Abstract
Background:
Patients are commonly evaluated at the emergency department (ED) with acute anterior cruciate ligament (ACL) tears, but providers without orthopaedics training may struggle to correctly diagnose these injuries.
Hypothesis:
It was hypothesized that few patients would be diagnosed with an ACL tear while in the ED and that these patients would be of lower socioeconomic status and more likely to have public insurance.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
The 2017 State Ambulatory Surgery and Services Database (SASD) and State Emergency Department Database (SEDD) from the state of Florida were utilized in this study. Cases with Current Procedural Terminology code 29888 (arthroscopically aided ACL reconstruction [ACLR]) were selected from the SASD, and data from the SEDD were matched to patients who had an ED visit for a knee injury within 120 days before ACLR. Chi-square analysis was used to test for differences in patient and surgical variables between the ED visit and nonvisit patient groups. A generalized linear model was created to model the effect of ED visit on total cost for an ACL injury.
Results:
While controlling for differences in patient characteristics and concomitant procedure usage, a visit to the ED added $4587 in total cost (P < .001). The ED visit cohort contained a greater proportion of patients with Medicaid (20.2% vs 9.1%), patients who were Black (18.4% vs 10.3%), and patients in the lowest income quartile (34.4% vs 25.0%) (P < .001 for all). In the ED visit cohort, 14.4% of patients received an allograft versus 10.1% in the non-ED visit cohort (P = .001) despite having a similar mean age. An ACL sprain was diagnosed in only 29 of the 645 (4.5%) patients who visited the ED.
Conclusion:
Utilizing the ED for care after an ACL injury was expensive, averaging a $4587 increase in total cost associated with ACLR. However, patients rarely left with a definitive diagnosis, with only 4.5% of patients who underwent ACLR being correctly diagnosed with an ACL tear in the ED. This additional cost was levied disproportionately on patients of low socioeconomic status and patients with Medicaid.
Keywords: ACL, economic and decision analysis, knee, ligaments, ED utilization
Injuries to the anterior cruciate ligament (ACL) are common, and the incidence of ACL tears and ACL reconstructions (ACLRs) is increasing.10,12 Orthopaedic surgeons using clinical examinations alone have been shown to have diagnostic accuracy at similar levels to that of magnetic resonance imaging for ACL tears.11,21 However, it has been shown that nonorthopaedic providers using traditional diagnostic maneuvers may not provide the same accuracy.1,8 Patients are commonly evaluated at the emergency department (ED) with acute ACL tears, but several studies7,8,20 have shown that non–orthopaedic-trained providers may struggle to correctly diagnose these injuries. Furthermore, previous studies4–6,25 have identified an association between delayed time to ACL surgery and higher rates of meniscal tears at the time of surgery, further clarifying the importance of a timely diagnosis.
Previous studies3,19 have demonstrated greater ED utilization among patients with Medicaid. Medicaid patients also face difficulty in obtaining follow-up appointments with orthopaedic providers, as 1 study17 found that only 14% of practices offered appointments for Medicaid patients after a hypothetical ED visit. Taken together, these studies suggest that lower socioeconomic patients may be at higher risk for utilizing emergency care for ACL diagnosis and referral. Moreover, previous cost-driver analyses of orthopaedic procedures have demonstrated increased costs among Medicaid and minority populations.2,15 With this in mind, we sought to compare the patients who utilized the ED for care after an ACL injury with those who did not as well as to quantify the cost of these episodes of care. We hypothesized that the cohort of patients utilizing the ED would be of lower socioeconomic status and more likely to have public insurance. We also hypothesized that few of these patients would be diagnosed with an ACL tear while in the ED, despite the added cost associated with this visit.
Methods
Data Source
The 2017 State Ambulatory Surgery and Services Database (SASD) and State Emergency Department Database (SEDD) from Florida were utilized in this study. These databases contain information derived from discharge records on outpatient surgeries (SASD) and ED visits that did not result in admission to the hospital (SEDD). Florida is 1 of few states that includes unique, anonymized patient identifier variables in these databases, allowing for the tracking of patients across different episodes of care. Variables contained in the SASD and SEDD include patient characteristics, Current Procedural Terminology (CPT) codes, International Classification of Diseases, 10th Revision (ICD-10) codes, and operative variables. Notably, for the SEDD, a variable denoting the ICD-10 code of the reason for the visit is included. Institutional review board approval was not necessary, as no direct patient identifiers were used.
