Abstract
The study aimed to: a) Identify distinct trajectories of change in depressive symptoms by mid-treatment during psychotherapy for late-life depression with executive dysfunction; b) examine if non-response by mid-treatment predicted poor response at treatment end; c) identify baseline characteristics predicting an early non-response trajectory by mid-treatment. A sample of 221 adults 60 years and older with major depression and executive dysfunction were randomized to 12 weeks of either Problem-Solving Therapy or Supportive Therapy. We used Latent Growth Mixture Models (LGMM) to detect subgroups with distinct trajectories of change in depression by mid-treatment (6th week). We conducted regression analyses with LGMM subgroups as predictors of response at treatment end. We used random forest machine learning algorithms to identify baseline predictors of LGMM trajectories. We found that approximately 77.5% of participants had a declining trajectory of depression in weeks 0–6, while the remaining 22.5% had a persisting depression trajectory, with no treatment differences. The LGMM trajectories predicted remission and response at treatment end. A random forests model with high prediction accuracy (80%) showed that the strongest modifiable predictors of the persisting depression trajectory were low perceived social support, followed by high neuroticism, low treatment expectancy, and low perception of the therapist as accepting. Our results suggest that modifiable risk factors of early non-response to psychotherapy can be identified at the outset of treatment and addressed with targeted personalized interventions. Therapists may focus on increasing meaningful social interactions, addressing concerns related to treatment benefits, and creating a positive working relationship.
Introduction
Psychotherapy is an important part of the treatment armamentarium for late-life depression because it is well accepted by older adults and because intolerance of therapeutic dosages, modest efficacy, and drug interactions reduce the usefulness of antidepressants.1 Meta-analysis of psychotherapy studies in late-life depressive syndromes documented that psychotherapy and pharmacotherapy have comparable efficacy.2
More than 35% of patients with late-life depression have executive dysfunction.3 Clinical and neuroimaging studies suggest that executive dysfunction and its underlying pathophysiology predicts slow, poor, and unstable response of late-life depression to antidepressants,4,5 necessitating non-pharmacological treatments. The only available randomized controlled trial of psychotherapy in older adults with major depression and executive dysfunction documented that both Problem Solving Therapy (PST) and Supportive Therapy led to comparable improvement in depression and disability in the first 6 weeks of treatment.6,7 However, PST participants had a more prominent reduction of depression at weeks 9 and 12. Nonetheless, over 50% of patients with major depression did not respond to either therapy by treatment end.6
Responding to the need to increase the efficacy of psychotherapy for late-life depression with executive dysfunction, we focused on predictors of early response. Early response to psychotherapy predicts favorable long-term outcomes in depressed younger adults.8–10 Little is known about predictors of early response to psychotherapy in late-life depression and no studies exist in late-life depression with executive dysfunction. Detecting early risk factors of non-response may improve the efficacy of psychotherapy by informing the selection of targeted interventions.8,10
This study analyzed data of the COPE-D project, a two-site, randomized controlled trial, which compared the efficacy of 12 weekly sessions of PST with supportive therapy in older adults with major depression and executive dysfunction6,7 and had three aims. First, it sought to identify subgroups of depressed older patients with executive dysfunction with distinct trajectories of change in depressive symptoms by mid-treatment (six sessions). Second, it tested the hypotheses that, relative to participants with little improvement of depression by mid-treatment, participants with greater depression reduction by mid-treatment had higher remission and response rates and lower depression severity at treatment end. Third, it sought to identify baseline characteristics that predict membership to the subgroup of participants with a trajectory of minimal change in depression severity by mid-treatment. We used machine learning models because of their high sensitivity and replicability of findings and their ability to detect complex (non-linear) multidimensional interactions among predictors.11,12
Methods
Participants
The participants were recruited by Weill Cornell Medicine and the University of California at San Francisco (UCSF) between December 2002 and November 2007. The study was approved by the institutional review board of both institutions. Inclusion criteria were: a) Age of ≥ 60 years; b) Non-psychotic Major Depression by SCID-R)/DSM-IV13; c) 24-item Hamilton Depression Rating Scale (HAM-D)≥2014; d) Mini-Mental State Examination (MMSE)≥2415; e) Mattis Dementia Rating Scale Initiation/ Perseveration domain (DRS-IP) ≤3316; and f) Stroop Color-Word Test≤2517. Exclusion criteria were: a) Intent to attempt suicide in the near future; b) Current psychotherapy or psychopharmacological treatment; c) Axis I diagnosis other than unipolar depression or generalized anxiety disorder; d) antisocial personality disorder (by DSM-IV); e) dementia diagnosis by DSM-IV; f) history of head trauma; g) acute or severe medical illness; and h) inability to perform any activities of daily living even with assistance.
Measures
The primary outcome was depression severity, assessed weekly with HAM-D. Predictors were all continuous variables and included: (a) Disability [12-item World Health Organization Disability Assessment Schedule II (WHODAS-II)18)]; (b) cognitive impairment [Mini-Mental Status Exam (MMSE)15]; (c) executive functioning [Initiation Perseveration Domain of Mattis Dementia Rating Scale (DRS)]; (d) neuroticism [NEO; subscale of the Neuroticism, Extroversion, Openness Scale19]; (e) apathy [Apathy Evaluation Scale20]; (f) social support [4 subscales of the Duke Social Support Index21]; (g) treatment expectancy [4-item Treatment Rationale Scale22]; (h) quality of the therapeutic relationship [Client Perception of Therapist Scale (CPTS)23]; (i) Pain intensity [from the 36-Item Short-Form Health Survey (SF-36)24]; and (j) vascular profile [The Framingham Vascular Risk Profile Scale25]. Measures were administered by trained research assistants who were unaware of treatment condition and study hypotheses.
Treatments
Participants received 12 weekly sessions of either PST or supportive therapy (ST)7 by four doctorate-level clinical psychologists and four licensed social workers. Therapists demonstrated treatment fidelity and adherence to both treatment manuals.6,7
Problem-Solving Therapy (PST).
The first 5 weeks of therapy focused on training in a 5-step problem-solving model, teaching participants to set goals, develop ways to reach them, formulate action plans and assess their progress towards goals. The remaining sessions focused on enhancing the learned skills. The last two sessions focused on relapse prevention planning.
Supportive Therapy (ST).
