Abstract
There are different methods of artificial liver support for patients with acute liver dysfunction (ALD). However, CytoSorb (CS) might be a new approved option for those patients. Question of interest is whether the elimination performance of CS was comparable to that of advanced organ support (ADVOS). Patients, treated with CS (integrated into high-flux dialysis) or ADVOS and a total bilirubin > 10 mg/dl were included. Laboratory parameters were evaluated before starting therapy (d0) and 12–24 h thereafter (d1). The Wilcoxon-test with associated samples was used for statistical analysis. Thirty-nine patients (33 CS, 6 ADVOS) were included. The median bilirubin at d0 was 16.9 and 17.7 mg/dl and at d1 was 13.2 and 15.9 mg/dl, in the CS and ADVOS group, respectively. There was a significant bilirubin reduction as well in the CS group (p < 0.001, median relative reduction: 22.5%) as in the ADVOS group (p = 0.028, median relative reduction: 22.8%). There was no significant difference in the relative bilirubin reduction between CS and ADVOS therapies. The use of CytoSorb and ADVOS in patients with ALD led to a significant and comparable decrease in total bilirubin. The easy use of CS might be an advantage compared to other procedures.
Subject terms: Liver diseases, Hepatotoxicity
Introduction
Despite the further development of modern intensive care medicine, acute liver dysfunction (ALD) is associated with high mortality in intensive care unit (ICU) patients1. The different entities of liver failure are divided into primary and secondary reasons. Reasons for primary liver dysfunction are hepatotoxic medication or viral infection, leading to an acute liver failure (ALF)2,3. More often, liver failure occurs secondarily due to cholestasis and hypoxic liver injury as the most important reasons for ALD in the critically ill4. Secondary ALD can also be caused by sepsis or cardiac shock with an acute and possible irreversible dysfunction of the hepatocytes5. However, there is no uniform definition of ALD in critically ill patients. In conclusion, both forms can result in coagulopathy, encephalopathy, and increase in cholestasis and liver integration parameters.
The main problem associated with ALD, especially when caused by cholestasis, is that toxic substances, such as bile acids (BAs), are no longer removed from the liver. The accumulation in the blood and liver can result in permanent damage of the hepatocytes6. Furthermore, the accumulation of ammonia can lead to cerebral edema with the risk of persistent cerebral injury7.
Bilirubin is a surrogate parameter for cholestatic impairment and may reflect impaired biliary secretion8. Horvatits et al. showed that the level of BAs is correlated with bilirubin serum levels in the critically ill. Thus, bilirubin can be used to estimate the amount of BA, because its quantification is less widely established than the quantification of bilirubin9. Hence, critically ill patients, with higher bilirubin levels in the blood, were found to have higher mortality compared to those with normal bilirubin levels10,11.
The main aim in the treatment of ALD is to prevent patients from permanent hepatocyte damage, which often leads to liver transplantation or death12. Therefore, metabolic disorder, coagulation disorder, neurological disorder, and sepsis caused by different pathogens should be treated as effectively as possible as a supportive therapeutic concept13.
In addition to these regimens, liver support systems are an option for supportive therapy. The concept of these systems is to clear blood of hepatotoxic substances, such as cytokines, BA, and endotoxins to avoid further damage of the hepatocytes. A recently published systematic meta-analysis showed evidence of the reduction in mortality with liver support systems14. However, different systems are available. One opportunity is to implement plasma exchange, which can improve outcomes15, but is expensive and can lead to hypotension and bleeding complications16,17. Another approach is albumin dialysis, for example, with Advanced Organ Support (ADVOS) or MARS18,19. ADVOS is an advanced hemodialysis system combining different forms of organ support (kidney, lung, liver) using three circuits: the extracorporeal blood circuit, the dialysate circuit, and the albumin multi circuit. It aims to remove water-bound and albumin-bound toxins, in addition to CO2, and correct acid–base disturbances. Although case studies have shown this effect, it has not yet been established in daily intensive care practice20,21.
Since 2017, case reports have described the elevation of bilirubin and BA and the support of liver excretory function using the cytokine adsorber CytoSorb (CS)22–24. Furthermore, Calabró et al. published the first clinical trial that evaluated the effect of CS on bilirubin levels in 40 critically ill patients25. In 2019, Gemelli et al. described the in vitro kinetics of the elimination of bilirubin via CS as a novel tool that can be used in patients with ALD26.
