Abstract
Introduction: Wide-awake local anesthesia and no tourniquet (WALANT) has come a long way. It has been reported to be successful in the surgery of distal radius and ulna fractures. We report a case of olecranon fracture plating under WALANT. Methods: Surgery was performed with the patient fully conscious where tumescent anesthesia was injected into the surgical site without application of tourniquet 30 minutes before the first incision. Posterior approach to the elbow was used, and the fracture was fixed with anatomical locking plates. Results: The surgery was successfully completed without pain. The numerical pain rating score was 0 throughout the surgery. Conclusions: The use of WALANT for surgical fixation can be expanded beyond the hand and wrist. This is a safe and simple option for patients at high risk of general anesthesia, producing similar surgical outcomes without intraoperative and postoperative complications.
Keywords: elbow fractures, plating, local anesthesia, WALANT, open reduction and internal fixation, lidocaine
Introduction
Fractures of the olecranon represent common elbow injury which constitutes 10% of all upper extremity lesions.1 They are usually treated surgically rather than conservatively depending on the type of fracture. For a simple transverse, noncomminuted type of fracture, tension band wiring is a standard procedure. Plate osteosynthesis is otherwise recommended for a more comminuted and complex fracture pattern.2
Wide-awake local anesthesia and no tourniquet (WALANT) provides an alternative that does not subject patient to the adverse effect of general anesthesia. It has been reported to be effective in hand and distal forearm surgery in providing analgesia and causing minimal blood loss.3,4 In this procedure, surgery is performed with the patient in a fully conscious state where tumescent anesthesia is injected into the surgical site without application of tourniquet.
The WALANT approach has not been used in fracture fixation proximal to the distal forearm. We describe the technique used in administering local anesthesia solution for olecranon fracture plating.
Materials and Methods
Anatomy
The periosteum has the most dense sensory innervation, followed by bone marrow and then mineralized bone.5 In long bones, trans-cortical vessels (TCVs) form the mainstay of blood circulation. When injected subperiosteally, lidocaine will diffuse through TCVs to block the sensory fibers subsequently in the marrow and mineralized bone.6
Technique
For WALANT solution preparation, we used a combination of lidocaine (1%), 1:100 000 epinephrine, and 10:1 8.4% sodium bicarbonate. To adhere to the maximum safe dose of 7 mg/kg lidocaine when epinephrine is added, the maximum dose for a 70 kg patient would amount to 49 mL of lidocaine (1%).
It is recommended that the surgical approach and the length of incision be predetermined based on the fracture configuration. We used a posterior approach as it provides better exposure over the fracture site as well as the elbow joint. The incision line was drawn with a surgical marker on the skin distal to the fracture and up until the humeral supracondylar region preoperatively as a guide for WALANT solution injection area.
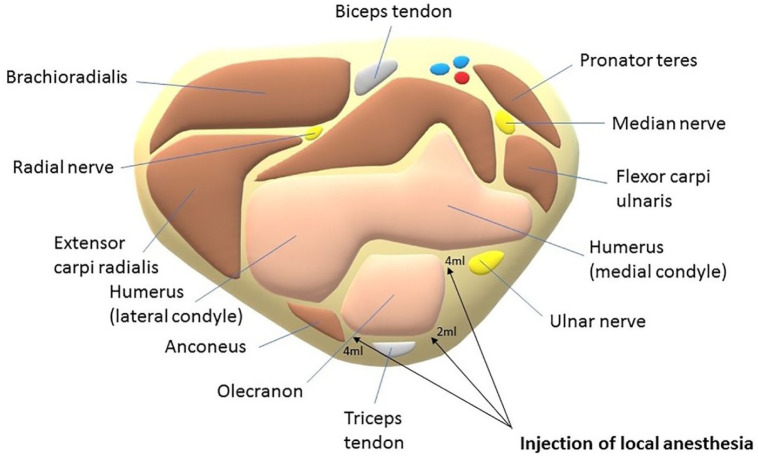
First, a total of 10 mL of subcutaneous local anesthesia was infiltrated using a 27-gauge needle along the predrawn midline elbow skin incision (marked with dotted lines in Figure 1). We ensured that at least 1 cm of visible or palpable subcutaneous local anesthetic was injected distally and proximally to the site of the planned incision.
Figure 1.
