Abstract
Background:
There is increasing concern of iatrogenic hip instability after capsulotomy during surgery. Greater emphasis is now being placed on capsular closure during surgery. There are no prospective studies that address whether capsular closure has any effect on outcomes.
Purpose/Hypothesis:
The purpose of this study was to evaluate patient outcomes after interportal capsulotomy repair compared with no repair. We hypothesized that restoration of normal capsular anatomy with interportal repair will achieve clinical outcomes similar to those for no repair.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
Adult patients with femoral acetabular impingement indicated for hip arthroscopy were randomized into either the capsular repair (CR) or the no repair (NR) groups. All patients underwent standard hip arthroscopy with labral repair with or without CAM/pincer lesion resection. Clinical outcomes were measured via the Hip Outcome Score–Activities of Daily Living (HOS-ADL) subscale, Hip Outcome Score–Sport Specific (HOS-SS) subscale, modified Harris Hip Score (mHHS), visual analog scale for pain, International Hip Outcome Tool, and Veterans RAND 12-Item Health Survey (VR-12).
Results:
A total of 54 patients (56 hips) were included (26 men and 30 women) with a mean age of 33 years. The HOS-ADL score significantly improved at 2 years in both the NR group (from 68.1 ± 20.5 to 88.6 ± 20.0; P < .001) and the CR group (from 59.2 ± 18.8 to 91.7 ± 12.3; P < .001). The HOS-SS score also significantly improved in both the NR group (from 41.1 ± 25.8 to 84.1 ± 21.9; P < .001) and the CR group (from 32.7 ± 23.7 to 77.7 ± 23.0; P < .001). Improvement was noted for all secondary outcome measures; however, there was no significant difference between the groups at any time point. Between 1 and 2 years, the NR group showed significant worsening on the HOS-ADL (–1.21 ± 5.09 vs 4.28 ± 7.91; P = .044), mHHS (1.08 ± 10.04 vs 10.12 ± 11.76; P = .042), and VR-12 Physical (–2.15 ± 5.52 vs 4.49 ± 7.30; P = .014) subsets compared with the CR group.
Conclusion:
There was significant improvement in the VR-12 Physical subscale at 2 years postoperatively in the capsular CR group compared with the NR group. Capsular closure appears to have no detrimental effect on functional outcome scores after hip arthroscopy. We recommend restoration of native anatomy if possible when performing hip arthroscopy.
Keywords: femoroacetabular impingement, hip arthroscopy, cartilage, biomechanics of ligament
The use of hip arthroscopy has increased significantly over the past decade as a tool to treat nonarthritic hip disorders. As surgical techniques and instrumentation have evolved, arthroscopic procedures to address femoroacetabular impingement (FAI) and labral tears requiring repair or reconstruction have become commonplace. For the suitable patient, short- and medium-term outcomes clearly suggest benefit to these procedures. As the number of arthroscopic hip procedures continues to increase, our understanding of possible complications as well as nuances of the surgery continues to evolve.
Among the most devastating of these complications is postoperative hip dislocation secondary to instability. While rarely reported in the literature, its possibility has certainly been noticed among hip arthroscopists.1,10,13,20,22 Benali and Katthagen1 reported on a case of iatrogenic instability in a 49-year-old woman after resection of a labral tear and pincer lesion. Matsuda10 reported on a case of postoperative hip dislocation also occurring after labral resection and overdistraction to retrieve a loose body, ultimately necessitating a mini-open casulorrhaphy. Sansone et al22 reported on 2 cases of iatrogenic dislocation after capsulorrhaphy and iliopsoas tenotomy, raising the question of the necessity of some of the dynamic stabilizers of the hip.
Unaddressed laxity is now a known source of failure after primary arthroscopic hip surgery and an indication for revision surgery. Central to both of these problems is the ongoing debate as to whether the hip capsule should be routinely closed at the end of the procedure. Hip joint stability is dependent upon both static and dynamic stabilizers. Static stabilization of the hip is imparted by the osseous congruity of the femoroacetabular joint, the labrum, and the capsuloligamentous complex. The dynamic stabilizers include the hip girdle musculature, as well as proprioceptive and neuromuscular stabilization.
During arthroscopy, an interportal capsulotomy is typically performed to gain access to the central and peripheral compartments of the hip joint and address any intra-articular femoral or acetabular chondral pathology or labral tearing. While in the past, capsular entry sites have been left unrepaired because of concerns of overconstraint and the belief that a pseudocapsule re-forms in its place to maintain stability, the data supporting this argument are limited. Newer data suggest that the trend is changing. In 2015, Gupta et al6 found that 48% of high-volume hip arthroscopists routinely close the capsule, as compared with only 11% who routinely do not close the capsule. Frank et al5 and Domb et al4 have previously reviewed the effects of capsular closure in retrospective series, with differing outcomes. However, the effect of capsular closure on patient outcomes has not yet been fully elucidated.
While recent studies do suggest that capsular repair may be beneficial, to date, there are no prospective randomized studies that address the clinical benefit or detriment of capsular closure after hip arthroscopy. The purpose of this study was to evaluate whether capsular closure significantly improves clinical outcomes after hip arthroscopy. We hypothesized that restoration of normal capsular anatomy with interportal repair will achieve clinical outcomes similar to those of no repair.
