Abstract
Study design:
Multicenter study.
Objectives:
The COVID-19 pandemic has obligated physicians to recur to additional resources and make drastic changes regarding the standard physician-patient encounter. In the last century, there has been a substantial improvement in technology, which over the years has opened the door to a new form of medical practicing known as telemedicine.
Methods:
Healthcare workers from three hospitals involved in the care for COVID-19 patients in the united states were invited to share their experience using telemedicine to deliver clinical care to their patients.
Results:
Since the appearance of this worldwide outbreak, social distancing has been a key factor in preventing the spread of the virus, for which measures have been taken to limit physical contact. Because of the ongoing situation, telemedicine has been progressively incorporated into the physician-patient encounters and quickly has become an essential component in the day-today medical practice.
Conclusions:
It is feasible to deliver viable spine practice with the use of telemedicine. A proper patient selection of patients requiring virtual treatment versus those requiring in-person visits should be considered.
Keywords: telemedicine, COVID-19, Thomas Jefferson University, multicenter experiences
Introduction
There is a significant bond and relationship between a patient and the physician. This relationship has developed over the last thousand years to direct face-to-face interactions and personal encounters. Over the last century, there have been significant developments in technology and communication. Telemedicine was slowly entering into the physician-patient relationship. Recently with quarantine and need for social distancing, this tool has now become a required instrument in physicians’ care armamentarium. This article summarizes the key resources and options spine surgeons have in the exploration of this technology.
The physician-patient encounter has relied on the physician being a combination of scientist, counselor, and healer. Traditionally, encounters with patients have included a substantial tactile component, including the introductory handshake and a “high-touch” physical examination portion. Notwithstanding, many of us have emphasized to our trainees over the years the importance of the oral component of the encounter—active listening, appropriate probing, and verbal explanations and counseling. The telehealth encounter facilitates the oral and visual components of our encounters with patients but limits us in some aspects of the tactile physical examination. While there are clear limitations of the telehealth encounter, there are also several advantages that are not always self-evident—patients feel more comfortable being in their own environment rather than the intimidating doctor’s office. Some patients appear to cherish that their physician has gotten to see them as individuals in their own homes. Additionally, calling in via a telephone or video encounter is seen by many patients as an added courtesy that their physician is extending them. Parking fees and tickets become a nonissue, and the time saved traveling, checking in, and waiting at the doctor’s office is mostly eliminated.
Multicenter Experiences
Thomas Jefferson University Hospitals, Department of Neurosurgery
Telemedicine at Thomas Jefferson University Hospital grew out of a strong telehealth program for vascular neurosurgery. Over 10 years ago, Jefferson understanding the need to provide high-quality neurosurgical vascular care to the outlying communities had established a neuroscience network. This has now grown to involve 35 hospitals within a 100-mile radius of Philadelphia, with a significant component of direct physician to patient contact through a telemedicine program (Figure 1).
Figure 1.
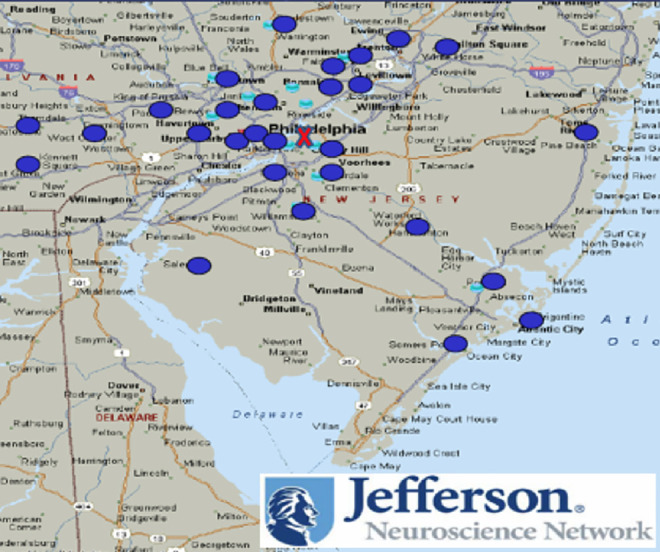
Jefferson Health Neuroscience Network Locations.
The ability of the patient to have a dialogue directly with their health care provider without leaving their home has significant advantages. However, there were numerous obstacles that were overcome to develop this program. Specifically, previously the limited use of comprehensive electronic medical record systems that could collaborate with a telemedicine platform proved to be a significant barrier to provide smooth care via telemedicine. Some unforeseen technical and legal difficulties arose, and was further complicated by the fact that the neurosurgical and spine patient population also needed a detailed neurological exam.
