Abstract
Objective:
To assess concerns and healthcare-related behaviors of patients with autoimmune rheumatic diseases during the COVID-19 pandemic.
Methods:
Adults from the United States with rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), and systemic lupus erythematosus (SLE) from the ArthritisPower Patient-Powered Research Network and CreakyJoints patient community completed surveys. Concerns and behaviors were compared among patients with different autoimmune conditions, disease-modifying anti-rheumatic drug (DMARD) use, and geographic measures of urban status, income, education, and COVID-19 activity.
Results:
Among 1,517 participants (925 RA, 299 PsA, 185 AS, 108 SLE), mean age was 55.1 years, 88.3% were female, and 89.5% white. COVID-19 concerns were similar across the country and were higher in biologic users (p < 0.001). Avoidance of doctor’s office visits (56.6%) or laboratory testing (42.3%) and use of telehealth (29.5%) were more common in urban areas. Among participants on DMARDs without COVID-19 or other respiratory illness, 14.9% stopped a DMARD, with 78.7% of DMARD interruptions not recommended by a physician. DMARD stopping was more common participants with lower socioeconomic status and in participants who avoided an office visit [OR 1.46(1.04–2.04)] or reported lack of telehealth availability [OR 2.26(1.25–4.08)].
Conclusion:
In the early months of the COVID-19 pandemic, patients with RA, PsA, AS, and SLE frequently avoided office visits and laboratory testing. DMARD interruptions commonly occurred without the advice of a physician and were associated with socioeconomic status, office visits, and telehealth availability, highlighting the need for adequate healthcare access and attention to vulnerable populations during the pandemic.
Key Indexing Terms: Spondyloarthritis, rheumatoid arthritis, systemic lupus erythematosus, anti-rheumatic drugs, COVID-19, health behavior
Introduction
COVID-19, caused by SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2)(1,2) may be of particular concern to patients with autoimmune rheumatic diseases such as rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), and systemic lupus erythematosus (SLE). These patients are at increased risk of infections, with immunosuppression and common comorbidities further affecting infection risk.(3)(3,4)
To better understand how the COVID-19 pandemic has affected these patients, the ArthritisPower Patient-Powered Research Network (PPRN) registry (www.ArthritisPower.org)(5) launched a study to capture patient experiences during the pandemic across the United States, hypothesizing that patients with autoimmune diseases would have high levels of concerns about COVID-19 and frequent disruptions in office visits, routine monitoring, and disease modifying anti-rheumatic drug (DMARD) use which would vary geographically.
Methods
Study population
Adults >18 years-old in the ArthritisPower PPRN or CreakyJoints patient community were sent email invitations. The ArthritisPower PPRN(5,6) is a patient-led online registry of patients with inflammatory arthritis and other rheumatic conditions created as a joint venture of the patients and patient advocates of the Global Healthy Living Foundation, the CreakyJoints patient community, and researchers at the University of Alabama at Birmingham. Participants of partnering patient organizations were directed to a landing page (www.rheumcovid.com). Results are presented for surveys completed March 29-May 26, 2020 from participants in the United States with diagnoses of RA, PsA, SpA, or SLE. Participants provided consent and the protocol was approved by the Advarra Institutional Review Board (Protocol 00042873).
Data collection
Participants reported demographics, zip code, comorbidities, rheumatic conditions, and use of DMARDs. For participants indicating multiple autoimmune conditions, a hierarchical approach was taken (SLE > PsA > AS > RA) similar to previous studies.(7)
Participants were asked about their concerns about COVID-19 (5-point Likert scale), respiratory illnesses within the previous 2 weeks, COVID-19 testing/diagnoses, avoidance of office visits or laboratory/diagnostic testing, use and availability of telehealth (“telephone or telehealth visit”) , and DMARD interruptions.
