Abstract
Background
Resilience can be defined as the maintenance or quick recovery of mental health during or after periods of stressor exposure, which may result from a potentially traumatising event, challenging life circumstances, a critical life transition phase, or physical illness. Healthcare professionals, such as nurses, physicians, psychologists and social workers, are exposed to various work‐related stressors (e.g. patient care, time pressure, administration) and are at increased risk of developing mental disorders. This population may benefit from resilience‐promoting training programmes.
Objectives
To assess the effects of interventions to foster resilience in healthcare professionals, that is, healthcare staff delivering direct medical care (e.g. nurses, physicians, hospital personnel) and allied healthcare staff (e.g. social workers, psychologists).
Search methods
We searched CENTRAL, MEDLINE, Embase, 11 other databases and three trial registries from 1990 to June 2019. We checked reference lists and contacted researchers in the field. We updated this search in four key databases in June 2020, but we have not yet incorporated these results.
Selection criteria
Randomised controlled trials (RCTs) in adults aged 18 years and older who are employed as healthcare professionals, comparing any form of psychological intervention to foster resilience, hardiness or post‐traumatic growth versus no intervention, wait‐list, usual care, active or attention control. Primary outcomes were resilience, anxiety, depression, stress or stress perception and well‐being or quality of life. Secondary outcomes were resilience factors.
Data collection and analysis
Two review authors independently selected studies, extracted data, assessed risks of bias, and rated the certainty of the evidence using the GRADE approach (at post‐test only).
Main results
We included 44 RCTs (high‐income countries: 36). Thirty‐nine studies solely focused on healthcare professionals (6892 participants), including both healthcare staff delivering direct medical care and allied healthcare staff. Four studies investigated mixed samples (1000 participants) with healthcare professionals and participants working outside of the healthcare sector, and one study evaluated training for emergency personnel in general population volunteers (82 participants). The included studies were mainly conducted in a hospital setting and included physicians, nurses and different hospital personnel (37/44 studies).
Participants mainly included women (68%) from young to middle adulthood (mean age range: 27 to 52.4 years). Most studies investigated group interventions (30 studies) of high training intensity (18 studies; > 12 hours/sessions), that were delivered face‐to‐face (29 studies). Of the included studies, 19 compared a resilience training based on combined theoretical foundation (e.g. mindfulness and cognitive‐behavioural therapy) versus unspecific comparators (e.g. wait‐list). The studies were funded by different sources (e.g. hospitals, universities), or a combination of different sources. Fifteen studies did not specify the source of their funding, and one study received no funding support.
Risk of bias was high or unclear for most studies in performance, detection, and attrition bias domains.
At post‐intervention, very‐low certainty evidence indicated that, compared to controls, healthcare professionals receiving resilience training may report higher levels of resilience (standardised mean difference (SMD) 0.45, 95% confidence interval (CI) 0.25 to 0.65; 12 studies, 690 participants), lower levels of depression (SMD −0.29, 95% CI −0.50 to −0.09; 14 studies, 788 participants), and lower levels of stress or stress perception (SMD −0.61, 95% CI −1.07 to −0.15; 17 studies, 997 participants). There was little or no evidence of any effect of resilience training on anxiety (SMD −0.06, 95% CI −0.35 to 0.23; 5 studies, 231 participants; very‐low certainty evidence) or well‐being or quality of life (SMD 0.14, 95% CI −0.01 to 0.30; 13 studies, 1494 participants; very‐low certainty evidence). Effect sizes were small except for resilience and stress reduction (moderate). Data on adverse effects were available for three studies, with none reporting any adverse effects occurring during the study (very‐low certainty evidence).
Authors' conclusions
For healthcare professionals, there is very‐low certainty evidence that, compared to control, resilience training may result in higher levels of resilience, lower levels of depression, stress or stress perception, and higher levels of certain resilience factors at post‐intervention.
The paucity of medium‐ or long‐term data, heterogeneous interventions and restricted geographical distribution limit the generalisability of our results. Conclusions should therefore be drawn cautiously. The findings suggest positive effects of resilience training for healthcare professionals, but the evidence is very uncertain. There is a clear need for high‐quality replications and improved study designs.
Plain language summary
Psychological interventions to foster resilience in healthcare professionals
Background The work of healthcare professionals (e.g. nurses, physicians, psychologists, social workers) can be very stressful. They often carry a lot of responsibility and are required to work under pressure. This can adversely affect their physical and mental health. Interventions to protect them against such stresses are known as resilience interventions. Previous systematic reviews suggest that resilience interventions can help workers cope with stress and protect them against adverse consequences for their physical and mental health.
Review question Do psychological interventions designed to foster resilience improve resilience, mental health and other factors associated with resilience in healthcare professionals?
Search dates The evidence is current to June 2019. The results of an updated search of four key databases in June 2020 have not yet been included in the review.
Study characteristics We found 44 randomised controlled trials (studies in which participants are assigned to either an intervention or a control group by a procedure similar to tossing a coin). The studies tested a range of resilience interventions in participants aged on average between 27 and 52.4 years.
Healthcare professionals were the focus of 39 studies, with a total of 6892 participants. Four studies included mixed samples (1000 participants) of healthcare professionals and non‐healthcare participants. One study of resilience training for emergency workers examined 82 volunteers.
Of the included studies, 19 compared a combined resilience intervention (e.g. mindfulness and cognitive‐behavioural therapy) versus unspecific comparators (e.g. a wait‐list control receiving the training after a waiting period). Most interventions (30/44) were performed in groups, with high training intensity of more than 12 hours or sessions (18/44), and were delivered face‐to‐face (i.e. with direct contact and face‐to‐face meetings between the intervention provider and the participants; 29/44).
The included studies were funded by different sources (e.g. hospitals, universities), or a combination of different sources. Fifteen studies did not specify the source of their funding, and one study received no funding support.
Certainty of the evidence A number of things reduce the certainty about whether or not resilience interventions are effective. These include limitations in the methods of the studies, different results across studies, the small number of participants in most studies, and the fact that the findings are limited to certain participants, interventions and comparators.
Key results For healthcare professionals, resilience training may improve resilience, and may reduce symptoms of depression and stress immediately after the end of treatment. Resilience interventions do not appear to reduce anxiety symptoms or improve well‐being. However, the evidence found in this review is limited and very uncertain. This means that, at present, we have very little confidence that resilience interventions make a difference to these outcomes. Further research is very likely to change the findings.
Very few studies reported on the longer‐term impact of resilience interventions. Studies used a variety of different outcome measures and intervention designs, making it difficult to draw general conclusions from the findings. Potential adverse events were only examined in three studies, showing no undesired effects. More research is needed of high methodological quality and with improved study designs.
Summary of findings
Summary of findings 1. Resilience interventions compared to control condition for healthcare professionals.
| Resilience interventions compared to control condition for healthcare professionals | ||||||
|
Patient or population: healthcare professionals including healthcare staff delivering direct medical care (e.g. nurses, physicians, hospital personnel) and allied healthcare staff (e.g. social workers, psychologists); aged 18 years and older, irrespective of health status Setting: Any healthcare sectors (e.g. psychiatric departments, intensive care unit, surgery, family medicine, internal medicine) Intervention: Any psychological resilience intervention focused on fostering resilience or the related concepts of hardiness or post‐traumatic growth by strengthening well‐evidenced resilience factors that are thought to be modifiable by training (see Appendix 3), irrespective of content, duration, setting or delivery mode Comparison: no intervention, wait‐list control, treatment as usual (TAU), active control, attention control | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with control | Risk with resilience interventions | |||||
|
Resilience Measured by: investigators measured resilience using different instruments; higher scores mean higher resilience Timing of outcome assessment: post‐intervention |
See comment | The mean resilience score in the intervention groups was, on average, 0.45 standard deviations higher (0.25 higher to 0.65 higher) | ‐ | 690 (12 RCTs) | ⊕⊝⊝⊝ Very lowa | SMD of 0.45 represents a moderate effect size (Cohen 1988b). |
|
Mental health and well‐being: anxiety Measured by: investigators measured anxiety using different instruments; lower scores mean lower anxiety Timing of outcome assessment: post‐intervention |
See comment | The mean anxiety score in the intervention groups was, on average, 0.06 standard deviations lower (0.35 lower to 0.23 higher) | ‐ | 231 (5 RCTs) | ⊕⊝⊝⊝ Very lowb | SMD of 0.06 represents a small effect size (Cohen 1988b). |
|
Mental health and well‐being: depression Measured by: investigators measured depression using different instruments; lower scores mean lower depression Timing of outcome assessment: post‐intervention |
See comment | The mean depression score in the intervention groups was, on average, 0.29 standard deviations lower (0.50 lower to 0.09 lower) | ‐ | 788 (14 RCTs) | ⊕⊝⊝⊝ Very lowc | SMD of 0.29 represents a small effect size (Cohen 1988b). |
|
Mental health and well‐being: stress or stress perception
Measured by: investigators measured stress or stress perception using different instruments; lower scores mean lower stress or stress perception Timing of outcome assessment: post‐intervention |
See comment | The mean stress or stress perception score in the intervention groups was, on average, 0.61 standard deviations lower (1.07 lower to 0.15 lower) | ‐ | 997 (17 RCTs) | ⊕⊝⊝⊝ Very lowd | SMD of 0.61 represents a moderate effect size (Cohen 1988b). |
|
Mental health and well‐being: well‐being or quality of life Measured by: investigators measured well‐being or quality of life using different instruments; higher scores mean higher well‐being or quality of life Timing of outcome assessment: post‐intervention |
See comment | The mean well‐being or quality of life score in the intervention groups was, on average, 0.14 standard deviations higher (0.01 lower to 0.30 higher) | ‐ | 1494 (13 RCTs) |
⊕⊝⊝⊝ Very lowe | SMD of 0.14 represents a small effect size (Cohen 1988b). |
| Adverse events | There were no adverse events reported in association with study participation in three studies. | ‐ | 784 (3 RCTs) |
⊕⊝⊝⊝ Very lowf | ‐ | |
|
*The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RCT: Randomised controlled trial; SD: standard deviation;SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aDowngraded two levels due to study limitations (unclear risk of selection and detection bias, high and unclear risk of attrition bias, high risk of performance bias), one level due to unexplained inconsistency (I2 = 41%), and one level due to indirectness (studies limited to certain participants (young and middle‐aged adults), interventions (e.g. group setting, face‐to‐face delivery, moderate and high intensity, mindfulness‐based training and combination) and comparators (no intervention, wait‐list)). bDowngraded two levels due to study limitations (unclear risk of selection and detection bias, unclear and high risk of performance bias, high risk of attrition bias), one level due to indirectness (studies limited to certain participants (middle‐aged adults)), and two levels due to imprecision (< 400 participants; 95% CI wide and inconsistent). cDowngraded two levels due to study limitations (unclear risk of selection and detection bias, unclear and high risk of performance bias, high risk of attrition bias), one level due to unexplained inconsistency (I2 = 42%), one level due to indirectness (studies limited to certain participants (middle‐aged adults), interventions (e.g. group setting, face‐to‐face delivery, moderate and high intensity, mindfulness‐based training and combination) and comparators (no intervention)), and one level due to imprecision (95% CI wide and inconsistent). dDowngraded two levels due to study limitations (unclear risk of selection and detection bias, high and unclear risk of attrition bias, high risk of performance bias), one level due to unexplained inconsistency (I2 = 90%), and one level due to indirectness (studies limited to certain participants (young and middle‐aged adults), interventions (e.g. group setting, face‐to‐face delivery, moderate and high intensity, mindfulness‐based training and combination) and comparators (no intervention, wait‐list)). eDowngraded two levels due to study limitations (unclear risk of selection and detection bias, unclear and high risk of attrition bias, high risk of performance bias), one level due to unexplained inconsistency (I2 = 31%), one level due to indirectness (studies limited to certain participants (young and middle‐aged adults), interventions (e.g. group setting, face‐to‐face delivery, moderate and high intensity, mindfulness‐based trainings and combination) and comparators (no intervention, wait‐list)), and one level due to imprecision (95% CI wide and inconsistent). fDowngraded two levels due to study limitations (unclear risk of selection and detection bias, high and unclear risk of attrition and other bias (no or unclear systematic and validated assessment of adverse events), high risk of performance bias), and one level due to indirectness (studies limited to certain interventions (e.g. combined setting, face‐to‐face delivery, high intensity, mindfulness‐based training)).
Background
For a description of abbreviations used in this review, please see Appendix 1.
Description of the condition
Since the introduction of Antonovsky’s salutogenesis as a basis for health promotion (Antonovsky 1979), and the Ottawa Charter for Health Promotion (WHO 1986), the concept of resilience has stimulated extensive research. Resilience describes the phenomenon in which an individual does not, or only temporarily experiences mental health problems despite being subjected to psychological or physical stressors of short (acute) or long (chronic) duration (Kalisch 2015; Kalisch 2017). By definition, resilience presupposes the exposure to substantial risk or adversity (Earvolino‐Ramirez 2007; Jackson 2007; Luthar 2000a; Masten 2001).
Stressor exposure in healthcare professionals and its consequences
Healthcare professionals are exposed to a large number of environmental and psychosocial stressors (Aiken 2001; Hannigan 2004; Jennings 2008; Kumar 2016; Lambert 2004). Substantial patient‐related stressors include, for example, physical or verbal aggression from patients or relatives or both, (daily) exposure to diseases, suffering, and death or even patient suicides (Jackson 2007; McAllister 2009; McCann 2013). Work‐related stressors may include time pressure, the responsibility of medical decision‐making, as well as social expectations of health professionals (Lateef 2011; McAllister 2009; McCann 2013). Healthcare staff moreover can be exposed to many organisational adversities such as interdisciplinary teamwork, inflexible hierarchies, staff downsizing, increasing administrative effort and technological changes such as new diagnostic tools (Jackson 2007; McAllister 2009; McCann 2013; Zander 2013). Especially in the nursing professions, high job demands are linked to low financial rewards.
Chronic stressor exposure has a potential impact on mental health. Some of the above‐mentioned factors were shown to be associated with employees' mental health problems in general (Gray 2019; Harvey 2017; Marchand 2015). For the healthcare sector in particular, for example, high workload (e.g. long working hours; Adriaenssens 2015; Anderson 2017; Van Ham 2006; Shanafelt 2009; Shanafelt 2016), demanding work situations (e.g. in emergency ward; Adriaenssens 2011; Adriaenssens 2015), workplace violence (Pekurinen 2017; Shi 2017), lack of recognition (Adriaenssens 2015; Van Ham 2006) and administrative burdens (Anderson 2017; Van Ham 2006) have been shown to be associated with burnout symptoms and mental health problems. Physicians and other employees in the healthcare industry have been shown to report debilitating sleep disorders (Kim 2018b; Schlafer 2014). Healthcare professionals are at increased risk of developing burnout symptoms (e.g. high emotional exhaustion; Aiken 2001; Hannigan 2004) and stress‐related mental disorders (Gracino 2016; Harvey 2009; Robertson 2010; Weinberg 2000; Wieclaw 2006), such as depression (Frank 1999; Gong 2014; Tomioka 2011) and post‐traumatic stress disorder (Jonsson 2003; Mealer 2009; Ong 2016). They also have higher rates of substance misuse (Horsfall 2014) and have been shown to report increased perceived stress (Leonelli 2017). Due to emotional stressors, such as working with traumatised patients, healthcare workers also commonly report compassion fatigue and secondary traumatic stress (Adams 2006). Furthermore, compared to other disciplines, higher suicide rates for healthcare staff (e.g. physicians) have been demonstrated (Horsfall 2014; Meltzer 2008). In the face of chronic stressors and the resulting impact on physical and mental health, healthcare workers have higher numbers of days absent due to illness (Moberly 2018; Michie 2003) and report reduced job satisfaction (Kuburović 2016; Lu 2016), which is often associated with job termination and understaffing, especially in the nursing sector. For example, based on a cross‐sectional observational study in 10 European countries, Heinen 2013 found that 5% to 17% of nurses from participating medical and surgical hospital wards intended to leave the profession. For new nursing‐school graduates, high first‐year turnover rates (i.e. the percentage of employees leaving in the first year after training) have been reported (35% to 61%; Pine 2007).
Overall, based on these findings, the concept of resilience has become increasingly important in healthcare professionals in recent years (Hart 2014; Jackson 2007; McAllister 2009; McCann 2013).
Definition of resilience
Three different approaches have been discussed for a definition of resilience (Hu 2015; Kalisch 2015). Trait resilience is defined as personal resources or static, positive personality characteristics that enhance individual adaptation (Block 1996; Nowack 1989; Wagnild 1993). This approach has largely been superceded by a view of resilience as an outcome rather than a static personality trait (Kalisch 2015; Mancini 2009); that is, mental health despite significant stress or trauma. According to this outcome‐oriented definition, resilience is partially determined by several resilience factors (Kalisch 2015). To date, a large range of genetic, psychological, social and environmental factors have been discussed that often overlap and may interact (Bengel 2012; Bonanno 2013; Carver 2010; Connor 2006; Earvolino‐Ramirez 2007; Feder 2011; Forgeard 2012; Haglund 2007; Iacoviello 2014; Kuiper 2012; Mancini 2009; Michael 2003; Ozbay 2007; Rutten 2013; Sapienza 2011; Sarkar 2014; Southwick 2005; Southwick 2012; Stewart 2011; Wu 2013; Zauszniewski 2010). Psychosocial resilience factors that are well‐evidenced according to the current state of knowledge and are thought to be modifiable include: meaning or purpose in life, a sense of coherence, positive emotions, hardiness, self‐esteem, active coping, self‐efficacy, optimism, social support, cognitive flexibility (including positive reappraisal and acceptance), and religiosity or spirituality or religious coping (see Appendix 2: level 1). Most recently, resilience has been conceptualised as a multidimensional and dynamic process (Johnston 2015; Kalisch 2015; Kent 2014; Mancini 2009; Norris 2009; Rutten 2013; Sapienza 2011; Southwick 2012). This resilient process is characterised either by a trajectory of undisturbed mental health during or after adversities, or by temporary dysfunctions followed by successful recovery (Kalisch 2015). In general, resilience is viewed as the outcome of an interaction between individuals and their environment (Cicchetti 2012; Rutten 2013), which may be influenced through personal (e.g. optimism) as well as environmental (e.g. social support) resources (Haglund 2007; Iacoviello 2014; Kalisch 2015; Southwick 2005; Wu 2013). As such, resilience is modifiable and can be improved by interventions (Bengel 2012; Connor 2006; Southwick 2011).
Interventions to foster resilience
Interventions to foster resilience have been developed for and conducted in a variety of clinical and non‐clinical populations using various formats, such as multimedia programmes or face‐to‐face settings, and have been delivered in a group or individual context (see Bengel 2012 and Southwick 2011 for an overview). To date, several training programmes that focus specifically on fostering resilience in healthcare professionals have also been tested (e.g. Mealer 2014; Sood 2011). However, the empirical evidence about the efficacy of these interventions is still unclear and requires further research.
Description of the intervention
There is little consensus so far about when to consider a programme as ‘resilience training’, or what components are needed for effective programmes (Leppin 2014). The diversity across resilience‐training programmes in their theoretical assumptions, the operationalisation of the construct, and the inclusion of core components reflect the current state of knowledge (Joyce 2018; Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016), with leading guidelines still under discussion (compare Kalisch 2015; Robertson 2015).
Most training programmes, whether individual or group‐based, are implemented face‐to‐face. Alternative formats include online interventions or combinations of different formats. Resilience‐training programmes often use methods such as discussions, role plays, practical exercises and homework to reinforce training content. Moreover, they mostly contain a psycho‐educative element to provide information on the concept of resilience or specific training elements (e.g. cognitive restructuring).
In general, resilience interventions are based on different psychotherapeutic approaches: cognitive‐behavioural therapy (CBT; Abbott 2009); acceptance and commitment therapy (ACT; Ryan 2014); mindfulness‐based therapy (Geschwind 2011); attention and interpretation therapy (AIT; Sood 2014); problem‐solving therapy (Bekki 2013); and stress inoculation (Farchi 2010). A number of training programmes focus on fostering single or multiple psychosocial resilience factors, without being assignable to a certain approach. Few interventions base their work on a defined resilience model (Schachman 2004; Steinhardt 2008).
How the intervention might work
Depending on the underlying resilience concept, resilience interventions target different resources and skills. The theoretical foundations of training programmes and the hypotheses on how they might maintain or regain mental health are as diverse as their content. Currently, no empirically‐validated theoretical framework exists that outlines the mode of action of resilience interventions (Bengel 2012; Leppin 2014).
As resilience as an outcome is determined by several potentially modifiable resilience factors (see Description of the condition), resilience interventions might work by strengthening these factors (see Appendix 3 for examples of possible training methods). However, depending on the underlying theoretical foundation, there are different theories of change on how certain factors and hence resilience might be affected.
From the 'cognitive‐behavioural perspective', stress‐related mental dysfunctions (e.g. depression) are considered to be the result of dysfunctional thinking (Beck 2011; Benjamin 2011). When confronted with adversity, people show maladaptive behavioural responses or experience negative mood states, or both, due to irrational cognitions (Beck 1976; Ellis 1975). This is in line with other stress and resilience theories, assuming that not the stressor itself but its cognitive appraisal may lead to stress reactions (e.g. Kalisch 2015; Lazarus 1987). Modifying cognitive processes into more adaptive patterns of thought will therefore probably produce more adaptive responses to stress (Beck 1964). By challenging an individual’s maladaptive thoughts and by teaching coping strategies, CBT‐based resilience interventions might be beneficial in promoting the resilience factors of cognitive flexibility and active coping.
As one form of CBT, 'stress inoculation therapy’ is based on the assumption that exposing individuals to milder forms of stress can strengthen coping strategies and the individual’s confidence in using his/her coping repertoire (Meichenbaum 2007). Resilience‐training programmes grounded in stress inoculation therapy might therefore foster resilience by enhancing factors such as self‐efficacy.
Problem‐solving therapy is closely related to CBT and is based on problem‐solving theory. According to the ’problem‐solving’ model of stress and adaptation, effective problem‐solving can attenuate the negative effects of stress and adversity on well‐being by moderating or mediating the effects of stressors on emotional distress (Nezu 2013). Resilience interventions based on problem‐solving that enhance an individual’s positive problem orientation and resourceful problem‐solving might foster the participants’ psychological adaptation to stress by increasing the resilience factor of active coping.
According to 'acceptance and commitment therapy' (ACT) (Hayes 2004; Hayes 2006), psychopathology is primarily the consequence of psychological inflexibility (Hayes 2006), which is also relevant when an individual is confronted with stressors. By teaching acceptance and mindfulness skills (e.g. being in contact with the present moment), and also commitment and behaviour‐change skills (e.g. values, committed action), several resilience factors might be fostered in ACT‐based resilience interventions (e.g. cognitive flexibility, purpose in life). In particular, the acceptance of a full range of emotions taught in ACT might result in a better adjustment to stressful conditions.
In 'mindfulness‐based therapy' (e.g. mindfulness‐based stress reduction (MBSR; Stahl 2010); attention and interpretation therapy (AIT; Sood 2010)), mindfulness is characterised by the non‐judgmental awareness of the present moment and its accompanying mental phenomena (e.g. body sensations, thoughts, emotions). Since practitioners learn to accept whatever occurs in the present moment, they are thought to adapt more efficiently to stressors (Grossman 2004; Shapiro 2005). As being more aware of the 'here and now' possibly enhances the sensitivity for positive aspects in life, mindfulness‐based resilience interventions might also help participants to gain a brighter outlook for the future (i.e. optimism) or to experience positive emotions more regularly. Teaching mindfulness might also increase participants’ cognitive flexibility by learning to accept negative situations and emotions.
Independent of the underlying theory, resilience training might work differently depending on the respective 'delivery format' and 'intervention setting' (Robertson 2015; Vanhove 2016). For example, interventions implemented face‐to‐face could work better than online formats in increasing resilience, due to the more direct contact between trainers and participants (Vanhove 2016), which might also increase compliance. Resilience training in an individual setting could be more efficient than group‐based interventions as trainers might be better able to attend to participants’ individual needs and provide feedback more easily (Vanhove 2016). On the other hand, group‐based interventions could enhance the participants’ social resources. No previous review has examined the role of training duration on effect sizes of resilience interventions. As participants have the opportunity to apply the taught skills in daily life, high‐intensity resilience interventions that include weekly sessions over several weeks (e.g. combined with homework assignments or daily practice) could be more efficient than low‐intensity training (e.g. single session). Joyce 2018, who examined the role of the theoretical foundation of resilience interventions for the first time, found positive effect sizes on resilience for CBT‐based, mindfulness‐based and mixed interventions (e.g. CBT and mindfulness) compared to control. However, differences in the effects of resilience training based on other theoretical foundations have not been considered so far.
Why it is important to do this review
To date, a large number of systematic reviews and meta‐analyses have investigated various forms of intervention to foster healthcare professionals' mental health (see Appendix 4). Although some of these reviews also identified interventions to foster resilience (e.g. Lamothe 2016; Ruotsalainen 2015), the primary review question did not specifically refer to identifying such programmes.
A considerable number of systematic reviews and meta‐analyses of interventions to foster resilience (see Appendix 4) have synthesised the efficacy of resilience‐training programmes in clinical and non‐clinical adult populations (Bauer 2018; Joyce 2018; Leppin 2014; Macedo 2014; Massey 2019; Milne 2016; Pallavicini 2016; Pesantes 2015; Petriwskyj 2016; Reyes 2018; Robertson 2015; Skeffington 2013; Townshend 2016; Vanhove 2016; Van Kessel 2014; Wainwright 2019) or at least searched for 'resilience' and related constructs (Deady 2017; Tams 2016). Thus far, there are only three relevant meta‐analyses (Joyce 2018; Leppin 2014; Vanhove 2016). Overall, previous reviews agree in their conclusion that resilience interventions can generally improve resilience, mental health and (job) performance. Nevertheless, there are some methodological and quality differences between the reviews, which complicate statements about the efficacy of resilience training or result in a variety of effect sizes (see Appendix 4). These include, for example, heterogeneous eligibility criteria and definitions of resilience training, rather simple and limited search strategies, the lack of a review protocol or PROSPERO registration for most reviews, and different guidelines for the conduct and reporting of the review.
With respect to healthcare professionals (see Appendix 4), 11 systematic reviews (Cleary 2018; Concilio 2019; Delgado 2017; Elliott 2012; Foster 2019; Fox 2018; Gillman 2015; Gilmartin 2017; Robertson 2016; Rogers 2016; Wright 2017) and one meta‐analysis (Lavin Venegas 2019) have synthesised evidence on the efficacy of resilience‐training programmes in this target group, with two other reviews also searching for 'resilience' (Hunter 2016; Pezaro 2017). The 14 publications either investigated healthcare staff in general, in primary or in dementia care (Cleary 2018); specific groups of healthcare workers (e.g. physicians, Fox 2018); or combinations of healthcare professionals and healthcare students (Gilmartin 2017). Overall, they found mixed results for the efficacy of resilience‐training programmes. On the one hand, they found some benefits to healthcare professionals; for example, in improving resilience or mental health outcomes (e.g. anxiety, perceived stress; Cleary 2018; Gilmartin 2017; Pezaro 2017; Rogers 2016; Wright 2017). On the other hand, as pointed out by many authors of previous publications (Fox 2018; Lavin Venegas 2019), the reviews' conclusions are also restricted by current limitations of resilience intervention research (e.g. heterogeneous definitions of resilience, low methodological rigour of studies). Comparable to reviews in other populations, the publications also suffer from methodological weaknesses that limit the robustness of their findings (see Appendix 4). Most importantly, the number of RCTs included in previous reviews is rather limited (0 to 9 RCTs among 5 to 33 included studies in the 14 reviews), and the search period covered by the reviews is up to June 2018 (Foster 2019), thus precluding any conclusions about the efficacy of resilience interventions in healthcare professionals that have been developed since then.
In our review, which seeks to address the methodological weaknesses of previous reviews, we were particularly interested in psychological resilience interventions offered to this target group. The interventions had to be scientifically founded, that is, they had to address one or more of the resilience factors stated above that are known to be associated with resilience in adults according to the current state of research (compare Appendix 2: levels 1a to 1c). They also had to state the intention of promoting resilience or a related construct (hardiness, post‐traumatic growth). Lastly, the trained population had to fulfil the condition of potential stress or trauma exposure (the concept implicated for resilience); that is, being employed as a healthcare professional (see Description of the condition), in order to clearly distinguish genuine resilience interventions from other interventions focused on fostering associated constructs such as mental health (Windle 2011a).
Resilience as a concept of prevention is highly current, and there is increasing interest worldwide in promoting mental health and preventing disease (WHO 1986; WHO 2004). Due to chronic stressor exposure in health professions, and the potential negative consequences for the employees’ health, patient care and economic consequences (see Description of the condition), healthcare workers are viewed as one of the most important target groups for resilience interventions (McCann 2013). This review therefore aims to provide further and more detailed evidence about which interventions are most likely to foster resilience and prevent stress‐related mental health problems in healthcare professionals. The evidence base for this review might contribute to improving existing interventions and to facilitating the future development of training programmes. In this way, researchers, practitioners and policy‐makers could benefit from our work.
Objectives
To assess the effects of interventions to foster resilience in healthcare professionals, that is, healthcare staff delivering direct medical care (e.g. nurses, physicians, hospital personnel) and allied healthcare staff (e.g. social workers, psychologists) (see Differences between protocol and review).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), including cluster‐RCTs.
Types of participants
Adults aged 18 years and older, who are employed as healthcare professionals, i.e. healthcare staff delivering direct medical care such as physicians, nurses, hospital personnel, and allied healthcare staff working in health professions, as distinct from medical care (e.g. psychologists, social workers, counsellors, physical therapists, occupational therapists, speech therapists, medical assistants, medical technicians) (see Differences between protocol and review).
Participants were included irrespective of health status.
At the time of the intervention, individuals had to be exposed to potential risk or stressors, which was ensured by focusing on healthcare staff in this review (see Description of the condition; Differences between protocol and review).
We included studies involving mixed samples (e.g. ambulance personnel and firefighters) in the review. These studies were also considered in meta‐analysis (see Data synthesis) if data for healthcare professionals were reported separately or could be obtained by contacting the study authors.
Types of interventions
Any psychological resilience intervention, irrespective of content, duration, setting or delivery mode.
For the purpose of this review, we define psychological resilience interventions as follows: interventions focused on fostering resilience or the related concepts of hardiness or post‐traumatic growth by strengthening well‐evidenced resilience factors that are thought to be modifiable by training (see above and Appendix 2; level 1). In order to use highly objective inclusion criteria, we considered only interventions that explicitly defined the objective of fostering resilience, hardiness, or post‐traumatic growth by using one or more of these terms in the publication (see Differences between protocol and review).
Studies of pharmacological (e.g. treatment with antidepressants) and physical (e.g. exercise) interventions, as well as relaxation techniques (e.g. progressive muscle relaxation), were only considered if these interventions were part of psychological resilience training. We did not include studies that merely examined the efficacy of disorder‐specific psychotherapy (e.g. CBT for depression).
The comparators we considered in this review include no intervention, wait‐list control, treatment as usual (TAU), active control, and attention control. We use the term ‘attention control’ for alternative treatments that mimicked the amount of time and attention received (e.g. by trainer) in the treatment group. We also considered active controls to involve an alternative treatment (no TAU; for example, treatment developed specifically for the study), but that did not control for the amount of time and attention in the intervention group and was not attention control in a narrow sense.
Types of outcome measures
Due to the different ways in which resilience has been operationalised in previous research, resilience as an intervention outcome could not always be guaranteed in studies. We therefore also defined assessments of psychological adaptation (e.g. mental health) as primary outcomes.
Secondary outcomes included a range of psychological factors associated with resilience, according to the current state of knowledge, and were selected based on conceptual clarity and measurability (level 1a and 1b; see Appendix 2).
Measures for the assessment of psychological resilience and psychological adaptation, as well as resilience factors, are specified on the basis of previous reviews of resilience interventions (Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016) and reviews of resilience measurements (Pangallo 2015; Windle 2011b); see Helmreich 2017 and Appendix 5, Appendix 6, Appendix 7 in this review, respectively.
We considered self‐rated and observer‐ or clinician‐rated measures, as well as study outcomes, at all time points. The absence of the primary or secondary outcomes described above was not an exclusion criterion for this review.
Primary outcomes
Resilience*, measured by improvements in specific resilience scales (Bengel 2012; Earvolino‐Ramirez 2007; Pangallo 2015; Windle 2011b), such as the Resilience Scale for Adults (Friborg 2003).
-
Mental health and well‐being, subsumed into the categories below, and measured by improvements in the respective assessment scales, such as the Depression Anxiety and Stress Scale (DASS‐21; Lovibond 1995). See Appendix 6 for further examples.
Anxiety*
Depression*
Stress or stress perception*
Well‐being or quality of life* (e.g. well‐being, life satisfaction, (health‐related) quality of life, vitality, vigour)
Adverse events*
Secondary outcomes
Resilience factors (Bengel 2012; Haglund 2007; Iacoviello 2014; Southwick 2005; Southwick 2012; Wu 2013), whenever they were available as outcomes, assessed by an increase in the respective instruments (e.g. Life Orientation Test ‐ Revised (LOT‐R); Scheier 1994). For further examples see Appendix 7.
Social support
Optimism
Self‐efficacy
Active coping
Self‐esteem
Hardiness (although hardiness is often used as a synonym for resilience in the literature, we conceptualised it as a resilience factor in this review. See Appendix 2)
Positive emotions
We extracted and report data on secondary outcomes whenever they were assessed. If possible, we calculated and reported effect sizes.
Where data were available, we used outcomes marked by an asterisk (*) to generate the ‘Summary of findings’ table. In case of insufficient information, we provide a narrative description of the evidence.
Search methods for identification of studies
We ran the first searches for this review in October 2016, based on the MEDLINE search strategy in the protocol (Helmreich 2017) before changing the inclusion criteria of the review to focus on healthcare professionals (see Differences between protocol and review). For the top‐up searches in June 2019, we added a new section to the original search strategy, using search terms to limit the search to healthcare sector workers and students.
Electronic searches
We searched the electronic sources listed below.
Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 6) in the Cochrane Library, which includes the Cochrane Developmental, Psychosocial and Learning Problems Specialised Register (searched 26 June 2019).
MEDLINE Ovid (1946 to 21 June 2019).
Embase Ovid (1974 to 2019 Week 25).
PsycINFO Ovid (1806 to June Week 3 2019).
CINAHL EBSCOhost (Cumulative Index to Nursing and Allied Health Literature; 1981 to 24 June 2019).
PSYNDEX EBSCOhost (1977 to 24 June 2019).
Web of Science Core Collection Clarivate (Science Citation Index; Social Science Citation Index; Conference Proceedings Citation Index ‐ Social Science & Humanities; Conference Proceedings Citation Index ‐ Science; 1970 to 26 June 2019).
International Bibliography of the Social Sciences ProQuest (IBSS; 1951 to 25 June 2019).
Applied Social Sciences Index & Abstracts ProQuest (ASSIA; 1987 to 24 June 2019).
ProQuest Dissertations & Theses (PQDT; 1743 to 24 June 2019).
Cochrane Database of Systematic Reviews (CDSR; 2019, Issue 6) in the Cochrane Library (searched 26 June 2019).
Database of Abstracts of Reviews of Effects (DARE; 2015, Issue 4) in the Cochrane Library (final issue; searched 27 October 2016)
Epistemonikos (epistemonikos.org; all available years).
ERIC EBSCOhost (Education Resources Information Center Institute of Education Sciences; 1966 to 26 June 2019).
Current Controlled Trials (controlled-trials.com; 1 January 1990 to 24 June 2019).
ClinicalTrials.gov (clinicaltrials.gov; 1 January 1990 to 24 June 2019).
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; who.int/trialsearch; 1 January 1990 to 24 June 2019).
The search strategies for each database are reported in Appendix 8 (up to 2016) and for the revised inclusion criteria Appendix 9 (2016 onwards). We used the Cochrane Highly Sensitive Search Strategy to identify RCTs in Medline (Lefebvre 2019). We adapted the search terms and syntax for other databases. The searches were not restricted by language, publication status or publication format. Our search was limited to the period January 1990 onwards. We applied this restriction to account for the fact that the resilience concept and its operationalisation have developed significantly over the past decades (Fletcher 2013; Hu 2015; Kalisch 2015; Pangallo 2015). Because of the lack of homogeneity for the period 1990 to 2014 (Robertson 2015), it is likely that using a broader time frame would have made it even more difficult to detect resilience‐training studies with similar resilience concepts and assessments. Moreover, it appeared plausible to concentrate on the period 1990 to the present, since the idea of resilience as an outcome and as a modifiable process has only emerged in recent years, and paved the way for the development of resilience‐promoting interventions (Bengel 2009; Southwick 2011). The idea of fostering resilience by specific training was therefore relatively new (Leppin 2014). This can also be seen in the review by Macedo 2014, who searched for studies on resilience interventions every year until 2013 but only found RCTs published after 1990.
As resilience‐training programmes should be adapted to scientific findings on a regular basis, and with the current research focusing on the detection of general resilience mechanisms (Kalisch 2015; Luthar 2000a), the last five years seemed especially important in synthesising the evidence on newly‐developed resilience training.
We performed a further scoping search of four key databases (CENTRAL, CINAHL EBSCOhost, PsycINFO Ovid, ClinicalTrials.gov) in June 2020 prior to the publication of this review. The results are awaiting classification and will be incorporated into the review at the next update.
Searching other resources
In addition to the electronic search, we inspected the reference lists of all included RCTs and relevant reviews, and contacted researchers in the field as well as the authors of selected studies, to check if there are any unpublished or ongoing studies. If data were missing or unclear, we contacted the study author.
Data collection and analysis
In successive sections, we report only the methods we used in this review. Preplanned but unused methods are reported in Table 2.
1. Unused methods table.
| Section | Proposed methods | Reason for non‐use |
| Measures of treatment effect | Dichotomous data We planned to analyse dichotomous outcomes by calculating the risk ratio (RR) of a successful outcome (i.e. improvement in relevant variables) for each trial. We would have expressed uncertainty in each result using 95% confidence intervals (CIs). | We only identified two studies with dichotomous data for depression (West 2014; West 2015). Both studies also provided continuous primary outcome data relevant for this review (burnout) and could be combined in meta‐analysis with other studies reporting continuous outcomes. |
| Unit of analysis issues | Cluster‐randomised trials In cluster‐randomised trials, if the clustering had been ignored and the unit of analysis had been different from the unit of allocation (‘unit‐of‐analysis error’) (Whiting‐O'Keefe 1984), P values might have been artificially small and resulted in false‐positive conclusions (Higgins 2019b). Had we found such cases, we would have accounted for clustering in the data and followed the recommendations given in the literature (Higgins 2019b; White 2005). For those cluster‐randomised trials that did not report correct standard errors, we would have tried to recover correct standard errors by applying the usual formula for the variance inflation factor 1 + (M ‐ 1) ICC, where M is the average cluster size and ICC the intra‐cluster correlation coefficient (Higgins 2019b). Had it not been possible to extract ICC values from the study, we would have used the average ICC of all cluster‐randomised trials in our review that investigated the same primary outcome scale in a similar setting. Had this not been available, we would have used the average ICC of all other cluster‐randomised trials in our review. If no such studies had been available, we would have used ICC = 0.05 as a conservative guess for the primary analysis, and added a sensitivity analysis using ICC = 0.10. We planned to conduct sensitivity analyses based on the unit of randomisation as well as the ICC estimate in cluster‐randomised trials (see Sensitivity analysis). | No cluster‐RCT was included in this review. |
| Multiple treatment groups Had multiple groups in a study been relevant, we would have accounted for the correlation between the effect sizes from multi‐arm studies in a pair‐wise meta‐analysis (Higgins 2019b). We would have treated each comparison between a control group and a treatment group as an independent study. We would have multiplied the standard errors of the effect estimates by an adjustment factor to account for correlation between effect estimates. In doing so, we would have acknowledged heterogeneity between different treatment groups. | For studies with multiple treatment groups, we considered only one intervention group to be relevant for the review and meta‐analyses, on the basis of the independent judgement of two review authors. Thus, in a pair‐wise meta‐analysis we did not have to account for the correlation between the effect sizes for multi‐arm studies. | |
| If there had been an adequate evidence base, we would have considered performing a network meta‐analysis (see Data synthesis). | The evidence base was not sufficient to conduct a network meta‐analysis. | |
| Dealing with missing data | If standard deviations could neither be recovered from reported results nor obtained from the authors, we would have considered single imputation by pooling within‐treatment standard deviations from all other studies, provided that fewer than five studies had missing standard deviations. If more than five studies had missing standard deviations, we would have performed multiple imputation on the basis of the hierarchical model fitted to the non‐missing standard deviations. | We found no studies using the same scale that had missing standard deviations. In addition, missing standard deviations could always be recovered from alternative statistical values or could be obtained from the study authors. |
| Data synthesis | Had a study reported more than one resilience scale, we would have used the scale with better psychometric qualities (as specified in Appendix 3 in Helmreich 2017), to calculate effect sizes. | All studies measuring resilience only used one resilience scale. |
| If a study had provided data from two instruments used equally often in the included RCTs, two review authors (AK, IH) would have identified the appropriate measure through discussion (compare Stoffers‐Winterling 2012). | This did not occur in this review. | |
| Network meta‐analyses (NMAs) would have been merely exploratory and would only have been conducted if the review results had a sufficient and adequate evidence base. Network meta‐analyses offer the possibility of comparing multiple treatments simultaneously (Caldwell 2005). They combine both direct (head‐to‐head) and indirect evidence (Caldwell 2005; Mills 2012), by using direct comparisons of interventions within RCTs, as well as indirect comparisons across trials on the basis of a common reference group (e.g. an identical control group) (Li 2011). As yet, a network meta‐analysis on resilience‐training programmes does not exist. According to Mills 2012, Linde 2016 and the Cochrane Handbook for Systematic Reviews of Interventions (Chaimani 2019), there are three important conditions for the conduct of NMAs: transitivity, homogeneity, consistency. Had an NMA been possible (i.e. the three conditions are fulfilled), we would have conducted an analysis, with expert statistical support as suggested by Cochrane (Chaimani 2019), using a frequentist approach in R (Rücker 2015; Viechtbauer 2010). For sensitivity analyses, the same models would have been fitted by the restricted maximum likelihood method (Piepho 2012; Piepho 2014; Rücker 2015). We would have considered categorising resilience training into seven groups, based on the underlying training concept: (1) cognitive behavioural therapy; (2) acceptance and commitment therapy; (3) mindfulness‐based therapy; (4) attention and interpretation therapy; (5) problem‐solving therapy; (6) stress inoculation therapy; and (7) multimodal resilience training. We might have included additional groups after the full literature search had been conducted. Reference groups that could have been included in the NMA were attention control, wait‐list, treatment as usual or no intervention. We planned to investigate inconsistency and flow of evidence in accordance with recommendations in the literature (e.g. Dias 2008; Chaimani 2019; König 2013; Krahn 2013; Krahn 2014; Lu 2006; Lumley 2002; Rücker 2015; Salanti 2008; White 2012b). |
The evidence base was not sufficient to support a network meta‐analysis. | |
| Summary of findings | Depending on the assessment of heterogeneity and possible effect modifiers (see Subgroup analysis and investigation of heterogeneity), we would have created several ‘Summary of findings’ tables; for example, for the clinical status of study populations or the comparator group. | We identified no consistent effect modifiers over the primary outcomes in subgroup analyses and therefore created no separate ‘Summary of findings’ tables. |
| Sensitivity analysis | If cluster‐randomised trials had been included, we would have performed sensitivity analyses based on the ICC estimate in cluster‐randomised trials that had not adjusted for clustering, by excluding cluster‐RCTs where standard errors were not corrected or corrected only on the basis of an externally‐estimated ICC. In an additional sensitivity analysis, we would have replaced all externally‐estimated ICCs that were less than 0.10, by 0.10. Finally, we would have conducted a sensitivity analysis for the unit of randomisation, by limiting the analysis to individually‐randomised trials. | No cluster‐RCT was included in this review. |
| ICC: Intra‐cluster correlation coefficient; RCT(s): randomised controlled trial(s) | ||
This table provides details of analyses that had been planned and described in the protocol (Helmreich 2017), including revisions made at review stage, but were not applied, as they were not required or not feasible.
Selection of studies
Two review authors (AK, IH) independently screened titles and abstracts in order to determine eligible studies. Clearly irrelevant papers were excluded immediately. At full text level, two review authors (AK, IH), working independently, checked eligibility in duplicate. We calculated inter‐rater reliability at both stages (title and abstract screening and full text screening), resolving any disagreements in study selection by discussion. Where we could not reach a consensus, a third review author (AC or KL) arbitrated. If necessary, we contacted the study authors to seek additional information. We recorded all decisions in a PRISMA flow diagram (Moher 2009).
We assessed the feasibility of the selection criteria a priori, by screening 500 studies in order to attain acceptable inter‐rater reliability (see Differences between protocol and review). There was a good agreement between the review authors (kappa = 0.72), and thus no need to refine or clarify the criteria. For scientific reasons, however, we adapted the eligibility criteria during review development (see Differences between protocol and review).
Data extraction and management
We developed a data extraction sheet (see Appendix 10), based on Cochrane guidelines (Li 2019), and tested it on 10 randomly‐selected included studies. This initial test resulted in sufficient agreement between the review authors. For each included study, two review authors (AK, IH) independently extracted the data in duplicate. The extraction sheet contained the following aspects:
source and eligibility;
study methods (e.g. design);
allocation process;
participant characteristics;
interventions and comparators;
outcomes and assessment instruments (means and standard deviations in any standardised scale);
results;
miscellaneous aspects.
We resolved any disagreements in data collection by discussion. Where we could not reach a consensus, a third review author (AC or KL) arbitrated. If necessary, we contacted the study authors to seek additional information.
Assessment of risk of bias in included studies
Two review authors (AK, IH) independently assessed the risks of bias of the included studies. We checked the risk of bias for each study using the criteria presented in the Cochrane Handbook for Systematic Reviews of Interventions, hereafter referred to as the Cochrane Handbook (Higgins 2011b), and set out in Appendix 11. We resolved any disagreements by discussion or by consulting a third review author (AC or KL). In accordance with Cochrane’s tool for assessing risk of bias (Higgins 2011a), we critically assessed the following domains:
sequence generation and allocation concealment (selection bias);
blinding of participants and personnel (performance bias);
blinding of outcome assessment (detection bias);
incomplete outcome data (attrition bias); and
selective outcome reporting (reporting bias).
We also considered the baseline comparability between study conditions as part of selection bias (random‐sequence generation), which is not defined in the Cochrane Handbook. In the first part of the assessment, we describe what was reported to have happened in the study for each domain, before assigning a judgement about the risk of bias (low, high or unclear) for the entry.
Measures of treatment effect
Dichotomous data
We did not need to use our preplanned methods for analysing dichotomous outcomes (Helmreich 2017), as only two studies reported dichotomous data and both studies also provided continuous data that we were able to combine in a meta‐analysis.
Continuous data
Because the included resilience‐training studies used different measurement scales to assess resilience and related constructs (see Table 3, Table 4), we used the standardised mean difference (SMD) effect sizes (Cohen's d) and their 95% confidence intervals (CIs) for continuous data in the pair‐wise meta‐analyses. We calculated effect sizes on the basis of means, standard deviations and sample sizes for each study condition. Where data were not provided, we computed Cohen's d from alternative statistics (e.g. t test, change scores). We assessed the magnitude of effect for continuous outcomes using the criteria for interpreting SMDs suggested in the Cochrane Handbook: a value of 0.2 indicates a small effect; a moderate effect is represented by 0.5; and 0.8 indicates a large effect (Schünemann 2019a).
2. Primary outcomes: scales used.
| Outcomes | Number of studies | Studies and instruments |
| Resilience | 21 |
|
| Anxiety | 12 |
|
| Depression | 24 |
|
| Stress or stress perception | 22 |
|
| Well‐being or quality of life | 20 |
|
aFor depression, we preferred depression scales over burnout scales if both forms of measure were reported. bIn two trials (West 2014; West 2015) we preferred continuous measures of burnout over dichotomous measures of depression, as they offered the possibility of being combined with other trials reporting continuous outcomes in meta‐analyses. cThe authors reportd that they would measure resilience with the emotional exhaustion subscale of the MBI. However, as this measure aims to assess burnout, we grouped the study under 'Depression' in this table. dFor trials reporting both general measures of well‐being or quality of life and work‐related assessments (e.g. job satisfaction, work‐related vitality), we preferred general measures.
3. Secondary outcomes: scales used.
| Outcomes | Number of studies | Studies and instruments |
| Social support (perceived) | 3 |
|
| Optimism | 3 |
|
| Self‐efficacy | 11 |
|
| Active coping | 5 |
|
| Self‐esteem | 1 |
|
| Hardiness | 1 |
|
| Positive emotions | 3 |
|
Unit of analysis issues
Cluster‐randomised trials
As allocation of individuals to different conditions in resilience intervention studies partly occurs by groups (e.g. work sites, hospitals), we intended to include cluster‐randomised trials along with individually‐randomised trials. Since we identified no cluster‐randomised trial, we have only included individually‐randomised trials in meta‐analyses.
Repeated observations on participants
If there were longitudinal designs with repeated observations of participants, we defined several outcomes based on different periods of follow‐up and conducted separate analyses, as recommended in the Cochrane Handbook (Higgins 2019a). One analysis included all studies with measurement at the end of intervention (post‐test), other analyses were based on the period of follow‐up (short‐term: three months or less; medium‐term: more than three to six months; and long‐term: more than six months). We rated assessments as post‐intervention if performed within one week after the intervention. We counted assessments at more than one week after the intervention as short‐term follow‐up.
Studies with multiple treatment groups
If selected studies contained two or more intervention groups, two review authors (AK, IH) determined which group was relevant to the review and the particular meta‐analysis, based on the inclusion criteria for interventions (see Types of interventions). For all studies that included several intervention groups, we considered only one intervention group relevant for the review (see Types of interventions).
Dealing with missing data
In the case of studies where there were missing data, such as missing standard deviations (SDs), or where healthcare professionals had been combined with other participants, we contacted the study authors to inquire if the missing data or subgroup (summary outcome) data were available. Following the recommendations in the Cochrane Handbook (Higgins 2019a), we computed missing SDs of continuous outcomes on the basis of other statistical information (e.g. t values, P values).
To obtain missing summary outcome data for studies solely conducted in healthcare professionals, we contacted the study authors (at least twice) to request the respective data (i.e. means, SDs and sample sizes for the relevant study conditions or alternative information to calculate the SMDs; see Measures of treatment effect).
In the case of missing outcome data due to attrition, we did not ask for individual‐level missing data and performed no re‐analysis using imputation methods. We rated studies with high levels of missing data (≥ 10%), that used no imputation methods at high risk of attrition bias (see Assessment of risk of bias in included studies). If the study authors had reported a complete‐case analysis as well as imputed data, we used the summary outcome data based on the imputed data set (e.g. baseline observation carried forward (BOCF) or ideally expectation maximization or multiple imputation).
We describe in detail those studies in which authors provided additional data not originally reported (e.g. number of participants analysed) in the Characteristics of included studies tables. We recorded missing data and attrition levels for each included study in the ‘Risk of bias’ tables (beneath the Characteristics of included studies tables). We also conducted a sensitivity analysis to examine the consequences of excluding studies with high levels of missing data (≥ 10% missing data in the respective outcome) on the results and subsequent conclusions of the review (see Sensitivity analysis).
Assessment of heterogeneity
We assessed the presence of clinical heterogeneity by comparing the study and study population characteristics across all eligible studies (e.g. by generating descriptive statistics). In accordance with the Cochrane Handbook (Deeks 2019), we explored if studies were sufficiently homogeneous in participant characteristics, interventions and outcomes.
We assessed methodological diversity by inspecting the included studies for variability in study design and risks of bias (e.g. method of randomisation). In accordance with previous reviews, which already described great heterogeneity in resilience intervention studies (Joyce 2018; Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016), we discussed similarities and differences between included studies in terms of these study characteristics in the Results and Discussion sections.
To assess statistical heterogeneity between included studies within each pair‐wise meta‐analysis (i.e. heterogeneity in observed treatment effects that exceeds sampling error alone), we relied on forest plots, Chi2 test, the tau2 statistic and the I2 statistic, as suggested by Deeks 2019. We also considered G2 to take small‐study effects into account (Rücker 2011). G2 indicates the proportion of unexplained variance, after having allowed for possible small‐study effects. No statistical heterogeneity is indicated by a G2 near zero. Significant statistical heterogeneity is indicated by a P value on the Chi2 test lower than 0.10. Since resilience‐training studies are often conducted with relatively small sample sizes (e.g. Loprinzi 2011; Sood 2014), we acknowledge that the Chi2 test has only limited power in such cases. Tau2 also provides an estimate of the between‐study variance in a random‐effects meta‐analysis. The I2 is a descriptive statistic, which equally reflects the percentage of total variation across studies that is due to heterogeneity rather than chance. In accordance with guidelines (Deeks 2019), we supposed non‐important heterogeneity for I2 values of 0% to 40%, moderate heterogeneity for I2 values of 30% to 60%, substantial heterogeneity for I2 values of 50% to 90%, and considerable heterogeneity for I2 values between 75% and 100%. We also calculated the 95% prediction intervals from random‐effects meta‐analyses (see Data synthesis; pooled analyses with more than two studies) to present the extent of between‐study variation (Deeks 2019).
Where we observed heterogeneity (e.g. I2 greater than 50%, with consideration of the direction of effects and strength of evidence for heterogeneity (P value)), we conducted several subgroup analyses to investigate potential explanations (see Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
We only performed analyses for reporting bias if there were at least 10 studies for an outcome. We assessed potential publication bias by inspecting (contour‐enhanced) funnel plots (plotting the effect estimates of trials against their standard errors on reversed scales) (Page 2019; Peters 2008). We considered the fact that funnel plot asymmetry does not necessarily reflect publication bias, but can stem from a number of reasons (Page 2019). To differentiate between real asymmetry and chance, we followed the recommendations in Page 2019, and also used Egger’s test (regression test; Egger 1997) to check for funnel plot asymmetry.
Data synthesis
We synthesised the results, in narrative and tabular form, by describing the resilience interventions, their theoretical concept (when possible), as well as the populations and outcomes studied (see Results). We performed the statistical analyses either in Review Manager 5 (RevMan 5; Review Manager 2014) or R (R 2019; libraries used: meta (Balduzzi 2019), metafor (Viechtbauer 2010) and metasens (Schwarzer 2019)), when appropriate.
We combined outcome measures of included studies through pair‐wise meta‐analyses (any resilience training versus control), in order to determine summary (pooled) intervention effects of resilience‐training programmes in healthcare professionals. The decision to summarise numerical results of RCTs in pair‐wise meta‐analyses depended on the number of studies found (at least two studies for a specific outcome and time point) as well as the homogeneity of the included studies by population (for age, sex), resilience interventions (i.e. comparable content and modalities), comparisons, outcomes measured (i.e. same prespecified outcome albeit with different assessment tools), and the methodological quality (risk of bias) of selected studies. We conducted meta‐analyses if intervention studies did not differ excessively in their content, if outcomes (measures) were not too diverse, and if there were no individual studies predominantly at high risk of bias.
For summary statistics for continuous data, we reported SMDs using an inverse‐variance random‐effects model. We used random‐effects pair‐wise meta‐analyses since we anticipated a certain degree of heterogeneity between studies, as indicated by the results of previous reviews (Joyce 2018; Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016), and given the nature of the interventions. We calculated the 95% prediction intervals from random‐effects meta‐analyses (see Assessment of heterogeneity). As part of our sensitivity analyses, we also performed fixed‐effect analyses (see Sensitivity analysis). We analysed separately continuous data reported as means and standard deviations in some studies and outcomes where standardised mean differences and the respective standard error were obtained from different data (e.g. independent t test). We subsequently combined these values using the generic invariance method in Review Manager 5 (Review Manager 2014).
We also included studies with mixed samples (i.e. healthcare professionals and non‐healthcare professionals) in meta‐analyses if the subgroup data for healthcare professionals were reported separately or could be obtained from the study authors. If subgroup data were not available, we provide a narrative report of the findings of these studies in a separate section (see Effects of interventions > Studies with mixed samples) for each outcome.
All studies measuring resilience used only one resilience scale. If a study reported more than one instrument for mental health and well‐being outcomes or for a specific resilience factor, we used the measure most often used among the included studies for effect size calculation. For the outcome of depression, we preferred depression scales over burnout scales if both measures were reported. For studies reporting both general measures of well‐being or quality of life and work‐related assessments (e.g. job satisfaction, work‐related vitality), we preferred general measures.
Once we had produced a summary of the evidence to date, and only if a pair‐wise meta‐analysis (any resilience training versus control) was possible, we checked whether the data were also suitable for a network meta‐analysis (NMA). There was not enough evidence to perform a NMA.
Subgroup analysis and investigation of heterogeneity
As we detected substantial heterogeneity for several outcomes (see Effects of interventions), we examined the characteristics of studies that may be associated with this diversity (Deeks 2019). The selection of potential effect modifiers is based on experience with previous reviews (Joyce 2018; Leppin 2014; Robertson 2015; Vanhove 2016). Where we could extract the necessary data, we performed the following subgroup analyses, classifying the RCTs as follows.
Setting of resilience interventions (group setting vs individual setting vs combined setting vs setting not specified).
Delivery format of resilience interventions (face‐to‐face vs online or mobile‐based vs telephone vs bibliotherapy vs laboratory vs multimodal delivery vs delivery not specified).
Intensity of resilience interventions (low intensity vs moderate intensity vs high intensity). Low‐intensity training includes interventions with a total duration of up to five hours or up to three sessions, respectively, if no duration in hours or minutes was indicated. Moderate intensity refers to training programmes including more than five hours to 12 hours, or more than three to 12 or fewer sessions. We categorised resilience interventions with more than 12 hours or more than 12 sessions, respectively, as high‐intensity training.
Theoretical foundation of resilience‐training programmes (CBT vs stress inoculation vs problem‐solving training vs ACT vs mindfulness‐based therapy vs AIT vs coaching vs positive psychology vs combination vs unspecific resilience training). 'Combination' refers to resilience interventions that were based on two or more explicit theoretical foundations, such as CBT and ACT or CBT and mindfulness. Unspecific training programmes include resilience interventions fostering one or several resilience factors but without specifying any explicit theoretical foundation, or where the underlying framework could not be assigned to a specific theoretical foundation.
Comparator group in intervention studies (attention control vs active control vs wait‐list control vs TAU vs no intervention vs control group not further specified). Attention control groups refer to an alternative treatment that mimicked the amount of time and attention received (e.g. by the trainer) in the intervention group. In this review, we use the term ‘active control’ for alternative treatment (no standard care; for example, treatment developed specifically for the treatment study) but that did not control for the amount of time and attention in the intervention group, and was not attention control in a narrow sense.
We calculated pooled effect sizes for each subgroup. Subgroup analyses were restricted to primary outcomes with at least 10 studies included in a meta‐analysis (Deeks 2019). Except for training intensity (post hoc addition), we prespecified all subgroup analyses in the protocol (Helmreich 2017). For delivery format, theoretical foundation and comparator, we added some subgroups based on the evidence we found.
Sensitivity analysis
We also restricted sensitivity analyses to primary outcomes with at least 10 trials in the meta‐analysis.
We performed sensitivity analyses:
based on the underlying concept of resilience, by limiting pooled analyses to scales assessing resilience as a state‐like outcome;
excluding studies at high risk of attrition and reporting bias (see Risk of bias in included studies), respectively; we conducted subgroup analyses to test if studies judged at low and unclear risk of bias could be pooled in analysis;
limiting the analyses to registered studies, as intended (Helmreich 2017), with registration identified depending on whether we found a trial registration or whether the authors claimed to have registered a study (see Characteristics of included studies);
limiting the analyses to those studies with low levels of missing data (less than 10% in the relevant primary outcome);
restricting the analyses to studies with less than 10% missing primary outcome data and where missing data had been imputed or accounted for by fitting a model for longitudinal data;
using a fixed‐effect pair‐wise meta‐analyses, to test the robustness of the findings.
Summary of findings and assessment of the certainty of the evidence
In this review, we used the software developed by the GRADE Working Group: GRADEpro: Guideline Development Tool (GRADEpro GDT) to create a 'Summary of findings' table for the comparison: resilience interventions versus control conditions for healthcare professionals.
We included all primary outcomes at post‐test in the 'Summary of findings' table. For each outcome, we assessed the certainty of the body of evidence using the GRADE approach proposed by the GRADE working group (Schünemann 2013; Schünemann 2019b), across the following five GRADE considerations:
limitations in the design and implementation of available studies (i.e. unclear or high risk of bias of studies contributing to the respective outcome; Guyatt 2011a);
indirectness of evidence (i.e. included studies limited to certain participants, intervention types, or comparators; Guyatt 2011b);
unexplained heterogeneity or inconsistency of results (i.e. heterogeneity based on variation of effect estimates, CIs, the statistical test of heterogeneity and I2, but the subgroup analyses fail to identify a plausible explanation; Guyatt 2011c);
imprecision of results (i.e. small number of participants included in an outcome and wide CIs; Guyatt 2011d); and
high probability of publication bias (i.e. high risk of selective outcome reporting bias for studies contributing to the outcome based on funnel plot asymmetry, Egger's test, different results of published vs unpublished studies, and whether the evidence consisted of many small studies with potential conflicts of interest) (Guyatt 2011e).
According to the GRADE system, for sufficient statistical precision, meta‐analyses of continuous outcomes should include sample sizes of at least 400 participants. Where there was both substantial inconsistency (I2 ≥ 60%) for an outcome and imprecision, we did not downgrade for imprecision, as the heterogeneity might have influenced the CI (i.e. precision), and we did not wish to double‐downgrade for the same problem.
Two review authors (AK, IH), working independently, assessed the certainty of the evidence, resolving any disagreements by discussion or by consulting a third review author (AC, KL). We interpreted the magnitude of effect for continuous outcomes according to the criteria suggested in the Cochrane Handbook (Schünemann 2019a) (i.e. 0.2 as small effect, 0.5 as moderate effect, 0.8 as large effect).
We rated the certainty of evidence as high, moderate, low or very low (Schünemann 2013). High‐certainty evidence indicates high confidence that the true effect lies close to that of the estimate of effect. Very‐low certainty evidence indicates that we have very little confidence in the effect estimate and that the true effect is likely to be substantially different from the estimate of effect.
Results
Description of studies
Results of the search
We ran the first searches for this review in October 2016 according to the protocol (Helmreich 2017). We used the strategies in Appendix 8 to find studies in which the participants included any adults aged 18 years and older. Due to the large number of potentially eligible studies, we decided to split the review and changed the inclusion criteria to focus on healthcare sector workers and students (see Differences between protocol and review). Before running the top‐up searches in June 2019, we revised the original search strategy by limiting the population to healthcare sector workers and students (Appendix 9). Following these searches, we further revised the inclusion criteria to healthcare professionals only, which is the focus of this review.
In total, the database searches retrieved 37,737 records. We found an additional 663 records by searching other resources. Following de‐duplication, we screened the remaining 24,703 records by title and abstract. We deemed 21,629 records to be irrelevant and sought the full texts of the remaining 3074 records for further assessment. At the level of title/abstract screening, we achieved a good agreement (kappa = 0.70) between review authors for the original search, and an excellent agreement for the top‐up searches (kappa = 0.99). The full text screening resulted in excellent inter‐rater reliability for both the original search (kappa = 0.95) and the top‐up searches (kappa = 1).
After revising the eligibility criteria to focus broadly on the healthcare sector (including healthcare professionals; see Differences between protocol and review), we identified 80 studies that were performed in any of these groups. We also identified nine ongoing studies and 29 studies awaiting classification. We found six additional reports of studies during the top‐up searches.
Finally, after revising the eligibility criteria to focus on healthcare professionals, we reassessed these 118 studies (from 144 reports). In total, for healthcare professionals, we included 44 studies (from 59 reports). We excluded a total of 3000 full text reports (see Figure 1). This total includes the 16 reports (13 excluded studies), which we needed to examine in detail to determine eligibility, and which are described in the Characteristics of excluded studies tables. We identified eight studies awaiting classification (see Studies awaiting classification) and five ongoing studies (see Ongoing studies). For further details of our screening process, see the study flow diagram (Figure 1). We present the results of both searches in more detail in Appendix 12.
1.
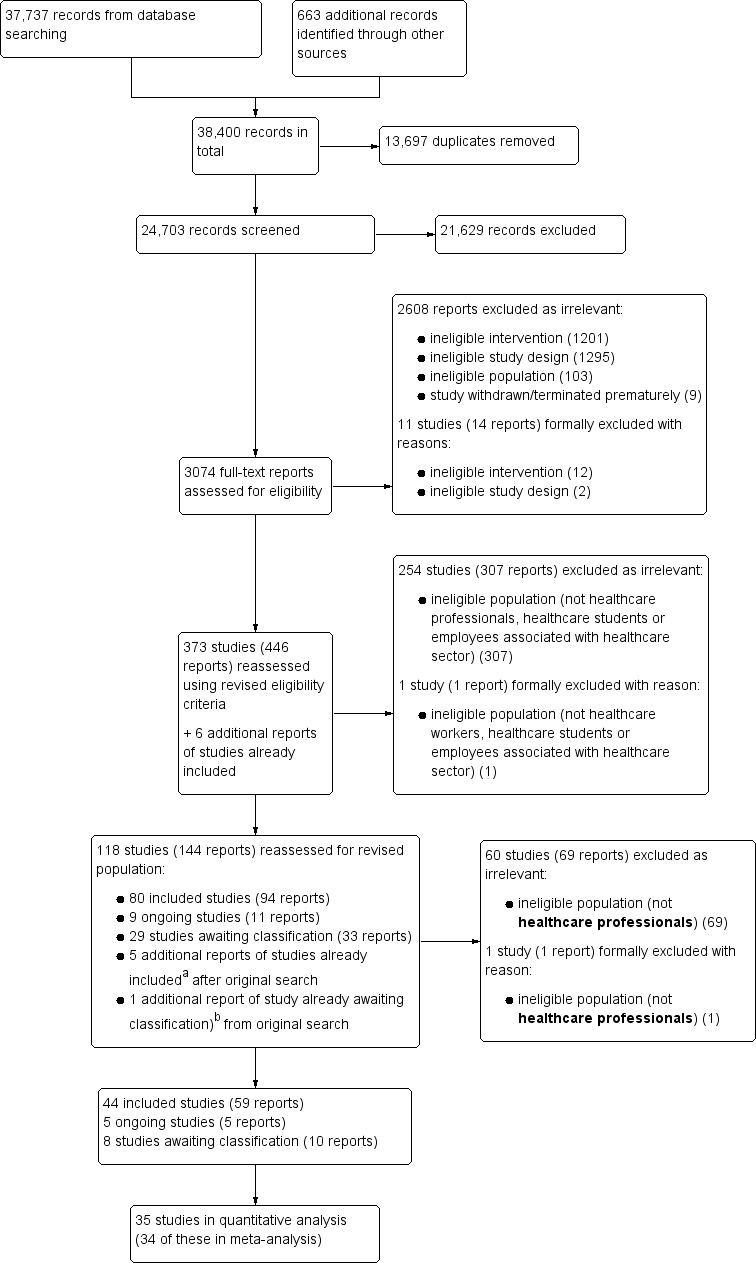
Study flow diagram combining all searches.
aDuchemin 2015; Mistretta 2018; Schroeder 2016.
bVan Berkel 2014.
From an updated (pre‐publication) search of four key databases in June 2020, we have added 12 studies (from 12 reports) to the Characteristics of studies awaiting classification tables. The results of these studies are not yet included in this review and will be incorporated at the next update.
Included studies
We present the corresponding references for the description of included studies in Appendix 13.
Study design
All but one (NCT02603133) of the 44 included studies were parallel‐group designs, and were published between 1997 and 2019; the exceptions are three completed but unpublished trials (ISRCTN69644721, NCT02603133, NCT03645798). One study was termed a cluster‐RCT in the report (Mistretta 2018), but according to additional information received from the study authors, there were no groups or clusters for each of the three conditions. After discussion with the statistician (JK), we judged the study to be individually randomised with stratification for the participants’ schedule availability.
Location
Nineteen studies were conducted in the USA, six took place in Germany, four in China, and three in Australia, Iran and the UK, respectively. One study was performed in Canada (Smith 2019) and the Netherlands (Strijk 2011), while the remaining studies took place in Israel (Berger 2011), Italy (Villani 2013), Poland (Cieslak 2016), and Sri Lanka (Gelkopf 2008).
Settings
Training programmes were performed in clinics or specific hospital departments (e.g. Department of Radiology) in 24 studies. For 11 studies, the intervention site was not further specified. As four studies included online or mobile resilience interventions, there was no concrete venue and participants could participate regardless of location. One intervention took place in the laboratory (Stetz 2007). Two resilience training programmes were conducted in mixed settings (e.g. online training plus face‐to‐face sessions with implementation site not further specified). Other intervention sites included the Chinese Auxiliary Medical Service (Cheung 2014) and a non‐governmental organisation (Gelkopf 2008).
Participants
Participants were mainly women of young to middle age. Studies rarely examined healthcare professionals between the ages of 50 and 65 years. Most studies evaluated a resilience‐training programme in nurses. The total number of adults working as healthcare professionals (see Types of participants) randomised across 39 of the 44 included studies was 6892 (original search: 5552, top‐up searches: 1340; including two completed but unpublished studies: NCT02603133; NCT03645798).
For four studies with mixed samples (Cieslak 2016; Gelkopf 2008; ISRCTN69644721; Wild 2016), the total number of participants randomised or planned to be randomised (ISRCTN69644721) was 1000 participants. The original number of healthcare workers randomised in these mixed studies was unclear and could not be confirmed by the study authors. Varker 2012 randomised 82 volunteers from the general population to evaluate a resilience intervention developed for emergency personnel. Overall, 11 studies randomised 100 or more participants and five studies randomised 30 participants or fewer.
Where data on age were available, the mean age across 25 studies (no mixed studies) ranged from 27 to 52.4 years (standard deviation (SD) ranging from 2.1 to 12.6 years), with an average of 37.74 years (mean SD 6.70 years). In one study of volunteers in the general population (Varker 2012), it was 28.4 (SD 10.4) years. For mean age, three of the four mixed studies reported a range of 37.49 to 48.65 years (SD ranging from 9.78 to 12.77 years) for the total samples (including healthcare professionals), with an average of 42.52 years (mean SD 10.98 years). Sood 2011 indicated a mean age in the intervention group of 46.8 (SD 8.3) years and of 50.2 (SD 5.7) years in the control group. Three studies did not report mean age, but only the age range of participants (Calder Calisi 2017; Hosseinnejad 2018; Khoshnazary 2016), three studies reported alternative information on age (e.g. the percentage below a specific age; Mirzaeirad 2019; Poulsen 2015; Stetz 2007). For eight studies, the age of the sample was not further specified or is unclear (ISRCTN69644721; Klatt 2015; Mealer 2014; NCT02603133; NCT03645798; Tierney 1997; West 2014; West 2015).
Women outnumbered men in 23 studies. Women were also in the majority in one study evaluating a resilience‐training programme in volunteers in the general population (Varker 2012). By contrast, men dominated in five studies and four studies included only women. In one study (Sood 2011), the gender distribution was comparable across the two arms. For six studies, the sex of participants was unclear. For example, Fei 2019 investigated nurses but did not indicate whether or not male nurses were also considered. The same applied to Tierney 1997. For 32 studies presenting the total numbers of men and women investigated, the proportion of women was 68.6%. Women outnumbered men in three of the four mixed studies, and for one study, the sex of participants was unclear (ISRCTN69644721). The proportion of women in three mixed studies reporting total numbers for gender was approximately 64.9%.
Fifteen studies included solely nurses, and 14 were conducted among physicians. Eight studies were conducted with hospital personnel (e.g. physicians and other hospital personnel). The remaining studies included general medical personnel, such as military medical personnel (Cheung 2014; Stetz 2007). Four of the 44 studies were performed with mixed samples, i.e. healthcare professionals combined with other individuals such as ambulance personnel and other emergency services, including the police. Relevant subgroups within these studies included: health service professionals (Cieslak 2016), mental health workers (Gelkopf 2008), and ambulance service personnel (Wild 2016; ISRCTN69644721). Although Varker 2012 was performed in the general population as a proof‐of‐concept study, we have included it in this review, as the resilience intervention was developed for emergency services personnel.
Twenty‐nine of the 44 studies assessed mental health at baseline. All studies measuring mental health used self‐report (screening) measures covering one or a small number of mental dysfunctions (e.g. Beck Depression Inventory (BDI), Luthar 2017). None of the studies conducted comprehensive baseline diagnostics by the use of a structured interview (e.g. Mini‐International Neuropsychiatric Interview; (MINI)). Fifteen studies provided no data about the mental health status of the sample. For three unpublished trials (ISRCTN69644721; NCT02603133; NCT03645798) and one study published as a conference abstract (Smith 2019), the baseline mental health status was unclear, although all of them assessed mental health at pretest. Five studies included only mentally‐healthy participants (Chesak 2015; Cheung 2014; Sood 2011; Sood 2014) or participants showing symptoms below a cut‐off on a screening instrument (Stetz 2007). Lin 2019 did not include participants taking mood‐modulating drugs. For Mirzaeirad 2019, the lack of mental stress was an inclusion criterion.
Interventions
All 44 studies examined the effects of a psychological intervention to foster resilience, hardiness, or post‐traumatic growth compared to a control condition in healthcare professionals. Most studies evaluated group interventions (30/44) of high training intensity (18/44), that were delivered face‐to‐face (29/44) and were based on a combination of theoretical foundations (19/44).
Multiple treatment arms
Six studies had multiple intervention arms. Due to high dropout in the social support‐enhancing module in Cieslak 2016, only the self‐efficacy‐enhancing module was analysed. As the fourth intervention group (IG) in Medisauskaite 2019 completed all modules of IG1 to IG3, including how to manage distress and develop resilience, we considered it relevant for this review. From the mindfulness‐based resilience training (MBRT) and a smartphone resilience training in Mistretta 2018, we accepted the MBRT since it focused more on resilience factors and less on general issues such as sleep and productivity. From three interventions in Stetz 2007 we chose the combination of virtual reality‐stress inoculation training (VR‐SIT) and coping training (CT; e.g. relaxation) as relevant, since this intervention content was compatible with another included study (Villani 2013), which also considered SIT and relaxation techniques. In Tierney 1997, we preferred the hardiness class (IG1) over a time‐management class (IG2) for this review. From a new resilience intervention (e.g. dealing with difficult emotions; IG1) and four weeks of reading material about mental health and well‐being (IG2) in ISRCTN69644721, we chose IG1. For one unpublished study (NCT02603133) it was unclear whether it only included one intervention arm (sequential and non‐sequential rollout of resilience tools in cohort 1) or whether these should be considered as separate IGs.
Intervention setting
Thirty interventions were performed in groups. Eight studies were conducted in a variety of training settings, and four were individual‐setting interventions. For two studies, the setting was not specified (Medisauskaite 2019; NCT02603133).
Delivery format
Twenty‐nine of the 44 studies delivered resilience interventions face‐to‐face. Ten studies used a multimodal delivery of interventions (e.g. web‐based intervention and daily diary). Three studies examined online or mobile‐based resilience‐training programmes, and one study tested an intervention that was conducted in a laboratory setting and unlikely to be a face‐to‐face contact (Stetz 2007). For one study (Medisauskaite 2019) the delivery format was unclear.
Training intensity
Treatment duration varied between a single 40‐minute intervention session (Varker 2012) and, depending on whether the number of hours or sessions were reported, 87 hours (i.e. 12‐weekly six‐hour sessions and three five‐hour supervision sessions; Berger 2011) or approximately 77 sessions in total (Strijk 2011). Three interventions were provided over a six‐month period or even longer (NCT03645798; Strijk 2011; West 2015). Overall, 18 studies included high‐intensity training (i.e. > 12 hours or > 12 sessions). Fifteen RCTs investigated moderate‐intensity interventions (i.e. > 5 to ≤ 12 hours or > 3 to ≤ 12 sessions), whereas seven studies evaluated low‐intensity training (i.e. ≤ 5 hours or ≤ 3 sessions in total). Training intensity was unclear for four studies (Alexander 2015; Khoshnazary 2016; Medisauskaite 2019; Mirzaeirad 2019).
Theoretical foundations
We categorised the interventions into eight groups, based on their content and the descriptions provided by the study authors. We present a synthesis of the characteristics of studies within a specific theoretical foundation and the respective intervention content in Appendix 14.
Nineteen studies included interventions based on a combination of two or more explicit theoretical foundations (e.g. CBT and mindfulness). Of these, two studies were based on mindfulness (e.g. MBSR) and CBT or cognitive therapy (Mealer 2014; Wild 2016); in addition, Mealer 2014 also included written exposure therapy based on Pennebaker 1986. Two studies (Ireland 2017; Lin 2019) combined MBSR (e.g. Kabat‐Zinn 1990) with mindfulness‐based cognitive therapy (MBCT; e.g. Teasdale 2000), with Ireland 2017 also including elements of ACT. Similarly, Mistretta 2018 incorporated aspects of mindfulness and ACT. Two studies (Berger 2011; Gelkopf 2008) investigated a programme based on resiliency manuals for elementary school children (e.g. ERASE (Enhancing Resiliency Among Students Experiencing Stress) Stress; Berger 2007; Gelkopf 2009) that included cognitive‐behavioural components, art therapy, body‐oriented strategies, narrative therapy and meditative practices. Six studies, all conducted in Germany, were designed on principles of CBT and solution‐focused group work, with some studies (Bernburg 2016; Bernburg 2019; Mache 2016) also including mindfulness (and acceptance training; Bernburg 2019). Six combined interventions could not be clustered any further (Calder Calisi 2017; Fei 2019; Smith 2019; Tierney 1997; Varker 2012; West 2014). In 11 RCTs, unspecific resilience‐training programmes were conducted. All of these studies aimed at fostering one or several prespecified resilience factors (see Appendix 2; level 1; e.g. social support, active coping, self‐esteem, optimism), but indicated no concrete theoretical foundation of training. Five studies evaluated mindfulness‐based resilience interventions, with most training programmes based on MBSR (Lebares 2018) or used a modified version of MBSR (e.g. MBSR combined with elements of compassion skills training). Three interventions used AIT, with a focus on strengthening the attention for novel aspects of the world and to delay judgements. Stress inoculation was represented in two studies, with both also teaching coping strategies for stressful situations. Two programmes only included elements of CBT (Cieslak 2016; Clemow 2018); one intervention was based on positive psychology (NCT03645798) and focused on positive experiences (e.g. 'three good things'). A resilience‐training programme based on a coaching approach was tested in one study (Strijk 2011).
Comparators
Forty‐three studies involved only one comparator. For one unpublished study (NCT02603133), the number of control groups was not clear, based on the trial registration. Below, we describe in more detail the control groups used in the included studies.
Most studies included no intervention comparators (14/44), wait‐list control groups (13/44), followed by active control (6/44), attention control (4/44), and TAU (4/44). Two studies did not further specify the control group (Khoshnazary 2016; Mirzaeirad 2019). Two studies used a design where a control group plus resilience intervention was compared to the control group alone (Poulsen 2015; Strijk 2011). For NCT02603133, we were unsure about the number of control groups, and whether the study included only a wait‐list control or also an active control (see lecture on safety culture). We were not able to resolve this uncertainty by contacting the study authors.
In six studies, active control groups included a lecture covering topics related to stress (Chesak 2015); a befriending seminar that gave tools for emotional support to disaster volunteer workers (Gelkopf 2008); an extra hour break‐time over 10 weeks (Ireland 2017); written educational material about recovery and self‐care practices (Poulsen 2015); written information about a healthy lifestyle in general (e.g. diet, physical activity, relaxation) (Strijk 2011); and an online intervention with tailored information on mental health for emergency personnel (e.g. sleep, stress, mindfulness) (Wild 2016).
Of the four studies contrasting a resilience intervention with an attention control group, two used a web‐based educational intervention on coping with stress at work and indirect exposure to trauma (Cieslak 2016) and a face‐to‐face group intervention on topics such as perseverance, complications, self‐care and the ethos of surgery, along with daily home practice requirements and a retreat hike focusing on the relaxing properties of nature (Lebares 2018). Other attention control comparators included accident management training to learn tips and strategies on how to react when involved in a traffic accident (Varker 2012), and video clips representing natural environments delivered by mobile phones (Villani 2013).
In two studies, treatment as usual (TAU) referred to minimally‐enhanced usual care by self‐help materials (brochure) for blood pressure reduction and physician referrals (Clemow 2018) or usual psychological instruction from the hospital (NCT03645798). For two studies, the content of the TAU group was not further specified (Alexander 2015; Hosseinnejad 2018).
Outcome measures
The included RCTs used a diversity of outcome measures. However, some studies measuring the same outcome (e.g. perceived stress) used the same instrument (e.g. Perceived Stress Scale; Cohen 1988a). All outcomes were based on self‐reported assessments and most studies used validated scales.
Primary outcomes
We defined treatment efficacy as an improvement in resilience, assessed with specific resilience scales, or an improvement in four categories of mental health and well‐being (i.e. anxiety, depression, stress or stress perception, well‐being or quality of life). For each outcome, the studies used heterogeneous scales (see details in Table 3). Among the 44 included studies, most (24 studies) assessed depression (e.g. depressive symptoms), followed by stress or stress perception (22 studies), resilience using a resilience scale (21 studies), well‐being or quality of life (20 studies) and anxiety (12 studies).
Secondary outcomes
The authors of the included studies also used a heterogeneous group of instruments to assess the secondary outcomes (see details in Table 4). For each secondary outcome, most included studies assessed self‐efficacy (11 studies), followed by active coping in five studies. Social support, optimism and positive emotions were assessed by three studies, respectively, while both self‐esteem and hardiness were outcome measures in only one study.
Funding sources
Funding sources for the included studies were various: in five studies respectively, they included different hospitals or hospital grants (e.g. Mayo Clinic), and universities (e.g. certain faculties) and university research funds. In two studies apiece, further funding was provided by the National Institutes of Health (NIH), ministries, different foundations, and state/regional and city initiatives for health care. Single studies were supported by the US army (Stetz 2007), research grants (e.g. for student research; Cheung 2014) and research programmes (e.g. specifically for resilience; Duchemin 2015). Seven studies reported a combination of funding sources (e.g. university and national institute, hospital grant and gift, university and charity, hospital funds and EU grant Horizon 2020, NIH and foundations, hospital and university). For 15 studies, funding sources were not specified or could not be retrieved from the available information (e.g. conference abstract) (West 2015). One study received no funding support (Bernburg 2016).
Excluded studies
We excluded 3000 irrelevant full text reports.
We excluded 13 studies (from 16 reports) that seemed to merit inclusion but on closer inspection did not (see Characteristics of excluded studies). We excluded nine of these studies because they did not explicitly state the aim of fostering resilience, hardiness or post‐traumatic growth through the intervention, or we were advised by the study authors that resilience was not the primary focus of the study, or both (Chang 2008; Dyrbye 2016; Imamura 2019; NCT03753360; NCT03914898; Rowe 1999; Speckens 2019; Strauss 2018; Watanabe 2019). Two studies were excluded due to ineligible study design Lahn 2014; Maunder 2010). Two studies were excluded for ineligible population, since they did not examine healthcare professionals (Bian 2011; NCT02417051). The reasons for excluding these studies are presented in detail in Appendix 15.
Studies awaiting classification
We identified eight studies (from 10 reports) awaiting classification.
For four studies, resilience was only rarely mentioned in the reports, i.e. the focus of the intervention on fostering resilience, hardiness or post‐traumatic growth was unclear and could not be obtained from the study authors (Aranda Auserón 2018; NCT03613441; NCT03781336; Ruehl 2013). For example, Ruehl 2013 measured post‐traumatic growth as an exploratory measure following a written emotional expression intervention in a diverse group of nursing staff, but it was unclear whether the study primarily focused on fostering this construct. Similarly, Aranda Auserón 2018 examined a mindfulness and self‐compassion programme in primary‐care health professionals to reduce stress and prevent burnout, but it was unclear if resilience was the primary focus of the study (resilience was mentioned only once).
We could not clearly determine the study design of Ouyang 2017, since the full text was not available and we received no response from the investigators. The same applied to Mainwaring 2018 (available as a conference abstract), for which we obtained no response from the authors. For two studies, it was unclear whether the sample also included healthcare workers (Kim 2018a; Van Berkel 2014).
Details of these studies can be found in the Characteristics of studies awaiting classification tables.
The 12 studies from the updated search in June 2020 were also added to the Characteristics of studies awaiting classification tables. They will be incorporated into this review at the update stage.
Ongoing studies
We also found five ongoing studies (from five reports) that are likely to meet our inclusion criteria (ACTRN12617000290392; JPRN UMIN000031435; NCT03518359; NCT03645512; NCT03759795). These studies were all RCTs with parallel assignment. ACTRN12617000290392 compared the six‐week online programme 'Doctors Working Well' (e.g. modules on stress management, emotion monitoring and regulation) to an active control (protected individual study time) in junior medical doctors. In a Japanese trial (JPRN UMIN000031435), medical professionals working in the field of oncology or palliative care (or both) were randomised to either the MHALO programme (mindfulness for health professionals building resilience and compassion) or a no‐intervention control. NCT03518359 compared the mindfulness‐based enhanced stress resilience training (ESRT: six‐weekly classes plus daily homework and retreat; e.g. sustained attention, emotional regulation, meta‐cognition) with active control (stress management) in medical interns from different departments. NCT03645512 included critical care nurses at Florida Hospital to determine whether the Corporate Athlete® Resilience (CAR) training programme (a holistic approach focusing on moving between stress and strategic recovery) had a significant impact on the nurses' resilience and stress mindset compared to a wait‐list control. The Bournemouth University resilience training for surgeons (BURTS), based on acceptance and commitment training (ACTr; Flaxman 2013) was contrasted with a wait‐list control in a sample of trainee and consultant surgeons (NCT03759795). In contrast to other ongoing studies, the intervention group did not receive only one treatment, but followed a maximum of three intervention periods (e.g. mindfulness training) of eight weeks each.
Further details of these studies can be found in the Characteristics of ongoing studies tables.
Risk of bias in included studies
The main flaws we found for risks of bias (≥ 20% high risk) across the 44 studies were in the following domains: performance bias, detection bias, attrition bias, and reporting bias (see Figure 2 and Figure 3 for ‘Risk of bias’ graphs, and Characteristics of included studies tables for further information). For selection bias, a large number of studies provided insufficient information to judge the risk of bias adequately. We identified most variability across studies for attrition and reporting bias.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Sequence generation
We rated 15 studies at low risk of bias, since the investigators described a random component in the sequence‐generation process (e.g. computer‐generated random sequence generation). For four of these studies, there was verified baseline comparability between study groups in sociodemographic characteristics (i.e. potential confounding factors) as well as outcome variables (Fei 2019; Lin 2019; Medisauskaite 2019; West 2014). For the other 11 studies, there was evidence of a genuine random assignment (e.g. random‐number generation), but the authors provided no information about potential baseline differences in sociodemographic and outcome measures (Berger 2011; Bernburg 2016; Bernburg 2019; Chesak 2015; Duchemin 2015; Lebares 2018; Mache 2015a; Mache 2016; Mache 2017; Poulsen 2015; Strijk 2011).
We rated 20 studies as having unclear risk of bias because there was no description of the sequence‐generation process (Alexander 2015; Calder Calisi 2017; Cieslak 2016; Clemow 2018; Hosseinnejad 2018; Ireland 2017; Khoshnazary 2016; Klatt 2015; Loiselle 2018; Luthar 2017; Mache 2015b; Mealer 2014; Mistretta 2018; Schroeder 2016; Sood 2011; Stetz 2007; Tierney 1997; Varker 2012; Villani 2013; Wild 2016). Thirteen of these RCTs also did not specify the baseline comparability of groups for (some) sociodemographic characteristics or outcomes of interest, or both (Calder Calisi 2017; Cieslak 2016; Hosseinnejad 2018; Ireland 2017; Klatt 2015; Mache 2015b; Mealer 2014; Sood 2011; Stetz 2007; Tierney 1997; Varker 2012; Villani 2013; Wild 2016). Based on the limited information in the conference abstracts or trial registrations, we considered five further studies at unclear risk of bias (ISRCTN69644721; NCT02603133; NCT03645798; Smith 2019; West 2015).
We judged four studies to be at high risk of selection bias since, despite the fact that randomisation, baseline comparability in sociodemographic characteristics or outcomes (or both) could not be verified on the basis of analysis (Cheung 2014; Gelkopf 2008; Mirzaeirad 2019; Sood 2014).
Allocation concealment
Allocation concealment was not well reported. Only two of the 44 studies had an adequate description of the allocation concealment process and we considered them to be at low risk of bias for this domain. Clemow 2018 described randomisation being done by calling an off‐site person holding the randomisation envelopes, using the random‐sized randomisation blocks provided by the study statistician. Strijk 2011 affirmed that randomisation was done by an independent researcher after the baseline assessment, that is, after participant enrolment was completed.
We rated the remaining 42 studies at unclear risk of bias. Four of these studies described the randomisation process being concealed from participants or personnel recruiting participants, or both, but neglected to specify further the method of allocation concealment (Luthar 2017; Medisauskaite 2019; Sood 2014; West 2014). For one study (Stetz 2007) we received additional information from the authors ("computed a number with SPSS to randomly select"), which did not match the description in one of the reports (see Stetz 2007; pseudo‐randomisation based on availability).
Three studies (plus West 2014 already mentioned above) affirmed that individuals or units were stratified (e.g. by gender, type of work) and randomly assigned to either the resilience intervention or a control group (Duchemin 2015; Lebares 2018; Wild 2016); however, the study authors did not describe how they designed this process.
Authors of 29 studies provided either insufficient or no information about the allocation concealment process (Alexander 2015; Berger 2011; Bernburg 2016; Bernburg 2019; Calder Calisi 2017; Chesak 2015; Cheung 2014; Cieslak 2016; Fei 2019; Gelkopf 2008; Hosseinnejad 2018; Ireland 2017; Khoshnazary 2016; Klatt 2015; Lin 2019; Loiselle 2018; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mealer 2014; Mirzaeirad 2019; Mistretta 2018; Poulsen 2015; Schroeder 2016; Sood 2011; Tierney 1997; Varker 2012; Villani 2013).
There was limited information in the conference abstracts or trial registrations of five studies to reach a decision on the risk of bias (ISRCTN69644721; NCT02603133; NCT03645798; Smith 2019; West 2015).
Blinding
Blinding of participants and personnel
Nine of the 44 studies assessed one or several objective outcomes such as salivary cortisol, sleep tracking by acceleration sensors or blood pressure (Clemow 2018; Duchemin 2015; Lebares 2018; Luthar 2017; Mistretta 2018; NCT02603133; NCT03645798; Stetz 2007; Strijk 2011). Although study personnel were not blinded in most of these studies (see next paragraph on subjective outcomes below), we judged those studies to be at low risk of performance bias in relation to objective outcomes.
For subjective outcomes, we rated three studies at unclear risk of performance bias (Cieslak 2016; Medisauskaite 2019; Villani 2013). Cieslak 2016 and Villani 2013 performed (blended) online or mobile‐based resilience interventions without specifying blinding of participants and personnel. Medisauskaite 2019 did not describe the implementation of the training programme.
We judged 36 studies to be at high risk of performance bias because resilience interventions were performed entirely face‐to‐face (Alexander 2015; Berger 2011; Bernburg 2016; Bernburg 2019; Cheung 2014; Fei 2019; Gelkopf 2008; Ireland 2017; Klatt 2015; Khoshnazary 2016; Lebares 2018; Lin 2019; Loiselle 2018; Luthar 2017; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mirzaeirad 2019; Poulsen 2015; Schroeder 2016; Smith 2019; Sood 2011; Strijk 2011; Tierney 1997; Varker 2012; West 2014; West 2015; Wild 2016), or included face‐to‐face elements (Calder Calisi 2017; Chesak 2015; Duchemin 2015; Mealer 2014; Mistretta 2018; Sood 2014; ISRCTN69644721), resulting in a lack of blinding of personnel. We also rated the following five studies at high risk of performance bias: In Clemow 2018, research staff were also not blinded to group assignment and although the blinding of participants was unclear, we rated the study at high risk of bias due to the face‐to‐face delivery of resilience training. Hosseinnejad 2018 described the study as a double‐blind clinical study, but, given the trial registration (no blinding specified) and the face‐to‐face delivery of the intervention, we judged the study to be at high risk of performance bias. For NCT02603133 and NCT03645798, we considered the outcomes to be likely to have been influenced by a lack of blinding, as the studies were described as open‐label with no masking (NCT02603133) or as single‐blinded in the trial registration (NCT03645798). Stetz 2007 included a resilience intervention that was performed in a laboratory. Although there was no face‐to‐face contact, the study personnel were not blinded, as verbal communication with participants was possible, and participants were observed by the intervention providers.
Blinding of outcome assessment
We considered all nine studies measuring objective outcomes to be at low risk of detection bias. Although six of these studies did not adequately describe the blinding of outcome assessment (Duchemin 2015; Lebares 2018; Luthar 2017; Mistretta 2018; Stetz 2007; Strijk 2011), we judged them to be at low risk of detection bias since we assessed the objective outcomes (e.g. physiological parameters) as unlikely to be influenced by the lack of blinding. We applied the same rating to two other studies that used objective outcomes, even though there was insufficient information in the trial registrations (NCT02603133; NCT03645798), as well as one study with no general blinding of research staff (Clemow 2018).
In the assessment of subjective outcomes, we considered seven studies to be at unclear risk of detection bias because the authors did not adequately describe the blinding of the assessment (Cieslak 2016; Lebares 2018; Mache 2016; Medisauskaite 2019; Sood 2014; Stetz 2007; Villani 2013) and the risk of performance bias (i.e. especially blinding of participants) was low or unclear (see blinding of participants and personnel).
We rated 37 studies at high risk of detection bias; 31 studies because, due to (potential) performance bias (especially no blinding of participants), we judged that the participants' responses to questionnaires may be likely to be affected by the lack of blinding (i.e. knowledge and beliefs about the intervention they received) (Alexander 2015; Berger 2011; Bernburg 2016; Bernburg 2019; Calder Calisi 2017; Chesak 2015; Cheung 2014; Duchemin 2015; Fei 2019; Gelkopf 2008; Hosseinnejad 2018; Ireland 2017; Khoshnazary 2016; Klatt 2015; Lin 2019; Loiselle 2018; Luthar 2017; Mache 2015a; Mache 2015b; Mache 2017; Mealer 2014; Mirzaeirad 2019; Mistretta 2018; Poulsen 2015; Schroeder 2016; Sood 2011; Strijk 2011; Tierney 1997; Varker 2012; West 2014; Wild 2016). Based on the information available in the conference abstracts or trial registrations, we rated five further studies at high risk of detection bias for the same reason (ISRCTN69644721; NCT02603133; NCT03645798; Smith 2019; West 2015). For Clemow 2018, the blinding of participants, who completed self‐report questionnaires was unclear (see blinding of participants and personnel). However, as research staff were not blinded to group assignment in general, we judged the blinding of outcome assessment to be unlikely and also rated the study at high risk of detection bias.
Incomplete outcome data
We assessed 17 studies as having low risk of attrition bias because they met at least one of the following criteria: there were no missing outcome data (Alexander 2015; Duchemin 2015; Ireland 2017; Lebares 2018: no missing data for psychological variables and two exclusions from fMRI analysis not related to true outcome; Villani 2013); the losses were similar across intervention and control groups; the reasons for missing data were unlikely to be related to true outcome (e.g. health reasons); the losses were not substantial (< 10% from number of randomised participants; e.g. five dropouts from 90 participants in Mache 2015b); and/or study authors accounted for dropouts and losses to follow‐up by using statistical analyses that aimed to reduce bias (e.g. multiple imputation) or prevent false positive conclusions (e.g. baseline observation carried forward) (Bernburg 2019; Clemow 2018; Gelkopf 2008; Khoshnazary 2016; Mache 2015a; Mache 2015b; Mache 2016; Mealer 2014; Mistretta 2018; Sood 2014; Strijk 2011; Varker 2012). An intention‐to‐treat (ITT) analysis was performed in four studies (Clemow 2018; Mistretta 2018; Sood 2014; Strijk 2011).
Overall, we rated 11 of the 44 studies at unclear risk of bias. One study did not fully account for dropouts throughout the study or whether this differed between groups (Stetz 2007). Hosseinnejad 2018 did not specify the number of participants analysed and we had to derive these indirectly from other statistical values in the report, with the help of the statistician (JK). Three studies reported results for all participants randomised (Berger 2011, Fei 2019, Tierney 1997), but did not state the amount of potential missing data and potential imputation. Similarly, Bernburg 2016 described the dropout rate (loss to follow‐up) as very low and analysed all 54 randomised participants, but did not report the attrition rate. In Klatt 2015, the number of participants allocated to each group (n = 17) was provided by the original authors, but the amount of potential missing data was not further specified. We therefore also judged these studies to be at unclear risk of bias. We could not judge the risk of attrition bias from the information available in the conference abstracts or trial registrations for four studies (ISRCTN69644721; NCT02603133; NCT03645798; Smith 2019), which we consequently rated at unclear risk of bias.