Case Selection
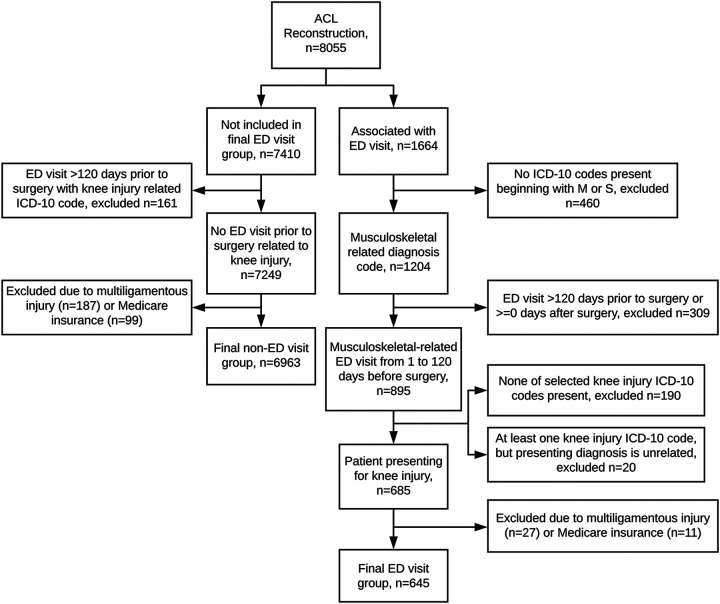
All cases in the SASD with CPT code 29888 (arthroscopically aided ACLR) from January 1 to December 31, 2017, were selected. Two patient groups were then created: 1 group that utilized the ED for care related to the ACL injury within the 120 days prior to surgery and 1 group that did not. The 120-day cutoff was chosen to give a high degree of confidence that the ACL injury occurred before the ED visit. All ICD-10 codes associated with the ED visit were documented. Patients with multiligamentous injuries (determined by CPT codes 27405, 27427, and 29889 used at the time of ACLR) or with Medicare were also excluded, as many of these patients would be significantly older than any other group. For the final ED visit group, total charges from the ED visit were added to the charges for the ACLR. A full description of the inclusion criteria is presented in Figure 1. After exclusion, there were 645 patients in the ED visit cohort and 6963 patients in the nonvisit cohort.
Figure 1.
Flowchart of study inclusion criteria. ACL, anterior cruciate ligament; ED, emergency department; ICD-10, International Classification of Diseases, 10th Revision.
Total charges were used here as a proxy variable for cost, a methodology that has been utilized in several previous orthopaedic publications.2,13–15,22 The following variables were utilized in the cost model: patient age, sex, insurance, race, income quartile of the patient’s ZIP code, surgeon volume, surgical facility volume, concomitant meniscal repair, and allograft usage. For surgeon and facility volume, cutoffs >25 cases and >125 cases per year were used, respectively, to determine high volume. The surgeon volume cutoff represents at least 1 case every 2 weeks, and the facility volume cutoff was derived from previous publications.9,16 Concomitant meniscal repair was determined by CPT codes 29882 and 29883. Allograft usage was determined by Healthcare Common Procedure Coding System (HCPCS) codes C1762, C1763, and C1776. Income quartiles were defined as follows: <$44,000; $44,000 to $55,999; $56,000 to $73,999; ≥$74,000 (all in 2017 U.S. dollars).
Statistical Analysis
Chi-square analysis was first used to test for differences in patient and surgical variables between the ED visit and nonvisit groups. A generalized linear model with total charges as the outcome variable was then used to model how much cost an ED visit added while controlling for differences in patient characteristics and operative factors between the groups. SPSS Version 26.0 (IBM) was used for analysis.
