Abstract
Purpose:
While mentorship is described extensively in academic medical literature, there are few descriptions of mentorship specific to radiation oncology. The goal of the current study is to investigate the state of mentorship in radiation oncology through a scoping review of the literature.
Methods and Materials:
A search protocol was defined according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Predefined search terms and medical subject headings were used to search PubMed for English Language articles published after January 1, 1990 on mentorship in radiation oncology. Additionally, in-press articles from major radiation oncology and medical education journals were searched. Three reviewers determined article eligibility. Included articles were classified based on predefined evaluation criteria.
Results:
14 publications from 2008–2019 met inclusion criteria. The most commonly described form of mentorship was the dyad (64.3%), followed by team (14.3%), and peer (7.1%); two articles did not specify mentorship type (14.3%). The most commonly mentored participants were residents (35.7%), followed by medical students (35.7%) and attendings (21.4%); one study included participants of all levels (7.1%). Thirteen studies (92.9%) identified an experimental study design, most of which were cross-sectional (42.9%), followed by cohort studies (28.6%) and before/after (21.4%). Median sample size, reported in 12 of 13 experimental studies, was 132 (coefficient of variation 1.06. Although outcomes varied widely, the majority described successful implementation of mentorship initiatives with high levels of participant satisfaction.
Conclusion:
While few initiatives are currently reported, the present study suggests that these initiatives are successful in promoting career development and increasing professional satisfaction. The interventions overwhelmingly described mentorship dyads; other forms of mentorship are either less common or understudied. Limitations included interventions not being evaluated in a controlled setting, and many were assessed using surveys with low response rates. This review highlights rich opportunities for future scholarship to develop, evaluate, and disseminate radiation oncology mentorship initiatives.
Keywords: radiation oncology, mentorship
Introduction
Mentorship is an effective tool for career advancement with potential benefits including enhanced productivity, accelerated promotion, and higher compensation (1). The definition of mentorship is nuanced and should be distinguished from similar concepts such as teaching, sponsorship, leadership, apprenticeship, or advisorship, with the understanding that mentorship can have variable overlap with the aforementioned concepts. Healy and Welchert define mentorship as “a dynamic, reciprocal relationship between an advanced career incumbent (mentor) and a beginner (protégé), aimed at promoting the development of both” (2).
The classic mentorship dynamic of the dyad, consisting of a single senior mentor and a single junior mentee, is the oldest and most well-known form of mentorship (3). Several other forms of mentorship exist as well, including teams and peer groups (Table 1) (4–7). Mentorship in medicine has been studied extensively in other fields, with benefits including increased mentee satisfaction, faster promotion, and improved job retention (8–11). Mentors have also reported benefits such as increased job satisfaction, improved teaching skills, and increased sense of departmental comradery (12). Formal mentorship programs have also been shown to be cost-effective for academic institutions as improved faculty retention achieved savings in faculty recruitment greater than the cost of the mentorship program (13). To date, little has been published regarding the state of mentorship in radiation oncology, a medical specialty that relies heavily on the apprenticeship model and self-directed learning.
Table 1.
Types of mentorship
| Type of Mentorship | Description |
|---|---|
| Dyad | A single senior mentor works with a single junior mentee. |
| Multiple Dyad | Multiple senior mentors work with a single mentee on different topics. |
| Functional Dyad | A single senior mentor works with the mentee on one topic. |
| Speed Mentoring | Mentors and mentees meet for a brief one-time event. |
| Distance Mentoring | All mentee/mentor communication is made over a distance. |
| Team Mentorship | Also called committee mentoring, in which multiple senior mentors work with a single mentee, no mentor is limited to a single topic, and there is interaction among the different mentors. |
| Peer Mentorship | Peers of approximately the same rank fill both the mentee and mentor roles. |
| Facilitated Peer Mentorship | A senior mentor oversees Peer Mentorship. |
Given the importance of mentorship in the medical profession, there is value in understanding the state of mentorship initiatives in radiation oncology. The goal of this study is to consolidate the existing radiation oncology mentorship literature in order to help with the development, evaluation, and dissemination of radiation oncology mentorship initiatives and to help identify areas of improvement.
