Abstract
There are over 3.5 million breast cancer survivors living in the United States. Key elements of breast cancer survivorship care include monitoring for disease recurrence, addressing medical and psychosocial consequences of treatment, and educating about lifestyle interventions which decrease risk of recurrence, improve quality of life, and improve outcome. We have developed the PAVING the Path to Wellness Program for Breast Cancer Survivors in order to provide education on evidence-based topics from lifestyle medicine, with the goal to help women adopt healthy habits and improve well-being after cancer treatment. The 12-week program includes all 6 pillars of lifestyle medicine, as well as positive psychology, gratitude, and goal setting work. The PAVING the Path to Wellness Program for Breast Cancer Survivors empowers breast cancer survivors with knowledge regarding evidence-based lifestyle recommendations and helps them achieve an improved sense of well-being following treatment. On completion of the program, participants specifically reported an improvement in attitude and well-being. Next steps involve developing a strategy to offer this program to a larger group of cancer survivors.
Keywords: breast cancer, survivorship, exercise, nutrition, stress resiliency
‘PAVING the Path to Wellness is an innovative program that focuses on 12 key topics, with the goal to encourage participants to pursue positive lifestyle changes and optimize their health and well-being.’
Community lifestyle medicine programs are a powerful way to help individuals adopt and sustain healthy behaviors. The PAVING the Path to Wellness program was initially offered at Spaulding Rehabilitation Hospital in 2012, with the goal to optimize health and recovery for stroke survivors. Since that time, this program has been expanded to reach different patient populations. The program has been modified to optimize the health and recovery of those who have sustained traumatic brain injury. More recently, this program has also been adapted to enhance the quality of life, well-being, and outcome for women who have undergone treatment for breast cancer. Prior to the COVID-19 pandemic, the PAVING the Path to Wellness program was delivered in person only. However, during the pandemic, this program has been offered successfully in a virtual format via Zoom.
PAVING the Path to Wellness is an innovative program that focuses on 12 key topics, with the goal to encourage participants to pursue positive lifestyle changes and optimize their health and well-being. The PAVING program been shown to empower individuals to adopt healthy habits, including engaging in regular physical activity, making nutritious food choices, and achieving regular sleep patterns.1 An important goal of the program is to encourage participants to adopt a growth mindset for all aspects of daily life. Participants learn about the importance of setting SMART (Specific, Measurable, Action oriented, Realistic, Time sensitive) goals, and they are encouraged to identify personal strengths and find meaning and purpose. Participants are introduced to a variety of options to incorporate more physical activity, nutritious foods, stress reduction, and other healthy behaviors into daily life. Each of the topics covered in the program involves a didactic component, group discussion, exercises, and goal setting. The program also encourages participants to support one another and develop social connections.
The PAVING the Path to Wellness Program covers the following 12 topics (see Figure 1):
Figure 1.

Graphic depicting all 12 areas of the program.
Physical Activity: Aerobic exercise, strength training, and stretching are covered, as well as strategies to incorporate more movement into daily living.
Attitude: Participants are introduced to “growth mindset” concept, and encouraged to have an attitude of openness throughout the sessions.
Variety: Whether trying new vegetables, a different form of physical activity, or a new stress resiliency practice, “Variety” is emphasized throughout the lifestyle pillars.
Investigations: Participants enjoy investigating which lifestyle behaviors feel best for their body and are empowered to lead healthier lives.
Nutrition: Nutrition content encourages increasing nutrient density, preferring whole foods over processed foods, and helps participants gain skills through cooking classes.
Goal Setting: Through learning to set SMART goals, successful behavior change becomes more likely.
Stress Resiliency: Participants are introduced to a variety of stress resiliency tools including deep breathing, the relaxation response, and mindfulness-based stress reduction.
Time Outs: Participants learn the benefits of taking breaks from unhealthy influences, prolonged sitting, difficult conversations, and negative self-talk. A “time out” allows for increased clarity and overall well-being.
Energy: Increasing the use of natural sources of energy such as healthful foods, exercise, and connecting with friends allows participants to increase vitality through healthy behaviors.
