Abstract
Objectives:
To investigate occlusal stability from the early mixed to the permanent dentition in children after early treatment with the eruption guidance appliance (EGA).
Materials and Methods:
Of 46 participants who received 1-year early EGA treatment, 35 attended a follow-up examination at age 12. Group 1 (n = 21) started their EGA treatment at mean age 7.7 years, and group 2 at 9.1 years. Following 1-year treatment, the EGA was used as a retainer. Changes in overjet, overbite, sagittal molar relationship, and anterior crowding were measured on casts obtained before EGA treatment, after EGA treatment, and at follow-up to evaluate occlusal stability.
Results:
Mean overjet, overbite, sagittal molar relation, and mandibular crowding improved significantly during the study period. Participants with good compliance during the retention period had significantly smaller overjet and overbite values than those with poor compliance.
Conclusions:
Early correction of increased overjet, overbite, and class II molar relation with the EGA is maintainable and can also be effective in the permanent dentition, provided the EGA is worn regularly as a retainer.
Keywords: Early treatment, Stability
INTRODUCTION
The eruption guidance appliance (EGA) is a preformed removable appliance that combines the effects of a functional appliance with the effects of a positioner. Due to its soft elastomeric material, alignment of teeth in the dental arches occurs concomitantly with correction of overjet, overbite, and class II molar relationship. Other reported indications for EGA treatment are open bite, gummy smile, and scissors bite.1–4 Early EGA treatment has also been applied as a comprehensive treatment, in which active treatment is performed in one phase during the early mixed dentition and followed by retention with the same appliance. Retention until the end of growth is recommended to ensure stability.
Studies have reported favorable short-term results in patients who received early EGA treatment, including significant improvements in overjet, overbite, crowding, and sagittal molar relationships and considerable reduction in the need for further orthodontic treatment.1–6
Follow-up studies on EGA treatment outcomes are few, but those that exist show best long-term results for overjet and sagittal molar relationship.7
More follow-up data are needed to evaluate the potential benefits of EGA treatment. The aim of this study was to investigate occlusal stability from the early mixed to the permanent dentition in children who had 1-year early treatment with the EGA. The second aim was to examine whether a delay in the initiation of early EGA treatment affected treatment outcomes.
MATERIALS AND METHODS
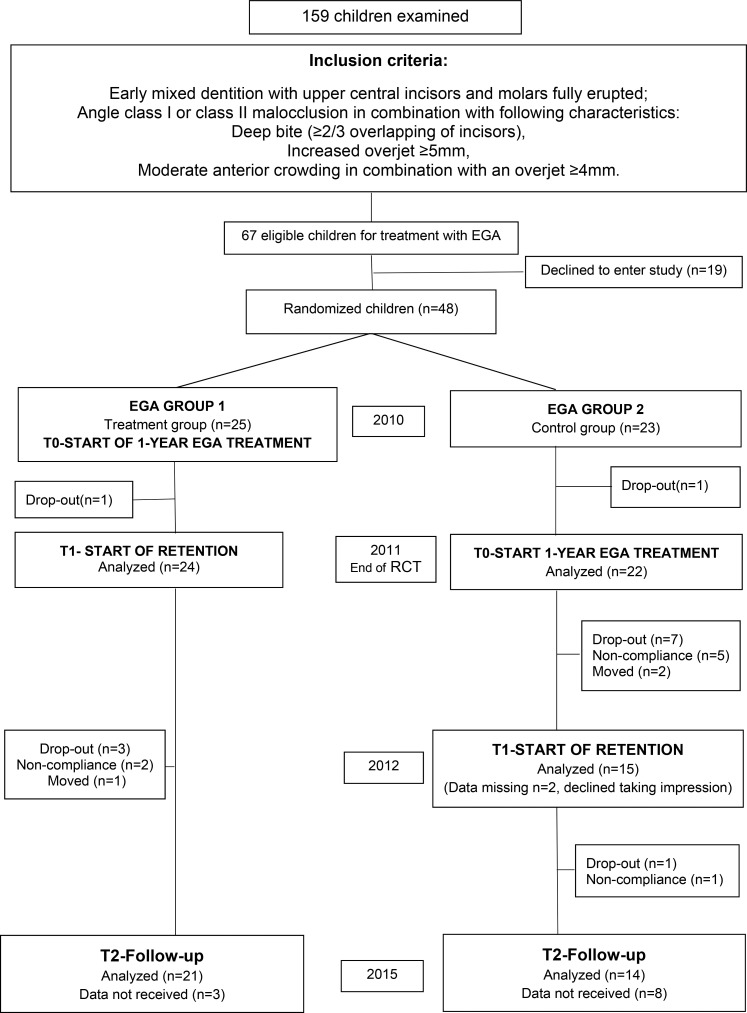
This prospective study used data and patients from a randomized clinical trial (RCT) started in 2010, when this study was approved by the Regional Ethical Committee, Tromsø, Norway (REK 2010/1510-8). The 1-year report on the outcome of this trial was published in 2015.6 The original participants were randomly allocated into one of the following two groups: EGA Group1 and EGA Group2. EGA Group1 served as the treatment group for the RCT; in this group, participants started treatment in 2010, at a mean age of 7.7 years (standard deviation [SD] ± 0.5). EGA Group2 served as the control group for the RCT; in this group, participants started treatment after the 1-year RCT, at a mean age of 9.1 years (SD ± 0.6). The participants and inclusion criteria are described in Figure 1.
