Abstract
Study Design:
A cross-sectional magnetic resonance imaging (MRI)–based anatomical study.
Objectives:
Instrumentation of the thoracic spine may be challenging due to the unique pedicle morphology and the proximity of vital structures. As prior morphological studies have mostly been done in Caucasians, our study aims to determine the optimal pedicle screw size for transpedicular fixation in an Asian population.
Methods:
A retrospective analysis of 400 patients who had undergone MRI of the thoracic spine was performed. A total of 3324 pedicles were included. Pedicle morphology was graded qualitatively based on the size of its cancellous channel, and quantitatively with the following parameters: pedicle transverse diameter, pedicle screw path length, and pedicle angle. Subgroup analysis based on gender was performed.
Results:
Mean pedicle transverse diameter was the narrowest at the T4 (2.9 ± 1 mm) and T5 (3.1 ± 1.1 mm) level. The mean pedicle screw path length progressively increased from T1 (34 ± 4.6 mm) to T12 (47 ± 4.6 mm). The mean pedicle angle was the largest at T1 (34° ± 7.9°) and decreased caudally, to 9.4° ± 3.8° at the T12 level. Females had significantly lower mean pedicle diameter and screw path length than males at every vertebral level; however, they had a larger pedicle angle at T8 to T10. The most common size of the pedicle cancellous channel was more than 4 mm.
Conclusion:
Morphological differences in the Asian pedicle suggest that caution needs to be taken during thoracic spine instrumentation, particularly in Asian females who have significantly smaller pedicles. In such cases, the use of alternative techniques or intraoperative navigation may be useful.
Keywords: anatomy, aorta, pedicle screw, spine, thoracic vertebrae
Introduction
Transpedicular screw fixation is extensively used in spine surgery due to its biomechanical advantages over other methods of fixation.1,2 It is frequently used in a setting of deformity correction and for the treatment of spinal instability due to tumor, infection, or trauma.3,4 However, there are challenges associated with transpedicular screw fixation, especially in the thoracic spine, due to the unique morphology of the pedicle and its close proximity to vital structures. Although the morphology of the thoracic pedicle has been studied extensively in cadavers and computed tomography (CT) scans, there is limited knowledge on the morphology of the thoracic spine in an Asian population.5-8 Therefore, the aim of our study was to perform a magnetic resonance imaging (MRI)–based morphological analysis of the thoracic spine in our Asian population in order to determine the safety margins for transpedicular screw fixation.
Methods
Institutional review board approval was obtained for this study (DSRB 2018/00 831). A retrospective analysis of 400 patients who had undergone MRI of the thoracic spine from 2017 to 2018 was performed. All patients underwent MRI for the investigation of thoracic back pain or for screening purposes as part of a workup due to pathology elsewhere in the cervical or lumbar spine. Vertebrae with disease such as tumor, infection, trauma, or deformity were excluded from the study. A total of 3324 pedicles (1662 vertebrae) were included for the final study. All MRI scans were performed with a 1.5-T MR unit (Philips Ingenia, Eindhoven, Netherlands) with a maximum gradient strength of 45 mT/m and 200 mT/m per millisecond slew rate. The T2-weighted imaging parameters were TR/TE: 2000/90; matrix 1280 × 1280, with a 4 mm slice thickness. The patients’ demographic data such as age, race, gender, weight, height, and body mass index (BMI), was also collected.
Morphological Analysis
The method we adopted for morphological analysis of each vertebra was similar to that described by Olsewski et al9 and Vaccaro et al.7
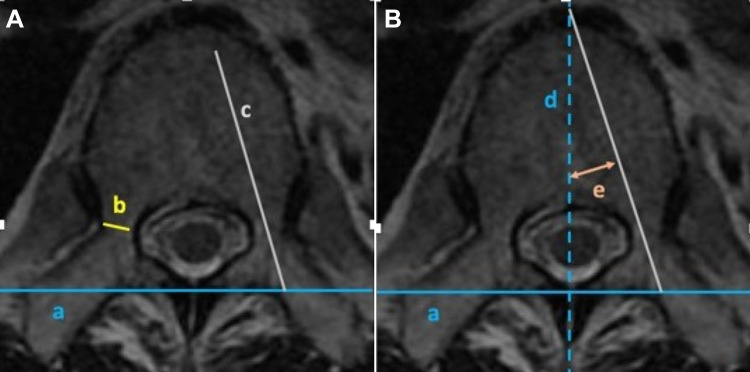
The following reference lines were drawn at each vertebrae level: (a) a horizontal line drawn across the 2 transverse processes (intertransverse line) (Figure 1A), and (b) a line drawn from the spinous process perpendicular to the intertransverse line (anteroposterior mid-sagittal line) (Figure 1B).
