Abstract
Background
HIV-related stigma and psychological distress among people living with HIV (PLHIV) pose a public health challenge in most African countries. This study aims to investigate the association between HIV-related stigmatizing attitudes and psychological distress amongst PLHIV in South Africa using the 2012 nationally representative population-based household survey.
Methods
The data used in the analysis were collected using a multi-stage stratified cluster sampling design. Bivariate and multivariate logistic regression models were used to identify factors associated with stigma among PLHIV with psychological distress. A total of 2521 HIV positive individuals that responded to the question on psychological distress, 34.3% had psychological distress and 37.9% experienced high levels of HIV related stigmatizing attitudes. Stigmatizing attitudes among PLHIV with psychological distress were significantly less likely among those with secondary level education [aOR = 0.67 (95% CI: 0.44–1.01), p = 0.050], those with correct knowledge about HIV and rejection of myths about HIV [aOR = 0.58 (95% CI: 0.38–0.89), p = 0.013], and those who ever tested for HIV [aOR = 0.65 (95% CI: 0.42–1.01), p = 0.054].
Conclusion
The findings suggest a need to reinvigorate stigma-reduction interventions in the national HIV response with emphasis on HIV awareness and education campaigns. In addition, HIV testing services should be reinforced through communication strategies targeted against HIV stigmatization, discrimination and fear. There is also a need to continuously engage PLHIV in programs through counselling and support interventions for acceptance of HIV positive status and to help them cope with HIV-related stigma.
Keywords: People living with HIV, Stigma, Psychological distress, South Africa
Highlights
-
•
Stigmatising attitudes were more likely in older age group compared to the youth.
-
•
Stigmatising attitudes were less likely among those with higher levels of educational attainment.
-
•
Stigmatising attitudes were more likely among others race groups compared to Black Africans.
-
•
Stigmatising attitudes were more likely among those residing in rural / farm areas compared to urban areas.
1. Background
HIV-related stigma is one of the biggest challenges facing people living with HIV (PLHIV) and has been associated with poor mental health (Rueda et al., 2016). Stigma has been shown to have a negative impact on quality of life for people living with HIV (Ebrahimi Kalan et al., 2019; Rasoolinajad et al., 2018). Evidence suggests that psychosocial distress and general substance use increase amongst stigmatized PLHIV (Zhang et al., 2016). In addition, individuals with substance use disorders may engage in reckless behaviours or be exposed to heightened risks and likelihood of victimization (Zhang et al., 2016). PLHIV are more likely to be the victims of abuse, assault, and other violent crimes relative to seronegative individuals (Campbell et al., 2008).
Stigma has also been linked with health-related risk factors including poor seeking healthcare and non-adherence to antiretroviral therapy (Kinsler et al., 2007; Dlamini et al., 2009; Rubens et al., 2018). Furthermore, experiences of social rejection, disapproval, and discrimination related to HIV may heighten a person's sense of shame regarding their illness and serve to lessen their motivation to maintain optimal health (Clum et al., 2009). Evidence shows that stigma is associated with concealment of HIV status and avoidance of health care for fear of being identified and stigmatized (Parker et al., 2007). Therefore, HIV-related stigma poses as a significant obstacle to the treatment and prevention of HIV/AIDS (Sambisa et al., 2010). In addition, HIV-related stigma can result in negative self-image that may in turn exert subtle negative influences on social interactions and affect behavioural outcomes such as engagement in risk behaviour (Clum et al., 2009). Consequently, PLHIV experiencing higher levels of HIV-related stigma are at increased risk of transmitting the infection to others (Rubens et al., 2018).
HIV-related stigma has been consistently associated with poor mental health outcomes (Rueda et al., 2016; Parcesepe et al., 2018). Evidence shows that PLHIV are two to three times likely to develop mental disorders than HIV negative people (Huang et al., 2018; Remien et al., 2019; Yi et al., 2015). Psychological problems such as depression and anxiety are among the most common comorbidities among PLHIV across the world (Obadeji et al., 2014; Pappin et al., 2012; Ngum et al., 2017). Research studies in different countries across the sub-Saharan Africa have reported high prevalence rates of mental disorders among PLHIV (Lawler et al., 2011; Minya et al., 2013; Siakwa et al., 2015). The presence of mental disorders among PLHIV is also associated with numerous health and healthcare seeking behaviours such as poor adherence to medications and low rates of retention in HIV care (Joska et al., 2014; Nel & Kagee, 2011; Springer et al., 2012).
While HIV-related stigma and psychological distress are each independent barriers to health seeking behaviour, HIV prevention and ART initiation, the interrelationship between these two remains poorly understood. Several studies have examined constructs of stigma and psychological distress, however, the role of HIV-related stigma mechanisms on the effect of psychological mechanisms on health outcomes remains complex due to a number of mediating pathways (Mitzel et al., 2015 Turan et al., 2016; Helms et al., 2016). The mediating pathways involved are important in designing interventions aimed at reducing the effects of HIV-related stigma and induced psychological distress (Turan et al., 2017).
Since HIV-positive serostatus is often not evident, managing social relationships and serostatus disclosure to avoid stigma and discrimination has been suggested as an added source of stigma induced stress among PLHIV (Swendeman et al., 2006). Different intervention strategies have been proposed, one that targets stigma (both externalized and internalized) and another that treats depression and addresses other mediating psychosocial factors (Turan et al., 2017). However, these are complex constructs that cannot be seen as a simple single notion. Programs with adequate resources may even target all these mechanisms in a comprehensive intervention strategy to maximize the probability of success in reducing the effects of HIV-related stigma on the well-being of PLHIV (Turan et al., 2017). However, more nuanced and deeper understanding of how different mechanisms affect health outcomes among PLHIV is important in designing interventions aimed at reducing the effects of HIV-related stigma.
