Abstract
Objective:
Insomnia is a risk factor for suicide, and the risk of suicide after accounting for population wakefulness is disproportionately highest at night. This study investigated whether this risk varied across months and/or methods of suicide.
Methods:
Time, date, method (e.g. firearm, poisoning) and demographic information for 35,338 suicides were collected from the National Violent Death Reporting System for the years 2003–2010. Time of fatal injury was grouped into one-hour bins and compared to the estimated hourly proportion of the population awake from the American Time Use Survey for 2003–2010. Negative binomial modeling then generated hourly incidence risk ratios of suicide. Risks were then aggregated into four categories: Morning (06:00 to 11:59), Afternoon (12:00 to 17:59), Evening (18:00 to 23:59), and Night (00:00 to 05:59).
Results:
The risk of suicide was higher at night across all months (p<0.001) and methods (p<0.001). The average nocturnal risk across months was 3.18 (SD 0.314), with the highest risk in May (3.90) and the lowest in November (2.74). The average nocturnal risk across methods was 3.09 (SD 0.472), with the highest risk for fire (3.75) and the lowest for drowning (2.44). Additionally, nocturnal risk elevated within all demographics (all p<0.001). However, there were no month-by-time or method-by-time interactions across demographics (all p>0.05).
Conclusions:
Regardless of month or method, the incidence risk of suicide at night is higher than any other time of day. Additionally, demographic subgroups did not differentially experience higher risks across months or mechanisms at night.
Keywords: nocturnal wakefulness, suicide, suicide methods, sleep and suicide
INTRODUCTION
Sleep and circadian rhythms play a significant role in suicidality. Pigeon and colleagues reported that disturbed sleep increased the risk of suicide ideation, attempts, and completions by 2 to 3 times, and that this effect was specifically related to insomnia and nightmares1. Insomnia increases the risk of suicide attempts by 3.5 times in adults, with a 5.5 times increase in the 25–44 year old demographic2. Insomnia is strongly associated with current suicidality in undergraduates3–5 and military personnel6,7. Insomnia also predicts future suicidality across adults6,8–12. Case-control studies show that insomnia and sleep disturbance are more prevalent among suicide completers than among matched controls13,14. From these studies, it is clear that difficulty with sleep contributes to suicidal behavior.
Three recent studies highlight nocturnal wakefulness as a risk factor for suicide15,16. Perlis and colleagues extracted the time of fatal injury for over 35,000 suicides, combined this with estimations of the waking population size, and determined that the number of suicides at night vastly exceeded the number of expected suicides given the proportion of the population awake at that time15. This equated to a 3.6 times risk of suicide at night that was consistent across demographics. Additionally, Ballard and colleagues experimentally investigated the role of nocturnal wakefulness in suicidality with a single-night polysomnography study. They found participants with suicidal ideation were more likely to be awake at 4AM, that wakefulness between 4 and 5AM was associated with suicidal thinking the next day, and that these effects were independent of depression severity and other covariates. Finally, there is a circadian pattern in suicides among individuals who are heavily intoxicated (blood alcohol levels of 80 mg/dl or more), with a peak in suicide counts at 9:00PM17. Thus nocturnal wakefulness is associated with a heightened risk of suicidal thinking and behavior and this risk may be modifiable by alcohol or other substances.
Given the concordance between epidemiological and experimental data, it is imperative to determine the mechanisms connecting suicidality to nocturnal wakefulness. The interpersonal-psychological theory of suicide suggests that suicidality is associated with isolation and thwarted belongingness, both of which can be exacerbated when individuals are awake and alone during the night18–20. From a neurobiological perspective, nocturnal wakefulness in the context of sleep deprivation is associated with reduced frontal cortical connectivity and impaired cognition21–23, both of which may increase suicidality through altered decision-making, poor impulse control, and disrupted risk/reward evaluations. Unfortunately, the paucity of data and inconsistent methods limits inferences on these mechanisms24.
However, where experimental data are lacking, population level data can provide insight. Suppose that the nocturnal risk of suicide varied across calendar months, specifically by increasing during the summer. This would lend support to current theories about temperature and light exposure as environmental factors driving suicidal behavior25–30. Alternatively, suppose the nocturnal risk of suicide was disproportionately elevated for a particular method of suicide. This would provide useful information for public health interventions regarding that specific method. Therefore, the present study explored whether the nocturnal risk of suicide varied across months or methods of suicide, and whether this risk was influenced by demographic or geographic factors.
METHODS
Datasets
The datasets used for this analysis have been described previously15. Briefly, suicide data were collected from the United States National Violent Death Reporting System (NVDRS; www.cdc.gov/violenceprevention/nvdrs/31) for the years 2003 to 2010. The NVDRS collects data from participating states through medical examiner and police reports. These include the estimated time of death/fatal injury, the month in which the suicide occurred, the age (including minors), race, ethnicity, and sex of the victim, and the primary method used to commit suicide. Population wakefulness data were drawn from the American Time Use Survey (ATUS; www.bls.gov/tus/data.htm32) for the same years. ATUS data are collected annually by telephone from individuals 15 years and older across the United States. The ATUS provides information on the percentage of the population awake at each clock hour, including subdivisions by demographic (race, ethnicity, age, and sex), and month.
