Abstract
Background
High-energy tibial plateau fractures are challenges in treatment with controversy over operative stabilisation, especially for fractures with metaphyseal–diaphyseal dissociation. Treatment with percutaneous or minimally invasive direct reduction techniques, usually associated with circular external fixation, has generated interest although there is no consensus regarding the type of external fixation to be used.
Aim
This study aims to compare the two hybrid circular external fixation mountings used to treat the high-energy tibial plateau fractures.
Methods
Two different groups of hybrid circular external fixation frame mountings were assembled using composite tibiae with proximal metaphyseal osteotomies simulating tibial plateau fractures with metaphyseal–diaphyseal dissociation. The standard all-wire frame mounting was assembled, and the comparison frame mounting had the distal K-wires replaced with half-pins. Both groups were tested through cyclic loading between 300 and 1000 N for 10,000 cycles. Interfragmentary linear and rotational displacements were analysed.
Results
The standard frame mounting behaved similarly to a classic Ilizarov frame, allowing greater axial movement (mean, 3.76 ± 0.26 mm in the standard group and 3.02 ± 0.23 mm in the test group) and smaller mediolateral displacement compared with the test frame (mean, 0.17 ± 0.16 mm compared to 0.56 ± 0.12 mm). The test frame behaved more similarly to a linear external fixator and provided greater axial stability, similar anteroposterior displacement, and lower mediolateral stability. Despite these differences, in both groups the axial displacement was greater than the prejudicial nonaxial movements.
Conclusion
Increasing the number of half-pins and decreasing the number of K-wires in hybrid circular external fixation generate frames that tend to behave more similarly to the linear external fixators.
How to cite this article
Cardoso GS, Amorim R, Penha FM, et al. Biomechanical Analysis of the Behaviour at the Metaphyseal–Diaphyseal Junction of Complex Tibial Plateau Fractures Using Two Circular Fixator Configurations. Strategies Trauma Limb Reconstr 2020;15(3):138–145.
Keywords: Axial movement, Circular external fixation, Metaphyseal–diaphyseal dissociation
Introduction
Fractures of the proximal tibia account for 5 to 11% of all tibial fractures1 and about 1.2% of all fractures.2 The magnitude, type and direction of forces that injure the knee dictate the fracture pattern. Complex fractures of the tibial plateau are difficult to treat and represent one of the most challenging problems in orthopaedic surgery3,4; their treatment continues to be controversial.5,6
Previously, the standard accepted treatment for such fractures was open reduction and internal fixation with plates and screws through an extensive anterior incision.7 However, while this technique is optimal for fracture visualisation, reduction and fixation, it requires an extensive soft tissue dissection over the predominantly subcutaneous proximal end of the tibia. The combination of damage from the energy dissipated through the soft tissues from the original injury and extensive surgical dissection led to a high complication rate, including skin necrosis and infection.8–10
With the realisation of the detrimental effects of excessive dissection of the tenuous soft tissue envelope and devascularisation of the osseous fragments, a number of alternative treatment methods have been introduced.5 The Ilizarov technique solves many problems encountered in managing such fractures and provides a method for closed reduction and fixation that does not necessitate excessive soft tissue stripping.3,4 This technique is particularly useful considering its ability to correct the deformity in multiple planes, even in the postoperative period. The frame is assembled using three or four rings depending on the proximity of the fracture to the joint. Tensioned fine wires then are positioned across the proximal part of the tibia, where the fracture lines hinder the use of half-pins. Fixation of the shaft to the distal rings can be performed with K-wires or percutaneous-threaded half-pins or both.4,11
Attempts have been made to simplify the application and the configuration of frame mountings to improve patient comfort while maintaining frame stability. One method has been through reducing the number of wires in the hope that it decreases the potential infection and the soft tissue impalement issues associated with the wires and substituting with half-pins. Half-pins have been adapted to the Ilizarov frame due to their biomechanical properties that allow for creation of a more rigid frame and decreased soft tissue complications12; however, the introduction of half-pins in a construct could potentially lead to cantilever bending during loading.13
Due to the modularity and subsequent variability of frame mountings, different frame configurations are used clinically, and whilst the most exhibit good healing rates, nonunion and malunion complications still occur.4,10,12,14 Fracture healing is a complex biologic process that is also affected substantially by the mechanical properties of osteosynthesis. A rigid system can produce nonunion, delayed healing, or disuse osteoporosis through stress shielding, whereas an overly flexible system can produce malunion, nonunion and pin–bone interface problems.15
One cause of failure that might inhibit healing is the presence of excessive shear stresses produced by an asymmetric axial fracture site motion.12 Accordingly, the rigidity of the osteosynthesis should be sufficient to inhibit excessive initial fragment movement and be sufficiently flexible to allow enough axial load transfer to stimulate healing.
