Supplemental Digital Content is available in the text.
Key Words: distrust, race and ethnicity, sex, veterans
Abstract
Background:
On April 23, 2014, US media outlets broadcast reports of excessive wait times and “secret” waitlists at some Veterans Affairs (VA) hospitals, precipitating legislation to increase Veterans’ access to private sector health care.
Objective:
The aims were to assess changes in Veterans’ distrust in the VA health care system before and after the media coverage and explore sex and racial/ethnic differences in the temporal patterns.
Methods:
Veterans completed semistructured interviews on health care satisfaction from June 2013 to January 2015, including a validated scale of health system distrust (range: 1–5). We used linear splines with knots at 90-day intervals to assess changes in distrust before and after April 23, 2014 (“day 0”) in linear mixed models. To explore sex and racial/ethnic differences in temporal patterns, we stratified models by sex and tested for interactions of race/ethnicity with time.
Results:
For women (n=600), distrust scores (mean=2.09) increased by 0.45 in days 0–90 (P<0.01), then decreased by 0.45 in days 90–180 (P<0.01). Among men (n=575), distrust scores (mean=2.05) increased by 0.18 in days 0–90 (P=0.059). Distrust levels were significantly higher for Black versus White women (time adjusted mean difference=0.21) and for Black and Hispanic versus White men (differences=0.26 and 0.18). However, the temporal patterns did not vary by race/ethnicity for women or men (interaction P=0.85 and 0.21, respectively).
Conclusions:
Health system distrust increased in women following media coverage of VA access problems and was higher in Black/Hispanic versus White Veterans at all time periods. Such perceptions could influence Veteran decisions to seek health care in the community rather than VA.
On April 23, 2014, national media outlets released stories of excessive wait times and “secret” waitlists at select Veterans Affairs (VA) Medical Centers, with some Veterans dying while waiting for care. This news coverage fueled ongoing political debate over access to VA care, and was one of many factors contributing to the United States Congress passing the 2014 Veterans Access, Choice and Accountability Act.1 This legislation expanded Veteran eligibility to receive health care purchased by the VA from the private sector.2
While the negative publicity influenced policy and health system changes, the impact of this media coverage on Veterans’ distrust of the VA health care system is unknown. Health system distrust involves unfavorable expectations or wariness of an organization’s competence and values.3,4 It is associated with lower adherence to treatment recommendations and poorer health.5–9 Health system distrust tends to be higher for women versus men and Black versus White patients10–13 because of negative health care encounters, personal experiences of discrimination,10,14 and the legacy of systemic racism and unethical medical experiments.15
We sought to determine whether patterns of health system distrust changed following the media coverage on April 23, 2014 (ie, April 23), and to explore sex and racial/ethnic differences in the temporal patterns. Leveraging data from a national survey of patient experiences with VA health care conducted from June 2013 to January 2015, we hypothesized that Veterans interviewed after April 23 would have higher ratings of distrust than those interviewed before April 23. We further hypothesized these differences would be greater for women versus men and Black/Hispanic versus White Veterans.
METHODS
Design
This study surveyed health system distrust in a diverse sample of VA outpatients who were interviewed as part of the Disparities in Satisfaction with Care (DISC) parent study.16 DISC used a multistep recruitment and consent process to enroll Veterans from 25 largely minority-serving VA medical centers to participate in telephone interviews about their satisfaction with VA health care.16 The study was approved by Institutional Review Boards at the authors’ institutions.
Recruitment
As reported elsewhere,16 DISC used VA administrative records to identify Veteran outpatients from 25 VA medical centers in Fiscal Year 2012–2013 and to select a stratified, random sample of Veterans from each site.16 The study sites were geographically diverse and served relatively large proportions of racial/ethnic minority Veterans. From each site, 90 Veterans were selected in each of 6 strata (male and female Veterans of White, Black, and Hispanic race/ethnicity). Selected individuals were mailed a description of the study with the choice to opt-out of screening by telephone or mail. Those not opting out were telephoned to confirm study eligibility, then interviewed by a professional survey organization following oral consent and written permission for audiorecording. Veterans were paid $35 for their participation.
