Key Points
Question
Can an automated measurement of central macular fluid volume (CMFV) with optical coherence tomography improve the diagnostic accuracy for diabetic macular edema (DME)?
Findings
In this cross-sectional study of 215 patients with diabetes, the area under the receiver operating characteristic curve of CMFV for the diagnosis of center-involved DME was 0.907, larger than that for central subfield thickness (0.832). When the specificity was set at 95%, the sensitivity of CMFV was higher than that of central subfield thickness (79% vs 54%).
Meaning
The findings suggest that an automated measurement of CMFV using optical coherence tomography may improve the diagnostic accuracy for DME.
Abstract
Importance
Diabetic macular edema (DME) is the predominant cause of visual impairment in patients with type 1 or 2 diabetes. Automated fluid volume measurements using optical coherence tomography (OCT) may improve the diagnostic accuracy of DME screening.
Objective
To assess the diagnostic accuracy of an automated central macular fluid volume (CMFV) quantification using OCT for DME.
Design, Setting, and Participants
A cross-sectional observational study was conducted at a tertiary academic center among 215 patients with diabetes (1 eye each) enrolled from January 26, 2015, to December 23, 2019. All participants underwent comprehensive examinations, 6 × 6-mm macular structural OCT horizontal raster scans, and 6 × 6-mm macular OCT angiography volumetric scans. From January 1 to March 30, 2020, 2 retinal specialists reviewed the structural OCT scans independently and diagnosed DME if intraretinal or subretinal fluid was present. Diabetic macular edema was considered center involved if fluid was present within the central fovea (central 1-mm circle). A third retinal specialist arbitrated any discrepancy. The mean central subfield thickness (CST) within the central fovea was measured on structural OCT horizontal raster scans. A deep learning algorithm automatically quantified fluid volumes on 6 × 6-mm OCT angiography volumetric scans and within the central foveas (CMFV).
Main Outcomes and Measures
The area under the receiver operating characteristic curve (AUROC) and the sensitivity and specificity of CST and CMFV for DME diagnosis.
Results
We enrolled 1 eye each of 215 patients with diabetes (117 women [54.4%]; mean [SD] age, 59.6 [12.4] years). Diabetic macular edema was present in 136 eyes; 93 cases of DME were center involved. The AUROC of CMFV for diagnosis of center-involved DME (0.907 [95% CI, 0.861-0.954]) was greater than the AUROC of CST (0.832 [95% CI, 0.775-0.889]; P = .02). With the specificity set at 95%, the sensitivity of CMFV for detection of center-involved DME (78.5% [95% CI, 68.8%-86.3%]) was higher than that of CST (53.8% [95% CI, 43.1%-64.2%]; P = .002). Center-involved DME cases not detected by CST but detected by CMFV were associated with a thinner CST (290.8 μm [95% CI, 282.3-299.3 μm] vs 369.4 μm [95% CI, 347.1-391.7 μm]; P < .001), higher proportion of previous macular laser treatment (11 of 28 [39.3%; 95% CI, 21.5%-59.4%] vs 12 of 65 [18.5%; 95% CI, 9.9%-30.0%]; P = .03), and female sex (20 of 28 [71.4%; 95% CI, 51.3%-86.8%] vs 31 of 65 [47.7%; 95% CI, 35.1%-60.5%]; P = .04).
Conclusions and Relevance
These findings suggest that an automated CMFV is a more accurate diagnostic biomarker than CST for DME and may improve screening for DME.
This cross-sectional study assesses the diagnostic accuracy of an automated central macular fluid volume quantification using optical coherence tomography for diabetic macular edema (DME).
Introduction
Diabetic retinopathy (DR) is the leading cause of preventable vision loss in the working-age population worldwide.1 Diabetic retinopathy causes vision loss mainly owing to 2 conditions: diabetic macular edema (DME) and proliferative diabetic retinopathy. Among them, DME is the predominant cause of vision loss.2,3 Screening for DR with retinal photography is universally considered cost-effective and important for the prevention of blindness from DR.4 However, screening for DME with retinal photography only has a sensitivity of 60% to 73% and a specificity of 67% to 79%.5
In recent years, optical coherence tomography (OCT) has supplanted stereoscopic fundus photography and fundus biomicroscopy for the diagnosis of DME.6,7,8,9,10,11 Optical coherence tomography detects key, clinically relevant features in DME, including macular thickening and intraretinal and subretinal fluid.6,12,13,14 Optical coherence tomography has the potential to improve DME screening, as reported previously.3,15
Central subfield thickness (CST) has been used extensively as a quantifiable biomarker when using OCT for DME assessment.16,17,18,19,20 The threshold of CST for DME diagnosis is commonly defined as the mean machine-specific OCT-measured thickness of normative eyes of an individual with diabetes without macular edema plus 2 SDs. In the Diabetic Retinopathy Clinical Research Network (DRCR.net) study, based on a study of 67 female and 55 male patients with diabetes and no or minimal DR and no macular thickening on clinical examination, DME was defined as CST, as measured using Heidelberg Spectralis OCT scans, of 320 μm or more in male patients and 305 μm or more in female patients.21
However, CST can vary substantially among individuals owing to many factors, such as age, sex, and refractive status.22,23,24,25,26,27 This variation in the normal population suggests that DME diagnosed based on CST measurement may not be ideal owing to the overlap between the normal healthy population and patients with diabetes. Because of the overlap among healthy and diseased eyes, theoretically there will always be some false-positive and false-negative cases no matter what CST threshold is used. In addition, CST may increase owing to other macular pathologic characteristics, such as an epiretinal membrane. A 2015 Cochrane review demonstrated that a CST measurement on an OCT scan is not sufficiently accurate to detect DME.6 For every 10 patients with DR, 5 of whom have clinically significant macular edema (CSME), 1 of 5 without CSME would be wrongly diagnosed as having CSME, and about 1 of 5 with CSME would be missed.