Geographic data
County rural versus urban status was defined using National Center for Health Statistics classification.(8) Tertiles of COVID-19 activity in the patient’s county relative to all other counties in the United States on the survey date were defined using the cumulative cases per capita on that date, weighting counties by population.(9) Zip-code-based median household income and education from the American Community Survey 2014–2018 5-year estimates were also divided into tertiles.(10)
Statistical analysis
Median scores for concerns about COVID-19 were graphed among states/territories with ≥5 respondents. Kruskal-Wallis tests assessed for differences in concerns by geography (9 census divisions), autoimmune disease, biologic/Janus kinase inhibitor (JAKi) use, urban versus rural geography, and by tertiles of zip-code based median household income, education, and county-based COVID-19 cases per capita.
The proportions of participants who had avoided an office visit, avoided testing, had a telehealth visit, or who stopped medications were compared in the same subgroups of interest using univariate logistic regression to assess for statistical differences. DMARD stopping was assessed among participants reporting DMARD use, primarily evaluating patients without a respiratory illness or COVID-19 diagnosis to avoid participants who stopped DMARDs because of illness.
Results
Invitation emails were opened by 14,001 individuals, with 2,895 clicking to access the study and 1,935 completing the baseline survey as of May 26th. Excluding 20 participants outside the United States and 398 without an autoimmune condition of interest left 1,517 participants representing all 50 states and Puerto Rico (Figure 1). Mean age was 55.1, 88.3% of participants were female, and 89.5% were white (Table 1).
Figure 1: Location of participants and concerns about COVID-19.