Prior to March 2020, Jefferson institution had devoted significant resources and placed the use of telemedicine as a priority for the enterprise. Despite this leadership-instituted objective, only 50 to 60 telemedicine appointments were being done daily. By mid-April these numbers increased to 3000 daily. This was accomplished in that there were structures in place such to facilitate this process. Unfortunately, this new technology requires significant investment to run successfully. The office administrator developed a patient flow pattern where all images and notes would be placed in the medical record in advance, the patient would be registered into the EHR (electronic health record), and prior to the visit each patient was called and instructed on the use of the telemedicine platform. Therefore, as demand accelerated the staff already had significant knowledge and experience with this technology.
With the COVID-19 crisis, having a robust telemedicine program has provided the ability to ensure continuity of care and patient accessibility to their surgeons. In order to promote the use of this technology, the government relaxed HIPPA and reimbursement criteria (www.hhs.gov), such as to provide physicians the opportunity to better care for their patients.1 Some of these offer the ability to use widely available commercial platforms to deliver health care, such as Facetime (Apple), Skype, and others. Furthermore, through the Social Security Act, Section 1135 (www.cms.gov), state law limits telemedicine visits within state boundaries; this has been temporarily relaxed during the declared state of emergency, allowing to communicate without traditional state law boundary barriers.
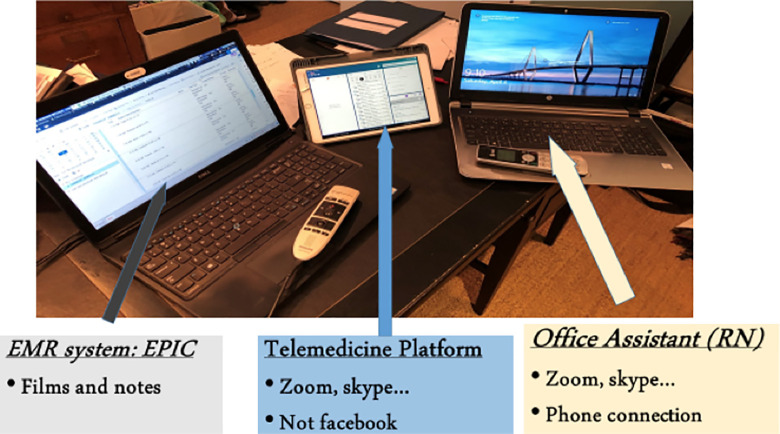
Due to the current COVID-19 pandemic performing telemedicine through a remote location so as to maximize social distancing has become paramount in the spine department. However, there is also a need to continually communicate with ancillary staff to coordinate care. This is accomplished through a 3-part system. First, using a secure electronic medical record system with remote access capabilities, in our case EPIC, serves to document and review patient’s medical records and imaging studies. Second, a telemedicine platform is then used to establish direct video and audio communication with the patient; these services are provided by Cantu. Third, a system to have a constant and reliable communication channel with the office staff, which can be done via conference call or bidirectional meeting software such as Zoom (Figure 2).
Figure 2.
Virtual-equipment and tools used in telemedicine.
A very common issue presented during telemedicine visits is the loading and visualizing of patient imaging studies. Patients have the option of having images done at a Jefferson facility where they remain in our PACS (Philips) system; they also can mail their discs, and those are then loaded by staff in the office. In addition, we also provide the patient with an electronic link to the Life Image System, which allows them to load their disc electronically. Last, over the last several years, we have established relationships and contact with outside commercial radiology sites, providing us direct web access to review patient imaging.
Walter Reed National Military Medical Center, Department of Orthopedic Surgery
Virtual health within the military started out of necessity to deliver care across the world. The military is tasked with delivering care at diverse locations such as the Middle East, Africa, and on a carrier in the middle of the Pacific Ocean. To accomplish this, the military partnered with multiple organizations in pushing out telehealth platforms. Additionally, due to licensing requirements within federal facilities, the military providers are able to conduct virtual visits more regularly across multiple states and even countries.
Prior to the COVID crisis, the standard office telemedicine visit was conducted using Adobe Connect, a platform enabling encrypted synchronous video conferencing and screen sharing for imaging review. As seen with our civilian colleagues, the platforms authorized for utilization have been expanded with the current crisis; however, we have continued to leverage our Adobe connect platform given its capabilities. Previously patients would either have to be located in a state that we were licensed or be in a federal facility. However, with the current crisis, patients are able to conduct virtual visits from home anywhere in the world. We are strongly encouraging both patients and providers to conduct as much as possible virtually in an effort to decrease risk of coronavirus transmission.