Figure 1.
Magnetic resonance axial cut image of the T6 vertebrae: (A) the intertransverse line (a), transverse pedicle diameter (b), and pedicle screw path length (c); (B) the anterior-posterior midsagittal line (d) and pedicle angle (e).
The following morphological parameters were measured at each vertebrae level:
Pedicle transverse diameter (TD)—the inner cortical diameter at the narrowest part of the pedicle isthmus (Figure 1A).
Pedicle screw path length (SPL)—the hypothetical length of a pedicle screw, measured as the distance from the posterior cortex of the lamina through the longitudinal axis of the pedicle (Figure 1A).
Pedicle angle (PA)—the angle between the longitudinal axis of the pedicle and the midsagittal line (Figure 1B).
Pedicle morphology was also assessed qualitatively using the following classification as described by Sarwahi et al10: type A, pedicle cancellous channel of more than 4 mm; type B, cancellous channel of 2 to 4 mm; type C, cortical channel of 2 to 4 mm; type D, cortical or cancellous channel of less than 2 mm. The morphological parameters were measured by 3 different members of the study team.
Statistical analysis was performed using Stata, version 13 (StataCorp LP, College Station, TX), with statistical significance being defined as a P value of <.05. The mean and standard deviation for each morphological parameter was calculated, and the Student’s unpaired t test was used to compare morphological parameters between gender. One-way analysis of variance (ANOVA) was used to compare the measurements between vertebral levels.
Results
Patient Demographics
A total of 400 patients were included in the study, comprising 237 males and 167 females, with a male:female ratio of 1.4:1. The mean age of the patients was 61.6 ± 16.9 years (range, 19-98 years). Body mass index (BMI) measurements were available for 238 patients, and the mean BMI was 24.8 ± 5.1 kg/m2 (range, 14.6-45.6 kg/m2). All patients were of Asian descent. There were 324 Chinese patients (81%), 44 Indian patients (11%), and 32 Malay patients (8%).
There were 3324 pedicles (1662 vertebrae) included in the study. The tabulated results of the mean pedicle SPL, pedicle TD, and PA of the study population are shown in Table 1. The mean pedicle TD was the narrowest at the T4 (2.9 ± 1 mm) and T5 (3.1 ± 1.1 mm) level, and largest at T12 (5.6 ± 1.4 mm). The mean pedicle SPL progressively increased from T1 (34 ± 4.6 mm) to T12 (47 ± 4.6 mm). The mean PA was the largest at T1 (34° ± 7.9°) and decreased caudally, to 9.4° ± 3.8° at the T12 level. One-way ANOVA was done to evaluate all the parameters, which revealed that the mean pedicle TD, pedicle SPL, and PA were different at different thoracic levels (P < .001).
Table 1.
Pedicle Screw Path Length, Diameter, and Angle at the Various Vertebral Levels.
| Level (n = 1662) | Pedicle Transverse Diameter (mm), Mean ± SD | Pedicle Screw Path Length (mm), Mean ± SD | Pedicle Angle (deg), Mean ± SD |
|---|---|---|---|
| T1 (n = 45) | 5.6 ± 1.2 | 34.0 ± 4.6 | 34.0 ± 7.9 |
| T2 (n = 86) | 4.2 ± 1.2 | 36.0 ± 5.7 | 25.9 ± 6.2 |
| T3 (n = 122) | 3.2 ± 1.0 | 37.0 ± 5.5 | 20.1 ± 4.6 |
| T4 (n = 159) | 2.9 ± 1.0 | 38.6 ± 5.0 | 17.4 ± 3.8 |
| T5 (n = 174) | 3.1 ± 1.1 | 40.4 ± 5.1 | 16.4 ± 3.4 |
| T6 (n = 180) | 3.3 ± 1.1 | 42.1 ± 5.4 | 15.5 ± 3.1 |
| T7 (n = 170) | 3.5 ± 1.0 | 43.5 ± 4.9 | 14.5 ± 3.2 |
| T8 (n = 179) | 3.6 ± 1.2 | 44.8 ± 5.3 | 13.6 ± 3.3 |
| T9 (n = 168) | 3.9 ± 1.1 | 45.4 ± 5.1 | 13.0 ± 3.1 |
| T10 (n = 165) | 4.5 ± 1.3 | 44.9 ± 4.9 | 11.9 ± 3.5 |
| T11 (n = 127) | 5.5 ± 1.4 | 45.1 ± 4.8 | 11.1 ± 4.1 |
| T12 (n = 87) | 5.6 ± 1.4 | 47.0 ± 4.6 | 9.4 ± 3.8 |
Most of the pedicles were of type A morphology (2804 pedicles, 84%), while 504 pedicles (15%) were of type B morphology, and 16 pedicles (0.5%) were of type C morphology. There were no type D pedicles in our study (Table 2).
