Abstract
As the worst global pandemic of the past century, coronavirus disease 2019 (COVID-19) has had a disproportionate effect on maintenance dialysis patients and their health care providers. At a virtual roundtable on June 12, 2020, Dialysis Outcomes and Practice Patterns Study (DOPPS) investigators from 15 countries in Asia, Europe, and the Americas described and compared the effects of COVID-19 on dialysis care, with recent updates added. Most striking is the huge difference in risk to dialysis patients and staff across the world. Per-population cases and deaths among dialysis patients vary more than 100-fold across participating countries, mirroring burden in the general population. International data indicate that the case-fatality ratio remains at 10% to 30% among dialysis patients, confirming the gravity of infection, and that cases are much more common among in-center than home dialysis patients. This latter finding merits urgent study because in-center patients often have greater community exposure, and in-center transmission may be uncommon under optimal protocols. Greater telemedicine use is a welcome change here to stay, and our community needs to improve emergency planning and protect dialysis staff from the next pandemic. Finally, the pandemic’s challenges have prompted widespread partnering and innovation in kidney care and research that must be sustained after this global health crisis.
Index Words: COVID-19, dialysis, risk, international, DOPPS
Introduction
First identified in Wuhan, China, in late 2019, the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the cause of the worst global pandemic in our lifetimes. To better understand the impact of coronavirus disease 2019 (COVID-19) on dialysis patients globally, we hosted a virtual roundtable on June 12, 2020, with Dialysis Outcomes and Practice Patterns Study (DOPPS) investigators around the world to capture their early pandemic experiences, both objective and personal. This report summarizes presentations from 15 countries in Asia, Europe, and the Americas, along with updates based on more recent impressions and the most current epidemiologic data.
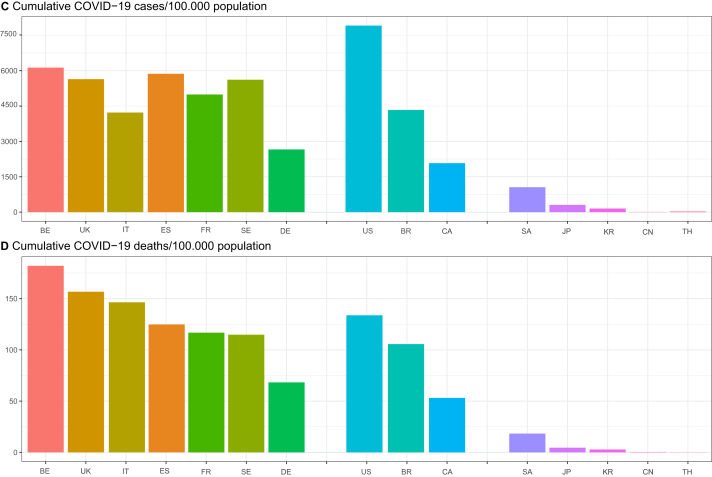
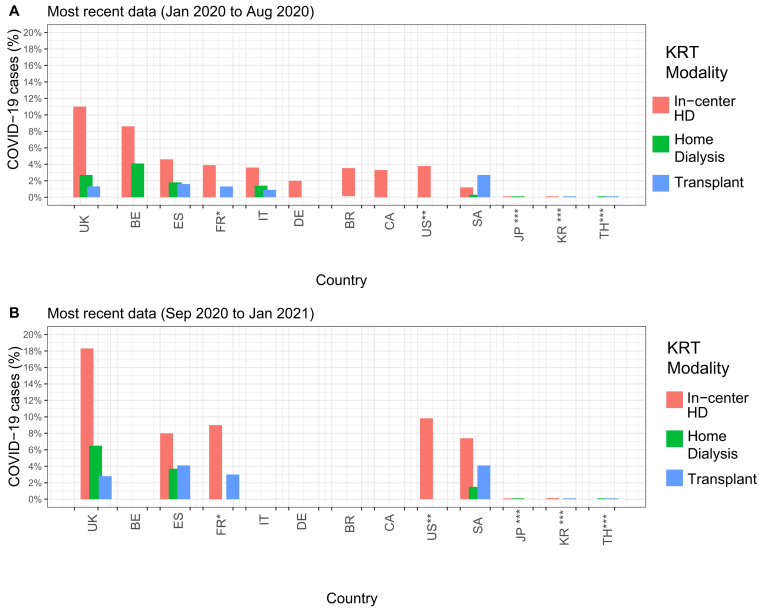
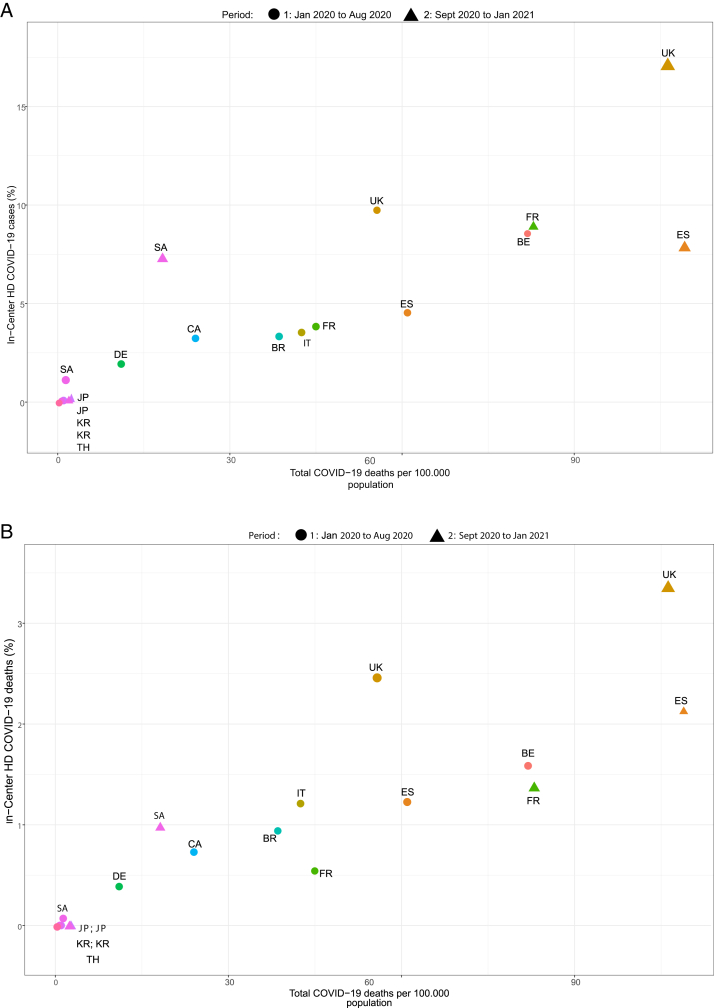
The impact of COVID-19 has varied dramatically, with cases and deaths in the general population varying more than 100-fold across participating countries (Fig 1).1 Our panelists summarized national data for dialysis populations based on registry reports, claims-based reports, or society surveys (Fig 2; Table 12, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16) and contextualized these findings.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13,17 Predictably but sobering, per-population cases and deaths among dialysis patients vary by 10- to 100-fold, as in the general population (Fig 3). Common across countries, published center and regional experiences report lower infection risk among home dialysis patients but also confirm that outcomes among infected persons are poor for both home and in-center dialysis patients, with case-fatality ratios of at least 1 in 10 for persons diagnosed using targeted testing.
Figure 1.