University of Michigan, Department of Orthopedic Surgery
Michigan Medicine began using EPIC as our electronic medical record provider several years ago. EPIC has a telemedicine platform that allows us to take care of patients virtually. Telehealth became an initiative across our institution in order to provide care for patients living in the far reaches of the state. Initially, these appointments were limited to postoperative and follow-up care. For several reasons, new patients were not seen virtually—the primary reason being our inability to perform a physical exam. Before the COVID-19 crisis, we developed a hands-free exam that could be implemented virtually and serve as a proxy for the traditional in office physical exam.
When developing our hands-free exam, our goal was to create a system that was highly sensitive and allowed us to screen for surgical pathology. Additionally, we wanted it to be reproducible in order to follow the exam of patients longitudinally. The traditional physical exam uses manual muscle strength testing to assess weakness on a 0 to 5 numerical scale. This scale was developed in the 1940s and is highly subjective, with poor intraobserver and interobserver reliability. We replaced this with objective strength testing that could be performed at home with household objects. Additionally, we included functional tests that are equally if not more useful in determining which patients should undergo surgery. With the implementation of this exam, we have been able to successfully see all patients virtually. Initially, our virtual exams were extremely time consuming as we needed to coach our patients through each step. This has been somewhat mitigated with a set of detailed instructions that are sent to the patient prior to their visit. Additionally, we are conducting a research study to assess if patients can fill out the objective parts of their exam prior to their visit saving even more time. We also found it considerably easier to conduct a virtual exam if there was a family member or friend present to operate the camera for the patient. Anecdotally, we have been extremely pleased with the ability of the hands-free virtual exam to diagnose patients as well as to follow them longitudinally.
Discussion
In 2006, Hersh et al2 performed a systematic review of telemedicine services and concluded that there were significant gaps in the evidence on the effectiveness of the use of telemedicine. At the time, this technology was being particularly utilized by visual-based services such as dermatology, wound care, and ophthalmology. These services have come a long way since then.
A 2017 Virtual Visits Consumer Choice Survey from Advisory Board noted that 77% of health care consumers would consider seeing a provider through a virtual encounter, and 19% of consumers had already experienced a telemedicine-based visit.3 Furthermore, Buvik et al performed a comparison between video-assisted remote consultation against standard orthopedic consultation on 389 patients (199 remote consultations and 190 standard consultations) using the primary outcome of patient satisfaction and health measured through EQ-5D and EQ-VAS,4 and 86% of remote consultation patients preferred video-based consultation visits for the next encounter and this further resulted in significant cost savings.4,5 Several other studies such as the one by Hjelm6 note that the major benefits of a telemedicine platform were improved access to information, improved access to care, improved communication to health care providers, quality control of screening programs, and reduced health care costs.
A significant limitation that telemedicine presents is the dependence on the patient to elicit findings on physical and neurological examinations. Wainner et al in 2003 demonstrated that spinal exams can be performed and reported by the patient with useful results.7 The Telemedicine Neurological Exam fundamentally consists of 3 components: a motor exam, sensory examination, and special tests. We have utilized elastic bands, filaments, and prestructural tasks to perform these exams remotely and have validated results. In the present situation, it is not feasible to perform a full physical examination to meet Medicare billing requirements.8 Therefore, it is recommended that physicians use time billing for new and established patients.
Another strategy that is gaining momentum is the use of smartphone-based applications, as this further promotes accessibility and ease of use.9 According to the Pew Research Center, 96% of Americans own a cellphone, and 81% own a smartphone10; given the widespread use of these devices, a multitude of mobile health applications are being developed.11-13 At the moment, however, there is limited evidence to validate the effectiveness of this method as an equalizer to an in-person clinical encounter. Some authors present an interesting proposal, which is the use of mobile health smartphone applications or “apps” to aid in behavior alteration of patients, specially of secondary or modifiable risk factors.9,11-15 There has not been a study done directly evaluating the use of apps in the spine population; however, multiple studies have shown that these mobile apps can be effective in reducing smoking, aiding with weight loss, diabetes management, and daily physical activity tracking, all of which become important for preventing complications in the preoperative and especially the postoperative care in the spine population.15-21 In the perioperative setting, a study by Stewart et al22 showed that the use of a smartphone application with real-time notifications and reminders reduced last-minute cancellations of spine surgery as the patients were more engaged, making them less likely to miss key preoperative instructions such as stopping a blood thinner.