Recruitment began in all 25 sites simultaneously and continued until target numbers of interviews within all 6 strata were completed within sites. The response rate among 1929 eligible Veterans was 63.3%.16 For the current analysis, we focused on DISC participants who completed the health system distrust measure. We excluded data from 16 participants from racial/ethnic groups other than White, Black, or Hispanic as the numbers were too small to make meaningful comparisons.
Measures
Participants self-reported sociodemographic and clinical characteristics previously shown to correlate with patient experiences with care and ratings of distrust (Table 1; age, sex, race/ethnicity, level of education, depression, and medical comorbidity).10,17–20 Participants were also asked if they received all of their health care from the VA.
TABLE 1.
Baseline Characteristics of Individuals Interviewed Before or After the 2014 Media Coverage of Waitlists for VA Health Care, Stratified by Sex
| Women | Men | |||||
|---|---|---|---|---|---|---|
| Characteristics | Interview Before April 23, 2014 (n=239), N (%) | Interview After April 23, 2014 (n=361), N (%) | P | Interview Before April 23, 2014 (n=249), N (%) | Interview After April 23, 2014 (n=326), N (%) | P |
| Race/ethnicity | 0.38 | <0.001 | ||||
| White | 87 (36.4) | 119 (33.0) | 117 (47.0) | 84 (25.8) | ||
| Black | 82 (34.3) | 117 (32.4) | 71 (28.5) | 112 (34.4) | ||
| Hispanic | 70 (29.3) | 125 (34.6) | 61 (24.5) | 130 (39.9) | ||
| Age (mean, SD) | 49.2 (13.7) | 50.6 (13.4) | 0.21 | 61.7 (13.5) | 59.8 (13.6) | 0.10 |
| Education | 0.47 | 0.048 | ||||
| ≤High school | 14 (6.0) | 31 (8.7) | 61 (24.7) | 71 (21.9) | ||
| Trade school/some college | 110 (47.0) | 160 (44.7) | 98 (39.7) | 162 (49.9) | ||
| ≥College graduate | 110 (47.0) | 167 (46.7) | 88 (35.6) | 92 (28.3) | ||
| No. health conditions (mean, SD)* | 2.3 (0.1) | 2.5 (0.1) | 0.09 | 2.5 (0.1) | 2.5 (0.1) | 0.95 |
| Depression † | 98 (41.0) | 188 (52.2) | 0.01 | 88 (35.5) | 135 (47.8) | 0.13 |
| Received all health care at VA | 129 (54.0) | 238 (65.9) | <0.01 | 151 (60.9) | 222 (68.3) | 0.07 |
| Days before/following April 23, 2014 | ||||||
| >180 d prior | 55 (23.0) | 64 (25.7) | ||||
| 91–180 d prior | 27 (11.3) | 41 (16.5) | ||||
| 0–90 d prior | 157 (65.7) | 144 (57.8) | ||||
| 0–90 d after | 205 (56.8) | 205 (52.5) | ||||
| 91–180 d after | 132 (36.6) | 132 (40.5) | ||||
| >180 d after | 24 (6.7) | 24 (7.1) | ||||
Number of health conditions (0–12) at the time of the interview, from the self-report Charlson comorbidity index.
Depression, from the Charlson comorbidity index, was self-reported at the time of the interview.
VA indicates Veterans Affairs.
In addition to sex and race/ethnicity, the independent variable of interest was time. We counted the number of days between the interview date and the beginning of media exposure, with “Day 0” defined as April 23.
We measured distrust using the Health Care System Distrust scale (see Table, Online Digital Supplement 1, for scale items, http://links.lww.com/MLR/C229). This validated, multidimensional instrument assesses trust in an institution’s competence and values21 through 9 Likert-type items ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). Items are coded so that higher scores correspond to greater distrust. We calculated an overall distrust score as the average of item responses for participants with <3 missing items. Analogous to mean imputation, this is a standard approach for handling small amounts of missing data. We repeated these procedures for the 2 distrust subscales: competence and values.21
Statistical Analyses
In descriptive analyses, we used median spline plots to assess unadjusted patterns of distrust over time for the overall sample, by sex and by race/ethnicity. Because the preliminary graphs suggested changing slopes over time and unique patterns for women versus men, we operationalized time with a series of linear splines and stratified all statistical analyses by sex.
