Abstract
Rationale:
Quantitative health disparities research has increasingly employed intersectionality as a theoretical tool to investigate how social characteristics intersect to generate health inequality. Yet, intersectionality was not designed to quantify, predict, or identify health disparities, and, as a result, multiple criticisms against its misapplication in health disparities research have been made. As such, there is an emerging need to evaluate the growing body of quantitative research that aims to investigate health disparities through an intersectional lens.
Methods:
We conducted a systematic review from earliest records to January 2020 to (i) describe the scope of limitations when applying intersectionality to quantitative health disparities research, and (ii) identify recommendations to improve the future integration of intersectionality with this scholarship. We identified relevant publications with electronic searches in PubMed and CA Web of Science. Studies eligible for inclusion were English-language publications that used quantitative methodologies to investigate health disparities among adults in the U.S. while explicitly claiming to adopt an intersectional perspective. Out of 1,279 articles reviewed, 65 were eligible for inclusion.
Results:
Our review found that, while the value of intersectionality to the study of health disparities is evident, the existing research struggles with meeting intersectionality’s fundamental assumptions. In particular, four limitations were found to be widespread: narrowing the measurements of intersectionality, intersectional groups, and health outcomes; placing primacy on the study of certain intersectional groups to the neglect of others; overlooking underlying explanatory mechanisms that contribute to the health disparities experienced by intersectional groups; and, lacking in the use of life-course perspectives to show how health disparities vary across different life stages.
Conclusion:
If the goal of health equality is to be achieved among diverse intersectional groups, future research must be assisted by the collection and examination of data that overcomes these limitations.
Keywords: Intersectionality, Quantitative Methods, Health Disparities, Race/Ethnicity, Gender, Socioeconomic Status, Social Determinants of Health, Health Equity
1. INTRODUCTION
Despite substantial improvements in medical technology and disease prevention over the past decades, health disparities persist across social lines. Those in marginalized groups defined by social characteristics—sex/gender, race/ethnicity, socioeconomic status, and sexual orientation, among others—continue to experience elevated risks of chronic conditions and poor mental and physical health domestically and globally (World Health Organization 2011). Life-course perspectives highlight how these marginalized groups are disproportionately subjected to an accumulating series of health-damaging risks and inaccessibility to health-promoting resources beginning early in life (DiPrete and Eirich 2006). In turn, this places marginalized groups on a trajectory of deteriorating health earlier in life compared to their non-marginalized counterparts, with evidence, albeit mixed, suggesting that some health disparities may widen with age (Ferraro and Farmer 1996). In the quest for health equality, such glaring health disparities have illuminated the need for a more comprehensive understanding of the social determinants of health rooted in these characteristics.
Recently, scholars have acknowledged intersectionality, with its focus on how multiple systems of oppression (e.g., racism, sexism, classism, and heterosexism) are co-produced (Collins 1991), as being particularly well-suited to the study of health disparities. Indeed, intersectionality has enjoyed rapid theoretical expansion and popularity, earning the reputation of being the “most important theoretical contribution that women’s studies, in conjunction with related fields, has made so far” (McCall 2005: 1771). Intersectionality emerged in academic discourse shortly after the rise of 1960s-1980s U.S. Black feminism and its criticisms of prior feminist and antiracist movements that overlooked the interests of Black women. That is, feminist discourse tended to cater to concerns of White middle-class women while antiracist discourse primarily served the interests of Black men. Intersectionality, with its focus on how multiple systems of oppression mutually construct one another to produce unique adversities, seemed a fitting response to the inadequacy of prior social movements to delineate the social inequalities experienced by Black women (Collins 1991).
Since the 1960s, the core tenets of intersectionality have been applied by numerous social justice movements. The Combahee River Collective (1977), for example, released a landmark statement widely recognized as the first writing to criticize the interlocking systems of oppression that shape the lives and identities of Black women. Yet, the term wasn’t introduced in academic circles until legal and critical race scholar Kimberle Crenshaw (1991) coined it to illuminate the need for an “intersectional” theoretical framework for addressing violence against Black women. Since then, its development has been guided by several core features, including its emphasis on multiple and interlocking social identities; a paradigmatic shift away from attempts to parse out social identities to understand lived experience; and the notion that social identities are fluid, shifting, and mutually constructing, as well as embedded in their corresponding macro power structures and processes (Else-Quest and Hyde 2016a; Hankivsky 2012). With this foundation, intersectionality has been recognized as a fruitful theoretical and analytic strategy for social inequality research (Choo and Ferree 2010).
In applying intersectionality to the study of population health, Bowleg (2012) offered five ways that an intersectional framework can advance health disparities research:
Intersectionality offers a unifying linguistic and conceptual framework for researchers interested in studying how multiple social statuses shape health.
It encourages researchers to conceptualize and analyze the complex social inequalities that the most disadvantaged social groups in society endure.
The framework illuminates the insidious ways in which macro power structures, rather than operating in isolation, intertwine to get “under the skin” and generate glaring health disparities above and beyond individual-level factors.
Research that incorporates intersectionality can inform population-level interventions and policy changes to address the health needs of historically oppressed groups.
By encouraging data collection on health and supporting the analysis of intersecting social statuses beyond simply sex/gender and race/ethnicity, the framework facilitates a more nuanced analysis of health disparities.
The applicability of an intersectional perspective to health disparities research is made evident by several reviews that frame intersectionality as a valuable tool to study how intersecting statuses shape health (e.g., Bauer and Scheim 2019a; Bowleg 2012; Green, Evans, and Subramanian 2017; Hankivsky 2012; Viruell-Fuentes, Miranda, and Abdulrahim 2012). A search conducted through PubMed is rather telling in this regard. Using keywords relevant to intersectionality and health disparities for publications before 2010 yielded only eight results. Of these eight publications, only three were empirical research articles; the remaining five were theoretical or conceptual pieces offering insights about the integration of intersectionality and health research. An identical PubMed search for studies published in 2010 or after, however, returned 300 articles. An emerging body of intersectional health research is now well-established, although much of it is qualitative (Bauer 2014).
The development of intersectionality in quantitative health disparities research has been slow, however. Although recommendations now exist on how to quantitatively model intersectionality (for example, see Bauer and Scheim 2019a; Else-Quest and Hyde 2016b; Evans et al. 2018), there has been little consensus as to whether it is possible to quantify the complexities of intersectionality. In fact, other scholars have speculated that quantitative health research may not be well-suited to incorporating intersectionality because it is a conceptual framework that was not initially designed to quantify, predict, or describe health outcomes. This issue, as scholars have noted (Bowleg 2008; McCall 2005), may lie in intersectionality’s apparent incompatibility with positivism, the epistemology that undergirds much quantitative health research. While positivism asserts that a sole “true” and objective reality can be discovered through well-designed and value-neutral research, intersectionality illuminates the many socially constructed realities that those who inhabit various intersections experience (Bowleg 2008, 2012). As a result, multiple scholars have urged caution against the misuse or misapplication of intersectionality in quantitative research and have even suggested that such methodologies may need to be reimagined to truly examine the forces generating inequality among multiply marginalized groups (Bauer and Scheim 2019a; Bowleg 2016; Green et al. 2017; McCall 2005).
These criticisms form the foundation of multiple limitations in quantitative intersectional health research (Bowleg 2012; Else-Quest and Hyde 2016a, 2016b). These limitations primarily stem from misunderstandings regarding how to properly apply intersectionality’s theoretical assertions to quantitative methodologies. One overarching concern lies in problematic and narrow operationalizations of the intersectional groups under investigation, intersectionality, and the health outcomes of interest. For example, binary measures of social statuses (e.g., Black vs. non-Black) are antithetical to intersectionality insofar as they fail to reflect the fluid and dynamic nature of intersectional identities (Choo and Ferree 2010; McCall 2005). Yet another major limitation concerns the elements of intersectionality that are needed to classify as a true intersectional inquiry in a quantitative research design. Specifically, there appears to be a preference for studying race/ethnicity and sex/gender while other intersectional groups defined by sexual orientation, age, nativity/immigrant status, and other social characteristics have received less attention (Hankivsky 2012; Hankivsky and Grace 2015).
Other limitations concern attending to the underlying explanatory mechanisms that contribute to the poor health of intersectional groups across the life course, such as exposure to life adversities in childhood and adulthood (Bauer 2014; Else-Quest and Hyde 2016a). This problem occurs, at least in part, because mediation analysis in quantitative health disparities research may not be adequately identifying key explanatory mechanisms that lead to poor health for intersectional groups even though mediation is a critical feature of health disparities research (Naimi et al. 2016).
While multiple investigators have repeatedly called attention to these issues, there has not yet been a systematic attempt to determine how pervasive these limitations are in the literature. As a result, it remains unclear whether this budding body of scholarship has done justice to intersectionality by adhering to its foundational assertions. Does the existing body of intersectional quantitative scholarship on health disparities truly address the interrelatedness of multiple intersecting identities, health disparities within and across intersectional groups throughout the life course, and the relevant power-laden explanatory mechanisms responsible for generating such inequity?
To answer this question, we conduct a systematic review of quantitative health disparities research that explicitly uses an intersectional perspective. Our focus is not on empirical findings. Rather, because intersectionality’s application in quantitative health disparities research is in its nascent stages, we aim to highlight limitations that may be slowing the development of intersectionality in this literature. A systematic review is suited for pinpointing these limitations because of its ability to provide a transparent and objective evaluation of the current state of the literature and to identify patterns and trends across multiple studies (Egger, Davey, and O’Rourke 2001). Furthermore, systematic reviews are appropriate when a body of research is still in its early stages of development to identify any weaknesses where improvements are needed as well as recommendations for future research directions (Petticrew and Roberts 2006).
2. METHODS
Following best practices for reporting systematic reviews on health, the present review follows the PRISMA guidelines (see Supplementary Table S1). This systematic review was conducted by both authors who worked together to identify which publications were eligible for review and what data should be extracted from the sample of eligible publications (Johnson and Hennessey 2019).
2.1. Inclusion Criteria
Four inclusion criteria were used to screen for eligible studies. First, we included studies that utilized a quantitative methodology, such as multivariate regression or multilevel modeling. Second, studies had to explicitly reference “intersectionality” (or variations of the term) in the article title, abstract, and/or body of text as guiding their analysis. Third, we included studies published in English that used data based in the United States, with a majority of the U.S. sample comprising those who are at least 18 years of age. It is difficult to synthesize the international literature on this topic because the foundational tenets underlying intersectionality differ across sociohistorical contexts (Hulko 2009; Kerner 2012). For instance, in Germany, there is no consensus whether race, ethnicity, nationality, and religion should be combined to describe the experience of racism or whether these should be considered separate characteristics representing discrete forms of oppression (Kerner 2012). In a U.S. context, however, these characteristics serve as the basis for distinct aspects of a person’s intersectional location and experiences with oppression. This issue has led some scholars to conclude that, in European contexts, there is “no consensus about what adequate theoretical accounts of intersectionality … should look like” (Kerner 2012: 203).