Results
Across all patients, the mean age was 29.3 years (95% CI, 29.0-29.6 years), and 61.1% (95% CI, 60.0%-62.1%) of patients were men. For patients in the ED visit cohort, the mean time from ED visit to surgery was 51.4 days (95% CI, 49.2-53.5 days).
We first assessed patient characteristics for the ED visit cohort compared with the nonvisit cohort (Table 1). Patients with prior ED visits were more likely to be on Medicaid (20.2% vs 9.1%, P < .001), reside in a ZIP code of the lowest income quartile (34.4% vs 25.0%, P < .001), and identify as Black (18.4% vs 10.3%, P < .001). In addition, the patients with a prior ED visit were more likely to undergo ACLR at a low-volume facility (74.6% vs 61.3%, P < .001) and have the surgery performed by a low-volume surgeon (49.0% vs 40.8%, P < .001). While patients in the ED visit cohort were more likely to receive an allograft (14.4% vs 10.1%, P = .001), they were not significantly more likely to undergo concomitant meniscal repair (84.0% to 81.9%, P = .221). Patients in the ED visit group were also slightly older, with a mean age of 30.3 years compared with 29.2 years in the nonvisit group (P = .034). There was no significant difference between the 2 groups in regards to patient sex (P = .556).
Table 1.
Characteristics of Patients Evaluated at the ED for a Knee Injury Within 120 Days Before ACLRa
| Parameter | ED Visit Before ACLR | ||
|---|---|---|---|
| No | Yes | P Value | |
| Sex | .556 | ||
| Male | 61.2 | 60.0 | |
| Female | 38.8 | 40.0 | |
| Insurance | <.001 | ||
| Medicaid | 9.1 | 20.2 | |
| Private | 76.6 | 62.0 | |
| Other | 14.3 | 17.8 | |
| Race | <.001 | ||
| White | 60.7 | 55.3 | |
| Black | 10.3 | 18.4 | |
| Hispanic | 21.2 | 20.9 | |
| Asian | 1.4 | 0.9 | |
| Other | 6.4 | 4.3 | |
| Income quartileb | <.001 | ||
| 1 | 25.0 | 34.4 | |
| 2 | 30.0 | 33.4 | |
| 3 | 28.7 | 24.1 | |
| 4 | 16.2 | 8.1 | |
| Surgeon volume | <.001 | ||
| Low | 40.8 | 49.0 | |
| High | 59.2 | 51.0 | |
| Facility volume | <.001 | ||
| Low | 61.3 | 74.6 | |
| High | 38.7 | 25.4 | |
| Meniscal repair | .221 | ||
| No | 81.9 | 84.0 | |
| Yes | 18.1 | 16.0 | |
| Allograft | .001 | ||
| No | 89.9 | 85.6 | |
| Yes | 10.1 | 14.4 | |
| Age, y, mean (95% CI) | 29.2 (28.9-29.5) | 30.3 (29.0-31.3) | .034 |
aData are presented as percentage unless otherwise noted. Bolded P values indicate statistically significant difference (P < .05). ACLR, anterior cruciate ligament reconstruction; ED, emergency department.
bAs determined by ZIP code.
A generalized linear model of the cost of ACLR (Table 2) was created to assess the added cost of an ED visit while controlling for differences in patient characteristics and surgical practices between the 2 cohorts. While controlling for other factors, an ED visit for a knee injury before ACLR added $4587 in cost (P < .001). Other significant predictors included patient insurance, race, surgeon and facility volume, concomitant meniscal repair, and allograft usage. Patients with Medicaid insurance as compared with private insurance had greater costs ($5577, P < .001). Costs differed by patient race, as Black patients ($2553, P = .001), Hispanic patients ($4054, P < .001), and patients of other race ($3462, P < .001) had higher costs compared with white patients. Having the ACLR performed by a high-volume surgeon lowered costs (–$1357, P = .010), as did surgery at a high-volume facility (–$5747, P < .001). Surgical cost drivers included concomitant meniscal repair ($6533, P < .001) and usage of an allograft ($16,386, P < .001).
Table 2.