Coronavirus disease 2019 (COVID-19) cases and deaths in general population, by participating country. Peak cases per day, per 100,000 population for (A) January to August 2020 and (B) September 2020 to January 2021. (C) Cumulative cases, per 100,000 population (as of January 31, 2021). (D) Cumulative deaths, per 100,000 population (as of January 31, 2021). Abbreviations: BE, Belgium (A: April 15, 2020; B: October 29, 2020); BR, Brazil (A: July 29, 2020; B: January 7, 2021); CA, Canada (A: April 5, 2020; B: January 3, 2021); CN, China (A: February 13, 2020; B: January 21, 2021); DE, Germany (A: March 27, 2020; B: December 30, 2020); ES, Spain (A: August 31, 2020; B: January 25, 2021); FR, France (A: April 12, 2020; B: November 2, 2020); IT, Italy (A: March 21, 2020; B: November 13, 2020); JP, Japan (A: July 30, 2020; B: January 8, 2021); KR, South Korea (A: March 3, 2020; B: December 24, 2020); SA, Saudi Arabia (A: June 17, 2020; B: September 1, 2020); SE, Sweden (A: June 14, 2020; B: December 29, 2020); TH, Thailand (A: March 22, 2020; B: January 29, 2021); UK, United Kingdom (A: April 2, 2020; B: January 8, 2021); US, United States (A: July 16, 2020; B: January 2, 2021). Source: Our World in Data.1
Figure 2.
Proportion of coronavirus disease 2019 (COVID-19) cases among kidney replacement therapy (KRT) patients, by modality. Most recent data as of: (A) August 31, 2020, and (B) January 31, 2021. Data are from Table 1. Red bar indicates in-center hemodialysis (HD) except (∗) all dialysis for France (FR) and (∗∗) all KRT for United States (US). Abbreviations: BE, Belgium; BR, Brazil; CA, Canada; DE, Germany; ES, Spain; IT, Italy; JP, Japan; KR, South Korea; SA, Saudi Arabia; TH, Thailand; UK, United Kingdom.
Table 1.
Confirmed COVID-19 Cases and Case-Fatality Ratios Among Patients Receiving Kidney Replacement Therapy, by Participating Country
| No. of KRT Patients (% in-center HD, home dialysis, transplant)a |
Date for COVID-19 Data |
Cases by KRT Modalityb |
Case-Fatality Ratio by KRT Modality |
Source of COVID-19 Data; Comments | |||||
|---|---|---|---|---|---|---|---|---|---|
| In-center HD | Home Dialysis | Transplant | In-center HD | Home Dialysis | Transplant | ||||
| Europe | |||||||||
| Belgium | 14,797 (51%, 5%, 44%) | 5/31/20 | 8.6% | 4.1% | — | 18.6% | 10% | – | Groupement de Néphrologues Francophones de Belgique Registry2 |
| United Kingdom | 66,612 (37%, 7%, 56%) | 6/3/20 | 9.8% | 2.5% | 1.2% | 25.3% | 41.2% | 27% | UK Renal Registry3 |
| 12/29/20 | 17.3% | 6% | 2.7% | 19.6% | 22.5% | 16.8% | |||
| Spain | 61,764 (40%, 5%, 55%) | 7/4/20 | 4.6% | 1.8% | 1.6% | 27% | 21% | 24% | Spanish Society of Nephrology Registry4 |
| 1/2/21 | 8% | PD 3.7%/HHD 4.3% | 4.1% | 26.7% | PD 23.4%/HHD 12.5% | 19.6% | |||
| Italy | 60,441c (51%, 7%, 42%) | 4/23/20 | 3.6% | 1.4% | 0.9% | 34% | 46% | 25% | Italian Society of Nephrology COVID Survey5,6 |
| France | 87,275 (51%, 4%, 45%) | 7/8/20 | 3.9% (all dialysis) | — | 1.3% | 14.2% (all dialysis) | — | 19% | Renal Epidemiology and Information Network Registry7 |
| 12/2/20 | 9.0% (all dialysis) | — | 3.0% | 15.0% | — | 14.0% | |||
| Germany | — | 5/24/20 | 2% | — | — | 20% | — | — | German Covid-19 Dialysis Registry; preliminary data from 14,000 patients8 |
| Americas | |||||||||
| United States | 733,010 (63%, 8%, 29%) | 6/11/20 | 3.8% (all KRT) | — | — | 24.9%d | — | — | Cases from Medicare preliminary COVID-19 data snapshot report, shown for Medicare-only patients9 |
| 11/21/20 | 9.8% (all KRT) | — | |||||||
| Canada | 37,647 (44%, 14%, 42%) | 7/9/20 | 3.3% | — | — | 22.5% | — | — | COVID-19 data for Ontario and Quebec only; cases were <0.1% in other provinces. Sources: Ontario: Ontario Renal Reporting System and Ontario Renal Network. Quebec: author communication with medical directors |
| Brazil | 133,500 (92%, 8%, —) | 7/30/20 | 3.4% | 28% | National survey by Brazilian Society of Nephrology and Brazilian Association of Dialysis and Transplant Centers10) | ||||
| Asiab | |||||||||
| Saudi Arabia | 27,599 (64%, 5%, 31%) | 7/21/20 | 1.2% | 0.3% | 2.7% | 7.0% | 0% | 4.8% | Author communication with Saudi Center for Organ Transplantation (Alghonaim, February 2021) |
| 12/31/20 | 7.4% | 1.5% | 4.1% | 13.4% | 10% | 7.3% | |||
| Japan | 372,508 (95%, 3%, 2%) | 8/7/20 | <0.1% (158 cases) | <0.1% (2 cases) | — | 14% (22 deaths) | 0% | — | Japanese Association of Dialysis Physicians11 |
| 12/25/20 | 0.1% (513 cases) | 0.1% (9 cases) | — | 13.3% (68 deaths) | 33.3% (3 deaths) | — | |||
| Korea | 108,873 (75%, 6%, 19%) | 7/5/20 | <0.1% (23 cases) | 0% (no cases) | <0.1% (6 cases) | 13% (3 deaths) | No cases | 1 death | Korean Society of Nephrology COVID-19 Task Force Team (www.ksn.or.kr) and Korea Disease Control and Prevention Agency12,13 |
| 1/8/21 | 0.13% (107 cases) | 0% (no cases) | <0.1% (6 cases) | 8 (9 deaths) | No cases | 1 death | |||
| Thailand | 99,760 (68%, 27%, 5%) | 7/12/20 | 0% (no cases) | <0.1% (1 case) | <0.1% (3 cases) | No cases | 1 death | 0% | Author communication with Nephrology Society of Thailand(Adisorn Lampaopong, MD) and Thai Transplantation Society (Natavudh Townamchai, MD), January 2021 |
| 1/31/21 | 0% (no cases) | <0.1% (1 case) | <0.1% (4 cases) | No cases | 1 death | 1 death | |||
Note: For each country, most recent data from January 2020 to August 2020 are provided in first row; if available, most recent data from September 2020 to January 2021 are provided in second row. Data not available for cells with “—”. Countries not shown: Sweden (national data collection underway by the Swedish Renal Registry) and China (national data not available; see text for regional publications).
Abbreviations: COVID-19, coronavirus 2019; HD, hemodialysis; HHD, home hemodialysis; KRT, kidney replacement therapy; PD, peritoneal dialysis.
Number (modality) of KRT patients from US Renal Data System 2018 Annual Data Report,14 except Italy5 and Korea.15
If <1%, number of cases is provided; cases by KRT modality are also shown in Fig 2.
Number of patients at sites responding to the COVID-19 Survey, comprising 90% of KRT patients in Italy.5
National data not available for case-fatality ratio in United States; case-fatality ratio of 24.9% was among 438 patients with COVID-19 infection at a mid-size national dialysis provider (as of June 1, 2020).16
Figure 3.