In the context of clinical routine, ADVOS dialysis and CS were used at two ICUs at the LMU hospital in patients with ALD. There is a lack of data assessing the effect of CS in patients with ALD, particularly compared with other liver support systems such as ADVOS. Therefore, a retrospective data analysis was performed including patients between April 2015 and May 2020. The effectiveness of both systems, particularly with respect to total bilirubin elimination, was evaluated and compared.
Methods
Study setting
This was a monocentric, retrospective observational study investigating the influence of ADVOS and CS therapy in critically ill patients with acute liver dysfunction (ALD). Patients were included between April 2015 and May 2020 during their stay at two ICUs at the LMU hospital, Munich.
Laboratory testing and data collection
All clinical chemical parameters were determined with standard clinical chemistry tests at the institute of laboratory medicine. For data evaluation, demographic data, clinical variables, and laboratory variables were collected from the laboratory and patient information system. Baseline characteristics (age, gender, body mass index (BMI), extracorporeal membrane oxygenation (ECMO), 7-day mortality, in-hospital mortality, sequential organ failure assessment (SOFA) score, Simplified Acute Physiology Score (SAPS), model end stage liver disease (MELD) score, norepinephrine demand, reason for admission to ICU, and reason for ALD were evaluated on the treatment day. Laboratory data were collected one day before and during the intervention.
Study population
All patients, who were treated with CS (integrated into high-flux dialysis (Fresenius Ultraflux AV 600S, surface area 1.4 m2)) or ADVOS, were screened for evaluation. Patients were only included in the study population when the therapy was longer than 90 min, total bilirubin level in the serum was > 10 mg/dl before the start of therapy, and bilirubin was measured 12–24 h after starting therapy. Figure 1 shows, based on the screened primary patients, the patients excluded in each case by the exclusion criteria. The remaining patients are the study population presented below. Regardless of the number of treatments with CS or ADVOS received by patients during their stay at the ICU, only the first treatment with the indication “acute liver dysfunction or hyperbilirubinemia” was evaluated. The treating physician was responsible for establishing the indication and selecting the liver replacement procedure.
Figure 1.
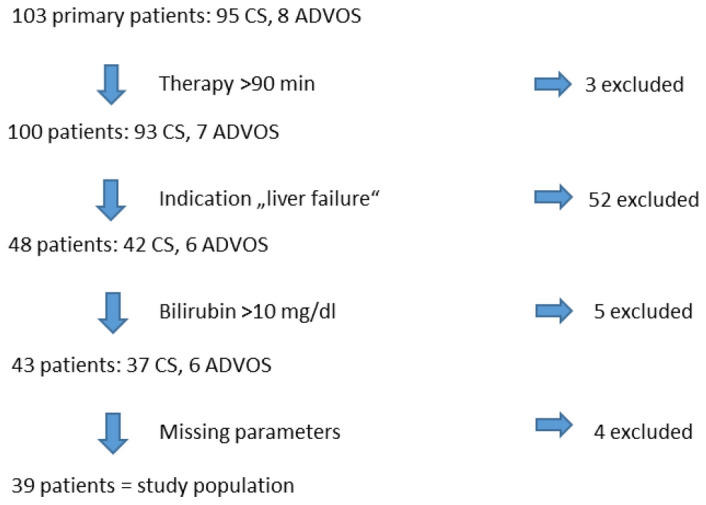
Selection of the study population. CS: CytoSorb, ADVOS: advanced organ support.
Blood sampling
In the data evaluation, three timepoints were considered depending on CS or ADVOS treatment:
d−1: 24–36 h before start of ADVOS/CS
d0: 0–12 h before the start of ADVOS/CS
d1: 12–24 h after starting ADVOS/CS (= end of ADVOS/CS)
Statistical analysis
Statistical analysis was performed with IBM SPSS statistics (Version 26.0. IBM Corp., Armonk, NY, USA) and Python (Version 3.5.2, Packages Pandas 0.24.2 and scipy 1.4.1). Because the laboratory variables did not have a normal distribution according to the Shapiro–Wilk test, non-parametric tests were used. Continuous variables are given as median and interquartile range (IQR) or with minimum and maximum. U-test was used to identify differences in baseline parameters in both groups. The effect of CS and ADVOS treatment on the reduction in total bilirubin, serum alanine aminotransferase (ALT), serum aspartate aminotransferase (AST), glutamine-glutamyl transferase (GGT), alkaline phosphatase (AP), norepinephrine demand, and SAPS II was investigated. To describe the change of these parameters before and during blood purification, the Wilcoxon test with associated samples was used. Furthermore, it was used to identify differences in the bilirubin elimination of CS and ADVOS patients. The relative change of the parameters (%) was calculated with: 100 − ((100/parameter d0) * parameter d1).