Most biomechanical studies performed with circular external fixators applied only unidirectional axial loads12 and analysed only the stiffness characteristics of different mountings.16 Surprisingly, only a few studies have analysed the interfragmentary displacement which is a more pertinent parameter related to fracture healing.13,16 Yang et al.16 reported the importance of measuring relative displacements at the fracture site when investigating the mechanical properties of the fixators. A cyclic model more accurately represents the postoperative period when a patient is performing early range of motion exercises and the affected limb is subjected to forces during activities of daily living.1,13 Accordingly, we have compared the interfragmentary displacement between the two different hybrid Ilizarov frame mountings used to treat high-energy tibial plateau fractures under cyclic axial loading.
This biomechanical study was designed to answer the following research questions: (1) What type and magnitude of interfragmentary strain occurs on loading of a simulated high- energy tibial plateau fracture in an Ilizarov frame under physiologic levels of axial loading? (2) How is interfragmentary strain altered by substitution of fine wires for half-pins under these conditions?
Methods
Eight fourth-generation composite tibiae (Sawbones, Vashon Island, WA, USA) from a single-manufacturing batch were used in this biomechanical study. The distal end of each tibial composite was rigidly fixed with bone cement to a metallic device specially designed for that purpose, to allow positioning of the specimen in the test machine and permit loading in an upright position, as described by Ali et al.17
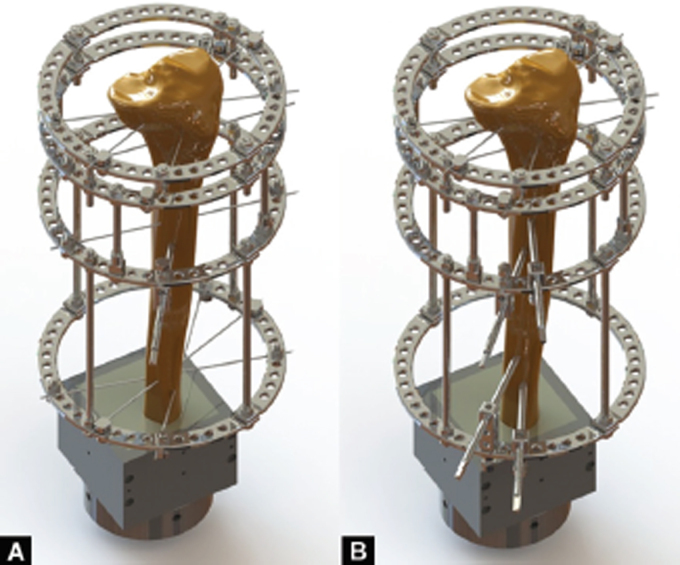
The frame was comprised of 160-mm-diameter rings, 1.8-mm K-wires, 8-mm threaded rods and 6-mm half-pins. One manufacturer supplied all fixator components. The frame was assembled with four rings connected to each other by four threaded equidistant rods. The wires were positioned at pre-established sites, after which they were tightened on the insertion end by a cannulated bolt and nut and tensioned to 110 kg using the tensioner on the opposite end. The distal block then was assembled as either the standard frame or the test frame (Fig. 1). The standard frame was assembled in the hybrid configuration described by Catagni et al.4 and included four tensioned wires and one half-pin. The test frame was assembled by replacing the wires in the standard frame with two half-pins in each ring, similarly to one of the assemblies tested by Pugh et al.14 and as currently in use for treatment of these complex fractures by the Group of Limb Reconstruction at the Governador Celso Ramos Hospital in Florianópolis, Brazil. The half-pins were positioned at established sites; each half-pin was inserted manually and fixed to the cube with screws. Figure 1 shows both configurations.
Figs. 1A and B.
Standard (A) and test (B) frame-mounting designs showing the positioning of the K-wires and half-pins
After the frame mounting was completed, the connecting threaded rods between the two fixation blocks were removed and a 10-mm-wide ostectomy was performed using an automated thin blade saw. A template was used to create a reproducible cut. The resultant gap in the tibial metaphysis simulated the comminution found in Schatzker VI and AO 41A3, C2 and C3 fractures. The connecting threaded rods then were repositioned.
Each specimen was mounted and fixed onto a materialtesting machine (MTS Corporation, Minneapolis, MN, USA) with the loading cell attached to one specially designed device. Axial loading was applied to the centre of the condyles parallel to the mechanical axis of the tibia. The load sharing was such that 70% of the applied load was supported by the medial tibial plateau and 30% by the lateral one. To this end, a special fixture was designed that allowed a split of the applied compressive load by adjusting the distances from the load application axis to the condylar centres. Although the axial loading does not represent all the forces encountered physiologically, due to uneven positioning of the bone fixation elements, the mechanical system is prone to produce nonaxial movements. Furthermore, a cyclic loading regimen more accurately reflects the postoperative period,1 so the specimens were loaded cyclically between 300 and 1000 N for 10,000 cycles at 1 Hz.13
The relative movement between fragments was evaluated and registered for 15 seconds at pre-established cycles (1,225, 2,225, 4,000, 5,000, 7,000 and 9,000 cycles). Data were recorded from each osseous fragment corresponding to the three spatial directions (axial [y], mediolateral [x] and anteroposterior [z]) and the three spatial rotations (around y-axis [pitch], around x-axis [roll] and around z-axis [yaw]). An optoelectronic measurement device with 0.1 mm accuracy was used to evaluate these parameters (OptiTrack, Corvallis, OR, USA). Three OptiTrack marking flags were rigidly affixed to each of the two bone fragments close to the ostectomy gap (Fig. 2).
