest CT-scans.
Summary
The characteristic GGO seen in peripheral areas of both lungs is a classical pattern of SARS-CoV-2 infections.
Funding
This a systematic review, so we didn’t receive any funding for this study.
Informed consent
This is systematic review therefore there was no need of informed consent or approval from Institutional review board.
Ethical approval
Institutional Review Board approval was not required because this is systematic review.
Study subjects or cohorts overlap
This is systematic review, all the data for this study was obtained from previously reported studies.
Methodology
This is systematic Review-metanalysis based on PRISMA strategy.
Declaration of Competing Interest
There is no conflict of Interest among authors.
This is systematic review and this study don’t have any relationship with any company.
Contributor Information
Ahmed Ishfaq, Email: ahmed.ishfaq45@gmail.com.
Syed Muhammad Yousaf Farooq, Email: yousafgelani@gmail.com.
Amber Goraya, Email: amber.goraya@yahoo.com.
Muhammad Yousaf, Email: Muhammad.yousaf@rsmi.uol.edu.pk.
Syed Amir Gilani, Email: profgilani@gmail.com.
Aafia Kiran, Email: kiranchaudhrey@gmail.com.
Muhammad Ayoub, Email: ayubgulzar@gmail.com.
Akhter Javed, Email: akhtarjaveeduol28@gmail.com.
Raham Bacha, Email: dr.rahambacha@gmail.com.
References
- 1.Shi Y., Wang Y., Shao C., Huang J., Gan J., Huang X. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020;27:1451–1454. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giovanetti M., Benvenuto D., Angeletti S., Ciccozzi M. The first two cases of 2019‐nCoV in Italy: where they come from? J. Med. Virol. 2020;92(May(5)):518–521. doi: 10.1002/jmv.25699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paraskevis D., Kostaki E.G., Magiorkinis G., Panayiotakopoulos G., Sourvinos G., Tsiodras S. Full-genome evolutionary analysis of the novel corona virus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event. Infect. Genet. Evol. 2020;79(April):104212. doi: 10.1016/j.meegid.2020.104212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.W-j Guan, Z-y Ni, Hu Y., W-h Liang, C-q Ou, J-x He. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bai Y., Yao L., Wei T., Tian F., Jin D.-Y., Chen L. Presumed asymptomatic carrier transmission of COVID-19. J. Am. Med. Assoc. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Yu T. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;15(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. 395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Z., McGoogan M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 8.Liu H., Manzoor A., Wang C., Zhang L., Manzoor Z. The COVID-19 outbreak and affected countries stock markets response. Int. J. Environ. Res. Public Health. 2020;17(8):2800. doi: 10.3390/ijerph17082800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Han Y., Yang H. The transmission and diagnosis of 2019 novel coronavirus infection disease (COVID‐19): a Chinese perspective. J. Med. Virol. 2020;92(June(6)):639–644. doi: 10.1002/jmv.25749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song J., Wang H., Liu Y., Wu W., Dai G., Wu Z., Zhu P., Zhang W., Yeom K.W., Deng K. End-to-end automatic differentiation of the coronavirus disease 2019 (COVID-19) from viral pneumonia based on chest CT. Eur. J. Nucl. Med. Mol. Imaging. 2020;47(October(11)):2516–2524. doi: 10.1007/s00259-020-04929-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li M., Lei P., Zeng B., Li Z., Yu P., Fan B. Coronavirus disease (COVID-19): spectrum of CT findings and temporal progression of the disease. Acad. Radiol. 2020;5:603–608. doi: 10.1016/j.acra.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang H.-W., Yu J., Xu H.-J., Lei Y., Pu Z.-H., Dai W.-C. Corona virus international public health emergencies: implications for radiology management. Acad. Radiol. 2020;4:463–467. doi: 10.1016/j.acra.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AM. J. Roentgenol. 2020;215:87–93. doi: 10.2214/AJR. [DOI] [PubMed] [Google Scholar]
