Abstract
Purpose:
To assess firework-inflicted ocular trauma in the German capital during the week around New Year’s Eve with regards to patient characteristics and age, severity of injuries, and their management and outcome.
Methods:
A retrospective chart review of all patients presenting to the department of ophthalmology of Charité—University Medicine Berlin during a 7-day period around New Year’s Eve in the years 2014–2017 was performed. Patients with ocular complaints and injuries caused by fireworks were included. We recorded demographic data, active role, visual acuity at presentation and at last follow-up, the most pertinent clinical findings, management and outcome with regards to visual acuity, and integrity of the eye.
Results:
A total of 146 patients with 165 injured eyes were included. Median age at presentation was 23 (4–58) years, and 71.2% were male. Fifty-one patients (34.9%) were less than 18 years old. Ninty-seven patients (66.4%) sustained minor, 34 (23.3%) sustained moderate, and 15 (10.3%) sustained severe injuries. Severe trauma was seen in younger patients (median age: 12, range: 4–58 years) than mild and moderate trauma (median age: 23, range: 4–45 years) and resulted in loss of light perception in two eyes and in a visual acuity of only light perception in three eyes. One eye was enucleated.
Conclusion:
Ocular trauma inflicted by fireworks can have serious consequences for ocular morbidity and visual acuity, especially in severe trauma which affected younger patients. To significantly reduce firework-inflicted trauma, a ban of private fireworks in densely populated areas and in the vicinity of children should be considered.
Keywords: Ocular, trauma, fireworks, explosive, children
Introduction
Fireworks, particularly if used by non-professionals, may inflict severe trauma and even cause death. Due to the physical energy released during firework explosions, injuries of the eye and hands are a frequent and well-described problem.1–5
The private, non-professional use of fireworks is common in Germany around New Year’s Eve.
The German Explosives Act (“Sprengstoffgesetz”) and related regulations allow the purchase of category F2 (formerly class II) pyrotechnical devices, such as rockets, firecrackers, and compound firework devices, by adults (legal age 18 years) during 3 days before the New Year.6,7 Category F2 fireworks are defined as “fireworks which present a low hazard and low noise level and which are intended for outdoor use in confined areas” by the European directive 2013/29/EU. According to this directive, the maximum noise level for the designation to the F2 category must not exceed 120 dB at a safety distance, which is usually 8 m.8
There have been calls to limit private firework activities in order to reduce the incidence of associated injuries. In 1984, the World Health Organization (WHO) recommended banning the production of firework devices completely.4
The preventive potential of legal regulations concerning private fireworks is reflected in the smaller incidence in countries or areas with stricter laws compared to others which lack them.3,9 In Northern Ireland, the ban of fireworks was lifted in 1996 which resulted in an increased incidence and increased portion of firework-induced ocular trauma (0.85% of all eye and adnexal trauma during the ban, 2.9% after the ban was lifted).10
In this study, we recorded and analyzed ocular trauma associated with fireworks during the week around New Year’s Eve in a tertiary eye hospital in Berlin, Germany over a 4-year period.
Methods
A retrospective chart review of all patients presenting to the department of ophthalmology of Charité—University Medicine Berlin, a tertiary care center, during the week around New Year’s Eve (December 28—January 3) for the years from 2014 to 2017 was performed. We included patients with ocular complaints (e.g. due to a subtarsal foreign body) or injuries caused by fireworks. Patients under the age of 18 years were defined as minors, and patients 18 years and older were defined as adults. The retrospective chart review followed the ethical standards of the Declaration of Helsinki. The patients’ consent for publication of images used in this report was obtained.
Diagnostic work-up and treatment
Patients were primarily presenting to our Emergency department and were triaged by trained nurses according to the Manchester Triage System. Depending on the complaints, the cases were assigned to the different services including trauma surgery, maxillofacial surgery, ENT, neurosurgery, neurology, ophthalmology, and others. The primary assigned serviced involved other specialties in the case of newly revealed injuries.