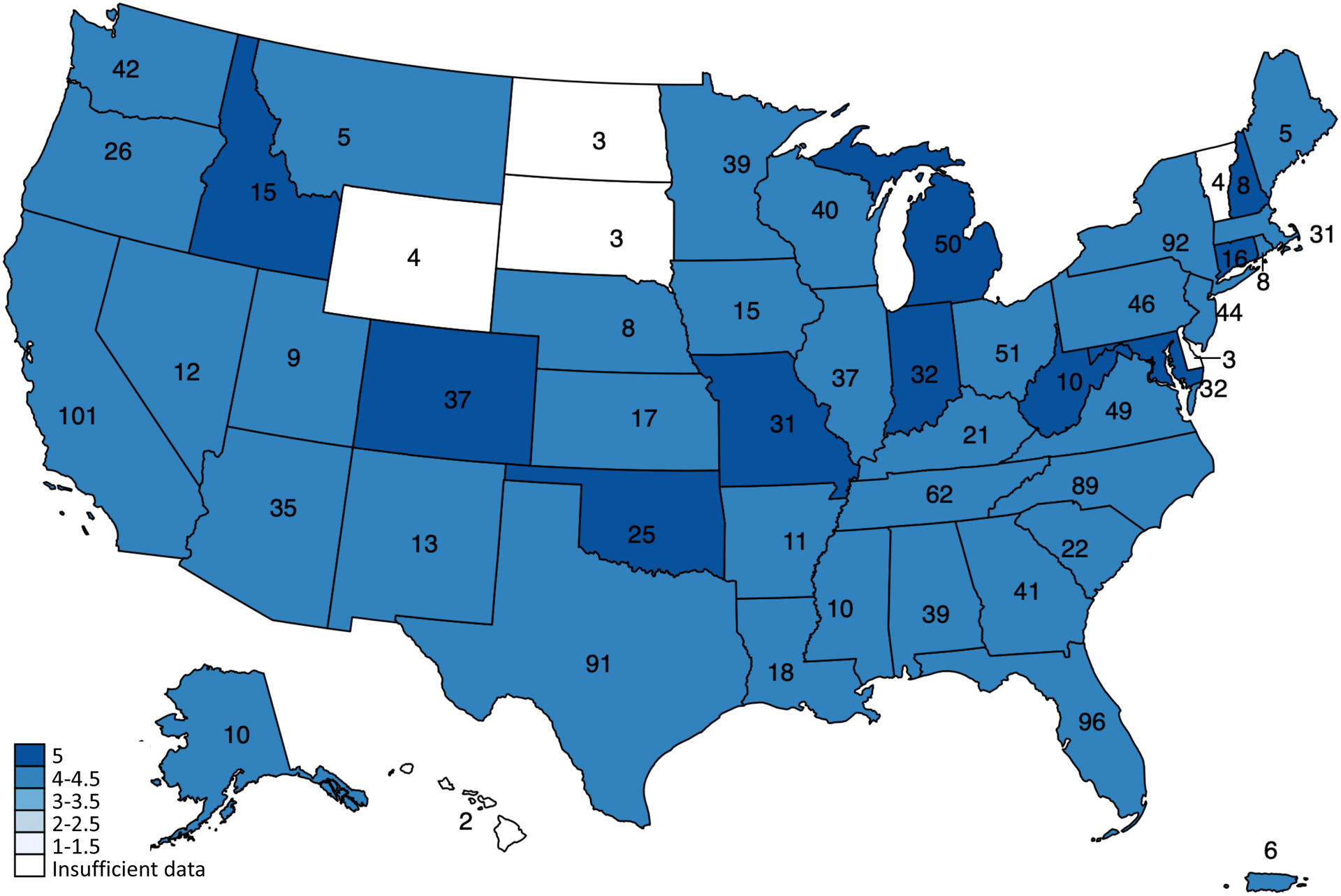
Number of participants by state/territory are shown. Colors represent median participant concern about COVID-19 in each state on a 5-point Likert scale, excluding states with <5 participants.
Table 1:
Participant Demographic and Clinical Characteristics
| N = 1,517 | |
|---|---|
| Age, years | 55.1 +/− 11.7 |
| Female | 1,340 (88.3%) |
| Caucasian | 1,358 (89.5%) |
| Hispanic | 75 (4.9%) |
| Rural | 214/1,454 (14.1%) |
| Autoimmune condition | |
| Rheumatoid arthritis | 925 (61.0%) |
| Psoriatic arthritis | 299 (19.7%) |
| Ankylosing spondylitis | 185 (12.2%) |
| Systemic lupus erythematosus | 108 (7.1%) |
| Medications | |
| Biologic DMARD | 790 (52.1%) |
| Janus kinase inhibitor | 158 (10.4%) |
| Methotrexate | 946 (62.4%) |
| Hydroxychloroquine | 537 (35.4%) |
| Glucocorticoids | 402 (26.5%) |
| Non-steroidal anti-inflammatory drugs | 373 (24.6%) |
| Comorbidities | |
| Hypertension | 621 (40.9%) |
| Lung disease | 518 (34.2%) |
| Diabetes mellitus | 179 (11.8%) |
| Heart disease | 121 (8.0%) |
| Kidney disease | 80 (5.3%) |
| Malignancy | 33 (2.2%) |
| Current smoking | 141 (9.3%) |
| PROMIS Anxiety, T-score* | 59.8 +/− 8.5 |
Number (%) and mean +/− standard deviation shown. Rural status shown among participants with available zip code.
PROMIS Anxiety short form with range of 1–100, U.S. adult population mean=50 and standard deviation=10
DMARD: disease modifying anti-rheumatic drug
A physician diagnosis of COVID-19 was reported by 11 participants (0.7%), with 243 (13.9%) reporting a respiratory illness without a diagnosis of COVID-19. 23.8% of participants who were not ill and 47.9% of participants reporting a respiratory illness wanted to be tested but were not. The most common barriers to testing were that the test was not available (43.0%) or not offered/recommended (36.8%) (Supplemental Table 1).