Variable Definitions
Clock hours were grouped into four time categories: night (0000 to 0559), morning (0600 to 1159), afternoon (1200 to 1759), and evening (1800 to 2359). Months and suicide methods (guns, asphyxia, poison, fall, vehicle, sharp weapons, drowning, and fire) were reported as part of the NVDRS dataset and assessed as categorical variables. Demographics included sex (Male or Female), age (15 to 24, 25 to 34, 35 to 44, 45 to 54, 55 to 64, 65 to 74, and 75 or older), race (White, Black, Asian, Other), and ethnicity (Hispanic, Non-Hispanic) based on the data available from the NVDRS and ATUS datasets. Geographic analyses were conducted in two ways. First, latitude effects were assessed by comparing states that were clearly at or above 40°N (“Above40”), or clearly at or below 35°N (“Below35”). The goal of this analysis was to address variations in seasonal light exposure by taking the most extreme data available. States in between these latitudes were not used. The second analysis divided states into four regions (West, Midwest, South, and Northeast) in accordance with the American Association of Suicidology33 to determine regional effects on suicide risks.
Generating Incidence Risk Ratios
The statistical analysis used quasi-Poisson and negative binomial regression to generate incidence risk ratios. The choice between quasi-Poisson and negative binomial regression depended on the number of suicides observed in each category, as smaller counts are more accurately modeled using quasi-Poisson regression. Suicide counts were modeled as functions of time of day, month or method, and their interaction. Empirically, at least 5 suicides at each time were required for adequate model fit, so any categories which did not have at least 5 suicides per time of day were eliminated. Population wakefulness was estimated based on ATUS survey responses. These proportions were adjusted for the relevant month and demographic subgroup (sex, age, race, and ethnicity) and entered as an offset/exposure variable in the model. Modeling counts in this way produces an incidence risk ratio (IRR), which represents the increased risk of suicide at that level (e.g. month, time) as compared to a reference level. Ordinarily, this reference would be another level within the same categorical variable (e.g. comparing Blacks to Whites). Effect coding is an alternative approach which compares each level to the grand mean across levels (e.g. comparing Blacks to the average across all races). To avoid arbitrary assignment of a reference level, effect coding was used in both the by-months and by-methods analyses. For months, effect coding was used for time, month, and the interaction. For methods, effect coding was used only for time, as comparisons were made only within method. Effect coding was achieved using package ‘wec’ in R34. Statistical tests of significance were conducted using one or two-way ANOVA depending on the particular model used. All analyses were conducted using R (version 3.5.1) and graphs were generated using ggplot235.
RESULTS
Summary of the Data
A total of 35,338 suicides were extracted from the NVDRS dataset between 2003 and 2010. Some cases included missing data and were excluded as appropriate in analyses (e.g. month of death was present, but not method). Table 1 shows the suicide counts by Time of Day, Month, and Method of Suicide across demographic variables. By raw counts, most suicides occurred in the Afternoon (N=11,381), in May (N=3,196), and by firearms (N=21,397). More males committed suicide than females (N=28,700 males vs. N=6,636 females), and suicide counts were highest among 45–54 year olds (N=7,252), whites (N=31,239), and non-Hispanics (N=33,394). The number of suicides was roughly equivalent between states categorized as Above40 (N=6,165) and Below35 (N=6,995). By region, most suicides were in the South (N=19,996), with fewer suicides in the West (N=7,620), Midwest (N=4,150), and Northeast (N=3,504).
Table 1:
Suicide counts by time of day, month, and method across demographic factors.
| F | M | 15–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | >75 | White | Black | Asian | Other | Non-Hispanic | Hispanic | >40 | <35 | Midwest | Northeast | South | West | ||
