Abstract
Background
Neuregulin 4 (Nrg4), a novel adipokine enriched in brown adipose tissue has been observed to negatively regulate de novo hepatic lipogenesis and limit nonalcoholic fatty liver disease (NAFLD) progression to nonalcoholic steatohepatitis (NASH) in rodents. However, the role of Nrg4 in human NAFLD remains unclear to date. We analysed Nrg4 plasma levels and its association with liver disease severity together with the transcriptional profile of the Nrg4 pathway in liver and visceral adipose tissue (VAT) of NAFLD patients.
Methods
Plasma Nrg4 levels were measured in 65 NAFLD patients and 43 healthy controls (HC). Hepatic steatosis and fibrosis were diagnosed and quantified with chemical shift MRI and transient elastography respectively. Furthermore, blood lipid levels, HOMA-IR and systemic pro-inflammatory cytokines (TNF-α, IL-6 and IFN-γ) were analysed. Microarray analyses to assess differences in the Nrg4 and its receptor family ErbB pathway in liver and VAT from an independent patient group with biopsy proven NAFL (simple steatosis) (n = 4), NASH (n = 5) and normal liver (n = 6) were performed.
Results
Plasma Nrg4 levels were not significantly different between NAFLD patients and HC (p = 0.622). Furthermore, plasma Nrg4 levels did not correlate with the hepatic fat fraction (r = -0.028, p = 0.829) and were not significantly different between NAFLD patients with or without hepatic fibrosis (p = 0.087). Finally, the expression profile of 82 genes related to the Nrg4-ErbB pathway in liver and VAT was not significantly different between NAFL, NASH or obese controls.
Conclusion
Our study does not support a role for Nrg4 in the pathophysiology of human NAFLD.
Introduction
Nonalcoholic fatty liver disease (NAFLD) affects 25% of the general population worldwide [1]. It is a disease spectrum ranging from simple steatosis (NAFL) to nonalcoholic steatohepatitis (NASH) that can lead to cirrhosis [2]. NAFLD is strongly associated with metabolic comorbidities including obesity, metabolic syndrome and type 2 diabetes. Recently, metabolic associated fatty liver disease (MAFLD) has been proposed as a new name for NAFLD, reflecting its complex pathophysiology in a milieu of systemic metabolic dysfunction [3, 4]. Multiple factors such as adipose tissue dysfunction, insulin resistance, dietary habits, microbiome perturbations and genetic predisposition all contribute to the development and progression of NAFLD [5]. Recently the role of brown adipose tissue (BAT) in the pathophysiology of NAFLD has gained interest after the discovery of BAT in adults and its reduced activity in overweight and obese subjects [6]. An inverse correlation between BAT presence (measured with PET-CT) and NAFLD prevalence was observed in humans [7]. BAT can increase energy expenditure through heat production (via the unique expression of uncoupling protein 1) and is therefore a potential therapeutic target for metabolic diseases like obesity, type 2 diabetes and NAFLD [8]. In addition, BAT secretes regulatory molecules—also called “batokines”—such as neuregulin 4 (Nrg4), fibroblast growth factor 21 (FGF-21), interleukin-6 (IL-6) and insulin-like growth factor 1 (IGF1) [9] that might directly target peripheral tissues such as liver, white adipose tissue (WAT), pancreas, and bone in an endocrine manner [9].
Three pre-clinical studies in mice suggested a protective role of Nrg4 for the development and progression of NAFLD [10–12]. Nrg4 is a member of the epidermal growth factor (EGF) family of extracellular ligands and is highly expressed in adipose tissue, mainly in BAT and to a lesser extend in WAT. Wang et al. observed that Nrg4 deficiency exacerbates hepatic steatosis and insulin resistance in mice [10]. They showed that Nrg4 activates ErbB3/ErbB4 signalling in cultured primary mouse hepatocytes and negatively regulates de novo lipogenesis mediated by the LXR/SREBP1c pathway. Furthermore, Guo et al. observed an increase in the degree of hepatic fibrosis and hepatic inflammation associated with Nrg4 deficiency in a NASH mouse model suggesting that Nrg4 plays a role in the progression from simple steatosis to NASH [11]. Finally, Ma et al. observed that, in mice, gene transfer mediated Nrg4 overexpression blocks high-fat diet induced weight gain, insulin resistance and hepatic lipogenesis [12].
However, only two studies assessed the potential role of Nrg4 in human subjects with NAFLD [13, 14]. One study observed decreased Nrg4 plasma levels in children with NAFLD compared to children without NAFLD [13]. Another study observed decreased plasma levels of Nrg4 in adults with NAFLD compared with those without, but no association with the degree of hepatic steatosis quantified with ultrasound was observed [14].
Thus despite promising data in animal studies, the pathophysiological significance of Nrg4 in human NAFLD remains unclear to date. Therefore, in this study, we assessed the level of circulating Nrg4 in our well-characterized cohort of NAFLD patients and compared these with healthy controls. Furthermore, the association of plasma Nrg4 with the degree of hepatic steatosis (measured by chemical shift MRI) and systemic inflammatory and metabolic parameters were assessed. Finally, in an independent cohort, via microarray analysis we assessed hepatic and visceral adipose tissue gene expression changes in the Nrg4 pathway in relation to biopsy-assessed NAFLD severity.