For the ophthalmological exam, best-corrected visual acuity (BCVA) was measured at distance (5 m) with the patient wearing the best correction whenever possible. In case optotypes could not be discerned, finger counting, hand motion, and light perception were tested. Intraocular pressure (Goldmann applanation or rebound tonometry using the ICare device in children and palpation when neither was possible) was measured. Pupillary examination as well as inspection of the adnexa was done, and the anterior segment was examined using slitlamp biomicroscopy (in uncooperative children, loupes were used in combination with a light source). The ocular fundus was examined using indirect ophthalmoscopy. B-scan ultrasonography was performed whenever the view to the fundus was obstructed, except for cases of suspected penetrating injury. For suspected intraocular foreign bodies and for suspected orbital trauma including bony fractures, an urgent computed tomography (CT) scan was ordered. Additional diagnostic work-up such as optical coherence tomography (OCT) or corneal topography was performed according to the clinical findings at follow-up appointments.
In patients with severe trauma and obvious penetrating or perforating wounds, urgent examination under general anesthesia and, if deemed necessary by the treating ophthalmologist, surgical exploration and treatment were performed.
For minor injuries such as corneal erosions, topical antibiotics and/or steroids were prescribed as indicated. Minor eyelid repair was performed in the emergency department on an outpatient basis. For more delicate or extensive surgery, especially surgery performed under general anesthesia and intraocular surgery, for intravenous drug application or an intensive eye drop regimen (e.g. in alkali burns) patients were hospitalized. Intravenous antibiotics were administered in cases of open-globe trauma to prevent endophthalmitis and in extensive eyelid or orbital injuries. Tetanus vaccination as indicated was given in our emergency department.
Data collection and analyzed parameters
For this study, the digital charts of all emergency cases presenting during the study period were reviewed. Whenever the inclusion criteria were fulfilled, we recorded and analyzed the time of initial presentation, laterality of the injured eye, and demographic details including age, gender, and location of residence. When available, the role of the injured was categorized as actively participating versus passively watching (bystander). We studied the most relevant clinical features at presentation, the management (conservative vs surgical), and types of primary and number of secondary procedures. For hospitalized patients, the German Diagnosis-Related Group (G-DRG) charges of the primary hospital stay were recorded to assess the direct cost of care. Additional costs, for example, from outpatient follow-up visits or work loss were not available. BCVA was used as the endpoint for visual outcome and was reported as the logarithm of the minimum angle of resolution (logMAR). Low visual acuity values were transformed to logMAR as suggested by Bach and colleagues:11,12 finger counting to 1.9 logMAR, hand motion to 2.3 logMAR, light perception to 2.7 logMAR, and no light perception to 3.0 logMAR. Furthermore, preservation of the globe was analyzed.
Information from all follow-up visits of all cases until 31 December 2018 was included.
Statistical analysis
We followed the terminology of ophthalmic trauma as proposed by Kuhn et al.13 To facilitate statistical analysis, we used the grading system of eye injuries devised by Karlson and colleagues.14,15 In this system, minor trauma includes corneal abrasion, foreign body on the eye, traumatic iritis, conjunctival hemorrhage, orbital fractures (excluding blowout fractures and extensive fractures) as well as superficial and smaller periorbital abrasions, contusions, and lacerations. Contusio bulbi (closed-globe injury without full-thickness corneal or scleral wound,13 that is, accompanied by commotion retinae), hyphema, blowout fractures, and periorbital burns larger than 2.5 cm or affecting subcutaneous tissue, involving contaminated or avulsed tissue or multiple (>2) minor lacerations were deemed moderate trauma. Injuries including corneal laceration and full-thickness corneal wounds, scleral laceration, intraocular foreign bodies, optic nerve injuries, alkaline burns, traumatic cataract, retinal detachment, extensive orbital fractures as well as lid avulsion and lid laceration with tear duct involvement are graded as severe trauma.
Data collection and simple analysis for descriptive statistics was performed using Microsoft® Excel® (Redmond, WA, USA). For further analysis, IBM® SPSS® Statistics, version 25 (Armonk, NY, USA) was used.
To test for the contribution of severe injuries, open-globe injuries, or surgical therapy among the age groups, cross tables, and a chi-square test were used. For the comparison of the difference between the age in two separate groups, we used a t-test.