Fig. 2.
Photograph of the specimen positioned on the testing machine with OptiTrack marking flags attached for testing
The characteristics of each frame mounting were analysed by determining the difference between the position and the orientation of each bone fragment during the cycles.
Statistical Package for the Social Sciences (SPSS) version 21 (IBM Corporation, New York, NY, USA) was used for statistical analysis. Analyses of repetitive measures were performed to evaluate the intragroup differences. The Mann–Whitney U-test was used for comparisons between groups. The level of significance was p < 0.05.
RESULTS
The overall results are shown in Figures 3 and 4 and Tables 1 and 2. There was no breakage of external fixator components during cyclic loading. When the stability of each frame mounting was evaluated over time, the fragment movement or rotation over time between the subjects in each group did not differ (p > 0.05).
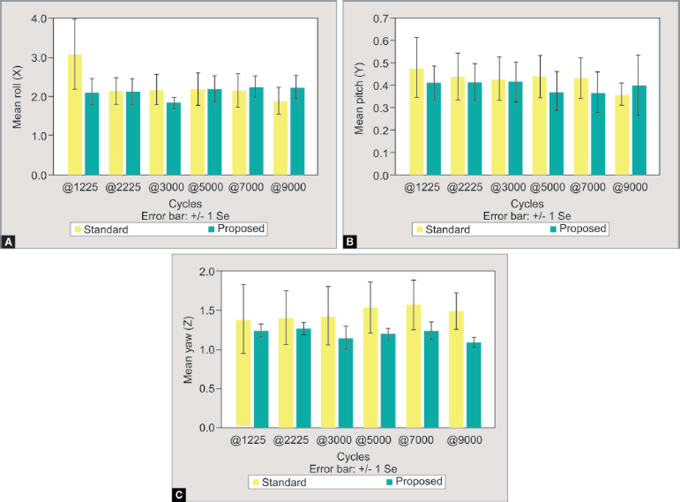
Figs. 3A to c.
The mean relative mediolateral, axial and anteroposterior displacements (mm) over time for standard and test frames
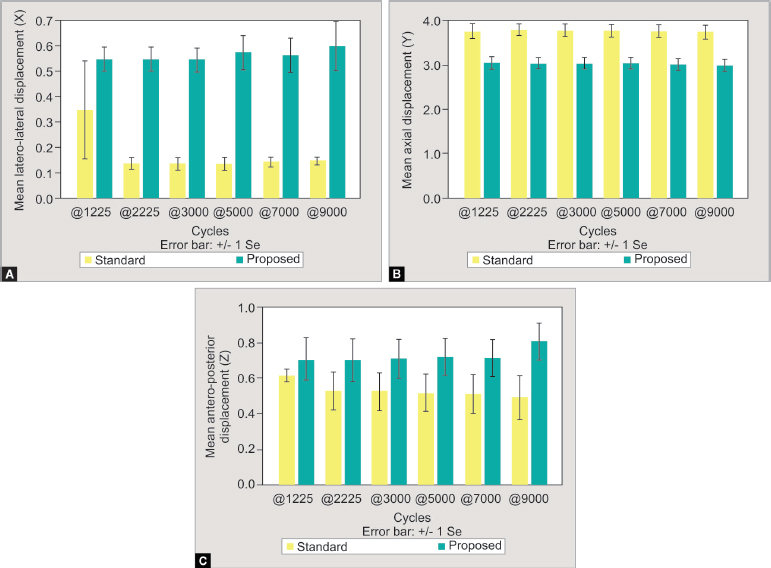
Figs. 4A to C.
The mean relative rotation (degrees) between the markers in the x (roll), y (pitch) and z (yaw) axes over time for standard and test frames
Table 1.