Methods
Study populations and definition of metabolic variables
All patients were included between July 2015 and April 2019 in our Maastricht NAFLD cohort. Participants were recruited via the outpatient clinics of the division of Hepatology of the Maastricht University Medical Centre+ and Zuyderland medical hospital and via CO-EUR, a second line treatment facility for eating disorders. Inclusion criteria were (1) age between 18 and 65 years, (2) NAFLD diagnosis based on imaging (any form of imaging showing steatosis) or biopsy and confirmation of steatosis by MRI fat quantification and (3) (BMI) ≥25 kg/m2. Exclusion criteria were excessive alcohol use (>7 units/week for women, >14 units/week for men), secondary causes of hepatic fat accumulation (e.g. alcohol, medication, Wilson’s disease, viral infections, starvation or parenteral nutrition), pregnancy or breastfeeding, diagnosis of liver cirrhosis and current or prior diagnosis of malignancy within the last 5 years. Anthropometric measurements, venous blood sample, transient elastography (fibroScan®) and chemical shift MRI of the liver were performed in each participant. Healthy controls (HC) were recruited via public advertising on websites and in local newspapers. HC were aged between 18 and 67 years with a BMI < 25 kg/m2, had no excessive alcohol consumption (≤7 units/week for women, ≤14 units/week for men) and had identical exclusion criteria compared to the NAFLD subjects. This study was approved by the Medical Ethics Committee of the Maastricht University Medical Centre (ClinicalTrials.gov Identifier: NCT02422238) and performed according the declaration of Helsinki (latest amendment of 2013, Fortaleza, Brazil). Prior to participation, all participants gave written informed consent.
Liver biopsy procedure and histological assessment were performed as previously described [15]. Insulin resistance (IR) was defined by means of the homeostasis model of assessment-insulin resistance (HOMA-IR) with the following formula HOMA-IR = (fasting plasma insulin (μIU/mL) x fasting plasma glucose (mmol/L))/22.5 [16]. In subjects on insulin therapy (n = 3), HOMA-IR was not calculated. Metabolic syndrome was diagnosed based on the updated International Diabetes Federation (IDF) definition with abdominal obesity defined as waist circumference ≥94cm or ≥80 cm in male and female participants respectively [17]. The definition of type 2 diabetes mellitus (DM2) at baseline included any patient with an HbA1c ≥6.5% or a fasting plasma glucose of ≥7 mmol/l or a patient with current treatment for DM2 [18].
In an independent cohort of 15 obese patients, the expression of Nrg4 related genes in liver and visceral adipose tissue were assessed via microarray analysis. These 15 patients were selected based on the availability of both liver and fat biopsies from our previously published study in 113 patients from three academic hospitals (Leuven, Antwerp and Pretoria). These patients underwent liver biopsy and collection of visceral adipose tissue (VAT) during bariatric surgery [15]. A detailed description of the inclusion and exclusion criteria of these subjects is reported previously [15]. In brief, subjects were included between 2010 and 2011. Liver and VAT were obtained during bariatric surgery and liver histology was assessed by an expert liver pathologist blinded to all clinical information according to the NASH–Clinical Research Network Scoring System criteria [19]. Patients with inadequate liver biopsy specimens (<2 cm and/or <5 portal tracts), with underlying cirrhosis, or borderline features of NASH (NAFLD activity score [NAS], 3–4) were excluded from the analysis. Patients were divided in three groups: (1) obese: less than 5% steatosis, NAFLD activity score (NAS) of 0 (n = 6); (2) NAFL: NAFLD without inflammation or NASH, NAS less than 4 (n = 4); (3) NASH: NAS of 5 or greater and fibrosis score of 0–1 (n = 5). This study was approved by the the Medical ethics committee of KU Leuven/UZ Leuven, the ethical committee of the Antwerp University Hospital and the University of Pretoria Ethics Committee. Prior to participation, all participants gave written informed consent.
Plasma Nrg4 and cytokine analyses
Fasting venous blood samples were collected from each subject and stored at − 80°C until analysis. When performing the assay, samples were brought to room temperature. Plasma Nrg4 levels were measured by using enzyme-linked immunosorbent assay (ELISA) (Catalogue No. CSB-EL016080HU; Cusabio, Wuhan, China) according to the guidelines of the manufacturer. Plasma levels of interleukin 6 (IL-6), tumor necrosis factor alpha (TNF-α), and interferon gamma (IFN-γ) were assessed in duplicate on multiplex V-Plex kits from Meso Scale Discovery (MSD, Meso Scale Discovery, Rockville, USA) according to the guidelines of the manufacturer.
Magnetic resonance hepatic fat quantification
Upon inclusion, all NAFLD patients underwent a chemical shift MRI (1,5T or 3T Philips) of the liver to diagnose NAFLD and quantify the hepatic fat fraction (HFF). A commercially available version of mDIXON sequence package was used to acquire fat, water, in-phase (IP) and opposed-phase (OP) images. HFF was measured on three MRI sections. On each section four circular regions of interest (ROIs) of 5 cm2 were drawn in the liver. Artefact, vascular and biliary structures were avoided and the ROI was copied from the IP image OP image. The mean signal intensity (SI) loss of all 12 ROIs was calculated with the following formula: (SI IP- SI OP)/ 2*SI IP*100% [20]. Based on a previous study comparing this method with MR spectroscopy the applied cut-off to diagnose hepatic steatosis was 3.6% [21].