Purpose: Identifying priorities, examining life’s meaning, and seeing the bigger picture in life allows participants to align their behaviors with their purpose.
Sleep: Through evaluation of the quantity and quality of their sleep and what enhances/detracts from sleep, participants are prepared to make their nights more restful.
Social Connections: Throughout the course, high-quality connections with family, friends, and community are emphasized and meaningful connections with others in the cohort are experienced.
The PAVING the Path to Wellness Program for Breast Cancer Survivors
There are over 3.5 million breast cancer survivors living in the United States.2 Breast cancer survivors have unique medical and psychosocial needs that should be addressed during the survivorship phase. Key elements of breast cancer survivorship care include monitoring for recurrence, addressing medical and psychosocial consequences of cancer treatment, and providing education about lifestyle interventions which decrease risk of recurrence, improve quality of life, and improve outcome.3 Following completion of treatment for breast cancer, many survivors experience weight gain and cardiometabolic changes,4 decreased physical functioning,5 and fatigue.6 The American Society of Clinical Oncology (ASCO) and American Cancer Society (ACS) have provided evidence-based guidelines for breast cancer survivorship care.3 There is growing evidence that poor diet, obesity, and inactivity are associated with an increased risk for recurrence and mortality from breast cancer.7,8 Thus, an important component of breast cancer survivorship care includes proactive assessment of diet, exercise, and other lifestyle factors.
Adoption of healthy behaviors after a diagnosis of breast cancer has been shown to reduce the risk of second cancers, reduce the risk of other comorbidities, and potentially reduce the risk of disease recurrence.7,9,10 Furthermore, adoption of a healthy lifestyle after a diagnosis of breast cancer may also reduce symptoms related to prior cancer treatment and improve quality of life.11 Amy Comander has modified the PAVING the Path to Wellness Program for Breast Cancer Survivors in order to educate participants on evidence-based topics from lifestyle medicine, with the goal to help women adopt healthy habits and improve well-being after treatment for breast cancer. The PAVING program provides breast cancer survivors with the tools needed to focus on weight management and physical activity, both of which are associated with improved overall and cancer-specific survival in women with a history of early stage breast cancer.7,9 The program also provides participants with opportunity to develop social connections and support from other cancer survivors and enables participants to thrive after cancer treatment.
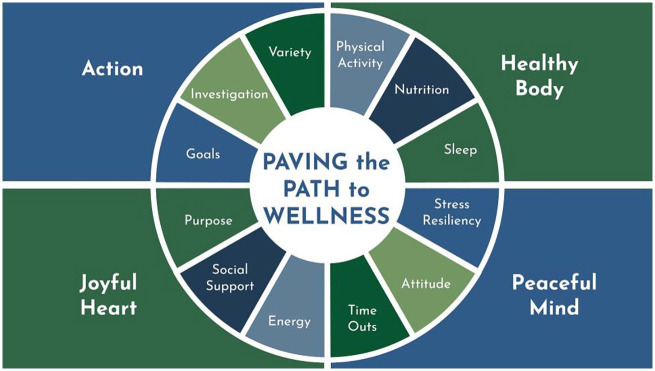
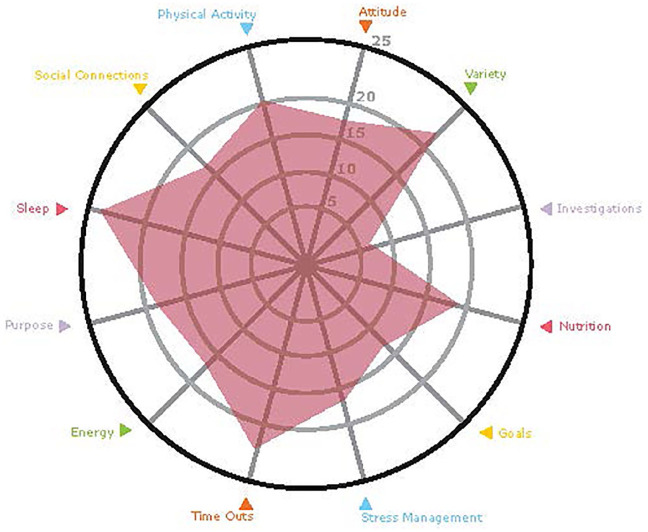
The first 12-week program was offered in person in the fall of 2019. Women with a diagnosis of breast cancer, of any stage, were eligible for the program. The first 12-week session of the PAVING the Path to Wellness Program, held in September 2019, involved 14 participants. At the first session, participants assessed wellness using the PAVING Wheel (see Figures 2 and 3). The PAVING Wheel is currently used in the Physician Wellbeing course offered through the American College of Lifestyle Medicine. Participants explore each area of the wheel by answering questions in a Likert-type scale that addresses key components to each step. After answering the questions, participants plot their answers on a wheel that creates a radar plot (see Figure 4). There is no “right or wrong answer”—each person’s wheel reflects their own individual journey and provides an opportunity for the individual to reflect on what is working well, and which specific areas may need more focus.