Results
During the 7-day period around 31 December of the years 2014–2017, 146 patients (165 eyes) presented with firework-associated ocular complaints. In 87% of patients, the injuries were unilateral, and in 53.9% of patients, the right eye was affected.
Each year, 1 January was the day when most patients presented with firework-inflicted ocular trauma (106 patients, 72.6%). On 31 December, 21 patients (14.4%) presented, followed by 2 January with 15 (10.3%), 3 January with 2, and 29 and 30 December with 1 patient (Figure 1).
Figure 1.
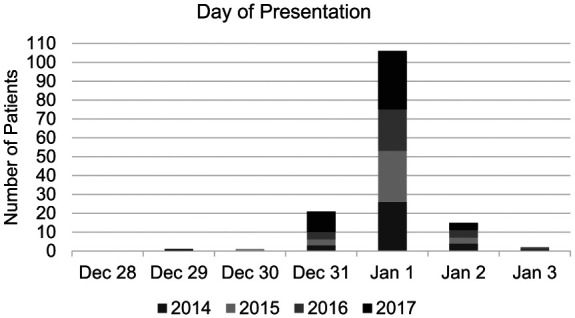
Day of initial presentation of patients with firework-inflicted ocular trauma for the years 2014-2017.
The median number of patients per year was 34 (range: 31–47). Comparing 2017 with the 3 years before, the number of presenting patients was notably higher (n = 47) than from 2014 to 2016 (33 patients on average) and there were more cases of severe trauma (8 cases vs 3.5 cases on average from 2014 to 2016). Data on whether the patient was a bystander or an active user of the fireworks was available for 41 patients (28.1%). Of these, 61% patients stated that they were injured as passive bystanders.
Demographic data
The median age of the 146 patients was 23 (range: 4–58) years. Of the 146 patients, 104 (71.2%) were male and 101 (69.2%) were younger than 30 years (Figure 2). Of the 146 patients, 51 (34.9%) were under the age of 18 years, and most of them were male (37 patients, 72.5%).
Figure 2.
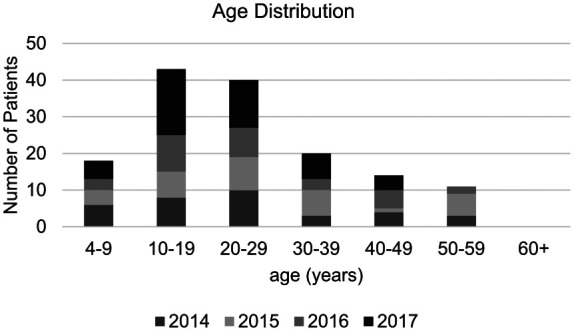
Age distribution of patients with firework-inflicted ocular trauma in 2014-2017.
While 113 patients (77.4%) were residents of the German capital city, 33 (22.6%) were either referred to our hospital from outside of Berlin or visiting for the holiday.
Initial diagnosis and severity of injuries
The most relevant features of firework-inflicted ocular trauma revealed by the primary examination are listed in Table 1.
Table 1.
Initial diagnosis at first presentation of patients with firework-inflicted ocular trauma in the years 2014-2017.
| Number of affected patients per diagnosis | Proportion of affected patients (146 = 100%) (%) | |
|---|---|---|
| Corneal abrasion or superficial punctate epithelial surface defects | 59 | 40.4 |
| Conjunctival or corneal foreign body | 32 | 21.9 |
| Smaller periocular abrasions or burns | 29 | 19.9 |
| Eye lash burn | 17 | 11.6 |
| Conjunctival or corneal powder deposits | 15 | 10.3 |
| Subconjunctival hemorrhage | 6 | 4.1 |
| Hyphema including microhyphema | 29 | 19.9 |
| Commotio retinae | 16 | 11.0 |
| Deeper or extensive lid laceration | 9 | 6.2 |
| Iris sphincter tear or distored pupil | 8 | 5.5 |
| Vitreous hemorrhage | 6 | 4.1 |
| Iridodialysis | 4 | 2.7 |
| Angle recession | 1 | 0.7 |
| Perforating corneal or scleral wound | 5 | 3.4 |
| Eyelid avulsion | 4 | 2.7 |
| Conjunctival or corneal burn | 4 | 2.7 |
| Traumatic cataract, phakolysis, and lens luxation | 4 | 2.7 |
| Choroidal bleed | 2 | 1.4 |
| Ora dialysis or tear | 2 | 1.4 |
| Retinal detachment | 1 | 0.7 |
| Lamellar corneal wound | 1 | 0.7 |
| Subretinal bleed | 1 | 0.7 |
| Choroidal tear | 1 | 0.7 |
| Choroidal infarction | 1 | 0.7 |
| Total | 256 |
According to the grading system by Karlson and Klein,14 97 cases (66.4%) were classified as minor, 34 (23.3%) as moderate, and 15 (10.3%) as severe injuries (Table 2). Five eyes of five patients (3.4%) sustained open-globe injuries.