Transient elastography
In all NAFLD patients liver stiffness measurement (LSM) was performed using the FibroScan® (touch 502, Echosens, Paris, France). Both the M probe (3,5 MHz) and the XL probe (2,5 MHz) were available for this study. Only measurements with at least 10 valid measurements (during one examination), a minimal success rate of 60% and interquartile range/median for liver stiffness estimation ≤ 30% were accepted for further analysis. Examinations that did not meet these conditions were classified as failures. The final result of LSM is the median of the valid (at least 10) individual measurements. The applied FibroScan® cut-off value for histological grade 2 fibrosis (F2, significant fibrosis) or grade 3 fibrosis (F3, advanced fibrosis) were 7.0 kPa and 8.7 kPa, respectively [22].
Microarray analysis
Microarray analysis was based on the analysis of the previous microarray readings [15]. In short, microarray hybridization was performed according to the manufactures instructions on Affymetrix Primeview arrays (Affymetrix, Inc, Santa Clara, CA). Additionally, pathway analysis related to Nrg4 and its receptor ErbB was performed with the internet-based DAVID Bioinformatics Resource 6.8 program (National Institute of Allergy and Infectious Diseases [NIAID], NIH, Bethesda, MD). We identified the Kyoto Encyclopedia of Genes and Genomes (KEGG) Has:04012 ErbB signaling pathway with 85 genes that were further investigated and compared in the microarray results of visceral adipose tissue (VAT) and liver. Three genes were excluded, as they were not hybridized and if gene duplicates were found, the one with the higher Robust Multi-array Average (RMA) expression were kept. The results were analyzed in the R programming environment version 4.0.2 and visualized with Pheatmap version 1.0.12.
Statistical analysis
Data were analysed with IBM SPSS statistics version 25 (IBM Statistics for Macintosh, Chicago, IL, USA). The normality of data distribution was evaluated visually and by means of shapiro-wilk test. Data are presented as means ± SD for normally distributed continuous variables and as percentages for categorical variables, or as median (interquartile range; 25th percentile to 75th percentile) for continuous variables lacking a normal distribution. Student’s test was used to compare normal distrusted data between two groups, while Mann-Whitney U-tests was used to compare skewed distributed variables between two groups. Chi-square test was used to compare categorical variables between groups. As demographic factors may influence the relationship between NAFLD and circulating Nrg4 levels a multivariable linear regression analysis was performed. Spearman’s rho correlation coefficient was used to analyse the correlation between plasma Nrg4 levels and the hepatic fat fraction, blood lipid profile, markers of insulin resistance and inflammatory cytokines levels. Microarray data were compared between groups using a moderated t-statistic [23, 24] implemented in the limma package (version 3.12.1) and correcting for multiple testing with Benjamini-Hochberg [25]. A two-sided P-value of <0.05 was considered statistically significant. Missing data was not imputed, but reported upon in the results. We did not perform a sample size calculation as this study was performed as a sub-analysis of a longitudinal cohort study. Nrg4 was analysed in all included participants of this cohort study until April 2019.
Results
Baseline characteristics
Plasma Nrg4 levels were measured in 65 NAFLD patients and 43 healthy controls (HC). Demographic, anthropometric and biochemical parameters of all participants are presented in Table 1. NAFLD patients were older and had a higher BMI than HC. Furthermore, plasma levels of TNF-α and IL-6 were significantly higher in NAFLD patients compared to HC (p<0.001). Twenty-two NAFLD patients (38%) had clinically significant fibrosis (transient elastography value of ≥7 kPa).
Table 1. Baseline characteristics.
| Variable (standard value) | NAFLD (n = 65) | HC (n = 43) | P-value |
|---|---|---|---|
| Gender (female) | 34 (52%) | 22 (51%) | 0.724 |
| Age (years) | 54 (45;61) | 40 (25; 52) | 0.001 |
| BMI (kg/m2) | 32.37 (±4.75) | 22.24 (±2.10) | <0.001 |
| Metabolic Syndrome (Yes) | 39 (61%) | 0 (0%) | <0.001 |
| DM2 (Yes) | 16 (25%) | 0 (0%) | <0.001 |
| HbA1c (4.4–6.2%) | 5.6 (5.3; 6.5) | - | |
| Fasting Glucose (3.1–6.1mmol/L) | 6.0 (5.3; 6.8) | - | |
| HOMA-IR (n = 58) | 3.29 (2.32; 5.11) | - | |
| Total cholesterol (5.0–6.4 mmol/L) | 5.11 (±0.95) | - | |
| LDL-C (3.5–4.4 mmol/L) | 3.13 (±0.93) | - | |
| HDL-C (>0.9 mmol/l) | 1.26 (±0.41) | - | |
| Triglycerides (0.80–1,94 mmol/l) | 1.49 (1.05; 2.29) | - | |
| ALT (F <34, M <45U/L) | 40 (29; 60) | - | |
| AST (F <31, M <35U/L) | 28 (24; 38) | - | |
| γ-GTP (F <38, M <55U/L) | 42 (25; 67) | - | |
| AP (F <98, M <115U/L) | 90 (76; 106) | - | |
| Ferritin (F 20–150, M 20–250 ug/l) | 132 (61; 238) | - | |
| Albumin (35–55 g/l) | 40.68 (±3.14) | - | |
| CRP (<6 mg/l) | 2 (1; 4) | - | |
| Hepatic fat fraction (< 5%) | 16.86 (11.86; 26.14) | - | |
| LSM (kPa) (n = 60) | 6.1 (5.1–8.1) | - | |
| • F2 (7–8.7 kPa) (yes/total) | 8/60 (13%) | ||
| • ≥ F3 (≥8.7 kPa) (yes/total) | 14/60 (25%) | ||
| TNF-α (pg/ml) | 3.02 (2.34; 3.73) | 2.14 (1.70; 2.60) | <0.001 |
| IL-6 (pg/ml) | 0.50 (0.34; 0.67) | 0.23 (0.14; 0.37) | <0.001 |
| IFN-γ (pg/ml) | 3.15 (2.26; 5.33) | 3.38(1.84; 5.05) | 0.566 |
Values are presented as mean (±SD) (normal distributed data) or median (Q1; Q3) (skewed data) for continuous variables or number (% of group) for categorical variables. Student’s T-test (normal distributed data) or Mann‐Whitney U tests (skewed data) was used to determine statistically significant differences (P < 0.05) between groups. Chi-square test was used to compare categorical variables between groups. HOMA-IR was not available in seven subjects, three used insulin therapy and in four subjects data were missing. In five participants FibroScan® results were not obtained. F, Female; M, Male; BMI, body mass index; HbA1c, hemoglobin A1c; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; ALT, alanine transaminase; AST, aspartate transaminase; γ-GTP, gamma-glutamyltranspeptidase; AP, alkaline phosphatase; LSM, liver stiffness measurement; TNF- α, tumor necrosis factor alpha; IL-6, interleukin 6; IFN-γ, interferon gamma.