Methods
Study Design
A power analysis was conducted to determine the study size with a significance of .05 for 2-tailed sidedness. The Hip Outcome Score–Activities of Daily Living (HOS-ADL) subscale was used as the primary outcome measure. We used a minimal clinically important difference of 10 points based on previous studies, with a standardized power of 0.8. Under these parameters, we calculated the need for 34 patients to be entered into this study. We set a total patient enrollment goal of 56 patients in order to allow for higher standard deviations in the outcome score than expected.
After institutional review board approval, all patients who met study inclusion and exclusion criteria and who signed informed consent were enrolled in this prospective study. Study enrollment was from November 2013 to March 2016. Criteria for study inclusion were patients (1) aged between 18 and 65 years who were scheduled to undergo primary hip arthroscopy by the senior author (M.B.B.), (2) who carried a diagnosis of FAI with labral tearing, and (3) who were scheduled to undergo hip arthroscopy with labral repair and osteoplasty. Exclusion criteria included (1) a narrowed femoroacetabular joint space measuring <2 mm on plain radiographs, (2) acetabular dysplasia with a center-edge angle <25°, (3) a history of prior surgery on the hip, acetabular fracture, avascular necrosis, Legg-Calve-Perthes disease, or lumbar radiculopathy, and (4) evidence of significant hypermobility defined by a Beighton scale >6.
Randomization and Blinding
Upon enrollment by clinical research staff, each patient was assigned a study number in accordance with the order in which he or she enrolled. Group assignment was then determined using a random-number generator to randomize participants to either the no interportal capsular repair (NR) group or the complete capsular repair (CR) group. Patients were blinded to their group assignment from the time of enrollment in the study through 2-year follow-up survey completion.
Unlike our standard practice, patients agreed not to receive copies of their operative report so as not to be unblinded. Operative reports were, however, made accessible to the patients upon specific request to the surgeon or staff. This request would then be noted within the study results. The surgeon and operative staff were necessarily unblinded at the time of surgery. All postoperative study data collection was performed solely by electronic survey so as to minimize the possible introduction of bias by the unblinded surgeon.
Radiographic Analysis
All patients consenting to study participation underwent our standard radiographic hip series, consisting of anteroposterior and modified Dunn views as well as magnetic resonance imaging. Radiographs were obtained with the coccyx positioned approximately 1 cm above the pubic symphysis and the obturator foramina and greater trochanters symmetric. The alpha angle and lateral center-edge angle of Wiberg were measured on plain radiographs using a digital picture archiving and communication system.
Data Collection and Functional Outcome Analysis
Data were collected using the Surgical Outcome System (Arthrex), a survey-based response system that regularly connects with operative patients for a period of 2 years. The primary patient-reported outcomes (PROs) surveyed included the HOS-ADL subscale, Hip Outcome Score–Sport Specific (HOS-SS) subscale, modified Harris Hip Score (mHHS), visual analog scale (VAS) for pain, International Hip Outcome Tool (iHOT-12), and Veterans RAND 12-Item Health Survey (VR-12). Patient characteristics and surgical procedure were recorded, and PRO scores were obtained at 3 months, 6 months, 1 year, and 2 years postoperatively.
Surgical Technique
All patients were placed supine on the operative table, and traction was applied using an arthroscopic hip patient positioning system. And 18-gauge spinal needle was used to create an air arthrogram and allow for full distraction of the joint. An anterolateral portal was created using fluoroscopic guidance, followed by a midanterior portal using an outside-in approach. Once completed, a diagnostic arthroscopy was performed. An interportal capsulotomy was created with a beaver blade, transecting the capsule between the 11- and 3-o’clock positions. Treatment of any labral or acetabular pathology was performed as indicated, including labral repair ± chondroplasty. The traction was then removed and an osteoplasty was performed as necessary using multiple fluoroscopic views to ensure complete cam resection. Once complete, capsular closure of the distal limb of any T-capsulotomy was performed. Patients in the CR group then underwent interportal capsulotomy closure. Capsular closure was accomplished using simple sutures with knots tied on the superficial aspect of the hip capsule. In all patients, a spinal needle was then percutaneously placed under direct arthroscopic visualization to lie immediately superficial to the capsule, and 3 mL of platelet-rich plasma (PRP) was injected (Angel System 2%; Arthrex) through the spinal needle.
Rehabilitation
The same rehabilitation protocol was used for all patients. Patients were placed into protective ankle supports at the end of the surgery to prevent inadvertent external rotation upon awaking from anesthesia and for use during sleep for the first week after surgery. They were made 50% weightbearing with the use of crutches for 3 weeks and were discharged home the same day as the surgery. A hinged hip brace was to be worn while ambulating and was unlocked from 0° to 90° immediately. Patients were also instructed to avoid hip hyperflexion and hyperextension but could begin using a stationary bicycle on postoperative day 1.
Statistical Analysis
The statistical program IBM SPSS Version 22 (IBM Corp) was used to analyze the data. The Shapiro-Wilk test was applied to ensure that the data were normally distributed. Intergroup comparisons of continuous variables with normally distributed data were assessed using a t test, and intergroup comparisons of continuous variables with data that were not normally distributed were analyzed using a Mann-Whitney U test. Chi-square tests were also used to assess categorical data. The significance level was set at P < .05.