Table 2.
Age and severity of firework-inflicted ocular injuries in the years 2014-2017, grading according to Karlson and Klein14.
| Minor injury | Moderate injury | Severe injury | |
|---|---|---|---|
| Minors | 36 (70.6%) | 6 (11.8%) | 9 (17.6%) |
| Adults | 61 (64.2%) | 28 (29.5%) | 6 (6.3%) |
Among minors, there was more severe trauma and less moderate trauma compared with the adult cohort (p = 0.012, chi-square test). The median age of patients with severe trauma was 12 years (range: 4–58 years) versus 23 years (range: 4–45 years) of patients with moderate and minor trauma (95% confidence interval (CI): −14.3 to −1.4, p = 0.02, t-test). Of the five patients with open globe injuries, three were minors and two were adults, accounting for 5.8% and 2.1% in their respective age groups (p = 0.232).
Management
The majority of patients were treated as outpatients. Twenty-one individuals (14.4%) were admitted to the hospital, three of them for solely non-ophthalmological indications (in one case, extensive facial burn with a comminuted nasal fracture and in two cases, complex finger fractures). In four cases, admission was prompted by the ocular injury as well as the accompanying trauma (complex hand injury, complex orbital fracture, severe facial burn, and open-skull fracture in one case each). Ocular injuries leading to admission were graded as moderate in three cases (all adults) and severe in 15 cases (nine minors and six adults). The median duration of the hospital stay was 5 days (range: 2–40 days), and the median cost of inpatient care was 3.056 Euro (range: 1.199–60.138 Euro).
Of the 146 patients, 17 (11.6%) required ophthalmosurgical treatment. Eight were minors and nine were adults (15.7% and 9.5% of their respective age group; p = 0.265). The primary surgical procedures were scleral or corneal wound repair (5 cases), eyelid repair (4 cases), examination under general anesthesia with or without foreign body removal (3 cases), peritomy combined with transplantation of amniotic membrane (2 cases), scleral buckling surgery with cryopexy (1 case), vitrectomy (1 case), and iris suture (1 case).
In 10 patients (6.8%), more than one surgery was necessary. Secondary procedures included phacoemulsification/lentectomy, transplantation of amniotic membrane, and enucleation. The median number of secondary procedures was 1 (range: 0–4).
Outcome
The majority of cases of mild or moderate trauma was followed by ophthalmologists in private practice. Data for those patients regarding further treatment and the outcome was not available for analysis. For 30 cases, follow-up data were available, and 19 cases were followed by our institution for at least 2 weeks (median: 81 days, range: 14–461 days).
Seven patients with moderate trauma were followed at our institution for more than a week and had a median visual acuity of 0.1 (range: 0–0.6) logMAR at their last visit (median 37 days after presentation, range: 10–350 days).
In patients with severe trauma, median visual acuity was 1.0 logMAR (range: 0–3) after a median follow-up of 134 (range: 3–461) days. Two eyes lost light perception (3 logMAR; both male, 12 and 27 years; upon presentation, visual acuity could not be measured in the younger patient, whereas there was no light perception in the older patient), three eyes of three male patients had light perception (11, 12, and 45 years old); in one case, final visual acuity was 0 logMAR (male, 23 years).