Participants were encouraged to speak about their depression and contributing life events. Therapists assumed an empathetic therapeutic stance aiming to create a nonjudgmental environment and refrained from other specific theory-driven interventions.
Statistical Analysis
Trajectories of Depression from Baseline to Mid-treatment.
We utilized Latent Growth Mixture Models (LGMM)8,9,26 to discover latent subgroups with distinct trajectories of HAM-D change from baseline to mid-treatment (6th week). LGMM assumes that each individual belongs to one latent trajectory class based on their HAM-D trajectory. We fitted LGMM models with K (K=2 to 5) trajectories and selected the K with the minimum Bayesian Information Criterion (BIC). We calculated the 95% Bootstrap-t confidence intervals for slope from 1000 bootstrap samples.
Prediction of Response by Treatment End.
We conducted three regression analyses with LGMM subgroups as predictors of the 12th week outcomes: (a) HAM-D; (b) remission status (HAM-D ≤10); (c) response status (≥ 50% reduction in HAM-D from entry to week 12). The variance explained by each model was represented by adjusted R2 for the HAM-D comparison and by area under the curve (AUC) for logistic regression models for response and remission. We tested the association between LGMM trajectories and response outcomes in two ways – first, unadjusted using chi-square and independent two-sample t-tests and controlling the family wise error rate (FWER) at 5% for multiple comparisons using Holm’s step-down procedure; and second, adjusting for age, gender, treatment, site, and HAM-D score at baseline as covariates in a regression model.
Baseline Prediction of Response Trajectories with Random Forests.
We employed a machine learning algorithm, random forests, which considers complex interactions of baseline predictors. A random forest is an ensemble of classification trees that are fit on bootstrapped samples of data and predictions are averaged over all trees. A sequence of 500 to 5000 trees were grown to stabilize prediction error in a training set (75% of the sample; balanced for treatment condition). This allowed us to ensure that all predictors and all subjects have sufficient representation by growing a sufficiently large number of trees. We used the remaining 25% of data (test set) to estimate the overall prediction error of random forests using standard measures as prediction accuracy, specificity, sensitivity, positive and negative predictive values. The test set was held out from all aspects of training. We imputed missing values of predictors using proximity from random forest implemented with the ‘randomForest’ package in R. Since the random forest is a black-box algorithm, we rank the importance of each predictor using the Gini impurity index, a measure of the purity of each terminal node or leaf of a tree, averaged across all trees. It is higher when more observations in a leaf belong to one response class.
Prediction Model by a Classification Tree.
Although a random forests algorithm reduces the variance of the estimated prediction accuracy by averaging over multiple trees, it does not offer information on the contribution of each predictor. For that reason we employed a single classification tree, which yields a flow chart like structure that finds sub-groups by repeated splitting, where each split is based on a single predictor. Each subgroup is represented as a terminal node (‘leaf’) and the most frequent response trajectory class determines the subgroup’s predicted early-response trajectory. A limitation of the classification tree is its high variability across samples. To address this limitation, we picked the five strongest predictors of the random forests based on the Gini impurity index. We pruned the tree to avoid overfitting by restricting the minimum observations for each split to n=10.
Results
A total of 221 participants were randomly assigned to PST or ST. The CONSORT table and characteristics of participants were reported elsewhere.6
Trajectories of Early Response to Psychotherapy
LGMM analysis sought to identify distinct trajectories of depression severity during the first 6 weeks of treatment in the entire sample. We found two distinct linear trajectories (BIC= 8556.0; Figure 1), an early response trajectory with declining HAM-D by mid-treatment and an early non-response trajectory with a persisting severity of depression (HAM-D).The average posterior probabilities for membership in the response trajectories were 96.8% and 97.8% for each group. Out of the 218 participants, 169 participants (77.5%) had an early response trajectory with a linear trend over 6 weeks (estimate of slope = −0.33, 95% Bootstrap-t CI: −0.40, −0.32), whilethe remaining 22.5% had an early non-response trajectory showing minimal change of depression severity over 6 weeks (estimate of slope = −0.10, Bootstrap-t CI: −0.22, −0.06).Of the 169 participants in the early response trajectory subgroup, 50.3% had received PST.