Cumulative coronavirus disease 2019 (COVID-19) (A) cases and (B) deaths (as percent of all dialysis patients) by cumulative deaths per 100,000 in general population. Dialysis data are shown for in-center hemodialysis (HD) patients except for France (FR; all dialysis patients) and United States (US; all kidney replacement therapy patients). Population data are as of date of dialysis data. Abbreviations: BE, Belgium (1: May 2020); BR, Brazil (1: July 2020); CA, Canada (1: July 2020); DE, Germany (1: July 2020); ES, Spain (1: July 2020; 2: January 2021); FR (1: July 2020; 2: December 2020); IT: Italy (1: April 2020); JP, Japan (1: August 2020; 2: December 2020); KR: South Korea (1: July 2020; 2: January 2021); SA, Saudi Arabia (1: July 2020; 2: December 2020); TH, Thailand (1: June 2020); UK, United Kingdom (1: June 2020; 2: December 2020); US (1: July 2020; 2: November 2020). Source: Table 1 (dialysis data) and Our World in Data (population data).1
Now over 1 year into this pandemic and with vaccination providing the real hope for eventual containment, the picture emerging from the early pandemic period is of dialysis staff working courageously, even heroically, to keep patients safe and cared for, and of dialysis patients doing their utmost to reduce their infection risk. Lessons learned from these extraordinary circumstances have been adopted quickly, with our community functioning in many ways as a higher-level learning health system,18 sharing information, partnering, and issuing interim guidance at speeds and across divides as never before.19, 20, 21, 22 Despite these commendable achievements, the pandemic provides stark illustration that the dialysis community is inexorably linked to society, beholden to circumstances outside our control. In parts of the world, dialysis patients and staff have remained generally shielded by effectively adopted public health prevention and containment measures while in others, the most scrupulous attention at the dialysis clinic cannot overcome the impact of uncontained community spread on patients with kidney failure, among those at very highest risk from the scourge of COVID-19.
National Experiences
Asia
On a per-population basis, the number of COVID-19 cases and deaths has to date been strikingly lower in many Asian countries than elsewhere. Especially impressive, we see this trend across diverse cultures, geographies, and country income groups across the continent. Box 123 provides panelists’ impressions of some reasons for success in countries that have limited the spread of COVID-19 infection in the general population.
Box 1. Panelists’ Impressions of Some Reasons for Success in Countries With Relatively Less Spread of COVID-19 in the General Population.
Europe
Germany
-
•
The federally organized German health care system mandates reporting for proven or serious suspected SARS-CoV-2 cases
-
•
Local authorities have run contact tracing programs since very early in the pandemic
-
•
The Robert Koch Institute (Germany’s public health institute)23 issues case reporting contact risk stratification at the local level, enabling health care operations to adjust accordingly while maintaining efficient operations
Americas
Canada
-
•
The government quickly closed the border to all foreign nationals and all provinces declared States of Emergency, closing schools and nonessential businesses and enforcing physical distancing measures
-
•
Public and private in-home gatherings were prohibited
-
•
Mask wearing, although initially not mandatory, was practiced by government officials and most of the population in public spaces
-
•
Messaging from all levels of government was repeated, authoritative, and generally consistent
Asia
Japan
-
•
Strict preventive practices were implemented quickly, including the expectation for all to wash hands, wear masks, socially distance, and stay home as much as possible
-
•
These practices generally align with deeply rooted Japanese cultural practices, such as very little “skinship” (hugging or shaking hands) and not wearing shoes in the house, and have been closely followed
Korea
-
•
RT-PCR use has been widespread since early in the pandemic (1 million tests as of June 11), and drive-thru screening centers were quickly set up
-
•
Contact tracing has been scrupulous from the start
-
•
Asymptomatic or mild cases of COVID-19 were isolated in therapeutic living centers; this limited spread and avoided acute shortages of hospital beds
Thailand
-
•
The Thai government deployed a “soft” lockdown, securing the country border, stopping international and interprovincial transports, executing a night curfew, and shutting nonessential establishments
-
•
Public campaigns promoting hygienic practices were implemented to wear face masks, observe social distancing, and stay at home, bolstered by millions of grassroots volunteers and media support
-
•
Coercive measures included contact tracing, quarantining suspected cases, and confining international travelers in state quarantine centers
Abbreviations: COVID-19, coronavirus disease 2019; RT-PCR, reverse transcriptase-polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
China (Liangying Gan, Beijing)
SARS-CoV-2 emerged in Wuhan, China, in late 2019, and comprehensive control measures were implemented rapidly.24 Algorithms launched in January 2020 for all hemodialysis (HD) patients included screening using computed tomography of the chest because results were faster and potentially more sensitive for early disease than reverse transcriptase-polymerase chain reaction (RT-PCR). As of March 2020, a total of 154 of 7,154 (2.2%) patients from all 65 centers in Wuhan had SARS-CoV-2 infection by RT-PCR.25 Of these, 82% had an abnormality on computed tomography of the chest, 21% were asymptomatic, and 19% were severely or critically ill. Deaths were not reported. Among 818 peritoneal dialysis (PD) patients in Wuhan, 8 had COVID-19 diagnosed, with 2 deaths.26 The outbreak in Wuhan dialysis units declined sharply after late January 2020.
Early in the COVID-19 pandemic, several Chinese associations published recommendations for dialysis centers across the nation27,28 that most facilities implemented quickly. Screening of in-center HD patients in Hubei (outside Wuhan) and Guangdong provinces indicated SARS-CoV-2 seropositivity of 3.3% as of March 2020, with >95% asymptomatic.29 Here in Beijing, diagnosed SARS-CoV-2 infection in dialysis patients has been rare. Our center implemented strict infection control measures in mid-January 2020. Although it was diagnosed in 1 of our HD patients 18 days after symptom onset in February, no contacts in the dialysis unit developed COVID-19 infection. Measures were strengthened further, dialysis shifts were modified to isolate possible COVID-19 cases, and terminal disinfection was performed after each dialysis shift. To our knowledge, there have been no documented new cases among dialysis patients in Beijing. Though successful, staffing and resources are strained and we look forward to returning to normal conditions after the pandemic has passed.
Japan (Kazuhiko Tsuruya, Nara)
Japan has had success to date controlling SARS-CoV-2 infection. We have had waves in the general population in April 2020, in August 2020, and somewhat larger since late December 2020. The low penetrance of COVID-19 infection in Japan has been attributed to strict preventive strategies that align well with deeply rooted Japanese cultural practices (Box 1).
Among patients undergoing dialysis, there were 522 documented cases of SARS-CoV-2 infection as of December 2020 despite having one of the world's largest dialysis populations.11 Academic and professional societies involved in dialysis therapy quickly proposed strategies and recommendations for the prevention and management of COVID-19 infection.23 This guidance is generally aligned with best practices elsewhere and has been strictly followed.
Korea (Yong-Lim Kim, Daegu)
In Korea, new cases peaked at the end of February 2020 and again in the middle of December 2020. From the start, screening, case isolation, and contact tracing were adopted rapidly and widely (Box 1). All in all, success has been achieved despite no border shutdown or travel restriction. The impact on society and the economy has been profound but less than feared. Daegu, with a 2.5 million metropolitan population, was the original COVID-19 epicenter in Korea, with 0.3% prevalence and 2.5% case-fatality ratio in the general population. The first patient with COVID-19 infection receiving in-center HD on February 19, 2020, resulted in 302 people placed on contact isolation.30 From the earliest days, most HD centers educated patients to self-assess for symptoms before arriving for dialysis. Symptomatic patients were tested immediately by RT-PCR. Confirmed cases were transferred to an HD center with a negative pressure room. Close contacts with negative test results were isolated for 2 weeks and dialyzed in cohorted sessions. To date, case load has been low in Daegu and across Korea, and no PD patients have been infected (Table 1).
Thailand (Talerngsak Kanjanabuch, Bangkok)
Thailand was one of the first countries outside China with a confirmed SARS-CoV-2 case, in mid-January 2020. Containment policies (Box 1) were implemented rapidly and successfully. Compliance was high because traffic density was 15% to 20% less than usual, with 95% face mask and 89% hand sanitizer use.31,32 To date, there has been only 1 documented case (who died) among a Thai dialysis population of approximately 100,000.33 Recommendations from health authorities and kidney organizations were disseminated in April 2020. Among these, health care providers are expected to use telemedicine to monitor patients’ health and keep patients informed about the latest safety guidance. The lesson to date from Thailand has been that voluntary compliance by nearly all citizens and voluntary service of grassroots public health activists cooperating with a large cadre of health authorities can effectively contain this pandemic, at the same time protecting our patients with kidney failure. Efforts are now focused on combatting the country’s second wave, which began in late December 2020.