Generalized Linear Model of Total Cost of Care Associated With ACLRa
| Parameter | Cost (2017 USD) | 95% CI | P Value |
|---|---|---|---|
| Intercept | $37,862 | $36,391 to $39,334 | <.001 |
| ED visit | $4587 | $2949 to $6226 | <.001 |
| Other payer | $322 | –$992 to $1636 | .631 |
| Medicaid | $5577 | $3966 to $7189 | <.001 |
| Private insurance | Referent | ||
| Other race | $3462 | $1562 to $5362 | <.001 |
| Asian | –$1106 | –$4994 to $2782 | .577 |
| Hispanic | $4054 | $2891 to $5217 | <.001 |
| Black | $2553 | $1035 to $4072 | .001 |
| White | Referent | ||
| High surgeon volume | –$1357 | –$2392 to –$323 | .010 |
| High facility volume | –$5747 | –$6803 to –$4690 | <.001 |
| Meniscal repair | $6533 | $5338 to $7728 | <.001 |
| Allograft | $16,386 | $14,892 to $17,880 | <.001 |
| Age | $29 | –$9 to $67 | .130 |
aBolded P values indicate statistical significance (P < .05). ED, emergency department; USD, U.S. dollars.
Table 3 shows the diagnoses for the ED visit cohort and how often they were each present. Some patients had several of these diagnoses listed upon discharge from the ED. The most common diagnosis was Pain in Knee (n = 437), followed by Unspecified Injury, Lower Leg (n = 185), Sprain of Unspecified Site of Knee (n = 180), and Knee Effusion (n = 87). An ACL sprain was diagnosed in 29 of the 645 patients in the ED cohort, giving a diagnosis rate of 4.5% in patients who later underwent ACLR.
Table 3.
Diagnoses of Patients Visiting the ED for Knee-Related Injuries Within 120 Days Before ACLRa
| ICD-10 Code | Diagnosis | No. of Patients |
|---|---|---|
| M25.561/2 | Pain in knee | 437 |
| S89.91/2 | Unspecified injury, lower leg | 185 |
| S83.91/2X | Sprain of unspecified site of knee | 180 |
| M25.461/2 | Knee effusion | 87 |
| S80.01/2 | Contusion of knee | 47 |
| M23.91/2 | Unspecified internal derangement, knee | 44 |
| S83.511/2 | ACL sprain | 29 |
| S86.911/2 | Unspecified muscle/tendon sprain, lower leg | 20 |
| S83.411/2 | MCL sprain | 16 |
| M79.604/5 | Pain in leg | 13 |
| S83.8X1/2a | Sprain other specified parts, knee | 10 |
| M25.569 | Pain in unspecified knee | 6 |
| S83.104/5 | Unspecified dislocation of knee | 3 |
aACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; ICD-10, International Classification of Diseases, 10th Revision; MCL, medial collateral ligament.
Discussion
As was hypothesized, this study found that ED visits for ACL tears are expensive, adding $4587 in total costs, yet they have little diagnostic utility. Here, we found that among patients who were evaluated at the ED for an ACL injury, only 4.5% were diagnosed with an ACL sprain upon discharge. Of patients who underwent ACLR, most left the ED with a nonspecific knee injury diagnosis. Guillodo et al8 found that 26% of patients with ACL tears were diagnosed upon evaluation at the ED, whereas Parwaiz et al20 found a rate of 10.3%. In contrast, this study used a statewide database that captures data from many emergency centers, which may explain why the diagnosis rate found here is much lower than previously reported. Orthopaedic surgeons using clinical examinations have been shown to have a high degree of accuracy in diagnosing ACL tears.11,21 However, nonorthopaedic providers may not have as sensitive of clinical examinations as their orthopaedic counterparts.1,8,20 Therefore, the large number of nonspecific knee injury diagnoses seen in the ED visit cohort may be explained by lack of on-site orthopaedic providers in many of the centers studied here. Another contributing factor is the difficulty of performing a knee examination in the setting of an acute injury. Patients may have pain, swelling, or guarding of the knee, all of which decrease the sensitivity of even the most experienced provider’s examination. As such, referral to an orthopaedic specialist remains critical for patients who visit the ED with persistently painful or unstable acute knee injuries.