The key pathogenesis of DME is exudative fluid accumulation in the macula.3 The fluid does not exist in the macula of normal healthy eyes. Therefore, directly measuring the fluid, the intrinsic feature of DME, may be more sensitive and specific than measuring the thickness for diagnosing DME.
With the advancement of OCT technology, dense OCT volumetric macular scans can be acquired within seconds. These dense OCT scans, such as volumetric scans for OCT angiography (OCTA), provide high-resolution, 3-dimensional structural information, enabling us to obtain accurate measurements.28 We hypothesize that measuring the macular fluid volume on dense volumetric OCT scans may provide a higher diagnostic accuracy than measuring CST for screening DME.
Methods
This study included participants of 2 prospective OCTA studies (NIH R01 EY027833 and R01 EY024544) performed at the Casey Eye Institute, Oregon Health & Science University. The details of the studies have been published.29,30,31,32,33 The study adhered to the tenets of the Declaration of Helsinki34 and complied with the Health Insurance Portability and Accountability Act of 1996. The study was approved by the institutional review board of Oregon Health & Science University. All participants provided written informed consent to participate in the OCTA studies.
The inclusion criteria included age between 18 and 85 years and type 1 diabetes of greater than 5 years’ duration or type 2 diabetes of any duration. The exclusion criteria included pregnant or lactating women, those unable to consent or cooperate with OCT or OCTA scans, those with significant nondiabetic ocular diseases (such as age-related macular degeneration), or those with a history of intraocular surgery, except intravitreal injections or cataract surgery, within 4 months prior to screening. Only 1 eye of each participant was included in the study. Participants were compensated $80 for each completed study visit.
All participants underwent a medical history inquiry, comprehensive clinical examinations, and ocular imaging. The clinical examinations included Early Treatment Diabetic Retinopathy Study (ETDRS) protocol visual acuity, intraocular pressure, slitlamp biomicroscopy, and indirect binocular ophthalmoscopy. Imaging procedures included standard 7-field ETDRS color fundus photography, 6 × 6-mm macular structural OCT raster scans (19 horizontal B-scans, automatic real-time tracking function activated and set at a mean of 9 frames; Spectralis) and 6 × 6-mm macular OCTA volumetric (400 × 400 A lines) scans (Avanti; OptoVue). A retinal specialist (T.S.H.) assessed the severity of DR based on standard 7-field ETDRS color fundus photographs using the ETDRS severity scale.
Two retinal specialists (Q.S.Y. and K.T.) reviewed the structural OCT raster scans independently masked to the volumetric OCTA images and other clinical data, and they diagnosed DME if intraretinal or subretinal fluid was detected. Diabetic macular edema was classified into center involved or non–center involved according to the involvement of the central fovea (central 1-mm circle). In case of disagreement, a third retinal specialist (T.S.H.) arbitrated.
Central subfield thickness, defined as the mean thickness within the 1-mm circle centered on the fovea, was measured via structural OCT raster scans using embedded software (Heyex, version 6.8.3; Heidelberg Engineering). The segmentations of the internal limiting membrane and retinal pigment epithelium Bruch membrane were manually checked for accuracy. Scans with inaccurate segmentations were manually corrected (only for 4 eyes) or excluded (1 eye only) from the analysis. A deep learning–based algorithm automatically quantified the macular fluid volume on 6 × 6-mm volumetric OCTA scans (overall macular fluid volume) and within the 1-mm circle centered on the fovea (central macular fluid volume [CMFV]).35 The location of the foveal center was manually labeled by a retinal specialist (Q.S.Y.) on en face angiographic images.
We performed statistical analysis using SPSS for Windows, version 25.0 (IBM SPSS Inc). Descriptive statistics included mean, SD, range, and percentages where appropriate. The intraclass correlation coefficient (ICC) and κ value were used to analyze the intergrader reproducibility of the DME diagnosis. The ICC was also calculated to assess the intravisit repeatability of the fluid volume quantification. The association between DR severity and DME diagnosis was analyzed using Spearman correlation analysis. The area under the receiver operating characteristic curve (AUROC) for DME diagnosis was calculated for CST and fluid volumes. The AUROCs of CST and CMFV were compared using the method of DeLong et al.36 The corresponding sensitivity was calculated when the specificity was fixed at 95%. The sensitivities were compared using the McNemar test. All P values were from 2-sided tests and results were deemed statistically significant at P < .05.
Results
We enrolled 1 eye each of 215 patients with diabetes (117 women [54.4%] and 98 men [45.6%]; mean [SD] age, 59.6 [12.4] years), including 36 without DR, 49 with mild nonproliferative DR, 23 with moderate nonproliferative DR, 42 with severe nonproliferative DR, and 65 with proliferative DR (Table 1 and Table 2). The mean (SD) best-corrected visual acuity was 78.2 (8.2) ETDRS letters (95% CI, 77.0-79.4 ETDRS letters). The mean (SD) duration of diabetes was 20.4 (12.4) years (95% CI, 18.6-22.2 years). The clinical characteristics of the study participants are summarized in Table 1 and Table 2.