Figure 2.
Radar plot of PAVING STEPSS: Participants answer questions about each of the steps and calculate a subtotal for each of the 12 sections and then plot them on the PAVING Wheel.
Figure 3.
PAVING STEPSS Wheel identifying all 12 steps and how they correlate to healthy body (physical activity, nutrition, sleep), peaceful mind (stress resiliency, attitude, time out), joyful heart (purpose, social connection, energy), and action (goals, investigations, variety).
Figure 4.
Example of a completed radar plot.
Each participant in the PAVING program is given a workbook and a copy of The Lifestyle Medicine Handbook: An Introduction to the Power of Healthy Habits, co-authored by Dr Beth Frates and colleagues, as well as a workbook. At the beginning of each session, the physician leader welcomes participants and facilitates a discussion about how each individual incorporated last week’s topic into her routine. The participants welcome the opportunity to share successes and struggles, while receiving feedback from their peers and physician facilitator. Next, the physician or guest expert presents content on the weekly PAVING step. This informational component lasts for approximately 45 minutes, and includes a didactic component, and also provides opportunities for participants to ask questions and comment. The PAVING step content is modified for increased relevance to the specific patient group. For example, in the week focused on the “Stress Resilience” for breast cancer survivors, the facilitator shared literature highlighting how resilience improving strategies improve health outcomes.12 Sessions typically conclude with about 30 minutes of participants sharing their insights from the presentation in the large group, or in small breakout Zoom rooms.
At the final 12-week session, each participant completes another PAVING Wheel and has the opportunity to reflect on the progress she has made over the course of the 12 weeks. The 12th weekly session focuses on the importance of “Social Connections.” During this final week, the participants know each other well and have formed strong bonds with one another. The social connections that have been formed in these PAVING groups are quite remarkable, and the groups have continued to meet on their own for support. This aspect of ongoing social support has also been shown to be of great benefit for breast cancer survivors.13
Description of the PAVING the Path to Wellness Program in a Virtual Format
The PAVING program was offered to a second group of breast cancer survivors in March 2020, and this program involved 12 participants. While the first session was held in person, due to the COVID-19 pandemic, the program was quickly transitioned to a virtual format. The remaining 11 sessions were held virtually, using Zoom. Transitioning the program to a virtual format presented a number of logistical challenges, and there was concern that participants would not be able to engage as fully with one another and form social connections. However, the participants seemed to adjust extremely well to the online format and appreciated the opportunity to join without the typical travel time, parking costs, babysitting, or navigating the actual facility. In addition, traveling to a facility can be challenging for patients recovering from recent surgery or experiencing treatment side-effects. Although there was a loss of being physically present with the group, overall the feedback from participants was tremendously positive. The participants enjoyed the use of “breakout rooms” in Zoom that enabled them to connect with one another.