We considered 16 studies to be at high risk of attrition bias. In six of them, the reasons for missing data were unlikely to be related to true outcome (e.g. similar levels of missing data between groups with a difference of two or less lost individuals); however, reasons were not further specified or study authors did not impute the missing data but performed available‐case analysis (i.e. participants for whom outcomes were obtained at assessments) or per‐protocol analysis (i.e. only participants who complied with their allocated intervention or attended a certain number of sessions), or both (Chesak 2015; Lin 2019; Luthar 2017; Mirzaeirad 2019; Schroeder 2016; West 2014). Calder Calisi 2017 did not provide sufficient information about dropouts such as the number of participants randomised to each group or attrition per group. However, based on the number of participants analysed, we supposed a per‐protocol analysis and considered the study to be at high risk of bias. In eight of the 16 studies at high risk of attrition bias (Cheung 2014; Loiselle 2018; Mache 2017; Medisauskaite 2019; Poulsen 2015; Sood 2011; West 2015; Wild 2016), reasons for missing data were likely to be related to true outcome, due to imbalance in missing data between groups. In addition, an available‐case or per‐protocol analysis (or both) was conducted in six of these studies (Cheung 2014; Loiselle 2018; Mache 2017; Medisauskaite 2019; Poulsen 2015; Sood 2011). In Wild 2016, it was unclear how many participants were analysed. For West 2015, we received information about the number of missing data per group and the available‐case analysis from the study authors. Finally, in Cieslak 2016 missing data in the self‐efficacy‐enhancing group and the education module (control) were imputed using expectation maximisation in order to perform an intention‐to‐treat analysis. Nevertheless, we considered the study to be at high risk of bias because only two of three groups initially randomised were analysed, due to high dropout in the social support‐enhancing module.
Selective reporting
To assess potential reporting bias for 29 non‐registered studies or studies without a pre‐published study protocol (Alexander 2015; Berger 2011; Bernburg 2016; Bernburg 2019; Calder Calisi 2017; Chesak 2015; Cieslak 2016; Duchemin 2015; Fei 2019; Gelkopf 2008; Ireland 2017; Khoshnazary 2016; Klatt 2015; Lin 2019; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mealer 2014; Mirzaeirad 2019; Poulsen 2015; Schroeder 2016; Sood 2011; Sood 2014; Stetz 2007; Tierney 1997; Varker 2012; Villani 2013; West 2015), we considered whether the outcome measures described in the Methods section of the paper were reported in the Results section. For West 2015, we were able to judge the risk of reporting bias, based on the respective sections in the conference abstract.
We considered 25 non‐registered studies to be free of reporting bias because the published results corresponded to those expected in these types of studies (Alexander 2015; Berger 2011; Bernburg 2016; Bernburg 2019; Calder Calisi 2017; Chesak 2015; Fei 2019; Gelkopf 2008; Ireland 2017; Khoshnazary 2016; Klatt 2015; Lin 2019; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mealer 2014; Mirzaeirad 2019; Poulsen 2015; Schroeder 2016; Sood 2011; Sood 2014; Tierney 1997; Villani 2013; West 2015).
We rated four non‐registered studies at high risk of bias, largely because not all of the prespecified outcomes were reported (Cieslak 2016; Duchemin 2015; Stetz 2007; Varker 2012). Cieslak 2016 randomly assigned participants to one of two intervention groups (self‐efficacy‐enhancing module, social support‐enhancing module) or a control group. However, due to high dropout in the social support‐enhancing module, only the results for two groups were analysed and reported.
Fifteen studies were prospectively or retrospectively registered (Cheung 2014; Clemow 2018; Hosseinnejad 2018; ISRCTN69644721; Lebares 2018; Loiselle 2018; Luthar 2017; Medisauskaite 2019; Mistretta 2018; NCT02603133; NCT03645798; Smith 2019; Strijk 2011; West 2014; Wild 2016). In addition, one study also provided a study protocol (Strijk 2011). Of these registered studies, we considered five studies to be at low risk of reporting bias as the published reports included all expected outcomes in the prespecified way (Cheung 2014; Lebares 2018; Loiselle 2018; Medisauskaite 2019; Wild 2016). Although actual helping behaviour as a prespecified outcome was not reported in Cheung 2014, we judged this study to be at low risk of bias as the study authors justified the non‐reporting by the small number of participants reporting this outcome, and unfeasible statistical analyses.
For three registered trials (ISRCTN69644721; NCT02603133; NCT03645798), we could not determine the risk of reporting bias on the basis of trial registrations, as the studies were completed but unpublished trials or no further information could be provided from the study authors during the publication process. The same applied to Smith 2019, for whom only a conference abstract was available.
We judged six registered trials at high risk of reporting bias because not all of the prespecified outcomes (Luthar 2017; Strijk 2011; West 2014) or time points (Hosseinnejad 2018; Mistretta 2018) were reported, and/or reported outcomes had not been prespecified (Clemow 2018; Luthar 2017; Mistretta 2018; Strijk 2011; West 2014).
Other potential sources of bias
We assessed the baseline comparability between study groups after randomisation as part of selection bias (random‐sequence generation) (see Allocation (selection bias)).
Effects of interventions
See: Table 1
See: Table 1.
Overall, across the included studies in healthcare professionals, we were able to perform 22 pooled analyses that combined at least two studies.
We present the different outcome measures that we used to assess the primary and secondary outcomes in the included studies in Table 3 and Table 4, respectively. For the primary outcomes of resilience and well‐being or quality of life, as well as all secondary outcomes (social support, optimism, self‐efficacy, active coping, self‐esteem, hardiness, positive emotions), positive values indicate a higher (i.e. better) level of the corresponding outcome in the intervention group compared to the control group (e.g. higher resilience), whereas negative values refer to lower levels of the outcome in the intervention arm. For the remaining primary outcomes of anxiety, depression and stress or stress perception, negative values indicate a lower (i.e. better) degree of these outcomes in the intervention arm (e.g. fewer depressive symptoms) compared to the control arm, while positive values refer to a higher level of depression, anxiety and stress or stress perception in the intervention group compared to control.
P values are reported exactly and where provided by study authors, unless P values are < 0.001, in which case they are expressed as P < 0.001. T values and P values of Egger's tests were rounded.
Comparison 1. Resilience intervention versus control condition in healthcare professionals
Primary outcomes
Resilience
Post‐intervention
Overall, 16 studies (three with mixed samples: Cieslak 2016; ISRCTN69644721; Wild 2016) evaluated the effect of resilience intervention compared to control groups on resilience immediately post‐intervention. Twelve studies reported data suitable for quantitative analysis (Bernburg 2019; Khoshnazary 2016; Klatt 2015; Lebares 2018; Lin 2019; Loiselle 2018; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mealer 2014; Schroeder 2016). The pooled effect estimate suggests evidence of a moderate effect of resilience interventions on resilience at post‐intervention (standardised mean difference (SMD) 0.45, 95% confidence interval (CI) 0.25 to 0.65; P < 0.001; I2 = 41%; Tau2 = 0.05; P for heterogeneity = 0.07; G2 = 66.9%; 95% prediction interval: −0.25 to 1.14; 12 studies, 690 participants; Analysis 1.1; very‐low certainty evidence, see Table 1).
1.1. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 1: Resilience: post‐intervention
For resilience at post‐intervention, we found no evidence of asymmetry in funnel plots or Egger’s test (t = −1.04; df = 10; P = 0.32; see Appendix 16).
Based on statistical indicators, we found moderate heterogeneity for resilience at post‐test.
Single study results
One study also measuring resilience at post‐intervention (NCT03645798) could not be pooled with the studies above, since we could not obtain the data from the study authors.
Studies with mixed samples
We were unable to pool three mixed studies measuring resilience at post‐intervention with the studies above, due to unavailable subgroup data (post‐traumatic growth in Cieslak 2016 and Wild 2016) or unpublished data that could not be obtained from the study authors (ISRCTN69644721). For the total sample of 168 health and human service professionals (e.g. physicians, nurses, education specialists, police officers), Cieslak 2016 demonstrated a significant group effect on post‐traumatic growth (Post‐traumatic Growth Inventory‐Short form; F = 6.10, P = 0.013) at post‐intervention, with lower values in the resilience training (mean = 3.04 (standard deviation (SD) = 0.78)) compared to attention control (mean = 3.18 (SD = 0.77)). Wild 2016, for the total sample of employees or volunteers working as front‐line or office‐based staff in one of four emergency services (police, fire and rescue, ambulance, search and rescue; 430 participants randomised; number analysed not specified), reported no significant difference in the level of resilience (Connor‐Davidson Resilience Scale) between resilience training and active control at post‐intervention (F = 0.42, P = 0.66; intervention arm: mean = 67.90 (SD = 17.03); control arm: mean = 68.48 (SD = 15.26)).
Short‐term follow‐up (≤ 3 months)
The effect of resilience‐training programmes versus control groups on resilience at short‐term follow‐up was assessed in 15 individually‐randomised studies (three with mixed samples: Cieslak 2016; ISRCTN69644721; Wild 2016), of which 11 studies could be combined into a meta‐analysis (Bernburg 2019; Chesak 2015; Cheung 2014; Lin 2019; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Schroeder 2016; Sood 2011; Sood 2014). The pooled SMD for resilience was 0.42 (95% CI 0.17 to 0.67; P = 0.001; I2 = 71%; Tau2 = 0.11; P for heterogeneity < 0.001; G2 = 85.4%; 95% prediction interval: −0.40 to 1.24; 11 studies, 1325 participants; Analysis 1.2), suggesting evidence of a moderate difference between the resilience‐training programme and control group (moderate effect size).
1.2. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 2: Resilience: short‐term follow‐up (≤ 3 months)
Based on funnel plots and Egger’s test, we identified statistically significant asymmetry for resilience at short‐term follow‐up (Egger’s test: t = 4.01; df = 9; P = 0.003).
Statistical indicators suggested substantial heterogeneity for resilience at short‐term follow‐up.
Single study results
One study available as a conference abstract (Smith 2019), which also measured resilience at short‐term follow‐up, could not be pooled with the studies above, since we could not obtain data by contacting the authors. For 29 nurses, Smith 2019 indicated no evidence of a difference in the change in resilience (CD‐RISC) between baseline and one‐month follow‐up (P = 0.84) or three‐month follow‐up (P = 0.26) between resilience training and control.
Studies with mixed samples
Due to unavailable subgroup data (Cieslak 2016; Wild 2016) or unpublished data (ISRCTN69644721), we could not pool three mixed studies assessing resilience at short‐term follow‐up with the aforementioned studies. For the total sample of 168 participants, Cieslak 2016 reported no significant group effect on post‐traumatic growth at one‐month follow‐up (F = 3.54, P = 0.062). Lower scores of post‐traumatic growth were shown in the intervention arm (mean = 3.03 (SD = 0.81)) compared to the attention control arm (mean = 3.10 (SD = 0.79)). Wild 2016, for the total sample of four emergency services (including ambulance personnel; 430 participants randomised; number analysed not specified), also reported no significant between‐group difference in resilience at three‐month follow‐up (F value see Resilience – post‐intervention; intervention arm: mean = 68.67 (SD = 16.17); control arm: mean = 70.23 (SD = 14.69)).
Medium‐term follow‐up (> 3 to ≤ 6 months)
Two studies comparing a resilience intervention to control at medium‐term follow‐up provided suitable data for quantitative analysis (684 participants) and showed little or no evidence of a difference between the resilience intervention and control in resilience (SMD 0.35, 95% CI −0.41 to 1.11; P = 0.37; I2 = 87%; Tau2 = 0.27; P for heterogeneity = 0.005; G2 = 0%; 95% prediction interval: incalculable due to only two studies; moderate effect size; 2 studies, 684 participants; Analysis 1.3).
1.3. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 3: Resilience: medium‐term follow‐up (> 3≤ 6 months)
For resilience at medium‐term follow‐up, we found considerable heterogeneity (e.g. I2 of 87%), whereas G2 indicated no statistical heterogeneity.
Long‐term follow‐up (> 6 months)
At long‐term follow‐up, only two studies assessed the effects of resilience intervention compared to control on self‐reported resilience and could be combined in a meta‐analysis (Bernburg 2019; Lebares 2018). The pooled SMD on resilience was 0.30 (95% CI −0.08 to 0.68; P = 0.12; I2 = 0%; Tau2 = 0; P for heterogeneity 0.97; G2 = 0%; 95% prediction interval: incalculable due to only two studies; 2 studies, 107 participants; Analysis 1.4), indicating little or no evidence of a difference between the resilience‐training programme and control group.
1.4. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 4: Resilience: long‐term follow‐up (> 6 months)
Statistical indicators consistently suggested no heterogeneity for resilience at long‐term follow‐up.
Mental health and well‐being: anxiety
Post‐intervention
Eight studies (including two with mixed samples: ISRCTN69644721; Wild 2016) evaluated the effect of resilience intervention compared to control on self‐reported anxiety immediately post‐intervention. Five studies reported data suitable for quantitative analysis (Calder Calisi 2017; Mealer 2014; Medisauskaite 2019; Mistretta 2018; Villani 2013). The pooled effect estimate suggests little or no evidence of an effect of resilience training on post‐intervention anxiety (SMD −0.06, 95% CI −0.35 to 0.23; P = 0.67; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.99; G2 = 0.5%; 95% prediction interval: −0.19 to 0.06; 5 studies, 231 participants; Analysis 1.5; very‐low certainty evidence, see Table 1).
1.5. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 5: Anxiety: post‐intervention
Based on statistical indicators, there was no heterogeneity for anxiety at post‐intervention.
Single study results
Stetz 2007 (see Stetz 2008) also assessed the effect of resilience training compared to control on post‐intervention anxiety, but could not be combined with the above studies. The study authors only reported summary data for the Multiple Affect Adjective Check List‐Revised (e.g. depression, anxiety, and positive affect subscale) and found evidence for a group difference in psychological stress (F = 3.3, P < 0.001; 63 participants randomised, number analysed not specified).
Studies with mixed samples
For two studies with mixed samples, we were unable to retrieve the subgroup data for healthcare professionals from the study authors (ISRCTN69644721; Wild 2016). For the total sample (including ambulance personnel; 430 participants randomised; number analysed not specified), Wild 2016 found no evidence of a between‐group difference between resilience training and active control in anxiety (General Anxiety Disorder Scale‐7) at post‐test (intervention arm: mean = 3.15 (SD = 3.08); control arm: mean = 3.27 (SD = 3.43)). For the unpublished study, ISRCTN69644721, we were unable to obtain data on anxiety from the study authors.
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, seven studies compared the impact of a resilience intervention versus control on anxiety. We were able to combine four studies into analysis (Chesak 2015; Mistretta 2018; Sood 2011; Sood 2014). The pooled SMD for short‐term self‐reported anxiety was −0.63 (95% CI −0.98 to −0.27; P < 0.001; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.95; G2 = 0%; 95% prediction interval: −1.40 to 0.15; 4 studies, 133 participants; Analysis 1.6), providing evidence for a moderate difference between groups favouring resilience training for this outcome (moderate effect size).
1.6. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 6: Anxiety: short‐term follow‐up (≤ 3 months)
For anxiety at short‐term follow‐up, we found no heterogeneity based on statistical indicators.
Single study results
We could not pool one study (Varker 2012) with the aforementioned studies because it evaluated a resilience intervention developed for healthcare personnel in individuals from the general population (proof‐of‐concept study; 77 participants). The effect of a resilience intervention on anxiety compared to attention control was assessed at one‐month follow‐up (Depression Anxiety and Stress Scale). However, the study authors only reported summary data (multivariate analysis of variance (MANOVA) results) for depression, anxiety and stress with a significant time × group interaction (F = 2.89, P < 0.05). Post hoc analyses for anxiety were not reported.
Studies with mixed samples
Two mixed studies measuring anxiety at short‐term follow‐up could not be pooled with the above studies, due to unavailable subgroup or unpublished data for healthcare professionals (Wild 2016; ISRCTN69644721). Comparable with post‐intervention, Wild 2016 found no evidence of a between‐group difference in anxiety at three‐month follow‐up (intervention arm: mean = 2.83 (SD = 3.32); control arm: mean = 3.02 (SD = 3.76)) for the total sample (including ambulance personnel; 430 participants randomised; number analysed not specified).
Mental health and well‐being: depression
Post‐intervention
Overall, 20 studies (including three mixed studies: Cieslak 2016; ISRCTN69644721; Wild 2016) assessed the effect of a resilience intervention versus control on self‐reported depression (or burnout; see Helmreich 2017 and Appendix 6 in this review) at post‐intervention. For one study investigating healthcare and non‐healthcare professionals, we were able to retrieve the relevant subgroup data from the study authors (Cieslak 2016). Comparable with the original study, we performed an intention‐to‐treat analysis based on expectation‐minimisation (EM) imputation for healthcare professionals (n = 134; e.g. nurses, physicians, psychotherapists, social workers) included in Cieslak 2016. Analysis of 14 studies providing suitable data for effect size calculation (Alexander 2015; Calder Calisi 2017; Cieslak 2016; Ireland 2017; Lebares 2018; Loiselle 2018; Luthar 2017; Mache 2017; Mealer 2014; Medisauskaite 2019; Mistretta 2018; Schroeder 2016; West 2014; West 2015) suggested evidence for a small difference between resilience training and control group for post‐intervention depression (SMD −0.29, 95% CI −0.50 to −0.09; P = 0.005; I2 = 42%; Tau2 = 0.06; P for heterogeneity = 0.05; G2 = 89.3%; 95% prediction interval: −0.95 to 0.37; 14 studies, 788 participants; Analysis 1.7; very‐low certainty evidence, see Table 1).
1.7. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 7: Depression: post‐intervention
Based on funnel plots and Egger’s test, we found no statistically significant asymmetry for depression at post‐intervention (see Appendix 16; Egger’s test: t = −0.10; df = 12; P = 0.93).
From the statistical indicators of heterogeneity, I2 suggested moderate heterogeneity, whereas other values (e.g. Chi2 test; G2) indicated substantial heterogeneity for depression at post‐test.
Single‐study results
Four other studies comparing the effect of resilience training to control on post‐intervention depression could not be pooled with the above studies for different reasons. Duchemin 2015 (32 participants) provided no post‐test values for burnout, but only a narrative report of no change in burnout scores (emotional exhaustion, depersonalisation, personal accomplishment subscales of Maslach Burnout Inventory) between pre‐ and post‐test. The number of participants with scores above 26 on emotional exhaustion was reduced by 34% in the resilience‐training group compared to no change in the wait‐list control group (no P value reported). As Stetz 2007 only reported summary outcome data (MANOVA results), there was insufficient information to estimate an intervention effect and to include it in Analysis 1.7. For two unpublished studies (NCT02603133; NCT03645798) we could not obtain the data from the study authors.
Studies with mixed samples
For two studies with mixed samples, we could not obtain the subgroup data for healthcare professionals from the study authors (ISRCTN69644721; Wild 2016). For the total sample (including ambulance personnel; 430 participants randomised; number analysed not specified), Wild 2016 found no evidence of a difference between resilience training and active control for depression (Patient Health Questionnaire‐9) at post‐test (intervention arm: mean = 3.48 (SD = 3.18); control arm: mean = 3.81 (SD = 4.42)). For the unpublished study (ISRCTN69644721) we could not obtain the subgroup data from the authors.
Short‐term follow‐up (≤ 3 months)
The effect of resilience training compared to control on self‐reported depression at short‐term follow‐up was evaluated in 13 studies (including three mixed studies: Cieslak 2016; ISRCTN69644721; Wild 2016). Using the subgroup data provided by the study authors, we conducted an EM imputation in Cieslak 2016 (comparable to original study). An analysis of eight studies (including one mixed study with available subgroup data: Cieslak 2016), that could be combined (Berger 2011; Cieslak 2016; Clemow 2018; Luthar 2017; Mache 2017; Mistretta 2018; Schroeder 2016; West 2014) revealed evidence of a moderate difference between groups favouring resilience training for this outcome (SMD −0.52, 95% CI −0.81 to −0.23; P < 0.001; I2 = 50%; Tau2 = 0.08; P for heterogeneity = 0.05; G2 = 97.0%; 95% prediction interval: −1.33 to 0.29; 8 studies; 545 participants; Analysis 1.8; moderate effect size).
1.8. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 8: Depression: short‐term follow‐up (≤ 3 months)
For depression at short‐term follow‐up, substantial heterogeneity was indicated by all statistical values.
Single study results
Since we could not access data for one study available only as a conference abstract (Smith 2019), we could not combine this study, which also measured depression (burnout) at short‐term follow‐up, with the aforementioned studies. For 29 nurses (intervention arm: 16; control arm: 13), the authors reported a significant difference between resilience training and control in burnout scores (Professional Quality of Life Scale‐5) at one‐month follow‐up (P = 0.04). As mentioned above (see Anxiety – short‐term follow‐up), Varker 2012 only reported summary data for depression at one‐month follow‐up (MANOVA results with anxiety, depression and stress) in individuals from the general population (77 participants). The authors demonstrated a statistically significant time × group interaction (F = 2.89, P < 0.05): While depression scores decreased in the intervention group, they increased in the control group. For one unpublished study, NCT02603133, we could not obtain the data from the study authors.
Studies with mixed sample
Two mixed studies measuring the effects of resilience intervention versus control on depression at short‐term follow‐up could not be pooled with the above studies (ISRCTN69644721; Wild 2016). Comparable to post‐intervention, Wild 2016, based on the data for the total sample (including ambulance personnel; 430 participants randomised; number analysed not specified) also found no evidence for a difference in depression at three‐month follow‐up (intervention arm: mean = 3.17 (SD = 3.61); control arm: mean = 3.41 (SD = 4.08)). For one unpublished trial (ISRCTN69644721), we could not obtain the (subgroup) results for depression at this time point from the study authors.
Medium‐term follow‐up (> 3 to ≤ 6 months)
At medium‐term follow‐up, one study assessed the impact of resilience training compared to control on self‐reported burnout (Mache 2017). Using the emotional exhaustion subscale of the Maslach Burnout Inventory (range: 1 (best) to 6 (worst)), Mache 2017 found a mean difference (MD) of −0.40 (95% CI −0.75 to −0.05; P = 0.03; 1 study, 60 participants; Analysis 1.9), indicating evidence for a difference between the resilience training and control groups.
1.9. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 9: Depression: medium‐term follow‐up (> 3 ≤ 6 months)
Long‐term follow‐up (> 6 months)
The effects of a resilience intervention compared to control on self‐reported depression or burnout at long‐term follow‐up were measured by two studies that could be combined into a meta‐analysis (Lebares 2018; West 2014). The pooled SMD was 0.09 (95% CI −0.33 to 0.51; P = 0.68; I2 = 0%; Tau2 = 0; P for heterogeneity 0.56; G2 = 0%; 95% prediction interval: incalculable due to only two studies; 2 studies, 87 participants; Analysis 1.10), indicating little or no evidence for a difference between the resilience‐training programme and control groups for depression at long‐term follow‐up.
1.10. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 10: Depression: long‐term follow‐up (> 6 months)
Statistical indicators consistently suggested no heterogeneity for depression at long‐term follow‐up.
Mental health and well‐being: stress or stress perception
Post‐intervention
Eighteen studies evaluated the effect of a resilience intervention compared to control groups on self‐reported stress symptoms or the subjective perception of stress immediately post‐intervention. We were able to combine 17 studies (Bernburg 2016; Bernburg 2019; Calder Calisi 2017; Duchemin 2015; Fei 2019; Ireland 2017; Lebares 2018; Lin 2019; Loiselle 2018; Luthar 2017; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mistretta 2018; Schroeder 2016; West 2014). The pooled effect estimate suggests evidence for a moderate effect of resilience interventions on stress or stress perception at post‐intervention (SMD −0.61, 95% CI −1.07 to −0.15; P = 0.01; I2 = 90%; Tau2 = 0.79; P for heterogeneity < 0.001; G2 = 98.7%; 95% prediction interval: −2.86 to 1.65; 17 studies, 997 participants; Analysis 1.11; very‐low certainty evidence, see Table 1).
1.11. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 11: Stress or stress perception: post‐intervention
We found no indication of asymmetry for stress or stress perception immediately post‐intervention (see Appendix 16; Egger’ test: t = −0.34; df = 15; P = 0.74).
For stress or stress perception at post‐test, all statistical values indicated substantial to considerable heterogeneity.
Single study results
One study also measuring stress or stress perception at post‐intervention could not be pooled with the studies above for the following reason: in Mirzaeirad 2019 (80 participants), the relative proportion of participants with low, moderate and high (nursing) stress at post‐intervention were presented (intervention arm: low stress = 3 (7.5%), moderate = 33 (82.5%), high = 4 (10%); control arm: low stress = 0, moderate = 22 (55%), high = 18 (45%)). The investigators reported a significant between‐group difference favouring resilience training in perceived stress (P < 0.001).
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, 17 studies compared the impact of resilience training on self‐reported stress or stress perception to control. Fourteen studies reported data suitable for quantitative analysis and could be combined (Bernburg 2016; Bernburg 2019; Chesak 2015; Lin 2019; Luthar 2017; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mistretta 2018; Schroeder 2016; Sood 2011; Sood 2014; West 2014). Analysis of these studies suggests evidence for a moderate difference between groups favouring resilience training in stress or stress perception within three months post‐intervention (SMD −0.46, 95% CI −0.67 to −0.25; P < 0.001; I2 = 53%; Tau2 = 0.08; P for heterogeneity = 0.01; G2 = 99.1%; 95% prediction interval: −1.14 to 0.22; 14 studies, 788 participants; Analysis 1.12).
1.12. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 12: Stress or stress perception: short‐term follow‐up (≤ 3 months)
Based on funnel plots and Egger’s test, we found no statistically significant asymmetry for stress or stress perception at short‐term follow‐up (Egger’s test: t = −1.32; df = 12; P = 0.21).
For stress or stress perception at short‐term follow‐up, results for statistical heterogeneity were mixed, with I2 indicating moderate to substantial heterogeneity (53%), while others (e.g. G2) suggested substantial heterogeneity.
Single study results
Three studies also measuring stress or stress perception at short‐term follow‐up could not be pooled with the studies above. We could not obtain the data after contacting the authors for one study available as a conference abstract (Smith 2019). As mentioned above (see Anxiety), Varker 2012, as a proof‐of‐concept study, only reported summary data for stress (MANOVA results with anxiety, depression and stress) in individuals from the general population. The study authors found a significant time × group interaction (F = 2.89, P < 0.05; 77 participants). Post hoc tests revealed a larger reduction in stress in the intervention arm compared to the control arm. The findings for perceived stress (nursing stress) at three‐month follow‐up in Mirzaeirad 2019 (80 participants) were only reported indirectly by analysis of covariance (ANCOVA) results (F = 108.141; P < 0.001).
Medium‐term follow‐up (> 3 to ≤ 6 months)
At medium‐term follow‐up, one study reported on stress or stress perception (Mache 2017). Using the Perceived Stress Questionnaire (range: 1 (best) to 4 (worst)), the authors reported a significant difference (P < 0.01) in favour of the intervention arm at six‐month follow‐up (intervention arm: mean = 2.80 (SD = 0.70); control arm: mean = 3.20 (SD = 0.62)). The MD also indicated evidence of an effect of the resilience intervention on stress or perception of stress at medium‐term follow‐up (MD −0.40, 95% CI −0.73 to −0.07; P = 0.02; 1 study, 60 participants; Analysis 1.13).
1.13. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 13: Stress or stress perception: medium‐term follow‐up (> 3 ≤ 6 months)
Long‐term follow‐up (> 6 months)
Three studies measured the effects of resilience intervention compared to control on self‐reported stress or stress perception at long‐term follow‐up and could be combined in a meta‐analysis (Bernburg 2019; Lebares 2018; West 2014). The pooled SMD was −0.39 (95% CI −0.84 to 0.05; P = 0.09; I2 = 47%; Tau2 = 0.07; P for heterogeneity 0.15; G2 = 94.0%; 95% prediction interval: −4.85 to 4.07; 3 studies, 173 participants; Analysis 1.14), suggesting little or no evidence for a difference between a resilience‐training programme and control group for stress or stress perception at long‐term follow‐up.
1.14. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 14: Stress or stress perception: long‐term follow‐up (> 6 months)
For stress or stress perception at long‐term follow‐up, we partly found moderate heterogeneity (e.g. I2, Chi2 test), while G2 suggested substantial heterogeneity.
Mental health and well‐being: well‐being or quality of life
Post‐intervention
At post‐intervention, 17 studies (including two with mixed samples: ISRCTN69644721; Wild 2016) assessed the effect of a resilience intervention compared to control on self‐reported well‐being or quality of life. Thirteen studies provided data suitable for quantitative analysis (Bernburg 2016; Calder Calisi 2017; Duchemin 2015; Klatt 2015; Lin 2019; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mistretta 2018; Strijk 2011; West 2014; West 2015). The analysis revealed little or no evidence of an effect of training (SMD 0.14, 95% CI −0.01 to 0.30; P = 0.07; I2 = 31%; Tau2 = 0.02; P for heterogeneity = 0.13; G2 = 93.4%; 95% prediction interval: −0.41 to 0.75; 13 studies, 1494 participants; Analysis 1.15; very‐low certainty evidence, see Table 1).
1.15. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 15: Well‐being or quality of life: post‐intervention
We found no statistical indication of asymmetry for well‐being or quality of life at post‐intervention (see Appendix 16; Egger’s test: t = 1.91; df = 11; P = 0.08).
We found mixed results for heterogeneity, with three indicators (e.g. I2) representing moderate heterogeneity, while G2 indicated substantial heterogeneity.
Single study results
Two unpublished trials (NCT02603133; NCT03645798) also assessed the effect of a resilience intervention compared to control on post‐intervention happiness (NCT02603133) and job satisfaction (NCT03645798), but could not be pooled with the abovementioned studies because we were unable to obtain the data from the study authors.
Studies with mixed samples
We were unable to include two mixed studies examining healthcare and non‐healthcare professionals in the meta‐analysis for well‐being or quality of life at post‐test, as relevant subgroup data were not available (ISRCTN69644721; Wild 2016). For the total sample investigated (including ambulance personnel; 430 participants randomised; number analysed not specified), Wild 2016 found no significant difference between resilience training and active control on well‐being (Warwick‐Edinburgh Mental Wellbeing scale) at post‐test (F = 0.06, P = 0.94; intervention arm: mean = 50.70 (SD = 9.37); control arm: mean = 51.28 (SD = 9.93)). For one unpublished trial (ISRCTN69644721) subgroup data for ambulance personnel were not available from the study authors.
Short‐term follow‐up (≤ 3 months)
The effect of resilience training compared to control on self‐reported well‐being or quality of life at short‐term follow‐up was evaluated in 15 studies (including two with mixed samples: ISRCTN69644721; Wild 2016). Analysis of 12 studies for which quantitative results were available (Bernburg 2016; Cheung 2014; Hosseinnejad 2018; Lin 2019; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mistretta 2018; Sood 2011; Sood 2014; West 2014), suggested little or no evidence for an effect of training (SMD 0.07, 95% CI −0.04 to 0.18; P = 0.22; I2 = 1%; Tau2 = 0; P for heterogeneity = 0.43; G2 = 91.3%; 95% prediction interval: −0.21 to 0.46; 12 studies, 1413 participants; Analysis 1.16).
1.16. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 16: Well‐being or quality of life: short‐term follow‐up (≤ 3 months)
Based on funnel plots and Egger’s test, we identified statistically significant asymmetry for well‐being or quality of life at short‐term follow‐up (Egger’s test: t = 2.43; df = 10; P = 0.04).
For well‐being or quality of life at short‐term follow‐up, we also found mixed results for statistical heterogeneity, with three indicators (e.g. I2) suggesting no important heterogeneity, whereas G2 indicated substantial heterogeneity.
Studies with mixed samples
Two studies with mixed samples also compared the effects of a resilience intervention to control on well‐being or quality of life at short‐term follow‐up, but could not be combined in analysis due to unavailable subgroup data. Wild 2016, for the total sample from four emergency services (430 participants randomised; number analysed not specified), found no significant between‐group difference in well‐being (F = 0.06, P = 0.94; intervention arm: mean = 50.56 (SD = 9.02); control arm: mean = 50.88 (SD = 9.43)). For the unpublished trial (ISRCTN69644721) we could not obtain subgroup data for ambulance personnel from the study authors.
Medium‐term follow‐up (> 3 to ≤ 6 months)
All three studies comparing a resilience intervention to control at medium‐term follow‐up provided suitable data for quantitative analysis and showed little or no evidence for a difference between the resilience intervention and control on well‐being or quality of life (SMD −0.08, 95% CI −0.31 to 0.16; P = 0.52; I2 = 73%; Tau2 = 0.03; P for heterogeneity = 0.02; G2 = 97.7%; 95% prediction interval: −2.71 to 2.56; 3 studies, 1414 participants; Analysis 1.17).
1.17. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 17: Well‐being or quality of life: medium‐term follow‐up (> 3 ≤ 6 months)
Based on statistical indicators, we found substantial heterogeneity for well‐being or quality of life at medium‐term follow‐up.
Long‐term follow‐up (> 6 months)
At long‐term follow‐up, only one study compared the effects of a resilience intervention to control on quality of life (West 2014). Using a single‐item linear analogue question (range 0 (worst) to 10 (best)), the study authors found an increase in quality of life of 1.5% in the intervention arm compared to 1.8% in the control arm (P = 0.63). Similarly, the MD also indicated little or no effect of training on quality of life at 12 months post‐intervention (MD −0.20, 95% CI −0.94 to 0.54; P = 0.59; 1 study, 66 participants; Analysis 1.18).
1.18. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 18: Well‐being or quality of life: long‐term follow‐up (> 6 months)
Secondary outcomes
Resilience factors: social support
Post‐intervention
Studies with mixed samples
Only one (mixed) study (Wild 2016) assessed perceived social support at post‐intervention. Since we could not obtain subgroup data from the study authors, we could not calculate a mean difference. For the total sample (i.e. employees or volunteers working as front‐line or office‐based staff in one of four emergency services: police, fire and rescue, ambulance, search and rescue; 430 participants randomised; number analysed not specified), Wild 2016 reported no significant differences between the intervention and control group in perceived social support (13 items for social support) at home (F = 0.402, P = 0.67) or at work (F = 0.896, P = 0.40), at post‐intervention (at home: intervention arm: mean = 33.63 (SD = 6.44), control arm: mean = 32.83 (SD = 7.09); at work: intervention arm: mean = 27.20 (SD = 6.59), control arm: mean = 27.14 (SD = 7.16)).
Short‐term follow‐up (≤ 3 months)
We combined data from two studies to estimate the effects of a resilience intervention compared to control on social support at short‐term follow‐up (Cheung 2014; Clemow 2018). The pooled SMD for social support was −0.07 (95% CI −0.22 to 0.08; P = 0.36; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.96; G2 = 0%; 95% prediction interval: incalculable due to only two studies; 2 studies, 825 participants; Analysis 1.19), suggesting little or no evidence for an effect of a resilience intervention on social support within three months post‐intervention.
1.19. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 19: Social support: short‐term follow‐up (≤ 3 months)
For social support at short‐term follow‐up, we found no heterogeneity based on statistical indicators.
Studies with mixed samples
Wild 2016 reported on perceived social support at short‐term follow‐up in a mixed sample. However, subgroup data for ambulance personnel were not available. For the total sample (i.e. four emergency services: police, fire and rescue, ambulance, search and rescue; 430 participants randomised; number analysed not specified), the investigators reported no significant difference between the intervention and control group in perceived social support (13 items for social support) at home (F = 0.402, P = 0.67) or at work (F = 0.896, P = 0.40) at the three‐month follow‐up (at home: intervention arm mean = 34.17 (SD = 6.51), control arm mean = 33.28 (SD = 7.80); at work: intervention arm mean = 27.67 (SD = 6.60), control arm mean = 26.79 (SD = 7.08)).
Medium‐term follow‐up (> 3 to ≤ 6 months)
At medium‐term follow‐up, Cheung 2014 reported lower values for social support (Multidimensional Scale of Perceived Social Support; range 1 (worst) to 7 (best)) in the intervention group (mean = 4.94 (SD = 1.11) compared to wait‐list control (mean = 5.04 (SD = 1.08)). However, the authors identified no significant time × treatment interaction (F = 0.85, P > 0.05) and no significant change in social support in both groups over time. Similarly, the MD for this outcome also indicated little or no evidence for a difference in social support at medium‐term follow‐up (MD −0.10; 95% CI −0.27 to 0.07; P = 0.25; 1 study, 624 participants; Analysis 1.20).
1.20. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 20: Social support: medium‐term follow‐up (> 3 ≤ 6 months)
Optimism
Post‐intervention
At post‐intervention, three studies (including one mixed study: Gelkopf 2008) reported the effects of a resilience intervention compared to control on self‐reported optimism (Gelkopf 2008; Mache 2015a; Mache 2015b). We obtained the subgroup data for healthcare professionals in Gelkopf 2008 from the study authors. The analysis revealed a moderate effect favouring resilience training (SMD 0.41, 95% CI 0.10 to 0.72; P = 0.009; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.93; G2 = 0%; 95% prediction interval: −1.58 to 2.40; 3 studies, 169 participants; Analysis 1.21).
1.21. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 21: Optimism: post‐intervention
For optimism at post‐test, no heterogeneity was indicated by any statistical values.
Short‐term follow‐up (≤ 3 months)
Two studies assessed the effect of a resilience‐training programme versus control on optimism at short‐term follow‐up (Mache 2015a; Mache 2015b). We combined the data from the two studies, which suggested evidence for a moderate effect of resilience training on optimism within three months post‐intervention (SMD 0.44, 95% CI 0.12 to 0.76; P = 0.008; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.72; G2 = 0%; 95% prediction interval: incalculable due to only two studies; 2 studies, 153 participants; Analysis 1.22).
1.22. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 22: Optimism: short‐term follow‐up (≤ 3 months)
Statistical indicators consistently suggested no heterogeneity for optimism at short‐term follow‐up.
Self‐efficacy
Post‐intervention
Eight individually‐randomised studies assessed the effect of a resilience intervention compared to control on self‐reported self‐efficacy at post‐intervention (with three studies with mixed samples: Cieslak 2016; Gelkopf 2008; Wild 2016); including two of the mixed studies (Cieslak 2016: EM imputation performed; Gelkopf 2008: subgroup data from the study authors), we had six studies providing data suitable for quantitative analysis (Bernburg 2019; Cieslak 2016; Gelkopf 2008; Mache 2015a; Mache 2015b; Mache 2016). The analysis revealed evidence for a moderate difference favouring resilience training for self‐efficacy at post‐test (SMD 0.43, 95% CI 0.25 to 0.62; P < 0.001; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.52; G2 = 45.4%; 95% prediction interval: −0.004 to 0.88; 6 studies, 461 participants; Analysis 1.23).
1.23. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 23: Self‐efficacy: post‐intervention
We found mixed results for heterogeneity in self‐efficacy at post‐intervention, with some indicators suggesting no heterogeneity (e.g. I2), whereas G2 was of moderate size.
Single study results
For the unpublished study NCT03645798, we were unable to retrieve any data from the authors.
Studies with mixed samples
Wild 2016 also assessed self‐efficacy at post‐intervention, but we were unable to combine these data with the studies above, due to unavailable subgroup data for ambulance personnel. For the total sample (430 participants randomised; number analysed not specified) including employees or volunteers from four emergency services, Wild 2016 reported no significant difference (F = 1.85, P = 0.16) between resilience training and active control in self‐reported self‐efficacy (General Self‐Efficacy Scale) at post‐intervention (intervention arm: mean = 31.74 (SD = 4.49); control arm: mean = 31.91 (SD = 4.74)).
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, nine studies reported on self‐efficacy, including two mixed studies involving healthcare and non‐healthcare professionals (Cieslak 2016; Wild 2016). After having received the relevant subgroup data for Cieslak 2016 and performing EM imputation for this study, we combined the data from seven studies (Berger 2011; Bernburg 2019; Cheung 2014; Cieslak 2016; Mache 2015a; Mache 2015b; Mache 2016), comparing the impact of a resilience‐training programme to control on self‐efficacy. The pooled effect estimate (SMD) was 0.32 (95% CI 0.13 to 0.51; P = 0.001; I2 = 51%; Tau2 = 0.03; P for heterogeneity = 0.06; G2 = 69.6%; 95% prediction interval: −0.30 to 0.96; 7 studies, 1258 participants; Analysis 1.24), suggesting a small effect of resilience training on self‐reported self‐efficacy within three months post‐intervention.
1.24. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 24: Self‐efficacy: short‐term follow‐up (≤ 3 months)
For self‐efficacy at short‐term follow‐up, we found moderate to substantial heterogeneity.
Single study results
One further study reporting on self‐reported self‐efficacy at short‐term follow‐up could not be included in the meta‐analysis. Smith 2019 had no quantitative findings for self‐efficacy (measured by the Occupational Coping Self‐Efficacy Questionnaire for Nurses; see NCT03017469) in the conference abstract, and we could not retrieve the data from the study authors.
Studies with mixed samples
We were unable to pool data from Wild 2016, investigating employees or volunteers from four emergency services, with the studies above, due to unavailable subgroup data for ambulance personnel. For the total sample (430 participants randomised; number analysed not specified), the study authors reported no significant difference (F = 1.85, P = 0.16) between resilience training and active control in self‐reported self‐efficacy (General Self‐Efficacy Scale) at three‐month follow‐up (intervention arm: mean = 31.96 (SD = 4.56); control arm: mean = 32.52 (SD = 4.30)).
Medium‐term follow‐up (> 3 to ≤ 6 months)
In one study measuring self‐efficacy (13‐item self‐efficacy scale; range 1 (worst) to 4 (best)) at medium‐term follow‐up (Cheung 2014), higher scores for self‐efficacy were found in the intervention arm (mean = 3.01 (SD = 0.38)) than the control arm (mean = 2.84 (SD = 0.45)). The study authors reported a significant time × treatment interaction (F = 30.28, P < 0.001), with a sustained increase in self‐efficacy in the intervention arm at six‐months follow‐up compared to no change in the control arm. The MD also suggested evidence of an effect of resilience training on this outcome at medium‐term follow‐up (MD 0.17, 95% CI 0.10 to 0.24; P < 0.001; 1 study, 624 participants; Analysis 1.25).
1.25. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 25: Self‐efficacy: medium‐term follow‐up (> 3 ≤ 6 months)
Long‐term follow‐up (> 6 months)
Only one study compared the effects of a resilience intervention to control on self‐reported self‐efficacy at long‐term follow‐up (Bernburg 2019). Using the Self‐Efficacy, Optimism and Pessimism (SWOP‐K9) scale (range 0 (worst) to 4 (best)), the investigators reported a significant between‐group difference for self‐efficacy at nine‐month follow‐up (P = 0.01; probable typo in Table 2). The MD indicated little or no evidence of an effect of training on self‐efficacy at long‐term follow‐up (MD 0.19, 95% CI −0.02 to 0.40; P = 0.08; 1 study, 86 participants; Analysis 1.26).
1.26. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 26: Self‐efficacy: long‐term follow‐up (> 6 months)
Active coping
Post‐intervention
Four studies (including two studies with mixed samples: Gelkopf 2008; Wild 2016) assessed the effect of a resilience intervention compared to control on the resilience factor of active coping at immediate post‐intervention. For Gelkopf 2008, we received the relevant subgroup data from the investigators, resulting in three studies providing data suitable for quantitative analysis (Gelkopf 2008; Medisauskaite 2019; Villani 2013). The pooled SMD, was 0.28 (95% CI −0.31 to 0.87; P = 0.35; I2 = 52%; Tau2 = 0.14; P for heterogeneity = 0.12; G2 = 93.6%; 95% prediction interval: −5.85 to 6.41; 3 studies, 137 participants; Analysis 1.27), suggesting little or no evidence for a difference between resilience training and control in post‐intervention active coping.
1.27. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 27: Active coping: post‐intervention
For active coping at post‐intervention, moderate to substantial heterogeneity was indicated by statistical values.
Studies with mixed samples
Wild 2016 also assessed active coping at post‐intervention, but could not be pooled with the aforementioned studies, due to unavailable subgroup data for ambulance personnel. For the total sample (i.e. employees or volunteers working as front‐line or office‐based staff in one of four emergency services: police, fire and rescue, ambulance, search and rescue; 430 participants randomised; number analysed not specified), Wild 2016 reported no evidence of a between‐group difference in active coping at post‐test (intervention arm: mean = 5.45 (SD = 1.53); control arm: mean = 5.38 (SD = 1.56); P value not reported)).
Short‐term follow‐up (≤ 3 months)
From the two studies comparing the effects of resilience training to control on active coping at short‐term follow‐up (including the mixed study by Wild 2016), Cheung 2014 reported lower scores of active coping (adaptive coping) assessed by the Brief Coping Orientations to Problems Experience (Brief COPE) scale (range for adaptive coping: 1 (worst) to 4 (best)) in the intervention arm (mean = 2.51 (SD = 0.65)) than in the control arm (mean = 2.53 (SD = 0.62)). The MD for this study indicated little or no evidence of effect of a resilience intervention compared to wait‐list control on active coping at short‐term follow‐up (MD −0.02, 95% CI −0.11 to 0.07; P = 0.67; 1 study, 733 participants; Analysis 1.28).
1.28. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 28: Active coping: short‐term follow‐up (≤ 3 months)
Studies with mixed samples
Wild 2016 could not be pooled with Cheung 2014, as we were not able to obtain the subgroup data for healthcare professionals from the authors. Similarly to post‐intervention, the study showed no evidence of a difference between resilience training and active control for the total sample (four emergency services; 430 participants randomised; number analysed not specified) at short‐term follow‐up (intervention arm: mean = 5.37 (SD = 1.55); control arm: mean = 5.66 (SD = 1.57); P value not presented).
Medium‐term follow‐up (> 3 ≤ 6 months)
At medium‐term follow‐up, only one study assessed the effects on active coping. Cheung 2014 reported lower scores of active coping (adaptive coping) assessed by the Brief COPE scale (range for adaptive coping: 1 (worst) to 4 (best)) in the intervention arm (mean = 2.57 (SD = 0.62)) than in the control arm (mean = 2.6 (SD = 0.57)). The study authors found a significant time × treatment interaction (F = 4.09, P < 0.05), with an increase in active coping in the control arm compared to no change in the intervention arm. The MD for this study indicated little or no evidence of an effect of resilience intervention compared to wait‐list control on active coping at medium‐term follow‐up (MD −0.03, 95% CI −0.12 to 0.06; P = 0.53; 1 study, 624 participants; Analysis 1.29).
1.29. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 29: Active coping: medium‐term follow‐up (> 3 ≤ 6 months)
Self‐esteem
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, one study (Berger 2011) compared the effect of a resilience intervention to control on self‐esteem. Using the Rosenberg Self‐Esteem Scale (RSE; range 10 (worst) to 40 (best)), the study authors found an increase in self‐esteem in the intervention arm after training (mean = 37.4 (SD = 3.5)) compared to the control arm (mean = 32.1 (SD = 3.9)), but no significant time x group interaction (F = 2.8, P > 0.05). The MD indicated evidence for an effect of the resilience intervention on this outcome (MD 5.30, 95% CI 3.67 to 6.93; P < 0.001; 1 study, 80 participants; Analysis 1.30).
1.30. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 30: Self‐esteem: short‐term follow‐up (≤ 3 months)
Hardiness
Post‐intervention
One study assessed the effects of hardiness training compared to a no‐intervention control on hardiness at post‐intervention (Tierney 1997). Using the Personal Views Survey, Tierney 1997 reported higher values of hardiness in the intervention arm (mean = 78.16 (SD = 6.98)) compared to the control arm (mean = 74.64 (SD = 8.71)), with no significant difference in change scores between the two conditions. The MD also showed little or no evidence of a difference in favour of the resilience intervention for post‐intervention hardiness (MD 3.52, 95% CI −1.19 to 8.23; P = 0.14; 1 study, 43 participants; Analysis 1.31).
1.31. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 31: Hardiness: post‐intervention
Medium‐term follow‐up (> 3 to ≤ 6 months)
At medium‐term follow‐up, Tierney 1997 showed similar hardiness scores (Personal Views Survey) in the two groups (intervention arm: mean = 75.73 (SD = 5.85); control arm: mean = 75.49 (SD = 7.40)). We computed the MD, which indicated little or no evidence for an effect of resilience training compared to the no‐intervention control on hardiness at six‐month follow‐up (MD 0.24, 95% CI −3.74 to 4.22; P = 0.91; 1 study, 43 participants; Analysis 1.32).
1.32. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 32: Hardiness: medium‐term follow‐up (> 3 ≤ 6 months)
Positive emotions
Post‐intervention
Three studies assessed the effect of a resilience intervention compared to control on self‐reported positive emotions at immediate post‐intervention. Two studies (Fei 2019; Lin 2019) provided data suitable for quantitative analysis. The pooled effect estimate revealed a large effect in favour of resilience training on positive emotions at post‐test (SMD 0.85, 95% CI 0.17 to 1.53; P = 0.01; I2 = 82%; Tau2 = 0.20; P for heterogeneity = 0.02; G2 = 0%; 95% prediction interval: incalculable due to only two studies; 2 studies, 212 participants; Analysis 1.33).
1.33. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 33: Positive emotions: post‐intervention
For positive emotions at post‐test, we found substantial to considerable heterogeneity based on several indicators (i.e. I2 of 82%), whereas G2 suggested no heterogeneity.
Single study results
One further study also measured the effects of a resilience intervention compared to control on positive emotions at post‐intervention, but could not be pooled with the aforementioned studies. Stetz 2007 (see final report Stetz 2008) only reported summary data of analyses (two‐way MANOVA results for the Multiple Affect Adjective Check List‐Revised, including, for example, depression, anxiety and positive affect), and demonstrated a significant effect for the participants’ psychological stress levels (F = 3.3, P < 0.001; 63 participants randomised, number analysed not specified). Single results for the outcomes relevant for this review were not reported.
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, only one study compared the effects of a resilience intervention to wait‐list control on self‐reported positive emotions (Lin 2019). Using the positive affect subscale of the Positive and Negative Affect Schedule (range: 10 (worst) to 50 (best)), the investigators found a significant time x group interaction on positive affect at three‐month follow‐up (F = 6.62; P < 0.01) in favour of the resilience training (intervention arm: mean = 33.21 (SD = 7.38); control arm: mean = 29.00 (SD = 5.62)). The MD also indicated evidence for a positive effect of resilience training on positive emotions at short‐term follow‐up (MD 4.21, 95% CI 1.49 to 6.93; P = 0.002; 1 study, 90 participants; Analysis 1.34).
1.34. Analysis.

Comparison 1: Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes), Outcome 34: Positive emotions: short‐term follow‐up (≤ 3 months)
Adverse events
Only three studies assessed the potential adverse or undesired effects of resilience training in healthcare professionals, all of them reporting no such effects (Lebares 2018; Loiselle 2018; Strijk 2011). Most studies in healthcare professionals provided no data on potential adverse effects.
Subgroup analyses
We performed five subgroup analyses for four of our primary outcomes at post‐intervention, the exception being anxiety. For resilience, stress or stress perception and well‐being or quality of life, we also conducted five subgroup analyses at short‐term follow‐up.
Resilience
None of the subgroup analyses showed any evidence of a significant subgroup effect at post‐intervention: setting (Chi2 = 0.68; df = 1; P = 0.41; I2 = 0%; Analysis 2.1); delivery format (Chi2 = 0.12; df = 1; P = 0.73; I2 = 0%; Analysis 2.2); training intensity (Chi2 = 2.99; df = 2; P = 0.22; I2 = 33.1%; Analysis 2.3); theoretical foundation (Chi2 = 3.02; df = 2; P = 0.22; I2 = 33.7%; Analysis 2.4); or study comparator (Chi2 = 2.59; df = 3; P = 0.46; I2 = 0%; Analysis 2.5).
2.1. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 1: Resilience: post‐intervention, subgroup analysis: setting
2.2. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 2: Resilience: post‐intervention, subgroup analysis: delivery format
2.3. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 3: Resilience: post‐intervention, subgroup analysis: intensity
2.4. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 4: Resilience: post‐intervention, subgroup analysis: theoretical foundation
2.5. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 5: Resilience: post‐intervention, subgroup analysis: comparator
Two subgroup analyses showed evidence of a significant subgroup effect at short‐term follow‐up: training intensity (Chi2 = 17.84; df = 2; P < 0.001; I2 = 88.8%; Analysis 2.8), where compared to control, high‐intensity training (SMD 0.46, 95% CI 0.26 to 0.66; P < 0.001; 7 studies, 494 participants), but not low‐intensity (SMD 0.53, 95% CI −0.14 to 1.20; P = 0.12; 3 studies, 98 participants) or moderate‐intensity training (SMD −0.05, 95% CI −0.20 to 0.09; P = 0.50; 1 study, 733 participants) appeared to increase resilience; and theoretical foundation (Chi2 = 21.43; df = 3; P < 0.001; I2 = 86.0%; Analysis 2.9), where compared to control, mindfulness‐based (SMD 1.05, 95% CI 0.22 to 1.88; P = 0.01; 1 study, 26 participants) and combined training programmes (SMD 0.43, 95% CI 0.24 to 0.62; P < 0.001; 6 studies, 468 participants) appeared to increase resilience, but not AIT‐based (SMD 0.53, 95% CI −0.14 to 1.20; P = 0.12; 3 studies, 98 participants) or unspecified resilience interventions (SMD −0.05, 95% CI −0.20 to 0.09; P = 0.50; 1 study; 733 participants). The remaining subgroup analyses showed no evidence of a significant subgroup difference: setting (Chi2 = 4.81; df = 2; P = 0.09; I2 = 58.5%; Analysis 2.6); delivery format (Chi2 = 0.12; df = 1; P = 0.72; I2 = 0%; Analysis 2.7); or study comparator (Chi2 = 0.63; df = 2; P = 0.73; I2 = 0%; Analysis 2.10).
2.8. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 8: Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: intensity
2.9. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 9: Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: theoretical foundation
2.6. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 6: Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: setting
2.7. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 7: Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: delivery format
2.10. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 10: Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: comparator
Depression
None of the subgroup analyses showed any evidence of a significant subgroup effect at post‐intervention: setting (Chi2 = 5.34; df = 3; P = 0.15; I2 = 43.9%; Analysis 2.11); delivery format (Chi2 = 1.42; df = 2; P = 0.49; I2 = 0%; Analysis 2.12); training intensity (Chi2 = 0.26; df = 2; P = 0.88; I2 = 0%; Analysis 2.13); theoretical foundation (Chi2 = 2.44; df = 3; P = 0.49; I2 = 0%; Analysis 2.14); or study comparator (Chi2 = 7.08; df = 4; P = 0.13; I2 = 43.5%; Analysis 2.15).
2.11. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 11: Depression: post‐intervention, subgroup analysis: setting
2.12. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 12: Depression: post‐intervention, subgroup analysis: delivery format
2.13. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 13: Depression: post‐intervention, subgroup analysis: intensity
2.14. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 14: Depression: post‐intervention, subgroup analysis: theoretical foundation
2.15. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 15: Depression: post‐intervention, subgroup analysis: comparator
Stress or stress perception
None of the subgroup analyses showed any evidence of a significant subgroup effect at post‐intervention: setting (Chi2 = 1.22; df = 1; P = 0.27; I2 = 17.8%; Analysis 2.16); delivery format (Chi2 = 1.34, df = 1; P = 0.25; I2 = 25.2%; Analysis 2.17); training intensity (Chi2 = 0.23; df = 1; P = 0.63; I2 = 0%; Analysis 2.18); theoretical foundation (Chi2 = 3.49; df = 2; P = 0.17; I2 = 42.6%; Analysis 2.19); or study comparator (Chi2 = 1.01; df = 3; P = 0.80; I2 = 0%; Analysis 2.20).
2.16. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 16: Stress or stress perception: post‐intervention, subgroup analysis: setting
2.17. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 17: Stress or stress perception: post‐intervention, subgroup analysis: delivery format
2.18. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 18: Stress or stress perception: post‐intervention, subgroup analysis: intensity
2.19. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 19: Stress or stress perception: post‐intervention, subgroup analysis: theoretical foundation
2.20. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 20: Stress or stress perception: post‐intervention, subgroup analysis: comparator
None of the subgroup analyses showed any evidence of a significant subgroup effect at short‐term follow‐up: setting (Chi2 = 1.46; df = 2; P = 0.48; I2 = 0%; Analysis 2.21); delivery format (Chi2 = 0.03; df = 1; P = 0.87; I2 = 0%; Analysis 2.22); training intensity (Chi2 = 1.74; df = 2; P = 0.42; I2 = 0%; Analysis 2.23); theoretical foundation (Chi2 = 5.28; df = 3; P = 0.15; I2 = 43.2%; Analysis 2.24); or study comparator (Chi2 = 5.68; df = 2; P = 0.06; I2 = 64.8%; Analysis 2.25).
2.21. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 21: Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: setting
2.22. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 22: Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: delivery format
2.23. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 23: Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: intensity
2.24. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 24: Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: theoretical foundation
2.25. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 25: Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: comparator
Well‐being or quality of life
One subgroup analysis showed evidence of a significant subgroup effect at post‐intervention for theoretical foundation (Chi2 = 10.79; df = 3; P = 0.01; I2 = 72.2%; Analysis 2.29): the SMDs were 0.83 (95% CI 0.32 to 1.33; P = 0.001; 2 studies, 66 participants) for mindfulness‐based training; −0.02 (95% CI −0.17 to 0.13; P = 0.79; 1 study, 730 participants) for coaching‐based training; 0.14 (95% CI −0.03 to 0.31; P = 0.10; 9 studies, 591 participants) for combined training programmes; and 0 (95% CI −0.38 to 0.38; P = 1.00; 1 study, 107 participants) for unspecified resilience training. The remaining subgroup analyses provided no evidence of a significant subgroup difference: setting (Chi2 = 3.17; df = 1; P = 0.07; I2 = 68.5%; Analysis 2.26); delivery format (Chi2 = 1.51; df = 1; P = 0.22; I2 = 33.9%; Analysis 2.27); training intensity (Chi2 = 1.15; df = 1; P = 0.28; I2 = 13.3%; Analysis 2.28); or study comparator (Chi2 = 4.58; df = 2; P = 0.10; I2 = 56.3%; Analysis 2.30).
2.29. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 29: Well‐being or quality of life: post‐intervention, subgroup analysis: theoretical foundation
2.26. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 26: Well‐being or quality of life: post‐intervention, subgroup analysis: setting
2.27. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 27: Well‐being or quality of life: post‐intervention, subgroup analysis: delivery format
2.28. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 28: Well‐being or quality of life: post‐intervention, subgroup analysis: intensity
2.30. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 30: Well‐being or quality of life: post‐intervention, subgroup analysis: comparator
None of the subgroup analyses showed any evidence of a significant subgroup effect at short‐term follow‐up: setting (Chi2 = 2.23; df = 2; P = 0.33; I2 = 10.5%; Analysis 2.31); delivery format (Chi2 = 0.45; df = 1; P = 0.50; I2 = 0%; Analysis 2.32); training intensity (Chi2 = 0.40; df = 2; P = 0.82; I2 = 0%; Analysis 2.33); theoretical foundation (Chi2 = 0.45; df = 2; P = 0.80; I2 = 0%; Analysis 2.34); or study comparator (Chi2 = 3.21; df = 2; P = 0.20; I2 = 37.6%; Analysis 2.35).
2.31. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 31: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: setting
2.32. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 32: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: delivery format
2.33. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 33: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: intensity
2.34. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 34: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: theoretical foundation
2.35. Analysis.

Comparison 2: Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes), Outcome 35: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: comparator
Sensitivity analyses
We performed six sensitivity analyses for the primary outcomes of depression (at post‐intervention only), stress or stress perception and well‐being or quality of life at post‐intervention and short‐term follow‐up. With respect to resilience, we conducted a sensitivity analysis of the underlying resilience concept at post‐test only; it was not possible at short‐term follow‐up since all studies used a state‐oriented scale. In addition, the planned sensitivity analysis regarding reporting bias was not possible for resilience, due to all studies being at low risk of reporting bias. No sensitivity analysis was performed for anxiety.
Resilience
Post‐intervention
Underlying resilience concept: Following the exclusion of one study using a trait scale of resilience, we found evidence of a moderate effect in favour of resilience training (SMD 0.45, 95% CI 0.24 to 0.67; P < 0.001; 11 studies, 669 participants; Analysis 3.1).
Attrition bias: Following the exclusion of four studies at high risk of bias, we found no evidence of a subgroup difference between studies at low and unclear risk of bias (Chi2 = 0; df = 1; P = 0.97; I2 = 0%; Analysis 3.2), indicating that these studies could be combined in a sensitivity analysis. We found evidence of a moderate effect in favour of resilience training (SMD 0.50, 95% CI 0.30 to 0.71; P < 0.001; 8 studies, 466 participants; Analysis 3.2).
Trial registration: Following the exclusion of 10 studies without trial registration, we found little or no evidence of an effect of resilience intervention (SMD −0.07, 95% CI −0.82 to 0.67; P = 0.84; 2 studies, 54 participants; Analysis 3.3).
Level of missing data: Following the exclusion of four studies with ≥ 10% missing data in primary outcome or other outcomes, we found evidence of a moderate effect of resilience training (SMD 0.50, 95% CI 0.30 to 0.71; P < 0.001; 8 studies, 466 participants; Analysis 3.4).
Managing missing data: Following the exclusion of five studies with missing data of ≥ 10% and no imputation of missing data, we found evidence of a moderate effect in favour of training (SMD 0.45, 95% CI 0.25 to 0.65; P < 0.001; 7 studies, 393 participants; Analysis 3.5).
Fixed‐effect pair‐wise meta‐analysis: We found evidence of a moderate difference in favour of resilience training (SMD 0.47, 95% CI 0.31 to 0.62; P < 0.001; 12 studies, 690 participants; Analysis 3.6).
3.1. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 1: Resilience: post‐intervention, sensitivity analysis for resilience scale (underlying state concept)
3.2. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 2: Resilience: post‐intervention, sensitivity analysis for attrition bias (low or unclear risk of bias) including subgroup analysis
3.3. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 3: Resilience: post‐intervention, sensitivity analysis for trial registration (registered trials)
3.4. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 4: Resilience: post‐intervention, sensitivity analysis for level of missing data (< 10% missing data)
3.5. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 5: Resilience: post‐intervention, sensitivity analysis for coping with missing data (< 10% missing data, imputation of missing data or accounting for missing data by model for longitudinal data)
3.6. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 6: Resilience: post‐intervention, sensitivity analysis (fixed‐effect analysis)
Short‐term follow‐up (≤ 3 months)
Attrition bias: Following the exclusion of six studies at high risk of bias, we found evidence of a small effect of resilience training (SMD 0.31, 95% CI 0.09 to 0.54; P = 0.007; 5 studies, 337 participants; Analysis 3.7).
Trial registration: Following the exclusion of 10 studies without trial registration, we found little or no evidence of an effect of training (MD −0.03; 95% CI −0.12 to 0.06; P = 0.50; 1 study, 733 participants; Analysis 3.8).
Level of missing data: Following the exclusion of seven studies with high levels of missing data, we found a moderate effect in favour of the resilience intervention (SMD 0.36, 95% CI 0.13 to 0.58; P = 0.002; 4 studies, 311 participants; Analysis 3.9).
Managing missing data: Following the exclusion of six studies with missing outcome data of ≥ 10% and no imputation of missing data, we found evidence of a small effect of training (SMD 0.31, 95% CI 0.09 to 0.54; P = 0.007; 5 studies, 337 participants; Analysis 3.10).
Fixed‐effect pair‐wise meta‐analysis: We found evidence of a small effect of resilience training compared to control (SMD 0.18, 95% CI 0.07 to 0.29; P = 0.001; 11 studies, 1325 participants; Analysis 3.11).
3.7. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 7: Resilience: short‐term follow‐up (≤ 3 months), sensitivity analysis for attrition bias (low risk of bias)
3.8. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 8: Resilience: short‐term follow‐up (≤ 3 months), sensitivity analysis for trial registration (registered trials)
3.9. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 9: Resilience: short‐term follow‐up (≤ 3 months), sensitivity analysis for level of missing data (< 10% missing data)
3.10. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 10: Resilience: short‐term follow‐up (≤ 3 months), sensitivity analysis for coping with missing data (< 10% missing data, imputation of missing data or accounting for missing data by model for longitudinal data)
3.11. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 11: Resilience: short‐term follow‐up (≤ 3 months), sensitivity analysis (fixed‐effect analysis)
Depression
Post‐intervention
Attrition bias: Following the exclusion of nine studies at high risk of bias, we found evidence of a moderate effect in favour of resilience training (SMD −0.41; 95% CI −0.72 to −0.11; P = 0.008; 5 studies; 169 participants; Analysis 3.12).
Reporting bias: Following the exclusion of four studies at high risk of bias, there was little or no evidence of an effect of training (SMD −0.30; 95% CI −0.61 to 0.01; P = 0.06; 10 studies; 510 participants; Analysis 3.13).
Trial registration: Following the exclusion of eight studies without trial registration, we found little or no evidence of an effect of training (SMD −0.10; 95% CI −0.33 to 0.14; P = 0.41; 6 studies; 289 participants; Analysis 3.14).
Level of missing data: Following the exclusion of eight studies with high levels of missing data, we found evidence of a moderate effect in favour of resilience intervention (SMD −0.34; 95% CI −0.60 to −0.09; P = 0.009; 6 studies; 239 participants; Analysis 3.15).
Managing missing data: Following the exclusion of six studies with missing outcome data of ≥ 10% and no imputation of missing data, we found evidence of a small effect in favour of resilience training (SMD −0.33; 95% CI −0.53 to −0.14; P < 0.001; 8 studies; 410 participants; Analysis 3.16).
Fixed‐effect pair‐wise meta‐analysis: There was evidence of a small effect of resilience training (SMD −0.28; 95% CI −0.43 to −0.14; P < 0.001; 14 studies; 788 participants; Analysis 3.17).
3.12. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 12: Depression: post‐intervention, sensitivity analysis for attrition bias (low risk of bias)
3.13. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 13: Depression: post‐intervention, sensitivity analysis for reporting bias (low risk of reporting bias)
3.14. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 14: Depression: post‐intervention, sensitivity analysis for trial registration (registered trials)
3.15. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 15: Depression: post‐intervention, sensitivity analysis for level of missing data (< 10% missing data)
3.16. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 16: Depression: post‐intervention, sensitivity analysis for coping with missing data (<10% missing data, imputation of missing data or accounting for missing data by model for longitudinal data)
3.17. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 17: Depression: post‐intervention, sensitivity analysis (fixed‐effect analysis)
Stress or stress perception
Post‐intervention
Attrition bias: Following the exclusion of seven studies at high risk of bias, we found no evidence of a subgroup difference between studies at low and unclear risk of bias (Chi2 = 0.73; df = 1; P = 0.39; I2 = 0%; Analysis 3.18), indicating that these studies could be combined in a sensitivity analysis. We found evidence of a large effect of resilience training (SMD −0.75, 95% CI −1.47 to −0.02; P = 0.04; 10 studies, 621 participants; Analysis 3.18).
Reporting bias: Following the exclusion of four studies at high risk of bias, we found evidence of a large effect in favour of resilience training (SMD −0.81; 95% CI −1.38 to −0.25; P = 0.005; 13 studies, 822 participants; Analysis 3.19).
Trial registration: Following the exclusion of 12 studies without trial registration, there was little or no evidence of an effect of resilience intervention (SMD −0.15, 95% CI −0.43 to 0.14; P = 0.31; 5 studies, 197 participants; Analysis 3.20).
Level of missing data: Following the exclusion of six studies with high levels of missing data, we found little or no evidence of an effect of resilience training (SMD −0.64, 95% CI −1.30 to 0.02; P = 0.06; 11 studies, 690 participants; Analysis 3.21).
Managing missing data: Following the exclusion of five studies with missing outcome data of ≥ 10% and no imputation of missing data, we found evidence of a moderate effect in favour of resilience training (SMD −0.62, 95% CI −1.23 to −0.01; P = 0.05; 12 studies, 727 participants; Analysis 3.22).
Fixed‐effect pair‐wise meta‐analysis: There was evidence of a moderate effect of resilience training (SMD −0.56, 95% CI −0.70 to −0.42; P < 0.001; 17 studies, 997 participants; Analysis 3.23).
3.18. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 18: Stress or stress perception: post‐intervention, sensitivity analysis for attrition bias (low or unclear risk of bias) including subgroup analysis
3.19. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 19: Stress or stress perception: post‐intervention, sensitivity analysis for reporting bias (low risk of bias)
3.20. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 20: Stress or stress perception: post‐intervention, sensitivity analysis for trial registration (registered trials)
3.21. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 21: Stress or stress perception: post‐intervention, sensitivity analysis for level of missing data (< 10% missing data)
3.22. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 22: Stress or stress perception: post‐intervention, sensitivity analysis for coping with missing data (< 10% missing data, imputation of missing data or accounting for missing data by model for longitudinal data)
3.23. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 23: Stress or stress perception: post‐intervention, sensitivity analysis (fixed‐effect analysis)
Short‐term follow‐up (≤ 3 months)
Attrition bias: Following the exclusion of seven studies at high risk of bias, we found no evidence of a subgroup difference between studies at low and unclear risk of bias (Chi2 = 1.52; df = 1; P = 0.22; I2 = 34%; Analysis 3.24), indicating that these studies could be combined in a sensitivity analysis. There was evidence of a small effect of resilience training (SMD −0.30, 95% CI −0.52 to −0.07; P = 0.009; 7 studies, 427 participants; Analysis 3.24).
Reporting bias: Following the exclusion of three studies at high risk of bias, we found evidence of a moderate effect in favour of resilience training (SMD −0.52, 95% CI −0.75 to −0.29; P < 0.001; 11 studies, 644 participants; Analysis 3.25).
Trial registration: Following the exclusion of 11 studies without trial registration, there was little or no evidence of an effect of resilience training (SMD −0.22; 95% CI −0.71 to 0.28; P = 0.39; 3 studies, 144 participants; Analysis 3.26).
Level of missing data: Following the exclusion of seven studies with high levels of missing data, we found evidence of a small effect in favour of resilience training (SMD −0.27, 95% CI −0.53 to −0.00; P = 0.05; 7 studies, 471 participants; Analysis 3.27).
Managing missing data: Following the exclusion of five studies with missing outcome data of ≥ 10% and no imputation of missing data, we found evidence of a small effect of resilience intervention (SMD −0.27, 95% CI −0.49 to −0.06; P = 0.01; 9 studies, 534 participants; Analysis 3.28).
Fixed‐effect pair‐wise meta‐analysis: we found evidence of a moderate effect in favour of resilience intervention (SMD −0.43, 95% CI −0.58 to −0.29; P < 0.001; 14 studies, 788 participants; Analysis 3.29).
3.24. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 24: Stress or stress perception: short‐term follow‐up (≤ 3 months), sensitivity analysis for attrition bias (low or unclear risk of bias) including subgroup analysis
3.25. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 25: Stress or stress perception: short‐term follow‐up (≤ 3 months), sensitivity analysis for reporting bias (low risk of bias)
3.26. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 26: Stress or stress perception: short‐term follow‐up (≤ 3 months), sensitivity analysis for trial registration (registered trials)
3.27. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 27: Stress or stress perception: short‐term follow‐up (≤ 3 months), sensitivity analysis for level of missing data (< 10% missing data)
3.28. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 28: Stress or stress perception: short‐term follow‐up (≤ 3 months), sensitivity analysis for coping with missing data (<10% missing data, imputation of missing data or accounting for missing data by model for longitudinal data)
3.29. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 29: Stress or stress perception: short‐term follow‐up (≤ 3 months), sensitivity analysis (fixed‐effect analysis)
Well‐being or quality of life
Post‐intervention
Attrition bias: Following the exclusion of five studies at high risk of bias, we found no evidence of a subgroup difference between studies at low and unclear risk of bias (Chi2 = 1.43; df = 1; P = 0.23; I2 = 30.1%; Analysis 3.30), indicating that these studies could be combined in a sensitivity analysis. There was little or no evidence of an effect of resilience training (SMD 0.15, 95% CI −0.06 to 0.35; P = 0.17; 8 studies, 1112 participants; Analysis 3.30).
Reporting bias: Following the exclusion of four studies at high risk of bias, we found evidence of a small effect of resilience intervention (SMD 0.20, 95% CI 0.03 to 0.36; P = 0.02; 9 studies, 628 participants; Analysis 3.31).
Trial registration: Following the exclusion of 10 studies without trial registration, we found little or no evidence of an effect of training (SMD −0.04, 95% CI −0.18 to 0.10; P = 0.56; 3 studies, 834 participants; Analysis 3.32).
Level of missing data: Following the exclusion of six studies with high levels of missing data, we found little or no evidence of an effect of resilience intervention (SMD 0.20, 95% CI −0.06 to 0.46; P = 0.14; 7 studies, 412 participants; Analysis 3.33).
Managing missing data: Following the exclusion of four studies with missing outcome data of ≥ 10% and no imputation of missing data, we found little or no evidence of an effect of training (SMD 0.11, 95% CI −0.08 to 0.29; P = 0.27; 9 studies, 1179 participants; Analysis 3.34).
Fixed‐effect pair‐wise meta‐analysis: We found little or no evidence of an effect of resilience training (SMD 0.08, 95% CI −0.02 to 0.19; P = 0.13; 13 studies, 1494 participants; Analysis 3.35).
3.30. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 30: Well‐being or quality of life: post‐intervention, sensitivity analysis for attrition bias (low or unclear risk of bias) including subgroup analysis
3.31. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 31: Well‐being or quality of life: post‐intervention, sensitivity analysis for reporting bias (low risk of bias)
3.32. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 32: Well‐being or quality of life: post‐intervention, sensitivity analysis for trial registration (registered trials)
3.33. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 33: Well‐being or quality of life: post‐intervention, sensitivity analysis for level of missing data (< 10% missing data)
3.34. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 34: Well‐being or quality of life: post‐intervention, sensitivity analysis for coping with missing data (<10% missing data, imputation of missing data or accounting for missing data by model for longitudinal data)
3.35. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 35: Well‐being or quality of life: post‐intervention, sensitivity analysis (fixed‐effect analysis)
Short‐term follow‐up (≤ 3 months)
Attrition bias: Following the exclusion of five studies at high risk of bias, there was no evidence of a subgroup difference between studies at low and unclear risk of bias (Chi2 = 2.89; df = 1; P = 0.09; I2 = 65.4%; Analysis 3.36), indicating that these studies could be combined in a sensitivity analysis. We found little or no evidence of an effect of resilience training (SMD 0.14, 95% CI −0.05 to 0.33; P = 0.16; 7 studies, 422 participants; Analysis 3.36).
Reporting bias: Following the exclusion of three studies at high risk of bias, we found little or no evidence of an effect of resilience intervention (SMD 0.03, 95% CI −0.08 to 0.14; P = 0.59; 9 studies, 1227 participants; Analysis 3.37).
Trial registration: Following the exclusion of eight studies without trial registration, we found little or no evidence of an effect of training (SMD 0.10, 95% CI −0.17 to 0.36; P = 0.46; 4 studies, 919 participants; Analysis 3.38).
Level of missing data: Following the exclusion of seven studies with high levels of missing data, we found little or no evidence of an effect of resilience training (SMD 0.04, 95% CI −0.17 to 0.25; P = 0.70; 5 studies, 348 participants; Analysis 3.39).
Managing missing data: Following the exclusion of five studies with missing outcome data of ≥ 10% and no imputation of missing data, we found little or no evidence of an effect of training (SMD 0.04, 95% CI −0.15 to 0.24; P = 0.66; 7 studies, 411 participants; Analysis 3.40).
Fixed‐effect pair‐wise meta‐analysis: We found little or no evidence of an effect of resilience training (SMD 0.06, 95% CI −0.04 to 0.17; P = 0.24; 12 studies, 1413 participants; Analysis 3.41).
3.36. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 36: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), sensitivity analysis for attrition bias (low or unclear risk of bias) including subgroup analysis
3.37. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 37: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), sensitivity analysis for reporting bias (low risk of bias)
3.38. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 38: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), sensitivity analysis for trial registration (registered trials)
3.39. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 39: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), sensitivity analysis for level of missing data (<10% missing data)
3.40. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 40: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), sensitivity analysis for coping with missing data (<10% missing data, imputation of missing data or accounting for missing data by model for longitudinal data)
3.41. Analysis.

Comparison 3: Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes), Outcome 41: Well‐being or quality of life: short‐term follow‐up (≤ 3 months), sensitivity analysis (fixed‐effect analysis)
Discussion
Summary of main results
We identified 44 randomised controlled trials (RCTs) that fulfilled the inclusion criteria of this review, four of which were conducted in mixed samples and one study assessed the impact of resilience training for healthcare workers in general‐population volunteers.
There is very‐low certainty evidence (meaning that the true effect may differ markedly from the estimated effect) that resilience interventions might be more effective than control for improving resilience, self‐reported symptoms of depression, and stress or stress perception at post‐test. Effect sizes ranged from small to moderate. We found little or no evidence of an effect of training on anxiety symptoms at post‐intervention. At short‐term follow‐up (three months or less post‐intervention), the effect size of the reduction in depressive symptoms increased from small to moderate. The possible moderate effects for resilience and for stress or stress perception found at post‐test slightly decreased, but were also maintained. We also found very‐low certainty evidence of a moderate effect in favour of resilience training on anxiety symptoms. At medium‐term follow‐up (more than three months to six months or less), we no longer found evidence of a difference between the resilience intervention and control for resilience, while a single study (Mache 2017) still provided evidence of a decrease in burnout and stress symptoms. At long‐term follow‐up (more than six months), the positive effects of training on the primary outcomes were no longer evident. We found little or no evidence of an effect of training on well‐being or quality of life at any time point. Anxiety was not measured at medium‐ and long‐term follow‐up by any study.
For the secondary outcomes at post‐test and short‐term follow‐up, we found evidence of small and moderate effects in favour of resilience training for optimism, self‐efficacy, self‐esteem (only short‐term follow‐up), and positive emotions that were only maintained in the medium term for self‐efficacy (single study: Cheung 2014). There was little or no evidence for a difference between training and control for social support, active coping, and hardiness at any assessment. Not all of the secondary outcomes were measured at each time point; a long‐term follow‐up was only available for self‐efficacy.
Subgroup analyses for the primary outcomes at post‐test and short‐term follow‐up (except anxiety and depression) indicated no consistent effect modifiers. The subgroup analysis of training intensity for resilience at short‐term follow‐up provided evidence of a difference in favour of high‐intensity training. For theoretical foundation, the subgroup analyses for well‐being or quality of life at post‐test and for resilience at short‐term follow‐up showed evidence of a difference in favour of mindfulness‐based resilience interventions (both outcomes) and combined programmes (resilience). Beyond that, however, we identified little or no evidence of differences in the efficacy of resilience training for the primary outcomes depending on setting, delivery format, training intensity, theoretical foundation or study comparator. The analyses are restricted by the small number of studies for some of the subgroups, the limited quality of included studies, and the weighting of subgroup analyses for certain subgroups.
With respect to sensitivity analysis at post‐test and short‐term follow‐up (except for anxiety and depression), we mostly found no evidence of an effect of resilience training when excluding studies without trial registration or a published study protocol. The exclusion of studies at high risk of attrition bias, reporting bias or with high levels of missing data, as well as sensitivity analyses related to the management of missing data and the use of fixed‐effect instead of random‐effects models, partly led to changes in the evidence found. Removing studies measuring resilience with a trait scale (post‐test) left the evidence unchanged for a positive effect on resilience.
Overall, the evidence included in this review is of very low certainty, meaning that we can draw no clear conclusions.
Overall completeness and applicability of evidence
The review highlights some issues about the overall completeness and applicability of the evidence for the effects of resilience interventions in healthcare workers (for details, see Appendix 17).
Participants
Since stress‐related mental disorders are more prevalent in women (Kuehner 2017; Li 2017; Riecher‐Rössler 2017; WHO 2019), and since women report lower resilience (Kunzler 2018), the high proportion of women among the study participants may be explained by a higher interest in women to participate in resilience interventions. The applicability of the findings of this review to men may be limited, since gender differences in the prevalence of stress‐related mental disorders may reflect differences in biological vulnerability, social roles, or stress reactivity (Nazroo 1998; Verma 2011; WHO 2019), thereby causing a potentially different effect of resilience training in men and women.
Concerning the participants' age, middle‐aged participants (50 to 65 years) before their retirement were rarely examined. Moran 1998 postulated a curvilinear association with a higher stressor exposure in emergency workers at the beginning and by the end of their working life compared to a moderate level of work experience. Similarly, the period before retirement as an important transitional event may be stressful (Bossé 1991; Selye 1980). Thus, employees aged 50 to 65 years might benefit differently, perhaps to a greater extent, from resilience interventions. The evidence from this review does not allow us to answer this question.
With regard to healthcare sectors, the included studies were mainly conducted in a hospital setting, and included physicians, nurses and different hospital personnel (37/44 studies), with various medical departments represented.
About two‐thirds of the 44 studies assessed mental health at baseline. The clinical relevance of mental symptoms, i.e. whether symptom load justified a diagnosis of mental disorder, is unclear for most studies, since no study screened for mental disorders using a structured interview. However, to get a clear picture of the participants' baseline mental health could be important, as the large effect sizes in some studies (e.g. Bernburg 2019) might in part also be explained by the inclusion of participants with a pre‐existing burden of mental symptoms or even clinical diagnoses.
For location, the evidence was concentrated in North America, Europe and Asia (including the Near East), with only three studies from Australia. The applicability of the findings to other locations and ethnicities (e.g. South America, Africa, Oceania) therefore remains unclear. Of the 44 included studies, 36 were conducted in high‐incomecountries (e.g. USA) and eight in upper‐middle income countries (e.g. China). We therefore recommend some caution about the cross‐cultural applicability of the evidence.
In summary, the findings may be most applicable to the young and middle‐aged, to female healthcare workers, to those living in high‐income countries.
Interventions
Although the benefits of online‐ and mobile‐based interventions (e.g. 24/7 availability) have recently been discussed (Cuijpers 2017; Heber 2017; Heron 2010), we identified only three studies delivered in this format. In addition, most of the interventions were of high or moderate intensity, with treatment durations varying considerably. Except for ACT and PST, all theoretical foundations prespecified in our protocol (Helmreich 2017) have been tested in RCTs found in this review. The number of RCTs varies, with most studies investigating combined theoretical foundations. Overall, the findings of this review are mostly applicable to group interventions of high intensity, delivered face‐to‐face and using a combination of theoretical approaches.
Comparators
For attention and active controls, there was considerable heterogeneity of setting, delivery format and content, rendering comparability between single‐study comparisons difficult.
The primary use of no‐intervention and wait‐list controls, in particular, is problematic, since these control groups were shown to yield inflated effect sizes compared to active comparators in psychotherapy research (Mohr 2014). In our review, however, subgroup analyses testing comparators did not reach statistical significance for any outcome, which might also be attributable to the small number of studies in the subgroups of active and attention control compared to no intervention and wait‐list control.
Outcomes
Different measures for resilience were used in the review (see Table 3). For the potential effect of the underlying concept of resilience, the exclusion of trait‐based resilience measures did not modify the effect size on resilience at post‐test. However, this finding might be associated with only one study (Lebares 2018) using a trait‐based measure.
Although there is still no consensus about the definition of resilience, two aspects are viewed as essential: the exposure to substantial risk or adversity, and the maintenance or fast recovery of mental health despite this adversity (Earvolino‐Ramirez 2007). By considering studies of healthcare professionals – a target group often exposed to significant stressors – that assessed resilience or another measure of psychological adjustment, we ensured a greater homogeneity between the included studies.
A large variety of assessments were also admitted for the primary outcomes of mental health and well‐being (e.g. burnout and depression scales for depression; Helmreich 2017). This diversity of measures has to be considered as a potential source of heterogeneity in our meta‐analyses, and might have an impact on the interpretation of results.
Althoughresilience factors, such as social support, are discussed as well‐evidenced resilience factors (see Helmreich 2017), relatively few of the included studies assessed these outcomes at the different periods of follow‐up.
Since most of the included studies had small samples, the attrition bias found for 16 studies has to be interpreted with caution.
Potential adverse effects were not specified in most included studies (see Adverse events in Effects of interventions), and only three studies reported no adverse or undesired effects. For psychotherapy, however, several possible adverse outcomes have been discussed (e.g. emotional arousal; Berk 2009; Moritz 2019). As resilience interventions often include confronting participants with individual problems (e.g. by teaching structured problem‐solving), some of these training programmes might also have the potential to harm certain participants.
Lastly, very few studies had medium‐ or long‐term follow‐up assessments, which limited our ability to examine whether any benefits of resilience interventions are sustained in the long term.
Quality of the evidence
Using the GRADE approach (Schünemann 2013; Schünemann 2019b), we rated the overall certainty of evidenceat post‐intervention for all primary outcomes as very low, for the following reasons: First, important methodological limitations reduced the certainty of the evidence offered by most included studies. There was unclear and high risk of bias for several domains across the studies, especially high risk of bias in blinding of participants and personnel, loss to follow‐up and unclear methods of sequence generation, allocation concealment and blinding of outcome assessment. Selective outcome reporting was occasionally an issue.
Second, four outcomes had moderate (I2 > 30%) or substantial (stress or stress perception, I2 = 90%) levels of unexplained heterogeneity and only partially overlapping CIs, leading to inconsistency.
Third, for all (primary) outcomes at post‐intervention, the evidence was indirect, as studies were limited to certain participants (e.g. young to middle‐aged adults), particular versions of resilience intervention (e.g. group setting, face‐to‐face delivery, mindfulness‐based and combined theoretical foundation) and certain comparators (e.g. no intervention, wait‐list).
Finally, due to the small number of participants included in the meta‐analysis for anxiety (fewer than 400 participants), inconsistent messages of the 95% CI for the intervention effect (anxiety, well‐being or quality of life), and the 95% CI encompassing both a very small treatment effect and crossing the threshold for appreciable benefit of the intervention (depression), imprecision was a problem for three outcomes at post‐intervention.
We did not downgrade for publication bias for any of the primary outcomes at post‐intervention. Based on funnel plots (see Appendix 16, except for anxiety) and Egger's test, there was no statistical or visual evidence of asymmetry (see also Effects of interventions, except for anxiety). The funnel plots were symmetrical in shape and, if available, the results of grey literature did not differ from other published studies for the (non‐)evidence or the direction of effect (resilience, depression, stress or stress perception, well‐being or quality of life). Due to the scarcity of larger studies across the primary outcomes at post‐test (with the exception of Strijk 2011 for well‐being or quality of life), a small‐study effect was difficult to assess and cannot be ruled out completely. Nevertheless, an overestimation of effects in smaller studies seemed unlikely, since the meta‐analyses mostly included small studies with significant as well as non‐significant results. Although the evidence was largely based on small studies, there was no indication of conflicts of interest of relevance for the post‐test meta‐analyses.
Three primary outcomes: we also examined funnel plots and Egger's test at short‐term follow‐up (> 10 studies), and found similar results for stress or stress perception, with no indication of publication bias. Despite statistical and (slight) visual evidence of funnel plot asymmetry for resilience and well‐being or quality of life at short‐term follow‐up, we also did not assume there was publication bias for these outcomes for several reasons: ‘Negative’ studies (i.e. statistically non‐significant studies) had also been published and studies appeared to be missing in the area of high statistical significance (P < 0.01), making publication bias unlikely according to the Cochrane Handbook (Page 2019). In addition, the results of one unpublished study in both meta‐analyses (Cheung 2014) did not differ from other published studies. For both outcomes, the evidence was based on a multitude of small studies (resilience: 10/11, well‐being or quality of life: 11/12 studies). In such cases, according to the GRADE approach (Guyatt 2011e), publication bias should be suspected if most of these studies have been commercially funded or when conflicts of interest are assumed. For resilience and well‐being or quality of life, a potential conflict of interest was indicated from the authors or likely for three studies (Chesak 2015; Sood 2011; Sood 2014). However, as these studies represented a minority and several of them also included non‐significant results, there was insufficient evidence of publication bias. Other forms of selection bias (language bias, location or database bias, multiple publication bias, provision of data bias, citation bias, outcome reporting bias) could not explain the funnel plot asymmetry. For both outcomes, the non‐significant finding of Cheung 2014 as an unpublished study could indicate a potential time‐lag bias. Again, small‐study effects were difficult to assess for both outcomes due to the lack of larger studies, but were unlikely, as both significant and non‐significant results were reported by small studies. Besides, the effect size did not differ according to study size due to true heterogeneity (Page 2019), as there were no consistent clinical (e.g. population, setting or delivery format of resilience intervention) or methodological differences between studies of different size. Finally, we must consider whether alternative explanations of funnel plot asymmetry for both outcomes might refer to artefacts due the use of SMDs or chance (Page 2019). More details about the assessment and exclusion of publication bias for the primary outcomes of this review are presented in Appendix 18.
Regarding adverse events, we were unable to assess several GRADE domains (e.g. precision, publication bias), due to the small number of studies documenting any adverse effects of study participation (e.g. by verbal feedback from participants; Lebares 2018; Loiselle 2018; Strijk 2011). Based on the narrative reports in these studies, we downgraded this outcome for study limitations and indirectness.
Overall, the GRADE certainty rating was very low for all primary outcomes at post‐intervention, which means that there is a high degree of uncertainty about the estimates of effect observed. Future research in this area is very likely to substantially impact the effect estimates of resilience interventions.
Potential biases in the review process
Search methods
Appendix 19 includes further information on how we prevented potential biases in the search methods for this review. Except for five completed but unpublished studies (ISRCTN69644721; NCT02603133; NCT03645798; Smith 2019; West 2015), we were able to retrieve the full texts for all included studies. In accordance with the Cochrane Developmental, Psychosocial and Learning Problems (CDPLP) editorial team, we considered alternative sources (e.g. trial register entry) for these five studies. In eight cases, we could find no contact data from the investigators, or received no reply from the study authors, or the responses were inadequate and did not provide sufficient information to enable us to reach a decision about the eligibility of the studies (see Characteristics of studies awaiting classification). We attempted to conduct a comprehensive search; however, the fact that 12 studies have not yet been incorporated, and will only be added in the update of this review could be considered a potential source bias.
Correspondence with the authors was required for 32 included studies. For three studies, for which we aimed to double‐check the available information (e.g. number of participants analysed) or to receive unadjusted outcome data by contacting the authors, we decided to rely on the reports and to include the studies in the meta‐analyses despite the missing response (Fei 2019; Loiselle 2018; Medisauskaite 2019). For four studies, we used alternative statistical information to include them in quantitative analysis (Calder Calisi 2017; Clemow 2018; Hosseinnejad 2018: Klatt 2015). For three studies (ISRCTN69644721; NCT03645798; Smith 2019), we received information that no data could be provided, as the studies were completed, and in the process of analysis or publication. For three further studies (NCT02603133; Stetz 2007; Wild 2016), the primary investigators responded to our first inquiry, but not to a second inquiry, or were not able to provide the relevant subgroup data at the time of data analysis (Wild 2016).
Post hoc changes
We made a post hoc change to the eligibility criteria for the Types of interventions (see Differences between protocol and review) by subsequently limiting the study selection to interventions that explicitly stated the aim of fostering resilience, hardiness or post‐traumatic growth. Although the change raises the possibility of bias in the review process, we felt it was necessary to guarantee highly‐objective eligibility criteria and transparency. We do not believe that this departure from the protocol (Helmreich 2017) is a serious bias. Due to the focus on interventions with the mention of at least one of the three terms, general health‐promoting interventions (e.g. well‐being therapy, chronic disease self‐management, self‐management training after negative life events) not meeting this criterion were excluded from this review. However, other psychological interventions in healthcare professionals that are eventually more economical than the theoretical approaches found in this review might also foster mental health, despite stressors (i.e. resilience), although not being labelled as 'resilience training'.
We also made a post hoc change to the eligibility criteria for Types of participants (see Differences between protocol and review) by limiting the review to healthcare professionals. Although the change raises the possibility of bias, we felt it was necessary because the restriction to healthcare professionals guarantees a systematic review with sufficiently homogeneous comparisons.
Further potential biases
Even within each type of theoretical foundation, there was partial clinical heterogeneity, in terms of intervention setting, delivery or intensity. However, as there is still no consensus or 'gold standard' about how to design resilience‐training programmes leading to variety (see previous reviews, e.g. Leppin 2014), we decided to pool the data. We took this decision as this review had a larger evidence base than previous meta‐analyses and we were able to investigate potential heterogeneity by subgroup analysis.
Beyond the five main results for the primary outcomes at post‐test, the large number of the pooled analyses, subgroup and sensitivity analyses in this review might have increased the probability of a type I error, potentially leading to false positive results.
Another important limitation of this review is the unknown stressor or risk exposure in most included studies (see Implications for research). Although employment in the healthcare sector might be associated with substantial stressors among participants of the included studies, we did not apply a proven risk or stressor exposure as an inclusion criterion of this review (see Types of participants), but only potential stressor exposure. However, based on the definition of resilience (Windle 2011a), the effects of resilience interventions on resilience cannot be determined without ensuring a significant risk. The missing assessment of stressor exposure is a general problem of resilience‐intervention research (Chmitorz 2018).
Agreements and disagreements with other studies or reviews
Studies or reviews in different clinical and non‐clinical adult populations
As mentioned under Why it is important to do this review, the efficacy of resilience interventions for adult populations has been previously examined in 13 systematic reviews and five meta‐analyses. Overall, the reviews largely found positive effects of resilience training on different outcomes (e.g. resilience, mental health, physical health, performance), but many review authors have pointed out the need for further research associated with aspects such as the low methodological quality of the primary studies. Many of the reviews also considered study designs other than RCTs (e.g. Bauer 2018; Massey 2019) and focused on certain target groups (e.g. Milne 2016; Pallavicini 2016; Pesantes 2015; Petriwskyj 2016) or certain forms of intervention (e.g. Deady 2017). The number of RCTs specifically on resilience training was therefore rather limited, making comparisons with our review difficult.
Some of the previous reviews (Joyce 2018; Macedo 2014; Leppin 2014; Robertson 2015; Vanhove 2016) used broader eligibility criteria (e.g. clinical and non‐clinical individuals) and identified more RCTs compared to other reviews, facilitating comparisons with our work. Despite varying inclusion criteria, the findings of our review largely agree with this previous research, although our review is based on evidence from a much larger body of studies. Furthermore, our review is focused on healthcare professionals, which is different from the mixed target groups in the previous reviews. For example, Macedo 2014 (seven RCTs), whilst not pooling any data, identified some degree of effectiveness of resilience‐training programmes. Similarly, Robertson 2015 (eight RCTs) found indications of benefit for personal resilience, mental health, well‐being and work performance in employees. With the exception of well‐being as well as job performance, which we did not examine here, these findings were confirmed by this review. With respect to the positive short‐term effects for resilience and depressive symptoms up to three months post‐intervention, our review is largely consistent with several meta‐analyses, which also found small‐to‐moderate positive effects of resilience training on resilience up to three months post‐intervention (Joyce 2018: 17 RCTs; Leppin 2014: 25 RCTs) and small proximal effects (≤ 1 month post‐intervention) on psychological deficits (e.g. depressive symptoms) (Vanhove 2016: 14 RCTs). In contrast to Vanhove 2016, who also identified positive effects on well‐being (≤ 1 month post‐intervention), we found little or no evidence of an effect on this outcome. On the other hand, this result is consistent with Leppin 2014 (quality of life), whereas we found different evidence of training effects on depressive symptoms (small‐to‐moderate reduction) compared with Leppin 2014 (no evidence of effect). The delayed effect on anxiety between post‐test and short‐term follow‐up in our review is comparable with Vanhove 2016, who only found maintained effects of training for the prevention of psychological deficits at more than one month after training. Consistently with Leppin 2014, the study comparator was also not identified as an effect modifier in our review. Based on our subgroup analyses, we could not replicate the findings of previous reviews (Joyce 2018; Vanhove 2016), which identified advantages in favour of group versus individual settings (Vanhove 2016), individual setting and classroom‐based (group) format versus computer‐based delivery (Vanhove 2016), or positive effects of CBT‐based, mindfulness‐based and mixed interventions (Joyce 2018). This inconsistency might be explained by the limited number of studies in some subgroup analyses of our review, the weighting of subgroup analyses for certain subgroups (e.g. group setting), and the lack of studies in certain subgroups (e.g. online‐ and mobile‐based delivery; CBT‐based interventions). We also used a different definition of 'combined' interventions (i.e. other compilations than mindfulness and CBT) from Joyce 2018.
Studies or reviews in healthcare professionals
With respect to healthcare staff, 13 systematic reviews and one meta‐analysis have so far synthesised the efficacy of resilience‐training programmes in this target group, although not all of them have focused solely on interventions (see Why it is important to do this review). Comparable with our review, four previous publications examined healthcare workers in general (Cleary 2018) or combined healthcare professionals and students (Gilmartin 2017; Rogers 2016; Pezaro 2017). However, most only targeted certain subgroups of healthcare workers (e.g. nurses, midwives, physicians; Concilio 2019; Delgado 2017; Elliott 2012; Foster 2019; Fox 2018; Gillman 2015; Hunter 2016; Robertson 2016; Lavin Venegas 2019; Wright 2017). Similar to the problems for the reviews described above, most previous reviews in healthcare staff (except for Elliott 2012) also included study designs other than RCTs. The number of RCTs on resilience training was therefore rather limited (i.e. 0 to 9 RCTs among 5 to 33 included studies in the 14 reviews), in contrast with our review which identified 44 RCTs across various groups of healthcare staff. Since the review questions of some of the 14 reviews did not solely focus on the construct of resilience or on intervention studies, the primary studies included here did not always explicitly mention the intention of fostering resilience. Instead, broader mental health interventions (e.g. Gilmartin 2017) or programmes targeting aspects of care (e.g. Elliott 2012) were also considered, which renders comparisons with our review difficult.