Results
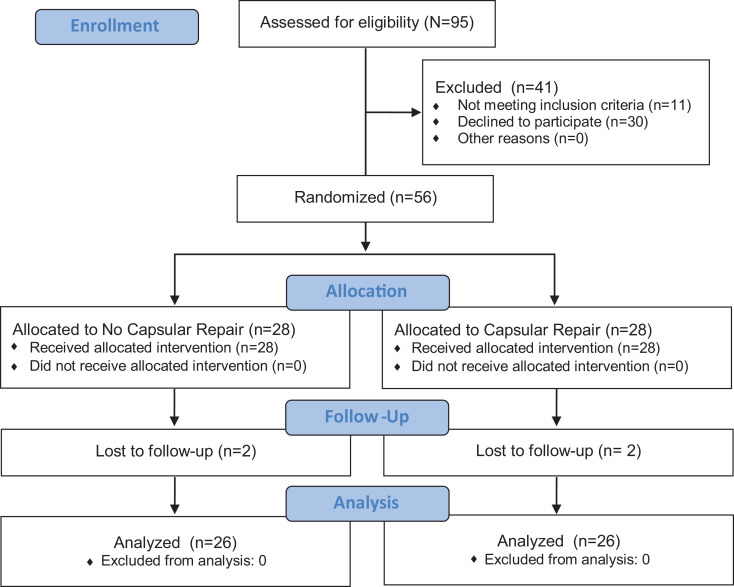
A total of 55 adult patients (56 hips) meeting criteria were recruited for this study; 28 patients were randomized to each group (Table 1 and Figure 1). For all patients, the mean age at the time of surgery was 32.7 ± 9.1 years (range, 19-53 years) and the average body mass index (BMI) was 25.1 ± 4.5 kg/m2. There were 28 patients within each group. Two patients from each group were lost to follow-up at 6 months, and 2 patients from each group were lost between the 1- and 2-year postoperative time period. There was no crossover between groups. No patient requested his or her operative report before the 2-year postoperative time period. All data available were used for analysis regardless of whether the patient was subsequently lost to follow-up. The NR group had 8 women and 20 men, and the CR group had 22 women and 6 men (P < .001). Radiographically, the average alpha angle was 64.4° ± 9.89°, and the average lateral center-edge angle was 33.9° ± 6.1°.
Table 1.
Patient Characteristicsa
| All Patients | NR Group | CR Group | P Value | |
|---|---|---|---|---|
| Patients | 56 | 28 | 28 | |
| Sex | <.001 | |||
| Male | 26 | 20 | 6 | |
| Female | 30 | 8 | 22 | |
| Age, y | 32.7 ± 9.1 | 33.7 ± 9.7 | 31.8 ± 8.6 | .43 |
| Height, cm | 66.5 ± 3.9 | 70.7 ± 4.2 | 66.5 ± 3.9 | <.001 |
| Weight, kg | 169.7 ± 43.8 | 184.9 ± 45.1 | 153.9 ± 36.8 | <.001 |
| BMI, kg/m2 | 25.1 ± 4.5 | 25.7 ± 4.1 | 24.4 ± 4.9 | .15 |
| Side of surgery | .59 | |||
| Right | 30 | 16 | 14 | |
| Left | 26 | 12 | 14 | |
| Preoperative center-edge angle, deg | 33.9 ± 6.1 | 34.1 ± 6.0 | 33.6 ± 6.3 | .77 |
| Preoperative alpha angle, deg | 64.4 ± 9.9 | 64.9 ± 10.6 | 63.9 ± 9.2 | .71 |
| Labral tear size, h | 2.4 ± 1.0 | 2.7 ± 1.0 | 2.1 ± 0.9 | .07 |
| Acetabular rim trimming | 48 | 26 | 22 | |
| Femoral osteochondroplasty | 56 | 28 | 28 | |
| Labral repair | 56 | 28 | 28 |
aData are presented as number of patients or mean ± SD. BMI, body mass index; CR, capsular repair; NR, no repair.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flowchart of study enrollment process.
There was a significant difference in the distribution of men and women across both groups, with a higher proportion of women in the CR group than in the NR group. The NR group participants were slightly older and had a higher BMI, but this difference was not significant. However, the NR group participants were significantly taller and heavier compared with the CR group. There were no significant differences in laterality, center-edge angle, alpha angle, hours of tear size, or complications between the groups. Nonetheless, it should be noted that the CR group experienced no complications. The distribution of acetabuloplasty pincer, cartilage chondral damage, debridement or microfracture, debridement microfracture, and T-capsulotomy across the groups was also not significantly different.
Clinical Outcomes
The NR group had a higher mean score for each preoperative clinical measure apart from the preoperative VAS score; however, no significant differences were found between the groups. For all patients, there was a significant improvement at 2 years in the HOS-ADL, HOS-SS, iHOT-12, mHHS, VAS, and VR-12 Physical subscale (P < .001 for all) as compared with the preoperative scores (Table 2).
Table 2.