Ethics approval and consent to participate
Ethical approval was obtained from the ethical review committee of the Ludwig-Maximilians-Universität (registration number 20-477). Data collection was in accordance with the review board and therefore with all valid guidelines. Informed consent of the patients is given as part of the ethics approval process.
Results
Demographic and clinical data
In total, 39 patients (33 CS, 6 ADVOS) were included in the evaluation. Reason for admission to the ICU in patients treated with CS was, in descending order: ARDS (24.2%), septic shock (15.2%), polytrauma (15.2%), liver transplantation (12.1%), ALF (12.1%), lung transplantation (6.1%), cardiogenic shock (6.1%), and other reasons (9.0%). The reasons for admission in patients treated with ADVOS were acute liver failure (50.0%), cardiogenic shock (33.3%), and liver transplantation (16.7%). The reasons for ALD in both groups were, in descending order: septic multiorgan failure (25.6%), hypoxic liver failure (23.1%), acute-on-chronic liver failure (17.9%), liver graft failure (12.8%), secondary sclerosing cholangitis (10.3%), and different reasons (10.3%). Seven patients had a preexisting liver cirrhosis. The reasons for hypoxic liver failure were hemorrhagic shock, cardiogenic shock and pulmonary embolism. The median age was 55 years and 69% of the patients were male. An ECMO therapy was necessary in 29% of the patients and the in—hospital mortality was 82%. The median SAPS II at the treatment day (d0) was 80 points, indicating a mortality of 92.5%. The median MELD score before therapy was 35 points. Detailed patient characteristics are displayed in Table 1.
Table 1.
Patient characteristics.
| All patients: n (%) or median [range: min, max] | CytoSorb: n (%) or median [Range: min, max] | ADVOS: n (%) or median [Range: min, max] | Differences in both groups (p-value) | |
|---|---|---|---|---|
| No. of patients | 39 (100) | 33 (100) | 6 (100) | |
| Age, years | 55 [18, 80] | 55 [18, 76] | 46 [19, 80] | 0.84 |
| Gender, male/female | 27 (69.2) / 12 (30.8) | 23 (69.7)/10 (30.3) | 4 (66.7) / 2 (33.3) | 0.92 |
| BMI, kg/m2 | 27.7 [16.2, 55.1] | 27.8 [16.2, 55.1] | 26.0 [18.8, 35.2] | 0.56 |
| ECMO therapy | 11 (28.2) | 10 (30.3) | 1 (16.7) | 0.61 |
| 7-days mortality | 12 (30.8) | 10 (30.3) | 2 (33.3) | 0.92 |
| In-hospital mortality | 32 (82.1) | 28 (84.8) | 4 (66.7) | 0.51 |
| SOFA score d0 | 20 [12, 23] | 20 [12, 23] | 21 [18, 23] | 0.48 |
| SAPS II d0 | 80 [47, 111] | 80 [47, 109] | 72 [50,111] | 0.53 |
| MELD score d0 | 35.0 [25.4, 52.9] | 33.6 [25.4, 52.9] | 38.5 [30.5, 44.8] | 0.10 |
| MELD score d1 | 34.4 [25.8, 52.3] | 33.8 [25.8, 52.3] | 38.5 [30.1, 45.8] | 0.23 |
| Total bilirubin (mg/dl) d-1 | 16.8 [4.2, 40.2] | 14.2 [4.2, 40.2] | 18.5 [11.7, 26.9] | 0.35 |
| Total bilirubin (mg/dl) d0 | 17.3 [10.2, 41.1] | 16.9 [10.2, 41.1] | 17.7 [10.7, 28.0] | 0.89 |
| Total bilirubin (mg/dl) d1 | 13.3 [5.2, 25.6] | 13.2 [5.2, 25.6] | 15.9 [6.8, 21.9] | 0.81 |
SOFA, sequential organ failure assessment; SAPS, Simplified Acute Physiology Score; ADVOS, advanced organ support; BMI, body mass index; ECMO, extracorporeal membrane oxygenation.