Figure 1.
Participants and the study design during the 5-year study.
All treatments were performed at the Public Dental Service Competence Center of Northern Norway by two postgraduate students (RM, MD) under the supervision of a specialist (KKN). The appliance used was LM-Activator (Plandent Oy, Helsinki, Finland), a modification of the EGA (Figure 2). The participants were instructed to wear the EGA every night and for 2 hours during the day for 1 year. Following this 1-year active treatment period, they were instructed to continue to wear the EGA every other night as a retainer, and regular check-ups were scheduled every 6 months. At age 12, all children who completed the 1-year RCT were invited to attend a follow-up examination and an interview performed by a specialist orthodontist (RM).
Figure 2.
LM-Activator, a modification of the eruption guidance appliance (EGA).
Data Collection
Dental casts and measurements.
All children had dental casts made before EGA treatment (T0), after completion of treatment (T1), and at follow-up (T2). One investigator (RM) performed all measurements on blinded casts with a digital caliper to the nearest 0.01mm.
The measurements of overjet (mm), overbite (mm), and sagittal molar relationship (angle classification) were described in detail in the 1-year report in 2015.6 The space for six anterior teeth was estimated separately for the maxilla and the mandible at T0, T1, and T2. At T0 and T1, the distance from the distal surface of the left deciduous canine to the distal surface of the right canine was measured with a flexible multithreaded wire (Dentaflex .0175; Dentaurum Corp., Ispringen, Germany) following the anterior arch circumference. If a deciduous canine was missing (n = 5), the distance was measured from the mesial surface of the first primary molar. The width of the permanent incisors and canines at T2 was measured between the anatomical contact points of each tooth. The difference between summed width of the six anterior teeth and the anterior arch length indicated the estimated available space. More than 1.5 mm lack of space at T0 was defined as crowding.8
At T2, Little's Index of Irregularity (LII) was used to describe displacement/crowding of the anterior teeth.9 LII values up to 3.5 mm were considered clinically acceptable.10
Compliance
Compliance in wearing the EGA as a retainer was evaluated during the follow-up interview and from the observations written in the journals. Based on this information, compliance was categorized as good (wear of the appliance mainly as instructed), moderate (wear less than instructed, with varying regularity), or poor (occasional/no wear).