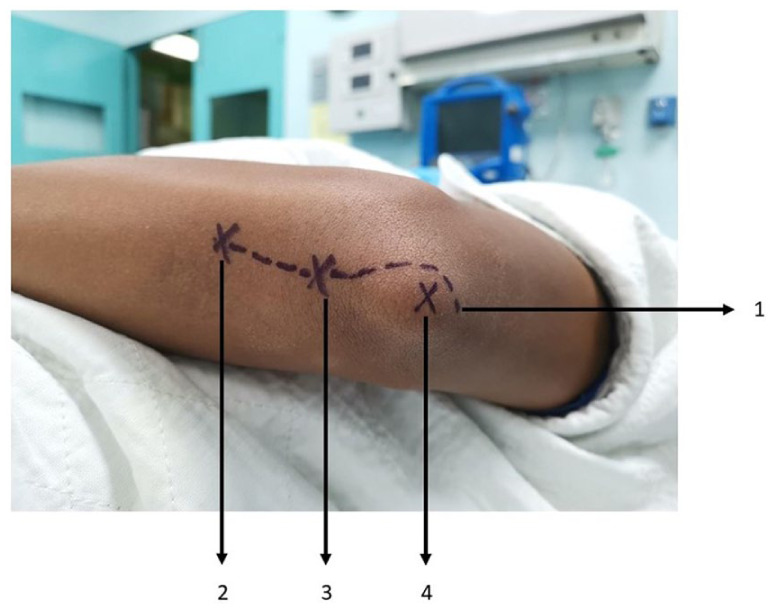
Schematic outline of techniques: 1—10 mL of tumescent analgesia along the planned skin incision; 2—10 mL of local anesthesia at the distal aspect of plate location; 3—10 mL of local anesthesia at the middle aspect of plate location; 4—10 mL of local anesthesia at the tip of olecranon.
Subsequently, another layer of local anesthesia is injected subperiosteally for the desired effect of painless surgery during reduction and plating of the olecranon fracture (Figure 2). From a total of 30 mL of solution, a 10-mL aliquot was injected using a 23-gauge needle at 3 different areas from proximal to distal as marked by “X” in Figure 1. The distance between each injection was 2.5 cm. In total, 40 mL of the solution was used, with 10 mL at the subcutaneous layer and 30 mL at the subperiosteal layer.
Figure 2.
Cross section of the olecranon for injection of anesthesia to the subperiosteal layer. Of the 10 mL for each marking, 2 mL is injected at the posterior border of the olecranon and 4 mL each at the medial and lateral aspect of the olecranon.
It is ideal to allow the local anesthesia a duration of at least 30 minutes to take effect. It takes an average of 25 minutes for maximal cutaneous vasoconstriction to occur with 1:100 000 epinephrine.7
Prior to the skin incision, we assessed the pain score by manipulating the fracture site using the numerical pain rating scale (NPRS). We proceeded with surgery only if the patient had an NPRS score of 0. The patient’s vital signs, bleeding, and NPRS were recorded at 10-minute intervals throughout the surgery, and the patient was observed for any adverse reactions.
The WALANT technique offers a good view of the fracture pattern and intra-articular involvement over the elbow joint due to minimal bleeding and less soft tissue swelling. It also allows us to assess the reduction of fracture and stability of plate fixation by observing the patient’s movement of elbow. In the absence of tourniquet, the patient can freely move the upper limb without restriction or discomfort.
Pearls and Pitfalls
As the ulnar nerve lies close to the medial side of the olecranon, extra care should be taken when injecting anesthesia around it. The needle should be constantly on the ulna bone before injecting the local anesthesia. This ensures that the local anesthesia is given subperiosteally. However, the local anesthesia might still trickle out if the periosteum is not intact and will cause an ulnar nerve block.
Case Illustration
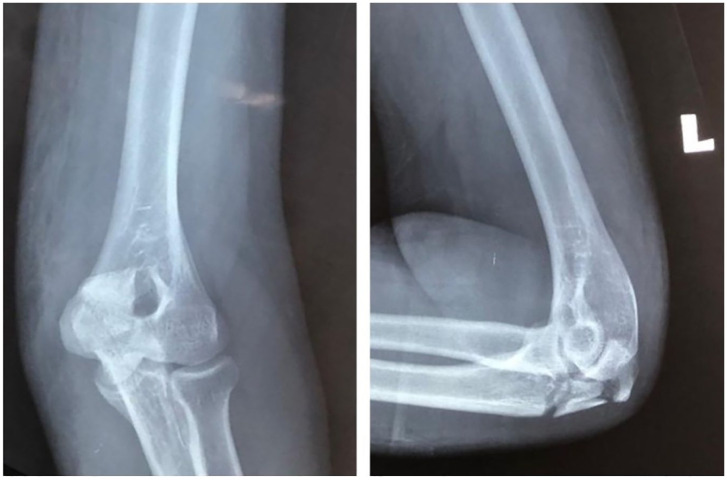
A 40-year-old man fell on his left elbow during a road traffic accident. After trauma, he complained of pain, swelling, and inability to move his left elbow. He also had a head injury due to the fall. Examination revealed tenderness and deformity over the left elbow. There was no neurovascular deficit over the left upper limb. Plain radiograph of his left elbow joint revealed a comminuted fracture of the olecranon (Figure 3). Computed tomography of his brain revealed a mild traumatic brain injury. He was observed in the neurosurgical ward for 1 week, and his neurosurgical status was stable.