| Total | 6636 | 28700 | 5000 | 5659 | 6740 | 7252 | 4686 | 2688 | 2943 | 31239 | 2701 | 526 | 686 | 33384 | 1618 | 6165 | 6995 | 4150 | 3504 | 19996 | 7620 | |
| Time of Day | Morning | 1706 | 7705 | 967 | 1222 | 1653 | 1956 | 1454 | 922 | 1183 | 8408 | 651 | 123 | 188 | 8896 | 425 | 1649 | 1784 | 1067 | 1058 | 5185 | 2082 |
| Afternoon | 2299 | 9081 | 1456 | 1601 | 2169 | 2498 | 1643 | 916 | 956 | 10155 | 814 | 180 | 172 | 10839 | 444 | 2127 | 2272 | 1426 | 1117 | 6506 | 2314 | |
| Evening | 1703 | 7519 | 1452 | 1649 | 1891 | 1920 | 1086 | 585 | 498 | 8123 | 757 | 136 | 156 | 8711 | 423 | 1504 | 1916 | 940 | 873 | 5414 | 1977 | |
| Night | 928 | 4395 | 1125 | 1187 | 1027 | 878 | 503 | 265 | 306 | 4553 | 479 | 87 | 170 | 4938 | 326 | 885 | 1023 | 717 | 456 | 2891 | 1247 | |
| Month | Jan | 525 | 2288 | 422 | 409 | 549 | 568 | 375 | 213 | 249 | 2492 | 212 | 38 | 56 | 2648 | 143 | 510 | 579 | 335 | 292 | 1583 | 598 |
| Feb | 515 | 2137 | 377 | 454 | 494 | 537 | 332 | 214 | 214 | 2339 | 214 | 43 | 48 | 2514 | 105 | 451 | 563 | 298 | 241 | 1518 | 587 | |
| Mar | 607 | 2520 | 444 | 468 | 566 | 686 | 430 | 228 | 277 | 2778 | 236 | 45 | 53 | 2939 | 152 | 557 | 631 | 336 | 310 | 1764 | 713 | |
| Apr | 572 | 2347 | 410 | 509 | 555 | 586 | 415 | 175 | 233 | 2582 | 219 | 39 | 53 | 2754 | 136 | 490 | 590 | 340 | 303 | 1696 | 572 | |
| May | 596 | 2600 | 436 | 534 | 669 | 599 | 399 | 257 | 259 | 2819 | 238 | 53 | 68 | 3028 | 141 | 561 | 616 | 359 | 338 | 1797 | 697 | |
| Jun | 564 | 2449 | 455 | 476 | 555 | 615 | 403 | 224 | 260 | 2659 | 229 | 49 | 58 | 2846 | 137 | 520 | 591 | 378 | 300 | 1691 | 641 | |
| Jul | 563 | 2617 | 437 | 517 | 604 | 663 | 423 | 231 | 270 | 2806 | 251 | 40 | 71 | 3001 | 158 | 553 | 615 | 378 | 292 | 1793 | 712 | |
| Aug | 595 | 2452 | 435 | 501 | 580 | 623 | 412 | 224 | 231 | 2711 | 234 | 40 | 49 | 2888 | 135 | 512 | 603 | 347 | 320 | 1737 | 637 | |
| Sep | 575 | 2369 | 420 | 455 | 529 | 657 | 389 | 248 | 221 | 2579 | 244 | 35 | 76 | 2787 | 124 | 526 | 539 | 349 | 294 | 1650 | 648 | |
| Oct | 522 | 2483 | 433 | 489 | 584 | 587 | 387 | 233 | 267 | 2670 | 218 | 50 | 49 | 2824 | 149 | 536 | 613 | 359 | 281 | 1714 | 647 | |
| Nov | 508 | 2256 | 370 | 440 | 575 | 550 | 345 | 220 | 236 | 2424 | 219 | 47 | 59 | 2621 | 119 | 487 | 527 | 338 | 277 | 1531 | 611 | |
| Dec | 494 | 2182 | 361 | 407 | 480 | 581 | 376 | 221 | 226 | 2380 | 187 | 47 | 46 | 2534 | 119 | 462 | 528 | 333 | 256 | 1522 | 557 | |
| Method | Asphyxia | 1291 | 5646 | 1512 | 1577 | 1519 | 1197 | 528 | 190 | 197 | 5796 | 616 | 234 | 217 | 6275 | 605 | 1231 | 1232 | 963 | 1119 | 3429 | 1418 |
| Drowning | 134 | 286 | 40 | 71 | 77 | 99 | 62 | 42 | 27 | 313 | 79 | 21 | 3 | 404 | 14 | 120 | 68 | 49 | 102 | 209 | 58 | |
| Fall | 273 | 670 | 165 | 156 | 206 | 202 | 102 | 50 | 59 | 780 | 97 | 48 | 4 | 885 | 50 | 263 | 102 | 95 | 244 | 419 | 182 | |
| Fire | 75 | 165 | 29 | 39 | 50 | 70 | 38 | 9 | 5 | 177 | 42 | 15 | 5 | 226 | 11 | 61 | 34 | 29 | 59 | 114 | 37 | |
| Gun | 2794 | 18603 | 2760 | 3070 | 3636 | 4146 | 3113 | 2144 | 2405 | 19261 | 1587 | 132 | 352 | 20482 | 681 | 3390 | 4636 | 2265 | 1138 | 13212 | 4759 | |
| Poison | 1764 | 2113 | 265 | 488 | 929 | 1173 | 666 | 172 | 171 | 3593 | 175 | 36 | 62 | 3687 | 165 | 750 | 761 | 544 | 489 | 1941 | 884 | |
| Sharp Weapon | 96 | 457 | 37 | 71 | 110 | 147 | 91 | 44 | 50 | 488 | 38 | 12 | 11 | 523 | 30 | 106 | 82 | 70 | 127 | 264 | 90 | |
| Vehicle | 169 | 590 | 170 | 146 | 174 | 171 | 55 | 23 | 15 | 639 | 60 | 26 | 28 | 699 | 56 | 193 | 63 | 96 | 217 | 283 | 163 |
Suicide Months Analysis
The first question was whether, after accounting for population wakefulness, the hourly incidence risk ratio of suicide varied across months. The results are shown in Figure 1. May showed the highest risk (3.9 ± 0.48), while November had the lowest risk (2.7 ± 0.34). However, a two-way ANOVA for month, time of day, and an interaction showed that the incidence risk varied significantly across time of day (p<0.001), but not across months (p=0.33) or by the interaction (p=1.00). A post-hoc Wald test showed that incidence risk at Night was significantly higher than any other time of day (p<0.001). The average incidence risk at night across months was 3.18 (SD: 0.314).