Second, developmental factors significantly differentiate the way intersectional identities are experienced by children/adolescents versus adults. The developmental change and identity exploration youth experience indicate that this age group’s intersectional social location is highly malleable and subject to change. Processes that youth often undergo such as racial/ethnic socialization and acculturation can instill multiple and conflicting identities that fluctuate over time (Narvaez et al. 2009). In fact, Erikson (1968) characterized adolescence as a time of “identity crisis” whereby some individuals are wholly unclear about who they are and who they would like to be. One’s identification with a particular intersectional social location is therefore unlikely to stabilize for some individuals until adulthood (Schwartz et al. 2013). Thus, since the very definition of intersectionality varies across culture and age, we include only those studies conducted on U.S. adults to ensure some degree of uniformity across studies. Finally, we only included studies where a specified outcome was specifically related to a health condition, issue, or diagnosis.
2.2. Health Disparity
Growing interest in the concepts of “health disparity” and “health inequality” has not led to a consensus on how either term is defined (Carter-Pokras and Baquet 2002). To bring some clarity and specificity to these terms, we rely on the definition outlined in Healthy People 2020. We define a health disparity as “a particular type of health difference that is closely linked with social or economic disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater social or economic obstacles to health based on their racial or ethnic group, religion, socioeconomic status, sex/gender, mental health, cognitive, sensory, or physical disability, sexual orientation, geographic location, or other characteristics historically linked to discrimination or exclusion” (U.S. Department of Health and Human Services 2008: 28). We favor this definition because 1) it dovetails with intersectionality’s emphasis on multiple social characteristics and 2) its scope includes any disease or illness.
2.3. Intersectionality
We employ McCall’s (2005) three distinct operationalizations of intersectionality: intercategorical, intracategorical, and anticategorical complexity approaches. We identify the reviewed publications as using one or a combination of these approaches according to a two-step procedure. First, if the authors explicitly claimed to adopt a particular approach, they were categorized as such. We checked whether such claims aligned with McCall’s description. Second, if no claim was made, we categorized the study using the following definitions. The intercategorical approach, the most commonly used in health disparities research (Green et al. 2017), involves systematic comparisons of various inequalities between groups defined by social position and identity. This approach takes as its departure point the a priori assumption that inequalities between well-defined social groups exist and such inequalities should be identified and investigated. Having somewhat of a “natural fit” with quantitative health disparities research, this approach takes shape in one of two ways. First, a full set of dummy variables can be used to represent particular intersectional locations. For example, using the nexus of race and gender, one can create four race–gender intersectionality statuses. Second, researchers may regress a host of main and/or interactional effects of two or more social statuses on a health outcome. A prototypical example of this is found in the study by Brown and Hargrove (2013) who regressed main effects of race/ethnicity and gender on health in addition to specifying models including gender × race/ethnicity interactions. The underlying assumption is that the interactional effects (being both Mexican-American and a woman) should more adequately capture how intersectional group membership effects health compared to the effects of separate social characteristics (being Mexican-American and also being a woman).
The intracategorical complexity approach focuses on the richness of within-group differences. Thus, it is those “particular social groups at neglected points of intersection” that shape the center of analysis (McCall 2005: 1774). We categorized studies as intracategorical if the primary focus was on a subpopulation and within-group health heterogeneity at one or more marginalized intersectional locations. For example, Pérez and colleagues (2018) focused exclusively on Black adults and investigated health variation at two intersectional locations (sex/gender and sexual orientations).
Lastly, the anticategorical complexity approach’s primary goal is the problematization and deconstruction of social categories altogether because “a wide range of different experiences, identities, and social locations fail to fit neatly” into a sole category (McCall 2005: 1777). The anticategorical approach critiques social categorization schemes since they fail to acknowledge the rich diversity found within social groups and can reify an inequitable social hierarchy where some groups are afforded more status and privilege than others. It should be noted that the anticategorical approach is the most critical of social categories defined by race/ethnicity, sex/gender, and other social characteristics that form the core foci of intersectionality. Therefore, this approach is the least amenable to health disparities researchers wishing to adopt an intersectional lens. Although one study (Persmark et al. 2019) explicitly claims to use the anticategorical approach, we found that social categories undergird the analyses in all of the studies in our sample; that is, none of the reviewed publications are truly anticategorical in the way that McCall (2005) describes.
2.4. Search Strategy and Data Extraction
To identify relevant studies, we searched for English-only articles published at any time through our latest search (January 2020) on both PubMed/Medline and Clarivate Analytics (CA) Web of Science (including Science Citation Index Expanded, Social Sciences Citation Index, Arts and Humanities Citation Index, and Emerging Sources Citation Index). For our PubMed search, we employed both Medical Subject Heading (MeSH) terms and free keywords to identify relevant published articles (see Supplementary Table S2). Some examples of terms and keywords related to health disparities were health status disparity, minority health, social determinants of health, and health inequality. To ensure articles utilized an intersectional theoretical framework, we also used intersectionality, intersectional, and intersectionalities as keywords. Finally, we included MeSH terms and keywords for a variety of terms related to health conditions, ranging from specific terms like alcohol to cardiovascular as well as more general terms like chronic disease and illness. This search returned 303 abstracts. When we conducted a similar search in CA Web of Science with relevant Boolean operators, 976 abstracts were returned. We removed 197 publications after determining they were duplicates. Subsequently, we carefully screened each title and abstract according to the aforementioned criteria. In total, our PubMed/Medline and CA Web of Science searches returned 51 relevant studies that met all criteria (see Figure 1). In situations where researchers have difficulty locating studies, screening reference lists is a useful way to reduce the chance of missing relevant publications (Horsley, Dingwall, and Sampson 2011). While screening references of the search-identified articles, we found an additional 14 studies that were not indexed by either the PubMed/Medline or CA Web of Science databases because they were published in niche journals with limited resources for indexation.
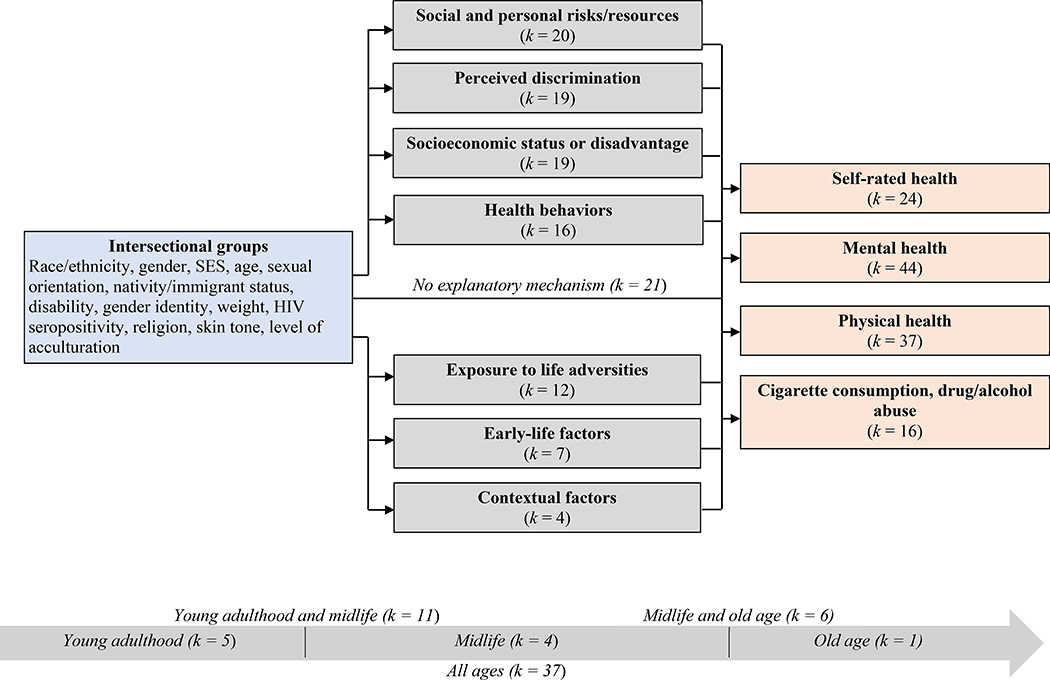
Fig. 1.
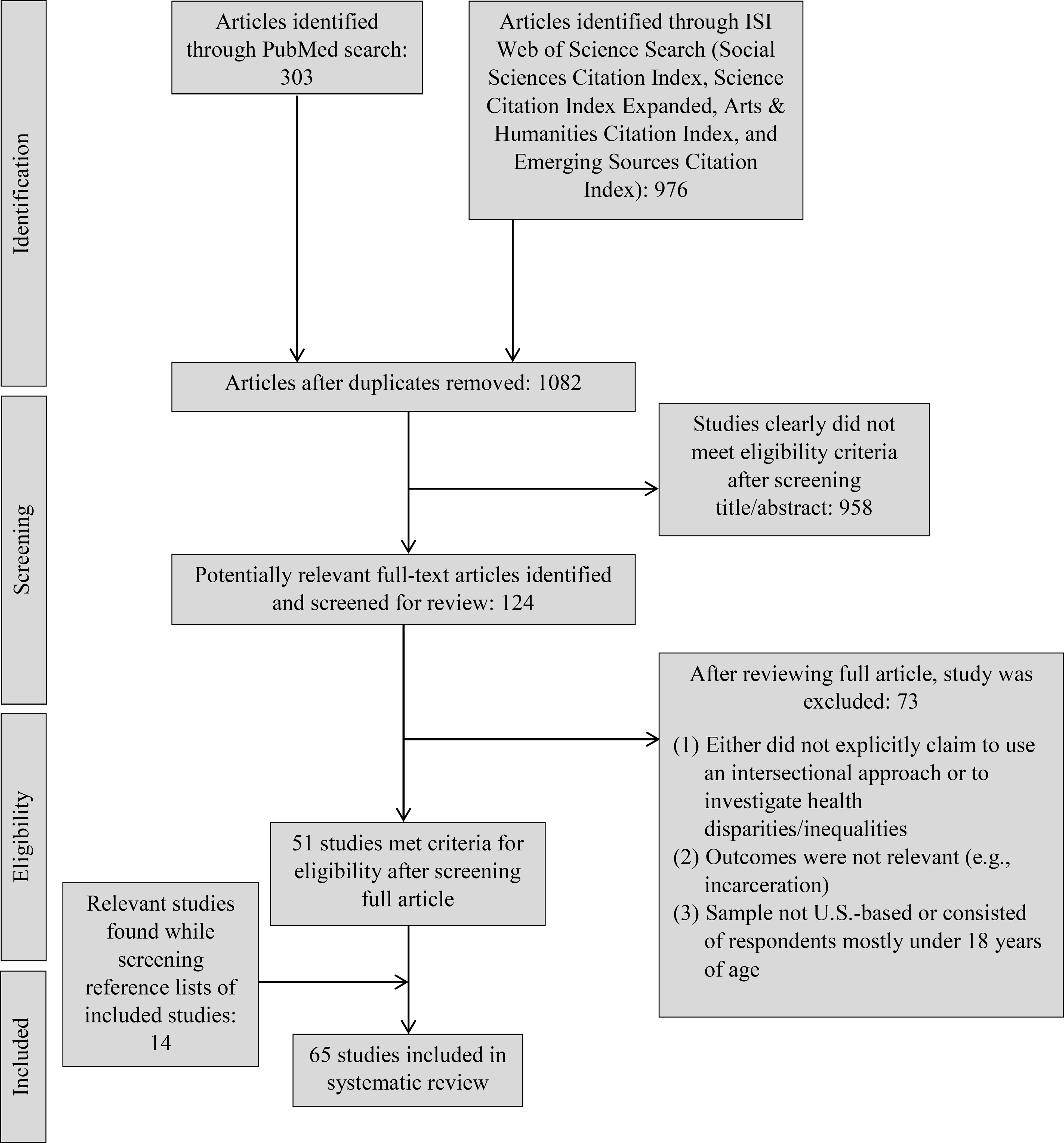
Flow of studies into the review.