Patient-Reported Outcomes for All Patientsa
| Preoperative | Postoperative | P Value | |
|---|---|---|---|
| All Patients | |||
| HOS-ADL | 63.7 ± 20.0 | 88.9 ± 17.9 | <.001 |
| HOS-SS | 36.8 ± 24.8 | 79.4 ± 24.3 | <.001 |
| iHOT-12 | 39.6 ± 20.0 | 73.7 ± 25.4 | <.001 |
| mHHS | 53.0 ± 18.7 | 83.6 ± 21.4 | <.001 |
| VAS | 4.7 ± 2.1 | 1.8 ± 2.2 | <.001 |
| VR-12 Physical | 33.7 ± 10.3 | 49.7 ± 10.1 | <.001 |
| VR-12 Mental | 53.6 ± 16.1 | 51.9 ± 10.3 | .28 |
| NR Group | |||
| HOS-ADL | 69.7 ± 19.4 | 85.1 ± 23.7 | <.001 |
| HOS-SS | 41.1 ± 25.8 | 76.4 ± 34.8 | <.001 |
| iHOT-12 | 40.6 ± 21.0 | 73.6 ± 31.1 | <.001 |
| mHHS | 54.9 ± 18.1 | 82.9 ± 24.7 | <.001 |
| VAS | 4.6 ± 2.3 | 1.9 ± 2.5 | <.001 |
| VR-12 Physical | 35.1 ± 10.6 | 47.4 ± 12.1 | <.001 |
| VR-12 Mental | 50.0 ± 10.7 | 53.3 ± 10.5 | .12 |
| CR Group | |||
| HOS-ADL | 59.3 ± 18.7 | 90.1 ± 14.8 | <.001 |
| HOS-SS | 32.9 ± 23.7 | 79.6 ± 25.0 | <.001 |
| iHOT-12 | 36.3 ± 19.5 | 74.8 ± 23.5 | <.001 |
| mHHS | 51.1 ± 19.4 | 84.4 ± 18.6 | <.001 |
| VAS | 4.9 ± 2.1 | 1.8 ± 1.9 | <.001 |
| VR-12 Physical | 32.3 ± 9.9 | 51.7 ± 7.8 | <.001 |
| VR-12 Mental | 48.8 ± 11.7 | 51.9 ± 10.3 | .880 |
aData are presented as mean ± SD. CR, capsular repair; HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SS, Hip Outcome Score–Sport Specific; iHOT-12, International Hip Outcome Tool; mHHS, modified Harris Hip Score; NR, no repair; VAS, visual analog scale; VR-12, Veterans RAND 12-Item Health Survey.
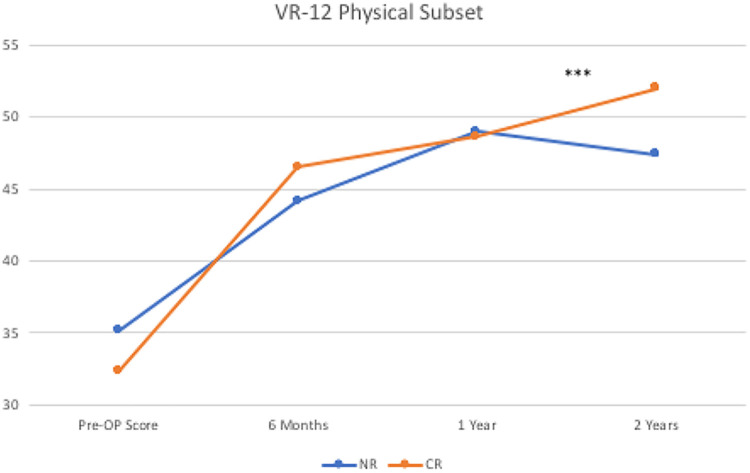
Table 3 displays the mean scores for all outcome measures. There was a significant difference between the CR and NR groups in terms of the change in VR-12 Physical subscale scores from preoperatively to 2 years postoperatively (P = .03). During this period, the CR group experienced a mean score change of 21.86 ± 8.73, compared with 13.96 ± 12.74 for the NR group (Figure 2). No other significant differences were found between the groups at 3 months, 6 months, 1 year, or 2 years postoperatively.
Table 3.