Table 1. Demographic and Clinical Characteristics of the Study Participants.
| Parameter | Value (N = 215) |
|---|---|
| Age, mean (SD) [range], y | 59.6 (12.4) [22-85] |
| Sex, No. | |
| Men | 98 |
| Women | 117 |
| Body height, mean (SD) [range], m | 1.70 (0.10) [1.42-1.96] |
| Body weight, mean (SD) [range], kg | 92.4 (21.0) [53-175] |
| BMI, mean (SD) [range] | 32.0 (6.8) [19.8-66.5] |
| Type 1 diabetes, No. (%) | 58 (27.0) |
| Duration of diabetes, mean (SD) [range], y | 20.4 (12.4) [1-59] |
| Most recent HbA1c, mean (SD) [range], % | 7.6 (1.6) [4.6-14.0] |
| Systolic blood pressure, mean (SD) [range], mm Hg | 131 (21) [72-195] |
| Diastolic blood pressure, mean (SD) [range], mm Hg | 73 (15) [39-117] |
| History of hypertension, No. (%) | 158 (73.5) |
| Axial length, mean (SD) [range], mm | 23.7 (1.1) [21.2-26.3] |
| Intraocular pressure, mean (SD) [range], mm Hg | 14.5 (3.6) [5-24] |
| BCVA, mean (SD) [range] | |
| ETDRS letter score | 78.2 (8.2) [93-40] |
| Snellen equivalent | 20/30 (1.5) lines [20/14-20/160] |
| Central subfield thickness, mean (SD) [range], μm | 303.1 (71.5) [180-686] |
| Central macular fluid volume, mean (SD) [range], mm3 | 0.0101 (0.0348) [0.0000-0.3384] |
Abbreviations: BCVA, best-corrected visual acuity; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); ETDRS, Early Treatment Diabetic Retinopathy Study; HbA1c, hemoglobin A1c.
SI conversion factor: To convert HbA1c to proportion of total hemoglobin, multiply by 0.01.
Table 2. Diabetic Retinopathy Stage.
| Stage | With DME | With CIDME | ||||
|---|---|---|---|---|---|---|
| No. (%) | BCVA (ETDRS letter score), mean (SD) [range] | BCVA (Snellen equivalent), mean (SD) [range] | No. (%) | BCVA (ETDRS letter score), mean (SD) [range] | BCVA (Snellen equivalent), mean (SD) [range] | |
| Diabetes without DR (level <20) (n = 36) | 3 (8.3) | 76.0 (10.1) [85-65] | 20/30 (2.0 lines) [20/20-20/50] | 2 (5.6) | 81.5 (5.0) [85-78] | 20/25 (1 line) [20/20-20/30] |
| Mild NPDR (level 20-35) (n = 49) | 26 (55.1) | 75.4 (9.2) [89-49] | 20/32 (1.8 lines) [20/16-20/100] | 20 (40.8) | 76.3 (9.2) [89-49] | 20/30 (1.8 lines) [20/16-20/100] |
| Moderate NPDR (level 43-47) (n = 23) | 21 (91.3) | 78.1 (7.9) [90-63] | 20/30 (1.5 lines) [20/16-20/50] | 13 (56.5) | 77.4 (9.6) [90-63] | 20/30 (2 lines) [20/16-20/60] |
| Severe NPDR (level 53) (n = 42) | 38 (90.5) | 77.6 (6.5) [90-61] | 20/30 (1.3 lines) [20/16-20/60] | 26 (61.9) | 77.0 (7.2) [90-61] | 20/30 (1.4 lines) [20/16-20/60] |
| PDR (level ≥61) (n = 65) | 48 (73.8) | 74.3 (9.3) [93-40] | 20/32 (1.8 lines) [20/16-20/160] | 32 (49.2) | 73.6 (9.3) [90-40] | 20/32 (1.9 lines) [20/16-20/160] |
Abbreviations: BCVA, best-corrected visual acuity; CIDME, center-involved DME; DME, diabetic macular edema; DR, diabetic retinopathy; ETDRS, Early Treatment Diabetic Retinopathy Study; NPDR, nonproliferative diabetic retinopathy; PDR, proliferative diabetic retinopathy.
Diabetic macular edema was detected in 136 of 215 eyes (63.3%) using structural OCT raster scans. Ninety-three of the 136 cases of DME involved the center. Diabetic macular edema could appear in patients with any stage of DR, but prevalence increased with severity of clinical DR grading (Table 1 and Table 2). The diagnosis of DME was consistent between the retinal specialists in 203 of 215 cases (94.4%) (κ = 0.877), with an ICC of 0.935. The diagnosis of center-involved DME was consistent between the retinal specialists for 192 of 215 (89.3%) cases (κ = 0.791), with an ICC of 0.884. A total of 190 of 215 eyes underwent repeated volumetric OCTA scans within the same visit. The ICC for CMFV for these 190 eyes was 0.978, and the ICC for overall fluid volume measurement was 0.976, demonstrating good intravisit repeatability of fluid volume quantification.
The AUROC of overall fluid volume for DME (including center-involved DME and non–center-involved DME) diagnosis was 0.809 (95% CI, 0.748-0.870) (eFigure 1 in the Supplement). The AUROC of CMFV for DME diagnosis was 0.841 (95% CI, 0.789-0.893), which was larger than the AUROC of CST (0.730; 95% CI, 0.664-0.796; P = .002) (eFigure 2 in the Supplement). The corresponding Youden index J was 0.639 (95% CI, 0.535-0.721) for CMFV and 0.423 (95%, CI 0.301-0.501) for CST. When the specificity was fixed at 95%, the sensitivity for detecting DME was 64.0% (95% CI, 55.3%-72.0%) using CMFV (threshold, 0.000041 mm3), which was better than the sensitivity using CST (threshold, 314.5 μm) of 42.6% (95% CI, 34.2%-51.4%; P < .001) (eTable in the Supplement).
For a center-involved DME diagnosis, the AUROC of CMFV was 0.907 (95% CI, 0.861-0.954), larger than the AUROC of CST 0.832 (95% CI, 0.775-0.889; P = .02) (Figure 1 and Figure 2). The Youden index J was 0.760 (95% CI, 0.656-0.831) for CMFV and 0.560 (95% CI, 0.436-0.643) for CST. When the specificity was fixed at 95%, the corresponding sensitivity for detection of center-involved DME was 78.5% (95% CI, 68.8%-86.3%) for CMFV (threshold, 0.000225 mm3) and 53.8% (95% CI, 43.1%-64.2%) for CST (threshold, 321.5 μm) (P = .002). With the use of the DRCR.net study center-involved DME definition of CST of 320 μm or more in male patients or 305 μm or more in female patients, the sensitivity for center-involved DME diagnosis was 60.2%, and the specificity for center-involved DME diagnosis was 90.2% (Table 3).21
Figure 1. Receiver Operating Characteristic Curves and Precision Recall Curves for Center-Involved Diabetic Macular Edema.