The COVID-19 pandemic has presented challenges for survivorship care.14 However, the pandemic has also provided an opportunity to innovate how health care providers deliver care to our patients, and telemedicine is playing an increasingly important role. A recent Pew Research Center study has reported that the vast majority of Americans own a smartphone of some kind, and nearly three quarters of US adults now own desktop or laptop computers.15 During the pandemic, there has been rapid use of telemedicine for virtual visits, as well as the opportunity to provide group virtual visits for cancer survivors. Based on this recent experience with the PAVING program, the participants adapted well to the online format. Many logistical challenges remain, including (1) training both the healthcare providers, and survivors, for use of a virtual platform; (2) variation access to the internet and cellular service; and (3) inexperience with using virtual platforms. Despite these challenges, use of a virtual platform will permit greater access to survivorship care, such as the PAVING program. Additional challenges in transitioning live groups to virtual groups include teaching participants online Zoom etiquette; answering participant technical questions; sharing screens; using breakout rooms; encouraging participants to participate in this virtual format; and learning to manage the discussion while monitoring the “chat” simultaneously. There are a number of strategies that can make the Zoom experience more engaging for participants. Such strategies include incorporating interactive audience response platforms such as “Poll Everywhere,” Zoom breakout rooms, and the “chat” feature.
The virtual format allows for participants and guest experts to join from remote locations, which would not have been possible with in-person sessions. Despite the location differences, the participants from remote locations quickly connected with the others in the group due to the shared breast cancer experience. Since there is no travel time, parking fees, issues with child care or eldercare, participants are more likely to attend regularly. In addition, those participants who are having a challenging day and would not be able to make the trip to the clinic or hospital are able to join in with the click of a button.
Reflections on the PAVING the Path to Wellness Program for Breast Cancer Survivors
On review of the surveys from both the Fall 2019 and Spring 2020 groups, participants responded favorably to the program in terms of making important lifestyle changes, and reported improved knowledge, attitudes, and skills. For example, many participants made dietary changes that included adopting a whole food, plant-based diet. A number of participants have learned to prioritize exercise, including walking, biking, or exercising with a personal trainer. One participant recently purchased a treadmill desk.
We have received excellent feedback from the participants:
The PAVING program has been so important for me because it connected me to others who’ve gone through cancer treatment. My PAVING pals immediately understand what I’m talking about when I express a concern or fear. In fact, these are the only people I can talk to openly about breast cancer and that’s been invaluable in helping me move forward in my life. Cancer will always be a part of my life but I want to keep it in perspective, and PAVING and my PAVING pals have helped me do just that.
When you have cancer, life feels completely out of control. After participating in the PAVING program, I know that I have a better handle on controlling my fears and doing what I can to remain healthy.
When I heard that Dr Comander was starting the PAVING program, I was the first to sign up! It was exactly what I was looking for after going through chemotherapy, a double mastectomy, and radiation. I enjoyed going to the class every week and focusing on a different topic. My favorites were “Purpose” and “Investigation.” I learned so much, and loved so many aspects of the classes: meeting the other amazing women, learning from Dr Comander and the other staff and professionals she brought in, hearing about so many resources to try. The in-person cooking class was amazing, too! The women in the class decided to continue on as a support group and we still meet twice a month to share resources and support each other. I highly recommend the PAVING course with Dr Comander!
Personally, as a physician and breast cancer survivor who has been a part of other breast cancer survivor groups that are not as supportive and focused solely on disease rather than enhancing health, being a part of PAVING was especially rewarding. (Dr Michelle Tollefson)
As the facilitator, it has been incredibly rewarding to see the great benefits that these women have derived from the group’s teachings, and to witness the strong connections formed in the group. (Dr Amy Comander)
Conclusion
The PAVING the Path to Wellness Program for Breast Cancer Survivors is a successful survivorship program that empowers participants with evidence-based recommendations about lifestyle interventions which have been shown to decrease risk of recurrence, improve quality of life, and improve outcome from breast cancer. Upon completion of the program, participants report an improved sense of well-being. An unexpected outcome of the PAVING program is that the PAVING groups continue to meet on their own for ongoing support and education, and the participants have even established their own private Facebook group and created a PAVING program newsletter.