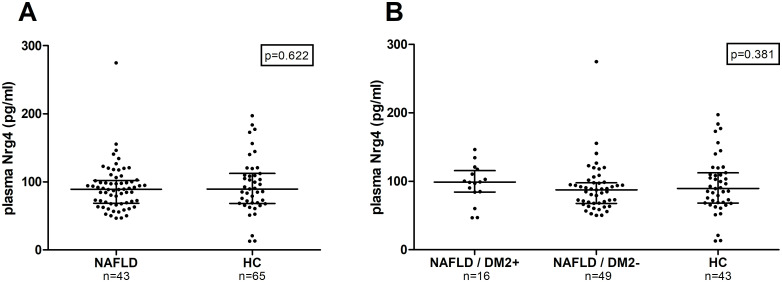
Plasma Nrg4 levels in NAFLD patients with and without DM2 compared to healthy controls
Plasma Nrg4 levels were not significantly different between NAFLD patients and HC (respectively 89.2 [68.6; 102.2] vs. (89.5 [68.2; 112.2]; data expressed as median and [interquartile range (Q1, Q3)] (p = 0.622) (Fig 1A). Previous reports showed that the presence of type 2 diabetes may influence the level of circulating NRG4 levels [26]. We observed no difference in plasma Nrg4 levels between NAFLD patients with DM2 (n = 16), NAFLD patients without DM2 (n = 49) and HC (n = 43) (P = 0.381) (Fig 1B). As gender and age may influence Nrg4 levels and thus their relationship with the presence of NAFLD, a multivariable linear regression was performed. The multivariable models include age, gender and presence of NAFLD (yes vs. no) as independent variables. In this model no association between the presence NAFLD and circulating Nrg4 levels was observed (B = 7.773 (95% CI -1.891; 17.357)) in NAFLD patients (for detail see S1 Table).
Fig 1. Plasma Nrg4 levels in NAFLD patients versus healthy controls.
Values are presented in scatter plots with median line (Q1, Q3). Plasma Nrg4 levels were compared between groups with the Mann-Whitney U-tests (A) and Kruskall Wallis test (B). Plasma Nrg4 levels in (A) HC versus NAFLD patients, (B) NAFLD patients with and without DM2 and HC. DM2, type 2 diabetes mellitus.
Association between plasma Nrg4 levels and hepatic steatosis
No correlation between the hepatic fat fraction measured by MRI and plasma Nrg4 levels was observed in NAFLD patients (r = -0.028, p = 0.829) (Fig 2). No statistically significant difference in plasma Nrg4 levels between NAFLD patients with fibrosis (F2-3, ≥7.0 kPa) and NAFLD patients without fibrosis (F0-2, <7.0 kPa) was observed (F0-1: 84.5 [63.2; 97.9], F2-3: 95.8 [69.6; 112.9] (median [Q1, Q3]) P = 0.087).
Fig 2. Association between plasma Nrg4 levels and NAFLD severity.
Values are presented in scatter plots with median line and (Q1, Q3). Spearman correlation was used for correlation analysis and Mann-Whitney U-tests for comparison between two groups. (A) Spearman correlation between hepatic fat fraction and plasma Nrg4 levels in NAFLD patients. (B) Plasma Nrg4 levels in NAFLD patients without clinically significant hepatic fibrosis (F0-1), versus NAFLD patients with clinically significant hepatic fibrosis (F2-3).
Correlation of plasma Nrg4 levels with metabolic risk factors in NAFLD patients
No correlation of plasma Nrg4 levels with BMI, fasting glucose, HbA1c, HOMA-IR, cholesterol and triglycerides levels was observed (Table 2). Plasma Nrg4 levels only were moderately negatively correlated with HDL-Cholesterol (ρ = -0.254, P = 0.041). Pro-inflammatory cytokines might reduce the expression of Nrg4 [10]. However, we found no correlation between Nrg4 levels and plasma pro-inflammatory cytokines. All investigated correlations were visualised in scatter plots in S1 Fig. Also in the complete study population (including NAFLD patients and HC) no correlation between plasma Nrg4 and BMI, TNF-α, IL-6 and IFN-γ (n = 108) was found (all p> 0.05; S2 Table).