We first compared the sociodemographic characteristics of participants who were interviewed before versus after April 23. We used χ2 and t test statistics to compare group differences in categorical and continuous variables, respectively. To assess the temporal trends in distrust before and after day 0, we evaluated the slopes of a piecewise linear function defined over the DISC interview period (ie, −299 to 274 d) in terms of linear splines with knots defined at 90-day intervals, centered at day 0. The linear mixed effect models included fixed effects for race/ethnicity and a random effect for site. To account for the possibility that patient sociodemographic characteristics may have differed across groups interviewed before versus after April 23, we repeated the study analyses controlling for participant sociodemographic characteristics collected at the time of their interview. Then, to explore racial/ethnic differences in patterns of distrust over time, we reran the study models with race/ethnicity by linear spline interaction terms.
In sensitivity analyses, we assessed possible nonlinearity by comparison to cubic splines and ran the study models separately for the competence and values subscales. All analyses were conducted in Stata v15 and 2-tailed P-values <0.05 were considered statistically significant throughout.
RESULTS
Of 1206 DISC participants, 1175 (97.4%) White, Black, or Hispanic women and men completed the distrust measure. Within this study sample, 687 Veterans (n=18–38 per site) were interviewed after April 23.
Characteristics of Participants Interviewed Before and After the Media Exposure
There were few differences in the sociodemographic characteristics of participants interviewed before versus after April 23 (Table 1). A smaller percentage of women interviewed before April 23 had depression (41% vs. 52%, P=0.01) or received all of their health care in the VA (54% vs. 66%, P<0.01), compared with those interviewed after this date. Men interviewed before April 23 were more often White (47% vs. 26%, P<0.001) with 4-year college degrees (36% vs. 28%, P=0.048) than those interviewed after this date.
Patterns of Veterans Affairs Health System Distrust Over Time, by Sex and Race/Ethnicity
In bivariate analyses, women and men exhibited unique patterns of health system distrust after the media exposure (Fig. 1). Among women, the average rating of distrust before day 0 was 2.09 (SD=0.64). There was no change in the level of distrust during the time interval before day 0 (ie, time slopes were not significantly different from 0). However, after the media exposure, levels of distrust increased by 0.005 per day (0.45 overall) over the subsequent 90 days (P<0.001), followed by a significant decrease in distrust of −0.005 per day (0.45 overall) over days 91–180 (P<0.01).
FIGURE 1.
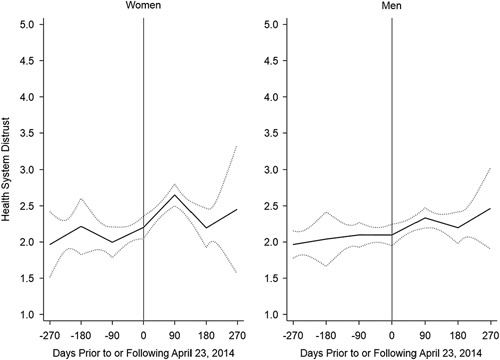
Predicted rating of health system distrust before and after the 2014 media coverage of waitlists for Veterans Affairs health care, stratified by sex. Time is represented here as the number of days before or following April 23, 2014 (“Day 0”), when news of Veterans Affairs waitlists was first reported by cable news network. Solid lines are predicted ratings of health system distrust, and dashed lines are the 95% upper and lower confidence intervals, estimated from a mixed effect linear regression that included fixed effects for time (operationalized as linear splines with nodes at 90-day intervals) and race/ethnicity, and a random effect for site.
Among men, the average rating of distrust before day 0 was 2.05 (SD=0.64). There were no changes in levels of health system distrust over time (ie, time slopes were not significantly different from 0), except for a borderline significant increase in distrust in days 0–90 following the media exposure (0.002 per day, 0.18 over 90 d; P=0.059). The time patterns for women and men were largely unchanged when controlling for other measured sociodemographic characteristics (Table 2).
TABLE 2.