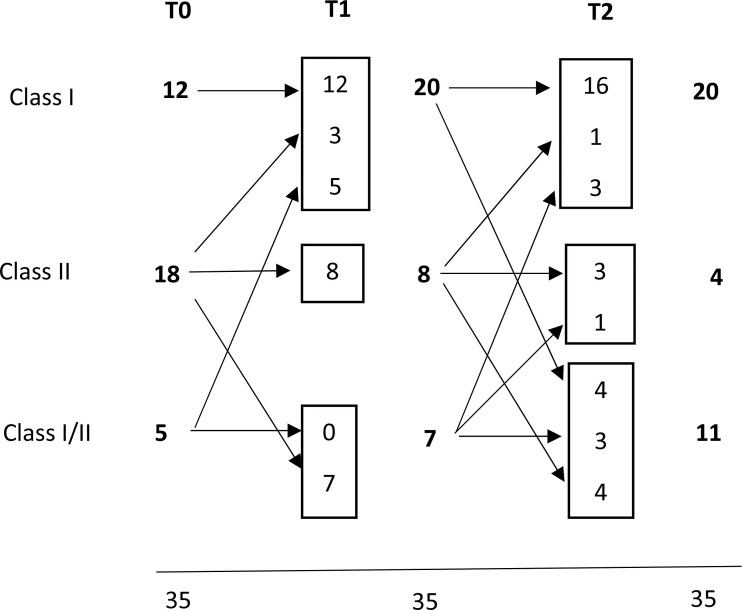
Cephalometric Analysis
Lateral cephalograms of both EGA groups were taken at T0 and T2 using the same X-ray unit (Cranex D; Soredex, Tuusula, Finland) at a natural head position. One investigator (RM) traced all cephalograms after they were blinded (Figure 3) using FACAD software (Ilexis AB, Linköping, Sweden). The cephalometric values of EGA-treated participants were compared with subjects from the Norwegian growth study, which included untreated children with clinically acceptable normal occlusion.11
Figure 3.
Cephalometric measurements used in the study.
Method Error
A total of 25 randomly selected casts were remeasured after an interval of at least 4 weeks. The intraclass correlation coefficient (ICC) and κ were used to analyze the reliability of the repeated measurements. The ICCs with 95% confidence intervals (CI) for the continuous variables were overjet 0.97 (95% CI 0.93–0.99), overbite 0.99 (95% CI 0.97–0.99), LII 0.97 (95% CI 0.94–0.99), available space 0.98 (95% CI 0.98–0.99). The mean κ for categorical variables was 0.97 (range 0.82–1.00), indicating almost perfect agreement.12 The mean ICC for the duplicate cephalometric measurements was 0.95 (range 0.87–0.99).6
Statistics
All statistical analyses were performed in SPSS for Windows 22.0 (SPSS Inc., Chicago, Ill). The Kolmogorov–Smirnov test was used to check the normality of the data. Differences between EGA groups were analyzed with independent t-tests and χ2 tests. The paired-sample t-test was used to determine changes from T0 to T2 within groups. P values less than .05 were considered statistically significant.
RESULTS
A total of 35 children attended follow-up examination at age 12 (76%, mean age 12.1 years [SD ± 0.9]; Figure 1). Three participants from EGA Group1 dropped out during the retention period; seven from EGA Group2 dropped out before the end of active treatment and one during the retention period. The reasons for dropping out were noncompliance (n = 8) or moving out of the district (n = 3). Among the 35 study participants, average retention time between T1 and T2 was 3.4 years (SD ± 0.4) in EGA Group1 and 2.4 years (SD ± 0.5) in EGA Group2.
From T0 to T2, mean overjet and overbite decreased significantly, and no significant differences between the EGA groups were found at T2 (Table 1). Between T1 and T2, the mean overjet increased by 0.7 mm (SD ± 1.4) and overbite by 0.7 mm (SD ± 0.9). At T0, 17 of 35 participants had deep bite with gingival impingement. At T2, no participants showed deep overbite, but five had increased overjet (5.1–5.9 mm).
Table 1.
Overjet and Overbite Before Treatment (T0), After 1-Year Treatment (T1), and at Follow-Up (T2) in the Two Groups of Participants Treated With the Eruption Guidance Appliance (EGA)a
| Overjet in mm, Mean (SD) |
Overbite in mm, Mean (SD) |
|||||
| T0 |
T1 |
T2 |
T0 |
T1 |
T2 |
|
| EGA group 1, n = 21 | 4.9 (1.2) | 2.6 (1.3) | 3.5 (1.2) | 3.4 (1.4) | 1.9 (1.1) | 2.8 (0.9) |
| EGA group 2, n = 14 | 5.1 (1.4) | 2.6 (1.1) | 2.9 (1.1) | 4.5 (1.1) | 3.0 (1.1) | 3.2 (1.3) |
| Total, N = 35 | 5.0 (1.3) | 2.6 (1.2) | 3.3 (1.2) | 3.8 (1.4) | 2.3 (1.2) | 3.0 (0.9) |
| P (Between Groups) | .676 | .922 | .152 | .018* | .009** | .256 |
Statistical methods: Independent samples t-test to compare means between groups; paired sample t-test to analyze changes from T0 to T2.
Significance of change from T0 to T2 in the total group: overjet, ***P < .000; overbite, ***P < .000.