Table 2. Spearman’s rank correlations with plasma Nrg4 levels and metabolic parameters in NAFLD patients (n = 65).
| Spearman’s rank (ρ) | p-value | |
|---|---|---|
| BMI | 0.005 | 0.967 |
| Fasting Glucose | 0.196 | 0.126 |
| HbA1c | 0.221 | 0.077 |
| HOMA-IR (n = 58) | 0.127 | 0.341 |
| Total Cholesterol | -0.164 | 0.192 |
| HDL-C | -0.254 | 0.041 |
| LDL-C | -0.116 | 0.357 |
| Triglycerides | 0.147 | 0.244 |
| TNF-α | -0.138 | 0.273 |
| IL-6 | -0.185 | 0.140 |
| IFN-γ | 0.124 | 0.324 |
BMI, body mass index; HbA1c, haemoglobin A1c; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TNF- α, tumor necrosis factor alpha; IL-6, interleukin 6; IFN-γ, interferon gamma.
Microarray analysis on the NrG4-ErbB signalling pathway in the liver and visceral adipose tissue in relation to NAFLD severity
Baseline characteristics of 15 obese subjects included in the microarray analysis are presented in S3 Table. Hepatic and visceral adipose tissue gene expression profiles were compared between six obese subjects without NAFLD, four NAFL and five NASH patients (Fig 3). No significant difference was seen in Nrg4 expression between subjects without NAFLD, with NAFL or with NASH. Additionally, none of the average Robust Multi-array Average (RMA) expressions in the 82 investigated genes related to the Nrg4-ErbB signalling pathway in both liver and visceral adipose tissue were altered between these groups (Fig 3). This means the KEGG:04012 ErbB pathway was under no condition significantly enriched. The Robust Multi-array (RMA) expressions of the 82 investigated genes related to the Nrg4-ErbB signalling pathway of all individual subjects are presented in S1 Fig.
Fig 3. Heatmap of 82 NrG4-ErbB signalling pathway related genes.
Visualised as average Robust Multi-array Average (RMA) expressions in the liver and visceral adipose tissue of obese, NAFLD and NASH patients.
Discussion
Nrg4 has been identified as an endocrine factor secreted by brown adipose tissue that selectively binds to the liver and inhibits hepatic lipogenesis in mice and hepatocyte cell culture [10]. Therefore, it is crucial to explore whether these findings can be translated to human NAFLD. In the present study, we did not find a difference of plasma Nrg4 levels between well-characterized NAFLD patients and HC. Furthermore, plasma Nrg4 levels were not correlated with the degree of hepatic steatosis measured by chemical shift MRI in NAFLD patients. In an independent cohort, microarray analysis revealed no hepatic gene expression changes related to NrG4 and its receptor family ErbB between biopsied obese patients with NAFL, NASH and normal livers.
In this study, we provide the first data on Nrg4 in a European NAFLD cohort. Plasma Nrg4 levels were only studied in two Asian NAFLD studies (one pediatric, one adult) that both observed decreased plasma Nrg4 levels in NAFLD patients compared to controls [13, 14]. This discrepancy might be attributed to difference in study population and design. In both studies ultrasound was used to diagnose and quantify hepatic steatosis. However, ultrasonography has poor sensitivity to detect and quantify hepatic steatosis and is therefore suboptimal to investigate the correlation between circulating Nrg4 levels and the presence or degree of hepatic steatosis [27]. Chemical shift MRI on the other hand is an accurate and reproducible method to diagnose and quantify hepatic steatosis [28]. Differences in BAT volume and activity have been observed between different ethnicities and should be subject of further study [29].
The liver is the target tissue of Nrg4 in mice, likely through its direct binding to the ErbB receptors [10]. Therefore, we investigated the expression of 82 genes of the Nrg4 related ErbB signalling pathway in the liver of obese patients without NAFLD, NAFL and NASH patients without fibrosis. No significant difference in enrichment of any of the genes was observed, arguing against a significant role of Nrg4 in NAFLD pathophysiology. Furthermore, it has been observed that Nrg4 mRNA levels in human adipose tissue inversely correlated with body fat mass and liver fat content [10]. However, our microarray analysis did not show a difference of Nrg4 expression level in visceral adipose tissue between the same NAFL, NASH and controls. This discrepancy might be related to a difference in patient number. Wang et al. performed mRNA analysis in 642 adipose tissue samples, although the method of hepatic fat quantification and the number of subjects in which liver fat was quantified was not mentioned [10]. Nrg4 binding is restricted to the liver in rodents, but it remains to be shown that Nrg4 signalling is restricted to the liver in humans as well given the wide-spread expression of ErbB3 and ErbB4 in humans [30]. Our microarray analysis did not reveal significant changes of any of the ErbB pathway related genes in VAT between the different groups. This suggests that if plasma Nrg4 may act on VAT tissue, this effect is not altered in NAFLD patients.
To elucidate the mechanism behind the adipose tissue Nrg4 deficiency in obese mice, treatment of brown and white adipocytes with TNF-α was performed and resulted in a decreased Nrg4 expression in BAT and WAT [10]. Therefore, it was hypothesised that the systemic pro-inflammatory activity associated with the metabolic syndrome contributes to the obesity-induced downregulation of Nrg4 in BAT and WAT [10]. To investigate this hypothesis, we analysed plasma TNF-α, IL-6 and IFN-γ levels in our study population. Although plasma TNF-α and IL-6 levels were significantly increased in NAFLD patients compared to HC, none of the pro-inflammatory cytokines correlated with plasma Nrg4 levels. Further studies are needed to explore the mechanism behind Nrg4 induction and secretion.