Table 2.
Pedicle Morphology at the Various Vertebral Levels.
| Level (n = 3324) | Type A | Type B | Type C |
|---|---|---|---|
| T1 (n = 90) | 90 | — | — |
| T2 (n = 172) | 156 | 16 | — |
| T3 (n = 244) | 205 | 37 | 2 |
| T4 (n = 318) | 230 | 84 | 4 |
| T5 (n = 348) | 252 | 96 | — |
| T6 (n = 360) | 272 | 88 | — |
| T7 (n = 340) | 292 | 48 | — |
| T8 (n = 358) | 313 | 41 | 4 |
| T9 (n = 336) | 296 | 38 | 2 |
| T10 (n = 330) | 293 | 35 | 2 |
| T11 (n = 254) | 240 | 12 | 2 |
| T12 (n = 174) | 165 | 9 | — |
| Total | 2804 (84.4%) | 504 (15.2%) | 16 (0.4%) |
Gender Differences in Morphology
Subgroup analysis based on gender was performed. There was no difference in age or BMI between the male and female groups of patients (P < .05).
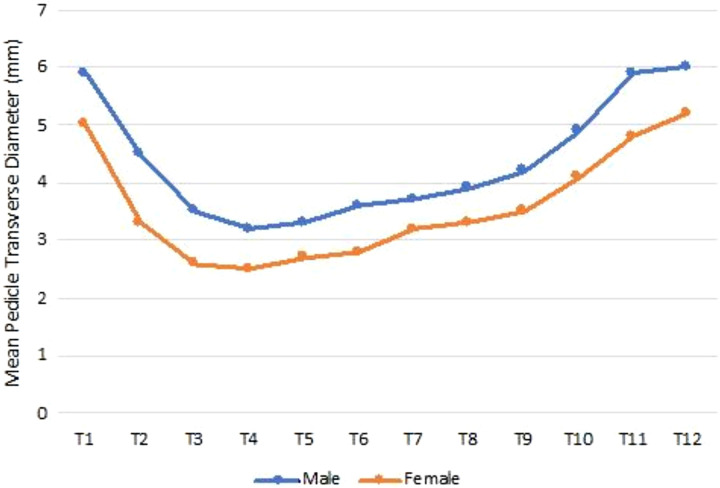
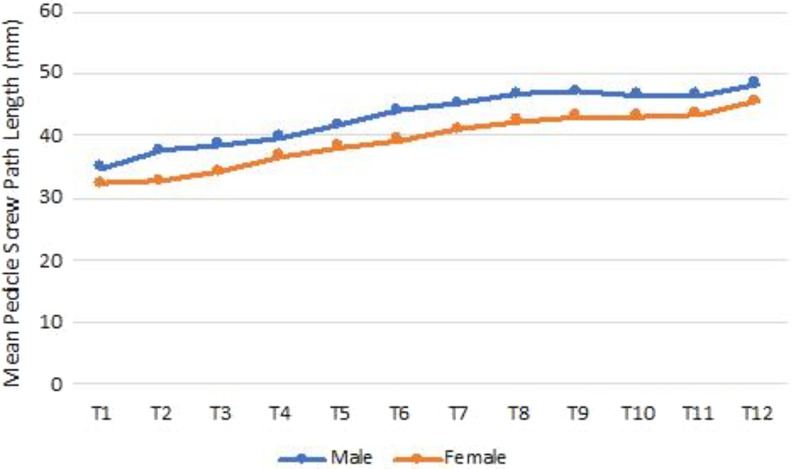
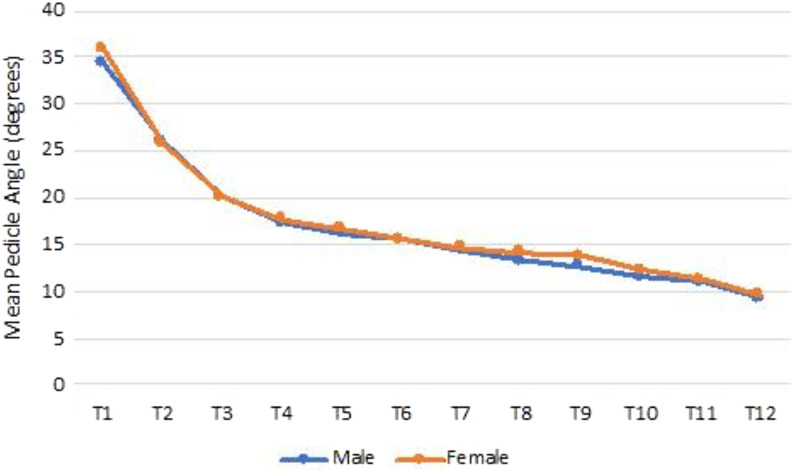
The mean pedicle TD was significantly larger in males than in females at every vertebral level (P < .05) (Figure 2). Mean pedicle SPL also was significantly longer in males than in females at every vertebral level (P < .001) (Figure 3). There was no difference in the mean PA between the male and female groups of patients at every level, except for T8, T9, and T10 (P < .05). The mean PA at T8 to T10 was larger in females than in males (Figure 4).
Figure 2.
Mean pedicle transverse diameter by gender.
Figure 3.
Mean pedicle screw path length by gender.
Figure 4.
Mean pedicle angle by gender.
Discussion
Pedicle screw fixation of the spine allows for 3-column fixation and has been shown to be biomechanically superior to other spinal fixation constructs.2,11,12 However, pedicle screw fixation in the thoracic spine may be challenging for various reasons. First, the pedicles are significantly smaller than in the lumbar spine; and second, vital structures such as the aorta are in close proximity, with cadaver studies demonstrating hardly any epidural space between the thoracic pedicle and dura.13 With such a narrow margin of error in the thoracic spine, it is crucial to understand the anatomy and morphology of the thoracic pedicle in order to achieve the maximum benefits that transpedicular screw fixation can offer, with avoidance of complications. This is especially pertinent in the Asian population due to the differences in body