P < .05; ** P < .01.
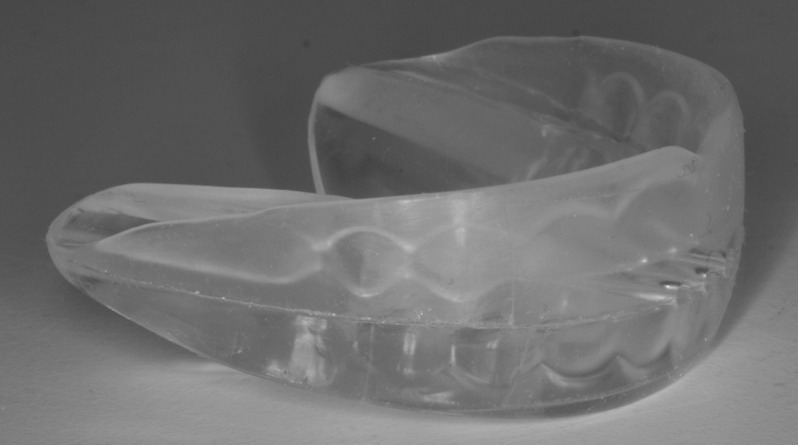
Sagittal molar relationship improved significantly from T0 to T2 (P = .024), with no significant difference between the EGA groups at T0, T1, or T2. All children with initial unilateral class I/II changed to class I between T0 and T1, whereas full class II changed more often to unilateral class I/II in that same time and continued to improve from T1 to T2 (Figure 4).
Figure 4.
Changes in angle classification among participants from before treatment (T0) to follow-up (T2).
At T2, maxillary anterior teeth showed more irregularity than the mandibular anteriors, with mean LII values of 2.4 mm (SD ± 2.3) and 1.1 mm (SD ± 1.5), respectively. Clinically unacceptable irregularity was registered in 3 participants in the mandible, and in 10 participants in the maxilla. The LII values for the maxilla or the mandible did not differ significantly between the EGA groups (P values .353 and .745, respectively).
At T0, 23 of the 35 participants showed anterior crowding in either one or both jaws. The mean estimated lack of space was −4.5 mm in the maxilla and −4.1 mm in the mandible (Table 2). For the rest, the estimated mean spaces in the anterior segments were 1.2 mm (SD ± 2.2) and −0.03 mm (SD ± 1.3), respectively. Among those with initial crowding, the anterior space conditions improved significantly between T0 and T2 in both jaws, whereas among those with no initial crowding, the changes were minimal.
Table 2.
Estimated Space Available for Anterior Teeth in the Maxilla and the Mandible Before Treatment (T0), After 1-Year Treatment (T1), and at Follow-Up (T2) Among the Participants in Relation to Crowding Before Treatment Start (T0)a
| Children With No Anterior Crowding at T0 |
Children With Anterior Crowding at T0 |
|||||||||||
| n |
Estimated Available Space in mm, Mean (SD) |
P |
n |
Estimated Available Space in mm, Mean (SD) |
P |
|||||||
| T0 |
T1 |
T2 |
Change T2–T0 |
Change T2–T1 |
T0 |
T1 |
T2 |
Change T2–T0 |
Change T2–T1 |
|||
| Maxilla | ||||||||||||
| EGA group 1 | 8 | 1.5 (2.6) | 1.0 (2.0) | 2.1 (1.6) | .326 | .016* | 13 | −4.9 (2.6) | −3.8 (1.6) | −1.1 (1.8) | .000*** | .000*** |
| EGA group 2 | 7 | 0.9 (1.8) | −0.1 (1.6) | 1.0 (2.5) | .886 | .156 | 7 | −3.9 (1.4) | −2.4 (2.2) | −0.8 (1.9) | .004** | .171 |
| Total | 15 | 1.2 (2.2) | 0.6 (1.8) | 1.6 (1.8) | .481 | .012* | 20 | −4.5 (2.2) | −3.3 (1.9) | −1.0 (1.8) | .000*** | .000*** |
| Mandible | ||||||||||||
| EGA group 1 | 9 | −0.2 (1.4) | 0.04 (1.1) | 0.4 (0.4) | .300 | .483 | 12 | −4.5 (2.5) | −2.3 (2.1) | −0.2 (1.4) | .000*** | .000*** |
| EGA group 2 | 3 | 0.5 (0.8) | 1.5 (1.5) | 1.0 (1.6) | .432 | .451 | 11 | −3.6 (1.9) | −1.7 (1.8) | 0.03 (0.8) | .000*** | .021* |
| Total | 12 | −0.03 (1.3) | 0.4 (1.3) | 0.5 (0.8) | .199 | .785 | 23 | −4.1 (2.2) | −2.0 (1.9) | −0.1 (1.8) | .000*** | .000*** |
Crowding = estimated lack of space > −1.5 mm; no crowding = estimated space available ≤ −1.5 mm). SD indicates standard deviation; EGA, eruption guidance appliance.