Figure 1:
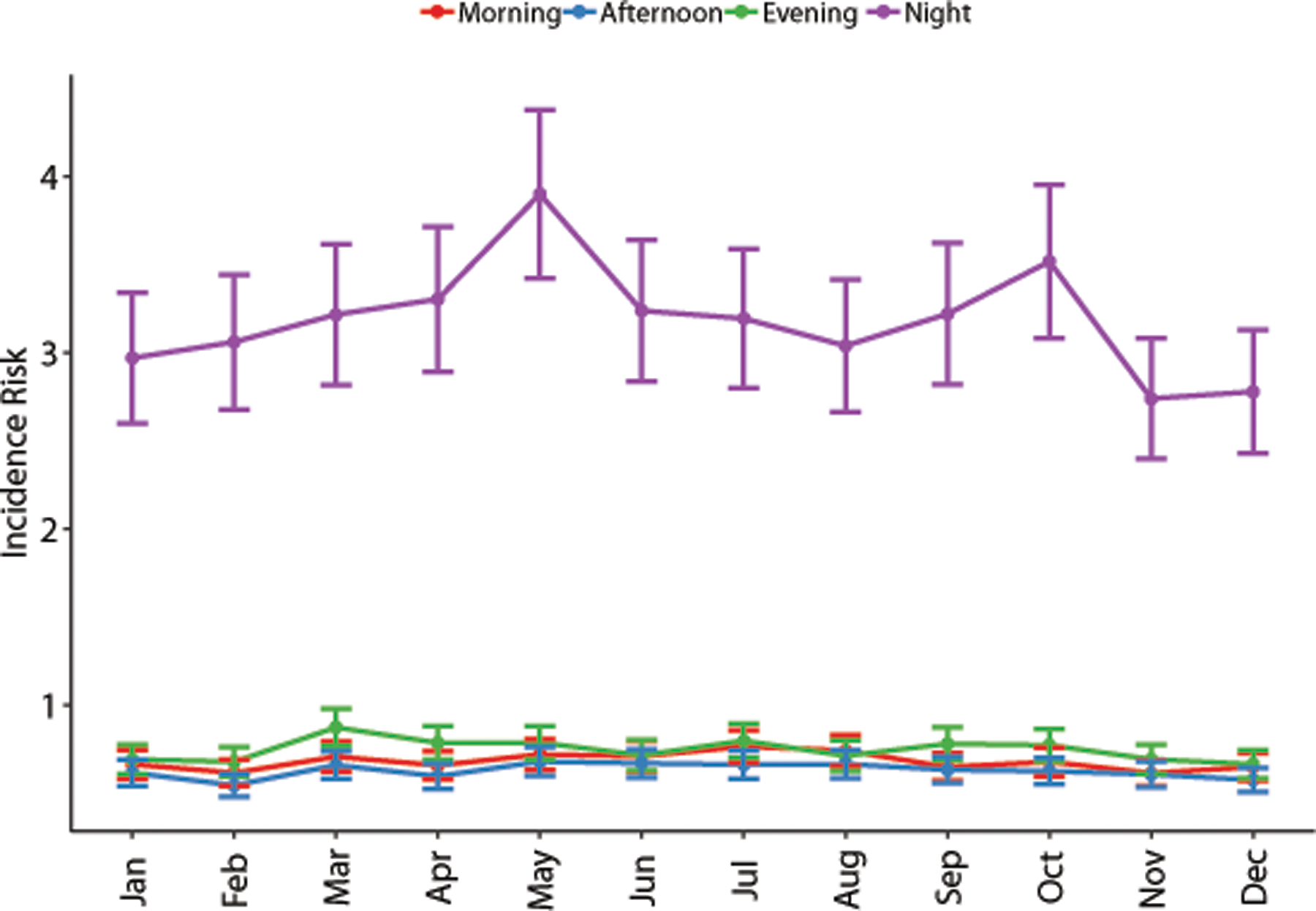
The risk of suicide by time of day across months. The incidence risk ratios were much higher at night as compared to the average across all times of day. Risk peaks in May and October, although these increases were not statistically significant. Night: 12AM to 6AM; Morning: 6AM to 12PM; Afternoon: 12PM to 6PM; Evening: 6PM to 12AM. Risk ratios are plotted as mean ± standard error.
In subgroup analyses, each demographic was evaluated separately for an effect of time of day by month. These results are presented in Figure 2; women tended to have slightly higher nighttime risks than men, nighttime risk appeared to decrease with age, and Hispanics tended to have higher nocturnal risks than non-Hispanics. However, a two-way ANOVA found that, while IRRs varied significantly across time for men and women, all ages, all races, Hispanics and non-Hispanics, all latitudes, and all regions (all p<0.001), they were not significantly different across months, nor was there a significant month by time of day interaction (all p>0.05).
Figure 2:
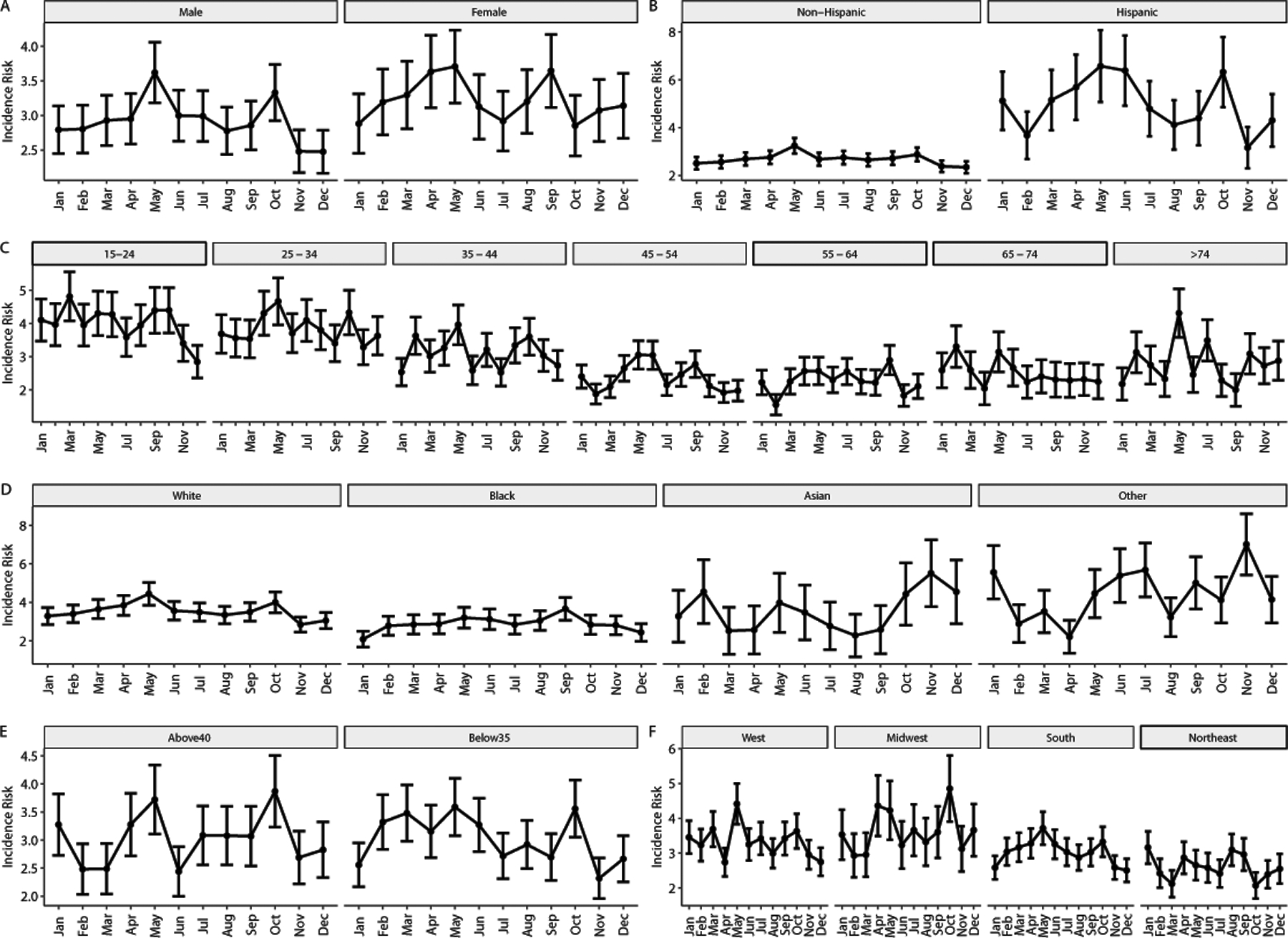
The nocturnal risk of suicide across months by demographic characteristics. Incidence risk ratios were generated within demographic categories (e.g. for males separately from females), so comparisons across demographics were not made. No statistically significant effects for time of day by demographic were noted. Risk ratios are plotted as mean ± standard error.
Suicide Method Analysis
The second question was whether the incidence risk ratio of suicide varied by time across suicide methods. An initial two-way ANOVA evaluating time by method showed that risk varied significantly by time of day and by method (both p<0.001), but that the interaction was not significant (p=0.3026). Thus, no method had a significantly higher risk at a specific time than any other method at that same time. Post-hoc Wald tests found that the risk was highest at night and for guns (both p<0.001). The average incidence risk at night across methods was 3.09 (SD 0.472). However, suicide counts were heavily skewed across methods, with more than half of the suicides involving firearms. Therefore, the risk of each method at each time of day was evaluated independently, as opposed to comparing risks across methods. Effect coding was used to compare the risk at each time to the grand mean across the day within each method. Figure 3 shows the IRRs for each method at each time.