- 15.Li X., Zeng X., Liu B., Yu Y. COVID-19 infection presenting with CT halo sign. Radiol. Cardiothoracic Imaging. 2020;2 doi: 10.1148/ryct.2020200026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.JF-W Chan, Yuan S., Kok K.-H., KK-W To, Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pan F., Ye T., Sun P. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020;295(3):715–721. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang X., Liu C., Hong L., Yuan C., Ding J., Jia Q. CT findings of patients infected with SARS-CoV-2. BMC Med. Imaging. 2020;20:1–6. doi: 10.1186/s12880-020-00471-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khaliq M., Raja R., Khan N., Hanif H.J.C. An analysis of high-resolution computed tomography chest manifestations of COVID-19 patients in Pakistan. Cureus. 2020;12:e9373. doi: 10.7759/cureus.9373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li X., Zeng W., Li X., Chen H., Shi L., Li X. CT imaging changes of corona virus disease 2019 (COVID-19): a multi-center study in Southwest China. J. Transl. Med. 2020;18:1–8. doi: 10.1186/s12967-020-02324-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020 doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ng M.-Y., Lee E.Y., Yang J., Yang F., Li X., Wang H. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol. Cardiothoracic Imaging. 2020;2 doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shang Y., Xu C., Jiang F., Huang R., Li Y., Zhou Y. Clinical characteristics and changes of chest CT features in 307 patients with common COVID-19 pneumonia infected SARS-CoV-2: a multicenter study in Jiangsu, China. Int. J. Infect. Dis. 2020;96:157–162. doi: 10.1016/j.ijid.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yurdaisik I., Nurili F. Evaluation of chest CT findings in 50 Coronavirus disease 2019 (COVID-19) patients treated in Turkey. Cureus. 2020;12 doi: 10.7759/cureus.8252. [DOI] [Google Scholar]
- 26.Sultan O.M., Al-Tameemi H., Alghazali D.M., Abed M., Ghniem M.N.A., Hawiji D.A. Pulmonary ct manifestations of COVID-19: changes within 2 weeks duration from presentation, Egypt. J. Radiol. Nucl. Med. 2020;51:1–7. doi: 10.1186/s43055-020-00223-0. [DOI] [Google Scholar]
- 27.Gao L., Zhang J., Research C. Pulmonary high-resolution computed tomography (HRCT) findings of patients with early-stage coronavirus disease 2019 (COVID-19) in Hangzhou, China. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.923885. e923885-923881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Caruso D., Zerunian M., Polici M., Pucciarelli F., Polidori T., Rucci C. Chest CT features of COVID-19 in Rome, Italy. Radiology. 2020;296:79–85. doi: 10.1148/radiol.2020201237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pan Y., Guan H., Zhou S., Wang Y., Li Q., Zhu T. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur. Radiol. 2020;30:3306–3309. doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cartocci G., Colaiacomo M.C., Lanciotti S., Andreoli C., De Cicco M.L., Brachetti G. Chest CT for early detection and management of coronavirus disease (COVID-19): a report of 314 patients admitted to emergency department with suspected pneumonia. Radiol. Med. 2020;125:931–942. doi: 10.1007/s11547-020-01256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pakdemirli E., Mandalia U., Monib S. Positive chest CT features in patients with COVID-19 pneumonia and negative real-time polymerase chain reaction test. Cureus. 2020;12:e9942. doi: 10.7759/cureus.9942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li Y., Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am. J. Roentgenol. 2020;214:1280–1286. doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- 33.Sabri Y.Y., Nassef A.A., Ibrahim I.M.H., Abd El Mageed M.R., Khairy CT chest for COVID-19, a multicenter study—experience with 220 Egyptian patients, Egypt. J. Radiol. Nucl. Med. 2020;51:1–15. doi: 10.1186/s43055-020-00263-6. [DOI] [Google Scholar]
- 34.Zhang R., Ouyang H., Fu L., Wang S., Han J., Huang K. CT features of SARS-CoV-2 pneumonia according to clinical presentation: a retrospective analysis of 120 consecutive patients from Wuhan city. Eur. Radiol. 2020;30:4417–4426. doi: 10.1007/s00330-020-06854-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhan J., Li H., Yu H., Liu X., Zeng X., Peng D. 2019 novel coronavirus (COVID-19) pneumonia: CT manifestations and pattern of evolution in 110 patients in Jiangxi, China. Eur. Radiol. 2020;31(2):1059–1068. doi: 10.1007/s00330-020-07201-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu X., Yu C., Qu J., Zhang L., Jiang S., Huang D. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur. J. Nucl. Med. Mol. Imaging. 