P < .05, ** P < .01, *** P < .001.
From T0 to T2, the mean mandibular intercanine width in children with initial crowding increased from 25.0 (SD ± 1.7) mm to 25.9 (SD ± 1.2) mm (P = .045), whereas the group with no crowding showed an opposite tendency from 27.1 (SD ± 1.9) mm to 26.0 (SD ± 0.9) mm (P = .094). At T0, the intercanine width was significantly smaller among those with crowding when compared with those without (P = .009); by T2 the difference disappeared.
From T0 to T2, the ANB angle decreased significantly (P = .000), and the lower incisor proclination increased significantly (P = .000) in the EGA-treated children (Table 3). No significant differences in cephalometric values were found between EGA Group1 and Group2. Compared to the Norwegian growth study, female participants had considerably more proclined lower incisors. Otherwise, no major differences in cephalometric values were seen.
Table 3.
Mean Values (Degrees) and Standard Deviations (SD) of Cephalometric Variables in Participants Treated With the Eruption Guidance Appliance (EGA) and in Untreated Children From the Norwegian Growth Study, Nittedala
| Cephalometric Values |
EGA-Treated Children, Mean (SD) |
Untreated Children, Mean (SD) |
EGA Versus Untreated, P |
|||||||||
| Boys, n = 15 |
Girls, n = 20 |
Boys, n = 35 |
Girls, n = 39 |
Boys |
Girls |
|||||||
| T0 |
T2 |
T0 |
T2 |
9yr |
12yr |
9yr |
12yr |
T0 |
T2 |
T0 |
T2 |
|
| SNA, ° | 84.4 (3.2) | 84.9 (2.9) | 80.3 (3.7) | 81.1 (4.1) | 82.3 (3) | 84.0 (2.4) | 80.8 (3.4) | 82.0 (3.5) | .031* | .259 | .606 | .558 |
| SNB, ° | 80.2 (4.0) | 81.7 (3.2) | 76.2 (3.2) | 78.3 (3.4) | 78.9 (3.5) | 80.0 (3.0) | 78.0 (3.2) | 79.0 (3.3) | .254 | .078 | .045* | .488 |
| ANB, ° | 4.2 (2.3) | 3.2 (2.4) | 4.1 (1.7) | 2.7 (1.7) | 3.4 (2.1) | 4.0 (1.9) | 2.8 (2.2) | 3.0 (2.0) | .236 | .214 | .025* | .569 |
| ML/NSL, ° | 31 (5.3) | 28.9 (5.7) | 33 (5.7) | 31.0 (5.6) | 33.4 (5.9) | 32.6 (5.7) | 35 (4.6) | 33.5 (4.7) | .181 | .040* | .151 | .075 |
| NL/NSL, ° | 5.5 (2.2) | 4.8 (3.5) | 9.5 (3.4) | 8.5 (3.0) | 6.1 (2.8) | 6.1 (2.2) | 7.7 (2.5) | 7.8 (2.8) | .465 | .117 | .025* | .378 |
| Ili/ML, ° | 94.7 (5.3) | 98.8 (3.8) | 96.8 (6.4) | 99.2 (5.2) | 94.6 (5.9) | 95.6 (6.2) | 92.7 (5.1) | 92.9 (5.9) | .955 | .071 | .000*** | .000*** |
Statistical analysis: Independent sample t-test. ¤ Inclusion criteria used in the Norwegian growth study: Norwegian Caucasian origin, normal occlusion (minor rotations and spacing less than 1 mm were accepted), no apparent facial disharmony, no orthodontic treatment. T0 = before treatment, T2 = follow-up examination at age 12.
P < .05, ** P < .01, *** P < .001.