Comparison of Outcome Measures Between Groupsa
| NR Group | CR Group | P Value | |
|---|---|---|---|
| HOS-ADL | |||
| Preop | 68.1 ± 20.5 | 59.2 ± 18.8 | .12 |
| 6 mo | 84.0 ± 18.5 | 84.8 ± 17.6 | .76 |
| 2 y | 88.6 ± 20.0 | 91.7 ± 12.3 | .93 |
| ▵ preop–2 y | 21.67 ± 23.94 | 31.68 ± 14.58 | .12 |
| HOS-SS | |||
| Preop | 41.1 ± 25.8 | 32.7 ± 23.7 | .21 |
| 6 mo | 65.0 ± 32.1 | 64.5 ± 28.7 | .98 |
| 2 y | 84.1 ± 21.9 | 77.7 ± 23.0 | .4 |
| ▵ preop–2 y | 43.77 ± 29.87 | 49.68 ± 24.21 | .51 |
| iHOT-12 | |||
| Preop | 39.8 ± 21.0 | 39.4 ± 19.5 | .85 |
| 6 mo | 67.4 ± 25.2 | 68.0 ± 22.3 | .89 |
| 2 y | 75.9 ± 24.6 | 75.0 ± 21.2 | .71 |
| ▵ preop–2 y | 38.49 ± 27.22 | 36.46 ± 31.83 | .83 |
| mHHS | |||
| Preop | 54.9 ± 18.1 | 51.1 ± 19.4 | .48 |
| 6 mo | 79.9 ± 18.9 | 75.9 ± 17.8 | .25 |
| 2 y | 85.6 ± 21.0 | 86.5 ± 17.0 | .98 |
| ▵ preop–2 y | 31.31 ± 22.70 | 36.31 ± 14.86 | .42 |
| VAS pain | |||
| Preop | 4.6 ± 2.3 | 4.9 ± 2.0 | .67 |
| 6 mo | 1.8 ± 1.8 | 1.8 ± 1.8 | .92 |
| 2 y | 1.8 ± 2.2 | 1.5 ± 1.7 | .87 |
| ▵ preop–2 y | –2.40 ± 2.48 | –3.54 ± 2.42 | .15 |
| VR-12 Physical | |||
| Preop | 35.1 ± 10.6 | 32.3 ± 9.9 | .35 |
| 6 m | 44.2 ± 10.4 | 46.5 ± 13.2 | .3 |
| 2 y | 49.1 ± 10.4 | 51.2 ± 8.3 | .53 |
| ▵ preop–2 y | 13.96 ± 12.74 | 21.86 ± 8.73 | .03b |
| VR-12 Mental | |||
| Preop | 50.0 ± 10.7 | 47.6 ± 12.8 | .49 |
| 6 mo | 54.6 ± 8.0 | 50.1 ± 14.8 | .44 |
| 2 y | 53.4 ± 9.3 | 50.9 ± 9.6 | .27 |
| ▵ preop–2 y | 5.68 ± 11.26 | 2.53 ± 10.62 | .37 |
aData are presented as mean ± SD. CR, capsular repair; HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SS, Hip Outcome Score–Sport Specific; iHOT-12, International Hip Outcome Tool; mHHS, modified Harris Hip Score; NR, no repair; preop, preoperative; VAS, visual analog scale; VR-12, Veterans RAND 12-Item Health Survey.
bSignificant difference between groups.
Figure 2.
Preoperative (Pre-OP), 3-month, 6-month, 1-year, and 2-year Veterans RAND 12-Item Health Survey (VR-12) physical subscale outcomes in patients undergoing no capsular repair (NR) and complete capsular repair (CR). ***Significant difference between groups.
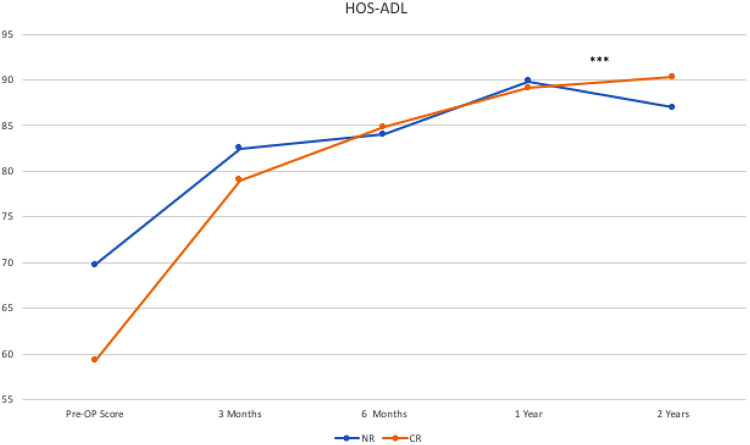
Both groups showed significant improvements on the HOS-ADL at the 2-year follow-up compared with preoperatively (Table 2). Patients in the NR group improved from 68.1 ± 20.5 to 88.6 ± 20.0 postoperatively (P < .001), and patients in the CR group improved from 59.2 ± 18.8 to 91.7 ± 12.3 postoperatively (P < .001). There was also significant improvement on the HOS-SS, with patients in the NR group improving from 41.1 ± 25.8 preoperatively to 84.1 ± 21.9 postoperatively (P < .001), and patients in the CR group improving from 32.7 ± 23.7 preoperatively to 77.7 ± 23.0 postoperatively (P < .001).
Likewise, there was significant improvement in both groups regarding the iHOT-12 scores at 2-year follow-up, with patients in the NR group improving from 39.8 ± 21.0 preoperatively to 75.9 ± 24.6 postoperatively (P < .001), and patients in the CR group improving from 39.4 ± 19.5 preoperatively to 75.0 ± 21.2 postoperatively (P < .001).
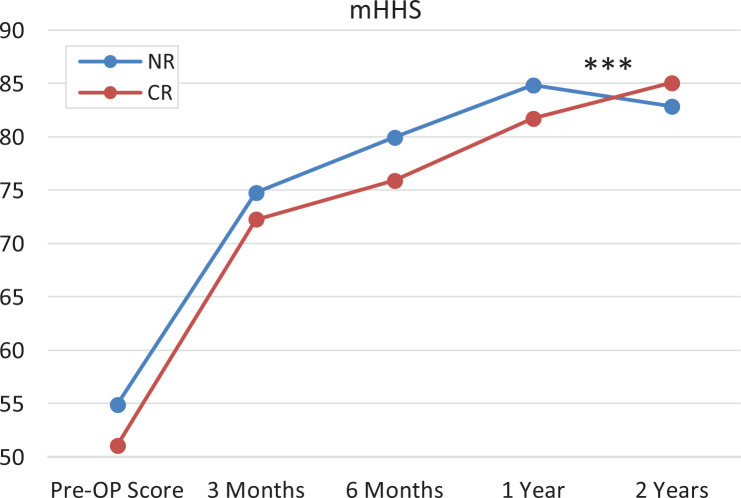
A comparison between groups of the VR-12 Physical subscale scores at different time points indicated an inflection point between 1 and 2 years postoperatively (–2.15 ± 5.52 vs 4.49 ± 7.30; P = .014) (Figure 2). Subset analysis showed similar inflection patterns between 1 and 2 years postoperatively on the HOS-ADL (–1.21 ± 5.09 vs 4.28 ± 7.91; P = .044) and the mHHS (1.08 ± 10.04 vs 10.12 ± 11.76; P = .042) (Figures 3 and 4).