Figure 3:
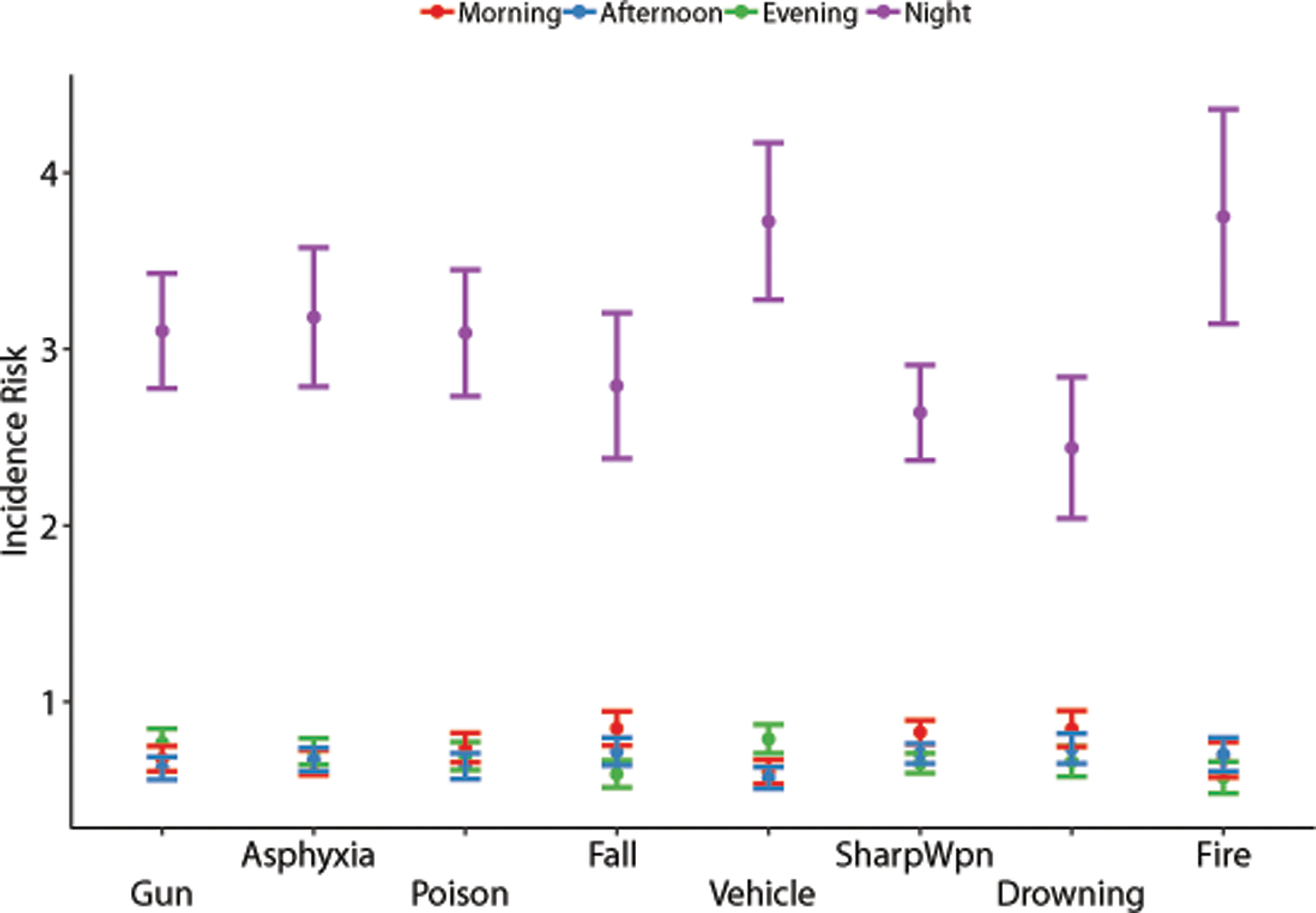
The risk of suicide by time of day across methods of suicide. The incidence risk ratios were higher at night as compared to the average risk across all times of day. While vehicles and fires showed an elevated risk, this increase was not statistically significant. Night: 12AM to 6AM; Morning: 6AM to 12PM; Afternoon: 12PM to 6PM; Evening: 6PM to 12AM. Risks are plotted as mean +/− standard error. Risk ratios are plotted as mean ± standard error.
As in the by-months analysis, IRRs were evaluated across sex, age, race, ethnicity, latitude, and region. These results are presented in Figure 4. Nocturnal risk for each method did not vary by sex, age, race, ethnicity, or geography. A two-way ANOVA showed that IRRs varied significantly by time of day and method for all demographic groups (all p<0.001), reiterating that the risk of suicide is not equivalent across all times or every method. However, the interaction between time of day and method was not significant for any subgroup (all p>0.05). Thus, there was no method of suicide that was systematically more common in any particular demographic or geographic group.
Figure 4:

The nocturnal risk of suicide across suicide methods by demographic characteristics. Incidence risk ratios were generated within demographic categories, so no comparisons across demographics were made. The only statistically significant effect present was the increased nocturnal risk of death by fire in northern states; no other statistical differences were noted. Risk ratios are plotted as mean ± standard error. Categories for which no ratio is present did not have at least 5 suicides at each time of day, and were therefore excluded from analysis.
DISCUSSION
This study found that the nocturnal risk of suicide is approximately three times that of the across day average after accounting for population wakefulness. Additionally, the increased risk at night remained constant regardless of month or method of suicide. While differences may exist across demographics and methods, these differences are not dependent on time of day. These findings reinforce previous results in suggesting that nocturnal wakefulness is a significant risk factor for suicide.
Suicide Months Analysis