Compliance during the retention period varied. Roughly one in three participants (31%) had good compliance in wearing the EGA. The rest had moderate (40%) or poor (29%) compliance. The compliant participants showed practically no relapse in overjet and overbite and had significantly smaller overjet and overbite at T2 than those with compromised compliance (Table 4).
Table 4.
Occlusal Characteristics in Relation to Retention Compliance at T2a
| Retention Compliance |
P |
|||||
| Good (A), n = 11 |
Moderate (B), n = 14 |
Poor (C), n = 10 |
A vs B |
A vs C |
B vs C |
|
| Overjet, mm | 2.8 (1.2) | 3. 0(0.8) | 4.3 (1.1) | .602 | .005** | .002** |
| Overbite, mm | 2.4 (1.1) | 3.0 (1.2) | 3.5 (0.8) | .222 | .023* | .286 |
| LII maxilla, mm | 2.5 (2.9) | 2.6 (2.2) | 2.0 (2.2) | .917 | .670 | .510 |
| LII mandible, mm | 0.6 (1.2) | 0.9 (1.0) | 1.8 (2.1) | .584 | .123 | .138 |
LLI indicates Little Irregularity Index. Statistical analysis: independent-sample t-tests.
P < .05, ** P < .01.
DISCUSSION
In this report, the focus was on net occlusal and dental changes from the early mixed to the permanent dentition to evaluate the outcome and stability of comprehensive one-phase early EGA therapy. Reduced wear of the EGA as a retainer was part of the plan to maintain early treatment results until the permanent dentition. These results in 12-year-old children cannot be considered as final because growth, especially in boys, will continue for approximately 2 to 3 more years. Retention until the end of growth is recommended to stabilize the present outcome.
The most common reason for dropping out was children's lack of motivation to wear the EGA. Regardless of randomization, the drop-out rate was clearly higher in EGA Group2, which was the control group of the initial RCT. It seems that the initial allocation to a control group reduced treatment motivation, which became apparent when this group later started their own treatment. Loss of participants in EGA Group2 reduced the original power of the study and may have caused some underestimation of the differences between the two groups. The design of the original RCT changed when the controls also received treatment. Therefore, in the cephalometric analyses, historical data from untreated Norwegian children was used as the reference group.
Previous studies have suggested that the early mixed-dentition stage, preferably before the eruption of the maxillary incisors, is optimal for starting EGA treatment because during that stage nighttime wear of the appliance is enough to correct malocclusions.1–4 The EGA Group1 was treated mainly during the early mixed dentition, when lateral incisors were still erupting, whereas Group2 had reached the latent period between the early and late mixed dentition before treatment initiation. The results suggested that, after maxillary central incisors have fully erupted, delaying treatment initiation a few years may not influence the treatment outcome.
In this study, the active treatment with the EGA was limited to 1 year, which is clearly shorter than in other EGA studies. Nevertheless, this time proved generally sufficient to correct all occlusal characteristics except maxillary anterior irregularity.6 Decreased wear of the EGA as a retainer seemed sufficient to stabilize the treatment outcome, but did not further improve the alignment of incisors. One explanation for the deficient maxillary anterior alignment may be the short treatment time because Keski-Nisula et al.4 reported good correction of maxillary crowding after EGA treatment, which lasted an average of about 3 years. Their subjects were also a few years younger than the current subjects at treatment initiation; their maxillary incisors had not yet erupted. Correcting existing maxillary anterior irregularity seems to require more treatment time and effort than just guiding the erupting incisors into their correct positions in the arch. Four hours of daytime wear seems to be particularly important for the alignment of maxillary incisors, whereas for overjet/overbite correction, regular nighttime wear may sometimes be enough.3,4
Little evidence has been available on treatment outcomes with the EGA in the longer term. Janson et al.7 reported postretention outcomes 6 years after EGA treatment and found that improvements in overjet and sagittal molar relationship were fairly stable in the postretention stage, but overbite and mandibular incisor alignment relapsed considerably. The present results reflected outcomes about 3 years after active treatment and were roughly in line with the aforementioned results, although fundamental methodological differences prevent real comparison. The results were based on EGA treatment alone and included all follow-up participants, irrespective of their compliance or treatment outcome. Conversely, Janson et al.7 selected their participants from a bigger sample of EGA patients based on best treatment outcomes and compliance, and patients with finishing fixed appliance treatment were also included.7 Their reported treatment time was also more than three times longer than that in the current study patients.