The overall discrepancy between the animal studies and our data could be partly explained by the difference in Nrg4 analysis. While we measured plasma Nrg4, Wang et al. solely focused on Nrg4 expression in tissues [10]. Circulating Nrg4 levels are the result of Nrg4 secretion not only by adipocytes, but also by liver, pancreas and muscles [31]. Plasma Nrg4 levels therefore not necessarily perfectly correlate with mRNA expression in an individual organ or tissue. However, in addition to our assessment of plasma Nrg4, also via microarray analysis we found no changes in the Nrg4/ErbB pathway in liver and visceral adipose tissue.
In previous studies, NAFLD-related metabolic factors including BMI, HOMA-IR or DM2 were both positively [32–34] and negatively [13, 35–37] associated with circulating Nrg4 levels in humans. In line with a recent meta-analysis on circulating Nrg4 levels in diabetic patients, we observed no correlation between BMI, HOMA-IR, fasting glucose, blood triglycerides levels and plasma Nrg4 levels [26]. The clinical significance of the observed negative but weak correlation between plasma Nrg4 levels and HDL-C, in line with the finding of Chen et al. in diabetic individuals, is doubtful given the unclear role of BAT function on cholesterol levels [38] and even might be the result of multiple testing error [33, 34, 37].
Our study has some limitations. Firstly, the current gold standard to diagnose and stage NAFLD, a liver biopsy, was not performed in our NAFLD cohort in which we analysed Nrg4 plasma levels. However, chemical shift MRI is a highly valid and reproducible alternative to qualitatively and quantitatively assess hepatic fat content [39]. Furthermore, compared to liver biopsy, MRI hepatic fat quantification is not prone to sampling error. Secondly, causality between circulating Nrg4 levels and hepatic steatosis or fibrosis development could not be investigated because of the cross-sectional nature of the study. Thirdly, HC were not screened for the presence of hepatic steatosis but had no history of liver disease, diabetes or hypertension and a BMI <25 kg/m2 and therefore NAFLD prevalence is expected to be below 7% [40]. Finally, HC were significantly younger than NAFLD patients. However, in a recent study age was not correlated with circulating Nrg4 levels in 311 DM2 patients [37].
In conclusion, no difference in plasma Nrg4 levels between NAFLD patients and HC were observed and plasma Nrg4 levels were not correlated with the degree of hepatic steatosis, insulin sensitivity and systemic pro-inflammatory cytokines. Finally, gene expression profiles of the Nrg4 related ErbB pathway in liver and VAT were not significantly changed between NAFL, NASH or obese controls. Therefore, our study does not support the pre-clinical finding that Nrg4 deficiency associates with increased hepatic lipogenesis and NAFLD progression. Notwithstanding, future human studies are needed to further assess the pathophysiological role and therapeutic potential of Nrg4 in human NAFLD.
Supporting information
B: unstandardized regression coefficient, 95% CI: 95% confidence interval. The multivariable models include age, gender and presence of NAFLD as independent variables. Assumptions for linear regression were met since there were no influential outliers based on Cooks distance ≤ 0.184, and collinearity was met as indicated by variance inflation factor values ≤ 1.201. R square of the model was 0.054.
(DOCX)
TNF- α, tumor necrosis factor alpha; IL-6, Interleukin 6; IFN-γ, interferon gamma.
(DOCX)
Values are presented as median (Q1; Q3) (skewed data) for continuous variables or number (% of group) for categorical variables. LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; ALT, alanine transaminase; AST, aspartate transaminase; γ-GTP, gamma-glutamyltranspeptidase; AP, alkaline phosphatase.
(DOCX)
Scatter plot of Nrg4 levels with (A) BMI, (B) Fasting glucose, (C) HbA1C, (D) HOMA-IR, (E) total cholesterol, (F) HDL-C, (G) HDL-C, (H) Triglycerides, (I) TNF-α, (J) IL-6 and (K) IFN-γ. BMI, body mass index; HbA1c, haemoglobin A1c; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TNF-α, tumor necrosis factor alpha; IL-6, interleukin 6; IFN-γ, interferon gamma.
(PDF)
Robust Multi-array (RMA) expressions in the liver and visceral adipose tissue of obese, NAFLD and NASH patients.
(PDF)
Data Availability
Yes - all data are fully available without restriction.