After the patients are discharged, apps can help in the effective remote monitoring of postoperative recovery and prevention of avoidable complications. In 2016, Debono et al23 followed 60 patients postoperative recovery at home after having had a lumbar mircodisckectomy with the use of a mobile application; they concluded the mobile app was a useful tool for outpatient monitoring of recovery, and it also helped minimize the need for in-person visits for postoperative patients. An integral part of the postoperative spine care is the assessment of wound healing and prevention of infections; Martínez-Ramos et al24 looked at this in 2009, and the study results suggested that the review of patient-provided images of the wound by the physician was an effective way of monitoring that expected healing was occurring, and they also found that the use of this system greatly improved patient satisfaction among participants.
Other concerns are potential malpractice exposure to physicians using a telemedicine platform. Each physician should review their situation with their malpractice providers for their individual status. However, in general, the malpractice claim using this modality are rare. Fogel and Kvedar reviewed the number of cases of medical malpractice in direct care to consumer telemedicine, and noted no medical malpractice were identified.25 Kramer et al raised concerns about malpractice liability and stated that most of the telemedicine-related malpractice issues to date have occurred when a physician has issued a prescription over the telephone or internet without first examining the individual in person.26
Individual states’ law may raise complex legal issues related to malpractice once their legal requirements to practice of telemedicine are diverse. Some states require full in-state licensure; others offer a specific telemedicine registration; some allow intra-specialty consultations while others make exemptions for emergency consultations.27 Each physician should carefully review their situation, as once the telemedicine care delivered increases, it is likely that malpractice issues related to spine surgery care will also increase.
Conclusion
The use of telemedicine in the spine population has proven to be a challenging endeavor. We, however, present our experiences in maintaining a viable spine practice with the use of this technology during the global pandemic of COVID-19. Since the emergence of telemedicine as a concept, there have been tremendous advances in its implementation, making this solution more comprehensive and with significant improvement of patient satisfaction. At the moment, concessions have been made by the government, loosening regulations on the use of telehealth.
Moving forward, we hope to leverage the knowledge gained in telemedicine throughout this current crisis into an expanded practice. This crisis will allow us to better understand the most appropriate patients to be seen and treated virtually versus in-person visits, and this additional knowledge will help guide clinical practice post COVID. Patients will continue to expect some level of virtual health having seen the advantages of doing so during this crisis. As physicians we will have to adapt to this increased demand post crisis. Additionally, once the CMS 1135 waiver is removed, we need to understand the regulations governing telemedicine, ensuring we deliver the most appropriate care. Our experience during this crisis will lead to long-lasting changes in the way health care is delivered and to the regulations guiding telemedicine.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Daniel Franco, MD  https://orcid.org/0000-0003-0714-4288
https://orcid.org/0000-0003-0714-4288
Glenn A. Gonzalez, MD  https://orcid.org/0000-0002-5051-3141
https://orcid.org/0000-0002-5051-3141
Kevin Hines, MD  https://orcid.org/0000-0003-1700-174X
https://orcid.org/0000-0003-1700-174X
Aria Mahtabfar, MD  https://orcid.org/0000-0002-4026-7821
https://orcid.org/0000-0002-4026-7821
References
- 1. US Department of Health and Human Services. Emergency situations: preparedness, planning, and response. Accessed May 20, 2020. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/index.html
- 2. Hersh WR, Hickam DH, Severance SM, Dana TL, Krages KP, Helfand M. Diagnosis, access and outcomes: update of a systematic review of telemedicine services. J Telemed Telecare. 2006;12(suppl 2):S3–S31. [DOI] [PubMed] [Google Scholar]
- 3. Advisory Board. What do consumers want from virtual visits? Published April 27, 2017. Accessed May 20, 2020. https://www.advisory.com/research/market-innovation-center/research-briefs/2017/virtual-visits-briefing
- 4. Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21:e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomized controlled trial. J Telemed Telecare. 2019;25:451–459. [DOI] [PubMed] [Google Scholar]