Health System Distrust Before and After the 2014 Media Coverage of Waitlists for VA Health Care, Stratified by Sex
| Women | Men | |||||
|---|---|---|---|---|---|---|
| Characteristic | β | 95% CI | P | β | 95% CI | P |
| Days before or following April 23, 2014 | ||||||
| >180 d prior | 0.002 | −0.006 to 0.010 | 0.68 | 0.001 | −0.005 to 0.005 | 0.99 |
| 91–180 d prior | −0.002 | −0.007 to 0.003 | 0.45 | 0.001 | −0.004 to 0.005 | 0.77 |
| 0–90 d prior | 0.002 | −0.001 to 0.005 | 0.16 | −0.001 | −0.003 to 0.002 | 0.93 |
| 1–90 d following | 0.005 | 0.002 to 0.007 | <0.001 | 0.002 | −0.001 to 0.005 | 0.05 |
| 91–180 d following | −0.005 | −0.009 to −0.001 | <0.01 | −0.001 | −0.004 to 0.002 | 0.52 |
| >180 d following | 0.003 | −0.008 to 0.014 | 0.57 | 0.001 | −0.005 to 0.008 | 0.71 |
| Race/ethnicity | ||||||
| White (reference) | 1.0 | 1.0 | ||||
| Black | 0.205 | 0.059 to 0.350 | <0.01 | 0.263 | 0.138 to 0.388 | <0.001 |
| Hispanic | 0.022 | −0.130 to 0.174 | 0.78 | 0.177 | 0.051 to 0.304 | <0.01 |
| Age | −0.005 | −0.010 to 0.001 | 0.05 | −0.001 | −0.005 to 0.003 | 0.52 |
| Education | ||||||
| ≤High school (reference) | 1.0 | 1.0 | ||||
| Trade school/some college | −0.035 | −0.270 to 0.199 | 0.77 | 0.012 | −0.116 to 0.140 | 0.84 |
| ≥College graduate | 0.012 | −0.229 to 0.248 | 0.92 | 0.026 | −0.113 to 0.165 | 0.72 |
| No. health conditions | 0.071 | 0.023 to 0.120 | <0.01 | 0.004 | −0.032 to 0.165 | 0.90 |
| Depression | 0.060 | −0.106 to 0.226 | 0.48 | 0.374 | 0.240 to 0.509 | <0.001 |
| Received all health care at VA | −0.135 | −0.260 to −0.010 | 0.03 | −0.260 | −0.370 to −0.149 | <0.001 |
β coefficients, obtained from mixed effect linear regressions, represent adjusted differences in average distrust ratings. Time, operationalized as number of days before or following media coverage of VA waitlists, is represented as a series of linear splines with nodes at 90-day intervals. Positive spline coefficients indicate that, accounting for measured characteristics of participants interviewed in each time period, ratings of distrust increased monotonically with each day during the time interval. Negative spline coefficients indicate that, accounting for measured characteristics of participants interviewed in each time period, ratings of distrust decreased monotonically during the time interval. β coefficients for the covariates are interpreted as differences in distrust after accounting for the interview date. For instance, the β for Black women is 0.205, indicating that ratings of distrust were 0.21 points higher on average in all time periods than ratings for women.
CI indicates confidence interval; VA, Veterans Affairs.
Racial/ethnic differences in levels of distrust were also observed (Table 2). Specifically, distrust levels were 0.21 points higher for Black than White women (P=0.001), and 0.26 and 0.18 points higher for Black and Hispanic men, compared with White men (P<0.01 for each pairwise comparison).
Whereas levels of distrust were higher among racial/ethnic minorities than for White Veterans stratified by sex, the disparity patterns did not differ over time (Figure, Supplemental Digital Content 2, http://links.lww.com/MLR/C230). The interactions of race/ethnicity and time in predicting distrust were nonsignificant (P-values for joint tests of interaction were P=0.85 and 0.21 in the models for women and men, respectively).
Sensitivity Analyses
In sensitivity analyses, models that considered cubic splines offered no superior performance to those with linear splines (P’s>0.05). The pattern of results for the competence and values subscales mirrored the pattern for the overall distrust score (results not shown).
DISCUSSION
This study examined distrust of the VA health care system at a time of intense public scrutiny and political pressure to privatize care for Veterans. In a national sample, we found low levels of distrust in men and women before media broadcasts of VA waitlists, followed by increases in health system distrust among women in the first 90 days after the broadcasts. Black and Hispanic Veterans had consistently higher levels of distrust compared with White Veterans, which did not change following the media release. The findings illustrate how some Veterans’ trust in the health care system can waver when institutions are stressed by negative events.