Seasonal effects on suicide have been described in both the northern and southern hemispheres. Holopainen and colleagues found that suicide peaks occurred in May and October, which they hypothesized was due to dramatic changes in temperature30. This reinforced an earlier finding that Finnish suicides were highest in spring, when solar radiation was highest36. A study of young people in the more equatorial country of Turkey found a peak in suicide attempts in the summer37. In Brazil, Bando and colleagues found that male suicide peaked in late spring and reached a minimum in late fall, while females peaked in summer and reached their minimum in winter38. The increased risk for suicide in spring was also present in Danish suicide completers with a history of mood disorders39. The springtime increase in suicides has been correlated with increased light exposure, possibly through modulation of serotonergic activity25–29. Whatever the mechanism, season appears to play a role in suicide risk.
Contrary to this literature, the present study found that the risk of suicide was highest at night across all months, and that no month showed a significantly different risk than any other. While Figure 1 appears to show an increase in nocturnal suicide risk in May and October, this finding was not statistically significant and cannot be interpreted further. If a seasonal effect does exist for suicide risk, it is likely insignificant compared to the time of day, and future research on seasons and suicide should account for time of day.
Suicide Methods Analysis
It is interesting that the nocturnal risk of suicide did not vary across methods of suicide. From a practical standpoint, some methods might be less accessible at night than others (e.g. there are fewer cars/trains active at night to be hit by). Nevertheless, in accordance with the hypofrontality theory advanced by Perlis and colleagues, this suggests that nocturnal wakefulness may be more associated with the initial decision to commit suicide than the choice of method23. This also accords with other evidence of disinhibited behaviors at night, such as those around food choices. Individuals who go to bed later are more likely to consume hedonistic and energy-rich foods, such as fast foods and sodas40,41. Similarly, a survey of Australian children and adolescents found that those who were awake later at night had a higher intake of “extra foods” and a lower diet quality42. In the case of suicide and food choice, nocturnal wakefulness may be driving impulsive decision-making through impaired cortical activity. However, experimental studies are needed to explore this hypothesis.