Mean relative displacements between bone fragments in the three axes of movement (mediolateral, axial and anteroposterior) during time for standard and test frames
| Mediolateral displacement (mm) | Axial displacement (mm) | Anteroposterior displacement(mm) | |||||
|---|---|---|---|---|---|---|---|
| Cycles | Mean | SD | Mean | SD | Mean | SD | |
| Standard frame | 1,225 | 0.347 | 0.387 | 3.757 | 0.327 | 0.615 | 0.074 |
| 2,225 | 0.137 | 0.047 | 3.783 | 0.281 | 0.526 | 0.213 | |
| 3,000 | 0.136 | 0.050 | 3.776 | 0.286 | 0.525 | 0.216 | |
| 5,000 | 0.136 | 0.053 | 3.763 | 0.284 | 0.519 | 0.211 | |
| 7,000 | 0.143 | 0.032 | 3.754 | 0.293 | 0.509 | 0.221 | |
| 9,000 | 0.147 | 0.032 | 3.733 | 0.315 | 0.491 | 0.250 | |
| Total | 0.174 | 0.164 | 3.761 | 0.264 | 0.531 | 0.186 | |
| Test frame | 1,225 | 0.547 | 0.093 | 3.039 | 0.275 | 0.707 | 0.242 |
| 2,225 | 0.546 | 0.096 | 3.036 | 0.258 | 0.702 | 0.240 | |
| 3,000 | 0.543 | 0.097 | 3.039 | 0.253 | 0.708 | 0.220 | |
| 5,000 | 0.572 | 0.135 | 3.035 | 0.254 | 0.719 | 0.209 | |
| 7,000 | 0.546 | 0.140 | 3.012 | 0.265 | 0.714 | 0.210 | |
| 9,000 | 0.599 | 0.193 | 2.987 | 0.255 | 0.807 | 0.208 | |
| Total | 0.562 | 0.117 | 3.024 | 0.231 | 0.726 | 0.200 | |
SD, standard deviation.
Table 2.
Mean relative rotations between bone fragments over each movement axis (roll, pitch and yaw) over time using the standard and test frames
| Rotation over x-axis – roll (°) | Rotation over y-axis – pitch (°) | Rotation over z-axis – yaw (°) | |||||
|---|---|---|---|---|---|---|---|
| Cycles | Mean | SD | Mean | SD | Mean | SD | |
| Standard frame | 1,225 | 3.070 | 1.803 | 0.478 | 0.269 | 1.379 | 0.886 |
| 2,225 | 2.130 | 0.696 | 0.437 | 0.208 | 1.396 | 0.679 | |
| 3,000 | 2.172 | 0.778 | 0.429 | 0.195 | 1.425 | 0.737 | |
| 5,000 | 2.177 | 0.842 | 0.438 | 0.187 | 1.535 | 0.654 | |
| 7,000 | 2.157 | 0.851 | 0.431 | 0.181 | 1.564 | 0.635 | |
| 9,000 | 1.882 | 0.703 | 0.359 | 0.101 | 1.486 | 0.457 | |
| Total | 2.264 | 0.982 | 0.428 | 0.177 | 1.464 | 0.467 | |
| Test frame | 1,225 | 2.109 | 0.693 | 0.411 | 0.148 | 1.237 | 0.170 |
| 2,225 | 2.121 | 0.662 | 0.413 | 0.165 | 1.265 | 0.155 | |
| 3,000 | 1.813 | 0.310 | 0.415 | 0.178 | 1.147 | 0.287 | |
| 5,000 | 2.189 | 0.670 | 0.372 | 0.175 | 1.196 | 0.147 | |
| 7,000 | 2.242 | 0.578 | 0.366 | 0.185 | 1.236 | 0.226 | |
| 9,000 | 2.237 | 0.611 | 0.399 | 0.273 | 1.090 | 0.128 | |
| Total | 2.118 | 0.553 | 0.396 | 0.171 | 1.195 | 0.189 | |
SD, standard deviation.
When groups were compared individually in each pre-established cycle acquisition for relative displacement in the mediolateral direction (x-axis), no significant (p = 0.343) differences were seen in 1,225 cycles. In the remaining measurements (2,225, 3,000, 5,000, 7,000 and 9,000 cycles), the relative mediolateral displacement was significantly (p = 0.029) greater in the test frame group.
Numerically, the axial displacement at 1,225 cycles was greater for the standard frame group (3.757 ± 0.327 mm) compared to the alternative frame (3.039 ± 0.275 mm) but not statistically significant (p = 0.057). To detect possible slippage of the wires under load, we cut the wires close to the slotted boltedges. During testing, none of the wires were noted to have been loosened from the frame as we did not observe macroscopic slippage of the wires within the bolts. We believe that the difference in the axial displacement at 1,225 cycles is due to the different rigidity characteristics of the two assemblies. With the remaining measurements at 2,225, 3,000, 5,000, 7,000 and 9,000 cycles, the relative axial displacement was significantly (p = 0.029) greater in the standard frame group. The axial displacement for the standard frame was 3.754 ± 0.293 at 7000th cycle and 3.733 ± 0.315 for 9,000 cycles, suggesting no progressive slippage or loss of tension in the wires. The same finding was seen in the test frame, for which the axial displacement was 3.012 ± 0.265 at 7000th cycle and 2.987 ± 0.255 for 9,000 cycles. The axial displacement for both the frames appeared to have reached a steady state at 9,000 cycles but this could not be confirmed as the test was not continued for greater numbers of cycles.