Timely referral to a specialist is also paramount when considering the added risk of knee injury in the ACL-deficient knee. Time to surgery after an ACL injury has been found to result in a higher incidence of meniscal tears in patients who had been ACL deficient for 12 months.4,25 Even shorter delays in surgery may be significant, as Everhart et al6 found that surgery more than 5 months after initial injury increases the odds of high-grade chondral damage by 3.11 times, and an 8-week delay increases the odds of a meniscal injury requiring operative treatment. For the ED cohort in this study, the mean time to surgery was 51.4 days, and 36% of patients had surgery after the 8-week time frame established by Everhart et al. For these patients, leaving the ED without a specific diagnosis or a timely follow-up with an orthopaedic specialist may have contributed to delayed surgery. These patients may be at risk of secondary meniscal injury during the ACL-deficient period. Therefore, orthopaedic surgeons receiving referrals from ED visits related to knee injuries ought to be aware of the possibility of an undiagnosed ACL injury and cognizant of how much time has passed between the ED visit and the referral. For patients who are being evaluated more than 8 weeks after the initial injury, providers should consider the possibility of meniscal injuries if an ACL tear is suspected.
The cost burden associated with ED visits in this study was levied disproportionately on patients who are Black, have Medicaid insurance, or live in a ZIP code of a lower income quartile. Patients who are of low socioeconomic status would potentially benefit the most from cost-effective care, yet our results show that these patients face higher costs associated with greater ED utilization. One explanation for these findings is that patients of lower socioeconomic status face barriers to accessing other venues of care, such as primary care physicians. In particular, Medicaid patients have been previously shown to have greater ED utilization than privately insured patients.3,19 While we do not know the costs of initial evaluation for the nonvisit cohort in this study, the cost of a visit to an urgent care center or outpatient office has been shown to be lower than that of an ED visit.18,24 Moreover, patients who were able to directly access orthopaedic specialist care would have a higher rate of injury diagnosis without the added burden of an ED visit. However, it is also well known that Medicaid patients have poor odds of accessing direct orthopaedic care.17,23,26 Our results demonstrate that this comes at a significant cost to the healthcare system, as accessing care through the ED added $4587 to the total cost of care.
In addition to higher costs, patients in the ED visit cohort were less likely to have surgery performed by a high-volume surgeon or at a high-volume facility and were more likely to receive an allograft, despite a similar mean age of 29.3 years. Low-volume surgeons performing ACLR have been found to have higher 90-day hospital readmission rates, and their patients have higher odds of revision ACLR.16 Similarly, low-volume surgeons and facilities have higher allograft utilization, which itself was the largest independent cost driver in this study.9 Thus, the association between the ED visit cohort and low-volume surgeons may thus explain the greater allograft utilization, and there may also be injury characteristics that we were unable to account for. However, the additional cost of an allograft is undeniable. As with the cost of visiting the ED, the cost of an allograft is disproportionately levied on patients who are of a lower socioeconomic status or have Medicaid.
Although we found that ED visits for ACL injuries often led to nonspecific diagnoses, the results of this study should not discourage patients from seeking the ED in the setting of an acute knee injury. Instead, our results demonstrate the need for greater access to same-day musculoskeletal care, especially in underserved areas. In particular, patients who have Medicaid have been shown to have poor access to orthopaedic care.17,23,26 Areas that have a higher density of Medicaid enrollees could thus benefit from expanded provider coverage. This could include primary care sports medicine physicians or advanced practice providers at urgent care orthopaedic clinics. This can also include athletic trainer coverage at schools. Increased access to primary care providers is important as well. These venues would provide a more time- and cost-effective point of initial care for patients with acute knee injuries. In addition, for patients who do utilize the ED, ensuring timely orthopaedic follow-up may not only improve continuity of care and quick diagnosis but also ensure prompt specialist consultation and surgery if necessary.