Figure 3.
Preoperative (Pre-OP), 3-month, 6-month, 1-year, and 2-year Hip Outcome Score–Activities of Daily Living (HOS-ADL) subscale outcomes in patients undergoing no capsular repair (NR) and complete capsular repair (CR). ***Significant difference between groups.
Figure 4.
Preoperative (Pre-OP), 3-month, 6-month, 1-year, and 2-year modified Harris Hip Score (mHHS) subscale outcomes in patients undergoing no capsular repair (NR) and complete capsular repair (CR). ***Significant difference between groups.
Revisions and Complications
No patients in either group reported any immediate or short-term complications from the procedure, which are noted at the time of patient follow-up (Table 4). Four patients in the NR group returned at a later date for similar hip arthroscopy procedures on the contralateral hip. These were not included within the study (except for the single patient noted previously), as they were outside the collection period.
Table 4.
Labral Tear and Chondral Damagea
| NR Group | CR Group | P Value | |
|---|---|---|---|
| Tear size, h | 2.67 ± 1.0 | 2.14 ± 0.94 | .08 |
| Complications | 0 | 0 | |
| Yes | Yes | ||
| Associated cartilage damage | 9 | 4 | .09 |
| Chondroplasty–acetabulum | 6 | 2 | |
| Chondroplasty–femoral head | 0 | 1 | |
| Microfracture | 3 | 1 | |
| T-capsulotomy | 5 | 8 | .26 |
aData are presented as number of patients or mean ± SD. CR, capsular repair; NR, no repair.
Post Hoc Analysis
To address the lack of statistical significance and potential type 2 error (falsely concluding no difference when a meaningful one may in fact exist), we examined Patient Acceptable Symptom State (PASS) scores. The PASS is the score that reflects the point at which patients consider themselves in a satisfactory state of health. Chahal et al3 reported 87 as the PASS for the HOS-ADL in patients undergoing hip arthroscopy. Using this threshold, there were 5 patients in the NR group who did not reach the PASS at 1 year, compared with 6 in the CR group. At 2 years, both groups had 5 patients each not reaching the PASS. We also looked at a recent report on PASS scores on the iHOT-12, in which Robinson et al21 reported 59.5 as the PASS in patients undergoing hip arthroscopy. Using this threshold, there were 4 patients in both groups who did not reach the PASS at 1 year and 3 patients in both groups who did not reach the PASS at 2 years. Both of these findings support the conclusion that there was no significant difference between groups in this trial.
Discussion
Arthroscopists now routinely use capsulotomies to address cam or pincer impingement as well as chondral-labral pathology, with favorable short- and midterm outcomes.8,9,11,15–17,19,24 However, long-term follow-up suggests that there is a slow decline in outcome, often without a clear cause or mechanism. In a series of patients undergoing revision hip arthroscopy, Philippon et al17 found that 35% of patients with refractory hip pain had unaddressed instability. Philippon et al18 and Byrd and Jones2 have both reported significant ultimate conversion rates to total hip arthroscopy (12%-28%). The concern for ongoing instability, and certainly for postoperative subluxation or dislocation, serves as a constant reminder for the need to improve our technical ability to address intra-articular pathology without causing further destabilization to the hip complex.1,10,20
Telleria et al23 assessed the standard anterolateral and midanterior portals established during hip arthroscopy in a cadaveric model and found that these portals violate the iliofemoral ligament just inside the lateral and medial borders, respectively. The interportal capsulotomy, therefore, was found to traverse the majority of the width of the iliofemoral ligament. In a biomechanical study, Hewitt et al7 showed that the iliofemoral ligament is stiffer and withstands greater force than either the ischiofemoral ligament or the pubofemoral ligament. Additionally, if visualization of a distal femoral neck cam is needed, a T-shaped capsulotomy is often performed—further disrupting the integrity of this ligament. In a study of 15 fresh-frozen cadavers, Myers et al14 showed that, if injured, both the acetabular labrum and iliofemoral ligament should be surgically repaired to restore native hip rotation and translation.12
In a retrospective review of patients undergoing hip arthroscopy for FAI, Frank et al5 found improved HOS-SS at the 6-month, 1-year, and 2-year time points in patients who underwent complete repair of a T-capsulotomy as compared with partial repair of the distal limb. The patients in the partial CR group were also found to have a higher revision rate of 13% compared with none in the complete CR group.
