Abstract
Introduction and importance
The usefulness of laparoscopic surgery in the treatment of Spigelian hernias and the appropriate insufflation pressure remains unclear.
Case presentation
Case 1 involved an 81-year-old woman presented with a right abdominal protrusion. CT scan demonstrated a defect in the abdominal wall at the lateral edge of the right rectus abdominis muscle. We diagnosed as Spigelian hernia and performed laparoscopic hernia repair. The insufflation pressure was set at 10 cm H 2 O, and the IPOM method was selected as the repair method. Case 2 involved a 74-year-old male presented with a right abdominal painful bulging. Strangulation was released and CT scan demonstrated a defect in the abdominal wall at the lateral edge of the right rectus abdominis muscle. We diagnosed as Spigelian hernia and performed laparoscopic hernia repair. The insufflation pressure was set at 10 cmH 2 O, and the repair was performed by the hybrid method.
Clinical discussion
In both cases, the positions of the hernia portals marked preoperatively based on the tender areas and confirmed laparoscopically were not accurate. Although Spigelian hernia is a rare disease and various laparoscopic techniques have been reported in recent years, laparoscopic surgery is very useful to obtain an accurate diagnosis and to observe the abdominal wall from inside the abdominal cavity under insufflation, and it is better to decide the repair method according to the situation of each case and institution.
Conclusion
Laparoscopic surgery is important for accurate diagnosis in surgery of Spiegel's hernia, and insufflation pressure of 10 cmH2O was sufficient.
Keywords: Spigelian hernia, Laparoscopic, Hybrid, IPOM, Insufflation, Case report
Highlights
-
•
Laparoscopic surgery, which allows direct visualization under insufflation and accurate identification of the defect location, is necessary for optimal treatment of Spigelian hernias.
-
•
Although there have been few reports on the appropriate insufflation pressure, in this study, 10 cm H2O was sufficient for diagnosis and treatment.
1. Introduction
Spigelian hernia is a rare abdominal wall hernia arising from the Spigelian fascia between the semilunar line and the lateral border of the rectus abdominis [1]. Although the fascial defects are often small and easily strangulated, they are often already retracted at the time of examination, in which case it is not always easy to identify the defect of hernia from the body surface and diagnosis becomes difficult [[2], [3], [4]]. Ultrasonography and CT scan are used for diagnosis [[5], [6], [7], [8]], but ultimately, surgical findings are the most important for surgeon. Although simple suture closure has been conventionally used for treatment, a low recurrence rate has been reported in surgery using mesh [9], and although reports of laparoscopic surgery have increased in recent years, there are still no clear guidelines regarding the optimal technique. Despite this increase in laparoscopic surgery, the therapeutic significance of laparoscopic surgery is still unclear, and the appropriate insufflation pressure is unknown. In this article, we report on our experience with two cases of Spigelian hernia and clarify the advantages of laparoscopic surgery, as well as discuss the literature. This work has been reported in line with the SCARE criteria [10].
2. Presentation of cases
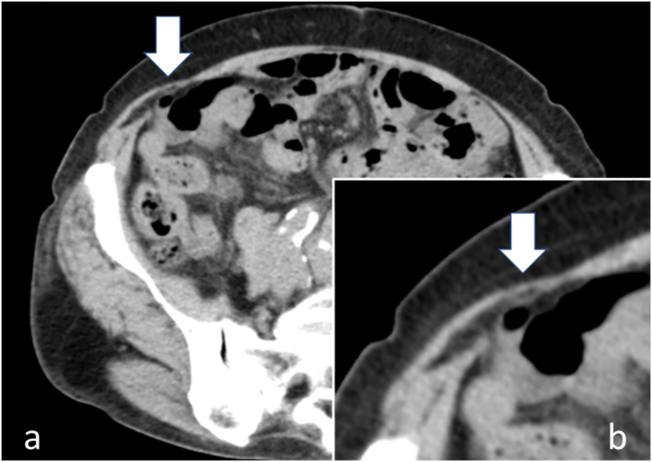
Case 1 is a 75-year-old woman with a history of appendicitis surgery at the age of 16 and right inguinal hernia surgery at the age of 72. She presented with a complaint of right abdominal distension that had persisted for several months. She was 140 cm in height, 40.0 kg in weight, and had a body mass index (BMI) of 20.4. Physical examination revealed surgical scars on the right inguinal region and lower abdomen, and a hernia between the surgical scar of appendicitis on the right lower abdomen and the right costal arch, which bulged to the size of 4 cm in the standing position and disappeared in the supine position. The bulge was clearly different from the surgical scar and there was no redness or tenderness, and thinning of the abdominal wall was palpable in the same area. Blood tests were unremarkable, and CT scan of the abdomen showed a defect in the right abdominal wall and minor prolapse of intra-abdominal fatty tissue at the outer border of the right rectus abdominis muscle (Fig. 1).