Saudi Arabia (Mohammed Alghonaim, Riyadh)
Saudi Arabia confirmed its first SARS-CoV-2 case on March 2, 2020, later than many countries. The number of known cases and fatalities increased sharply through summer 2020, attributed to increased screening toward a 40% population target. Cases have been lower since, without a steep second wave to date. A total of 472 dialysis staff have tested positive, with no deaths (author communication with Saudi Center for Organ Transplantation, Alghonaim, February 2021). Our experience since 2012 with the Middle East respiratory syndrome coronavirus epidemic has helped prepare for COVID-19. Infection control measures introduced then are now applied with heightened vigilance. Visual (“eyeball”) triage is done in all dialysis centers, with some adding twice-weekly home triage calls. Waiting areas have been eliminated, and universal personal protective measures are mandatory. These measures will likely continue after the pandemic is over.
Europe
Many European countries, along with their dialysis patients and staff, experienced the brunt of the early pandemic in the first months of 2020 (Fig 1).34 In most Western European countries, containment of COVID-19 infection improved before a second large wave hit late in 2020.
Belgium (Laura Labriola, Brussels)
The first Belgian case of COVID-19 was diagnosed on February 4, 2020, with lockdown on March 18, peak on April 7, 2020, and then exponential decline. On the French-speaking side,2 almost all dialysis units had cases and a few had large outbreaks involving 19% to 65% of patients. Aggressive detection and case isolation policies, coupled with systematic mask use, were introduced early in our unit and others. Many HD units had infected staff, with some in-unit contamination likely despite personal protective equipment use. Continuity of care was maintained in all facilities without designating COVID-19–only units, although this proved challenging in units with large outbreaks.
France (Pablo Urena Torres, Saint Ouen)
France was hard hit early on by COVID-19.7 At the AURA Nord dialysis center, we saw the first COVID-19–infected patient on March 16, 2020, a young man who was admitted to intensive care and died 6 weeks later. Our cases peaked at the end of March 2020, decreasing thereafter with the last on April 22, 2020. Overall, 35 of our 260 (13%) HD patients were infected, with 20 hospitalized and 3 deaths. Among our 15 home HD patients, 2 were diagnosed retrospectively by positive SARS-CoV-2 serology tests. To control the pandemic, we isolated cases suspected or confirmed by RT-PCR or computed tomography of the chest, and 3 of our 12 dialysis shifts became COVID-19 shifts. Our infection containment measures were successful overall despite resource constraints. Following the 8-week lockdown ending in May 2020, SARS-CoV-2 was diagnosed in only a few dialysis patients nationwide through the summer. The second wave started in September 2020 and ended mid-December 2020. Among our dialysis patients at AURA Nord, 14 were infected, with 1 death.
Germany (Werner Kleophas, Dusseldorf)
The first larger COVID-19 outbreak in Germany hit on February 26, 2020. As the virus spread, hot spots were linked to working conditions, especially meat factories. From the beginning, cases were identified among dialysis patients and staff. Responses were issued rapidly by authorities and the German Society of Nephrology.8,35 Providers, associations, and experts met frequently to establish best practices for diagnosis, triage, isolation, transportation, hygiene, personal protective equipment use, and more, and a national registry was implemented. Meticulous federal and local interventions (Box 1), implemented early and followed seriously by the general public, have helped limit the pandemic’s spread.36 As such, COVID-19 per-population cases and deaths were among the lowest in Europe during the first wave and remain so despite a protracted second wave since October 2020.
Italy (Gianpaolo Reboldi, Perugia)
Italy was hit overwhelmingly early in the COVID-19 pandemic, and its population with kidney failure was not spared.37,38 The Italian Society of Nephrology (SIN) published survey results from all 454 kidney care centers as of June 2020.5 Infection risk differed substantially by geographical latitude, and home treatment was linked to lower risk for SARS-CoV-2 infection. The SIN’s recommended preventive measures were adopted by all centers. Most centers tested only symptomatic patients and staff, whereas 16% and 30% adopted “test-all” policies for patients and staff, respectively. All centers restricted dialysis unit access, 62% conducted telephone triage between sessions, and 88% changed to individual transport for confirmed or suspected cases. The SIN’s second COVID-19 survey is underway as of late 2020.
Spain (Aleix Cases, Barcelona)
The Registry of the Spanish Society of Nephrology publishes updated data on COVID-19 infection and fatalities among dialysis patients.4,39,40 Similar to Spain’s general population, cases increased exponentially during March 2020 and decreased thereafter. A very high proportion of dialysis patients with SARS-CoV-2 infection were hospitalized, with nursing home residents at especially high risk. Initial infection prevention and control efforts were challenging because of shortages of personal protective equipment and diagnostic tests. Nonetheless, dialysis unit protocols issued by the health authorities, along with the societies, were implemented widely,41 including promoting individual transport to sessions. Positive cases were usually transferred to the reference hospital for HD until cleared by negative RT-PCR results, while more recently, satellite COVID-19 units have been established.
Spain faced a second wave from September through November 2020 and a third wave since January 2021, with an especially heavy impact on hospitalization and mortality in the general (and likely dialysis) population. Nationally, calls have been made for independent evaluation of the early pandemic response.42 Despite this, the situation in Spanish dialysis units has progressively normalized because of increasing familiarity with the new protocols and procedures.
Sweden (Stefan Jacobson, Stockholm)
The Stockholm region has been most affected by COVID-19. When the pandemic first struck, there was rapid coordinated reorganization among the hospital systems, with the large acute university hospitals focusing on COVID-19 and doubling intensive care unit (ICU) capacity within days. New teams and collaborations were established swiftly, with close to 100% of ICU beds occupied by COVID-19–infected patients and most using ventilators.43 The Swedish Renal Registry is collecting COVID-19 data from all dialysis centers, not yet available. During the first wave, only 10% to 15% of HD patients at our center with RT-PCR–positive SARS-CoV-2 required hospitalization. Most had no or mild symptoms and continued to receive outpatient dialysis, even among older and frail persons. Our dialysis practice isolated COVID-19 cases to specific dialysis facilities. To increase capacity, patients receiving 4 or 5 dialysis sessions per week were reduced to thrice weekly, but not less. The outpatient clinic switched almost entirely to telemedicine visits, which has worked well and will continue after the pandemic.
United Kingdom (Indranil Dasgupta, Birmingham)
The United Kingdom has among the world’s highest mortality from COVID-19, with serious first, second, and now (since December 2020) third waves. UK Renal Registry data show that patients with kidney failure have been disproportionately affected.3 At the pandemic’s onset, dialysis centers quickly reorganized as “hot” and “cold” sites, at which confirmed or suspected cases would dialyze separately from others. Group transport was discouraged. Some patients (up to 20% in many centers) were carefully selected to receive twice-weekly HD with monthly quality assurance review. Staff absences peaked at 30%, and personnel from other areas (including research) were deployed to HD units, ICUs, and renal wards. The high incidence of COVID-19 acute kidney injury (29% of patients ventilated in the ICU developed acute kidney injury, with 80% mortality) strained dialysis units as they supported ICUs with intermittent HD and in some cases acute PD, while continuous kidney replacement therapy capacity was almost overwhelmed.