No differences were seen between groups when the relative displacements in the anteroposterior direction (z-axis) and in any axes of rotation (roll, pitch and yaw) were compared. There were no differences in the mechanical behaviour seen during the different acquisitions over time in each frame-mounting group and no hardware failures during testing indicating that the hardware withstood the applied load. Considering that the test was concluded after 10,000 cycles, it is not possible to affirm if a steady state was reached for axial displacement or tangential displacements on both the tested constructs.
Discussion
Many clinical studies reporting on high-energy tibial plateau fractures treated with classic or hybrid circular external fixation have reported the mean external fixator usage times of between 12 and 19 weeks without fatigue failure of the external fixator components during this period of clinical use.3–5,9,10,17,18 Despite the insufficient number of cycles applied in this study that might have determined the behaviour of the two assemblies that reflected both union and consolidation periods in clinical practice, both frame mountings performed the test without hardware failure.
Pugh et al. concluded that hybrid frames with two levels of fixation in the periarticular segment were stiffer than frames with only one ring, as used in both assemblies for this study.16 The current results showed that external fixation devices with more half-pins replacing the K-wires have different mechanical properties than those that use more K-wires, which agreed with the previous studies.14,16,19–22 These mechanical differences reflect the distinct properties of two different biomechanical systems. Circular external fixators that use many half-pins tend to result in frames with a more unilateral distribution of the components as half-pins tend to be inserted on the subcutaneous surface of the tibia. This creates a resemblance to monolateral external fixators in mechanical behaviour. When subjected to axial loading, linear external fixators behave as cantilevers and sustain bending movements associated with axial displacement.16 The Ilizarov classic circular external fixators use transfixing K-wires exclusively for bone fixation and behave in a distinctive biomechanical manner which permits greater axial flexibility and induces pure axial movement when axial loading is applied.19,20,21–23 This relative axial flexibility associated with bending stability is beneficial for uniform callus formation.16,24,25
Interfragmentary movements are more important to the consolidation process than the forces passing through the bone fragments.26 In animal studies, 1-mm axial movements were associated with a shorter consolidation period.25 However, excessive axial movements and nonaxial movements of any kind that result in shear forces impede bone healing.27 Therefore, an ideal circular external fixation frame mounting would limit angular, translational and rotational movements and allow isolated axial movements.12 When we compared the magnitude of the interfragmentary displacements between the tested groups, we found that the standard frame mounting with K-wires and one half-pin behaved similarly to the classic Ilizarov assembly and allowed greater axial movement (y-axis) and minor mediolateral movement (x-axis) compared with the test frame assembly.
Although these findings may not represent the clinical postoperative period accurately, the testing results demonstrate that there are differences in the mechanical behaviour of the two assemblies.
The increased interfragmentary laterolateral mobility (x-axis) seen in the test frame mounting, i.e., 0.56 ± 0.12 mm compared to 0.17 ± 0.16 mm, may be explained by the complete replacement of K-wires by half-pins in the distal segment; consequent to the local anatomic restrictions of safe corridors, these half-pins are placed on the anteromedial aspect of the tibia and connected to one side of the rings only, and may be responsible for the asymmetric behaviour under loading. Therefore, the test frame provides higher axial stability than the standard assembly, an anteroposterior stability (z-axis) similar between the two groups, and less mediolateral stability.
Mechanical tests comparing eight different assemblies of classic and hybrid circular external fixation in composite femurs revealed that mediolateral movements were the major displacements observed in hybrid circular external fixators.28 However, no previous studies have compared the rotation around the coordinated axes in the assemblies of circular external fixation. The current study has shown no differences between the rotations around the coordinated axes when the two assemblies were compared.
Both frame-mounting groups in this work exhibited mechanical behaviour that tended to be optimal; by this it is meant that the movement of greater magnitude allowed was axial (mean, 3.76 ± 0.26 mm in the standard group and 3.02 ± 0.23 mm in the test group), while in other axes of motion this had averages below 0.8 mm in both groups. The magnitude of these movements can be controlled by increasing the circular external fixation mounting rigidity.12 In assemblies using only tensioned wires for bone fixation, two rings and two tensioned wires per ring are required in each bone fragment to obtain a frame mounting highly resistant to angular displacements that limit shear between bone fragments.16,19,22,23 With the combination of half-pins in hybrid circular external fixation frames, increases in the rigidity of the system are expected.29,30 While half-pins allow micromovements similar to those allowed by K-wires,31 other studies have reported that assemblies with half-pins allow more angular and translational movements when subjected to axial loading than assemblies that use K-wires exclusively.23,28
In an in vivo study of tibial osteotomies treated with hybrid circular external fixators that were comprised of half-pins and K-wires, shear movements surpassed the axial compression.32 In contrast, we observed in both groups that the axial movement (y-axis) overcame movements in other axes. Nevertheless, the hybrid external fixator, which used more half-pins in its mounting (test frame), exhibited mechanical behaviour tending toward that expected of unilateral external fixators, i.e., smaller axial movement and greater mediolateral movement than the standard frame. These differences might have been magnified by the load intensity applied during the tests since most of the biomechanical tests performed previously have used lower loads than those in the current study.15,16,28
Two millimetres of interfragmentary movement in hybrid circular assemblies and up to 2.7 mm of movement in classic circular assemblies when subjected to axial loading of 200 N, equivalent to about 20-kg force, correspond clinically to partial load-bearing.12 We found that even when subjecting both assemblies to an axial load of 1000 N, we obtained an interfragmentary average deviation of 3.02 ± 0.23 mm in the test frame and 3.76 ± 0.26 mm in the standard frame, which was only 1.5 and 1.4 times, respectively, those observed by Gessmann et al.12 when subjecting the assemblies to 200 N load.