Funding Statement
J. Verbeek - seeding grant of the School of Nutrition and Translational Research in Metabolism (NUTRIM), Maastricht University, The Netherlands. https://www.maastrichtuniversity.nl/research/school-nutrition-and-translational-research-metabolism The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. Epub 2015/12/29. 10.1002/hep.28431 . [DOI] [PubMed] [Google Scholar]
- 2.Cotter TG, Rinella M. Nonalcoholic Fatty Liver Disease 2020: The State of the Disease. Gastroenterology. 2020;158(7):1851–64. Epub 2020/02/18. 10.1053/j.gastro.2020.01.052 . [DOI] [PubMed] [Google Scholar]
- 3.Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. Journal of Hepatology. 2020;73(1):202–9. 10.1016/j.jhep.2020.03.039 [DOI] [PubMed] [Google Scholar]
- 4.Eslam M, Sanyal AJ, George J, Sanyal A, Neuschwander-Tetri B, Tiribelli C, et al. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology. 2020;158(7):1999–2014.e1. 10.1053/j.gastro.2019.11.312 [DOI] [PubMed] [Google Scholar]
- 5.Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism. 2016;65(8):1038–48. 10.1016/j.metabol.2015.12.012 [DOI] [PubMed] [Google Scholar]
- 6.van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM, Drossaerts JMAFL, Kemerink GJ, Bouvy ND, et al. Cold-Activated Brown Adipose Tissue in Healthy Men. New England Journal of Medicine. 2009;360(15):1500–8. 10.1056/NEJMoa0808718 . [DOI] [PubMed] [Google Scholar]
- 7.Yilmaz Y, Ones T, Purnak T, Ozguven S, Kurt R, Atug O, et al. Association between the presence of brown adipose tissue and non-alcoholic fatty liver disease in adult humans. Alimentary Pharmacology & Therapeutics. 2011;34(3):318–23. 10.1111/j.1365-2036.2011.04723.x [DOI] [PubMed] [Google Scholar]
- 8.Scheja L, Heeren J. Metabolic interplay between white, beige, brown adipocytes and the liver. J Hepatol. 2016;64(5):1176–86. Epub 2016/02/02. 10.1016/j.jhep.2016.01.025 . [DOI] [PubMed] [Google Scholar]
- 9.Villarroya F, Cereijo R, Villarroya J, Giralt M. Brown adipose tissue as a secretory organ. Nature Reviews Endocrinology. 2017;13(1):26–35. 10.1038/nrendo.2016.136 [DOI] [PubMed] [Google Scholar]
- 10.Wang GX, Zhao XY, Meng ZX, Kern M, Dietrich A, Chen Z, et al. The brown fat-enriched secreted factor Nrg4 preserves metabolic homeostasis through attenuation of hepatic lipogenesis. Nat Med. 2014;20(12):1436–43. Epub 2014/11/18. 10.1038/nm.3713 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guo L, Zhang P, Chen Z, Xia H, Li S, Zhang Y, et al. Hepatic neuregulin 4 signaling defines an endocrine checkpoint for steatosis-to-NASH progression. J Clin Invest. 2017;127(12):4449–61. Epub 2017/11/07. 10.1172/JCI96324 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma Y, Gao M, Liu D. Preventing High Fat Diet-induced Obesity and Improving Insulin Sensitivity through Neuregulin 4 Gene Transfer. Sci Rep. 2016;6:26242-. 10.1038/srep26242 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang R, Yang F, Qing L, Huang R, Liu Q, Li X. Decreased serum neuregulin 4 levels associated with non-alcoholic fatty liver disease in children with obesity. Clin Obes. 2019;9(1):e12289. Epub 2018/11/10. 10.1111/cob.12289 . [DOI] [PubMed] [Google Scholar]
- 14.Dai YN, Zhu JZ, Fang ZY, Zhao DJ, Wan XY, Zhu HT, et al. A case-control study: Association between serum neuregulin 4 level and non-alcoholic fatty liver disease. Metabolism. 2015;64(12):1667–73. Epub 2015/10/20. 10.1016/j.metabol.2015.08.013 . [DOI] [PubMed] [Google Scholar]
- 15.du Plessis J, van Pelt J, Korf H, Mathieu C, van der Schueren B, Lannoo M, et al. Association of Adipose Tissue Inflammation With Histologic Severity of Nonalcoholic Fatty Liver Disease. Gastroenterology. 2015;149(3):635–48.e14. 10.1053/j.gastro.2015.05.044 [DOI] [PubMed] [Google Scholar]
- 16.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9. Epub 1985/07/01. 10.1007/BF00280883 . [DOI] [PubMed] [Google Scholar]
- 17.Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the Metabolic Syndrome. Circulation. 2009;120(16):1640–5. 10.1161/CIRCULATIONAHA.109.192644 [DOI] [PubMed] [Google Scholar]
- 18.American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33 Suppl 1(Suppl 1):S62–S9. 10.2337/dc10-S062 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41(6):1313–21. 10.1002/hep.20701 [DOI] [PubMed] [Google Scholar]
- 20.Cassidy FH, Yokoo T, Aganovic L, Hanna RF, Bydder M, Middleton MS, et al. Fatty liver disease: MR imaging techniques for the detection and quantification of liver steatosis. Radiographics: a review publication of the Radiological Society of North America, Inc. 2009;29(1):231–60. Epub 2009/01/27. 10.1148/rg.291075123 . [DOI] [PubMed] [Google Scholar]
- 21.Kim H, Taksali SE, Dufour S, Befroy D, Goodman TR, Petersen KF, et al. Comparative MR study of hepatic fat quantification using single-voxel proton spectroscopy, two-point dixon and three-point IDEAL. Magn Reson Med. 2008;59(3):521–7. 10.1002/mrm.21561 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong VW, Vergniol J, Wong GL, Foucher J, Chan HL, Le Bail B, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology (Baltimore, Md). 2010;51(2):454–62. Epub 2010/01/27. 10.1002/hep.23312 . [DOI] [PubMed] [Google Scholar]