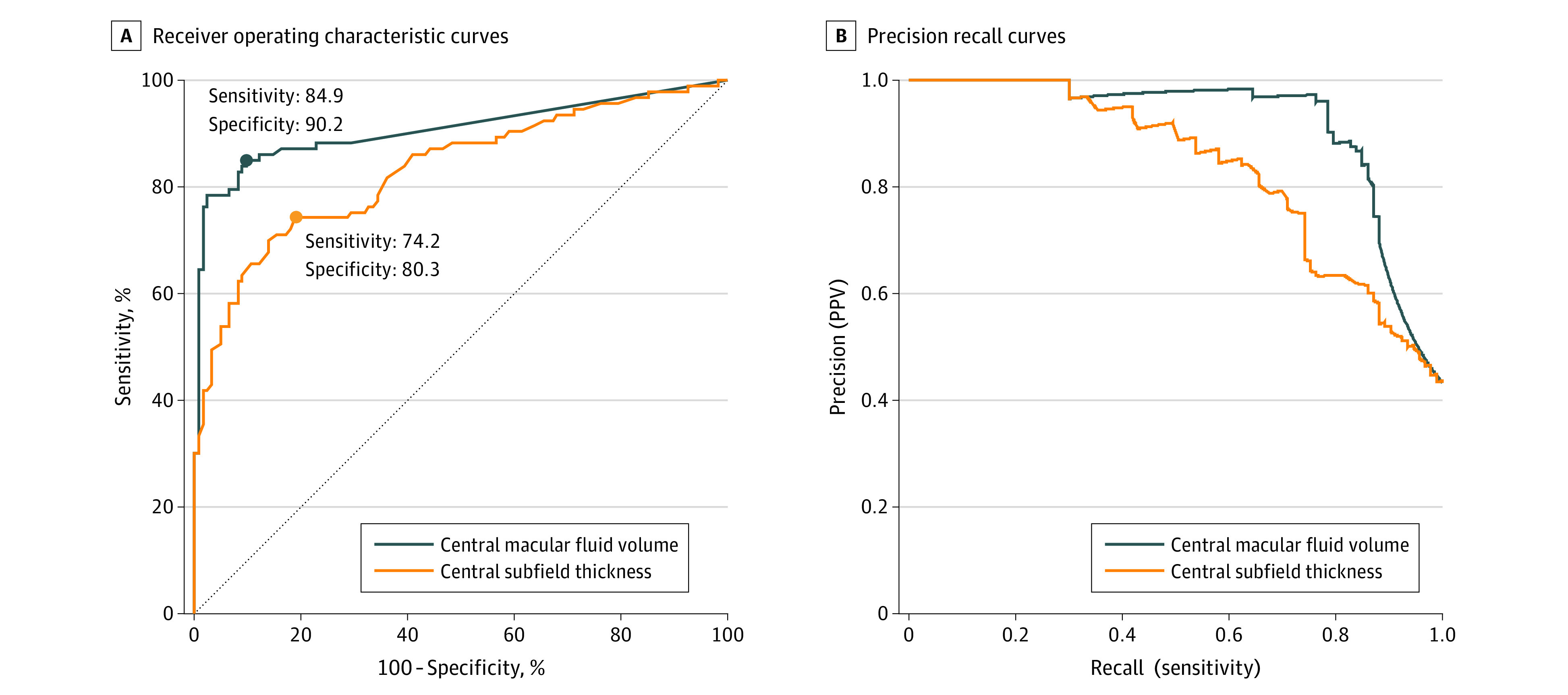
The blue and orange dots show operating points that were closest to the left upper corner. The diagonal dashed line indicates where sensitivity = 1 − specificity. PPV indicates positive predictive value.
Figure 2. Center-Involved Diabetic Macular Edema.
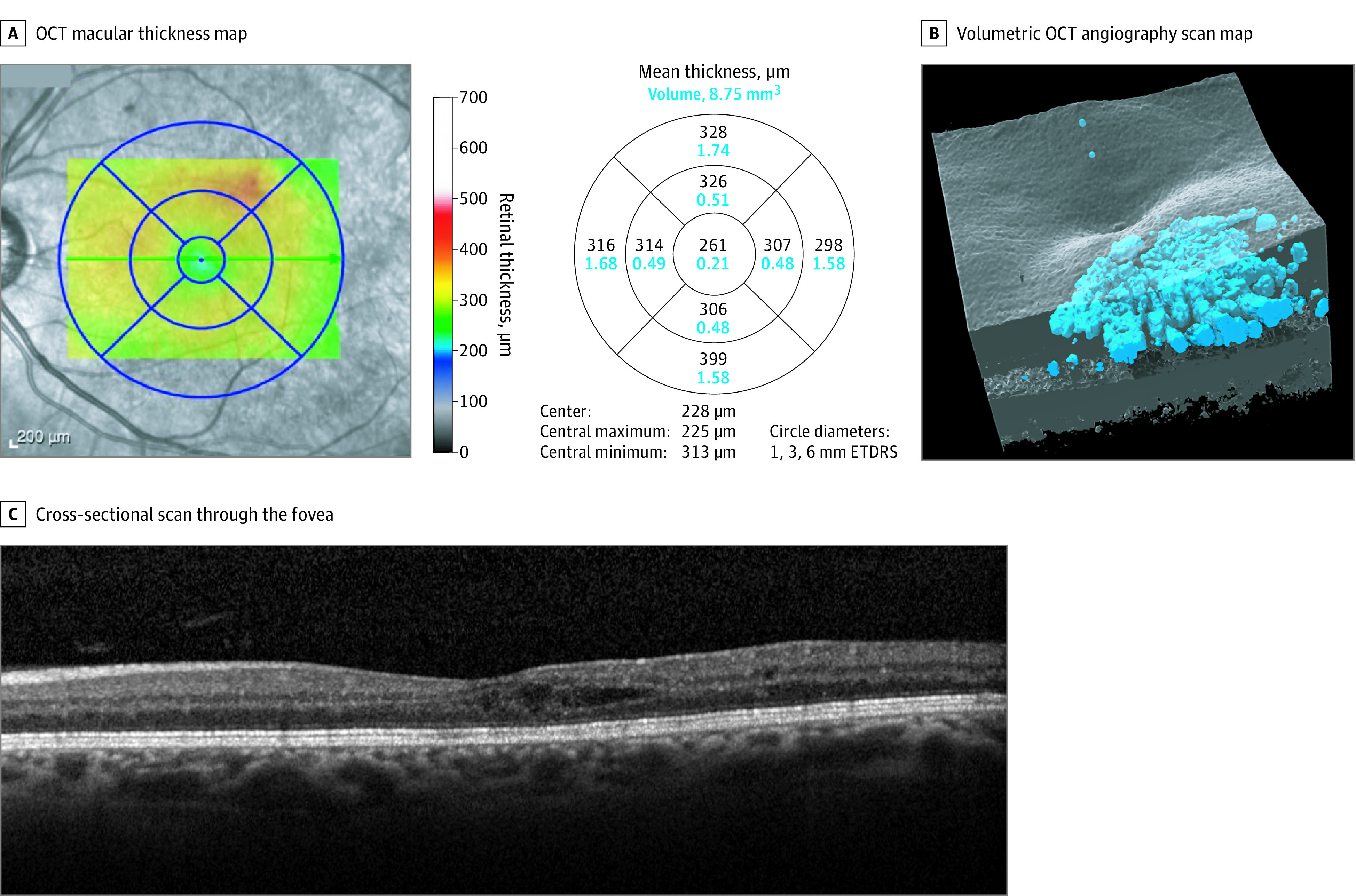
A, Optical coherence tomography (OCT) macular thickness map. B, 3-Dimensional rendering of the volumetric OCT angiography scan volume. The blue indicates automatically detected fluid. C, Cross-sectional scan through the fovea. The central macular fluid volume (0.043768 mm3) from the OCT angiography scan determined the diagnosis of diabetic macular edema but central subfield thickness (261 μm) did not. ETDRS indicates Early Treatment Diabetic Retinopathy Study.
Table 3. CIDME by Manual Grading vs CMFV, CST, or DRCR.net study standard.
| Grading | Threshold, No./total No. (%) | Total No. | |
|---|---|---|---|
| 0 | 1 | ||
| CIDME by manual grading vs CMFV theshold, No./total No. (%) | |||
| 0 | 116/122 (95.1) | 6/122 (4.9) | 122 |
| 1 | 20/93 (21.5) | 73/93 (78.5) | 93 |
| Total No. | 136 | 79 | 215 |
| CIDME by manual grading vs CST threshold, No./total No. (%) | |||
| 0 | 116/122 (95.1) | 6/122 (4.9) | 122 |
| 1 | 43/93 (46.2) | 50/93 (53.8) | 93 |
| Total No. | 159 | 56 | 215 |
| CIDME by manual grading vs CST ≥320 μm in men or ≥305 μm in women, No./total No. (%)a | |||
| 0 | 110/122 (90.2) | 12/122 (9.8) | 122 |
| 1 | 37/93 (39.8) | 56/93 (60.2) | 93 |
| Total No. | 147 | 68 | 215 |
Abbreviations: CIMDE, center-involved diabetic macular edema; CMFV, central macular fluid volume; CST, central subfield thickness; DRCR.net, Diabetic Retinopathy Clinical Research Network.
CST of 320 μm or more in men or 305 μm or more in women is the standard for CIDME used in the DRCR.net study.21
For screening purposes, a higher specificity could limit false-positive cases to avoid unneeded referral and reduce the burden to the health care system. However, to reduce missed cases, a higher sensitivity with trade-off specificity is preferred. When the specificity was fixed at 80%, the sensitivity of CMFV for detection of center-involved DME was 87.1% (95% CI, 78.5%-93.1%), higher than that of CST (74.2%; 95% CI, 64.1%-82.7%; P = .004).