During the 3-year retention period, relapse in mean overjet and overbite was statistically significant but clinically small. The 3.3 mm mean overjet with a relatively small range at 12 years of age indicates that most children had normal overjet. Regarding overbite, the relapse between T1 and T2 was half of the initial correction, but the magnitude was less than 1 mm. More important was the finding that the initially common deep bite with soft tissue impingement had totally disappeared at follow-up, suggesting that EGA was effective in eliminating deep bite in the developing dentition.
Studies have shown that distal molar occlusion in the primary and early mixed dentition generally does not self-correct but is transferred into the permanent dentition.13,14 One year was enough for all unilateral class I/II patients to correct to class I, whereas full class II molar relationships more often half-corrected to unilateral class I/II, but continued to correct during the retention period, suggesting that even decreased wear of the EGA as a retainer may promote the development of normal sagittal occlusion. It should be kept in mind that also naturally individual growth of the children contributed to the sagittal correction, although its role was not analyzed separately.
During dental development, nature's mechanisms for aligning the bigger permanent anterior teeth in the dental arch are transverse growth, spaces between primary incisors, and labial inclination of the anterior incisors.15 Concomitantly with sagittal and vertical correction of the occlusion, EGA treatment aligns crowded incisors via transverse and labial expansion of the anterior segment.1,2,4 To achieve stability, the space must be gained before the eruption of permanent canines, when natural transverse growth of the dental arches can be used in the treatment.15,16 The space in the anterior segment is gained by choosing an EGA that is one to two sizes larger in the incisal area than the measured mesio-distal width of the incisors. However, care must be taken to ensure that the oversized EGA feels comfortable and does not reduce a patient's willingness to wear it.
Methods for evaluating anterior irregularity/space discrepancy from the early mixed to the permanent dentition are limited because common indices, for example, LII, are applicable only in the permanent dentition. Therefore, a modified method proposed by Moyers was used to examine changes in anterior space conditions.15 Referring to Moorrees, a −1.5 mm arch length/tooth size discrepancy at T0 as a cut-off point for crowding was applied, and minor space discrepancies as well as spacing were regarded as normal for that developmental stage.8,14 In the current study, the improvement of lower anterior crowding during EGA treatment consisted of labial expansion and enhanced transverse growth, including natural growth until the eruption of the canines, that could not be separated in this study design. The increase of intercanine width in children who initially had mandibular crowding may indicate that EGA treatment in the early mixed dentition has the potential to “normalize” transverse alveolar development in children with lower anterior crowding. At age 12, the mean mandibular intercanine width in the patients (26 mm, SD ± 1.1) did not differ from the corresponding value of Finnish children of same age and with normal occlusion.17
Maintaining patients' interest in retaining the treatment result was a challenge. According to the evidence, compliance with a removable retainer declined with increasing time from termination of active orthodontic treatment.18 This was also observed among the current study participants because only one third had good compliance during retention, which resulted in better stability of overjet and overbite when compared with those with compromised compliance. However, this should be interpreted with care because patients tend to overestimate their use of appliances.19,20
CONCLUSIONS
Early correction of increased overjet, overbite, and class II molar relation with EGA is maintainable and can also be effective in the permanent dentition, provided the EGA is worn regularly as a retainer.
During the early mixed-dentition stage, postponing treatment by 1 year may not influence the treatment outcome.