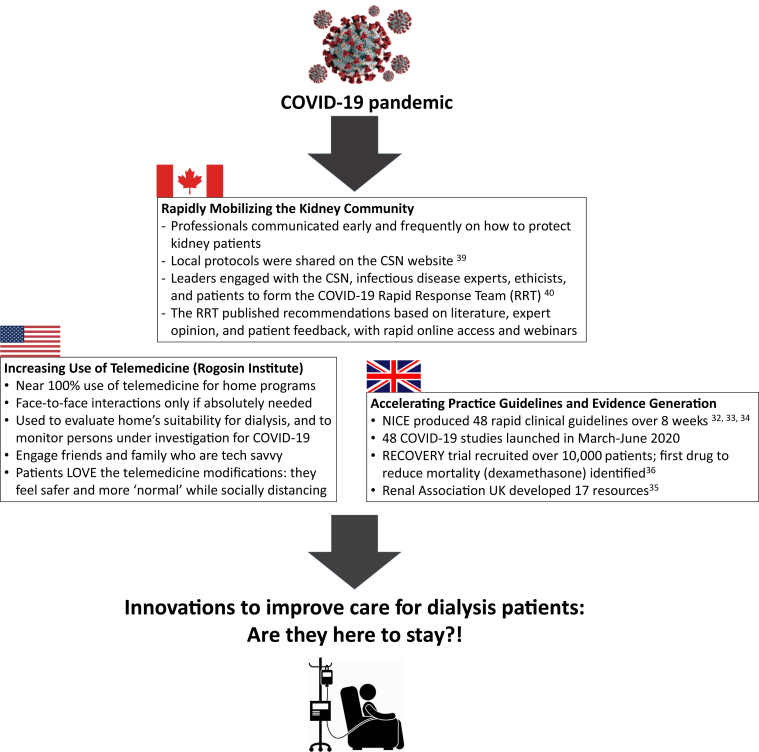
Several lessons were learned from the early pandemic experience. New models of care are likely to be incorporated in the future, such as virtual outpatient reviews, more use of intermittent HD and PD in the ICU, twice-weekly HD at dialysis initiation if residual kidney function is adequate, and others. We may see an increase in home dialysis, as well as early kidney transplantation facilitated in England by the new opt-out organ donation law. A silver lining of the pandemic is that clinical practice guidelines and clinical trial operations in the United Kingdom have been remarkably productive (Fig 4).44, 45, 46, 47, 48 These are commendable achievements and we can hope they will lead to new efficiencies in bringing innovations to the bedside after the pandemic’s end.
Figure 4.
Examples of information sharing, partnering, and innovation during the coronavirus disease 2019 (COVID-19) pandemic that we can learn from to accelerate transformation after the pandemic ends. Abbreviations: CSN, Canadian Society of Nephrology; NICE, National Institute for Health and Care Excellence; RRT, renal replacement therapy.
Americas
Many countries in the Western hemisphere faced the stark reality that SARS-CoV-2 was uncontrolled over the pandemic’s first year (Fig 1), attributed variously to insufficient public health guidance, resources, or personal accountability. We present experiences from Brazil, 2 initially hard-hit areas of the United States, and Canada, where containment measures were more successful.
Brazil (Roberto Pecoits-Filho, Curitiba)
Brazil is among the countries worst hit by COVID-19 infection worldwide. In Brazil, 80% of dialysis centers are covered by a public health care system, already financially strapped and now severely strained by the pandemic. The Brazilian Society of Nephrology issued COVID-19 management recommendations in May 2020.49 In a nationwide survey through June 2020, a total of 12% of dialysis staff had confirmed or suspected COVID-19 infection, with 2 reported deaths.10 Cases and case-fatality ratios among dialysis patients were much higher than in the general population and higher still in regions such as the Northeast and North with lower economic resources.
Maintenance dialysis units are responsible for dialysis support for many patients with acute kidney injury, mainly through intermittent HD. Because ∼30% of severely affected patients with COVID-19 infection require dialysis, staff and resources have been markedly strained. Virtual clinic visits are now much more common for PD patients. Kidney transplants, typically 5,000 per year, are projected to decrease by at least 50% in 2020.
Canada (Rita Suri, Montreal)
Canada’s first case of COVID-19 infection was identified in late January 2020. By March, coordinated public health strategies were issued and followed widely (Box 1). By mid-June 2020, the country had successfully flattened the curve.50 Quebec was hardest hit by far, with about 3-fold higher cases and deaths per population than Ontario, the most populous province. Mirroring the general population early on, Quebec had more cases among dialysis patients than Ontario, with little to no infection in other provinces. Many dialysis patients acquiring COVID-19 resided in long-term care facilities, where outbreaks were common, and most other cases were acquired in the community. Person-to-person transmission within the HD unit was rare, reported in <5% of Ontario’s 97 HD centers and none of Quebec’s 55 units, though at the time of the writing, updated counts are not yet available (Dr. Peter Blake, Director of Ontario Renal Network, Aug 10, 2020, and unpublished data Quebec Renal Network Study - currently under review).
Early on, the Canadian kidney community rapidly mobilized, developing, implementing, and sharing best practices (Fig 4).51,52 Perhaps the limited spread of COVID-19 infection among patients with kidney disease, particularly among in-center HD patients, may be attributed in part to hypervigilant monitoring, diligence, and information sharing. Since October 2020, as infection has become more widespread across the country, cases and deaths among dialysis patients have occurred in most provinces, though at the time of the writing, updated counts are not yet available.
United States
Vesh Srivatana, New York City, NY
The Rogosin Institute is a nonprofit dialysis provider with 1,300 dialysis patients, including 150 receiving PD and 70 receiving home HD. As of July 2020, we had 240 confirmed SARS-CoV-2 cases, including 235 (21.8%) in-center HD patients and only 12 (5.4%) home dialysis patients. Our organization has created dedicated COVID-19 shifts and made numerous other modifications. To address staff apprehension and morale, we limited time in the unit and ensured coverage in the event of illness. Many of our staff are now proud to care for this vulnerable population at this extraordinary time. Our home dialysis program has moved to near 100% telemedicine, which has been a huge success (Fig 4). When needed, we engage friends and family who are tech savvy. Patients have enthusiastically embraced the telemedicine modifications. They are relieved that they can isolate at home and avoid public transport and other dense spaces, as the general population can do.
Rachel Perlman, Ann Arbor, MI
Ann Arbor is 1 hour from Detroit, an early COVID-19 “hot spot” highlighting health care inequities by race. African Americans comprise 14% of the state’s population but 40% of COVID-19 deaths.53 The governor of Michigan issued a stay-at-home order on March 15, 2020, soon after the state’s first cases were diagnosed. The number of new cases declined markedly after May 2020, though increased dramatically since October 2020 along with the sustained second wave nationwide.
When the pandemic began, uncertainty led to fear that dialysis patients could be exposed to COVID-19 through the health system, that it might spread rapidly through the HD unit, and that it could be brought home to families. Though the fear subsided, we became weary that COVID-19 was not going away soon. Until mid-2020, we did not have capacity to test all symptomatic dialysis patients, let alone screen asymptomatic patients. Among our 3 outpatient units, 1 evening shift was designated the “COVID shift.” Happily, staff were very willing to volunteer for this shift. Even our patients who did not always “follow the rules” reported strict social distancing, and we had good treatment adherence, perhaps because COVID-19 scared patients. Our large home dialysis program shifted to telemedicine visits when possible and was greatly appreciated by patients.
Vaccination
The first SARS-CoV-2 vaccines were approved in December 2020 in 10 of our panel’s 15 countries: China (Sinopharm), the United Kingdom (Pfizer/BioNTech, Oxford/AstraZeneca), Saudi Arabia (Pfizer/BioNTech), Canada, the United States, and the 6 other European countries (Moderna, Pfizer/BioNTech). Approval in Brazil followed in January 2021 (Oxford/AstraZeneca, Sinopharm).1 Thailand, Japan, and Korea all began vaccinating in February 2021. Although dialysis staff are highest, or nearly highest, priority in all countries, extensive vaccination of patients will be a challenge for months to come. A diagnosis of kidney failure qualifies for first priority vaccination, among non–health care workers, in a few countries but is somewhat lower tier in most. In the United States, states and local communities have discretion regarding prioritization and allocation of limited vaccine supply. Dialysis providers are advocating for direct allocation to dialysis centers, but this is uncommon to date.54 Until this changes, some of our most vulnerable dialysis patients will be unvaccinated for months to come.