Evidence shows that the mechanisms of how stigma affects psychological distress among PLHIV may be explained by several biological, environmental, social, economic and demographic factors (Tran et al., 2019). Therefore, the understanding of mechanisms between HIV-related stigma and psychological distress may be influenced by mediating contextual factors. Characterizing contexts of the populations of interest is important and should be incorporated in designing interventions to reduce stigma (Tran et al., 2019). This paper examines factors associated with HIV related stigmatizing attitudes among HIV-positive people in South Africa who are psychologically distressed using the 2012 nationally representative population-based HIV household survey.
2. Methods
2.1. Data source
This study used data from the 2012 South African National HIV Prevalence, Incidence and Behaviour Survey, a nationally representative population-based household survey, described in detail elsewhere (Shisana et al., 2014). Briefly, participants were selected using multi-stage cluster sampling design. A systematic probability sample of 15 households was drawn from each of 1000 enumeration areas (EAs) selected randomly from strata defined by locality type and province from the updated 2007 master sample of census EAs. All members belonging to selected household were asked to participate in the survey.
2.2. Study procedure
The survey administered age-appropriate questionnaires to consenting participants, soliciting information on demographic factors, and HIV-related knowledge, attitudes, practice, sexual history and behaviours including questions on HIV-related stigma (Shisana et al., 2014). Dried blood spots (DBS) specimens were also collected from participants who consented for HIV testing. Samples were tested for HIV antibodies using a testing algorithm with three different immunoassays (Vironostika HIV Uni-Form II plus O, Biomeriux, Boxtel, The Netherlands; Advia Centaur XP, Siemens Medical Solutions Diagnostics, Tarrytown, NJ, USA; (Roche Elecys 2010 HIV Combi, Roche Diagnostics, Mannheim, Germany).
The current study is based on a sub-sample of youth and adult individuals 15 years and older who tested positive for HIV who responded to questions which measured both HIV-related stigma and psychological distress during the interviews.
2.3. Measures
2.3.1. Primary outcome
The primary outcome measure of the HIV stigma scale was based on a question relating to attitudes and beliefs against PLHIV with 7 items measuring various aspects of HIV-related stigma (Shisana et al., 2005): (1) Would you buy food if you knew that a shopkeeper or food seller had HIV? (2) Would you be willing to care for a family member with AIDS? (3) If a teacher has HIV but is not sick, he or she should be allowed to continue teaching? (4) Is it a waste of money to train or give a promotion to someone with HIV/AIDS? (5) Would you want to keep the HIV positive status of a family member a secret? (6) Are you comfortable talking to at least one member of your family about HIV/AIDS? (7) A person would be foolish to marry a person who is living with HIV/AIDS?
Exploratory factors analysis was used to analyse responses to these questions (yes = 1, no = 2, not sure = 3). A varimax orthogonal rotation was used to assess the underlying domains of stigma and reduce the number of items needed (Fabrigar et al., 1999). Eigenvalues were used to identify factors that account for most variance within the items, and Cronbach's Alpha was used to assess the reliability of factor loadings. Variables with a factor loading of at least 0.4 and factors with an eigenvalue of at least 1 were retained for the final analysis (DeVellis, 1991). A simple HIV stigma index score was then calculated by summing the scores across all the items. Scores below the mean were classified as low levels of stigma and those above as high levels of stigma. The index variable was dichotomized into a binary outcome measure of low stigma = 0 and high stigma = 1. A Cronbach's Alpha of 0.60 or greater was considered sufficient to determine reliability.
The HIV stigma index scale was stratified by the presence and absence of psychological distress using respondent's experience of anxiety and depressive disorders measured using the Kessler 10 scale (Kessler et al., 2003), which consists of 10 items that describe how they felt during the previous 30 days. How often did you feel: Tired out for no good reason? So nervous that nothing could calm you down? Hopeless; Restless or fidgety: So restless that you could not sit still; Depressed? That everything was an effort? So sad that nothing could cheer you up? Worthless?’ Responses to these items were recorded using a 5-point Likert scale (1 = never, 2 = rarely, 3 = some of the time, 4 = most of the time, 5 = all of the time). This scale has been validated among low- and middle-income countries including South Africa (Andrews & Slade, 2001; Spies et al., 2009). The scores from these responses were then summed to calculate a total score indicating whether the respondents were likely to experience psychological distress. Raw scores were then summed to calculate a total score indicating whether the respondents were likely to be well (score below 20), experiencing mild (score 20–24), moderate (score 25–29) or severe (score 30 and above) psychological distress (Andrews & Slade, 2001). The scores were then dichotomized into those who scored <19 absence of psychological distress = 1) and those who scored ≥20 (presence of psychological distress = 2).
2.3.2. Explanatory variables
Explanatory variables included socio-demographic factors such as age in years (15–24, 25–34, 35–49, 50 years and older), sex (male and female), race groups (black African and other races), educational level (primary/no education, secondary, tertiary), employment status (unemployed and employed), asset-based SES (low and high) and locality type (urban formal, urban informal, rural informal/tribal areas, rural formal/farm areas). This also included HIV-related knowledge and awareness factors such as correct knowledge and rejection of myths about HIV (no and yes), ever test for HIV (no and yes), know HIV results (no and yes), self-perceived risk of HIV infection (no and yes), exposure to ARVs (no and yes), self-rated health (fair/poor and good/excellent).