Domb and colleagues4 reviewed prospectively collected outcomes data on 403 patients undoing hip arthroscopy with 2-year follow-up. In their series, postoperative unadjusted univariate analysis showed greater improvement in the CR group over unrepaired capsulotomy with regard to HOS-ADL and the Non-Arthritic Hip Score. However, significance was lost once confounding variables were controlled. They concluded that capsular repair appeared to be safe and did not negatively affect clinical outcomes; however, capsular repair did not show superiority over unrepaired capsulotomy with regard to PROs. It should be noted that in their study, surgeon discretion was used when choosing whether the patient would undergo capsular repair. As a result, the unrepaired group tended to be older and larger male patients who, during arthroscopy, were found to have greater injury to the acetabular cartilage.
Our results indicate that capsular repair does not negatively affect PROs after primary arthroscopic hip preservation surgery, although clear evidence of benefit was not demonstrated. In both the CR and the NR group, all postoperative PROs except for the VR-12 Mental subscale were significantly improved as compared with preoperative baselines. This study also found statistically significant between-group differences in the VR-12 Physical subset score between 1 and 2 years postoperatively. However, it remains to be seen if this shift between 1-year and 2-year outcomes represents a true inflection point at the 2-year time period that may signal faster degeneration in the NR groups as compared with the CR group. Further follow-up periods may be necessary to delineate whether this trend continues.
While BMI, reflecting body habitus, and preoperative alpha angle and center-edge angle, reflecting overall preoperative deformity, were similar between groups, post hoc analysis revealed an unequal distribution of men and women despite preoperative randomization. This likely accounted for the statistically significant differences in both height and weight between groups. These findings introduce unexpected bias into our results and may confound interpretation. This is especially significant given that there were more women within the capsular closure group, and higher rates of closure in this group may balance out outcomes that otherwise might have been different.
As Frank et al5 discuss in their study, use of the mHHS and HOS as outcome measures for hip arthroscopy also has limitations. The mHHS is limited by its ceiling effects, as it was initially designed as a disease-specific score for hip osteoarthritis. The HOS-SS subscale asks patients to rate their difficulty in participating in different activities, such as running 1 mile, jumping, swinging golf clubs, landing, starting/stopping quickly, making cutting and lateral movements, and participating in low-impact activities; their ability to perform an activity without modification; and their ability to participate in a chosen sport for a chosen duration. The HOS is limited because while it is a patient-reported, hip-specific outcome instrument, it is not patient derived. The VR-12 is a generic instrument developed to measure health-related quality of life.
In contrast to mHHS and HOS, the iHOT-12 instrument was specifically designed and validated for young, active patients with hip disorders, and its inclusion within the study outcomes represents a significant strength of our study. The iHOT-12 instrument asks patients to rate their awareness of disability, hip pain, and hip pain after activity; ability to get up off the ground, walk long distances, and carry/push/pull heavy objects; concern over pivoting/cutting during sport; trouble with grinding/catching or clicking; and trouble with sexual activity. The categorical improvement of iHOT-12 scores in both the CR and NR groups represents the most specific improvement in PRO measures to date for young patients with hip disorders.
Our prospective findings were similar to those of Domb et al,4 whose retrospective review of nonrandomized patients showed no significant differences between patients who underwent capsular closure versus nonrepair, with the exception of seeing significant differences in the 2-year VR-12 Physical subscale. Certainly, it does appear that capsular closure does not negatively affect outcomes in patients at the 2-year time point. It may be that lack of capsular closure may contribute to faster deterioration of the hip joint, with increasing negative changes in outcome scores at the 2-year time point, although this may also be because of chance. Further evaluation of these patients will be necessary to assess medium- to long-term outcomes with regard to capsular closure and to ascertain whether initial trends seen between 1 and 2 years postoperatively will continue as time progresses.
Limitations
The limitations of this study include the unblinded nature of the surgeons with regard to capsular treatment. While unavoidable in our current study, we tried to minimize the effect this might have by looking solely at PROs that we felt would be least affected by surgeon knowledge. Surprisingly, no patient requested copies of their operative report during the 2-year follow-up. Thus, we feel that patient blinding was satisfactorily maintained throughout the trial period.
In contrast to previous studies, one of the strengths of our series was the equally distributed and overall younger age of patients. However, as mentioned previously, the statistically significant sex differences between groups, despite randomization, serve as a confounding factor. This is made more significant because there were more women within the capsular closure group—reflecting the current practice of some hip arthroscopists who preferentially perform capsular closure within female patients over concern for increased laxity and resultant capsular compliance. Experimentally, capsular compliance, ligamentous laxity, and atraumatic instability remain difficult to control. As Domb et al4 noted in their study, diagnosis of pathology within the capsule itself remains difficult to quantify. As with many biological variables, its presence exists on a spectrum—from contracted to hyperlaxity—and there exist few clinical and radiological signs to quantify this preoperatively.
During the study period, PRP was used routinely and was employed in all cases in an effort to help enhance healing. While this may represent a theoretical confounding factor between cases where the capsule was closed and where it was not, we do not feel that this, ultimately, is the case. More recent data since the time of our collection period have not shown there to be any benefit to PRP administration at the time of hip arthroscopy.
Additionally, the purpose of this study was to ascertain the differences between interportal capsulotomy and no repair, exclusive of a larger T-capsulotomy. In cases with larger cam lesions requiring increased surgical exposure for cam resection, a T-cut was created and, therefore, repaired regardless of study group in order to normalize the comparison. Our clinical experience has been that this portion of the capsule routinely heals and so should not pose a significant confounding variable to the series.