Next steps will involve developing a strategy to scale this program to serve more patients. There has been interest in the program beyond the Boston area with the virtual format, the possibilities for including people all over the country and even internationally are exciting. It will be important to have an adept and PAVING method trained lifestyle medicine practitioner who can engage the group in a virtual format. Having an additional person to be on the call to assist with technical support (for the presenter, guests, and participants) and reviewing the chat box would be beneficial and free the physician to focus solely on the content and group engagement. Administrative tasks involved with course coordination and execution can take a considerable amount of time whether online or in-person. Having an assistant to support the facilitator would make the process easier and more manageable moving forward.
Knowing the tremendous need and enormous potential for lifestyle medicine group interventions like the PAVING the Path to Wellness Program, we look forward to working with and collaborating with fellow lifestyle medicine practitioners to advance this type of transformational patient experience.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
Contributor Information
Amy Comander, Harvard Medical School, Massachusetts General Hospital Cancer Center, Boston, Massachusetts.
Beth Frates, Harvard Medical School, Spaulding Rehabilitation Hospital, Boston, Massachusetts.
Michelle Tollefson, Metropolitan State University of Denver, Denver, Colorado.
References
- 1. Frates EP, Crane ME. Lifestyle medicine consulting walking meetings for sustained weight loss. BMJ Case Rep. 2016;2016:bcr2015213218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7-30. [DOI] [PubMed] [Google Scholar]
- 3. Runowicz CD, Leach CR, Henry NL, et al. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. J Clin Oncol. 2016;34:611-635. [DOI] [PubMed] [Google Scholar]
- 4. Vance V, Mourtzakis M, McCargar L, Hanning R. Weight gain in breast cancer survivors: prevalence, pattern and health consequences. Obes Rev. 2011;12:282-294. [DOI] [PubMed] [Google Scholar]
- 5. Marinac C, Patterson RE, Villasenor A, Flatt SW, Pierce JP. Mechanisms of association between physical functioning and breast cancer mortality: evidence from the Women’s Healthy Eating and Living Study. J Cancer Surviv. 2014;8:402-409. [DOI] [PubMed] [Google Scholar]
- 6. Bardwell WA, Ancoli-Israel S. Breast cancer and fatigue. Sleep Med Clin. 2008;3:61-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schmid D, Leitzmann MF. Association between physical activity and mortality among breast cancer and colorectal cancer survivors: a systematic review and meta-analysis. Ann Oncol. 2014;25:1293-1311. [DOI] [PubMed] [Google Scholar]
- 8. Parada H, Jr, Sun X, Tse CK, Olshan AF, Troester MA. Lifestyle patterns and survival following breast cancer in the Carolina Breast Cancer Study. Epidemiology. 2019;30:83-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chlebowski RT, Aragaki AK, Anderson GL, et al. Association of low-fat dietary pattern with breast cancer overall survival: a secondary analysis of the women’s health initiative randomized clinical trial. JAMA Oncol. 2018;4:e181212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project Expert Report 2018. Diet, nutrition, and physical activity and breast cancer survivors. Revised 2018. Accessed December 24, 2020. wcrf.org/sites/default/files/Breast-cancer-survivors-report.pdf [Google Scholar]
- 11. Smith AW, Alfano CM, Reeve BB, et al. Race/ethnicity, physical activity, and quality of life in breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2009;18:656-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Seiler A, Jenewein J. Resilience in cancer patients. Front Psychiatry. 2019;10:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kroenke CH, Michael YL, Poole EM, et al. Postdiagnosis social networks and breast cancer mortality in the After Breast Cancer Pooling Project. Cancer. 2017;123:1228-1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nekhlyudov L, Duijts S, Hudson SV, et al. Addressing the needs of cancer survivors during the COVID-19 pandemic. J Cancer Surviv. 2020;14:601-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pew Research Center. Mobile fact sheet. Demographics of mobile device ownership and adoption in the United States. Published June 12, 2019. Accessed November 20, 2020. https://www.pewresearch.org/internet/fact-sheet/mobile/