habitus compared with the Caucasian population, on whom most morphological studies have previously been done.6-8 Previous studies done to evaluate the thoracic pedicle morphology in an Asian population have small study sizes, with no MRI-based study done to date.14-16 The aim of our study was to establish the thoracic pedicle morphology based on MRI, in a large Asian population.
In our study, we found that the smallest inner diameter of the thoracic pedicle was at T4 and T5, and the mean pedicle diameter from T3 to T9 was consistently less than 4 mm. In particular, the mean diameter in females was 2.5 to 2.7 mm at those levels. Similarly, Datir et al14 reported that the mean diameter at T4 was 3.6 mm and suggested that a 4-mm screw should be used with caution in the mid-thoracic region in an Asian population. This is in contrast to a Caucasian-based study by Zindrick et al8 who found that the mean pedicle width at T5 varied from 2.5 to 7 mm, with a mean diameter of 4.7 mm, which is larger than that in our Asian population studied. With regard to gender differences, although Hou et al17 have previously reported no difference in pedicle diameter except at T9 and T12, our study found that female pedicle diameter was significantly narrower at every thoracic level.
In determining the appropriate pedicle screw size, consideration needs to be given that in the presence of a cancellous channel, the pedicle may be able to accommodate a larger screw size than its endosteal width due to its viscoelastic expansion and plastic deformation.18,19 Nevertheless, while the screw diameter needs to be maximized to provide optimum stability and confer adequate pull-out strength, care needs to be taken in the thoracic region to avoid pedicle wall blow-out and its potential complications.
Our findings suggest that extra caution needs to be taken when instrumenting the mid-thoracic level due to the narrow pedicle diameter, particularly in Asian females at T4 and T5 with a narrow or absent cancellous channel, as pedicle expansion during screw insertion will be limited. Preoperative planning is crucial in such cases to anticipate possible breaches and if necessary, the utilization of hooks, the “in-out-in” technique, or intraoperative navigation can be considered to facilitate better fixation.