2020;47:1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu J., Wu X., Zeng W., Guo D., Fang Z., Chen L. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Invest. Radiol. 2020;55:257–261. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li Y., Cao J., Zhang X., Liu G., Wu X., Wu B. Chest CT imaging characteristics of COVID-19 pneumonia in preschool children: a retrospective study. BMC Pediatr. 2020;20:1–8. doi: 10.1186/s12887-020-02140-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wen Z., Chi Y., Zhang L., Liu H., Du K., Li Z. Coronavirus disease 2019: initial detection on chest CT in a retrospective multicenter study of 103 Chinese subjects. Radiol. Cardiothoracic Imaging. 2020;2 doi: 10.1148/ryct.2020200092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lomoro P., Verde F., Zerboni F., Simonetti I., Borghi C. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur. J. Radiol. Open. 2020;7(January):100231. doi: 10.1016/j.ejro.2020.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Albtoush O.M., Al-Shdefat R.B., Al-Akaileh A. Chest CT scan features from 302 patients with COVID- 19 in Jordan. Eur. J. Radiol.Open. 2020;7(January):100295. doi: 10.1016/j.ejro.2020.100295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yun Y., Wang Y., Hao Y., Xu L., Cai Q. The time course of chest CT lung changes in COVID-19 patients from onset to discharge. Eur. J. Radiol.Open. 2021;8(January):100305. doi: 10.1016/j.ejro.2020.100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ieong Cm, Xu X., Kong Sc, Luo L. Evaluation of chest CT and clinical features of COVID-19 patient in Macao. Eur. J. Radiol.Open. 2020;7(January):100275. doi: 10.1016/j.ejro.2020.100275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Uysal E., Kilinçer A., Cebeci H., Özer H., Demir N.A., Öztürk M., Koplay M. Chest CT findings in RT-PCR positive asymptomatic COVID-19 patients. Clinl. Imaging. 2021;77(September):37–42. doi: 10.1016/j.clinimag.2021.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carvalho A., Cunha R., Lima B.A., Pereira J.M., Madureira A.J. Chest CT imaging features of COVID-19 pneumonia: first radiological insights from Porto, Portugal. Eur. J. Radiol.Open. 2020;7(January):100294. doi: 10.1016/j.ejro.2020.100294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lei H., Li Y., Xiao S., Lin C., Norris S., Wei D. Routes of transmission of influenza A H1N1, SARS CoV, and corna virus in air cabin: comparative analyses. Int. J. Ind. Env. Health. 2018;28:394–403. doi: 10.1111/ina.12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Otter J.A., Donskey C., Yezli S., Douthwaite S., Goldenberg S., Weber D.J. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. Can. J. Infect. Control. 2016;92:235–250. doi: 10.1016/j.jhin.2015.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chan J.F., Yuan S., Kok K.H., To K.K., Chu H., Yang J., Xing F., Liu J., Yip C.C., Poon R.W., Tsoi H.W. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.E.J.B.B.M.J. Mahase China coronavirus: WHO declares international emergency as death toll exceeds 200. Brit. Med. J. 2020:368. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- 50.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W., Tao Q., Sun Z., Xia L.J.R. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020:200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klopfenstein T., Toko L., Royer P.-Y., Lepiller Q., Gendrin V., S.J.M.E..M.I. Zayet Features of anosmia in COVID-19. Med. Et Malad. Infect. 2020 doi: 10.1016/j.medmal.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hani C., Trieu N.H., Saab I., Dangeard S., Bennani S., Chassagnon G., Revel M.-P.J.D. Imaging, i., COVID-19 pneumonia: a review of typical CT findings and differential diagnosis. Diag. Intv. Imag. 2020 doi: 10.1016/j.diii.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P., Ji W.J.R. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020:200432. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J., Fan Y., C.J.T.L.I.D. Zheng Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Himoto Y., Sakata A., Kirita M., Hiroi T., Kobayashi K.I., Kubo K., Kim H., Nishimoto A., Maeda C., Kawamura A., Komiya N. Diagnostic performance of chest CT to differentiate COVID-19 pneumonia in non-high-epidemic area in Japan. Jpn. J. Radiol. 