Figure 1.
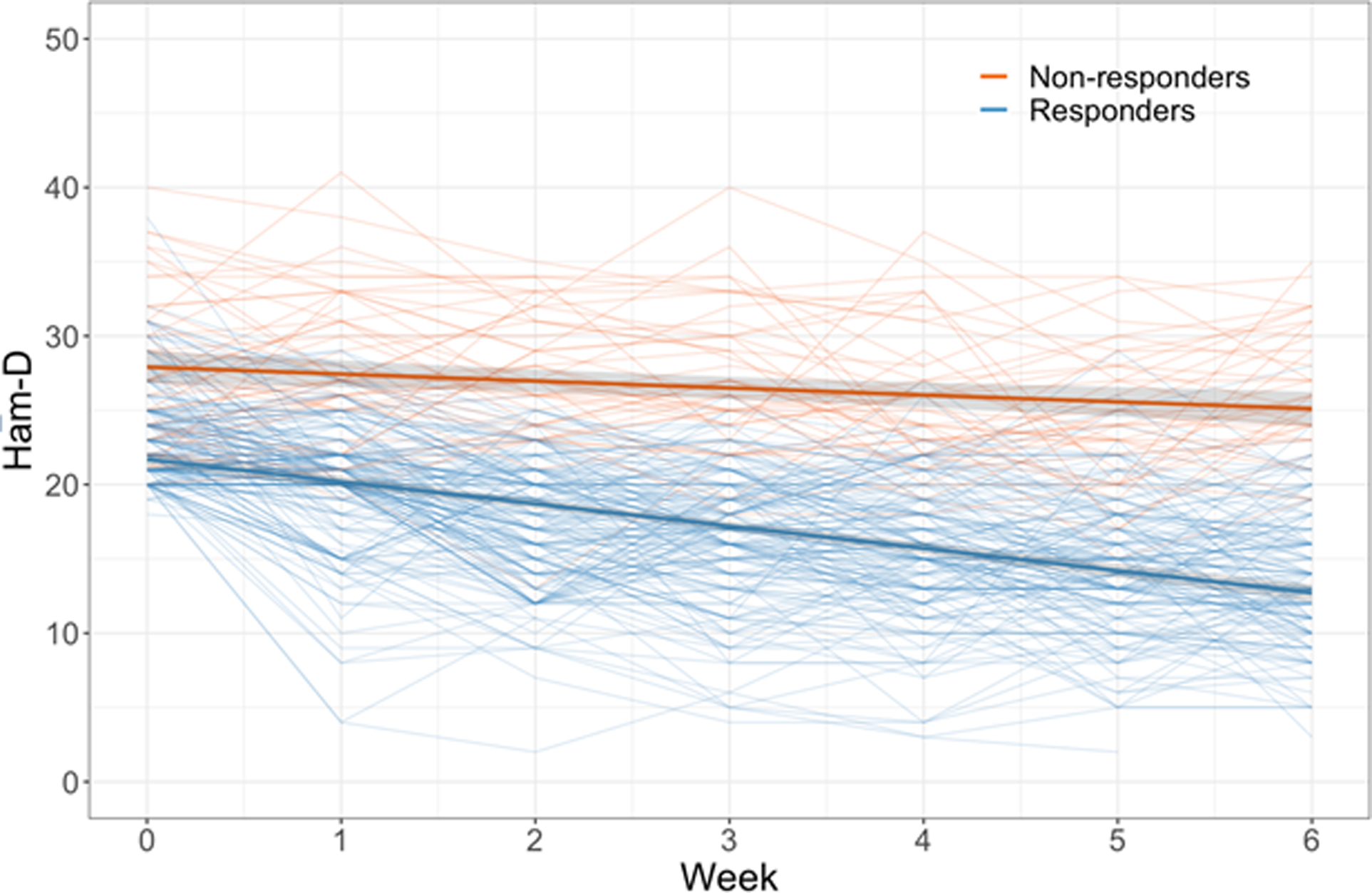
Latent Growth Mixture Model (LGMM) of estimated growth curves of depression severity from baseline to Week 6
Note. HAMD = 24-item Hamilton Depression Rating Scale. The Figure presents two LGMM trajectories of change over 6 weeks in 12-weeks of treatment, with 95% Confidence Intervals. Orange color represents early non-responders (22.5%). Blue color represents early responders (77.5%).
At baseline, participants with an early response trajectory had less severe depression than participants with a trajectory of early non-response (Table 1). They also had greater perceived social support, lower neuroticism, greater expectancy for treatment efficacy, and lower capacity to get along with others. Demographic variables (age, marital status, and ethnicity) or treatment condition were not significantly different across LGMM trajectories.
Table 1.
Clinical and demographic characteristics of members of Latent Growth Mixture Model (LGMM) classes of estimated growth curves of depression severity
| LGMM Class | |||||
|---|---|---|---|---|---|
| Variables of Interest | Early non-response 49 (22.5%) | Early response 169 (77.5%) | t/Chi-sq § | p-value | |
| 1. Sex (women N, %) | 32 (65.3%) | 112 (66.3%) | 0.00§ | 1 | |
| 2. Treatment (N, %) | 0.253§ | 0.615 | |||
| ST | 27 (55.1%) | 84 (49.7%) | |||
| 3. Age, years | 72.2 (8.56) | 73.3 (7.49) | −0.748 | 0.457 | |
| 4. Education, years | 15.2 (2.75) | 15.2 (2.81) | −0.037 | 0.971 | |
| 5. Number of Depressive Episodes | 2.4 (1.33) | 2.2 (2.4) | 0.713 | 0.477 | |
| 6. HAM-D Score at Baseline | 27.8 (5.08) | 23.3 (3.4) | 5.859 | < .001 | *** |
| 7. MMSE (Overall Cognitive Impairment) | 27.6 (1.69) | 27.9 (1.7) | −0.791 | 0.431 | |
| 8. DRS Initiation-Perseveration (Executive Dysfunction) | 31.3 (4.15) | 32.6 (3.37) | −1.932 | 0.058 | |
| DRS Attention | 44.7 (2.53) | 44.8 (2.14) | −0.417 | 0.678 | |
| DRS Memory | 31.5 (2.85) | 31.9 (2.63) | −0.911 | 0.366 | |
| DRS Construction | 11.2 (1.09) | 11.6 (0.79) | −2.185 | 0.033 | |
| DRS Conceptualization | 63.4 (3.55) | 63.3 (3.27) | 0.181 | 0.857 | |
| 9. Neuroticism (NEO) | 17.1 (4.93) | 14.4 (5.06) | 3.347 | 0.001 | ** |
| 10. Social Support Inventory (Duke) | |||||
| Perceived Support (Duke) | 12.8 (5.04) | 15.7 (4.1) | −3.656 | 0.001 | ** |
| Instrumental Support (Duke) | 17 (4.58) | 18.1 (3.89) | −1.547 | 0.126 | |
| Social Interaction (Duke) | 4.5 (2.77) | 5.2 (2.53) | −1.541 | 0.128 | |
| Social Network (Duke) | 1.8 (2.68) | 2.7 (3.28) | −1.833 | 0.070 | |
| 11. Disability (WHODAS-II) | |||||
| Getting around | 5.8 (2.46) | 5.3 (2.63) | 1.168 | 0.246 | |
| Self-care | 3.6 (1.95) | 2.9 (1.45) | 2.315 | 0.024 | |
| Getting along with Others | 4.3 (1.91) | 3.2 (1.49) | 3.599 | 0.001 | ** |
| Participation in Society | 6.2 (2.07) | 5.3 (1.78) | 2.879 | 0.005 | |
| Understanding & Communicating | 5.1 (1.89) | 4.2 (1.84) | 2.911 | 0.005 | |
| Life Activities | 4.2 (1.59) | 3.6 (1.34) | 1.985 | 0.053 | |
| 12. Pain (MOS) | |||||
| Pain Intensity | 1.8 (0.63) | 1.9 (0.69) | −0.426 | 0.671 | |
| Pain Interference with Activities | 2 (0.82) | 2.1 (0.76) | −0.986 | 0.328 | |
| 13. Vascular Profile Total | 0.9 (1.15) | 0.9 (1.09) | 0.132 | 0.896 | |
| 14. Apathy Evaluation Scale (AES) Total | 47.7 (8.86) | 51.4 (7.07) | −2.432 | 0.018 | |
| 15. Treatment Expectancy Scale | 25 (9.47) | 30.6 (8.82) | −3.675 | <.001 | ** |
| 16. Perception of Therapist (LORR) | |||||
| Understanding | 22.8 (9.47) | 24.8 (7.97) | −1.291 | 0.201 | |
| Accepting | 37.7 (15.79) | 41.8 (13.83) | −1.617 | 0.110 | |
| Critical | 10 (4.21) | 9.6 (2.91) | 0.526 | 0.601 | |
| Authoritarian | 13.6 (7.2) | 14.4 (7.34) | −0.655 | 0.514 | |
| Encouraging | 8.5 (5.21) | 8.4 (5.36) | 0.123 | 0.902 | |
Note. HAM-D = Hamilton Depression Rating Scale; MMSE = Mini Mental Status Exam; DRS = Mattis Dementia Rating Scale; LGGM = Latent Growth Mixture Model;
Numeric variables are presented with summary statistics of mean and standard deviation as well as test statistic from independent two-sample t-test. Categorical variables are presented with summary statistics of frequency and percentage as well as test statistic from chi-squared test;
p≤.1;
p≤.05;
p≤.001 after multiple comparison adjustment using family wise error rate (FWER).