Concerns about COVID-19
Overall 698 (46.0%) participants were “extremely” and 515 (34.0%) “moderately” concerned about COVID-19, and 803 (52.9%) and 414 (27.3%) noted that their autoimmune disease “extremely” or “moderately” affected their concerns about COVID-19, respectively (Supplemental Figure 1). Levels of concern were high across the United States (Figure 1, Supplemental Figure 2), with no significant difference by geography, urban versus rural, median household income, or education level. Concerns were higher in participants receiving biologics/JAKi (p < 0.01, Supplemental Figure 1).
Impacts on healthcare
Avoidance of doctor’s office visits, laboratory testing, and other testing was reported by 56.6%, 42.3%, and 36.0% of participants, respectively, with higher rates in participants with SLE (all p<0.05). Participants receiving a biologic/JAKi, those in urban or higher COVID-19 activity counties, and participants with greater COVID-19 concerns were more likely to avoid office visits or testing (Table 2, Supplemental Table 2).
Table 2:
Association of patient characteristics with healthcare utilization and medication interruptions
| N | Avoid going to the doctor’s office | Avoid getting laboratory tests | Avoid other tests (e.g. x-ray) |
Had a telehealth visit | Stopped medications** | |
|---|---|---|---|---|---|---|
| All patients | 1,517 | 858 (56.6%) | 641 (42.3%) | 546 (36.0%) | 448 (29.5%) | 169/1,132 (14.9%) |
| Rheumatoid arthritis | 925 | 515 (55.7%) | 377 (40.8%) | 314 (33.9%) | 263 (28.4%) | 97/733 (13.2%) |
| Psoriatic arthritis | 299 | 168 (56.2%) | 124 (41.5%) | 113 (37.8%) | 95 (31.8%) | 41/213 (19.2%)* |
| Ankylosing spondylitis | 185 | 104 (56.2%) | 82 (44.3%) | 68 (36.8%) | 54 (29.2%) | 22/115 (19.1%) |
| SLE | 108 | 71 (65.7%)* | 58 (53.7%)* | 51 (47.2%)* | 36 (33.3%) | 9/71 (12.7%) |
| No biologic or JAKi | 569 | 344 (60.5%) | 261 (45.9%) | 207 (36.4%) | 162 (28.5%) | 33/307 (10.7%) |
| Biologic or JAKi | 948 | 514 (54.2%)* | 380 (40.1%)* | 339 (35.8%) | 286 (30.2%) | 136/825 (16.5%)* |
| Urban county | 1,240 | 718 (57.9%) | 543 (43.8%) | 453 (36.5%) | 381 (30.7%) | 146/933 (15.6%) |
| Rural county | 214 | 108 (50.5%)* | 73 (34.1%)* | 68 (31.8%) | 48 (22.4%)* | 19/156 (12.2%) |
| Median household income of zip code | ||||||
| Lowest tertile | 274 | 147 (53.6%) | 112 (40.9%) | 105 (38.3%) | 77 (28.1%) | 35/200 (17.5%) |
| Middle tertile | 483 | 273 (56.5%) | 200 (41.4%) | 152 (31.5%) | 134 (27.7%) | 39/360 (10.8%)* |
| Highest tertile | 703 | 410 (58.3%) | 308 (43.8%) | 267 (38.0%) | 222 (31.6%) | 92/533 (17.3%) |
| Education of zip code (% greater than high school) | ||||||
| Lowest tertile | 168 | 93 (55.4%) | 73 (43.5%) | 69 (41.1%) | 51 (30.4%) | 25/117 (21.4%) |
| Middle tertile | 445 | 253 (56.9%) | 189 (42.5%) | 155 (34.8%) | 117 (26.3%) | 44/328 (13.4%)* |
| Highest tertile | 850 | 486 (57.2%) | 359 (42.2%) | 301 (35.4%) | 265 (31.2%) | 97/650 (14.9%) |
| County COVID-19 cases per capita | ||||||
| Lowest tertile | 518 | 282 (54.4%) | 200 (38.6%) | 178 (34.4%) | 143 (27.6%) | 54/379 (14.2%) |
| Middle tertile | 480 | 276 (57.5%) | 204 (42.5%) | 159 (33.1%) | 147 (30.6%) | 57/368 (15.5%) |
| Highest tertile | 456 | 268 (58.8%) | 212 (46.5%)* | 184 (40.4%) | 139 (30.5%) | 54/342 (15.8%) |
| Concerned about COVID-19 | ||||||
| Not at all, slightly, or somewhat concerned | 304 | 117 (38.5%) | 86 (28.3%) | 74 (24.3%) | 78 (25.7%) | 19/218 (8.7%) |
| Moderately or extremely concerned | 1,213 | 741 (61.1%)* | 555 (45.8%)* | 472 (38.9%)* | 370 (30.5%) | 150/914 (16.4%)* |
Proportions compared to the reference groups (rheumatoid arthritis, no biologic/JAKi, urban residence, lowest tertile of median household income, education, or COVID-19 cases per capita, and lower COVID-19 concern) using univariate logistic regression (odds ratios and confidence intervals in Supplemental Table 2)
