A 36-year-old man with moderate-to-severe left neck pain, local swelling, and tenderness was seen at the emergency room. Over the prior 4 days he had received beta-lactam antibiotic therapy with no improvement. One month before he experienced mild symptomatic coronavirus disease 2019 (COVID-19). The PCR-based test performed at the emergency room was still positive. The remaining personal history was negative. The routine laboratory parameters were within reference range and autoimmunity screening results were negative (Table 1 ).
Table 1.
Laboratory results.
| Normal value | Patient’s value | |
|---|---|---|
| Rheumatoid factor | 0–14 U/mL | 6.3 |
| Beta2-microglobulin | 0.8–2.4 mg/L | 2.3 |
| Interleukin 6 | 0–7 pg/mL | 1.5 |
| ANA | Pos 1:160 | Negative |
| IgA EMA | Negative | Negative |
| ANCA | Negative <1:20 | Negative |
| Anti- MPO | Negative <3.5 | 0.1 |
| Anti-PR3 | Negative <2 | 0.1 |
ANA, anti-nuclear antibodies; IgA EMA, IgA anti-endomysial antibodies; ANCA, anti-neutrophil cytoplasmic antibodies; Anti-MPO, anti-myeloperoxidase antibodies; Anti-PR3, anti-proteinase-3 antibodies.
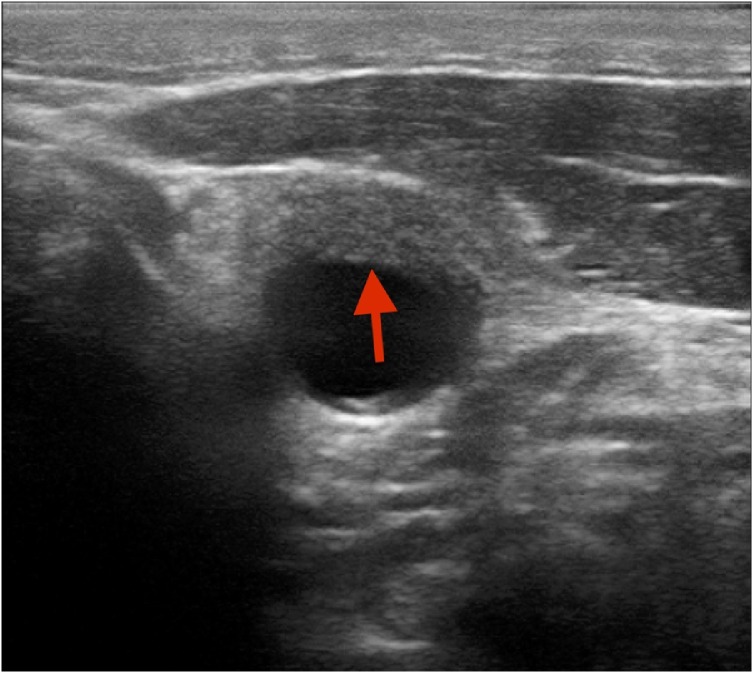
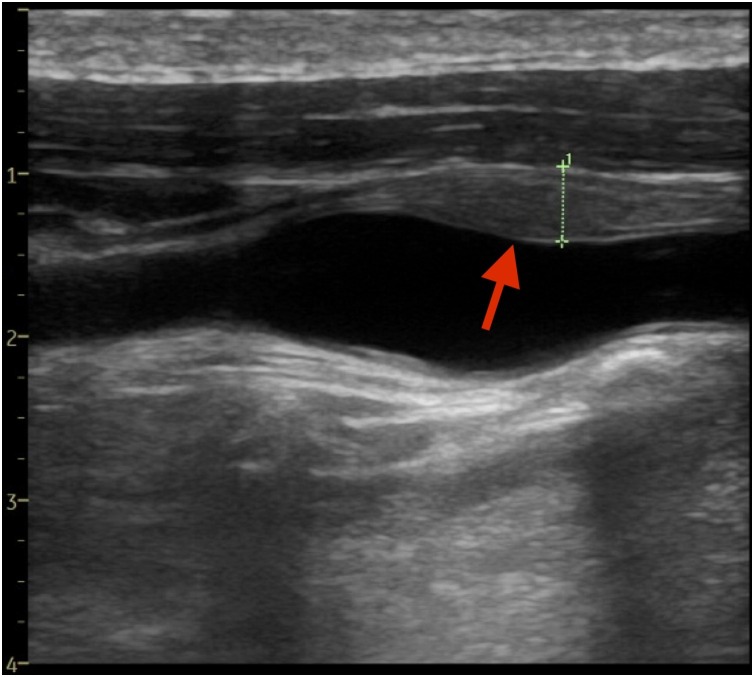
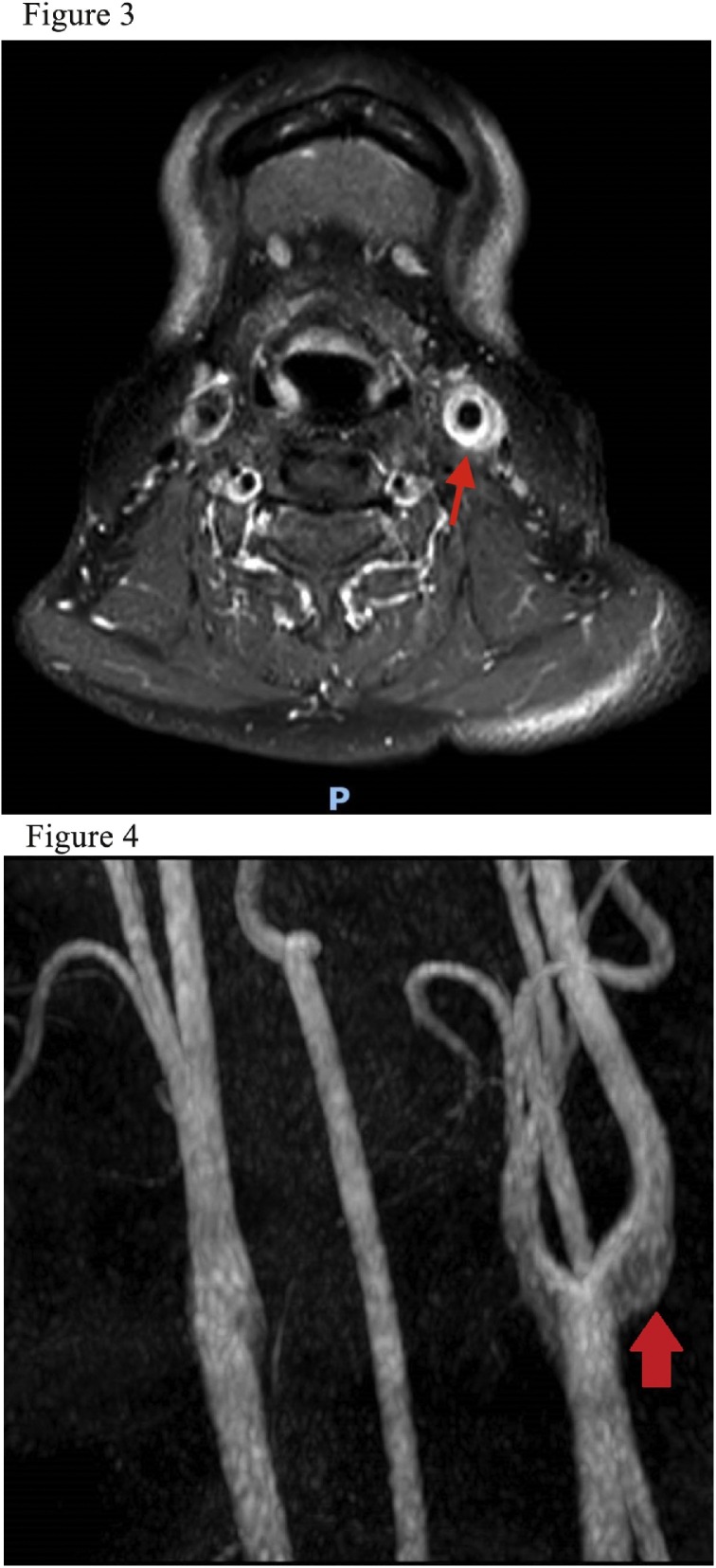
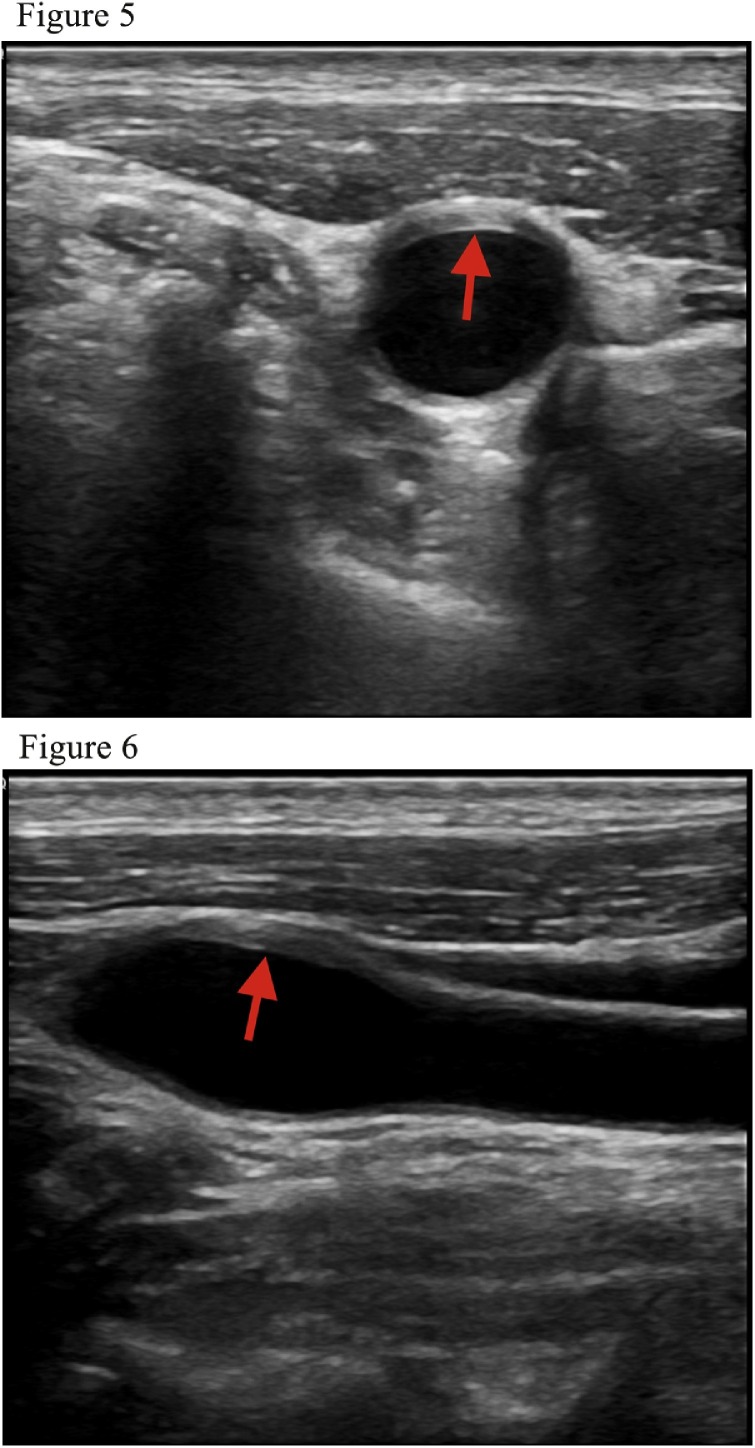