Trajectories of Early Response and Prediction of Outcomes at Treatment End
Regression models examined the relationship of the early response/non-response LGMM trajectories and three outcomes at treatment end: a) HAM-D score at week 12; b) treatment response, i.e. 50% reduction of HAM-D from baseline to week 12; and c) remission (HAM-D ≤10 at week 12). The LGMM trajectories were significantly associated with these outcomes (Table 2). All participants with early non-response trajectories were also non-responders (i.e. did not achieve 50% reduction in symptom severity) at treatment end.
Table 2.
Association of LGMM classified early responders vs. early non-responders by mid-treatment (week 6) and outcome of depression at treatment end (week 12)
| Predictor | Outcome | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|---|
| Estimate/OR (95% CI) | p-value | R2/AUC§ | Estimate/OR(95% CI) | p-value | R2/AUC§ | ||
| Early response vs. early non-response classes | HAM-D score at week 12 | −12.27(−14.48, −10.06) | <.001 | 0.40 | −10.66(−13.13, −8.20) | <.001 | 0.45 |
| 50% Reduction (week 12 – baseline) | 10.48(3.94, 36.36) | <.001 | 0.65§ | 14.88 (4.82, 59.32) | <.001 | 0.75§ | |
| Remission (HAM-D ≤10 at week 12) | 15.87(4.62, 99.85) | <.001 | 0.65§ | 12.03 (3.24, 78.46) | 0.001 | 0.74§ | |
Note. HAM-D = Hamilton Depression Rating Sale; OR = Odds Ratio; AUC = Area Under the Curve. Early responders vs. early non-responders classified by LGMM are the predictors of each outcome at treatment. For the prediction of HAM-D at treatment end, a Gaussian regression model was fitted for HAM-D at week 6 and week 12 and the adjusted R2 is reported. Logistic regression model was fitted for the binary outcome variables response and remission and AUC in the ROC curve is reported. Adjusted models controlled for age, gender, treatment, site, and HAM-D score at baseline.
We conducted sensitivity analysis to assess the effects of missing data on the robustness of the association between early response trajectory subgroups and the remission (HAM-D<10) and response (50% HAM-D reduction) outcomes at treatment end. We fitted the models considering two extreme scenarios for the 33 participants with missing HAM-D scores at week 12: (a) Any individual with a missing HAM-D was considered a responder/remitter; (b) any individual with a missing HAM-D was considered a non-responder/non-remitter. The associations between LGMM trajectories and response/remission status at treatment end remained, and the results of regression models were not biased due to missing cases.
Predictors of the Early Response Trajectory: Machine Learning Models
Random Forests.
Severity of depression (HAM-D) at baseline was not introduced in the random forests model because baseline severity of depression was part of the LGMM model that classified the trajectories of depression severity. This model demonstrated overall high prediction accuracy (80.0%) of predicting the early response, sensitivity (66.7%), specificity (97.5%), positive predictive values (PPV; 83.3%) and negative predictive values (NPV; 79.6%). The model was well-calibrated (Brier score = 0.15). We ensured that our training and testing sets are balanced in distribution of responders and non-responders and overall clinical characteristics of patients included. Based on the relative reduction in the Gini Impurity Index, the strongest predictors of early response/non-response were perceived social support, followed by neuroticism, treatment expectancy, age, and perception of therapist as accepting (Figure 2). For an average early non-responder (averaged over all predictors), increasing perceived social support by one standard deviation from the mean increased the probability of early response by 11.8 % and 12% for PST and ST respectively. Similarly, increasing treatment expectancy scores by one standard deviation increased the probability of early response by 12.4% and 11.4% for PST and ST respectively. Lowering neuroticism by one standard deviation from the mean increased the probability of becoming an early responder by 4.8% and 5.2% for PST and ST, respectively.
Figure 2.