Figure 3.
Preoperative radiograph of the left elbow showing comminuted fracture of the left olecranon.
He was counseled for open reduction and internal fixation for olecranon fracture. General anesthesia may subject the injured brain to new insults such as hypotension, hypoxemia, glucose irregularities, carbon dioxide irregularities, fever, and increase in intracranial pressure, which may lead to secondary brain injury.8 These complications may adversely affect the outcome. Therefore, an option for performing olecranon plating under WALANT was offered. The patient agreed for the surgery after being thoroughly explained regarding the procedure.
At the time of injection, his NPRS was 1, so he felt a needle sensation during subperiosteal injection of anesthesia over the olecranon. However, throughout the surgery, he was comfortable and consistently reported an NPRS of 0 (Figures 4 and 5; Supplemental Video A). There was no numbness over the ulnar nerve distribution. He denied any episode of shortness of breath, chest pain, and dizziness during and after the surgery. Bleeding was minimal throughout the surgery with good visibility (Figure 6). No additional local anesthesia was needed during the surgery as his NPRS was consistently 0.
Figure 4.

Patient lifting his left arm comfortably during painting, showing no tourniquet was applied.
Figure 5.

Patient lifting his left arm with the fracture site exposed.
Figure 6.

Intraoperative picture showing clear operative field with minimal bleeding.
He started to feel pain 6 hours after surgery. Oral analgesics were prescribed for pain control. He felt more comfortable the day after the surgery and was able to perform elbow range of motion as tolerated. Postoperative plain radiograph showed an acceptable fracture fixation (Figure 7). He was discharged home the next day, and follow-up at 1 month showed good elbow function.
Figure 7.
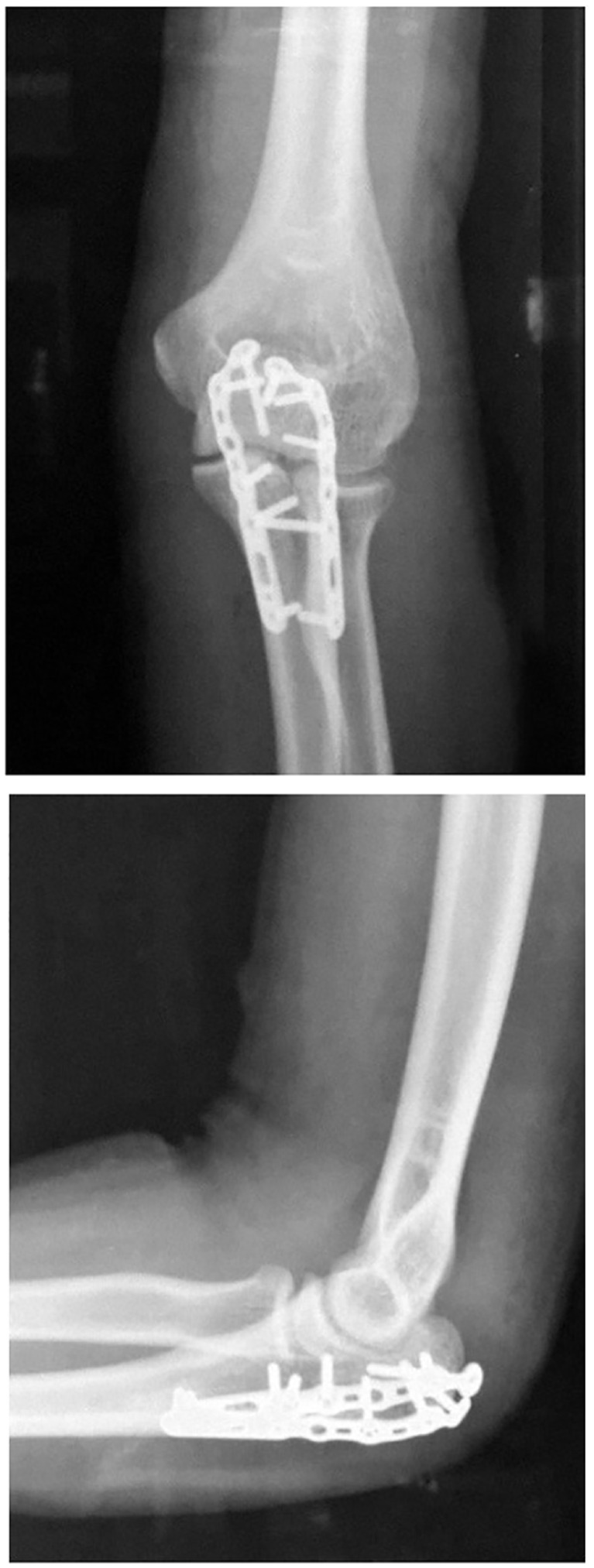
Postoperative radiograph of the left elbow showing anatomical reduction of the olecranon fracture with double locking plates.