Data were extracted based on the previously mentioned concerns regarding intersectionality’s application to this body of literature. The following information was extracted from each study: the study design (cross-sectional or longitudinal), characteristics of the sample (e.g., sufficient to cover different stages of the life course and subpopulation), the operationalization of intersectionality, the specific intersectional/reference groups, health outcomes, and explanatory mechanisms. Extraction of these data covers a wide range of potential theoretical and methodological limitations that may be affecting intersectionality’s development in quantitative health disparities scholarship.
2.5. Risk of Bias Assessment
Following recommendations by Johnson and Hennessey (2019), we use a previously established framework to evaluate the quality of each study. We used relevant criteria from Petticrew and Roberts’ (2006) framework, commonly used for appraising quantitative survey research (see Supplementary Table S3). We chose this framework because the reviewed studies utilize a questionnaire/survey design to obtain data. However, this systematic review focuses on an evaluation of intersectionality’s application to quantitative health disparities research rather than the specific design used. As such, we removed appraisal criteria that applied only to the quality of the study design and were therefore irrelevant to the objective of our review. The excluded criteria pertain to how the survey/questionnaire was carried out, the response rate, information about the denominator, and descriptions and appropriateness of statistical tests and post-hoc analyses. With these excluded, the framework offers 10 appraisal criteria to evaluate the quality of publications pertaining to adequate descriptions and appropriateness of the overall survey/questionnaire, sample, data, and measures.
We created a three-tiered scoring system (‘Good,’ ‘Fair,’ ‘Poor’) according to whether the study met each of the 10 appraisal criteria to indicate its overall quality. All studies earned a ‘good’ or ‘fair’ rating, leading us to conclude that were no errors significant enough to warrant a study’s removal due to trustworthiness of the study or interpretation of its results.
2.6. Analytic Approach
In reporting our findings, we perform a narrative review of the extracted data from all reviewed publications. Such a qualitative presentation of findings is appropriate when the purpose of the review is on theory development in a particular body of literature (Johnson and Hennessey 2019). We structure our findings based on different components of each study where limitations are likely to arise based on concerns previously voiced in the literature: (i) the study design and sample characteristics, (ii) the operationalization of intersectionality, (iii) the intersectional and reference groups, (iv) health outcomes, and (v) explanatory mechanisms. Following recommendations made by Petticrew and Roberts (2006), we synthesized each of these components from all reviewed studies in Table S4. For a more accessible viewing of these findings, Table 1 offers the five most frequently investigated health outcomes and explanatory mechanisms and Figure 2 provides a conceptual overview of all reviewed studies. Below, we summarize the results of Table S4, making sure to provide sufficient descriptions of any challenges/limitations that directly bear on intersectionality’s application to this body of research.
Table 1.
Five Most Commonly Studied Explanatory Mechanisms and Health Outcomes
| Explanatory mechanisms | No. of citing studies | Health outcomes | No. of citing studies |
|---|---|---|---|
| Social and personal risks/resources | 20 | Self-rated health or health-related quality of life | 24 |
| Perceived discrimination | 19 | Depressive symptoms/episodes | 20 |
| Socioeconomic status or disadvantage | 19 | Cigarette consumption or alcohol/drug abuse | 16 |
| Health behaviors | 16 | BMI | 8 |
| Exposure to life adversities | 12 | Functional limitations/disability | 7 |
Fig. 2.
Conceptual overview of reviewed studies.
3. RESULTS
3.1. Design and Sample Characteristics
Out of a total of 65 publications, 38 different datasets were utilized, indicating that there are multiple datasets used to study intersectional health disparities. The most commonly used dataset was the Health and Retirement Study (HRS), appearing in seven studies and one of the few longitudinal datasets available with measures of health. Other datasets that were used in at least three studies included the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC, k = 5), the National Health Interview Survey (NHIS, k = 4), the Health and Nutrition Examination Survey (k = 4), and the General Social Survey (GSS, k = 3). Although these datasets were not necessarily designed to be compatible with intersectionality, they contain various measures of health, sociodemographic characteristics, and relevant explanatory mechanisms that are required for research on this topic. The majority of reviewed publications (k = 45) used a cross-sectional design.
Although few in number, some studies used datasets that were explicitly designed to capture how health varies among intersectional groups but mostly used either cross-sectional or, if longitudinal, contain only one or two follow-ups with short time intervals (e.g., one year). Examples of such datasets include Project STRIDE: Stress, Identity, and Mental Health or Black Women in a Study of Epidemics. This indicates a significant lack of longitudinal datasets designed with relevant measures for intersectional health disparities research.
Over half of the studies (k = 36) did not discern between different stages of the life span (e.g., young adulthood from ages 18–39, midlife from ages 40–64, or old age 65+), instead pooling together respondents of all ages. Five studies examined health disparities in young adulthood. Eleven studies examined both young adulthood and midlife, and six examined both midlife and old age. Four focused on midlife only, and only one study examined health disparities solely in old age. Taken together, there are few studies on how health disparities are experienced differently at various stages of life, especially in midlife and old age. In contrast, young adulthood receives the most attention among the three life course stages, perhaps because several datasets focus on the health of younger persons (e.g., Add Health).
3.2. Operationalization of Intersectionality
Forty-six studies (71%) operationalized intersectionality using a solely intercategorical complexity approach. This is perhaps unsurprising given that it is thought to have a “natural fit” with quantitative health research given its systematically comparative orientation (Evans et al. 2018; Green et al. 2017). Thus, most studies compared a health outcome across at least two well-defined intersectional groups rather than focusing solely on one such group. One study operationalized intersectionality using both intercategorical and intracategorial complexity approaches, one used both intercategorical and anticategorical complexity approaches, seventeen studies (26%) used a solely intracategorical approach by examining only one subpopulation, and no studies employed a solely anticategorical approach. Of the studies that employed an intracategorical approach, the intersectional groups chosen for investigation were, for example, sexual minorities at differing racial/ethnic intersections; Latinx men and women; and transgender women.
3.3. Intersectional and Reference Groups
Most studies (k = 49) compared health across intersectional groups defined by at least three social characteristics (e.g., race/ethnicity, sex/gender, and sexual orientation). A somewhat common approach (k = 15) was to examine some combination of race/ethnicity, sex/gender, and/or SES, reflecting the primacy of these “big three” categories in the literature. In fact, intersecting groups defined by race/ethnicity, sex/gender, and SES were used as the starting point for analysis for almost every health outcome examined. Most of the remaining studies examined the intersections of race/ethnicity, sex/gender, and a third social status other than SES, such as sexual orientation (k = 12) or age (k = 7). In some cases, studies examined health at the intersection of race/ethnicity, sex/gender, SES, and a fourth social characteristic, most commonly age (k = 10).
It is notable that sexual orientation appeared as a social characteristic of interest almost as often as race/ethnicity or sex/gender. As such, several studies (k = 20) looked at intersections of sexual orientation and some combination of race/ethnicity, sex/gender, SES, age, disability, cohabiting status, weight, gender identity, and nativity status. This signals a growing understanding that lesbian, gay, and bisexual individuals experience unique health outcomes contingent upon their statuses as men or women, Black or White, low- or high-SES, cisgender or genderqueer, and so on. Overall, these findings indicate that considerable attention is paid towards intersectional groups defined by race/ethnicity, sex/gender, SES, age, and sexual orientation. Intersectional groups that were given far less consideration included those defined by nativity status, level of acculturation, or immigration status (k = 4); gender identity (k = 4); skin tone (k = 2); cohabiting/marital status (k = 2); disability (k = 1); weight (k = 1); religion (k = 1); and HIV seropositivity (k = 1).
Out of those 51 studies that compared at least two intersectional groups, the majority of studies (k = 42) provided explicit information regarding choice of reference group. All but two publications (k = 40) chose the most privileged group as the referent. Examples include White cisgender or heterosexual men and native-born Whites. In the two publications where a marginalized intersectional group was chosen as the referent, the two groups consisted of women with low levels of acculturation and same-sex cohabiters.
3.4. Health Outcomes
In 65 reviewed publications, only 20 different health issues or conditions were investigated, indicating significant overlap in health conditions examined across studies. Thirty-seven studies investigated physical health, 44 examined mental health problems and/or diagnoses, 24 examined general measures of self-rated health or health-related quality of life, and 16 examined cigarette consumption or drug/alcohol issues. Many studies investigated disparities in multiple health outcomes simultaneously instead of focusing on a single condition or health domain. For instance, some studies looked at multiple mental health diagnoses (e.g., depressive and anxiety disorders), others examined multiple physical health issues (e.g., functional limitations and chronic conditions), and still others examined physical and mental health problems together (e.g., depressive symptoms and chronic conditions).
The most frequently studied health outcome overall was self-rated health or health-related quality of life, appearing in 24 studies as a health outcome of interest. Self-rated health is typically operationalized as a single-item measure of how one is generally feeling physically, mentally, or overall.
Forty-four studies investigated disparities in various mental health problems or diagnoses and wellbeing. By far, the most frequently examined mental health outcomes were depressive symptoms or episodes (k = 20), making depression the second most selected health outcome overall. Other mental health problems that appear in the literature include various mental health diagnoses (k = 6), psychological distress (k = 6), and psychological well-being (k = 3). There are several mental health issues that receive little attention. These include sleep-related issues (k = 2), social well-being and social anxiety (k = 2), suicidal ideation or self-harm (k = 3), and post-traumatic stress (k = 2). These results indicate that the existing body of scholarship is focused on a narrow range of mental health problems, namely, depressive symptoms or episodes.
The third most selected health outcome was cigarette consumption or alcohol/drug issues (k = 16). Among these 16 publications, only five had an exclusive focus on drug/alcohol abuse or cigarette consumption, while the remaining examined these outcomes simultaneously with either physical and/or mental health outcomes.