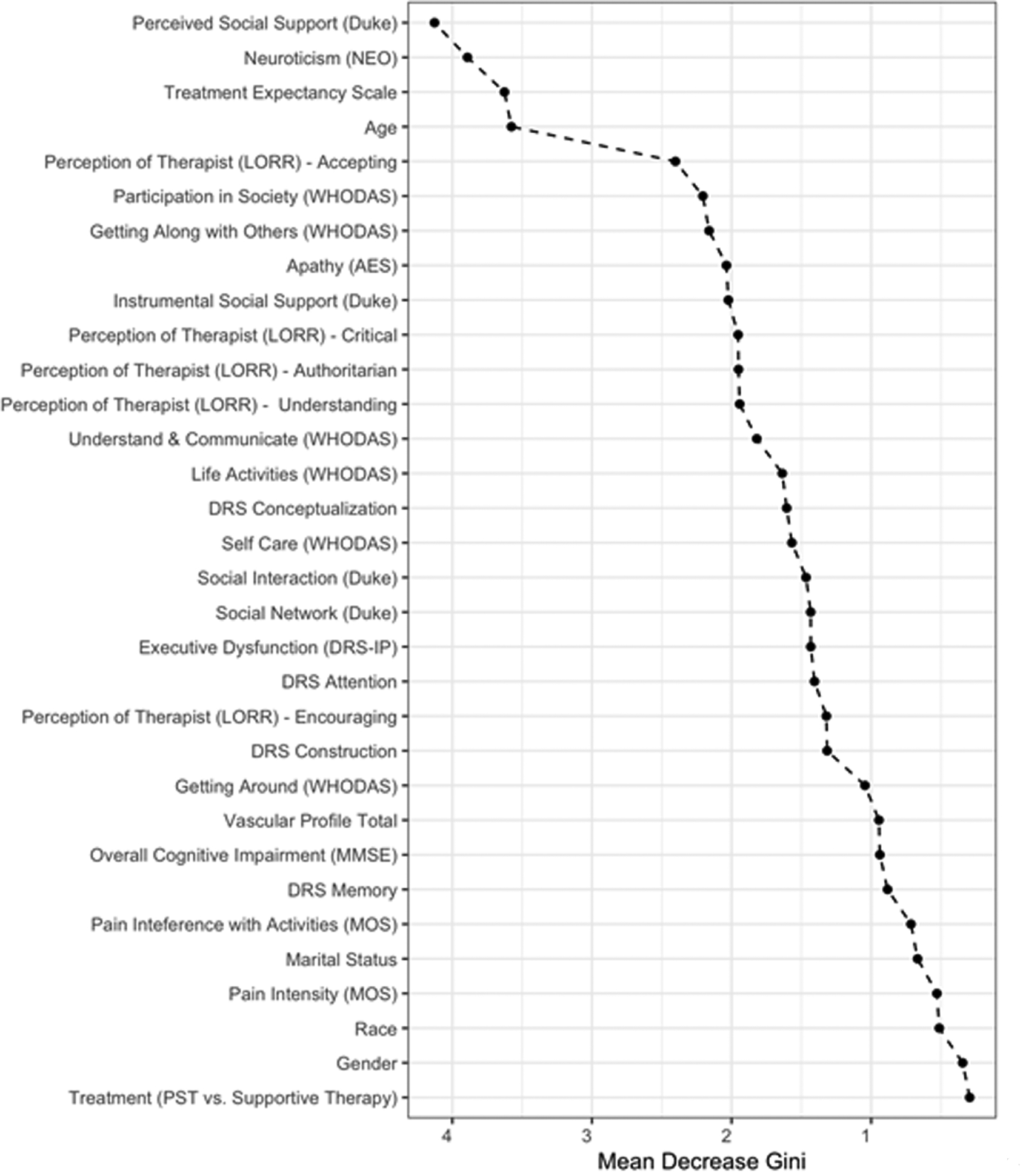
Variable importance in predicting membership in growth curves of depression severity (from baseline to week 6) estimated by random forests
Note. Predictors are presented from top to bottom in order of importance. The horizontal axis represents mean decrease in Gini Impurity Index (a weighted average of reduction in leaf node impurities
Classification Tree.
We constructed a classification tree using the three strongest predictors of early response of the random forest tree model. The classification tree highlights the probability of early-response in participants with combinations of these three predictors (Figure 3).
Figure 3.
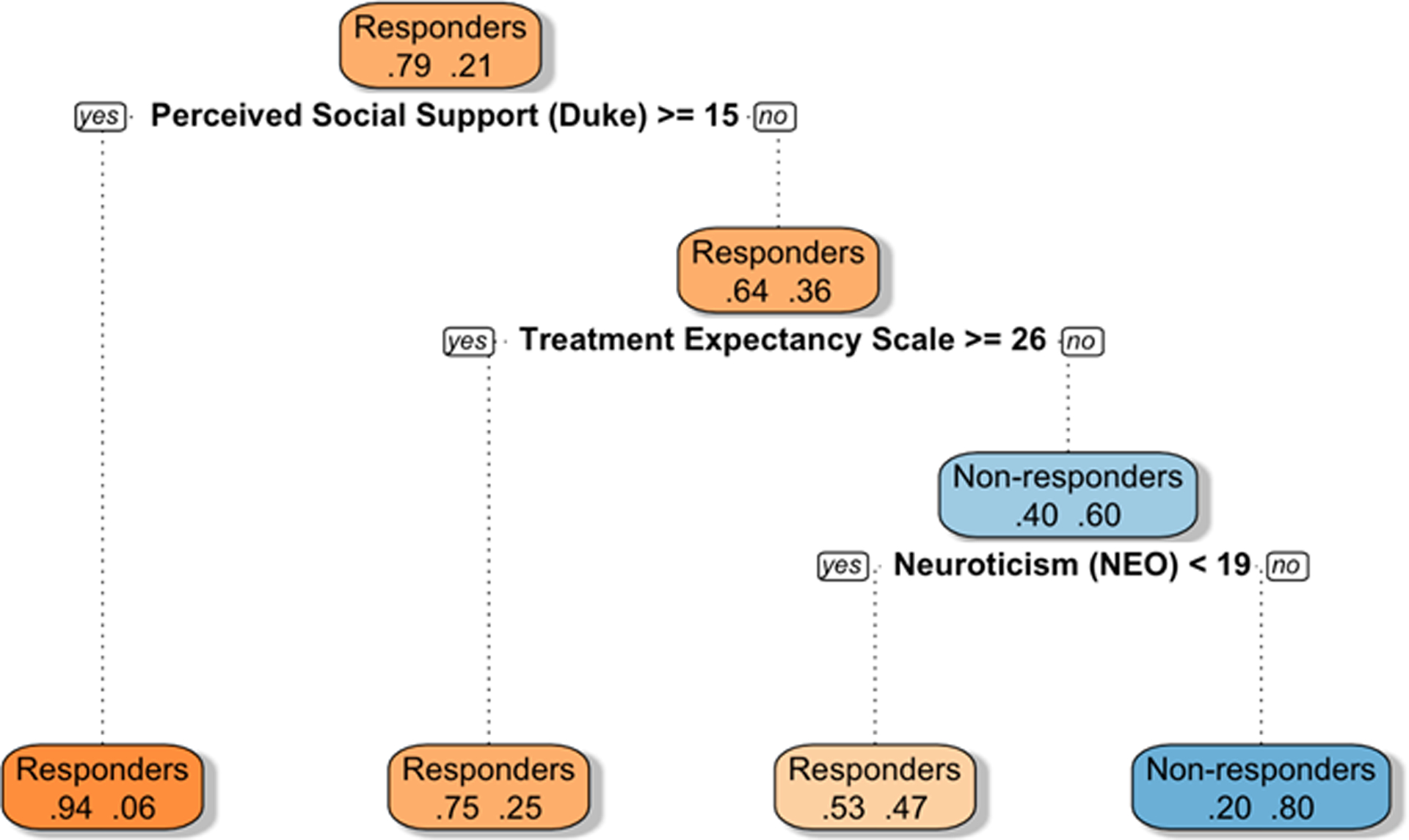
Single Interpretable Classification Tree
Note. The classification tree offers a clinical view of early response prediction. Probabilities of belonging to the right vs. left branch in the next split of the tree are presented within each box. Orange boxes signify higher probability to be an early responder and blue boxes signify a higher probability to be an early non-responder. Darker hues signify higher probability. Specifically, the top box indicates that 79% of participants, who had scores of perceived social support ≥15 had a 94% likelihood of being early responders. In contrast, 21% of participants of the top box had social support scores <15 and a lower overall likelihood to be early responders; among them, those with positive treatment expectancy scores ≥26 had a 75% probability of early response. Participants with social support scores <15 and treatment expectancy scores <26 still had a 53% probability of early response if their neuroticism score was below 19.