This review is most comparable with Cleary 2018, who only included psychological interventions prospectively designed to enhance resilience and considered different groups of healthcare workers. The RCTs on resilience training in physicians (Mache 2015b; Mache 2016; Sood 2011; Sood 2014), nurses (Chesak 2015; Mealer 2014) and different hospital personnel (Klatt 2015), identified by Cleary 2018, were also included in our review, except for Rowe 2006 (additional reference to Rowe 1999) and Maunder 2010. Our searches also identified the latter two studies but we excluded them for the following reasons: We did not consider Maunder 2010 to be an RCT as the study involved a random assignment to three different doses of resilience intervention, but without a control group. We excluded Rowe 2006 due to an 'ineligible intervention', since the focus of the training did not seem to be on fostering hardiness (i.e. hardiness was only examined as a correlate of burnout as the main study outcome). With respect to the subgroup of physicians, the same applies to Fox 2018. The RCTs included here (Klatt 2015; Mache 2015a; Mache 2016; Mache 2017; Rowe 2000 (second reference to Rowe 1999); Sood 2011; Sood 2014) were also included in our review, except for Rowe 2000 (excluded for the same reasons as Rowe 2006). Furthermore, we found a large number of the non‐RCTs reported in Cleary 2018 and Fox 2018 during the study identification process for our review. The only previous meta‐analysis (Lavin Venegas 2019), which included 17 studies (4 RCTs) on resilience training in physicians, was not able to perform pooled analysis for resilience due to heterogeneity in study designs and outcome measures. With regard to burnout, meta‐analyses were only performed for observational studies; one RCT (Dyrbye 2016) showed no evidence of a difference between resilience training and control for burnout. We did not include the latter study in our review, as resilience or a related construct was not mentioned in the publication. Lavin Venegas 2019 only conducted subgroup analyses for primary care physicians on the basis of two non‐RCTs, and found no evidence of a difference for burnout. The findings of these two reviews are therefore hardly comparable, although some subgroup analyses of our review also had limited power and were heavily weighted for a certain subgroup.
Authors' conclusions
Implications for practice.
There is very uncertain evidence that resilience interventions are effective in improving resilience or certain resilience‐related factors such as optimism, self‐reported symptoms of depression, and stress or stress perception at post‐test (small and moderate effect sizes).
The generalisability and applicability of the available evidence is limited by the scarcity of studies with long‐term follow‐up, the divergent efficacy measures used to assess resilience, the heterogeneous design and content of interventions (with a dominance of high‐intensity face‐to‐face interventions delivered in a group setting), and the limited geographical locations (i.e. high‐income countries). In addition, we rated the certainty of the evidence from this review as being very low across all primary outcomes at post‐test. We therefore cannot draw strong conclusions about the effects of resilience interventions, as the true effect may be markedly different from the estimated effect.
We know little about the longer‐term effects of resilience training on most outcomes, because few studies included follow‐up assessments. Booster sessions were not conducted in any of the included studies.
The limited evidence that resilience training improves well‐being or quality of life and several resilience factors might indicate the need to adapt the current intervention techniques used.
Overall, the results of our review provide very uncertain evidence about whether resilience‐training programmes may be helpful in stabilising and improving the mental health of healthcare professionals as an occupational group with high stressor exposure.
Implications for research.
The findings of this review point to the need for further research of high methodological quality in order to determine the efficacy of resilience interventions in healthcare professionals.
For future research, a consensus on the definition of resilience and adequate outcome measures to be used consistently across the field would be important. Following the growing consensus on resilience as a dynamic outcome (Bonanno 2015; Kalisch 2017), intervention studies might be guided by this definition and examine resilience as a primary outcome (Chmitorz 2018). Due to only five studies measuring healthcare professionals' stressor exposure (Berger 2011; Cieslak 2016; Gelkopf 2008; Varker 2012; Wild 2016), it remains unclear whether healthcare professionals really benefit from resilience training by being better able to cope with stressors. Future studies should therefore measure resilience as a person’s mental health in relation to individual stressor load. Only if the risk or stressor exposure (which is different from the subjective perception of stress) is assessed, may researchers gain knowledge about the changes in resilience by an intervention. In addition to the number of stressors, certain covariates such as the type of stressors (e.g. micro‐ versus macro‐stressors, psychological versus physiological stressors, acute versus chronic stressors) or the perceived severity of stressors should be assessed.
Study designs; there is a need for improved comparators, at least treatment as usual (TAU) or ideally active and attention control (Chmitorz 2018), to allow fair comparisons between resilience intervention and control. As already suggested (Chmitorz 2018), resilience‐training programmes could be implemented during or after the presence of a stressor. However, future studies should also use designs in which resilience training is provided prior to circumscribed stress situations (e.g. rotation of a physician to an emergency ward), in order to draw conclusions on resilience effects of the intervention, and to see whether the training does indeed improve resilience to the specific stress situation (Chmitorz 2018; Kalisch 2015). In general, pre‐ and post‐assessments of the outcome indicators (e.g. for resilience) should be conducted, with future studies also filling the gap of longer follow‐up periods and measuring the stressor exposure before, throughout and after the intervention. Also, it could be interesting to investigate whether booster sessions might help maintaining the effects of training over time. To ensure sufficient statistical power, the use of adequate sample sizes based on a priori analyses seems to be an urgent need in this field. Intervention studies might also benefit from comprehensive baseline diagnostics of mental health (e.g. clinical interview) and better reporting of eligibility criteria for pre‐existing mental symptoms. This would allow for more precise conclusions about whether resilience training reduces (clinically relevant) mental symptoms. Furthermore, the conceptual implications of the resilience concept would require a baseline mental health assessment. In order to investigate the effects of interventions on resilience (i.e. mental health in relation to stressor load) and to determine a specific 'resilience pattern or trajectory' under consideration, the status of psychological functioning as an outcome of interest at baseline is important. For example, when researchers are interested in testing the effects of an intervention in stressor‐exposed individuals on the resilience trajectory of sustained mental health (see also Description of the condition), they would have to prove a positive mental health level at baseline and at post‐intervention. On the other hand, researchers considering a sample with elevated levels of mental symptoms at pre‐test would be able to investigate the resilience trajectory of recovery or even of post‐traumatic growth, i.e. an increased level of functioning compared to outset prior to stressors. Beyond RCTs, dismantling designs could be helpful in clarifying the efficacy of single components of resilience training.
In general, there is a need for better reporting of intervention studies using international guidelines such as the CONSORT statement (Schulz 2010). To guarantee higher transparency of study conduct and reporting, primary investigators could register trials or publish study protocols according to the SPIRIT guidelines (Standard Protocol Items: Recommendations for Interventional Trials; Chan 2013a; Chan 2013b).
Finally, future studies in this field should focus more on male participants and on employees above the age of 50. Research efforts should be intensified in low‐ and middle‐income countries in order to reach more robust conclusions about the effectiveness of training across various settings. For certain formats of intervention (e.g. online‐ and mobile‐based), more studies would be desirable.
In sum, there is still a need for additional evidence to answer the question about which resilience interventions are really effective in healthcare professionals and how they should ideally be implemented.
History
Protocol first published: Issue 2, 2017 Review first published: Issue 7, 2020
Acknowledgements
The authors wish to acknowledge the support of the Cochrane Developmental, Psychosocial and Learning Problems (DPLP) editorial team, based at Queen's University Belfast and the University of Bristol. We would like to thank especially: Professor Geraldine Macdonald, Co‐ordinating Editor; Dr Joanne Duffield, Managing Editor; Dr Sarah Davies, Deputy Managing Editor; Gemma O'Loughlin, Former Assistant Managing Editor; and Margaret Anderson, Information Specialist, for their advice and assistance throughout the editorial process. We would also like to acknowledge the support and recommendations of members of the Cochrane Editorial Unit.
The authors are grateful to Editor, Dr Nuala Livingstone of DPLP and Cochrane Editorial and Methods Department, and the following peer reviewers for their time and comments: Professor Kate M Bennett, Department of Psychology, University of Liverpool; Dr Srini Chary, University of Calgary; Dr Martha Höfler, Mercator Institute, University of Cologne, and ResilienzExpertise, Bonn; and Dr Dimitris Mavridis, University of Ioannina.
We highly appreciate the contributions of Johanna Greesz, Svenja Kamp, Svenja Frenzel, Anastasia Doré, Paul Ludolph, Bruno Richter, Sophie Walter, Manpreet Blessin, Alice Zobel, and Charlotte Böhme to the completion of this review. We thank Steffen Reinecke and Donya A Gilan for their kind assistance with the translations of some of the included studies.
We thank the Ministry of Science (MWWK) of the State Rhineland‐Palatinate, Germany, for the funding provided for this review.
Appendices
Appendix 1. Glossary
Glossary of relevant terms in this review
Acceptance and commitment therapy: form of psychotherapy (third wave of cognitive behaviour therapy) that uses acceptance and mindfulness strategies (e.g. being in contact with present moment) and commitment and behaviour‐change skills (e.g. values, committed action) in order to increase psychological flexibility
Active control (in this review): alternative treatment (no standard care; for example, treatment developed specifically for the treatment study) that does not control for the amount of time and attention in the intervention group, and is not attention control in a narrow sense
Adverse event: an adverse outcome that occurs during or after the use of an intervention but is not necessarily caused by it
Arm(e.g. intervention arm, control arm): group of participants allocated to the intervention or control group
Attention and interpretation therapy: mindfulness‐based approach to reduce stress and increase resilience that teaches to delay judgements and to focus the attention on the novelty of the world as well as higher‐order principles (e.g. acceptance, gratitude)
Attention control: alternative treatment in the control group that mimics the amount of time and attention received (e.g. by the trainer) in the intervention group
Attrition: loss of participants during the course of a study (also referred to as loss to follow‐up)
Attrition bias: systematic differences between comparison groups in withdrawals or exclusions of participants from the results of a study (e.g. number or reasons, or both)
Available‐case analysis: analysis in which data are analysed for every participant for whom the outcome was obtained; subset may be defined after considering exposure to treatment, availability of measurements
Allied healthcare professionals: healthcare staff working in allied health professions distinct from medical care (e.g. psychologists, social workers, counsellors, physical therapists, occupational therapists, speech therapists, medical assistants, medical technicians)
Baseline characteristics: values of demographic, clinical and other variables collected for each participant at the beginning of a study, before the intervention is administered
Baseline comparability: data on the potential (statistical) differences between the study groups in baseline characteristics
Bias: a systematic error or deviation in results or inferences from the truth
Bibliotherapy: resilience intervention is delivered via a self‐help book/self‐help materials
Blinding: process of preventing those involved in a trial from knowing to which comparison group a particular participant belongs. The risk of bias is minimised when as few people as possible know who is receiving the experimental intervention and who the control intervention. Participants, outcome assessors, and analysts are all candidates for being blinded
Cluster randomised trial: a trial in which clusters of individuals (e.g. clinics, geographical areas), rather than individuals themselves, are randomised to different arms
Coaching: resilience intervention uses a coaching approach (e.g. executive coaching, life coaching); individual problems of one or several clients are discussed with a coach; coaching approaches often include goal setting
Cochrane Handbook for Systematic Reviews of Interventions(formerly Cochrane Reviewers’ Handbook): document containing guidance and advice on how to prepare and maintain Cochrane reviews
Cognitive‐behavioural therapy/training (CBT): form of psychotherapy that is based on the assumption that mental health problems (e.g. depression) result from dysfunctional thinking and therefore aims to modify cognitive processes (e.g. identify and challenge dysfunctional thoughts in order to find functional ones)
Combined setting: resilience interventions delivered as combination of group and individual setting
Combined theoretical foundation/combination: resilience interventions that are based on two or more explicit theoretical foundations, such as CBT and ACT or CBT and mindfulness
Comorbidity: presence of one or more diseases or conditions other than those of primary interest
Concealment of allocation: process used to ensure that the person deciding to enter a participant into a randomised controlled trial does not know the comparison group into which that individual will be allocated. This is distinct from blinding, and is aimed at preventing selection bias. Some attempts at concealing allocation are more prone to manipulation than others, and the method of allocation concealment is used as an assessment of the quality of a trial
Conference abstract: short summary of presentations at conferences, which may be published
Confidence interval: a measure of the uncertainty around the main finding of a statistical analysis. Estimates of an effect, such as the standardised mean difference comparing an experimental intervention with a control, are usually presented as a point estimate and a 95% confidence interval. This means that if someone were to keep repeating a study in other samples from the same population, 95% of the confidence intervals from those studies would contain the true value of the unknown quantity. Wider intervals indicate lower precision; narrow intervals, greater precision
Conflict of interest: personal, financial, or other interests that could have influenced a person's contributions to a study
Control group/control: comparison group that receives no intervention, identical training after waiting period or an alternative intervention
Degrees of freedom: concept that refers to the number of independent contributions to a sampling distribution (such as Chi2 distribution)
Detection bias: systematic difference between comparison groups in how outcomes are ascertained, diagnosed or verified
Dichotomous data: data that can take one of two possible values, such as depressive/non‐depressive (depending on cut‐off for clinically relevant mental disorder)
Effect size: 1. generic term for the estimate of effect of treatment for a study; 2. dimensionless measure of effect used for continuous data when different scales (e.g. for measuring resilience) are used to measure an outcome
Estimate of effect: observed relationship between an intervention and an outcome expressed as standardised mean difference in this review
Face‐to‐face: resilience intervention delivered via face‐to‐face contact between trainer and one or several participants
F test: statistical hypothesis test derived from the F distribution; typically used to compare continuous data between more than two groups
False positive: a falsely drawn positive conclusion
Fixed‐effect model (in meta‐analysis): model that calculates a pooled effect estimate using the assumption that all observed variation between studies is caused by the play of chance; studies assumed to be measuring the same overall effect
Follow‐up: observation over a period of time of study/trial participants to measure outcomes under investigation; in this review: short‐term: three months or less; medium‐term: more than three to six months; and long‐term follow‐up: more than six months
Forest plot: graphical representation of the individual results of each study included in a meta‐analysis together with the combined meta‐analysis result; plot also allows readers to see the heterogeneity among the results of the studies. The results of individual studies are shown as squares centred on each study’s point estimate. A horizontal line runs through each square to show each study’s confidence interval (in this review: 95% confidence interval). The overall estimate from the meta‐analysis and its confidence interval are shown at the bottom, represented as a diamond. The centre of the diamond represents the pooled point estimate, and its horizontal tips represent the confidence interval.
Funnel plot: graphical display of some measure of study precision plotted against effect size that can be used to investigate whether there is a link between study size and treatment effect; one possible cause of an observed association is reporting bias
Grey literature: kind of material that is not published in easily accessible journals or databases (e.g. conference proceedings that include the abstracts of the research presented at conferences, unpublished theses, etc.)
Group setting: resilience intervention delivered in group of several participants
Hardiness: a (modifiable) personality characteristic ('a hardy person') that consists of three elements (challenge, commitment and control); partly used as synonym of resilience; in this review, hardiness is viewed as one of several resilience factors which partially determines resilience as outcome
Healthcare professionals: healthcare staff delivering direct medical care (e.g. nurses, physicians, hospital personnel)
Heterogeneity: 1. used in a general sense to describe the variation in, or diversity of, participants, interventions, and measurement of outcomes across a set of studies; 2. used specifically, as statistical heterogeneity, to describe the degree of variation in the effect estimates from a set of studies
Heterogeneous: used to describe a set of studies or participants with sizeable heterogeneity
Homogeneous: 1. used in a general sense to mean that the participants, interventions, and measurement of outcomes are similar across a set of studies; 2. used specifically to describe the effect estimates from a set of studies where they do not vary more than would be expected by chance
Individual setting: resilience interventions delivered in one‐on‐one setting
Intention to treat analysis: a strategy for analysing data from a randomised controlled trial; all participants are included in the arm to which they were allocated, whether or not they received (or completed) the intervention given to that arm. Intention‐to‐treat analysis prevents bias caused by the loss of participants, which may disrupt the baseline equivalence established by randomisation and which may reflect non‐adherence to the protocol
Inter‐rater reliability: degree of stability exhibited when a measurement is repeated under identical conditions by different raters; reliability refers to the degree to which the results obtained by a measurement procedure can be replicated. Lack of inter‐rater reliability may arise from divergences between observers or instability of the attribute being measured
Interaction: situation in which the effect of one independent variable on the outcome is affected by the value of a second independent variable
Intervention: the process of intervening on people in an experimental study (in this review: by resilience‐training programmes)
Intervention group: a group of participants in a study receiving a particular intervention (in this review: resilience intervention)
Laboratory delivery: resilience intervention is provided in the laboratory (under standardised conditions)
Mean: an average value, calculated by adding all the observations and dividing by the number of observations
Mean difference: difference between two estimated means (e.g. used in this review to present the results for single studies that could not be combined in meta‐analysis together with other studies)
MeSH headings (Medical Subject Headings): terms used by the United States National Library of Medicine to index articles in Index Medicus and MEDLINE. The MeSH system has a tree structure in which broad subject terms branch into a series of progressively narrower subject terms.
Meta‐analysis: use of statistical techniques in a systematic review to integrate the results of included studies
Mindfulness‐based training: intervention that aims to foster mindfulness (i.e. non‐judging awareness of the present moment and its accompanying mental phenomena, like body sensations, thoughts and emotions), by teaching formal and informal mindfulness practices (e.g. body scan, breathing awareness) (e.g. mindfulness‐based stress reduction, MBSR)
Mixed samples: studies with samples including healthcare professionals and participants from the non‐healthcare sector (e.g. ambulance personnel and firefighters)
Multimodal delivery: intervention is delivered by a combination of different formats (e.g. face‐to‐face and online)
No intervention control: control group that received no intervention
Online‐ or mobile‐based delivery: resilience intervention is delivered online/internet‐based or via smartphones (e.g. smartphone application)
Outcome: a component of a participant's clinical and functional status after an intervention has been applied, which is used to assess the effectiveness of an intervention
P value: the probability (ranging from zero to one) that the results observed in a study (or results more extreme) could have occurred by chance if in reality the null hypothesis was true. In a meta‐analysis, the P value for the overall effect assesses the overall statistical significance of the difference between the intervention groups, whilst the P value for the heterogeneity statistic assesses the statistical significance of differences between the effects observed in each study.
Parallel group trial: a trial that compares two groups of people concurrently, one of which receives the intervention of interest and one of which is a control group; some parallel trials have more than two comparison groups
Participant: an individual who is studied in a trial
Per protocol analysis: an analysis of the subset of participants from a randomised controlled trial who completed the trial or complied with the protocol sufficiently (e.g. specific dose of treatment) to ensure that their data would be likely to exhibit the effect of treatment; this subset may be defined after considering exposure to treatment and absence of major protocol violations. The per protocol analysis strategy may be subject to bias as the reasons for non‐compliance may be related to treatment.
Performance bias: systematic differences between intervention groups in care provided apart from the intervention being evaluated; for example, if participants know they are in the control group, they might act differently, and if intervention providers are aware of the group a particular participant is in, they might act differently. Blinding of study participants (both the recipients and providers of intervention) is used to protect against performance bias.
Positive psychology: scientific study of character strengths and positive aspects of human life (e.g. happiness) that allow individuals to thrive; interventions based on positive psychology aim to foster these factors
Post‐traumatic growth (also stress‐related growth): often used synonymously with resilience; however, in contrast to resilience (i.e. maintaining or restoring mental health after a stressor), post‐traumatic or stress‐related growth refers to increasing the level of functioning compared to that prior to the stressor
Post‐test/post‐intervention: the assessment immediately after the end of treatment (in this review: within one week after the end of training)
Precision: a measure of the likelihood of random errors in the results of the meta‐analysis; the greater the precision, the less random error. Confidence intervals around the estimate of effect from each study are one way of expressing precision, with a narrower confidence interval meaning more precision.
Primary outcome: the outcome of greatest importance
Primary study: ‘original research’ in which data are collected
Problem‐solving training: closely related to CBT; training based on problem‐solving theory (e.g. to foster a positive problem orientation and to teach structured problem‐solving)
Random allocation: method that uses the play of chance to assign participants to comparison groups in a trial, e.g. by using a random numbers table or a computer‐generated random sequence. Random allocation implies that each individual or unit being entered into a trial has the same chance of receiving each of the possible interventions. It also implies that the probability that an individual will receive a particular intervention is independent of the probability that any other individual will receive the same intervention.
Random‐effects model (in meta‐analysis): a statistical model in which both within‐study sampling error (variance) and between‐studies variation are included in the assessment of the uncertainty (confidence interval) of the results of a meta‐analysis; when there is heterogeneity among the results of the included studies beyond chance, random‐effects models will give wider confidence intervals than fixed‐effect models
Randomisation: the process of randomly allocating participants into one of the arms of a controlled trial. There are two components to randomisation: the generation of a random sequence; and its implementation, ideally in a way so that those entering participants into a study are not aware of the sequence (concealment of allocation).
Randomised controlled trial: study in which two or more conditions, possibly including a control intervention or no intervention, are compared by being randomly allocated to participants
Reporting bias: bias caused by only a subset of all the relevant data being available. The publication of research can depend on the nature and direction of the study results. Studies in which an intervention is not found to be effective are sometimes not published. In addition, a published report might present a biased set of results (e.g. only outcomes or subgroups where a statistically significant difference was found).
Resilience: maintenance or fast recovery of mental health during or after substantial adversities; different definitions exist, however, there is a consensus about two essentials: 1. exposure to substantial stressors or adversities; 2. successful coping with these adversities
Resilience factor: psychological or social factors associated to resilience, e.g. optimism
Search strategy: 1. the methods used to identify trials within the review's scope (including searching electronic databases, trial registers, personal contact with researchers/study authors and checking reference lists); 2. the combination of terms used to identify studies in an electronic database such as MEDLINE
Secondary outcome: an outcome used to evaluate additional effects of the intervention deemed a priori as being less important than the primary outcomes
Selection bias: systematic differences between comparison groups in prognosis or responsiveness to treatment; random allocation with adequate concealment of allocation protects against selection bias. Other means of selecting who receives the intervention are more prone to bias because decisions may be related to prognosis or responsiveness to treatment
Sensitivity analysis: analysis used to determine how sensitive the results of the systematic review are to changes in how it was done; sensitivity analyses are used to assess how robust the results are to uncertain decisions or assumptions about the data and the methods that were used.
Single blind: single masked
Standard deviation: measure of the spread or dispersion of a set of observations, calculated as the average difference from the mean value in the sample
Standard error: standard deviation of the sampling distribution of a statistic; measurements taken from a sample of the population will vary from sample to sample. The standard error is a measure of the variation in the sample statistic over all possible samples of the same size. The standard error decreases as the sample size increases.
Standardised mean difference: difference between two estimated means divided by an estimate of the standard deviation; used to combine results from studies using different ways of measuring the same concept, e.g. resilience or mental health. By expressing the effects as a standardised value, the results can be combined since they have no units.
Stress inoculation: form of CBT; psychotherapeutic method to prepare participants to deal with stressors successfully and to achieve coping strategies by exposing them to milder forms of stress
Subgroup analysis: an analysis in which the intervention effect is evaluated in a defined subset of the participants/interventions in a trial, or in complementary subsets, such as by intervention setting or delivery format
Telephone delivery: resilience intervention that are provided via the telephone (e.g. calls between trainer and participant)
Training intensity: intensity of intervention as indicated by the number of sessions or the number of hours (i.e. duration); in this review: low intensity: total duration of ≤ five hours or ≤ three sessions; moderate intensity: > 5 hours to ≤ 12 hours or > 3 to ≤ 12 sessions; high intensity: > 12 hours or > 12 sessions
Treatment as usual (TAU): the control group receives a (established) standard treatment (synonyms: standard care, usual care)
t test: a statistical hypothesis test derived from the t distribution; used to compare continuous data in two groups
Trialist: refers to a person conducting or publishing a controlled trial
Type I error (also false positive): conclusion that a treatment works, when it actually does not work; the risk of a Type I error is often called alpha. In a statistical test, it describes the chance of rejecting the null hypothesis when it is in fact true.
Unspecific theoretical foundation/unspecific training programmes: resilience interventions fostering one or several resilience factors but without specifying any explicit theoretical foundation or where the underlying framework cannot be assigned to a certain theoretical approach
Unspecified/not specified setting, delivery, training intensity or comparator: no information on the respective intervention characteristic or the comparator are available and could not be received by the study authors
Variable: a factor that differs among and between groups of people, e.g. patient characteristics such as age, sex, and smoking, or measurements such as blood pressure or depression score; there can also be treatment or condition variables (e.g. length of treatment dose) and outcome variables
Wait‐list control: control group receiving the training after a waiting period
Footnotes
This glossary is based, in part, on the glossary of the Cochrane Community (Cochrane Community 2020).
Appendix 2. Evidence rating of modifiable resilience factors
Although an immense number of factors have been discussed in the literature, only a set of psychosocial factors has been scientifically validated as being appropriate determinants of resilience by cross‐sectional and longitudinal (frequently observational) studies in different populations (e.g. patients affected by physical diseases like cancer, diabetes, spinal cord injury, coronary heart disease, etc.; different caregiver groups; individuals after trauma exposure). Upon closer examination, only some of the discussed resilience factors may be viewed as well‐evidenced factors that have also been found to be protective in systematic reviews and meta‐analyses (level 1). These factors are most likely to be related to adult resilience, as they were proven in different populations facing various adversities and stressors. However, it has to be kept in mind that the chosen factors represent the current state of knowledge on psychosocial resilience‐promoting factors, and that other factors, which are not yet well researched, could also contribute to resilience.
| Level of evidence and criteria | Resilience factors |
Level 1: strong evidence (SRs and MAs)
| |
| Level 1a: there is evidence for this factor from several SRs AND several MAs (both across different populations) |
|
| Level 1b: there is evidence for this factor from several SRs AND a single MA (both across different populations) |
|
| Level 1c: there is evidence for this factor from several SRs (across different populations) AND a single MA (in the same population) |
|
Level 2: moderate evidence (only SRs or single MA)
| |
| Level 2a: there is evidence for this factor from several SRs (across different populations) OR there is no evidence from SRs, but from a MA (across different populations) |
|
| Level 2b: there is evidence for this factor from several SRs (in the same population) |
|
| Level 2c: there is evidence for this factor from a single SR (in the same population) |
|
Level 3: weak evidence (no SR or MA)
| |
|
|
| MA: Meta‐analysis; SR: Systematic review | |
Footnotes
Results of systematic reviews and meta‐analyses based on a literature search for potentially modifiable resilience factors in MEDLINE (search strategy: respective resilience factor.tw. AND (review or meta‐analy$).tw.; search limited to “All adults (19 plus years)” and 1990‐2016).
aCognitive flexibility and religiosity or spirituality are multidimensional concepts resulting in highly ambiguous operationalisations. Cognitive flexibility comprises several concepts, such as positive reappraisal and acceptance (Southwick 2005). Religiosity or spirituality combines affective, behavioural and cognitive dimensions, each measured differently (Ano 2005; Pargament 2000; Salsman 2015).
Appendix 3. Examples of training methods to address resilience factors
| Evidence‐based resilience factor | Examples of training methods to address the resilience factor |
| Meaning in life or purpose in life | Introduce the benefits of purpose in life; support individuals in identifying important sources of meaning (e.g. social relationships, work) as well as in setting priorities and guiding values for their life (e.g. Sood 2011) |
| Sense of coherence (comprehensibility, meaningfulness, manageability) | Promote the understanding of external life challenges, personal beliefs and emotions; encourage participants to reflect on personal (internal or external) resources and to use them more frequently (e.g. Tan 2016) |
| Positive emotions or positive affect | Psychoeducation on emotions; mindfulness techniques; support individuals in identifying pleasant activities to enhance positive emotions (e.g. Jennings 2013) |
| Hardiness (challenge, commitment, control) | Situational reconstruction (i.e. imagination of stressful circumstances); focusing (i.e. reflection on bodily sensations of emotional upset) (e.g. Maddi 1998; Maddi 2009) |
| Self‐esteem | Support participants in identifying personal strengths |
| Active coping (e.g. problem‐solving, planning) | Introduce the problem‐solving model and familiarise participants with the use of active coping strategies in stressful situations (e.g. making action plans) (e.g. Abbott 2009; Bekki 2013; Sahler 2013) |
| Self‐efficacy | Support participants in identifying personal strengths and other sources of self‐efficacy (e.g. social connections); support individuals in realising previous successes (e.g. coping of negative situations) |
| Optimism or positive attributional style | Teach participants to adopt a more positive attributional style for stressful (i.e. external, unstable, specific) and pleasant events (i.e. internal, stable, global); encourage individuals to gain a brighter outlook for the future by enhancing their attention for and the discovery of positive aspects in their lives (e.g. Carver 2010; Sadow 1993) |
| Social support | Encourage the individual’s reflection on his or her current network (i.e. magnitude of social network, positive or negative aspects in social relationships); enhance the individual’s support network by providing them with communication techniques (e.g. Kent 2011; Schachman 2004; Sood 2011; Steinhardt 2008) |
| Cognitive flexibility (e.g. positive reappraisal, acceptance of negative situations and emotions) | Positive reappraisal: introduction of ABC (Activating Event, Belief, Consequence) Technique of Irrational Beliefs (Ellis 1957) of cognitive therapy; train participants in identifying and challenging maladaptive thoughts and replacing them by more positive ones (e.g. Abbott 2009; Farchi 2010; Songprakun 2012; Steinhardt 2008) Acceptance: relaxation or mindfulness techniques |
| Religiosity or spirituality or religious coping (e.g. frequent religious attendance) | Spiritual exercises like meditation or yoga; psychoeducation on coping strategies like regular praying or participating in religious community activities (e.g. worship) (e.g. Sood 2011) |
Appendix 4. Previous systematic reviews and meta‐analyses and their methodological weaknesses
Systematic reviews and meta‐analyses of various types of interventions to foster healthcare professionals' mental health; e.g. CIPSRT 2016; Boellinghaus 2014; Buddeberg‐Fischer 2006; Burton 2017; Car 2018; Carrieri 2018; Chesak 2019b; Cochran 2017; De Oliveira 2019; Edwards 2003; Guillaumie 2017; Hannigan 2004; Harris 2018; Jones 2000; Lamothe 2016; Maben 2018; McVicar 2003; Mimura 2003; Panagioti 2017; Paris 2010; Petrie 2019; Raj 2016; Regehr 2014; Romppanen 2017; Ruotsalainen 2015; Smith 2003; Trowbridge 2016; West 2016.
Systematic reviews and meta‐analyses on resilience interventions in clinical and non‐clinical adult populations
| Category | Details of previous reviews/meta‐analyses |
| Number of reviews and meta‐analyses |
|
| Methodological characteristics | Eligibility critiera: heterogeneous eligibility criteria (e.g. concerning study design) and definitions of resilience training (e.g. the aim of fostering resilience was not always stated in the included primary studies |
| Search strategy: Some reviews used rather simple, limited search strategies to identify relevant studies (e.g. only resilience/hardiness combined with training terms in, for example, Joyce 2018; Robertson 2015; restriction to English language), which may bias the search results. | |
| Review protocol/registration: A review protocol or PROSPERO registration was available for four publications only (Bauer 2018; Leppin 2014; Townshend 2016; Wainwright 2019). | |
| Review according to guidelines: Most reviews report having been conducted according to the PRISMA or alternative guidelines such as the guidance for undertaking reviews in health care (CRD 2009; e.g. Milne 2016; Van Kessel 2014). | |
| Quality assessment of included studies: Most reviews performed a quality assessment of the primary studies (the exceptions being Milne 2016; Pallavicini 2016; Reyes 2018; Skeffington 2013; Vanhove 2016, who only judged publication bias; we were also unable to verify if Tams 2016 conducted a quality assessment because we could not retrieve the full text). For studies included in several reviews, the reported risk of bias also differed between publications (e.g. detection bias for Abbott 2009 differed between Leppin 2014 and Robertson 2015). |
Footnotes
aDeady 2017 and Tams 2016 searched for 'resilience' and related constructs, but did not formulate specific eligibility criteria concerning resilience‐training programmes.
Systematic reviews and meta‐analyses on resilience interventions in healthcare professionals
| Category | Details of previous reviews/meta‐analyses |
| Number of reviews and meta‐analyses |
|
| Methodological characteristics |
Eligibility critiera:
|
Search strategy:
| |
| Review protocol/registration: The absence of a published protocol or protocol registration for most of these reviews (the exceptions being Gillman 2015; Gilmartin 2017; Pezaro 2017; Lavin Venegas 2019) also reduces transparency and comparability in the reviews' procedures and potentially restricts the evidence found. | |
| Review according to guidelines: Several reviews did not specify whether they had been conducted according to guidelines, such as PRISMA or Cochrane guidelines, or other validated frameworks (e.g. Elliott 2012; Gillman 2015; Hunter 2016; Robertson 2016; Rogers 2016; Wright 2017). | |
Quality assessment of included studies:
|
Footnotes
aTaylor 2018 identified resilience training as an alternative intervention to assess the impact of Schwartz Center Rounds on healthcare staff. However, as the review aimed to synthesise the evidence base on Schwartz Center Rounds, we did not consider it to be a 'resilience review'.
Appendix 5. Potential instruments for the measurement of psychological resilience based on previous reviews (Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016) and additional literature searchesa
| N° | Measure | Theory and item selection | Internal consistency | Validity | Rating |
| 1 | Resilience Scale (RS‐25) (Wagnild 1993)b |
+ | +++ | +++ | 6✦ |
| 2 | Brief Resilience Scale (BRS) (Smith 2008) |
+ | +++ | +++ | 6✦ |
| 3 | Ego Resiliency (Klohnen 1996)b |
+ | ++ | +++ | 5✦ |
| 4 | Connor ‐ Davidson Resilience Scale (CD‐RISC) (Connor 2003) |
+ | ++ | +++ | 5✦ |
| 5 | Resilience Scale for Adults (RSA33) (Friborg 2005) |
+ | ++ | +++ | 5✦ |
| 6 | Trauma Resilience Scale (TRS37) (Madsen 2010) |
+ | +++ | ++ | 5✦ |
| 7 | Ego ‐ Resiliency Scale (ER89) (Block 1996)b |
‐ | ++ | +++ | 5✧ |
| 8 | Resilience Scale (RS‐14) (Wagnild 2009)b |
+ | +++ | + | 4✦ |
| 9 | Resilience Scale for Adults (RSA37) (Friborg 2003) |
+ | ++ | ++ | 4✦ |
| 10 | Resilience at Work Scale (Winwood 2013) |
+ | ++ | ++ | 4✦ |
| 11 | Workplace Resilience Inventory (WRI) (McLarnon 2013) |
+ | ++ | ++ | 4✦ |
| 12 | Multidimensional Trauma Recovery and Resiliency Scale (MTRR) (Harvey 2003) |
+ | +++ | + | 4✦ |
| 13 | Resiliency Attitudes and Skills Profile (RASP) (Hurtes 2001) |
+ | +++ | + | 4✦ |
| 14 | Resilience Appraisals Scale (RAS) (Johnson 2010) |
‐ | +++ | + | 4✧ |
| 15 | Revised Ego Resiliency 89 Scale (ER89‐R) (Alessandri 2007)b |
+ | ++ | + | 3✦ |
| 16 | Ego Resiliency (Bromley 2006)b |
+ | ++ | + | 3✦ |
| 17 | Connor ‐ Davidson Resilience Scale (CD‐RISC‐10) (Campbell‐Sills 2007) |
+ | ++ | + | 3✦ |
| 18 | Resilience Scale for Adults (RSA45) (Hjemdal 2001) |
+ | +++ | ‐ | 3✦ |
| 19 | Brief Resilient Coping Scale (BRCS) (Sinclair 2004) |
+ | + | ++ | 3✦ |
| 20 | Trauma Resilience Scale (TRS48) (Madsen 2010) |
+ | +++ | ‐ | 3✦ |
| 21 | Child and Youth Resilience Measure ‐ 28 (CYRM‐28) (Liebenberg 2012; Ungar 2008) |
+ | +++ | ‐ | 3✦ |
| 22 | Post‐traumatic Growth Inventory (PTGI) (Tedeschi 1996)c |
+ | ++ | + | 3✦ |
| 23 | Adolescent Resilience Scale (Oshio 2002; Oshio 2003) |
‐ | ++ | + | 3✧ |
| 24 | Resilience and Reintegration (20 items drawn from Spirit Core Scale) (Waite 2004) |
‐ | +++ | ‐ | 3✧ |
| 25 | Psychological resilience (Windle 2008) |
+ | ++ | ‐ | 2✦ |
| 26 | Child and Youth Resilience Measure ‐ 12 (CYRM‐12) (Liebenberg 2013) |
+ | ++ | ‐ | 2✦ |
| 27 | Resilience scale (Bekki 2013) |
+ | ++ | ‐ | 2✦ |
| 28 | Perceived resilience (Van der Kleij 2011) |
‐ | ++ | ‐ | 2✧ |
| 29 | Romanian Scale of Resilience to Occupational Stress (SROS) (Aniţei 2012) |
‐ | ‐ | ‐ | 0✧ |
Footnotes
The resilience scales are specified hierarchically according to psychometric quality criteria.
Theory & item selection: ‐ (✧): no description of theory or item selection process available; and + (✦): description of theory or item selection process available.
Internal consistency (Cronbach’s alpha): ‐ (0): no information; + (1): α < 0.70; ++ (2): α ≥ 0.70; and +++ (3): α > 0.90.
Validity (convergent/divergent or criterion validity): ‐ (0): no information; + (1): correlations (r) with construct‐related measures or criterions available, all correlations < 0.50 or resilience measure only correlated with original instrument/long‐form or no correlations but alternative results reported (e.g. odds ratio); ++ (2): correlations (r) with construct‐related measures or criterions available, ≤ 50% of correlations ≥ 0.50; and +++ (3): correlations (r) with construct‐related measures or criterions available, > 50% of correlations ≥ 0.50.
aAt the time of prespecifying these measures and the publication of the protocol (Helmreich 2017), the systematic review of Joyce 2018 had not yet been published and was not considered in the development of this appendix. bScales assessing resilience as a personality characteristic. cScale assessing post‐traumatic growth.
Appendix 6. Possible assessment instruments for the measurement of mental health and well‐being based on intervention studies included in previous reviews and meta‐analyses (Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016)a
-
Anxiety
Depression Anxiety and Stress Scales (DASS‐21) (Lovibond 1995)
Smith Anxiety Scale (SAS) (Smith 2007)
Beck Anxiety Inventory (BAI) (Beck 1993)
State‐Trait Anxiety Inventory (STAI) (Spielberger 1970)
-
Depression
Depression Anxiety and Stress Scales (DASS‐21) (Lovibond 1995)
Center for Epidemiological Studies ‐ Depression Scale (CES‐D) (Radloff 1977)
Maslach Burnout Inventory (MBI) (Maslach 1997)
Oldenburg Burnout Inventory (Demerouti 2010)
Beck Depression Inventory (BDI) (Beck 1961)
Beck Depression Inventory ‐ II (BDI‐II) (Beck 1996)
Visual Analog Scale ‐ Fatigue (VAS‐Fatigue) (Wolfe 2004)
Patient Health Questionnaire for Depression (PHQ‐D) (Spitzer 1999)
Hospital Anxiety and Depression Scale (HADS) (Zigmond 1983)
Time Urgency Scale (TUS) (Landy 1991)
-
Stress or stress perception
Depression Anxiety and Stress Scales (DASS‐21) (Lovibond 1995)
Perceived Stress Scale (PSS) (Cohen 1988a)
Personal Stress Scale (PSS) (self‐developed) (Petree 2012)
Subjective Units of Distress (SUDS) (Wolpe 1958)
Visual Analog Scale (VAS) (Arnetz 1985; Hasson 2005)
Stress and Perception of Control Scale (SPOCS) (unpublished instrument) (Rose 2013)
-
Well‐being or life satisfaction or quality of life or vitality or vigour
-
Well‐being
-
Life satisfaction:
Satisfaction with Life Scale (Diener 1985)
-
(Health‐related) Quality of life (QOL):
Linear Analog Self‐Assessment Scale (QOL‐LASA) (Locke 2007)
Medical Outcomes Study (MOS) 36‐item short‐form health survey (SF‐36) (Ware 1994)
World Health Organization Quality of Life – BREF (WHOQOL‐BREF) (WHOQOL Group 1998)
-
Vitality
Subscale of the MOS 36‐item short‐form health survey (SF‐36) (Ware 1994)
-
Vigour
Work Vigour subscale of the Utrecht Work Engagement scale (Schaufeli 2002)
-
aAt the time of prespecifying these measures and the publication of the protocol, the systematic review of Joyce 2018 had not yet been published and was not considered in the development of this appendix.
Appendix 7. Possible assessment instruments for the measurement of resilience factors based on intervention studies included in previous reviews and meta‐analyses (Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016)a
-
Social support
Interpersonal Support Evaluation List ‐ 12 (ISEL‐12) (Cohen 1983a)
Personal Resources Questionnaire (PRQ‐85) (Brandt 1981)
Social Provisions Scale (Cutrona 1987)
Subscale Interpersonal relations of the Health‐Promoting Lifestyle Profile II (Walker 1987)
Interpersonal Relationship Inventory (IPR) (Tilden 1990)
Support questionnaire (Cushway 1996)
MOS Social Support Survey (Sherbourne 1991)
Total of four scales devised by Moos (1979) for perceived social support (Maddi 1998)
-
Optimism
Life Orientation Test ‐ Revised (LOT‐R) (Scheier 1994)
-
Self‐efficacy
Coping self‐efficacy (CSE) (Chesney 2003)
Self‐efficacy scale (Sherer 1982)
Teachers’ Sense of Efficacy Questionnaire (TSES) (Tschannen‐Moran 2001)
New General Self‐Efficacy Scale (NGSE) (Chen 2004)
Coping Efficacy Scale (self‐developed) (Bekki 2013)
-
Active coping
Brief Coping Orientations to Problems Experienced scale (Brief COPE) (Carver 1997)
Ways of Coping Questionnaire (WOC) (Folkman 1988)
Coping Styles Questionnaire (CSQ) (Williams 1997)
Coping Styles (self‐developed) (Bekki 2013)
-
Self‐esteem
Rosenberg Self‐Esteem Scale (RSES) (Rosenberg 1965)
Self‐Esteem Rating Scale (SERS) (Nugent 1993)
-
Hardiness
HardiSurvey III ‐ R (Maddi 2001)
Personal Views Survey (Maddi 1987)
Hardiness Scale or College Student Hardiness Measure (CSHM) (Atri 2007a; Atri 2007b; Kanekar 2010)
Cognitive Hardiness Scale (Nowack 1990)
-
Positive emotions or positive affect
Positive and Negative Affect Schedule (PANAS) (Watson 1988)
Positive and Negative Affect Schedule Expanded Form (PANAS‐X) (Watson 1994)
Authentic Happiness Inventory (AHI; unpublished measure) (Abbott 2009)
aAt the time of prespecifying these measures and the publication of the protocol (Helmreich 2017), the systematic review of Joyce 2018 had not yet been published and was not considered in the development of this appendix.
Appendix 8. Search strategies up to 2016
In order to get a comprehensive understanding of the evidence in the field of psychological resilience interventions, and to identify training programmes that can really be assumed to enhance resilience in adults based on scientific findings, we performed a literature search that combined and complemented the search approaches from previous reviews and meta‐analyses.
In contrast to the search strategy of Joyce 2018, Leppin 2014, Robertson 2015 and Vanhove 2016, who used very narrow search terms (e.g. ‘resilience programme’ or 'hardiness training’), we also searched for broader intervention terms. These broader search terms were based on the search performed by Macedo 2014, but were also supplemented by new terms (e.g. ‘acceptance and commitment therapy’, ‘stress management’, ‘mindfulness’).
We searched the databases below in October 2016 using search strategies based on the original inclusion criteria for this review.
Cochrane Central Register of Controlled Trials (CENTRAL)
Searched 27 October 2016 [5168 records]
#1 [mh "Resilience, Psychological"] #2 [mh "social adjustment"] #3 [mh "Adaptation, Psychological"] #4 ("post‐traumatic growth" or "posttraumatic growth" or "stress‐related growth") #5 (positiv* near/1 (adapt* or adjust*)) #6 (psychol* near/1 (adapt* or adjust*)) #7 (resilien* or hardiness*) #8 (cope or coping) #9 ((withstand* or overcom* or resist* or recover* or thriv* or adapt* or adjust* or bounc* back) near/5 (stress* or trauma* or adversit*)) #10 {or #1‐#9} #11 [mh psychotherapy] #12 MeSH descriptor: [Stress, Psychological] this term only and with qualifier(s): [Therapy ‐ TH] #13 (psychotherap* or psycho next therap*) #14 (behav* near/3 (intervention* or program* or therap*)) #15 ((cognit* or cognitive next behavior* or CBT) near/3 (intervention* or program* or therap*)) #16 (psycho* near/3 (intervention* or program* or therap*)) #17 relaxation #18 mindful* #19 (counsel*ing or coaching) #20 (third next wave next (psycho* or therap*)) #21 cognit* next restructur* #22 positive next psychology #23 (refram* or re next fram* or reapprais*) #24 (stress near/1 (inoculation or manag* or reduc* or resist*)) #25 (anxiety near/3 manage*) #26 "acceptance and commitment " #27 [mh "Combined Modality Therapy"] #28 (multimodal* or multi next modal* or combined modal*) #29 [mh "Health promotion"] #30 (health near/3 (educat* or promot*)) #31 {or #11‐#30} #32 #10 and #31, Publication Year from 1990 to 2016, in Trials
MEDLINE OVID
Searched 28 October 2016 [6723 records]
1 Resilience, Psychological/ 2 social adjustment/ 3 Adaptation, Psychological/ 4 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw,kf. 5 (positiv$ adj1 (adapt$ or adjust$)).tw,kf. 6 (psychol$ adj1 (adapt$ or adjust$)).tw,kf. 7 (resilien$ or hardiness$).tw,kf. 8 (cope or coping).tw,kf. 9 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj5 (stress$ or trauma$ or adversit$)).tw,kf. 10 or/1‐9 11 exp psychotherapy/ 12 Stress, Psychological/th 13 (psychotherap$ or psycho‐therap$).tw,kf. 14 (behav$ adj3 (intervention$ or program$ or therap$)).tw,kf. 15 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw,kf. 16 (psycho$ adj3 (intervention$ or program$ or therap$)).tw,kf. 17 relaxation.tw,kf. 18 mindful$.tw,kf. 19 (counsel?ing or coaching).tw,kf. 20 (third wave adj (psycho$ or therap$)).tw,kf. 21 cognit$ restructur$.tw,kf. 22 positive psychology.tw,kf. 23 (refram$ or re‐fram$ or reapprais$).tw,kf. 24 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw,kf. 25 (anxiety adj3 manage$).tw,kf. 26 "acceptance and commitment ".tw,kf. 27 Combined Modality Therapy/ 28 (multimodal or multi‐modal or combined modal$).tw,kf. 29 exp Health promotion/ 30 (health adj3 (educat$ or promot$)).tw,kf. 31 or/11‐30 32 10 and 31 33 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kf. 34 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kf. 35 or/32‐34 36 randomized controlled trial.pt. 37 controlled clinical trial.pt. 38 randomi#ed.ab. 39 placebo$.ab. 40 drug therapy.fs. 41 randomly.ab. 42 trial.ab. 43 groups.ab. 44 or/36‐43 45 exp animals/ not humans.sh. 46 44 not 45 47 35 and 46 48 limit 47 to yr="1990 ‐Current"
Embase OVID
Searched 26 October 2016 [6709 records]
1 exp coping behavior/ 2 psychological adjustment/ 3 social adaptation/ 4 "personal resource"/ 5 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw,kw. 6 (positiv$ adj1 (adapt$ or adjust$)).tw,kw. 7 (psychol$ adj1 (adapt$ or adjust$)).tw,kw. 8 (resilien$ or hardiness$).tw,kw. 9 (cope or coping).tw,kw. 10 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj5 (stress$ or trauma$ or advers$)).tw,kw. 11 or/1‐10 12 exp psychotherapy/ 13 posttraumatic stress disorder/th [Therapy] 14 mental stress/th [Therapy] 15 (psychotherap$ or psycho‐therap$).tw,kw. 16 (behav$ adj3 (intervention$ or program$ or therap$)).tw,kw. 17 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw,kw. 18 (psycho$ adj3 (intervention$ or program$ or therap$)).tw,kw. 19 mindful$.tw,kw. 20 exp counseling/ 21 (counsel?ing or coaching).tw,kw. 22 mindfulness/ 23 mindful$.tw,kw. 24 (third wave adj (psycho$ or therap$)).tw,kw. 25 cognit$ restructur$.tw,kw. 26 positive psychology.tw,kw. 27 (refram$ or re‐fram$ or reapprais$).tw,kw. 28 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw,kw. 29 (anxiety adj3 manage$).tw,kw. 30 "acceptance and commitment ".tw,kw. 31 (multimodal$ or multi‐modal$ or combined modal$).tw,kw. 32 exp health promotion/ 33 (health adj3 (educat$ or promot$)).tw,kw. 34 or/12‐33 35 11 and 34 36 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kw. 37 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kw. 38 or/35‐37 39 Randomized controlled trial/ 40 controlled clinical trial/ 41 Single blind procedure/ 42 Double blind procedure/ 43 triple blind procedure/ 44 Crossover procedure/ 45 (crossover or cross‐over).tw. 46 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 47 Placebo/ 48 placebo.tw. 49 prospective.tw. 50 factorial$.tw. 51 random$.tw. 52 assign$.ab. 53 allocat$.tw. 54 volunteer$.ab. 55 or/39‐54 56 38 and 55 57 limit 56 to yr="1990 ‐Current" 58 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/ 59 human/ or normal human/ or human cell/ (18144770) 60 58 and 59 61 58 not 60 62 57 not 61
PsycINFO OVID
Searched 27 October 2016 [5005 records]
1 "resilience (psychological)"/ 2 "adaptability (personality)"/ 3 emotional adjustment/ 4 coping behavior/ 5 posttraumatic growth/ 6 protective factors/ 7 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw. 8 (positiv$ adj1 (adapt$ or adjust$)).tw. 9 (psychol$ adj1 (adapt$ or adjust$)).tw. 10 (resilien$ or hardiness$).tw. 11 (cope or coping).tw. 12 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj3 (stress$ or trauma$ or advers$)).tw. 13 or/1‐12 14 exp psychotherapy/ 15 exp cognitive techniques/ 16 psychotherapeutic techniques/ 17 relaxation therapy/ 18 mindfulness/ 19 stress management/ 20 (psychotherap$ or psycho‐therap$).tw. 21 (behav$ adj3 (intervention$ or program$ or therap$)).tw. 22 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw. 23 (psycho$ adj3 (intervention$ or program$ or therap$)).tw. 24 relaxation.tw. 25 mindful$.tw. 26 (counsel?ing or coaching).tw. 27 (third wave adj (psycho$ or therap$)).tw. 28 cognit$ restructur$.tw. 29 positive psychology.tw. 30 (refram$ or re‐fram$ or reapprais$).tw. 31 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw. 32 (anxiety adj3 manage$).tw. 33 "acceptance and commitment".tw. 34 multimodal treatment approach/ 35 (multimodal$ or multi‐modal$ or combined modal$).tw. 36 health promotion/ 37 (health adj3 (educat$ or promot$)).tw. 38 or/14‐37 39 13 and 38 40 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw. 41 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw. 42 or/39‐41 43 clinical trials/ 44 longitudinal studies/ 45 exp program evaluation/ 46 treatment effectiveness evaluation/ 47 random$.tw. 48 (allocat$ or assign$).tw. 49 ((clinic$ or control$) adj trial$).tw. 50 ((control$ or experiment$ or intervention$) adj3 group$).tw. 51 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 52 (crossover$ or "cross over$").tw. 53 (placebo$ or (usual adj1 treatment$) or wait$ list).tw. 54 prospectiv$.tw. 55 (crossover or cross‐over).tw. 56 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 57 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw. 58 or/43‐57 59 42 and 58 60 limit 59 to yr="1990 ‐Current"
CINAHL EBSCO
Searched 28 October 2016 [1355 records]
1 (MH "Hardiness") 2 (MH "Social Adjustment") 3 (MH "Adaptation, Psychological") 4 TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") 5 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) 6 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) 7 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) 8 (MH "Coping") 9 TI (cope OR coping) OR AB (cope OR coping) 10 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 11 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 12 (MH "Psychotherapy+") 13 (MH "Stress, Psychological/TH") 14 TI (psychotherap* OR psychotherap*) OR AB (psychotherap* OR psychotherap*) 15 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) 16 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 17 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) 18 TI relaxation OR AB relaxation 19 TI mindful* OR AB mindful* 20 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) 21 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) 22 TI "cognit* restructur*" OR AB "cognit* restructur*" 23 TI "positive psychology" OR AB "positive psychology" 24 TI (refram* OR refram* OR reapprais*) OR AB (refram* OR refram* OR reapprais*) 25 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 26 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) 27 TI "acceptance and commitment" OR AB "acceptance and commitment" 28 (MH "Combined Modality Therapy") 29 TI (multimodal OR multimodal OR "combined modal*") OR AB (multimodal OR multimodal OR "combined modal*") 30 (MH "Health Promotion+") 31 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) 32 S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 33 S11 AND S32 34 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 35 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 36 S33 S34 OR S35 37 PT randomized controlled trial 38 TI "randomi?ed control* trial*" OR AB "randomi?ed control* trial*" 39 TI "control* clinical trial*" OR AB "control* clinical trial*" 40 AB randomi?ed 41 AB placebo* 42 AB randomly 43 AB trial 44 S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 45 S36 AND S44 46 S36 AND S44, Limiters Published Date: 1990010120161031
PSYNDEX EBSCO
Searched 27 October 2016 [156 records]
1 DE "Resilience (Psychological)" 2 DE "Emotional Adjustment" OR DE "Social Adjustment" 3 DE "Posttraumatic Growth" 4 TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR SU ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 5 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) OR SU (positiv* N1 (adapt* OR adjust*)) 6 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) OR SU (psychol* N1 (adapt* OR adjust*)) 7 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) OR SU (resilien* OR hardiness*) 8 DE "Coping Behavior" 9 TI (cope OR coping) OR AB (cope OR coping) OR SU (cope OR coping) 10 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR SU ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 11 DE "Psychological Stress" 12 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 13 DE "Psychotherapy" OR DE "Adlerian Psychotherapy" OR DE "Adolescent Psychotherapy" OR DE "Affirmative Therapy" OR DE "Analytical Psychotherapy" OR DE "Autogenic Training" OR DE "Behavior Therapy" OR DE "Brief Psychotherapy" OR DE "Brief Relational Therapy" OR DE "Child Psychotherapy" OR DE "Client Centered Therapy" OR DE "Cognitive Behavior Therapy" OR DE "Conversion Therapy" OR DE "Eclectic Psychotherapy" OR DE "Emotion Focused Therapy" OR DE "Existential Therapy" OR DE "Experiential Psychotherapy" OR DE "Expressive Psychotherapy" OR DE "Eye Movement Desensitization Therapy" OR DE "Feminist Therapy" OR DE "Geriatric Psychotherapy" OR DE "Gestalt Therapy" OR DE "Group Psychotherapy" OR DE "Guided Imagery" OR DE "Humanistic Psychotherapy" OR DE "Hypnotherapy" OR DE "Individual Psychotherapy" OR DE "Insight Therapy" OR DE "Integrative Psychotherapy" OR DE "Interpersonal Psychotherapy" OR DE "Logotherapy" OR DE "Narrative Therapy" OR DE "Network Therapy" OR DE "Persuasion Therapy" OR DE "Primal Therapy" OR DE "Psychoanalysis" OR DE "Psychodrama" OR DE "Psychodynamic Psychotherapy" OR DE "Psychotherapeutic Counseling" OR DE "Rational Emotive Behavior Therapy" OR DE "Reality Therapy" OR DE "Relationship Therapy" OR DE "Solution Focused Therapy" OR DE "Supportive Psychotherapy" OR DE "Transactional Analysis" OR DE Individualpsychologische Therapie" OR DE "Jugendlichenpsychotherapie" OR DE "Affirmative Therapie" OR DE "Analytische Psychotherapie (C. G. Jung)" OR DE "Autogenes Training" OR DE "Verhaltenstherapie" OR DE "Kurzpsychotherapie" OR DE "Beziehungsorientierte Kurzpsychotherapie" OR DE "Kinderpsychotherapie" OR DE "Klientenzentrierte Psychotherapie" OR DE "Kognitive Verhaltenstherapie" OR DE "Konversionstherapie (Homosexualität)" OR DE "Eklektische Psychotherapie" OR DE "Emotionsfokussierte Therapie" OR DE "Existenzialtherapie" OR DE "Erfahrungsorientierte Psychotherapie" OR DE "Expressive Psychotherapie" OR DE "Augenbewegungsdesensibilisierung" OR DE "Feministische Therapie" OR DE "Geriatrische Psychotherapie" OR DE "Gestalttherapie" OR DE "Gruppenpsychotherapie" OR DE "Geleitete Fantasievorstellung" OR DE "Humanistische Psychotherapie" OR DE "Hypnotherapie" OR DE "Einzelpsychotherapie" OR DE "Einsichtstherapie" OR DE "Integrative Psychotherapie" OR DE "Interpersonelle Psychotherapie" OR DE "Logotherapie" OR DE "Narrative Therapie" OR DE "Netzwerktherapie" OR DE "Persuasionstherapie" OR DE "Primärtherapie" OR DE "Psychoanalytische Therapie" OR DE "Psychodrama" OR DE "Psychodynamische Psychotherapie" OR DE "Psychotherapeutische Beratung" OR DE "Rational‐Emotive Verhaltenstherapie" OR DE "Realitätstherapie" OR DE "Relationship Therapy" OR DE "Lösungsorientierte Therapie" OR DE "Unterstützende Psychotherapie" OR DE "Transaktionsanalyse" 14 TI (psychotherap* OR psycho‐therap*) OR AB (psychotherap* OR psycho‐therap*) OR SU (psychotherap* OR psychotherap*) 15 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) 16 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR SU ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 17 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) OR SU (psycho* N3 (intervention* OR program* OR therap*)) 18 TI relaxation OR AB relaxation OR SU relaxation 19 TI mindful* OR AB mindful* OR SU mindful* 20 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) OR SU (counsel?ing OR coaching) 21 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) OR SU ("third wave" N1 (psycho* OR therap*)) 22 TI "cognit* restructur*" OR AB "cognit* restructur*" OR SU "cognit* restructur*" 23 TI "positive psychology" OR AB "positive psychology" OR SU "positive psychology" 24 TI (refram* OR re‐fram* OR reapprais*) OR AB (refram* OR re‐fram* OR reapprais*) OR SU (refram* OR re‐fram* OR reapprais*) 25 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR SU (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 26 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) OR SU (anxiety N3 manage*) 27 TI "acceptance and commitment" OR AB "acceptance and commitment" OR SU "acceptance and commitment" 28 TI (multimodal OR multi‐modal OR "combined modal*") OR AB (multimodal OR multi‐modal OR "combined modal*") OR SU (multimodal OR multi‐modal OR "combined modal*") 29 DE "Health Promotion" 30 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) OR SU (health N3 (educat* OR promot*)) 31 S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 32 S12 AND S31 33 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR SU (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 34 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR SU (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 35 S32 OR S33 OR S34 36 TI "randomi?ed control* trial*" OR AB "randomi?ed control* trial*" 37 TI "control* clinical trial*" OR AB "control* clinical trial*" 38 AB randomi?ed 39 AB placebo* 40 AB randomly 41 AB trial 42 S36 OR S37 OR S38 OR S39 OR S40 OR S41 43 S35 AND S42
Web of Science Core Collection (SCI, SSCI, CPCI‐S, CPCI‐SSH)
Searched 1990 to 2 November 2016 [2812 records]
# 19 #17 AND #16 Refined by: WEB OF SCIENCE CATEGORIES: ( PSYCHIATRY OR PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH OR PSYCHOLOGY CLINICAL OR PSYCHOLOGY MULTIDISCIPLINARY OR PSYCHOLOGY OR PSYCHOLOGY DEVELOPMENTAL OR NURSING OR SOCIAL WORK OR EDUCATION EDUCATIONAL RESEARCH ) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 18 #17 AND #16 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 17 TS=(random* or trial* or assign* or control* or group* or placebo* or blind* or prospectiv* or longitudinal* or meta‐analys* or systematic review*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 16 #14 or #15 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 15 TS=((resilience or hardiness) near/3 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 14 #13 AND #6 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 13 #12 OR #11 OR #10 OR #9 OR #8 OR #7 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 12 TS=(health near/3 (educat* or promot*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 11 TS= ((multimodal* or "multi modal*" or "combined modal*") NEAR/3 (treat* or therap* or intervention* or program*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 10 TS=("acceptance and commitment") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 9 TS=((anxiety near/1 manag*) or relaxation or mindful* or counsel*ing or coaching or "third wave" or refram* or "re fram*" or "cognitive restructur*" or "positive psychology") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 8 TS=(stress near/3 (inoculat* or manag* or reduc* or resist*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 7 TS=((psychotherap* or "psycho therap*") or CBT or mindful* or (behav* near/3 (intervention* or program* or therap*)) OR ((cognit* or "cognitive behavior*" or CBT) near/3 (intervention* or program* or therap*)) OR (psycho* near/3 (intervention* or program* or therap*))) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 6 #5 OR #4 OR #3 OR #2 OR #1 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 5 TS= ((withstand* or overcom* or resist* or recover* or thriv* or adapt* or adjust* or "bounc* back" ) near/1 (stress* or trauma* or advers*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 4 TS=(psychol* near/1 (adapt* or adjust*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 3 TS=(positiv* near/1 (adapt* or adjust*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 2 TS=("post traumatic growth" or "posttraumatic growth" or "stress related growth") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 1 TS=(resilien* or hardiness*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016
International Bibliography of the Social Sciences (IBSS) PROQUEST
Searched 3 November 2016 [593 records]
((MAINSUBJECT.EXACT("Coping") OR TI(resilien* OR hardiness) OR AB(resilien* OR hardiness)) OR (TI((psychol* OR social) NEAR/1 (adapt* OR adjust*)) OR AB((psychol* OR social) NEAR/1 (adapt* OR adjust*))) OR (TI(positiv* NEAR/1 (adapt* OR adjust*)) OR AB(positiv* NEAR/1 (adapt* OR adjust*))) OR (TI("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (TI(cope OR coping) OR AB(cope OR coping)) OR (TI((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") NEAR/5 (stress* OR trauma* OR adversit*)) OR AB((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") NEAR/5 (stress* OR trauma* OR adversit*)))) AND ((MAINSUBJECT.EXACT("Psychotherapy") OR MAINSUBJECT.EXACT("Cognitive therapy") OR MAINSUBJECT.EXACT("Group therapy") OR TI(psychotherap* OR psycho‐therap*) OR AB(psychotherap* OR psycho‐therap*) OR TI(behav* NEAR/3 (intervention* OR program* OR therap*)) OR AB(behav* NEAR/3 (intervention* OR program* OR therap*)) OR TI(cognit* OR "cognitive behavior*" OR CBT) OR AB(cognit* OR "cognitive behavior*" OR CBT) OR TI(psycho* NEAR/3 (intervention* OR program* OR therap*)) OR AB(psycho* NEAR/3 (intervention* OR program* OR therap*)) OR TI(relaxation OR mindful* OR counsel?ing OR coaching OR "third wave") OR AB(relaxation OR mindful* OR counsel?ing OR coaching OR "third wave") OR TI(cognit* NEAR/1 restructur*) OR AB(cognit* NEAR/1 restructur*) OR TI("positive psychology") OR AB("positive psychology")) AND yr(1960‐2019)) AND (MAINSUBJECT.EXACT("Clinical trials") OR (TI(control* OR group OR random* OR placebo* OR longitudinal OR prospective* OR blind* OR trial*) OR AB(control* OR group OR random* OR placebo* OR longitudinal OR prospective* OR blind* OR trial*))) Limited to 1990 to 2016
Applied Social Sciences Index & Abstracts ProQuest (ASSIA) PROQUEST
Searched 28 October 2016 [634 records]
1 SU.EXACT("Resilience") 2 SU.EXACT("Hardiness") 3 SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment") 4 SU.EXACT("Adaptation") 5 ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 6 ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) 7 ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) 8 ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) 9 ti(cope OR coping) OR ab(cope OR coping) 10 ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) 11 SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress") 12 SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress") 13 SU.EXACT("Psychotherapy") 14 ti((psychotherap* OR psychotherap*)) OR ab((psychotherap* OR psychotherap*)) 15 ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) 16 ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) 17 ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) 18 ti(relaxation) OR ab(relaxation) 19 ti(mindful*) OR ab(mindful*) 20 ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) 21 ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*))) 22 ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) 23 ti(("positive psychology")) OR ab(("positive psychology")) 24 ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) 25 ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) 26 ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) 27 ti("acceptance and commitment") OR ab("acceptance and commitment") 28 ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) 29 SU.EXACT("Health promotion" OR "Mental health promotion") 30 ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) 31 SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*)))) 32 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))))) 33 ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 34 ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 35 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 36 ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*) 37 ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*) 38 ti(randomi?ed) OR ab(randomi?ed) 39 ti(placebo*) OR ab(placebo*) 40 ti(randomly) OR ab(randomly) 41 ti(trial) OR ab(trial) 42 (ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)) 43 ((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) 44 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) AND pd(19900101‐20161231)
ProQuest Dissertations & Theses (PQDT) PROQUEST
Searched 28 October 2016 [989 records]
1 SU.EXACT("Resilience") 2 SU.EXACT("Hardiness") 3 SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment") 4 SU.EXACT("Adaptation") 5 ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 6 ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*))) 7 ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*))) 8 ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*) 9 ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping) 10 ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) 11 SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress") 12 SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress") 13 SU.EXACT("Psychotherapy") 14 ti((psychotherap* OR psychotherap*)) OR ab((psychotherap* OR psychotherap*)) 15 ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*))) 16 ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) 17 ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*))) 18 ti(relaxation) OR ab(relaxation) OR diskw(relaxation) 19 ti(mindful*) OR ab(mindful*) OR diskw(mindful*) 20 ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching 21 ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*))) 22 ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*)) 23 ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology")) 24 ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*)) 25 ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) 26 ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*)) 27 ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment") 28 ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*")) 29 SU.EXACT("Health promotion" OR "Mental health promotion") 30 ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))) 31 SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*)))) 32 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))))) 33 ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 34 ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 35 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 36 ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*) 37 ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*) 38 ti(randomi?ed) OR ab(randomi?ed) 39 ti(placebo*) OR ab(placebo*) 40 ti(randomly) OR ab(randomly) 41 ti(trial) OR ab(trial) 42 (ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)) 43 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial) 44 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) AND pd(19900101‐20161231
Cochrane Database of Systematic Reviews (CDSR)
Searched 27 October 2016 [57 records]
#1(resilien* or hardiness*):ti,ab #2(post next traumatic growth or posttraumatic growth or stress next related growth) #3(positiv* near/1 (adapt* or adjust*)):ti,ab #4(psychol* near/1 (adapt* or adjust*)):ti,ab #5{or #1‐#4} #6(behav* or psycho* or cbt or cognit* or mindful* or reframe* or re next fram*):ti,ab #7(stress near/3 (inoculat* or manag* or reduc* or resist*)):ti,ab #8(anxiety near/3 manag*):ti,ab #9"acceptance and commitment":ti,ab #10(multimodal* or multi next modal* or combined next modal*):ti,ab #11(health near/3 (educat* or promot*)):ti,ab #12{or #6‐#11} Publication Year from 1990 to 2016, in Cochrane Reviews (Reviews and Protocols) #13#5 and #12
Database of Abstracts of Reviews of Effects (DARE)
Searched 27 October 2016 [3 records]
#1(resilien* or hardiness*):ti,ab #2(post next traumatic growth or posttraumatic growth or stress next related growth) #3(positiv* near/1 (adapt* or adjust*)):ti,ab #4(psychol* near/1 (adapt* or adjust*)):ti,ab #5{or #1‐#4} #6(behav* or psycho* or cbt or cognit* or mindful* or reframe* or re next fram*):ti,ab #7(stress near/3 (inoculat* or manag* or reduc* or resist*)):ti,ab #8(anxiety near/3 manag*):ti,ab #9"acceptance and commitment":ti,ab #10(multimodal* or multi next modal* or combined next modal*):ti,ab #11(health near/3 (educat* or promot*)):ti,ab #12{or #6‐#11} Publication Year from 1990 to 2016, in Other Reviews #13#5 and #12
Epistemonikos (epistemonikos.org)
Searched 28 October 2016 [173 records]
1 (title:(resilien* OR hardiness*) OR abstract:(resilien* OR hardiness*)) 2 (title:("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR abstract:("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) 3 (title:("positive adaptation" OR "positive adjustment") OR abstract:("positive adaptation" OR "positive adjustment")) 4 (title:("psychological adaptation" OR "psychological adjustment") OR abstract:("psychological adaptation" OR "psychological adjustment")) 5 OR/#1‐#4 6 #5; Publication year (Custom year range): 1990 – 2016; Publication type: Systematic Review; Systematic review question: All; Cochrane review: All; Type of meta‐analysis: All
ERIC EBSCO
Searched 28 October 2016 [206 records]
1 DE "Resilience (Psychology)" 2 DE "Social Adjustment" OR DE "Emotional Adjustment" 3 TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") 4 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) 5 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) 6 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) OR SU (resilien* 7 TI (cope OR coping) OR AB (cope OR coping) OR SU (cope OR coping) 8 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 9 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 10 DE "Psychotherapy" OR DE "Milieu Therapy" OR DE "Relaxation Training" 11 TI (psychotherap* OR psychotherap*) OR AB (psychotherap* OR psychotherap*) OR SU (psychotherap* OR psychotherap*) 12 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) 13 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 14 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) 15 TI relaxation OR AB relaxation OR SU relaxation 16 TI mindful* OR AB mindful* 17 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) OR SU (counsel?ing OR coaching) 18 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) 19 TI "cognit* restructur*" OR AB "cognit* restructur*" OR SU "cognit* restructur*" 20 TI "positive psychology" OR AB "positive psychology" 21 TI (refram* OR refram* OR reapprais*) OR AB (refram* OR refram* OR reapprais*) 22 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR SU (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 23 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) 24 TI "acceptance and commitment" OR AB "acceptance and commitment" 25 TI (multimodal OR multimodal OR "combined modal*") OR AB (multimodal OR multimodal OR "combined modal*") 26 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) OR SU (health N3 (educat* OR promot*)) 27 S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 28 S9 AND S27 29 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 30 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 31 S28 OR S29 OR S30 32 TI "randomi?ed control* trial*" OR AB "randomi? ed control* trial*" 33 TI "control* clinical trial*" OR AB "control* clinical trial*" 34 AB randomi?ed 35 AB placebo* 36 AB randomly 37 AB trial 38 S32 OR S33 OR S34 OR S35 OR S36 OR S37 39 S31 AND S38 40 S31 AND S38, Limiters Date Published:1990010120161031
Current Controlled Trials (ISRCTN registry; http://www.isrctn.com)
Searched 24 November 2016 [47 records]
Text search: (((resilience OR hardiness OR "posttraumatic growth" OR stress OR trauma) AND (psychotherap OR relaxation OR mindfulness OR coaching OR "positive psychology" OR reappraisal OR "stress inoculation" OR "stress management" OR multimodal OR "health promotion")) OR ((resilience OR hardiness) AND (training OR program OR intervention OR promot OR prevent OR enhanc OR learn OR teach OR educat OR increas or develop OR manag OR therap OR protocol OR treat)))
ClinicalTrials.gov (clinicaltrials.gov)
Searched 24 November 2016 [675 records]
title = resilience OR hardiness OR posttraumatic growth OR stress OR trauma condition = resilience OR hardiness OR posttraumatic growth OR stress OR trauma intervention = resilience training OR hardiness training OR psychotherapy OR relaxation OR mindfulness OR coaching OR positive psychology OR reappraisal OR stress inoculation OR stress management OR multimodal OR health promotion Limitation: 01/01/1990 – 03/11/2016
WHO ICTRP (apps.who.int/trialsearch)
Searched 24 November 2016 [879 records]
title = resilience OR hardiness OR posttraumatic growth OR stress OR trauma condition = resilience OR hardiness OR posttraumatic growth OR stress OR trauma intervention = resilience training OR hardiness training OR psychotherapy OR relaxation OR mindfulness OR coaching OR positive psychology OR reappraisal OR stress inoculation OR stress management OR multimodal OR health promotion Recruitment status: ALL Limitation: 01/01/1990 – 03/11/2016
Appendix 9. Search strategies 2016 onwards
Cochrane Central Register of Controlled Trials (CENTRAL)
Searched 26 June 2019 [218 records]
#1 [mh "Resilience, Psychological"] #2 [mh "social adjustment"] #3 [mh "Adaptation, Psychological"] #4 ("post‐traumatic growth" or "posttraumatic growth" or "stress‐related growth") #5 (positiv* near/1 (adapt* or adjust*)) #6 (psychol* near/1 (adapt* or adjust*)) #7 (resilien* or hardiness*) #8 (cope or coping) #9 ((withstand* or overcom* or resist* or recover* or thriv* or adapt* or adjust* or bounc* back) near/5 (stress* or trauma* or adversit*)) #10 {or #1‐#9} #11 [mh psychotherapy] #12 MeSH descriptor: [Stress, Psychological] this term only and with qualifier(s): [therapy ‐ TH] #13 (psychotherap* or psycho next therap*) #14 (behav* near/3 (intervention* or program* or therap*)) #15 ((cognit* or cognitive next behavior* or CBT) near/3 (intervention* or program* or therap*)) #16 (psycho* near/3 (intervention* or program* or therap*)) #17 relaxation #18 mindful* #19 (counsel*ing or coaching) #20 (third next wave next (psycho* or therap*)) #21 cognit* next restructur* #22 positive next psychology #23 (refram* or re next fram* or reapprais*) #24 (stress near/1 (inoculation or manag* or reduc* or resist*)) #25 (anxiety near/3 manage*) #26 "acceptance and commitment" #27 [mh "Combined Modality Therapy"] #28 (multimodal* or multi next modal* or combined modal*) #29 [mh "Health promotion"] #30 (health near/3 (educat* or promot*)) #31 {or #11‐#30} #32 MeSH descriptor: [Health Personnel] explode all trees #33 (health* NEAR/3 (personnel or profession* or worker* or practitioner* or provider* or staff)) #34 (medical NEAR/3 (personnel or profession* or worker* or practitioner* or provider* or staff)) #35 (care* NEAR/1 (personnel or profession* or worker* or practitioner* or provider* or staff)) #36 (doctor* or physician* or general practitioner* or ("primary care" NEAR/2 practitioner*) or surgeon*) #37 (nurse* or nursing) #38 ((hospital or ambulance) NEAR/1 (staff or personnel)) #39 ((intensive NEAR/2 care) or ICU) #40 ((allied NEXT health*) NEAR/2 (personnel* or profession* or worker* or practitioner* or provider* or staff)) #41 (psychologist* or psychotherapist* or psychiatrist* or mental NEXT health NEXT clinician* or mental NEXT health NEXT profession* or mental NEXT health NEXT worker* or social NEXT worker*) #42 (paramedic* or para NEXT medic* or ambulance ) #43 (first or emergency or disaster) NEAR/1 (response or responder*) #44 (professional NEAR/1 (caregiver* or care‐giver*)) #45 (anesthetist* or anaesthetist* or audiologist* or dental NEXT hygienist* or dentist* or dietitian* or midwi*e* or nutritionist* or pathologist* or physiologist* or physiotherapist* or therapist or osteopath* or sonographer* or radiographer* or radiotherapist* or ((radiology or radiation) NEAR/1 ( technician* or technologist* or assistant* or scientist*)) or ((anesthesia or anesthesiologist) NEAR/1 (technician* or assistant*)) or (surgical NEAR/1 (technician* or technologist*)) or orthotist* or orthoptist* or podiatrist* or perfusionist*) #46 (counsellor* or counselor*) #47 ((clinical or medical*) NEAR/1 (technician* or technologist* or assistant* or scientist*)) #48 (public NEXT health NEXT service* or public NEXT health NEXT agenc*) #49 (secondary NEXT trauma* or (work* NEAR/2 trauma NEXT survivor*)) #50 ((nursing or medical or midwifery or premedical or paramedic or psychology or physical NEXT therapy or occupational NEXT therapy) NEAR/2 student*) #51 college NEXT student* #52 {OR #32‐#51} #53 #10 and #31 with Publication Year from 1990 to 2016, in Trials [ Note: Final line 2016] #54 #10 and #31 AND #52 with Publication Year from 2016 to 2019, in Trials [ Note: Final line 2019]
MEDLINE OVID
Searched 25 June 2019 [725 records]
1 Resilience, Psychological/ 2 social adjustment/ 3 Adaptation, Psychological/ 4 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw,kf. 5 (positiv$ adj1 (adapt$ or adjust$)).tw,kf. 6 (psychol$ adj1 (adapt$ or adjust$)).tw,kf. 7 (resilien$ or hardiness$).tw,kf. 8 (cope or coping).tw,kf. 9 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj5 (stress$ or trauma$ or adversit$)).tw,kf. 10 or/1‐9 11 exp psychotherapy/ 12 Stress, Psychological/th 13 (psychotherap$ or psycho‐therap$).tw,kf. 14 (behav$ adj3 (intervention$ or program$ or therap$)).tw,kf. 15 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw,kf. 16 (psycho$ adj3 (intervention$ or program$ or therap$)).tw,kf. 17 relaxation.tw,kf. 18 mindful$.tw,kf. 19 (counsel?ing or coaching).tw,kf. 20 (third wave adj (psycho$ or therap$)).tw,kf. 21 cognit$ restructur$.tw,kf. 22 positive psychology.tw,kf. 23 (refram$ or re‐fram$ or reapprais$).tw,kf. 24 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw,kf. 25 (anxiety adj3 manage$).tw,kf. 26 "acceptance and commitment ".tw,kf. 27 Combined Modality Therapy/ 28 (multimodal or multi‐modal or combined modal$).tw,kf. 29 exp Health promotion/ 30 (health adj3 (educat$ or promot$)).tw,kf. 31 or/11‐30 32 10 and 31 33 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kf. 34 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kf. 35 or/32‐34 36 randomized controlled trial.pt. 37 controlled clinical trial.pt. 38 randomi#ed.ab. 39 placebo$.ab. 40 drug therapy.fs. 41 randomly.ab. 42 trial.ab. 43 groups.ab. 44 or/36‐43 45 exp animals/ not humans.sh. 46 44 not 45 47 35 and 46 48 Health personnel/ 49 (health$ adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kf. 50 ((medical care adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)) or (medical adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff))).tw,kf. 51 (care adj1 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kf. 52 (doctor$ or physician$ or general practitioner$ or (primary care adj2 practitioner$) or surgeon$).tw,kf. 53 (nurse$ or (nursing adj3 assistant$) or (nursing adj3 staff)).tw,kf. 54 nursing.tw,kf. 55 ((hospital or ambulance) adj1 personnel).tw,kf. 56 ((intensive adj2 care) or ICU or (intensive adj2 care adj2 unit adj3 personnel$)).tw,kf. 57 ((allied health$) adj2 (personnel or profession$ or worker$ or practitioner* or provider$ or staff)).tw,kf. 58 (psychologist$ or psychotherapist$ or psychiatrist$ or (mental health adj2 clinician$) or (mental health adj2 profession$) or (mental health adj2 worker$)).tw,kf. 59 (social worker$).tw,kf. 60 (paramedic$ or ambulance or medic$ or ((first or emergency or disaster) adj1 (response or responder$))).tw,kf. 61 (professional adj1 (caregiver$ or care‐giver$)).tw,kf. 62 ((physical therapist$) or physiotherapist$ or occupational therapist$ or recreational therapist$ or music therapist$ or art therapist$ or dietitian$ or nutritionist$ or ((speech and language) adj1 therapist$) or speech pathologist$ or audiologist$ or exercise physiologist$ or osteopath$ or sonographer$ or radiographer$ or radiotherapist$ or ((radiology or radiation) adj1 (therapist$ or technician$ or technologist$ or assistant$ or scientist$)) or respiratory therapist$ or ((anesthesia or anesthesiologist) adj1 (technician$ or assistant$)) or dental hygienist$ or (surgical adj1 (technician$ or technologist$)) or orthotist$ or orthoptist$ or podiatrist$ or perfusionist$).tw,kf. 63 counsel?or$.tw,kf. 64 ((clinical or clinical laboratory or medical$ or medical$ laboratory) adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kf. 65 ((human or health) adj1 service adj3 profession$).tw,kf. 66 (public health adj2 (service or agency)).tw,kf. 67 (secondary traumati?ation or (work$ adj2 (trauma survivor$))).tw,kf. 68 ((nursing or medical or premedical or paramedic or psychology or physical therapy or occupational therapy) adj2 student$).tw,kf. 69 (college adj2 student$).tw,kf. 70 ((nurs$ adj1 (graduate$ or education)) or (medic$ adj1 train$) or (student adj1 nurse$)).tw,kf. 71 or/48‐70 72 47 and 71 73 limit 72 to yr="1990 ‐Current" 74 limit 73 to yr="2016 ‐Current"
Embase Ovid
Searched 25 June 2019 [991 records]
1 exp coping behavior/ 2 psychological adjustment/ 3 Psychological resilience/ [Annotation: New Emtree term in 2017] 4 social adaptation/ 5 "personal resource"/ 6 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw,kw. 7 (positiv$ adj1 (adapt$ or adjust$)).tw,kw. 8 (psychol$ adj1 (adapt$ or adjust$)).tw,kw. 9 (resilien$ or hardiness$).tw,kw. 10 (cope or coping).tw,kw. 11 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj5 (stress$ or trauma$ or advers$)).tw,kw. 12 or/1‐11 13 exp psychotherapy/ 14 posttraumatic stress disorder/th [Therapy] 15 mental stress/th [Therapy] 16 (psychotherap$ or psycho‐therap$).tw,kw. 17 (behav$ adj3 (intervention$ or program$ or therap$)).tw,kw. 18 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw,kw. 19 (psycho$ adj3 (intervention$ or program$ or therap$)).tw,kw. 20 mindful$.tw,kw. 21 exp counseling/ 22 (counsel?ing or coaching).tw,kw. 23 mindfulness/ 24 mindful$.tw,kw. 25 (third wave adj (psycho$ or therap$)).tw,kw. 26 cognit$ restructur$.tw,kw. 27 positive psychology.tw,kw. 28 (refram$ or re‐fram$ or reapprais$).tw,kw. 29 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw,kw. 30 (anxiety adj3 manage$).tw,kw. 31 "acceptance and commitment ".tw,kw. 32 (multimodal$ or multi‐modal$ or combined modal$).tw,kw. 33 exp health promotion/ 34 (health adj3 (educat$ or promot$)).tw,kw. 35 or/13‐34 36 12 and 35 37 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kw. 38 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kw. 39 or/36‐38 40 exp health care personnel/ 41 (health$ adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kw. 42 (medical adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kw. 43 (care adj1 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kw. 44 (doctor$ or physician$ or general practitioner$ or (primary care adj2 practitioner$) or surgeon$).tw,kw. 45 (nurse$1 or nursing).tw,kw. 46 ((hospital or ambulance) adj1 personnel).tw,kw. 47 ((intensive adj2 care) or ICU).tw,kw. 48 (allied health$ adj2 (personnel$ or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kw. 49 (psychologist$ or psychotherapist$ or psychiatrist$ or mental health clinician$ or mental health profession$ or mental health worker$).tw,kw. 50 social worker$.tw,kw. 51 (paramedic$ or ambulance or medic$).tw,kw. 52 ((first or emergency or disaster) adj1 (response or responder$)).tw,kw. 53 (professional adj (caregiver$ or care‐giver$)).tw,kw. 54 (physical therapist$ or physiotherapist$ or occupational therapist$ or recreational therapist$ or music therapist$ or art therapist$ or dietitian$ or nutritionist$ or ((speech and language) adj1 therapist$) or speech pathologist$ or audiologist$ or exercise physiologist$ or osteopath$ or sonographer$ or radiographer$ or radiotherapist$ or ((radiology or radiation) adj1 (therapist$ or technician$ or technologist$ or assistant$ or scientist$)) or respiratory therapist$ or ((anesthesia or anesthesiologist) adj1 (technician$ or assistant$)) or dental hygienist$ or (surgical adj1 (technician$ or technologist$)) or orthotist$ or orthoptist$ or podiatrist$ or perfusionist$).tw,kw. 55 counsel?or$.tw,kw. 56 (clinical adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kw. 57 (clinical laboratory adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kw. 58 (medical$ adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kw. 59 (medical$ laboratory adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kw. 60 (public health service$ or public health agenc$).tw,kw. 61 (secondary traumati?ation or (work$ adj2 trauma survivor$)).tw,kw. 62 ((nursing or medical or premedical or paramedic or psychology or physical therapy or occupational therapy) adj2 student$).tw,kw. 63 college student$.tw,kw. 64 ((nurs$ adj1 graduate$) or (nurs$ adj1 education) or (medic$ adj1 train$)).tw,kw. 65 or/40‐64 66 39 and 65 67 Randomized controlled trial/ 68 controlled clinical trial/ 69 Single blind procedure/ 70 Double blind procedure/ 71 triple blind procedure/ 72 Crossover procedure/ 73 (crossover or cross‐over).tw. 74 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 75 Placebo/ 76 placebo.tw. 77 prospective.tw. 78 factorial$.tw. 79 random$.tw. 80 assign$.ab. 81 allocat$.tw. 82 volunteer$.ab. 83 or/67‐82 84 66 and 83 85 limit 84 to yr="2016 ‐Current"
PsycINFO Ovid
Searched 26 June 2019 [454 records]
All years searched in 2019 to correct for possible errors in the 2016 search
1 "resilience (psychological)"/ 2 "adaptability (personality)"/ 3 emotional adjustment/ 4 coping behavior/ 5 posttraumatic growth/ 6 protective factors/ 7 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw. 8 (positiv$ adj1 (adapt$ or adjust$)).tw. 9 (psychol$ adj1 (adapt$ or adjust$)).tw. 10 (resilien$ or hardiness$).tw. 11 (cope or coping).tw. 12 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj3 (stress$ or trauma$ or advers$)).tw. 13 or/1‐12 14 exp psychotherapy/ ) 15 exp cognitive techniques/ 16 psychotherapeutic techniques/ 17 relaxation therapy/ 18 mindfulness/ 19 stress management/ 20 (psychotherap$ or psycho‐therap$).tw. 21 (behav$ adj3 (intervention$ or program$ or therap$)).tw. 22 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw. 23 (psycho$ adj3 (intervention$ or program$ or therap$)).tw. 24 relaxation.tw. 25 mindful$.tw. 26 (counsel?ing or coaching).tw. 27 (third wave adj (psycho$ or therap$)).tw. 28 cognit$ restructur$.tw. 29 positive psychology.tw. 30 (refram$ or re‐fram$ or reapprais$).tw. 31 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw. 32 (anxiety adj3 manage$).tw. 33 "acceptance and commitment".tw. 34 multimodal treatment approach/ 35 (multimodal$ or multi‐modal$ or combined modal$).tw. 36 health promotion/ 37 (health adj3 (educat$ or promot$)).tw. 38 or/14‐37 39 13 and 38 40 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw. 41 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw. 42 or/39‐41 43 exp health personnel/ 44 exp therapists/ 45 exp clinicians/ 46 exp counselors/ 47 home care personnel/ 48 professional measures/ 49 rescue workers/ 50 exp social workers/ 51 (health$ adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw. 52 (medical adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw. 53 (care adj1 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw. 54 (doctor$ or physician$ or general practitioner$ or (primary care adj2 practitioner$) or surgeon$).tw. 55 (nurse$1 or nursing).tw. 56 ((hospital or ambulance) adj1 personnel).tw. 57 ((intensive adj2 care) or ICU).tw. 58 (allied health$ adj2 (personnel$ or profession$ or worker$ or practitioner$ or provider$ or staff)).tw. 59 (psychologist$ or psychotherapist$ or psychiatrist$ or mental health clinician$ or mental health profession$ or mental health worker$).tw. 60 social worker$.tw. 61 (paramedic$ or ambulance or medic$).tw. 62 ((first or emergency or disaster) adj1 (response or responder$)).tw. 63 (professional adj (carer$ or caregiver$ or care‐giver$)).tw. 64 (physical therapist$ or physiotherapist$ or occupational therapist$ or recreational therapist$ or music therapist$ or art therapist$ or dietitian$ or nutritionist$ or ((speech and language) adj1 therapist$) or speech pathologist$ or audiologist$ or exercise physiologist$ or midwi?e$ or osteopath$ or sonographer$ or radiographer$ or radiotherapist$ or ((radiology or radiation) adj1 (therapist$ or technician$ or technologist$ or assistant$ or scientist$)) or respiratory therapist$ or ((anesthesia or anesthesiologist) adj1 (technician$ or assistant$)) or dental hygienist$ or (surgical adj1 (technician$ or technologist$)) or orthotist$ or orthoptist$ or podiatrist$ or perfusionist$).tw. 65 counsel?or$.tw. 66 (clinical adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw. 67 (clinical laboratory adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw. 68 (medical$ adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw. 69 (medical$ laboratory adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw. 70 (public health service$ or public health agenc$).tw. 71 (secondary trauma$ or (work$ adj2 trauma survivor$)).tw. 72 ((nursing or medical or premedical or paramedic or psychology or physical therapy or occupational therapy) adj2 student$).tw. 73 ((nursing or medical or midwifery or premedical or paramedic or psychology or physical therapy or occupational therapy) adj2 student$).tw. 74 college student$.tw. (154347) 75 ((nurs$ adj1 graduate$) or (nurs$ adj1 education) or (medic$ adj1 train$)).tw. (7743) 76 or/43‐75 77 42 and 76 78 clinical trials/ 79 longitudinal studies/ 80 exp program evaluation/ 81 treatment effectiveness evaluation/ 82 random$.tw. 83 (allocat$ or assign$).tw. 84 ((clinic$ or control$) adj trial$).tw. 85 ((control$ or experiment$ or intervention$) adj3 group$).tw. 86 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 87 (crossover$ or "cross over$").tw. 88 (placebo$ or (usual adj1 treatment$) or wait$ list).tw. 89 prospectiv$.tw. 90 (crossover or cross‐over).tw. 91 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 92 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw. 93 or/78‐92 94 77 and 93 95 limit 94 to yr="2016 ‐Current"
CINAHL EBSCO
Searched 24 June 2019 [476 records]
1 (MH "Hardiness") 2 (MH "Social Adjustment") 3 (MH "Adaptation, Psychological") 4 TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") 5 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) 6 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) 7 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) 8 (MH "Coping") 9 TI (cope OR coping) OR AB (cope OR coping) 10 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 11 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 12 (MH "Psychotherapy+") 13 (MH "Stress, Psychological/TH") 14 TI (psychotherap* OR psychotherap*) OR AB (psychotherap* OR psychotherap*) 15 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) 16 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 17 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) 18 TI relaxation OR AB relaxation 19 TI mindful* OR AB mindful* 20 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) 21 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) 22 TI "cognit* restructur*" OR AB "cognit* restructur*" 23 TI "positive psychology" OR AB "positive psychology" 24 TI (refram* OR refram* OR reapprais*) OR AB (refram* OR refram* OR reapprais*) 25 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 26 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) 27 TI "acceptance and commitment" OR AB "acceptance and commitment" 28 (MH "Combined Modality Therapy") 29 TI (multimodal OR multimodal OR "combined modal*") OR AB (multimodal OR multimodal OR "combined modal*") 30 (MH "Health Promotion+") 31 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) 32 S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 33 S11 AND S32 34 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 35 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 36 S33 OR S34 OR S35 37 MH randomized controlled trials 38 MH double‐blind studies 39 MH single‐blind studies 40 MH random assignment 41 MH pretest‐posttest design 42 MH cluster sample 43 TI (randomised OR randomized) 44 AB (random*) 45 TI (trial) 46 MH (sample size) AND AB (assigned OR allocated OR control) 47 MH (placebos) 48 PT (randomized controlled trial) 49 AB (control W5 group) 50 MH (crossover design) OR MH (comparative studies) 51 AB (cluster W3 RCT) 52 MH animals+ 53 MH (animal studies) 54 TI (animal model*) 55 S52 OR S53 OR S54 56 MH (human) 57 S55 NOT S56 58 S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 59 S58 NOT S57 60 S36 AND S59 61 (MH "Health Personnel") OR (MH "Health professional") 62 TI (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR AB (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR SU (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) 63 TI (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR TI (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 64 TI (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 65 TI (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) OR surgeon*) OR AB (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) or surgeon*) OR SU (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) or surgeon*) 66 TI (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) OR AB (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) OR SU (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) 67 (MH "nursing") 68 TI nursing OR AB nursing OR SU nursing 69 TI ((hospital OR ambulance) N1 personnel) OR AB ((hospital OR ambulance) N1 personnel) OR SU ((hospital OR ambulance) N1 personnel) 70 TI ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) OR AB ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) OR SU ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) 71 TI ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR AB ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR SU ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) 72 TI (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR AB (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR SU (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) 73 TI (social N1 worker*) OR AB (social N1 worker*) OR SU (social N1 worker*) 74 TI (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) OR AB (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) OR SU (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) 75 TI (professional N1 caregiver*) OR AB (professional N1 caregiver*) OR SU (professional N1 caregiver*) 76 TI ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) OR AB ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) OR SU ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) 77 TI counsel?or* OR AB counsel?or* OR SU counsel?or* 78 TI ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) OR AB ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) OR SU ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) 79 TI ((human or health) N1 service N1 profession*) OR AB ((human or health) N1 service N1 profession*) OR SU ((human or health) N1 service N1 profession*) 80 TI (public N1 health N1 (service or agency)) OR AB (public N1 health N1 (service or agency)) OR SU (public N1 health N1 (service or agency)) 81 TI ("secondary traumati?ation" or (work* N2 (trauma survivor*))) OR AB ("secondary traumati?ation" or (work* N2 (trauma survivor*))) OR SU ("secondary traumati?ation" or (work* N2 (trauma survivor*))) 82 TI ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) OR AB ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) OR SU ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) 83 TI (college N1 student*) OR AB (college N1 student*) OR SU (college N1 student*) 84 TI (nursing N1 (graduates OR education)) OR AB (nursing N1 (graduates OR education)) OR SU (nursing N1 (graduates OR education)) OR TI (medical N2 train*) OR AB (medical N2 train*) OR SU (medical N2 train*) OR TI (student N1 nurse*) OR AB (student N1 nurse*) OR SU (student N1 nurse*) 85 S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 86 S60 AND S85 87 S60 AND S85, Limiters ‐ Published Date: 19900101‐20190631 88 S60 AND S85, Limiters ‐ Published Date: 20161001‐20190631
PSYNDEX EBSCO
Searched 24 June 2019 [31 records]