2.4. Statistical analysis
Descriptive statistics were used to summarize characteristics of the study sample. Bivariate logistic regression was used to assess the factors associated with high levels of stigmatizing attitudes among HIV positive individuals with psychological distress. Statistically significant variables were entered into multivariate logistic regression analysis. All models accounted for the complex survey design. Crude and adjusted odds ratios (aOR) with 95% confidence intervals (CI) and a p-value ≤ 0.05 were considered statistically significant. All statistical analyses were conducted using the Stata software package All statistical analysis was done in Stata version 15.0 software using “svy” commands to introduce command to take into account complex survey design (Stata Corp, College Station, Texas, USA).
3. Results
3.1. Sample characteristics and HIV-related stigma
Table 1 presents sample characteristics of the study sample and the prevalence of high levels of stigmatizing attitudes among HIV positive individuals with psychological distress. The sample consisted mainly of those 25–34 years, was predominantly female and Black African. The majority were married, had secondary level education, unemployed, were from low SES households and resided in urban and rural informal areas. Most respondents did not have correct knowledge and rejection of myths about HIV, never tested for HIV, and did not know their HIV status. About half perceived themselves as being at risk of HIV infection. The majority were not on ARVs and reported excellent/good self-rated health.
Table 1.
Socio-demographic characteristics and prevalence of high levels of stigmatizing attitudes among HIV positive individuals with psychological distress.
| Variables | Study sample |
High levels of stigmatizing attitudes |
|||
|---|---|---|---|---|---|
| Total | % | n | % | CI | |
| Age in years | |||||
| 15 to 24 | 384 | 11.9 | 101 | 27.5 | 17.2–40.8 |
| 25 to 34 | 890 | 40.3 | 274 | 37.5 | 28.7–47.2 |
| 35 to 49 | 879 | 38.4 | 320 | 40.2 | 32.0–49.0 |
| 50 years and older | 368 | 9.4 | 126 | 41.8 | 30.3–54.3 |
| Sex | |||||
| Male | 784 | 38.4 | 209 | 45.1 | 34.9–55.8 |
| Female | 1737 | 61.6 | 612 | 34.7 | 28.8–41.1 |
| Race groups | |||||
| Black African | 2293 | 97.3 | 758 | 38.1 | 32.8–43.6 |
| Other races | 228 | 2.7 | 63 | 31.6 | 15.8–53.2 |
| Marital status | |||||
| Not married | 2029 | 80.9 | 676 | 37.9 | 32.3–43.8 |
| Married | 456 | 19.1 | 123 | 38.4 | 24.7–54.3 |
| Educational level | |||||
| Primary/no education | 555 | 21.3 | 194 | 56.1 | 45.4–66.3 |
| Secondary | 1493 | 74.4 | 473 | 31.9 | 25.4–39.2 |
| Tertiary | 81 | 4.3 | 19 | 32.8 | 11.7–64.4 |
| Employment status | |||||
| Unemployed | 1510 | 63 | 534 | 35.5 | 29.6–41.7 |
| Employed | 885 | 37 | 248 | 40.9 | 30.6–52.0 |
| Asset based SES | |||||
| Low | 2016 | 80.3 | 648 | 40.2 | 34.5–46.2 |
| High | 479 | 19.7 | 159 | 29.2 | 17.9–43.6 |
| Locality type | |||||
| Urban formal | 871 | 40.4 | 279 | 35.7 | 26.1–46.5 |
| Urban informal | 500 | 13.4 | 164 | 17.5 | 11.3–26.3 |
| Rural informal/tribal areas | 818 | 41.5 | 283 | 45.6 | 38.4–53.0 |
| Rural formal/farm areas | 332 | 4.6 | 95 | 56.5 | 43.7–68.4 |
| Correct knowledge and myth rejection about HIV | |||||
| No | 2013 | 81.3 | 666 | 39 | 33.1–45.3 |
| Yes | 508 | 18.7 | 155 | 32.5 | 23.1–43.6 |
| Ever test for HIV | |||||
| No | 474 | 19.4 | 128 | 42.6 | 29.6–56.6 |
| Yes | 2041 | 80.6 | 693 | 36.9 | 31.3–42.9 |
| Know HIV results | |||||
| No | 1895 | 94.7 | 647 | 36.4 | 30.5–42.7 |
| Yes | 97 | 5.3 | 29 | 37.6 | 19.0–60.8 |
| Self-perceived risk of HIV | |||||
| No | 1239 | 48.6 | 454 | 38.2 | 31.0–45.9 |
| Yes | 1221 | 51.4 | 340 | 38.3 | 30.7–46.5 |
| Exposure to ARVs | |||||
| No | 1738 | 69.7 | 529 | 39.7 | 32.9–46.9 |
| Yes | 781 | 30.3 | 291 | 34.3 | 27.1–42.3 |
| Self-rated health | |||||
| Fair/poor | 700 | 28.4 | 356 | 36.6 | 29.0–44.9 |
| Good/excellent | 1811 | 71.6 | 465 | 38.9 | 32.0–46.3 |
CI-confidence interval, SES = socio-economic status.