Importantly, despite the incentives for patients treated with a circular external fixator, whether hybrid or classic, to bear full weight on treated limbs, many fail to do so and partially limit load-bearing using crutches or walkers.4,33 Consequently, it would be impossible to observe the displacements obtained in this study in clinical practice because the magnitude of the load applied in this trial usually exceeded the load exerted by patients during treatment.
Most studies of the biomechanics of circular external fixation frames have not used assemblies that are mirrored in clinical practice, e.g., by using synthetic cylinders as analogues to the tibia; this disregards the safe corridors that are imposed by the constraints of human anatomy and thus influence how the assembly can be constructed.12,13,20,31,34,35 To facilitate future comparisons with other studies, we used anatomic models and assemblies like those used in clinical practice to treat lesions involving the proximal tibia4 and applied a standardised-loading regimen as described by Higgins et al.1 for biomechanical tests involving fractures of the tibial plateau. As in other studies, only unidirectional loads were applied despite recognising that more complex loads occur during normal human gait.30,36 Henderson et al. applied axial, bending and torsional loads separately when comparing different frame mountings and concluded that even so it does not replicate true multidirectional dynamic loading during gait.13
Study Limitations
The complexity and infinite possible configurations of the devices used in clinical practice restrict extrapolation and comparisons with other studies. Any change or slight variation in the parameters of the assemblies could change the biomechanical conditions in the bone defect.12,25,34
The frame assemblies have been tested in axial loading only which does not represent all the forces encountered physiologically. However, due to asymmetrical location of the bone fixation elements – as dictated by the safe corridors of anatomy – the mechanical system is prone to produce nonaxial movements. So, as the main objective of the investigation was to compare the stability of both designs, we opted to use this simple experimental approach. In addition, the effect of the soft tissue envelope, the stabilising effect of the fibula and the natural stabilisation caused by bone contact and gradually by bone healing could not be assessed in the current study model and should be considered when interpreting the current results.
Conclusion
Although there is no consensus in the literature about the magnitude of the stress, rotation and interfragmentary movement that might inhibit bone healing19,30,37 and, taking into account this study's limitations, the results of this work help in the understanding of the biomechanics and mechanical environment to which the circular external fixator is subjected. An understanding of the load, displacements and biomechanical behaviour at the interfragmentary interval during gait is important, particularly in cases in which there is no contact between bone fragments or in cases in which there is extensive bone comminution.