1 DE "Resilience (Psychological)" 2 DE "Adaptability (Personality)" 3 DE "Emotional Adjustment" OR DE "Social Adjustment" 4 DE "Coping Behavior" 5 DE "Posttraumatic Growth" 6 DE "Protective Factors" 7 TI ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR SU ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 8 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) OR SU (positiv* N1 (adapt* OR adjust*)) 9 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) OR SU (psychol* N1 (adapt* OR adjust*)) 10 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) OR SU (resilien* OR hardiness*) 11 TI (cope OR coping) OR AB (cope OR coping) OR SU (cope OR coping) 12 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR SU ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 13 DE "Psychological Stress" 14 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 15 DE "Psychotherapy" OR DE "Adlerian Psychotherapy" OR DE "Adolescent Psychotherapy" OR DE "Affirmative Therapy" OR DE "Analytical Psychotherapy" OR DE "Autogenic Training" OR DE "Behavior Therapy" OR DE "Brief Psychotherapy" OR DE "Brief Relational Therapy" OR DE "Child Psychotherapy" OR DE "Client Centered Therapy" OR DE "Cognitive Behavior Therapy" OR DE "Conversion Therapy" OR DE "Eclectic Psychotherapy" OR DE "Emotion Focused Therapy" OR DE "Existential Therapy" OR DE "Experiential Psychotherapy" OR DE "Expressive Psychotherapy" OR DE "Eye Movement Desensitization Therapy" OR DE "Feminist Therapy" OR DE "Geriatric Psychotherapy" OR DE "Gestalt Therapy" OR DE "Group Psychotherapy" OR DE "Guided Imagery" OR DE "Humanistic Psychotherapy" OR DE "Hypnotherapy" OR DE "Individual Psychotherapy" OR DE "Insight Therapy" OR DE "Integrative Psychotherapy" OR DE "Interpersonal Psychotherapy" OR DE "Logotherapy" OR DE "Narrative Therapy" OR DE "Network Therapy" OR DE "Persuasion Therapy" OR DE "Primal Therapy" OR DE "Psychoanalysis" OR DE "Psychodrama" OR DE "Psychodynamic Psychotherapy" OR DE "Psychotherapeutic Counseling" OR DE "Rational Emotive Behavior Therapy" OR DE "Reality Therapy" OR DE "Relationship Therapy" OR DE "Solution Focused Therapy" OR DE "Supportive Psychotherapy" OR DE "Transactional Analysis" OR DE "Individualpsychologische Therapie" OR DE "Jugendlichenpsychotherapie" OR DE "Affirmative Therapie" OR DE "Analytische Psychotherapie (C. G. Jung)" OR DE "Autogenes Training" OR DE "Verhaltenstherapie" OR DE "Kurzpsychotherapie" OR DE "Beziehungsorientierte Kurzpsychotherapie" OR DE "Kinderpsychotherapie" OR DE "Klientenzentrierte Psychotherapie" OR DE "Kognitive Verhaltenstherapie" OR DE "Konversionstherapie (Homosexualität)" OR DE "Eklektische Psychotherapie" OR DE "Emotionsfokussierte Therapie" OR DE "Existenzialtherapie" OR DE "Erfahrungsorientierte Psychotherapie" OR DE "Expressive Psychotherapie" OR DE "Augenbewegungsdesensibilisierung" OR DE "Feministische Therapie" OR DE "Geriatrische Psychotherapie" OR DE "Gestalttherapie" OR DE "Gruppenpsychotherapie" OR DE "Geleitete Fantasievorstellung" OR DE "Humanistische Psychotherapie" OR DE "Hypnotherapie" OR DE "Einzelpsychotherapie" OR DE "Einsichtstherapie" OR DE "Integrative Psychotherapie" OR DE "Interpersonelle Psychotherapie" OR DE "Logotherapie" OR DE "Narrative Therapie" OR DE "Netzwerktherapie" OR DE "Persuasionstherapie" OR DE "Primärtherapie" OR DE "Psychoanalytische Therapie" OR DE "Psychodrama" OR DE "Psychodynamische Psychotherapie" OR DE "Psychotherapeutische Beratung" OR DE "Rational‐Emotive Verhaltenstherapie" OR DE "Realitätstherapie" OR DE "Relationship Therapy" OR DE "Lösungsorientierte Therapie" OR DE "Unterstützende Psychotherapie" OR DE "Transaktionsanalyse" 16 DE "Cognitive Techniques" 17 DE "Psychotherapeutic Techniques" 18 DE "Relaxation Therapy" 19 DE "Mindfulness" 20 DE "Stress Management" 21 TI (psychotherap* OR psycho‐therap*) OR AB (psychotherap* OR psycho‐therap*) OR SU (psychotherap* OR psycho‐therap*) 22 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) OR SU (behav* N3 (intervention* OR program* OR therap*)) 23 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR SU ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 24 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) OR SU (psycho* N3 (intervention* OR program* OR therap*)) 25 TI relaxation OR AB relaxation OR SU relaxation 26 TI mindful* OR AB mindful* OR SU mindful* 27 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) OR SU (counsel?ing OR coaching) 28 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) OR SU ("third wave" N1 (psycho* OR therap*)) 29 TI "cognit* restructur*" OR AB "cognit* restructur*" OR SU "cognit* restructur*" 30 TI "positive psychology" OR AB "positive psychology" OR SU "positive psychology" 31 TI (refram* OR re‐fram* OR reapprais*) OR AB (refram* OR re‐fram* OR reapprais*) OR SU (refram* OR re‐fram* OR reapprais*) 32 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR SU (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 33 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) OR SU (anxiety N3 manage*) 34 TI "acceptance and commitment" OR AB "acceptance and commitment" OR SU "acceptance and commitment" 35 DE "Multimodal Treatment Approach" 36 TI (multimodal OR multi‐modal OR "combined modal*") OR AB (multimodal OR multi‐modal OR "combined modal*") OR SU (multimodal OR multi‐modal OR "combined modal*") 37 DE "Health Promotion" 38 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) OR SU (health N3 (educat* OR promot*)) 39 S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 40 S14 AND S39 41 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR SU (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 42 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR SU (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 43 S40 OR S41 OR S42 44 DE "Clinical Trials" 45 DE "Longitudinal Studies" 46 DE "Program Evaluation" 47 DE "Treatment Effectiveness Evaluation" 48 TI random* OR AB random* 49 TI (allocat* OR assign*) OR AB (allocat* OR assign*) 50 TI (clinic* OR control*) N1 trial*)) OR AB (clinic* OR control*) N1 trial*)) 51 TI ((control* OR experiment* OR intervention*) N3 group*) OR AB ((control* OR experiment* OR intervention*) N3 group*) 52 TI ((singl* OR doubl* OR trebl* OR tripl*) N3 (blind* OR mask*)) OR AB ((singl* OR doubl* OR trebl* OR tripl*) N3 (blind* OR mask*)) 53 TI (crossover* OR "cross over*") OR AB (crossover* OR "cross over*") 54 TI (placebo* OR (usual N1 treatment*) OR waitlist OR wait‐list) OR AB (placebo* OR (usual N1 treatment*) OR waitlist OR wait‐list) 55 TI prospectiv* OR AB prospectiv* 56 TI (crossover OR cross‐over) OR AB (crossover OR cross‐over) 57 TI ((singl* OR doubl* OR tripl* OR trebl*) N1 (blind* OR mask*)) OR AB ((singl* OR doubl* OR tripl* OR trebl*) N1 (blind* OR mask*)) 58 TI ((effectiveness OR evaluat*) N3 (stud* OR research*)) OR AB ((effectiveness OR evaluat*) N3 (stud* OR research*)) 59 S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 60 S43 AND S59 61 DE "Health Personnel" OR DE "Health professional" 62 TI (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR AB (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR SU (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) 63 TI (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR TI (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 64 TI (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 65 TI (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) OR surgeon*) OR AB (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) or surgeon*) OR SU (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) or surgeon*) 66 TI (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) OR AB (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) OR SU (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) 67 DE "nursing" 68 TI nursing OR AB nursing OR SU nursing 69 TI ((hospital OR ambulance) N1 personnel) OR AB ((hospital OR ambulance) N1 personnel) OR SU ((hospital OR ambulance) N1 personnel) 70 TI ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) OR AB ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) OR SU ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) 71 TI ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR AB ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR SU ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) 72 TI (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR AB (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR SU (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) 73 TI (social N1 worker*) OR AB (social N1 worker*) OR SU (social N1 worker*) 74 TI (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) OR AB (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) OR SU (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) 75 TI (professional N1 caregiver*) OR AB (professional N1 caregiver*) OR SU (professional N1 caregiver*) 76 TI ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) OR AB ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) OR SU ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) 77 TI counsel?or* OR AB counsel?or* OR SU counsel?or* 78 TI ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) OR AB ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) OR SU ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) 79 TI ((human or health) N1 service N1 profession*) OR AB ((human or health) N1 service N1 profession*) OR SU ((human or health) N1 service N1 profession*) 80 TI (public N1 health N1 (service or agency)) OR AB (public N1 health N1 (service or agency)) OR SU (public N1 health N1 (service or agency)) 81 TI ("secondary traumati?ation" or (work* N2 (trauma survivor*))) OR AB ("secondary traumati?ation" or (work* N2 (trauma survivor*))) OR SU ("secondary traumati?ation" or (work* N2 (trauma survivor*))) 82 TI ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) OR AB ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) OR SU ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) 83 TI (college N1 student*) OR AB (college N1 student*) OR SU (college N1 student*) 84 TI (nursing N1 (graduates OR education)) OR AB (nursing N1 (graduates OR education)) OR SU (nursing N1 (graduates OR education)) OR TI (medical N2 train*) OR AB (medical N2 train*) OR SU (medical N2 train*) OR TI (student N1 nurse*) OR AB (student N1 nurse*) OR SU (student N1 nurse*) 85 S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 86 S60 AND S85 87 S60 AND S85, Limiters ‐ Published Date: 1990‐2019 88 S60 AND S85, Limiters ‐ Published Date: 2016‐2019
Web Of Science Core Collection (SCI, SSCI, CPCI‐S, CPCI‐SSH)
Searched 26 June 2019 [515 records]
#40 #18 AND #38 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2016‐2019 #39 #16 AND #17 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 #38 #37 OR #36 OR #35 OR #34 OR #33 OR #32 OR #31 OR #30 OR #29 OR #28 OR #27 OR #26 OR #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #37 TS=("college student*") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #36 TS=((nursing or medical or premedical or paramedic or psychology or "physical therapy" or "occupational therapy") NEAR/2 student*) #35 ts=("secondary trauma*" or (work* NEAR/2 "trauma survivor*")) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #34 TS=("public health service*" or "public health agenc*") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #33 TS=((clinical or medical*) NEAR/1 (technician* or technologist* or assistant* or scientist*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #32 TS=(counsellor* or counselor*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #31 TS=(anesthetist* or anaesthetist* or audiologist* or "dental hygienist*" or dentist* or dietitian* or "midwi*e*" or nutritionist* or pathologist* or physiologist* or physiotherapist* or therapist or osteopath* or sonographer* or radiographer* or radiotherapist* or ((radiology or radiation) NEAR/1 ( technician* or technologist* or assistant* or scientist*)) or ((anesthesia or anesthesiologist) NEAR/1 (technician* or assistant*)) or (surgical NEAR/1 (technician* or technologist*)) or orthotist* or orthoptist* or podiatrist* or perfusionist*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #30 TS=(professional NEAR/1 (caregiver* or care‐giver*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #29 TS=((first or emergency or disaster) NEAR/1 (response or responder*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #28 TS=(paramedic* or para‐medic* or ambulance ) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #27 ts=(psychologist* or psychotherapist* or psychiatrist* or "mental health clinician*" or "mental health profession*" or "mental health worker*" or "social worker*") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #26 TS= ("allied health*" NEAR/2 (personnel* or profession* or worker* or practitioner* or provider* or staff)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #25 TS=((intensive NEAR/2 care) or ICU) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #24 TS=((hospital or ambulance) NEAR/1 (staff or personnel)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #23 ts=(nurse* or nursing) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #22 TS=(doctor* or physician* or general practitioner* or ("primary care" NEAR/2 practitioner*) or surgeon*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #21 TS=(care* NEAR/1 (personnel or profession* or worker* or practitioner* or provider* or staff)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #20 TS=(medical NEAR/3 (personnel or profession* or worker* or practitioner* or provider* or staff)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #19 TS=(health* NEAR/3 (personnel or profession* or worker* or practitioner* or provider* or staff)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #18 #17 AND #16 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #17 TS=(random* or trial* or assign* or control* or group* or placebo* or blind* or prospectiv* or longitudinal* or meta‐analys* or systematic review*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #16 #14 or #15 #15 TS=((resilience or hardiness) near/3 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #14 #13 AND #6 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #13 #12 OR #11 OR #10 OR #9 OR #8 OR #7 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #12 TS=(health near/3 (educat* or promot*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #11 TS= ((multimodal* or "multi modal*" or "combined modal*") NEAR/3 (treat* or therap* or intervention* or program*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #10 TS=("acceptance and commitment") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #9 TS=((anxiety near/1 manag*) or relaxation or mindful* or counsel*ing or coaching or "third wave" or refram* or "re fram*" or "cognitive restructur*" or "positive psychology") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #8 TS=(stress near/3 (inoculat* or manag* or reduc* or resist*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #7 TS=((psychotherap* or "psycho therap*") or CBT or mindful* or (behav* near/3 (intervention* or program* or therap*)) OR ((cognit* or "cognitive behavior*" or CBT) near/3 (intervention* or program* or therap*)) OR (psycho* near/3 (intervention* or program* or therap*))) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #6 #5 OR #4 OR #3 OR #2 OR #1 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years # 5 TS= ((withstand* or overcom* or resist* or recover* or thriv* or adapt* or adjust* or "bounc* back" ) near/1 (stress* or trauma* or advers*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years # 4 TS=(psychol* near/1 (adapt* or adjust*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years # 3 TS=(positiv* near/1 (adapt* or adjust*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years # 2 TS=("post traumatic growth" or "posttraumatic growth" or "stress related growth") TS=(resilien* or hardiness*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years
International Bibliography of the Social Sciences (IBSS) PROQUEST
Searched 25 June 2019 [135 records]
(((MAINSUBJECT.EXACT("Coping") OR TI(resilien* OR hardiness) OR AB(resilien* OR hardiness)) OR (TI((psychol* OR social) NEAR/1 (adapt* OR adjust*)) OR AB((psychol* OR social) NEAR/1 (adapt* OR adjust*))) OR (TI(positiv* NEAR/1 (adapt* OR adjust*)) OR AB(positiv* NEAR/1 (adapt* OR adjust*))) OR (TI("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (TI(cope OR coping) OR AB(cope OR coping)) OR (TI((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") NEAR/5 (stress* OR trauma* OR adversit*)) OR AB((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") NEAR/5 (stress* OR trauma* OR adversit*)))) AND ((MAINSUBJECT.EXACT("Psychotherapy") OR MAINSUBJECT.EXACT("Cognitive therapy") OR MAINSUBJECT.EXACT("Group therapy") OR TI(psychotherap* OR psycho‐therap*) OR AB(psychotherap* OR psycho‐therap*) OR TI(behav* NEAR/3 (intervention* OR program* OR therap*)) OR AB(behav* NEAR/3 (intervention* OR program* OR therap*)) OR TI(cognit* OR "cognitive behavior*" OR CBT) OR AB(cognit* OR "cognitive behavior*" OR CBT) OR TI(psycho* NEAR/3 (intervention* OR program* OR therap*)) OR AB(psycho* NEAR/3 (intervention* OR program* OR therap*)) OR TI(relaxation OR mindful* OR counsel?ing OR coaching OR "third wave") OR AB(relaxation OR mindful* OR counsel?ing OR coaching OR "third wave") OR TI(cognit* NEAR/1 restructur*) OR AB(cognit* NEAR/1 restructur*) OR TI("positive psychology") OR AB("positive psychology")) AND (MAINSUBJECT.EXACT("Clinical trials") OR (TI(control* OR group OR random* OR placebo* OR longitudinal OR prospective* OR blind* OR trial*) OR AB(control* OR group OR random* OR placebo* OR longitudinal OR prospective* OR blind* OR trial*)))) Limited to publication year 2016‐2019
Applied Social Sciences Index & Abstracts ProQuest (ASSIA) PROQUEST
Searched 24 June 2019 [41 records]
1 SU.EXACT("Resilience") 2 SU.EXACT("Hardiness") 3 ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 4 ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) 5 ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) 6 SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) 7 ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 8 ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 9 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 10 ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*) 11 ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*) 12 ti(randomi?ed) OR ab(randomi?ed) 13 ti(placebo*) OR ab(placebo*) 14 ti(randomly) OR ab(randomly) 15 ti(trial) OR ab(trial) 16 (ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)) 17 ((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) 18 ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) 19 ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) 20 ti(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) 21 ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) 22 SU.EXACT("nursing") 23 ti(nursing) OR ab(nursing) 24 ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) 25 ti(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") OR ab(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") 26 ti(social N/1 worker*) OR ab(social N/1 worker*) 27 ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) 28 ti(physiotherapist* OR (occupational N/1 therapist*)) OR ab(physiotherapist* OR (occupational N/1 therapist)) 29 ti(counsel?or*) OR ab(counsel?or*) 30 ti((human or health) N/1 service N/1 profession*) OR ab((human or health) N/1 service N/1 profession*) 31 ti(public N/1 health N/1 (service or agency)) OR ab(public N/1 health N/1 (service or agency)) 32 ti("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) OR ab("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) 33 ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) 34 ti(college N/1 student*) OR ab(college N/1 student*) 35 (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))) OR (ti((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))) OR (ti(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*)) OR (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))) OR SU.EXACT("nursing") OR (ti(nursing) OR ab(nursing)) OR (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))) OR (ti(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") OR ab(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*")) OR (ti(social N/1 worker*) OR ab(social N/1 worker*)) OR (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))) OR (ti(physiotherapist* OR (occupational N/1 therapist*)) OR ab(physiotherapist* OR (occupational N/1 therapist))) OR (ti(counsel?or*) OR ab(counsel?or*)) OR (ti((human or health) N/1 service N/1 profession*) OR ab((human or health) N/1 service N/1 profession*)) OR (ti(public N/1 health N/1 (service or agency)) OR ab(public N/1 health N/1 (service or agency))) OR (ti("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) OR ab("secondary traumati?ation" OR (work* N/2 ("trauma survivor*")))) OR (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)) OR (ti(college N/1 student*) OR ab(college N/1 student*)) 36 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))) 37 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))), 2016‐10‐01 ‐ 2019‐06‐20 38 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))) 39 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))), 2016‐10‐01 ‐ 2019‐06‐20 40 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*)) 41 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*)), 2016‐10‐01 ‐ 2019‐06‐20 42 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))) 43 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))), 2016‐10‐01 ‐ 2019‐06‐20 44 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND SU.EXACT("nursing") 45 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND SU.EXACT("nursing"), 2016‐10‐01 ‐ 2019‐06‐20 46 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing) OR ab(nursing)) 47 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing) OR ab(nursing)), 2016‐10‐01 ‐ 2019‐06‐20 48 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))) 49 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))), 2016‐10‐01 ‐ 2019‐06‐20 50 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") OR ab(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*")) 51 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") OR ab(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*")), 2016‐10‐01 ‐ 2019‐06‐20 52 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(social N/1 worker*) OR ab(social N/1 worker*)) 53 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(social N/1 worker*) OR ab(social N/1 worker*)), 2016‐10‐01 ‐ 2019‐06‐20 54 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))) 55 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))), 2016‐10‐01 ‐ 2019‐06‐20 56 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(physiotherapist* OR (occupational N/1 therapist*)) OR ab(physiotherapist* OR (occupational N/1 therapist))) 57 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(physiotherapist* OR (occupational N/1 therapist*)) OR ab(physiotherapist* OR (occupational N/1 therapist))), 2016‐10‐01 ‐ 2019‐06‐20 58 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(counsel?or*) OR ab(counsel?or*)) 59 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(counsel?or*) OR ab(counsel?or*)), 2016‐10‐01 ‐ 2019‐06‐20 60 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR anag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((human or health) N/1 service N/1 profession*) OR ab((human or health) N/1 service N/1 profession*)) 61 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR anag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((human or health) N/1 service N/1 profession*) OR ab((human or health) N/1 service N/1 profession*)), 2016‐10‐01 ‐ 2019‐06‐20 62 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(public N/1 health N/1 (service or agency)) OR ab(public N/1 health N/1 (service or agency))) 63 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(public N/1 health N/1 (service or agency)) OR ab(public N/1 health N/1 (service or agency))), 2016‐10‐01 ‐ 2019‐06‐20 64 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) OR ab("secondary traumati?ation" OR (work* N/2 ("trauma survivor*")))) 65 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) OR ab("secondary traumati?ation" OR (work* N/2 ("trauma survivor*")))), 2016‐10‐01 ‐ 2019‐06‐20 66 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*))OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)) 67 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*))OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)), 2016‐10‐01 ‐ 2019‐06‐20 68 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(college N/1 student*) OR ab(college N/1 student*)) 69 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(college N/1 student*) OR ab(college N/1 student*)), 2016‐10‐01 ‐ 2019‐06‐20 Subsequent (individual) export of results in lines S37, S39, S41, S43, S45, S47, S49, S51, S53, S55, S57, S59, S61, S63, S65, S67, S69
ProQuest Dissertations & Theses (PQDT) PROQUEST
Searched 24 June 2019 [22 records]
1 SU.EXACT("Resilience") 2 SU.EXACT("Hardiness") 3 ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 4 ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) 5 ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) 6 SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) 7 ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 8 ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 9 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 10 ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*) 11 ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*) 12 ti(randomi?ed) OR ab(randomi?ed) 13 ti(placebo*) OR ab(placebo*) 14 ti(randomly) OR ab(randomly) 15 ti(trial) OR ab(trial) 16 (ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)) 17 ((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) 18 ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) 19 ti(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR ab(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 20 ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) 21 ti(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) 22 ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) 23 SU.EXACT(“nursing”) 24 ti(nursing) OR ab(nursing) 25 ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) 26 ti(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR ab(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) 27 ti(social N/1 worker*) OR ab(social N/1 worker*) 28 ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) 29 ti(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) OR ab(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) 30 ti(counsel?or*) OR ab(counsel?or*) 31 ti(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) OR ab(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) 32 ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) 33 ti(college N/1 student*) OR ab(college N/1 student*) 34 ti(nursing N/1 (graduates OR education)) OR ab(nursing N/1 (graduates OR education)) 35 (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))) OR (ti(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR ab(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR (ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))) OR (ti(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*)) OR (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))) OR SU.EXACT(“nursing”) OR (ti(nursing) OR ab(nursing)) OR (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))) OR (ti(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR ab(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”)) OR (ti(social N/1 worker*) OR ab(social N/1 worker*)) OR (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))) OR (ti(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) OR ab(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*))) OR (ti(counsel?or*) OR ab(counsel?or*)) OR (ti(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) OR ab(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”)))) OR (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)) OR (ti(college N/1 student*) OR ab(college N/1 student*)) OR (ti(nursing N/1 (graduates OR education)) OR ab(nursing N/1 (graduates OR education))) 36 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))) 37 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))), 2016‐10‐01 ‐ 2019‐06‐20 38 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR ab(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) 39 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR ab(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))), 2016‐10‐01 ‐ 2019‐06‐20 40 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))) 41 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))), 2016‐10‐01 ‐ 2019‐06‐20 42 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*)) 43 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*)), 2016‐10‐01 ‐ 2019‐06‐20 44 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))) 45 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))), 2016‐10‐01 ‐ 2019‐06‐20 46 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND SU.EXACT(“nursing”) 47 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND SU.EXACT(“nursing”), 2016‐10‐01 ‐ 2019‐06‐20 48 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing) OR ab(nursing)) 49 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing) OR ab(nursing)), 2016‐10‐01 ‐ 2019‐06‐20 50 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))) 51 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))), 2016‐10‐01 ‐ 2019‐06‐20 52 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR ab(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”)) 53 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR ab(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”)), 2016‐10‐01 ‐ 2019‐06‐20 54 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(social N/1 worker*) OR ab(social N/1 worker*)) 55 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(social N/1 worker*) OR ab(social N/1 worker*)), 2016‐10‐01 ‐ 2019‐06‐20 56 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))) 57 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))), 2016‐10‐01 ‐ 2019‐06‐20 58 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) OR ab(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*))) 59 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) OR ab(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*))), 2016‐10‐01 ‐ 2019‐06‐20 60 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(counsel?or*) OR ab(counsel?or*)) 61 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(counsel?or*) OR ab(counsel?or*)), 2016‐10‐01 ‐ 2019‐06‐20 62 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) OR ab(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”)))) 63 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) OR ab(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”)))), 2016‐10‐01 ‐ 2019‐06‐20 64 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)) 65 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)), 2016‐10‐01 ‐ 2019‐06‐20 66 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(college N/1 student*) OR ab(college N/1 student*)) 67 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(college N/1 student*) OR ab(college N/1 student*)), 2016‐10‐01 ‐ 2019‐06‐20 68 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing N/1 (graduates OR education)) OR ab(nursing N/1 (graduates OR education))) 69 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing N/1 (graduates OR education)) OR ab(nursing N/1 (graduates OR education))), 2016‐10‐01 ‐ 2019‐06‐20 Subsequent (individual) export of results in lines S37, S39, S41, S43, S45, S47, S49, S51, S53, S55, S57, S59, S61, S63, S65, S67, S69
Cochrane Database of Systematic Reviews (CDSR)
Searched 26 June 2019 (5 records)
IDSearchHits #1(resilien* or hardiness*):ti,ab #2(post next traumatic next growth or posttraumatic NEXT growth or stress next related next growth):ti,ab #3(positiv* near/1 (adapt* or adjust*)):ti,ab #4(psychol* near/1 (adapt* or adjust*)):ti,ab #5{or #1‐#4} #6(behav* or psycho* or cbt or cognit* or mindful* or reframe* or re next fram*):ti,ab #7(stress near/3 (inoculat* or manag* or reduc* or resist*)):ti,ab #8(anxiety near/3 manag*):ti,ab #9"acceptance and commitment":ti,ab #10(multimodal* or multi next modal* or combined next modal*):ti,ab #11(health near/3 (educat* or promot*)):ti,ab #12{or #6‐#11} #13#5 and #12 with Cochrane Library publication date Between Oct 2016 and Jun 2019, in Cochrane Reviews, Cochrane Protocolss
Epistemonikos (epistemonikos.org)
Searched 24 June 2019 [6 records]
1 (title:(resilien* OR hardiness*) OR abstract:(resilien* OR hardiness*)) 2 (title:("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR abstract:("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) 3 (title:("positive adaptation" OR "positive adjustment") OR abstract:("positive adaptation" OR "positive adjustment")) 4 (title:("psychological adaptation" OR "psychological adjustment") OR abstract:("psychological adaptation" OR "psychological adjustment")) 5 OR/#1‐#4 6 (title:("health personnel*" OR "health profession*" OR "health professional*" OR "health worker*" OR "health practitioner*" OR "health provider*" OR "health staff") OR abstract:("health personnel*" OR "health profession*" OR "health professional*" OR "health worker*" OR "health practitioner*" OR "health provider*" OR "health staff")) 7 (title:("healthcare personnel*" OR "healthcare profession*" OR "healthcare professional*" OR "healthcare worker*" OR "healthcare practitioner*" OR "healthcare provider*" OR "healthcare staff") OR abstract:("healthcare personnel*" OR "healthcare profession*" OR "healthcare professional*" OR "healthcare worker*" OR "healthcare practitioner*" OR "healthcare provider*" OR "healthcare staff")) 8 (title:("health care personnel*" OR "health care profession*" OR "health care professional*" OR "health care worker*" OR "health care practitioner*" OR "health care provider*" OR "health care staff") OR abstract:("health care personnel*" OR "health care profession*" OR "health care professional*" OR "health care worker*" OR "health care practitioner*" OR "health care provider*" OR "health care staff")) 9 OR/#6‐#8 10 AND/#5‐#9; Publication year (Custom year range): 1990 – 2019; Publication type: Systematic Review; Systematic review question: All; Cochrane review: All; Type of meta‐analysis: All
ERIC EBSCOhost
26 June 2019 (505 records)
All years searched in 2019 as there were errors in the 2016 search
S1DE "Resilience (Psychology)" Database ‐ ERIC S2DE "Social Adjustment" OR DE "Emotional Adjustment" Database ‐ ERIC S3TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") Database ‐ ERIC S4TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) Database ‐ ERIC S5TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) Database ‐ ERIC S6TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) OR SU (resilien*) Database ‐ ERIC S7TI (cope OR coping) OR AB (cope OR coping) OR SU (cope OR coping) Database ‐ ERIC S8TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) Database ‐ ERIC S9S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 Database ‐ ERIC S10DE "Psychotherapy" OR DE "Milieu Therapy" OR DE "Relaxation Training" Database ‐ ERIC S11TI (psycho‐therap* OR psychotherap* ) OR AB (psychotherap* OR psychotherap*) OR SU (psycho‐therap* OR psychotherap*) Database ‐ ERIC S12TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) Database ‐ ERIC S13TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) Database ‐ ERIC S14TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) Database ‐ ERIC S15TI relaxation OR AB relaxation OR SU relaxation Database ‐ ERIC S16TI mindful* OR AB mindful* Database ‐ ERIC S17TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) OR SU (counsel?ing OR coaching) Database ‐ ERIC S18TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) Database ‐ ERIC S19TI ("cognit* restructur*") OR AB ("cognit* restructur*") OR SU ("cognit* restructur*") Database ‐ ERIC S20TI "positive psychology" OR AB "positive psychology" Database ‐ ERIC S21TI (refram* OR refram* OR reapprais*) OR AB (refram* OR refram* OR reapprais*)Interface ‐ EBSCOhost Research Databases Database ‐ ERIC S22TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR SU (stress N1 (inoculation OR manag* OR reduc* OR resist*)) Database ‐ ERIC S23TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) Database ‐ ERIC S24TI "acceptance and commitment" OR AB "acceptance and commitment" Database ‐ ERIC S25TI (multimodal OR multimodal OR "combined modal*") OR AB (multimodal OR multimodal OR "combined modal*") Database ‐ ERIC S26TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) OR SU (health N3 (educat* OR promot*)) Database ‐ ERIC S27S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 Database ‐ ERIC S28S9 AND S27 Database ‐ ERIC S29((DE "Health Occupations" OR DE "Allied Health Occupations" OR DE "Medical Education" OR DE "Health Personnel" OR DE "Allied Health Personnel" OR DE "Mental Health Workers" OR DE "Nurses" OR DE "Physicians" OR DE "Psychologists" OR DE "Graduate Medical Education" OR DE "Nursing Education" OR DE "Allied Health Occupations Education" OR DE "Clinical Experience" OR DE "Medical Schools" OR DE "Medical Students" OR DE "Premedical Students" Database ‐ ERIC S30DE "Counselors" OR DE "School Social Workers" OR DE "Social Work" Database ‐ ERIC S31TI(health* N3 (personnel or profession* or worker* or practitioner* or provider* or staff)) OR AB(health* N3 (personnel or profession* or worker* or practitioner* or provider* or staff)) Database ‐ ERIC S32TI(medical N3 (personnel or profession* or worker* or practitioner* or provider* or staff)) OR AB(medical N3 (personnel or profession* or worker* or practitioner* or provider* or staff)) Database ‐ ERIC S33TI(care N1 (personnel or profession* or worker* or practitioner* or provider* or staff)) OR AB(care N1 (personnel or profession* or worker* or practitioner* or provider* or staff))Database ‐ ERIC S34TI(doctor* or physician* or general practitioner* or (primary care N2 practitioner*) or surgeon*) OR AB(doctor* or physician* or general practitioner* or (primary care N2 practitioner*) or surgeon*) Database ‐ ERIC S35TI(nurse* or nursing) OR AB(nurse* or nursing) Database ‐ ERIC S36TI(hospital or ambulance) OR AB(hospital or ambulance) Database ‐ ERIC S37TI((intensive N2 care) or ICU) OR AB((intensive N2 care) or ICU) Database ‐ ERIC S38TI(allied health* N2 (personnel* or profession* or worker* or practitioner* or provider* or staff)) OR AB(allied health* N2 (personnel* or profession* or worker* or practitioner* or provider* or staff)) Database ‐ ERIC S39TI(psychologist* or psychotherapist* or psychiatrist* or mental health clinician* or mental health profession* or mental health worker*) OR AB(psychologist* or psychotherapist* or psychiatrist* or mental health clinician* or mental health profession* or mental health worker*) Database ‐ ERIC S40TI(social worker*) OR AB(social worker*) Database ‐ ERIC S41TI(paramedic* or para‐medic* or ambulance ) OR AB(paramedic* or para‐medic* or ambulance ) Database ‐ ERIC S42TI(first or emergency or disaster) N1 (response or responder*)) OR AB(first or emergency or disaster) N1 (response or responder*)) Database ‐ ERIC S43TI(professional N1 (caregiver* or care‐giver*)) OR AB(professional N1 (caregiver* or care‐giver*)) Database ‐ ERIC S44TI (physical therapist* or physiotherapist* or occupational therapist* or recreational therapist* or music therapist* or art therapist* or dietitian* or nutritionist* or ((speech and language) N1 therapist*) or speech pathologist* or audiologist* or exercise physiologist* or osteopath* or sonographer* or radiographer* or radiotherapist* or ((radiology or radiation) N1 (therapist* or technician* or technologist* or assistant* or scientist*)) or respiratory therapist* or ((anesthesia or anesthesiologist) N1 (technician* or assistant*)) or dental hygienist* or (surgical N1 (technician* or technologist*)) or orthotist* or orthoptist* or podiatrist* or perfusionist*) OR AB (physical therapist* or physiotherapist* or occupational therapist* or recreational therapist* or music therapist* or art therapist* or dietitian* or nutritionist* or ((speech and language) N1 therapist*) or speech pathologist* or audiologist* or exercise physiologist* or osteopath* or sonographer* or radiographer* or radiotherapist* or ((radiology or radiation) N1 (therapist* or technician* or technologist* or assistant* or scientist*)) or respiratory therapist* or ((anesthesia or anesthesiologist) N1 (technician* or assistant*)) or dental hygienist* or (surgical N1 (technician* or technologist*)) or orthotist* or orthoptist* or podiatrist* or perfusionist*) Database ‐ ERIC S45TI(counsel*or* ) OR AB(counsel*or* ) S46TI((clinical OR medical*) N1 (technician* or technologist* or assistant* or scientist*)) OR AB((clinical OR medical*) N1 (technician* or technologist* or assistant* or scientist*)) Database ‐ ERIC S47TI(public health service* or public health agenc*) OR AB(public health service* or public health agenc*) Database ‐ ERIC S48TI(secondary trauma* or (work* N2 trauma survivor*)) OR AB(secondary trauma* or (work* N2 trauma survivor*)) Database ‐ ERIC S49TI (nursing or medical or midwifery OR premedical or paramedic or psychology or physical therapy or occupational therapy) N2 student*) OR AB (nursing or medical or midwifery OR premedical or paramedic or psychology or physical therapy or occupational therapy) N2 student*) Database ‐ ERIC S50TI(college student*) OR AB(college student*) Database ‐ ERIC S51TI((nurs* N1 graduate*) or (nurs* N1 education) or (medic* N1 train*)) OR AB((nurs* N1 graduate*) or (nurs* N1 education) or (medic* N1 train*)) Database ‐ ERIC S52S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 Database ‐ ERIC S53S28 AND S52 Database ‐ ERIC S54DE "Meta Analysis" OR DE "Evaluation Research" OR DE "Control Groups" OR DE "Experimental Groups" OR DE "Longitudinal Studies" OR DE "Followup Studies" OR DE "Program Effectiveness" OR DE "Program Evaluation" Database ‐ ERIC S55(random* or trial* or group or experiment* or PROSPECTIVE* OR longitudinal or BLIND* or CONTROL* or treatment as usual or TAU) Database ‐ ERIC S56S54 OR S55 Database ‐ ERIC S57S53 AND S56 Database ‐ ERIC
Current Controlled Trials (ISRCTN registry; http://www.isrctn.com)
Searched 24 June 2019 [33 records]
Text search: (((((resilience OR hardiness OR "posttraumatic growth" OR stress OR trauma) AND (psychotherap OR relaxation OR mindfulness OR coaching OR "positive psychology" OR reappraisal OR "stress inoculation" OR "stress management" OR multimodal OR "health promotion")) OR ((resilience OR hardiness) AND (training OR program OR intervention OR promot OR prevent OR enhanc OR learn OR teach OR educat OR increas or develop OR manag OR therap OR protocol OR treat)))) AND ("health personnel" OR "health professional" OR "health worker" OR "health practitioner" OR "health provider" OR "health staff" OR students OR "human service professional")) Date assigned from 01/10/2016 to 24/06/2019
ClinicalTrials.gov (clinicaltrials.gov)
Searched 24 June 2019 [147 records]
Condition or disease = resilience OR hardiness OR posttraumatic growth OR stress OR trauma Other terms = health personnel OR health professional OR health worker OR health practitioner OR health provider OR health staff OR students OR human service professional Study type: Interventional studies (clinical trials) Intervention/treatment: resilience training OR hardiness training OR psychotherapy OR relaxation OR mindfulness OR coaching OR positive psychology OR reappraisal OR stress inoculation OR stress management OR multimodal OR health promotion Title or acronym: resilience OR hardiness OR posttraumatic growth OR stress OR trauma Study start: 01/10/2016 to 24/06/2019
WHO ICTRP (apps.who.int/trialsearch)
Searched 24 June 2019 [145 records]
title = health personnel OR health professional OR health worker OR health practitioner OR health provider OR health staff OR students OR human service professional intervention = resilience OR hardiness OR posttraumatic growth OR stress OR trauma OR psychotherapy OR relaxation OR mindfulness OR coaching OR positive psychology OR reappraisal OR stress inoculation OR stress management OR multimodal OR health promotion Recruitment status: ALL Date of registration: 01/10/2016 – 24/06/2019
Appendix 10. Data collection/extraction sheet (items according to Li 2019)
| Source |
|
| Eligibility |
|
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Results |
|
| Miscellaneous aspects |
|
| CI: Confidence interval; ID: Identifier; SD: Standard deviation. | |
Footnotes
aFull description required for standard items in ‘Risk of bias’ tool.
Appendix 11. Criteria for 'Risk of bias’ assessment in included RCTs (according to Higgins 2011b)
| Item | Judgement | Description |
| 1. Random sequence generation (selection bias). We will describe the method used to generate the allocation sequence in sufficient detail for each included trial to allow an assessment of whether it should produce comparable groups | Low risk | The investigators describe a random component in the sequence generation process such as:
|
| High risk | The researchers describe a (systematic or non‐systematic) non‐random component in the sequence generation process such as:
|
|
| Unclear risk | Insufficient information to permit a judgement of ‘Low risk’ or ‘High risk’. | |
| 2. Allocation concealment (selection bias). For each RCT we will describe the method used to conceal the allocation sequence in sufficient detail to determine whether intervention allocations could have been foreseen in advance of, or during, enrolment. | Low risk | Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation:
|
| High risk | Participants or investigators enrolling participants could possibly foresee assignment and thus introduce selection bias because one of the following methods was used:
|
|
| Unclear risk | Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement (e.g. if the use of assignment envelopes is described, but it remains unclear whether envelopes were sequentially numbered, opaque and sealed). | |
| 3. Blinding of participants and personnel (performance bias): objective outcomes. For each included trial, we will describe all methods used to blind trial participants and personnel from knowledge of which intervention a participant received. We will provide any information relating to whether the intended blinding was effective. We will assess blinding separately for different classes of outcomes. Outcomes will be divided into objective (e.g. cortisol) and subjective (e.g. self‐reported resilience and other psychological outcomes). We will consider the same outcomes at different time points. | Low risk | Any one of the following:
|
| 4. Blinding of participants and personnel (performance bias): subjective outcomes. For each included trial we will describe all methods used to blind trial participants and personnel from knowledge of which intervention a participant received. We will provide any information relating to whether the intended blinding was effective. We will assess blinding separately for different classes of outcomes. Outcomes will be divided into objective (e.g. cortisol) and subjective (e.g. self‐reported resilience and other psychological outcomes). We will consider the same outcomes at different time points. | Low risk | Blinding of participants and intervention providers, and unlikely that the blinding could have been broken. |
| High risk | Any one of the following:
|
|
| Unclear risk | Insufficient information to permit a judgement of ‘Low risk’ or ‘High risk’. | |
| 5. Blinding of outcome assessors (detection bias): objective outcomes. For each included trial we will describe all methods used to blind outcome assessors from knowledge of which intervention a participant received. We will provide any information relating to whether the intended blinding was effective. We will assess blinding separately for different classes of outcomes. Outcomes will be divided into objective (e.g. cortisol) and subjective (e.g. self‐reported resilience and other psychological outcomes). We will consider the same outcomes at different time points. | Low risk | Any one of the following:
|
| 6. Blinding of outcome assessors (detection bias): subjective outcomes. For each included trial we will describe all methods used to blind outcome assessors from knowledge of which intervention a participant received. We will provide any information relating to whether the intended blinding was effective. We will assess blinding separately for different classes of outcomes. Outcomes will be divided into objective (e.g. cortisol) and subjective (e.g. self‐reported resilience and other psychological outcomes). We will consider the same outcomes at different time points. | Low risk | Any one of the following:
|
| High risk | Any one of the following:
|
|
| Unclear risk | Insufficient information to permit a judgement of ‘Low risk’ or ‘High risk’. | |
| 7. Incomplete outcome data (attrition bias). For each RCT we will describe the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. We will state whether attrition and exclusions were reported, the numbers included at each stage (compared with the total number of participants randomised), reasons for attrition or exclusions (where reported), and whether missing data were balanced across groups or were related to outcomes. Where sufficient data are reported, or can be provided by the trial authors, we will re‐include missing data in the analyses. | Low risk | Any one of the following:
|
| High risk | Any one of the following:
|
|
| Unclear risk | Insufficient reporting of attrition or exclusions to permit a judgement of ‘Low risk’ or ‘High risk’ (e.g. number randomised not stated, no reasons for missing data provided, number of dropouts not reported for each group). | |
| 8. Selective outcome reporting (reporting bias). For each included trial we will describe how the possibility of selective outcome reporting was examined and what was found. | Low risk | Any of the following:
|
| High risk | Any one of the following:
|
|
| Unclear risk | Insufficient information to permit a judgement of ‘Low risk’ or ‘High risk’. | |
| RCT: Randomised controlled trial. | ||
Appendix 12. Detailed results of both searches
Using the original search strategy (Appendix 8), our database searches retrieved 32,184 records (including 1601 from trials registers). We found an additional 100 records by searching other resources. Following de‐duplication, we screened the remaining 20,410 records by title and abstract. We deemed 18,116 records to be irrelevant and sought the full text of the remaining 2294 records for further assessment. On the level of title/abstract screening, we achieved a good agreement (kappa = 0.70) between review authors. We retrieved 2294 full text reports. Based on the original eligibility criteria of this review (see Differences between protocol and review), 251 studies met the inclusion criteria. We identified 18 ongoing studies and 46 studies awaiting classification (in total: 315 studies from 376 reports). We excluded 1918 reports as irrelevant (Excluded studies). The full text screening for the first search resulted in excellent inter‐rater reliability (kappa = 0.95).
After revising the eligibility criteria to focus on healthcare professionals based on a broad definition of this target group (see Differences between protocol and review), we reassessed the studies found by the initial screening. From these, we identified 49 studies that were performed in any of these groups. We also identified one ongoing study and 10 studies awaiting classification. Finally, after revising the eligibility criteria to focus on healthcare professionals, we reassessed these 60 studies. From these, we identified 28 studies that fulfilled our inclusion criteria (Criteria for considering studies for this review). We also identified one study awaiting classification (see Studies awaiting classification). The results of the original search are presented in Figure 114.
4.
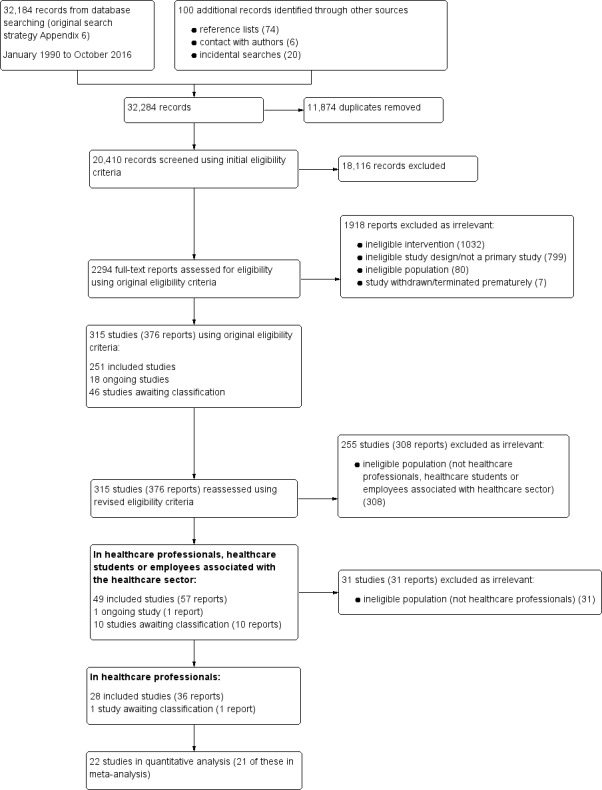
Study flow diagram for original searches (January 1990 to October 2016).
From 2016 onwards, we refined our search strategy to focus broadly on the healthcare sector (including healthcare professionals; Appendix 9. The searches yielded 6116 records (5553 + 563). Based on these broad criteria, we identified six additional reports of studies identified by earlier searches. We newly identified 31 studies that were performed in any of these groups, eight ongoing studies and 19 studies awaiting classification. We reassessed these 58 studies according to the narrower population, which is the focus of this review (healthcare professionals only). From these, we identified 16 studies that fulfilled our inclusion criteria. We also identified five ongoing studies and seven studies awaiting classification. The full text screening for the top‐up searches also resulted in excellent inter‐rater reliability (kappa = 1). The results of the top‐up searches are presented in Figure 115.
5.
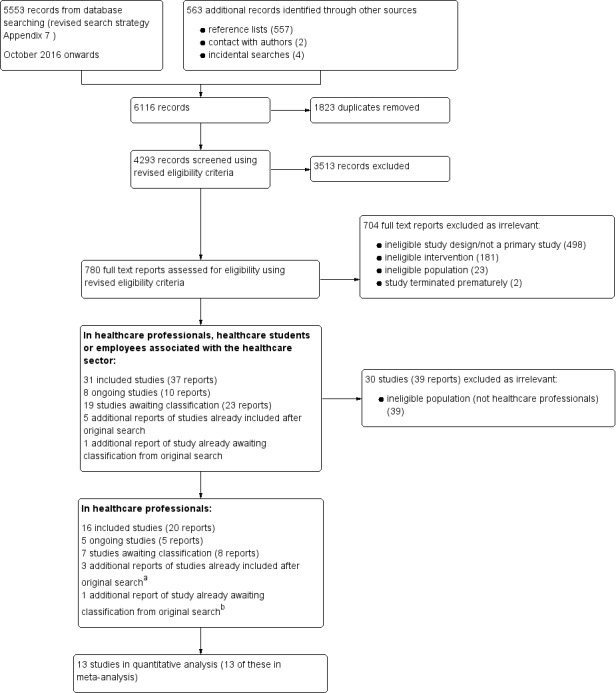
Study flow diagram for revised searches (October 2016 onwards).
aDuchemin 2015; Mistretta 2018; Schroeder 2016.
bVan Berkel 2014.
Appendix 13. References concerning the description of included studies
| Key characteristics of included studies | Number of included studies with respective references |
| Location |
|
| Settings (venue or implementation sites of interventions) |
|
| Participants ‐ number randomised |
|
| Participants ‐ age |
|
| Participants ‐ gender |
|
| Participants ‐ target group |
|
| Participants ‐ mental health assessment at baseline |
|
| Intervention ‐ setting |
|
| Intervention ‐ delivery format |
|
| Intervention ‐ training intensity |
|
| Intervention ‐ theoretical foundation | See Appendix 14 |
| Comparator |
|
| Funding sources |
|
| TAU: Treatment as usual | |
Footnotes
Appendix 14. Intervention content depending on theoretical foundation
| Theoretical foundation (number of studies) | Studies | Characteristics of studies within theoretical foundation | Intervention content |
| Combined resilience interventions (19) | Berger 2011; Bernburg 2016; Bernburg 2019; Calder Calisi 2017; Fei 2019; Gelkopf 2008; Ireland 2017; Lin 2019; Mache 2015a; Mache 2015b; Mache 2016; Mache 2017; Mealer 2014; Mistretta 2018; Smith 2019; Tierney 1997; Varker 2012; West 2014; Wild 2016 |
|
|
| Unspecific resilience interventions (11) | Alexander 2015; Cheung 2014; Hosseinnejad 2018; ISRCTN69644721; Khoshnazary 2016; Luthar 2017; Medisauskaite 2019; Mirzaeirad 2019; NCT02603133, Poulsen 2015; West 2015 |
|
|
| Mindfulness‐based resilience interventions (5) | Duchemin 2015; Klatt 2015; Lebares 2018; Loiselle 2018; Schroeder 2016 |
|
|
| Attention and interpretation therapy (3) | Chesak 2015; Sood 2011; Sood 2014 |
|
|
| Stress inoculation (2) | Stetz 2007; Villani 2013 |
|
|
| Cognitive‐behavioural therapy (2) | Cieslak 2016; Clemow 2018 |
|
|
| Positive psychology (1) | NCT03645798 |
|
|
| Coaching approaches (1) | Strijk 2011 |
|
|
| ACT: Acceptance and commitment therapy; CBT: cognitive‐behaviour therapy; CD: compact disc; ERASE stress: Enhancing resiliency among students experiencing stress; IG: intervention group; MBCT: Mindfulness‐based cognitive therapy; MBSR: Mindfulness‐based stress reduction; MP3: MPEG (moving picture experts group) audio layer‐3; SIT: stress inoculation training; USB: universal serial bus | |||
Footnotes
Appendix 15. Detailed exclusion reasons for excluded studies
We excluded 13 studies that seemed to merit inclusion but on closer inspection did not (see Characteristics of excluded studies).
Most of these studies (nine studies) were excluded as they did not explicitly state the aim of fostering resilience, hardiness or post‐traumatic growth through the intervention and/or we received the information from the study authors that resilience was not the primary focus of the study (Chang 2008; Dyrbye 2016; Imamura 2019; NCT03753360; NCT03914898; Rowe 1999; Speckens 2019; Strauss 2018; Watanabe 2019). Chang 2008 only mentioned the concept of resilience in the discussion section, but did not explicitly state the aim of promoting resilience. Speckens 2019, who tested a mindfulness intervention for medical residents of different fields, identified resilience as one issue in qualitative interviews but did also not aim to foster the participants' resilience. For two study protocols (Imamura 2019; Strauss 2018), we received the information from the study authors that resilience was not the primary focus and not measured in these studies. We excluded two studies that mentioned resilience in the trial registration, study protocol or a publication reporting baseline results of an RCT, but not in the final report (Dyrbye 2016; Watanabe 2019). We did not consider the study by Rowe 1999, and the corresponding follow‐up reports, since hardiness, although mentioned several times in the reports, was only examined as correlate of burnout (main outcome of the study) and not the primary aim of the intervention. According to the primary investigators of the completed, but unpublished study NCT03914898, the content of the intervention programme did include resilience elements. Nevertheless, as the corresponding report (currently under review but provided to us by the study authors) only mentioned the term resilience when referring to other studies, we decided against including the study in this review. For NCT03753360, we obtained the information from the investigators that fostering resilience was not the primary focus of the intervention, but rather a secondary outcome. Therefore, we excluded this study also due to the ineligible intervention.
Two studies were excluded due to ineligible study design. Lahn 2014 was excluded because the "heartfelt emotion" (p 9) condition, which trained the resilience factor positive emotions and would have been relevant for this review, only served as second control condition and not as the intervention arm in this study. We excluded Maunder 2010 as the study involved a random assignment to three different doses of resilience intervention, but no control group.
Since they did not examine healthcare professionals, two studies were excluded due to ineligible population. NCT02417051 was conducted in a sample of active disaster responders that participated in relief efforts after Hurricane Sandy but included no healthcare professionals. We excluded Bian 2011 for a similar reason, as it evaluated the effectiveness of a coping training intervention for the Chinese Special Service Military Personnel as civil emergency responders. Although the training was provided partially by soldiers from a medical military team, healthcare professionals were not among the participants.
Appendix 16. Funnel plots
In order to assess reporting bias and to examine potential funnel plot asymmetry (see Assessment of reporting biases), we drew contour‐enhanced funnel plots for the comparison between resilience intervention and control for the four primary outcomes at post‐test with 10 or more included studies in the meta‐analysis (see Effects of interventions).
We drew a contour‐enhanced funnel plot for resilience at post‐intervention (Figure 116), which shows slight visual evidence of asymmetry (see Appendix 18).
6.
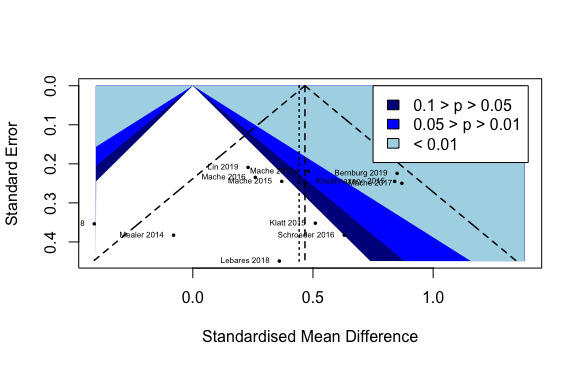
Figure A1. Contour‐enhanced funnel plot of comparison: comparison 1 Resilience intervention vs control, healthcare professionals, Resilience: post‐intervention.
The contour‐enhanced funnel plot for depression at post‐test (Figure 117) is rather symmetrical in shape and shows no visual evidence of asymmetry (see Appendix 18).
7.
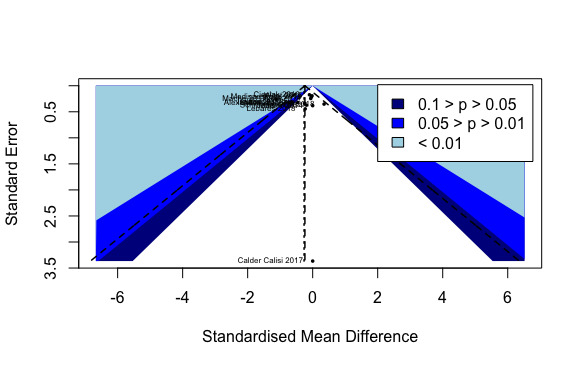
Figure A2. Contour‐enhanced funnel plot of comparison: comparison 1 Resilience intervention vs control, healthcare professionals, Depression: post‐intervention.
For stress or stress perception at post‐intervention, we also drew a contour‐enhanced funnel plot (Figure 118), which provides slight visual evidence of asymmetry (see Appendix 18).
8.
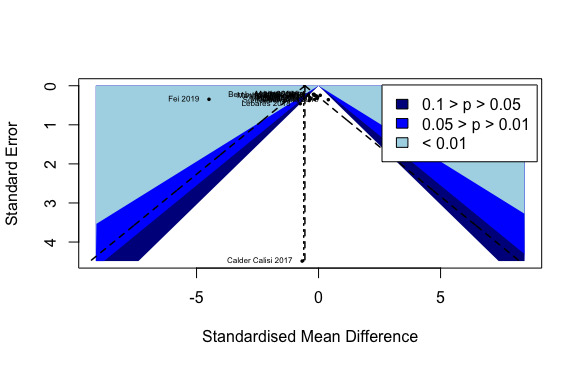
Figure A3. Contour‐enhanced funnel plot of comparison: comparison 1 Resilience intervention vs control, healthcare professionals, Stress or stress perception: post‐intervention.
Finally, the contour‐enhanced funnel plot for well‐being or quality of life at post‐intervention (Figure 119) is rather symmetrical in shape and shows no visual evidence of asymmetry (see Appendix 18).
9.
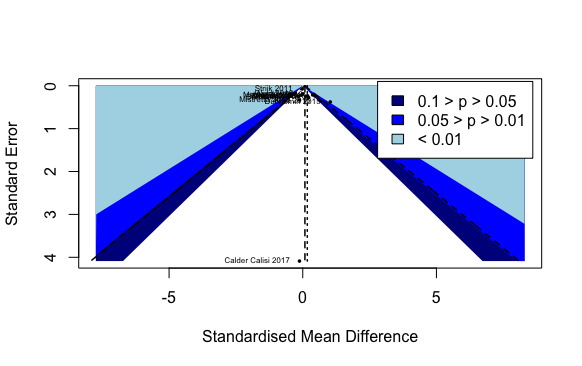
Figure A4. Contour‐enhanced funnel plot of comparison: comparison 1 Resilience intervention vs control, healthcare professionals, Well‐being or quality of life: post‐intervention.
Appendix 17. Further details on the overall completeness and applicability of evidence
Participants
Gender: Most study participants were female (e.g. proportion of female participants in 32 studies solely conducted in healthcare staff and reporting total numbers for participants' sex: 68.6%).
Age: The included studies mainly considered young professionals (e.g. junior physicians in Bernburg 2016) and middle‐aged employees up to approximately 50 years of age (Strijk 2011) (e.g. mean age across 25 studies solely conducted in healthcare workers and reporting age: 37.74 (SD 6.70) years).
Healthcare sectors: Various medical departments were represented (e.g. Psychiatry, Cardiology, Emergency, Surgery, Intensive Care Unit), with no clear majority of a certain healthcare sector.
-
Mental health at baseline:
15 of the 44 studies provided no data about the mental health status of the sample or only reported to include healthy participants.
All studies measuring mental functioning, used self‐report (screening) measures covering one or a small number of mental dysfunctions.
Comprehensive baseline diagnostics of mental health by the use of a structured interview were not conducted.
Five studies only included mentally healthy participants or individuals showing symptoms below a cut‐off in a screening measure. Two studies only considered participants without mental stress (not further specified) or without taking mood‐modulating drugs.
Overall, drawing from those studies assessing mental health, the severity of impairment ranged between (mostly) no mental symptoms (e.g. Strijk 2011; Wild 2016) to moderate and high levels of mental dysfunctions at least in a certain proportion of the sample, for example, compared to normative samples (e.g. Cheung 2014; Mealer 2014; West 2014).
-
Study location:
Most studies were from North America (20 studies), Europe (12 studies), and Asia (including the Near East; 9 studies). Only three studies were from Australia.
Thirty‐six studies took place in high‐income countries: Australia, Canada, Germany, Israel, Italy, Poland, The Netherlands, UK, and USA.
Eight studies were conducted in upper‐middle‐income countries: China, Iran, and Sri Lanka.
Interventions
The evidence found is restricted to certain types of intervention settings, delivery formats, training intensities and theoretical foundations.
Thirty of the 44 studies assessed the effectiveness of resilience interventions in group setting, whereas only eight were conducted in combined settings and four in individual settings (unclear setting for two studies).
The same pattern was seen for the delivery format of interventions with the majority of studies (29/44) investigating face‐to‐face delivery, followed by multimodal delivery (10/44; e.g. web‐based intervention and daily diary). We identified only three studies delivered in an online‐ or mobile‐based format.
Most of the interventions were of relatively high or moderate intensity (high: 18/44: > 12 hours or sessions; moderate: 15/44) compared to low‐intensity trainings (7/44) and studies with unclear training intensity (4/44). Treatment durations ranged considerably from a 40‐minute single session to 87 hours or 77 sessions in total.
Except for ACT and sole problem‐solving approaches, all theoretical foundations pre‐specified (Helmreich 2017) have been tested in RCTs found in this review. The number of RCTs varies with most studies investigating combined theoretical foundations (e.g. CBT and mindfulness).
Outcomes
Different measures for resilience in the review (see Table 3), ranging from resilience scales measuring resilience as trait (e.g. RS‐14), as summary of resilience factors (e.g. CD‐RISC) or as outcome (e.g. BRS).
Footnotes
ACT: acceptance and commitment therapy; BRS: Brief Resilience Scale; CBT: cognitive behavioural therapy; CD‐RISC: Connor‐Davidson Resilience Scale; RCTs: randomised controlled trials; RS‐14: Resilience Scale, 14 items; SD: standard deviation
Appendix 18. Assessment of publication bias for the primary outcomes (except anxiety)
| Outcome, time point (number of included studies) | Assessment of publication bias |
| Resilience, post‐test (12 studies) |
|
| Resilience, short‐term follow‐up (11 studies) |
|
| Depression, post‐test (14 studies) |
|
| Stress or stress perception, post‐test (17 studies) |
|
| Stress or stress perception, short‐term follow‐up (14 studies) |
|
| Well‐being or quality of life, post‐test (13 studies) |
|
| Well‐being or quality of life, short‐term follow‐up (12 studies) |
|
| df: Degrees of freedom; P: P value of Egger's test; SMD: standardised mean difference; t: T value of Egger's test. | |
Footnotes
aAccording to the GRADE approach (Guyatt 2011e), publication bias should be suspected when available evidence comes from a number of small studies, most of which have been commercially funded or when conflicts of interest are assumed.
Appendix 19. Prevention of potential biases by the search methods of this review
We performed extensive searches of relevant databases, checked reference lists, and considered grey literature. The search process was designed in conjunction with, and supervised by, the Cochrane Developmental, Psychosocial and Learning Problems (CDPLP) Information Specialist, in order to minimise bias in the acquisition of potentially relevant references. We contacted the authors of (included) studies to ask for, for example, full texts or additional data where reported data were insufficient or missing. In all phases of the review process, we repeatedly (at least twice) tried to contact the study authors by email, when needed.
Regarding data analysis, correspondence with the authors was required for 32 included studies. For 19 studies, the replies we received allowed us to include these studies in quantitative analysis (e.g. West 2014).
Data and analyses
Comparison 1. Resilience intervention versus control condition for healthcare professionals: main analyses (primary and secondary outcomes).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Resilience: post‐intervention | 12 | 690 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.25, 0.65] |
| 1.2 Resilience: short‐term follow‐up (≤ 3 months) | 11 | 1325 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.17, 0.67] |
| 1.3 Resilience: medium‐term follow‐up (> 3≤ 6 months) | 2 | 684 | Std. Mean Difference (IV, Random, 95% CI) | 0.35 [‐0.41, 1.11] |
| 1.4 Resilience: long‐term follow‐up (> 6 months) | 2 | 107 | Std. Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.08, 0.68] |
| 1.5 Anxiety: post‐intervention | 5 | 231 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.35, 0.23] |
| 1.6 Anxiety: short‐term follow‐up (≤ 3 months) | 4 | 133 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐0.98, ‐0.27] |
| 1.7 Depression: post‐intervention | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.50, ‐0.09] |
| 1.8 Depression: short‐term follow‐up (≤ 3 months) | 8 | 545 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.81, ‐0.23] |
| 1.9 Depression: medium‐term follow‐up (> 3 ≤ 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.10 Depression: long‐term follow‐up (> 6 months) | 2 | 87 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.33, 0.51] |
| 1.11 Stress or stress perception: post‐intervention | 17 | 997 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.07, ‐0.15] |
| 1.12 Stress or stress perception: short‐term follow‐up (≤ 3 months) | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.67, ‐0.25] |
| 1.13 Stress or stress perception: medium‐term follow‐up (> 3 ≤ 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.14 Stress or stress perception: long‐term follow‐up (> 6 months) | 3 | 173 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.84, 0.05] |
| 1.15 Well‐being or quality of life: post‐intervention | 13 | 1494 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.01, 0.30] |
| 1.16 Well‐being or quality of life: short‐term follow‐up (≤ 3 months) | 12 | 1413 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.04, 0.18] |
| 1.17 Well‐being or quality of life: medium‐term follow‐up (> 3 ≤ 6 months) | 3 | 1414 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.31, 0.16] |
| 1.18 Well‐being or quality of life: long‐term follow‐up (> 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.19 Social support: short‐term follow‐up (≤ 3 months) | 2 | 825 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.22, 0.08] |
| 1.20 Social support: medium‐term follow‐up (> 3 ≤ 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.21 Optimism: post‐intervention | 3 | 169 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [0.10, 0.72] |
| 1.22 Optimism: short‐term follow‐up (≤ 3 months) | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.12, 0.76] |
| 1.23 Self‐efficacy: post‐intervention | 6 | 461 | Std. Mean Difference (IV, Random, 95% CI) | 0.43 [0.25, 0.62] |
| 1.24 Self‐efficacy: short‐term follow‐up (≤ 3 months) | 7 | 1258 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [0.13, 0.51] |
| 1.25 Self‐efficacy: medium‐term follow‐up (> 3 ≤ 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.26 Self‐efficacy: long‐term follow‐up (> 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.27 Active coping: post‐intervention | 3 | 137 | Std. Mean Difference (IV, Random, 95% CI) | 0.28 [‐0.31, 0.87] |
| 1.28 Active coping: short‐term follow‐up (≤ 3 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.29 Active coping: medium‐term follow‐up (> 3 ≤ 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.30 Self‐esteem: short‐term follow‐up (≤ 3 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.31 Hardiness: post‐intervention | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.32 Hardiness: medium‐term follow‐up (> 3 ≤ 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.33 Positive emotions: post‐intervention | 2 | 212 | Std. Mean Difference (IV, Random, 95% CI) | 0.85 [0.17, 1.53] |
| 1.34 Positive emotions: short‐term follow‐up (≤ 3 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only |
Comparison 2. Resilience intervention versus control condition for healthcare professionals: subgroup analyses (primary outcomes).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Resilience: post‐intervention, subgroup analysis: setting | 12 | 690 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.25, 0.65] |
| 2.1.1 Group setting | 9 | 557 | Std. Mean Difference (IV, Random, 95% CI) | 0.50 [0.33, 0.67] |
| 2.1.2 Combined setting | 3 | 133 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.66, 0.97] |
| 2.2 Resilience: post‐intervention, subgroup analysis: delivery format | 12 | 690 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.25, 0.65] |
| 2.2.1 Face‐to‐face | 9 | 500 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.24, 0.71] |
| 2.2.2 Combined delivery | 3 | 190 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.13, 0.88] |
| 2.3 Resilience: post‐intervention, subgroup analysis: intensity | 12 | 690 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.25, 0.65] |
| 2.3.1 Moderate intensity | 2 | 67 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.85, 0.95] |
| 2.3.2 High intensity | 9 | 550 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.27, 0.66] |
| 2.3.3 Unclear intensity | 1 | 73 | Std. Mean Difference (IV, Random, 95% CI) | 0.84 [0.36, 1.32] |
| 2.4 Resilience: post‐intervention, subgroup analysis: theoretical foundation | 12 | 690 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.25, 0.65] |
| 2.4.1 Mindfulness‐based | 3 | 83 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.48, 0.82] |
| 2.4.2 Combination | 8 | 534 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.26, 0.67] |
| 2.4.3 Unspecific resilience training | 1 | 73 | Std. Mean Difference (IV, Random, 95% CI) | 0.84 [0.36, 1.32] |
| 2.5 Resilience: post‐intervention, subgroup analysis: comparator | 12 | 690 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.25, 0.65] |
| 2.5.1 Attention control | 1 | 21 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.52, 1.24] |
| 2.5.2 Waitlist control | 5 | 272 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.03, 0.79] |
| 2.5.3 No intervention control | 5 | 324 | Std. Mean Difference (IV, Random, 95% CI) | 0.43 [0.17, 0.69] |
| 2.5.4 Unspecified comparator | 1 | 73 | Std. Mean Difference (IV, Random, 95% CI) | 0.84 [0.36, 1.32] |
| 2.6 Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: setting | 11 | 1325 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.17, 0.67] |
| 2.6.1 Group setting | 9 | 1267 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [0.15, 0.68] |
| 2.6.2 Individual setting | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | 1.04 [0.28, 1.81] |
| 2.6.3 Combined setting | 1 | 26 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.94, 0.60] |
| 2.7 Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: delivery format | 11 | 1325 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.17, 0.67] |
| 2.7.1 Face‐to‐face | 8 | 1169 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.14, 0.77] |
| 2.7.2 Combined delivery | 3 | 156 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.04, 0.76] |
| 2.8 Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: intensity | 11 | 1325 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.17, 0.67] |
| 2.8.1 Low intensity | 3 | 98 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [‐0.14, 1.20] |
| 2.8.2 Moderate intensity | 1 | 733 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.20, 0.09] |
| 2.8.3 High intensity | 7 | 494 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.26, 0.66] |
| 2.9 Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: theoretical foundation | 11 | 1325 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.17, 0.67] |
| 2.9.1 Mindfulness‐based | 1 | 26 | Std. Mean Difference (IV, Random, 95% CI) | 1.05 [0.22, 1.88] |
| 2.9.2 Attention and interpretation therapy | 3 | 98 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [‐0.14, 1.20] |
| 2.9.3 Combination | 6 | 468 | Std. Mean Difference (IV, Random, 95% CI) | 0.43 [0.24, 0.62] |
| 2.9.4 Unspecific resilience training | 1 | 733 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.20, 0.09] |
| 2.10 Resilience: short‐term follow‐up (≤ 3 months), subgroup analysis: comparator | 11 | 1325 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.17, 0.67] |
| 2.10.1 Active control | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.68 [0.04, 1.32] |
| 2.10.2 Waitlist control | 6 | 993 | Std. Mean Difference (IV, Random, 95% CI) | 0.40 [0.01, 0.80] |
| 2.10.3 No intervention control | 4 | 292 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [0.11, 0.71] |
| 2.11 Depression: post‐intervention, subgroup analysis: setting | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.50, ‐0.09] |
| 2.11.1 Group setting | 9 | 457 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.69, ‐0.13] |
| 2.11.2 Individual setting | 1 | 134 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.68, 0.01] |
| 2.11.3 Combined setting | 3 | 106 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.32, 0.69] |
| 2.11.4 Unclear setting | 1 | 91 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.46, 0.38] |
| 2.12 Depression: post‐intervention, subgroup analysis: delivery format | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.50, ‐0.09] |
| 2.12.1 Face‐to‐face | 10 | 499 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.65, ‐0.05] |
| 2.12.2 Combined delivery | 3 | 198 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.55, 0.01] |
| 2.12.3 Unclear delivery format | 1 | 91 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.46, 0.38] |
| 2.13 Depression: post‐intervention, subgroup analysis: intensity | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.50, ‐0.09] |
| 2.13.1 Moderate intensity | 6 | 395 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.47, 0.01] |
| 2.13.2 High intensity | 6 | 262 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.82, 0.11] |
| 2.13.3 Unclear intensity | 2 | 131 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.98, 0.32] |
| 2.14 Depression: post‐intervention, subgroup analysis: theoretical foundation | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.50, ‐0.09] |
| 2.14.1 Mindfulness‐based | 3 | 83 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.42, 0.45] |
| 2.14.2 Cognitive behavioural therapy | 1 | 134 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.68, 0.01] |
| 2.14.3 Combination | 6 | 293 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.87, ‐0.01] |
| 2.14.4 Unspecific resilience training | 4 | 278 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.53, 0.08] |
| 2.15 Depression: post‐intervention, subgroup analysis: comparator | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.50, ‐0.09] |
| 2.15.1 Attention control | 2 | 155 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.64, ‐0.00] |
| 2.15.2 Active control | 1 | 44 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐1.26, ‐0.04] |
| 2.15.3 Treatment as usual | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.35, ‐0.07] |
| 2.15.4 Waitlist control | 4 | 215 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.28, 0.32] |
| 2.15.5 No intervention control | 6 | 334 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.71, 0.05] |
| 2.16 Stress or stress perception: post‐intervention, subgroup analysis: setting | 17 | 997 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.07, ‐0.15] |
| 2.16.1 Group setting | 15 | 918 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.12, ‐0.15] |
| 2.16.2 Combined setting | 2 | 79 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.85, 0.52] |
| 2.17 Stress or stress perception: post‐intervention, subgroup analysis: delivery format | 17 | 997 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.07, ‐0.15] |
| 2.17.1 Face‐to‐face | 14 | 838 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.26, ‐0.15] |
| 2.17.2 Combined delivery | 3 | 159 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.81, 0.35] |
| 2.18 Stress or stress perception: post‐intervention, subgroup analysis: intensity | 17 | 997 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.07, ‐0.15] |
| 2.18.1 Moderate intensity | 6 | 307 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐2.24, 0.58] |
| 2.18.2 High intensity | 11 | 690 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.75, ‐0.20] |
| 2.19 Stress or stress perception: post‐intervention, subgroup analysis: theoretical foundation | 17 | 997 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.07, ‐0.15] |
| 2.19.1 Mindfulness‐based | 4 | 115 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.63, 0.28] |
| 2.19.2 Combination | 12 | 843 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.38, ‐0.20] |
| 2.19.3 Unspecific resilience training | 1 | 39 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.68, 0.58] |
| 2.20 Stress or stress perception: post‐intervention, subgroup analysis: comparator | 17 | 997 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.07, ‐0.15] |
| 2.20.1 Attention control | 1 | 21 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.65, 0.15] |
| 2.20.2 Active control | 1 | 44 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.95, 0.25] |
| 2.20.3 Waitlist control | 6 | 316 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.91, 0.05] |
| 2.20.4 No intervention control | 9 | 616 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.51, 0.02] |
| 2.21 Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: setting | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.67, ‐0.25] |
| 2.21.1 Group setting | 12 | 730 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.67, ‐0.20] |
| 2.21.2 Individual setting | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.68, ‐0.17] |
| 2.21.3 Combined setting | 1 | 26 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐1.24, 0.32] |
| 2.22 Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: delivery format | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.67, ‐0.25] |
| 2.22.1 Face‐to‐face | 10 | 596 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.74, ‐0.18] |
| 2.22.2 Combined delivery | 4 | 192 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.78, ‐0.20] |
| 2.23 Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: intensity | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.67, ‐0.25] |
| 2.23.1 Low intensity | 3 | 97 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.16, ‐0.32] |
| 2.23.2 Moderate intensity | 2 | 76 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.93, 0.01] |
| 2.23.3 High intensity | 9 | 615 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.68, ‐0.12] |
| 2.24 Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: theoretical foundation | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.67, ‐0.25] |
| 2.24.1 Mindfulness‐based | 1 | 26 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐1.97, ‐0.29] |
| 2.24.2 Attention and interpretation therapy | 3 | 97 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.16, ‐0.32] |
| 2.24.3 Combination | 9 | 626 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.60, ‐0.08] |
| 2.24.4 Unspecific resilience training | 1 | 39 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.34, ‐0.04] |
| 2.25 Stress or stress perception: short‐term follow‐up (≤ 3 months), subgroup analysis: comparator | 14 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.67, ‐0.25] |
| 2.25.1 Active control | 1 | 39 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.45, ‐0.14] |
| 2.25.2 Waitlist control | 5 | 260 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐0.96, ‐0.45] |
| 2.25.3 No intervention control | 8 | 489 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.55, ‐0.01] |
| 2.26 Well‐being or quality of life: post‐intervention, subgroup analysis: setting | 13 | 1494 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.01, 0.30] |
| 2.26.1 Group setting | 11 | 718 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [0.01, 0.37] |
| 2.26.2 Combined setting | 2 | 776 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.17, 0.13] |
| 2.27 Well‐being or quality of life: post‐intervention, subgroup analysis: delivery format | 13 | 1494 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.01, 0.30] |
| 2.27.1 Face‐to‐face | 10 | 1335 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.07, 0.16] |
| 2.27.2 Combined delivery | 3 | 159 | Std. Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.16, 0.95] |
| 2.28 Well‐being or quality of life: post‐intervention, subgroup analysis: intensity | 13 | 1494 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.01, 0.30] |
| 2.28.1 Moderate intensity | 4 | 210 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [‐0.16, 0.84] |
| 2.28.2 High intensity | 9 | 1284 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.06, 0.17] |
| 2.29 Well‐being or quality of life: post‐intervention, subgroup analysis: theoretical foundation | 13 | 1494 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.01, 0.30] |
| 2.29.1 Mindfulness‐based | 2 | 66 | Std. Mean Difference (IV, Random, 95% CI) | 0.83 [0.32, 1.33] |
| 2.29.2 Coaching | 1 | 730 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.17, 0.13] |
| 2.29.3 Combination | 9 | 591 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.03, 0.31] |
| 2.29.4 Unspecific resilience training | 1 | 107 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.38, 0.38] |
| 2.30 Well‐being or quality of life: post‐intervention, subgroup analysis: comparator | 13 | 1494 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.01, 0.30] |
| 2.30.1 Active control | 1 | 730 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.17, 0.13] |
| 2.30.2 Waitlist control | 5 | 309 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [0.03, 0.79] |
| 2.30.3 No intervention control | 7 | 455 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.09, 0.28] |
| 2.31 Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: setting | 12 | 1413 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.04, 0.18] |
| 2.31.1 Group setting | 10 | 1355 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.06, 0.16] |
| 2.31.2 Individual setting | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | 0.62 [‐0.12, 1.36] |
| 2.31.3 Combined setting | 1 | 26 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.77, 0.77] |
| 2.32 Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: delivery format | 12 | 1413 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.04, 0.18] |
| 2.32.1 Face‐to‐face | 9 | 1260 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.06, 0.23] |
| 2.32.2 Combined delivery | 3 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.11, 0.52] |
| 2.33 Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: intensity | 12 | 1413 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.04, 0.18] |
| 2.33.1 Low intensity | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.29, 0.93] |
| 2.33.2 Moderate intensity | 3 | 850 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.23, 0.53] |
| 2.33.3 High intensity | 7 | 505 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.06, 0.29] |
| 2.34 Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: theoretical foundation | 12 | 1413 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.04, 0.18] |
| 2.34.1 Attention and interpretation therapy | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.29, 0.93] |
| 2.34.2 Combination | 8 | 542 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.05, 0.28] |
| 2.34.3 Unspecific resilience training | 2 | 813 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.35, 0.73] |
| 2.35 Well‐being or quality of life: short‐term follow‐up (≤ 3 months), subgroup analysis: comparator | 12 | 1413 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.04, 0.18] |
| 2.35.1 Waitlist control | 4 | 881 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.15, 0.42] |
| 2.35.2 Treatment as usual | 1 | 80 | Std. Mean Difference (IV, Random, 95% CI) | 0.51 [0.07, 0.95] |
| 2.35.3 No intervention control | 7 | 452 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.11, 0.26] |
Comparison 3. Resilience intervention versus control condition for healthcare professionals: sensitivity analyses (primary outcomes).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alexander 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): target recruitment and enrolment was 50 participants, with 25 in each group. This recruitment goal allowed for 10% attrition, with the expectation that 40 participants would complete the study; assumption based on a power analysis in G*Power, which indicated that for a repeated measures ANOVA with interaction effects, a minimum sample of 40 was needed to find significance with a moderate effect size (Cohen’s f = 0.25), α = 0.05, power = 0.80, and an estimated correlation among repeated measures of 0.40 Imputation of missing data: not applicable since all participants remained in the study |
|
| Participants |
Country: USA Setting: urban (560‐bed) teaching hospital as host of yoga research study Age: mean = 46.38 (SD = 10.23) years Sample size (randomised): 40 Sex: 39 women, 1 man Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: in MBI: burnout, emotional exhaustion: IG = 17.60 (10.36), CG = 20.40 (13.19); burnout, depersonalisation: IG = 4.05 (5.09), CG = 4.35 (3.83); burnout, personal accomplishment: IG = 37.15 (8.53), CG = 36.10 (9.93) Population description: nurses within partner hospital system Inclusion criteria: 1) being a nurse within the partner hospital system; 2) no prior experience with yoga practice; 3) willingness to complete 8 weekly sessions and homework exercises; 4) willingness to be randomly assigned to IG or CG Exclusion criteria: 1) serious illness or major orthopedic diagnoses of the neck, back, pelvis, or lower extremities that could interfere with completion of the yoga intervention protocol Attrition (withdrawals and exclusions): information received from authors (Alexander 2019 [pers comm]): all participants remained in the study Reasons for missing data: not relevant |
|
| Interventions |
Intervention: yoga intervention (supervised yoga instruction) (n = 20)
Control: treatment as usual (not further specified) (n = 20) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors to get the information about potential attrition and missing data in the study as well as the number of participants analysed for the outcomes reported in Table 3 (Alexander 2019 [pers comm]). Study start/end date: not specified Funding source: following financial support for the research, authorship, and/or publication of this article: research supported by the Research and Creative Activities Fund of Texas Christian University Declaration of interest: no potential conflicts of interest with respect to the research, authorship, and/or publication of this article Ethical approval needed/obtained for study: approved by the IRB at the affiliated university Comments by study authors: not specified Miscellaneous outcomes by the review authors: information received from authors (Alexander 2019 [pers comm]): all participants remained in the study Correspondence: Gina K. Alexander, PhD, Assistant Professor, Texas Christian University, Harris College of Nursing and Health Sciences, TCU Box 298620, Fort Worth, Texas 76129, USA; g.alexander@tcu.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After individuals completed consent forms and baseline assessments, they were enrolled in the study and randomized to the intervention (yoga) or usual care control group." Quote: "no significant differences in demographics were found between the control and experimental groups, suggesting that the two groups were similar in demographic makeup and the research team did not need to control for demographic characteristics in the primary analyses." Quote: "No significant differences between the intervention and control groups were found at baseline (p > .05)." Judgement comment: insufficient information about random sequence generation to permit judgment of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic characteristics and outcome variables (P > .05) on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: information received from authors: all participants remained in the study |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Berger 2011.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
|
| Participants |
Country: Israel Setting: well baby clinics Age: mean = 48.5 (SD = 7.26) years Sample size (randomised): 80 Sex: 80 women Comorbidity (mean (SD) of respective measures in indicated, if available at baseline): baseline results for secondary traumatisation factors (ProQOL scale) compared to norms based on 2 large‐scale studies, of CP samples and MHCPs in the USA: higher levels of compassion fatigue (22.5% in this sample vs 13% in CP and 13.2% in the MHCP) and burnout (32.5% in this sample vs 23% in CP and 13% in MHCP) and higher levels of lack of compassion satisfaction (68.7% in this sample vs 37.0% in CP and 39.3% in MHCP) Population description: 90 well baby clinic nurses living under chronic threat of war and terror; from the most affected areas in the north and the south of Israel Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: well baby clinic staff preparedness programme (n = 42)
Control: wait‐list control (n = 38) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) 3‐month follow‐up (3 months post‐intervention during follow‐up session) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: intervention took place between February and May 2007; exact study dates not specified Funding source: funding of the intervention by the ministry of health (no other roles) Declaration of interest: none declared Ethical approval needed/obtained for study: ethical approval by University of Haifa ethics committee Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Marc Gelkopf, Lev‐Hasharon Mental Health Center, POB 90000, Netanya 42100, Israel; emgelkopf@013.net.il; Tel.: +972 54 571 4344/9 8981169; fax: +972 9 894 5054: Rony Berger: riberger@netvision.net.il |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "From the 80 who agreed, using a random number generator procedure, 42 WBC nurses received the intervention, while 38 were put on a control condition waiting list (WL)." Quote: "The demographic and exposure data are presented in Table 1. Univariate analyses comparing all the demographic and exposure variables showed no significant differences between the groups." Judgement comment: The investigators describe a random component in the sequence generation process (random‐number generator) and there is verified baseline comparability of groups for demographic and exposure variables.; baseline comparability for outcome variables unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (unclear if there were any missing data and if missing data were imputed, for example) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available, but it is clear that the published report includes all expected outcomes, including those that were prespecified |
Bernburg 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
|
| Participants |
Country: Germany Setting: department of paediatric clinics (of 10 hospitals) Age: mean = 27 (SD = 2.1) years Sample size (randomised): 54 Sex: 38 women, 16 men Comorbidity (mean (SD) of respective measures in indicated, if available at baseline: not specified Population description: junior physicians working in department of paediatric clinics from 10 hospitals Inclusion criteria: 1) employment in paediatrics; 2) working full‐time in a hospital; 3) work experience of < 2 years; 4) being able and willing to participate; 5) agreement to complete 3 questionnaires Exclusion criteria: not specified Attrition (withdrawals and exclusions): high response rate; dropout rate (loss to follow‐up) was very low; number of withdrawals or exclusions not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: PCT (n = 26)
Control: no intervention; comparison group did not receive any support related to the intervention topic such as any other psychosocial skills training, counselling, or therapy (n = 28) |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (after 3‐month intervention); 3) 3‐month follow‐up (3 months post‐intervention/6 months after baseline) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: performed between May 2014 to October 2014 Funding source: no funding support Declaration of interest: no conflicts of interest declared Ethical approval needed/obtained for study: ethical approval by the Free University Berlin Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Monika Bernburg: akinomber@hotmail.com; corresponding author: Stefanie Mache, Institute of Occupational Medicine, Social Medicine and Environmental Medicine, Goethe‐University, Theodor‐Stern‐Kai 7, 60590 Frankfurt am Main, Germany; Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf, Seewartenstrasse 10, 20459 Hamburg, Germany; s.mache@uke.de |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Study participants were randomized into two groups (intervention and comparison group): (1) names of the pediatricians were listed in alphabetical order and (2) afterwards each name got a random number. The numbers had been allocated from number tables to the intervention or comparison group." Quote: "The fact that, although the comparison group and the intervened group shared similar levels of perceived job stress at baseline" Quote: "Baseline data on socio‐demographic differences indicate only small, insignificant differences between our intervention and comparison group." Judgement comment: The investigators describe a random component in the sequence generation process (random‐number table) and there is verified baseline comparability of groups for some sociodemographic variables and perceived stress.; baseline comparability for other outcome variables (job satisfaction, work engagement) unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (online questionnaires); but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "The high response rate in this study demonstrates a further strength: the drop‐out rate (loss to follow‐up) was very low." Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (dropout rate is unclear; unclear if missing data were imputed, for example) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available, but it is clear that the published report includes all expected outcomes, including those that were prespecified |
Bernburg 2019.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. without the 6 participants who were excluded due to sickness absence) |
|
| Participants |
Country: Germany Setting: nurses working in psychiatric hospital departments; training modules conducted off‐duty; training setting not specified Age: mean = 32.03 (SD = 2.4) years Sample size (randomised): 92 Sex: 69 women, 17 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: perceived stress in PSQ: IG = 3.34 (0.49), CG = 3.49 (0.50) Population description: nurses working in psychiatric hospital departments Inclusion criteria: 1) employment as a full‐time nurse in a psychiatric hospital department; 2) time to take part in the study over the whole time period; 3) written consent to finish the surveys (at baseline and 3 follow‐up periods) Exclusion criteria: not specified Attrition (withdrawals and exclusions): 6 exclusions (group not specified) Reasons for missing data: sickness absence (n = 6) |
|
| Interventions |
Intervention: mental health promotion intervention (n = not specified; after n = 6 total exclusions: n = 44)
Control: wait‐list control (n = not specified; after n = 6 total exclusions: n = 42); no training, but answers to all surveys included in the study |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (at 3 months, i.e. at the end of 3‐month intervention; follow‐up 1); 3) 3‐month follow‐up (at 6 months, i.e. 3 months after end of 3‐month intervention; follow‐up 2); 4) 9‐month follow‐up (at 12 months, i.e. 9 months after 3‐month intervention; follow‐up 3) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to ask about the number of exclusions per group and whether it is correct that they performed per‐protocol analysis with n = 44 in IG and n = 42 in CG for the outcomes reported in Table 2 (Mache 2019a [pers comm]). Study start/end date: not specified Funding source: not specified Declaration of interest: no conflict of interest to disclose Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Monika Bernburg: akinomber@hotmail.com; corresponding author: Stefanie Mache, Institute of Occupational Medicine, Social Medicine and Environmental Medicine, Goethe‐University, Theodor‐Stern‐Kai 7, 60590 Frankfurt am Main, Germany; Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf, Seewartenstrasse 10, 20459 Hamburg, Germany; s.mache@uke.de |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "This study is designed as randomized controlled pilot study." Quote: "Afterwards, these nurses were randomized into two study groups through a computer‐generated algorithm." Quote: "Socio‐demographics are illustrated in Table 1. We found no significant differences between intervention and WCG with regard to gender, age, and working experience." Judgement comment: The investigators describe a random component in the sequence generation process (computer‐generated algorithm) and there is verified baseline comparability of groups for sociodemographic characteristics (see Table 1); baseline comparability for outcomes (i.e. statistical (non) significance in Table 2) not specified |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (online surveys); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Due to sickness absence, six nurses were excluded. So in the end, 44 nurses were included in the intervention group (IG) and 42 nurses took part in the waitlist control group (WCG)." Judgement comment: reasons for missing data unlikely to be related to true outcome (see reasons for missing data: sickness absence); number of participants randomised to each group and excluded from each group not stated; per‐protocol analysis (only participants who took part in 2 groups) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Calder Calisi 2017.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): power not specified; small sample size of pilot study a limitation, as does not allow for a large enough change between the 2 groups pre‐ and post‐intervention Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. 7 dropouts excluded) |
|
| Participants |
Country: USA
Setting: Massachusetts General Hospital
Age: range = 27 ‐ 60 years
Sample size (randomised): 53
Sex: 53 women (nurses)
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: state anxiety (State Trait Anxiety Inventory, STAI): IG = 38.40 (6.65), CG = 38.14 (7.56); anxiety (Visual Analog Scale, VAS; range = 0 (no anxiety) to 7 (most anxiety)): IG = 3.92 (1.44), CG = 3.59 (1.26); depression (VAS; range = 0 ‐ 7): IG = 2.68 (1.49), CG = 2.86 (1.58) Population description: (cardiac) nurses Included criteria: not specified Excluded criteria: not specified Attrition (withdrawals and exclusions): 7 (13.2%) discontinued the study Reasons for missing data: not specified as participants provided no reasons for withdrawing a |
|
| Interventions |
Intervention: Relaxation Response (RR) (n randomised = not specified; after 7 dropouts, n = 24)
Control: wait‐list control (n randomised not specified; after n = 7 dropouts: n = 22; eligible to receive the class at the end of the study, if they so desired) |
|
| Outcomes |
Outcomes collected and reported:
Time points measure and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to receive the means and SDs for all outcomes at post‐intervention (instead of change scores), but received no response to 2 inquiries Study start/end date: not specified Funding source: Make a Difference Grant at Massachusetts General Hospital Declaration of interest: not specified Ethical approval needed/obtained for study: approved by hospital IRB Comments by study authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Catherine Calder Calisi, Massachusetts General Hospital, 36 Arrowwood Street, Methuen, Massachusetts 01844; ccalder1@partners.org |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "This pilot study used a randomized, wait‐list control, quantitative study design" Quote: "The nurses who agreed to voluntary participation were randomized into either the wait‐list control group or the intervention group." Quote: "As shown in Table 1, the two study groups were well balanced at baseline with respect to state‐trait anxiety as well as the semantic differential scale measures of anxiety, depression, well‐being, work‐related stress, and confidence teaching the RR." Judgement comment: insufficient information about random sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for outcome variables on the basis of analysis (see Table 1; all P values > 0.31); baseline comparability for sociodemographic characteristics not specified |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (in part face‐to‐face intervention in class) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Forty‐six nurses (all female) completed the study (24 nurses in the intervention group and 22 nurses in the control group) of the 53 registered nurses who enrolled in the study." Quote: "However, 7 participants (13.2%) discontinued the study without providing reasons for withdrawal." Judgement comment: unclear if reasons for missing data are related to true outcome (number of participants randomised to each group is not stated; n = 7 dropouts, but unclear which group); per‐protocol analysis (i.e. only participants who completed the study) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available, but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Chesak 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; per‐protocol analysis with participants who complied with allocated intervention and for whom outcomes were obtained |
|
| Participants |
Country: USA Setting: nurse orientation programme at Mayo Clinic Age: mean = 28.16 (SD = 8.29) years Sample size (randomised): 55 Sex: 38 women, 2 men (in analysed sample) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: anxiety GAD‐7: IG = 3.11 (2.76), CG = 4.25 (2.77) Population description: nurses who were new to the institution or transitioning to a new unit or new role and who were undergoing new‐nurse orientation Inclusion criteria: 1) registered nurses (RN) who were enrolled in 1 of 2 designated nurse orientation classes; 2) RNs who were willing and able to participate in all aspects of the study; 3) RNs who were provided with, understood, and signed the informed consent Exclusion criteria: 1) if they reported currently or recently (within the past 6 months) experiencing a psychotic episode; 2) if they reported a clinically significant acute psychiatric event, or a physical illness Attrition (withdrawals and exclusions): 4 withdrawals before the intervention (IG = 2, CG = 2); total number of withdrawals: n = 15 (IG = 8/27 (29.6%), CG = 7/28 (25%)); i.e. 40 completed the study (IG = 19, CG = 21) Reasons for missing data: 4 withdrawals before the intervention: declined to participate in allocated group prior to first group session; not exactly specified for further withdrawals (nurse participants who voluntarily dropped out of the study: inability to make time for the programme) |
|
| Interventions |
Intervention: Stress Management and Resiliency Training (SMART) (n = 27)
Control: active control (n = 28)
|
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Time points measured and reported: 1) pre‐intervention; 2) 3‐month follow‐up (3 months after single‐session intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: not specified Funding source: not specified Declaration of interest: Dr Sood has a proprietary interest in a company that teaches resiliency programmes. The other authors have no financial or proprietary interest in the subject matter of this article. Ethical approval needed/obtained for study: IRB‐approved trial Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Sherry S. Chesak, PhD, Department of Nursing, Mayo Clinic, 200 First St. SW Rochester, Minnesota 55905Tel: (507) 255‐3236; chesak.sherry@mayo.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized into either the intervention or control group through the use of a random number generator." Judgement comment: The investigators describe a random component in the sequence generation process (random‐number generator); no information about comparability of groups at baseline or respective analysis (statistical (non)significance of differences in demographic variables unclear; baseline comparability for outcome variables not specified |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (online questionnaires); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "55 consented and were randomized ‐ 27 into the intervention arm and 28 into the control arm. Prior to the first group session, 2 participants from each group declined to participate." Quote: "Analysis was restricted to participants who completed the study, including all follow‐up assessments." Quote: "Forty subjects (19 intervention, 21 control) completed the baseline and follow‐up assessments. Some subjects did not complete all scales at both time points. Data are presented only for those who completed the given scale at both baseline and follow‐up." Judgement comment: reasons for missing data unlikely to be related to true outcome with relative balance in missing data between groups (IG: n = 8, CG: n = 7); no reasons for missing data stated for each group; per‐protocol analysis with participants who complied with allocated intervention and for whom outcomes were obtained |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available, but it is clear that the published report includes all expected outcomes, including those that were prespecified |
Cheung 2014.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): Based on a small effect size of Cohen’s d = 0.2 for the outcome measures, and an attrition rate of 30% during the 6‐month follow‐up, sample sizes of 259 in each arm could achieve a power of 0.80 to detect a significant difference. A total sample of 518 was needed (Machin 1997); however, interest from the AMS was higher than expected and the total sample size immediately pre‐training (n = 802) was higher than the sample size that was needed Imputation of missing data: no imputation of missing data; per‐protocol analysis (only participants who completed allocated intervention, i.e. without 2 participants in IG who did not complete PFA intervention) and available case analysis (only participants for whom outcomes were obtained) |
|
| Participants |
Country: China (including Hong Kong) Setting: AMS of the Hong Kong Special Administrative Region Age: mean = 37.38 (SD = 11.78) years Sample size (randomised): 918 Sex: 412 women, 391 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: general psychopathology in GHQ‐28: IG = 0.67 (0.31), CG = 0.60 (0.32); psychological distress in DASS‐21: IG = 0.80 (0.57), CG = 0.76 (0.57); distress from traumatic exposure IES‐R: IG = 0.68 (0.64), CG = 0.60 (0.67); significantly higher depression and anxiety symptoms than normative sample of university students (P < 0.001); significantly lower stress symptoms than normative sample (P < 0.001) Population description: members of AMS of the Hong Kong Special Administrative Region, a government division responsible for providing voluntary supplementary medical and health service in times of community emergency; voluntary first responders of the AMS with and without previous trauma exposure Inclusion criteria: 1) first responders, including fire fighters, police, ambulance officers, rescuers and auxiliary medical personnel; 2) with and without previous trauma exposure (see appendix of the publication, information from trial registration) Exclusion criteria: interested individuals with psychiatric history or current diagnosis of psychiatric disorders (see appendix of the publication, information from trial registration) Attrition (withdrawals and exclusions): between randomisation and pre‐intervention assessment: 116 withdrawals (IG = 63, CG = 53); between pre‐ and post‐intervention (during training): 2 withdrawals (IG = 2); 67 withdrawals between post‐intervention and 3‐month follow‐up (IG = 29; CG = 38); 109 withdrawals between 3‐month follow‐up and 6‐month follow‐up (IG = 45; CG = 64); completion rate for total trial (i.e. from pre‐intervention assessment to 6‐month follow‐up): IG = 80%, CG = 75% Reasons for missing data: not specified |
|
| Interventions |
Intervention: PFA (n = 458)
Control: wait‐list control (n = 460) |
|
| Outcomes |
Outcomes collected and reported: Primary outcomes:
Secondary outcomes:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (only IN IG); 3) 3‐month follow‐up (3‐months post‐intervention); 6) 6‐month follow‐up (6 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: April 2011 to November 2011 Funding source: Chinese University of Hong Kong (CUHK) Direct Grant for Research #2009.2.041; Student Research Grant (see trial registration) Declaration of interest: not specified Ethical approval needed/obtained for study: ethics approvals from Survey and Behavioral Research Ethics Committee and Clinical Research Ethics Committee Comments by authors: registered at the CUHK Centre for Clinical Trials, Clinical Trials Registry (CUHK‐CCT00278) Miscellaneous outcomes by the review authors: dissertation Correspondence: Yee Lai Eliza Cheung, School of Public Health and Primary Care, CUHK; eliza.cheung@cuhk.edu.hk; chair: Prof. Yeung Shan Samuel Wong; supervisor: Prof. Ying Yang Emily Chan; The Jockey Cluc School of Public Health and Primary Care, CUHK, Ngan Shing St, Sha Tin, Hongkong; emily.chan@cuhk.edu.hk |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Computerized randomization was conducted using SPSS." Quote: "Participants were then randomly assigned to the waitlist control group or the PFA group using random numbers generated by SPSS." Quote: "Means and standard deviations of outcome variables across conditions at Time 1, Time 1b (post‐training), Time 2 (3‐month follow‐up), and Time 3 (6‐month follow‐up) were presented in Table 9. Daggers denote significant differences of the baseline scores between intervention and control group" Quote: "At Time 1, no significant differences were found between intervention and control groups for age, gender, income, occupations, education, marital status, and previous training in post‐disaster psychological interventions" Quote: "Meanwhile, significant difference was found for trauma history between intervention and controls groups, χ²=63.40, p<.001. There was 67.8% of the intervention group reported prior traumatic experience while 39.8% of the control did that. Intervention group reported proportionately more prior traumatic experience than control group despite randomization." Judgement comment: The investigators describe a random component in the sequence generation process (computerised randomisation) and there is verified baseline comparability between groups for most sociodemographic characteristics except for trauma history/prior traumatic experience between groups; no significant baseline differences between groups in most outcome variables (psychological distress, distress from exposure to trauma, maladaptive coping, resilience and social support); however, significant baseline differences in self‐efficacy, knowledge of PFA and disaster mental health, general psychopathology, adaptive coping and life satisfaction |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Quote: "Investigators and authorized research assistants were responsible for data collection and consolidation. Main researcher who was also the trainer in the Psychological first aid training had access only to the anonymous dataset for further analyses due to the protection of participants’ anonymity." Judgement comment: insufficient information about blinding of outcome assessment (paper‐pencil and online questionnaires; unclear if investigators and research assistants responsible for data collection were blinded); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Figure 4. Algorithm of the randomized controlled study" Quote: "Among the 458 participants assigned to training intervention, 395 of them joined 9 identical training sessions on the training days from April to June 2011. A total of 393 completed pre‐post questionnaires (Appendix VI) were received at Time 1 and Time 1b, 364 participants completed the 3‐month follow‐up questionnaire at Time 2, and 319 at 6‐ month follow‐up at Time 3. Among the waitlist control group, 407 out of 460 filled the questionnaires and 53 withdrew from the study before it starts and 369 participants completed the 3‐month follow‐up questionnaire. At 6‐month follow up, 305 filled in the questionnaire (Figure 4 for the flow of the study). The completion rate of intervention arm is 80% while that of control group is 75%." Judgement comment: reasons for missing data likely to be related to true outcome with imbalance in missing data between groups (over study course: IG: n = 139; CG: n = 155); reasons for missing data in groups not stated; available‐case analysis (only participants for whom outcomes were obtained; see Table 9) and per‐protocol analysis (only participants who completed allocated intervention, i.e. without n = 2 participants in IG who did not complete PFA intervention) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: trial registration available (registered at the CUHK Centre for Clinical Trials,Clinical Trials Registry (Appendix V); CUHK_CCT00278); all of the study’s prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way; only actual psychological support provided/actual helping behaviour was not analysed and could therefore not be reported (too small numbers for statistical analyses) |
Cieslak 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Power (power sample size calculation, level of power achieved): not specified Unit of randomisation: individuals Imputation of missing data: 85 in IG2 excluded due to high dropout; for missing data in IG1 and CG: multiple imputation method (imputation with regression procedures; estimated maximisation); intention‐to‐treat analysis for these 2 groups only |
|
| Participants |
Country: Poland Setting: health and human service professionals; setting not specified; designated website Age: mean = 37.49 (SD = 10.39) years Sample size (randomised): 253 (in total randomised to 3 groups); 168 participants in IG1 and CG reported here Sex: 131 women, 37 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: STSS: IG1 = 2.26 (0.58), CG = 2.42 (0.66); burnout (OLBI) at baseline: IG1 = 2.86 (0.51); CG = 3.00 (0.71) Population description: health and human service professionals (e.g. physicians, nurses, first responders, social workers, psychotherapists, education specialists, police officers and firefighters, other human service providers) exposed indirectly to traumatic events at work Inclusion criteria: 1) providing services for survivors of traumatic events for at least 1 year; 2) experiencing indirect exposure to a traumatic event at work; 3) consent for participating in an internet‐based programme aiming at the enhancement of psychosocial resources improving mental health Exclusion criteria: professionals without exposure to trauma Attrition (withdrawals and exclusions): IG2 = 85 exclusions due to high dropout at post‐intervention (62%) and follow‐up (78%); 86 (51.2%) exclusions in 2 other groups because did not respond to questionnaire at post‐intervention (IG1 = 46/87 (52.9%), CG = 40/81 (49.4%)); 100 (59.5%) did not respond to questionnaires at follow‐up (IG1 = 54/87 (62.1%), CG = 46/81 (56.8%)); only 68 participants completed all IG1/CG procedures and participated in 3 measurements Reasons for missing data: 54/168 participants in IG1 and CG gave reasons for withdrawal: e.g. personal reasons not related to intervention (39%), technical problems with website or internet access (15%) |
|
| Interventions | In total, 2 intervention groups (self‐efficacy‐enhancement module and social support‐enhancing module) and 1 control group (educational module); social support‐enhancing module (n = 85) was not included in analyses due to high dropout Intervention: self‐efficacy enhancement module of 'The Helpers’ Stress' (n = 87)
Control: attention control (educational module of “The Helpers’ Stress”) (n = 81)
|
|
| Outcomes |
Outcomes collected and reported:
(indirect exposure to traumatic events at work is not an outcome measure; only assessed at time 1) Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 1‐month follow‐up (1‐month post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to get the information whether Cieslak 2016 and Rogala 2016 were two reports on the same study. We also asked for the subgroup data for health and human service professionals (physicians, nurses, first responders, social workers, psychotherapists) (Rogala 2019 [pers comm]). Study start/end date: recruitment between October 2012 and May 2013; exact study dates not specified Funding source: created as part of the N N106 139537 grant awarded by the Ministry of Science and Higher Education and currently administered by Narodowe Centrum Nauki (contract No. 1395/B/H03/2009/37), implemented at the SWPS (University of Social Sciences and Humanities). Project manager: Dr Roman Cieślak Declaration of interest: research conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest Ethical approval needed/obtained for study: approved by the IRB at the SWPS University of Social Sciences and Humanities Comments by authors: not specified Miscellaneous outcomes by the review authors: Rogala 2016 in Polish (translated) Correspondence: Roman Cieslak, Department of Psychology, SWPS University of Social Sciences and Humanities, Warsaw, Poland and Trauma Health and Hazards Center, Department of Psychology, University of Colorado Colorado Springs, Colorado Springs, CO, USA; rcieslak@uccs.edu; Anna Rogala: SWPS University, Chodakowska 19/31, 03‐815 Warsaw; anna.rogala@swps.edu.pl |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Po rejestracji uczestnicy, którzy zapoznali się z regulaminem bada‐ nia i podpisali zgodę na udział w nim, zostali losowo przydzieleni do jednego z 3 modułów interwencyjnych" ["After registration, participants who read the test regulations and signed consent to participate in it were randomly assigned to one of the three intervention modules"] Quote: "Interwencja składała się z modułu 1 – wzmacniają‐ cego przekonania o własnej skuteczności, modułu 2 – wzmacniającego spostrzegane wsparcie społeczne oraz modułu 3 – edukacyjnego. Każdy z uczestników bada‐ nia został losowo przypisany do jednego z nich." ["The intervention consisted of module 1 ‐ strengthening the conviction of its own effectiveness, module 2 ‐ reinforcing perceived social support and module 3 ‐ educational. Each of the study participants was randomly assigned to one of them."] Quote: "Respondents were randomly assigned to the experimental and control groups: the self‐efficacy enhancement intervention (n = 87) or an education active control group (n = 81)." Quote: "Participants assigned to the two groups did not differ across the study variables. In particular, non‐significant effects were found for age, F(1,166) = 0.95, p = 0.33, gender, χ 2 = (1, N = 168) = 0.46, p = 0.27, profession, χ 2 = (8, N = 165) = 4.40, p = 0.82, the duration of employment, F(1,166) = 0.09, p = 0.76, T1 indirect exposure, F(1,166) = 2.87, p = 0.09, self‐efficacy at T1, F(1,166) = 2.53, p = 0.11, STS at T1, F(1,166) = 2.75, p = 0.10, and SPTG at T1, F(1,166) = 0.97, p = 0.33." Judgement comment: insufficient information about random sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic variables and some outcome measures (self‐efficacy, secondary traumatic stress, secondary post‐traumatic growth); baseline comparability for other outcome variables (2nd measure for self‐efficacy, burnout, work engagement) unclear |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Finally, our study does not conform to all standards of fully randomized controlled trials, applying blinding procedures and evaluating the fidelity of the intervention processes. Thus, any conclusions should be treated with caution." Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | Unclear risk | Quote: "Finally, our study does not conform to all standards of fully randomized controlled trials, applying blinding procedures" Judgement comment: insufficient information about blinding of participants and personnel to permit judgement of ‘Low risk’ or ‘High risk’ (web‐based intervention, in part interactive; unclear if no blinding procedures refers to performing the intervention or outcome assessment) |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Quote: "Finally, our study does not conform to all standards of fully randomized controlled trials, applying blinding procedures and evaluating the fidelity of the intervention processes. Thus, any conclusions should be treated with caution." Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ (online questionnaires; unclear if no blinding procedures refers to performing the intervention or outcome assessment) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "FIGURE 1 | Flow of participants in a study." Quote: "Only 68 participants completed all experimental/control group procedures and participated in the measurements at T1, T2, and T3. Overall, 54 participants dropped out from the experimental condition, and 46 dropped out from the control condition, making a total of 100 (59.5%)." Quote: "Spośród 168 uczestników badania, którzy wypełnili skale w pomiarze 1. (T1), 51,2% osób nie wypełniło kwestionariuszy w pomiarze 2. (T2), a odsetek ten wzrósł do 59,5% w pomiarze 3. (T3). W celu sprawdzenia, czy danych brakowało w sposób losowy, zastosowano test MCAR Little’a (Missing Completely at Random). Jego wynik okazał się nieistotny statystycznie (Chi 2 (2216) = 1596,86, p = 1), co potwierdziło losowość braków danych. Różnica między 2 modułami w zakresie liczby osób, które wycofały się z badania, nie była statystycznie istotna (Chi 2 (1, N = 168) = 0,48, p = 0,49)." ["Of the 168 study participants who completed the scale in Measure 1 (T1), 51.2% did not complete the questionnaires in Measure 2. (T2), and this proportion increased to 59.5% in measurement 3 (T3). In order to check whether the data was missing randomly, the MCA Little's (Missing Completely at Random) test was used. His result turned out to be statistically insignificant (Chi2 (2216) = 1566.86, p = 1), which confirmed the randomness of missing data. The difference between the two modules in terms of the number of people who withdrew from the study was not statistically significant (Chi2 (1, N = 168) = 0.48, p = 0.49)."] Quote: "Braki danych uzupełniono, stosując metodę wielokrotnego podstawiania (multiple imputation method). W fazie podstawiania wprowadzono 3 skale mierzące odpowiednio: przekonania o własnej skuteczności, wypalenie zawodowe i zaangażowanie w pracę (jako predyktory i zmienne podstawiane), a także rodzaj modułu interwencyjnego (wyłącznie jako predyktor). Liczba podstawień wyniosła 5. Po zastosowaniu metody wielokrotnego podstawiania uzyskano dane od 168 osób we wszystkich 3 pomiarach." ["Data deficiencies were completed using the multiple imputation method. In the substitution phase, 3 scales were introduced, measuring, respectively: self‐efficacy convictions, occupational burnout and involvement in work (as predictors and substitutable variables), and the type of intervention module (only as a predictor). The number of substitutions was 5. After applying the multiple substitution method, data from 168 people in all 3 measurements were obtained."] Quote: "Missing data were imputed with regression procedures (estimated maximization). In line with suggestions to apply intention–to–treat analysis for the experimental studies with health‐related outcomes (Gupta, 2011), data from dropouts were also imputed. Missing data analysis indicated that data were missing completely at random, with Little’s χ 2 = (2035) = 1732.05, p = 1.00. Thus, the final analysis was conducted with a sample of N = 168." Quote: "Due to high drop‐out rate at T2 and T3 in social support enhancement module, we excluded from analysis participants assigned to this condition." Quote: "Dodatkowo wykluczono z analizy dane pochodzące od uczestników badania, którzy zostali przypisani do modułu wzmacniającego spostrzegane wsparcie społeczne (N = 85) ze względu na wysoki odsetek osób (78%), które nie wypełniły kwestionariuszy w drugim (T2) i trzecim pomiarze (T3) (tzw. drop‐out) (ryc. 1)." ["In addition, data derived from study participants assigned to the self‐efficacy enhancing module (N = 85) were excluded from the analysis due to the high percentage of people (78%) who did not fill in questionnaires in the second (T2) and third measurement ( T3) (so‐called drop‐out) (Figure 1)."] Quote: "Compared to completers, those who dropped out did not differ in self‐efficacy at T1, F(1,166) = 2.23, p = 0.11, STS at T1, F(1,166) = 2.80, p = 0.10, SPTG at T1, F(1,166) = 1.66, p = 0.20, the indirect exposure to trauma at work, F(1,166) = 2.75, p = 0.10, gender, χ 2 = (1, N = 168) = 0.41, p = 0.52, age, F(1,158) = 0.95, p = 0.33, profession, χ 2 = (8, N = 165) = 3.11, p = 0.93), and the duration of employment, F(1,157) = 1.72, p = 0.19, η 2 = 0.01. Finally, the dropout rates were the same for the experimental and the control groups, χ 2 = (1, N = 168) = 0.71, p = 0.40." Quote: "Those who dropped out were asked to provide reasons for not completing the study. The open–ended question was applied. Among those who responded (n = 54) the most frequent reasons to discontinue were personal reasons unrelated to the trial (39%) and the technical problems with the website or internet access (15%)." Quote: "For participants who did not complete the study, a short questionnaire was sent asking for the reason. 54 people answered, which as the reason for the resignation gave, among others personal reasons not related to the intervention (39%) and technical problems on the website of the intervention (15%)." Judgement comment: high dropout of participants in social support‐enhancing module and exclusion of these participants from the analysis; reasons for missing data in 2 other groups (self‐efficacy‐enhancing and educational module) unlikely to be related to true outcome (missing data at random); missing data were imputed (multiple imputation method); intention‐to‐treat analysis |
| Selective reporting (reporting bias) | High risk | Quote: "Efektywność interwencji została więc zmierzona przez porównanie wyników uczestników przypisanych do modułu edukacyjnego i modułu wzmacniającego przekonania o własnej skuteczności. Hipotezy dotyczące modułu interwencji mającego na celu wzmacnianie spostrzeganego wsparcia społecznego nie mogły więc być zweryfikowane." ["Thus, the effectiveness of the intervention was measured by comparing the results of the participants assigned to the educational module and the self‐efficacy enhancing module. Hypotheses regarding the intervention module aimed at strengthening the perceived social support could not be verified."] Judgement comment: no study protocol available; prespecified hypotheses on the social support enhancing module could not be tested due to high dropout, so only data on the self‐efficacy‐enhancing module and the educational module were analysed; within these analyses, all prespecified outcomes and time points have been reported |
Clemow 2018.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: imputation for psychosocial outcomes not specified; for blood pressure measures: multilevel, repeated‐measures regression analysis to generate full information maximum likelihood estimates of the group‐specific average change in systolic blood pressure (SBP) and diastolic blood pressure (DBP); per‐protocol analysis (i.e. only participants in IG who attended at least 6 sessions) and available‐case analysis (i.e. only participants in both groups who completed follow‐up assessments) + intention‐to‐treat analysis (n = 92) |
|
| Participants |
Country: USA Setting: delivered in workplace (large urban medical centre) Age: mean = 48.5 (SD = 8.7) years Sample size (randomised): 92 Sex: 71 women, 21 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depression CES‐D: IG = 14.5 (8.7), CG = 11.2 (10.2); burnout, emotional exhaustion (MBI): IG = 19.2 (10.8), CG = 23.2 (12.6); burnout, depersonalisation: IG = 5.4 (5.2), CG = 4.2 (4.4); burnout, personal accomplishment: IG = 32.3 (9.7), CG = 31.5 (11.3) Population description: employees (aged 18 – 70 years) of a large urban medical centre identified through workplace blood pressure (BP) screenings Inclusion criteria: 1) employees of large urban medical centre; 2) aged 18 ‐ 70 years; 3) whose screening BP (average of 3 measurements) was ≥ 140 mm Hg SBP or 90 mm Hg (DBP) and whose average readings did not exceed 180/110 mm Hg at both screening and subsequent baseline evaluation Exclusion criteria: 1) pregnancy; 2) end‐stage renal disease Attrition (withdrawals and exclusions): 11 dropouts after randomisation (IG = 6, CG = 5; i.e. did not complete follow‐up assessment); 2 participants (in IG) later found to have been ineligible Reasons for missing data: not specified (n = 11); average BP measurement computed in error ‐ actually below cut‐off (n = 2 ineligible after randomisation) |
|
| Interventions |
Intervention: LifeSkills workshop (stress and anger management intervention/workshop on cognitive‐behavioural coping skills) (n = 46)
Control: TAU (minimally enhanced) (n = 46)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) 2‐month follow‐up (i.e. 2 months/approximately 60 days post‐intervention); BP also assessed at screening (to test eligibility) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to obtain the means and SDs for perceived stress in both groups at each time point. We also asked for the means and SDs for all outcomes at 2‐month follow‐up (instead of change scores); no response received to 2 inquiries Study start/end date: start of data collection in 2003; see trial registration: until August 2006 Funding source: funding provided by NIH grant #HL67584 from the National Heart, Lung, and Blood Institute; funded with a Small Business Innovation Research (SBIR) grant from the National Institutes of Health (NIH) through Williams LifeSkills, Inc, Durham, North Carolina Declaration of interest: Redford B. Williams and Virginia P. Williams are founders and major stockholders in Williams LifeSkills, Inc. Their involvement in the project, as noted in the Methods section, was limited to treatment fidelity and initial training and initial supervision in the intervention. They also assisted in the editing of the manuscript. Otherwise, the design and conduct of the study, the data collection and analyses, and interpretation of results occurred independently of the developers of the intervention. The other authors have no conflicts to disclose. Ethical approval needed/obtained for study: approved by IRB at Columbia University Medical Center Comments by study authors: trial is registered at clinicaltrials.gov (Identifier NCT01262066) Miscellaneous outcomes by the review authors: not relevant Correspondence: Lynn P. Clemow, Department of Medicine, Center for Behavioral Cardiovascular Health, Columbia University Medical Center, New York, NY, USA; Department of Family and Community Medicine, Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ, USA; clemowlp@rwjms.rutgers.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Those who agreed to participate were randomly assigned to one of two groups: intervention (LifeSkills workshop) or minimally enhanced usual care." Quote: "Randomization was done by calling an off‐site person holding the randomization envelopes, using random‐sized randomization blocks provided by the study statistician (J.E.S.), in accordance with CONSORT (Consolidated Standards of Reporting Trials) guidelines [43]." Quote: "No significant differences were observed between the intervention and control groups on demographic and clinical characteristics at baseline (Table 1)." Quote: "Baseline psychosocial characteristics did not vary between treatment and control groups (Table 3)." Quote: "At baseline, SBP and DBP were similar between the two groups." Judgement comment: insufficient information about random sequence generation to permit judgement of ‘Low risk’ or ‘High risk’ (exact method of random sequence generation is not described); RCT and verified baseline comparability of groups for sociodemographic and clinical characteristics (Table 1; all Ps > 0.08) and outcome variables (Table 2: physiological outcomes: SBP, DBP: Ps > 0.35; Table 3, subjective outcomes) on the basis of analysis |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was done by calling an off‐site person holding the randomization envelopes, using random‐sized randomization blocks provided by the study statistician (J.E.S.), in accordance with CONSORT (Consolidated Standards of Reporting Trials) guidelines [43]." Judgement comment: Participants and investigators enrolling participants could not foresee assignment (allocation by off‐site person holding randomisation envelopes). |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Quote: "First, research staff were not blinded to participant group assignment." Judgement comment: no blinding of study personnel (also face‐to‐face intervention); blinding of participants unclear, but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "First, research staff were not blinded to participant group assignment." Judgement comment: no blinding of study personnel (also face‐to‐face intervention); blinding of participants unclear, but the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Quote: "First, research staff were not blinded to participant group assignment." Quote: "However, we attempted to mitigate the potential influence of this problem by using automated BP measurements, which are blinded to group assignment and less susceptible to bias than manual BP measurements." Judgement comment: research staff not blinded in general; therefore, probably also no blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Quote: "First, research staff were not blinded to participant group assignment." Judgement comment: research staff not blinded in general; therefore, probably also no blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Fig 1 | CONSORT diagram." Quote: "Eleven participants dropped out after randomization (six in the intervention group and five in the usual care control group). Two participants, both in the intervention group, were later found to have been ineligible because their average BP measurements were computed in error and were actually below the cutoff." Quote: "An intent‐to‐treat analysis was performed on all randomized participants. A multilevel, repeated‐measures regression analysis was performed to generate full information maximum likelihood estimates of the group‐specific average change in SBP and DBP between baseline and the 2‐month posttreatment assessments and to estimate and test the differential change between the intervention and usual care groups. Consistent with intent‐to‐treat principles, all participants who were randomized, including two participants who were subsequently deemed ineligible (described below), were included in the analysis" Quote: "All 92 participants who were randomized were included in the analysis." Quote: "In secondary analyses, we repeated the previous analyses after restricting the sample to those who completed the protocol (i.e., those in the control group who completed the follow‐up assessment [n = 41] and those in the intervention group who attended at least six sessions and completed the follow‐up assessment [n = 39])." Judgement comment: reasons for missing outcome data are unlikely to be related to true outcome with relative balance in missing data between groups (dropouts: IG: n = 6, CG: n = 5); per‐protocol analysis (i.e. only participants who attended at least 6 sessions in IG) and available‐case analysis (i.e. only participants who completed follow‐up assessment) as well as intention‐to‐treat analysis |
| Selective reporting (reporting bias) | High risk | Judgement comment: trial registration (NCT01262066) available; several reported outcomes (psychosocial variables) were not prespecified; PRE‐SPECIFIED: change in mean office blood pressure, covarying hostility and hostility x time (hostility assessed via Cook‐Medley questionnaire); REPORTED: (diastolic/systolic) blood pressure; hostility; depression; burnout (emotional exhaustion, depersonalisation, personal accomplishment), work strain (skill discretion, decision‐making authority, job demands), assertiveness (passive behaviour, aggressive, assertive), social support (belonging, appraisal, tangible), ruminative response (depressive rumination, reflection, brooding); perceived stress is prespecified in the report, but not reported |
Duchemin 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified; small sample size as limitation Imputation of missing data: no missing data; intention‐to‐treat analysis |
|
| Participants |
Country: USA Setting: large academic medical centre (SICU) Age: mean = 44.2 years Sample size (randomised): 32 Sex: 28 women, 4 men Comorbidity (mean (SD) of respective measures in indicated, if available at baseline: perceived stress (PSS): 12% of participants with low stress (< 10), 37% with high stress (> 16); stress scale: 37% with cut‐off value of stress > 14; burnout‐emotional exhaustion (MBI): 28% with cut‐off score > 26; burnout‐depersonalisation: 7.78 (5.53); burnout‐personal accomplishment: 36.5 (7.449) Population description: personnel, 18 years or older, from the SICU of a large academic medical centre Inclusion criteria: 1) any personnel working in the SICU; 2) having contact with the patients or their families Exclusion criteria: 1) individuals practising mindfulness, yoga, or exercising more than 30 minutes a day; 2) individuals with third trimester pregnancy; 3) individuals with a history of recent surgery if it limited ability to perform the gentle yoga movements Attrition (withdrawals and exclusions): no withdrawals or exclusions Reasons for missing data: not applicable since no missing data |
|
| Interventions |
Intervention: workplace‐adapted mindfulness‐based intervention (MBI) (n = 16)
Control: wait‐list control (n = 16) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention (1 week before intervention); 2) post‐intervention (1 week after intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors to ask for the means and SDs for all outcomes for the 2 groups at pre‐ and post‐intervention and to inquire whether FFMQ and ProQOL were measured as outcomes or only correlates. Data for some outcomes were sent by the authors (perceived stress, DASS‐21 stress, work stress, salivary alpha‐amylase, work satisfaction) of which not all were specified in the report (work satisfaction) (Klatt 2018 [pers comm]). Study start/end date: not specified Funding source: funded in part by the OSU Harding Behavioral Health Stress, Trauma and Resilience program Declaration of interest: none declared Ethical approval needed/obtained for study: approved by the university IRB, and all participants provided signed informed consent Comments by authors: not specified Miscellaneous outcomes by the review authors: conference abstract Klatt 2012 is a second reference to this study Correspondence: Anne‐Marie Duchemin, Department of Psychiatry, The Ohio State University, 1670 Upham Drive, Columbus, Ohio 43210, USA; anne‐marie.duchemin@osumc.edu; Tel: 614‐293‐5517, Fax: 614‐293‐7599 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The study adhered to the CONSORT guidelines for randomized trials 23. Eligible participants were randomized 1:1 using Graphpad software to intervention group or waiting list control group, with stratification by gender and type of work." Quote: "There were no significant differences between the two groups for age (p = 0.9496, t= 0.0638), years of experience (p = 0.9485, t = 0.06512), or years working in the SICU (p = 0.8702, t = 0.1648)." Quote: "On the PSS, only 12% of participants had a score < 10 (low stress), while 37% had a score > 16 (high stress). There was no significant difference between the two groups at baseline (p = 0.0910, t = 1.746)." Quote: "On the DASS stress subscale, 37% had score > 14, the cut‐off value for stress, with no significant difference between the two groups (p = 0.1552, t = 1.458)." Quote: "On the Maslach’s burnout inventory, the average emotional exhaustion subscale score was 23.12±10.1 with 28% of participants having scores > 26 and no difference between intervention and control groups (p = 0.3185, t = 1.0124)." Quote: "The scores were 7.78±5.53 for depersonalization and 36.5±7.449 for personal accomplishment with no significant difference between the groups (p = 0.685, t = 0.4909 and p = 0.3508, t = 0.9477 respectively)." Quote: "The average value for all participants was 93.6 ±15.9 units/ml (mean ± SEM) with no difference between the two groups (p = 0.6812, t = 0.4152)." (salivary α amylase) Quote: "Participants scored the stress level of their work at 7.15 ± 1.89 on a scale of 1 to 10 (with 10 being most stressful) at baseline with no significant difference between the two groups (p=0.8833, t= 0.1480)." Judgement comment: The investigators describe a random component in the sequence generation process (randomisation via software) and there is verified baseline comparability between groups for sociodemographic characteristics (age, years of experience, years working in SICU) and some outcomes of interest for the review on the basis of analysis.; baseline comparability between groups in mindfulness and burnout (ProQOL) unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: insufficient information about blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "There was no drop‐out and all participants completed the 2 sets of assessments." Quote: "Intention to treat “analyses which included all subjects randomized were performed." Judgement comment: no missing outcome data |
| Selective reporting (reporting bias) | High risk | Judgement comment: no study protocol available, but not all of the study's prespecified outcomes have been reported (for ProQOF and FFMQ only correlations with other outcomes reported but no intervention effects in contrast to other outcomes) |
Fei 2019.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
|
| Participants |
Country: China Setting: training sessions performed in a classroom of the hospital's teaching department Age: mean = 32.21 (SD = 6.48) years Sample size (randomised): 122 Sex: not specified (unclear if male nurses included) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: perceived stress (PSS): IG = 45.38 (5.15), CG = 45.13 (4.19); both groups above cut‐off for high stress Population description: nurses from 3 Chinese tertiary hospitals Inclusion criteria: 1) full‐time nurses; 2) signature of the employee's agreement with the hospital; 3) understanding of the objective of the intervention and voluntary participation in the study Exclusion criteria: 1) nursing student; 2) not wishing to participate; 3) severe organic disease; 4) taking medication for mood regulation; 5) have suffered major traumatic events in the last 6 months; 6) having experience in emotional resilience or similar training Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: emotional resilience training (n = 61)
Control: no intervention (n = 61) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to get the information whether N = 122 (61 in each group) were also analysed for sleep quality and the respective subscales. We also asked if there had been any dropouts/losses to follow‐up in the study or if there were no missing data at all, but received no response to 2 inquiries. Study start/end date: not exactly specified; recruitment in December 2018 Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: approval of the ethics committees obtained Comments by study authors: not specified Miscellaneous outcomes by the review authors: article in Spanish (translated) Correspondence: Yang Fei, Yangtze University, Jingzhou, Hubei Province, 434023, China; cjdxhlx@sohu.com |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Lot 122 enfermeros incluidos el estudio fron ditidos en el grupo experimental y el grupo control segúnmé to do aleatorio de ta bla numérica, con 61 miembros en da da grupo." [The 122 nurses included in the study were divided into the experimental group and the control group according to a random numerical table method, with 61 members in each group.] Quote: "Como se muestra en la Tabla 2, los 61 enfermeros del grupo control tienen entre 22 y 46 años, con un promedio de 31,74±6,11 años, mientras que los del grupo experimental tienen entre 22 y 45 años, con un promedio de 32,67±6,85. No hay diferencias estadísticamente significativas de la información general entre ambos grupos." [As shown in Table 2, the 61 nurses in the control group are between 22 and 46 years old, with an average of 31.74 ± 6.11 years, while those in the experimental group are between 22 and 45 years old, with an average of 32.67 ± 6.85. There are no statistically significant differences in general information between the two groups.] Quote: "Como se observa en la Tabla 3, no hay diferencia significativa en tensión, pérdida de control y puntaje total en el estrés percibido entre el grupo control y el experimental antes de la intervención (t=‐0,099, P=0,921)." [As seen in Table 3, there is no significant difference in tension, loss of control and total score on perceived stress between the control and experimental groups before the intervention ( t = ‐0.099, P = 0.921).] Quote: "Como puede verse en la Tabla 4, no hay una diferencia significativa en las puntuaciones en las emociones positivas y negativas entre el grupo experimental y el grupo de control antes de la intervención (P> 0,157)." [As can be seen in Table 4, there is no significant difference in the scores on positive and negative emotions between the experimental group and the control group before of the intervention (P> 0.157).] Quote: "Se puede observar en la Tabla 5 que no hay diferencias significativas en la calidad del sueño entre el grupo experimental y el de control antes de la intervención (P>0,05)" [It can be seen in Table 5 that there are no significant differences in sleep quality between the experimental and the control group before the intervention (P> 0.05)] Judgement comment: The investigators describe a random component in the sequence generation process (random‐number table) and there is verified baseline comparability of groups for sociodemographic characteristics (Table 2) and outcomes of interest (Table 3 ‐ 5) on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (N = 122 analysed for perceived stress and positive/negative affect; number of participants analysed for sleep quality not specified; unclear if there were no missing data at all or if missing data were imputed) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Gelkopf 2008.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified, relatively small sample size Imputation of missing data: no imputation of missing data; per‐protocol analysis (only participants who took part completely in allocated intervention) |
|
| Participants |
Country: Sri Lanka Setting: local, nongovernmental, grassroots organisation called Sumithrayo Age: mean = 48.65 (SD = 12.77) years Sample size (randomised): 62 Sex: 46 women, 14 men (in analysed sample) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: education and mental health volunteer workers who working with disaster survivors; had been working on‐site giving immediate physical help (ranging from recovering and burying bodies to building camps and providing makeshift kitchens) as well as providing emotional support and counselling to survivors and their families Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): 2/37 (5.4%) dropouts in IG Reasons for missing data: personal reasons (n = 2) |
|
| Interventions |
Intervention: 'Training the trainer' course based on ERASE (Enhancing Resiliency Among Students Experiencing Stress) Stress programme (n = 37)
Control: active control (Befriending seminar) (n = 25)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors to get the information on whether the mental health volunteers included in the study were healthcare professionals and if the authors could provide the summary outcome data for this subgroup only (Gelkopf 2019 [pers comm]). Study start/end date: not specified Funding source: financial support by the Silverton Foundation Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Marc Gelkopf; Lev Hasharon Mental Health Center, POB 9000, Netanya 42100, Israel; emgelkopf@013.net.il |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "From the list of 62 participants, 37 were randomly chosen 2 weeks before the training (using the Excel computer application random number generator) to participate in the ERASE Stress training program." Quote: "Except for a nonsignificant tendency for a higher income level in the experimental group, results suggest no difference between the experimental and control groups on the demographic and exposure variables. This suggests that the groups were of similar backgrounds (see Table 2)." Quote: "Differences between the experimental and control groups showed more personal optimism in the control group, t(68) = 3.4, p < .001; the experimental group showed more rumination, t(68) = 5.2, p < .001, and catastrophizing, t(68) = 4.3, p < .001." Judgement comment: The investigators describe a random component in the sequence generation process (computer random‐number generator) and there is verified baseline comparability of groups for most sociodemographic characteristics except for income (different results in table 2 and text); significant baseline differences in some outcomes of interest (optimism, rumination, catastrophising) on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Of those registered for the ERASE Stress training program, 35 completed the entire 4‐day, 30‐hr workshop that was given over 2 weekends. Two participants dropped out for personal reasons. All participants who registered for the Befriending seminar completed it." Judgement comment: reasons for missing outcome data unlikely to be related to true outcome with relative balance in missing data between groups (IG: n = 2 for personal reasons; CG: n = 0); per‐protocol analysis (only participants who took part completely in allocated intervention) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Hosseinnejad 2018.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): a priori sample size calculation (95% CI, 80% power) revealed required sample size of 40 in each group Imputation of missing data: not specified |
|
| Participants |
Country: IranSetting: nursing personnel from Shafa Hospital; training setting not specifiedAge: range = 24 ‐ 45 yearsSample size (randomised): 80Sex: 73 women, 7 menComorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: nursing personnel from Shafa Hospital Inclusion criteria: 1) male and female nurses working in Shafa Hospital in Rasht; 2) with work experience of between 1 and 30 years; 3) with a minimum undergraduate degree; 4) 22 – 60 years old (see also trial registration) Exclusion criteria: 1) nurses who did not have the opportunity to take part in the research; 2) persons who could not attend at least 2 sessions of resilience training; 3) nurses with a high resilience score (CD‐RISC) (see also trial registration) Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: resiliency skills training course (n = 40)
Control: TAU (n = 40)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) 1‐month follow‐up (1 month post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors about potential missing data (withdrawals/exclusions) in the study and if the assessment took place at pre‐intervention and at 1 month after end of treatment, or also at 3‐month follow‐up (as specified in trial registration). We also asked for the means and SDs of job satisfaction in the 2 groups at each time point with the number of participants analysed and more details about the content of the routine programme in the CG.; no response to 2 inquiries Study start/end date: see trial registration: expected recruitment start date: 23 October 2017; expected recruitment end date: 22 November 2017 Funding source: see trial registration: University of Social Welfare and Rehabilitation as sponsor Declaration of interest: no conflict of interest declared Ethical approval needed/obtained for study: ethics committee license obtained from University of Social Welfare and Rehabilitation Sciences Comments by study authors: trial registration: IRCT2017091636207N1 (Registered in Guilan University of Medical Sciences Healing Hospital and for co‐operation with Nursing Officers and Practitioners) Miscellaneous outcomes by the review authors: article in Persian (translated) Correspondence: Fatemeh Hosseinnejad (MSc); corresponding author: Narges Arsalani (PhD), Department of Nursing, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran; nargesarsalani@gmail.com |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Eighty nursing personnel from Shafa Hospital in Rash were recruited and randomly assigned to experimental and control groups." Quote: "Results showed no difference between the two group of intervention and control in terms of demographic characteristics." Judgement comment: insufficient information about random sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic characteristics (e.g. age, gender, marital status) on the basis of analysis; baseline comparability for outcomes not specified |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "اين مطالعه از نوع كارآزمايي باليني دو گروهي دربرگيرنده گروه آزمون و گروه شاهد بود." [This study was a double‐blind clinical trial that included experimental and control groups] Quote: see also trial registration: blinding: not blinded Judgement comment: according to publication, double‐blind clinical trial; however, according to trial registration no blinding occurred; face‐to‐face intervention, i.e. blinding probably broken and the outcome is likely to be influenced by the lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (e.g. n = 40 participants randomised to each group; but number of participants analysed not stated for each group; unclear if there were any missing data and if missing data were imputed) |
| Selective reporting (reporting bias) | High risk | Quote: "(IRCT2017091636207N1)" Judgement comment: trial registration available (IRCT2017091636207N1); and the study’s prespecified outcomes seem to have been reported in the prespecified way; however, in the trial registration the second assessment is specified for a 3‐month follow‐up (i.e. 3 months after the intervention), whereas the publication reports a 1‐month follow‐up |
Ireland 2017.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified; sample size was a weakness of the current study and possibly precluded several simple effects from reaching conventional levels of significance Imputation of missing data: not applicable since there were no withdrawals or exclusions |
|
| Participants |
Country: Australia Setting: medical interns from large hospital ED; exact training setting not specified Age: mean = 26.88 (SD = 4.79, range = 22 ‐ 48) years Sample size (randomised): 44 Sex: 28 women, 16 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: burnout (CBI): IG = 2.55 (0.52), CG = 2.65 (0.75) Population description: intern doctors completing their practicum rotation in the ED of a major metropolitan hospital Included criteria: not specified Excluded criteria: not specified Attrition (withdrawals and exclusions): information received from authors (Ireland 2019 [pers comm]): no withdrawals or exclusions; all participants stayed in the trial for the full length of time Reasons for missing data: not applicable since there were no withdrawals or exclusions |
|
| Interventions |
Intervention: Mindfulness training programme (for participants named as "resiliency and mindfulness program") (n = 23)
Control: active control (n = 21)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) during intervention (week 5 of 10‐week intervention); 3) post‐intervention (in final session, i.e. week 10) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to get the information about possible withdrawals/exclusions in the 2 groups and the number of participants analysed in each group (Ireland 2019 [pers comm]). Study start/end date: not specified Funding source: not specified Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article. Ethical approval needed/obtained for study: ethics approval through the host institution Comments by study authors: not specified Miscellaneous outcomes by the review authors: information received from authors (Ireland 2019 [pers comm]): There were no withdrawals or exclusions.; number of participants analysed in each group: full sample as reported in the article; all participants stayed in the trial for the full length of time Correspondence: Michael J. Ireland, School of Psychology and Counselling, University of Southern Queensland, PO Box 4196, Springfield Central, Queensland 4300, Australia; Michael.Ireland@usq.edu.au |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Following the provision of signed consent and the completion of the first testing session, participants were randomly assigned to the intervention (n = 23) or control group (n = 21)." Quote: "A randomized control trial methodology (with 44 intern doctors) was utilized to test this hypothesis." Quote: "Conditions were equivalent pretest in prior with regards to experience with meditation/mindfulness (F = 0.08, p = 0.776, g 2 < 0.01), the appeal of meditation/ mindfulness (F = 0.73, p = 0.401, g 2 = 0.02), and expectations of the potential helpfulness of meditation/mindfulness (F < 0.01, p = 0.963, g 2 < 0.01)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability for experience with meditation/mindfulness, appeal of meditation/mindfulness and expectations of mindfulness; insufficient information about baseline comparability (statistical significance) for sociodemographic characteristics (e.g. age, sex) and outcomes of interest (see T1 in Table 1) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: information received from authors: no withdrawals or exclusions; all participants stayed in the trial for the full length of time |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
ISRCTN69644721.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
|
| Participants |
Country: UK Setting: 4 Mind sites: Peterborough and Fenland, Tyneside, Wirral, or London (City, Hackney and Waltham Forest) Age: not specified Sample size (randomised): 255 (targeted) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: adults aged 18 to 67 years old who work in 1 of the 4 emergency services: police, fire and rescue, ambulance, and search and rescue Inclusion criteria: 1) adults aged 18 to 67 years old; 2) fluent in English; 3) work in 1 of the 4 emergency services: police, fire and rescue, ambulance, and search and rescue Exclusion criteria: Participants who were depressed or suffering from post‐traumatic stress disorder and who required treatment for these conditions. Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention 1: new resilience intervention (n not specified)
Intervention 2: digital‐only intervention (n not specified)
Control: wait‐list control (n not specified; received new resilience intervention 4 months later) |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 3‐month follow‐up (3 months post‐intervention); time points reported not specified Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the dates the trial was completed and published and if the authors could provide the summary outcome data for the 2 groups (Wild 2018 [pers comm]). Study start/end date: October 2016 – April 2017 Funding source: University of Oxford; Mind, the mental health charity (UK) Declaration of interest: not specified Ethical approval needed/obtained for study: approved by Medical Sciences Inter‐Divisional Research Ethics Committee, 14 October 2016, ref: R47862/RE001 Comments by authors: not specified Miscellaneous outcomes by the review authors: information received from authors (Wild 2018 [pers comm]): trial completed but unpublished; study conducted at 4 Mind centres in Peterborough and Fenland, Tyneside, Wirral, or London Correspondence: Dr Jennifer Wild (primary contact), Department of Experimental Psychology, University of Oxford, South Parks Road, Oxford, OX1 3UD, United Kingdom; Jennifer.wild@psy.ox.ac.uk |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (see trial registration): "Participants are then randomly allocated to one of three groups." Quote (see trial registration): "Emergency workers will be randomly allocated to receive one of the following three interventions: 1. The new resilience intervention (...), 2. The digital‐only intervention (...), 3. The wait‐list condition (...)" Judgement comment: based on trial registration, insufficient information about random‐sequence generation to permit judgement of 'Low risk' or 'High risk'; no judgement on baseline comparability in sociodemographic and outcome variables possible based on trial registration |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: based on trial registration, insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk' |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: based on trial registration, blinding of participants and personnel probably not done (1 group includes face‐to‐face group sessions) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: based on trial registration, insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: no judgement possible based on trial registration |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: no judgement possible based on trial registration |
Khoshnazary 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. only participants who completed the study, excluding the 3 withdrawals in the IG) |
|
| Participants |
Country: Iran
Setting: nurses in a psychiatric department; training setting not specified (probably at home, in part, due to written training)
Age: range = 24 ‐ 55 years
Sample size (randomised): 76
Sex: 51 women, 22 men (after 3 withdrawals)
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: nurses in psychiatric department Inclusion criteria: 1) providing consent to take part in the study; 2) having a bachelor’s degree or higher; 3) working morning, evening or night shifts at Roozbeh Psychiatric Hospital; 4) having at least 1 year's experience at Roozbeh Psychiatric Center; 5) no emotional‐intelligence training experience Exclusion criteria: 1) failure to participate or to participate appropriately in emotional intelligence training; 2) boredom or illness that prevented participation or continued collaboration at the time of the study; 3) moving to another centre; 4) incomplete completion of questionnaire or failure to return the questionnaire during the procedure; 5) psychosocial problems; 6) use of drugs Attrition (withdrawals and exclusions): 3 withdrawals in IG Reasons for missing data: not specified |
|
| Interventions |
Intervention: emotional intelligence (EI) training (n = 38)
Control: not specified (n = 38)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes | Contact with authors: no correspondence required Study start/end date: not exactly specified; recruitment in 2014 Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: approved by Ethics Committee of University of Social Welfare and Rehabilitation Sciences (code: 8.4931.IR.USWR.REC) Comments by study authors: article is the result of a Master's Degree in Nursing at the University of Social Welfare and Rehabilitation Sciences Miscellaneous outcomes by the review authors: article in Persian (translated) Correspondence: S. Khoshnazary; corresponding author: M. A. Hosseini, PhD, Associate Professor, Nursing Department, University of Social Welfare & Rehabilitation Sciences, Tehran, Iran; mahmaimy2020@gmail.com | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The people divided two groups. Intervention and control groups in sample random method." Quote: "Results showed that no different between two group of intervention and control about demographic characteristics." Quote: "مرتبط اصلی های یافته در <b>329/72 ± 29/91 مداخله گروه در مداخله از قبل هیجانی هوش اختالف آماري نظر از که بود 326/73 ± 36/55 کنترل گروه در و اجرای از بعد .)p=0/501( نداشت وجود گروه دو بین معناداري" [In the main findings related to the purpose of the study, the mean score of emotional intelligence before intervention in the intervention group was 329.72 (29.91) and in the control group was 326.73 (36.55) which was not statistically significant (p = .501).] Quote: "داشت وجود گروه دو بین <b>مداخله گروه در مداخله از قبل آوری تاب نمره میانگین که بود 57/70 ± 15/14 شاهد گروه در و 61/71 ± 12/47 نداشت وجود گروه دو بین معناداري اختالف آماري نظر از گروه در آوری تاب نمره میانگین مداخله اجرای از بعد .)p=0/098(</b> 58/92 ± 13/71 به کنترل" [The mean pre‐intervention resiliency score in the intervention group was 61.71 (12.47) and in the control group was 57.70 (15.14) with no statistically significant difference between the two groups (p = 0.098).] Quote: "می زیر شرح به ،پژوهش <b>:شامل شناختی جمعیت متغیرهای داد نشان مطالعه نتایج میزان ،)p=0/408( تاهل ،)p=0/118( سن ،)p=0/08( جنس سازمانی پست ،)p=0/501( کاری سابقه ،)p=0/369( تحصیالت ،)p=0/09( کاری اضافه ،)p=0/82( استخدامی وضعیت ،)p=0/25( دو در ،)p=0/194( دیگر محلی در اشتغال ،)p=0/77( کاری شیفت</b> نداشته وجود گروه دو بین" [The results showed that there were no significant differences between the two groups in demographic variables including sex (p = 0.08), age (p = 0.188), marital status (p = 0.408), educational level (p = 0.369), work experience (p = 0.501), organizational position (p = 0.25), employment status (p = 0.82), overtime (p = 0.09), shift work (p = 0.77) and other employment (p = 0.194).] Judgement comment: insufficient information about random sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic characteristics and outcomes of interest on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: control group not further specified; blinding of participants and participants probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by the lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "3 دوره 33 ها یافته <b>گروه از نفر سه که داشتند شرکت نفر 76 پژوهش این در 73 نهایت در و دادند انصراف پژوهش در مشارکت ادامه از مداخله بودن همسان بخش دو در ،تحقیق این هاي یافته.ماندند باقی نفر</b> فرضیه محوریت با اصلی هاي" [The study involved 76 people, with three of the intervention group withdrawing from participation in the study, and 73 remained.] Judgement comment: reasons for missing data likely to be related to true outcome with slight imbalance in missing data between groups (IG: n = 3 withdrawals; CG: n = 0); no reasons specified; per‐protocol analysis (i.e. only participants who completed trial, without n = 3 withdrawals in IG) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Klatt 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
|
| Participants |
Country: USA Setting: ICUs Age: see Population description; age not specified Sample size (randomised): 34 (information received from authors; Klatt 2019 [pers comm]) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: employees at ICUs Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: Mindfulness in Motion (MIM) (n = 17; information received from authors; Klatt 2019 [pers comm])
Control: wait‐list control (n = 17; information received from authors; Klatt 2019 [pers comm]) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention (1 week before the intervention); 2) post‐intervention (1 week after last session) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors to ask for the number of participants allocated to and analysed in each group, as well as the means and SDs for resiliency for the 2 groups at each time point. We also inquired whether the authors performed an intention‐to‐treat analysis. We received the information about the number of participants in each group from the authors (Klatt 2019 [pers comm]). Study start/end date: not specified Funding source: financial contributions to the project by the following entities at the Ohio State University: Stress, Trauma, and Resilience (STAR) Program, Health System Administration, Critical Care Nursing, and the Faculty Associates Program through the Women’s Place Declaration of interest: Subsequent to the completion of this research conducted at the Ohio State University, Dr Klatt has served as a consultant to Mindful Management, Limited Liability Company to whom The Ohio State University has licensed the rights of the individual practice CD/DVD; all other authors have nothing to disclose. Ethical approval needed/obtained for study: IRB approval from The Ohio State University Comments by authors: not specified Miscellaneous outcomes by the review authors: information recevied from authors: 17 participants in each group (Klatt 2019 [pers comm]) Correspondence: Maryanna Klatt, Department of Family Medicine, The Ohio State University College of Medicine; Maryanna.Klatt@osumc.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "To determine the intervention feasibility/efficacy, we conducted a randomized wait‐list control group in Intensive Care Units (ICUs)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; no information about comparability of groups at baseline or respective analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information on blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires and the self‐measurement of breath counts may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "The intervention is well received with 97% retention rate." Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’; information received from authors: n = 17 participants allocated to each group; for some results, n = 34 participants analysed; however the amount of potential missing data not stated |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified (pre‐specified paired t‐tests were reported) |
Lebares 2018.
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): study was not powered to detect statistically significant inter‐group differences and comprises a convenience sample; consistent with recommendations for pilot trials. No focus on statistical power but use of linear mixed‐effects modelling (ANCOVA) for multivariate analysis, with baseline scores as a covariate; of relevance to future trials. Power calculations suggest that a sample size of 40 participants in a 2‐group comparison will have 80% power to detect an effect size expressed as partial η2 of 0.17 Imputation of missing data: no imputation of missing data; no missing data reported for most outcomes; 2 excluded from fMRI analysis | |
| Participants |
Country: USA
Setting: postgraduate year 1 surgery residents at University of California, San Francisco; training setting not specified
Age: mean = 28.3 (SD = 2.4) years
Sample size (randomised): 21
Sex: 8 women, 13 men
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: burnout (abbreviated MBI): IG = 23.92 (6.83), CG = 25.33 (7.62); depression (PHQ‐9): IG = 1.67 (1.56), CG = 0.89 (0.93) Population description: first‐year surgery residents Inclusion criteria: 1) postgraduate year 1 surgery residents at University of California, San Francisco (UCSF); 2) without a current mindfulness meditation practice; 3) who provided written and oral informed consent Exclusion criteria: 1) previous experience with mindfulness practice; 2) chronic inflammatory illness; 3) current pregnancy Attrition (withdrawals and exclusions): 0 lost to follow‐up in IG and 0 withdrew from CG; 1 participant initially assigned to CG mistakenly attended first IG sessions and finally participated in IG. 2 excluded from fMRI analysis Reasons for missing data: implanted metal, protocol glitch (n = 2 exclusions from fMRI analysis) |
|
| Interventions |
Intervention: Modified MBSR (modMBSR) (n = 11; after participant assigned to CG mistakenly attended first IG session and finally participated in IG; n = 12)
Control: attention control (n = 10; after 1 participant assigned to CG mistakenly attended first IG session and finally participated in IG; n = 9)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: information in part received from authors (Lebares 2019 [pers comm]): 1) pre‐intervention (before start of internship/intern year; always mid‐June); 2) post‐intervention (information from authors: within 1 week of the end of training/3½ months after baseline, i.e. 8‐week training approximately 1½ months after baseline during internship); 3) approximately 8½‐month follow‐up (approximately 12 months after baseline in May of the following year; i.e. 8½ months after end of training which took place at 3½ months after baseline) Adverse events: no adverse patient events reported for study participation |
|
| Notes |
Contact with authors: We contacted the authors to get more information about the assessments (time 2 immediately post‐intervention, but 1½ months after training/3½ months after baseline; time 3 at 10 months after end of training/12 months after baseline?) and the number of participants analysed for the psychological outcomes (see different information in 2 flow diagrams of reports) (Lebares 2019 [pers comm]). Study start/end date: data collection from June 2016 – June 2017; data analysis from June 2017 to December 2017 Funding source: LEBARES 2018: Ms Desai was supported by National Institutes of Health grant R25#125451‐03 Short Term Research Education Program to Increase Diversity in Health‐Related Research (The National Institutes of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication); LEBARES 2019: Dr Staffaroni supported by grants from the National Institutes of Health and grants from Larry L. Hillblom Foundation during the conduct of the study Declaration of interest: LEBARES 2018: no disclosures were reported; LEBARES 2019: Dr Staffaroni reported grants from the National Institutes of Health and grants from Larry L. Hillblom Foundation during the conduct of the study. No other disclosures were reported Ethical approval needed/obtained for study: all aspects of the intervention and assessment were approved in full by the UCSF IRB Comments by study authors: LEBARES 2018: this article was presented at the American College of Surgeons 104th Annual Clinical Congress, Scientific Forum; October 24, 2018; Boston, Massachusetts; trial registration: ClinicalTrials.gov identifier: NCT03141190 Miscellaneous outcomes by the review authors: acronym: Mindful Surgeon; information concerning time points in part received from authors (Lebares 2019 [pers comm]); LEBARES 2018 reports the feasibility results of the pilot, longitudinal, randomised clinical trial to investigate the feasibility of modified MBSR for use by surgical interns; LEBARES 2019 reports an additional analysis of this trial including findings for psychological outcomes, executive functioning, motor skills and neural substrates activated in emotion regulation Stated purpose of the study: LEBARES 2018: to test the feasibility and acceptability of modified Mindfulness‐Based Stress Reduction (MBSR) training during surgical residency; LEBARES 2019: to explore potential benefits to stress, cognition, and performance in postgraduate year 1 (PGY‐1) surgery residents receiving modified mindfulness‐based stress reduction (modMBSR) Correspondence: Carter C. Lebares, MD, Department of Surgery, University of California, 513 Parnassus Ave, HSW 1601, San Francisco, CA 94143‐0790; carter.lebares@ucsf.edu; San Francisco |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "pilot randomized clinical trial of modified MBSR vs an active control was conducted" Quote: "We randomized 21 PGY‐1 surgery residents (8 [38%] women) using Wesleyan University’s Research Randomizer 54 to either the modMBSR arm (n = 11; 4 [36%] women) or control arm (n = 10; 4 [40%] women), blocking for sex and surgical subspecialty designation." Quote: "Balancing for sex and subspecialty designation, we randomized participants to modified MBSR (n = 12) or an active control (n = 9) using third‐party block randomization following described operationalized methods." Judgement comment: The investigators describe a random component in the sequence generation process (computer‐generated randomisation: Wesleyan University's Research Randomizer), but there is no information about comparability of groups at baseline or respective analysis (e.g. for sociodemographic characteristics in Table 1 no statistical (non‐)significance specified) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Quote: "Eligible participants were postgraduate year 1 (PGY‐1) surgery residents at UCSF, without a current mindfulness meditation practice who provided written and oral informed consent and were blinded to assignment." Judgement comment: blinding of participants ensured; blinding of personnel probably not done (face‐to‐face intervention), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "Eligible participants were postgraduate year 1 (PGY‐1) surgery residents at UCSF, without a current mindfulness meditation practice who provided written and oral informed consent and were blinded to assignment." Judgement comment: blinding of participants ensured; blinding of personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: insufficient information about blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "One participant was initially allocated to the active control but did not receive the intervention owing to inadvertently attending the modMBSR training class during week 1. She was therefore reassigned to the modMBSR intervention group." Quote: "Two participants did not have functional magnetic resonance imaging (fMRI) scans analyzed. One was never scanned owing to implanted metal, and the other was scanned but data were incomplete (protocol glitch) and could not be analyzed." Quote: "We randomized 21 PGY‐1 surgery residents (8 [38%] women) using Wesleyan University’s Research Randomizer 54 to either the modMBSR arm (n = 11; 4 [36%] women) or control arm (n = 10; 4 [40%] women), blocking for sex and surgical subspecialty designation. A participant assigned to the control group mistakenly attended the first modMBSR session, resulting in final participation and analysis of modMBSR (n = 12; 5 [42%] women) and control (n = 9; 3 [33%] women) (Table 1 and Figure 1)." Judgement comment: no missing outcome data for psychological assessment, executive function testing and motor skills testing reported; overall: 1 participant initially allocated to CG did not receive allocated active control due to mistakenly attending an IG session; n = 2 excluded from fMRI, but reasons for missing data are unlikely to be related to true outcome (see reasons for missing data: implanted metal, protocol glitch) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: trial registration (NCT03141190) available and all of the study’s pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way |
Lin 2019.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. without 11 participants in IG who missed more than 2 sessions) and available‐case analysis (i.e. only participants who completed (valid) questionnaires) |
|
| Participants |
Country: mainland China Setting: nurses from general hospital; training setting not specified Age: mean = 31.50 (SD = 6.90) years Sample size (randomised): 110 Sex: 84 women, 6 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: nurses from 2 tertiary‐level general hospitals Inclusion criteria: 1) being employed as a full‐time nurse Exclusion criteria: 1) being a student nurse; 2) suffering from serious somatic disease; 3) taking mood‐regulating drugs; 4) having suffered a major traumatic event in the past 6 months; 5) having participated in mindfulness training previously Attrition (withdrawals and exclusions): 20 (IG = 11 missed weekly sessions more than twice, CG = 9 did not complete questionnaire or submitted invalid questionnaires) Reasons for missing data: not specified |
|
| Interventions |
Intervention: modMBSR (n = 55)
Control: wait‐list control (n = 55)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 3‐month follow‐up (3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: exact study dates not specified; group intervention for 8 weeks from 25 April 2017 to 16 June 2017 Funding source: receipt of the following financial support for the research, authorship, and/or publication of this article: study supported by a grant from the General Program of Science and Technology Plan for Health Care in Dongguan City of Guangdong Province (2016105101286) Declaration of interest: no potential conflicts of interest with respect to the research, authorship, and/or publication of this article Ethical approval needed/obtained for study: approval by Ethical Committee of Xiangya Nursing School (approval number 2015078) Comments by study authors: funder played no role in the study design, data collection, data analysis, manuscript preparation, or decision to publish the report Miscellaneous outcomes by the review authors: not relevant Correspondence: Lin Lin; corresponding author: Guoping He, MD, Xiangya Nursing School of Central South University, No. 172, Tongzipo Road, Yuelu District, Changsha, Hunan 410013, China; lily453125836@126.com |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "This study utilized a randomized controlled design. Eligible participants were randomized 1:1 using a computer‐generated random number table to the intervention group or the wait‐list control group." Quote: "No significant differences were observed between the two groups for any of the demographic characteristics (see Table 2)." Quote: "No significant effect of group or time or the Group × Time interaction on job satisfaction was identified between the two groups (p > .05)" Quote: "The results of the simple effects analysis (independent‐ samples t tests and one‐way ANOVA) were as follows: First, when the time points were fixed, no significant differences in perceived stress, positive affect, negative affect, or resilience were noted between the two groups at baseline (p > .05)" Judgement comment: The investigators describe a random component in the sequence generation process (computer‐generated random‐number table) and there is verified baseline comparability of groups for sociodemographic characteristics (see Table 2; all Ps > 0.07) and most outcome of interest (perceived stress, positive affect, negative affect, resilience; P > 0.05) on the basis of analysis; baseline comparability for job satisfaction not exactly specified, but no significant group effect on job satisfaction in repeated‐measures ANOVA reported which provides some evidence for baseline comparability in this outcome |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (online questionnaires); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "In the intervention group, 11 participants missed the weekly sessions more than twice. In the control group, six participants did not complete the questionnaire, and three participants submitted invalid questionnaires." Quote: "Therefore, the effective sample size was 90, including 44 in the intervention group and 46 in the control group." Judgement comment: reasons for missing data unlikely to be related to true outcome with relative balance in missing data between groups (IG: n = 11 missed weekly sessions more than twice; CG: n = 9 did not complete questionnaires or submitted invalid questionnaires); no reasons for missing data in each group provided; per‐protocol analysis (i.e. only participants who missed fewer than 2 weekly intervention sessions) and available‐case analysis (only participants who provided (valid) questionnaires) with 90 participants |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Loiselle 2018.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): There is an effect size of 0.6225 when using change scores for treatment and control groups, and their respective standard deviations, from a recent study using the Transcendental Meditation (TM) technique as an intervention and measuring burnout with the MBI (Elder 2014). Applying Cohen’s power tables for P < 0.05 to this effect size, means the number of participants needed per group is 12; recruiting 20 participants per group allows for 20% attrition Imputation of missing data: no imputation of missing data; available‐case analysis (i.e. only participants who completed post‐intervention assessments) |
|
| Participants |
Country: USA
Setting: conducted at a medical school hospital and affiliated VA hospital
Age: mean = 45.1 (SD = 10.51) years
Sample size (randomised): 40
Sex: 23 women, 17 men
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified; burnout and depression values at pre‐intervention not reported Population description: academic physicians working at a medical school and hospital in a large midwestern metropolitan area Inclusion criteria: 1) being an academic attending physician at the Loyola Chicago School of Medicine or VA hospital; 2) commitment to attend all required sessions for learning the TM programme (intervention) and monthly follow‐ups; 3) agreeing to practice it twice daily for 20 minutes and to complete both pre‐and post‐testing (at 1 month and 4 months), including both the entry and exit interviews; additional criterion in trial registration = having a medical doctor degree Exclusion criteria: see trial registration; 1) current suicidal ideation (adverse event of suicidal ideation reporting excluded from study until such time event was resolved); 2) previous instruction in the TM technique Attrition (withdrawals and exclusions): 7 lost to follow‐up (i.e. did not complete post‐test/post‐test non‐compliance; IG = 6, CG = 1) Reasons for missing data: not specified |
|
| Interventions |
Intervention: TM technique (n = 21)
Control: wait‐list control (n = 19)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) during intervention (1‐month post‐test of 4‐month intervention period); 3) post‐intervention (4‐month post‐test; i.e. at the end of 4‐month intervention period) Adverse events: if adverse event reported through testing/interviews, reported to principal investigator who would speak to this study participant and recommend that they be seen in Employee Health; in case of suicidal ideation as adverse event, participant would be excluded from study until event was resolved; no adverse events reported during the study period |
|
| Notes | Contact with authors: We contacted the authors to ask for the unadjusted means and SDs for all outcomes at 1‐ and 4‐month assessment for both groups, but received no response to 2 inquiries. Study start/end date: see trial registration: August 2015 to September 2016 Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: approved by IRB at Maharishi University of Management in March 2015; followed by IRB for the chosen medical school approval in July 2015 Comments by study authors: trial registration: NCT03714204 Miscellaneous outcomes by the review authors: dissertation Correspondence: Marie Ellen Loiselle; principal investigator of study (NCT03714204): Carla L Brown, PhD, Strich School of Medicine; Gregory Gruener, MD (study director), Loyola University Medical Center, 2160 S. First Ave; Maywood, IL 60153 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Random assignment was to the experimental (TM) group (n=21) or the wait‐list control group (n=19)." Quote: "Forty academic physicians completed their informed consent, baseline testing and entry interview and were randomly assigned to either the TM (experimental) group (immediate intervention start; n=21) or control group (delayed intervention start; n=19)." Quote: "Analysis of the data did not show any significant difference between the experimental or control groups in either their baseline testing or demographics (all p values >.05)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic characteristics (see Table 1; all Ps > 0.123) and outcomes (i.e. baseline testing) on the basis of analysis (see Table 1) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (questionnaires administered in person by the researcher or as online survey); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Six of the TM group and one of the control group subjects dropped out of the study before the one‐ month posttest." Quote: "A total of 33 physicians completed both the 1‐month and 4‐month posttests (TM = 15; control = 18)." Judgement comment: reasons for missing data likely to be related to true outcome with imbalance in amount of missing data between groups (lost to follow‐up: IG: n = 6; CG: n = 1, i.e. did not complete post‐test); available‐case analysis (only participants for whom outcomes were obtained at all assessments) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: trial registration available (NCT03714204); and all of the study’s prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way |
Luthar 2017.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): Based on a power analysis, the study authors set out to include 40 women in the study; with this number and assuming α = 0.05, power was 0.80 to detect an effect size of partial η² of 0.17, and 0.65 to detect η² of 0.12 Imputation of missing data: 1 participant missing for parenting stress at time 2 and time 3 but all participants analysed in ANOVAs/ANCOVAs; no imputation specified; available‐case analysis for cortisol analysis (only participants for whom outcomes were obtained) |
|
| Participants |
Country: USA Setting: Mayo Clinic Age: mean = 39.06 (SD = 5.49) years Sample size (randomised): 40 Sex: 40 women Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depression (BDI): IG = 8.76 (6.34), CG = 8.58 (4.10); burnout, emotional exhaustion (MBI): IG = 32.7 (13.72), CG = 33.37 (10.21); burnout, depersonalisation: IG = 10.0 (7.78), CG = 9.58 (7.43); burnout, personal accomplishment: IG = 39.8 (5.14), CG = 37.32 (5.62); global symptoms: IG = 0.52 (0.47), CG = 0.43 (0.26) Population description: physician mothers at Mayo Clinic (physicians, PhD’s (doctor of philosophy) in clinical practice, NPs, and PAs) Inclusion criteria: having at least 1 child aged 18 years or younger Exclusion criteria: not specified Attrition (withdrawals and exclusions): PSYCHOLOGICAL MEASURES (parenting stress; information received from authors; Stonnington 2017 [pers comm]): post‐intervention: CG = 1/19 (5.3%); 3‐month follow‐up: CG = 1 (5.3%); BIOLOGICAL MEASURES (unclear if IG or CG): pre‐intervention: 1; post‐intervention: 1; 3‐month follow‐up: 7 Reasons for missing data: unclear (reasons for missing data in CG on parenting stress); cortisol: pregnancies and maternity leaves (n = 3), time schedules (n = 2), exclusions due to statistical outliers (n = 2; > 2 SDs from the mean) |
|
| Interventions |
Intervention: ACG (n = 21)
Control: no intervention (12 weekly hours of protected time to be used as desired) (n = 19) |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 3‐month follow‐up (3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to ask for the means and SDs for outcome measures in the 2 groups at each time point (Stonnington 2017 [pers comm]). Study start/end date: February 2015 to November 2015 (actual completion date according to trial registration: December 2016) Funding source: supported by a seed fund from Arizona State University to Luthar; Mayo Clinic funded and supported medical‐care professionals’ time to participate in study activities Declaration of interest: no conflict of interest with respect to publication of this article. Ethical approval needed/obtained for study: approved by the Mayo Clinic IRB Comments by authors: trial registration: ClinicalTrials.gov NCT02540473 URL: clinicaltrials.gov/show/NCT02540473 Miscellaneous outcomes by the review authors: not relevant Correspondence: Suniya S. Luthar, PhD, Arizona State University, 950 S. McAllister Drive, Tempe, AZ 85281; Suniya.Luthar@asu.edu; Phone: 914‐310‐1102; Trial registration: Cynthia Stonnington, MD, Associate Professor of Psychiatry, Mayo Clinic, Stonnington.Cynthia@mayo.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The first 40 eligible women were enrolled in the study. Participants were assigned randomly to the ACG intervention group (n = 21) or to the control group (n = 19)" Quote: "With blinded random assignment, of the 21 intervention women, 17 were physicians, and 4 were NP/PAs; among the 19 control mothers, 8 were physicians, 1 was a PhD, and 10 were NP/ PAs. Other than the difference in proportion of NP/PAs and physicians, the intervention and control groups did not differ in demographics, baseline adjustment or cortisol levels." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic variables and outcome variables |
| Allocation concealment (selection bias) | Unclear risk | Quote: "With blinded random assignment,..." Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ (exact method is not described, unclear if allocation was concealed from personnel and/or participants) |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: insufficient information about blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "On psychological measures, one participant was missing data on parenting stress at follow‐up. On biological measures, pregnancies and maternity leaves precluded draws from one woman throughout, and from two at the follow‐up. An additional two could not schedule times to provide samples at follow‐up, and two were statistical outliers and removed from the analysis (>2 SD from the mean). Thus, at baseline and after the intervention, there were 39 of 40 the women who had cortisol levels measured at baseline and after the intervention, and 35 of 40 at follow‐up." Judgement comment: reasons for missing data unlikely to be related to true outcome (see reasons for missing data): psychological outcomes: IG: n = 0; CG: n = 1 in parenting stress (information received from authors; here no reasons for missing data reported, but relative balance between IG and CG); biological outcomes: n = 7 missing (due to pregnancy/maternity leave, schedule problems, n = 2 outliers removed from analysis); missing data in biological outcomes not reported for each group separately; available‐case analysis for cortisol (only participants for whom outcomes were obtained at 3 time points) |
| Selective reporting (reporting bias) | High risk | Judgement comment: trial registration is available (NCT02540473); not all of the prespecified (secondary) outcomes were reported and several reported outcomes were not prespecified: PRESPECIFIED: Primary outcome: level of depression (BDI); Secondary outcomes: Biomarker of stress C‐reactive protein, biomarker of stress nerve‐growth factor, professional functioning (MBI), perceived social support (Quality of Social Support Scale), parenting stress (PSI); REPORTED: level of depression (BDI); professional functioning (MBI); parenting stress (PSI); Global symptoms (BSI); self‐compassion (Self‐Compassion Scale); feeling loved (4 items); physical affection (3 items); plasma cortisol (secondary outcome) |
Mache 2015a.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data |
|
| Participants |
Country: Germany Setting: clinic departments specialising in surgical medicine Age: mean = 27 (SD = 2.5) years Sample size (randomised): 69 (according to authors: 69 randomised, but after randomisation, 1 was excluded in IG and 68 were analysed) Sex: 39 women, 29 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: perceived stress (PSQ): IG = 59.3 (18.5), CG = 56.7 (18.7); both groups above cut‐off for moderate stress level; IG near cut‐off for high stress Population description: surgeons in their first year of work from 4 clinic departments specialising in surgical medicine Inclusion criteria: 1) employment as a surgeon in a hospital department; 2) working full‐time; 3) working experience of less than a year; 4) being able and willing to participate; 5) agreement to complete a survey at least 2 times Exclusion criteria: not specified Attrition (withdrawals and exclusions): 1 exclusion in IG Reasons for missing data: health reasons (sickness absence) |
|
| Interventions |
Intervention: multicomponent mental competency and stress management training (n = 36)
Control: no intervention (n = 33) (control group did nothing related to the intervention topic: any other psychosocial skill training, counselling or therapy (according to contact with authors: possibility of a later participation was announced) |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (after 3‐month intervention); 3) 3‐month follow‐up (3 months post‐intervention/6 months after baseline) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors to get the information about the number of participants randomised and potential per‐protocol analysis. We also asked about the form of control group (no intervention or wait‐list control) (Mache 2017a [pers comm]). Study start/end date: inclusion of participants between March and August 2014; exact study dates not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: ethical approval by the Free University Berlin Comments by authors: not specified Miscellaneous outcomes by the review authors: no intervention control group according to information from authors Correspondence: Stefanie Mache, PhD, Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf, Seewartenstrasse 10, 20459 Hamburg, Germany; s.mache@uke.de; stefanie.mache@bgv.hamburg.de |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Surgeons were randomized into 2 groups (intervention and comparison group). Names of the surgeons were listed in alphabetical order. Random numbers had been assigned to each name. After this, the numbers had been allocated from random number tables to the intervention or control group." Quote: "Baseline data on gender, age, and perceived health indicate only small, insignificant differences between intervention and comparison group." Judgement comment: The investigators describe a random component in the sequence generation process (random‐number tables) and there is verified baseline comparability of groups for sociodemographic variables and perceived health; baseline comparability for outcome variables unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (online questionnaires); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Of the 36 participants in the intervention group, 1 surgeon was excluded owing to health reasons (sickness absence). In summation, 35 physicians participated in the intervention group and 33 participated in the comparison group." Judgement comment: reasons for missing data unlikely to be related to true outcome (only 1 exclusion in IG due to health reasons) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available, but it is clear that the published report includes all expected outcomes, including those that were prespecified |
Mache 2015b.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): A sample size of a minimum of 40 physicians was selected for this pilot study after weighing statistical considerations along with logistical and resource constraints. A sample size of 40 provides a statistical power (2‐tailed, α = 0.05) of > 85%. Imputation of missing data: no imputation of missing data; per‐protocol analysis (only participants who took part in allocated intervention) and available‐case analysis (only participants for whom outcomes were obtained at 3 time points) |
|
| Participants |
Country: Germany Setting: several clinic departments specialising in different medical specialties (e.g. internal medicine, paediatrics, neurology, and gynaecology) Age: mean = 28 years Sample size (randomised): 90 (according to information from authors; Mache 2017b [pers comm]) Sex: 51 women, 34 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: perceived stress (PSQ): IG = 58.1 (19.3), CG = 56.7 (19.8); both groups above cut‐off for moderate stress level Population description: hospital physicians from several clinic departments specialising in different medical specialties (e.g. internal medicine, paediatrics, neurology, and gynaecology); junior physicians in their first year after graduation Inclusion criteria: 1) employment as a hospital doctor; 2) working at least full‐time; 3) working experience of less than a year; 4) being able and willing to participate; 5) agreement to complete a survey at least twice Exclusion criteria: not specified Attrition (withdrawals and exclusions): 5 (IG = 3/45 (6.7%) exclusions, CG = 2/45 (4.4%) did not complete follow‐up questionnaires) Reasons for missing data: health reasons such as operation, accident (IG = 3), did not respond to follow‐up questionnaires, reasons not specified (CG = 2) |
|
| Interventions |
Intervention: psychosocial resilience training (n = 45; according to information from authors; Mache 2017b [pers comm])
Control: no intervention (n = 45; according to information from authors; Mache 2017b [pers comm]) (received no training but answered the questionnaire at baseline and follow‐up) |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Time points measured: 1) pre‐intervention; 2) post‐intervention (after 3‐month intervention); 3) 3‐month follow‐up (3 months post‐intervention/6 months after baseline) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors for the number of participants randomised and potential per‐protocol analysis (Mache 2017b [pers comm]) Study start/end date: 96 junior physicians included between February and August 2014; exact study dates not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified if approved; all procedures in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975 Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Dr Stefanie Mache, Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf, Seewartenstrasse 10, 20459 Hamburg, Germany; s.mache@uke.de |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "physicians were randomized into an intervention and control group." Quote: "Baseline data on gender, age, and perceived health indicate only small, insignificant differences between the control and the intervention group." Judgement comment: insufficient information about random sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic characteristics and perceived health; baseline comparability for outcome variables unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (online questionnaires); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Of the 45 participants in the intervention group, three were excluded due to health reasons (operation, accident). In addition, two participants of the control group did not respond to the follow‐up questionnaires. In sum, 42 physicians took part in the intervention group, and 43 participated in the control group." Judgement comment: 90 randomised (according to information received from authors); in part, reasons for missing data unlikely to be related to true outcome with relative balance in missing data between groups (IG: 3 exclusions due to health reasons), CG: 2 did not complete follow‐up (reasons not specified); available‐case analysis (only participants for whom outcomes were obtained at 3 time points) and per‐protocol analysis (only participants who took part in allocated intervention) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available, but it is clear that the published report includes all expected outcomes, including those that were prespecified |
Mache 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified; small sample size Imputation of missing data: no imputation of missing data; information received from authors (Mache 2018 [pers comm]): per‐protocol analysis (only participants who took part in allocated intervention and were not excluded) |
|
| Participants |
Country: Germany Setting: psychiatric clinics/hospital departments specialising in psychiatric medicine Age: mean = 33 (SD = 2.3) years Sample size (randomised): 76 Sex: 51 women, 21 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: perceived stress (PSQ): IG = 61.2 (18.9), CG = 59.8 (17.7); IG with high level of stress, CG with moderate level of stress Population description: physicians working in psychiatric units from 12 hospital departments in the North of Germany specialising in psychiatric medicine Inclusion criteria: 1) employment as a psychiatrist in a psychiatric department; 2) working full‐time; 3) being able and willing to take part in the study; 4) agreement to complete a survey at least 3 times Exclusion criteria: not specified Attrition (withdrawals and exclusions): 4 exclusions (information received from authors; Mache 2018 [pers comm]): IG = 1/38 (2.6%), CG = 3/38 (7.9%)) Reasons for missing data: health reasons (sickness absence) |
|
| Interventions |
Intervention: self‐care skills training/psychosocial skills training combined with cognitive behavioural and solution‐focused counselling (n = 38 according to information received from authors; after exclusions: n = 37)
Control: no intervention (n = 38 according to information received from authors; after exclusions: n = 35) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured: 1) pre‐intervention; 2) post‐intervention (after 3‐month intervention); 3) 3‐month follow‐up (3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors for the number of participants randomised and potential per‐protocol analysis (Mache 2018 [pers comm]). Study start/end date: not specified Funding source: not specified Declaration of interest: no conflicts of interest reported Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Stefanie Mache, Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf, Seewartenstraße 10, 20459 Hamburg, Germany; s.mache@uke.de |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The study was designed as a controlled trial." Quote: "Seventy‐six psychiatrists gave their consent to join the self‐care training. These physicians were randomised into two groups through a computer‐generated algorithm." Quote: "Only small, insignificant differences between intervention and control group have been found in baseline data on gender, age and working experience." Judgement comment: The investigators describe a random component in the sequence‐generation process (computer random‐number generator) and there is verified baseline comparability between groups for sociodemographic characteristics.; baseline comparability for outcome variables unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "single‐blind trial" Judgement comment: only participants were blinded; no blinding of personnel (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ (online questionnaires) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Of the 76 participants participants four needed to be excluded due to health reasons (sickness absence). In sum, 37 physicians took part in the intervention group (IG) and 35 participated in the control group (CG)." Judgement comment: reasons for missing data unlikely to be related to true outcome (4 exclusions due to health reasons, IG: 1, CG: 3); information received from authors: per‐protocol analysis (only participants who took part in allocated intervention and were not excluded) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Mache 2017.
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): statistical power analysis performed and showed that a sample size of 80 would provide statistical power (2‐tailed, α = 0.05) of > 85%; therefore, size of the included study groups was considered sufficient for this pilot study, after weighing statistical considerations along with logistical and resource constraints Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. without 2 participants in IG who participated in < 80% of training sessions) and available‐case analysis (i.e. only participants for whom outcomes were obtained at follow‐up assessments) | |
| Participants |
Country: Germany
Setting: junior physicians in gynaecology and obstetrics; exact training setting not specified (training sessions performed off duty)
Age: mean = 27.5 (SD = 2.2) years
Sample size (randomised): 80
Sex: 54 women, 26 men
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: emotional exhaustion (subscale of MBI): IG = 4.10 (0.63), CG = 4.19 (0.71) Population description: junior physicians in gynaecology and obstetrics Included criteria: 1) employment in gynaecology/obstetrics; 2) being employed full‐time; 3) a maximum of 2 years of work experience in gynaecology or obstetrics; 4) participation in the study during the next 9 months; 5) access to the internet and e‐mail Excluded criteria: not specified Attrition (withdrawals and exclusions): exclusions (from follow‐up analyses): n = 2 in IG; withdrawals (losses to follow‐up at follow‐ups 1 to 3): follow‐up 1: 6 (IG: 1, CG: 5); follow‐up 2: 5 further losses to follow‐up (IG: 4, CG: 1); follow‐up 3: 7 further losses to follow‐up (IG: 2, CG: 5) Reasons for missing data: for 2 exclusions: participation in < 80% of training sessions; reasons for losses to follow‐up at assessments in 2 groups not specified |
|
| Interventions |
Intervention: coping skills training/psychosocial skills training (n = 40)
Control: no intervention (n = 40)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (after final session of training; follow‐up 1); 3) 3‐month follow‐up (3 months after final session of training; follow‐up 2); 4) 6‐month follow‐up (6 months after final session of training; follow‐up 3) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to ask whether they performed available‐case analysis with participants for whom outcomes were obtained at follow‐up assessments (Mache 2019b [pers comm]). Study start/end date: not specified Funding source: not specified Declaration of interest: no conflict of interest declared Ethical approval needed/obtained for study: approved by IRB of the Free University Berlin Comments by study authors: not specified Miscellaneous outcomes by the review authors: information received from authors (Mache 2019b [pers comm]): correct that available‐case analysis only with participants for whom outcomes were obtained at follow‐up assessments for outcomes reported in Table 2 of the publication (e.g. assessment II: n = 37 in IG and n = 35 in CG) Correspondence: Stefanie Mache; Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf, Seewartenstrasse 10, 20459 Hamburg, Germany; Institute of Occupational Medicine, Social Medicine and Environmental Medicine, Goethe‐University, Theodor‐SternKai 7, 60590 Frankfurt Am Main, Germany; s.mache@uke.de |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "In a two‐arm randomized controlled trial junior physicians working in clinic departments of Gynecology and Obstetrics were divided into two groups: (1) intervention group (IG) and (2) control group (CG)." Quote: "second the participants were randomized into two groups (intervention and control group). This procedure was supported by a computer generated list of numbers." Quote: "The demographic variables including gender, age, years of working experiences are shown in Table 1. 69 % of the physicians in the intervention group were women (n = 26) and 31 % were men (n = 12). The comparison group include 70 % female physicians (n = 28) and 30 % male physicians (n = 12). The average age in the intervention group was 27 years (SD 2.1) with an average time of working experience as a physician of 1 year (SD 1.8). All the gynecologists were employed full‐ time. Comparing both groups (IG and CG) baseline data on socio‐demographic differences indicate insignificant differences." Judgement comment: The investigators describe a random component in the sequence‐generation process (computer‐generated list of numbers)and there is verified baseline comparability of groups for sociodemographic characteristics (age, gender, relationship status, work characteristics, place of work); baseline comparability for outcome variables (see T0 in Table 2) unclear (i.e. statistical significance not specified) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ (method of concealment is not described) |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (online surveys); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Fig. 1 Flow chart of the study design" Quote: "Of the 80 junior physicians enrolled, all completed the baseline measures. Two physicians of the IG were excluded for the follow‐up analyses because they participated in less than 80 % of the training sessions." Quote: "As illustrated in Fig. 1, during follow‐up 1, 37 of the participants in the IG (98 %) gave responses, and 33 (n = 87 %) gave responses for follow‐up 2. Finally, 31 physicians of the IG (82 %) answered the last survey (follow‐up 3). Participants who failed to complete the follow‐up surveys did not differ in their baseline responses from those who complied with the study protocol." Judgement comment: reasons for missing data likely to be related to true outcome with slight imbalance in missing data between groups (n = 2 excluded in IG due to < 80% participation in training sessions; follow‐up 1: IG: n = 1, CG: n = 5; follow‐up 2: IG: n = 5, CG: n = 6; follow‐up 3: IG: n = 7, CG: n = 11); per‐protocol analysis (i.e. exclusion of physicians participating in < 80% of training sessions); available‐case analysis (only participants for whom outcomes were obtained at follow‐up assessments) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Mealer 2014.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not done because the intent was to determine feasibility and acceptability; recruitment was not based on a power calculation Imputation of missing data: no imputation of missing data for 2 participants withdrawn before intervention; per‐protocol analysis (only participants who took part in allocated intervention); missing data in scales inferred by mean of remaining items |
|
| Participants |
Country: USA Setting: academic institution, ICU Age: see Population description; age not specified Sample size (randomised): 29 Sex: 24 women, 5 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: 100% of the ICU nurses (n = 27) were positive for symptoms of anxiety (HADS, score ≥ 8) and 77% were positive for symptoms of depression (HADS score ≥ 8); high rate of burnout syndrome (MBI): 81% were positive for emotional exhaustion, 77% were positive for depersonalisation, and 77% were positive for a decrease in personal accomplishment; median resilience score (CD‐RISC) was 73 (range = 67 ‐ 77); 44% of the ICU nurses met the diagnostic criteria for post‐traumatic stress disorder Population description: ICU nurses from an academic institution; medical, surgical, burn, and cardiac ICUs Inclusion criteria: 1) currently working 20 hours a week at the ICU bedside; 2) had no underlying medical condition that would be a contraindication to exercise; 3) scored 82 or less on the CD‐RISC Exclusion criteria: 1) were unable to participate in a 2‐day educational workshop or 2) had a medical condition that would limit exercise Attrition (withdrawals and exclusions): 2 withdrawn before start of the training period (IG = 1/14 (7.1%), CG = 1/15 (6.7%)) Reasons for missing data: not specified |
|
| Interventions |
Intervention: multimodal resilience training programme (n = 14)
Control: no intervention (but assessment of exercise) (n = 15) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (within 1 week post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the means and SDs for outcome measures in the 2 groups at each time point (Mealer 2017 [pers comm]). Study start/end date: recruited from October 2012 to December 2012; exact study dates not specified Funding source: funded by a grant from the National Institutes of Health (grant number K24 HL‐089223‐07) Declaration of interest: not specified Ethical approval needed/obtained for study: approved by the Colorado Multiple IRB Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Meredith Mealer, Division of Pulmonary Sciences and Critical Care Medicine, Department of Medicine, University of Colorado School of Medicine, 12700 E 19th Ave, C‐272, Aurora, CO 80045; Meredith.Mealer@ucdenver.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Of the 29 remaining ICU nurses, 14 were randomized to the intervention arm and 15 were randomized to the control arm." Quote: "Measures of PTSD, burnout syndrome, resiliency, and symptoms of anxiety or depression did not differ significantly between the 2 groups" Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for outcome variables; baseline comparability for sociodemographic variables (statistical (non)significance of differences, see Table 1) unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (blinding for data assessed within the intervention via REDCap data management system (e.g. time spent exercising, MBSR practices) and for data analysis, but unclear who delivered the questionnaires to the participants); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Two participants withdrew from the study before the start of the 12‐week training period: 1 from the intervention arm and 1 from the control arm. Therefore, 27 participants participated in the 12‐week trial (intervention arm, n = 13; control arm, n = 14)." Quote: "No participants dropped out of the study." Quote: "Missing items on scales were inferred by using the mean of the remaining items on the scale." Judgement comment: reasons for missing data unlikely to be related to true outcome with balance in missing data between groups (IG: n = 1; CG: n = 1 before start of intervention period); reasons not specified; per‐protocol analysis (only participants who took part in allocated intervention) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available, but it is clear that the published report includes all expected outcomes, including those that were prespecified |
Medisauskaite 2019.