Of the 37 studies that investigated disparities in physical health, the following health conditions were most frequently investigated: BMI (k = 8), chronic conditions (k = 7), functional limitations or disabilities (k = 7), cardiovascular risk factors (i.e. hypertension; k = 7), and biomarkers (i.e. C-reactive protein; k = 4). This makes BMI the fourth most selected health outcome overall, followed by functional limitations. While other physical health issues were also considered, they rarely appeared in the literature as a health outcome of interest. These include physical activity (k = 2), cancer-related outcomes (i.e. breast cancer tumor characteristics; k = 1), sexually transmitted diseases or infections (k = 1), and mortality (k = 1). Taken together, the results indicate that a small subset of physical health outcomes are repeatedly examined to the neglect of other important health conditions. This is especially true for BMI, chronic conditions, functional limitations, and cardiovascular risk factors. Furthermore, because operationalizations of both chronic conditions and functional limitations almost always use count measures, information on specific chronic or functional issues is obscured.
3.5. Explanatory Mechanisms
Nearly a third (k = 21) of studies specified no explanatory mechanisms whatsoever. Thus, a sizable minority of studies treated intersectional groups as a primary predictor in their investigation of health disparities. Of those that did specify one or more explanatory mechanisms (k = 44), social and personal risks and/or resources were the most investigated explanatory mechanisms, appearing in 20 studies overall. Social and personal risks include health-damaging factors such as emotion regulation difficulties or cynical hostility. Social and personal resources were speculated to have beneficial effects on health and included social/emotional support, social network size, marital status, having children, coping tools, self-esteem, religiosity, and LGBT activism.
In line with intersectionality’s emphasis on oppression, 19 studies investigated perceived discrimination (e.g., racism, sexism, heterosexism), making it the second most selected explanatory mechanism in the literature. One of these 19 studies examined cortisol levels (rather than discrimination explicitly) to examine the biological impact of discrimination. Nineteen studies also selected socioeconomic status or disadvantage/strain. SES was operationalized with measures of educational attainment, income, and/or access to health care (e.g., health insurance). A large number of studies (k = 16) examined health behaviors as an explanatory mechanism for observed health disparities. Specifically, health behaviors include BMI/diet, smoking status, heavy drinking, physical activity, currently using medication, doctor visits, and sleep quality.
Compared to the aforementioned explanatory mechanisms, substantially fewer studies (k = 12) specified exposure to life adversities as an explanatory mechanism, which includes such affronts as microaggressions, harassment, or victimization; the internalization of stigmatizing attitudes; chronic stressors, strains, or burdens; traumatic or stressful life events; and intimate partner violence. Notably, certain life adversities receive far more attention than others. While chronic stress, strains, or burdens appear in seven publications, intimate partner violence has only been examined as a potential contributor to health disparities in one study.
It is worth noting that among all the explanatory mechanisms, social and personal resources are the only factors that are hypothesized to have protective benefits for health. Other explanatory mechanisms, such as health behaviors or perceived discrimination, are conceptualized as risk factors that have uniformly harmful effects on health. Taken together, our findings indicate the literature has tended to overlook health-promoting factors.
Two explanatory mechanisms remain significantly understudied. The first can be grouped as contextual factors (k = 4), such as neighborhood characteristics (e.g., local crime rate) and level of comfortability being a minority in one’s community or family. The second includes early-life factors, only examined in seven studies as potential contributors to health disparities. Among the five studies that did investigate early-life mechanisms, childhood and adolescent socioeconomic status, adolescent academic achievement, BMI, and exposure to childhood physical or sexual abuse were selected. Thus, explanatory mechanisms for health disparities are almost always assumed to occur solely in adulthood, leading to a significant lack of information regarding how childhood insults are associated with poor health later in life.
4. DISCUSSION
Scholars have made the value of intersectionality to quantitative health disparities research more than evident as an effective method to examine how intersecting (and previously neglected) social characteristics shape health disparities (Bauer 2014; Bauer and Scheim 2019a; Bowleg 2012; Green et al. 2017; Hankivsky 2012; Viruell-Fuentes et al. 2012). However, intersectionality, a perspective that takes multiple social categories as its starting point for analysis, carries considerable limitations when applied to quantitative health disparities research. In our systematic review of the literature, we found these limitations to be widespread. Here we summarize our findings and then offer recommendations regarding how to stimulate the application of intersectionality to this body of scholarship.
4.1. Limited measurement of intersectionality, intersectional groups, and health outcomes.
Corroborating the claims of previous scholars (Evans et al. 2018), our review indicates that most research employs an operationalization of intersectionality that aligns with the intercategorical complexity approach (see Table S4). As a result, there exists a rapidly expanding body of scholarship that thoroughly investigates heterogeneity in health between intersectional groups—especially those at the intersections of race/ethnicity, sex/gender, and SES. Yet, our review illustrates that between-group comparisons, on their own, provide only a limited view of health disparities when within-group heterogeneity becomes obscured. Thus, regardless of how many intersectional groups are examined, the existing body of scholarship cannot fully discriminate between those who will get sick and those who will not if those individuals are situated at the same intersections (Green et al. 2017).
Furthermore, among studies that use the intercategorical approach, virtually all use binary measures for intersectional group membership (e.g., “Black”/“non-Black”). Such measures lead to homogenization of diverse groups, leading to a dearth of information regarding how health varies for subpopulations that have been rendered invisible under a monolithic category (e.g., “non-Black”). Second, dichotomous measures cannot capture the fluid and dynamic nature of intersectional group membership (Choo and Ferree 2010; McCall 2005). Indeed, dichotomous measures run the risk of perpetuating binary categorization schemes as “natural distinctions, despite the fact that they, like all classification schemes, are socially constructed” (Westbrook and Saperstein 2015: 535).
Our review also makes evident that much of intersectional health disparities research investigates a narrow cluster of health outcomes (see Table 1). In general, there exists a strong tendency to study self-rated health which captures how one is generally feeling. Although self-rated health is useful as a broad measure of overall health, it cannot measure disparities in specific illnesses that intersectional groups endure. In terms of specific physical health issues, our review indicates that BMI, functional limitations/disability, and chronic conditions are popular outcomes of interest. These outcomes obscure disparities in specific illnesses because chronic conditions and functional limitations are operationalized as count measures. In terms of mental health outcomes, significant attention is paid toward depressive symptoms/episodes while virtually all other mental health problems are understudied. This has contributed to a shortage of investigations of health disparities in numerous illnesses, diseases, and diagnoses.
4.2. Who is compared to whom?
Although intersectionality rejects a priori rankings of social characteristics in terms of their relative salience in generating health disparities (Hankivsky 2012; Hankivsky and Grace 2015), our review indicates that most research tends to prioritize three social characteristics—race/ethnicity, sex/gender, and SES—as the starting point for analysis (see Table S4). While an intersectional theoretical framework reminds us that a wide array of social characteristics are relevant to the study of health disparities, only a limited number of studies look beyond these “big three” to include intersections of sexual orientation, age, disability, and nativity or immigrant status. Even fewer examine intersectional groups defined by gender identity, religion, or region.
Furthermore, because of intersectionality’s emphasis on marginalized groups, our review reveals ambiguity surrounding whether multiply-privileged groups (e.g., White men) and mixed-privileged groups (e.g., Black men) are deemed appropriate for analysis (Levine-Rasky 2011). Our findings indicate that, overall, privileged groups are rarely the focus of intersectional investigations of health disparities. Instead, such groups are specified as the referent to which all other intersectional groups are compared to, preventing a nuanced examination of how privilege contributes to health disparities. However, intersectionality acknowledges the fact that everyone inhabits social groups enmeshed in systems of stratification, meaning that privileged groups are appropriate for intersectional analysis (Cole 2009). Indeed, while marginalization plays a significant role in the production of health disparities, unearned advantage and privilege jointly contribute as well; therefore, it may not be possible to achieve health equity without critical investigation of both groups (Nixon 2019).
4.3. Overlooking key explanatory mechanisms.
Intersectionality highlights power-laden explanatory mechanisms rooted in macro-level structures that meaningfully explain why intersectional groups experience disproportionally poor health outcomes (Bauer 2014; Bauer and Scheim 2019a; Green et al. 2017). In this vein, our review indicates that multiple publications selected such mechanisms to explain the poor health outcomes experienced by intersectional groups (see Table 1). In fact, perceived discrimination was a frequently selected mechanism (appearing in over a quarter of the reviewed publications) in addition to being the third most selected mechanism overall. Exposure to life adversities was also examined as an explanatory mechanism in a smaller number of studies; yet, some life adversities have been summarily neglected. For instance, while exposure to chronic strain was investigated frequently as an explanatory mechanism, intimate partner violence was only investigated in one publication. Additional life adversities that are significantly overlooked include microaggressions, childhood adversities more generally (e.g., sexual, physical, and emotional abuse), and hate crimes. Thus, any one study may capture only a fraction of the life adversities that intersectional groups experience.
It is noteworthy that nearly one-third (32%) of the reviewed publications specified no explanatory mechanisms whatsoever in their investigation of health disparities among intersectional groups. When no explanatory mechanisms are specified, the intersectional groups under investigation are often treated as proxies for explanatory mechanisms that might contribute to observed health disparities. This invariably leads to an implicit assumption that intersectional group membership can independently explain variation in health, and therefore membership in such groups becomes “risky” to health in and of itself (Bowleg 2008; Green et al. 2017). If explanatory mechanisms are not explored, it is impossible to identify modifiable factors that contribute to health (in)equity, making it difficult to assist in the formulation of health-promoting interventions (Bauer and Scheim 2019b).
4.4. Limited mediation analysis.
A related and widespread limitation is that mediation analyses in which explanatory mechanisms are examined are not comprehensive enough to reflect the reality of the specific factors driving health disparities among intersectional groups. First, mediation analysis is often carried out under the assumption that any and all health disparities can be fully or mostly explained by differential exposure to the harmful explanatory mechanisms under investigation (Thoits 2010). However, mounting evidence suggests that, regardless of differential exposure, vulnerability to the harmful effects of a particular explanatory mechanism can vary by the intersectional group and health domain under investigation (Diderichsen, Hallqvist, and Whitehead 2019). For instance, although racial/ethnic minority membership is associated with disproportionate exposure to discrimination, it is also linked to the possession of social and personal resources (e.g., religiosity) that can render this group less vulnerable to discrimination’s adverse impact on mental health (Keyes 2009). Therefore, overlooking differential vulnerability may yield biased mediating (indirect) effects of discrimination by exaggerating its negative effect on racial/ethnic minorities’ mental health.
In sum, differential exposure provides only a partial picture of how explanatory mechanisms contribute to health disparities among intersectional groups. Future research would benefit from considering both differential exposure and vulnerability to better assist health-promoting policies target the intersectional groups most vulnerable to health issues (Diderichsen et al. 2019). This may be accomplished in two ways. First, mediation analyses that examine the interaction between intersectional groups and mediators can determine how a mediator differentially impacts health for different populations. Furthermore, relatively newly developed mediation techniques are now able to explicitly address both the effects of differential exposure and vulnerability on health (e.g., VanderWeele 2014); however, they remain underutilized in intersectional quantitative health research.