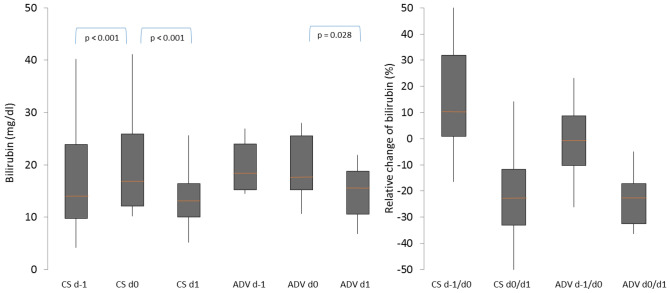
Effect of CytoSorb and ADVOS on bilirubin elimination
The relative change (%) in total bilirubin during the time periods (d − 1/d0) and (d0/d1) for both CS and ADVOS therapy was analyzed. There was a significant increase in total bilirubin in the period prior to CS treatment (p < 0.001) with a median relative increase of 10.3% (IQR: 8.8, 31.9%). In contrast, there was no significant change of total bilirubin in the period prior to ADVOS therapy (p = 0.917) with a median relative change of − 6.6% (IQR: − 10.2, 8.8%). There was also a significant decrease in total bilirubin during CS therapy (p < 0.001; median relative change 22.5% (IQR: 11.8, 33.1%)) and during ADVOS treatment (p = 0.028; median relative change 22.8% (IQR: 17.1, 32.5%)). However, there was no significant difference in bilirubin elimination in both groups. Figure 2 shows the course of total bilirubin and relative change of bilirubin prior and during CS and ADVOS therapies as box plots.
Figure 2.
Development and relative reduction in bilirubin levels in patients with CytoSorb and ADVOS therapy. d–1: day before treatment, d0: shortly before treatment, d1: directly after treatment, CS: CytoSorb, ADV: advanced organ support; orange line represents the median, grey boxes the interquartile range and the whiskers are limited to 1.5 times the interquartile range.
Changes of other parameters during blood purification
Other relevant parameters in patients with ALD are ALT, AST, GGT, and AP. Moreover, relevant outcome parameters are the reduction of norepinephrine, and the reduction of SAPS II. The change in these parameters during CS therapy and ADVOS therapy (d0–d1) was analyzed. Table 2 displays both the primary data and the statistical results. There was a significant reduction in ALT (p = 0.007), AST (p = 0.016), GGT (p = 0.013), SAPS II (p = 0.01) and norepinephrine demand (p = 0.012) in patients treated with CS. A significant change was not seen in patients with ADVOS therapy.
Table 2.
Changes in different parameters during blood purification.
| Parameter | CS therapy | ADVOS therapy | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | z-value | p-value | Mean | SD | z-value | p-value | |
| ALT (U/l) d0 | 614 | 1707 | 620 | 1067 | ||||
| ALT (U/l) d1 | 395 | 1112 | 462 | 725 | ||||
| ΔALT (d0–d1) | 219 | 715 | − 2.68 | 0.007* | 159 | 344 | − 0.52 | 0.600 |
| AST (U/l) d0 | 1512 | 4338 | 1211 | 2525 | ||||
| AST (U/l) d1 | 1033 | 3003 | 951 | 1827 | ||||
| ΔAST (d0–d1) | 479 | 1447 | − 2.41 | 0.016* | 260 | 709 | − 0.31 | 0.753 |
| GGT (U/l) d0 | 307 | 392 | 369 | 398 | ||||
| GGT (U/l) d1 | 276 | 375 | 356 | 392 | ||||
| ΔGGT (d0–d1) | 32 | 78 | − 2.50 | 0.013* | 13 | 37 | − 0.67 | 0.500 |
| AP (U/l) d0 | 390 | 92 | ||||||
| AP (U/l) d1 | 364 | 81 | ||||||
| ΔAP (d0–d1) | 26 | 67 | − 1.19 | 0.233 | ||||
| SAPS II d0 | 79 | 14 | 76 | 20 | ||||
| SAPS II d1 | 73 | 11 | 77 | 17 | ||||
| ΔSAPS II (d0–d1) | 6 | 9 | − 3.3 | 0.01* | − 1 | 6 | − 0.3 | 0.79 |
| Nor (mg/dl) d0 | 2.0 | 2.5 | 2.0 | 1.5 | ||||
| Nor (mg/dl) d1 | 1.4 | 1.2 | 1.5 | 1.4 | ||||
| ΔNor (d0–d1) | 0.6 | 1.7 | − 2.5 | 0.012* | 0.5 | 1.3 | − 0.81 | 0.41 |
CS: CytoSorb, ADVOS: advanced organ support, CI: confidence interval, SD: standard deviation, ALT: serum alanine aminotransferase, AST: serum aspartate aminotransferase, GGT: glutamine-glutamyl transferase, AP: alkaline phosphatase, SAPS: Simplified Acute Physiology Score, Nor: norepinephrine demand, d: day.