Results from this study have implications for current care seeking. Since 2014, the VA has greatly expanded community care initiatives (eg, Veterans Choice Program, MISSION Act) that allow eligible Veterans to receive health care purchased by the VA from the private sector, and trust in the health care system is one factor in Veteran intentions to use VA versus non-VA health care options.22,23 Whereas our study was largely conducted before these expansions, our finding that distrust was higher for Veterans receiving only some versus all of their health care in the VA suggests that Veterans who distrust the VA may be more inclined to seek outside care. Events that erode Veteran trust in the VA could potentially lead more Veterans to choose community care when they are eligible for it. Conducting research into the quality of care at VA versus community care settings and developing educational tools to inform Veterans about the VA’s unique services and strengths could help to improve Veterans’ trust and confidence in choosing the VA.
Our findings of sex differences in temporal patterns and persisting racial/ethnic disparities do suggest that concentrated efforts may be needed to earn the trust of Veterans who belong to historically marginalized groups. Women’s propensity for distrust could stem from harassment in the military or health care settings,24–26 and the VA is working to remedy situations that make women leery of the VA. Bystander training, one intervention to address sex discrimination and harassment, could be evaluated for its potential to mitigate health system distrust.27 In addition, attending to institutional racism and experiences of discrimination in VA health care settings28 could be a first step toward earning the trust of Black men and women and Hispanic men. For all patients from historically marginalized groups, human-centered design, a framework for working with patients in co-designing health system reforms, may help to improve their trust in the health care system.29
This study has limitations. First, results are derived from a stratified sample of patients drawn from largely minority-serving VA facilities and may not generalize to all Veterans. Second, in four facilities study recruitment was complete within 180 days of April 23, 2014, reducing the precision of our estimates of distrust >180 days following the media reporting. Third, the samples of Veterans from specific sex and race/ethnicity groups interviewed within each 90-day time interval were small. This may have limited our power to detect statistical differences in temporal patterns for subgroups of minority women and men. Finally, the observational study design limits causal interpretations.
CONCLUSIONS
At a time when media coverage focused on VA access problems and “secret” waitlists, women’s distrust of the VA health care system increased. Efforts to enhance Veterans’ trust in the VA health care system will continue to be important as Veterans currently have more options to choose VA-supported health care in the community from non-VA providers.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
Footnotes
This work was supported by Department of Veterans Affairs Health Services Research and Development Merit Review (IIR 100144) and Service Directed Research (13-425) awards, and the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538 and KL2TR002539. The views expressed here are those of the authors and do not represent those of the Department of Veterans Affairs, National Institutes of Health, or the United States Government.
The authors declare no conflict of interest.
Contributor Information
Audrey L. Jones, Email: Audrey.Jones3@va.gov.
Michael J. Fine, Email: Michael.Fine@va.gov.
Peter A. Taber, Email: Peter.Taber@hsc.utah.edu.
Leslie R.M. Hausmann, Email: Leslie.Hausmann@va.gov.
Kelly H. Burkitt, Email: Kelly.Burkitt@va.gov.
Roslyn A. Stone, Email: ajones0719@gmail.com.
Susan L. Zickmund, Email: Susan.Zickmund@va.gov.
REFERENCES
- 1.Veterans Access, Choice, and Accountability Act of 2014, Public Law 113-146, 128 Stat. 1754. August 7, 2014.