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): appropriate sample size was calculated using G*Power software: repeated measures, within‐between subject interaction (α error probability = 0.05; power = 0.95; 2 groups; measured at 2 time points; 0.5 correlation between repeated measures; medium effect size F of 0.25) (Faul 2007); calculated actual power was 0.95 for sample of 54 participants, 27 participants in each group Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. main comparison: without 23 participants in IG4 who did not complete the intervention; identical to remaining 3 trial groups in overall analysis) and available‐case analysis (i.e. only participants for whom outcomes were obtained and who completed questionnaires; i.e. excluding participants lost to follow‐up) | |
| Participants |
Country: UK
Setting: doctors; training; setting not specified
Age: for all 5 groups, mean = 47.88 (SD = 11.21) years
Sample size (randomised): 381 (randomised) to 5 groups; 150 participants in the main comparison (IG4 vs CG)
Sex: 42 women, 49 men (out of 91 analysed from IG4 and CG)
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: burnout, emotional exhaustion (MBI): IG = 3.26 (1.41), CG = 3.2 (1.4); burnout, depersonalisation: IG = 1.98 (1.49), CG = 1.68 (1.29); burnout, personal accomplishment: IG = 4.42 (0.83), CG = 4.41 (0.84); anxiety (GAD‐7): IG = 0.96 (0.81), CG = 0.88 (0.74); psychiatric morbidity (GHQ): IG = 2.14 (0.57), CG = 2.17 (0.61); alcohol dependence (AUDIT): IG = 7.5% (3), CG = 10.6% (5) Population description: doctors who currently practice medicine Inclusion criteria: see trial registration; 1) medical doctors across all specialties and professional grades who have regular contact with patients and work in the UK Exclusion criteria: not specified Attrition (withdrawals and exclusions): 154 overall. IG1 = 33 (15 = did not complete intervention, 16 = lost to follow‐up, 2 = came back after more than 23 days (also excluded from analysis)); IG2 = 31 (14 = did not complete intervention, 17 = lost to follow‐up); IG3 = 31 (15 = did not complete intervention, 15 = lost to follow‐up, 1 = came back after more than 23 days (also excluded from analysis)); IG4 = 36 (23 = did not complete intervention, 11 = lost to follow‐up, 2 = came back after 23 questionnaires (also excluded from analysis)); CG = 23 (4 = did not complete questionnaire, 19 = lost to follow‐up) Reasons for missing data: not specified |
|
| Interventions | In total, 5 trial groups:
Intervention: induction programme (see trial registration; trial group 4) (n = 75)
Control: no intervention (n = 75)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to check if the treatment duration was 1e week and if the time 2 assessment took place immediately post‐intervention or at 1‐week follow‐up.; no response to 2 inquiries Study start/end date: see trial registration: July 2016 to November 2016 Funding source: see trial registration: Birkbeck College, University of London; RCT was not funded or determined by Focus Games or any organisation involved with the app/board game Declaration of interest: After the RCT was completed, the authors and Focus Games transformed the intervention into an app that is currently being trialled in several NHS hospitals for use by doctors and other clinicians. The authors, Focus Games and the National Health Service Practitioner Health Programme also developed a board game for healthcare professionals. The RCT was not funded or determined by Focus Games or any organisation involved with the app/board game. The RCT was conducted for PhD research and it took place a year before Focus Games got in touch with the authors Ethical approval needed/obtained for study: approved by BEI (School of Business, Economics and Informatics) Ethics Committee at Birkbeck, University of London in May 2016; institutional ethics approval covering all data sources, and NHS local approval covering NHS trusts that agreed to invite their doctors to take part in the trial Comments by study authors: study protocol registered before the study began at the US National Institute of Health (Identifier: NCT02838290; ClinicalTrials.gov, 2016) Miscellaneous outcomes by the review authors: not relevant Correspondence: Dr Asta Medisauskaite, Research Department of Medical Education, UCL Medical School, London, UK; a.medisauskaite@ucl.ac.uk |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "This was a randomized controlled trial comprising of two independent variables: time and trial group." Quote: "Blindly to the researchers, Qualtrics software randomly assigned doctors to one of 5 trial groups" Quote: "doctors were randomly and blindly assigned to one of 5 trial groups." Quote: "Table 1 shows that there were no significant differences between the two trial groups at baseline, (p > .05; see table 1)." Judgement comment: The investigators describe a random component in the sequence‐generation process (Qualtrics software); baseline comparability reported for control group vs trial group 4 (main focus of our review) and comparison control group and all experimental groups, respectively; MAIN COMPARISON (control group vs trial group 4): verified baseline comparability of groups for sociodemographic characteristics and outcome variables of interest on the basis of analysis (see Table 1; P > 0.05; see Supplement 2 Table 1 for secondary outcome variables in all groups; P > 0.12); CONTROL GROUP & ALL EXPERIMENTAL GROUPS: verified baseline comparability for most sociodemographic characteristics (except for gender, P = 0.03) and outcome variables on the basis of analysis (Supplementary material 1, Table 1 and 2) |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Blindly to the researchers, Qualtrics software randomly assigned doctors to one of 5 trial groups" Quote: "doctors were randomly and blindly assigned to one of 5 trial groups." Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ ("blindly assigned"; but method of concealment is not described in sufficient detail; unclear if random‐sequence generation was also concealed from participants) |
| Blinding of participants and personnel (performance bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of participants and personnel to permit judgement of ‘Low risk’ or ‘High risk’ (e.g. unclear if online intervention or face‐to‐face) |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Judgement comment: reasons for missing outcome data likely to be related to true outcome, with imbalance in numbers for missing data across groups (IG4: 23 did not complete intervention, 11 lost to follow‐up, 2 questionnaire came back after more than 23 days; CG 3 did not complete the questionnaire, 19 lost to follow‐up); per‐protocol analysis (i.e. only participants who completed the intervention(s) and available‐case analysis (only participants for whom outcomes were obtained, i.e. who completed questionnaires) |
| Selective reporting (reporting bias) | Low risk | Quote: "The study protocol was registered before the study began at the US National Institute of Health (Identifier: NCT02838290; ClinicalTrials.gov, 2016)." Judgement comment: trial registration available (NCT02838290) available and all of the study’s prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way (secondary outcomes for all groups reported in Supplementary material 2) |
Mirzaeirad 2019.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): according to a priori sample size calculation at least 34 persons required in each group according to similar studies Imputation of missing data: not specified |
|
| Participants |
Country: Iran
Setting: hospital (intervention performed in the place of hospital training courses)
Age: 42 (52.5%) < 31 years, 28 (35%) > 31 years
Sample size (randomised): 80 (after exclusions)
Sex: 66 women, 14 men
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: nurses Inclusion criteria: 1) undergraduates with at least 1 year of hospital experience and specialty areas (operating room, children and emergency); 2) lack of physical disabilities or mental stress; 3) failure to receive interventions or classes related to stress reduction during the past year in the workplace; 4) absence of severe stress and emotional crisis (e.g. death of first‐degree relatives during last year) Exclusion criteria: 1) participants stating that they had any disabling physical and psychological problems; 2) unwillingness to co‐operate or continue participating in the study Attrition (withdrawals and exclusions): 4 (IG = 2, CG = 2) Reasons for missing data: IG = lack of full participation in the workshop (n = 2); CG = change of location (n = 1), unwillingness to continue co‐operation (n = 1) |
|
| Interventions |
Intervention: resilience‐skills training (n = 40; after exclusions)
Control: not specified (n = 40; after exclusions) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 1‐month follow‐up (1 month post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the number of participants randomised to each group and to ask for the means and SDs for the outcome of nursing stress in the 2 groups at each time point. We also asked for the treatment duration in weeks/months and whether the authors performed a per‐protocol analysis, but received no response to 2 inquiries. Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: approved by Ethics Committee of the University of Social Welfare and Rehabilitation Sciences Comments by study authors: article is taken from the dissertation of Seiedeh Zahra Mirzaeirad at the University of Social Welfare and Rehabilitation Sciences (Moral Code 144.1394.REC.USWR.IR) Miscellaneous outcomes by the review authors: article in Persian (translated) Correspondence: Seiedeh Zahra Mirzaeirad; corresponding author: Narges Arsalani, Associate Professor, Department of Nursing, Faculty of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran; nargesarsalani@gmail.com |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The present study is quasi‐experimental. Participants included nurses working in hospitals in Golestan province who were randomly selected and randomly assigned to participate in the study." Quote: "ی گردد. یافته ها <b>در جدول 4 توزیع بر عالوه ، متغ یرهای نشان شناختی جمعیت م ی دهد که گروه دو به همگن توزیع با متغیرها سایر جنسیت متغیر از بغیر یافتند اختصاص شاهد و مداخله ( 15 / 1 < P</b> ) . جدول 3 نشان" ["In Table 2, in addition to the distribution of demographic variables, it is shown that except for gender, other variables were homogeneously distributed between the intervention and control group (p > .05)."] Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic characteristics (see Table 2; except for gender) and outcome variable nursing stress on the basis of analysis (see Table 3) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be related to true outcome |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "پایان مداخله،۴۰ پرسشنامه تکمیل شده مورد بررسی قرار گرفت. " [At the end of the intervention, 40 completed questionnaires were evaluated.] Quote: " از این تعداد در گروه آزمون ۴ نفر به سبب عدم شرکت کامل در کارگاه آموزشی، در گروه شاهد یک نفر به علت تغییر محل خدمت و یک نفر به علت عدم تمایل به ادامه همکاردند. [Four participants were excluded, 2 from the study group due to lack of full participation in the workshop, one in the control group due to change of location and one due to unwillingness to continue cooperation.] Judgement comment: reasons for missing data likely to be related to true outcome (see reasons for exclusions in both groups); per‐protocol analysis |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Mistretta 2018.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: according to report, clusters based on schedule availability; additional information received from authors (Mistretta 2018 [pers comm]): not multiple groups/clusters for each treatment; judged as misnamed study with individual randomisation stratified for schedule availability Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified; intention‐to‐treat analysis |
|
| Participants |
Country: USA Setting: Mayo Clinic (major tertiary healthcare institution) Age: mean = 46.0 (SD = 12.6, range = 22‐80) years Sample size (randomised): 60 Sex: 52 women, 8 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: average stress scores (DASS‐21) suggested mild levels of stress (7.9 (3.5)); average scores for depression (DASS‐21; 4.8 (3.7)) and anxiety (DASS‐21; 4.0 (2.9)) fell within range, suggesting relatively little depression and anxiety; mean well‐being WHO (Five) Well‐Being Index, WHO‐5) scores at baseline were 12.9 (4.1) indicating moderate levels of well‐being; mean baseline score for the burnout subscales (MBI‐HSS) suggest moderate level of emotional exhaustion (23.9 (11.8)) above normative levels, a low level of depersonalisation (5.5 (5.1)), and a moderate level of personal accomplishment (37.1 (6.4)) Population description: employees at the Mayo Clinic in Arizona, a large research hospital and medical centre Inclusion criteria: 1) being an employee working at Mayo Clinic, Arizona; 2) aged 18 years or older; 3) owning a smartphone; 4) scoring at least 5 on the DASS‐21 stress subscale Exclusion criteria: not specified Attrition (withdrawals and exclusions): post‐intervention: 6 provided no post‐intervention data; 3‐month follow‐up: 16 provided no follow‐up data with similar attrition rates across groups (IG1 = 6/22 (27.2%); IG2 = 5/23 (21.7%), CG = 5/15 (33.3%)) Reasons for missing data: not specified |
|
| Interventions |
Intervention 1: Mindfulness‐Based Resilience Training (MBRT) (n = 22)
Intervention 2: Smartphone Resilience Training (n = 23)
Control: no intervention (were offered training at the conclusion of trial) (n = 15) |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 3‐month follow‐up (3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors to get more information about the cluster randomisation (Mistretta 2018 [pers comm]). Study start/end date: not specified (April 2015 ‐ March 2016 according to trial registration) Funding source: Mayo Clinic Arizona‐Research Funds and Horizon 2020 Declaration of interest: Christopher Lorenz is a Director of Soma Analytics. Ethical approval needed/obtained for study: approved by Mayo Clinic IRB Comments by authors: trial registration: ClinicalTrials.gov Registration number: NCT02419430; URL: clinicaltrials.gov/ct2/show/study/NCT02419430 Miscellaneous outcomes by the review authors: information received from authors (Mistretta 2018 [pers comm]) that there were no multiple groups for each treatment and that ICCs could not be calculated. Correspondence: Erin G. Mistretta, Department of Psychology, Arizona State University, 950 S. McAllister Ave., Room 237, P.O. Box 871104, Tempe, AZ 85287; egmistretta@asu.edu; Trial registration: Cynthia Stonnington, MD, Associate Professor of Psychiatry, Mayo Clinic, Stonnington.Cynthia@mayo.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Eligible participants were randomized using a cluster randomization procedure based on schedule availability." Quote: "Once participants agreed upon a time, they were then randomized to either the Mindfulness Based Resilience Training (MBRT) intervention (n = 22), the smartphone resilience intervention app (n = 23), or the control group (n = 15)." Quote: "Results of ANOVA and chi‐square analyses (adjusted with Bonferroni correction) comparing groups on demographic characteristics and baseline levels of functioning showed that the groups were comparable on all measures. Furthermore, there were no significant differences in baseline MBI scores when comparing participants based on job roles (data not shown). Thus, randomization was successful in creating groups that were equivalent at baseline." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic variables and outcome variables on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: blinding of participants and personnel probably not done for MBRT intervention (face‐to‐face intervention); blinding of participants and personnel for smartphone resilience intervention app unclear; review authors judge that the outcome (sleep monitoring via actigraphy) is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done for MBRT intervention (face‐to‐face intervention); blinding for smartphone resilience intervention app unclear; outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: insufficient information on possible blinding of outcome assessment, but the review authors judge that the outcome measurement (sleep monitoring via actigraphy) is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias for MBRT intervention (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Rates of Attrition. Of the 60 participants randomized to groups, 54 (90%) provided post‐intervention data, 44 (73%) provided three‐month follow‐up data, and 74% of participants completed measures at all three time points. The rates of attrition were similar across groups with 27.2% attrition for MBRT, 21.7% attrition for smartphone resilience training, and 33.3% attrition for the control group (p = .76)." Quote: "There were no significant differences in baseline measures or demographics between those who completed the intervention and those who did not." Quote: "One‐way ANOVA’s [pre‐treatment, post‐treatment, 3‐month follow‐up] using intent‐to‐treat analyses for each group separately revealed that both the MBRT and the Smartphone groups showed improvements over time in key outcomes, whereas the control group showed no evidence of change" Judgement comment: reasons for missing outcome data unlikely to be related to true outcome with balance in missing data between groups (IG1: 27.2% attrition, IG2: 21.7%, CG: 33.3%, P = 0.76); intention‐to‐treat analysis |
| Selective reporting (reporting bias) | High risk | Judgement comment: trial registration available (NCT02419430); several reported outcomes were not prespecified; follow‐up period prespecified was not reported; PRESPECIFIED: DASS‐21 from baseline to 6 months; REPORTED: WHO‐5, DASS‐21, MBI‐HSS, SCS, compassion to others, daily affect, relationship quality, valued action, and sleep monitoring via smartphone app at baseline, post‐intervention and 3‐month follow‐up |
NCT02603133.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: sequential assignment Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
|
| Participants |
Country: USA Setting: NICU Age: not specified Sample size (randomised): 2650 (actual enrolment) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: NICU healthcare professionals Method of recruitment: not specified Inclusion criteria: 1) age: 18 ‐ 85 years; 2) location: newborn centre, i.e. the NICU or a step‐down unit; 3) provider: a) primary work place is the Newborn Center, b) full‐time equivalent of ≥ 40%, c) date of hire more than 4 weeks before start of the intervention; 4) provider groups: a) attendings that identify your newborn centre as their primary site of work (not physicians from satellite NICUs), b) NICU fellows, c) nurse practitioners, d) physician assistants, e) nurses, including nurse leadership (managers, educators), f) nurse assistant, g) respiratory‐care providers, h) transport specialists if primarily neonatal transport team, i) newborn centre social worker, j) newborn centre clerks, k) newborn centre pharmacists, l) newborn centre physical, occupational, speech, and developmental therapists, m) newborn centre nutritionists, n) newborn centre lactation consultants Exclusion criteria: 1) location: labour and delivery or the newborn nursery; 2) provider: work is delivered mostly outside the newborn centre (this may affect providers who deliver services across the hospital such as residents, surgeons, anaesthetists, consultants, nutritionists, physical therapists/occupational therapists (these are included if they are mostly dedicated to the newborn centre); 3) float personnel; 4) those who do not speak English; 5) those who cannot operate computer or smart phone Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: web‐based implementation for the science of enhancing resilience (WISER 2.0) (n not specified)
Control: wait‐list control (n not specified); however, contradicting information in trial registration whether cohort 2 serves as wait‐list control for cohort 1 vs receives lecture on safety culture (unrelated to burnout intervention) or both |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Other outcome
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) 10 days; 3) 1 month; 4) 6 months; 5) 12 months; time points reported not specified Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the status of the trial (which changed from ongoing study to completed but unpublished study during the review process) (Profit 2018 [pers comm]). We also asked for more information about the study design and the form of control group (1 inquiry), but did not receive a response at the time of writing the review Study start/end date: July 2016 to August 2018 (actual study completion date) Funding source: Stanford University; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD); Duke University Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: information received from authors: trial completed but unpublished (Profit 2018 [pers comm]; based on information in trial registration not clearly enough if 2 or 3 cohorts and if wait‐list or active control (see lecture on safety culture), due to different information provided Correspondence: primary investigator: 1) Jochen Profit MD, Associate Professor of Pediatrics, Director of Perinatal Health Systems Research, Stanford University, USA; profit@stanford.edu; 2) J. Bryan Sexton, PhD; Duke University, USA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (see trial registration): "The investigators will test the efficacy of the WISER Program in the NICU setting using a stepped‐wedge mixed‐methods randomized controlled trial (swRCT) at six tertiary care NICUS." Quote (see trial registration): "Two blocks with 3 NICUS will be randomly assigned to one of two intervention cohorts." Quote (see trial registration): "Participants are individually randomized to one of two cohorts." Judgement comment: based on trial registration, insufficient information about random‐sequence generation to permit judgement of 'Low risk' or 'High risk'; no judgement on baseline comparability for sociodemographic and outcome variables possible based on trial registration |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: based on trial registration, insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk' |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Quote (see trial registration): "Masking: None (Open Label)" Judgement comment: open‐label study; based on trial registration probably no blinding of participants and personnel, but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote (see trial registration): "Masking: None (Open Label)" Judgement comment: open‐label study; based on trial registration probably no blinding of participants and personnel and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Quote (see trial registration): "Masking: None (Open Label)" Judgement comment: based on trial registration, insufficient information about blinding of outcome assessment (unclear if 'no masking' refers to outcome assessment), but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Quote (see trial registration): "Masking: None (Open Label)" Judgement comment: based on trial registration, insufficient information about blinding of outcome assessment (unclear if 'no masking' refers to outcome assessment); however, due to performance bias (no masking), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: no judgement possible based on trial registration |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: no judgement possible based on trial registration |
NCT03645798.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): sample size calculation conducted with statistical software; effect size was 0.67, power was 0.80, and margin of error type I was 0.05; accordingly, sample size was 64 Imputation of missing data: not specified in trial registration |
|
| Participants |
Country: ChinaSetting: nurses; online/mobile‐based intervention (Wechat‐based)Age: not specified Sample size (randomised): probably 102Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: nurses Inclusion criteria: 1) registered nurses or licensed practical nurses; 2) who provide direct care to residents; 3) whose MBI‐GS scores are no less than 1.5; 4) who do not take any hormone therapy; 5) are Chinese speakers Exclusion criteria: 1) student nurses; 2) those who suffer from diseases that influence their hormone levels; 3) those who participated in similar studies; 4) those who have no interest in this study Attrition (withdrawals and exclusions): 102 nurses who met inclusion criteria and were randomly selected for study; only 73 participants completed the study (IG = 33; CG = 40) Reasons for missing data: not specified |
|
| Interventions |
Intervention: Wechat‐based “Three good things” positive psychotherapy (after dropouts: n = 33)
Control: TAU (after dropouts: n = 40)
|
|
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes:
Other outcomes:
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (i.e. immediately after 6‐month intervention); time points reported not specified Adverse events: not specified in trial registration |
|
| Notes | Contact with authors: We contacted the authors to see if the trial was published in the meantime, but received no response to 2 inquiries. Study start/end date: see trial registration: July 2015 to January 2016 Funding source: Central South University Declaration of interest: not specified Ethical approval needed/obtained for study: approval by IRB of Xiangya Nursing School, Central South University Comments by study authors: not specified Miscellaneous outcomes by the review authors: no information about publication status received from authors; corresponding study protocol and statistical analysis plan: clinicaltrials.gov/ProvidedDocs/98/NCT03645798/Prot_SAP_000.pdf Correspondence: Jingping Zhang (study director), Central South University, Changsha, Hunan, China, 410013; jpzhang1965@163.com | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (see trial registration): "A randomized, controlled trial was conducted for 73 Chineses nurses from The Second Xiangya Hospitcal of Central South University (33 in the experimental group, 40 in the control group)." Judgement comment: based on trial registration, insufficient information about random‐sequence generation to permit judgement of 'Low risk' or 'High risk'; no judgement on baseline comparability for sociodemographic and outcome variables possible based on trial registration |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: based on trial registration, insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk' |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Quote: "Masking: Single (Investigator)" Judgement comment: online intervention (Wechat group) vs normal psychological instruction from hospital; based on trial registration, single‐blinded study (i.e. investigators blinded), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "Masking: Single (Investigator)" Judgement comment: online intervention (Wechat group) vs normal psychological instruction from hospital; based on trial registration, single‐blinded study (i.e. investigators blinded) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: based on trial registration, insufficient information about blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: based on trial registration, insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote (see trial registration): "102 nurses who met the inclusion criteria were randomly selected for the study. However, only 73 completed the study, with 33 in the experimental group and 40 in the control group." Judgement comment: no judgement possible based on trial registration (number of participants randomised to each group not stated; number of dropouts not specified for each group; n = 73 completed the study, but unclear if only n = 73 were analysed) |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: no judgement possible based on trial registration |
Poulsen 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): Working from these bases, a medium effect size (f = 0.4), with α = 0.05 and β = 0.95 was chosen because of the exploratory nature of this study and the clinical significance of even relatively moderate effects from training. With 2 groups of participants (IG and CG), a total sample of 64 was required, and therefore 80 participants were recruited to allow for dropouts and incomplete data sets. Imputation of missing data: no imputation of missing data; available‐case analysis (only participants with complete data sets) |
|
| Participants |
Country: Australia Setting: radiation oncology departments of 2 hospitals Age: 5 (7%) aged 25 years, 26 (37%) aged 25 ‐ 35 years, 14 (20%) aged 36 ‐ 45 years, 25 (36%) aged > 45 years (in analysed sample; after exclusion of 10 participants) Sample size (randomised): 80 Sex: 58 women, 12 men (in analysed sample; after exclusion of 10 participants) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: radiation therapists and oncology nurses Inclusion criteria: 1) being a radiation therapist or an oncology nurse; no gender, religious or racial restrictions Exclusion criteria: not specified Attrition (withdrawals and exclusions): 10/40 (25%) participants in IG only excluded from analysis Reasons for missing data: incomplete data sets |
|
| Interventions |
Intervention: written educational material + recovery training programme/workshop on recovery from job stress (n = 40)
Control: active control (written educational information only) (n = 40)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) at the end of every week (during 6 weeks); 3) 6‐week follow‐up (6 weeks post‐intervention: 1‐day intervention; at the end of the 6‐week period); time points during 6 weeks indirectly reported in MANOVAs and for REQ in figure Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: not specified Funding source: funded by the Princess Alexandra Hospital Research Foundation Declaration of interest: conflict of interest: Anne A. Poulsen is Director of Work Life Balance Solutions (Queensland). Ethical approval needed/obtained for study: ethical clearance obtained from the Hospital Ethics Committee, which oversaw research at the 2 hospitals where the ONs and RTs worked Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Dr Anne A. Poulsen, Mater Medical Research Institute, 31 Raymond Tce, South Brisbane, Queensland 4101, Australia; a.poulsen@uq.edu.au |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants who completed consent forms and a pre‐training questionnaire were randomised using computer‐generated random integers to either the experimental (i.e. workshop plus written educational information) or control (i.e. written educational information‐only) group" Quote: "Demographic data for experimental and control groups are presented in Table 1. There were no significant differences between the two groups for any background variables, allowing data analysis to proceed without their consideration as potential confounds." Quote: "Participants in both groups were proportionally equivalent for gender, age, marital status and caregiver responsibilities." Quote: "Figure 1a (REQ score) shows these data and indicates that, although they were not statistically significant, the mean scores for the experimental group were higher at baseline than those for the control group." Judgement comment: The investigators describe a random component in the sequence generation (computer‐generated random integers)and there is verified baseline comparability of groups for sociodemographic variables and 1 outcome measure (REQ total score).; baseline comparability for other outcomes (perceived sleep quality, satisfaction with self‐care practices) unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Quote: "A strength of the current study was the use of a randomised, controlled design with questionnaires that could not be identified by the staff directly involved in the programme trainings, or by others involved in data entry or analysis." Judgement comment: probably blinding of data entry and analysis, but insufficient information about blinding of outcome assessment (i.e. who delivered the questionnaires to participants); due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "There were 80 participants in total with 40 being randomised to the experimental arm and 40 in the control arm. There were 10 participants with incomplete datasets, leaving a total of 70 who were evaluable." Judgement comment: reasons for missing data likely to be related to true outcome with imbalance in missing data between groups (IG: n = 10, CG: n = 0); available‐case analysis or even complete‐case analysis (only participants with complete datasets) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Schroeder 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; per‐protocol analysis (only participants who took part in allocated intervention) and available‐case analysis (only participants for whom outcomes were obtained at 3 time points) |
|
| Participants |
Country: USA Setting: family medicine and internal medicine departments at Providence Health and Services in Portland, Oregon Age: mean = 42.76 (SD = 8.43, range = 32‐61) years Sample size (randomised): 33 Sex: 24 women, 9 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: MASL: burnout, emotional exhaustion: IG = 26.68 (8.48), CG = 24.52 (10.57); burnout, depersonalisation: IG = 20.87 (8.42), CG = 19.47 (7.90); burnout, personal accomplishment: IG = 40.25 (5.92), CG = 37.52 (6.43) Population description: primary care physicians from the family medicine and internal medicine departments at Providence Health and Services in Portland, Oregon Inclusion criteria: 1) employed as a primary care physician by Providence Medical Group (PMG); 2) working at least 30% time in direct patient care; 3) aged between 25 and 75 years; 4) willing to be randomised to the IG or CG; 5) no prior participation in the same mindfulness‐based intervention (MBI) offered at PMG Exclusion criteria: not specified Attrition (withdrawals and exclusions): after randomisation: 2 withdrawals (IG = 1/16 (6.3%), CG = 1/17 (5.9%)); post‐intervention assessment: 2 withdrawals in CG only (2/17 (11.8%)); follow‐up assessment: 3 withdrawals (IG = 2/16 (12.5%), CG = 1/17 (5.9%)) Reasons for missing data: after randomisation: lack of time or scheduling conflicts; at post‐intervention assessment or at follow‐up assessment: not specified |
|
| Interventions |
Intervention: Mindful Medicine Curriculum (MMC) (n = 16)
Control: wait‐list control (n = 17) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (within 1 week after weekend‐long intervention); 3) 3‐months follow‐up (3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: recruitment and data collection between December 2014 and May 2015 Funding source: funded by Providence Health System Clinical Transformation Council Declaration of interest: not specified Ethical approval needed/obtained for study: approved by the Providence Health and Services IRB Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Michael S. Christopher, PhD, School of Professional Psychology, Pacific University, 190 SE 8th Avenue, Suite 260, Hillsboro, OR 97123; mchristopher@pacificu.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After completing the baseline measures, participants were randomized 1:1 into the intervention or a waitlist control." Quote: "There were no significant differences between the intervention (n = 17) and waitlist control (n = 16) group on any demographic variables (all Ps >.05)." Quote: "The intervention and control groups did not differ on any outcome measures at baseline (all Ps >.05)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic characteristics and outcome variables |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Figure 1 shows the participant flow. A total of 33 physicians provided written consent to enroll in the study, completed the baseline assessment, and were randomized to the MBI or waitlist control. Two participants (1 MBI and 1 waitlist control) withdrew (citing lack of time or scheduling conflicts) after randomization. Two waitlist control group participants withdrew from the study before postintervention assessment, and 2 MBI participants and 1 waitlist control group participant did not complete 3‐month follow‐up." Judgement comment: reasons for missing data unlikely to be related to true outcome with relative balance in missing data between groups (over study course: IG: n = 3; CG: n = 4; reasons for missing data unclear for most missing data); per‐protocol analysis (only participants who took part in allocated intervention) and available‐case analysis (only participants for whom outcomes were obtained at 3 time points) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified (MPQ only assessed in IG at 3‐month follow‐up) |
Smith 2019.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): planned sample size was 40 (n = 29 in conference abstract) Imputation of missing data: not specified in conference abstract |
|
| Participants |
Country: CanadaSetting: critical care and trauma nurses at St Michael’s (tertiary academic hospital in Toronto); exact training setting not specifiedAge: mean = 33 yearsSample size (randomised): 29Sex: 26 women, 3 menComorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: nurses in critical care and trauma settings/acute care nurses Inclusion criteria: see trial registration; 1) nurse in the MSICU and TNICU and the medical/surgical floor; 2) full‐time or part‐time employment status; 3) approval of clinical leader manager; 4) receipt of written informed consent Exclusion criteria: see trial registration; 1) casual employment status; 2) inability to attend intervention days Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: wellness intervention ARISE (n = 16)
Control: no intervention (n = 13)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) 1‐month follow‐up (1 month post‐intervention); 3) 3‐month follow‐up (3 months post‐intervention); reported in conference abstract: changes between pre‐intervention and 1‐month follow‐up (resilience, burnout, compassion satisfaction, secondary trauma) and pre‐intervention and 3‐month follow‐up (resilience) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to see if the study was already published (Smith 2019 [pers comm]). Study start/end date: according to trial registration: February 2017 to October 2017 Funding source: sponsor according to trial registration: St. Michael's Hospital, Toronto Declaration of interest: not specified in trial registration or conference abstract Ethical approval needed/obtained for study: not specified in trial registration or conference abstract Comments by study authors: trial registration: NCT03017469 Miscellaneous outcomes by the review authors: conference abstract; presented at 2019 48th Critical Care Congress of SSCM (Society of Critical Care Medicine), San Diego; manuscript in preparation according to authors Correspondence: Orla Smith, PhD, Li Ka Shing Knowledge Institute, St. Michael's Hospital, Toronto, Canada; SmithO@smh.ca; Tel: 416‐864‐6060 ext. 3179 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We conducted a randomized controlled trial (NCT03017469)" Judgement comment: based on trial registration and conference abstract, insufficient information about random‐sequence generation to permit judgement of 'Low risk' or 'High risk'; based on conference abstract, no information about comparability of groups at baseline or respective analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: based on trial registration and conference abstract, insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk' |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: based on trial registration and conference abstract, no blinding of participants and personnel (face‐to‐face intervention; see trial registration: no masking) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: based on trial registration and conference abstract, insufficient information about blinding of outcome assessment; however, due to performance bias (no masking), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "29 nurses participated (n=16 in the ARISE group and n=13 in the control group)." Judgement comment: based on conference abstract, insufficient information of attrition or exclusions to permit a judgement of ‘Low risk’ or ‘High risk’ (e.g. unclear if there were any missing data and if missing data were imputed) |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: trial registration (NCT03017469) available; no judgement possible based on conference abstract |
Sood 2011.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): A sample size of 40 was selected for this pilot study after weighing statistical considerations along with logistical and resource constraints. In general, for a continuous outcome variable, a sample size of 40 provides statistical power (2‐tailed, α = 0.05) of > 85% to detect a difference of 1 SD between groups. Imputation of missing data: no imputation of missing data; per‐protocol analysis with participants who complied with allocated intervention and for whom outcomes were obtained |
|
| Participants |
Country: USA Setting: Department of Medicine Faculty, clinic Age: IG mean = 46.8 (SD = 8.3) years, CG mean = 50.2 (SD = 5.7) years (unclear for total sample as number of participants considered for baseline characteristics not specified) Sample size (randomised): 40 Sex: comparable gender distribution across 2 study arms (IG = 55% men; CG = 50% men) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: anxiety (SAS): IG = 55.2 (13.6), CG = 50.5 (23.0) Population description: physicians of Department of Medicine Faculty, all academic clinicians Inclusion criteria: 1) being a faculty member of the Department of Medicine; 2) being able and willing to participate Exclusion criteria: 1) a recent (within the past 6 months) psychotic episode; 2) clinically significant, acute, unstable neurological, psychiatric, hepatic, renal, cardiovascular, or respiratory disease that prevented participation in the study Attrition (withdrawals and exclusions): of the 40 enrolled, 32 (80%) physicians completed the study; 8/20 (40%) participants in the CG declined to participate after randomisation and prior to filling out any assessments Reasons for missing data: scheduling issues in CG |
|
| Interventions |
Intervention: SMART (n = 20)
Control: wait‐list control (n = 20)
|
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Time points measured and reported: 1) pre‐intervention; 2) 2‐month follow‐up (8 weeks after single session intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: not specified Funding source: Department of Medicine, Mayo Clinic, Rochester, MN Declaration of interest: none disclosed Ethical approval needed/obtained for study: study protocol reviewed and approved by Mayo Foundation IRB Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Amit Sood, MD, Complementary and Integrative Medicine Program, Division of General Internal Medicine, Mayo Clinic, 200 First Street SW, Rochester, MN 55905, USA; sood.amit@mayo.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After obtaining the informed consent, physicians were randomly assigned to one of two groups an active arm or a wait‐list control arm." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and no apparent baseline differences between randomised groups for mean age, gender, baseline stress and resilience measures; verified baseline comparability of groups for some sociodemographic variables (age, gender) and outcome measures (stress, resilience); but statistical (non)significance not reported and baseline comparability for other variables also unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Figure 1. Flow diagram of the progress in a randomized clinical trial to assess the effect of resiliency training among physicians." Quote: "Of the 40 enrolled (all academic clinicians), 32 (80%) physicians completed the study. Eight participants (all in the control arm) declined to participate after randomization and prior to filling out any assessments because of scheduling issues (Fig. 1)." Judgement comment: reasons for missing outcome data likely to be related to true outcome with imbalance in numbers for missing data (only missing data in CG, n = 8); per‐protocol analysis with participants who complied with allocated intervention and for whom outcomes were obtained |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available, but it is clear that the published report includes all expected outcomes, including those that were prespecified |
Sood 2014.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): A sample size of 40 was calculated after weighing statistical and logistical considerations. To detect a difference between groups with a 2‐sided, 5% significance level and power of 85% using continuous outcomes, a sample size of 20 participants per group was necessary; level of power achieved not specified Imputation of missing data: for 4 participants (IG = 2, CG = 2) who did not complete the week 12 assessments, baseline values were carried forward to week 12, to provide the most conservative estimate of efficacy; intention‐to‐treat analysis |
|
| Participants |
Country: USA Setting: Department of Radiology, Mayo Clinic, Rochester Age: mean = 47.8 (SD = 7.09) years Sample size (randomised): 26 Sex: 11 women, 15 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: faculty members of the Department of Radiology at Mayo Clinic (physicians or scientists) Inclusion criteria: 1) staff members (physicians or scientists) within the Department of Radiology; 2) able and willing to participate in all aspects of the study; 3) able to understand and sign the informed consent Exclusion criteria: 1) a psychotic episode within the previous 6 months; 2) clinically significant, acute, unstable neurological, psychiatric, hepatic, renal, cardiovascular, or respiratory disease that would prevent participation in the study Attrition (withdrawals and exclusions): 4 (IG = 2/13 (15.4%), CG = 2/13 (15.4%)) completed the baseline questionnaires but did not complete the 12‐week questionnaires Reasons for missing data: scheduling issue |
|
| Interventions |
Intervention: SMART (n = 13)
Control: wait‐list control (n = 13) |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Time points measured and reported: 1) pre‐intervention; 2) 3‐month follow‐up (3 months after single‐session intervention, at week 12) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: enrolment for the study ran from April 2010 to May 2011; end date not specified Funding source: supported by a Mayo Clinic Department of Radiology Small Grant No.94147001 and gift from Terrance D. and Judith A. Paul Declaration of interest: not specified Ethical approval needed/obtained for study: study protocol was reviewed and approved by the IRB Comments by authors: study methods overlap with those described in previously published studies Miscellaneous outcomes by the review authors: not relevant Correspondence: Varun Sharma, MD, Division of General Internal Medicine, Mayo Clinic, 200 First Street SW, Rochester, MN 55905; vdsharma.md@gmail.com |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "After obtaining informed consent, participants were assigned to one of two groups: an active arm or a wait‐list control arm using a simple randomization schedule generated by the Department of Biomedical Statistics and Informatics." Quote: "Mean scores at baseline differed significantly between groups (two‐sample t test, P = 0.021)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’ (only "randomization schedule", exact method not described); RCT, but not verified baseline comparability of groups for outcome quality of life; baseline comparability for sociodemographic variables and other outcomes of interest unclear |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The allocation sequence was available only to the study coordinator and concealed from the researchers involved in recruitment." Judgement comment: investigators enrolling participants could not foresee assignment; unclear if allocation was also concealed from participants; exact method not described |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "single‐blind trial" Judgement comment: blinding of study personnel not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding; blinding of participants probably ensured (single‐blind trial) |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Quote: "Subjects were de‐identified and assigned a coded study identification number. This code was maintained by the statistician and unavailable to study investigators ensuring blinding of the investigators to the outcome measures." Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of 'Low risk' or 'High risk' (unclear who provided the questionnaires to the participants, e.g. blinded investigators?) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Flow diagram of the progress in a randomized clinical trial to assess the effect of SMART program among radiologists." Quote: "Two subjects from each arm completed the baseline questionnaires but did not complete the 12‐week questionnaires" Quote: "For the four subjects (two SMART and two Control) who did not complete the week 12 assessments, the baseline values were carried forward to week 12 to provide the most conservative estimate of efficacy." Judgement comment: reasons for missing data unlikely to be related to true outcome with balance in missing data between groups (IG: n = 2, CG: n = 2); baseline‐observation‐carried‐forward (BOCF) for missing outcome data; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available, but it is clear that the published report includes all expected outcomes, including those that were prespecified |
Stetz 2007.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified for final report Imputation of missing data: not specified |
|
| Participants |
Country: USA Setting: volunteers attending medical class at Fort Rucker, Alabama; Fort Drum, New York; or Fort Benning, Georgia (i.e. army); training in research laboratory Age: see Population description; 35 (60%) under the age of 30 years old Sample size (randomised): 63 Sex: 16 women, 47 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline screening: none of the participants showed high rates of PTSD at baseline; 3 main PTSD symptoms reported as “moderately” or “quite a bit” (p. 243): “Repeated, disturbing dreams of a stressful military experience” (26%); “Repeated, disturbing memories, thoughts, or images of a stressful military experience?” (25%); “Feeling as if your future will somehow be cut short.”; about 10% to 20% of participants reported similar levels of stress across the remaining items Population description: volunteers who were attending a combat medical class (military medical personnel) Inclusion criteria: 1) only volunteers who showed normal oral temperature (e.g. temperature between 98.2 and 98.6 ºF, see Shoemaker 1996); 2) only volunteers showing low stress symptoms on the PTSD Checklist– Military version (PCL‐M scores less than 4 and 5 on each item) Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention 1: Virtual Reality‐Stress Inoculation Training (VR‐SIT) (n = 18)
Intervention 2: Coping training (CT) (n = 18)
Intervention 3: combination of VR‐SIT and CT (n = 18)
Control: no intervention (n = 9) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: presence (PQ) after each VR session; MAACL‐R before and after each session; salivary amylase test before and after each exposure; PhysioLab monitoring throughout the session; time points reported: no single time points reported, only results from MANOVA Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the randomisation process and received the information that a list was generated and a number to randomly select was computed with SPSS (Stetz 2018 [pers comm]). We contacted the authors again to ask for the level of attrition in each group and the means and SDs for the outcome measures at each time point, but they had not responded to this inquiry at the time of writing Study start/end date: January to June 2007 Funding source: funded through the Army Medical Department Advanced Medical Technology Initiative, Telemedicine and Advanced Technology Research Center, US Army Medical Research and Materiel Command, Fort Detrick, Maryland Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: Stetz 2007 and Stetz 2008 are 2 reports on the same study; Stetz 2007 reports preliminary data on n = 25 medics Correspondence: MAJ Melba Stetz, PhD, Research Director, Psychology Department, Tripler Army Medical Center, Hawaii; Melba.Stetz@us.army.mil; , Tel: +1/ 808‐433‐1651 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Since we depended on students’ availability to participate in our study, we were only able to pseudo‐randomly assign them to either the control or one of the experimental groups, as defined below." Judgement comment: additional information from author about randomisation: "Yes, we made a list and computed a number w [with]/SPSS to randomly select."; insufficient information about random sequence generation to permit judgement of ‘Low risk’ or ‘High risk’ (according to publication Stetz 2008 only pseudo‐randomisation based on availability; according to information from author: SPSS‐generated random numbers); no information about comparability of groups at baseline or respective analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ (according to the Stetz 2008 publication only, pseudo‐randomisation based on availability, which would mean high risk of bias) |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: blinding of participants unclear; blinding of study personnel for Virtual Reality training sessions unclear; blinding of personnel for coping training probably not done (staff ask participants to use relaxation techniques while participants are sitting in a chamber), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants unclear; blinding of study personnel for Virtual Reality training sessions unclear; blinding of personnel for coping training probably not done (staff ask participants to use relaxation techniques while participants are sitting in a chamber); outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: insufficient information about blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (e.g. number and reasons of potential missing data in 4 groups not stated; unclear how many participants were analysed) |
| Selective reporting (reporting bias) | High risk | Judgement comment: no study protocol available; not all of the study’s prespecified outcomes have been reported (compare Stetz 2007 on preliminary results of sample to date: physiological outcomes and presence are prespecified and partly reported; Stetz 2008 on final results with 63 participants: no physiological outcomes are prespecified or reported; Stetz 2008: depression and positive affect subscale are not reported) |
Strijk 2011.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): sample size calculation based on differences between the IG and CG in changes in mean vitality score, measured by the UWES. Based on a study among 10,000 Dutch and Belgian employees, the baseline mean vitality score (range = 0 ‐ 6) was assumed to be 3.99 (SD = 1.11). For the sample size needed, a difference in the vitality mean score of 10% between the IG and CG after 6 months was considered relevant. This means an average difference in the vitality mean score of 0.4 (SD = 1.2) between both study groups. Assuming α = 0.05, power = 0.90, and 2‐sided tests, 189 participants per group were needed. Taking into account a loss of follow‐up of 15%, a sample size of 446 employees (223 employees in each group) needed to be included Imputation of missing data: complete‐case analysis with complete cases (Strijk 2013 (second reference to Strijk 2011)): 500 workers who completed questionnaire at baseline and at 12 months; Strijk 2012 (second reference to Strijk 2011): 575 workers who completed questionnaire at baseline and at 6 months); multiple imputation based on multivariate imputation by chained equations for intention‐to‐treat analysis (sensitivity analysis) |
|
| Participants |
Country: The Netherlands Setting: academic hospitals Age: mean = 52.4 (SD = 4.85) years Sample size (randomised): 730 Sex: 551 women, 179 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: mental health (36‐Item Short Form Survey Instrument): IG = 75.2 (14.8), CG = 77.6 (13.4) (score > 76.8 considered as good) Population description: all workers aged ≥ 45 years from 2 academic hospitals Inclusion criteria: workers were eligible if 1) aged ≥ 45 years; 2) worked ≥ 16 hours a week; 3) gave written informed consent; 4) had no risk of developing adverse health effects when becoming physically active (as assessed by the Physical Activity Readiness Questionnaire) Exclusion criteria: not specified Attrition (withdrawals and exclusions): post‐intervention (at 6 months) = 155 lost to follow‐up (IG = 74/367 (20.2%); CG = 81/363 (22.3%)); 6‐month follow‐up = 230 lost to follow‐up (IG = 117/367 (31.9%); CG = 113/363 (31.1%)) Reasons for missing data: post‐intervention: no time (n = 25), no interest/motivation (n = 10), health problems (n = 9), change of job (n = 5), other (n = 13), unknown reasons (n = 93); 6‐month follow‐up (12 months after baseline): no time (n = 34), no interest/motivation (n = 17), health problems (n = 13), change of job (n = 6), other (n = 52), unknown (n = 108) |
|
| Interventions |
Intervention: written information + Vital@Work intervention (Worksite lifestyle intervention (Vitality exercise programme, VEP)) (n = 367)
Control: active control (written information) (n = 363)
|
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Other outcome
Time points measured: 1) pre‐intervention; 2) post‐intervention (after 6‐month intervention/6 months after baseline); 3) 6‐month follow‐up (6 months post‐intervention/12 months after baseline) (only for outcomes reported in Strijk 2013 (second reference to Strijk 2011): general and work‐related vitality, work engagement, productivity, sick leave) Adverse events: participants reported no adverse events of intervention |
|
| Notes |
Contact with authors: We contacted the authors for the number of participants lost to follow‐up at 12 months in both groups (due to different numbers in the flow chart) (Van der Beek 2018 [pers comm]). Study start/end date: April 2009 to October 2010 at 2 locations Funding source: Vital@Work study financially supported by the ‘Foundation Institute GAK’ Declaration of interest: no competing interests to declare Ethical approval needed/obtained for study: approved by the Medical Ethics Committee of the VU University Center Amsterdam (VUmc) and of the Leiden University Medical Center (LUMC) Comments by authors: registered at the Dutch Trial Register under trial registration number: NTR1240 (http://www.trialregister.nl/trialreg/ admin/rctview.asp?TC=1240) Miscellaneous outcomes by the review authors: not relevant Correspondence: Jorien E. Strijk (je.strijk@vumc.nl); corresponding author: Prof. Allard J van der Beek; Department of Public and Occupational Health, EMGO+ Institute for Health and Care Research, VU University Medical Center; Body@Work, Research Center Physical Activity, Work and Health, TNO‐VUmc, Van der Boechorststraat 7, 1081 BT Amsterdam, The Netherlands; a.vanderbeek@vumc.nl |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The workers who consented to participate were, after baseline measurements, individually randomized to the intervention or control group using Random Allocation Software (version 1.0, May 2004, Isfahan University of Medical Sciences, Iran)." Quote: "...baseline characteristics of the study population are presented with no significant differences between the groups in any of these variables." Judgement comment: The investigators describe a random component in the sequence‐generation process (randomisation software) and there is verified baseline comparability between groups for sociodemographic characteristics; baseline comparability for outcome variables are unclear |
| Allocation concealment (selection bias) | Low risk | Quote: see study protocol: "Randomisation will be executed, after completing baseline measurements, by an independent researcher (i.e. research assistant) using Random Allocation Software (...)" Judgement comment: participants and investigators enrolling participants could probably not foresee assignment (random‐sequence generation by independent researcher after baseline assessments, i.e. after participant enrolment was completed) |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Quote: "Blinding of participants or intervention providers was impossible." Quote: "The research assistant notified each worker to which group he or she had been allocated" Judgement comment: no blinding of participants and personnel (face‐to‐face intervention), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "Blinding of participants or intervention providers was impossible." Quote: "The research assistant notified each worker to which group he or she had been allocated" Judgement comment: no blinding of participants and personnel (face‐to‐face intervention), and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Quote: "The research assistant notified each worker to which group he or she had been allocated and did not reveal the group allocation to the investigator responsible for data analyses." Judgement comment: insufficient information about blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Quote: "The research assistant notified each worker to which group he or she had been allocated and did not reveal the group allocation to the investigator responsible for data analyses." Judgement comment: insufficient information about blinding of outcome assessment (blinding of data analysis but unclear who distributed the questionnaires to the participants); however, due to performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "As presented in the study flow diagram (figure 1), a total of 730 workers completed the baseline questionnaire and were randomized to the intervention (N=367) or control group (N=363)." Quote: "In total, 500 workers completed the questionnaire 12 months after baseline and were, therefore, used for complete cases analyses. In addition, sensitivity analyses with imputed data among the total study population (N=730) were performed." Quote: "All analyses were performed according to the intention‐to‐treat principle. As possible effects of missing participants should be considered, it is recommended to perform both complete cases and sensitivity analyses with imputed data (41). For the sensitivity analyses, all missing data on the outcome measure were imputed using multiple imputations (MI) based on multivariate imputation by chained equations (42, 43). The MI procedure was performed in PASW (version 18.0, SPSS Inc, Chicago, IL, USA), in which 40 different data sets were generated." Quote: "Effects were analysed according to the intention‐to‐treat principle with complete cases (n=575) and imputed data (n=730) using linear regression analyses." Judgement comment: reasons for missing data likely to be related to true outcome with imbalance in missing data between groups (Lost to follow‐up 6 months: IG: 74, CG: 81, compare unknown reasons: IG: 35, CG: 58, compare no interest/motivation: IG: 6, CG: 4; 12 months: IG: 117, CG: 113, compare unknown reasons: IG: 46, CG: 62, compare no interest/motivation: IG: 11, CG: 6); complete‐case analysis with complete cases (Strijk 2013: 500 workers who completed questionnaire at baseline and at 12 months; Strijk 2012: 575 workers who completed questionnaire at baseline and at 6 months) and multiple imputation for intent‐to‐treat analysis (physical activity using accelerometers and VO2max in subsample) |
| Selective reporting (reporting bias) | High risk | Judgement comment: trial registration (NTR1240) and study protocol (Strijk 2009) available; not all of the prespecified outcomes have been reported; not all reported outcomes were prespecified; PRE‐SPECIFIED (in trial registration and study protocol): Primary: Vitality and lifestyle behaviour (Physical activity, dietary behaviour, alcohol consumption, smoking habits); Secondary: work engagement and productivity, general health status (also RAND‐36), quality of life, sick leave and cost effectiveness; in addition in study protocol: BMI, waist circumference combined with 2‐km UKK walking test; REPORTED: Primary: vitality (UWES), vitality (RAND‐36); Secondary: work engagement, productivity, sick leave; reported, but not specified if primary or secondary outcome: physical activity (SQUASH, accelerometers), aerobic fitness (2‐km UKK walking test for VO2max), dietary behaviour (fruit intake), mental health, need for recovery from work |
Tierney 1997.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): power not specified but, according to authors, small sample size to achieve statistical significance Imputation of missing data: not specified |
|
| Participants |
Country: USA Setting: suburban community hospital Age: see Population description; age not specified Sample size (randomised): 62 Sex: not specified (unclear if male nurses also included) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: staff nurses employed between 6 months and 2½ years at community hospital Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention 1: hardiness class (n = 21)
Intervention 2: time management class (n = 19)
Control: no intervention (n = 22) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 6‐month follow‐up (6 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: time management group is no‐attention control but second intervention group (see results: only no‐intervention group is indicated as CG) Correspondence: Mary Jo Tierney, Nurse Practitioner, San Mateo County, San Mateo, California |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Subjects were assigned randomly to one of three groups." Quote: "To determine whether there was a significant difference among the three groups at baseline, an analysis of variance was performed for the hardiness scores and subscales of all three groups at baseline. Table 1 shows that no significant difference existed among the three groups." Judgement comment: insufficient information about random sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for outcomes of interest on the basis of analysis; baseline comparability for sociodemographic characteristics is unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (e.g. unclear if there were any missing data in the 3 groups and if missing data were imputed) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Varker 2012.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; available‐case analysis (only participants who took part in video session and for whom outcomes were obtained) |
|
| Participants |
Country: Australia Setting: general community; not specified where training took place Age: mean = 28.4 (SD = 10.4, range = 18 ‐ 63) years Sample size (randomised): 82 Sex: 45 women, 35 men (in analysed sample of 80) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: post‐traumatic stress symptoms, depression, anxiety and stress at pre‐intervention (not specified) Population description: individuals from general population Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): Originally there were 82 participants who attended the first session; however, 2 participants failed to attend the second session (video and post‐intervention assessment) and were therefore excluded (group not specified); 1 participant was excluded from DASS‐21 analysis (not specified which group); 2 participants excluded from memory analysis (IG = 1, CG = 1) Reasons for missing data: not specified (n = 2), exclusion for DASS‐21 analysis as outlier (n = 1); exclusions for memory analysis as failed to complete memory components at post‐intervention and follow‐up (n = 2) |
|
| Interventions |
Intervention: inoculation resilience training (n = not specified)
Control: attention control (non‐intervention 'pragmatic' training group) (n = not specified)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured: 1) pre‐intervention; 2) post‐intervention (after training in week 1 and stressor exposure in week 2); 3) 1‐month follow‐up (1‐month post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the number of participants randomised to each group (before n = 3 exclusions), but they had not responded at the time of writing. Study start/end date: not specified Funding source: not specified Declaration of interest: All authors declare no conflict of interests in the preparation of this report. Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: not relevant Correspondence: Tracey Varker, Australian Centre for Posttraumatic Mental Health, University of Melbourne, Australia; Corresponding author: Grant J. Devilly, Griffith Health Institute School of Applied Psychology, Griffith University, Mt Gravatt Campus, Messines Ridge Road, Mt Gravatt, Qld 4122, Australia; grant@devilly.org; Tel.: +61 7 37353309; fax: +61 7 37353436 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Eighty individuals (35 male, 45 female) aged between 18 and 63 years (M age = 28.4, SD age = 10.4), were recruited from the general population through advertisements, and were randomly allocated (Devilly, 2007) to one of two conditions: inoculation or control" Quote: "There were no significant differences between the two groups in the distribution of age, gender, previous exposure to similar styles of video, history of trauma, prior consultation for emotional problems, blood phobia, anticipatory anxiety regarding what they were about to be shown, and group allocation sizes. Measures completed at Time 2 following the presentation of the video revealed no significant differences between each of the groups in the extent to which participants physically or mentally distracted themselves while viewing the video, the seriousness with which they rated the accident, nor levels of participant empathy with either the accident victims or the emergency workers. Overall, these results suggest that no significant differences existed within the group compositions (Inoculation vs Pragmatic Training Control) before the experimental phase." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic variables; baseline comparability for outcome variables unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Quote: "All data was collected by pencil‐and‐paper tests within a booklet that the ‘therapist’ did not see and, hence, the ‘therapist’ was blind to responses." Judgement comment: insufficient information about blinding of outcome assessment (therapists were blind to responses but unclear if therapists were also the outcome assessors who distributed the questionnaires); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Eighty individuals (35 male, 45 female) aged between 18 and 63 years (M age = 28.4, SD age = 10.4), were recruited from the general population through advertisements, and were randomly allocated (Devilly, 2007)" Quote: "Originally there were 82 participants who attended the first session, however 2 participants failed to attend the second session and were, therefore, excluded. As such, the attrition rate was very low at just 2.4%." Quote: "With respect to negative affect, descriptive statistics of the DASS21 showed one case to be an outlier, as indicated by a z score over 3.29 (p < .001; Tabachnik & Fidell, 2001), therefore this person was dropped from the DASS21 analysis." Quote: "The memory analysis was conducted for 78 participants, as 2 participants failed to complete the memory components of the post‐video and follow‐up questionnaires (1 control participant and 1 inoculation participant)." Judgement comment: n = 2 excluded (not specified which group and no reasons reported); 1 excluded in DASS‐21 analysis (outlier; not specified which group); 2 missings (IG: 1, CG: 1) in memory (failed to complete memory components of assessment); available‐case analysis (only participants who took part in video session and for whom outcomes were obtained) |
| Selective reporting (reporting bias) | High risk | Judgement comment: no study protocol available, but not all of the study’s prespecified outcomes have been reported (perceived social support) |
Villani 2013.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): power not specified; small sample size Imputation of missing data: not applicable since no dropouts or exclusions |
|
| Participants |
Country: Italy Setting: oncology hospitals Age: mean = 43 (SD = 8.80) years Sample size (randomised): 30 Sex: 30 women (oncology nurses) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: all participants with cut‐off of stress corresponding to higher quartile (Italien normative data) measured by Mesure du Stress Psycholyque (MSP); received from authors (Villani 2018 [pers comm]): state anxiety (STAI): IG = 43.64 (8.03), CG = 44.00 (9.91) Population description: female oncology nurses with permanent status employed in 6 oncology hospitals in Milan, Italy Inclusion criteria: 1) being a current oncology nurse with a minimum of 5 years of experience in the oncology ward; 2) having a permanent status, to avoid sources of stress related to temporary employment; 3) having a cut‐off level of stress corresponding to the higher quartile (Italian normative data), measured using the MSP Questionnaire Exclusion criteria: not specified Attrition (withdrawals and exclusions): information received from authors (Villani 2018 [pers comm]): no dropouts or exclusions during the study (only 8 participants excluded before randomisation because they did not meet the inclusion criteria) Reasons for missing data: not applicable since no dropouts or exclusions |
|
| Interventions |
Intervention: Mobile Stress Inoculation Training (M‐SIT) (n = 15)
Control: attention control (n = 15)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) end of session 1 (only state anxiety); 3) end of session 2 (only state anxiety); 4) end of session 3 (only state anxiety); 5) end of session 4 (only state anxiety); 6) end of session 5 (only state anxiety); 7) end of session 6 (only state anxiety); 8) post‐intervention (after all 8 training sessions) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the means and SDs for all outcomes at pre‐ and post‐intervention (after 8 sessions), the number of dropouts and the number of participants analysed in each group (Villani 2018 [pers comm]). Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: information on attrition and values on state anxiety received from authors (Villani 2018 [pers comm]) Correspondence: Daniela Villani, PhD, Department of Psychology, Catholic University of Sacred Heart, Milan, Italy; daniela.villani@unicatt.it |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were randomly allocated into two groups (15 participants for each condition)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; no information about comparability of groups at baseline or respective analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | Unclear risk | Judgement comment: self‐help intervention via mobile phones; insufficient information about blinding of participants and personnel to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: information received from authors: no dropout from 30 participants |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified (job content and perceived stress only assessed at pre‐intervention and no outcomes) |
West 2014.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): Of the 37 participants in each arm of the study, 34 (91.9%) provided survey responses. With this sample size, power was 80% to detect a moderate Cohen f2 effect size of 0.15; no sample size calculation reported Imputation of missing data: no imputation of missing data (information received from authors; West 2017 [pers comm]); per‐protocol analysis (with participants who took part in allocated intervention, i.e. without 2 participants in IG who withdrew consent) and available‐case analysis (with participants for whom outcomes were obtained) |
|
| Participants |
Country: USA Setting: Department of Medicine at the Mayo Clinic Rochester Age: see Population description; age not specified Sample size (randomised): 74 Sex: 25 women, 49 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: IG had slightly higher rates of high emotional exhaustion and overall burnout (MBI); burnout, n (%): full high depersonalisation: IG = 9 (24.3%), CG = 9 (25.7%); full high emotional exhaustion: IG = 17 (45.9%), CG = 12 (34.3%); full overall burnout: IG = 20 (54.1%), CG = 15 (42.9%); depression, n (%): positive depression screen (2‐question approach): IG = 11 (29.7%), CG = 11 (31.4%) Population description: practising physicians in the Mayo Clinic Department of Medicine Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): 2/37 (5.4%) in IG withdrew consent and therefore could not be analysed; number who did not complete assessments (information received from authors; West 2017 [pers comm]): pre‐intervention: n = 7; 3‐month follow‐up: 5 ‐ 6 for different outcomes; 12‐month follow‐up: 8) Reasons for missing data: not specified |
|
| Interventions |
Intervention: small‐group curriculum (n = 37)
Control: no intervention; could schedule and use this hour of protected time in any manner they believed was most useful but did not participate in the formal curriculum (n = 37) |
|
| Outcomes |
Outcomes collected and reported:
Outcomes reported:
Time points measured and reported: 1) pre‐intervention; 2) during intervention at 3 months (during 9‐month intervention); 3) during intervention at 6 months (during 9‐month intervention); 4) post‐intervention (at 9 months, i.e. end of 9‐month intervention); 5) 3‐month follow‐up (3 months post‐intervention); 6) 12‐month follow‐up (12 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to ask for the means and SDs for the outcomes at all time points and the procedures in dealing with missing data (West 2017 [pers comm]). Study start/end date: study conducted between September 2010 and June 2012 Funding source: supported by the Mayo Clinic Program on Professionalism and Ethics and the Department of Medicine at Mayo Clinic Rochester; funding source had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication Declaration of interest: no conflicts of interest reported Ethical approval needed/obtained for study: approved by the Mayo Clinic IRB Comments by authors: trial registration: clinicaltrials.gov Identifier: NCT0115997 Miscellaneous outcomes by the review authors: not relevant Correspondence: Colin P. West, MD, PhD, Division of General Internal Medicine, Department of Medicine, Mayo Clinic, 200 First St, Rochester, MN 55905; west.colin@mayo.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized in a concealed fashion into 2 groups via a computer‐generated algorithm. Randomization was stratified by sex and specialty (general internal medicine or other internal medicine specialty) using permuted blocks." Quote: "Baseline characteristics of the 2 trial groups were generally similar, with no statistically significant differences observed, although the intervention arm had slightly higher rates of high emotional exhaustion and overall burnout." Quote: "Because of baseline differences across groups for several variables, all analyses were adjusted for levels of distress at study onset." Judgement comment: The investigators describe a random component in the sequence‐generation process (computer‐generated algorithm) and there is verified baseline comparability of groups for sociodemographic characteristics and outcomes of interest on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Participants were randomized in a concealed fashion into 2 groups via a computer‐generated algorithm." Judgement comment: insufficient information to permit judgement of ‘Low risk’ or ‘High risk’; exact method of concealment not specified; unclear if random‐sequence generation was concealed from personnel and/or participants |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: Insufficient information about blinding of outcome assessment (online questionnaires); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Of the 37 participants in each arm of the study, 34 (91.9%) provided survey responses." Quote: "The changes in each well‐being metric from study baseline to study end, as well as at 3 and 12 months following the study, were analyzed according to the intent‐to‐treat principle using generalized estimating equations to account for the repeated‐measures design." Judgement comment: reasons for missing data unlikely to be related to true outcome with relative balance in missing data between groups (IG: 2 withdrawals, CG: 0; no reasons reported); no imputation of missing data (information received from authors); per‐protocol analysis (with participants who took part in allocated intervention, i.e. without 2 participants in IG who withdrew consent) and available‐case analysis (with participants for whom outcomes were obtained) |
| Selective reporting (reporting bias) | High risk | Judgement comment: trial registration available (clinicaltrials.gov/ct2/show/NCT01159977); several reported outcomes were not prespecified; PRESPECIFIED in trial registration: job satisfaction, burnout; AND: not all of the prespecified outcomes (prespecified in the publication) were reported; PRESPECIFIED in publication: job satisfaction, perceived stress, quality of life, empowerment and engagement at work, burnout, mental and physical well‐being, fatigue, empathy; REPORTED: all outcomes except for mental and physical well‐being, fatigue and empathy |
West 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified in conference abstract Imputation of missing data: not specified |
|
| Participants |
Country: USA Setting: academic internal medicine physicians; setting where intervention took place not specified Age: see Population description; age not specified Sample size (randomised): 125 Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: academic internal medicine physicians Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: COMPASS groups (COlleagues Meeting to Promote And Sustain Satisfaction) (n = 64)
Control: wait‐list control (n = 61) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: pre‐intervention and then quarterly assessments: 1) pre‐intervention; 2) during intervention (after 3 months); 3) post‐intervention (after 6‐month intervention); follow‐up assessments not specified; time pointsreported: absolute change in outcomes from baseline to 6 months Adverse events: not specified in conference abstract |
|
| Notes |
Contact with authors: We contacted the authors to see if the study was published in the meantime (West 2018 [pers comm]). We also asked for the (unpublished) summary data (West 2019 [pers comm]). Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: conference abstract; presented at 38th Annual Meeting of the Society of General Internal Medicine, Toronto, Canada, 2015; information received from authors (West 2019 [pers comm]): paper is currently being written, and has not yet been published; data for overall quality of life and burnout (emotional exhaustion, depersonalisation) sent by the authors (West 2019 [pers comm]) Correspondence: Colin P. West, Mayo Clinic, Rochester, Minnesota; West.Colin@mayo.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We conducted a randomized controlled trial of a 6‐month intervention involving 12 biweekly one‐hour meetings of self‐formed groups of 6–8 academic internal medicine physicians, termed COMPASS Groups (COlleagues Meeting to Promote And Sustain Satisfaction)." Quote: "At baseline, no statistically significant differences were observed between the study groups for any well‐being variable." Judgement comment: based on conference abstract, insufficient information about random‐sequence generation to permit judgement of 'Low risk' or 'High risk'; RCT and verified baseline comparability for well‐being (i.e. outcome) variables; baseline comparability for sociodemographic characteristics unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: based on conference abstract, insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk' |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: based on conference abstract, blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: based on conference abstract, insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Judgement comment: information received from authors: reasons for missing data likely to be related to true outcome with imbalance in missing data between groups (IG: 13, CG: 5); available‐case analysis |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available; based on conference abstract, all of the study’s prespecified outcomes that are of interest in the review have been reported in the prespecified way |
Wild 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
|
| Participants |
Country: UK Setting: emergency workers (police, fire and rescue, ambulance, search and rescue); setting not specified Age: mean = 41.41 (SD = 9.78) years Sample size (randomised): 430 Sex: 250 women, 180 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: previous traumas (trauma screener, range = 0 ‐ 21): IG = 4.498 (3.45), CG = 4.76 (3.28); (PTSD) (PCL‐5; range = 0 ‐ 84): IG = 8.965 (12.37), CG = 9.42 (13.75); AUDIT; (range = 0 ‐ 40): IG = 5.23 (4.08), CG = 5.19 (4.25); depression (PHQ‐9): IG = 3.89 (4.07), CG = 3.83 (3.85) Population description: employed or volunteering as front‐line or office‐based staff in 1 of the following emergency services: police, fire and rescue, ambulance, and search and rescue Inclusion criteria: being employed or volunteering as front‐line or office‐based staff in 1 of the following emergency services: police, fire and rescue, ambulance, and search and rescue Exclusion criteria: Participants who scored in the clinical range on measures of PTSD or depression, or those who expressed suicidal ideation, had a one‐to‐one discussion with the study’s psychologist. They were included in the study if they did not evidence risk, their symptoms were not interfering with their daily functioning and they did not wish to access treatment. Attrition (withdrawals and exclusions): post‐intervention: 82 did not complete post‐intervention assessment (IG = 61/317 (19.2%), CG = 21/113 (18.6%)); 3‐month follow‐up: 48 did not complete follow‐up assessment (IG = 35/317 (11%), CG = 13/113 (11.5%)) Reasons for missing data: not specified |
|
| Interventions |
Intervention: Mind’s resilience intervention (n = 317)
Control: active control: online control intervention (n = 113)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 3‐month follow‐up (3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to ask for the subgroup (summary outcome data) for ambulance personnel and the number of participants analysed, but they had not responded at the time of writing. Study start/end date: total study duration: May 2015 to March 2016 (see trial registry); March to November 2015: work with Local Minds to invite participants to take part in the study Funding source: sponsor: University of Oxford (UK), University Offices; funding: Mind, the mental health charity (UK) (see trial registration) Declaration of interest: not specified Ethical approval needed/obtained for study: ethical approval by Medical Sciences Division Research Ethics Committee at the University of Oxford Miscellaneous outcomes by the review authors: trial registration: ISRCTN79407277 Correspondence: Dr Jennifer Wild, Department of Experimental Psychology, University of Oxford, South Parks Road, Oxford, OX1 3UD, United Kingdom; jennifer.wild@psy.ox.ac.uk; Telephone: +44 (0)1865 618 612 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Our evaluation is a randomized controlled trial in which participants (N=430) were randomly allocated in a 3:1 ratio to receive Mind’s resilience intervention (N=317) or a control online intervention (N=113)." Quote: "All N=430 participants were randomized in a 3:1 ratio to receive the resilience intervention or the control intervention in four phases across nine sites in England. Random allocation was stratified by site and gender." Quote: "There were no significant differences on any of the demographic (age, previous trauma, number of years of education, service, marital status, gender, qualifications, ethnicity) and baseline measures between participants receiving the group or online conditions." No obvious differences in outcome variables between resilience and control groups at baseline to suggest unbalanced groups (compare repeated measures ANOVAs with three levels (baseline, post‐intervention and follow‐up) for resilience, well‐being, self‐efficacy, ability to problem solve and reach goals, nine coping behaviours in response to stress (e.g. active coping), rumination, maladaptive responses to intrusive memories (e.g. suppression), levels of social participation, feeling supported at home and work, severe stress (PTSD), depression, anxiety, alcohol use, and the number of days off per week. Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; RCT and verified baseline comparability of groups for sociodemographic variables and most outcome measures; baseline comparability in 'confidence in managing mental health' unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (online questionnaires/secure digital programme); however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Judgement comment: reasons for missing data likely to be related to true outcome with imbalance in missing data (post‐intervention IG: 61; CG: 21; 3‐month follow‐up: IG: 35; CG: 13); fewer participants in IG received the allocated intervention compared to CG (IG: 279/317, 88% vs CG: 105/113, 92.9%); reasons for missing data not provided for each group; unclear how many participants were analysed |
| Selective reporting (reporting bias) | Low risk | Judgement comment: trial registration available (ISRCTN79407277); all of the study’s prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way |
α: alpha (significance level); ACG: Authentic Connections Group; ACT: Acceptance and Commitment Therapy; AIT: Attention and Interpretation Therapy; AMS: Auxilliary Medical Service; ANCOVA: analysis of covariance; ANOVA: analysis of variance; β: beta (statistical power); AT: autogenic training; AUDIT: Alcohol Use Disorder Identification Scale; BDI: Beck Depression Inventory; BP: blood pressure; BRCS: Brief Resilience Coping Scale; Brief COPE: Coping Orientation to Problems Experience; BSI: Brief Symptom Index; CB: controlled breathing; CBI: Copenhagen Burnout Inventory; CBT: cognitive behavioural therapy; CD: compact disc; CD‐RISC: Connor‐Davidson Resilience Scale; CERQ: Cognitive Emotional Regulation Questionnaire; CES‐D: Centers for Epidemiology Studies ‐ Depression Scale; DVD: digital versatile disc; CG: control group; CMS: Coping Mechanism Scale; COPSOQ: Copenhagen Psychosocial Questionnaire; CP: civilian population; CPQ: Copenhagen Psychosocial Questionnaire; d: delta (Cohen's d, effect size); DASS: Depression Anxiety Stress Scale; DBP: diastolic blood pressure; ED: Emergency Department; EDDS: Eating Disorder Diagnostic Scale; e.g.: for example; EMA: Ecological Momentary Assessment; ERS: Effort‐Reward Scale; ERSQ‐27: Emotional Regulation Skills Questionnaire; EWS: Empowerment at Work Scale; f or f2: Cohen's f or f2 (effect size); FFMQ: Five‐facet mindfulness Questionnaire; fMRI: functional Magnetic Resonance Imaging; GAD‐7: Generalised Anxiety Disorder, 7‐item scale; GHQ: General Hospital Questionnaire; ICC: inter‐class correlation coefficient; IES‐R: Impact of Event Scale ‐ Revised; ICU: intensive care unit; IG: intervention group; IRB: Institutional Review Board; ISEL: Interpersonal Support Evaluation List; ISI: Insomnia Severity Index; MAAS: Mindful Attention and Awareness Scale; MAACL‐R: Multiple Affect Adjective Checklist ‐ Revised; MANOVA: multivariate analysis of variance; MASL: Maslach Burnout Inventory; MBCT: Mindfulness‐based Cognitive Therapy; MBI: Maslach Burnout Inventory; MBI: mindfulness‐based intervention; MBI‐GS: MBI‐General Survey; MBI‐HSS: Maslach Burnout Inventory ‐ Human Services Survey; MBRT: Mindfulness‐based Resilience Training; MBSR: Mindfulness‐based Stress Reduction; MHCP: Mental Health Care Providers; MSICU: Medical‐Surgical Intensive Care Unit; n: sample size (e.g. in respective study group); n2: eta2 (effect size); NICU: neonatal intensive care unit; NIH‐EXAMINER: National Institutes of Health Executive Abilities; NP: nurse practitioner; NSS: Nursing Stress Scale; OLBI: Oldenburg Burnout Inventory; PA: physician assistant; PAA: Personal Assertion Analysis; PANAS: Positive and Negative Affect Schedule; PCL: PTSD Checklist; PCT: Psychosocial Competency Training; PFA: Psychological First Aid; PHQ: Patient Health Questionnaire; PJSS: Physician Job Satisfaction Scale; PMR: progressive muscle relaxation; PQ: Presence Questionnaire; PRIME‐MD: Primary Care Evaluation of Mental Disorders; ProQoL: Professional Quality of Life; PSI: Parenting Stress Inventory; PSI: Physical Symtom Inventory; PSQ: Perceived Stress Questionnaire; PSQI: Pittsburgh Sleep Quality Index; PSS: Perceived Stress Scale; PSS‐SR: PTSD Symptom Scale ‐ Self‐Report; PTSD: Post‐traumaticc Stress Disorder; PVS: Personal Views Survey; QRI: Quality Relationship Inventory; RCT: randomised controlled trial; RIQ: Responses to Intrusions Questionnaire; RPMG: Relational Psychotherapy Mothers Group; RRS: Ruminative Response Scale; SAQ: Safety Attitudes Questionnaire; SAS: Smith Anxiety Scale; SBP: systolic blood pressure; SD: standard deviation; SICU: Surgical Intensive Care Unit; SMART: Stress Management and Resilience Training; STAI: State Trait Anxiety Inventory; STSS: Secondary Trauma Stress Scale; SWOP‐K9: Self‐efficacy Optimism and Pessimism; TAU: treatment as usual; TNICU: Trauma and Neurosurgery Intenisve Care Unit; UWES: Utrecht Work Engagement Scale; VA: Veterans Affairs; VR‐SIT: Virtual Reality ‐ Stress Inoculation Training; WEMWS: Warwick‐Edinburgh Mental Well‐being Scale; WES: Work Engagement Scale; WFCS: Work‐Family Conflict Scale; WSBMS: Work Stress and Burnout Management Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bian 2011 | Ineligible population (no healthcare professionals) |
| Chang 2008 | Ineligible intervention (no focus of the intervention on fostering resilience/psychological adaptation despite stress, hardiness or post‐traumatic growth; no resilience factors trained) |
| Dyrbye 2016 | Ineligible intervention (no focus of the intervention on fostering resilience/psychological adaptation despite stress, hardiness or post‐traumatic growth; no resilience factors trained) |
| Imamura 2019 | Ineligible intervention (no focus of the intervention on fostering resilience/psychological adaptation despite stress, hardiness or post‐traumatic growth; no resilience factors trained) based on information received from study authors (Kawakami 2019 [pers comm]) |
| Lahn 2014 | Ineligible study design |
| Maunder 2010 | Ineligible study design |
| NCT02417051 | Ineligible population (no healthcare professionals) |
| NCT03753360 | Ineligible intervention (no focus of the intervention on fostering resilience/psychological adaptation despite stress, hardiness or post‐traumatic growth; no resilience factors trained) |
| NCT03914898 | Ineligible intervention (no focus of the intervention on fostering resilience/psychological adaptation despite stress, hardiness or post‐traumatic growth; no resilience factors trained) |
| Rowe 1999 | Ineligible intervention (no focus of the intervention on fostering resilience/psychological adaptation despite stress, hardiness or post‐traumatic growth; no resilience factors trained) |
| Speckens 2019 | Ineligible intervention (no focus of the intervention on fostering resilience/psychological adaptation despite stress, hardiness or post‐traumatic growth; no resilience factors trained) |
| Strauss 2018 | Ineligible intervention (no focus of the intervention on fostering resilience/psychological adaptation despite stress, hardiness or post‐traumatic growth; no resilience factors trained) based on information received from study authors (Strauss 2019 [pers comm]) |
| Watanabe 2019 | Ineligible intervention (no focus of the intervention on fostering resilience/psychological adaptation despite stress, hardiness or post‐traumatic growth; no resilience factors trained) |
Characteristics of studies awaiting classification [ordered by study ID]
Almén 2020.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Aranda Auserón 2018.
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): A sample size of 50 participants was estimated, necessary for have a power of 80% to detect as significant differences between the pre‐ and post‐intervention situation of 0.6 SDs in the scores of the scales considered Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. only participants who completed training/attended at least 75% of sessions) |
| Participants |
Country: Spain Setting: health centre in Pamplona Age: mean = 49.9 (SD = 8.2) years (analysed sample) Sample size (randomised): 48 Sex: 38 women, 7 men (analysed sample) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: no psychiatric illness (see inclusion criteria); burnout in MBI: 1) emotional exhaustion: low (< 19): IG: 9 (41%), CG: 13 (59%); moderate (19 ‐ 26): IG: 3 (14%), CG: 3 (14%); high (> 26): IG: 10 (46%), CG: 6 (27%); 2) depersonalisation: low (< 6): IG: 10 (46%), CG: 11 (50%); moderate (6 ‐ 9): IG: 5 (23%), CG: 5 (23%); high (> 9): IG: 7 (32%), CG: 6 (27%); 3) personal accomplishment: low (> 39): IG: 8 (35%), CG: 9 (41%); moderate (39 ‐ 34): IG: 11 (48%), CG: 10 (45%); high (< 34): IG: 3 (14%), CG: 3 (14%) Population description: primary care health professionals Inclusion criteria: 1) informed consent; 2) committed to complete pre‐ and post‐tet questionnaires; 3) attend at least 75% of sessions and perform mindfulness and self‐compassion practices 45 minutes a day Exclusion criteria: 1) having completed programme of mindfulness or self‐compassion or both in the previous 6 months; 2) suffer from psychiatric illness that did not advise participating in the study Attrition (withdrawals and exclusions): 3 dropouts (IG: 2 (8%), CG: 1 (4%)) Reasons for missing data: for 3 dropouts/losses: IG: 2 lost due to not completing the programme; CG: 1 due to attending a mindfulness course during the study |
| Interventions |
Intervention: Mindfulness and Self‐Compassion Programme (n = 25)
Control: unspecified control group (n = 23)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
| Notes |
Contact with authors: We contacted authors for the potential focus of the intervention on fostering resilience, but received no response Study start/end date: not specified; course held during February ‐ March 2016 Funding source: partially funded by the Department of Health of the Government of Navarra, when obtaining the first prize in the II Research Ideas Competition Health in Primary Care Declaration of interest: The authors declare that there is no conflict of interest. Ethical approval needed/obtained for study: approved by the Ethics Committee of Clinical Research of Navarra Comments by study authors: not relevant Miscellaneous outcomes by the review authors: focus of intervention on resilience unclear (resilience only mentioned once in report) Correspondence: Gloria Aranda Auserón, Subdirección de Farmacia, Servicio Navarro de Salud‐Osasunbidea, Pamplona, Spain; garandaa@navarra.es |
Chesak 2019a.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Dyrbye 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Grabbe 2020.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Heath 2020.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Kim 2018a.
| Methods |
Study design: RCT including head‐to‐head comparison Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): With a predicted effect size of Cohen d = 0.4, an α level of.05, a desired power of 0.95, and a correlation of 0.5 among repeated measures, the estimated total sample size using G‐Power was 69 (23 participants per condition); considering a dropout rate of 20%, we aimed to recruit 87 participants Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. only participants who completed the study) |
| Participants |
Country: Korea Setting: training setting not exactly specified; employees and see method of recruitment, but training setting unclear Age: mean = 40.29 (SD = 10.82) years Sample size (randomised): 81 Sex: 67 women, 5 men (in analysed sample) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: Mini‐International Neuropsychiatric Interview during screening process to detect psychiatric disorders Population description: employees Inclusion criteria: 1) age between 19 and 65 years; 2) a score of ≥ 14 on the PSS at baseline; 3) possession of an Android smartphone; 4) currently employed full‐time Exclusion criteria: 1) age < 19 or > 65 years; 2) cognitive disorders, such as intellectual disability or dementia; 3) neurological disorders, including epilepsy, stroke, or others; 4) history of schizophrenia or bipolar I disorder; 5) current report of suicidal ideation; and 6) nonpharmacological treatment or counselling within the past 6 months Attrition (withdrawals and exclusions): AFTER RANDOMISATION (before treatment initiation): IG1: 4 dropouts; IG2: 1 dropout; DURING TREATMENT: IG1: 3 dropouts; CG: 1 dropout Reasons for missing data: AFTER RANDOMISATION; for 4 dropouts in IG1: trouble installing the app on their smartphone (n = 3); refused participation due to difficulty in scheduling appointments (n = 1); IG2: needed psychiatric treatment due to aggravation of psychiatric symptoms (n = 1); DURING TREATMENT: for 3 dropouts in IG1: personal schedules (n = 2), complained of unstable Wi‐Fi connection (n = 1); CG: dropout due to personal matters, but refused to give a detailed explanation (n = 1) |
| Interventions |
Intervention 1: educational material from self‐care condition (CG) + mobile videoconference‐based intervention on stress reduction and resilience enhancement (n = 25)
Intervention 2: educational material from self‐care condition (CG) + in‐person condition on stress reduction and resilience enhancement (n = 28)
Control: active control (self‐care condition) (n = 28)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 1‐month follow‐up (1 month post‐intervention) Adverse events: not specified |
| Notes |
Contact with authors: We contacted authors to get the information about the potential inclusion of healthcare professionals, but received no response to 2 inquiries. Study start/end date: recruitment between August 2017 and November 2017 Funding source: supported from a fund by the Ministry of Trade, Industry and Energy of South Korea (No. 10069105 to J‐HK) Declaration of interest: none declared Ethical approval needed/obtained for study: approved by the IRB of Seoul National University Bundang Hospital Comments by study authors: trial registration NCT03256682 Miscellaneous outcomes by the review authors: head‐to‐head comparison between mobile videoconference condition and in‐person condition, self‐care condition as control group (i.e. hypothesis that mobile videoconference intervention for stress reduction and resilience enhancement is superior to self‐care); unclear if study also included healthcare professionals Correspondence: Jeong‐Hyun Kim, Hanyang University Medical Center, Seoul, Republic Of Korea; ten.liamnah@3lairter |
Mainwaring 2018.
| Methods |
Study design: not specified in abstract; full text could not be retrieved or obtained from the study authors Study grouping: not specified Unit of allocation/randomisation: not specified Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants |
Country: USA Setting: medium‐size anaesthesia department (serving one of the busiest surgical and obstetric facilities on the east coast) Age: not specified Sample size (randomised): not specified Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: anaesthesia professionals working in a medium‐size anaesthesia department Included criteria: not specified Excluded criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: mindfulness‐based resilience training (n not specified)
Control: potential control group not specified in abstract (n not specified) |
| Outcomes |
Outcomes collected and reported: based on publication abstract 1) mindfulness; 2) resilience; 3) positive outlook and attitude (no statistical data reported) Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; overall changes between pre‐ and post‐intervention reported Adverse events: not specified in abstract |
| Notes |
Contact with authors: We contacted authors twice to ask for the corresponding full text, but did not receive a response Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not specified Miscellaneous outcomes by the review authors: study procedures (e.g. design) could not be determined based on abstract Correspondence: Prof. Jacqueline Mainwaring, Thomas Jefferson University; jacqueline.mainwaring@jefferson.edu |
Moffatt‐Bruce 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
NCT03613441.
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
| Participants |
Country: USA Setting: paediatric residency training at University of California Los Angeles's Mattel Children's Hospital Age: not specified Sample size (randomised): 82 (actual enrolment) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: residents in paediatrics training Inclusion criteria: 1) age: 18 years and older years; 2) paediatric resident at the University of California Los Angeles's Mattel Children's Hospital; 3) medicine/paediatric resident at University of California Los Angeles's Mattel Children's Hospital Exclusion criteria: none Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: Mindful Awareness Practices (MAPs) (n not specified)
Control: wait‐list control (n not specified; opportunity to receive intervention after study completion) |
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Outcomes reported: not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for the status of the trial (Irwin 2019 [pers comm]) and also whether the trial/intervention focused on resilience. The authors replied about the trial status, but gave no clear response concerning the potential study focus on resilience Study start/end date: June 2017 to April 2018 (actual study completion date) Funding source: University of California, Los Angeles Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: recruitment status: completed, unpublished trial; resilience only mentioned once in trial registration; focus on this construct is unclear Correspondence: Michael Irwin, MD (study director), University of California, Los Angeles, USA; michaelirwin1@mac.com |
NCT03781336.
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
| Participants |
Country: USA Setting: National Institutes of Health (NIH) Clinical Center Age: not specified Sample size (randomised): 82 (actual enrolment) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: NIH employees, contractors, or trainees Inclusion criteria: 1) age: 18 years and older; 2) any NIH employee, contractor, or trainee willing and able to participate in a 5‐week mindfulness‐based self‐care course during the work day; 3) English speaking Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: mindfulness‐based self‐care (n not specified)
Control: wait‐list control (n not specified; as intervention group offered during work hours, wait‐list group best described as TAU) |
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Outcomes reported: not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for the status of the trial and also whether the trial/intervention focus on resilience, but received no response from the authors Study start/end date: October 2017 to June 2018 (actual completion date) Funding source: National Institutes of Health Clinical Center Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not specified Miscellaneous outcomes by the review authors: recruitment status: completed, unpublished trial; resilience only mentioned once in trial registration; focus on this construct is unclear Correspondence: Rezvan Ameli, PhD (principal investigator), National Institutes of Health Clinical Center, USA; rezvan.ameli@nih.gov |
NCT04368676.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
NCT04372303.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
NCT04373382.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
NCT04384861.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Ouyang 2017.
| Methods |
Study design: not specified in abstract (randomisation unclear) Study grouping: not specified in abstract Unit of randomisation: individuals as unit of assignment; however, randomisation unclear Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants |
Country: not specified Setting: hospital Age: not specified in abstract Sample size (randomised): 160 Sex: 160 women Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: primary nurses Included criteria: not specified Excluded criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention 1: positive psychology group only receiving positive psychology (n = 40)
Intervention 2: professional training group receiving professional training (n = 40) Intervention 3: joint counselling group with professional training combined with positive psychology counselling (n = 40)
Control: no intervention (without counselling; n = 40) |
| Outcomes |
Outcomes collected and reported: based on abstract: 1) well‐being (General Well‐Being Schedule ); 2) resilience; 3) anxiety (Self‐Rating Anxiety Scale); 4) nurse satisfaction Time points measured and reported: based on abstract: 1) post‐intervention (after 3 months if intervention); group differences reported Adverse events: not specified in abstract |
| Notes |
Contact with authors: We were not able to identify contact data to ask for the full text and more information about the study procedures Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not specified Miscellaneous outcomes by the review authors: study procedures (e.g. design) could not be determined based on publication abstract; full text not available; no contact data for authors for inquiry identified Correspondence: no contact data identified |
Rodgers 2018.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Ruehl 2013.
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): Sample size was estimated using Cohen 1992 power tables’ suggestions for necessary Ns for sufficient power of 0.80. For a medium‐to‐large effect size with 2 groups, at an α level of P < 0.05, accounting for a 15% attrition rate, a minimum of 60 participants per group were initially required for the study. The current study was only able to recruit 29 participants due to extensive difficulty with participant recruitment Imputation of missing data: no imputation of missing data; per‐protocol and available‐case analysis (i.e. only participants who are finally left in the sample; n = 19) |
| Participants |
Country: USA Setting: psychology office at Rady Children’s Hospital San Diego (RCHSD) or participants' home (if face‐to‐face visits) or mail contact Age: mean = 34.5 (range = 23 ‐ 62) years Sample size (randomised): 29 Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depression (BDI‐II): IG: 5.20 (2.74), CG: 5.00 (5.29); burnout (MBI): IG: 62.00 (11.10), CG: 60.44 (6.13); secondary trauma (STSS): IG: 33.10 (5.80), CG: 27.78 (7.93) Population description: male and female nursing staff from different hospital units Inclusion criteria: 1) currently employed as nurse in the Haematology/Oncology, PICU or NICU at RCHSD for at least 3 months or employed as Emergency Room or Adult Psychiatric nurse working at the same facility for at least 3 months; 2) nurses required to hold one of the following nursing degrees: LVN (Licensed Vocational Nurses), RN (Registered Nurse), ASN, (Associate's Degree in Nursing), BSN (Bachelor of Science in Nursing), or MSN (Master of Science in Nursing); 3) self‐reported perceived stress: reported at least 1 work‐related or personal stressor (list of work‐related and personal‐life stressors); 4) report of a traumatic event or events: report experience of 1+ traumatic events, as measured by Traumatic Life Events Questionnaire; 5) employed at least 30 hours a week; 6) directly involved with patient care; 7) participants currently taking any medications, including psychotropic medications, must be stabilised on medications for at least 1 month prior to starting the study and were requested not to change medication status during the study; had to notify investigator of any medication changes; 8) read and write in English; 9) be able to write for required duration of 20 ‐ 30 minutes, on 3 separate occasions Exclusion criteria: 1) current medical diagnosis of a major chronic illness (i.e., heart disease, cancer, hypertension, diabetes, HIV, liver/kidney disease); 2) starting new medication, or with medication changes less than 1 month prior to study start dates; 3) individuals with symptoms of psychotic spectrum disorders, bipolar disorder, dissociative disorders, or organic brain damage, as indicated by a recent diagnosis, past/current hospitalisations, active psychosis, or use of antipsychotic medications not eligible; 4) reporting a current or recent suicidal ideation/threat within the past 6 months or suicidal attempt within the past year (were referred to psychiatric care); 5) participants currently in psychotherapy were asked not to change their psychotherapist during study and asked not to make any changes in their psychotherapy during the study Attrition (withdrawals and exclusions): 9 dropouts (attrition rate of 31%); 1 exclusion from final analysis Reasons for missing data: DROPOUTS: main reasons for attrition: participants too busy; 3 initially expressed interest in study participation, but did not return preliminary consents/questionnaires; 1 dropped for meeting exclusion medical criteria; 3 dropped prior to writing; 2 did not complete post‐ and follow‐up questionnaires; EXCLUSION: 1 (CG) excluded due to significant outlying variables |
| Interventions |
Intervention: written emotional expression intervention (n = 10 in analysed sample)
Control: attention control (n = 9 in analysed sample)
|
| Outcomes |
Outcomes collected and reported:
Post‐traumatic growth (PGI) and other variables as exploratory measure; further exploratory measures and moderators assessed (not presented here since no outcomes) Time points measured and reported: 1) pre‐intervention (1 week prior to first writing session); 2) post‐intervention (1 week after last writing session); 3) 6‐week follow‐up (5 weeks after 1st post‐test appointment, since post‐test is 1 week after last writing session ‐‐> 6 weeks after last writing session); NO OUTCOME MEASURE, but assessed before and after each writing session: PANAS as measure of current affective state (for manipulation check) Adverse events: not specified |
| Notes |
Contact with authors: We contacted authors for the potential focus of the intervention on fostering post‐traumatic growth, but received no response Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: probably approved by IRBs of Alliant International University, and Rady Children’s Hospital and Care Center, San Diego Comments by study authors: not specified Miscellaneous outcomes by the review authors: dissertation; post‐traumatic growth assessed as exploratory measure, but unclear if also primary focus of the study on fostering this construct Correspondence: no contact data for author Brooke D. Ruehl identified; therefore, contact to Melanie Greenberg, PhD (dissertation chair person); melanie@drmelaniegreenberg.com |
Van Berkel 2014.
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): The sample size was based on finding an effect on the primary outcome of this study, work engagement, measured using the UWES. An effect of a 10% increase in mean score was expected to be relevant and feasible. With a power of 90% and a 2‐sided α of 5%, both groups needed 89 participants. Accounting for a loss to follow‐up of 25% over 12 months, each group needed 119 workers at baseline, thus an initial total of 238 participants for the 2 groups Imputation of missing data: intention‐to‐treat analysis (linear mixed effects model; according to authors all 257 participants taken into analyses) and sensitivity analysis (linear regression analyses with complete cases at either time 1 (T1) or time 2 (T2), i.e. only participants with at least 1 follow‐up measurement) |
| Participants |
Country: The Netherlands Setting: intervention held in a room at the worksite (2 Dutch research institutes) Age: mean = 45.6 (SD = 9.5) years Sample size (randomised): 257 Sex: 173 women, 84 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: mental health (mental health scale 36‐Item Short Form Survey Instrument, RAND‐36): IG: 74.8 (12.9); CG: 73.6 (14.1) (range: 0 ‐ 100) Population description: employees from Dutch research institutes Inclusion criteria: 1) signed informed consent; 2) not being on sick leave for more than 4 weeks; 3) not being pregnant at the time of recruitment Exclusion criteria: not specified Attrition (withdrawals and exclusions): lost to follow‐up: post‐intervention (T1; at 6 months after baseline): n = 22 (IG: 8, CG: 14); 6‐month follow‐up (T2; at 12 months after baseline): n = 3 further lost to follow‐up in CG Reasons for missing data: reasons for losses to follow‐up: resignation (n = 6), no time (n = 11), personal reasons (n = 4), dissatisfied with control (n = 3), unknown (n = 1) |
| Interventions |
Intervention: active control (weblink to website about health promotion) + Mindful ‘Vitality In Practice’ intervention (Mindful VIP intervention) (n = 129)
Control: active control (n = 128)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (after 6‐month intervention; 6 months after baseline); 3) 6‐month follow‐up (6 months post‐intervention/12 months after baseline) Adverse events: not specified |
| Notes |
Contact with authors: We contacted authors for the potential inclusion of healthcare professionals and the respective subgroup data (if included), but had received no response at the time of writing the review Study start/end date: recruitment between April 2010 to November 2010; follow‐up assessment between October 2010 to November 2011 Funding source: part of a research intervention, ‘‘Vitality In Practice’’, which is financed by Fonds Nuts Ohra (Nuts Ohra Foundation) Declaration of interest: no competing interests Ethical approval needed/obtained for study: approved by the Medical Ethics Committee of the Vrije Universiteit (VU) University Medical Center Comments by study authors: Netherlands Trial Register NTR2199; study protocol available in Supplement (Van Berkel 2011) Miscellaneous outcomes by the review authors: unclear whether healthcare professionals were also included in this study; 2 reports of the same study, 1 of them focuses on lifestyle behaviours Correspondence: Jantien van Berkel; Corresponding author: Cécile R. L. Boot, Department of Public and Occupational Health ‐ Institute for Health and Care Research, VU University Medical Center and Body@Work, Research Center on Physical Activity, Work and Health (TNO‐VU) University Medical Center, Amsterdam, the Netherlands; crl.boot@vumc.nl |
Yeo 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
α: alpha (significance level); BAI: Beck Anxiety Inventory; BDI: Beck Depression Inventory; BRS: Brief Resilience Scale; CBT: cognitive behavioural therapy; CD: compact disc; CG: control group; d: delta (Cohen's d, effect size); e.g.: for example; FFMQ: Five‐Facet Mindfulness Questionnaire; IG: intervention group; IRB: Institutional Review Board; n: sample size (e.g. in respective study group); MAAS: Mindful Attention and Awareness Scale; MAPs: mindful awareness practices; MBI: Maslach Burnout Inventory; MBSR: Mindfulness‐based Stress Reduction; MSC: Mindful Self‐Compassion; NICU: Neonatal Intensive Care Unit; OFER15: Occupational Fatigue Exhaustion Recovery Scale; PANAS: Positive and Negative Affect Schedule; PGI: Post‐traumatic Growth Inventory; PICU: Paediatric Intensive Care Unit; POMS: Profile of Moods States; PSS: Perceived Stress Scale; PSQ: Perceived Stress Questionnaire; PSQI: Pittsburgh Sleep Quality Index; RAND‐36: Short Form Health Survey; RCT: randomised controlled trial; SCS: Self‐Compassion Scale; SD: standard deviation; SMART‐3RP: Stress Management and Resilience Training ‐ Relaxation Response Resilience Program; STSS: Secondary Trauma Stress Scale; TAU: treatment as usual; UWES: Utrecht Work Engagement Scale; VAS: Visual Analogue Scale
Characteristics of ongoing studies [ordered by study ID]
ACTRN12617000290392.
| Study name |
Public title: Doctors working well: a study evaluating an online stress management program for doctors Scientific title: A randomised controlled trial of an online intervention on resiliency, occupational stress, and burnout among junior medical doctors |
| Methods |
Study design: 2‐arm RCT Study grouping: parallel assignment Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants |
Country: Australia Setting: online, self‐guided intervention Age: see inclusion criteria; age not specified Sample size (randomised): 60 (targeted) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: registered junior medical doctors Inclusion criteria: 1) registered junior medical doctors (in this study, defined as being an intern, junior house, or senior house doctor); 2) practising in the West Moreton Hospital and Health Service district (Queensland, Australia); 3) aged 18 years or older Exclusion criteria: 1) aged younger than 18 years; 2) not a medical doctor; 3) practising outside the West Moreton Hospital and Health Service area Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: Doctors Working Well (n not specified)
Control: active control (n not specified)
|
| Outcomes |
Outcomes collected and reported:
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 3‐month follow‐up (exception: satisfaction with programme only at post‐intervention);time points reported not specified Adverse events: not specified |
| Starting date | Study start/end date: March 2017 (date of first enrolment) to July 2018 (anticipated date of last data collection); not yet recruiting according to trial registration |
| Contact information |
Principal investigator: Dr Bonnie Clough (according to trial registration); new contact since Dr Clough changed position: Dr Michael Ireland Address: School of Psychology and Counselling; University of Southern Queensland, Springfield Campus; 37 Sinnathamby Boulevard, Springfield Central, Queensland, 4300 Country Australia Email: Michael.Ireland@usq.edu.au Telephone: not specified |
| Notes |
Contact with authors: We contacted the authors for the trial status. According to the authors, the trial is still ongoing and there are no results yet (Ireland 2019 [pers comm]) Funding source: University of Southern Queensland; West Moreton Hospital and Health Service Declaration of interest: not specified Ethical approval needed/obtained for study: approved by West Moreton Hospital and Health Service Human Research Ethics Committee (HREC/16/QWMS/519) and University of Southern Queensland Human Research Ethics Committee (H17REA025) Comments by study authors: not specified Miscellaneous outcomes by the review authors: trial registration number: ACTRN12617000290392 (assigned 24 February 2017) |
JPRN UMIN000031435.
| Study name |
Public title: Mindfulness for health professionals building resilience and compassion (MHALO program) ‐ randomised control trial Scientific title: Mindfulness for health professionals building resilience and compassion (MHALO program) ‐ randomised control trial |
| Methods |
Study design: 2‐arm RCT Study grouping: parallel assignment Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants |
Country: Japan Setting: medical professionals; training setting not specified Age: see inclusion criteria; age not specified Sample size (randomised): 70 (targeted) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: medical professionals in the field of oncology or palliative care or both Inclusion criteria: 1) age 20 years to 65 years (men and women); 2) medical professionals who work in the field of oncology and/or palliative care; 3) those who will be able to participate/commit in the whole programme; 4) those who feels psychological distress or difficulty; 5) no history of psychiatric illness (including with more than 2 years of remission); 6) submission of written informed consent Exclusion criteria: 1) who are unable to be followed up for 3 months; 2) past experience of formal mindfulness‐based intervention; 3) serious physical illness; 4) judged by the research team as ineligible Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: Mindfulness for health professionals building resilience and compassion (MHALO program) (n not specified)
Control: no intervention (n not specified) |
| Outcomes |
Outcomes collected and reported:
Outcomes reported: not specified Time points measured and reported: not specified Adverse events: not specified |
| Starting date | Study start/end date: February 2018 (23 February 2018 date of first enrolment); end date not specified; recruiting according to trial registration |
| Contact information |
Principal investigator: Daisuke Fujisawa Address: Department of Neuropsychiatry, School of Medicine, Keio University, 35 Shinano‐machi, Shinjuku, Tokyo Email: dai_fujisawa@yhoo.co.jp Telephone: 03‐3353‐1211 |
| Notes |
Contact with authors: We contacted the authors for the trial status. According to the authors, the MHALO programme is currently in the final observation period and results will be published in several months (Fujisawa [pers comm]). Funding source: Keio University Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not specified Miscellaneous outcomes by the review authors: trial registration number: JPRN‐UMIN000031435 (assigned 23 February 2018) |
NCT03518359.
| Study name |
Public title: Enhanced Stress Resilience Training for Residents (ESRT‐R) Scientific title: Enhanced resilience training to improve mental health, stress and performance in resident physicians |
| Methods |
Study design: 2‐arm RCT Study grouping: parallel assignment Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants |
Country: USA Setting: Emergency Medicine, Internal Medicine, Paediatrics, Family Practice, Obstetrics and Gynaecology (OBGYN) and Surgery Departments of University of California San Francisco Age: see inclusion criteria; age not specified Sample size (randomised): 45 (actual enrolment) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified, but participants with lifetime history of organic mental illness excluded Population description: resident physicians/medical interns Inclusion criteria: 1) any consented medical intern from Emergency Medicine, Internal Medicine, Paediatrics, Family Practice, OBGYN and Surgery Departments in‐coming to University of California San Francisco in the study year; 2) aged 18 ‐ 64 years Exclusion criteria: 1) current personal mindfulness practice, once a week or more frequent; 2) use of medications with Central Nervous System effects; 3) lifetime history of an organic mental illness; 4) acute or chronic immune or inflammatory disorders; 5) pregnancy Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: Enhanced Stress Resilience Training (ESRT) (n not specified)
Control: active control (n not specified)
|
| Outcomes |
Outcomes collected and reported:
Outcomes reported: not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (9 ‐ 10 weeks after baseline); 3) 6‐month follow‐up; time points reported not specified Adverse events: not specified |
| Starting date | Study start/end date: June 2018; estimated primary completion date: June 2021; estimated study completion date: June 2022; active, not recruiting according to trial registration |
| Contact information |
Principal investigator: Carter K Lebares, MD; Ekaterina V Guvva, BS Address: University of Californisa, San Francisco, California, United States, 94143 Email: carter.lebares@ucsf.edu; ekaterina.guvva@ucsf.edu Telephone: 415‐502‐5588 |
| Notes |
Contact with authors: We contacted the authors for the trial status. According to the authors, the recruitment for study is closed and the results will be published in the next 6 months (Guvva 2019 [pers comm]). Funding source: University of California, San Francisco Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not specified Miscellaneous outcomes by the review authors: trial registration number: NCT03518359 (assigned 8 May 2018) |
NCT03645512.
| Study name |
Public title: Resilience intervention for critical care nurses Scientific title: A randomised controlled trial of a resilience intervention for critical care nurses |
| Methods |
Study design: 2‐arm RCT Study grouping: parallel assignment Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants |
Country: USA Setting: Florida Hospital (adult ICU), PICU, paediatric cardiac congenital intensive care (PCVICU), or Level 3 NICU at the Altamonte, Orlando, or Winter Park campus Age: see inclusion criteria; age not specified Sample size (randomised): 108 (actual enrolment) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified, but participants with high score on emotional exhaustion or depersonalisation of MBI excluded Population description: critical care nurses Inclusion criteria: 1) adult ≥ 18 years old; 2) employed as a critical care nurse at Florida Hospital in an adult ICU, PICU, PCVICU, or Level 3 NICU at the Altamonte, Orlando, or Winter Park campus; 3) able to speak, read, and understand English fluently; 4) able to provide informed consent; 5) meet ≥ 2 stress‐experience level parameters on the Stress Mindset Measure ‐ General (SMM‐G); 6) meet ≤ 4.3 on the BRS; 7) willing to attend a full‐day training programme at Human Performance Institute (HPI) on the designated training date; 8) willing and able to comply with all study procedures and requirements for the duration of the study Exclusion criteria: 1) meet < 2 stress‐experience level parameters on the SMM‐G; 2) meet > 4.3 on the BRS; 3) receive a high score of ≥ 27 on the Emotional Exhaustion domain and/or a high score of ≥ 13 on the Depersonalisation domain of the MMBI‐HSS) for Medical Personnel (MP) Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: Corporate Athlete® Resilience (CAR) Training Program (n not specified)
Control: wait‐list control (n not specified; 3‐month waiting period) |
| Outcomes |
Outcomes collected and reported:
Outcomes reported: not specified Time points measured and reported: 1) pre‐intervention; 2) 6‐month follow‐up (change from baseline score at 6‐months post CAR training); time points reported not specified Adverse events: not specified |
| Starting date | Study start/end date: October 2018; estimated study completion date: June 2019; active, not recruiting according to trial registration (i.e. study is ongoing, and participants are receiving an intervention or being examined, but potential participants are not currently being recruited or enrolled; last update posted: March 2019) |
| Contact information |
Principal investigator: Amanda T Sawyer, PhD Address: Florida Hospital; AdventHealth Research Institute, 301 E Princeton St., Orlando, Florida 32804, USA Email: Amanda.Sawyer@adventhealth.com Telephone: not specified |
| Notes |
Contact with authors: We contacted the authors for the trial status, but received no response Funding source: Florida Hospital Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not specified Miscellaneous outcomes by the review authors: trial registration number: NCT03645512 (assigned 24 August 2018) |
NCT03759795.
| Study name |
Public title: Bournemouth University Resilience Training for Surgeons (BURTS) Scientific title: Ameliorating the impact of complications and errors on surgeons: Resilience Training for Surgeons For more details, see study protocol: clinicaltrials.gov/ProvidedDocs/95/NCT03759795/Prot_001.pdf |
| Methods |
Study design: 2‐arm RCT Study grouping: parallel assignment Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified; 100 intended to recruit to allow for some attrition and still have approximately 45 participants per condition Imputation of missing data: not specified |
| Participants |
Country: United Kingdom Setting: local hospitals (initially Royal Bournemouth Hospital in Bournemouth, Dorset, and Poole Hospital in Poole, Dorset; later: John Radcliffe Hospital, Oxford, Southampton General Hospital, Southampton, and Portsmouth General Hospital) Age: see inclusion criteria; age not specified Sample size (randomised): 100 (estimated enrolment) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: trainee surgeons and consultant surgeons Inclusion criteria: 1) trainee surgeons and consultant surgeons; 2) 21 years to 75 years Exclusion criteria: none Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: Acceptance and Commitment Training (ACTr) (n not specified)
Control: wait‐list control (n not specified; same ACTr sessions offered once current study has ended) |
| Outcomes |
Outcomes collected and reported:
Outcomes reported: not specified Time points measured and reported: 1) 2 weeks before training session 1; 2) immediately before training session 2; 3) immediately before training session 3; 4) post‐intervention (within 2 weeks after completion of training session 3); 5) 3‐month follow‐up (12 weeks after training session 3); time points reported not specified Adverse events: not specified |
| Starting date | Study start/end date: December 2018; estimated study completion date: August 2020; recruiting according to trial registration (last update posted: January 2020) |
| Contact information |
Principal investigator: Dr Helen Bolderston Address: Bournemouth University, Poole House P252, Talbot Campus, Fern Barrow, Poole, BH12 5BB, UK Email: hbolderston@bournemouth.ac.uk Telephone: not specified |
| Notes |
Contact with authors: no contact with authors needed Funding source: see study protocol:
Declaration of interest: not specified Ethical approval needed/obtained for study: ethical approval sought from the university ethics team and the Integrated Research Application System Comments by study authors: not specified Miscellaneous outcomes by the review authors: trial registration number: NCT03759795 (assigned 30 November 2018) |
AAQ: Acceptance and Action Questionnaire; BRS: Brief Resilience Scale; CAMS‐R: Cognitive and Affective Mindfulness Scale ‐ Revised; CBI: Copenhagen Burnout Inventory; CD: compact disc; CD‐RISC: Connor‐Davidson Resilience Scale; CG: control group; DASS: Depression Anxiety Stress Scale; e.g.: for example; EMBQ: Energy Management Behaviors Questionnaire; FFMQ: Five‐Facet Mindfulness Questionnaire; GHQ: General Health Questionnaire; HPQ: Health Performance Questionnaire; IG: intervention group; MBI: Maslach Burnout Inventory; MBI‐HSS: MBI ‐ Human Services Survey; MBSR: Mindfulness‐based Stress Reduction; n: sample size (e.g. in respective study group); NICU: Neonatal Intensive Care Unit; PHQ: Patient Health Questionnaire; PICU: Paediatric Intensive Care Unit; POMS: Profile of Moods States; PSS: Perceived Stress Scale; RCT: randomised controlled trial; SCS: Self‐Compassion Scale; SD: standard deviation; Spielberger's STAI: Spielberger's State Trait Anxiety Inventory; SWLS: Satisfaction with Life Scale; VLQ: Value Living Questionnaire; WAAQ: Work‐related Acceptance and Action Questionnaire
Differences between protocol and review
All modifications to the methods specified in the protocol (Helmreich 2017) are described in the following section.
-
Title
We changed the title of the review due to the post hoc restriction to healthcare professionals (see Types of participants).
-
Due to the post hoc restriction to healthcare professionals, we adapted the Background sections (Description of the condition; Description of the intervention; How the intervention might work; Why it is important to do this review) for this target group, e.g. by adding current references about previous systematic reviews in this population.
-
Description of the intervention
We modified the first sentence of this section to illustrate that we refer to resilience intervention research in general.
To be consistent, we limited the number of references for each psychotherapeutic method to one reference.
-
How the intervention might work
We changed the order of appearance of the different psychotherapeutic approaches, to present theoretical approaches that are associated with cognitive‐behavioural therapy (CBT), such as stress inoculation and problem‐solving therapy, immediately after CBT, before discussing other theoretical approaches.
Instead of performing a subgroup analysis on the target group of training, we had planned to conduct a subgroup analysis of the training intensity, and added arguments for whether participants could benefit differently from differing training intensities.
To derive the planned subgroup analysis for the theoretical foundation, we modified the section by describing the recent results of Joyce 2018, who analysed the impact of theoretical foundations of resilience intervention for the first time. At the time of writing the protocol, this systematic review had not been published.
-
Why it is important to do this review
Compared to the protocol, we presented the need for doing this review by integrating the results of recently‐published systematic reviews in clinical and non‐clinical adult populations (e.g. Joyce 2018).
-
We modified the objectives of the review to refer only to healthcare professionals, reflecting the post hoc restriction to this population.
-
Post hoc change ‐ step 1: Initially, we planned to include clinical and non‐clinical populations (e.g. patients, employees, students, military) in this review (see Helmreich 2017). Based on a broad search strategy in October 2016, we identified 251 studies and 18 ongoing studies evaluating resilience‐training programmes in a variety of target groups. To be able to manage the large number of studies with many divergent target groups, we decided to de‐scope the review based on the populations investigated. This also allowed us to perform top‐up searches (i.e. for the period October 2016 to the present) that were specific for the respective target groups. We made the decision to de‐scope the review for two main reasons. First, using the database of 269 studies found by searches in October 2016, the review that we had originally planned might have been trumped by the publication of studies since this time point. Studies published since 2016, for example, using innovative delivery formats or different therapeutic methods than earlier studies might possibly have affected the results of subgroup analysis of the review (e.g. concerning delivery format). In addition, we expected a substantial number of new studies fulfilling the eligibility criteria of the review for the period end 2016 to 2019. Especially since 2015, there has been a significant growth in publications in this field. For example, by searching additional sources (e.g. reference lists, trial registers) or study protocols published until October 2016, we identified 26 RCTs published between 2017 and 2018. We also found 16 completed studies that had not yet been published (e.g. manuscripts in preparation or under review). Second, the RCTs identified were spread across a large number of comparisons (e.g. different target groups, theoretical foundations of interventions or control groups), which might have over‐scoped the review and resulted in substantial heterogeneity if we had included all 269 studies. Based on the number of studies identified for the healthcare sector (including healthcare professionals like physicians, healthcare students like medical students and employees associated with the healthcare sector such as human service professionals) in October 2016, we therefore decided to focus on RCTs in these populations. In June 2019, we performed top‐up searches focusing broadly on the healthcare sector, in order to guarantee a review of high credibility, which synthesises the latest evidence on the efficacy of psychological resilience interventions in this group at the time of publication.