Enucleation during the primary hospital stay was necessary in one case (0.68%, male, 27 years old, bystander). Until the end of the follow-up period on 31 December 2018, no further enucleations were performed.
Discussion
During the week around New Year’s Eve of the 4-year study period, 146 patients were treated at our institution in Berlin, Germany. Studies have shown that most patients injured by fireworks sustain trauma to other body parts, while the eye is injured in about one-third of cases.1,16 In the Netherlands, data from all emergency departments nationwide amounted to 434 patients (27% under the age of 15 years) with fireworks-associated injuries treated on 31 December 2017 and 1 January 2018—eye injuries accounted for 27% of all injuries.17
Agreeing with prior publications, patients in our study were predominately male (71.2%) and younger (69.2% younger than 30 years). This pattern seems to be consistent over the years. In their review of 26 articles including 7742 cases, Wisse et al.3 found a male predominance (75%, range: 66–95%) and more young patients (67%) among those injured. Newer literature by Chang et al.16 (89% male, 41% younger than 18 years), Unterlauft et al.5 (77%, 24.6% 18 years or younger), and Frimmel et al.18 (65% male) shows similar age and gender distributions for patients with ocular trauma due to firework.
Most injuries inflicted by fireworks are mild (66.4% in this study) and can be expected to heal without lasting damage. Similar to Wisse et al.,3 we found corneal abrasions in about 40%. Moderate trauma, including globe contusion accounts for 23.3% and severe trauma for 10.3% of our cases, meaning that, about one-third of firework-inflicted ocular injuries can potentially cause permanent sequelae, such as secondary glaucoma or central retinal atrophy (Figure 3).
Figure 3.
Right eye of a teenager, non-active role in firework, hit by a rocket. (a) iris sphincter tears; (b) optical coherence tomography (OCT) showing retinal swelling one day after the incident; (c) corresponding fundus photograph one day after the incident; (d) OCT showing macular atrophy two weeks after the incident, final BCVA 1.3 logMAR. Hospital admission for surgery due to zygomatic fracture.
Among those who suffered severe ocular injury, minors (under the age of 18 years) accounted for 60% (9 cases), similar to Jing et al.19 who analyzed severe firework-inflicted trauma and found 41.7% of affected patients to be 18 years or younger and 25% to be between 19 and 35 years old. Sacu et al.,15 who previously used the same severity classification as this study, reported minors to account for 72% of severe injuries. In contrast to these findings, Unterlauft et al.5 who studied firework-inflicted ocular injuries around New Year’s Eve from 2005 to 2013 at the University Hospital of Leipzig, Germany, reported a higher patient age among the severely injured compared to the other patients (median: 25 years, range: 7–72 years compared to 22.5 years, range: 1–63 years). The authors suggested that a faster reaction time in younger individuals could prevent severe injuries—an observation not supported by our findings. In fact, our data show that younger individuals are at high risk to sustain firework-inflicted ocular trauma in general and at a higher risk for several ocular trauma in particular. There may be different reasons for this finding, including a riskier behavior when handling firework actively and less awareness of the potential dangers of fireworks when watching it as a bystander in the younger age group. In younger patients, the impact of reduced vision will accumulate over the patients’ life, and the public should be informed about the health risks fireworks pose, particularly to the eye. Parents should know about these risks when supervising children close to fireworks. Policy makers need to consider these severe risks to the health of children, when deciding about the availability of fireworks for private use.
Visual acuity at last follow-up reflected the severity of ocular trauma sustained. In those with moderate trauma followed up at our institution (n = 7), median BCVA was 0.1 logMAR. Median BCVA in patients with severe trauma (follow-up BCVA available in all cases except the single primary enucleation) was significantly reduced to 1.0 logMAR. Taking into account the young age in the group of severe injuries (median 12 years, range: 4–45 years), the psychological, social, and economic burden is large and long-lasting.