Discussion
ALD is a common syndrome in critically ill patients with a variety of underlying conditions8. The increase in total bilirubin can be an expression of cholestasis or acute damage of the hepatocytes, and the sources causing the dysfunction are often not directly treatable. Therefore, symptomatic therapy is of great importance13. Since there is no clear description of ALD in the literature and liver replacement procedures are only considered in cases of severe hepatic impairment, we used a severely elevated bilirubin of > 10 mg/dl as an inclusion criterion. Due to this inclusion criterion, only extremely ill patients were included in our study population. This is reflected in the high median MELD score of 35 points, the high median SAPS II of 80 points, and an in-hospital mortality rate of 82%. Therefore, the mortality rate was lower than expected according to SAPS II (expected mortality: 92.5%). However, in the absence of a control group, it is not possible to make a statement about a reduction in mortality with the use of liver support systems. Nevertheless, other authors also dare to compare actual mortality with predicted mortality and also see lower values in observed mortality, as our study did27.
In contrast to newborns, hyperbilirubinemia in adult patients with an intact blood–brain barrier does not lead to direct toxic side effects28. However, bilirubin is an easy to measure surrogate parameter for the accumulation of BA in the critically ill29, because BA cannot be routinely determined, even in large clinics, due to a less widely established method30. An increase in BA can lead to potentially permanent damage to the hepatocytes, particularly in the case of cholestasis, endothelial injury in the kidney and lung tissues, and destruction of the erythrocytes31,32. Therefore, the use of liver support systems is very appropriate in cases of severe hepatic dysfunction.
Various blood purification systems are available as supportive therapeutic measures to eliminate toxic substances in patients with ALD33. In particular, methods of albumin dialysis have been frequently used in the past19. A recent publication on the use of ADVOS describes a moderate but significant decrease in bilirubin (6.9 → 6.5 mg/dl). This could also be due to the fact that bilirubin was only modestly elevated at baseline27. However, these systems are complex and expensive. In addition a survival benefit has not been demonstrated in a randomized study population34,35. This might explain why few patients have been treated with ADVOS at our ICU. However, a recently published meta-analysis on different liver support systems showed a reduction in mortality and an improvement in hepatic encephalopathy without favoring a special kind of device14. Therefore, it is important to know whether a new therapeutic option such as CS works at least as well as proven approaches such as ADVOS. According to the manufacturer's information, CS has a surface area of about 45,000 m2 and can eliminate molecules up to a size of 55 kDa. This includes the substances ammonia, bilirubin, and most bile acids26,33. However, with a molecule size of only 17 Da, ammonia can easily be removed by high-flux dialysis36. Since ammonia was not determined frequently enough in routine clinical practice, no statement can be made on this in our study. In contrast, although a significant reduction in AST (92 kDa), ALT (110 kDa), and GGT (64 kDa) occurred during CS treatment, these substances cannot be adsorbed by CS due to their molecular size. Therefore, the significant decrease during CS treatment might already reflect an improvement of liver function. In-vivo studies with measurement of these substances at the adsorbers’ in- and outlet could be useful to rule out clearance by CS. An elimination of transaminases also cannot be assumed to occur with ADVOS therapy. The absence of a reduction during ADVOS therapy might be explained by the small sample size.