Second, broadening the focus to health-promoting and contextual factors would provide valuable insight into the conditions whereby adverse effects of mediators may or may not be attenuated. Such mechanisms are rarely acknowledged despite playing a key role in the health of those in intersectional groups. Religiosity, for instance, is one such health-promoting mechanism that attenuates the association between discrimination and poor health, especially among older Black Americans (Krause 2006). Furthermore, contextual factors emanating from the lived and built environment provide the backdrop for how other mediators affect health. For instance, living in a crime-ridden neighborhood may increase intersectional groups’ likelihood of exposure to additional health-damaging life adversities, such as intimate partner violence (Stueve and O’Donnell 2008). Yet, other protective contextual factors (e.g., feeling comfortable as a minority in one’s community) might attenuate the effects of health-damaging mediators. Multi-level analyses that include such contextual factors have not yet been adequately explored in the extant literature.
4.5. Life-course perspectives?
Our systematic review reveals a preponderance of cross-sectional studies with samples comprising adults of all ages, thereby not allowing us to discern between different stages of the life course (see Figure 2). Undoubtedly, this is driven by a scarcity in longitudinal datasets that include necessary and relevant measures. Still, the use of cross-sectional data with respondents of all ages fosters a rather static view of how health disparities among intersectional groups are experienced across the life course. Life-course perspectives, however, highlight how health trajectories are heterogeneous, shaped by intersecting social characteristics beginning early in life (Kuh et al. 2003). Longitudinal data would therefore be invaluable to intersectional health disparities researchers attempting to illustrate how, using a life-course perspective, the accumulation of disadvantages stemming from one’s unique intersectional location shapes health over time. Only a small minority of publications incorporate a life course approach, either by examining how early-life risk factors contribute to health disparities in adulthood or, if longitudinal data is available, assessing trajectories in a health outcome across time. Otherwise, intersectional and life-course perspectives exist largely independent of one another.
Furthermore, life-course drivers that substantially explain health disparities across intersectional groups differ as one ages. Yet, few studies have investigated life course-specific mediators. As an example, certain indicators of socioeconomic status (e.g., income and wealth) are especially critical for the health of older adults who encounter higher rates of chronic illness and therefore benefit from high-quality medical care, healthy lifestyles, health-promoting social networks, and other factors afforded by financial assets (Cockerham 2005; Yang et al. 2020). However, the health-promoting effects of other socioeconomic resources, such as education, are weaker compared to income and wealth for older adults, particularly older Black adults (Shuey and Willson 2008). This suggests that specific components of SES are especially consequential for the generation of health disparities among older adults compared to their younger counterparts. Future intersectional research on age cohorts that have been overlooked will provide invaluable insight regarding how mechanisms may affect health differently depending on specific stages of the life course.
5. LIMITATIONS
To the best of our knowledge, this systematic review is the first to evaluate intersectional quantitative health disparities scholarship. In general, however, systematic reviews are subject to certain methodological drawbacks and limitations that should be acknowledged in light of the findings. First, there is no set of standardized search terms for indexing quantitative health disparities research explicitly using an intersectional lens. In addition, since intersectionality’s application to this body of research is still in its infancy, it is possible that terminology varies from study to study, rendering the discovery of all relevant publications difficult. To mitigate this, we relied upon a carefully crafted set of search terms designed to capture as many relevant studies as possible. Second, because English-only studies were eligible for inclusion, relevant studies published in other languages may have been omitted. Third, and similarly, due to resource restrictions, our search did not extend to gray literature. Fourth, any systematic review is necessarily limited by the quality of the studies reviewed. We attempted to overcome this limitation by performing a thorough critical appraisal of all reviewed publications using a well-established quality checklist (Petticrew and Roberts 2006). Studies included in this review were largely found to be of good quality, leading us to conclude that there were no errors large enough to warrant any study’s removal from final review.
6. FUTURE DIRECTIONS AND CONCLUDING REMARKS
By identifying shortcomings in the extant literature, this systematic review sheds light on a number of recommendations to better integrate intersectionality into quantitative health disparities research. First, many limitations stem from a lack of datasets that contain measures of social characteristics or explanatory mechanisms that align with the fundamental assertions of intersectionality. Substantial efforts should be made towards the development and collection of intersectionality-oriented data. At a minimum, researchers should include intersectional group membership measures beyond sex/gender and race/ethnicity, such as sexual orientation, disability, religion, nativity, and immigration status. Intersectionality also calls for the development of measures that reflect the fluid and shifting nature of social statuses (Choo and Ferree 2010; McCall 2005). Researchers should move “beyond the binary” to incorporate comprehensive self-report measures that reflect dynamic interpretations of identity across place, social context, and the life course (Else-Quest and Hyde 2016b; Westbrook and Saperstein 2015). For instance, measures of sexual orientation could include multiple factors that shape sexuality, such as sexual behavior, gender identity, and gender expression rather than simplistic “heterosexual/sexuality minority” responses. In a similar vein, the development of explanatory mechanisms should be prioritized with emphasis on capturing how those in intersectional groups uniquely experience them (e.g., Scheim and Bauer 2019).
In terms of operationalizations of intersectionality, McCall’s (2005) approach is considered the “gold standard,” but we found only seven studies that explicitly approached intersectionality in this way (mostly using an intercategorical approach) despite frequently citing her work. We suggest that future researchers more clearly explicate which of McCall’s three approaches guided their analysis as well as why and how they applied the particular approach. We also draw attention to operationalizations of intersectionality beyond the intercategorical complexity approach since it falls short of appreciating the nuanced heterogeneity in health within groups. Researchers may consider other approaches that problematize categorization schemes altogether, thereby offering a measure of intersectionality ripe for investigating how those situated at one previously neglected intersection differentially experience health.
There is an emerging area of research (e.g., Evans et al. 2018; Persmark et al., 2019) that evaluates discriminatory accuracy (DA; e.g., whether a model accurately classifies individuals into one of two categories, for example, having a disease or not). When applying measures of DA to intersectional health research, the results constitute a quantifiable measure of the individual differences in health that exist at the intersectional level. Thus far, these studies have found low DA for the intercategorical strata that they have examined (e.g., Evans et al. 2018). However, this does not necessarily suggest that one needs to follow the anticategorical approach and abandon the use of intersectional categories altogether. As Merlo (2018) notes, a finding of low DA may also imply that more intersectional locations are needed to fully capture heterogeneity in health (aligning with the intercategorical approach). More studies are needed to fully evaluate the DA of intersectional complexity.
Finally, a broader set of health outcomes should be considered. Indeed, scholars continue to make calls for explicitly intersectional research into illnesses and diseases that have been overlooked, such as kidney disease (Bruce, Griffith, and Thorpe 2015), cancer (Damaskos et al. 2018), HIV (Earnshaw, Bogart, and Dovidio 2013), and sleep health/disorders (Johnson et al. 2019). An intersectional analysis would be useful for identifying the populations most vulnerable to such health issues and the explanatory mechanisms that contribute to corresponding population-level disparities. For example, intersectional research has been proposed as a useful tool to advance health equity for vulnerable groups as varied as older adults living in rural communities (Poulin, Skinner, and Hanlon 2020) to transgender women who engage in sex work (Turner, Arayasirikul, and Wilson 2021).
In sum, this systematic review, the first to thoroughly evaluate the application of intersectionality to quantitative health disparities research, has identified multiple theoretical and methodological limitations that need to be overcome if the overarching goal of health equity is to be achieved. Although the studies reviewed here introduce innovative methods, measures, and analyses to capture how health varies across intersectional groups, many questions remain unanswered regarding whether quantitative health disparities research is doing justice to intersectionality. Intersectionality, with its transformative and critical edge, has the potential to help reach the goal of health equity even for the most vulnerable and marginalized groups in society. However, before it can truly inform public health policies that target a wide range of disparities, intersectionality should first be properly integrated with quantitative health disparities research.
Supplementary Material
Highlights.
Intersectionality is increasingly used to study how social statuses shape health.
Current systematic review is first on intersectional quantitative health disparities research.
Widespread limitations reduce intersectionality’s development in this literature.
Results highlight a need for data to match intersectionality’s core tenets.