Discussion
We chose the posterior approach to the elbow. With the initial preoperative WALANT injection, we were able to open and expose the fracture site. However, depending on the configuration of the fracture and presence of callus, additional WALANT solution could be injected into the deeper subperiosteal tissue before dissecting further.
Another point to address regarding this surgical approach is the patient’s position. The patient needs to be in the lateral decubitus position with the injured arm supported to provide a clear operating field and for adequate access for imaging. With the patient being awake throughout the surgery, staying in such a position for a prolonged duration is uncomfortable. The patient’s cooperation is very important. We did allow the patient some movement to get more comfortable during the surgery, but only to an extent that it does not interfere with the sterility of the operating field.
In conclusion, our study provides a new frontier for elbow surgery. We describe a safer, easier, and, more importantly, efficient anesthetic technique with WALANT for olecranon fracture fixation. This will hopefully open more possibilities to use WALANT in other elbow surgeries in the future.
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Amir Adham Ahmad  https://orcid.org/0000-0002-8976-8520
https://orcid.org/0000-0002-8976-8520
Shahril Shuhairi Sabari  https://orcid.org/0000-0001-5225-2654
https://orcid.org/0000-0001-5225-2654
Shalimar Abdullah  https://orcid.org/0000-0003-4509-842X
https://orcid.org/0000-0003-4509-842X
References
- 1. Rommens PM, Kuchle R, Schneider RU, et al. Olecranon fractures in adults: factors influencing outcome. Injury. 2004;35(11):1149-1157. doi: 10.1016/j.injury.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 2. Powell AJ, Farhan-Alanie OM, Bryceland JK, et al. The treatment of olecranon fractures in adults. Musculoskelet Surg. 2017;101(1):1-9. doi: 10.1007/s12306-016-0449-5. [DOI] [PubMed] [Google Scholar]
- 3. Ahmad AA, Yi LM, Ahmad AR. Plating of distal radius fracture using the wide-awake anesthesia technique. J Hand Surg Am. 2018;43(11):1045.e1-1045.e5. doi: 10.1016/j.jhsa.2018.03.033. [DOI] [PubMed] [Google Scholar]
- 4. Ahmad AA, Ikram MA. Plating of an isolated fracture of shaft of ulna under local anaesthesia and periosteal nerve block. Trauma Case Rep. 2017;12:40-44. doi: 10.1016/j.tcr.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chartier SR, Mitchell SAT, Majuta LA, Mantyh PW. The changing sensory and sympathetic innervation of the young, adult and aging mouse femur. Neuroscience. 2018;387:178-190. doi: 10.1016/j.neuroscience.2018.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grüneboom A, Hawwari I, Weidner D, et al. A network of trans-cortical capillaries as mainstay for blood circulation in long bones. Nat Metab. 2019;1(2):236-250. doi: 10.1038/s42255-018-0016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lalonde D. Minimally invasive anesthesia in wide awake hand surgery. Hand Clin. 2014;30(1):1-6. doi: 10.1016/j.hcl.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 8. Sviri GE, Aaslid R, Douville CM, et al. Time course for autoregulation recovery following severe traumatic brain injury. J Neurosurg. 2009;111(4):695-700. doi: 10.3171/2008.10.17686. [DOI] [PubMed] [Google Scholar]