In addition to the lower than expected mortality and the reduction in bilirubin, there was also a significant reduction in norepinephrine demand with the use of CS, resulting in hemodynamic stabilization. This could subsequently lead to better perfusion of the liver and thus also, if given, control the cause of ALD. The significant reduction in SAPS II during CS is another indicator of an improvement in the patient's outcome.
Our study showed that total bilirubin was effectively removed in both groups. Because there was no significant difference between the procedures, they can be considered to be at least equivalent in this respect. There was a significant increase in bilirubin prior to CS therapy, whereas bilirubin decreased in the ADVOS group. An increase in bilirubin before therapy could be indicative of worsening liver dysfunction. Therefore, it is possible that we have underestimated the effect of CS on the reduction in bilirubin because further accumulation during CS might occur due to ongoing hepatic injury. However, the data available on the therapy of ALD in general, and the use of blood purification systems in particular, remain insufficient17,20,37. Precisely because alternative systems are complex and difficult to use, CS could be a user-friendly alternative that can be easily integrated in, for example, high-flux dialysis. Recently, Tomescu et al. showed an improvement in liver functional tests using CS in patients with ALF38. Since 2019, CS has had a CE-mark (marking of conformity for medical devices) for the elimination of bilirubin22,33.
The present study has several limitations. Liver support therapy and measurement of laboratory parameters was performed in clinical routines, so a slight deviation of timepoints cannot be excluded. Furthermore, total bilirubin was used as a surrogate parameter for the BA level, because quantification was not available. A prospective study describing the effect of BA elimination would be desirable. Moreover, small amounts of total bilirubin can also be eliminated by high-flux dialysis and the elimination was therefore a combination of CS therapy and high-flux dialysis. Because there was no control group, advantages in terms of faster recovery of liver function or mortality cannot be established, and spontaneous changes in liver function cannot be assessed. It should also be noted that due to the difference in size of the groups and the lack of randomization, a significant difference between the two groups might not have been detected. Additionally, ADVOS was only available until 2017, so the treating physician had no longer the opportunity to choose between both systems. Furthermore, as data collection was over five years, a change in treatment decisions over time is possible. However, as guidelines did not differ in terms of liver support systems over the study period, different patient selection can be ruled out.
Conclusion
Liver support systems play an important role in the supportive therapy of patients with ALD, although they are often difficult to use and have many side effects. The use of ADVOS and CytoSorb (integrated into high-flux dialysis) led to a significant and comparable decrease in bilirubin in critically ill patients. An advantage of CS is its easy integration into high-flux dialysis, which allows its use at smaller hospitals. Prospective studies should follow to demonstrate further benefits of liver support, such as a decrease in mortality in patients with ALD.
Abbreviations
- ADVOS
Advanced organ support
- ALD
Acute liver dysfunction
- ALF
Acute liver failure
- ALT
Serum alanine aminotransferase
- AP
Alkaline phosphatase
- AST
Serum aspartate aminotransferase
- BA
Bile acid
- BMI
Body mass index
- ECMO
Extracorporeal membrane oxygenation
- GGT
Glutamine-glutamyl transferase
- ICU
Intensive care unit
- MELD
Model end stage liver disease
- SAPS
Simplified acute physiology score
- SOFA
Sequential organ failure assessment
Author contributions
C.S. and I.S. designed the study. C.S. was responsible for the acquisition of demographic and clinical data. C.S. and A.B.P. did the statistical analysis. C.S. and I.S. interpreted the results and wrote the manuscript. U.L., M.P., M.I. and M.Z. participated in study design and interpretation of results. All authors meet key authorship requirements and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