A carotid ultrasonography demonstrated eccentric hypo-/isoechoic smooth abnormal soft tissue (Figures A-1 and A-2 , red arrows) surrounding the carotid artery bifurcation and in the proximal internal carotid artery, with a thickness diameter of 5 mm and median length of 2 cm. No hemodynamically relevant stenosis or atherosclerotic plaques were present. Nuclear magnetic resonance confirmed the ultrasonographic findings concerning the size of the lesion and showed local contrast enhancement, as well as reactive lymphadenopathy, suggesting a focal vasculitis (Figures A-3 and A-4 , red arrows). Computed tomography angiography showed no thrombosis or carotid artery dissection and positron emission tomography did not show pathological areas of increased uptake along other vessels. The patient received levofloxacin and painkillers for 5 days. After one month, he was asymptomatic and a subsequent ultrasonographic exam showed no alterations of the carotid arteries (Figures B-1 and B-2 , red arrows).
Figure A-1.
Axial carotid ultrasonography shows eccentric hypo-/isoechoic smooth abnormal soft tissue (red arrows) in the proximal internal carotid artery with a thickness diameter of 5 mm.
Figure A-2.
Longitudinal carotid ultrasonography shows eccentric hypo-/isoechoic smooth abnormal soft tissue (red arrows) surrounding the carotid artery bifurcation and in the proximal internal carotid artery with a median length of 2 cm.
Figures A-3 and A-4.
Nuclear magnetic resonance shows local contrast enhancement and reactive lymphadenopathy, suggesting a focal vasculitis (red arrows).
Figure B-1 (axial) and B-2 (longitudinal).
After one month, carotid ultrasonography shows no alterations of the carotid arteries (red arrows).
A final diagnosis of transient perivascular inflammation of the carotid artery (TIPIC) syndrome (previously known as “carotidynia”) was made (Lecler et al., 2017). It is believed that this is the first published case of TIPIC syndrome associated with COVID-19. SARS-CoV2 causing COVID-19 can promote endothelial cell infection and inflammation (Varga et al., 2020). The carotid body could be a site of virus invasion due to local expression of angiotensin-converting enzyme receptors (Porzionato et al., 2020). Although no causal relationship between COVID-19 and TIPIC syndrome could be demonstrated in this patient, this observation should serve to generate hypotheses and must be confirmed in future studies with an appropriate design and size.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Funding source
There is no funding source.
Ethical approval
Not applicable.
References
- Lecler A., Obadia M., Savatovsky J. TIPIC syndrome: beyond the myth of carotidynia, a new distinct unclassified entity. AJNR Am J Neuroradiol. 2017;38(7):1391–1398. doi: 10.3174/ajnr.A5214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porzionato A., Emmi A., Stocco E. The potential role of the carotid body in COVID-19. Am J Physiol Lung Cell Mol Physiol. 2020;319(4) doi: 10.1152/ajplung.00309.2020. L620–L6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varga Z., Flammer A.J., Steiger P. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]