With regard to the mean pedicle SPL, we found the length was shortest at T1 and increased caudally, a trend similar to other morphological studies.8,14 A short screw may reduce the resistance to pull-out; however, there is a risk of anterior cortical perforation and injury to the aorta with longer screws. From our study, a 35-mm screw length appears to be ideal for the upper thoracic region (T1 to T5), while the lower thoracic region may accommodate a 40-mm screw safely.
The PA was the highest at T1 (34°) and gradually decreased caudally to 9.4° at T12, similar to that reported in other studies.13,14 However, we found that females had a significantly higher PA at T8 to T10 compared with males. We postulate that this may be due to females having a shorter SPL, hence a higher PA may be necessary to optimize the length of the screw.
Our study is the first in the literature to evaluate the morphology of a normal thoracic pedicle based on MRI. CT has traditionally been the modality of choice in evaluating pedicle diameter and length, as the accuracy of MRI may be affected by susceptibility artefacts between cancellous and cortical bone. However, other studies utilizing MRI to evaluate pedicle morphology in scoliosis have shown good concordance with data derived from CT.20 As for evaluating pedicle morphology qualitatively, Sarwahi et al21 showed that pedicle classification by types based on MRI showed 86.7% concordance relative to CT imaging. In addition, one limitation of CT in determining pedicle morphology accurately is that the axial cut obtained is often not in line with the pedicle axis, as alignment of the gantry is only in the sagittal plane.22 For accurate measurements, the CT images may require reformatting to align the axial view in the pedicle axis, as some other studies have done.23,24
The limitations of our study include the lack of inter- and intraobserver variability assessments. We sought to address this by briefing the reviewers together on the measurement protocols as described previously. For quantitative measurements, interobserver variability may be minimized by ensuring that measurements were taken using standardized reference lines. For qualitative assessments, the pedicle classification system we used has previously been demonstrated to have good interobserver reliability.10
Conclusion
Our study presents the largest series of thoracic pedicle morphology evaluation in the literature. Morphological differences in the Asian pedicle suggest that caution needs to be taken in instrumentation of the thoracic spine, especially in the mid-thoracic region, particularly in Asian females who have significantly smaller and shorter pedicles. In such cases, the use of hooks, the “in-out-in” technique or intraoperative navigation may be considered to achieve optimal fixation of the thoracic spine.
Acknowledgments
The authors sincerely thank Miss Novifandona, coordinator of Spine Service, Department of Orthopedic Surgery, Tan Tock Seng Hospital, Singapore, for her administrative support.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Arun-Kumar Kaliya-Perumal, MS  https://orcid.org/0000-0002-2747-4500
https://orcid.org/0000-0002-2747-4500
Jacob Yoong-Leong Oh, FRCS  https://orcid.org/0000-0002-2832-8433
https://orcid.org/0000-0002-2832-8433
References
- 1. Gaines RW, Jr. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82:1458–1476. [DOI] [PubMed] [Google Scholar]
- 2. Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2. 004;29:2040–2048. [DOI] [PubMed] [Google Scholar]
- 3. Kaliya-Perumal AK, Yeh YC, Niu CC, Chen LH, Chen WJ, Lai PL. Is convex derotation equally effective as concave derotation for achieving adequate correction of selective Lenke’s type- 1 scoliosis? Indian J Orthop. 2018;52:363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Li K, Zhang W, Liu D, et al. Pedicle screw fixation combined with intermediate screw at the fracture level for treatment of thoracolumbar fractures: a meta-analysis. Medicine (Baltimore). 2016;95:e4574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grivas TB, Savvidou O, Binos S, et al. Morphometric characteristics of the thoracolumbar and lumbar vertebrae in the Greek population: a computed tomography-based study on 900 vertebrae—“Hellenic Spine Society (HSS) 2017 Award Winner.” Scoliosis Spinal Disord. 2019;14:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Berry JL, Moran JM, Berg WS, Steffee AD. A morphometric study of human lumbar and selected thoracic vertebrae. Spine (Phila Pa 1976). 1987;12:362–367. [DOI] [PubMed] [Google Scholar]