The sample comprised 2521 HIV positive individuals that responded to the question on psychological distress, and 34.3% (95%CI: 30.5–38.3) had psychological distress. Of these, 37.9% (95% CI: 32.7–43.4) had high levels of stigmatizing attitudes for HIV. Table 1 shows that the prevalence of HIV related stigmatizing attitudes among HIV positive individuals with psychological distress was higher among those 50 years and older, other race groups, the married, those with no education or with primary level education, the unemployed, those from low SES households and those residing rural informal areas. The stigma levels were also higher among those who had no correct knowledge and rejection of myths about HIV, those who never tested for HIV, those who perceived themselves as being at risk of HIV, those not on ARTs and those who reported fair/poor self-rated health.
3.1. Factors associated with HIV related stigmatizing attitudes
3.1.1. Bivariate models
Table 2 presents results of the bivariate logistic regression models of the association between high levels stigmatizing attitudes among PLHIV with psychological distress. Increase in levels stigmatizing attitudes for HIV was significantly associated with other race groups, those residing in rural informal/tribal areas and rural formal/farm areas, and those who perceived themselves as being at risk of HIV infection. Decrease in levels stigmatizing attitudes for HIV was significantly associated with secondary and tertiary level education, high SES households, correct knowledge and rejection of myths about HIV, ever tested for HIV, and exposure to ARTs.
Table 2.
Bivariate regression models of factors associated with HIV related stigmatizing attitudes among PLHIV with psychological distress.
| Variables |
High levels of stigmatizing attitudes |
|||
|---|---|---|---|---|
| Age in years | OR | 95% CI | p-value | |
| 15 to 24 | 1 | |||
| 25 to 34 | 1.26 | 0.82 | 1.93 | 0.29 |
| 35 to 49 | 1.51 | 0.98 | 2.35 | 0.06 |
| 50 years and older | 1.62 | 0.95 | 2.75 | 0.08 |
| Sex | ||||
| Male | 1 | |||
| Female | 0.73 | 0.53 | 1.00 | 0.05 |
| Race groups | ||||
| Black African | 1 | |||
| Other races | 1.69 | 1.00 | 2.88 | 0.05 |
| Marital status | ||||
| Not married | 1 | |||
| Married | 0.88 | 0.59 | 1.32 | 0.543 |
| Educational level | ||||
| Primary/no education | 1 | |||
| Secondary | 0.60 | 0.41 | 0.88 | 0.01 |
| Tertiary | 0.43 | 0.14 | 1.30 | 0.14 |
| Employment status | ||||
| Unemployed | 1 | |||
| Employed | 1.17 | 0.85 | 1.61 | 0.35 |
| Asset based SES | ||||
| Low | 1 | |||
| High | 0.69 | 0.50 | 0.96 | 0.03 |
| Locality type | ||||
| Urban formal | 1 | |||
| Urban informal | 0.67 | 0.42 | 1.06 | 0.09 |
| Rural informal/tribal areas | 1.22 | 0.83 | 1.79 | 0.30 |
| Rural formal/farm areas | 2.07 | 1.25 | 3.41 | 0.00 |
| Correct knowledge and myth rejection about HIV | ||||
| No | 1 | |||
| Yes | 0.54 | 0.37 | 0.80 | 0.00 |
| Ever test for HIV | ||||
| No | 1 | |||
| Yes | 0.56 | 0.38 | 0.82 | 0.00 |
| Know HIV results | ||||
| No | 1 | |||
| Yes | 0.68 | 0.33 | 1.43 | 0.31 |
| Self-perceived risk of HIV | ||||
| No | 1 | |||
| Yes | 1.36 | 1.03 | 1.78 | 0.03 |
| Exposure to ARVs | ||||
| No | 1 | |||
| Yes | 0.75 | 0.56 | 1.00 | 0.05 |
| Self-rated health | ||||
| Fair/poor | 1 | |||
| Good/excellent | 0.95 | 0.74 | 1.21 | 0.66 |
CI-confidence interval, SES = socio-economic status.
3.1.2. Multivariate model
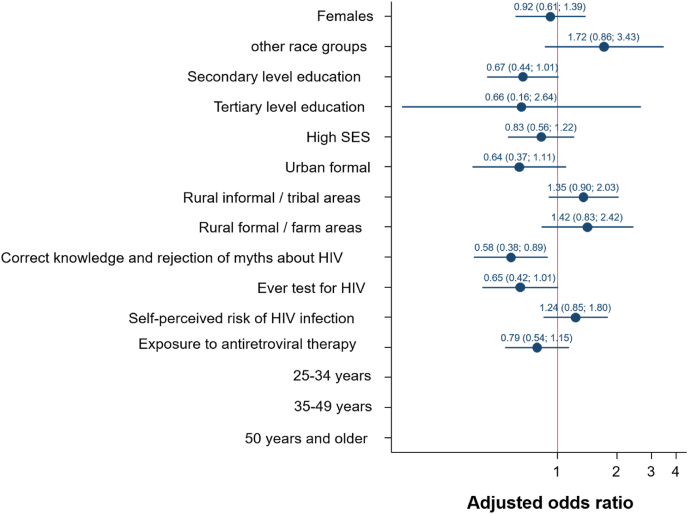
Fig. 1 multivariate logistic regression model of factors associated with high levels stigmatizing attitudes among PLHIV with psychological distress. HIV related stigmatizing attitudes among PLHIV with psychological distress was significantly less likely among those with secondary level education [aOR = 0.67 (95% CI: 0.44–1.01), p = 0.050] compared to no education/primary level education, those with correct knowledge and rejection of myths about HIV [aOR = 0.58 (95% CI: 0.38–0.89), p = 0.013] compared to their counterparts, and those who ever tested for HIV [aOR = 0.65 (95% CI: 0.42–1.01), p = 0.054].