When the specificity was fixed at 95%, there were 28 cases with center-involved DME detected based on CMFV but missed according to CST (eyes with CMFV ≥0.000225 mm3 but CST <321.5 μm). Compared with those detected using either CMFV or CST (eyes with CMFV ≥0.000225 mm3 and CST ≥321.5 μm), cases missed by CST (eyes with CMFV ≥0.000225 mm3 but CST <321.5 μm) were associated with a higher proportion of previous macular laser treatment (11 of 28 [39.3%; 95% CI, 21.5%-59.4%] vs 12 of 65 [18.5%; 95% CI, 9.9%-30.0%]; P = .03), female sex (20 of 28 [71.4%; 95% CI, 51.3%-86.8%] vs 31 of 65 [47.7%; 95% CI, 35.1%-60.5%]; P = .04), and a thinner CST (mean [SD] thickness, 290.8 [22.8] μm vs 369.4 [92.2] μm; P < .001), but they were not different in terms of age (mean [SD] age, 63.8 [8.7] years vs 59.3 [12.9] years; P = .09), axial length (mean [SD] length, 23.9 [0.8] mm vs 23.5 [1.0] mm; P = .11), duration of diabetes (mean [SD] duration, 19.2 [10.8] years vs 17.9 [11.2] years; P = .62), severity of DR (24 of 65 [36.9%] vs 8 of 28 [28.6%] proliferative DR; P = .67), or best-corrected visual acuity (BCVA) (mean [SD], 77.6 [9.0] letters vs 75.0 [8.6] letters; P = .19). There were 5 eyes with center-involved DME missed by CMFV but detected by CST (CMFV <0.000225 mm3 but CST ≥321.5 μm). We did not perform a statistical analysis for these eyes owing to the limited number. Four of the 5 eyes had relatively mild edema (CST of 327, 328, 334, and 334 μm, respectively), low signal strength for OCTA scans (signal strength index of 46, 52, 56, and 57, respectively), and good visual acuity (74, 77, 78, and 81 ETDRS letters, respectively). One eye with CST of 464 μm, signal strength index of 62, and visual acuity 80 ETDRS letters was missed by CMFV owing to a large microaneurysm located in the macular center and the fluid mainly distributed parafoveally, outside of the central 1 mm. This case was diagnosed as DME using overall fluid volume.