Conclusions
Infection with SARS-CoV-2 is grave for many dialysis patients, with case-fatality ratios in the 10% to 30% range to date among cases diagnosed by select testing. The most recent data have not shown any improvement in case-fatality ratios to date despite favorable trends in case-fatality ratios in national data (attributed to increased testing, among other reasons). In the pandemic’s early months, intense efforts centered on optimal testing, control, and cohorting strategies to protect dialysis patients and staff. Impressions from our panelists suggest that dialysis centers around the globe have by and large embraced recommended practices, with the caveat that access to diagnostic testing was suboptimal in hard-hit regions and still is in some locales.19, 20, 21, 22
Despite this, as we enter the second year of the pandemic, dialysis clinics continue to face vastly different realities, with the number of COVID-19 deaths logarithmically higher in some geographies than others, due overwhelmingly to community burden (Fig 3). As such, societal-level forces continue to put dialysis patients in some regions at undue risk from COVID-19. Notably, Fig 3 illustrates that the United Kingdom has the highest proportion of cases, and correspondingly deaths, among dialysis patients. Further evaluation is needed to understand whether this observation reflects reporting differences or true elevated risk.
This report is limited to high- and upper-middle–income countries and does not address the reality that lower-income countries may be less well positioned to limit the spread of COVID-19 in kidney care units and to support infected patients. DOPPS and the International Society of Nephrology are collecting COVID-19–related survey data from dialysis centers worldwide, with initial findings expected shortly.55
The intense challenges of the pandemic have prompted innovation across dialysis care in sufficiently resourced countries, proving that necessity is the mother of invention. Our panelists’ perspectives on some effects on dialysis care beyond COVID-19 are summarized in Table 2.8,56 Questions that will play out over the coming months and years include:
-
•
Will the advantages of telemedicine and home dialysis lead to greater use after the pandemic? Telemedicine is undoubtedly a big win but any shift to greater use of home dialysis is unclear. SARS-CoV-2 cases have been much higher among in-center HD than home dialysis patients. However, in-center HD patients are more likely to have community exposure, for example, as long-term care residents, and anecdotal data indicate that transmission is rare within in-center HD units following infection control protocols. As data accrue, this possibility merits urgent study and will surely underpin the extent to which COVID-19 drives longer-term uptake of home dialysis.
-
•
Will heightened universal precautions become the new standard of care after the pandemic to limit nosocomial infections? Although the likely decline in nosocomial infections would benefit all, sustaining this change will struggle against upfront costs and the temptation of complacency.
-
•
What is the new standard for emergency planning for the next pandemic? When resources allow,57 this should undoubtedly include review of emergency supply chain capacities, plans to rapidly deploy dialysis isolation shifts or centers, and resourcing to cover surges in acute dialysis needs without compromising long-term dialysis care. New urgent-PD and PD-first programs may be established by some sites.
-
•
How can we better protect staff from unacceptably high physical risks and stress that some have been exposed to? As a start, we need to understand the extent of the psychological impact of this pandemic on dialysis staff and ensure the availability of posttrauma support services. Moving forward, staffing protection and contingency plans need to be in place, and staff must have a real “voice at the table.”
-
•
Finally, can the kidney community join forces to more quickly bring innovation to market, develop the highest quality evidence, publish consensus guidelines, and share resources to meaningfully improve the lives of patients with kidney failure? Time will tell as, with society at large, we eventually emerge from this global health crisis.
Table 2.
Panelists’ Impressions About the Impact of COVID-19 on Dialysis Practice Locally
| In your local practice region, how did/do the following differ during the early COVID-19 period compared with before COVID-19?a |
Which changes will persist during the next year or beyond, compared with before COVID-19? | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Kidney Transplants | Home Dialysis Use | Use of Telemedicine for Home Dialysis Support | Use of Urgent- or Acute-Start PDb | Treatment Time/wk for In-center HD Patientsc | Availability of Dialysis Access Procedures | Transportation to/From Dialysis Unitd | Morale Among In-center HD Patients | Morale Among Dialysis Unit Staff | ||
| Europe | ||||||||||
| Belgium | ↓↓ | – | ↑↑ | NA | – | – | ↓ | ↓↓ | ↓ | Greater use of telemedicine; mask use for all patients/staff over at least the next y; morale remains decreased |
| United Kingdom | ↓↓ | ↑ | ↑↑ | ↑ | ↓ | ↓↓ | ↓ | ↓ | ↓↓ | Greater use of telemedicine, home dialysis, and twice-weekly HD at initiation |
| Spain | ↓↓ | – | ↑↑ | – | ↓ | ↓ | ↓ | ↓↓ | ↓↓ | Some personnel have been diagnosed with posttraumatic syndrome |
| Italy | ↓↓e | ↑ | ↑ | NA | – | – | ↓↓ | ↓ | ↓↓ | Greater use of telemedicine; we are recommending greater use of home therapy |
| Sweden | ↓↓ | – | ↑ | NA | ↓ | ↓ | ↓ | ↓ | ↓ | Greater use of telemedicine; we are aiming to increase use of home therapy |
| France | ↓↓ | ↑ | ↑ | NA | ↓ | – | – | ↓ | ↓ | Morale remains decreased |
| Germany | ↓ | – | – | – | – | ↓ | ↓ | – | – | Home dialysis use will continue to grow |
| Americas | ||||||||||
| United States (Ann Arbor) | ↓ | – | ↑↑ | – | – | ↓ | – | ↓ | ↓ | Greater use of telemedicine |
| United States (N Y) | ↓↓ | ↑ | ↑↑ | ↑↑ | ↓ | ↓↓ | ↓↓ | ↓↓ | ↓↓ | Greater use of telemedicine |
| Brazil | ↓↓ | ↓ | ↑↑ | – | – | ↓↓ | ↓ | ↓↓ | ↓↓ | Greater use of telemedicine |
| Canada | ↓↓ | ↓ | ↑ | – | – | – | ↓ | – | ↓ | Greater use of telemedicine will persist, home dialysis use expected to increase |
| Asia | ||||||||||
| Saudi Arabia | ↓↓ | – | ↑↑ | NA | ↓ | ↓ | – | ↓ | ↓ | Greater use of telemedicine |
| Japan | ↓↓ | – | – | – | – | – | – | ↑ | ↓↓ | Longer-term changes not expected |
| Korea | – | – | – | NA | – | – | – | ↓ | – | Longer-term changes not expected |
| China | ↓ | – | – | ↑ | – | ↓ | ↓ | – | ↓ | Longer-term changes not expected |
| Thailand | ↓↓ | – | ↑↑ | ↑ | – | ↓ | ↓ | ↓ | ↓ | Telemedicine use will remain higher, and we will strive to increase use of urgent-/acute-start PD |
Note: Panelists were asked to state impact on practice during the pandemic’s peak to date, as of August 2020.
Abbreviations: COVID-19, coronavirus disease 2019; HD, hemodialysis; NA, urgent or acute-start peritoneal dialysis is not available; PD, peritoneal dialysis.
Answer options: markedly decreased/worsened (↓↓), somewhat decreased/worsened (↓), unchanged (–), somewhat increased/improved (↑), markedly increased/improved (↑↑) .
Reference 56 provides another example of use of acute PD.
Question: How did treatment time per week change due to changes in prescription, adherence, availability of supplies, etc (↓ = shorter, ↑ = longer)?
Question: Did transportation of patients to/from the dialysis unit become easier (↑) or more challenging (↓)?
Reference 8.
Article Information
Authors’ Full Names and Academic Degrees
Bruce M. Robinson, MD, MS, Murilo Guedes, MD, Mohammed Alghonaim, MD, Aleix Cases, MD, Indranil Dasgupta, MD, Liangying Gan, MD, Stefan H. Jacobson, MD, Talerngsak Kanjanabuch, MD, Yong-Lim Kim, MD, Werner Kleophas, MD, Laura Labriola, MD, Rachel L. Perlman, MD, Gianpaolo Reboldi, MD, Vesh Srivatana, MD, Rita S. Suri, MD, Kazuhiko Tsuruya, MD, Pablo Urena Torres, MD, Ronald L. Pisoni, PhD, and Roberto Pecoits-Filho, MD, PhD.