The enucleation rate in our study was 0.68%, this compares favorably to the 3.9% reported by Wisse et al.3 who examined data published between 1969 and 2009. This might reflect today’s more advanced treatment options allowing more eyes to be saved. However, Chang et al.16 reported an enucleation rate of 10% between 2003 and 2013 and having more open-globe injuries (17% vs 3.4% in our study). This is likely due to the fact, that Chang et al. studied the experience of the sole level I trauma center for five U.S. states. Given the retrospective nature of this work, 127 patients (86.9%) were followed up by ophthalmologists outside our institution. Therefore, unfavorable outcomes like decreased visual acuity or enucleation might be underestimated by our report.
The costs for the initial hospitalization (G-DRG charge) for the 21 admitted patients totaled €123.449. Smith et al.1 provided information regarding inpatient charges between 1984 and 1988 in children and reported a median of US$7.716 per patient (US$867–US$14.168). In their analysis, the average charge for outpatients and inpatients was US$1385. However, the total cost of firework-inflicted ocular injuries including loss of work capacity for example, remains to be defined.
Our clinical perception of increasing numbers and severity of firework-inflicted ocular trauma is supported by the number of affected minors which rose from an average of 10.3 (2014–2016) to a total of 20 in 2017. Whether this reflects a general trend or whether it is simply an outlier remains to be seen. Special occasions, such as the bicentennial celebration of the American Independence Day in 1976 have been shown to lead to more injuries than previously reported.1
In comparison with our data, a study by Frimmel et al.18 from the University Hospital of Zurich, Switzerland, reports lower numbers of firework-induced ocular injuries for New Year’s Eve (two on average). In Zurich, there is a ban of private fireworks between 6 o’clock in the evening and 2 o’clock in the morning in the city center and public firework displays, highlighting the effectivity of stricter laws on private fireworks in public with regards to the prevention of ocular injuries.
Firework-inflicted injuries are a completely preventable health risk. Bull9 illustrated the steps toward a lower incidence in Norway. Initially, education considering the proper handling of fireworks and the use of safety goggles were propagated. These measures provided a non-significant effect on ocular injury. This led to a stricter legislation banning bottle rockets with the effect of reducing firework-inflicted trauma by half. International comparisons of the incidence of firework-inflicted trauma show that countries with stricter laws had 87% fewer ocular injuries than those with more liberal laws regarding the private use of fireworks.3
Because a significant portion of those with firework-inflicted injuries, particularly of those with severe injuries, are minors, strict laws regarding the use of fireworks can be expected to have a significant protective impact for this age group. Stricter laws cannot be compensated for by adult supervision as has been demonstrated repeatedly,1,2,4,19 especially because ocular firework-inflicted trauma often affects bystanders (47%).3 Chang et al.16 found spectators to be more likely to be affected by ocular injuries than by other injuries. In this study, however, data on the role of the patient was only available in about 28% of cases. Of these, 61% stated that they had been passive during the fireworks.
Conclusion
Our study contributes contemporary data on firework-induced ocular trauma in an urban metropolitan area where category F2 (formerly class II) pyrotechnical devices can be legally purchased by adults during 3 days of the year. Compared to other studies from Europe, we report a rather large number of treated patients around the New Year during a 4-year period. Minors seem to be at a higher risk for severe ocular trauma. In order to reduce the incidence of firework-inflicted trauma significantly, the German law that regulates the distribution and use of explosives could be modified to ban private fireworks at least in densely populated areas and especially in the vicinity of children.
Acknowledgments
The authors thank Florian Moerth, who helped clarify the details regarding German and EU legislation on pyrotechnical devices.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: The patients’ consent for publication of images used in this report was obtained.