Post hoc change ‐ step 2: Based on the top‐up searches in June 2019, we identified 31 studies and eight ongoing studies that had been performed in healthcare professionals, healthcare students, and employees associated with the healthcare sector. Combining these with the original search, we found a total of 80 RCTs and nine ongoing studies in this population. During the process of writing up this review, and the editorial process, we made further decisions about the eligibility criteria of this review for the 'Types of participants'. We further separated the pool of 80 RCTs into two groups: 1) healthcare professionals (i.e. with completed training) and 2) healthcare students. On the evidence base from the two searches, this review refers to healthcare professionals. In addition, we also considered studies with mixed samples, where healthcare professionals were included as a subgroup (total: 44 RCTs and five ongoing studies). A second review (Kunzer unpublished) refers to psychological interventions to foster resilience in healthcare students (total: 30 RCTs and three ongoing studies). We took this decision for the following empirical reasons. First, when summarising the 80 RCTs in a first review draft, we identified a substantial amount of heterogeneity for these studies that could only be partially explained by the planned subgroup analyses (see Table 2). Similarly, during internal peer review, the question arose about whether the research question of such a review (i.e. including healthcare professionals, students, and different employees associated with the healthcare sector) was too broad and the studies too heterogeneous to combine in the same review. We therefore decided to split the review into two publications, one for healthcare professionals and one for healthcare students, in order to create two focused reviews that are based on sufficiently homogeneous studies, are up‐to‐date, and provide a concise summary of the evidence for the reviews' readers. A second rationale behind the decision to further split the data is the stressor exposure in the two groups of healthcare professionals and healthcare students: Students and qualified staff have different stressor exposures and responsibilities, which might moderate the effect of resilience training. While healthcare professionals are exposed to stressors such as shift work, medical decision‐making or hierarchies, students are confronted with different kind of stressors (e.g. exams, challenging subjects). Thus, a split between these two groups seemed reasonable. Based on both searches, we had identified six studies in employees widely associated with the healthcare sector, whose samples were too heterogeneous (e.g. human service professionals, nurse managers) to combine them with healthcare professionals (e.g. physicians, nurses), that are mostly employed in clinical practice and patient care. In addition, it is questionable whether these employees can be viewed as front‐line healthcare staff and should be included in a review of this target group. We therefore decided to omit this group of studies.
Based on these two post hoc changes, which we had discussed with the CDPLP editorial team, we adapted the Types of participants section accordingly, to specify that this review covered healthcare professionals (i.e. healthcare staff delivering direct medical care such as physicians, nurses, hospital personnel) and allied healthcare staff working in allied health professions distinct from medical care (e.g. psychologists, social workers, counsellors, physical therapists, occupational therapists, speech therapists, medical assistants, medical technicians). Since we also identified several eligible studies in mixed samples, we stated that we would include these mixed samples in the review and also included them in meta‐analyses, provided we could obtain the data from the study authors for healthcare professionals as a discrete group.
-
We stated in the protocol that we planned to include broader, health‐promoting interventions (e.g. well‐being therapy), but in the full review we included only studies that explicitly defined the aim of fostering resilience, hardiness or post‐traumatic growth by using one or more of these terms in the publications. We made this modification on the basis of a post‐protocol amendment in consultation with the CDPLP editorial team and the Cochrane Editorial and Methods Department. During the initial process of literature extraction, we realised that it was not feasible to consider all health‐promoting interventions that aim to foster resilience in a broader sense (e.g. mental health, well‐being, psychological adaptation in a population with stressor exposure) without including the terms resilience, hardiness or post‐traumatic growth, for the following reasons. First, it appeared very difficult to decide between which of the very large number of interventions should be included in the review and which should not, since the relationship of the interventions to the concept of resilience was not made explicit in those interventions. This would have left the review authors having to make many assumptions with no objective criteria, resulting in reduced traceability of selection criteria and potentially low inter‐rater reliability at the end of screening. Second, since the objective of the review was to synthesise the current evidence on the efficacy of resilience training, including broader interventions could have biased the review’s conclusions, as fostering resilience was not explicitly formulated as an aim in any of those interventions.
-
Based on a suggestion during internal peer review, we added adverse events as a primary outcome of this review, and marked it with an asterisk for inclusion in the 'Summary of findings' table.
-
We planned to perform searches in October 2016 for a review of psychological resilience interventions in clinical and non‐clinical populations. However, due to post hoc modification of the inclusion criteria, the search processes for the review were based on a two‐step approach, with searches performed in October 2016 and top‐up searches in June 2019.
We expanded the description of the search process by adding details about using the Cochrane Highly Sensitive Search Strategy for MEDLINE and Embase, as specified in the Cochrane Handbook (Lefebvre 2019), in order to present the search strategy in sufficient detail.
We searched the Web of Science Core Collection databases simultaneously rather than individually (Science Citation Index; Social Science Citation Index; Conference Proceedings Citation Index ‐ Social Science & Humanities; Conference Proceedings Citation Index ‐ Science), since our institutional access to this database only offered this possibility.
-
We judged the feasibility of selection criteria after 500 instead of 50 studies screened due to the large number of records yield by the searches for this review.
-
Assessment of risk of bias in included studies
We reported that we considered the achieved baseline comparability between study conditions as part of selection bias (random‐sequence generation) in addition to the standard 'Risk of bias' domains in the Cochrane Handbook (Higgins 2011b). We had extracted this additional information from the included studies and judged it to be interesting for the readers of this review.
-
Continuous data: In the protocol we said we would calculate standardised mean difference (SMD) effect sizes because resilience‐training studies are likely to use different measures for resilience and related constructs. We therefore added a sentence about the variation in measurement scales between included studies and referred to Table 3 and Table 4 on the outcome scales used. We added the information on how we interpreted the magnitude of effect sizes (SMDs) for continuous outcomes in the review.
-
Repeated observations on participants: we explained when we judged post‐test in intervention studies as post‐intervention assessment and considered them in the respective meta‐analyses. Assessments at more than one week after the end of training were declared as post‐test by some study authors, although interim events between the end of the intervention and the assessment might have affected the effects measured. We wished to differentiate between such assessments and 'real' post‐tests with greater proximity to the end of training (i.e. within one week after the intervention ended).
-
We supplemented the procedure of dealing with missing data in the review by explaining how we would handle missing data in studies of mixed samples. We added this information as we also considered studies with mixed samples in the review (see point 4 above).
We added a sentence explaining how we managed missing/incomplete summary outcome data, as well as missing outcome data due to attrition.
-
We added a sentence explaining that we discuss the similarities and differences between the included studies (e.g. in terms of study characteristics) in the Results and Discussion section of the review.
We further described the conventions used to interpret I2 values on the basis of suggestions in the Cochrane Handbook (Deeks 2019), and added information about conducting subgroup analyses to investigate substantial heterogeneity (I2 ≥ 50%), in order to be transparent.
We added a sentence explaining that we calculated the 95% prediction intervals from random‐effects meta‐analyses to present the extent of between‐study variation according to the Cochrane Handbook (Deeks 2019).
-
Assessment of reporting biases
We had stated in the protocol that we would assess potential publication bias by drawing and inspecting funnel plots. In the review, we expanded the description of this process by adding the information about analysing reporting bias on the basis of at least 10 studies in the meta‐analysis for one outcome.
We inspected contour‐enhanced funnel plots for the primary outcomes, as they offer more graphical possibilities to detect a potential publication bias than standard funnel plots.
-
For several studies in the review that provided no means and SDs, but provided alternative data to calculate SMDs and the respective standard error, we described the procedure for combining these with other studies using the generic invariance method in RevMan. This information had been missing from the protocol (Helmreich 2017).
We expanded the description of how we managed scales for depression and burnout, as well as scales for general well‐being or quality of life and work‐related measures in the same study, because several included studies fitted this case.
We did not conduct a network meta‐analysis, as planned, due to the insufficient evidence base in the review.
-
Summary of findings
We added information about the inclusion of the primary outcomes at post‐test in the ‘Summary of findings’ table. We took the decision to restrict the outcomes to those assessed at post‐test following internal peer review. Adverse events are also included here (see Types of outcome measures and point 6 in this section).
We replaced the term 'quality of the evidence' with 'certainty of the evidence' throughout the review, in order to be consistent with current guidelines and preferences in the literature (Hultcrantz 2017).
We provided further details about the downgrading of studies for each of the five GRADE criteria (study limitations, indirectness, inconsistency, imprecision, publication bias).
We also explained how we interpreted effect sizes and rated the certainty of the evidence, as this information had been missing from the protocol (Helmreich 2017).
-
Subgroup analysis and investigation of heterogeneity
We omitted the preplanned sensitivity analysis on 'target group in resilience interventions', due to the review's revised focus on healthcare professionals only.
We added a post hoc analysis for training intensity; low‐intensity training included interventions with a total duration of five hours or less or three sessions or fewer (if no duration in hours or minutes was indicated); moderate intensity referred to training that included more than five hours to 12 hours or less, or more than three to 12 sessions or fewer; and high intensity to programmes of more than 12 hours or more than 12 sessions. We added this subgroup analysis post hoc due to the restriction to healthcare students (see point 2c).
We added a subgroup for mobile‐based delivery format to the preplanned analysis on delivery format, given the evidence found in this review.
We changed ‘multimodal intervention’ to ‘combined intervention’ to the preplanned analysis on theoretical foundation, to refer to resilience interventions that were based on two or more explicit theoretical foundations such as CBT and ACT or CBT and mindfulness. We also added coaching, positive psychology and unspecific resilience training. Non‐specific training programmes included resilience interventions fostering one or several resilience factors but without specifying any explicit theoretical foundation, or where the underlying framework could not be assigned to a certain theoretical foundation. We changed from 'multimodal' to 'combined intervention' in order to be consistent with other subgroup analyses (compare combined setting, combined delivery). We added the extra subgroups based on the evidence found in this review.
Lastly, we added active and attention control to the preplanned analysis on comparator groups, in order to distinguish between these groups. Attention‐control groups referred to an alternative treatment that mimicked the amount of time and attention received (e.g. by the trainer) in the intervention group. We used the term ‘active control’ for alternative treatment (no standard care; for example, treatment developed specifically for the treatment study) but that did not control for the amount of time and attention in the intervention group, and was not attention control in a narrow sense. We made these changes due to the evidence found in this review.
We added information about which subgroup analyses were prespecified and which were added post hoc.
-
We provided more detail on the planned sensitivity analyses based on risk of bias (i.e. restriction to studies at low and unclear risk of attrition as well as at low and unclear risk of reporting bias, respectively), as this information had been missing from the protocol (Helmreich 2017). We chose attrition and reporting bias as key domains for the sensitivity analyses, since most of the variability between included studies was evident in these domains.
Contributions of authors
Angela Kunzler: protocol writing, study selection, data extraction and assimilation, 'Risk of bias' assessment, GRADE assessment, statistical analysis and review writing. Angela Kunzler has overall responsibility for the review and is the guarantor for the review. Isabella Helmreich: protocol writing, study selection, data extraction, 'Risk of bias' assessment, GRADE assessment, review writing. Andrea Chmitorz: protocol writing, review writing, arbiter. Jochem König: protocol writing, expert statistical support, statistical analysis and review writing. Harald Binder: protocol writing, expert statistical support, statistical analysis and review writing. Michèle Wessa: protocol writing and review writing. Klaus Lieb: overall supervision of the review, protocol writing, review writing, arbiter.
All review authors agreed on this version before publication.
Sources of support
Internal sources
-
Leibniz Institute for Resilience Research (LIR) gGmbH, Wallstraße 7/7a, 55122 Mainz, Germany
Home institution of AMK, IH, MW and KL; support provided in the form of salary and resources.
-
Institute of Medical Biostatistics, Epidemiology and Informatics (IMBEI), University Medical Center of the Johannes Gutenberg University Mainz, Germany
Home institution of JK; support provided in the form of salary and resources.
-
Institute of Medical Biometry and Statistics, Faculty of Medicine and Medical Center ‐ University of Freiburg, Freiburg, Germany
Home institution of HB; support provided in the form of salary and resources.
External sources
-
Funding provided by the Ministry of Science (MWWK) of the State Rhineland‐Palatinate, Germany
Support provided in the form of resources.
Declarations of interest
Angela Kunzler – none known. Isabella Helmreich is a board‐certified cognitive‐behaviour therapist. Andrea Chmitorz is a board‐certified cognitive‐behaviour therapist. Jochem König – none known. Harald Binder – none known. Michèle Wessa is a board‐certified cognitive‐behaviour therapist. Klaus Lieb is a board‐certified cognitive‐behaviour therapist with a special interest in schema therapy. Klaus Lieb is an Editor with Cochrane Developmental, Psychosocial and Learning Problems. Klaus Lieb received funding for this review from the Ministry of Science (MWWK) of the State Rhineland‐Palatinate, Germany.
New
References
References to studies included in this review
Alexander 2015 {published data only}
- Alexander GR, Rollins K, Walker D, Wong L, Penings J. Yoga for self-care and burnout prevention among nurses. Workplace Health & Safety 2015;63(10):462-70. [DOI: 10.1177/2165079915596102] [PMID: ] [DOI] [PubMed] [Google Scholar]
Berger 2011 {published data only}
- Berger R, Gelkopf M. An intervention for reducing secondary traumatization and improving professional self-efficacy in well baby clinic nurses following war and terror: a random control group trial. International Journal of Nursing Studies 2011;48(5):601-10. [DOI: 10.1016/j.ijnurstu.2010.09.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bernburg 2016 {published data only}
- Bernburg M, Baresi L, Groneberg D, Mache S. Does psychosocial competency training for junior physicians working in pediatric medicine improve individual skills and perceived job stress. European Journal of Pediatrics 2016;175(12):1905-12. [DOI: 10.1007/s00431-016-2777-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bernburg 2019 {published data only}
- Bernburg M, Groneberg DA, Mache S. Mental health promotion intervention for nurses working in German psychiatric hospital departments: a pilot study. Issues in Mental Health Nursing 2019;40(8):706-11. [DOI: 10.1080/01612840.2019.1565878] [PMID: ] [DOI] [PubMed] [Google Scholar]
Calder Calisi 2017 {published data only}
- Calder Calisi C. The effects of the relaxation response on nurses' level of anxiety, depression, well-being, work-related stress, and confidence to teach patients. Journal of Holistic Nursing 2017;35(4):318-27. [DOI: 10.1177/0898010117719207] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chesak 2015 {published data only}
- Chesak SS, Bhagra A, Schroeder DR, Foy DA, Cutshall SM, Sood A. Enhancing resilience among new nurses: feasibility and efficacy of a pilot intervention. Ochsner Journal 2015;15(1):38-44. [PMC4365845] [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Cheung 2014 {published data only}
- Cheung YL. Psychological First Aid as a Public Health Disaster Response Preparedness Strategy for Responders in Critical Incidents and Disasters [PhD thesis]. Shatin (HK): Chinese University of Hong Kong, 2014. [Google Scholar]
Cieslak 2016 {published and unpublished data}
- Cieslak R, Benight CC, Rogala A, Smoktunowicz E, Kowalska M, Zukowska K, et al. Effects of internet-based self-efficacy intervention on secondary traumatic stress and secondary posttraumatic growth among health and human services professionals exposed to indirect trauma. Frontiers in Psychology 2016;7:1009. [DOI: 10.3389/fpsyg.2016.01009] [PMC4930928] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogala A, Smoktunowicz E, Żukowska K, Kowalska M, Cieślak R. The helpers’ stress: effectiveness of a web-based intervention for professionals working with trauma survivors in reducing job burnout and improving work engagement [Stres pomagających – efektywność interwencji internetowej dla osób pracujących z ofiarami traumy w obniżaniu wypalenia zawodowego i wzmacniaunia zaangażowania w pracę]. Medycyna Pracy 2016;67(2):223-37. [DOI: 10.13075/mp.5893.00220] [PMID: ] [DOI] [PubMed] [Google Scholar]
Clemow 2018 {published data only}
- Clemow LP, Pickering TG, Davidson KW, Schwartz JE, Williams VP, Shaffer JA, et al. Stress management in the workplace for employees with hypertension: a randomized controlled trial. Translational Behavioral Medicine 2018;8(5):761-70. [DOI: 10.1093/tbm/iby018] [PMC6128963 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duchemin 2015 {published and unpublished data}
- Duchemin AM, Steinberg BA, Marks DR, Vanover K, Klatt M. A small randomized pilot study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: effects on salivary α-amylase levels. Journal of Occupational and Environmental Medicine 2015;57(4):393–9. [DOI: 10.1097/JOM.0000000000000371] [PMC4624325] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klatt M, Steinberg BA, Marks DR, Duchemin AM. Changes in physiological and psychological markers of stress in hospital personnel after a low-dose mindfulness-based worksite intervention. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):O16. [DOI: 10.1186/1472-6882-12-S1-O16] [OA04.04] [PMC3373711] [DOI] [Google Scholar]
- Steinberg BA, Klatt M, Duchemin AM. Feasibility of a mindfulness-based intervention for surgical intensive care unit personnel. American Journal of Critical Care 2016;26(1):10-8. [DOI: 10.4037/ajcc2017444] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fei 2019 {published data only}
- Fei Y. Effects of emotional resilience training on nurses' perceived stress, positive and negative emotions and sleep quality [Efectos del entrenamiento de enfermeros en resiliencia emocional sobre el estrés percibido, las emociones positivas y negativas y la calidad del sueño]. Revista Argentina de Clínica Psicológica 2019;28(2):199-209. [DOI: 10.24205/03276716.2019.1106] [DOI] [Google Scholar]
Gelkopf 2008 {published and unpublished data}
- Gelkopf M, Ryan P, Cotton SJ, Berger R. The impact of "training the trainers" course for helping tsunami-survivor children on Sri Lankan disaster volunteer workers. International Journal of Stress Management 2008;15(2):117-35. [DOI: 10.1037/1072-5245.15.2.117] [DOI] [Google Scholar]
Hosseinnejad 2018 {published data only}
- Hosseinnejad F, Arsalani N, Rahgoui A, Biglarian A. Effectiveness of resiliency skills education on job satisfaction among nurses. Journal of Guilan University of Medical Sciences 2018;27(105):50-60. [No DOI available; magiran.com/p1814990] [Google Scholar]
Ireland 2017 {published data only}
- Ireland MJ, Clough B, Gill K, Langan F, O'Connor A, Spencer L. A randomized controlled trial of mindfulness to reduce stress and burnout among intern medical practitioners. Medical Teacher 2017;39(4):409-14. [DOI: 10.1080/0142159X.2017.1294749] [PMID: ] [DOI] [PubMed] [Google Scholar]
ISRCTN69644721 {published data only}
- ISRCTN69644721. An evaluation of a new resilience intervention for emergency workers [A randomised controlled trial to evaluate a new resilience intervention for emergency workers]. www.isrctn.com/ISRCTN69644721 (first received 25 October 2016).
Khoshnazary 2016 {published data only}
- Khoshnazary S, Hosseini MA, Fallahi Khoshknab M, Bakhshi E. The effect of emotional intelligence (EI) training on nurses' resiliency in Department of Psychiatry. Iranian Journal of Psychiatric Nursing 2016;3(4):29-37. [ijpn.ir/article-1-683-en.pdf] [Google Scholar]
Klatt 2015 {published and unpublished data}
- Klatt M, Steinberg BA, Duchemin AM. Mindfulness in motion (MIM): an onsite mindfulness based intervention (MBI) for chronically high stress work environments to increase resiliency and work engagement. Journal of Visualized Experiments 2015;101:e52359. [DOI: 10.3791/52359] [PMC4545050] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lebares 2018 {published data only}
- Lebares CC, Guvva EV, Delucchi KL, Kayser AS, Ascher NL, Harris HW. Mindful surgeon: a pilot feasibility and efficacy trial of mindfulness-based stress resilience training in surgery. Journal of the American College of Surgeons 2018;227(4 Suppl 2):e21. [DOI: 10.1016/j.jamcollsurg.2018.08.051] [DOI] [Google Scholar]
- Lebares CC, Guvva EV, Olaru M, Sugrue LP, Staffaroni AM, Delucchi KL, et al. Efficacy of mindfulness-based cognitive training in surgery: additional analysis of the mindful surgeon pilot randomized clinical trial. JAMA Network Open 2019;2(5):e194108. [DOI: 10.1001/jamanetworkopen.2019.4108] [PMC6632137 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebares CC, Hershberger AO, Guvva EV, Desai A, Mitchell J, Shen W, et al. Feasibility of formal mindfulness-based stress-resilience training among surgery interns: a randomized clinical trial. JAMA Surgery 2018;153(10):e182734. [DOI: 10.1001/jamasurg.2018.2734] [PMC6233792 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT03141190. Mindful mental training for surgeons to enhance resilience and performance under stress [Mindfulness training to improve mental health, stress and performance in physicians]. clinicaltrials.gov/ct2/show/NCT03141190 (first received 1 May 2017).
Lin 2019 {published data only}
- Lin L, He G, Yan J, Gu C, Xie J. The effects of a modified mindfulness-based stress reduction program for nurses: a randomized controlled trial. Workplace Health & Safety 2019;67(3):111-22. [DOI: 10.1177/2165079918801633] [PMID: ] [DOI] [PubMed] [Google Scholar]
Loiselle 2018 {published data only}
- Loiselle ME. Academic Physician Burnout and Transcendental Meditation: A Mixed Methods Randomized Controlled Trial [PhD thesis]. Fairfield (IA): Maharishi University of Management, 2018. [Google Scholar]
Luthar 2017 {published and unpublished data}
- Luthar SS, Curlee A, Tye SJ, Engelman JC, Stonnington CM. Fostering resilience among mothers under stress: "authentic connections groups" for medical professionals. Women's Health Issues 2017;27(3):382-90. [DOI: 10.1016/j.whi.2017.02.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mache 2015a {published and unpublished data}
- Mache S, Danzer G, Klapp B, Groneberg DA. An evaluation of a multicomponent mental competency and stress management training for entrants in surgery medicine. Journal of Surgical Education 2015;72(6):1102-8. [DOI: 10.1016/j.jsurg.2015.06.018] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mache 2015b {published and unpublished data}
- Mache S, Vitzthum K, Klapp BF, Groneberg DA. Evaluation of a multicomponent psychosocial skill training program for junior physicians in their first year at work: a pilot study. Family Medicine 2015;47(9):693-8. [PMID: ] [PubMed] [Google Scholar]
Mache 2016 {published and unpublished data}
- Mache S, Bernburg M, Baresi L, Groneberg DA. Evaluation of self-care skills training and solution-focused counselling for health professionals in psychiatric medicine: a pilot study. International Journal of Psychiatry in Clinical Practice 2016;20(4):239-44. [DOI: 10.1080/13651501.2016.1207085] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mache 2017 {published data only}
- Mache S, Baresi L, Bernburg M, Vitzthum K, Groneberg D. Being prepared to work in gynecology medicine: evaluation of an intervention to promote junior gynecologists professionalism, mental health and job satisfaction. Archives of Gynecology and Obstetrics 2017;295(1):153-62. [DOI: 10.1007/s00404-016-4223-6] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mealer 2014 {published and unpublished data}
- Mealer M, Conrad D, Evans J, Jooste K, Solyntjes J, Rothbaum B, et al. Feasibility and acceptability of a resilience training program for intensive care unit nurses. American Journal of Critical Care 2014;23(6):e97-105. [DOI: 10.4037/ajcc2014747] [PMID: ] [DOI] [PubMed] [Google Scholar]
Medisauskaite 2019 {published data only}
- Medisauskaite A, Kamau C. Reducing burnout and anxiety among doctors: randomized controlled trial. Psychiatry Research 2019;274:383-90. [DOI: 10.1016/j.psychres.2019.02.075] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mirzaeirad 2019 {published data only}
- Mirzaeirad SZ, Arsalani N, Dalvandi A, Rezasoltani P, Hoseini SD. The effect of resilience skills training on nursing stress of nursing staff in hospitals of Golestan province. Journal of Health Promotion Management 2019;8(2):41-8. [hpm.ir/article-1-881-en.html] [Google Scholar]
Mistretta 2018 {published data only}
- Mistretta EG, Davis MC, Temkit M, Lorenz C, Darby B, Stonnington CM. Resilience training for work-related stress among health care workers: results of a randomized clinical trial comparing in-person and smartphone-delivered interventions. Journal of Occupational and Environmental Medicine 2018;60(6):559-68. [DOI: 10.1097/JOM.0000000000001285] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Mistretta EG, Davis MC, Temkit M, Lorenz C, Stonnington CM. Resilience training for work-related stress among healthcare workers: results of a randomized clinical trial comparing in-person and smartphone delivered interventions. Psychosomatic Medicine 2017;79(4):A13. [DOI: 10.1097/PSY.0000000000000473] [DOI] [PubMed] [Google Scholar]
NCT02603133 {published data only}
- NCT02603133. Web-based implementation for the science of enhancing resilience study (WISER). clinicaltrials.gov/ct2/show/NCT02603133 (first received 6 November 2015).
NCT03645798 {published data only}
- NCT03645798. The effects of "three good things" positive psychotherapy on nurses' burnout [The effects of "three good things" positive psychotherapy on burnout, turnover intention, job performance, job satisfaction, self-efficacy, coping styles, resilience and blood cortisol of Chinese nurses]. clinicaltrials.gov/ct2/show/NCT03645798 (first received 16 August 2018).
Poulsen 2015 {published data only}
- Poulsen AA, Sharpley CF, Baumann KC, Henderson J, Poulsen MG. Evaluation of the effect of a 1-day interventional workshop on recovery from job stress for radiation therapists and oncology nurses: a randomised trial. Journal of Medical Imaging and Radiation Oncology 2015;59(4):491-8. [DOI: 10.1111/1754-9485.12322] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schroeder 2016 {published data only}
- Schroeder DA, Stephens E, Colgan D, Hunsinger M, Rubin D, Christopher MS. A brief mindfulness-based intervention for primary care physicians: a pilot randomized controlled trial. American Journal of Lifestyle Medicine 2016;12(1):83-91. [DOI: 10.1177/1559827616629121] [PMC6125016] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2019 {published data only}
- NCT03017469. Achieving resilience in acute care nurses (ARISE) [Achieving resilience in acute care nurses (ARISE): a randomized controlled trial of a multi-component intervention for nurses in critical care and trauma]. clinicaltrials.gov/ct2/show/NCT03017469 (first received 9 January 2017).
- Smith O, Faulkner K, Skiffington A, McShane J, Wan C, Krock M. A randomized controlled trial of an intervention to enhance resilience in acute care nurses (ARISE). Critical Care Medicine 2019;47(1):35. [DOI: 10.1097/01.ccm.0000550861.59004.b7] [104] [DOI] [Google Scholar]
Sood 2011 {published data only}
- Sood A, Prasad K, Schroeder D, Varkey P. Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. Journal of General Internal Medicine 2011;26(8):858-61. [DOI: 10.1007/s11606-011-1640-x] [PMC3138987] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sood 2014 {published data only}
- Sood A, Sharma V, Schroeder DR, Gorman B. Stress management and resiliency training (SMART) program among Department of Radiology faculty: a pilot randomized clinical trial. Explore 2014;10(6):358-63. [DOI: 10.1016/j.explore.2014.08.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stetz 2007 {published data only (unpublished sought but not used)}
- Stetz M, Long CP, Wiederhold B, Turner DD. Combat scenarios and relaxation training to harden medics against stress. Journal of CyberTherapy and Rehabilitation 2008;1(3):239-46. [GALE|A225437106] [Google Scholar]
- Stetz MC, Long CP, Schober WV Jr, Cardillo CG, Wildzunas RM. Stress assessment and management while medics take care of the VR wounded. Annual Review of Cybertherapy and Telemedicine 2007;5:165-71. [tinyurl.com/y2lth6bj] [Google Scholar]
Strijk 2011 {published and unpublished data}
- Strijk JE, Proper KI, Van Mechelen W, Van der Beek AJ. Effectiveness of a worksite lifestyle intervention on vitality, work engagement, productivity, and sick leave: results of a randomized controlled trial. Scandinavian Journal of Work, Environment & Health 2013;39(1):66-75. [DOI: 10.5271/sjweh.3311] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Strijk JE, Proper KI, Van der Beek AJ, Van Mechelen W. A process evaluation of a worksite vitality intervention among ageing hospital workers. International Journal of Behavioral Nutrition and Physical Activity 2011;8:58. [DOI: 10.1186/1479-5868-8-58] [PMC3127968] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strijk JE, Proper KI, Van der Beek AJ, Van Mechelen W. A worksite vitality intervention to improve older workers’ lifestyle and vitality-related outcomes: results of a randomised controlled trial. Journal of Epidemiology and Community Health 2012;66(11):1071-8. [DOI: 10.1136/jech-2011-200626] [PMC3465836] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tierney 1997 {published data only}
- Tierney MJ, Lavelle M. An investigation into modification of personality hardiness in staff nurses. Journal of Nursing Staff Development 1997;13(4):212-7. [PMID: ] [PubMed] [Google Scholar]
Varker 2012 {published data only (unpublished sought but not used)}
- Varker T, Devilly GJ. An analogue trial of inoculation/resilience training for emergency services personnel: proof of concept. Journal of Anxiety Disorders 2012;26(6):696-701. [DOI: 10.1016/j.janxdis.2012.01.009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Villani 2013 {published and unpublished data}
- Villani D, Grassi A, Cognetta C, Toniolo D, Cipresso P, Riva G. Self-help stress management training through mobile phones: an experience with oncology nurses. Psychological Services 2013;10(3):315-22. [DOI: 10.1037/a0026459] [PMID: ] [DOI] [PubMed] [Google Scholar]
West 2014 {published and unpublished data}
- West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Internal Medicine 2014;174(4):527-33. [DOI: 10.1001/jamainternmed.2013.14387] [PMID: ] [DOI] [PubMed] [Google Scholar]
West 2015 {published and unpublished data}
- West CP, Dyrbye LN, Satele D, Shanafelt T. A randomized controlled trial evaluating the effect of COMPASS (colleagues meeting to promote and sustain satisfaction) small group sessions on physician well-being, meaning, and job satisfaction. Journal of General Internal Medicine 2015;30 Suppl 2:S89. [DOI: 10.1007/s11606-015-3271-0] [DOI] [Google Scholar]
Wild 2016 {published data only (unpublished sought but not used)}
- Wild J. An Evaluation of Mind's Resilience Intervention for Emergency Workers; May 2016. www.mind.org.uk/media-a/4591/strand-3.pdf .
References to studies excluded from this review
Bian 2011 {published data only}
- Bian Y, Xiong H, Zhang L, Tang T, Liu Z, Xu R, et al. Change in coping strategies following intensive intervention for special-service military personnel as civil emergency responders. Journal of Occupational Health 2011;53(1):36-44. [DOI: 10.1539/joh.o10009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chang 2008 {published data only}
- Chang RR. Critical Incident Stress Debriefing and the Effect of Timing of Intervention on First Responders: A Preliminary Study [PhD thesis]. Lincoln (NE): University of Nebraska-Lincoln, 2008. [Google Scholar]
Dyrbye 2016 {published data only}
- Dyrbye LN, West CP, Richards ML, Ross HJ, Satele D, Shanafelt TD. A randomized, controlled study of an online intervention to promote job satisfaction and well-being among physicians. Burnout Research 2016;3(3):69-75. [DOI: 10.1016/j.burn.2016.06.002] [DOI] [Google Scholar]
- NCT01643694. Individualized electronic intervention to promote work engagement [Randomized controlled trial evaluating the effect of an individualized electronic intervention to promote resilience, meaning, and engagement for physicians]. clinicaltrials.gov/ct2/show/NCT01643694 (first received 27 June 2012).
Imamura 2019 {published data only}
- Imamura K, Tran TT, Nguyen HT, Kuribayashi K, Sakuraya A, Nguyen AQ, et al. Effects of two types of smartphone-based stress management programmes on depressive and anxiety symptoms among hospital nurses in Vietnam: a protocol for three-arm randomised controlled trial. BMJ Open 2019;9(4):e025138. [DOI: 10.1136/bmjopen-2018-025138] [PMC6500319 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lahn 2014 {published data only}
- Lahn MJ. Indices of Heart Rate Variability and Compassion in Healthcare Professionals Following Stress Resilience Training [PhD thesis]. Oakland (CA): Saybrook University, 2014. [Google Scholar]
Maunder 2010 {published data only}
- Maunder RG, Lancee WJ, Mae R, Vincent L, Peladeau N, Beduz MA, et al. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Services Research 2010;10:72. [DOI: 10.1186/1472-6963-10-72] [PMC2851711] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02417051 {published data only}
- NCT02417051. The efficacy of a brief resilience training program for hurricane Sandy disaster responders. clinicaltrials.gov/ct2/show/NCT02417051 (first received 10 April 2015).
NCT03753360 {published data only}
- NCT03753360. Online mindfulness program for stress management (IGEM) [Immunological and genomic effects of an online mindfulness program for stress management]. clinicaltrials.gov/ct2/show/NCT03753360 (first received 20 November 2018).
NCT03914898 {published data only}
- NCT03914898. Effect of nurse-led intervention programme professional quality of life and psychological distress in nurses [Effect of nurse-led intervention programme on compassion fatigue, burnout, compassion]. clinicaltrials.gov/show/nct03914898 (first received 8 April 2019).
Rowe 1999 {published data only}
- Rowe MM. Four-year longitudinal study of behavioral changes in coping with stress. American Journal of Health Behavior 2006;30(6):602-12. [DOI: 10.5555/ajhb.2006.30.6.602] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Rowe MM. Skills training in the long-term management of stress and occupational burnout. Current Psychology 2000;19(3):215–28. [DOI: 10.1007/s12144-000-1016-6] [DOI] [Google Scholar]
- Rowe MM. Teaching health-care providers coping: results of a two-year study. Journal of Behavioral Medicine 1999;22(5):511-27. [DOI: 10.1023/a:1018661508593] [PMID: ] [DOI] [PubMed] [Google Scholar]
Speckens 2019 {published data only}
- Speckens A, Verweij H, Van Ravesteijn H, Lagro-Janssen T. Mindfulness for medical, surgical and psychiatric residents [Mindfulness voor artsen in opleidingtot medisch specialist]. Tijdschrift voor Psychiatrie 2019;61(3):188-93. [PMID: ] [PubMed] [Google Scholar]
Strauss 2018 {published data only}ISRCTN11723441
- Strauss C, Gu J, Pitman N, Chapman C, Kuyken W, Whittington A. Evaluation of mindfulness-based cognitive therapy for life and a cognitive behavioural therapy stress-management workshop to improve healthcare staff stress: study protocol for two randomised controlled trials. Trials 2018;19(1):209. [DOI: 10.1186/s13063-018-2547-1] [PMC5879876] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Watanabe 2019 {published data only}
- Watanabe N, Horikoshi M, Shinmei I, Oe Y, Narisawa T, Kumachi M, et al. Brief mindfulness-based stress management program for a better mental state in working populations - Happy Nurse Project: a randomized controlled trial. Journal of Affective Disorders 2019;251:186-94. [DOI: 10.1016/j.jad.2019.03.067] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Almén 2020 {published data only}
- Almén N, Lisspers J, Öst LG, Sundin Ö. Behavioral stress recovery management intervention for people with high levels of perceived stress: a randomized controlled trial. International Journal of Stress Management 2020;27(2):183–94. [DOI: 10.1037/str0000140] [DOI] [Google Scholar]
Aranda Auserón 2018 {published data only}
- Aranda Auserón G, Elcuaz Viscarret MR, Fuertes Goñi C, Güeto Rubio V, Pascual Pascual P, Sainz de Murieta García de Galdeano E. Evaluation of the effectiveness of a mindfulness and self-compassion program to reduce stress and prevent burnout in primary care health professionals [Evaluación de la efectividad de un programa de mindfulness y autocompasión para reducir el estrés y prevenir el burnout en profesionales sanitarios de atención primaria]. Atencion Primaria 2018;50(3):141-50. [DOI: 10.1016/j.aprim.2017.03.009] [PMC6836985] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chesak 2019a {published data only}
- Chesak SS, Morin KH, Cutshall S, Carlson M, Joswiak ME, Ridgeway JL, et al. Stress Management and Resiliency Training in a nurse residency program: findings from participant focus groups. Journal for Nurses in Professional Development 2019;35(6):337-43. [DOI: 10.1097/NND.0000000000000589] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dyrbye 2019 {published data only}
- Dyrbye LN, Shanafelt TD, Gill PR, Satele DV, West CP. Effect of a professional coaching intervention on the well-being and distress of physicians: a pilot randomized clinical trial. JAMA Intern Med 2019;179(10):1406-14. [DOI: 10.1001/jamainternmed.2019.2425] [PMC6686971] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grabbe 2020 {published data only}
- Grabbe L, Higgins MK, Baird M, Craven PA, San Fratello S. The Community Resiliency Model® to promote nurse well-being. Nursing Outlook 2020;68(3):324-36. [DOI: 10.1016/j.outlook.2019.11.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Heath 2020 {published data only}
- Heath J, Walmsley LA, Aker RM, Ferrin S, Stone D, Norton JC. CPR to the Rescue! An interprofessional pilot program Cultivating Practices for Resilience (CPR) camp. Clinical Nurse Specialist 2020;34(2):63-9. [DOI: 10.1097/NUR.0000000000000506] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kim 2018a {published data only}
- Kim JI, Yun JY, Park H, Park SY, Ahn Y, Lee H, et al. A mobile videoconference-based intervention on stress reduction and resilience enhancement in employees: randomized controlled trial. Journal of Medical Internet Research 2018;20(10):e10760. [DOI: 10.2196/10760] [PMC6234345] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT03256682. The efficacy of mobile video counseling for employees with emotional labor [The efficacy of mobile video counseling targeted for stress reduction and resilience enhancement in employees with emotional labor]. clinicaltrials.gov/show/nct03256682 (first received 18 August 2017).
Mainwaring 2018 {published data only}
- Mainwaring J. Implementation of a mindfulness-based resilience practice for anesthesia providers. In: AANA (American Association of Nurse Anesthetists) 2018 Annual Congress; 2018 Sep 21-25; Boston (MA). 2018.
Moffatt‐Bruce 2019 {published data only}
- Moffatt-Bruce SD, Nguyen MC, Steinberg B, Holliday S, Klatt M. Interventions to reduce burnout and improve resilience: impact on a health system's outcomes. Clinical Obstetrics and Gynecology 2019;62(3):432-43. [DOI: 10.1097/GRF.0000000000000458] [PMID: ] [DOI] [PubMed] [Google Scholar]
NCT03613441 {published data only}
- NCT03613441. Impact of mindful awareness practices in pediatric residency training. clinicaltrials.gov/show/nct03613441 (first received 3 August 2018).
NCT03781336 {published data only}
- NCT03781336. Brief mindfulness meditation course to reduce stress in healthcare professionals [Brief mindfulness meditation course to reduce stress in healthcare professionals and trainees: a randomized clinical trial]. clinicaltrials.gov/ct2/show/NCT03781336 (first received 18 December 2018).
NCT04368676 {published data only}
- NCT04368676. Breath regulation and yogic exercise on online therapy for calm and happiness (BREATH). clinicaltrials.gov/show/nct04368676 (first received 30 April 2020).
NCT04372303 {published data only}
- NCT04372303. Effect of a compassion fatigue resiliency program. clinicaltrials.gov/show/nct04372303 (first received 4 May 2020).
NCT04373382 {published data only}
- NCT04373382. Peer champion support for hospital staff during and after the COVID-19 pandemic. clinicaltrials.gov/show/nct04373382 (first received 4 May 2020).
NCT04384861 {published data only}
- NCT04384861. Improving physician empathy, compassionate care and wellness. clinicaltrials.gov/show/nct04384861 (first received 12 May 2020).
Ouyang 2017 {published data only}
- Ouyang M, Yu Z, Hao Y. Effect of professional training combined with positive psychological intervention for reducing mental crisis of primary nurses [专业培训联合积极心理学干预减轻初责护士心理危机的效果]. Huli Yanjiu (Chinese Nursing Research) 2017;31(21):2585-8. [DOI: 10.3969/j.issn.1009-6493.2017.21.008] [DOI] [Google Scholar]
Rodgers 2018 {published data only}
- Rodgers RK. Mental and emotional self-management: an examination of psychological and physiological outcomes [PhD thesis]. Claremont (CA): Claremont Graduate University, 2018. [Google Scholar]
Ruehl 2013 {published data only}
- Ruehl BD. The Psychological and Physical Health Effects of Written Emotional Expression in Pediatric Hematology/Oncology, Intensive Care, and Neonatal Intensive Care Nursing Staff [PhD thesis]. San Diego (CA): Alliant International University, 2013. [Google Scholar]
Van Berkel 2014 {published data only}
- Van Berkel J, Boot CR, Proper KI, Bongers PM, Van der Beek AJ. Effectiveness of a worksite mindfulness-based multi-component intervention on lifestyle behaviors. International Journal of Behavioral Nutrition and Physical Activity 2014;11:9. [DOI: 10.1186/1479-5868-11-9] [PMC3905927] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Berkel J, Boot CR, Proper KI, Bongers PM, Van der Beek AJ. Effectiveness of a worksite mindfulness-related multi-component health promotion intervention on work engagement and mental health: results of a randomized controlled trial. PLoS ONE 2014;9(1):e84118. [DOI: 10.1371/journal.pone.0084118] [PMC3904825] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yeo 2019 {published data only}
- Yeo, CJJ, Barbieri A, Roman G, Wiesman J, Powell S. Using smartphone mindfulness apps to increase trainee resilience and reduce burnout. Neurology 2019;92(15 Suppl):P2.9-005. [DOI: No DOI available] [https://n.neurology.org/content/92/15_Supplement/P2.9-005.abstract] [Google Scholar]
References to ongoing studies
ACTRN12617000290392 {published data only}
- ACTRN12617000290392. Doctors Working Well: a study evaluating an online stress management program for doctors [A randomised controlled trial of an online intervention on resiliency, occupational stress, and burnout among junior medical doctors]. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=372318 (first received 24 February 2017).
JPRN UMIN000031435 {published data only}
- JPRN-UMIN000031435. Mindfulness for health professionals building resilience and compassion (MHALO program) - randomized control trial. who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000031435 (first received 23 February 2018).
NCT03518359 {published data only}
- NCT03518359. Enhanced stress resilience training for residents (ESRT-R) [Enhanced resilience training to improve mental health, stress and performance in resident physicians]. clinicaltrials.gov/ct2/show/NCT03518359 (first received 24 April 2018).
NCT03645512 {published data only}
- NCT03645512. Resilience intervention for critical care nurses [A randomized controlled trial of a resilience intervention for critical care nurses]. clinicaltrials.gov/ct2/show/NCT03645512 (first received 21 August 2018).
NCT03759795 {published data only}
- NCT03759795. Bournemouth University Resilience Training for Surgeons (BURTS) [Ameliorating the impact of complications and errors on surgeons: resilience training for surgeons]. clinicaltrials.gov/ct2/show/NCT03759795 (first received 13 November 2018).
Additional references
Abbott 2009
- Abbott J-A, Klein B, Hamilton C, Rosenthal A. The impact of online resilience training for sales managers on wellbeing and performance. E-Journal of Applied Psychology 2009;5(1):89-95. [DOI: 10.7790/ejap.v5i1.145] [DOI] [Google Scholar]
Abel 2002a
- Abel MH. Humor, stress, and coping strategies. Humor: International Journal of Humor Research 2002;15(4):365–81. [DOI: 10.1515/humr.15.4.365] [DOI] [Google Scholar]
Abel 2002b
- Abel MH, Maxwell D. Humor and effective consequences of a stressful task. Journal of Social and Clinical Psychology 2002;21(2):165-90. [DOI: 10.1521/jscp.21.2.165.22516] [DOI] [Google Scholar]
Abidin 1990
- Abidin RR. Parenting Stress Index (PSI). Charlottesville (VA): Pediatric Psychology Press, 1990. [Google Scholar]
Adams 2006
- Adams RE, Boscarino JA, Figley CR. Compassion fatigue and psychological distress among social workers: a validation study. American Journal of Orthopsychiatry 2006;76(1):103–8. [DOI: 10.1037/0002-9432.76.1.103] [PMC2699394] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Adriaenssens 2011
- Adriaenssens J, De Gucht V, Van der Doef M, Maes S. Exploring the burden of emergency care: predictors of stress‐health outcomes in emergency nurses. Journal of Advanced Nursing 2011;67(6):1317– 28. [DOI: 10.1111/j.1365-2648.2010.05599.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Adriaenssens 2015
- Adriaenssens J, De Gucht V, Maes S. Causes and consequences of occupational stress in emergency nurses, a longitudinal study. Journal of Nursing Management 2015;23(3):346–58. [DOI: 10.1111/jonm.12138] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ahern 2004
- Ahern J, Galea S, Fernandez WG, Koci B, Waldman R, Vlahov D. Gender, social support, and posttraumatic stress in postwar Kosovo. Journal of Nervous and Mental Disease 2004;192(11):762-70. [DOI: 10.1097/01.nmd.0000144695.02982.41] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ahmad 2010
- Ahmad S, Feder A, Lee EJ, Wang Y, Southwick SM, Schlackman E, et al. Earthquake impact in a remote South Asian population: psychosocial factors and posttraumatic symptoms. Journal of Traumatic Stress 2010;23(3):408-12. [DOI: 10.1002/jts.20535] [PMID: ] [DOI] [PubMed] [Google Scholar]
Aiken 2001
- Aiken LH, Clarke SP, Sloane DM, Sochalski JA, Busse R, Clarke H, et al. Nurses' reports on hospital care in five countries. Health Affairs 2001;20(3):43–53. [DOI: 10.1377/hlthaff.20.3.43] [PMID: ] [DOI] [PubMed] [Google Scholar]
Al‐Yagon 2009
- Al-Yagon M, Margalit M. Positive and negative affect among mothers of children with intellectual disabilities. British Journal of Developmental Disabilities 2009;55(109):109-27. [DOI: 10.1179/096979509799103070] [DOI] [Google Scholar]
Alessandri 2007
- Alessandri G, Vecchio GM, Steca P, Caprara MG, Caprara GV. A revised version of Kremen and Block's Ego Resiliency Scale in an Italian sample. TPM-Testing, Psychometrics, Methodology in Applied Psychology 2007;14(3-4):165-83. [www.tpmap.org/wp-content/uploads/2014/11/14.3.4.pdf] [Google Scholar]
Alexander 2001
- Alexander DA, Klein S. Ambulance personnel and critical incidents: impact of accident and emergency work on mental health and emotional well-being. British Journal of Psychiatry 2001;178(1):76-81. [DOI: 10.1192/bjp.178.1.76] [PMID: ] [DOI] [PubMed] [Google Scholar]
Alexander 2019 [pers comm]
- Alexander G. Potential withdrawals/exclusions in the study and number of participants analysed [personal communication]. Email to: A Kunzler 5 September 2019.
Alim 2008
- Alim TN, Feder A, Graves RE, Wang Y, Weaver J, Westphal M, et al. Trauma, resilience, and recovery in a high-risk African-American population. American Journal of Psychiatry 2008;165(12):1566-75. [DOI: 10.1176/appi.ajp.2008.07121939] [PMID: ] [DOI] [PubMed] [Google Scholar]
Allart 2013
- Allart P, Soubeyran P, Cousson-Gélie F. Are psychosocial factors associated with quality of life in patients with haematological cancer? A critical review of the literature. Psycho-Oncology 2013;22(2):241-9. [DOI: 10.1002/pon.3026] [PMID: ] [DOI] [PubMed] [Google Scholar]
Allen 2010
- Allen B, Brymer MJ, Steinberg AM, Vernberg EM, Jacobs A, Speier AH, et al. Perceptions of psychological first aid among providers responding to hurricanes Gustav and Ike. Journal of Traumatic Stress 2010;23(4):509-13. [DOI: 10.1002/jts.20539] [PMID: ] [DOI] [PubMed] [Google Scholar]
Anderson 2017
- Anderson JC, Pfeil S, Surawicz C. Strategies to combat physician burnout in gastroenterology. American Journal of Gastroenterology 2017;112(9):1356–9. [DOI: 10.1038/ajg.2017.251] [PMID: ] [DOI] [PubMed] [Google Scholar]
Andresen 1994
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventive Medicine 1994;10(2):77-84. [PMID: ] [PubMed] [Google Scholar]
Andrew 2008
- Andrew ME, McCanlies EC, Burchfiel CM, Charles LE, Hartley TA, Fekedulegn D, et al. Hardiness and psychological distress in a cohort of police officers. International Journal of Emergency Mental Health 2008;10(2):137-47. [PMID: ] [PubMed] [Google Scholar]
Aniţei 2012
- Aniţei M, Chraif M, Chiriac G. Resilience to stress evidence-based improvements in integrative psychotherapy working groups. Procedia - Social and Behavioral Sciences 2012;33:1042-6. [DOI: 10.1016/j.sbspro.2012.01.281] [DOI] [Google Scholar]
Ano 2005
- Ano GG, Vasconcelles EB. Religious coping and psychological adjustment to stress: a meta-analysis. Journal of Clinical Psychology 2005;61(4):461-80. [DOI: 10.1002/jclp.20049] [PMID: ] [DOI] [PubMed] [Google Scholar]
Antonovsky 1979
- Antonovsky A. Health, Stress and Coping: New Perspectives on Mental and Physical Well-being. San Francisco (CA): Jossey-Bass, 1979. [Google Scholar]
Antonovsky 1987
- Antonovsky A. Unraveling the mystery of health: how people manage stress and stay well. San Francisco: Jossey-Bass, 1997. [Google Scholar]
Arnetz 1985
- Arnetz BB, Fjellner B, Eneroth P, Kallner A. Stress and psoriasis: psychoendocrine and metabolic reactions in psoriatic patients during standardized stressor exposure. Psychosomatic Medicine 1985;47(6):528–41. [DOI: 10.1097/00006842-198511000-00003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Atal 2016
- Atal S, Cheng C. Socioeconomic health disparities revisited: coping flexibility enhances health-related quality of life for individuals low in socioeconomic status. Health and Quality of Life Outcomes 2016;14:7. [DOI: 10.1186/s12955-016-0410-1] [PMC4709869] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Atri 2007a
- Atri A. Role of Social Support, Hardiness and Acculturation as Predictors of Mental Health Among the International Students of Asian Indian Origin in Ohio [MS thesis]. Cincinnati (OH): University of Cincinnati, 2007. [DOI] [PubMed] [Google Scholar]
Atri 2007b
- Atri A, Sharma M, Cottrell R. Role of social support, hardiness, and acculturation as predictors of mental health among international students of Asian Indian origin. International Quarterly of Community Health Education 2007;27(1):59-73. [DOI: 10.2190/IQ.27.1.e] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bailey 2013
- Bailey A, Sharma M, Jubin M. The mediating role of social support, cognitive appraisal, and quality health care in black mothers' stress-resilience process following loss to gun violence. Violence and Victims 2013;28(2):233-47. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bakker 2005
- Bakker A, Demerouti E, Euwema M. Job resources buffer the impact of job demands on burnout. Journal of Occupational Health Psychology 2005;10(2):170–80. [DOI: 10.1037/1076-8998.10.2.170] [DOI] [PubMed] [Google Scholar]
Bakker 2007
- Bakker AB, Demerouti E. The Job Demands-Resources model: state of the art. Journal of Managerial Psychology 2007;22(3):309–28. [DOI: 10.1108/02683940710733115] [DOI] [Google Scholar]
Balduzzi 2019
- Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evidence-Based Mental Health 2019;22(4):153-60. [DOI: 10.1136/ebmental-2019-300117] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bamberger 1999
- Bamberger GG. Lösungsorientierte Beratung. Weinheim (DE): Beltz, 1999. [Google Scholar]
Bandura 1997
- Bandura A. Self-Efficacy: The Exercise of Control. New York (NY): WH Freeman & Company, 1997. [Google Scholar]
Barry 2003
- Barry LC, Guo Z, Kerns RD, Duong BD, Reid MC. Functional self-efficacy and pain-related disability among older veterans with chronic pain in a primary care setting. Pain 2003;104(1-2):131-7. [DOI: 10.1016/S0304-3959(02)00471-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bartone 1989
- Bartone PT, Ursano RJ, Wright KM, Ingraham LH. The impact of a military air disaster on the health of assistance workers: a prospective study. Journal of Nervous and Mental Disease 1989;177(6):317-28. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bauer 2018
- Bauer A, Newbury-Birch D, Robalino S, Ferguson J, Wigham S. Is prevention better than cure? A systematic review of the effectiveness of well-being interventions for military personnel adjusting to civilian life. PLoS ONE 2018;13(5):e0190144. [DOI: 10.1371/journal.pone.0190144] [PMC5931793] [PROSPERO registration number: CRD42015026341.] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bauer‐Wu 2005
- Bauer-Wu S, Farran CJ. Meaning in life and psycho-spiritual functioning: a comparison of breast cancer survivors and healthy women. Journal of Holistic Nursing 2005;23(2):172-90. [DOI: 10.1177/0898010105275927] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bech 2003
- Bech P, Olsen LR, Kjoller M, Rasmussen NK. Measuring well-being rather than the absence of distress symptoms: a comparison of the SF-36 Mental Health subscale and the WHO-Five Well-Being Scale. International Journal of Methods in Psychiatric Research 2003;12(2):85-91. [DOI: 10.1002/mpr.145] [PMC6878541] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4(6):561-71. [PMID: ] [DOI] [PubMed] [Google Scholar]
Beck 1964
- Beck AT. Thinking and depression. II. Theory and therapy. Archives of General Psychiatry 1964;10(6):561-71. [DOI: 10.1001/archpsyc.1964.01720240015003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beck 1972
- Beck AT, Beck RW. Screening depressed patients in family practice: a rapid technique. Postgraduate Medicine 1972;52(6):81–5. [DOI: 10.1080/00325481.1972.11713319] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beck 1976
- Beck AT. Cognitive Therapy and the Emotional Disorders. New York (NY): International Universities Press, 1976. [Google Scholar]
Beck 1993
- Beck AT, Steer RA. Beck Anxiety Inventory Manual. San Antonio (TX): Psychological Corporation, 1993. [Google Scholar]
Beck 1996
- Beck AT, Steer RA, Brown G. Manual for the Beck Depression Inventory-II. San Antonio (TX): Psychological Corporation, 1996. [Google Scholar]
Beck 2011
- Beck JS. Cognitive Behavior Therapy. Basics and Beyond. Second edition. New York (NY): The Guilford Press, 2011. [Google Scholar]
Bekki 2013
- Bekki JM, Smith ML, Bernstein B, Harrison C. Effects of an online personal resilience training program for women in STEM doctoral programs. Journal of Women and Minorities in Science and Engineering 2013;19(1):17-35. [DOI: 10.1615/JWomenMinorScienEng.2013005351] [DOI] [Google Scholar]
Bengel 2009
- Bengel J, Meinders-Lücking F, Rottmann N. Schutzfaktoren bei Kindern und Jugendlichen: Stand der Forschung zu Psychosozialen Schutzfaktoren für Gesundheit. Köln: BzgA, 2009. [Google Scholar]
Bengel 2012
- Bengel J, Lyssenko L. Resilienz und Psychologische Schutzfaktoren im Erwachsenenalter. Köln: BzgA, 2012. [Google Scholar]
Benjamin 2011
- Benjamin CL, Puleo CM, Settipani CA, Brodman DM, Edmunds JM, Cummings CM, et al. History of cognitive-behavioral therapy in youth. Child and Adolescent Psychiatric Clinics of North America 2011;20(2):179-89. [DOI: 10.1016/j.chc.2011.01.011] [PMC3077930] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Benson 2000
- Benson H, Klipper MZ. The Relaxation Response. New York (NY): HarperCollins, 2000. [Google Scholar]
Berger 2007
- Berger R, Pat-Horencyk R, Gelkopf M. School-based intervention for prevention and treatment of elementary-students' terror-related distress in Israel: quasi-randomized controlled trial. Journal of Traumatic Stress 2007;20(4):541–51. [DOI: 10.1002/jts.20225] [PMID: 17721962 ] [DOI] [PubMed] [Google Scholar]
Berk 2009
- Berk M, Parker G. The elephant on the couch: side-effects of psychotherapy. Australian and New Zealand Journal of Psychiatry 2009;43(9):787–94. [DOI: 10.1080/00048670903107559] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bernas 2000
- Bernas KH, Major DA. Contributors to stress resistance: testing a model of women's work-family conflict. Psychology of Women Quarterly 2000;24(2):170-8. [DOI: 10.1111/j.1471-6402.2000.tb00198.x] [DOI] [Google Scholar]
Besser 2014
- Besser A, Weinberg M, Zeigler-Hill V, Neria Y. Acute symptoms of posttraumatic stress and dissociative experiences among female Israeli civilians exposed to war: the roles of intrapersonal and interpersonal sources of resilience. Journal of Clinical Psychology 2014;70(12):1227-39. [DOI: 10.1002/jclp.22083] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bishop 2004
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, et al. Mindfulness: a proposed operational definition. Clinical Psychology: Science and Practice 2004;11(3):230-41. [DOI: 10.1093/clipsy/bph077] [DOI] [Google Scholar]
Bjørkløf 2013
- Bjørkløf GH, Engedal K, Selbak G, Kouwenhoven SE, Helvik AS. Coping and depression in old age: a literature review. Dementia and Geriatric Cognitive Disorders 2013;35(3-4):121-54. [DOI: 10.1159/000346633] [PMID: ] [DOI] [PubMed] [Google Scholar]
Blackburn 2015
- Blackburn L, Owens GP. The effect of self efficacy and meaning in life on posttraumatic stress disorder and depression severity among veterans. Journal of Clinical Psychology 2015;71(3):219-28. [DOI: 10.1002/jclp.22133] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bleich 2003
- Bleich A, Gelkopf M, Solomon Z. Exposure to terrorism, stress-related mental health symptoms, and coping behaviors among a nationally representative sample in Israel. JAMA 2003;290(5):612–20. [DOI: 10.1001/jama.290.5.612] [PMID: ] [DOI] [PubMed] [Google Scholar]
Block 1996
- Block J, Kremen AM. IQ and ego-resiliency: conceptual and empirical connections and separateness. Journal of Personality and Social Psychology 1996;70(2):349-61. [PMID: ] [DOI] [PubMed] [Google Scholar]
Boellinghaus 2014
- Boellinghaus I, Jones FW, Hutton J. The role of mindfulness and loving-kindness meditation in cultivating self-compassion and other-focused concern in health care professionals. Mindfulness 2014;5(2):129–38. [DOI: 10.1007/s12671-012-0158-6] [DOI] [Google Scholar]
Bonanno 2004
- Bonanno GA, Papa A, Lalande K, Westphal M, Coifman K. The importance of being flexible: the ability to both enhance and suppress emotional expression predicts long-term adjustment. Psychological Science 2004;15(7):482-7. [DOI: 10.1111/j.0956-7976.2004.00705.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bonanno 2011
- Bonanno GA, Pat-Horenczyk R, Noll J. Coping flexibility and trauma: The Perceived Ability to Cope With Trauma (PACT) scale. Psychological Trauma: Theory, Research, Practice, and Policy 2011;3(2):117-29. [DOI: 10.1037/a0020921] [DOI] [Google Scholar]
Bonanno 2013
- Bonanno GA, Diminich ED. Annual Research Review: positive adjustment to adversity--trajectories of minimal-impact resilience and emergent resilience. Journal of Child Psychology and Psychiatry, and Allied Disciplines 2013;54(4):378-401. [DOI: 10.1111/jcpp.12021] [PMC3606676] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bonanno 2015
- Bonanno GA, Romero SA, Klein SI. The temporal elements of psychological resilience: an integrative framework for the study of individuals, families, and communities. Psychological Inquiry 2015;26(2):139–69. [DOI: 10.1080/1047840X.2015.992677] [DOI] [Google Scholar]
Bookwala 2014
- Bookwala J. Spouse health status, depressed affect, and resilience in mid and late life: a longitudinal study. Developmental Psychology 2014;50(4):1241-9. [DOI: 10.1037/a0035124] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bossé 1991
- Bossé R, Aldwin CM, Levenson MR, Workman-Daniels K. How stressful is retirement? Findings from the Normative Aging Study. Journal of Gerontology 1991;46(1):P9-14. [DOI: 10.1093/geronj/46.1.p9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Brandt 1981
- Brandt PA, Weinert C. The PRQ - a social support measure. Nursing Research 1981;30(5):277-80. [PMID: ] [PubMed] [Google Scholar]
Broderick 2004
- Broderick JE, Stone AA, Smyth JM, Kaell AT. The feasibility and effectiveness of an expressive writing intervention for rheumatoid arthritis via home-based videotaped instructions. Annals of Behavioral Medicine 2004;27(1):50-9. [DOI: 10.1207/s15324796abm2701_7] [DOI] [PubMed] [Google Scholar]
Bromley 2006
- Bromley E, Johnson JG, Cohen P. Personality strengths in adolescence and decreased risk of developing mental health problems in early adulthood. Comprehensive Psychiatry 2006;47(4):315-24. [DOI: 10.1016/j.comppsych.2005.11.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Brooks 2003
- Brooks MV. Health-related hardiness and chronic illness: a synthesis of current research. Nursing Forum 2003;38(3):11-20. [PMID: ] [DOI] [PubMed] [Google Scholar]
Brymer 2006
- Brymer M, Jacobs A, Layne C, Pynoos R, Ruzek J, Steinberg A, et al. Psychological first aid: field operations guide, 2nd edition. www.ptsd.va.gov/professional/treat/type/PFA/PFA_2ndEditionwithappendices.pdf (accessed prior to 10 June 2019). [Available on www.ncptsd.va.gov] [Available on www.nctsn.org ]
Buddeberg‐Fischer 2006
- Buddeberg-Fischer B, Herta KD. Formal mentoring programmes for medical students and doctors--a review of the Medline literature. Medical Teacher 2006;28(3):248-57. [DOI: 10.1080/01421590500313043] [PMID: ] [DOI] [PubMed] [Google Scholar]
Burton 2012
- Burton CL, Yan OH, Pat-Horenczyk R, Chan IS, Ho S, Bonanno GA. Coping flexibility and complicated grief: a comparison of American and Chinese samples. Depression and Anxiety 2012;29(1):16-22. [DOI: 10.1002/da.20888] [PMC3242921] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burton 2017
- Burton A, Burgess C, Dean S, Koutsopoulou GZ, Hugh-Jones S. How effective are mindfulness-based interventions for reducing stress among healthcare professionals? A systematic review and meta-analysis. Stress and Health 2017;33(1):3–13. [DOI: 10.1002/smi.2673] [PMID: ] [DOI] [PubMed] [Google Scholar]
Butler 2009
- Butler LD, Koopman C, Azarow J, Blasey CM, Magdalene JC, DiMiceli S, et al. Psychosocial predictors of resilience after the September 11, 2001 terrorist attacks. Journal of Nervous and Mental Disease 2009;197(4):266-73. [DOI: 10.1097/NMD.0b013e31819d9334] [PMID: ] [DOI] [PubMed] [Google Scholar]
Caldwell 2005
- Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments combining direct and indirect evidence. BMJ 2005;331(7521):897-900. [DOI: 10.1136/bmj.331.7521.897] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cameron 1982
- Cameron R, Meichenbaum D. The nature of effective coping and the treatment of stress related problems: a cognitive-behavioural perspective. In: Goldberg L, Breznitz S, editors(s). Handbook of Stress: Theoretical and Clinical Aspects. New York (NY): Free Press, 1982:695–710. [Google Scholar]
Campbell‐Sills 2007
- Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. Journal of Traumatic Stress 2007;20(6):1019-28. [DOI: 10.1002/jts.20271] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cann 2010
- Cann A, Calhoun LG, Tedeschi RG, Taku K, Vishnevsky T, Triplett KN, et al. A short form of the Posttraumatic Growth Inventory. Anxiety, Stress, and Coping 2010;23(2):127-37. [DOI: 10.1080/10615800903094273] [PMID: ] [DOI] [PubMed] [Google Scholar]
Car 2018
- Car LT, Kyaw BM, Atun R. The role of eLearning in health management and leadership capacity building in health system: a systematic review. Human Resources for Health 2018;16(1):44. [DOI: 10.1186/s12960-018-0305-9] [PMC6122658 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carmody 2009
- Carmody J, Baer RA. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology 2009;65(6):627-38. [DOI: 10.1002/jclp.20555] [PMID: ] [DOI] [PubMed] [Google Scholar]
Carrieri 2018
- Carrieri D, Briscoe S, Jackson M, Mattick K, Papoutsi C, Pearson M, et al. 'Care under pressure': a realist review of interventions to tackle doctors' mental ill-health and its impacts on the clinical workforce and patient care. BMJ Open 2018;8(2):e021273. [DOI: 10.1136/bmjopen-2017-021273] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carver 1989
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of Personality and Social Psychology 1989;56(2):267-83. [DOI: 10.1037//0022-3514.56.2.267] [PMID: ] [DOI] [PubMed] [Google Scholar]
Carver 1997
- Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. International Journal of Behavioural Medicine 1997;4(1):92-100. [DOI: 10.1207/s15327558ijbm0401_6] [PMID: ] [DOI] [PubMed] [Google Scholar]
Carver 2010
- Carver CS, Scheier MF, Segerstrom SC. Optimism. Clinical Psychology Review 2010;30(7):879-89. [DOI: 10.1016/j.cpr.2010.01.006] [NIHMS174994] [PMC4161121] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Casale 2013
- Casale M, Wild L. Effects and processes linking social support to caregiver health among HIV/AIDS-affected carer-child dyads: a critical review of the empirical evidence. AIDS and Behavior 2013;17(5):1591-611. [DOI: 10.1007/s10461-012-0275-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chaimani 2019
- Chaimani A, Caldwell DM, Li T, Higgins JP, Salanti G. Chapter 11: Undertaking network meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Chan 2013a
- Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Annals of Internal Medicine 2013;158(3):200-7. [DOI: 10.7326/0003-4819-158-3-201302050-00583] [PMC5114123] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chan 2013b
- Chan AW, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. [DOI: 10.1136/bmj.e7586] [PMC3541470] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2004
- Chen G, Goddard TG, Casper WJ. Examination of the relationships among general and work-specific self-evaluations, work-related control beliefs, and job attitudes. Applied Psychology 2004;53(3):349-70. [DOI: 10.1111/j.1464-0597.2004.00175.x] [DOI] [Google Scholar]
Cheng 2014
- Cheng C, Lau HP, Chan MP. Coping flexibility and psychological adjustment to stressful life changes: a meta-analytic review. Psychological Bulletin 2014;140(6):1582-607. [DOI: 10.1037/a0037913] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chesak 2019b
- Chesak SS, Cutshall SM, Bowe CL, Montanari KM, Bhagra A. Stress management interventions for nurses: critical literature review. Journal of Holistic Nursing 2019;37(3):288–95. [DOI: 10.1177/0898010119842693] [DOI] [PubMed] [Google Scholar]
Chesney 2003
- Chesney MA, Chambers DB, Taylor JM, Johnson LM, Folkman S. Coping effectiveness training for men living with HIV: results from a randomized clinical trial testing a group-based intervention. Psychosomatic Medicine 2003;65(6):1038-46. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chmitorz 2018
- Chmitorz A, Kunzler A, Helmreich I, Tüscher O, Kalisch R, Kubiak T, et al. Intervention studies to foster resilience - a systematic review and proposal for a resilience framework in future intervention studies. Clinical Psychology Review 2018;59:78-100. [DOI: 10.1016/j.cpr.2017.11.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cicchetti 2012
- Cicchetti D, Rogosch FA. Gene x environment interaction and resilience: effects of child maltreatment and serotonin, corticotropin releasing hormone, dopamine, and oxytocin genes. Development and Psychopathology 2012;24(2):411-27. [DOI: 10.1017/S0954579412000077] [PMC3684053] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cieslak 2013
- Cieslak R, Shoji K, Luszczynska A, Taylor S, Rogala A, Benight CC. Secondary trauma self-efficacy: concept and its measurement. Psychological Assessment 2013;25(3):917–28. [DOI: 10.1037/a0032687] [PMID: ] [DOI] [PubMed] [Google Scholar]
CIPSRT 2016
- Canadian Institute for Public Safety Research and Treatment. Peer support and crisis-focused psychological intervention programs in Canadian first responders: blue paper. www.justiceandsafety.ca/rsu_docs/blue_paper_full_web_final_production_aug_16_2016.pdf (accessed 21 April 2020).
Cleary 2018
- Cleary M, Kornhaber R, Thapa, DK, West S, Visentin D. The effectiveness of interventions to improve resilience among health professionals: a systematic review. Nurse Education Today 2018;71:247-63. [DOI: 10.1016/j.nedt.2018.10.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cochran 2017
- Cochran C. Effectiveness and best practice of nurse residency programs: a literature review. Medsurg Nursing 2017;26(1):53-7. [PMID: ] [PubMed] [Google Scholar]
Cochrane Community 2020
- Cochrane Community. Glossary. community.cochrane.org/glossary (accessed 22 May 2020).
Cohen 1983a
- Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology 1983;13(2):99-125. [DOI: 10.1111/j.1559-1816.1983.tb02325.x] [DOI] [Google Scholar]
Cohen 1983b
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior 1983;24(4):385-96. [DOI: 10.2307/2136404] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cohen 1985
- Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors(s). Social Support: Theory, Research and Application. Dordrecht (NL): Martinus Nijhoff, 1985:73–94. [DOI: 10.1007/978-94-009-5115-0_5] [DOI] [Google Scholar]
Cohen 1988a
- Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan, S, Oskamp, S, editors(s). The Social Psychology of Health. Newbury Park (CA): Sage, 1988. [Google Scholar]
Cohen 1988b
- Cohen J. Statistical power analysis in the behavioral sciences. 2nd edition. Hillsdale (NJ): Lawrence Erlbaum Associates, Inc., 1988. [Google Scholar]
Cohen 1992
- Cohen J. A power primer. Psychological Bulletin 1992;112(1):155–9. [DOI: 10.1037/0033-2909.112.1.155] [DOI] [PubMed] [Google Scholar]
Cohen 1994
- Cohen S. Perceived Stress Scale. www.mindgarden.com/documents/PerceivedStressScale.pdf (accessed 21 April 2020).
Cohen 2003
- Cohen O, Savaya R. Sense of coherence and adjustment to divorce among Muslim Arab citizens of Israel. European Journal of Personality 2003;17(4):309-26. [DOI: 10.1002/per.493] [DOI] [Google Scholar]
Cohen 2006
- Cohen S, Alper CM, Doyle WJ, Treanor JJ, Turner RB. Positive emotional style predicts resistance to illness after experimental exposure to rhinovirus or influenza a virus. Psychosomatic Medicine 2006;68(6):809-15. [DOI: 10.1097/01.psy.0000245867.92364.3c] [PMID: ] [DOI] [PubMed] [Google Scholar]
Concilio 2019
- Concilio L, Lockhart JS, Oermann MH, Kronk R, Schreiber JB. Newly licensed nurse resiliency and interventions to promote resiliency in the first year of hire: an integrative review. Journal of Continuing Education in Nursing 2019;50(4):153-61. [DOI: 10.3928/00220124-20190319-05] [DOI] [Google Scholar]
Connor 2003
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety 2003;18(2):76-82. [DOI: 10.1002/da.10113] [PMID: ] [DOI] [PubMed] [Google Scholar]
Connor 2006
- Connor KM, Zhang W. Resilience: determinants, measurement, and treatment responsiveness. CNS Spectrums 2006;11(Suppl S12):5-12. [DOI: 10.1017/S1092852900025797] [DOI] [PubMed] [Google Scholar]
CRD 2009
- Centre for Reviews and Dissemination (CRD). Systematic Reviews: CRD's Guidance for Undertaking Reviews in Health Care. York (NYS): Univesity of York, 2009. [Google Scholar]
Cruz 2016
Cuijpers 2017
- Cuijpers P, Kleiboer A, Karyotaki E, Riper H. Internet and mobile interventions for depression: opportunities and challenges. Depression and Anxiety 2017;34(7):596-602. [DOI: 10.1002/da.22641] [PMID: 28471479 ] [DOI] [PubMed] [Google Scholar]
Cushway 1996
- Cushway D, Tyler PA, Nolan P. Development of a stress scale for mental health professionals. British Journal of Clinical Psychology 1996;35(2):279-95. [DOI: 10.1111/j.2044-8260.1996.tb01182.x] [DOI] [PubMed] [Google Scholar]
Cutrona 1987
- Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. In: Jones WH, Perlman D, editors(s). Advances in Personal Relationships. Greenwich (CT): JAI Press, 1987:37-67. [Google Scholar]
Dane unpublished manuscript
- Dane S. Reliabilities studies of the Hardiness Testing Sale. Unpublished manuscript.
De Oliveira 2019
- De Oliveira SM, De Alcantara Sousa LV, Vieira Gadelha MD, Do Nascimento VB. Prevention actions of burnout syndrome in nurses: an integrating literature review. Clinical Practice and Epidemiology in Mental Health 2019;15:64-73. [DOI: 10.2174/1745017901915010064] [PMC6446475 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deady 2017
- Deady M, Choi I, Calvo RA, Glozier N, Christensen H, Harvey SB. eHealth interventions for the prevention of depression and anxiety in the general population: a systematic review and meta-analysis. BMC Psychiatry 2017;17(1):310. [DOI: 10.1186/s12888-017-1473-1] [PMC5576307 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2019
- Deeks JJ, Higgins JP, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Dehghan 2012
- Dehghan Nayeri N. Principles of Nursing Management. Tehran: Boshra Publishing House, 2012. [Google Scholar]
Delgado 2017
- Delgado C, Upton D, Ranse K, Furness T, Foster K. Nurses’ resilience and the emotional labour of nursing work: an integrative review of empirical literature. International Journal of Nursing Studies 2017;70:71–88. [DOI: 10.1016/j.ijnurstu.2017.02.008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Demerouti 2003
- Demerouti E, Bakker AB, Vardakou I, Kantas A. The convergent validity of two burnout instruments: a multitrait-multimethod analysis. European Journal of Psychological Assessment 2003;19(1):12–23. [DOI: 10.1027//1015- 5759.19.1.12] [Google Scholar]
Demerouti 2010
- Demerouti E, Mostert K, Bakker AB. Burnout and work engagement: a thorough investigation of the independency of both constructs. Journal of Occupational Health Psychology 2010;15(3):209-22. [DOI: 10.1037/a0019408] [PMID: ] [DOI] [PubMed] [Google Scholar]
DeRoon‐Cassini 2010
- DeRoon-Cassini TA, Mancini AD, Rusch MD, Bonanno G. Psychopathology and resilience following traumatic injury: a latent growth mixture model analysis. Rehabilitation Psychology 2010;55(1):1-11. [DOI: 10.1037/a0018601] [PMID: ] [DOI] [PubMed] [Google Scholar]
Devilly 2007
- Devilly GJ, Varker T, Hansen K, Gist R. An analogue study of the effects of psychological debriefing on eyewitness memory. Behavior Research and Therapy 2007;45(6):1245–54. [DOI: 10.1016/j.brat.2006.08.022] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dias 2008
- Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Statistics in Medicine 2008;29(7-8):932-44. [DOI: 10.1002/sim.3767] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dias 2015
- Dias R, Santos RL, Sousa MF, Nogueira MM, Torres B, Belfort T, et al. Resilience of caregivers of people with dementia: a systematic review of biological and psychosocial determinants. Trends in Psychiatry and Psychotherapy 2015;37(1):12-9. [DOI: 10.1590/2237-6089-2014-0032] [PMID: ] [DOI] [PubMed] [Google Scholar]
Diener 1985
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. Journal of Personality Assessment 1985;49(1):71-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dolan 2006
- Dolan CA, Adler AB. Military hardiness as a buffer of psychological health on return from deployment. Military Medicine 2006;171(2):93-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Douglass 1983
- Douglass ME, Baker LD, Brooks WT. The New Time Management. Chicago (IL): Nightingale-Conant Corporation, 1983. [Google Scholar]
Downs 1998
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health 1998;52(6):377–84. [DOI: 10.1136/jech.52.6.377] [PMC1756728] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duits 1997
- Duits AA, Boeke S, Taams MA, Passchier J, Erdman RA. Prediction of quality of life after coronary artery bypass graft surgery: a review and evaluation of multiple, recent studies. Psychosomatic Medicine 1997;59(3):257-68. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dyrbye 2010
- Dyrbye LN, Power DV, Massie FS, Eacker A, Harper W, Thomas MR, et al. Factors associated with resilience to and recovery from burnout: a prospective, multi-institutional study of US medical students. Medical Education 2010;44(10):1016-26. [DOI: 10.1111/j.1365-2923.2010.03754.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dörfel 2008
- Dörfel D, Rabe S, Karl A. Coping strategies in daily life as protective and risk factors for post traumatic stress in motor vehicle accident survivors. Journal of Loss and Trauma 2008;13(5):422-40. [DOI: 10.1080/15325020701742136] [DOI] [Google Scholar]
Earvolino‐Ramirez 2007
- Earvolino-Ramirez M. Resilience: a concept analysis. Nursing Forum 2007;42(2):73-82. [DOI: 10.1111/j.1744-6198.2007.00070.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Edwards 2003
- Edwards D, Burnard P. A systematic review of stress and stress management interventions for mental health nurses. Journal of Advanced Nursing 2003;42(2):169-200. [DOI: 10.1046/j.1365-2648.2003.02600.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI: 10.1136/bmj.315.7109.629] [DOI] [PMC free article] [PubMed] [Google Scholar]
Elder 2014
- Elder C, Nidich S, Moriarty F, Nidich R. Effect of transcendental meditation on employee stress, depression, and burnout: a randomized controlled study. Permanente Journal 2014;18(1):19-23. [DOI: 10.7812/TPP/13-102] [PMC3951026] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ellawala 2004
- Ellawala N. Discovering Freedom: A Collection of Essays. Colombo (LK): Social Scientists’ Association, 2004. [Google Scholar]
Elliott 2012
- Elliott KE, Scott JL, Stirling C, Martin AJ, Robinson A. Building capacity and resilience in the dementia care workforce: a systematic review of interventions targeting worker and organizational outcomes. International Psychogeriatrics 2012;24(6):882-94. [DOI: 10.1017/S1041610211002651] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ellis 1957
- Ellis A. Rational psychotherapy and individual psychology. Journal of Individual Psychology 1957;13(1):38-44. [Google Scholar]
Ellis 1975
- Ellis A, Harper RA. A New Guide to Rational Living. Chatsworth (CA): Wilshire Book Company, 1975. [Google Scholar]
Epstein 1999
- Epstein RM. Mindful practice. JAMA 1999;282(9):833-9. [DOI: 10.1001/jama.282.9.833] [10478689] [DOI] [PubMed] [Google Scholar]
Eriksson 2006
- Eriksson M, Lindström B. Antonovsky's sense of coherence scale and the relation with health: a systematic review. Journal of Epidemiology and Community Health 2006;60(5):376-81. [DOI: 10.1136/jech.2005.041616] [PMC2563977] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eschleman 2010
- Eschleman KJ, Bowling NA, Alarcon GM. A meta-analytic examination of hardiness. International Journal of Stress Management 2010;17(4):277-307. [DOI: 10.1037/a0020476.supp] [DOI] [Google Scholar]
Farber 2000
- Farber EW, Schwartz JA, Schaper PE, Moonen DJ, McDaniel JS. Resilience factors associated with adaptation to HIV disease. Psychosomatics 2000;41(2):140-6. [DOI: 10.1176/appi.psy.41.2.140] [PMID: ] [DOI] [PubMed] [Google Scholar]
Farber 2003
- Farber EW, Mirsalimi H, Williams KA, McDaniel JS. Meaning of illness and psychological adjustment to HIV/AIDS. Psychosomatics 2003;44(6):485-91. [DOI: 10.1176/appi.psy.44.6.485] [PMID: ] [DOI] [PubMed] [Google Scholar]
Farchi 2010
- Farchi M, Gidron Y. The effects of "psychological inoculation" versus ventilation on the mental resilience of Israeli citizens under continuous war stress. Journal of Nervous and Mental Disease 2010;198(5):382-4. [DOI: 10.1097/NMD.0b013e3181da4b67] [PMID: ] [DOI] [PubMed] [Google Scholar]
Faul 2007
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 2007;39(2):175‐191. [DOI: 10.3758/bf03193146] [PMID: ] [DOI] [PubMed] [Google Scholar]
Feder 2011
- Feder A, Charney D, Collins K. Neurobiology of resilience. In: Southwick SM, Litz BT, Charney D, Friedman MJ, editors(s). Resilience and Mental Health: Challenges Across the Lifespan. Cambridge: Cambridge University Press, 2011. [Google Scholar]
Feder 2013
- Feder A, Ahmad S, Lee EJ, Morgan JE, Singh R, Smith BW, et al. Coping and PTSD symptoms in Pakistani earthquake survivors: purpose in life, religious coping and social support. Journal of Affective Disorders 2013;147(1-3):156-63. [DOI: 10.1016/j.jad.2012.10.027] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fernández‐Lansac 2012
- Fernández-Lansac V, Crespo López M, Cáceres R, Rodríguez-Poyo M. Resilience in caregivers of patients with dementia: a preliminary study. Revista Española de Geriatría y Gerontología 2012;47(3):102-9. [DOI: 10.1016/j.regg.2011.11.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Finnes 2019
- Finnes A, Ghaderi A, Dahl J, Nager A, Enebrink P. Randomized controlled trial of acceptance and commitment therapy and a workplace intervention for sickness absence due to mental disorders. Journal of Occupational Health Psychology 2019;24(1):198-212. [DOI: 10.1037/ocp0000097] [NCT01805583] [PMID: ] [DOI] [PubMed] [Google Scholar]
Flaxman 2013
- Flaxman PE, Bond FW, Livheim F. The Mindful and Effective Employee: An Acceptance and Commitment Therapy Training Manual for Improving Well-being and Performance. Oakland (CA): New Harbinger Publications, 2013. [Google Scholar]
Fletcher 2013
- Fletcher D, Sarkar M. Psychological resilience: a review and critique of definitions, concepts, and theory. European Psychologist 2013;18(1):12-23. [DOI: 10.1027/1016-9040/a000124] [DOI] [Google Scholar]
Foa 1986
- Foa EB, Kozak MJ. Emotional processing of fear: exposure to corrective information. Psychological Bulletin 1986;99(1):20–35. [DOI: 10.1037/0033-2909.99.1.20] [PMID: ] [DOI] [PubMed] [Google Scholar]
Folkman 1988
- Folkman S, Lazarus R. Ways of Coping Questionnaire Manual. Palo Alto (CA): Consulting Psychologists Press Inc, 1988. [Google Scholar]
Forgeard 2012
- Forgeard MJ, Seligman ME. Seeing the glass half full: a review of the causes and consequences of optimism. Pratiques Psychologiques 2012;18(2):107-20. [DOI: 10.1016/j.prps.2012.02.002] [DOI] [Google Scholar]
Forstmeier 2009
- Forstmeier S, Kuwert P, Spitzer C, Freyberger HJ, Maercker A. Posttraumatic growth, social acknowledgment as survivors, and sense of coherence in former German child soldiers of World War II. American Journal of Geriatric Psychiatry 2009;17(12):1030-9. [DOI: 10.1097/JGP.0b013e3181ab8b36] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fortney 2013
- Fortney L, Luchterhand C, Zakletskaia L, Zgierska A, Rakel D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: a pilot study. Annals of Family Medicine 2013;11(5):412-20. [DOI: 10.1370/afm.1511] [PMC3767709] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Foster 2019
- Foster K, Roche M, Delgado C, Cuzzillo C, Giandinoto JA, Furness T. Resilience and mental health nursing: an integrative review of international literature. International Journal of Mental Health Nursing 2019;28(1):71-85. [DOI: 10.1111/inm.12548] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fox 2018
- Fox S, Lydon S, Byrne D, Madden C, Connolly F, O'Connor P. A systematic review of interventions to foster physician resilience. Postgraduate Medical Journal 2018;94(1109):162-70. [DOI: 10.1136/postgradmedj-2017-135212] [PMID: ] [DOI] [PubMed] [Google Scholar]
Frank 1999
- Frank E, Dingle AD. Self-reported depression and suicide attempts among US women physicians. American Journal of Psychiatry 1999;156(12):1887-94. [DOI: 10.1176/ajp.156.12.1887] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fredrickson 2003
- Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. Journal of Personality and Social Psychology 2003;84(2):365–76. [NIHMS141511] [PMC2755263] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fresco 2006
- Fresco DM, Alloy LB, Reilly–Harrington N. Association of attributional style for negative and positive events and the occurrence of life events with depression and anxiety. Journal of Social and Clinical Psychology 2006;25(10):1140-60. [Google Scholar]
Friborg 2003
- Friborg O, Hjemdal O, Rosenvinge JH, Martinussen M. A new rating scale for adult resilience: what are the central protective resources behind healthy adjustment? International Journal of Methods in Psychiatric Research 2003;12(2):65-76. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Friborg 2005
- Friborg O, Barlaug D, Martinussen M, Rosenvinge JH, Hjemdal O. Resilience in relation to personality and intelligence. International Journal of Methods in Psychiatric Research 2005;14(1):29-42. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Friborg 2006
- Friborg O, Martinussen M, Rosenvinge JH. Likert-based vs semantic differential-based scorings of positive psychological constructs: a psychometric comparison of two versions of a scale measuring resilience. Personality and Individual Differences 2006;40(5):873-84. [DOI: 10.1016/j.paid.2005.08.015] [DOI] [Google Scholar]
Frommberger 1999
- Frommberger U, Stieglitz RD, Straub S, Nyberg E, Schlickewei W, Kuner E, et al. The concept of "sense of coherence" and the development of posttraumatic stress disorder in traffic accident victims. Journal of Psychosomatic Research 1999;46(4):343-8. [DOI: 10.1016/S0022-3999(98)00117-2] [DOI] [PubMed] [Google Scholar]
Fujisawa [pers comm]
- Fujisawa D. Trial and publication status [personal communication]. Email to: A Kunzler 31 July 2019.
Fuller‐Iglesias 2008
- Fuller-Iglesias H, Sellars B, Antonucci TC. Resilience in old age: social relations as a protective factor. Research in Human Development 2008;5(3):181-93. [DOI: 10.1080/15427600802274043] [DOI] [Google Scholar]
Fusz 2008
- Fusz I, Nübling M, Hasselhorn H-M, Schwappach D, Rieger MA. Working conditions and work-family conflict in German hospital physicians: psychosocial and organisational predictors and consequences. BMC Public Health 2008;8:353. [DOI: 10.1186/1471-2458-8-353] [DOI] [PMC free article] [PubMed] [Google Scholar]
Galatzer‐Levy 2012
- Galatzer-Levy IR, Burton CL, Bonanno GA. Coping flexibility, potentially traumatic life events, and resilience: a prospective study of college student adjustment. Journal of Social and Clinical Psychology 2012;31(6):542-67. [DOI: 10.1521/jscp.2012.31.6.542] [DOI] [Google Scholar]
Garnefski 2002
- Garnefski N, Kraaij V, Spinhoven P. CERQ: Manual for the Use of the Cognitive Emotion Regulation Questionnaire. Leiderdorp (NL): Datec, 2002. [Google Scholar]
Garnefski 2007
- Garnefski N, Kraaij V. The Cognitive Emotion Regulation Questionnaire. Psychometric features and prospective relationships with depression and anxiety in adults. European Journal of Psychological Assessment 2007;23(3):141–9. [DOI: 10.1027/1015-5759.23.3.141] [DOI] [Google Scholar]
Gelkopf 2009
- Gelkopf M, Berger R. A school-based, teacher-mediated prevention program (ERASE-Stress) for reducing terror-related traumatic reactions in Israeli youth: a quasi-randomized controlled trial. Journal of Child Psychology and Psychiatry 2009;50(8):962–71. [DOI: 10.1111/j.1469-7610.2008.02021.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gelkopf 2019 [pers comm]
- Gelkopf M. Number of mental health volunteers included in the study and summary outcome data for this subgroup [personal communication]. Email to: A Kunzler 19 March 2019.
Gelkopf unpublished manuscript
- Gelkopf M, Rifkind R, Berger M. The impact of a trauma-education program on medical students. Unpublished manuscript.
Geschwind 2010
- Geschwind N, Peeters F, Jacobs N, Delespaul P, Derom C, Thiery E, et al. Meeting risk with resilience: high daily life reward experience preserves mental health. Acta Psychiatrica Scandinavica 2010;122(2):129-38. [DOI: 10.1111/j.1600-0447.2009.01525.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Geschwind 2011
- Geschwind N, Peeters F, Drukker M, Van Os J, Wichers M. Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: a randomized controlled trial. Journal of Consulting and Clinical Psychology 2011;79(5):618-28. [DOI: 10.1037/a0024595] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gillman 2015
- Gillman L, Adams J, Kovac R, Kilcullen A, House A, Doyle C. Strategies to promote coping and resilience in oncology and palliative care nurses caring for adult patients with malignancy: a comprehensive systematic review. JBI Database of Systematic Reviews and Implementation Reports 2015;13(5):131-204. [DOI: 10.11124/jbisrir-2015-1898] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gilmartin 2017
- Gilmartin H, Goyal A, Hamati MC, Mann J, Saint S, Chopra V. Brief mindfulness practices for healthcare providers - a systematic literature review. American Journal of Medicine 2017;130(10):1219.e1-e17. [DOI: 10.1016/j.amjmed.2017.05.041] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gloria 2016
- Gloria CT, Steinhardt MA. Relationships among positive emotions, coping, resilience and mental health. Stress Health 2016;32(2):145-56. [DOI: 10.1002/smi.2589] [DOI] [PubMed] [Google Scholar]
Gong 2014
- Gong Y, Han T, Yin X, Yang G, Zhuang R, Chen Y, et al. Prevalence of depressive symptoms and work-related risk factors among nurses in public hospitals in southern China: a cross-sectional study. Scientific Reports 2014;4:7109. [DOI: 10.1038/srep07109] [PMC5384112] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gracino 2016
- Gracino ME, Lima Zitta AL, Mangili OC, Massuda EM. Physical and mental health of medical professionals: a systematic review. Saúde em Debate 2016;40(110):244-63. [DOI: 10.1590/0103-1104201611019] [DOI] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime), (accessed 21 April 2020).Available from: www.gradepro.org.
Graham 2001
- Graham J, Albery IP, Ramirez AJ, Richards MA. How hospital consultants cope with stress at work: implications for their mental health. Stress and Health 2001;17(2):85–9. [DOI: 10.1002/smi.884] [DOI] [Google Scholar]
Gray 2019
- Gray P, Senabe S, Naicker N, Kgalamono S, Yassi A, Spiegel JM. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: a realist review. International Journal of Environmental Research and Public Health 2019;16(22):4396. [DOI: 10.3390/ijerph16224396] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gross 1995
- Gross JJ, Levenson RW. Emotion elicitation using films. Cognition and Emotion 1995;9(1):87–108. [DOI: 10.1080/02699939508408966] [DOI] [Google Scholar]
Grossman 2004
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: a meta-analysis. Journal of Psychosomatic Research 2004;57(1):35-43. [DOI: 10.1016/S0022-3999(03)00573-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
Grote 2007
- Grote NK, Bledsoe SE, Larkin J, Lemay EP Jr, Brown C. Stress exposure and depression in disadvantage women: the protective effects of optimism and perceived control. Social Work Research 2007;31(1):19-33. [DOI: 10.1093/swr/31.1.19] [DOI] [Google Scholar]
Guardino 2013
- Guardino CM, Schetter CD. Coping during pregnancy: a systematic review and recommendations. Health Psychology Review 2013;8(1):70-94. [DOI: 10.1080/17437199.2012.752659] [PMC3904449] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gudex 1996
- Gudex C, Dolan P, Kind P, Williams A. Health state valuations from the general public using the visual analogue scale. Quality of Life Research 1996;5(6):521-31. [DOI: 10.1007/bf00439226] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guest 2015
- Guest R, Craig A, Nicholson Perry K, Tran Y, Ephraums C, Hales A, et al. Resilience following spinal cord injury: a prospective controlled study investigating the influence of the provision of group cognitive behavior therapy during inpatient rehabilitation. Rehabilitation Psychology 2015;60(4):311-21. [DOI: 10.1037/rep0000052] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guillaumie 2017
- Guillaumie L, Boiral O, Champagne J. A mixed-methods systematic review of the effects of mindfulness on nurses. Journal of Advanced Nursing 2017;73(5):1017-34. [DOI: 10.1111/jan.13176] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guvva 2019 [pers comm]
- Guvva K. Information if trial was still ongoing [personal communication]. Email to: A Kunzler 21 August 2019.
Guyatt 2011a
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). Journal of Clinical Epidemiology 2011;64(4):407-15. [DOI: 10.1016/j.jclinepi.2010.07.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence--indirectness. Journal of Clinical Epidemiology 2011;64(12):1303-10. [DOI: 10.1016/j.jclinepi.2011.04.014] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011c
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. Journal of Clinical Epidemiology 2011;64(12):1294-1302. [DOI: 10.1016/j.jclinepi.2011.03.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011d
- Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence--imprecision. Journal of Clinical Epidemiology 2011;64(12):1283-93. [DOI: 10.1016/j.jclinepi.2011.01.012] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011e
- Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines: 5. Rating the quality of evidence--publication bias. Journal of Clinical Epidemiology 2011;64(12):1277-82. [DOI: 10.1016/j.jclinepi.2011.01.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
Haglund 2007
- Haglund ME, Nestadt PS, Cooper NS, Southwick SM, Charney DS. Psychobiological mechanisms of resilience: relevance to prevention and treatment of stress-related psychopathology. Development and Psychopathology 2007;19(3):889-920. [DOI: 10.1017/S0954579407000430] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hahn 2011
- Hahn VC, Binnewies C, Sonnentag S, Mojza EJ. Learning how to recover from job stress: effects of a recovery training program on recovery, recovery-related self-efficacy, and well-being. Journal of Occupational Health Psychology 2011;16(2):202-16. [DOI: 10.1037/a0022169] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hannigan 2004
- Hannigan B, Edwards D, Burnard P. Stress and stress management in clinical psychology: findings from a systematic review. Journal of Mental Health 2004;13(3):235-45. [10.1080/09638230410001700871] [Google Scholar]
Harris 2018
- Harris M, Thomas G, Thomas M, Cafarella P, Stocks A, Greig J, et al. Supporting wellbeing in motor neurone disease for patients, carers, social networks, and health professionals: a scoping review and synthesis. Palliative & Supportive Care 2018;16(2):228-37. [DOI: 10.1017/S1478951517000700] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hart 2014
- Hart PL, Brannan JD, De Chesnay M. Resilience in nurses: an integrative review. Journal of Nursing Management 2014;22(6):720-34. [DOI: 10.1111/j.1365-2834.2012.01485.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hartley 2008
- Hartley SM, Vance DE, Elliott TR, Cuckler JM, Berry JW. Hope, self-efficacy, and functional recovery after knee and hip replacement surgery. Rehabilitation Psychology 2008;53(4):521-9. [DOI: 10.1037/a0013121] [DOI] [Google Scholar]
Harvey 2003
- Harvey MR, Liang B, Harney PA, Koenen K, Tummala-Narra P, Lebowitz L. A multidimensional approach to the assessment of trauma impact, recovery and resiliency. Journal of Aggression, Maltreatment & Trauma 2003;6(2):87-109. [DOI: 10.1300/J146v06n02_05] [DOI] [Google Scholar]
Harvey 2009
- Harvey SB, Laird B, Henderson M, Hotopf M. The Mental Health of Health Care Professionals. A Review for the Department of Health. London (LO): King’s College London, 2009. [Google Scholar]
Harvey 2017
- Harvey SB, Modini M, Joyce S, Milligan-Saville JS, Tan L, Mykletun A, et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occupational and Environmental Medicine 2017;74(4):301–10. [DOI: 10.1136/oemed-2016-104015] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hasson 2005
- Hasson D, Arnetz BB. Validation and findings comparing VAS vs. Likert scales for psychosocial measurements. International Electronic Journal Health Education 2005;8:178–92. [Google Scholar]
Hayes 2004
- Hayes SC, Follette VM, Linehan MM. Mindfulness and Acceptance. Expanding the Cognitive-Behavioral Tradition. New York (NY): The Guilford Press, 2004. [Google Scholar]
Hayes 2006
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behaviour Research and Therapy 2006;44(1):1-25. [DOI: 10.1016/j.brat.2005.06.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hayter 2014
- Hayter MR, Dorstyn DS. Resilience, self-esteem and self-compassion in adults with spina bifida. Spinal Cord 2014;52(2):167-71. [DOI: 10.1038/sc.2013.152] [PMID: ] [DOI] [PubMed] [Google Scholar]
He 2008
- He S, Zhang B, Bai L. Introduction of MMSS scale. Chinese Nursing Research 2008;22:1063. [DOI: 10.3969/j.issn.1009-6493.2008.12.045] [DOI] [Google Scholar]
Heber 2017
- Heber E, Ebert D, Lehr D, Cuijpers P, Berking M, Nobis S, et al. The benefit of web- and computer-based interventions for stress: a systematic review and meta-analysis. Journal of Medical Internet Research 2017;19(2):e32. [DOI: 10.2196/jmir.5774] [PMC5336602 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hebert 2007
- Hebert RS, Dang Q, Schulz R. Religious beliefs and practices are associated with better mental health in family caregivers of patients with dementia: findings from the REACH study. American Journal of Geriatric Psychiatry 2007;15(4):292-300. [DOI: 10.1097/01.JGP.0000247160.11769.ab] [PMID: ] [DOI] [PubMed] [Google Scholar]
Heinen 2013
- Heinen MM, Van Achterberg T, Schwendimann R, Zander B, Matthews A, Kózka M, et al. Nurses' intention to leave their profession: a cross sectional observational study in 10 European countries. International Journal of Nursing Studies 2013;50(2):174-84. [DOI: 10.1016/j.ijnurstu.2012.09.019] [PMID: ] [DOI] [PubMed] [Google Scholar]
Helgeson 2006
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology 2006;74(5):797-816. [DOI: 10.1037/0022-006X.74.5.797] [PMID: ] [DOI] [PubMed] [Google Scholar]
Henderson 2007
- Henderson N, Bonnie B. Resiliency in Action: Practical Ideas for Overcoming Risks and Building Strengths in Youth, Families & Communities. Washington DC: Public Library, 2007. [Google Scholar]
Hernandez 2013
- Hernandez M, Barrio C, Yamada AM. Hope and burden among Latino families of adults with schizophrenia. Family Process 2013;52(4):697-708. [DOI: 10.1111/famp.12042] [PMC5032651] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heron 2010
- Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. British Journal of Health Psychology 2010;5(Pt 1):1-39. [DOI: 10.1348/135910709X466063] [PMC2800172 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI: 10.1136/bmj.d5928] [PMC3196245] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011b
- Higgins JP, Altman DG, Sterne JA (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Higgins 2019a
- Higgins JPT, Li T, Deeks JJ (editors). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Higgins 2019b
- Higgins JP, Eldridge S, Li T (editors). Chapter 23: Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Hjemdal 2001
- Hjemdal O, Friborg O, Martinussen M, Rosenvinge JH. Preliminary results from the development and validation of a Norwegian scale for measuring adult resilience [Mestring og psykologisk motstandsdyktighet hos voksne: utvikling og foreløpig validering av et nytt instrument]. Tidsskrift for Norsk Psykologforening 2001;38:310-7. [Google Scholar]
Ho 2010
- Ho SM, Ho JW, Bonanno GA, Chu AT, Chan EM. Hopefulness predicts resilience after hereditary colorectal cancer genetic testing: a prospective outcome trajectories study. BMC Cancer 2010;10:279. [DOI: 10.1186/1471-2407-10-279] [PMC2891641] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Horsfall 2014
- Horsfall S. Doctors Who Commit Suicide While Under GMC Fitness to Practise Investigation. London (LO): General Medical Council, 2014. [Google Scholar]
Hu 2015
- Hu T, Zhang D, Wang J. A meta-analysis of the trait resilience and mental health. Personality and Individual Differences 2015;76:18-27. [DOI: 10.1016/j.paid.2014.11.039] [DOI] [Google Scholar]
Huang 2003
- Huang L, Yang T, Li Z. Applicability of the Positive and Negative Affect Scale in Chinese. Chinese Mental Health Journal 2003;17(1):54-6. [DOI: 10.3321/j.issn:1000-6729.2003.01.018] [DOI] [Google Scholar]
Huey 1997
- Huey SJ Jr, Weisz JR. Ego control, ego resiliency, and the five-factor model as predictors of behavioral and emotional problems in clinic-referred children and adolescents. Journal of Abnormal Psychology 1997;106(3):404-15. [DOI: 10.1037/0021-843X.106.3.404] [PMID: ] [DOI] [PubMed] [Google Scholar]
Huggard 2016
- Huggard P, Huggard J, Zhao B. Resilience, as understood by hospice palliative care clinicians. Palliative Medicine 2016;30(4):S1–S130. [DOI: 10.1177/0269216316631462] [DOI] [Google Scholar]
Hultcrantz 2017
- Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, et al. The GRADE Working Group clarifies the construct of certainty of evidence. Journal of Clinical Epidemiology 2017;87:4-13. [DOI: 10.1016/j.jclinepi.2017.05.006] [PMC6542664] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hunter 2016
- Hunter L. Making time and space: the impact of mindfulness training on nursing and midwifery practice. A critical interpretative synthesis. Journal of Clinical Nursing 2016;25(7-8):918-29. [DOI: 10.1111/ jocn.13164] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hurtes 2001
- Hurtes KP, Allen LR. Measuring resiliency in youth: the Resiliency Attitudes and Skills Profile. Therapeutic Recreation Journal 2001;35(4):333-47. [Google Scholar]
Hystad 2011
- Hystad SW, Eid J, Brevik JI. Effects of psychological hardiness, job demands, and job control on sickness absence: a prospective study. Journal of Occupational Health Psychology 2011;16(3):265-78. [DOI: 10.1037/a0022904] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hölzel 2011
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science 2011;6(6):537-59. [DOI: 10.1177/1745691611419671] [DOI] [PubMed] [Google Scholar]
Iacoviello 2014
- Iacoviello BM, Charney DS. Psychosocial facets of resilience: implications for preventing posttrauma psychopathology, treating trauma survivors, and enhancing community resilience. European Journal of Psychotraumatology 2014;5:1-10. [PMC4185137] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ireland 2019 [pers comm]
- Ireland M. Potential withdrawals/exclusions in the two groups and number of participants analysed in each group [personal communication]. Email to: A Kunzler 5 September 2019.