Authors’ Contributions
Study conception and design, acquisition of data, and/or analysis and interpretation of data; BMR, MG, MA, AC, ID, LG, SHJ, TK, YLK, WK, LL, RLP, GR, VS, RSS, KT, PUT, RLP, RPF. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
Global support for the ongoing DOPPS Program is provided without restriction on publications by a variety of funders. For details see https://www.dopps.org/AboutUs/Support.aspx.
Financial Disclosure
Drs Robinson, Guedes, Pisoni, and Pecoits-Filho are employees of Arbor Research Collaborative for Health, which administers the DOPPS. Dr Robinson has received consultancy fees or travel reimbursement in the last 3 years from AstraZeneca, GlaxoSmithKline, and Kyowa Kirin Co, all paid directly to his institution of employment. Dr Pecoits-Filho reports grants from Fresenius Medical Care; personal fees from George Clinical; nonfinancial support from Akebia, Novo Nordisk, and AstraZeneca; and personal fees from Retrophin, outside the submitted work. Dr Cases reports grants from Vifor Pharma and AB Biotics and consultancy fees from Astellas, AstraZeneca, Boehringer Ingelheim, GSK, Novo Nordisk, and Vifor Pharma, outside the submitted work. Drs Perlman, Alghonaim, Jacobson, Suri, Dasgupta, Urena Torres, Reboldi, and Gan have nothing to disclose. Dr Labriola reports other from Amgen, other from Amgen, and other from Vifor Pharma, outside the submitted work. Dr Kanjanabuch reports grants from National Research Council of Thailand, personal fees from VISTERA, during the conduct of the study; grants from Rachadaphiseksompot Endorsement Fund, Chulalongkorn University, and grants from Thailand Research Foundation, outside the submitted work. Dr Kim reports speaker honorarium from FibroGen. Dr Kleophas is an employee of DaVita Deutschland AG and has received speaker honorarium or travel reimbursement in the last 3 years from Aey Congresse, AstraZeneca Germany-Santis, bbw gGmbH, Baxter Deutschland, BDS Berliner Dialyseseminar, Boehringer Ingelheim Pharma GmbH & Co KGPP, Hexal AG, and Springer Medizin. Dr Srivatana reports personal fees from Baxter Healthcare, outside the submitted work. Dr Tsuruya has received honoraria and grants from Kyowa Kirin Co.
Acknowledgements
Jennifer McCready-Maynes, an employee of Arbor Research Collaborative for Health, assisted with editing this paper.
Peer Review
Received September 28, 2020. Evaluated by 3 external peer reviewers, with direct editorial input from the Editor-in-Chief. Accepted in revised form March 7, 2021.
Footnotes
Complete author and article information provided before references.
References
- 1.Roser M., Ritchie H., Ortiz-Ospina E., Hasell J. Coronavirus pandemic (COVID-19) 2020. OurWorldInData.orghttps://ourworldindata.org/coronavirus Published online at. Accessed January 21, 2021.
- 2.Collart F, Mazzoleni L, Baudoux T, et al. Epidémiologie du COVID-19 en Belgique Francophone. 5th Annual Congress of the Société Française de Néphrologie, Dialyse et Transplantation (SFNDT) 2020, 7-8th October, 2020. Abstract 00223.
- 3.The Renal Association COVID-19 surveillance report for renal centres in the UK. https://renal.org/audit-research/publications-presentations/report/covid-19-surveillance-reports Accessed December 29, 2020.
- 4.Spanish Society of Nephrology Updated information on COVID-19 from the S.E.N. Registry. https://mailchi.mp/senefro/registro-epidemiolgico-vhc-vhb-vih-1314998
- 5.Quintaliani G., Reboldi G., Di Napoli A. Exposure to novel coronavirus in patients on renal replacement therapy during the exponential phase of COVID-19 pandemic: survey of the Italian Society of Nephrology. J Nephrol. 2020;33:725–736. doi: 10.1007/s40620-020-00794-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vistoli F., Furian L., Maggiore U. COVID-19 and kidney transplantation: an Italian survey and consensus. J Nephrol. 2020;33:667–680. doi: 10.1007/s40620-020-00755-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agency de la biomedicine Situation de l’épidémie de Covid-19 chez les patients dialysés et greffés rénaux en France. https://www.agence-biomedecine.fr/IMG/pdf/bulletin_no28_version1.pdf Accessed December 2, 2020.
- 8.Galle J. Nierenersatztherapie in Zeiten von SARS-CoV 2 in Deutschland. Nieren-und Hochdruckkrankheiten. 2020;49:428–436. [Google Scholar]
- 9.Centers for Medicare & Medicaid Services Preliminary Medicare COVID-19 Data Snapshot. https://www.cms.gov/files/document/medicare-covid-19-data-snapshot-fact-sheet.pdf Accessed November 21, 2020.
- 10.Pio-Abreu A., do Nascimento M.M., Vieira M.A., de Menezes Neves P.D., Lugon J.R., Sesso R. High mortality of CKD patients on hemodialysis with Covid-19 in Brazil. J Nephrol. 2020;33:875–877. doi: 10.1007/s40620-020-00823-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Japanese Association of Dialysis Physicians. http://www.touseki-ikai.or.jp/htm/03_info/doc/corona_virus_infected_number_20200710.pdf Accessed December 25, 2020.
- 12.The Korean Society of Nephrology COVID-19 Task Force Team, Accessed January 8, 2021. www.ksn.or.kr.
- 13.Korean Koreas Disease Control and Prevention Agency, Accessed January 8, 2021. http://ncov.mohw.go.kr/en/
- 14.US Renal Data System . National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018. 2018 USRDS Annual Data Report: epidemiology of kidney disease in the United States. [Google Scholar]
- 15.Korean ESRD Registry. KSN 2020, Virtual Meeting, September 25-27, 2020, Accessed August 10, 2020. http://www.ksn.or.kr/rang_board/list.html?code=sinchart
- 16.Hsu C.M., Weiner D.E., Aweh G. COVID-19 infection among US dialysis patients: risk factors and outcomes from a national dialysis provider. Am J Kidney Dis. 2021;77:748–756. doi: 10.1053/j.ajkd.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Francis A., Madhavan S., Ikizler T.A. Global report, International Society of Nephrology. https://www.theisn.org/covid19/global-reports Accessed August 10 2020.
- 18.Friedman C., Rubin J., Brown J. Toward a science of learning systems: a research agenda for the high-functioning Learning Health System. J Am Med Inform Assoc. 2015;22(1):43–50. doi: 10.1136/amiajnl-2014-002977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Basile C., Combe C., Pizzarelli F. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centres. Nephrol Dial Transplant. 2020;35(5):737–741. doi: 10.1093/ndt/gfaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Sequera Ortiz P., Gili B.Q., de la Fuente G.D., Heras M.M., Lazo M.S., y Pino M.D. Protocol against coronavirus diseases in patients on renal replacement therapy: dialysis and kidney transplant. Nefrología (English Edition) 2020;40:253–257. doi: 10.1016/j.nefro.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kliger A.S., Silberzweig J. Mitigating risk of COVID-19 in dialysis facilities. Clin J Am Soc Nephrol. 2020;15(5):707–709. doi: 10.2215/CJN.03340320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hsu C.M., Weiner D.E. COVID-19 in dialysis patients: outlasting and outsmarting a pandemic. Kidney Int. 2020;98(6):1402–1404. doi: 10.1016/j.kint.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.COVID-19 Task Force Committee of the Japanese Association of Dialysis Physicians, Japanese Society for Dialysis Therapy, Japanese Society of Nephrology, et al. COVID-19 of dialysis patients in Japan: current status and guidance on preventive measures. Ther Apher Dial. 2020;24(4):361–365. doi: 10.1111/1744-9987.13531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xiong F., Tang H., Liu L. Clinical characteristics of and medical interventions for COVID-19 in hemodialysis patients in Wuhan, China. J Am Soc Nephrol. 2020;31(7):1387–1397. doi: 10.1681/ASN.2020030354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jiang H.J., Tang H., Xiong F. COVID-19 in peritoneal dialysis patients. Clin J Am Soc Nephrol. 2021;16:121–123. doi: 10.2215/CJN.07200520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Expert Team of Chinese Society of Blood Purification Administration Recommendations for prevention and control of novel coronavirus infection in blood purification center (room) Chin J Blood Purif. 2020;19(02):73–76. [Google Scholar]
- 28.COVID-19 Expert Team of Chinese Society of Nephrology Recommendations for prevention and control of novel coronavirus infection in blood purification center (room) from the Chinese Medical Association Nephrology Branch[J] Chin J Nephrol. 2020;36(2):82–84. [Google Scholar]
- 29.Xu X., Nie S., Sun J. The cumulative rate of SARS-CoV-2 infection in Chinese hemodialysis patients. Kidney Int Rep. 2020;5(9):1416–1421. doi: 10.1016/j.ekir.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cho J.H., Kang S.H., Park H.C. Hemodialysis with cohort isolation to prevent secondary transmission during a COVID-19 outbreak in Korea. J Am Soc Nephrol. 2020;31(7):1398–1408. doi: 10.1681/ASN.2020040461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bello W. How Thailand contained COVID-19. https://fpif.org/how-thailand-contained-covid-19/ Accessed June 15, 2020.