Fig. 1.
a: A defect in the abdominal wall at the lateral edge of the right rectus abdominis muscle and prolapse of fatty tissue (arrow). b: Enlarged view of Spigelian hernia (arrow).
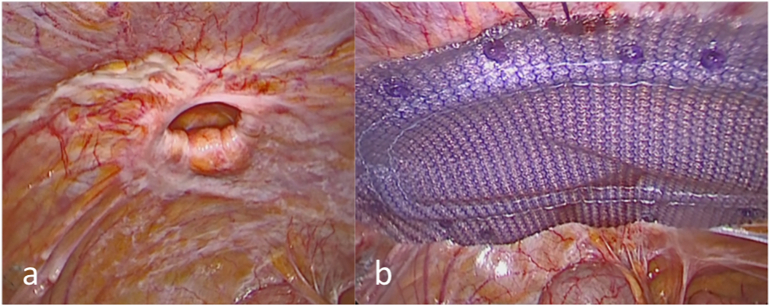
The patient was diagnosed as a hernia of the abdominal wall, and surgery was performed on a standby basis. The operation was performed by the first author, who had over 10 years of specialized surgical experiences. The site of the bulge was preoperatively marked before the surgery was performed. Under general anesthesia, pneumoperitoneum was started in the supine position by inserting a 12-mm camera port through umbilical incision. As the insufflation pressure increased, a defect of approximately 12 mm in size became distinct in the right abdomen (Fig. 2a), and the actual defect was located lateral to the preoperative marking site. The insufflation pressure was increased to 10 cmH2O. A 5-mm port was inserted into the upper left lower abdomen, and intraperitoneal onlay mesh repair (IPOM) using a Bard® Ventorio® ST (8 × 12 cm) was performed. Four stitches of 3–0 absorbable thread were used to fix the patch to the abdominal wall, and the intervening area was fixed with AbsorbatacTM (Medtronic) (Fig. 2b). The operation time was 63 min and the amount of blood loss was only a little.
Fig. 2.
a: Through a laparoscope, a 12-mm round defect is seen at the lateral edge of the right rectus abdominis muscle. b: The defect is fully covered with the BARD® VENTRIO® ST.
Although transient nausea was observed after the surgery, it resolved conservatively, and the patient was discharged on the fifth postoperative day.
Case 2 was an 84-year-old man with uncompensated liver cirrhosis who was taking diuretics. He requested an ambulance with a complaint of sudden onset of distension and pain in the right lower abdomen, and was rushed to our hospital. The patient was referred to our department after manual repair in the emergency department with the diagnosis of a strangulated abdominal wall hernia. The patient was 157 cm tall, weighed 56.3 kg, and had a BMI of 22.8. The patient complained of pain at the lateral border of the right rectus abdominis muscle about 1 cm cephalad from the right superior anterior iliac spine, but the defect was unclear on palpation.