- 7. Vaccaro AR, Rizzolo SJ, Allardyce TJ, et al. Placement of pedicle screws in the thoracic spine. Part I: morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–1199. [DOI] [PubMed] [Google Scholar]
- 8. Zindrick MR, Wiltse LL, Doornik A, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976). 1987;12:160–166. [DOI] [PubMed] [Google Scholar]
- 9. Olsewski JM, Simmons EH, Kallen FC, Mendel FC, Severin CM, Berens DL. Morphometry of the lumbar spine: anatomical perspectives related to transpedicular fixation. J Bone Joint Surg Am. 1990;72:541–549. [PubMed] [Google Scholar]
- 10. Sarwahi V, Sugarman EP, Wollowick AL, Amaral TD, Lo Y, Thornhill B. Prevalence, distribution, and surgical relevance of abnormal pedicles in spines with adolescent idiopathic scoliosis vs. no deformity: a CT-based study. J Bone Joint Surg Am. 2014;96:e92. [DOI] [PubMed] [Google Scholar]
- 11. Hackenberg L, Link T, Liljenqvist U. Axial and tangential fixation strength of pedicle screws versus hooks in the thoracic spine in relation to bone mineral density. Spine (Phila Pa 1976). 2002;27:937–942. [DOI] [PubMed] [Google Scholar]
- 12. Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine (Phila Pa 1976). 2001;26:2049–2057. [DOI] [PubMed] [Google Scholar]
- 13. Ebraheim NA, Jabaly G, Xu R, Yeasting RA. Anatomic relations of the thoracic pedicle to the adjacent neural structures. Spine (Phila Pa 1976). 1997;22:1553–1557. [DOI] [PubMed] [Google Scholar]
- 14. Datir SP, Mitra SR. Morphometric study of the thoracic vertebral pedicle in an Indian population. Spine (Phila Pa 1976). 2004;29:1174–1181. [DOI] [PubMed] [Google Scholar]
- 15. Liau KM, Yusof MI, Abdullah MS, Abdullah S, Yusof AH. Computed tomographic morphometry of thoracic pedicles: safety margin of transpedicular screw fixation in Malaysian Malay population. Spine (Phila Pa 1976). 2006;31:E545–E550. [DOI] [PubMed] [Google Scholar]
- 16. Lien SB, Liou NH, Wu SS. Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J. 2007;16:1215–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hou S, Hu R, Shi Y. Pedicle morphology of the lower thoracic and lumbar spine in a Chinese population. Spine (Phila Pa 1976). 1993;18:1850–1855. [DOI] [PubMed] [Google Scholar]
- 18. Cahill P, Rinella AS, Ghanayem A, et al. P8. Thoracic pedicle expansion after pedicle screw insertion in a pediatric cadaveric spine: a biomechanical analysis. Spine J. 2004;4(5 suppl):S93. [Google Scholar]
- 19. Misenhimer GR, Peek RD, Wiltse LL, Rothman SL, Widell EH, Jr. Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine (Phila Pa 1976). 1. 989;14:367–372. [DOI] [PubMed] [Google Scholar]
- 20. Liljenqvist UR, Allkemper T, Hackenberg L, Link TM, Steinbeck J, Halm HF. Analysis of vertebral morphology in idiopathic scoliosis with use of magnetic resonance imaging and multiplanar reconstruction. J Bone Joint Surg Am. 2. 002;84:359–368. [DOI] [PubMed] [Google Scholar]
- 21. Sarwahi V, Amaral T, Wendolowski S, et al. MRIs are less accurate tools for the most critically worrisome pedicles compared to CT scans. Spine Deform. 2016;4:400–406. [DOI] [PubMed] [Google Scholar]
- 22. O’Brien MF, Lenke LG, Mardjetko S, et al. Pedicle morphology in thoracic adolescent idiopathic scoliosis: is pedicle fixation an anatomically viable technique? Spine (Phila Pa 1976). 2000;25:2285–2293. [DOI] [PubMed] [Google Scholar]
- 23. Chen Y, Zeng J, Guan J, et al. Reformatted computed tomographic evaluation of the thoracic pedicle in a Chinese population for the surgical application of transpedicular screw placement. Surg Radiol Anat. 2010;32:463–468. [DOI] [PubMed] [Google Scholar]
- 24. Zhuang Z, Chen Y, Han H, et al. Thoracic pedicle morphometry in different body height population: a three-dimensional study using reformatted computed tomography. Spine (Phila Pa 1976). 2011;36:E1547–E1554. [DOI] [PubMed] [Google Scholar]