All data generated during this study are included in this article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Reuben A, et al. Outcomes in adults with acute liver failure between 1998 and 2013: an observational cohort study. Ann. Intern. Med. 2016;164(11):724–732. doi: 10.7326/M15-2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stravitz RT, Lee WM. Acute liver failure. Lancet. 2019;394(10201):869–881. doi: 10.1016/S0140-6736(19)31894-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Real M, et al. Drug-induced liver injury: highlights of the recent literature. Drug Saf. 2019;42(3):365–387. doi: 10.1007/s40264-018-0743-2. [DOI] [PubMed] [Google Scholar]
- 4.Horvatits T, Trauner M, Fuhrmann V. Hypoxic liver injury and cholestasis in critically ill patients. Curr. Opin. Crit. Care. 2013;19(2):128–132. doi: 10.1097/MCC.0b013e32835ec9e6. [DOI] [PubMed] [Google Scholar]
- 5.Lelubre C, Vincent JL. Mechanisms and treatment of organ failure in sepsis. Nat. Rev. Nephrol. 2018;14(7):417–427. doi: 10.1038/s41581-018-0005-7. [DOI] [PubMed] [Google Scholar]
- 6.Li T, Apte U. Bile acid metabolism and signaling in cholestasis, inflammation, and cancer. Adv. Pharmacol. 2015;74:263–302. doi: 10.1016/bs.apha.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kerbert AJ, Engelmann C, Jalan R. Neurocritical care management of hepatic encephalopathy and coma in liver failure. Semin. Respir. Crit. Care Med. 2018;39(5):523–537. doi: 10.1055/s-0038-1672180. [DOI] [PubMed] [Google Scholar]
- 8.Jenniskens M, et al. Cholestatic liver (dys)function during sepsis and other critical illnesses. Intensive Care Med. 2016;42(1):16–27. doi: 10.1007/s00134-015-4054-0. [DOI] [PubMed] [Google Scholar]
- 9.Horvatits T, et al. Liver injury and failure in critical illness. Hepatology. 2019;70(6):2204–2215. doi: 10.1002/hep.30824. [DOI] [PubMed] [Google Scholar]
- 10.Vitek L, et al. Association between plasma bilirubin and mortality. Ann. Hepatol. 2019;18(2):379–385. doi: 10.1016/j.aohep.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Kramer L, et al. Incidence and prognosis of early hepatic dysfunction in critically ill patients—a prospective multicenter study. Crit. Care Med. 2007;35(4):1099–1104. doi: 10.1097/01.CCM.0000259462.97164.A0. [DOI] [PubMed] [Google Scholar]
- 12.Olivo R, Guarrera JV, Pyrsopoulos NT. Liver transplantation for acute liver failure. Clin. Liver Dis. 2018;22(2):409–417. doi: 10.1016/j.cld.2018.01.014. [DOI] [PubMed] [Google Scholar]
- 13.Khan R, Koppe S. Modern management of acute liver failure. Gastroenterol. Clin. North Am. 2018;47(2):313–326. doi: 10.1016/j.gtc.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Alshamsi F, et al. Extracorporeal liver support in patients with liver failure: a systematic review and meta-analysis of randomized trials. Intensive Care Med. 2020;46(1):1–16. doi: 10.1007/s00134-019-05783-y. [DOI] [PubMed] [Google Scholar]
- 15.Larsen FS, et al. High-volume plasma exchange in patients with acute liver failure: an open randomised controlled trial. J. Hepatol. 2016;64(1):69–78. doi: 10.1016/j.jhep.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Yuan S, et al. Therapeutic plasma exchange: a prospective randomized trial to evaluate 2 strategies in patients with liver failure. Transfus. Apher. Sci. 2018;57(2):253–258. doi: 10.1016/j.transci.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Stahl K, et al. Therapeutic plasma exchange in acute liver failure. J. Clin. Apher. 2019;34(5):589–597. doi: 10.1002/jca.21737. [DOI] [PubMed] [Google Scholar]
- 18.Tsipotis E, Shuja A, Jaber BL. Albumin Dialysis for liver failure: a systematic review. Adv. Chronic Kidney Dis. 2015;22(5):382–390. doi: 10.1053/j.ackd.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 19.Falkensteiner C, et al. Comparison of the albumin dialysis devices molecular adsorbent recirculating system and ADVanced organ support in critically ill patients with liver failure—a retrospective analysis. Ther. Apher Dial. 2020;25:225–236. doi: 10.1111/1744-9987.13533. [DOI] [PubMed] [Google Scholar]