Fig. 1.
Multivariate regression models of factors associated with HIV related stigmatizing attitudes among PLHIV with psychological distress.
4. Discussion
This study used a nationally representative sample and shows that the prevalence of high levels of HIV related stigmatizing attitudes was higher among people with psychological distress compared to their counterparts. Despite many millions of rands spent on HIV education in South Africa, the results of the 2012 national survey indicated poor HIV knowledge (Shisana et al., 2014). In this sub-sample of HIV positive individuals, three quarters of the study sample had secondary level education but only 18.7% of the total sample knew the correct answers to the questions about HIV. Furthermore, although the majority of respondents indicated that they had tested for HIV, most did not know their HIV status, and about half perceived themselves at risk of HIV, and a third reported exposure to ARVs. These findings suggest a need for the involvement of the Department of Basic Education (DBE) in the response to the HIV epidemic through a life skills programme to improve HIV knowledge levels, especially because the majority of respondents reported secondary level education. This has been the case since year 2000 with little or success, and in 2017 DBE developed a new national policy which mandated it to provide curriculum-based Sexuality Education and access to Sexual Reproductive Health Services. The current observations suggest that the implementation of the new policy need to be monitored and regularly evaluated to improve HIV education, teach learners skills to reduce their risk of infection and reduce the associated stigma.
The findings revealed that HIV related stigmatizing attitudes were higher among those with psychological distress and varied by socio-demographic variables. HIV related stigmatizing attitudes were higher among older age group, males, those with lower education, those from low SES household, and those residing in urban and rural informal areas. The prevalence of HIV related stigmatizing attitudes was also higher among those who had no correct knowledge and rejection of myths about HIV, those who never tested for HIV, and those not on ART among PLHIV experiencing psychological distress.
Other studies also found that the prevalence of HIV related stigmatizing attitudes varies with socio-demographic and health-related factors and context (Bagchi et al., 2019; Emlet et al., 2015; Subedi et al., 2019). This probably reflects the complex nature of HIV-related stigma and the social process that interacts with socio-demographic factors, HIV-knowledge, HIV testing and exposure to ART to reinforce stigma and discrimination (Visse et al., 2009; Hargreaves et al., 2018).
In this study the results of the final model revealed that the odds of HIV related stigmatizing attitudes among PLHIV with psychological distress were low among those with higher levels of education. Evidence shows that people with low or no educational attainment are likely to have misconceptions about HIV and may not have appropriate information regarding HIV mode of transmission and treatment (Carlos et al., 2015; Letamo, 2019; Mondal et al., 2015; Sano et al., 2016). Furthermore, the findings showed that HIV related stigmatizing attitudes among PLHIV with psychological distress was less likely among those with correct knowledge and rejection of myths about HIV. HIV-related stigma has been associated with a lack of proper information regarding the spread of the disease and fear (Boushab et al., 2017). It has been demonstrated that increased education reduced stigma (Pulerwitz et al., 2010; Jacobi et al., 2020). Hence, the need to have more HIV education and skill building strategies.
Furthermore, HIV related stigmatizing attitudes among PLHIV with psychological distress was low among people who ever tested for HIV. There is considerable evidence showing an inverse relationship between HIV-related stigma and HIV testing (Mall et al., 2013; Okumu et al., 2017; Rubens et al., 2018). Studies show that voluntary counselling contributes to reducing HIV-related stigma because it provides information that may reduce misconceptions about HIV and minimise mental stress (James & Ryan, 2018; Jürgensen et al., 2013). These findings highlight the fact that one's initial prognosis, access to accurate information regarding HIV, and access to care and supportive services are important in dealing with HIV stigma and psychological induced distress.
This study has some limitations. It is based on a cross-sectional design, which is appropriate for identifying associations, and not suitable for exploring causal pathways. Although item nonresponse can never be totally prevented, gaps in the data matrix or missingness can pose serious problems in the analysis, because restricting the analysis to complete cases results in loss of information, and therefore estimates may be less efficient (De Leeuw, 2001). The data on both psychological distress and HIV-related stigma were collected through a self-reported questionnaire, therefore recall bias and social desirability bias may exist. In addition, others have also suggested that self-reports of stigma and discrimination are not reliable for measuring discrimination at the structural or social level (Meyer, 2003). There is a need for more evidence that the construct of HIV stigma scale and the Kessler psychological distress scale are relatively consistent across different settings or cross-cultural populations. Nonetheless, given the widespread stigma experienced by people with HIV and its fairly consistent manifestations, we hypothesize that the validated HIV Stigma 7-item scale will have relevance in a variety of settings in South Africa. Furthermore, the K10 scale has been validated and can be used to detect HIV related mood and anxiety disorders among HIV positive individuals (Spies et al., 2009).
Another limitation is that the focus of this study was on stigmatizing attitudes but the many studies that have explored stigma, including a multi-country African study, have noted that the stigma associated with people living with HIV, is both internal and external, and it is this combination that has such disastrous effects (Parcesepe et al., 2018). However, this study was unable to investigate internal stigma since it was not measured in the national survey. Nevertheless, the major strength of this study is the fact that it utilised data from a large nationally representative survey, which can be generalised to other PLHIV in the country.