Discussion
Slow improvement of depression by the sixth session of psychotherapy predicts poor outcomes at treatment end (week 12) in older patients with major depression and executive dysfunction. High severity of depression, perceived low social support, neuroticism, low expectations of improvement, younger age, and the perception of therapist as less accepting were the strongest predictors of slow change of depression during the first six weeks of psychotherapy. Modifiable risk factors for poor response to psychotherapy may be targeted early in treatment with appropriately selected interventions and improve treatment outcomes
Low perceived social support was the strongest modifiable predictor of early risk of non-response to psychotherapy. The perception of low social support is a risk factor for development of late-life depression.27 Primary care patients who perceived their social relationships as unsupportive had less improvement of depression in response to psychosocial interventions than patients who perceived their environment as supportive.28 Low perceived social support may be due to depression-related cognitive distortions of the support by others or due to the true absence of positive social interactions. Engagement of depressed older adults in rewarding social interactions with significant others predicted increase in behavioral activation and reduction of depression during ‘Engage’, a reward exposure psychotherapy.29 Patients’ negative misperceptions can be addressed through simple cognitive interventions aimed to reduce negativity bias, common in late-life depression.30 Clinicians can also involve family members in treatment to facilitate social support and increase patients’ access to social activities available in the community.
Neuroticism also predicted early non-response to psychotherapy. High overall neuroticism is associated with increased risk for development of depression in older adults,31 and low remission rates during treatment with sertraline.32 Neuroticism is also associated with volume loss and hyper-metabolism in threat perception brain structures in adults.33
Negative treatment expectancy at the outset predicted minimal response by mid-treatment. This finding is consistent with the results of a meta-analysis, which included 8,016 patients, and documented that negative treatment expectancy is associated with unfavorable treatment outcomes.34 The relationship of therapist perception to early response to psychotherapy is in line with meta-analysis findings in depressed younger adults.35 It is also consistent with meta-analyses demonstrating that non-specific therapeutic components, such as the therapeutic relationship, are associated with treatment response across psychotherapies.36,37
The observation that early non-responders to psychotherapy have high severity of depression at baseline parallels findings of classical studies,38 although a recent meta-analysis did not confirm the relationship of severity of depression to psychotherapy response.39 Older age was a predictor of early response to psychotherapy, an observation consistent with findings showing that psychotherapy in older adults is at least as effective as in younger adults.39 The type of psychotherapy (PST vs. supportive therapy) was not significantly associated with early response. This is not surprising since our PST and supportive therapy treated participants had similar trajectories of depression decline until the 6th week of treatment but PST led to a sharper depression decline after that point.6
The classification tree of the strongest predictors of early response offers a nuanced clinical view of early response prediction (Figure 3). Depressed patients who perceived their relationships with others as supportive had a high probability of early response. Even among participants with low perceived social support, those with high treatment expectancy had a high probability of early response, especially if they had low neuroticism scores. Among participants with low perceived social support and low expectations for improvement, those with low neuroticism were likely to have an early response to psychotherapy.
The perception of social support, the patient’s expectations of therapy, and the patients’ view of their therapist are all modifiable clinical factors. Systematic exposure to rewarding interactions with significant others may reduce depressive symptoms.29 When needed, therapists may address behavioral and social skill deficits and cognitive factors that contribute to the perception or maintenance of unsatisfying levels of social support. These approaches have been shown to improve both the perception of social support and the experience of depressive symptoms.40 Reinforcing realistic, positive treatment expectancy and addressing negative views about therapy and its outcomes early in treatment may improve outcomes. Therapists may explore patient perceptions of the therapeutic relationship early in treatment and project an accepting attitude. Neuroticism is a trait leading to disproportional emotional responses to stressors. Even though neuroticism persists, its impact may be reduced through stress management approaches and mindfulness-based interventions.41
This study has several limitations. Therapists were trained and offered both PST and supportive therapy. This design might have introduced a therapist preference bias if therapists favored one of the two treatments. This bias was mitigated by selecting therapists without previous experience in either treatment, by offering training and by continuously monitoring treatment fidelity. Another limitation is the reliance on interviewer-rated measures for all variables of interest, with the exception of executive dysfunction. We acknowledge that objective and performance-based measures are preferable when available. Further, our sample was well educated (mean of 15 years), limiting the generalizability of our finding to this subpopulation. Missing data in 12-week outcomes and baseline predictors is a limitation of this study. However, sensitivity analyses suggested that patterns of missing data did not bias our results. Further, 91% of those who started treatment remained in treatment until the end of the trial. Our study focused on identifying predictors of response to PST and Supportive Therapy in depression accompanied by executive dysfunction. Lack of a comparable analysis in depressed older adults without executive dysfunction prevents any conclusion on the generalizability of our findings to late-life, major depression without executive dysfunction. The absence of a treatment effect in our study suggests that these predictors may be relevant to other psychotherapy models. However, future focused studies will be needed to empirically test this assertion. Similarly, future studies could investigate whether early modification of the predictors identified in this study improves treatment response. Additionally, our study focused on early risk of nonresponse. Future studies may expand this inquiry into predictors of relapse and recurrence after attainment of remission. Management of suicide risk is important with this vulnerable population. Exploratory analysis showed that random forest and classification tree with an outcome variable of the suicidal ideation item of the HAM-D at baseline identified 3 of our 5 predictors as most important: perceived social support (most important predictor), neuroticism, and perception of the therapist as accepting. Active suicidal ideation (i.e. plan or intent in the near future) was an exclusion criterion in this trial and, therefore, we focused our inquiry on depression severity as an outcome.