- 32.You.gov [Internet] UK: Imperial College London. https://th.yougov.com/en-th/news/2020/05/19/thais-most-likely-wear-facemasks-asean/ Updated April 27, 2020. Accessed June 15, 2020.
- 33.Kanjanabuch T., Takkavatakarn K. Global dialysis perspective: Thailand. Kidney360. 2020;1:671–675. doi: 10.34067/KID.0000762020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jager K.J., Kramer A., Chesnaye N.C. Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int. 2020;98(6):1540–1548. doi: 10.1016/j.kint.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deutsche Gesellschaft für Nephrologie, Fachinformationen COVID-19, COVID-19 Register für Dialysepatienten. www.dgfn.eu Accessed August 10, 2020.
- 36.Robert Koch Institut, COVID-19 (Coronavirus SARS-CoV-2), Fallzahlen und Meldungen. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/nCoV.html Accessed August 10, 2020.
- 37.Alberici F., Delbarba E., Manenti C. A report from the Brescia Renal COVID Task Force on the clinical characteristics and short-term outcome of hemodialysis patients with SARS-CoV-2 infection. Kidney Int. 2020;98(1):20–26. doi: 10.1016/j.kint.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Società Italiana di Nefrologia Coronavirus disease (COVID-19) pandemic. https://sinitaly.org/coronavirus/ Accessed June 1, 2020.
- 39.Goicoechea M., Sánchez Cámara L.A., Macías N. COVID-19: clinical course and outcomes of 36 hemodialysis patients in Spain. Kidney Int. 2020;98(1):27–34. doi: 10.1016/j.kint.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Albalate M., Arribas P., Torres E. High prevalence of asymptomatic COVID-19 in haemodialysis: learning day by day in the first month of the COVID-19 pandemic. Alta prevalencia de COVID-19 asintomático en hemodiálisis. Aprendiendo día a día el primer mes de pandemia de COVID-19. Nefrologia. 2020;40(3):279–286. doi: 10.1016/j.nefro.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Soler M.J., Macia Heras M., Ortiz A., Del Pino y Pino MD., Salgueira Lazo M. Impact of the COVID-19 pandemic on Spanish Nephrology Services. Nefrologia. 2020;40(6):579–584. doi: 10.1016/j.nefro.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.García-Basteiro A., Alvarez-Dardet C., Arenas A. The need for an independent evaluation of the COVID-19 response in Spain. Lancet. 2020;396(10250):529–530. doi: 10.1016/S0140-6736(20)31713-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smolander J., Bruchfeld A. COVID-19 and kidney disease. Läkartidningen. 2020;117:20110. [PubMed] [Google Scholar]
- 44.NICE Guideline COVID-19 rapid guideline: chronic kidney disease. https://www.nice.org.uk/guidance/ng176/resources/covid19-rapid-guideline-chronic-kidney-disease-pdf-66141964574917 Published May 15, 2020. Accessed August 10, 2020.
- 45.NICE Guideline COVID 19 rapid guideline: renal transplantation. https://www.nice.org.uk/guidance/ng178/resources/covid-19-rapid-guideline-renal-transplantation-pdf-66141967934149 Published June 19, 2020. Accessed August 10, 2020. [PubMed]
- 46.NICE Guideline COVID-19 rapid guideline: dialysis service delivery. https://www.nice.org.uk/guidance/ng160/resources/covid19-rapid-guideline-dialysis-service-delivery-pdf-66141894031045 Published March 20, 2020. Accessed August 10, 2020. [PubMed]
- 47.The Renal Association RA resources for renal professionals. https://renal.org/health-professionals/covid-19/ra-resources Accessed June 2, 2021.
- 48.RECOVERY Collaborative Group; Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with Covid-19 - preliminary report. Published online July 17, 2020. N Engl J Med. doi:10.1056/NEJMoa2021436
- 49.Abreu A.P., Riella M.C., Nascimento M.M. The Brazilian Society of Nephrology and the Covid-19 pandemic. Braz J Nephrol. 2020;42(2):1–3. doi: 10.1590/2175-8239-JBN-2020-S101. suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Coronavirus disease 2019 (COVID-19): Epidemiology update. https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html?stat=num&measure=total#a2 Accessed August 10, 2020.
- 51.Canadian Society of Nephrology COVID-19 emergency preparedness for healthcare professionals. https://www.csnscn.ca/covid-19-emergency-preparedness-for-healthcare-professionals Accessed August 10, 2020.
- 52.Canadian Society of Nephrology CSN COVID-19 Rapid Response Team (CCRRT) recommendations to be published in the Canadian Journal of Kidney Health and Disease. https://www.csnscn.ca/CSN-covid-19-rapid-response-team-recommendations-CJKHD Accessed August 10, 2020. [DOI] [PMC free article] [PubMed]
- 53.Michigan Department of Health and Human Services Coronavirus disease. 2019 https://www.michigan.gov/mdhhs Accessed August 10, 2020. [Google Scholar]
- 54.Charnow J.A. Dialysis providers push for direct allocation of COVID-19 vaccines. Renal Urol News. February 8, 2021 https://www.renalandurologynews.com/home/news/nephrology/hemodialysis/covid-19-coronavirus-vaccination-dialysis-facilities/?utm_source=newsletter&utm_medium=email&utm_campaign=run-update-hay-20210211&cpn=NephMD,neph_all&hmSubId=xR2JxZBprFc1&hmEmail=e46ycjyxL55scYrNhPhHd1U8xuOOWIhqvptnfTrkYriCps_UdoHmWg2&NID=1154402360&c_id=&email_hash=0cc22b5ce832016ecae2f9b455c96c16&mpweb=1323-122502-356169 [Google Scholar]
- 55.International Society of Nephrology ISN teams up with DOPPS to survey the impact of Covid-19 on dialysis patients. https://www.theisn.org/blog/2020/07/03/isn-teams-up-with-dopps-to-survey-the- impact-of-covid-19-on-dialysis-patients/ Accessed August 10, 2020.
- 56.Shamy O., Sharma S., Winston J., Uribarri J. Peritoneal dialysis during the coronavirus disease-2019 (COVID-19) pandemic: acute inpatient and maintenance outpatient experiences. Kidney Med. 2020;2(4):377–380. doi: 10.1016/j.xkme.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.End stage renal disease community Covid-19 after-action report and improvement plan. Kidney community emergency response. November 3, 2020. https://www.kcercoalition.com/contentassets/8eab3e45afbd4286a269383dcdba97a7/kcercovidaarip_10272020508.pdf