- 23.Smyth GK. Linear models and empirical bayes methods for assessing differential expression in microarray experiments. Stat Appl Genet Mol Biol. 2004;3:Article3. Epub 2006/05/02. 10.2202/1544-6115.1027 . [DOI] [PubMed] [Google Scholar]
- 24.Smyth GK, Michaud J, Scott HS. Use of within-array replicate spots for assessing differential expression in microarray experiments. Bioinformatics. 2005;21(9):2067–75. Epub 2005/01/20. 10.1093/bioinformatics/bti270 . [DOI] [PubMed] [Google Scholar]
- 25.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society Series B (Methodological). 1995;57(1):289–300. [Google Scholar]
- 26.Wang Y, Huang S, Yu P. Association between circulating neuregulin4 levels and diabetes mellitus: A meta-analysis of observational studies. PLoS One. 2019;14(12):e0225705–e. 10.1371/journal.pone.0225705 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cleveland E, Bandy A, VanWagner LB. Diagnostic challenges of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Clin Liver Dis (Hoboken). 2018;11(4):98–104. Epub 2018/04/20. 10.1002/cld.716 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kang BK, Yu ES, Lee SS, Lee Y, Kim N, Sirlin CB, et al. Hepatic fat quantification: a prospective comparison of magnetic resonance spectroscopy and analysis methods for chemical-shift gradient echo magnetic resonance imaging with histologic assessment as the reference standard. Invest Radiol. 2012;47(6):368–75. Epub 2012/05/01. 10.1097/RLI.0b013e31824baff3 . [DOI] [PubMed] [Google Scholar]
- 29.Bakker LEH, Boon MR, van der Linden RAD, Arias-Bouda LP, van Klinken JB, Smit F, et al. Brown adipose tissue volume in healthy lean south Asian adults compared with white Caucasians: a prospective, case-controlled observational study. The Lancet Diabetes & Endocrinology. 2014;2(3):210–7. 10.1016/S2213-8587(13)70156-6 [DOI] [PubMed] [Google Scholar]
- 30.Pfeifer A. NRG4: an endocrine link between brown adipose tissue and liver. Cell Metab. 2015;21(1):13–4. Epub 2015/01/08. 10.1016/j.cmet.2014.12.008 . [DOI] [PubMed] [Google Scholar]
- 31.Harari D, Tzahar E, Romano J, Shelly M, Pierce JH, Andrews GC, et al. Neuregulin-4: a novel growth factor that acts through the ErbB-4 receptor tyrosine kinase. Oncogene. 1999;18(17):2681–9. 10.1038/sj.onc.1202631 [DOI] [PubMed] [Google Scholar]
- 32.Chen LL, Peng MM, Zhang JY, Hu X, Min J, Huang QL, et al. Elevated circulating Neuregulin4 level in patients with diabetes. Diabetes Metab Res Rev. 2017;33(4). Epub 2016/11/20. 10.1002/dmrr.2870 . [DOI] [PubMed] [Google Scholar]
- 33.Kurek Eken M, Yayla Abide C, Sahin Ersoy G, Altun Ensari T, Pekin O, Cevik O. Clinical significance of neuregulin 4 (NRG4) in gestational diabetes mellitus. Gynecol Endocrinol. 2018;34(7):605–8. Epub 2017/12/29. 10.1080/09513590.2017.1420772 . [DOI] [PubMed] [Google Scholar]
- 34.Kang YE, Kim JM, Choung S, Joung KH, Lee JH, Kim HJ, et al. Comparison of serum Neuregulin 4 (Nrg4) levels in adults with newly diagnosed type 2 diabetes mellitus and controls without diabetes. Diabetes Res Clin Pract. 2016;117:1–3. Epub 2016/06/23. 10.1016/j.diabres.2016.04.007 . [DOI] [PubMed] [Google Scholar]
- 35.Kralisch S, Hoffmann A, Kratzsch J, Blüher M, Stumvoll M, Fasshauer M, et al. The brown-fat-secreted adipokine neuregulin 4 is decreased in gestational diabetes mellitus. Diabetes Metab. 2018;44(2):150–4. Epub 2017/07/16. 10.1016/j.diabet.2017.06.001 . [DOI] [PubMed] [Google Scholar]
- 36.Cai C, Lin M, Xu Y, Li X, Yang S, Zhang H. Association of circulating neuregulin 4 with metabolic syndrome in obese adults: a cross-sectional study. BMC Med. 2016;14(1):165. Epub 2016/10/25. 10.1186/s12916-016-0703-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yan P, Xu Y, Wan Q, Feng J, Li H, Yang J, et al. Plasma Neuregulin 4 Levels Are Associated with Metabolic Syndrome in Patients Newly Diagnosed with Type 2 Diabetes Mellitus. Dis Markers. 2018;2018:6974191. Epub 2018/05/04. 10.1155/2018/6974191 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hoeke G, Kooijman S, Boon MR, Rensen PCN, Berbée JFP. Role of Brown Fat in Lipoprotein Metabolism and Atherosclerosis. Circulation Research. 2016;118(1):173–82. 10.1161/CIRCRESAHA.115.306647 [DOI] [PubMed] [Google Scholar]
- 39.Schwenzer NF, Springer F, Schraml C, Stefan N, Machann J, Schick F. Non-invasive assessment and quantification of liver steatosis by ultrasound, computed tomography and magnetic resonance. Journal of Hepatology. 2009;51(3):433–45. 10.1016/j.jhep.2009.05.023 [DOI] [PubMed] [Google Scholar]
- 40.Younossi ZM, Stepanova M, Negro F, Hallaji S, Younossi Y, Lam B, et al. Nonalcoholic fatty liver disease in lean individuals in the United States. Medicine (Baltimore). 2012;91(6):319–27. Epub 2012/11/03. 10.1097/MD.0b013e3182779d49 . [DOI] [PubMed] [Google Scholar]