Finally, the random forest algorithm models complex non-linear relationships between predictors but renders an opaque prediction algorithm. For this reason, we have presented a clinically useful classification tree. While overfitting is a potential problem in sample sizes similar to ours, it may not have affected our results given the large number of patients compared to predictors in our random forests tree analysis and the large number of trees included and pruned in the classification tree.
In conclusion, we observed that a trajectory of depression non-response detected by week 6 predicts poor response at treatment end. Predictors of early non-response include severity of depression, low perceived social support, high neuroticism, low treatment expectancy, younger age and perception of the therapist as less accepting. Modifiable predictors identified early in therapy can be addressed with targeted interventions. Encouraging rewarding meaningful social interactions may increase the perception of social support. Emotion regulation, stress management, mindfulness, and anxiety reduction techniques may be helpful in patients with high neuroticism. Clarifying the mechanisms of treatment, conveying realistic optimism about treatment efficacy, assuming an accepting, non-critical stance, and facilitating a strong therapeutic relationship may address the remaining modifiable risk factors of early non-response and improve treatment outcomes.
Funding:
This research was funded by National Institute of Mental Health grants P50 MH113838, R01 MH064099, R01 MH063982, T32 MH019132, K23 MH123864 and the Sanchez Foundation.
Footnotes
Conflicts of Interest: Dr. Alexopoulos serves on the Eisai Advisory Board and Otsuka Speakers Bureau. He also served on the Speakers Bureaus of Allergan and Takeda-Lundbeck and Janssen Advisory Board. Thomas Hull is an employee of ‘Talk Space.’ All other authors report no conflicts.
References
- 1.Kok RM, Reynolds CF. Management of depression in older adults. JAMA. 2017;317(20):2114. doi: 10.1001/jama.2017.5706 [DOI] [PubMed] [Google Scholar]
- 2.Alexopoulos GS, Sirey JA, Banerjee S, Jackson DS, Kiosses DN, Pollari C, et al. Two interventions for patients with major depression and Severe Chronic Obstructive Pulmonary Disease: Impact on dyspnea-related disability. Am J Geriatr Psychiatry. 2018;26(2):162–171. doi: 10.1016/j.jagp.2017.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manning KJ, Steffens DC. State of the science of neural systems in late-life depression: Impact on clinical presentation and treatment outcome. J Am Geriatr Soc. 2018;66:17–23. doi: 10.1111/jgs.15353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manning KJ, Alexopoulos GS, Banerjee S, Morimoto SS, Seirup JK, Klimstra SA, et al. Executive functioning complaints and escitalopram treatment response in late-life depression. Am J Geriatr Psychiatry. 2015;23(5):440–445. doi: 10.1016/j.jagp.2013.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alexopoulos GS, Manning K, Kanellopoulos D, McGovern A, Seirup JK, Banerjee S, et al. Cognitive control, reward-related decision making and outcomes of late-life depression treated with an antidepressant. Psychol Med. 2015;45(14):3111–3120. doi: 10.1017/S0033291715001075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Areán PA, Raue P, Mackin RS, Kanellopoulos D, McCulloch C, Alexopoulos GS. Problem-Solving Therapy and Supportive Therapy in older adults with major depression and executive dysfunction. Am J Psychiatry. 2010;167(11):1391–1398. doi: 10.1176/appi.ajp.2010.09091327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alexopoulos GS, Raue PJ, Kiosses DN, Mackin RS, Kanellopoulos D, McCulloch C, et al. Problem-Solving Therapy and Supportive Therapy in older adults with major depression and executive dysfunction. Arch Gen Psychiatry. 2011;68(1):33. doi: 10.1001/archgenpsychiatry.2010.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelley ME, Dunlop BW, Nemeroff CB, Lori A, Carrillo-Roa T, Binder EB, et al. Response rate profiles for major depressive disorder: Characterizing early response and longitudinal nonresponse. Depress Anxiety. 2018;35:992–1000. doi: 10.1002/da.22832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis CC, Simons AD, Kim HK. The role of early symptom trajectories and pretreatment variables in predicting treatment response to cognitive behavioral therapy. J Consult Clin Psychol. 2012;80(4):525–534. doi: 10.1037/a0029131 [DOI] [PubMed] [Google Scholar]
- 10.Persons JB, Thomas C. Symptom severity at week 4 of Cognitive-Behavior Therapy predicts depression remission. Behav Ther. 2018;50(4):791–802. doi: 10.1016/J.BETH.2018.12.002 [DOI] [PubMed] [Google Scholar]
- 11.Chekroud AM, Zotti RJ, Shehzad Z, Gueorguieva R, Johnson MK, Trivedi H, et al. Cross-trial prediction of treatment outcome in depression: a machine learning approach. Lancet Psychiatry. 2016;3:243–250. doi: 10.1016/S2215-0366(15)00471-X [DOI] [PubMed] [Google Scholar]
- 12.Lee Y, Ragguett R-M, Mansur RB, Boutilier JJ, Rosenblat JD, Trevizol A, et al. Applications of machine learning algorithms to predict therapeutic outcomes in depression: A meta-analysis and systematic review. Published online 2018. doi: 10.1016/j.jad.2018.08.073 [DOI] [PubMed]
- 13.First B, Spitzer R, Williams J, et al. Structured Clinical Interview for DSM-IV - Patient Version (SCID-P). American Psychiatric Press; 1995. [Google Scholar]
- 14.Hamilton M A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Folstein M, Folstein S, McHugh P. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 16.Mattis S Dementia Rating Scale Professional Manual. Psychological Assessment Resources; 1988. doi: 10.4236/psych.2012.33032 [DOI]