Conclusion
There were no significant differences in PROs at 2 years postoperatively in patients who underwent complete capsular closure versus patients who did not have interportal capsular closure. There was significant improvement in the HOS-ADL, HOS-SS, iHOT-12, mHHS, VAS, and VR-12 Physical scores across all patients by the 2-year time point. Significant postoperative improvement in the VR-12 Mental subscale was not found among patients who underwent partial versus complete capsular closure. The HOS-ADL, mHHS, and VR-12 Physical scores worsened between the 1- and 2-year time points in the NR group, but this difference did not reach statistical significance. Further study is needed to address longer-term outcomes between groups.
Acknowledgment
Special thanks to Tara Moore for her assistance with biostatistical analysis.
Footnotes
Final revision submitted April 29, 2020; accepted May 11, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: E.P.S. has received educational support from Smith & Nephew, Arthrex, and Gotham Surgical; grant support from DJO; and hospitality payments from Acumed. M.E.B. has received educational support from Smith & Nephew and Liberty Surgical, grant support from Arthrex, and hospitality payments from Stryker and DePuy/Medical Device Business Services. M.F. has received educational support from Arthrex and DePuy and grant support from Linvatec. D.N.P. has received hospitality payments from DePuy, Zimmer Biomet, Tornier, Ascension Orthopedics, RTI Surgical, Integra Lifesciences, Vericel, Smith & Nephew, and Skeletal Dynamics. M.B.B. has received educational support from Arthrex, consulting fees from Stryker, speaking fees from Arthrex and Vericel, honoraria from Vericel, and hospitality payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Asentral Inc (No. 2013-312A).
References
- 1. Benali Y, Katthagen BD. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy. 2009;25(4):405–407. [DOI] [PubMed] [Google Scholar]
- 2. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Relat Res. 2010;468(3):741–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chahal J, Van Thiel GS, Mather RC III, et al. The Patient Acceptable Symptomatic State for the modified Harris Hip Score and Hip Outcome Score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med. 2015;43(8):1844–1849. [DOI] [PubMed] [Google Scholar]
- 4. Domb BG, Stake CE, Finley ZJ, Chen T, Giordano BD. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthroscopy. 2015;31(4):643–650. [DOI] [PubMed] [Google Scholar]
- 5. Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634–2642. [DOI] [PubMed] [Google Scholar]
- 6. Gupta A, Suarez-Ahedo C, Redmond JM, et al. Best practices during hip arthroscopy: aggregate recommendations of high-volume surgeons. Arthroscopy. 2015;31(9):1722–1727. [DOI] [PubMed] [Google Scholar]
- 7. Hewitt JD, Glisson RR, Guilak F, Vail TP. The mechanical properties of the human hip capsule ligaments. J Arthroplasty. 2002;17(1):82–89. [DOI] [PubMed] [Google Scholar]
- 8. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21(12):1496–1504. [DOI] [PubMed] [Google Scholar]
- 9. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25(4):369–376. [DOI] [PubMed] [Google Scholar]
- 10. Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25(4):400–404. [DOI] [PubMed] [Google Scholar]
- 11. Mauro C, Voos JE, Kelly BT. Femoroacetabular impingement surgical techniques. Oper Tech Orthop. 2010;10:223–230. [Google Scholar]
- 12. McCormick F, Nwachukwu BU, Alpaugh K, Martin SD. Predictors of hip arthroscopy outcomes for labral tears at minimum 2-year follow-up: the influence of age and arthritis. Arthroscopy. 2012;28(10):1359–1364. [DOI] [PubMed] [Google Scholar]
- 13. Mei-Dan O, Young DA. A novel technique for capsular repair and labrum refixation in hip arthroscopy using the SpeedStitch. Arthrosc Tech. 2012;1(1):e107–e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39(suppl):85S–91S. [DOI] [PubMed] [Google Scholar]
- 15. Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91(1):16–23. [DOI] [PubMed] [Google Scholar]
- 16. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25(2):299–308, ix. [DOI] [PubMed] [Google Scholar]
- 17. Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35(11):1918–1921. [DOI] [PubMed] [Google Scholar]
- 18. Philippon MJ, Schroder ESBG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012;28(1):59–65. [DOI] [PubMed] [Google Scholar]
- 19. Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007;35(9):1571–1580. [DOI] [PubMed] [Google Scholar]
- 20. Ranawat AS, McClincy M, Sekiya JK. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. A case report. J Bone Joint Surg Am. 2009;91(1):192–197. [DOI] [PubMed] [Google Scholar]
- 21. Robinson PG, Maempel JF, Rankin CS, Gaston P, Hamilton DF. Evaluation of the Patient Acceptable Symptom State following hip arthroscopy using the 12 item International Hip Outcome Tool. BMC Musculoskelet Disord. 2020;21(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sansone M, Ahld, én M, J, ónasson P, Swärd L, Eriksson T, Karlsson J. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):420–423. [DOI] [PubMed] [Google Scholar]
- 23. Telleria JJ, Lindsey DP, Giori NJ, Safran MR. An anatomic arthroscopic description of the hip capsular ligaments for the hip arthroscopist. Arthroscopy. 2011;27(5):628–636. [DOI] [PubMed] [Google Scholar]
- 24. Voos JE, Mauro CS, Kelly BT. Femoroacetabular impingement in the athlete: compensatory injury patterns. Oper Tech Orthop. 2010;20:231–236. [Google Scholar]