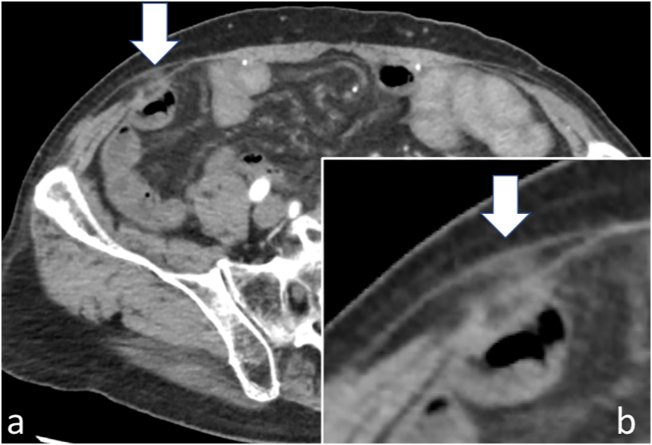
Blood tests showed abnormalities of Alb 3.2 g/dl, NH3 127 μg/dl, and Plt 58,000/μl, reflecting liver cirrhosis. CT scan showed irregularity of the liver surface, blunting of the margins, and a small amount of ascites fluid accumulation, as well as a defect in the abdominal wall at the outer border of the right rectus abdominis muscle, minor prolapse of intra-abdominal fatty tissue, and increased fatty tissue concentration (Fig. 3).
Fig. 3.
a: A defect in the abdominal wall at the lateral edge of the right rectus abdominis muscle and prolapse of fatty tissue (arrow). b: Enlarged view of Spigelian hernia (arrow).
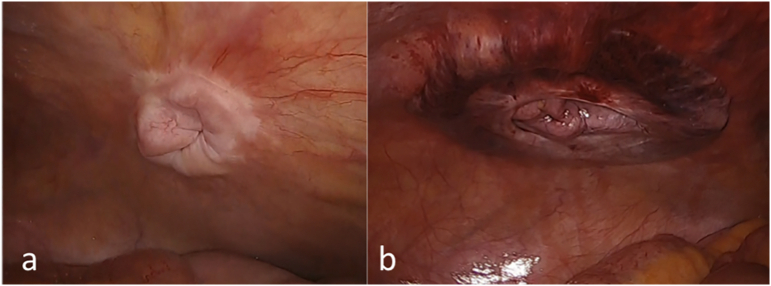
Since the abdominal symptoms were stable after the manual repair, we performed the surgery on a standby basis. The operation was performed by the first author, who had over 10 years of specialized surgical experiences. Under general anesthesia, A 12-mm camera port was inserted through umbilical incision in the supine position, and insufflation was started. With the increase of insufflation pressure, the defect of about 10 mm in size became clear (Fig. 4a). The actual defect was located lateral to the preoperative marking site. The insufflation pressure was increased to 10 cmH2O. A 4-cm skin incision was made along the dermatome line directly above the defect, and the external and internal oblique and transversus abdominis tendon membranes were incised to identify the hernia sac. The subperitoneum was dissected circumferentially while taking care not to tear the peritoneum, and a Bard® Ventralex® ST (6.4 × 6.4 cm) was inserted into the preperitoneal layer and spread circumferentially, and the spread was confirmed laparoscopically (Fig. 4b). The internal oblique tendon membrane was fixed with 3–0 absorbable sutures, and the external oblique tendon membrane was closed with 3–0 absorbable sutures. The operation time was 58 min and the amount of blood loss was only a little. The postoperative course was good, and the patient was discharged on the fourth postoperative day.
Fig. 4.
a: Through a laparoscope, a 10-mm round defect is seen at the lateral edge of the right rectus abdominis muscle. b: The defect is fully covered with the BARD® VENTRALEX® ST.