Acknowledgements:
Research reported in this publication was supported by grants from the National Institute on Aging of the US National Institutes of Health (R00AG052458); The National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number (U54MD013368).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
* Studies included in systematic review
- *Ailshire Jennifer A., and House James S. 2011. “The Unequal Burden of Weight Gain: An Intersectional Approach to Understanding Social Disparities in BMI Trajectories from 1986 to 2001/2002.” Social Forces 90(2): 397–423. doi: 10.1093/sf/sor001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Allen Julie Ober, Watkins Daphne C., Chatters Linda, Geronimus Arline T., and Johnson-Lawrence Vicki. 2019. “Cortisol and Racial Health Disparities Affecting Black Men in Later Life: Evidence from MIDUS II.” American Journal of Men’s Health Jul-Aug: 1–13. doi: 10.1177/1557988319870969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Allen Samuel H., and Leslie Leigh A. 2019. “Considering the Role of Nativity in the Health and Psychological Wellbeing of Black LGBT Adults.” Journal of Homosexuality 66(13): 1769–1796. doi: 10.1080/00918369.2018.1511134 [DOI] [PubMed] [Google Scholar]
- *Amroussia Nada, Pearson Jennifer L., and Gustafsson Per E. 2019. “What Drives Us Apart? Decomposing Intersectional Inequalities in Cigarette Smoking by Education and Sexual Orientation Among U.S. Adults.” International Journal for Equity in Health 18: 109. doi: 10.1186/s12939-019-1015-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Assari Shervin, Nikahd Amirmasoud, Reza Mohammad, Malckahmadi Maryam Moghani Lankarandi, and Zamanian Hadi. 2017. “Race by Gender Group Differences in the Protective Effects of Socioeconomic Factors Against Sustained Health Problems Across Five Domains.” Journal of Racial and Ethnic Health Disparities 4: 884–894. doi: 10.1007/s40615-016-0291-3 [DOI] [PubMed] [Google Scholar]
- Bauer Greta R. 2014. “Incorporating Intersectionality Theory Into Population Health Research Methodology: Challenges and the Potential to Advance Health Equity.” Social Science & Medicine 110: 10–17. doi: 10.1016/j.socscimed.2014.03.022 [DOI] [PubMed] [Google Scholar]
- Bauer Greta R., and Scheim Ayden I. 2019a. “Advancing Quantitative Intersectionality Research Methods: Intracategorical and Intercategorical Approaches to Shared and Differential Constructs.” Social & Social Medicine 226: 260–262. doi: 10.1016/j.socscimed.2019.03.018 [DOI] [PubMed] [Google Scholar]
- Bauer Greta R., and Scheim Ayden I. 2019b. “Methods for Analytic Intercategorical Intersectionality in Quantitative Research: Discrimination as a Mediator of Health Inequalities.” Social Science & Medicine 226: 236–245. doi: 10.1016/j.socscimed.2018.12.015 [DOI] [PubMed] [Google Scholar]
- *Bostwick Wendy B., Boyd Carol J., Hughes Tonda L., and West Brady. 2014. “Discrimination and Mental Health Among Lesbian, Gay, and Bisexual Adults in the United States.” American Journal of Orthopsychiatry 84(1): 35–45. doi: 10.1037/h0098851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Bostwick Wendy B., Hughes Tonda L., Steffen Alana, Veldhuis Cindy B., and Wilsnack Sharon C. 2019. “Depression and Victimization in a Community Sample of Bisexual and Lesbian Women: An Intersectional Approach.” Archives of Sexual Behavior 48: 131–141. doi: 10.1007/s10508-018-1247-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg Lisa. 2012. The phrase with the phrase Women and minorities: intersectionality—an important theoretical framework for public health. Am. J. Publ. Health 102, 1267–1273. 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg Lisa. 2008. “When Black + Lesbian + Woman ≠ Black Lesbian Woman: The Methodological Challenges of Qualitative and Quantitative Intersectionality Research.” Sex Roles 59: 312–325. doi: 10.1007/s11199-008-9400-z [DOI] [Google Scholar]
- Bowleg Lisa, and Bauer Greta. 2016. “Invited Reflection: Quantifying Intersectionality.” Psychology of Women Quarterly 40(3): 337–341. doi: 10.1177/0361684316654282 [DOI] [Google Scholar]
- *Brown Tyson H. 2018. “Racial Stratification, Immigration, and Health Inequality: A Life Course-Intersectional Approach.” Social Forces 1–33. doi: 10.1093/sf/soy013 [DOI] [Google Scholar]
- *Brown Tyson H., and Hargrove Taylor W. 2013. “Multidimensional Approaches to Examining Gender and Racial/Ethnic Stratification in Health.” Women, Gen der, and Families of Color 1(2): 180–206. doi: 10.5406/womgenfamcol.1.2.0180 [DOI] [Google Scholar]
- *Brown Tyson H., and Hargrove Taylor W. 2018. “Psychosocial Mechanisms Underlying Older Black Men’s Health.” Journals of Gerontology: Social Sciences 73(2): 188–197. doi: 10.1093/geronb/gbx091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Brown Tyson H., Richardson Liana J., Hargrove Taylor W., and Thomas Courtney S. 2016. “Using Multiple-Hierarchy Stratification and Life Course Approaches to Understand Health Inequalities: The Intersecting Consequences of Race, Gender, SES, and Age.” Journal of Health and Social Behavior 57(2): 200–222. doi: 10.1177/0022146516645165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce Marino A., Griffith Derek M., and Thorpe Roland J. Jr. 2015. “Stress and the Kidney.” Advances in Chronic Kidney Disease 22(1): 46–53. doi: 10.1053/j.ackd.2014.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Calabrese Sarah K., Meyer Ilan H., Overstreet Nicole M., Haile Rahwa, and Hansen Nathan B. 2015. “Exploring Discrimination and Mental Health Disparities Faced by Black Sexual Minority Women Using a Minority Stress Framework.” Psychology of Women Quarterly 39(3): 287–304. doi: 10.1177/0361684314560730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Carliner Hannah, Delker Erin, Fink David S., Keyes Katherine M., and Hasin Deborah S. 2016. “Racial Discrimination, Socioeconomic Position, and Illicit Drug Use Among US Blacks.” Social Psychiatry and Psychiatric Epidemiology 51: 551–560. doi: 10.1007/s00127-016-1174-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter-Pokras Olivia, and Baquet Claudia. 2002. “What is a ‘Health Disparity’?” Public Health Reports 117: 426–434. doi: 10.1093/phr/117.5.426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choo Hae Yoon, and Ferree Myra Marx. 2010. “Practicing Intersectionality in Sociological Research: A Critical Analysis of Inclusions, Interactions, and Institutions in the Study of Inequalities.” Sociological Theory 28(2): 129–149. doi: 10.1111/j.1467-9558.2010.01370.x [DOI] [Google Scholar]
- Cockerham William C. 2005. “Health Lifestyle Theory and the Convergence of Agency and Structure.” Journal of Health and Social Behavior 46: 51–67. doi: 10.1177/002214650504600105 [DOI] [PubMed] [Google Scholar]
- Cole Elizabeth R. 2009. “Intersectionality and Research in Psychology.” American Psychology 64(3): 170–180. doi: 10.1037/a0014564 [DOI] [PubMed] [Google Scholar]
- *Coley Sheryl L., de Leon Carlos F. Mendes, Ward Earlise C., Barnes Lisa L., Skarupski Kimberly A., and Jacobs Elizabeth A. 2017. “Perceived Discrimination and Health-Related Quality-of-Life: Gender Differences among Older African Americans.” Quality of Life Research 26(12): 3449–3458. doi: 10.1007/s11136-017-1663-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins Patricia Hill. 1991. Black Feminist Thought: Knowledge, Consciousness and the Politics of Empowerment. New York: Routledge. [Google Scholar]
- Crenshaw Kimberlé. 1991. “Mapping the Margins: Intersectionality, Identity Politics, and Violence Against Women of Color.” Stanford Law Review 43(6): 1241–1299. doi: 10.2307/1229039 [DOI] [Google Scholar]
- *Cummings Jason L., and Jackson Pamela Braboy. 2008. “Race, Gender, and SES Disparities in Self-Assessed Health, 1974–2004.” Research on Aging 30(2): 137–168. doi: 10.1177/0164027507311835 [DOI] [Google Scholar]
- Damaskos Penny, Amaya Beau, Gordon RuthAnn, and Walters Chasity Burrows. 2018. “Intersectionality and the LGBT Cancer Patient.” Seminars in Oncology Nursing 34(1): 30–36. doi: 10.1016/j.soncn.2017.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diderichsen Finn, Hallqvist Johan, and Whitehead Margaret. 2019. “Differential Vulnerability and Susceptibility: How to Make Use of Recent Development in Our Understanding of Mediation and Interaction to Tackle Health Inequalities.” International Journal of Epidemiology 48(1): 268–274. doi: 10.1093/ije/dyy167 [DOI] [PubMed] [Google Scholar]
- DiPrete Thomas A., and Eirich Gregory M. 2006. “Cumulative Advantage as a Mechanism for Inequality: A Review of Theoretical and Empirical Developments.” Annual Review of Sociology 32: 271–297. doi: 10.1146/annurev.soc.32.061604.123127 [DOI] [Google Scholar]
- *Divney AA, Echeverria SE, Thorpe LE, Trinh-Shevrin C, and Islam NS 2019. “Hypertension Prevalence Jointly Influenced by Acculturation and Gender in US Immigrant Groups.” American Journal of Hypertension 32(1): 104–111. doi: 10.1093/ajh/hpy130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw Valerie A., Smith Laramie R., Chaudoir Stephenie R., Amico K. Rivet, and Copenhaver Michael M. 2013. “HIV Stigma Mechanisms and Well-Being Among PLHW: A Test of the HIV Stigma Framework.” AIDS and Behavior 17: 1785–1795. doi: 10.1007/s10461-013-0437-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger Matthias, Smith George Davey, and O’Rourke Keith. 2001. “Introduction: Rationale, Potentials, and Promise of Systematic Reviews.” Pp. 3–19 in Systematic Reviews in Health Care: Meta-Analysis in Context, edited by Egger M, Smith GD, and Altman DG John Wiley & Sons. doi: 10.1002/9780470693926.ch1 [DOI] [Google Scholar]
- Else-Quest Nicole M., and Hyde Janet Shibley. 2016a. “Intersectionality in Quantitative Psychological Research: I. Theoretical and Epistemological Issues.” Psychology of Women Quarterly 40(2): 155–170. doi: 10.1177/0361684316629797 [DOI] [Google Scholar]
- Else-Quest Nicole M., and Hyde Janet Shibley. 2016b. “Intersectionality in Quantitative Psychological Research: II. Methods and Techniques.” Psychology of Women Quarterly 40(3): 319–336. doi: 10.1177/0361684316647953 [DOI] [Google Scholar]
- *English Devin, Rendina Jonathon, and Parsons Jeffrey T. 2018. “The Effects of Intersecting Stigma: A Longitudinal Examination of Minority Stress, Mental Health, and Substance Use Among Black, Latino, and Multiracial Gay and Bisexual Men.” Psychology of Violence 8(6): 669–679. doi: 10.1037/vio0000218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erikson Erik H. 1968. Identity: Youth and Crisis. New York, NY: W. W. Norton & Company. [Google Scholar]
- *Etherington Nicole. 2015. “Race, Gender, and the Resources that Matter: An Investigation of Intersectionality and Health.” Women & Health 55(7): 754–777. doi: 10.1080/03630242.2015.1050544 [DOI] [PubMed] [Google Scholar]
- *Evans Clare R., and Erickson Natasha. 2019. “Intersectionality and Depression in Adolescence and Early Adulthood: A MAIHDA Analysis of the National Longitudinal Study of Adolescent to Adult Health, 1995–2008.” Social Science & Medicine 220: 1–11. doi: 10.1016/j.socscimed.2018.10.019 [DOI] [PubMed] [Google Scholar]