Strengths and Limitations
This study has several strengths. Despite using a different statistical approach, the average nocturnal risk of suicide was in line with the risk reported by Perlis and colleagues15. Additionally, the analysis was based on a large sample size (over 35,000 suicides), with estimated population wakefulness adjusted for time of day and relevant demographics. However, this study has several limitations. First, it is unclear whether individuals who committed suicide at night were continuously awake until their suicide, or whether they had recently woken up. This distinction is important, as it might separate sleep deprivation from circadian effects. Second, the adjustment for wakefulness was not based on individuals who specifically have suicidal ideation, plans, or attempts. Thus, if suicide attempters systematically differ from the general population in the timing of wakefulness this approach would not account for this difference. Additionally, we were unable to separate minors out from the age 15 to 24 demographic as we did not have separate ATUS wakefulness estimates for minors and adults in this category. Finally, the small number of minority suicides reported prevented the calculation of some incidence risk ratios.
Future Directions
It is critical to understand what biological and psychological mechanisms are at work in individuals who commit suicide at night. If middle insomnia leads to increased catastrophic thinking, hopelessness, and thwarted belonging, then treatment of insomnia may help vulnerable individuals to avoid times of dangerous thinking. Alternatively, if nocturnal hypofrontality contributes to suicidal decision-making, then separating the role sleep and circadian rhythms on this hypofrontality may inform future interventions. Finally, these results need to be replicated in other suicidal behaviors, including attempts, planning, and ideation. This would help to determine whether nocturnal wakefulness serves as an acute trigger for suicide attempts, or whether accumulation of nocturnal wakefulness promotes all forms of suicidal behavior.
Conclusions
Suicide is a growing crisis, and a greater understanding of precipitating factors is needed. In accordance with previous work, this report shows that suicide risk is higher at night than any other time of day, and that this risk does not vary significantly by month, method, or demographic characteristics. The implication that nocturnal wakefulness is a universal factor for suicide risk suggests that biological or psychological mechanisms may play a role outside of social and environmental factors. Future work is needed to fully assess sleep and nocturnal wakefulness as acute risk factors for suicidal behavior.
Clinical Points.
Increasing evidence supports nocturnal wakefulness as a risk factor for suicide.
The suicide risk associated with nocturnal wakefulness does not appear dependent on season or method in which the suicide occurs.
Sleep disturbances in patients with a history or risk of suicidality should be treated to reduce suicide risk.
Funding Source:
Funding/Support:
Partial grant support for this study was provided by the following grants from the National Institutes of Health and the Veterans Administration: K24 AG055602 and R01 AG054521 (Dr. Perlis), R01 MD011600 (Dr. Grandner), and IK2 CX000655 (Dr. Chakravorty).
Role of the sponsors:
The funding providers had no role in the conduct of the study or the publication of the results.
Footnotes
Conflicts of interest: none.
Previously presented at the APSS SLEEP Conference in 2018.
REFERENCES
- 1.Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):e1160–1167. [DOI] [PubMed] [Google Scholar]
- 2.Lin HT, Lai CH, Perng HJ, et al. Insomnia as an independent predictor of suicide attempts: a nationwide population-based retrospective cohort study. BMC Psychiatry. 2018;18(1):117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bozzay ML, Karver MS, Verona E. Linking insomnia and suicide ideation in college females: The role of socio-cognitive variables and depressive symptoms in suicide risk. J Affect Disord. 2016;199:106–113. [DOI] [PubMed] [Google Scholar]
- 4.Nadorff MR, Anestis MD, Nazem S, Claire Harris H, Samuel Winer E. Sleep disorders and the interpersonal-psychological theory of suicide: independent pathways to suicidality? J Affect Disord. 2014;152–154:505–512. [DOI] [PubMed] [Google Scholar]
- 5.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide Life Threat Behav. 2013;43(2):139–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bryan CJ, Gonzales J, Rudd MD, et al. Depression Mediates the Relation of Insomnia Severity with Suicide Risk in Three Clinical Samples of U.S. Military Personnel. Depress Anxiety. 2015;32(9):647–655. [DOI] [PubMed] [Google Scholar]
- 7.Ribeiro JD, Pease JL, Gutierrez PM, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. 2012;136(3):743–750. [DOI] [PubMed] [Google Scholar]
- 8.Zuromski KL, Cero I, Witte TK. Insomnia symptoms drive changes in suicide ideation: A latent difference score model of community adults over a brief interval. J Abnorm Psychol. 2017;126(6):739–749. [DOI] [PubMed] [Google Scholar]
- 9.Chu C, Hom MA, Rogers ML, et al. Insomnia and suicide-related behaviors: A multi-study investigation of thwarted belongingness as a distinct explanatory factor. J Affect Disord. 2017;208:153–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernert RA, Hom MA, Iwata NG, Joiner TE. Objectively Assessed Sleep Variability as an Acute Warning Sign of Suicidal Ideation in a Longitudinal Evaluation of Young Adults at High Suicide Risk. J Clin Psychiatry. 2017;78(6):e678–e687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li SX, Lam SP, Yu MW, Zhang J, Wing YK. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. J Clin Psychiatry. 2010;71(11):1440–1446. [DOI] [PubMed] [Google Scholar]