5. Conclusion
The findings identified little or no education, insufficient HIV knowledge and myth rejection, and never testing for HIV, as factors associated with HIV-related stigmatizing attitudes among PLHIV experiencing psychological distress. The findings suggest a need to reinvigorate stigma-reduction interventions in the national HIV response with emphasis on HIV awareness and education campaigns. In addition, HIV testing services should be reinforced through communication strategies targeted against HIV stigmatization, discrimination and fear. These interventions should be targeted at multiple levels including the interpersonal institutions such as schools, and workplaces. There is also a need to continuously engage PLHIV in programs through counselling, social support, appropriate coping strategies (resilience and self-efficacy) for acceptance of HIV positive status and to help them adapt to any encountered difficulties due to HIV-related stigma and psychological distress.
Author statement
I am the lead author of this manuscript.
Ethical statement
The survey protocol was approved by the HSRC's Research Ethics Committee (REC: 5/17/11/10) and the Associate Director of Science of the National Center for HIV and AIDS, Viral Hepatitis, STD and TB Prevention at the Centers for Disease Control and Prevention (CDC) in Atlanta, GA, USA.
Acknowledgements
The data used in this paper were collected with support of the President's Emergency Plan for AIDS Relief (PEPFAR) through the CDC under the terms of 5U2GGH000570. Additional support was also received from the Bill & Melinda Gates Foundation, the South African National AIDS Council (SANAC) and the United Nations Children's Fund (UNICEF). The contents of the paper are solely the responsibility of the authors and do not necessarily represent the official views of CDC or any of the funders alike. The original data are archived and accessible from http://curation.hsrc.ac.za/doi10.14749-1500530684.
References
- Andrews G., Slade T. Interpreting scores on the Kessler psychological distress scale (K10) Australian & New Zealand Journal of Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842x.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- Bagchi A.D., Holzemer W., Peavy D. Predictors of enacted, internal, and anticipated stigma among PLHIV in New Jersey. AIDS Care. 2019;31(7):827–835. doi: 10.1080/09540121.2018.1554242. [DOI] [PubMed] [Google Scholar]
- Boushab B.M., Fall-Malick F.Z., Ould Cheikh Melaïnine M.L., Basco L.K. Forms of stigma and discrimination in the daily lives of HIV positive individuals in Mauritania. The Open AIDS Journal. 2017;11:12–17. doi: 10.2174/1874613601711010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell J.C., Baty M.L., Ghandour R.M., Stockman J.K., Francisco L., Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: A review. International Journal of Injury Control and Safety Promotion. 2008;15(4):221–231. doi: 10.1080/17457300802423224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlos S., Martínez-González M.Á., Burgueño E., López-Del Burgo C., Ruíz-Canela M., Ndarabu A., Tshilolo L., Tshiswaka P., Labarga P., de Irala J. Misconceptions about HIV infection in Kinshasa (Democratic Republic of Congo): A case-control study on knowledge, attitudes and practices. Sexually Transmitted Infections. 2015;91(5):334–337. doi: 10.1136/sextrans-2014-051734. [DOI] [PubMed] [Google Scholar]
- Clum G., Chung S.E., Ellen J.M. Mediators of HIV-related stigma and risk behavior in HIV infected young women. AIDS Care. 2009;21(11):1455–1462. doi: 10.1080/09540120902883069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Leeuw E.D. Reducing missing data in surveys: An overview of methods. Quality and Quantity. 2001;35:147–160. [Google Scholar]
- Dlamini P.S., Wantland D., Makoae L.N., Chirwa M., Kohi T.W., Greeff M., Naidoo J., Mullan J., Uys L.R., Holzemer W.L. HIV stigma and missed medications in HIV-positive people in five African countries. AIDS Patient Care and STDs. 2009;23:377–387. doi: 10.1089/apc.2008.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahimi Kalan M., Han J., Ben Taleb Z., Fennie K.P., Asghari Jafarabadi M., Dastoorpoor M., Hajhashemi N., Naseh M., Rimaz S. Quality of life and stigma among people living with HIV/AIDS in Iran. HIV AIDS (Auckl) 2019;11:287–298. doi: 10.2147/HIV.S221512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emlet C.A., Brennan D.J., Brennenstuhl S., Rueda S., Hart T.A., Rourke S.B. The impact of HIV-related stigma on older and younger adults living with HIV disease: Does age matter? AIDS Care. 2015;27(4):520–528. doi: 10.1080/09540121.2014.978734. [DOI] [PubMed] [Google Scholar]
- Fabrigar L., Wegener D., MacCallum R.S.E. Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods. 1999;4(3):272–299. doi: 10.1037/1082-989X.4.3.272. [DOI] [Google Scholar]