In conclusion, despite the differences in the mechanical behaviour between the test and standard frames, axial displacement overcame the displacements in other axes with both frames. The test construct (half-pins in the distal segment) shows larger shear motion at the fracture site. Clinical studies are needed to determine if there is a difference between the consolidation rates achieved with the standard and the test frames and if there is a difference in comfort for patients during treatment.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: how does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma. 2007;21(5):301–306. doi: 10.1097/BOT.0b013e3180500359. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/17485994 . [DOI] [PubMed] [Google Scholar]
- 2.Zeltser DW, Leopold SS. Classifications in brief: Schatzker classification of tibial plateau fractures. Clin Orthop Relat Res. 2013;471(2):371–374. doi: 10.1007/s11999-012-2451-z. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El Barbary H, Abdel Ghani H, Misbah H, et al. Complex tibial plateau fractures treated with Ilizarov external fixator with or without minimal internal fixation. Int Orthop. 2005;29(3):182–5. doi: 10.1007/s00264-005-0638-6. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Catagni M, Ottaviani G, Maggioni M. Treatment strategies for complex fractures of the tibial plateau with external circular fixation and limited internal fixation. J Trauma. 2007;63(5):1043–53. doi: 10.1097/ta.0b013e3181238d88. DOI: [DOI] [PubMed] [Google Scholar]
- 5.Ali AM. Outcomes of open bicondylar tibial plateau fractures treated with Ilizarov external fixator with or without minimal internal fixation. Eur J Orthop Surg Traumatol. 2013;23(3):349–55. doi: 10.1007/s00590-012-0989-9. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Wu CC, Tai CL. Plating treatment for tibial plateau fractures: a biomechanical comparison of buttress and tension band positions. Arch Orthop Trauma Surg. 2007;127(1):19–24. doi: 10.1007/s00402-006-0192-8. DOI: [DOI] [PubMed] [Google Scholar]
- 7.Zura RD, Browne JA, Black MD, et al. Current management of high-energy tibial plateau fractures. Curr Orthop. 2007;21(3):229–35. doi: 10.1016/j.cuor.2007.02.007. DOI: [DOI] [Google Scholar]
- 8.Ali AM, Saleh M, Bolongaro S, et al. The strength of different fixation techniques for bicondylar tibial plateau fractures – a biomechanical study. Clin Biomech. 2003;18(9):864–70. doi: 10.1016/s0268-0033(03)00149-9. DOI: [DOI] [PubMed] [Google Scholar]
- 9.Ariffin HM, Mahdi NM, Rhani SA, et al. Modified hybrid fixator for high-energy Schatzker V and VI tibial plateau fractures. Strateg Trauma Limb Reconstr. 2011;6(1):21–6. doi: 10.1007/s11751-011-0105-4. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramos T, Ekholm C, Eriksson BI, et al. The Ilizarov external fixator: a useful alternative for the treatment of proximal tibial fractures. A prospective observational study of 30 consecutive patients. BMC Musculoskelet Disord. 2013;14(1):11. doi: 10.1186/1471-247414-11. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKee MD, Pirani S, Stephen DJG. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures: results of a multicenter, prospective, randomized clinical trial. J Bone Joint Surg. 2006;88(12):2613–23. doi: 10.2106/jbjs.e.0141. DOI: Available at: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed7&NEWS=N&AN=2006608279 . [DOI] [PubMed] [Google Scholar]
- 12.Gessmann J, Citak M, Jettkant B, et al. The influence of a weight-bearing platform on the mechanical behavior of two Ilizarov ring fixators: tensioned wires vs. half-pins. J Orthop Surg Res. 2011;6:61. doi: 10.1186/1749-799X-6-61. DOI: Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3264501&tool=pmcentrez&rendertype=abstract . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henderson DJ, Rushbrook JL, Stewart TD, et al. What are the biomechanical effects of half-pin and fine-wire configurations on fracture site movement in circular frames? Clin Orthop Relat Res. 2016;474(4):1041–9. doi: 10.1007/s11999-015-4652-8. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pugh KJ, Wolinsky PR, Dawson JM, et al. The biomechanics of hybrid external fixation. J Orthop Trauma. 1999;13(1):20–6. doi: 10.1097/00005131-199901000-00006. DOI: [DOI] [PubMed] [Google Scholar]
- 15.Yilmaz E, Belhan O, Karakurt L, et al. Mechanical performance of hybrid Ilizarov external fixator in comparison with Ilizarov circular external fixator. Clin Biomech. 2003;18(6):518–22. doi: 10.1016/s0268-0033(03)00073-1. DOI: [DOI] [PubMed] [Google Scholar]
- 16.Yang L, Nayagam S, Saleh M. Stiffness characteristics and inter-fragmentary displacements with different hybrid external fixators. Clin Biomech. 2003;18(2):166–72. doi: 10.1016/S0268-0033(02)00175-4. DOI: [DOI] [PubMed] [Google Scholar]
- 17.Ali AM, Yang L, Hashmi M, et al. Bicondylar tibial plateau fractures managed with the Sheffield Hybrid Fixator. Biomechanical study and operative technique. Injury. 2001;32(Suppl. 4):SD86–91. doi: 10.1016/s0020-1383(01)00165-6. DOI: [DOI] [PubMed] [Google Scholar]