Limitations
Although this study used a large sample size that contained data from many different providers, it is not without limitations. The biggest limitation is that we could not be totally certain that the patients in the ED visit cohort were evaluated for the ACL injury that led to ACLR, as most of them were not actually diagnosed with an ACL injury. Given the anonymized nature of the data source, we could not examine the ED notes for physical examination findings consistent with ACL injury. It is possible that patients visited the ED for a different knee injury and sustained the ACL injury later, which would lead to a selection bias. However, we believe that our approach of using a 120-day period before patients with known ACL injuries underwent ACLR could give a high degree of confidence that the ED visit was for the initial ACL injury. We also may have selection bias in that we did not have a group of patients who visited the ED with an ACL tear but did not later undergo surgery. Thus, we do not know how many patients who did not have ACLR were without an accurate diagnosis. As we were using a claims-based database, there may also have been errors in coding or differences in billing practices between providers. Our use of total charges as a proxy for cost also has its limitations, as reimbursement to the provider may differ from charges. Charges may also not reflect the actual amount that the patient pays. Additionally, total charges did not capture postoperative costs related to out-of-work status or physical therapy. Although there are limitations to using total charges, previous studies2,13–15,22 have shown them to be informative in identifying patient characteristics and surgical drivers of cost. Finally, we were not able to quantify access to specialist orthopaedic care based on the hospital that patients initially visited, and we instead used proxies such as patient race, income level, and insurance to determine access to care. Future studies may seek to evaluate ED- and hospital-specific factors that affect access.
Conclusion
Utilizing the ED for care after an ACL injury is expensive, with a mean $4587 increase in total cost associated with ACLR. However, patients rarely leave with a definitive diagnosis, with only 4.5% of patients who underwent ACLR in this study being correctly diagnosed with an ACL tear in the ED. This additional cost was levied disproportionately on patients of low socioeconomic status and patients with Medicaid.
Footnotes
Final revision submitted November 15, 2020; accepted January 3, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.L.B. has received educational payments from Stryker and hospitality payments from Zimmer Biomet. B.D.O. has received consulting fees from DePuy, Linvatec, the Muscoloskeletal Transplant Foundation, and Medical Device Business Services; honoraria from Vericel; royalties from Linvatec; and is a paid associate editor for The American Journal of Sports Medicine. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Arastu MH, Grange S, Twyman R. Prevalence and consequences of delayed diagnosis of anterior cruciate ligament ruptures. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1201–1205. [DOI] [PubMed] [Google Scholar]
- 2. Bokshan SL, Mehta S, DeFroda SF, Owens BD. What are the primary cost drivers of anterior cruciate ligament reconstruction in the United States? A cost-minimization analysis of 14,713 patients. Arthroscopy. 2019;35(5):1576–1581. [DOI] [PubMed] [Google Scholar]
- 3. Capp R, Rooks SP, Wiler JL, Zane RD, Ginde AA. National study of health insurance type and reasons for emergency department use. J Gen Intern Med. 2014;29(4):621–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen KH, Chiang ER, Wang HY, Ma HL. Correlation of meniscal tear with timing of anterior cruciate ligament reconstruction in patients without initially concurrent meniscal tear. J Knee Surg. 2019;32(11):1128–1132. [DOI] [PubMed] [Google Scholar]
- 5. Dingel A, Aoyama J, Ganley T, Shea K. Pediatric ACL tears: natural history. J Pediatr Orthop. 2019;39(6 suppl 1):S47–S49. [DOI] [PubMed] [Google Scholar]