- Hargreaves J.R., Krishnaratne S., Mathema H., Lilleston P.S., Sievwright K., Mandla N.…Stangl A. Individual and community-level risk factors for HIV stigma in 21 Zambian and South African communities: Analysis of data from the HPTN071 (PopART) study. AIDS. 2018;32(6):783–793. doi: 10.1097/QAD.0000000000001757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms C.B., Turan J.M., Atkins G., Kempf M.C., Clay O.J., Raper J.L.…Turan B. Interpersonal mechanisms contributing to the association between HIV-related internalized stigma and medication adherence. AIDS and Behavior. 2016;21(1):238–247. doi: 10.1007/s10461-016-1320-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang X., Meyers K., Liu X., Li X., Zhang T., Xia W.…Ye R. The double burdens of mental health among AIDS patients with fully successful immune restoration: A cross-sectional study of anxiety and depression in China. Frontiers in Psychiatry. 2018;9:384. doi: 10.3389/fpsyt.2018.00384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C.A., Atanga P.N., Bin L.K., Fru A.J.C., Appel G., Mbone V.N.…Malfertheiner P. “My friend with HIV remains a friend”: HIV/AIDS stigma reduction through education in secondary schools—a pilot project in Buea, Cameroon. Journal of the International Association of Physicians in AIDS Care. 2020;19:1–7. doi: 10.1177/2325958219900713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James T.G., Ryan S.J. HIV knowledge mediates the relationship between HIV testing history and stigma in college students. Journal of American College Health. 2018;66(7):561–569. doi: 10.1080/07448481.2018.1432623. [DOI] [PubMed] [Google Scholar]
- Joska J.A., Obayemi A., Jr., Cararra H., Sorsdahl K. Severe mental illness and retention in anti-retroviral care: A retrospective study. AIDS and Behavior. 2014;18:1492–1500. doi: 10.1007/s10461-014-0709. [DOI] [PubMed] [Google Scholar]
- Jürgensen M., Fossgard I., Sandøy C.M., Fylkesnesa K. Effects of home-based voluntary counselling and testing on HIV-related stigma: Findings from a cluster-randomized trial in Zambia. Social Science & Medicine. 2013;81:18–25. doi: 10.1016/j.socscimed.2013.01.011. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kinsler J.J., Wong M.D., Sayles J.N., Davis C., Cunningham W.E. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care and STDs. 2007;21:584–592. doi: 10.1089/apc.2006.0202. [DOI] [PubMed] [Google Scholar]
- Lawler K., Mosepele M., Seloilwe E., Ratcliffe S., Steele K., Nthobatsang R., Steenhoff A. Depression among HIV-positive individuals in Botswana: A behavioral Surveillance. AIDS and Behavior. 2011;15:204–208. doi: 10.1007/s10461-009-9622-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letamo G. Misconceptions about HIV transmission among adolescents: Levels, trends and correlates from the Botswana AIDS impact surveys, 2001-2013: A short report. AIDS Care. 2019;31(1):48–52. doi: 10.1080/09540121.2018.1488030. [DOI] [PubMed] [Google Scholar]
- Mall S., Middelkoop K., Mark D., Wood R., Bekker L.G. Changing patterns in HIV/AIDS stigma and uptake of voluntary counselling and testing services: The results of two consecutive community surveys conducted in the Western Cape, South Africa. AIDS Care. 2013;25(2):194–201. doi: 10.1080/09540121.2012.689810. [DOI] [PubMed] [Google Scholar]
- Meyer I.H. Prejudice as stress: Conceptual and measurement problem. American Journal of Public Health. 2003;93(2):262–265. doi: 10.2105/ajph.93.2.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitzel L.D., Vanable P.A., Brown J.L., Bostwick R.A., Sweeney S.M., Carey M.P. Depressive symptoms mediate the effect of HIV-related stigmatization on medication adherence among HIV-infected men who have sex with men. AIDS and Behavior. 2015;19(8):1454–1459. doi: 10.1007/s10461-015-1038-6. [DOI] [PubMed] [Google Scholar]
- Mondal N.I., Hoque N., Chowdhury R.K., Hossain S. Factors Associated with misconceptions about HIV transmission among ever-married women in Bangladesh. Japanese Journal of Infectious Diseases. 2015;68:13–19. doi: 10.7883/yoken.JJID.2013.323. 69. [DOI] [PubMed] [Google Scholar]
- Nel A., Kagee A. Common mental health problems and antiretroviral therapy adherence. AIDS Care. 2011;23(11):1360–1365. doi: 10.1080/09540121.2011.565025. [DOI] [PubMed] [Google Scholar]
- Ngum P.N., Fon P.N., Ngu R.C., Verla V.S., Luma N.H. Depression among HIV/AIDS patients on highly active antiretroviral therapy in the southwest regional hospitals of Cameroon: A cross-sectional study. Neurology and Therapy. 2017;6(1):103–114. doi: 10.1007/s40120-017-0065-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obadeji A., Ogunlesi A.O., Adebowale T.O. Prevalence and predictors of depression in people living with HIV/AIDS attending an outpatient clinic in Nigeria. Iranian Journal of Psychiatry and Behavioral Sciences. 2014;8(1):26–31. [PMC free article] [PubMed] [Google Scholar]
- Okumu E., Jolly D.H., Alston L.M., Eley N.T., Laws M., MacQueen K.M. Relationship between Human Immunodeficiency Virus (HIV) knowledge, HIV-related stigma, and HIV testing among young black adults in a South Eastern City. Front Public Health. 2017;5(47) doi: 10.3389/fpubh.2017.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappin M., Wouters E., Booysen F.L. Anxiety and depression amongst patients enrolled in a public sector antiretroviral treatment programme in South Africa: A cross-sectional study. BMC Public Health. 2012;12(1):244. doi: 10.1186/1471-2458-12-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parcesepe A.M., Bernard C., Agler R., Ross J., Yotebieng M., Bass J.…Althoff K.N. Mental health and HIV: Research priorities related to the implementation and scale up of “treat all” in sub-Saharan Africa. Journal of Virus Eradication. 2018;4(2):16–25. doi: 10.1016/S2055-6640(20)30341-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R., Bajenja E., Karamagi E., Tindyebwa D. World Health and Population Report; 2007. AIDS –Related stigma: Perceptions of family caregivers and health volunteers in Western Uganda. [DOI] [PubMed] [Google Scholar]