p < 0.05 versus the reference group
Proportion stopping medications is among patients who were on immunosuppression/immunomodulatory therapy and did not report a respiratory illness or diagnosis of COVID-19
SLE: Systemic lupus erythematosus; JAKi: Janus kinase inhibitor
Telehealth visits were reported by 448 (29.5%) participants, more commonly by participants in urban locations (30.8% versus 22.4%, p=0.02) and in areas of higher COVID-19 activity (Table 2). Overall 951 (62.7%) participants reported that their doctor’s office offered telehealth, 474 (31.2%) did not know, and 92 (6.1%) reported that telehealth was not available.
DMARD interruptions
Among participants treated with DMARDs who did not report a respiratory illness or COVID-19 diagnosis, 169/1132 (14.9%) stopped a DMARD. More frequent stopping was associated with biologic/JAKi use, lower education, lower or higher median household income, and greater COVID-19 concerns (Table 2, Supplemental Table 2). Only 21.3% of these DMARD interruptions were recommended by a physician (Supplemental Table 3). Participants who avoided an office visit were more likely stop DMARDs [106/622(17.0%) versus 63/510(12.4%), OR 1.46(1.04–2.04), p=0.03)]. Telehealth use was not associated with stopping DMARDs [OR 1.04(0.72–1.49)], but DMARD stopping was more common among participants who reported that telehealth was not available [17/67(25.4%)] versus those reporting telehealth availability [91/695(13.1%)], OR 2.26(1.25–4.08), p<0.01], with even stronger associations among patients who avoided office visits [OR 3.01(1.43–6.34), p<0.01, Supplemental Table 4].
DMARD interruptions were reported by 48/172 (27.9%) and 7/11 (63.6%) patients reporting respiratory illness or COVID-19 diagnosis, respectively; 56.4% of these interruptions were recommended by a physician (Supplemental Table 3).
Sources of information
The news media (84.4%) and government websites (67.4%) were the most common sources for information about COVID-19 (Supplemental Table 5). Healthcare providers were more commonly a source of information among participants reporting a telehealth visit (63.4% vs. 34.9%, p < 0.001).
Discussion
This study of patients with common autoimmune rheumatic diseases across the United States during the early months of the COVID-19 pandemic found that participants had high levels of concern about COVID-19 and frequently avoided office visits and testing. Of particular concern, approximately 15% had stopped one of their DMARDs, especially patients who avoided office visits and did not have telehealth available.
Most medication interruptions in patients without illnesses occurred without a physician recommendation, similar to previous findings.(11) Although there are limited data on how immunosuppression affects the risk of severe COVID-19(12–14), medication interruptions can risk disease flares and glucocorticoid increases, both associated with infection risk.(15) The American College of Rheumatology recommends continuing DMARDs unless patients are exposed or infected,(16) but these recommendations may not reach or be accepted by patients. In this study, participants most frequently had obtained information about COVID-19 from news sources or government websites, which may not include information specific to patients with autoimmune disease. Participants who had avoided office visits or who reported that telehealth was not available were the most likely to have stopped DMARDs. Higher rates of stopping DMARDs among participants with lower socioeconomic status are concerning and require further investigation.