ORCID iDs: Matthias A Lenglinger  https://orcid.org/0000-0001-7341-1570
https://orcid.org/0000-0001-7341-1570
Daniel Pilger  https://orcid.org/0000-0003-3397-8139
https://orcid.org/0000-0003-3397-8139
Daniel J Salchow  https://orcid.org/0000-0003-3678-6183
https://orcid.org/0000-0003-3678-6183
References
- 1. Smith GA, Knapp JF, Barnett TM, et al. The rockets’ red glare, the bombs bursting in air: fireworks-related injuries to children. Pediatrics 1996; 98(1): 1–9. [PubMed] [Google Scholar]
- 2. Kuhn F, Morris R, Witherspoon CD, et al. Serious fireworks-related eye injuries. Ophthalmic Epidemiol 2000; 7: 139–148. [PubMed] [Google Scholar]
- 3. Wisse RPL, Bijlsma WR, Stilma JS. Ocular firework trauma: a systematic review on incidence, severity, outcome and prevention. Br J Ophthalmol 2010; 94(12): 1586–1591. [DOI] [PubMed] [Google Scholar]
- 4. Sundelin K, Norrsell K. Eye injuries from fireworks in western Sweden. Acta Ophthalmol Scand 2000; 78(1): 61–64. [DOI] [PubMed] [Google Scholar]
- 5. Unterlauft J, Wiedemann P, Meier P. Bulbustraumata durch Feuerwerkskörper von 2005 bis 2013. Klin Monatsbl Augenheilkd 2014; 231: 915–920. [DOI] [PubMed] [Google Scholar]
- 6. Gesetz über explosionsgefährliche Stoffe (Sprengstoffgesetz—SprengG), www.gesetze-im-internet.de/sprengg_1976/BJNR027370976.html (2017, accessed 5 November 2019).
- 7. Erste Verordnung zum Sprengstoffgesetz (1. SprengV), www.gesetze-im-internet.de/sprengv_1/BJNR021410977.html (2017, accessed 5 November 2019).
- 8. Directive 2013/29/EU of the European Parliament and of the Council. J Eur Union 2013; 56: 27–65, https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2013:178:0027:0065:en:PDF [Google Scholar]
- 9. Bull N. Legislation as a tool to prevent firework-related eye injuries. Acta Ophthalmol 2011; 89(8): e654–e655. [DOI] [PubMed] [Google Scholar]
- 10. Chan WC, Knox FA, McGinnity FG, et al. Serious eye and adnexal injuries from fireworks in Northern Ireland before and after lifting of the firework ban: an ophthalmology unit’s experience. Int Ophthalmol 2004; 25(3): 167–169. [DOI] [PubMed] [Google Scholar]
- 11. Bach M, Schulze-Bonsel K, Feltgen N, et al. Author response: numerical imputation for low vision states [electronic letter]. Invest Ophthalmol Vis Sci 2007; 26. 10.1177/2474126416680670 [DOI] [Google Scholar]
- 12. Schulze-Bonsel K, Feltgen N, Burau H, et al. Visual acuities “hand motion” and “counting fingers” can be quantified with the Freiburg visual acuity test. Invest Ophthalmol Vis Sci 2006; 47: 1236–1240. [DOI] [PubMed] [Google Scholar]
- 13. Kuhn F, Morris R, Witherspoon CD, et al. A standardized classification of ocular trauma. Graefes Arch Clin Exp Ophthalmol 1996; 234: 399–403. [DOI] [PubMed] [Google Scholar]
- 14. Karlson TA, Klein BE. The incidence of acute hospital-treated eye injuries. Arch Ophthalmol 1986; 104(10): 1473–1476. [DOI] [PubMed] [Google Scholar]
- 15. Sacu S, Segur-Eltz N, Stenng K, et al. Ocular firework injuries at New Year’s Eve. Ophthalmologica 2002; 216(1): 55–59. [DOI] [PubMed] [Google Scholar]
- 16. Chang IT, Prendes MA, Tarbet KJ, et al. Ocular injuries from fireworks: the 11-year experience of a US level I trauma center. Eye 2016; 30(10): 1324–1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nijman S, Valkenberg H, Eikendal T. PW 1429 A complete picture of new year’s eves fireworks injuries at Dutch emergency departments. Inj Prev 2018; 24(Suppl. 2): A233. [Google Scholar]
- 18. Frimmel S, Theusinger O, Kniestedt C. Analysis of ocular firework-related injuries and common eye traumata: a 5-year clinical study. Klin Monbl Augenheilkd 2017; 234(4): 611–616. [DOI] [PubMed] [Google Scholar]
- 19. Jing Y, Yi-qiao X, Yan-ning Y, et al. Clinical analysis of firework-related ocular injuries during Spring Festival 2009. Graefes Arch Clin Exp Ophthalmol 2010; 248(3): 333–338. [DOI] [PubMed] [Google Scholar]