- Pulerwitz J., A Michaelis A., Weiss E., Brown L., Mahendra V. Reducing HIV-related stigma: Lessons learned from horizons research and programs. Public Health Reports. 2010;125(2):272–281. doi: 10.1177/003335491012500218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasoolinajad M., Abedinia N., Noorbala A.A., Mohraz M., Badie B.M., Hamad A., Sahebi L. Relationship among HIV-related stigma, mental health and quality of life for HIV-positive patients in Tehran. AIDS and Behavior. 2018;22(12):3773–3782. doi: 10.1007/s10461-017-2023-z. [DOI] [PubMed] [Google Scholar]
- Remien R.H., Stirratt M.J., Nguyen N., Robbins R.N., Pala A.N., Mellins C.A. Mental health and HIV/AIDS: The need for an integrated response. AIDS. 2019;33(9):1411–1420. doi: 10.1097/QAD.0000000000002227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubens M., Saxena A., Ramamoorthy V., McCoy H.V., Beck-Sagué C., Jean-Gilles M. HIV-related stigma, quality of care, and coping skills: Exploring factors affecting treatment adherence among PLWH in Haiti. Journal of the Association of Nurses in AIDS Care. 2018;29(4):570–579. doi: 10.1016/j.jana.2018.02.002. [DOI] [PubMed] [Google Scholar]
- Rueda S., Mitra S., Chen S., Gogolishvili D., Globerman J., Chambers L.…Rourke S.B. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: A series of meta-analyses. BMJ Open. 2016;6(7) doi: 10.1136/bmjopen-2016-011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sambisa W., Curtis S., Mishra V. AIDS stigma as an obstacle to uptake of HIV testing: Evidence from a Zimbabwean national population-based survey. AIDS Care. 2010;22(2):170–186. doi: 10.1080/09540120903038374. [DOI] [PubMed] [Google Scholar]
- Sano Y., Roger A., Atuoye K.N., Hussey L.K., Bayne J.S.Z.G. Persistent misconceptions about HIV transmission among males and females in Malawi. BMC International Health and Human Rights. 2016;16(6) doi: 10.1186/s12914-016-0089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shisana O., Rehle T., Simbayi L., Parker W., Zuma K., Bhana A.…& The SABSSM Team . HSRC Press; Cape Town: 2005. South African National HIV prevalence, incidence, behaviour and communication Survey. [Google Scholar]
- Shisana O., Rehle T., Simbayi L.C., Zuma K., Jooste S., Zungu N.…& The SABSSM Team . HSRC Press; Cape Town: 2014. South African national HIV prevalence, incidence and behaviour survey. [DOI] [PubMed] [Google Scholar]
- Siakwa M., Okanlawon F.A., Druye A.A., Ankobil A., Aniweh Y., Dzah S. Prevalence of psychiatric disorders in HIV patients in the Central Region of Ghana. Journal of Community Medicine and Primary Health Care. 2015;27(1):79–85. [Google Scholar]
- Spies G., Kader K., Kidd M., Myer L., Stein D.J., Seedat S. Validity of the K-10 in detecting DSM-IV-defined depression and anxiety disorders among HIV-infected individuals. AIDS Care. 2009;21(9):1163–1168. doi: 10.1080/09540120902729965. [DOI] [PubMed] [Google Scholar]
- Springer S.A., Dushaj A., Azar M.M. The impact of DSM-IV mental disorders on adherence to combination antiretroviral therapy among adult persons living with HIV/AIDS: A systematic review. AIDS and Behavior. 2012;16:2119–2143. doi: 10.1007/s10461-012-0212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subedi B., Timilsina B.D., Tamrakar N. Perceived stigma among people living with HIV/AIDS in Pokhara, Nepal. HIV AIDS (Auckl) 2019;11:93–103. doi: 10.2147/HIV.S181231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran B.X., Phan H.T., Latkin C.A., Nguyen H.L.T., Hoang C.L., Ho C.H.S., Ho R.C.M. Understanding global HIV stigma and discrimination: Are contextual factors sufficiently studied? (GAPRESEARCH) International Journal of Environmental Research and Public Health. 2019;16(11):1899. doi: 10.3390/ijerph16111899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan B., Budhwani H., Fazeli P.L., Browning W.R., Raper J.L., Mugavero M.J., Turan J.M. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS and Behavior. 2017;21(1):283–291. doi: 10.1007/s10461-016-1451-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan B., Smith W., Cohen M.H., Wilson T.E., Adimora A.A., Merenstein D.…Turan J.M. Mechanisms for the negative effects of internalized HIV-related stigma on ART adherence in women: The mediating roles of social isolation and depression. Journal of Acquired Immune Deficiency Syndromes. 2016;72(2):198–205. doi: 10.1097/QAI.0000000000000948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi S., Chhoun P., Suong S., Thin K., Brody C., Tuot S. AIDS-related stigma and mental disorders among people living with HIV: A cross-sectional study in Cambodia. PloS One. 2015;10(3) doi: 10.1371/journal.pone.0121461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Li X., Liu Y., Qiao S., Zhou Y., Shen Z., Chen Y. Substance use and psychosocial status among people living with HIV/AIDS who encountered HIV stigma in China: Stratified analyses by socio-economic status. PloS One. 2016;11(11) doi: 10.1371/journal.pone.0165624. [DOI] [PMC free article] [PubMed] [Google Scholar]