2020;38:400–406. doi: 10.1007/s11604-020-00958-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zarifian A., Nour M.G., Rezayat A.A., Oskooei R.R., Abbasi B., Sadeghi R. Chest CT findings of coronavirus disease 2019 (COVID-19): a comprehensive meta-analysis of 9907 confirmed patients. Clin. Imag. 2021;1:101–110. doi: 10.1016/j.clinimag.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bao C., Liu X., Zhang H., Li Y., Liu J. Coronavirus disease 2019 (COVID-19) CT findings: a systematic review and meta-analysis. J. Am. Coll. Radiol. 2020;17:701–709. doi: 10.1016/j.jacr.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zheng Y., Wang L., Ben S. Meta‐analysis of chest CT features of patients with COVID‐19 pneumonia. J. Med. Viro. 2021;93:241–249. doi: 10.1002/jmv.26218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhu J., Zhong Z., Li H., Ji P., Pang J., Li B., Zhang J. CT imaging features of 4121 patients with COVID‐19: a meta‐analysis. J. Med. Viro. 2020;92:891–902. doi: 10.1002/jmv.25910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Duzgun S.A., Durhan G., Demirkazik F.B., Akpinar M.G., O.M.J.I.I..I. Ariyurek COVID-19 pneumonia: the great radiological mimicker. Insg. Imag. 2020;11:1–15. doi: 10.1186/s13244-020-00933-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li K., Wu J., Wu F., Guo D., Chen L., Fang Z., Li C.J.I.R. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest. Radiol. 2020 doi: 10.1097/RLI.0000000000000672. https://dx.doi.org/10.1097%2FRLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tabatabaei S.M.H., Talari H., Moghaddas F., Rajebi H.J.R.C.I. Computed tomographic features and short-term prognosis of coronavirus disease 2019 (COVID-19) pneumonia: a single-center study from Kashan, Iran. Radiol. Cardiothoracic Imaging. 2020:2. doi: 10.1148/ryct.2020200130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kanne J.P. Chest CT findings in 2019 novel coronavirus (2019-nCoV) infections from Wuhan, China: key points for the radiologist. Radiology. 2020 doi: 10.1148/radiol.2020200241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Henkel M., Weikert T., Marston K., Schwab N., Sommer G., Haslbauer J., Franzeck F., Anastasopoulos C., Stieltjes B., Michel A.J.R.C.I. Lethal COVID-19: Radiological-Pathological Correlation of the Lungs. Radiology. 2020;2 doi: 10.1148/ryct.2020200406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lang M., Som A., Carey D., Reid N., Mendoza D.P., Flores E.J., Li M.D., Shepard J.A., Little B.P. Pulmonary vascular manifestations of COVID-19 pneumonia. Radiol. Cardiothoracic Imaging. 2020;2 doi: 10.1148/ryct.2020200277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhou S., Wang Y., Zhu T., Xia L. CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, China, AJR Am. J.Roentgenol. 2020;214:1287–1294. doi: 10.2214/AJR.20.22975. [DOI] [PubMed] [Google Scholar]
- 67.Zuo H. Contribution of CT features in the diagnosis of COVID-19. Can. Respir. J. 2020;2020 doi: 10.1155/2020/1237418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shaghaghi S., Daskareh M., Irannejad M., Shaghaghi M., Kamel I. Target-shaped combined halo and reversed-halo sign, an atypical chest CT finding in COVID-19. Clin. Imaging. 2020;69:72–74. doi: 10.1016/j.clinimag.2020.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rao Bollineni V., Nieboer K.H., Döring S., Buls N., de Mey J. The role of CT imaging for management of COVID-19 in epidemic area: early experience from a University Hospital. Insights Imag. 2021;12:1–5. doi: 10.1186/s13244-020-00957-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhou X., Pu Y., Zhang D., Xia Y., Guan Y., Liu S., Fan L. CT findings and dynamic imaging changes of COVID-19 in 2908 patients: a systematic review and meta-analysis. Acta radiol. 2021;(February) doi: 10.1177/0284185121992655. 0284185121992655. https://doi.org/10.1177%2F0284185121992655. [DOI] [PubMed] [Google Scholar]
- 71.El Homsi M., Chung M., Bernheim A., Jacobi A., King M.J., Lewis S., Taouli B. Review of chest CT manifestations of COVID-19 infection. Eur. J. Radiol.Open. 2020;7(January):100239. doi: 10.1016/j.ejro.2020.100239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yang H., Lan Y., Yao X., Lin S., Xie B. The chest CT features of coronavirus disease 2019 (COVID-19) in China: a meta-analysis of 19 retrospective studies. Virol. J. 2020;17(December(1)):1–7. doi: 10.1186/s12985-020-01432-9. [DOI] [PMC free article] [PubMed] [Google Scholar]