3. Discussion
Spigelian hernia is a hernia of the abdominal wall arising from the Spigelian fascia between the semilunar line and the outer edge of the rectus abdominis muscle, and is reported to occur in about 2% of all abdominal wall hernias [1]. The area between the line connecting the right and left superior iliac spines and 6 cm from the cephalic side is called the Spigelian hernia belt, and is considered to be a favorable site for Spigelian hernia. The causes of Spigelian hernia are reported to be aging, obesity, high fertility, abdominal trauma, and heavy labor, and can be divided into the following three types according to the penetration formation of the membrane. There are three types of penetrating membranes: (1) penetrating the transversus abdominis tendon membrane, (2) penetrating the internal oblique abdominis tendon membrane, and (3) penetrating the external oblique abdominis tendon membrane. The most frequent type is (2), and our two cases were also classified as (2). Because the external oblique fascia is preserved, the hernia site is often obscured by physical examination, and in both of our cases, the preoperative marking of the hernia site and the actual position confirmed by laparoscopy were different, making preoperative identification of the hernia site difficult. The most advantageous aspect of laparoscopic surgery under insufflation for Spigelian hernia is the diagnosis. Basically, the defect in Spigelian hernias is small, although there are rare cases of huge hernias [11,12]. Because of the difficulty in identifying the hernia from the body surface, surgery without laparoscopy is likely to result in an inappropriately positioned skin incision, resulting in an unnecessarily large incision and an increased risk of bleeding and nerve injury. When laparoscopy is used, the position and size of the defect can be easily diagnosed because it becomes clear and directly visible with increased insufflation pressure. Although there have been no studies focusing on insufflation pressure, and the appropriate insufflation pressure is still unknown, in both of the present two cases, increasing the insufflation pressure to 10 cmH2O was sufficient for observation.
It has been reported that the long-term recurrence rate may be lower with mesh than with simple suture closure [9]. In recent years, laparoscopic surgery including robotic surgery has been increasingly used in reported cases of Spigelian hernia [[13], [14], [15], [16], [17]]. In the present study, we did not use the inexpensive transabdominal preperitoneal approach (TAPP) method, but rather the IPOM method, which we usually use for abdominal wall scar hernias at our hospital, in case 1. In case 2, considering the risk of developing spontaneous bacterial peritonitis (SBP) due to underlying uncompensated liver cirrhosis, we performed a hybrid surgery by inserting a mesh subperitoneally through a laparoscopic incision while viewing the defect. Although there is a possibility that the recurrence rate is lower with the mesh technique than with simple suture closure, the long-term results of the laparoscopic and robotic technique are still unclear, and therefore, the most proficient technique at the institution should be chosen, taking into consideration the size of the defect, history of abdominal surgery, and coexisting disease. Future reports including the long-term recurrence rate are expected.
4. Conclusion
In this study, we experienced two cases of Spigelian hernia treated laparoscopically with 10 cm H2O insufflation. In the treatment of Spigelian hernia, laparoscopy is very useful for diagnosis, because it allows direct observation from the abdominal cavity under insufflation, and its use is recommended for accurate diagnosis and selection of an appropriate approach.
Ethical approval
All procedures performed in the treatment of these patients were in accordance with the ethical standards of our institution and with the ethical guidelines of the Declaration of Helsinki.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Registration of research studies
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
All authors declare that there are no conflicts of interest.
Acknowledgements
I would like to express my gratitude to Dr. Nakatani for his surgical guidance and to Dr. Suganuma for his guidance in writing this paper.
Contributor Information
Yuji Takayama, Email: m02055yt@jichi.ac.jp.
Shinichiro Okada, Email: okada@jichi.ac.jp.
Kensuke Nakatani, Email: kensuken@jadecom.jp.
Toshiyuki Suganuma, Email: toshiyukis@jadecom.jp.
Toshiki Rikiyama, Email: trikiyama@jichi.ac.jp.