- 6. Everhart JS, Kirven JC, Abouljoud MM, DiBartola AC, Kaeding CC, Flanigan DC. Effect of delayed primary anterior cruciate ligament reconstruction on medial compartment cartilage and meniscal health. Am J Sports Med. 2019;47(8):1816–1824. [DOI] [PubMed] [Google Scholar]
- 7. Gage BE, McIlvain NM, Collins CL, Fields SK, Comstock RD. Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad Emerg Med. 2012;19(4):378–385. [DOI] [PubMed] [Google Scholar]
- 8. Guillodo Y, Rannou N, Dubrana F, Lefèvre C, Saraux A. Diagnosis of anterior cruciate ligament rupture in an emergency department. J Trauma. 2008;65(5):1078–1082. [DOI] [PubMed] [Google Scholar]
- 9. Inacio MCS, Paxton EW, Maletis GB, et al. Patient and surgeon characteristics associated with primary anterior cruciate ligament reconstruction graft selection. 2012;40(2):339–345. [DOI] [PubMed] [Google Scholar]
- 10. Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med. 2017;36(1):1–8. [DOI] [PubMed] [Google Scholar]
- 11. Kocabey Y, Tetik O, Isbell WM, Atay OA, Johnson DL. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy. 2004;20(7):696–700. [DOI] [PubMed] [Google Scholar]
- 12. Leathers MP, Merz A, Wong J, Scott T, Wang JC, Hame SL. Trends and demographics in anterior cruciate ligament reconstruction in the United States. J Knee Surg. 2015;28(5):390–394. [DOI] [PubMed] [Google Scholar]
- 13. Li L, Bokshan SL, Mehta SR, Owens BD. Disparities in cost and access by caseload for arthroscopic rotator cuff repair: an analysis of 18,616 cases. Orthop J Sports Med. 2019;7(6):2325967119850503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li L, Bokshan SL, Ready LV, Owens BD. The primary cost drivers of arthroscopic rotator cuff repair surgery: a cost-minimization analysis of 40,618 cases. J Shoulder Elbow Surg. 2019;28(10):1977–1982. [DOI] [PubMed] [Google Scholar]
- 15. Li LT, Chuck C, Bokshan SL, et al. High-volume and privately owned ambulatory surgical centers reduce costs in Achilles tendon repair. Orthop J Sports Med. 2020;8(4):2325967120912398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction. Trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10):2321–2328. [DOI] [PubMed] [Google Scholar]
- 17. Medford-Davis LN, Lin F, Greenstein A, Rhodes KV. “I broke my ankle”: access to orthopedic follow-up care by insurance status. Acad Emerg Med. 2017;24(1):98–105. [DOI] [PubMed] [Google Scholar]
- 18. Montalbano A, Rodean J, Kangas J, Lee B, Hall M. Urgent care and emergency department visits in the pediatric medicaid population. Pediatrics. 2016;137(4):e20153100. [DOI] [PubMed] [Google Scholar]
- 19. Moulin A, Evans EJ, Xing G, Melnikow J. Substance use, homelessness, mental illness and Medicaid coverage: a set-up for high emergency department utilization. West J Emerg Med. 2018;19(6):902–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Parwaiz H, Teo AQA, Servant C. Anterior cruciate ligament injury: a persistently difficult diagnosis. Knee. 2016;23(1):116–120. [DOI] [PubMed] [Google Scholar]
- 21. Rose NE, Gold SM. A comparison of accuracy between clinical examination and magnetic resonance imaging in the diagnosis of meniscal and anterior cruciate ligament tears. Arthroscopy. 1996;12(4):398–405. [DOI] [PubMed] [Google Scholar]
- 22. Rosenfeld SB, Schroeder K, Watkins-Castillo SI. The economic burden of musculoskeletal disease in children and adolescents in the United States. J Pediatr Orthop. 2018;38(4):e230–e236. [DOI] [PubMed] [Google Scholar]
- 23. Segal DN, Grabel ZJ, Shi WJ, Gottschalk MB, Boden SD. The impact of insurance coverage on access to orthopedic spine care. J Spine Surg (Hong Kong). 2018;4(2):260–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Singman EL, Smith K, Mehta R, et al. Cost and visit duration of same-day access at an academic ophthalmology department vs emergency department. JAMA Ophthalmol. 2019;137(7):729–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stone JA, Perrone GS, Nezwek TA, et al. Delayed ACL reconstruction in patients ≥40 years of age is associated with increased risk of medial meniscal injury at 1 year. Am J Sports Med. 2019;47(3):584–589. [DOI] [PubMed] [Google Scholar]
- 26. Timbie JW, Kranz AM, Mahmud A, Damberg CL. Specialty care access for Medicaid enrollees in expansion states. Am J Manag Care. 2019;25(3):e83–e87. [PMC free article] [PubMed] [Google Scholar]