- 6. Hjelm NM. Benefits and drawbacks of telemedicine. J Telemed Telecare. 2005;11:60–70. [DOI] [PubMed] [Google Scholar]
- 7. Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine (Phila Pa 1976). 2003:28:52–62. [DOI] [PubMed] [Google Scholar]
- 8. Centers for Medicare and Medicaid. 1997. Documentation guidelines for evaluation & management services. Accessed April 21, 2020. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
- 9. Goz V, Spiker WR, Brodke D. Mobile messaging and smartphone apps for patient communication and engagement in spine surgery. Ann Transl Med. 2019;7(suppl 5):S163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pew Research Center. Mobile fact sheet. Accessed May 20, 2020. https://www.pewresearch.org/internet/fact-sheet/mobile/
- 11. Lang M, Zawati MH. The app will see you now: mobile health, diagnosis, and the practice of medicine in Quebec and Ontario. J Law Biosci. 2018;5:142–173. doi:10.1093/jlb/lsy004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Baig MM, GholamHosseini H, Connolly MJ. Mobile healthcare applications: system design review, critical issues and challenges. Australas Phys Eng Sci Med. 2015;38:23–38. doi:10.1007/s13246-014-0315-4 [DOI] [PubMed] [Google Scholar]
- 13. Aitken M, Lyle J. Patient Adoption of mHealth: Use, Evidence and Remaining Barriers to Mainstream Acceptance. IMS Institute for Healthcare Informatics; 2015. Accessed May 20, 2020. https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/patient-adoption-of-mhealth.pdf [Google Scholar]
- 14. Morawski K, Ghazinouri R, Krumme A, et al. Association of a smartphone application with medication adherence and blood pressure control: the MedISAFE-BP randomized clinical trial. JAMA Intern Med. 2018;178:802–809. doi:10.1001/jamainternmed.2018.0447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cho YM, Lee S, Islam SMS, et al. Theories applied to m-Health interventions for behavior change in low- and middle-income countries: a systematic review. Telemed J E Health. 2018;24:727–741. doi:10.1089/tmj.2017.0249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Miller LC, Appleby PR, Christensen JL, et al. Virtual interactive interventions for reducing risky sex: adaptations, integrations, and innovations. In: Noar SM, Harrington NG, eds. EHealth Applications: Promising Strategies for Behavior Change. Taylor & Francis; 2012:79–95. [Google Scholar]
- 17. Doak CC, Doak LG, Root JH. Teaching Patients With Low Literacy Skills. Lippincott; 1985. [Google Scholar]
- 18. Devries KM, Kenward MG, Free CJ. Preventing smoking relapse using text messages: analysis of data from the txt2stop trial. Nicotine Tob Res. 2013;15:77–82. doi:10.1093/ntr/nts086 [DOI] [PubMed] [Google Scholar]
- 19. Patel N, Bagan B, Vadera S, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007;6:291–297. doi:10.3171/spi.2007.6.4.1 [DOI] [PubMed] [Google Scholar]
- 20. Glassman SD, Anagnost SC, Parker A, Burke D, Johnson JR, Dimar JR. The effect of cigarette smoking and smoking cessation on spinal fusion. Spine (Phila Pa 1976). 2000;25:2608–2615. doi:10.1097/00 007 632-200 010 150-00 011 [DOI] [PubMed] [Google Scholar]
- 21. Semple JL, Sharpe S, Murnaghan ML, et al. Using a mobile app for monitoring post-operative quality of recovery of patients at home: a feasibility study. JMIR Mhealth Uhealth. 2015;3:e18. doi:10.2196/mhealth.3929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Stewart JJ, Fayed I, Henault S, et al. Use of a smartphone application for spine surgery improves patient adherence with preoperative instructions and decreases last-minute surgery cancellations. Cureus. 2019;11:e4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Debono B, Bousquet P, Sabatier P, et al. Postoperative monitoring with a mobile application after ambulatory lumbar discectomy: an effective tool for spine surgeons. Eur Spine J. 2016;25:3536–3542. doi:10.1007/s00586-016-4680-4 [DOI] [PubMed] [Google Scholar]
- 24. Martínez-Ramos C, Cerdán MT, López RS. Mobile phone–based telemedicine system for the home follow-up of patients undergoing ambulatory surgery. Telemed J E Health. 2009;15:531–537. doi:10.1089/tmj.2009.0003 [DOI] [PubMed] [Google Scholar]
- 25. Fogel AL, Kvedar JC. Reported cases of medical malpractice in direct-to-consumer telemedicine. JAMA. 2019;321:1309–1310. doi:10.1001/jama.2019.0395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kramer GM, Kinn JT, Mishkind MC. Legal, regulatory, and risk management issues in the use of technology to deliver mental health care. Cogn Behav Pract. 2015;22:258–268. [Google Scholar]
- 27. Newton MJ. The promise of telemedicine. Surv Ophthalmol. 2003;59:559–567. [DOI] [PubMed] [Google Scholar]