- 17.Perret E The left frontal lobe of man and the suppression of habitual responses in verbal categorical behaviour. Neuropsychologia. 1974;12(3):323–330. doi: 10.1016/0028-3932(74)90047-5 [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. World Health Organization Disability Assessment Schedule (WHODAS II). WHO; 2000. [Google Scholar]
- 19.McCrae RR, John OP. An introduction to the five‐factor Model and its applications. J Pers. 1992;60(2):175–215. doi: 10.1111/j.1467-6494.1992.tb00970.x [DOI] [PubMed] [Google Scholar]
- 20.Marin RS, Biedrzycki RC, Firinciogullari S. Reliability and validity of the apathy evaluation scale. Psychiatry Res. 1991;38(2):143–162. doi: 10.1016/0165-1781(91)90040-V [DOI] [PubMed] [Google Scholar]
- 21.Koenig HG, Westlund RE, Linda George MK, Hughes DC, Blazer DG, Hybels C. Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics. 1993;34:61–69. doi: 10.1016/S0033-3182(93)71928-3 [DOI] [PubMed] [Google Scholar]
- 22.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry. 1972;3(4):257–260. doi: 10.1016/0005-7916(72)90045-6 [DOI] [Google Scholar]
- 23.Lorr M Client perceptions of therapists: A study of the therapeutic relation. J Consult Psychol. 1965;29(2):146–149. doi: 10.1037/h0021924 [DOI] [PubMed] [Google Scholar]
- 24.Mchorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. 1993;31(3):247–263. Accessed June 7, 2019. https://pdfs.semanticscholar.org/aa08/ac3c784705b96e2b6ae92b048642f9e67bda.pdf [DOI] [PubMed] [Google Scholar]
- 25.Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: A risk profile from the framingham study. Stroke. 1991;22:312–318. doi: 10.1161/01.STR.22.3.312 [DOI] [PubMed] [Google Scholar]
- 26.Proust-Lima C, Philipps V, Liquet B. Estimation of extended mixed models using latent classes and latent processes: the R package lcmm. Published online March 3, 2015. doi: 10.18637/jss.v078.i02 [DOI]
- 27.Schwarzbach M, Luppa M, Forstmeier S, König HH, Riedel-Heller SG. Social relations and depression in late life - A systematic review. Int J Geriatr Psychiatry. 2014;29(1):1–21. doi: 10.1002/gps.3971 [DOI] [PubMed] [Google Scholar]
- 28.Hallgren M, Lundin A, Tee FY, Burström B, Forsell Y. Somebody to lean on: Social relationships predict post-treatment depression severity in adults. Psychiatry Res. 2017;249:261–267. doi: 10.1016/j.psychres.2016.12.060 [DOI] [PubMed] [Google Scholar]
- 29.Solomonov N, Bress JN, Anne Sirey JA, Gunning FM, Flückiger C, Raue PJ, et al. Engagement in socially and interpersonally rewarding activities as a predictor of outcome in ‘Engage’ behavioral activation therapy for late-life depression. Am J Geriatr Psychiatry. 2019;27(6):571–578. doi: 10.1016/j.jagp.2018.12.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alexopoulos GS, Areán PA. A model for streamlining psychotherapy in the RDoC era: the example of “Engage”. Mol Psychiatry. 2014;19(1):14–19. doi: 10.1038/mp.2013.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kendler KS, Gatz M, Gardner CO, Pedersen NL. Personality and Major Depression. Arch Gen Psychiatry. 2006;63(10):1113. doi: 10.1001/archpsyc.63.10.1113 [DOI] [PubMed] [Google Scholar]
- 32.Steffens DC, Wu R, Grady JJ, Manning KJ. Presence of neuroticism and antidepressant remission rates in late-life depression: Results from the Neurobiology of Late-Life Depression (NBOLD) study. Int Psychogeriatrics. 2018;30(7):1069–1074. doi: 10.1017/S1041610217002551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kapogiannis D, Sutin A, Davatzikos C, Costa P, Resnick S. The five factors of personality and regional cortical variability in the baltimore longitudinal study of aging. Hum Brain Mapp. 2013;34(11):2829–2840. doi: 10.1002/hbm.22108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Constantino MJ, Arnkoff DB, Glass CR, Ametrano RM, Smith JZ. Expectations. J Clin Psychol. 2011;67(2):184–192. doi: 10.1002/jclp.20754 [DOI] [PubMed] [Google Scholar]
- 35.Flückiger C, Del Re AC, Wampold BE, Horvath AO. The alliance in adult psychotherapy: A meta-analytic synthesis. Psychotherapy. 2018;55(4):316–340. doi: 10.1037/pst0000172 [DOI] [PubMed] [Google Scholar]
- 36.Palpacuer C, Gallet L, Drapier D, Reymann JM, Falissard B, Naudet F. Specific and non-specific effects of psychotherapeutic interventions for depression: Results from a meta-analysis of 84 studies. J Psychiatr Res. 2017;87:95–104. doi: 10.1016/j.jpsychires.2016.12.015 [DOI] [PubMed] [Google Scholar]
- 37.Cuijpers P, Reijnders M, Huibers MJH. The role of common factors in psychotherapy outcomes. Annu Rev Clin Psychol. 2019;15(1):207–231. doi: 10.1146/annurev-clinpsy-050718-095424 [DOI] [PubMed] [Google Scholar]
- 38.Elkin I, Gibbons RD, Shea MT, Sotsky SM, Watkins JT, Pilkonis PA, et al. Initial severity and differential treatment outcome in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol. 1995;63(5):841–847. doi: 10.1037/0022-006X.63.5.841 [DOI] [PubMed] [Google Scholar]
- 39.Cuijpers P, Andersson G, Donker T, Van Straten A. Psychological treatment of depression: Results of a series of meta-analyses. Nord J Psychiatry. 2011;65(6):354–364. doi: 10.3109/08039488.2011.596570 [DOI] [PubMed] [Google Scholar]
- 40.Cowan MJ, Freedland KE, Burg MM, Saab PG, Youngblood ME, Cornell CE, et al. Predictors of treatment response for depression and inadequate social support - The ENRICHD randomized clinical trial. Psychother Psychosom. 2007;77(1):27–37. doi: 10.1159/000110057 [DOI] [PubMed] [Google Scholar]
- 41.Armstrong L, Rimes KA. Mindfulness-Based Cognitive Therapy for neuroticism (stress vulnerability): A pilot randomized study. Behav Ther. 2016;47(3):287–298. doi: 10.1016/j.beth.2015.12.005 [DOI] [PubMed] [Google Scholar]