- *Evans Clare R., Williams David R., Onnella Jukka-Pekka, and Subramanian SV 2018. “A Multilevel Approach to Modeling Health Inequalities at the Intersection of Multiple Social Identities.” Social Science & Medicine 203: 64–73. doi: 10.1016/j.socscimed.2017.11.011 [DOI] [PubMed] [Google Scholar]
- Ferraro Kenneth F., and Farmer Melissa M. 1996. “Double Jeopardy, Aging as Leveler, or Persistent Health Inequality? A Longitudinal Analysis of White and Black Americans.” Journal of Gerontology: Series B 51B(6): S319–S328. doi: 10.1093/geronb/51B.6.S319 [DOI] [PubMed] [Google Scholar]
- *Garbarski Dana. 2015. “Racial/Ethnic Disparities in Midlife Depressive Symptoms: The Role of Cumulative Disadvantage Across the Life Course.” Advances in Life Course Research 23: 67–85. doi: 10.1016/j.alcr.2014.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Glass Joseph E., Rathouz Paul J., Gattis Maurice, Young Sun Joo Jennifer C. Nelson, and Williams Emily C. 2017. “Intersections of Poverty, Race/Ethnicity, and Sex: Alcohol Consumption and Adverse Outcomes in the United States.” Social Psychiatry and Psychiatric Epidemiology 52: 515–524. doi: 10.1007/s00127-017-1362-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Gorman Bridget K., Denney Justin T., Dowdy Hilary, and Medeiros Rose Anne. 2015. “A New Piece of the Puzzle: Sexual Orientation, Gender, and Physical Health Status.” Demography 52: 1357–1382. doi: 10.1007/s13524-015-0406-1 [DOI] [PubMed] [Google Scholar]
- Green Mark A., Evans Clare R., and Subramanian SV 2017. “Can Intersectionality Theory Enrich Population Health Research?” Social Science & Medicine 178: 214–216. doi: 10.1016/j.socscimed.2017.02.029 [DOI] [PubMed] [Google Scholar]
- *Grollman Eric Anthony. 2014. “Multiple Disadvantaged Statuses and Health: The Role of Multiple Forms of Discriminations.” Journal of Health and Social Behavior 55(1): 3–19. doi: 10.1177/0022146514521215 [DOI] [PubMed] [Google Scholar]
- Hankivsky Olena. 2012. “Women’s Health, Men’s Health, and Gender and Health: Implications of Intersectionality.” Social Science & Medicine 74: 1712–1720. doi: 10.1016/j.socscimed.2011.11.029 [DOI] [PubMed] [Google Scholar]
- Hankivsky Olena, and Grace Daniel. 2015. “Understanding and Emphasizing Difference and Intersectionality in Multimethod and Mixed Methods Research.” In The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry, edited by Hesse-Biber SN and Johnson RB Oxford University Press. doi: 10.1093/oxfordhb/9780199933624.013.8 [DOI] [Google Scholar]
- *Hargrove Taylor W. 2018a. “BMI Trajectories in Adulthood: The Intersection of Skin Color, Gender, and Age among African Americans.” Journal of Health and Social Behavior 59(4): 501–519. doi: doi.org/ 10.1177/0022146518802439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hargrove Taylor W. 2018b. “Intersecting Social Inequalities and Body Mass Index Trajectories from Adolescence to Early Adulthood.” Journal of Health and Social Behavior 59(1): 56–73. doi: doi.org/ 10.1177/0022146517746672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hargrove Taylor W. 2019. “Light Privilege? Skin Tone Stratification in Health Among African Americans.” Sociology of Race and Ethnicity 5(3): 370–387. doi: 10.1177/2332649218793670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Harnois Catherine E., and Bastos Joao L. 2018. “Discrimination, Harassment, and Gendered Health Inequalities: Do Perceptions of Workplace Mistreatment Contribute to the Gender Gap in Self-Reported Health?” Journal of Health and Social Behavior 59(2); 283–299. doi: 10.1177/0022146518767407 [DOI] [PubMed] [Google Scholar]
- Horsley Tanya, Dingwall Orvie, and Sampson Margaret. 2011. “Checking Reference Lists to Find Additional Studies for Systematic Reviews.” The Cochrane Database of Systematic Reviews 8: MR000026. doi: 10.1002/14651858.MR000026.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hseigh Ning, and Ruther Matt. 2016. “Sexual Minority Health and Health Risk Factors: Intersection Effects of Gender, Race, and Sexual Identity.” American Journal of Preventive Medicine 50(6): 746–755. doi: 10.1016/j.amepre.2015.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hinze Susan W., Lin Jielu, and Andersson Tanetta E. 2012. “Can We Capture the Intersections? Older Black Women, Education, and Health.” Women’s Health Issues 22(1): e91–e98. doi: 10.1016/j.whi.2011.08.002 [DOI] [PubMed] [Google Scholar]
- Hulko Wendy. 2009. “The Time- and Context-Contingent Nature of Intersectionality and Interlocking Oppressions.” Affilia: Journal of Women and Social Work 24(1): 44–55. doi: 10.1177/0886109908326814 [DOI] [Google Scholar]
- Johnson Blair T., and Hennessy Emily A. 2019. “Systematic Reviews and Meta-Analyses in the Health Sciences: Best Practice Methods for Research Syntheses.” Social Science & Medicine 233: 237–251. doi: 10.1016/j.socscimed.2019.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson Dayna A., Jackson Chandra L., Williams Natasha J., and Alcantara Carmela. 2019. “Are Sleep Patterns Influenced by Race/Ethnicity – A Marker of Relative Advantage or Disadvantage? Evidence to Date.” Nature and Science of Sleep 11: 79–95. doi: 10.2147/NSS.S169312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kanchi Rania, Perlman Sharon E., Chernov Claudia, Wu Winfred, Tabaei Bahman P., Chau Trinh-Shevrin Nadia Islam, Seixas Azizi, Rodriguez-Lopez Jesica, and Thorpe Lorna E. 2018. “Gender and Race Disparities in Cardiovascular Disease Risk Factors among New York City Adults: New York City Health and Nutrition Examination Survey (NYC HANES) 2013–2014.” Journal of Urban Health 95: 801–812. doi: 10.1007/s11524-018-0287-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerner Ina. 2012. “Questions of Intersectionality: Reflections on the Current Debate in German Gender Studies.” European Journal of Women’s Studies 19(2): 203–218. doi: 10.1177/1350506811434666 [DOI] [Google Scholar]
- Keyes Corey L. M. 2009. “The Black-White Paradox in Health: Flourishing in the Face of Social Inequality and Discrimination.” Journal of Personality 77(6): 1677–1706. doi: 10.1111/j.1467-6494.2009.00597.x [DOI] [PubMed] [Google Scholar]
- *Khan Mariam, Ilcisin Misja, and Saxton Katherine. 2017. “Multifactorial Discrimination as a Fundamental Cause of Mental Health Inequities.” International Journal for Equity in Health 16(43). doi: 10.1186/s12939-017-0532-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- *King Tania L., Shields Marissa, Shakespeare Tom, Milner Allison, and Kavanagh Anne. 2019. “An Intersectional Approach to Understandings of Mental Health Inequalities Among Men With Disability.” SSM – Population Health 9: 100464. doi: 10.1016/j.ssmph.2019.100464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Klassen Ann C., Pankiewicz Aaron, Hsieh Stephanie, Ward Abigal, and Curriero Frank C. 2015. “The Association of Area-Level Social Class and Tobacco Use with Adverse Breast Cancer Characteristics among White and Black Women: Evidence from Maryland, 1992–2003.” International Journal of Health Geographics 14(13). doi: 10.1186/s12942-015-0007-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause Neal. 2006. “Religion and Health in Late Life.” Pp. 499–518 in Handbook of the Psychology of Aging, edited by Birren JE and Schaie KW Burlington, MA: Academic Press. [Google Scholar]
- Kuh Diana, Yoav Ben-Shlomo John Lynch, Hallqvist Johan, and Power Chris. 2003. “Life Course Epidemiology.” Journal of Epidemiology & Community Health 57(10): 778–783. doi: 10.1136/jech.57.10.778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kulick Alex, Wernick Laura J., Woodford Michael R., and Renn Kristen. 2017. “Heterosexism, Depression, and Campus Engagement Among LGBTQ College Students: Intersectional Differences and Opportunities for Healing.” Journal of Homosexuality 64(8): 1125–1141. doi: 10.1080/00918369.2016.1242333 [DOI] [PubMed] [Google Scholar]
- *Lefevor G. Tyler, Boyd-Rogers Caroline C., Sprague Brianna M., and Janis Rebecca A. 2019a. “Health Disparities Between Genderqueer, Transgender, and Cisgender Individuals: An Extension of Minority Stress Theory.” Journal of Counseling Psychology 66(4): 385–395. doi: 10.1037/cou0000339 [DOI] [PubMed] [Google Scholar]
- *Lefevor G. Tyler, Janis Rebecca A., Franklin Alexis, and Stone William-Michael. 2019b. “Distress and Therapeutic Outcomes Among Transgender and Gender Nonconforming People of Color.” The Counseling Psychologist 47(1): 34–58. doi: 10.1177/0011000019827210 [DOI] [Google Scholar]
- Levine-Rasky Cynthia. 2011. “Intersectionality Theory Applied to Whiteness and Middle-Classness.” Social Identities 17(2): 239–253. doi: 10.1080/13504630.2011.558377 [DOI] [Google Scholar]
- *Liu Hui, Reczek Corinne, Mindes Samuel C. H., and Shen Shannon. 2017. “The Health Disparities of Same-Sex Cohabitors at the Intersection of Race-Ethnicity and Gender.” Sociological Perspectives 60(3): 620–639. doi: 10.1177/0731121416663685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *López Nancy, Vargas Edward D., Juarez Melina, Cacari-Stone Lisa, and Bettez Sonia. 2018. “What’s Your ‘Street Race’? Leveraging Multidimensional Measures of Race and Intersectionality for Examining Physical and Mental Health Status Among Latinxs.” Sociology of Race and Ethnicity 4(1): 49–66. doi: 10.1177/2332649217708798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall Leslie. 2005. “The Complexity of Intersectionality.” Signs 30(3): 1771–1800. doi: 10.1086/426800 [DOI] [Google Scholar]
- *McClendon Juliette, Jackson Joshua J., Bogdan Ryan, and Oltmanns Thomas F. 2019. “Trajectories of Racial and Gender Health Disparities During Later Midlife: Connections to Personality.” Cultural Diversity and Ethnic Minority Psychology 25(3): 359–370. doi: 10.1037/cdp0000238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mereish Ethan H., and Bradford Judith B. 2014. “Intersecting Identities and Substance Use Problems: Sexual Orientation, Gender, Race, and Lifetime Substance Use Problems.” Journal of Studies on Alcohol and Drugs 75: 179–188. doi: 10.15288/jsad.2014.75.179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merlo Juan. 2018. “Multilevel Analysis of Individual Heterogeneity and Discriminatory Accuracy (MAIHDA) Within an Intersectional Framework.” Social Science & Medicine 203: 74–80. doi: 10.1016/j.socscimed.2017.12.026 [DOI] [PubMed] [Google Scholar]
- Naimi Ashley I., Schnitzer Mireille E., Moodie Erica E. M., and Bodnar Lisa M. 2016. “Mediation Analysis for Health Disparities Research.” American Journal of Epidemiology 184(4): 315–324. doi: 10.1093/aje/kwv329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narváez Rafael F., Meyer Ilan H., Kertzner Robert M., Ouellette Suzanne C., and Gordon Allegra R. 2009. “A Qualitative Approach to the Intersection of Sexual, Ethnic, and Gender Identities.” Identity: An International Journal of Theory and Research 9(1): 63–86. doi: 10.1080/15283480802579375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nixon Stephanie A. 2019. “The Coin Model of Privilege and Critical Allyship: Implications for Health.” BMC Public Health 1637. doi: 10.1186/s12889-019-7884-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Nowakowski Alexandra C. H., and Sumerau JE 2017. “Health Disparities in Nonreligious and Religious Older Adults in the United States: A Descriptive Epidemiology of 16 Common Chronic Conditions.” Secularism and Nonreligion 6(4): 1–15. doi: 10.5334/snr.85 [DOI] [Google Scholar]