- 12.Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. 2015;17(3):554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun L, Zhang J, Liu X. Insomnia Symptom, Mental Disorder and Suicide: A Case-Control Study in Chinese Rural Youths. Sleep Biol Rhythms. 2015;13(2):181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernert RA, Turvey CL, Conwell Y, Joiner TE Jr., Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: a longitudinal, population-based study of late life. JAMA Psychiatry. 2014;71(10):1129–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perlis ML, Grandner MA, Brown GK, et al. Nocturnal Wakefulness as a Previously Unrecognized Risk Factor for Suicide. J Clin Psychiatry. 2016;77(6):e726–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ballard ED, Vande Voort JL, Bernert RA, et al. Nocturnal Wakefulness Is Associated With Next-Day Suicidal Ideation in Major Depressive Disorder and Bipolar Disorder. J Clin Psychiatry. 2016;77(6):825–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chakravorty S, Smith RV, Perlis ML, Grandner MA, Kranzler HR. Circadian Pattern of Deaths Due to Suicide in Intoxicated Alcohol-Dependent Individuals. J Clin Psychiatry. 2018;79(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joiner TE. Why people die by suicide. Cambridge, Mass.: Harvard University Press; 2005. [Google Scholar]
- 19.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE Jr., The interpersonal theory of suicide. Psychol Rev. 2010;117(2):575–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Russell K, Allan S, Beattie L, Bohan J, MacMahon K, Rasmussen S. Sleep problem, suicide and self-harm in university students: A systematic review. Sleep Med Rev. 2019;44:58–69. [DOI] [PubMed] [Google Scholar]
- 21.Verweij IM, Romeijn N, Smit DJ, Piantoni G, Van Someren EJ, van der Werf YD. Sleep deprivation leads to a loss of functional connectivity in frontal brain regions. BMC Neurosci. 2014;15:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cajochen C, Brunner DP, Krauchi K, Graw P, Wirz-Justice A. Power density in theta/alpha frequencies of the waking EEG progressively increases during sustained wakefulness. Sleep. 1995;18(10):890–894. [DOI] [PubMed] [Google Scholar]
- 23.Perlis ML, Grandner MA, Chakravorty S, Bernert RA, Brown GK, Thase ME. Suicide and sleep: Is it a bad thing to be awake when reason sleeps? Sleep Med Rev. 2016;29:101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tubbs AS, Perlis ML, Grandner MA. Surviving the long night: The potential of sleep health for suicide prevention. Sleep Med Rev. 2019;44:83–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Makris GD, Reutfors J, Larsson R, et al. Serotonergic medication enhances the association between suicide and sunshine. J Affect Disord. 2016;189:276–281. [DOI] [PubMed] [Google Scholar]
- 26.Petridou E, Papadopoulos FC, Frangakis CE, Skalkidou A, Trichopoulos D. A role of sunshine in the triggering of suicide. Epidemiology. 2002;13(1):106–109. [DOI] [PubMed] [Google Scholar]
- 27.Voracek M, Fisher ML. Sunshine and suicide incidence. Epidemiology. 2002;13(4):492–493; author reply 493–494. [DOI] [PubMed] [Google Scholar]
- 28.Vyssoki B, Kapusta ND, Praschak-Rieder N, Dorffner G, Willeit M. Direct effect of sunshine on suicide. JAMA Psychiatry. 2014;71(11):1231–1237. [DOI] [PubMed] [Google Scholar]
- 29.Vyssoki B, Praschak-Rieder N, Sonneck G, et al. Effects of sunshine on suicide rates. Compr Psychiatry. 2012;53(5):535–539. [DOI] [PubMed] [Google Scholar]
- 30.Holopainen J, Helama S, Bjorkenstam C, Partonen T. Variation and seasonal patterns of suicide mortality in Finland and Sweden since the 1750s. Environ Health Prev Med. 2013;18(6):494–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paulozzi LJ, Mercy J, Frazier L Jr., Annest JL, Centers for Disease C, Prevention. CDC’s National Violent Death Reporting System: background and methodology. Inj Prev. 2004;10(1):47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Basner M, Fomberstein KM, Razavi FM, et al. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30(9):1085–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Drapeau CW, McIntosh JL. U.S.A suicide 2017: Official final data Washington, DC: American Association of Suicidology; December 10, 2018. 2018. [Google Scholar]
- 34.Te Grotenhuis M, Pelzer B, Eisinga R, Nieuwenhuis R, Schmidt-Catran A, Konig R. When size matters: advantages of weighted effect coding in observational studies. Int J Public Health. 2017;62(1):163–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wickham H ggplot2: Elegant Graphics for Data Analysis. Use R. 2009:1–212. [Google Scholar]
- 36.Partonen T, Haukka J, Nevanlinna H, Lonnqvist J. Analysis of the seasonal pattern in suicide. J Affect Disord. 2004;81(2):133–139. [DOI] [PubMed] [Google Scholar]
- 37.Akkaya-Kalayci T, Vyssoki B, Winkler D, et al. The effect of seasonal changes and climatic factors on suicide attempts of young people. BMC Psychiatry. 2017;17(1):365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bando DH, Volpe FM. Seasonal variation of suicide in the city of Sao Paulo, Brazil, 1996–2010. Crisis. 2014;35(1):5–9. [DOI] [PubMed] [Google Scholar]
- 39.Postolache TT, Mortensen PB, Tonelli LH, et al. Seasonal spring peaks of suicide in victims with and without prior history of hospitalization for mood disorders. J Affect Disord. 2010;121(1–2):88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring). 2011;19(7):1374–1381. [DOI] [PubMed] [Google Scholar]
- 41.Shechter A, Grandner MA, St-Onge MP. The Role of Sleep in the Control of Food Intake. Am J Lifestyle Med. 2014;8(6):371–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Golley RK, Maher CA, Matricciani L, Olds TS. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes (Lond). 2013;37(4):546–551. [DOI] [PubMed] [Google Scholar]