- 2.US Government Accountability Office. VA Health Care: Estimating Resources Needed to Provide Community Care. Washington, DC: United States Government Accountability Office; 2019. [Google Scholar]
- 3.Hall MA, Dugan E, Zheng B, et al. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79:613–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ozawa S, Sripad P. How do you measure trust in the health system? A systematic review of the literature. Soc Sci Med. 2013;91:10–14. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong K, Rose A, Peters N, et al. Distrust of the health care system and self-reported health in the United States. J Gen Intern Med. 2006;21:292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang TC, Matthews SA, Hillemeier MM. Effect of health care system distrust on breast and cervical cancer screening in Philadelphia, Pennsylvania. Am J Public Health. 2011;101:1297–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang TC, Matthews SA, Shoff C. Individual health care system distrust and neighborhood social environment: how are they jointly associated with self-rated health? J Urban Health. 2011;88:945–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whetten K, Leserman J, Whetten R, et al. Exploring lack of trust in care providers and the government as a barrier to health service use. Am J Public Health. 2006;96:716–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohseni M, Lindstrom M. Social capital, trust in the health-care system and self-rated health: the role of access to health care in a population-based study. Soc Sci Med. 2007;64:1373–1383. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong K, Putt M, Halbert CH, et al. Prior experiences of racial discrimination and racial differences in health care system distrust. Med Care. 2013;51:144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Armstrong K, McMurphy S, Dean LT, et al. Differences in the patterns of health care system distrust between Blacks and Whites. J Gen Intern Med. 2008;23:827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guerrero N, Mendes de Leon CF, Evans DA, et al. Determinants of trust in health care in an older population. J Am Geriatr Soc. 2015;63:553–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Myaskovsky L, Burkitt KH, Lichy AM, et al. The association of race, cultural factors, and health-related quality of life in persons with spinal cord injury. Arch Phys Med Rehabil. 2011;92:441–448. [DOI] [PubMed] [Google Scholar]
- 14.Boulware LE, Cooper LA, Ratner LE, et al. Race and trust in the health care system. Public Health Rep. 2003;118:358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griffith DM, Bergner EM, Fair AS, et al. Using mistrust, distrust, and low trust precisely in medical care and medical research advances health equity. Am J Prev Med. 2021;60:442–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zickmund SL, Burkitt KH, Gao S, et al. Racial, ethnic, and gender equity in Veteran satisfaction with health care in the Veterans Affairs health care system. J Gen Intern Med. 2018;33:305–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cunningham CO, Sohler NL, Korin L, et al. HIV status, trust in health care providers, and distrust in the health care system among Bronx women. AIDS Care. 2007;19:226–234. [DOI] [PubMed] [Google Scholar]
- 18.Gupta C, Bell SP, Schildcrout JS, et al. Predictors of health care system and physician distrust in hospitalized cardiac patients. J Health Commun. 2014;19(suppl 2):44–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chanfreau-Coffinier C, Gordon HS, Schweizer CA, et al. Mental health screening results associated with women Veterans’ ratings of provider communication, trust, and care quality. Womens Health Issues. 2018;28:430–438. [DOI] [PubMed] [Google Scholar]
- 20.Chaudhry S, Jin L, Meltzer D. Use of a self-report-generated Charlson Comorbidity Index for predicting mortality. Med Care. 2005;43:607–615. [DOI] [PubMed] [Google Scholar]
- 21.Shea JA, Micco E, Dean LT, et al. Development of a revised Health Care System Distrust scale. J Gen Intern Med. 2008;23:727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagner TH, Taylor T, Cowgill E, et al. Intended and unintended effects of large-scale adverse event disclosure: a controlled before-after analysis of five large-scale notifications. BMJ Qual Saf. 2015;24:295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haro E, Mader M, Noel PH, et al. The impact of trust, satisfaction, and perceived quality on preference for setting of future care among Veterans with PTSD. Mil Med. 2019;184:e708–e714. [DOI] [PubMed] [Google Scholar]
- 24.Kehle-Forbes SM, Harwood EM, Spoont MR, et al. Experiences with VHA care: a qualitative study of US women veterans with self-reported trauma histories. BMC Womens Health. 2017;17:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kimerling R, Pavao J, Valdez C, et al. Military sexual trauma and patient perceptions of Veteran Health Administration health care quality. Womens Health Issues. 2011;21(suppl):S145–S151. [DOI] [PubMed] [Google Scholar]
- 26.Klap R, Darling JE, Hamilton AB, et al. Prevalence of stranger harassment of women Veterans at Veterans Affairs medical centers and impacts on delayed and missed care. Womens Health Issues. 2019;29:107–115. [DOI] [PubMed] [Google Scholar]
- 27.Relyea MR, Portnoy GA, Klap R, et al. Evaluating bystander intervention training to address patient harassment at the Veterans Health Administration. Womens Health Issues. 2020;30:320–329. [DOI] [PubMed] [Google Scholar]
- 28.Hausmann LRM, Jones AL, McInnes SE, et al. Identifying healthcare experiences associated with perceptions of racial/ethnic discrimination among veterans with pain: a cross-sectional mixed methods survey. PLoS One. 2020;15:e0237650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wheelock A, Bechtel C, Leff B. Human-centered design and trust in medicine. JAMA. 2020;324:2369–2370. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.