- 20.Fuhrmann V, et al. Advanced organ support (ADVOS) in the critically ill: first clinical experience in patients with multiple organ failure. Ann. Intensive Care. 2020;10(1):96. doi: 10.1186/s13613-020-00714-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huber W, et al. First clinical experience in 14 patients treated with ADVOS: a study on feasibility, safety and efficacy of a new type of albumin dialysis. BMC Gastroenterol. 2017;17(1):32. doi: 10.1186/s12876-017-0569-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Acar U, et al. Impact of cytokine adsorption treatment in liver failure. Transpl. Proc. 2019;51(7):2420–2424. doi: 10.1016/j.transproceed.2019.01.167. [DOI] [PubMed] [Google Scholar]
- 23.Dhokia VD, et al. Novel use of Cytosorb haemadsorption to provide biochemical control in liver impairment. J. Intensive Care Soc. 2019;20(2):174–181. doi: 10.1177/1751143718772789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piwowarczyk P, et al. Hemoadsorption in isolated conjugated hyperbilirubinemia after extracorporeal membrane oxygenation support. Cholestasis of sepsis: a case report and review of the literature on differential causes of jaundice in ICU patient. Int. J. Artif. Organs. 2019;42(5):263–268. doi: 10.1177/0391398819834012. [DOI] [PubMed] [Google Scholar]
- 25.Calabro MG, et al. Blood purification with CytoSorb in critically Ill patients: single-center preliminary experience. Artif. Organs. 2019;43(2):189–194. doi: 10.1111/aor.13327. [DOI] [PubMed] [Google Scholar]
- 26.Gemelli C, et al. Removal of bilirubin with a new adsorbent system: in vitro kinetics. Blood Purif. 2019;47(1–3):10–15. doi: 10.1159/000492378. [DOI] [PubMed] [Google Scholar]
- 27.Fuhrmann V, et al. Registry on extracorporeal multiple organ support with the advanced organ support (ADVOS) system: 2-year interim analysis. Medicine (Baltimore) 2021;100(7):e24653. doi: 10.1097/MD.0000000000024653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Watchko JF. Bilirubin-induced neurotoxicity in the preterm neonate. Clin. Perinatol. 2016;43(2):297–311. doi: 10.1016/j.clp.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 29.Horvatits T, et al. Circulating bile acids predict outcome in critically ill patients. Ann. Intensive Care. 2017;7(1):48. doi: 10.1186/s13613-017-0272-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amplatz B, et al. Bile acid preparation and comprehensive analysis by high performance liquid chromatography-high-resolution mass spectrometry. Clin. Chim. Acta. 2017;464:85–92. doi: 10.1016/j.cca.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 31.Lang E, et al. Bile acid-induced suicidal erythrocyte death. Cell Physiol. Biochem. 2016;38(4):1500–1509. doi: 10.1159/000443091. [DOI] [PubMed] [Google Scholar]
- 32.Perez MJ, Briz O. Bile-acid-induced cell injury and protection. World J. Gastroenterol. 2009;15(14):1677–1689. doi: 10.3748/wjg.15.1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dominik A, Stange J. Similarities, differences, and potential synergies in the mechanism of action of albumin dialysis using the MARS albumin dialysis device and the CytoSorb hemoperfusion device in the treatment of liver failure. Blood Purif. 2020;50:1–10. doi: 10.1159/000508810. [DOI] [PubMed] [Google Scholar]
- 34.Niewinski G, et al. Intermittent high-flux albumin dialysis with continuous venovenous hemodialysis for acute-on-chronic liver failure and acute kidney injury. Artif. Organs. 2020;44(1):91–99. doi: 10.1111/aor.13532. [DOI] [PubMed] [Google Scholar]
- 35.Gerth, H.U., et al., Molecular adsorbent recirculating system (MARS) in acute liver injury and graft dysfunction: Results from a case-control study. PLoS One, 2017. 12(4): p. e0175529. [DOI] [PMC free article] [PubMed]
- 36.Cardoso FS, et al. Continuous renal replacement therapy is associated with reduced serum ammonia levels and mortality in acute liver failure. Hepatology. 2018;67(2):711–720. doi: 10.1002/hep.29488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chiu A, Fan ST. MARS in the treatment of liver failure: controversies and evidence. Int. J. Artif. Organs. 2006;29(7):660–667. doi: 10.1177/039139880602900703. [DOI] [PubMed] [Google Scholar]
- 38.Tomescu D etal. Haemoadsorption by CytoSorb(R) in patients with acute liver failure: a case series.IntJArtifOrgans, 2020, p. 391398820981383. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated during this study are included in this article.