There was a significant correlation between the central fluid volume and BCVA, with a correlation coefficient of −0.303 (P < .001), which was similar to the correlation coefficient between CST and BCVA of −0.339 (P < .001). There was also a significant correlation between CMFV and CST, with a correlation coefficient of 0.573 (P < .001) (eFigure 3 in the Supplement).
Discussion
Traditional DME screening with nonstereoscopic retinal photography depends on the detection of characteristics such as hard exudates, microaneurysm, and hemorrhages as surrogate markers.3 These surrogate markers have a sensitivity of only 60% to 73% and a specificity of only 67% to 79%.3,5 Optical coherence tomography is more sensitive than retinal photography for the detection of retinal thickening.6 Visual examination of the OCT images by a retinal specialist for the presence of intraretinal or subretinal fluid has the highest sensitivity and specificity for DME detection.15 However, using a retinal specialist to screen every patient with diabetes is usually not feasible and is an inefficient use of health care resources.37 Therefore, an automated quantifiable biomarker would be very useful for DME screening using OCT, particularly in settings without ophthalmologists. Retinal thickness can be automatically measured using many OCT systems, and the CST has been used in many clinical studies as an objective quantifiable parameter to detect CME and assess its severity.16,17,18,19,20 Optical coherence tomography is used in DME screening because it has better diagnostic sensitivity than retinal photography15 and is less costly than an examination by an ophthalmologist.
Despite its wide use, CST has several potential limitations as a diagnostic biomarker for DME. First, it ignores the macula outside the central fovea and thus is more likely to miss non–center-involved DME, which is consistent with our results. Second, CST may be confounded by normal human population variation. This finding was consistent with our result that showed center-involved DME to be missed by CST more frequently in women, who, on average, have thinner retina than men.21 Third, CST could be confounded by retinal atrophy due to DR, which may reduce its diagnostic sensitivity. This finding was supported by the fact that center-involved DME was missed by CST more frequently in eyes with previous focal laser treatment, which is associated with retinal atrophy.38
Because CMFV does not have these theoretical limitations, we hypothesized that it would be a better biomarker than CST for DME diagnosis. This hypothesis was found to be true for both center-involved and non–center-involved DME.
As a biomarker, CMFV could also be used to assess disease severity. Its performance in this role appears to be limited because there was only a moderate association between CMFV and BCVA (correlation coefficient, −0.303), similar to the association between CST and BCVA (correlation coefficient, −0.339). This finding is consistent with previous studies. Browning et al39 reported a correlation coefficient of 0.52 at baseline between CST and BCVA in 251 treatment-naive patients in the DRCR.net clinical trial. Most of the participants in our study were previously treated. Treatments such as focal laser may lessen the association between severity of macular edema and BCVA. It is not surprising that neither CMFV nor CST is limited in its ability to determine BCVA because they primarily assess edema and miss many known aspects of DR, such as structural disorganization and ischemia. Other OCT and OCTA biomarkers that capture these other features29,30,32,40 may be synergistic with CMFV and CST in determining BCVA. It remains unclear whether CMFV is associated with better clinical care.
Limitations
This study has some limitations. Central macular fluid volume may also be useful as a predictive and pharmacodynamic biomarker for anti–vascular endothelial growth factor and laser treatments. The cross-sectional design of the present study does not allow us to study these potential new applications; longitudinal treatment studies are needed. In eyes with a low signal strength index and mild DME with mainly parafoveal fluid, DME may be missed by measuring CMFV. However, these eyes that CMFV missed usually had relatively good visual acuity without an urgent need for treatment. In the present study, we used DME diagnosed by retinal specialists through reviewing structural OCT scans as the criterion standard for DME diagnosis. This simulates real-world practice because clinicians generally diagnose DME by reviewing structural OCT scans. We measured macular fluid volume on volumetric OCTA scans because they have a denser scanning, enabling an accurate measurement of the fluid volume. The 2 different OCT instruments and scan patterns may lead to some discrepancy. For example, some fluid detected on the dense volumetric OCTA scans may not be shown on structural OCT scans. Currently, structural OCT is widely available in ophthalmology worldwide, while OCTA is available to mostly retinal practices in developed countries and some main eye centers in developing countries.
The fact that our current deep learning–based algorithm requires dense OCTA volumetric scans to perform an accurate fluid volume measurement may limit its generalizability to more extensively available structural OCT scans with a less-dense scan pattern. Our inclusion and exclusion criteria (including patients with type 1 diabetes of >5-year duration or type 2 diabetes of any duration and age between 18 and 85 years and excluding pregnant or lactating women) may also limit the generalizability of study results. The present study does not determine whether CMFV is associated with better clinical care.