Irwin 2019 [pers comm]
- Irwin M. Trial and publication status [personal communication]. Email to: A Kunzler 31 July 2019.
Jackson 2007
- Jackson D, Firtko A, Edenborough M. Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: a literature review. Journal of Advanced Nursing 2007;60(1):1-9. [DOI: 10.1111/j.1365-2648.2007.04412.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jackson 2014
- Jackson T, Wang Y, Wang Y, Fan H. Self-efficacy and chronic pain outcomes: a meta-analytic review. Journal of Pain 2014;15(8):800-14. [DOI: 10.1016/j.jpain.2014.05.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jacobson 1938
- Jacobson E. Progressive Relaxation: A Physiological and Clinical Investigation of Muscular States and their Significance in Psychology and Medical Practice. Chicago (IL): University of Chicago Press, 1938. [Google Scholar]
Jennings 2008
- Jennings BM. Chapter 26. Work stress and burnout among nurses: role of the work environment and working conditions. In: Hughes RG, editors(s). Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US), 2008. [PubMed] [Google Scholar]
Jennings 2013
- Jennings PA, Frank JL, Snowberg KE, Coccia MA, Greenberg MT. Improving classroom learning environments by Cultivating Awareness and Resilience in Education (CARE): results of a randomized controlled trial. School Psychology Quarterly 2013;28(4):374-90. [DOI: 10.1037/spq0000035] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jha 2010
- Jha AP, Stanley EA, Kiyonaga A, Wong L, Gelfand L. Examining the protective effects of mindfulness training on working memory capacity and affective experience. Emotion 2010;10(1):54-64. [DOI: 10.1037/a0018438] [PMID: ] [DOI] [PubMed] [Google Scholar]
Johnson 2009
- Johnson RJ, Canetti D, Palmieri PA, Galea S, Varley J, Hobfoll SE. A prospective study of risk and resilience factors associated with posttraumatic stress symptoms and depression symptoms among Jews and Arabs exposed to repeated acts of terrorism in Israel. Psychological Trauma: Theory, Research, Practice, and Policy 2009;1(4):291-311. [DOI: 10.1037/a0017586] [DOI] [Google Scholar]
Johnson 2010
- Johnson J, Gooding PA, Wood AM, Tarrier N. Resilience as positive coping appraisals: testing the schematic appraisals model of suicide (SAMS). Behaviour Research and Therapy 2010;48(3):179-86. [DOI: 10.1016/j.brat.2009.10.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Johnson 2014
- Johnson DC, Thom NJ, Stanley EA, Haase L, Simmons AN, Shih P-AB, et al. Modifying resilience mechanisms in at-risk individuals: a controlled study of mindfulness training in marines preparing for deployment. American Journal of Psychiatry 2014;171(8):844-53. [DOI: 10.1176/appi.ajp.2014.13040502] [PMC4458258] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnson 2015
- Johnson AJ, Tottenham N. Regulatory skill as a resilience factor for adults with a history of foster care: a pilot study. Developmental Psychobiology 2015;57(1):1-16. [DOI: 10.1002/dev.21227] [PMC4302248] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnston 2015
- Johnston MC, Porteous T, Crilly MA, Burton CD, Elliott A, Iversen L, et al. Physical disease and resilient outcomes: a systematic review of resilience definitions and study methods. Psychosomatics 2015;56(2):168-80. [DOI: 10.1016/j.psym.2014.10.005] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2000
- Jones MC, Johnston DW. Reducing distress in first level and student nurses: a review of the applied stress management literature. Journal of Advanced Nursing 2000;32(1):66–74. [DOI: 10.1046/j.1365-2648.2000.01421.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jonsson 2003
- Jonsson A, Segesten K, Mattsson B. Post-traumatic stress among Swedish ambulance personnel. Emergency Medicine Journal 2003;20(1):79-84. [DOI: 10.1136/emj.20.1.79] [PMC1726002] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Joyce 2018
- Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018;8(6):e017858. [DOI: 10.1136/bmjopen-2017-017858] [PMC6009510 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Judkins 2005
- Judkins S, Rind R. Hardiness, job satisfaction, and stress among home health nurses. Home Health Care Management & Practice 2005;17(2):113-8. [DOI: 10.1177/10848223042700201] [DOI] [Google Scholar]
Kabat‐Zinn 1982
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General Hospital Psychiatry 1982;4(1):33-47. [DOI: 10.1016/0163-8343(82)90026-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kabat‐Zinn 1990
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of your Body and Mind to Face Stress. New York (NY): Delacourte Press, 1990. [Google Scholar]
Kabat‐Zinn 2013
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York, NY: Bantam Books, 2013. [Google Scholar]
Kalisch 2015
- Kalisch R, Müller MB, Tüscher O. A conceptual framework for the neurobiological study of resilience. Behavioral and Brain Sciences 2015;38:e92. [DOI: 10.1017/S0140525X1400082X] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kalisch 2017
- Kalisch R, Baker DG, Basten U, Boks MP, Bonanno GA, Brummelman E, et al. The resilience framework as a strategy to combat stress-related disorders. Nature Human Behaviour 2017;1(11):784-90. [DOI: 10.1038/s41562-017-0200-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Karstoft 2015
- Karstoft KI, Armour C, Elklit A, Solomon Z. The role of locus of control and coping style in predicting longitudinal PTSD-trajectories after combat exposure. Journal of Anxiety Disorders 2015;32:89-94. [DOI: 10.1016/j.janxdis.2015.03.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kasen 2014
- Kasen S, Wickramaratne P, Gameroff MJ. Religiosity and longitudinal change in psychosocial functioning in adult offspring of depressed parents at high risk for major depression. Depression and Anxiety 2014;31(1):63-71. [DOI: 10.1002/da.22131] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kaspersen 2003
- Kaspersen M, Matthiesen SB, Götestam KG. Social network as a moderator in the relation between trauma exposure and trauma reaction: a survey among UN soldiers and relief workers. Scandinavian Journal of Psychology 2003;44(5):415-23. [DOI: 10.1046/j.1467-9450.2003.00362.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kawakami 2019 [pers comm]
- Kawakami N. Potential focus on and measurement of resilience in the study Imamura 2019 [personal communication]. Email to: A Kunzler 7 August 2019.
Kent 2011
- Kent M, Davis MC, Stark SL, Stewart LA. A resilience-oriented treatment for posttraumatic stress disorder: results of a preliminary randomized clinical trial. Journal of Traumatic Stress 2011;24(5):591-5. [DOI: 10.1002/jts.20685] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kent 2014
- Kent M, Davis MC, Reich JW. The Resilience Handbook: Approaches to Stress and Trauma. New York: Routledge, 2014. [Google Scholar]
Kilic 2013
- Kilic SA, Dorstyn DS, Guiver NG. Examining factors that contribute to the process of resilience following spinal cord injury. Spinal Cord 2013;51(7):553-7. [DOI: 10.1038/sc.2013.25] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kim 2008
- Kim JS. Examining the effectiveness of solution-focused brief therapy: a meta-analysis. Research on Social Work Practice 2008;18(2):107-16. [DOI: 10.1177/1049731507307807] [DOI] [Google Scholar]
Kim 2018b
- Kim MS, Kim T, Lee D, Yook JH, Hong YC, Lee SY, et al. Mental disorders among workers in the healthcare industry: 2014 national health insurance data. Annals of Occupational and Environmental Medicine 2018;30:31. [DOI: 10.1186/s40557-018-0244-x] [PMC5934846] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
King 1998
- King LA, King DW, Fairbank JA, Keane TM, Adams GA. Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: hardiness, postwar social support, and additional stressful life events. Journal of Personality and Social Psychology 1998;74(2):420-34. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kivimäki 2005
- Kivimäki M, Vahtera J, Elovainio M, Helenius H, Singh-Manoux A, Pentti J. Optimism and pessimism as predictors of change in health after death or onset of severe illness in family. Health Psychology 2005;24(4):413-21. [DOI: 10.1037/0278-6133.24.4.413] [PMID: ] [DOI] [PubMed] [Google Scholar]
Klatt 2009
- Klatt MD, Buckworth J, Malarkey WB. Effects of low-dose mindfulness-based stress reduction (MBSR-Id) on working adults. Health Education & Behavior 2009;36(3):601–14. [DOI: 10.1177/1090198108317627] [PMID: ] [DOI] [PubMed] [Google Scholar]
Klatt 2018 [pers comm]
- Klatt M. Descriptive statistics (means and SDs) for the outcomes perceived stress, DASS-21 stress, work stress, salivary alpha-amylase and work satisfaction for two groups at pre- and post-intervention [personal communication]. Email to: A Kunzler 28 June 2018.
Klatt 2019 [pers comm]
- Klatt M. Number of participants analysed in each group [personal communication]. Email to: A Kunzler 22 February 2019.
Klohnen 1996
- Klohnen EC. Conceptual analysis and measurement of the construct of ego-resiliency. Journal of Personality and Social Psychology 1996;70(5):1067-79. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kneebone 2003
- Kneebone II, Martin PR. Coping and caregivers of people with dementia. British Journal of Health Psychology 2003;8(1):1-17. [DOI: 10.1348/135910703762879174] [PMID: ] [DOI] [PubMed] [Google Scholar]
Koenen 2003
- Koenen KC, Stellman JM, Stellman SD, Sommer JF Jr. Risk factors for course of posttraumatic stress disorder among Vietnam veterans: a 14-year follow-up of American Legionnaires. Journal of Consulting and Clinical Psychology 2003;71(6):980-6. [DOI: 10.1037/0022-006X.71.6.980] [PMID: ] [DOI] [PubMed] [Google Scholar]
Koenig 2007
- Koenig HG. Religion and remission of depression in medical inpatients with heart failure/pulmonary disease. Journal of Nervous and Mental Disease 2007;195(5):389-95. [DOI: 10.1097/NMD.0b013e31802f58e3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kok 2017
- Kok BE, Singer T. Phenomenological fingerprints of four meditations: differential state changes in affect, mind-wandering, meta-cognition, and interoception before and after daily practice across 9 months of training. Mindfulness 2017;8:218-31. [DOI: 10.1007/s12671-016-0594-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Korpershoek 2011
- Korpershoek C, Van der Bijl J, Hafsteinsdóttir TB. Self-efficacy and its influence on recovery of patients with stroke: a systematic review. Journal of Advanced Nursing 2011;67(9):1876-94. [DOI: 10.1111/j.1365-2648.2011.05659.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Krahn 2013
- Krahn U, Binder H, König J. A graphical tool for locating inconsistency in network meta-analyses. BMC Medical Research Methodology 2013;13:35. [DOI: 10.1186/1471-2288-13-35] [PMC3644268] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krahn 2014
- Krahn U, Binder H, König J. Visualizing inconsistency in network meta-analysis by independent path decomposition. BMC Medical Research Methodology 2014;14:131. [DOI: 10.1186/1471-2288-14-131] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kram 1985
- Kram KE, Isabella LA. Mentoring alternatives: the role of peer relationships in career development. Academy of Management Journal 1985;28(1):110–32. [DOI: 10.2307/256064] [DOI] [Google Scholar]
Krasner 2009
- Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009;302(12):1284-93. [DOI: 10.1001/jama.2009.1384] [PMID: ] [DOI] [PubMed] [Google Scholar]
Krause 2007
- Krause N. Evaluating the stress-buffering function of meaning in life among older people. Journal of Aging and Health 2007;19(5):792-812. [DOI: 10.1177/0898264307304390] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kristensen 2005a
- Kristensen TS, Hannerz H, Høgh A, Borg V. The Copenhagen Psychosocial Questionnaire--a tool for the assessment and improvement of the psychosocial work environment. Scandinavian Journal of Work, Environment & Health 2005;31(6):438–49. [DOI: 10.5271/sjweh.948] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kristensen 2005b
- Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work and Stress 2005;19(3):192–207. [DOI: 10.1080/02678370500297720] [DOI] [Google Scholar]
Kroenke 2001
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine 2001;16(9):603-13. [DOI: 10.1046/j.1525-1497.2001.016009606.x] [PMC1495268 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuburović 2016
- Kuburović NB, Dedić V, Djuricić S, Kuburović V. Determinants of job satisfaction of healthcare professionals in public hospitals in Belgrade, Serbia--cross-sectional analysis. Srpski Arhiv za Celokupno Lekarstvo 2016;144(3-4):165-73. [PMID: ] [PubMed] [Google Scholar]
Kuehner 2017
- Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry 2017;4(2):146-58. [DOI: 10.1016/S2215-0366(16)30263-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kuiper 1992
- Kuiper NA, Martin RA, Dance KA. Sense of humour and enhanced quality of life. Personality and Individual Differences 1992;13(12):1273-83. [DOI: 10.1016/0191-8869(92)90169-P] [DOI] [Google Scholar]
Kuiper 2012
- Kuiper NA. Humor and resiliency: towards a process model of coping and growth. Europe’s Journal of Psychology 2012;8(3):475-91. [DOI: 10.5964/ejop.v8i3.464] [DOI] [Google Scholar]
Kumar 2016
- Kumar S. Burnout and doctors: prevalence, prevention and intervention. Healthcare 2016;4(3):37. [DOI: 10.3390/healthcare4030037] [PMC5041038 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kunzer unpublished
- Kunzler AM, Helmreich I, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions to foster resilience in healthcare students. Cochrane Database of Systematic Reviews. [DOI] [PMC free article] [PubMed]
Kunzler 2018
- Kunzler AM, Chmitorz A, Bagusat C, Kaluza AJ, Hoffmann I, Schäfer M, et al. Construct validity and population-based norms of the German Brief Resilience Scale (BRS). European Journal of Health Psychology 2018;25(3):107-17. [DOI: 10.1027/2512-8442/a000016] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kvillemo 2014
- Kvillemo P, Bränström R. Coping with breast cancer: a meta-analysis. PLoS ONE 2014;9(11):e112733. [DOI: 10.1371/journal.pone.0112733] [PMC4244095] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
König 2013
- König J, Krahn U, Binder H. Visualizing the flow of evidence in network meta-analysis and characterizing mixed treatment comparisons. Statistics in Medicine 2013;32(30):5414-29. [DOI: 10.1002/sim.6001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kübler‐Ross 1997
- Kübler-Ross E. On Death and Dying. New York (NY): Scribner Classics, 1997. [Google Scholar]
Lagerveld 2012
- Lagerveld SE, Blonk RW, Brenninkmeijer V, Wijngaards-de Meij L, Schaufeli WB. Work-focused treatment of common mental disorders and return to work: a comparative outcome study. Journal of Occupational Health Psychology 2012;17(2):220-34. [DOI: 10.1037/a0027049] [PMID: 22308965] [DOI] [PubMed] [Google Scholar]
Lambert 2004
- Lambert VA, Lambert CE, Itano J, Inouye J, Kim S, Kuniviktikul W, et al. Cross-cultural comparison of workplace stressors, ways of coping and demographic characteristics as predictors of physical and mental health among hospital nurses in Japan, Thailand, South Korea and the USA (Hawaii). International Journal of Nursing Studies 2004;41(6):671-84. [DOI: 10.1016/j.ijnurstu.2004.02.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lamothe 2016
- Lamothe M, Rondeau É, Malboeuf-Hurtubise C, Duval M, Sultan S. Outcomes of MBSR or MBSR-based interventions in health care providers: a systematic review with a focus on empathy and emotional competencies. Complementary Therapies in Medicine 2016;24:19–28. [DOI: 10.1016/j.ctim.2015.11.001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Landy 1991
- Landy FJ, Rastegary H, Thayer J, Colvin C. Time urgency: the construct and its measurement. Journal of Applied Psychology 1991;76(5):644-57. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lappalainen 2007
- Lappalainen R, Lehtonen T, Skarp E, Taubert E, Ojanen M, Hayes SC. The impact of CBT and ACT models using psychology trainee therapists: a preliminary controlled effectiveness trial. Behavior Modification 2007;31(4):488-511. [DOI: 10.1177/0145445506298436] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lateef 2011
- Lateef F. Patient expectations and the paradigm shift of care in emergency medicine. Journal of Emergencies, Trauma, and Shock 2011;4(2):163–7. [DOI: 10.4103/0974-2700.82199] [PMC3132352] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lavin Venegas 2019
- Lavin Venegas C, Nkangu MN, Duffy MC, Fergusson DA, Spilg EG. Interventions to improve resilience in physicians who have completed training: a systematic review. PLoS ONE 2019;14(1):e0210512. [DOI: 10.1371/journal.pone.0210512] [PMC6336384] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lawler 1992
- Lawler KA, Schmied LA. A prospective study of women's health: the effects of stress, hardiness, locus of control, Type A behavior, and physiological reactivity. Women Health 1992;19(1):27-41. [DOI: 10.1300/J013v19n01_02] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lazarus 1987
- Lazarus RS, Folkman S. Transactional theory and research on emotions and coping. European Journal of Personality 1987;1(3):141-69. [DOI: 10.1002/per.2410010304] [DOI] [Google Scholar]
Lebares 2019 [pers comm]
- Lebares C. Information about time points and number of participants analysed for psychological outcomes [personal communication]. Email to: A Kunzler 30 August 2019.
Lechner 2007
- Lechner L, Bolman C, Van Dalen A. Definite involuntary childlessness: associations between coping, social support and psychological distress. Human Reproduction 2007;22(1):288-94. [DOI: 10.1093/humrep/del327] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lee 2013
- Lee JH, Nam SK, Kim AR, Kim B, Lee MY, Lee SM. Resilience: a meta-analytic approach. Journal of Counseling and Development 2013;91(3):269-79. [DOI: 10.1002/j.1556-6676.2013.00095.x] [DOI] [Google Scholar]
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Leonelli 2017
- Leonelli LB, Andreoni S, Martins P, Kozasa EH, Salvo VL, Sopezki D, et al. Perceived stress among primary health care professionals in Brazil. Revista Brasileira de Epidemiologia 2017;20(2):286-98. [DOI: 10.1590/1980-5497201700020009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Leppin 2014
- Leppin AL, Bora PR, Tilburt JC, Gionfriddo MR, Zeballos-Palacios C, Dulohery MM, et al. The efficacy of resiliency training programs: a systematic review and meta-analysis of randomized trials. PLoS ONE 2014;9(10):e111420. [DOI: 10.1371/journal.pone.0111420] [PMC4210242 ] [PROSPERO #CRD42014007185] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Levenstein 1993
- Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Luzi C, et al. Development of the Perceived Stress Questionnaire: a new tool for psychosomatic research. Journal of Psychosomatic Research 1993;37(1):19-32. [DOI: 10.1016/0022-3999(93)90120-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Li 2003
- Li C, Shi-Kan. The influence of distributive justice and procedural justice on job burnout [分配公平与程序公平对工作倦怠的影响]. Acta Psychologica Sinica 2003;35(5):677–84. [journal.psych.ac.cn/xlxb/EN/Y2003/V35/I05/677#1] [Google Scholar]
Li 2011
- Li T, Puhan MA, Vedula SS, Singh S, Dickersin K, The Ad Hoc Network Meta-analysis Methods Meeting Working Group. Network meta-analysis-highly attractive but more methodological research is needed. BMC Medicine 2011;9:79. [DOI: 10.1186/1741-7015-9-79] [PMC3159133] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2017
- Li SH, Graham BM. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatry 2017;4(1):73-82. [DOI: 10.1016/S2215-0366(16)30358-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Li 2019
- Li T, Higgins JP, Deeks JJ (editors). Chapter 5: Collecting data. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Liebenberg 2012
- Liebenberg L, Ungar M, Van de Vijver F. Validation of the Child and Youth Resilience Measure-28 (CYRM-28) among Canadian youth. Research on Social Work Practice 2012;22(2):219-26. [DOI: 10.1177/1049731511428619] [DOI] [Google Scholar]
Liebenberg 2013
- Liebenberg L, Ungar M, LeBlanc JC. The CYRM-12: a brief measure of resilience. Canadian Journal of Public Health 2013;104(2):e131-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Linde 2016
- Linde K, Rücker G, Schneider A, Kriston L. Questionable assumptions hampered interpretation of a network meta-analysis of primary care depression treatments. Journal of Clinical Epidemiology 2016;71:86-96. [DOI: 10.1016/j.jclinepi.2015.10.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Locke 2007
- Locke DE, Decker PA, Sloan JA, Brown PD, Malec JF, Clark MM, et al. Validation of single-item linear analog scale assessment of quality of life in neuro-oncology patients. Journal of Pain and Symptom Management 2007;34(6):628-38. [DOI: 10.1016/j.jpainsymman.2007.01.016] [PMC2732111] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Loprinzi 2011
- Loprinzi CE, Prasad K, Schroeder DR, Sood A. Stress Management and Resilience Training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: a pilot randomized clinical trial. Clinical Breast Cancer 2011;11(6):364-8. [DOI: 10.1016/j.clbc.2011.06.008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lovibond 1995
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd edition. Sydney (NSW): School of Psychology, University of New South Wales, 1995. [Google Scholar]
Lu 2006
- Lu G, Ades AE. Assessing evidence inconsistency in mixed treatment comparisons. Journal of the American Statistical Association 2006;101(474):447-59. [DOI: 10.1198/016214505000001302] [DOI] [Google Scholar]
Lu 2016
- Lu Y, Hu XM, Huang XL, Zhuang XD, Guo P, Feng LF, et al. Job satisfaction and associated factors among healthcare staff: a cross-sectional study in Guangdong Province, China. BMJ Open 2016;6(7):e011388. [DOI: 10.1136/bmjopen-2016-011388] [PMC4964254] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lua 2008
- Lua HJ. The Mediating Role of Work Stress and Burnout Management Self-Efficacy in the Job Demand–Resources Model [Master's thesis]. Warsaw: SWPS University of Social Sciences and Humanities, 2008. [Google Scholar]
Lumley 2002
- Lumley T. Network meta-analysis for indirect treatment comparisons. Statistics in Medicine 2002;21(16):2313-24. [DOI: 10.1002/sim.1201] [PMID: ] [DOI] [PubMed] [Google Scholar]
Luo 2015
- Luo T, Cheng X, Xiong Y. Relationship among resilience, coping style and mental health of newly recruited workers born after 1990 in manufacturing industry of Shenzhen City. Journal of Hygiene Research 2015;44(2):252-6. [PMID: ] [PubMed] [Google Scholar]
Luszczynska 2009
- Luszczynska A, Benight CC, Cieslak R. Self-efficacy and health-related outcomes of collective trauma. European Psychologist 2009;14(1):51-62. [DOI: 10.1027/1016-9040.14.1.51] [DOI] [Google Scholar]
Luthar 2000a
- Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Development 2000;71(3):543-62. [NIHMS21559] [PMC1885202] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luthar 2000b
- Luthar SS, Suchman NE. Relational psychotherapy mothers' group: a developmentally informed intervention for at-risk mothers. Development and Psychopathology 2000;12(2):235-53. [DOI: 10.1017/s0954579400002078] [PMC3313648] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luthar 2007
- Luthar SS, Suchman NE, Altomare M. Relational psychotherapy mothers’ group: a randomized clinical trial for substance abusing mothers. Development and Psychopathology 2007;19(1):243-61. [DOI: 10.1017/S0954579407070137] [PMC2190295 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luthar 2015
- Luthar SS. Mothering mothers. Research in Human Development 2015;12(3-4):295–303. [DOI: 10.1080/15427609.2015.1068045] [PMC4827931] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luthar 2017a
- Luthar SS, Eisenberg N. Resilient adaptation among at-risk children: harnessing science toward maximizing salutary environments. Child Development 2017;88(2):337–49. [DOI: 10.1111/cdev.12737] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lyon 2001
- Lyon DE, Younger JB. Purpose in life and depressive symptoms in persons living with HIV disease. Journal of Nursing Scholarship 2001;33(2):129-33. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lyubomirsky 1999
- Lyubomirsky S, Leppern HS. A measure of subjective happiness: preliminary reliability and construct validation. Social Indicators Research 1999;46(2):137-55. [DOI: 10.1023/A:1006824100041] [DOI] [Google Scholar]
Maben 2018
- Maben J, Taylor C, Dawson J, Leamy M, McCarthy I, Reynolds E, et al. A realist informed mixed-methods evaluation of Schwartz Center Rounds® in England. Health Services and Delivery Research 2018;6(37):1-262. [DOI: 10.3310/hsdr06370] [PMID: ] [DOI] [PubMed] [Google Scholar]
Macedo 2014
- Macedo T, Wilheim L, Gonçalves R, Coutinho ES, Vilete L, Figueira I, et al. Building resilience for future adversity: a systematic review of interventions in non-clinical samples of adults. BMC Psychiatry 2014;14:227. [DOI: 10.1186/s12888-014-0227-6] [PMC4149241 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mache 2017a [pers comm]
- Mache S. Number of participants randomised and potential per-protocol analysis; form of control group [personal communication]. Email to: A Kunzler 21 September 2017.
Mache 2017b [pers comm]
- Mache S. Number of participants randomised and potential per-protocol analysis [personal communication]. Email to: A Kunzler 21 September 2017.
Mache 2018 [pers comm]
- Mache S. Number of participants randomised and potential per-protocol analysis [personal communication]. Email to: A Kunzler 22 July 2018.
Mache 2019a [pers comm]
- Mache S. Correct that performed per-protocol analysis with n = 44 in IG and n = 42 in CG [personal communication]. Email to: A Kunzler 4 September 2019.
Mache 2019b [pers comm]
- Mache S. Correct that available case analysis with participants for whom outcomes were obtained at follow-up assessments [personal communication]. Email to: A Kunzler 4 September 2019.
Machin 1997
- Machin D, Campbell M, Fayers P, Pinol A. Sample Size Tables for Clinical Studies. 2nd edition. Malden, MA: Blackwell Science, 1997. [Google Scholar]
Maddi 1987
- Maddi SR. Hardiness training at Illinois Bell Telephone. In: Opatz J, editors(s). Health Promotion Evaluation. Stephens Point (WI): National Wellness Institute, 1987:101-15. [Google Scholar]
Maddi 1998
- Maddi SR, Kahn S, Maddi KL. The effectiveness of hardiness training. Consulting Psychology Journal: Practice and Research 1998;50(2):78-86. [DOI: 10.1037/1061-4087.50.2.78] [DOI] [Google Scholar]
Maddi 2001
- Maddi SR, Khoshaba DM. HardiSurvey III-R: Test Development and Internet Instruction Manual. Irvine (CA): Hardiness Institute, 2001. [Google Scholar]
Maddi 2009
- Maddi SR, Harvey RH, Khoshaba DM, Fazel M, Resurreccion N. Hardiness training facilitates performance in college. Journal of Positive Psychology 2009;4(6):566-77. [DOI: 10.1080/17439760903157133] [DOI] [Google Scholar]
Madsen 2010
- Madsen MD, Abell N. Trauma Resilience Scale: validation of protective factors associated with adaptation following violence. Research on Social Work Practice 2010;20(2):223-33. [DOI: 10.1177/1049731509347853] [DOI] [Google Scholar]
Malarkey 2013
- Malarkey WB, Jarjoura D, Klatt M. Workplace based mindfulness practice and inflammation: a randomized trial. Brain, Behavior, and Immunity 2013;27(1):145–54. [DOI: 10.1016/j.bbi.2012.10.009] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Malouff 2007
- Malouff JM, Thorsteinsson EB, Schutte NS. The efficacy of problem solving therapy in reducing mental and physical health problems: a meta-analysis. Clinical Psychology Review 2007;27(1):46‐57. [DOI: 10.1016/j.cpr.2005.12.005] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mancini 2009
- Mancini AD, Bonanno GA. Predictors and parameters of resilience to loss: toward an individual differences model. Journal of Personality 2009;77(6):1805-32. [DOI: 10.1111/j.1467-6494.2009.00601.x] [PMC4224188] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marchand 2015
- Marchand A, Durand P, Haines V, Harvey S. The multilevel determinants of workers’ mental health: Results from the SALVEO study. Social Psychiatry and Psychiatric Epidemiology 2015;50(3):445–59. [DOI: 10.1007/s00127-014-0932-y] [PMID: ] [DOI] [PubMed] [Google Scholar]
Martin‐Krumm 2003
- Martin-Krumm CP, Sarrazin PG, Peterson C, Famose J-P. Explanatory style and resilience after sports failure. Personality and Individual Differences 2003;35(7):1685-95. [DOI: 10.1016/S0191-8869(02)00390-2] [DOI] [Google Scholar]
Marty 2010
- Marty MA, Segal DL, Coolidge FL. Relationships among dispositional coping strategies, suicidal ideation, and protective factors against suicide in older adults. Aging and Mental Health 2010;14(8):1015-23. [DOI: 10.1080/13607863.2010.501068] [PMID: ] [DOI] [PubMed] [Google Scholar]
Maslach 1981
- Maslach C, Jackson SE. The measurement of experienced burnout. Journal of Organizational Behavior 1981;2(2):99–113. [DOI: 10.1002/job.4030020205] [DOI] [Google Scholar]
Maslach 1986
- Maslach C, Jackson SE. Maslach Burnout Inventory. Palo Alto (CA): Consulting Psychologists Press, 1986. [Google Scholar]
Maslach 1996
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd edition. Palo Alto (CA): Consulting Psychologists Press, 1996. [Google Scholar]
Maslach 1997
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. In: Zalaquett CP, Wood RJ, editors(s). Evaluating Stress: A Book of Resources. Lanham (MD): Scarecrow Education, 1997:191-218. [Google Scholar]
Massey 2019
- Massey CN, Feig EH, Duque-Serrano L, Wexler D, Moskowitz JT, Huffman JC. Well-being interventions for individuals with diabetes: a systematic review. Diabetes Research and Clinical Practice 2019;147:118-33. [DOI: 10.1016/j.diabres.2018.11.014] [PMC6370485 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Masten 2001
- Masten AS. Ordinary magic: resilience processes in development. Amercian Psychologist 2001;56(3):227-38. [PMID: ] [DOI] [PubMed] [Google Scholar]
McAllister 2009
- McAllister M, McKinnon J. The importance of teaching and learning resilience in the health disciplines: a critical review of the literature. Nurse Education Today 2009;29(4):371-9. [DOI: 10.1016/j.nedt.2008.10.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
McCann 2013
- McCann CM, Beddoe E, McCormick K, Huggard P, Kedge S, Adamson C, et al. Resilience in the health professions: a review of recent literature. International Journal of Wellbeing 2013;3(1):60-81. [DOI: 10.5502/ijw.v3i1.4] [DOI] [Google Scholar]
McCue 1991
- McCue JD, Sachs CL. A stress management workshop improves residents’ coping skills. Archives of Internal Medicine 1991;151(11):2273-7. [PMID: ] [PubMed] [Google Scholar]
McDonald 2013
- McDonald G, Jackson D, Wilkes L, Vickers MH. Personal resilience in nurses and midwives: effects of a work-based educational intervention. Contemporary Nurse 2013;45(1):134-43. [DOI: 10.5172/conu.2013.45.1.134] [PMID: ] [DOI] [PubMed] [Google Scholar]
McEwen 1998
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine 1998;338(3):171–9. [DOI: 10.1056/NEJM199801153380307] [PMID: ] [DOI] [PubMed] [Google Scholar]
McEwen 2003
- McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Hormones and Behavior 2003;43(1):2–15. [DOI: 10.1016/s0018-506x(02)00024-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
McIntosh 2012
- McIntosh RC, Rosselli M. Stress and coping in women living with HIV: a meta-analytic review. AIDS Behavior 2012;16(8):2144-59. [DOI: 10.1007/s10461-012-0166-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
McLarnon 2013
- McLarnon MJ, Rothstein MG. Development and initial validation of the Workplace Resilience Inventory. Journal of Personnel Psychology 2013;12(2):63-73. [DOI: 10.1027/1866-5888/a000084] [DOI] [Google Scholar]
McManus 2002
- McManus IC, Winder BC, Gordon D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet 2002;359(9323):2089-90. [DOI: 10.1016/S0140-6736(02)08915-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
McVicar 2003
- McVicar A. Workplace stress in nursing: a literature review. Journal of Advanced Nursing 2003;44(6):633–42. [DOI: 10.1046/j.0309-2402.2003.02853.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mealer 2009
- Mealer M, Burnham EL, Goode CJ, Rothbaum B, Moss M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depression and Anxiety 2009;26(12):1118-26. [DOI: 10.1002/da.20631] [PMC2919801 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mealer 2017 [pers comm]
- Mealer M. Descriptive statistics (means and SDs) for outcome measures in two groups at each time point [personal communication]. Email to: A Kunzler 11 September 2017.
Meichenbaum 1977
- Meichenbaum D. Cognitive-Behavioral Modification: An Integrative Approach. New York (NY): Plenum Press, 1977. [Google Scholar]
Meichenbaum 2007
- Meichenbaum D. Stress inoculation training: a preventative and treatment approach. In: Lehrer PM, Woolfolk RL, Sime WS, editors(s). Principles and Practice of Stress Management. 3rd edition. New York (NY): Guilford Press, 2007:497-518. [Google Scholar]
Meltzer 2008
- Meltzer H, Griffiths C, Brock A, Rooney C, Jenkins R. Patterns of suicide by occupation in England and Wales: 2001–2005. British Journal of Psychiatry 2008;193(1):73-6. [DOI: 10.1192/bjp.bp.107.040550] [PMID: ] [DOI] [PubMed] [Google Scholar]
Michael 2003
- Michael ST, Crowther MR, Schmid B, Allen RS. Widowhood and spirituality: coping responses to bereavement. Journal of Women & Aging 2003;15(2-3):145-65; discussion 185-7. [DOI: 10.1300/J074v15n02_09] [PMID: ] [DOI] [PubMed] [Google Scholar]
Michie 2003
- Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occupational and Environmental Medicine 2003;60(1):3-9. [DOI: 10.1136/oem.60.1.3] [PMC1740370] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mills 2012
- Mills EJ, Ioannidis JP, Thorlund K, Schünemann HJ, Puhan MA, Guyatt GH. How to use an article reporting a multiple treatment comparison meta-analysis. JAMA 2012;308(12):1246-53. [DOI: 10.1001/2012.jama.11228] [PMID: ] [DOI] [PubMed] [Google Scholar]
Milne 2016
- Milne T, Creedy DK, West R. Integrated systematic review on educational strategies that promote academic success and resilience in undergraduate indigenous students. Nurse Education Today 2016;36:387-94. [DOI: 10.1016/j.nedt.2015.10.008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Milte 2015
- Milte CM, Luszcz MA, Ratcliffe J, Masters S, Crotty M. Influence of health locus of control on recovery of function in recently hospitalized frail older adults. Geriatrics & Gerontology International 2015;15(3):341-9. [DOI: 10.1111/ggi.12281] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mimura 2003
- Mimura C, Griffiths P. The effectiveness of current approaches to workplace stress management in the nursing profession: an evidence based literature review. Occupational and Environmental Medicine 2003;60(1):10-5. [DOI: 10.1136/oem.60.1.10] [PMC1740380 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Min 2013
- Min JA, Yu JJ, Lee CU, Chae JH. Cognitive emotion regulation strategies contributing to resilience in patients with depression and/or anxiety disorders. Comprehensive Psychiatry 2013;54(8):1190-7. [DOI: 10.1016/j.comppsych.2013.05.008] [DOI] [PubMed] [Google Scholar]
Mistretta 2018 [pers comm]
- Mistretta E. Information concerning potential cluster randomisation [personal communication]. Email to: A Kunzler 30 August 2018.
Moberly 2018
- Moberly T. Sickness absence rates across the NHS. BMJ 2018;361:k2210. [DOI: 10.1136/bmj.k2210] [DOI] [PubMed] [Google Scholar]
Moffitt 2011
- Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proceedings of the National Academy of Sciences of the United States of America 2011;108(7):2693-8. [DOI: 10.1073/pnas.1010076108] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ 2009;339:b2535. [DOI: 10.1136/bmj.b2535] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohr 2014
- Mohr DC, Ho J, Hart TL, Baron KG, Berendsen M, Beckner V, et al. Control condition design and implementation features in controlled trials: a meta-analysis of trials evaluating psychotherapy for depression. Translational Behavioral Medicine 2014;4(4):407-23. [DOI: 10.1007/s13142-014-0262-3] [PMC4286544] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moran 1998
- Moran CC. Stress and emergency work experience: a non‐linear relationship. Disaster Prevention and Management 1998;7(1):38-46. [DOI: 10.1108/09653569810206271] [DOI] [Google Scholar]
Moritz 2019
- Moritz S, Nestoriuc Y, Rief W, Klein JP, Jelinek L, Peth J. It can't hurt, right? Adverse effects of psychotherapy in patients with depression. European Archives of Psychiatry and Clinical Neuroscience 2019;269(5):577-86. [DOI: 10.1007/s00406-018-0931-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
Morris 2013
- Morris MC, Rao U. Psychobiology of PTSD in the acute aftermath of trauma: integrating research on coping, HPA function and sympathetic nervous system activity. Asian Journal of Psychiatry 2013;6(1):3-21. [DOI: 10.1016/j.ajp.2012.07.012] [PMC3565157] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moskowitz 2009
- Moskowitz JT, Hult JR, Bussolari C, Acree M. What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychological Bulletin 2009;135(1):121-41. [DOI: 10.1037/a0014210] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mueller 1990
- Mueller CW, McCloskey JC. Nurses’ job satisfaction: a proposed measure. Nursing Research 1990;39(2):113-7. [DOI: 10.1097/00006199-199003000-00014] [DOI] [PubMed] [Google Scholar]
Myhren 2010
- Myhren H, Ekeberg O, Tøien K, Karlsson S, Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Critical Care 2010;14(1):R14. [DOI: 10.1186/cc8870] [PMC2875529] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Natvik 2011
- Natvik S, Bjorvatn B, Moen BE, Magerøy N, Sivertsen B, Pallesen S. Personality factors related to shift work tolerance in two- and three-shift workers. Applied Ergonomics 2011;42(5):719-24. [DOI: 10.1016/j.apergo.2010.11.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nazroo 1998
- Nazroo JY, Edwards AC, Brown GW. Gender differences in the prevalence of depression: artefact, alternative disorders, biology or roles? Sociology of Health & Illness 1998;20(3):312-30. [DOI: 10.1111/1467-9566.00104] [DOI] [Google Scholar]
Netemeyer 1996
- Netemeyer RG, Boles JS, McMurrian R. Development and validation of work family conflict and family-work conflict scales. Journal of Applied Psychology 1996;81(4):400–10. [DOI: 10.1037/0021-9010.81.4.400] [DOI] [Google Scholar]
Nezu 1988
- Nezu AM, Nezu CM, Blissett SE. Sense of humor as a moderator of the relation between stressful events and psychological distress: a prospective analysis. Journal of Personality and Social Psychology 1988;54(3):520-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nezu 2013
- Nezu AM, Nezu CM, D' Zurilla TJ. Problem-Solving Therapy. A Treatment Manual. New York (NY): Springer Publishing Company, 2013. [Google Scholar]
Norris 2009
- Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Social Science and Medicine 2009;68(12):2190-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Northouse 2002
- Northouse LL, Mood D, Kershaw T, Schafenacker A, Mellon S, Walker J, et al. Quality of life of women with recurrent breast cancer and their family members. Journal of Clinical Oncology 2002;20(19):4050-64. [DOI: 10.1200/JCO.2002.02.054] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nowack 1989
- Nowack KM. Coping style, cognitive hardiness, and health status. Journal of Behavioral Medicine 1989;12(2):145-58. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nowack 1990
- Nowack KM. Initial development of an inventory to assess stress and health risk. American Journal of Health Promotion 1990;4(3):173-80. [DOI: 10.4278/0890-1171-4.3.173] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nowlan 2015
- Nowlan JS, Wuthrich VM, Rapee RM. Positive reappraisal in older adults: a systematic literature review. Aging and Mental Health 2015;19(6):475-84. [DOI: 10.1080/13607863.2014.954528] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nuebling 2010
- Nuebling M, Hasselhorn HM. The Copenhagen Psychosocial Questionnaire in Germany: from the validation of the instrument to the formation of a job-specific database of psychosocial factors at work. Scandinavian Journal of Public Health 2010;38(3 Suppl):120–4. [DOI: 10.1177/1403494809353652] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nugent 1993
- Nugent WR, Thomas JW. Validation of a clinical measure of self-esteem. Research on Social Work Practice 1993;3(2):191-207. [Google Scholar]
Oettingen 2000
- Oettingen G, Honig G, Gollwitzer PM. Effective self-regulation of goal attainment. International Journal of Educational Research 2000;33:705–32. [www.socmot.uni-konstanz.de/sites/default/files/00_Oettingen_Hoenig_Gollitzer_Goal_Attain.pdf] [Google Scholar]
Ong 2006
- Ong AD, Bergeman CS, Bisconti TL, Wallace KA. Psychological resilience, positive emotions, and successful adaptation to stress in later life. Journal of Personality and Social Psychology 2006;91(4):730-49. [DOI: 10.1037/0022-3514.91.4.730] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ong 2016
- Ong YZ, Siddiqui S, John S, Chen Z, Chang S. The prevalence of post-traumatic stress disorder in intensive care unit staff and the common coping strategies used. Annals of the Academy of Medicine, Singapore 2016;45(5):215-8. [PMID: ] [PubMed] [Google Scholar]
Orengo 2001
- Orengo CA, Wei SH, Molinari VA, Hale DD, Kunik ME. Functioning in rheumatoid arthritis: the role of depression and self-efficacy. Clinical Gerontologist 2001;23(3-4):45-56. [DOI: 10.1300/J018v23n03_05] [DOI] [Google Scholar]
Oshio 2002
- Oshio A, Nakaya N, Kaneko H, Nagamine S. Development and validation of an Adolescent Resilience Scale. Japanese Journal of Counseling Science 2002;35:57-65. [Google Scholar]
Oshio 2003
- Oshio A, Kaneko H, Nagamine S, Nayaka M. Construct validity of the Adolescent Resilience Scale. Psychological Reports 2003;93(3 Pt 2):1217-22. [PMID: ] [DOI] [PubMed] [Google Scholar]
Owens 2009
- Owens GP, Steger MF, Whitesell AA, Herrera CJ. Posttraumatic stress disorder, guilt, depression, and meaning in life among military veterans. Journal of Traumatic Stress 2009;22(6):654-7. [DOI: 10.1002/jts.20460] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ozbay 2007
- Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D 3rd, Southwick SM. Social support and resilience to stress. Psychiatry 2007;4(5):35-40. [PMC2921311] [PMC free article] [PubMed] [Google Scholar]
Ozer 2003
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin 2003;129(1):52-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pace 2012
- Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. International Journal of Nursing Studies 2012;49(1):47-53. [DOI: 10.1016/j.ijnurstu.2011.07.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Page 2005
- Page K. Subjective Wellbeing in the Workplace [BA thesis]. Geelong, Victoria: Deakin University, 2005. [Google Scholar]
Page 2019
- Page MJ, Higgins JP, Sterne JA. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Pallavicini 2016
- Pallavicini F, Argenton L, Toniazzi N, Aceti L, Mantovani F. Virtual reality applications for stress management training in the military. Aerospace Medicine and Human Performance 2016;87(12):1021-30. [DOI: 10.3357/AMHP.4596.2016] [PMID: ] [DOI] [PubMed] [Google Scholar]
Panagioti 2017
- Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Internal Medicine 2017;177(2):195-205. [DOI: 10.1001/jamainternmed.2016.7674] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pangallo 2015
- Pangallo A, Zibarras L, Lewis R, Flaxman P. Resilience through the lens of interactionism: a systematic review. Psychological Assessment 2015;27(1):1-20. [DOI: 10.1037/pas0000024] [PMID: ] [DOI] [PubMed] [Google Scholar]
Papadatou 2000
- Papadatou D. A proposed model of health professionals grieving process. Omega: Journal of Death and Dying 2000;41(1):59–77. [DOI: 10.2190/TV6M-8YNA-5DYW-3C1E] [DOI] [Google Scholar]
Pargament 2000
- Pargament KI, Koenig HG, Perez L. The many methods of religious coping: development and initial validation of the RCOPE. Journal of Clinical Psychology 2000;56(4):519-43. [PMID: ] [DOI] [PubMed] [Google Scholar]
Paris 2010
- Paris M Jr, Hoge MA. Burnout in the mental health workforce: a review. Journal of Behavioral Health Services & Research 2010;37(4):519–28. [DOI: 10.1007/s11414-009-9202-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Park 2008
- Park CL, Edmondson D, Fenster JR, Blank TO. Meaning making and psychological adjustment following cancer: the mediating roles of growth, life meaning, and restored just-world beliefs. Journal of Consulting and Clinical Psychology 2008;76(5):863-75. [DOI: 10.1037/a0013348] [PMID: ] [DOI] [PubMed] [Google Scholar]
Park 2015
- Park M, Chang ER, You S. Protective role of coping flexibility in PTSD and depressive symptoms following trauma. Personality and Individual Differences 2015;82:102-6. [DOI: 10.1016/j.paid.2015.03.007] [DOI] [Google Scholar]
Paterson 2013
- Paterson C, Jones M, Rattray J, Lauder W. Exploring the relationship between coping, social support and health-related quality of life for prostate cancer survivors: a review of the literature. European Journal of Oncology Nursing 2013;17(6):750-9. [DOI: 10.1016/j.ejon.2013.04.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pekurinen 2017
- Pekurinen V, Willman L, Virtanen M, Kivimäki M, Vahtera J, Välimäki M. Patient aggression and the wellbeing of nurses: a cross-sectional survey study in psychiatric and non-psychiatric settings. International Journal of Environmental Research and Public Health 2017;14(10):1245. [DOI: 10.3390/ijerph14101245] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pennebaker 1986
- Pennebaker JW, Beall SK. Confronting a traumatic event: toward an understanding of inhibition and disease. Journal of Abnormal Psychology 1986;95(3):274-81. [DOI: 10.1037/0021-843X.95.3.274] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pesantes 2015
- Pesantes MA, Lazo-Porras M, Abu Dabrh AM, Ávila-Ramírez JR, Caycho M, Villamonte GY, et al. Resilience in vulnerable populations with type 2 diabetes mellitus and hypertension: a systematic review and meta-analysis. Canadian Journal of Cardiology 2015;31(9):1180-8. [DOI: 10.1016/j.cjca.2015.06.003] [PMC4556590 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Peter 2012
- Peter C, Müller R, Cieza A, Geyh S. Psychological resources in spinal cord injury: a systematic literature review. Spinal Cord 2012;50(3):188-201. [DOI: 10.1038/sc.2011.125] [PMID: 22124343] [DOI] [PubMed] [Google Scholar]
Peters 2008
- Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal of Clinical Epidemiology 2008;61(10):991-6. [DOI: 10.1016/j.jclinepi.2007.11.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Petree 2012
- Petree RD, Broome KM, Bennett JB. Exploring and reducing stress in young restaurant workers: results of a randomized field trial. American Journal of Health Promotion 2012;26(4):217-24. [DOI: 10.4278/ajhp.091001-QUAN-321] [PMID: ] [DOI] [PubMed] [Google Scholar]
Petrie 2019
- Petrie K, Crawford J, Baker ST, Dean K, Robinson J, Veness BG, et al. Interventions to reduce symptoms of common mental disorders and suicidal ideation in physicians: a systematic review and meta-analysis. Lancet Psychiatry 2019;6(3):225-34. [DOI: 10.1016/S2215-0366(18)30509-1] [DOI] [PubMed] [Google Scholar]
Petriwskyj 2016
- Petriwskyj A, Parker D, O'Dwyer S, Moyle W, Nucifora N. Interventions to build resilience in family caregivers of people living with dementia: a comprehensive systematic review. JBI Database of Systematic Reviews and Implementation Reports 2016;14(6):238-73. [DOI: 10.11124/JBISRIR-2016-002555] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pezaro 2017
- Pezaro S, Clyne W, Fulton EA. A systematic mixed-methods review of interventions, outcomes and experiences for midwives and student midwives in work-related psychological distress. Midwifery 2017;50:163-73. [DOI: 10.1016/j.midw.2017.04.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Piepho 2012
- Piepho HP, Williams ER, Madden LV. The use of two-way linear mixed models in multitreatment meta-analysis. Biometrics 2012;68(4):1269-77. [DOI: 10.1111/j.1541-0420.2012.01786.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Piepho 2014
- Piepho HP. Network-meta analysis made easy: detection of inconsistency using factorial analysis-of-variance models. BMC Medical Research Methodology 2014;14:61. [DOI: 10.1186/1471-2288-14-61] [PMC4049370] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pietrzak 2013
- Pietrzak RH, Cook JM. Psychological resilience in older U.S. veterans: results from the national health and resilience in veterans study. Depression and Anxiety 2013;30(5):432-43. [DOI: 10.1002/da.22083] [PMID: ] [DOI] [PubMed] [Google Scholar]
Piiparinen 2003
- Piiparinen RA, Smith JC. Stress symptoms of two groups before and after the terrorist attacks of 9/11/01. Perceptual and Motor Skills 2003;97(2):360-4. [DOI: 10.2466/pms.2003.97.2.360] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pine 2007
- Pine R, Tart K. Return on investment: benefits and challenges of baccalaureate nurse residency program. Nursing Economics 2007;25(1):13-8. [PMID: ] [PubMed] [Google Scholar]
Pisanti 2008
- Pisanti R, Lombardo C, Lucidi F, Lazzari D, Bertini M. Development and validation of a brief Occupational Coping Self-Efficacy Questionnaire for Nurses. Journal of Advanced Nursing 2008;62(2):238-47. [DOI: 10.1111/j.1365-2648.2007.04582.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pragodpol 2013
- Pragodpol P, Ryan C. Critical review of factors predicting health-related quality of life in newly diagnosed coronary artery disease patients. Journal of Cardiovascular Nursing 2013;28(3):277-84. [DOI: 10.1097/JCN.0b013e31824af56e] [PMID: ] [DOI] [PubMed] [Google Scholar]
Prati 2009
- Prati G, Pietrantoni L. Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: a meta-analysis. Journal of Loss and Trauma 2009;14(5):364-88. [DOI: 10.1080/15325020902724271] [DOI] [Google Scholar]
Profit 2018 [pers comm]
- Profit J. Trial and publication status [personal communication]. Email to: A Kunzler 2 April 2018.
Quale 2010
- Quale AJ, Schanke AK. Resilience in the face of coping with a severe physical injury: a study of trajectories of adjustment in a rehabilitation setting. Rehabilitation Psychology 2010;55(1):12-22. [DOI: 10.1037/a0018415] [PMID: ] [DOI] [PubMed] [Google Scholar]
R 2019 [Computer program]
- R Foundation for Statistical Computing R: A language and environment for statistical computing. Version 3.5.3. Vienna, Austria: R Foundation for Statistical Computing, 2019.Available at www.r-project.org.
Rabow 2001
- Rabow MW, McPhee SJ. Doctoring to heal: fostering well-being among physicians through personal reflection. Western Journal of Medicine 2001;174(1):66-9. [DOI: 10.1136/ewjm.174.1.66] [PMC1157069 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Radloff 1977
- Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Applied Psychological Measurement 1977;1(3):385-401. [DOI: 10.1177/014662167700100306] [DOI] [Google Scholar]
Raffety 1986
- Rafferty JP, Lemkau JP, Purdy RR, Rudisill JR. Validity of the Maslach Burnout Inventory for family practice physicians. Journal of Clinical Psychology 1986;42(3):488-92. [DOI: ] [3711351] [DOI] [PubMed] [Google Scholar]
Raj 2016
- Raj KS. Well-being in residency: a systematic review. Journal of Graduate Medical Education 2016;8(5):674–84. [DOI: 10.4300/JGME-D-15-00764.1] [PMC5180521] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramirez 1995
- Ramirez AJ, Graham J, Richards MA, Cull A, Gregory W, Leaning M, et al. Burnout and psychiatric disorder among cancer clinicians. British Journal of Cancer 1995;71(6):1263‐9. [DOI: 10.1038/bjc.1995.244] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Regehr 2014
- Regehr C, Glancy D, Pitts A, LeBlanc VR. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. Journal of Nervous and Mental Disease 2014;202(5):353–9. [DOI: 10.1097/NMD.0000000000000130] [PMID: ] [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Reyes 2018
- Reyes AT, Kearney CA, Lee H, Isla K, Estrada J. Interventions for posttraumatic stress with resilience as outcome: an integrative review. Issues in Mental Health Nursing 2018;39(2):166-78. [DOI: 10.1080/01612840.2017.1390801] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rezaeiian 2002
- Rezaeiian A. Basics of Organizational Behavior Management. Tehran: Side Publishing, 2012. [Google Scholar]
Ricard 2014
- Ricard M, Lutz A, Davidson RJ. Mind of the meditator. Scientific American 2014;311(5):38-45. [DOI: 10.1038 /scientificamerican1114-38] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rich unpublished manuscript
- Rich UL. An investigation into the modification of personality hardiness. Unpublished manuscript.
Riecher‐Rössler 2017
- Riecher-Rössler A. Sex and gender differences in mental disorders. Lancet Psychiatry 2017;4(1):8-9. [DOI: 10.1016/S2215-0366(16)30348-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Riley 2017
- Riley KE, Park CL, Wilson A, Sabo AN, Antoni, MH, Braun TD, et al. Improving physical and mental healthin frontline mental health care providers: yoga-based stress management versus cognitive behavioral stress management. Journal of Workplace Behavioral Health Volume 2017;32(1):26–48. [DOI: 10.1080/15555240.2016.1261254] [DOI] [PMC free article] [PubMed] [Google Scholar]
Robertson 2010
- Robertson N, Perry A. Institutionally based health care workers' exposure to traumatogenic events: systematic review of PTSD presentation. Journal of Traumatic Stress 2010;23(3):417-20. [DOI: 10.1002/jts.20537] [PMID: ] [DOI] [PubMed] [Google Scholar]
Robertson 2015
- Robertson IT, Cooper CL, Sarkar M, Curran T. Resilience training in the workplace from 2003 to 2014: a systematic review. Journal of Occupational and Organizational Psychology 2015;88(3):533-62. [DOI: 10.1111/joop.12120] [DOI] [Google Scholar]
Robertson 2016
- Robertson HD, Elliott AM, Burton C, Iversen L, Murchie P, Porteous T, et al. Resilience of primary healthcare professionals: a systematic review. British Journal of General Practice 2016;66(647):e423-33. [DOI: 10.3399/bjgp16X685261] [PMC4871308 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rogala 2019 [pers comm]
- Rogala A. Subgroup data for health and human service professionals (physicians, nurses, first responders, social workers, psychotherapists) [personal communication]. Email to: A Kunzler 8 March 2019.
Rogers 2016
- Rogers D. Which educational interventions improve healthcare professionals' resilience? Medical Teacher 2016;38(12):1236-41. [DOI: 10.1080/0142159x.2016.1210111] [DOI] [PubMed] [Google Scholar]
Romppanen 2017
- Romppanen J, Häggman-Laitila A. Interventions for nurses' well-being at work: a quantitative systematic review. Journal of Advanced Nursing 2017;73(7):1555-69. [DOI: 10.1111/jan.13210] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rose 2013
- Rose RD, Buckey JC Jr, Zbozinek TD, Motivala SJ, Glenn DE, Cartreine JA, et al. A randomized controlled trial of a self-guided, multimedia, stress management and resilience training program. Behaviour Research and Therapy 2013;51(2):106-12. [DOI: 10.1016/j.brat.2012.11.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rosenberg 1965
- Rosenberg M. Society and the Adolescent Self-Image. Princeton (NJ): Princeton University Press, 1965. [Google Scholar]
Ruotsalainen 2015
- Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews 2015, Issue 4. [DOI: 10.1002/14651858.CD002892.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rutten 2013
- Rutten BP, Hammels C, Geschwind N, Menne-Lothmann C, Pishva E, Schruers K, et al. Resilience in mental health: linking psychological and neurobiological perspectives. Acta Psychiatrica Scandinavica 2013;128(1):3-20. [DOI: 10.1111/acps.12095] [PMC3746114] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2014
- Ryan A. ACT and be READY: Evaluation of an ACT-based Resilience Training Program Delivered to People with Diabetes [PhD thesis]. Brisbane (QLD): The University of Queensland, 2014. [Google Scholar]
Ryff 1989
- Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology 1989;57(6):1069-81. [Google Scholar]
Rücker 2011
- Rücker G, Schwarzer G, Carpenter JR, Binder H, Schumacher M. Treatment-effect estimates adjusted for small-study effects via a limit meta-analysis. Biostatistics 2011;12(1):122-42. [DOI: 10.1093/biostatistics/kxq046] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rücker 2015 [Computer program]
- Available from: CRAN.R-project.org/package=netmeta Netmeta: network meta-analysis using frequentist methods. R package version 0.8-0. Rücker G, Schwarzer G, Krahn U, König J. Available from: CRAN.R-project.org/package=netmeta, 2015.
Sadow 1993
- Sadow D, Hopkins B. Resiliency training and empowerment among homeless, substance-abusing veterans: increasing a sense of self-efficacy and internal attribution of control as a result of resiliency training. Research Communications in Psychology, Psychiatry and Behavior 1993;18(3-4):121-34. [No DOI available] [Google Scholar]
Sahler 2013
- Sahler OJ, Dolgin MJ, Phipps S, Fairclough DL, Askins MA, Katz ER, et al. Specificity of problem-solving skills training in mothers of children newly diagnosed with cancer: results of a multisite randomized clinical trial. Journal of Clinical Oncology 2013;31(10):1329-35. [DOI: 10.1200/JCO.2011.39.1870] [NCT0023479] [PMC3607672] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saigh 1997
- Saigh PA. A comparative analysis of the future orientation ratings of traumatized youth. In: Annual meeting of the International Society of Traumatic Stress Studies; 1997 November 7-10; Montreal (QC). Montréal (QC), 1997.
Saksvik 2011
- Saksvik IB, Bjorvatn B, Hetland H, Sandal GM, Pallesen S. Individual differences in tolerance to shift work--a systematic review. Sleep Medicine Reviews 2011;15(4):221-35. [DOI: 10.1016/j.smrv.2010.07.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Salanti 2008
- Salanti G, Higgins JP, Ades AE, Ioannidis JPA. Evaluation of networks of randomized trials. Statistical Methods in Medical Research 2008;17(3):279-301. [DOI: 10.1177/0962280207080643] [PMID: ] [DOI] [PubMed] [Google Scholar]
Salsman 2015
- Salsman JM, Pustejovsky JE, Jim HS, Munoz AR, Merluzzi TV, George L, et al. A meta-analytic approach to examining the correlation between religion/spirituality and mental health in cancer. Cancer 2015;121(21):3769-78. [DOI: 10.1002/cncr.29350] [PMC4618157] [PMID: 26258536] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sapienza 2011
- Sapienza JK, Masten AS. Understanding and promoting resilience in children and youth. Current Opinion in Psychiatry 2011;24(4):267-73. [DOI: 10.1097/YCO.0b013e32834776a8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sarkar 2014
- Sarkar M, Fletcher D. Psychological resilience in sport performers: a review of stressors and protective factors. Journal of Sports Sciences 2014;32(15):1419-34. [DOI: 10.1080/02640414.2014.901551] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sattler 2014
- Sattler DN, Boyd B, Kirsch J. Trauma-exposed firefighters: relationships among posttraumatic growth, posttraumatic stress, resource availability, coping and critical incident stress debriefing experience. Stress and Health 2014;30(5):356-65. [DOI: 10.1002/smi.2608] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schachman 2004
- Schachman KA, Lee RK, Lederma RP. Baby boot camp: facilitating maternal role adaptation among military wives. Nursing Research 2004;53(2):107-15. [DOI: 10.1097/00006199-200403000-00006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schaefer 2013
- Schaefer SM, Morozink Boylan J, Van Reekum CM, Lapate RC, Norris CJ, Ryff CD, et al. Purpose in life predicts better emotional recovery from negative stimuli. PLoS ONE 2013;8(11):e80329. [DOI: 10.1371/journal.pone.0080329] [PMC3827458] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schaufeli 1996
- Schaufeli WB, Leiter MP, Maslach C, Jackson SE. Maslach Burnout Inventory - General Survey (MBI-GS). In: Maslach C, Jackson SE, Leiter MP, editors(s). Maslach Burnout Inventory Manual. 3rd edition. Palo Alto (CA): Consulting Psychologists Press, 1996. [Google Scholar]
Schaufeli 2002
- Schaufeli WB, Salanova M, González-Romá V, Bakker AB. The measurement of engagement and burnout: a two sample confirmatory factor analytic approach. Journal of Happiness Studies 2002;3(1):71-92. [Google Scholar]
Schaufeli 2003
- Schaufeli WB, Bakker AB. Utrecht Work Engagement Scale. Preliminary Manual. Utrecht (UT): Occupational Health Psychology Unit, Utrecht University, 2003. [Google Scholar]
Scheier 1994
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a re-evaluation of the Life Orientation Test. Journal of Personality and Social Psychology 1994;67(6):1063-78. [PMID: ] [DOI] [PubMed] [Google Scholar]
Schlafer 2014
- Schlafer O, Wenzel V, Högl B. Sleep disorders among physicians on shift work [Schlafstörungen bei Ärzten im Schichtdienst]. Anaesthesist 2014;63(11):844-51. [DOI: 10.1007/s00101-014-2374-z] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schnyder 2008
- Schnyder U, Wittmann L, Friedrich-Perez J, Hepp U, Moergeli H. Posttraumatic stress disorder following accidental injury: rule or exception in Switzerland? Psychotherapy and Psychosomatics 2008;77(2):111-8. [DOI: 10.1159/000112888] [PMID: ] [DOI] [PubMed] [Google Scholar]
Scholler 1999
- Scholler G, Fliege H, Klapp BF. Questionnaire of self-efficacy, optimism and pessimism: reconstruction, selection of items and validation of an instrument by means of examinations of clinical samples [Fragebogen zu Selbstwirksamkeit, Optimismus und Pessimismus. Restrukturierung, Itemselektion und Validierung eines Instrumentes an Untersuchungen klinischer Stichproben]. Psychotherapie, Psychosomatik, Medizinische Psychologie 1999;49(8):275-83. [PMID: ] [PubMed] [Google Scholar]
Schultz 1977
- Schultz JH. Il Training Autogeno. Milan (LOM): Feltrinelli, 1977. [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [DOI: 10.1136/bmj.c332] [PMC2844940] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schumm 2006
- Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. Journal of Traumatic Stress 2006;19(6):825-36. [DOI: 10.1002/jts.20159] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schwarzer 1995
- Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Weinman J, Wright S, Johnston M, editors(s). Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs. 35–7 edition. Windsor (BRK): NFER-NELSON, 1995. [Google Scholar]
Schwarzer 2008
- Schwarzer R, Hallum S. Perceived teacher self-efficacy as a predictor of job stress and burnout: mediation analyses. Applied Psychology 2008;57(s1):152-71. [DOI: 10.1111/j.1464-0597.2008.00359.x] [DOI] [Google Scholar]
Schwarzer 2019 [Computer program]
- metasens: Advanced Statistical Methods to Model and Adjust for Bias in Meta-Analysis. Schwarzer G, Carpenter JR, Rücker G, Version 0.4-0. Freiburg: Guido Schwarzer, 2019.Available at CRAN.R-project.org/package=metasens. [CRAN.R-project.org/package=metasens]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A (editors). GRADE Handbook for Grading the Quality of Evidence and the Strength of Recommendations. The GRADE Working Group, 2013. [Google Scholar]
Schünemann 2019a
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Schünemann 2019b
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Segovia 2012
- Segovia F, Moore JL, Linnville SE, Hoyt RE, Hain RE. Optimism predicts resilience in repatriated prisoners of war: A 37-year longitudinal study. Journal of Traumatic Stress 2012;25(3):330-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Selye 1965
- Selye H. The stress syndrome. American Journal of Nursing 1965;65(3):97–9. [DOI: 10.2307/3453119] [DOI] [Google Scholar]
Selye 1980
- Selye H. Stress, aging and retirement. Journal of Mind and Behavior 1980;1(1):93-110. [www.jstor.org/stable/43852812] [Google Scholar]
Senra 2015
- Senra H, Barbosa F, Ferreira P, Vieira CR, Perrin PB, Rogers H, et al. Psychologic adjustment to irreversible vision loss in adults: a systematic review. Ophthalmology 2015;122(4):851-61. [DOI: 10.1016/j.ophtha.2014.10.022] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shanafelt 2003
- Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. American Journal of Medicine 2003;114(6):513-9. [DOI: 10.1016/s0002-9343(03)00117-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shanafelt 2009
- Shanafelt TD, West CP, Sloan JA, Novotny PJ, Poland GA, Menaker R, et al. Career fit and burnout among academic faculty. Archives of Internal Medicine 2009;169(10):990–5. [DOI: 10.1001/archinternmed.2009.70] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shanafelt 2016
- Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, Sloan JA, Swensen SJ, Buskirk SJ. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clinic Proceedings 2016;91(4):422–31. [DOI: 10.1016/j.mayocp.2016.02.001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shand 2015
- Shand LK, Cowlishaw S, Brooker JE, Burney S, Ricciardelli LA. Correlates of post-traumatic stress symptoms and growth in cancer patients: a systematic review and meta-analysis. Psycho-oncology 2015;24(6):624-34. [DOI: 10.1002/pon.3719] [PMID: 25393527] [DOI] [PubMed] [Google Scholar]
Shapiro 2005
- Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. International Journal of Stress Management 2005;12(2):164-76. [DOI: 10.1037/1072-5245.12.2.164] [DOI] [Google Scholar]
Sherbourne 1991
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science and Medicine 1991;32(6):705-14. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sherer 1982
- Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The Self-efficacy Scale: construction and validation. Psychological Reports 1982;51(2):663-71. [DOI: 10.2466/pr0.1982.51.2.663] [DOI] [Google Scholar]
Shi 2017
- Shi L, Wang L, Jia X, Li Z, Mu H, Liu X, et al. Prevalence and correlates of symptoms of post-traumatic stress disorder among Chinese healthcare workers exposed to physical violence: a cross-sectional study. BMJ Open 2017;7(7):e016810. [DOI: 10.1136/bmjopen-2017-016810] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shoemaker 1996
- Shoemaker AL. What's normal? – Temperature, gender, and heart rate. Journal of Statistics Education 1996;4(2):1-4. [DOI: 10.1080/10691898.1996.11910512] [DOI] [Google Scholar]
Silver 2002
- Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. JAMA 2002;288(10):1235-44. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sinclair 2004
- Sinclair VG, Wallston KA. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment 2004;11(1):94-101. [PMID: ] [DOI] [PubMed] [Google Scholar]
Skeffington 2013
- Skeffington PM, Rees CS, Kane R. The primary prevention of PTSD: a systematic review. Journal of Trauma & Dissociation 2013;14(4):404-22. [DOI: 10.1080/15299732.2012.753653] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sloan 2012
- Sloan DM, Marx BP, Bovin MJ, Feinstein BA, Gallagher MW. Written exposure as an intervention for PTSD: a randomized clinical trial with motor vehicle accident survivors. Behaviour Research and Therapy 2012;50(10):627-35. [DOI: 10.1016/j.brat.2012.07.001] [PMC3433579] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 1990
- Smith JC. Cognitive Behavioral Relaxation Training: A New System of Strategies for Treatment and Assessment. New York (NY): Springer, 1990. [Google Scholar]
Smith 1993
- Smith JC. Creative Stress Management: The 1-2-3 COPE System. Englewood Cliffs (NJ): Prentice-Hall, 1993. [Google Scholar]
Smith 2003
- Smith A, Roberts K. Interventions for post-traumatic stress disorder and psychological distress in emergency ambulance personnel: a review of the literature. Emergency Medicine Journal 2003;20(1):75-8. [DOI: 10.1136/emj.20.1.75] [PMC1725987 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2007
- Smith C, Hancock H, Blake-Mortimer J, Eckert K. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complementary Therapies in Medicine 2007;15(2):77-83. [DOI: 10.1016/j.ctim.2006.05.001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Smith 2008
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The Brief Resilience Scale: assessing the ability to bounce back. International Journal of Behavioral Medicine 2008;15(3):194-200. [DOI: 10.1080/10705500802222972] [PMID: ] [DOI] [PubMed] [Google Scholar]
Smith 2009
- Smith BW, Tooley EM, Montague EQ, Robinson AE, Cosper CJ, Mullins PG. The role of resilience and purpose in life in habituation to heat and cold pain. Journal of Pain 2009;10(5):493-500. [DOI: 10.1016/j.jpain.2008.11.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Smith 2019 [pers comm]
- Smith O. Information if study was already published [personal communication]. Email to: A Kunzler 30 July 2019.
Solomon 1988
- Solomon Z, Mikulincer M, Avitzur E. Coping, locus of control, social support, and combat-related posttraumatic stress disorder: a prospective study. Journal of Personality and Social Psychology 1988;55(2):279-85. [PMID: ] [DOI] [PubMed] [Google Scholar]
Songprakun 2012
- Songprakun W, McCann TV. Effectiveness of a self-help manual on the promotion of resilience in individuals with depression in Thailand: a randomised controlled trial. BMC Psychiatry 2012;12:12. [DOI: 10.1186/1471-244X-12-12] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sood 2010
- Sood A. Train Your Brain. Engage Your Heart. Transform Your Life. A Two Step Program to Enhance Attention; Decrease Stress; Cultivate Peace, Joy and Resilience; and Practice Presence with Love. A course in Attention & Interpretation Therapy (AIT). Rochester (MN): Morning Dew Publications, 2010. [Google Scholar]
Southwick 2005
- Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annual Review of Clinical Psychology 2005;1:255-91. [DOI: 10.1146/annurev.clinpsy.1.102803.143948] [PMID: ] [DOI] [PubMed] [Google Scholar]
Southwick 2011
- Southwick SM, Pietrzak RH, White G. Interventions to enhance resilience and resilience-related constructs in adults. In: Southwick SM, Litz BT, Charney DS, Friedman MJ, editors(s). Resilience and Mental Health: Challenges Across the Lifespan. Cambridge: Cambridge University Press, 2011:289-306. [DOI: 10.1017/CBO9780511994791.022] [DOI] [Google Scholar]
Southwick 2012
- Southwick SM, Charney DS (editors). Resilience: The Science of Mastering Life's Greatest Challenges. Cambridge: Cambridge University Press, 2012. [Google Scholar]
Spielberger 1970
- Spielberger CD, Gorsuch RL, Lushene RE. STAI Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press, 1970. [Google Scholar]
Spitzer 1994
- Spitzer RL, Williams JB, Kroenke K, Linzer M, DeGruy FV 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA 1994;272(22):1749-56. [PMID: ] [PubMed] [Google Scholar]
Spitzer 1999
- Spitzer RL, Kroenke K, Williams JB, and the Patient Health Questionnaire Primary Study Group. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA 1999;282(18):1737-44. [DOI: 10.1001/jama.282.18.1737] [PMID: ] [DOI] [PubMed] [Google Scholar]
Spitzer 2006
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine 2006;166(10):1092-7. [DOI: 10.1001/archinte.166.10.1092] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stahl 2010
- Stahl B, Goldstein E. A Mindfulness-Based Stress Reduction Workbook. Oakland (CA): New Harbinger Publications, Inc, 2010. [Google Scholar]
Stamm 2005
- Stamm BH. The ProQOL Manual: The Professional Quality of Life Scale: Compassion Satisfaction, Burnout, and Compassion Fatigue/Secondary trauma scales. Latherville (MD): Sidran Press, 2005. [www.compassionfatigue.org/pages/ProQOLManualOct05.pdf] [Google Scholar]
Steinhardt 2008
- Steinhardt MA, Dolbier CL. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. Journal of American College Health 2008;56(4):445-53. [DOI: 10.3200/JACH.56.44.445-454] [PMID: ] [DOI] [PubMed] [Google Scholar]
Steinmetz 2012
- Steinmetz SE, Benight CC, Bishop SL, James LE. My Disaster Recovery: a pilot randomized controlled trial of an Internet intervention. Anxiety Stress Coping 2012;25:593–600. [DOI: 10.1080/10615806.2011.604869] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stetz 2018 [pers comm]
- Stetz M. Random sequence generation [personal communication]. Email to: A Kunzler 21 May 2018.
Stewart 2011
- Stewart DE, Yuen T. A systematic review of resilience in the physically ill. Psychosomatics 2011;52(3):199-209. [DOI: 10.1016/j.psym.2011.01.036] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stoffers‐Winterling 2012
- Stoffers-Winterling JM, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K. Psychological therapies for people with borderline personality disorder. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD005652.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stonnington 2016
- Stonnington CM, Darby B, Santucci A, Mulligan P, Pathuis P, Cuc A, et al. A resilience intervention involving mindfulness training for transplant patients and their caregivers. Clinical Transplantation 2016;30(11):1466-72. [DOI: 10.1111/ctr.12841] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stonnington 2017 [pers comm]
- Stonnington C. Descriptive statistics (means and SDs) for outcome measures in two groups at each time point [personal communication]. Email to: A Kunzler 16 August 2017.
Strand 2006
- Strand EB, Zautra AJ, Thoresen M, Ødegård S, Uhlig T, Finset A. Positive affect as a factor of resilience in the pain-negative affect relationship in patients with rheumatoid arthritis. Journal of Psychosomatic Research 2006;60(5):477-84. [PMID: ] [DOI] [PubMed] [Google Scholar]
Strauss 2019 [pers comm]
- Strauss C. Potential focus on and measurement of resilience in the study Strauss 2018 [personal communication]. Email to: A Kunzler 8 August 2019.
Sumer 2005
- Sumer N, Karanci AN, Berument SK, Gunes H. Personal resources, coping self-efficacy, and quake exposure as predictors of psychological distress following the 1999 earthquake in Turkey. Journal of Traumatic Stress 2005;18(4):331-42. [DOI: 10.1002/jts.20032] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tams 2016
- Tams R, Prangnell SJ, Daisley A. Helping families thrive in the face of uncertainty: strengths based approaches to working with families affected by progressive neurological illness. NeuroRehabilitation 2016;38(3):257-70. [DOI: 10.3233/nre-161317] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tan 2014
- Tan L, Wang MJ, Modini M, Joyce S, Mykletun A, Christensen H, et al. Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Medicine 2014;12:74. [DOI: 10.1186/1741-7015-12-74] [PMC4014627] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tan 2016
- Tan KK, Chan SW, Wang W, Vehviläinen-Julkunen K. A salutogenic program to enhance sense of coherence and quality of life for older people in the community: a feasibility randomized controlled trial and process evaluation. Patient Education and Counseling 2016;99(1):108-16. [DOI: 10.1016/j.pec.2015.08.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tao 2010
- Tao H, Hu J-C, Wang L, Liu X-H. Development of a scale for job satisfaction assessment in nurses. Academic Journal Second Military Medical University 2010;29(11):1292–6. [DOI: 10.3724/SP.J.1008.2009.01292] [DOI] [Google Scholar]
Taylor 2018
- Taylor C, Xyrichis A, Leamy MC, Reynolds E, Maben J. Can Schwartz Center Rounds support healthcare staff with emotional challenges at work, and how do they compare with other interventions aimed at providing similar support? A systematic review and scoping reviews. BMJ Open 2018;8(10):e024254. [DOI: 10.1136/bmjopen-2018-024254] [PMC6196967] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Teasdale 2000
- Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology 2000;68(4):615-23. [DOI: 10.1037/0022-006X.68.4.615] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tedeschi 1996
- Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. Journal of Traumatic Stress 1996;9(3):455-71. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tennant 2007
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS); development and UK validation. Health and Quality of Life Outcomes 2007;5:63. [DOI: 10.1186/1477-7525-5-63] [PMC2222612 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tilden 1990
- Tilden VP, Nelson CA, May BA. The IPR inventory: development and psychometric characteristics. Nursing Research 1990;39(6):337-43. [PMID: ] [PubMed] [Google Scholar]
Tomioka 2011
- Tomioka K, Morita N, Saeki K, Okamoto N, Kurumatani N. Working hours, occupational stress and depression among physicians. Occupational Medicine 2011;61(3):163-70. [DOI: 10.1093/occmed/kqr004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Townshend 2016
- Townshend K, Jordan Z, Stephenson M, Tsey K. The effectiveness of mindful parenting programs in promoting parents' and children's wellbeing: a systematic review. JBI Database of Systematic Reviews and Implementation Reports 2016;14(3):139-80. [DOI: 10.11124/JBISRIR-2016-2314] [PMID: ] [DOI] [PubMed] [Google Scholar]
Trowbridge 2016
- Trowbridge K, Mische Lawson L. Mindfulness-based interventions with social workers and the potential for enhanced patient-centered care: a systematic review of the literature. Social Work in Health Care 2016;55(2):101-24. [DOI: 10.1080/00981389.2015.1094165] [PMID: ] [DOI] [PubMed] [Google Scholar]
Truitt 2012
- Truitt M, Biesecker B, Capone G, Bailey T, Erby L. The role of hope in adaptation to uncertainty: the experience of caregivers of children with Down syndrome. Patient Education and Counseling 2012;87(2):233-8. [DOI: 10.1016/j.pec.2011.08.015] [PMC3816013] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsai 2015
- Tsai J, El-Gabalawy R, Sledge WH, Southwick SM, Pietrzak RH. Post-traumatic growth among veterans in the USA: results from the National Health and Resilience in Veterans Study. Psychological Medicine 2015;45(1):165-79. [DOI: 10.1017/S0033291714001202] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tsai 2016
- Tsai J, Sippel LM, Mota N, Southwick SM, Pietrzak RH. Longitudinal course of posttraumatic growth among US military veterans: results from the National Health and Resilience in Veterans Study. Depression and Anxiety 2016;33(1):9-18. [DOI: 10.1002/da.22371] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tschannen‐Moran 2001
- Tschannen-Moran M, Woolfolk Hoy A. Teacher efficacy: capturing an elusive construct. Teaching and Teacher Education 2001;17(7):783-805. [DOI: 10.1016/S0742-051X(01)00036-1] [DOI] [Google Scholar]
Ungar 2008
- Ungar M, Liebenberg L, Boothroyd R, Kwong WM, Lee TY, Leblanc J, et al. The study of youth resilience across cultures: lessons from a pilot study of measurement development. Research in Human Development 2008;5(3):166-80. [DOI: 10.1080/15427600802274019] [DOI] [Google Scholar]
Van Berkel 2011
- Van Berkel J, Proper KI, Boot CR, Bongers PM, Van der Beek AJ. Mindful “Vitality in Practice”: an intervention toimprove the work engagement and energy balance among workers; the development and design of the randomised controlled trial. BMC Public Health 2011;11:736. [DOI: 10.1186/1471-2458-11-736] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van der Beek 2018 [pers comm]
- Van der Beek A. Number of participants lost to follow-up at 12 month [personal communication]. Email to: A Kunzler 23 July 2018.
Van der Kleij 2011
- Van der Kleij R, Molenaar D, Schraagen JM. Making teams more resilient: effects of shared transformational leadership training on resilience. Proceedings of the Human Factors and Ergonomics Society Annual Meeting 2011;55(1):2158-62. [DOI: 10.1177/1071181311551450] [DOI] [Google Scholar]
Van der Zee 1993
- Van der Zee KI, Sanderman R. Het Meten van Gezondheidstoestand met de RAND-36: Een Handleiding [Measuring Health Status with the RAND-36: A Manual]. Groningen (GR): Noordelijk Centrum voor Gezondheidsvraagstukken, 1993. [Google Scholar]
Van Ham 2006
- Van Ham I, Verhoeven AA, Groenier KH, Groothoff JW, De Haan J. Job satisfaction among general practitioners: a systematic literature review. European Journal of General Practice 2006;12(4):174–80. [DOI: 10.1080/13814780600994376] [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Kessel 2013
- Van Kessel G. The ability of older people to overcome adversity: a review of the resilience concept. Geriatric Nursing 2013;34(2):122-7. [DOI: 10.1016/j.gerinurse.2012.12.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Kessel 2014
- Van Kessel G, MacDougall C, Gibbs L. Resilience-rhetoric to reality: a systematic review of intervention studies after disasters. Disaster Medicine and Public Health Preparedness 2014;8(5):452-60. [DOI: 10.1017/dmp.2014.104] [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Leeuwen 2012
Vanhove 2016
- Vanhove AJ, Herian MN, Perez AL, Harms PD, Lester PB. Can resilience be developed at work? A meta-analytic review of resilience-building programme effectiveness. Journal of Occupational and Organizational Psychology 2016;89(2):278-307. [DOI: 10.1111/joop.12123] [DOI] [Google Scholar]
Verma 2011
- Verma R, Balhara YP, Gupta CS. Gender differences in stress response: role of developmental and biological determinants. Industrial Psychiatry Journal 2011;20(1):4-10. [DOI: 10.4103/0972-6748.98407] [PMC3425245] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Viechtbauer 2010
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. Journal of Statistical Software 2010;36(3):1-48. [DOI: 10.18637/jss.v036.i03] [DOI] [Google Scholar]
Villani 2018 [pers comm]
- Villani D. Descriptive statistics (means and SDs) for outcomes at pre- and post-intervention (after 8 sessions); number of dropouts; number of participants analysed in each group [personal communication]. Email to: A Kunzler 11 May 2018.
Visser 2010
- Visser A, Garssen B, Vingerhoets A. Spirituality and well-being in cancer patients: a review. Psycho-Oncology 2010;19(6):565-72. [DOI: 10.1002/pon.1626] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wade 2001
- Wade SL, Borawski EA, Taylor HG, Drotar D, Yeates KO, Stancin T. The relationship of caregiver coping to family outcomes during the initial year following pediatric traumatic injury. Journal of Consulting and Clinical Psychology 2001;69(3):406-15. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wagnild 1993
- Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. Journal of Nursing Measurement 1993;1(2):165-78. [PMID: ] [PubMed] [Google Scholar]
Wagnild 2009
- Wagnild GM. The Resilience Scale User’s Guide for the US English Version of the Resilience Scale and the 14-Item Resilience Scale (RS-14). Worden (MT): The Resilience Center, 2009. [Google Scholar]
Wainwright 2019
- Wainwright E, Wainwright D, Coghill N, Walsh J, Perry R. Resilience and return-to-work pain interventions: systematic review. Occupational Medicine 2019;69(3):163-76. [DOI: 10.1093/occmed/kqz012] [PMID: ] [DOI] [PubMed] [Google Scholar]
Waite 2004
- Waite PJ, Richardson GE. Determining the efficacy of resiliency training in the work site. Journal of Allied Health 2004;33(3):178-83. [PMID: ] [PubMed] [Google Scholar]
Walker 1987
- Walker S, Sechrist KR, Pender NJ. The Health-Promoting Lifestyle Profile: development and psychometric characteristics. Nursing Research 1987;36(2):76-81. [PMID: ] [PubMed] [Google Scholar]
Walsh 2002
- Walsh K, King M, Jones L, Tookman A, Blizard R. Spiritual beliefs may affect outcome of bereavement: prospective study. BMJ 2002;324(7353):1551. [DOI: ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2014
- Wang F, Liu J, Liu L, Wang F, Ma Z, Gao D, et al. The status and correlates of depression and anxiety among breast-cancer survivors in Eastern China: a population-based, cross-sectional case–control study. BMC Public Health 2014;14:326. [DOI: 10.1186/1471-2458-14-326] [PMC3997219] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ware 1994
- Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston (MA): The Health Institute, New England Medical Center, 1994. [Google Scholar]
Warnecke 2011
- Warnecke E, Quinn S, Ogden K, Towle N, Nelson MR. A randomised controlled trial of the effects of mindfulness practice on medical student stress levels. Medical Education 2011;45(4):381-8. [DOI: 10.1111/j.1365-2923.2010.03877.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Watson 1988
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology 1988;54(6):1063-70. [PMID: ] [DOI] [PubMed] [Google Scholar]
Watson 1994
- Watson D, Clark LA. The PANAS-X: Manual for the Positive and Negative Affect Schedule-Expanded Form. Ames: The University of Iowa, 1994. [Google Scholar]
Watson 2005
- Watson D, Gamez W, Simms LJ. Basic dimensions of temperament and their relation to anxiety and depression: a symptom-based perspective. Journal of Research in Personality 2005;39(1):46-66. [DOI: 10.1016/j.jrp.2004.09.006] [DOI] [Google Scholar]
Waysman 2001
- Waysman M, Schwarzwald J, Solomon Z. Hardiness: an examination of its relationship with positive and negative long term changes following trauma. Journal of Traumatic Stress 2001;14(3):531-48. [DOI: 10.1023/A:1011112723704] [PMID: ] [DOI] [PubMed] [Google Scholar]
Weinberg 2000
- Weinberg A, Creed F. Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet 2000;355(9203):533-7. [DOI: 10.1016/S0140-6736(99)07366-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Weiss 2002
- Weiss MJ. Hardiness and social support as predictors of stress in mothers of typical children, children with autism, and children with mental retardation. Autism 2002;6(1):115-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
West 2016
- West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016;388(10057):2272–81. [DOI: 10.1016/S0140-6736(16)31279-X] [PMID: ] [DOI] [PubMed] [Google Scholar]
West 2017 [pers comm]
- West CP. Descriptive statistics (means and SDs) for outcomes at all time points [personal communication]. Email to: A Kunzler 18 September 2017.
West 2018 [pers comm]
- West CP. Information if study was published in the meantime [personal communication]. Email to: A Kunzler 16 July 2018.
West 2019 [pers comm]
- West CP. Summary data for both groups to consider unpublished study in meta-analysis [personal communication]. Email to: A Kunzler 28 May 2019.
White 2005
- White IR, Thomas J. Standardized mean differences in individually-randomized and cluster-randomized trials, with applications to meta-analysis. Clinical Trials 2005;2(2):141-51. [PMID: ] [DOI] [PubMed] [Google Scholar]
White 2012a
- White JH, Magin P, Attia J, Sturm J, Carter G, Pollack M. Trajectories of psychological distress after stroke. Annals of Family Medicine 2012;10(5):435-42. [DOI: 10.1370/afm.1374] [PMC3438211] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
White 2012b
- White IR, Barrett JK, Jackson D, Higgins JP. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Reseacrh Synthesis Methods 2012;3(2):111-25. [DOI: 10.1002/jrsm.1045] [DOI] [PMC free article] [PubMed] [Google Scholar]
Whiting‐O'Keefe 1984
- Whiting-O'Keefe QE, Henke C, Simborg DW. Choosing the correct unit of analysis in medical care experiments. Medical Care 1984;22(12):1101-14. [PMID: ] [DOI] [PubMed] [Google Scholar]
WHO 1986
- World Health Organization. Ottawa Charter of Health Promotion; 1986. www.euro.who.int/__data/assets/pdf_file/0004/129532/Ottawa_Charter.pdf?ua=1.
WHO 2004
- World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice: Summary Report; 2004. www.who.int/mental_health/evidence/en/promoting_mhh.pdf.
WHO 2019
- World Health Organization. Gender and women's mental health. Gender disparities and mental health: the facts. www.who.int/mental_health/prevention/genderwomen/en (accessed 21 April 2020).
Whooley 1997
- Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression: two questions are as good as many. Journal of General Internal Medicine 1997;12(7):439-45. [DOI: 10.1046/j.1525-1497.1997.00076.x] [PMC1497134] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHOQOL Group 1998
- WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine 1998;28(3):551-8. [DOI: 10.1017/s0033291798006667] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wieclaw 2006
- Wieclaw J, Agerbo E, Mortensen PB, Bonde JP. Risk of affective and stress related disorders among employees in human service professions. Occupational and Environmental Medicine 2006;63(5):314-9. [DOI: 10.1136/oem.2004.019398] [PMC2092492] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wild 2018 [pers comm]
- Wild J. Information if trial was completed and published; inquiry for provision of summary data [personal communication]. Email to: A Kunzler 5 August 2018.
Williams 1997
- Williams RA. Psychometrics of the Coping Styles Questionnaire (CSQ). Ann Arbo (MI): University of Michigan, 1997. [Google Scholar]
Williams 1999
- Williams ES, Konrad TR, Linzer M, McMurray J, Pathman DE, Gerrity M, et al. Refining the measurement of physician job satisfaction: results from the Physician Worklife Survey. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Medical Care 1999;37(11):1140-54. [DOI: 10.1097/00005650-199911000-00006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Windle 2008
- Windle G, Markland DA, Woods RT. Examination of a theoretical model of psychological resilience in older age. Aging and Mental Health 2008;12(3):285-92. [DOI: 10.1080/13607860802120763] [PMID: ] [DOI] [PubMed] [Google Scholar]
Windle 2011a
- Windle G. What is resilience? A review and concept analysis. Reviews in Clinical Gerontology 2011;21(2):152-69. [DOI: 10.1017/S0959259810000420] [DOI] [Google Scholar]
Windle 2011b
- Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health and Quality of Life Outcomes 2011;9:8. [DOI: 10.1186/1477-7525-9-8] [PMC3042897] [DOI] [PMC free article] [PubMed] [Google Scholar]
Winger 2016
- Winger JG, Adams RN, Mosher CE. Relations of meaning in life and sense of coherence to distress in cancer patients: a meta-analysis. Psycho-Oncology 2016;25(1):2-10. [DOI: 10.1002/pon.3798] [PMC4575247] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Winwood 2013
- Winwood PC, Colon R, McEwen K. A practical measure of workplace resilience: developing the resilience at work scale. Journal of Occupational and Environmental Medicine 2013;55(10):1205-12. [DOI: 10.1097/JOM.0b013e3182a2a60a] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wise 2012
- Wise EH, Hersh MA, Gibson CM. Ethics, self-care and well-being for psychologists: reenvisioning the stress-distress continuum. Professional Psychology: Research and Practice 2012;43(5):487-94. [DOI: 10.1037/a0029446] [DOI] [Google Scholar]
Wolfe 2004
- Wolfe F. Fatigue assessments in rheumatoid arthritis: comparative performance of visual analog scales and longer fatigue questionnaires in 7760 patients. Journal of Rheumatology 2004;31(10):1896-902. [PMID: ] [PubMed] [Google Scholar]
Wolpe 1958
- Wolpe J. Psychotherapy by Reciprocal Inhibition. Stanford (CA): Stanford University Press, 1958. [Google Scholar]
Wright 2008
- Wright LJ, Zautra AJ, Going S. Adaptation to early knee osteoarthritis: the role of risk, resilience, and disease severity on pain and physical functioning. Annals of Behavioral Medicine 2008;36(1):70-80. [DOI: 10.1007/s12160-008-9048-5] [PMC2613296] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wright 2017
- Wright EM, Matthai MT, Warren N. Methods for alleviating stress and increasing resilience in the midwifery community: a scoping review of the literature. Journal of Midwifery & Women's Health 2017;62(6):737-45. [DOI: 10.1111/jmwh.12651] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wu 2013
- Wu G, Feder A, Cohen H, Kim JJ, Calderon S, Charney DS, et al. Understanding resilience. Frontiers in Behavioral Neuroscience 2013;7:10. [DOI: 10.3389/fnbeh.2013.00010] [PMC3573269] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yang 2007
- Yang TZ, Guo JX, Chen B, Huang JJ, Cai HR, Liu LJ. Cognitive and behavioral strategies of stress management among Chinese urban residents. Chinese Journal of Preventive Medicine 2007;41(4):245-9. [PMID: ] [PubMed] [Google Scholar]
Yu 2007
- Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Social Behavior and Personality 2007;35:19-30. [DOI: 10.2224/sbp.2007.35.1.19] [DOI] [Google Scholar]
Zander 2013
- Zander B, Dobler L, Busse R. The introduction of DRG funding and hospital nurses' changing perceptions of their practice environment, quality of care and satisfaction: comparison of cross-sectional surveys over a 10-year period. International Journal of Nursing Studies 2013;50(2):219-29. [DOI: 10.1016/j.ijnurstu.2012.07.008] [PMID: 22846589] [DOI] [PubMed] [Google Scholar]
Zauszniewski 2010
- Zauszniewski J, Bekhet A, Suresky MJ. Resilience in family members of persons with serious mental illness. Nursing Clinics of North America 2010;45(4):613-26. [DOI: 10.1016/j.cnur.2010.06.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Zautra 2005
- Zautra AJ, Johnson LM, Davis MC. Positive affect as a source of resilience for women in chronic pain. Journal of Consulting and Clinical Psychology 2005;73(2):212-20. [DOI: 10.1037/0022-006X.73.2.212] [NIHMS71708] [PMC2593933] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2002
- Zhang J, Norvilitis JM. Measuring Chinese psychological well-being with Western developed instruments. Journal of Personality Assessment 2002;79(3):492–511. [DOI: 10.1207/S15327752JPA7903_06] [PMID: ] [DOI] [PubMed] [Google Scholar]
Zigmond 1983
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica 1983;67(6):361–70. [DOI: 10.1111/j.1600-0447.1983.tb09716.x] [DOI] [PubMed] [Google Scholar]
Zimet 1988
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment 1988;52(1):30-41. [DOI: 10.1207/s15327752jpa5201_2] [DOI] [PubMed] [Google Scholar]
Zuckerman 1965
- Zuckerman M, Lubin B. Manual for the Multiple Affect Adjective Check List. San Diego (CA): Educational and Industrial Testing Service, 1965. [Google Scholar]
References to other published versions of this review
Helmreich 2017
- Helmreich I, Kunzler A, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions for resilience enhancement in adults. Cochrane Database of Systematic Reviews 2017, Issue 2. [DOI: 10.1002/14651858.CD012527] [DOI] [Google Scholar]