References
- 1.Spangen L. Spigelian hernia. World J. Surg. 1989;13:573–580. doi: 10.1007/BF01658873. [DOI] [PubMed] [Google Scholar]
- 2.Khadka P., Sharma Dhakal S.K. Case report of ovary and fallopian tube as content of a Spigelian hernia - a rare entity. Int. J. Surg. Case Rep. 2017;31:206–208. doi: 10.1016/j.ijscr.2017.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cervantes B.Y.H., Lambert R.G., Lopez D.M., Gonzalez M.R., Edwin F. Giant intraparietal inguinal hernia misdiagnosed as spigelian hernia in an old woman. Pan. Afr. Med. J. 2020;36:117. doi: 10.11604/pamj.2020.36.117.21652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cesaro E. “Bulb-like” sign: small bowel closed loop obstruction in incarcerated Spigelian hernia. Radiol. Case Rep. 2021;16:520–523. doi: 10.1016/j.radcr.2020.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Capaccio E., Di Vito L., Derchi L.E. Epiploic appendage torsed within a spigelian hernia: US and CT findings. J. Clin. Ultrasound. 2012;40:310–313. doi: 10.1002/jcu.20872. [DOI] [PubMed] [Google Scholar]
- 6.Jamadar D.A. Sonography of inguinal region hernias. AJR Am. J. Roentgenol. 2006;187:185–190. doi: 10.2214/AJR.05.1813. [DOI] [PubMed] [Google Scholar]
- 7.Anilir E., Buyuker F., Tosun S., Alimoglu O. Incarcerated Spigelian hernia: s rare cause of abdominal wall tender mass. North Clin. Istanb. 2020;7:74–77. doi: 10.14744/nci.2018.09582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirabayashi T., Ueno S. Rare variant of inguinal hernia, interparietal hernia and ipsilateral abdominal ectopic testis, mimicking a spiegelian hernia. Case report. Tokai J. Exp. Clin. Med. 2013;38:77–81. [PubMed] [Google Scholar]
- 9.Larson D.W., Farley D.R. Spigelian hernias: repair and outcome for 81 patients. World J. Surg. 2002;26:1277–1281. doi: 10.1007/s00268-002-6605-0. [DOI] [PubMed] [Google Scholar]
- 10.Agha R.A. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Ndong, A. et al. Strangulated spigelian hernia with necrosis of the caecum, appendix and terminal ileum: an unusual presentation in the elderly. J. Surg. Case Rep. 2020, rjaa115, doi: 10.1093/jscr/rjaa115 (2020). [DOI] [PMC free article] [PubMed]
- 12.Di Furia M. Giant Spigelian hernia presenting as small bowel obstruction: case report and review of literature. Int. J. Surg. Case Rep. 2019;63:118–121. doi: 10.1016/j.ijscr.2019.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson P., Hickey L. Laparoscopic transabdominal preperitoneal (TAPP) groin hernia repair using n-butyl-2-cyanoacrylate (Liquiband(R)Fix8) for mesh fixation and peritoneal closure: learning experience during introduction into clinical practice. Hernia. 2019;23:601–613. doi: 10.1007/s10029-018-1861-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rankin A., Kostusiak M., Sokker A. Spigelian hernia: case series and review of the literature. Visc. Med. 2019;35:133–136. doi: 10.1159/000494280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kirkpatrick T., Zimmerman B., LeBlanc K. Initial experience with robotic hernia repairs: a review of 150 cases. Surg. Technol. Int. 2018;33:139–147. [PubMed] [Google Scholar]
- 16.Orthopoulos G., Kudsi O.Y. Feasibility of robotic-assisted transabdominal preperitoneal ventral hernia repair. J. Laparoendosc. Adv. Surg. Tech. A. 2018;28:434–438. doi: 10.1089/lap.2017.0595. [DOI] [PubMed] [Google Scholar]
- 17.Jamshidian M., Stanek S., Sferra J., Jamil T. Robotic repair of symptomatic Spigelian hernias: a series of three cases and surgical technique review. J. Robot. Surg. 2018;12:557–560. doi: 10.1007/s11701-017-0742-9. [DOI] [PubMed] [Google Scholar]