Conclusions
These data suggest that CMFV may be more accurate as a DME biomarker than the commonly used CST measurement, although the clinical relevance of this potential cannot be determined from this investigation. This result has practical implications because CMFV may be quantified automatically using our deep learning approach.35 The use of CMFV may improve the accuracy of OCT-based DME screening without the cost and subjectivity of grading by human experts.
eFigure 1. Receiver Operating Characteristic Curves and Precision Recall Curves of Macular Fluid Volume for Diabetic Macular Edema
eFigure 2. Receiver Operating Characteristic Curves and Precision Recall Curves of Central Macular Fluid Volume and Central Subfield Thickness for Diabetic Macular Edema
eFigure 3. Central Macular Fluid Volume vs Central Macular Thickness
eTable. Diabetic Macular Edema by Manual Grading vs by Central Macular Fluid Volume or Central Subfield Thickness
References
- 1.Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376(9735):124-136. doi: 10.1016/S0140-6736(09)62124-3 [DOI] [PubMed] [Google Scholar]
- 2.Yau JWY, Rogers SL, Kawasaki R, et al. ; Meta-Analysis for Eye Disease (META-EYE) Study Group . Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556-564. doi: 10.2337/dc11-1909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan GS, Cheung N, Simó R, Cheung GC, Wong TY. Diabetic macular oedema. Lancet Diabetes Endocrinol. 2017;5(2):143-155. doi: 10.1016/S2213-8587(16)30052-3 [DOI] [PubMed] [Google Scholar]
- 4.Wong TY, Sun J, Kawasaki R, et al. Guidelines on diabetic eye care: the International Council of Ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125(10):1608-1622. doi: 10.1016/j.ophtha.2018.04.007 [DOI] [PubMed] [Google Scholar]
- 5.Prescott G, Sharp P, Goatman K, et al. Improving the cost-effectiveness of photographic screening for diabetic macular oedema: a prospective, multi-centre, UK study. Br J Ophthalmol. 2014;98(8):1042-1049. doi: 10.1136/bjophthalmol-2013-304338 [DOI] [PubMed] [Google Scholar]
- 6.Virgili G, Menchini F, Casazza G, et al. Optical coherence tomography (OCT) for detection of macular oedema in patients with diabetic retinopathy. Cochrane Database Syst Rev. 2015;1:CD008081. doi: 10.1002/14651858.CD008081.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kinyoun J, Barton F, Fisher M, Hubbard L, Aiello L, Ferris F III; The ETDRS Research Group . Detection of diabetic macular edema: ophthalmoscopy versus photography—Early Treatment Diabetic Retinopathy Study Report Number 5. Ophthalmology. 1989;96(6):746-750. doi: 10.1016/S0161-6420(89)32814-4 [DOI] [PubMed] [Google Scholar]
- 8.Bhavsar KV, Subramanian ML. Risk factors for progression of subclinical diabetic macular oedema. Br J Ophthalmol. 2011;95(5):671-674. doi: 10.1136/bjo.2010.182337 [DOI] [PubMed] [Google Scholar]
- 9.Bressler NM, Miller KM, Beck RW, et al. ; Diabetic Retinopathy Clinical Research Network . Observational study of subclinical diabetic macular edema. Eye (Lond). 2012;26(6):833-840. doi: 10.1038/eye.2012.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Browning DJ, Fraser CM. The predictive value of patient and eye characteristics on the course of subclinical diabetic macular edema. Am J Ophthalmol. 2008;145(1):149-154. doi: 10.1016/j.ajo.2007.08.038 [DOI] [PubMed] [Google Scholar]
- 11.Browning DJ, Fraser CM, Clark S. The relationship of macular thickness to clinically graded diabetic retinopathy severity in eyes without clinically detected diabetic macular edema. Ophthalmology. 2008;115(3):533-539. doi: 10.1016/j.ophtha.2007.06.042 [DOI] [PubMed] [Google Scholar]
- 12.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254(5035):1178-1181. doi: 10.1126/science.1957169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruia S, Saxena S, Gemmy Cheung CM, Gilhotra JS, Lai TY. Spectral domain optical coherence tomography features and classification systems for diabetic macular edema: a review. Asia Pac J Ophthalmol (Phila). 2016;5(5):360-367. doi: 10.1097/APO.0000000000000218 [DOI] [PubMed] [Google Scholar]
- 14.Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic retinopathy Preferred Practice Pattern. Ophthalmology. 2020;127(1):66-P145. doi: 10.1016/j.ophtha.2019.09.025 [DOI] [PubMed] [Google Scholar]
- 15.Olson J, Sharp P, Goatman K, et al. Improving the economic value of photographic screening for optical coherence tomography–detectable macular oedema: a prospective, multicentre, UK study. Health Technol Assess. 2013;17(51):1-142. doi: 10.3310/hta17510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bressler NM, Beaulieu WT, Maguire MG, et al. ; Diabetic Retinopathy Clinical Research Network . Early response to anti–vascular endothelial growth factor and two-year outcomes among eyes with diabetic macular edema in Protocol T. Am J Ophthalmol. 2018;195:93-100. doi: 10.1016/j.ajo.2018.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bressler NM, Odia I, Maguire M, et al. ; DRCR Retina Network . Association between change in visual acuity and change in central subfield thickness during treatment of diabetic macular edema in participants randomized to aflibercept, bevacizumab, or ranibizumab: a post hoc analysis of the Protocol T randomized clinical trial. JAMA Ophthalmol. 2019;137(9):977-985. doi: 10.1001/jamaophthalmol.2019.1963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen QD, Brown DM, Marcus DM, et al. ; RISE and RIDE Research Group . Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119(4):789-801. doi: 10.1016/j.ophtha.2011.12.039 [DOI] [PubMed] [Google Scholar]
- 19.Reddy RK, Pieramici DJ, Gune S, et al. Efficacy of ranibizumab in eyes with diabetic macular edema and macular nonperfusion in RIDE and RISE. Ophthalmology. 2018;125(10):1568-1574. doi: 10.1016/j.ophtha.2018.04.002 [DOI] [PubMed] [Google Scholar]