- 18.Dendrinos GK, Kontos S, Katsenis D, et al. Treatment of high-energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br. 1996;78(5):710–7. doi: 10.1302/0301-620X.78B5.0780710. DOI: Available at: http://www.mjdrdypu.org/text.asp?2013/6/1/33/108637 . [DOI] [PubMed] [Google Scholar]
- 19.Aronson J, Harp JH. Mechanical considerations in using tensioned wires in a transosseous external fixation system. Clin Orthop Relat Res. 1992;(280):23–9. doi: 10.1097/00003086-199207000-00005. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/1611749 . [DOI] [PubMed] [Google Scholar]
- 20.Calhoun JH, Li F, Ledbetter BR, et al. Biomechanics of the Ilizarov fixator for fracture fixation. Clin Orthop Relat Res. 1992;(280):15–22. doi: 10.1097/00003086-199207000-00004. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/1611735 . [DOI] [PubMed] [Google Scholar]
- 21.Fleming B, Paley D, Kristiansen , et al. A biomechanical analysis of the Ilizarov external fixator. Clin Orthop Relat Res. 1989;(241):95–105. doi: 10.1097/00003086-198904000-00012. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/2924484 . [DOI] [PubMed] [Google Scholar]
- 22.Podolsky A, Chao EY. Mechanical performance of Ilizarov circular external fixators in comparison with other external fixators. Clin Orthop Relat Res. 1993;(293):61–70. doi: 10.1097/00003086199308000-00009. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/8339510 . [DOI] [PubMed] [Google Scholar]
- 23.Khalily C, Voor MJ, Seligson D. Fracture site motion with Ilizarov and “hybrid” external fixation. J Orthop Trauma. 1998;12(1):21–6. doi: 10.1097/00005131-199801000-00004. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/9447515 . [DOI] [PubMed] [Google Scholar]
- 24.Claes L, Heigele CA, Neidlinger-Wilke C, et al. Effects of mechanical factors on the fracture healing process. Clin Orthop Relat Res. 1998;(355S):S132–47. doi: 10.1097/00003086-199810001-00015. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/9917634 . [DOI] [PubMed] [Google Scholar]
- 25.Goodship AE, Kenwright J. The influence of induced micromovement upon the healing of experimental tibial fractures. J Bone Joint Surg Br. 1985;(67):650–5. doi: 10.1302/0301-620X.67B4.4030869. DOI: [DOI] [PubMed] [Google Scholar]
- 26.Augat P, Margevicius K, Simon J, et al. Local tissue properties in bone healing: influence of size and stability of the osteotomy gap. J Orthop Res. 1998;16(4):475–81. doi: 10.1002/jor.1100160413. DOI: [DOI] [PubMed] [Google Scholar]
- 27.Augat P, Burger J, Schorlemmer S, et al. Shear movement at the fracture site delays healing in a diaphyseal fracture model. J Orthop Res. 2003;21(6):1011–7. doi: 10.1016/S0736-0266(03)00098-6. DOI: [DOI] [PubMed] [Google Scholar]
- 28.Baran O, Havitcioglu H, Tatari H, et al. The stiffness characteristics of hybrid Ilizarov fixators. J Biomech. 2008;41(14):2960–3. doi: 10.1016/j.jbiomech.2008.07.030. DOI: [DOI] [PubMed] [Google Scholar]
- 29.Duda GN, Kassi JP, Hoffmann JE, et al. Mechanical behavior of Ilizarov ring fixators. Effect of frame parameters on stiffness and consequences for clinical use. Unfallchirurg. 2000;103(10):839–45. doi: 10.1007/s001130050630. DOI: [DOI] [PubMed] [Google Scholar]
- 30.Lenarz C, Bledsoe G, Watson JT. Circular external fixation frames with divergent half pins: A pilot biomechanical study. Clin Orthop Relat Res. 2008;466(12):2933–9. doi: 10.1007/s11999-008-0492-0. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khurana A, Byrne C, Evans S, et al. Comparison of transverse wires and half pins in Taylor Spatial Frame: a biomechanical study. J Orthop Surg Res. 2010;5(23) doi: 10.1186/1749-799X-5-23. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/20346178 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duda GN, Sollmann M, Sporrer S, et al. Interfragmentary motion in tibial osteotomies stabilized with ring fixators. Clin Orthop Relat Res. 2002;(396):163–72. doi: 10.1097/00003086-200203000-00025. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/11859239 . [DOI] [PubMed] [Google Scholar]
- 33.Hasler CC, Krieg AH. Current concepts of leg lengthening. J Child Orthop. 2012;6(2):89–104. doi: 10.1007/s11832-012-0391-5. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bronson DG, Samchukov ML, Birch JG, et al. Stability of external circular fixation: a multi-variable biomechanical analysis. Clin Biomech. 1998;13(6):441–8. doi: 10.1016/s0268-0033(98)00007-2. DOI: [DOI] [PubMed] [Google Scholar]
- 35.Davidson AW, Mullins M, Goodier D, et al. Ilizarov wire tensioning and holding methods: a biomechanical study. Injury. 2003;34(2):151–4. doi: 10.1016/s0020-1383(02)00045-1. DOI: [DOI] [PubMed] [Google Scholar]
- 36.Aquarius R, Van Kampen A, Verdonschot N. Rapid pre-tension loss in the Ilizarov external fixator: an in vitro study. Acta Orthop. 2007;78(5):654–60. doi: 10.1080/17453670710014356. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/17966025 . [DOI] [PubMed] [Google Scholar]
- 37.Kummer FJ. Biomechanics of the Ilizarov external fixator. Clin Orthop Relat Res. 1992;(280):11–4. doi: 10.1097/00003086-199207000-00003. DOI: Available at: http://www.ncbi.nlm.nih.gov/pubmed/1611730 . [DOI] [PubMed] [Google Scholar]