Participants in urban areas more frequently avoided office visits or testing for their autoimmune condition, and these areas were also the areas with the most telehealth use. These observations could be due to increased concerns or restrictions around clinic office visits, greater availability of or access to healthcare providers, or greater availability of telehealth technology/infrastructure in these areas. Although socioeconomic status was not associated with telehealth use, participants tended to be of higher socioeconomic status and might be more likely to be telehealth users; continued assessment of inequities in access to care and the optimal use of telehealth are important as the pandemic continues.(17)
Several limitations are important to note. Patients who are members of online communities or networks and survey respondents may have different concerns and behaviors than the general population. Respondents were primarily white, and results may differ in racial/ethnic minority populations. Participants self-reported autoimmune and COVID-19 diagnoses, although were specifically asked about physician diagnoses. We could not evaluate whether medication interruptions contributed to disease flares.
In conclusion, participants with autoimmune rheumatic disease across the United States were highly concerned about COVID-19 and frequently avoided office visits or tests. Participants often stopped medications without the advice of a physician, especially those who had missed office visits and did not have telehealth access. Physicians should ask patients about medication concerns and interruptions, proactively contact patients who have missed visits, and ensure patients are aware of available options for accessing care. Continued assessment of disruptions in care, with a particular focus on vulnerable populations, is of critical importance as the pandemic continues.
Supplementary Material
Acknowledgements:
We would like to recognize the partnering patient organizations that are disseminating this survey including Lupus Allied Disease Association (LADA), International Foundation for Autoimmune & Autoinflammatory Arthritis (IFAA), American Bone Health, and Myositis Support and Understanding, Jennifer Walker and Kristine Carandang for reviewing and editing the survey, and the patients who have contributed and continue to participate in this ongoing project.
Sources of support:
MG is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases at the National Institutes of Health (K23 AR073931-01). “The Arthritis and Rheumatic Disease COVID-19 Project” has received sponsorship support specifically from the Patient-Centered Outcomes Institute (PCORI), Eli Lilly and Company, and Janssen Pharmaceutical.
Conflict of Interest:
Michael George has received research support from Bristol-Myers Squibb for unrelated work. Joshua Baker has received consulting fees from Bristol-Myers Squibb and Gilead. Peter Merkel has received consulting feeds from AbbVie, AstraZeneca, Biogen, Boeringher-Ingelheim, Bristol-Myers Squibb, Celgene, ChemoCentryx, CSL Behring, Forbius, Genentech/Roche, Genzyme/Sanofi, GlaxoSmithKline, InflaRx, Insmed, Jannsen, Kiniksa, Magenta, Pfizer, Sparrow, and Talaris and research support from AstraZeneca, Boeringher-Ingelheim, Bristol-Myers Squibb, Celgene, ChemoCentryx, Forbius, Genentech/Roche, Genzyme/Sanofi, GlaxoSmithKline, and InflaRx and royalties from UpToDate. Maria Danila has received consulting fees from Amgen, Novartis, and Sanofi Regeneron and research support from Genentech, Pfizer, Boehringer, and Horizon for unrelated work. Jeffrey Curtis has received consulting fees from AbbVie, Amgen, Bristol-Myers Squibb, Corrona, Janssen, Lilly, Myriad, Pfizer, Regeneron, Roche, and UCB and research support from AbbVie, Amgen, Bristol-Myers Squibb, Corrona, Janssen, Lilly, Myriad, Pfizer, Regeneron, Roche, UCB. David Curtis, Kelly Gavigan, W Benjamin Nowell, and Shilpa Venkatachalam have no personal conflicts of interests to disclose and are employees of the Global Healthy Living Foundation (GHLF). GHLF receives grants, sponsorships and contracts from pharmaceutical manufacturers and private foundations. A full list of GHLF funders is publicly available here: https://www.ghlf.org/our-partners/.