- 20.Sepah YJ, Sadiq MA, Boyer D, et al. ; READ-3 Study Group . Twenty-four-month outcomes of the Ranibizumab for Edema of the Macula in Diabetes—Protocol 3 with High Dose (READ-3) Study. Ophthalmology. 2016;123(12):2581-2587. doi: 10.1016/j.ophtha.2016.08.040 [DOI] [PubMed] [Google Scholar]
- 21.Chalam KV, Bressler SB, Edwards AR, et al. ; Diabetic Retinopathy Clinical Research Network . Retinal thickness in people with diabetes and minimal or no diabetic retinopathy: Heidelberg Spectralis optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53(13):8154-8161. doi: 10.1167/iovs.12-10290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dai W, Tham YC, Cheung N, et al. Macular thickness profile and diabetic retinopathy: the Singapore Epidemiology of Eye Diseases Study. Br J Ophthalmol. 2018;102(8):1072-1076. doi: 10.1136/bjophthalmol-2017-310959 [DOI] [PubMed] [Google Scholar]
- 23.Gupta P, Sidhartha E, Tham YC, et al. Determinants of macular thickness using spectral domain optical coherence tomography in healthy eyes: the Singapore Chinese Eye study. Invest Ophthalmol Vis Sci. 2013;54(13):7968-7976. doi: 10.1167/iovs.13-12436 [DOI] [PubMed] [Google Scholar]
- 24.Hashemi H, Khabazkhoob M, Yekta A, Emamian MH, Nabovati P, Fotouhi A. The distribution of macular thickness and its determinants in a healthy population. Ophthalmic Epidemiol. 2017;24(5):323-331. doi: 10.1080/09286586.2017.1290808 [DOI] [PubMed] [Google Scholar]
- 25.Kelty PJ, Payne JF, Trivedi RH, Kelty J, Bowie EM, Burger BM. Macular thickness assessment in healthy eyes based on ethnicity using Stratus OCT optical coherence tomography. Invest Ophthalmol Vis Sci. 2008;49(6):2668-2672. doi: 10.1167/iovs.07-1000 [DOI] [PubMed] [Google Scholar]
- 26.Tariq YM, Li H, Burlutsky G, Mitchell P. Ethnic differences in macular thickness. Clin Exp Ophthalmol. 2011;39(9):893-898. doi: 10.1111/j.1442-9071.2011.02593.x [DOI] [PubMed] [Google Scholar]
- 27.von Hanno T, Lade AC, Mathiesen EB, Peto T, Njølstad I, Bertelsen G. Macular thickness in healthy eyes of adults (N = 4508) and relation to sex, age and refraction: the Tromsø Eye Study (2007-2008). Acta Ophthalmol. 2017;95(3):262-269. doi: 10.1111/aos.13337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jia Y, Bailey ST, Hwang TS, et al. Quantitative optical coherence tomography angiography of vascular abnormalities in the living human eye. Proc Natl Acad Sci U S A. 2015;112(18):E2395-E2402. doi: 10.1073/pnas.1500185112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hwang TS, Gao SS, Liu L, et al. Automated quantification of capillary nonperfusion using optical coherence tomography angiography in diabetic retinopathy. JAMA Ophthalmol. 2016;134(4):367-373. doi: 10.1001/jamaophthalmol.2015.5658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hwang TS, Hagag AM, Wang J, et al. Automated quantification of nonperfusion areas in 3 vascular plexuses with optical coherence tomography angiography in eyes of patients with diabetes. JAMA Ophthalmol. 2018;136(8):929-936. doi: 10.1001/jamaophthalmol.2018.2257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hwang TS, Jia Y, Gao SS, et al. Optical coherence tomography angiography features of diabetic retinopathy. Retina. 2015;35(11):2371-2376. doi: 10.1097/IAE.0000000000000716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hwang TS, Zhang M, Bhavsar K, et al. Visualization of 3 distinct retinal plexuses by projection-resolved optical coherence tomography angiography in diabetic retinopathy. JAMA Ophthalmol. 2016;134(12):1411-1419. doi: 10.1001/jamaophthalmol.2016.4272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.You QS, Guo Y, Wang J, et al. Detection of clinically unsuspected retinal neovascularization with wide-field optical coherence tomography angiography. Retina. 2020;40(5):891-897. doi: 10.1097/IAE.0000000000002487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 35.Guo Y, Xiong H, Hormel T, Wang J, Hwang T, Jia Y. Automated volumetric segmentation of retinal fluid on optical coherence tomography using deep learning. Invest Ophthalmol Vis Sci. 2019;60(11):026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837-845. doi: 10.2307/2531595 [DOI] [PubMed] [Google Scholar]
- 37.Bragge P, Gruen RL, Chau M, Forbes A, Taylor HR. Screening for presence or absence of diabetic retinopathy: a meta-analysis. Arch Ophthalmol. 2011;129(4):435-444. doi: 10.1001/archophthalmol.2010.319 [DOI] [PubMed] [Google Scholar]
- 38.Rutledge BK, Wallow IH, Poulsen GL. Sub-pigment epithelial membranes after photocoagulation for diabetic macular edema. Arch Ophthalmol. 1993;111(5):608-613. doi: 10.1001/archopht.1993.01090050042025 [DOI] [PubMed] [Google Scholar]
- 39.Browning DJ, Glassman AR, Aiello LP, et al. ; Diabetic Retinopathy Clinical Research Network . Relationship between optical coherence tomography–measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology. 2007;114(3):525-536. doi: 10.1016/j.ophtha.2006.06.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Z, Camino A, Zhang M, et al. Automated detection of photoreceptor disruption in mild diabetic retinopathy on volumetric optical coherence tomography. Biomed Opt Express. 2017;8(12):5384-5398. doi: 10.1364/BOE.8.005384 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Receiver Operating Characteristic Curves and Precision Recall Curves of Macular Fluid Volume for Diabetic Macular Edema
eFigure 2. Receiver Operating Characteristic Curves and Precision Recall Curves of Central Macular Fluid Volume and Central Subfield Thickness for Diabetic Macular Edema
eFigure 3. Central Macular Fluid Volume vs Central Macular Thickness
eTable. Diabetic Macular Edema by Manual Grading vs by Central Macular Fluid Volume or Central Subfield Thickness