- *Parker Myra, Duran Bonnie, and Walters Karina. 2017. “The Relationship Between Bias-Related Victimization and Generalized Anxiety Disorder Among American Indian and Alaska Native Lesbian, Gay, Bisexual, Transgender, Two-Spirit Community Members.” International Journal of Indigenous Health 12(2): 64–83. doi: 10.18357/ijih122201717785 [DOI] [Google Scholar]
- *Pérez Ashley E., Gamarel Kristi E., van den Berg Jacob J., and Operario Don. 2018. “Sexual and Behavioral Health Disparities Among African American Sexual Minority Men and Women.” Ethnicity & Health. doi: 10.1080/13557858.2018.1444149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Perry Brea L., Pullen Erin L., and Oser Carrie B. 2012. “Too Much of a Good Thing? Psychosocial Resources, Gendered Racism, and Suicidal Ideation Among Low Socioeconomic Status African American Women.” Social Psychology Quarterly 75(4): 334–359. doi: 10.1177/0190272512455932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Perry Brea L., Harp Kathi L. H., and Oser Carrie B. 2013. “Racial and Gender Discrimination in the Stress Process: Implications for African American Women’s Health and Well-Being.” Sociological Perspectives 56(1): 25–48. doi: 10.1525/sop.2012.56.1.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Persmark Anna, Wemrell Maria, Evans Clare R., Subramanian SV, Leckie George, and Merlo Juan. 2019. “Intersectional Inequalities and the U.S. Opioid Crisis: Challenging Dominant Narratives and Revealing Heterogeneities.” Critical Public Health. 30(4): 398–414doi: 10.1080/09581596.2019.1626002 [DOI] [Google Scholar]
- Petticrew Mark, and Roberts Helen. 2006. Systematic Reviews in the Social Sciences: A Practical Guide. Oxford, UK: Blackwell Publishing. [Google Scholar]
- *Platt Lisa F., and Scheitle Christopher S. 2018. “Sexual Orientation and Psychological Distress: Differences by Race and Gender.” Journal of Gay & Lesbian Mental Health 22(3): 204–225. doi: 10.1080/19359705.2018.1437583 [DOI] [Google Scholar]
- Poulin Laura I. L., Skinner Mark W., and Hanlon Neil. 2020. “Rural Gerontological Health: Emergent Questions for Research, Policy, and Practice.” Social Science & Medicine 113065. doi: 10.1016/j.socscimed.2020.113065 [DOI] [PubMed] [Google Scholar]
- *Pudrovska Tetyana. 2014. “Early-Life Socioeconomic Status and Mortality at Three Life Course Stages: An Increasing Within-Cohort Inequality.” Journal of Health and Social Behavior 55(2): 181–195. doi: 10.1177/0022146514531986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Pudrovska Tetyana, Either Eric N., Logan Ellis S., and Sherman-Wilkins Kyler J. 2014. “Gender and Reinforcing Associations Between Socioeconomic Disadvantage and Body Mass over the Life Course.” Journal of Health and Social Behavior 55(3): 283–301. doi: 10.1177/0022146514544525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Richardson Liana J., and Brown Tyson H. 2016. “(En)gendering Racial Disparities in Health Trajectories: A Life Course and Intersectional Analysis.” SSM – Population Health 2: 425–435. doi: 10.1016/j.ssmph.2016.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Richman Aliza D. 2018. “Concurrent Social Disadvantages and Chronic Inflammation: The Intersection of Race and Ethnicity, Gender, and Socioeconomic Status.” Journal of Racial and Ethnic Health Disparities 5: 787–797. doi: 10.1007/s40615-017-0424-3 [DOI] [PubMed] [Google Scholar]
- *Rodriguez-Seijas Craig, Eaton Nicholas R., Panchankis John E. 2019. “Prevalence of Psychiatric Disorders at the Intersection of Race and Sexual Orientation: Results from the National Epidemiologic Survey of Alcohol and Related Conditions-III.” Journal of Consulting and Clinical Psychology 87(4): 321–331. doi: 10.1037/ccp0000377 [DOI] [PubMed] [Google Scholar]
- *Rosenfield Sarah. 2012. “Triple Jeopardy? Mental Health at the Intersection of Gender, Race, and Class.” Social Science & Medicine 74: 1791–1801. doi: 10.1016/j.socscimed.2011.11.010 [DOI] [PubMed] [Google Scholar]
- Scheim Ayden I., and Bauer Greta R. 2019. “The Intersectional Discrimination Index: Development and Validation of Measures of Self-Reported Enacted and Anticipated Discrimination for Intercategorical Analysis.” Social Science & Medicine 226: 225–235. doi: 10.1016/j.socscimed.2018.12.016 [DOI] [PubMed] [Google Scholar]
- Schwartz Seth J., Zamboanga Byron L., Luyckx Koen, Meca Alan, and Ritchie Rachel A. 2013. “Identity in Emerging Adulthood: Reviewing the Field and Looking Forward.” Emerging Adulthood 1(2): 96–113. doi: 10.1177/216769681347978 [DOI] [Google Scholar]
- *Seng Julia S., Lopez William D., Sperlich Mickey, Hamama Lydia, and Reed-Meldrum Caroline D. 2012. “Marginalized Identities, Discrimination Burden, and Mental Health: Empirical Exploration of an Interpersonal-Level Approach to Modeling Intersectionality.” Social Science & Medicine 75: 2437–2445. doi: 10.1016/j.socscimed.2012.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuey Kim M., and Willson Andrea E. 2008. “Cumulative Disadvantage and Black-White Disparities in Life-Course Health Trajectories.” Research on Aging 30(2): 200–225. doi: 10.1177/0164027507311151 [DOI] [Google Scholar]
- *Siordia Carlos. 2015. “Prevalence of Self-Care and Ambulatory Disability in Baby Boom and Generation-X Birth-Cohorts by Intersectional Markers of Social Stratification.” Race and Social Problems 7: 257–268. doi: 10.1007/s12552-015-9155-4 [DOI] [Google Scholar]
- Stueve Ann, and O’Donnell Lydia. 2008. “Urban Young Women’s Experiences of Discrimination and Community Violence and Intimate Partner Violence.” Journal of Urban Health 85: 386–401. doi: 10.1007/s11524-008-9265-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Combahee River Collective. 1977. “A Black Feminist Statement.” Pp. 272–282 in Home Girls: A Black Feminist Analogy, edited by Smith B New York: Kitchen Table: Women of Color Press. [Google Scholar]
- Thoits Peggy A. 2010. “Stress and Health: Major Findings and Policy Implications.” Journal of Health and Social Behavior 51(S): S41–S53. doi: 10.1177/0022146510383499 [DOI] [PubMed] [Google Scholar]
- *Thomeer Mieke Beth. 2013. “Sexual Minority Status and Self-Rated Health: The Importance of Socioeconomic Status, Age, and Sex.” American Journal of Public Health 103: 881–888. doi: 10.2105/AJPH.2012.301040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Trinh Mai-Han, Agenor Madina, Austin S. Bryn, and Jackson Chandra L. 2017. “Health and Healthcare Disparities Among U.S. Women and Men at the Intersection of Sexual Orientation and Race/Ethnicity: A Nationally Representative Cross-Sectional Study.” BMC Public Health 17: 964. doi: 10.1186/s12889-017-4937-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner Caitlin M., Arayasirikul Sean, and Wilson Erin C. 2021. “Disparities in HIV-Related Risk and Socioeconomic Outcomes Among Trans Women in the Sex Trade and Effects of a Targeted, Anti-Sex-Trafficking Policy.” Social Science & Medicine 113664. doi: 10.1016/j.socscimed.2020.113664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2008. Phase I Report: Recommendations for the Framework and Formation of Healthy People 2020. Washington, DC: The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives; for 2020. [Google Scholar]
- VanderWeele Tyler J. 2014. “A Unification of Mediation and Interaction: A Four-Way Decomposition.” Epidemiology 25(5): 749–761. doi: 10.1097/EDE.0000000000000121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Van Dyke, Miriam E, Vaccarino Viola, Dunbar Sandra B., Pemu Priscilla, Gibbons Gary H., Quyyumi Arshed A., and Lewis Tene T. 2017. “Socioeconomic Status Discrimination and C-Reactive Protein in African-American and White Adults.” Psychoneuroendocrinology 82: 9–16. doi: 10.1016/j.psyneuen.2017.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Versey H. Shellae, and Kaplan George A. 2012. “Mediation and Moderation of the Association Between Cynical Hostility and Systolic Blood Pressure in Low-Income Women.” Health Education & Behavior 39(2): 219–228. doi: 10.1177/1090198111414884 [DOI] [PubMed] [Google Scholar]
- Viruell-Fuentes Edna A., Miranda Patricia Y., and Abdulrahim Sawsan. 2012. “More than Culture: Structural Racism, Intersectionality Theory, and Immigrant Health.” Social Science & Medicine 75: 2099–2106. doi: 10.1016/j.socscimed.2011.12.037 [DOI] [PubMed] [Google Scholar]
- *Vu Milkie, Li Jingjing, Haardorfer Regine, Windle Michael, and Berg Carla J. 2019. “Mental Health and Substance Use Among Women and Men at the Intersections of Identities and Experiences of Discrimination: Insights from the Intersectionality Framework.” BMC Public Health 19: 108. doi: 10.1186/s12889-019-6430-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Walsemann Katrina M., Goosby Bridget J., and Farr Deeonna. 2016. “Life Course SES and Cardiovascular Risk: Heterogeneity Across Race/Ethnicity and Gender.” Social Science & Medicine 152: 147–155. doi: 10.1016/j.socscimed.2016.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Warner David F., and Brown Tyson H. 2011. “Understanding How Race/Ethnicity and Gender Define Age-Trajectories of Disability: An Intersectional Approach.” Social Science & Medicine 72: 1236–1248. doi: 10.1016/j.socscimed.2011.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbrook Laurel, and Saperstein Aliya. 2015. “New Categories Are Not Enough: Rethinking the Measurement of Sex and Gender in Social Surveys.” Gender & Society 29(4): 534–560. doi: 10.1177/0891243215584758 [DOI] [Google Scholar]
- *Williamson Timothy J., Mahmood Zanjbeel, Kuhn Taylor P., and Thames April D. 2017. “Differential Relationships Between Social Adversity and Depressive Symptoms by HIV-Status and Racial/Ethnic Identity.” Health Psychology 36(2): 133–142. doi: 10.1037/hea0000458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Wilson Erin C., Chen Yea-Hung, Arayasirikul Sean, Raymond H. Fisher, and McFarland Willi. 2016. “The Impact of Discrimination on the Mental Health of Tran*Female Youth and the Protective Effect of Parental Support.” AIDS and Behavior 20: 2203–2211. doi: 10.1007/s10461-016-1409-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. 2011. Closing the Gap: Policy into Practice on Social Determinants of Health. Rio de Janeiro, Brazil: World Conference on Social Determinants of Health. [Google Scholar]
- Yang Claire Yang, Schorpp Kristen, Boen Courtney, Johnson Moira, and Harris Kathleen Mullan. 2020. “Socioeconomic Status and Biological Risks for Health and Illness Across the Life Course.” Journals of Gerontology: Social Sciences 75(3): 613–624. doi: 10.1093/geronb/gby108 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.