References
- 1.Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature Nature Publishing Group; 2020;579:270–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020; [DOI] [PubMed] [Google Scholar]
- 3.Listing J, Gerhold K, Zink A. The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatol Oxf Engl 2013;52:53–61. [DOI] [PubMed] [Google Scholar]
- 4.Ogdie A, Maliha S, Shin D, Love TJ, Baker J, Jiang Y, et al. Cause-specific mortality in patients with psoriatic arthritis and rheumatoid arthritis. Rheumatol Oxf Engl 2017;56:907–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patient-Centered Outcomes Research Institute. ArthritisPower (ARthritis Partnership with Comparative Effectiveness Researchers). Available at: https://www.pcori.org/research-results/2015/arthritispower-arthritis-partnership-comparative-effectiveness-researchers. Accessed May 28, 2020.
- 6.Nowell WB, Curtis D, Thai M, Wiedmeyer C, Gavigan K, Venkatachalam S, et al. Digital Interventions to Build a Patient Registry for Rheumatology Research. Rheum Dis Clin North Am 2019;45:173–86. [DOI] [PubMed] [Google Scholar]
- 7.Ogdie A, Yu Y, Haynes K, Love TJ, Maliha S, Jiang Y, et al. Risk of Major Cardiovascular Events in Patients with Psoriatic Arthritis, Psoriasis and Rheumatoid Arthritis: A population-based cohort study. Ann Rheum Dis 2015;74:326–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. Urban Rural Classification Scheme for Counties. 2019. Available at: https://www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed May 26, 2020.
- 9.USAFacts. US Coronavirus Cases by County. Available at: https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/. Accessed May 26, 2020.
- 10.U.S. Census Bureau. American Community Survey 2014–2018 5-Year Estimates. Accessed through Social Explorer 2020. New York City, NY. Available at: Accessed through http://www.socialexplorer.com/pub/reportdata/HtmlResults.aspx?reportid=R12543316. Accessed May 5, 2020. [Google Scholar]
- 11.Michaud K, Wipfler K, Shaw Y, Simon TA, Cornish A, England BR, et al. Experiences of Patients With Rheumatic Diseases in the United States During Early Days of the COVID-19 Pandemic. ACR Open Rheumatol 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haberman R, Axelrad J, Chen A, Castillo R, Yan D, Izmirly P, et al. Covid-19 in Immune-Mediated Inflammatory Diseases - Case Series from New York. N Engl J Med 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Favalli EG, Ingegnoli F, De Lucia O, Cincinelli G, Cimaz R, Caporali R. COVID-19 infection and rheumatoid arthritis: Faraway, so close! Autoimmun Rev 2020;19:102523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gianfrancesco M, Hyrich KL, Al-Adely S, Carmona L, Danila MI, Gossec L, et al. Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann Rheum Dis 2020;79:859–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Au K, Reed G, Curtis JR, Kremer JM, Greenberg JD, Strand V, et al. High disease activity is associated with an increased risk of infection in patients with rheumatoid arthritis. Ann Rheum Dis 2011;70:785–91. [DOI] [PubMed] [Google Scholar]
- 16.Mikuls TR, Johnson SR, Fraenkel L, Arasaratnam RJ, Baden LR, Bermas BL, et al. American College of Rheumatology Guidance for the Management of Adult Patients with Rheumatic Disease During the COVID-19 Pandemic. Arthritis Rheumatol Hoboken NJ 2020; [DOI] [PubMed] [Google Scholar]
- 17.Feldman CH, Ramsey‐Goldman R. Widening Disparities Among Patients With Rheumatic Diseases in the COVID-19 Era: An Urgent Call to Action. Arthritis Rheumatol 2020;72:1409–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