REFERENCES
- 1.Bergersen EO. The eruption guidance applinaces:how it works,how to use it. Funct Orthod. 1984;131:28–29. [PubMed] [Google Scholar]
- 2.Bergersen EO. The eruption guidance myofunctional appliance:case selection, timing,motivation,indications and contraindications in its use. Funct Orthod. 1985;2:17–21. 24. [PubMed] [Google Scholar]
- 3.Methenitou S BS, Ramamathan G, Bergersen EO. The prevention of overbite and overjet development in the 3 to 8 year old by controlled nighttime guidance of incisal eruption:a study of 43 individuals. J Pedod. 1990;14:218–230. [PubMed] [Google Scholar]
- 4.Keski-Nisula K, Hernesniemi R, Heiskanen M, Keski-Nisula L, Varrela J. Orthodontic intervention in the early mixed dentition: A prospective, controlled study on the effects of the eruption guidance appliance. Am J Orthod Dentofacial Orthop. 2008;133(2):254–260. doi: 10.1016/j.ajodo.2006.05.039. [DOI] [PubMed] [Google Scholar]
- 5.Janson GRP, da Silva CCA, Bergersen EO, Henriques JFC, Pinzan A. Eruption guidance effects in the treatment of Class II,Divison 1 maloccusions. Am J Orthod Dentofacial Orthop. 2000;117:119–129. doi: 10.1016/s0889-5406(00)70222-8. [DOI] [PubMed] [Google Scholar]
- 6.Myrlund R, Dubland M, Keski-Nisula K, Kerosuo H. One year treatment effects of the eruption guidance appliance in 7- to 8-year-old children: a randomized clinical trial. Eur J Orthod. 2015;37:128–134. doi: 10.1093/ejo/cju014. [DOI] [PubMed] [Google Scholar]
- 7.Janson G, Nakamura A, Chiqueto K, Castro R, de Freitas MR, Henriques JFC. Treatment stability with the eruption guidance appliance. Am J Orthod Dentofacial Orthop. 2007;131:717–728. doi: 10.1016/j.ajodo.2005.04.048. [DOI] [PubMed] [Google Scholar]
- 8.Moorrees CFA, Chadha JM. Available Space For The Incisors During Dental Development - A Growth Study Based On Physiologic Age. Angle Orthod. 1965;35:12–22. doi: 10.1043/0003-3219(1965)035<0012:ASFTID>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Little RM. The Irregularity Index: A quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 10.Little RM, Riedel RA, Artun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop. 1988;93:423–428. doi: 10.1016/0889-5406(88)90102-3. [DOI] [PubMed] [Google Scholar]
- 11.El-Batoui A, Øgaard B, Bishara SE. Longitudinal cephalometric standards for Norwegians between the ages of 6 and 18 years. Eur J Orthod. 1994;16:501–509. doi: 10.1093/ejo/16.6.501. [DOI] [PubMed] [Google Scholar]
- 12.Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 13.Bishara SE, Hoppens BJ, Jakobsen JR, Kohout FJ. Changes in the molar relationship between the deciduous and permanent dentitions: A longitudinal study. Am J Orthod Dentofacial Orthop. 1988;93:19–28. doi: 10.1016/0889-5406(88)90189-8. [DOI] [PubMed] [Google Scholar]
- 14.Moorrees CFA, Grøn A-M, Lebret LML, Yen PKJ, Fröhlich FJ. Growth studies of the dentition: A review. Am J Orthod. 1969;55:600–616. doi: 10.1016/0002-9416(69)90037-2. [DOI] [PubMed] [Google Scholar]
- 15.Moyers RE. Vol. 126. Chicago: 1991. Handbook of orthodontics 4th ed; pp. 235–238. [Google Scholar]
- 16.Bishara SE, Ortho D, Jakobsen JR, Treder J, Nowak A. Arch width changes from 6 weeks to 45 years of age. Am J Orthod Dentofacial Orthop. 1997;111:401–409. doi: 10.1016/s0889-5406(97)80022-4. [DOI] [PubMed] [Google Scholar]
- 17.Heikinheimo K, Nyström M, Heikinheimo T, Pirttiniemi P, Pirinen S. Dental arch width, overbite,and overjet in a Finnish population with normal occlusion between the ages of 7 and 32 years. Eur J Orthod. 2012;34:418–426. doi: 10.1093/ejo/cjr025. [DOI] [PubMed] [Google Scholar]
- 18.Pratt MC, Kluemper GT, Lindstrom AF. Patient compliance with orthodontic retainers in the postretention phase. Am J Orthod Dentofacial Orthop. 2011;140:196–201. doi: 10.1016/j.ajodo.2010.02.035. [DOI] [PubMed] [Google Scholar]
- 19.Pauls A, Nienkemper M, Panayotidis A, Wilmes B, Drescher D. Effects of wear time recording on the patient's compliance. Angle Orthod. 2013;83:1002–1008. doi: 10.2319/010913-25.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hyun P, Preston CB, Al-Jewair TS, Park-Hyun E, Tabbaa S. Patient compliance with Hawley retainers fitted with the SMART® sensor: A prospective clinical pilot study. Angle Orthod. 2015;85:263–269. doi: 10.2319/030814-163.1. [DOI] [PMC free article] [PubMed] [Google Scholar]