Methods and Materials
A scoping review protocol was defined using Preferred Reporting Items for Systematic Reviews and Meta Analyses extension for scoping reviews (PRISMA-ScR) guidelines and the PICOS (population, intervention, comparison, outcome, and setting) framework was used to evaluate individual articles for inclusion (14–16). Scoping reviews are used, “to identify the types of available evidence in a given field.”(17). The populations defined were medical students, radiation oncology residents, radiation oncology fellows, and attending physicians. Interventions were the mentorship initiative. If present, separate groups of individuals that did not receive mentorship were identified as “control groups.” The outcome was the reported result from the intervention. Only articles in the English language (including translated articles) published between January 1, 1990 and January 22, 2020 were considered. This start date was chosen as it approximates the modern era of radiation oncology with routine use of three-dimensional imaging for treatment planning and intensity-modulated radiation therapy (1). Included articles were required to: (A) meet the definition of mentorship above; (B) describe a mentorship initiative related to career development (as opposed to a particular skill); and (C) describe radiation oncologists directly mentoring radiation oncologists or trainees (2). Excluded articles included letters to the editor, comments, interviews, or meeting abstracts.
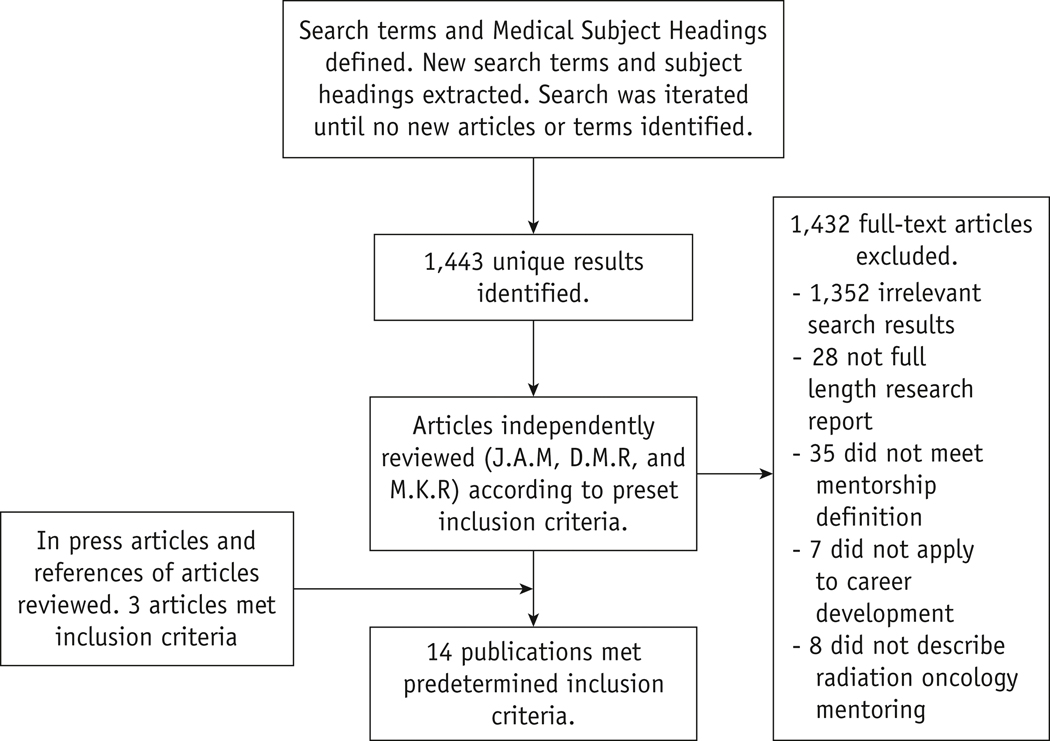
PubMed was queried for full text peer-reviewed publications meeting these criteria using predefined search terms and Medical Subject Headings. New search terms and subject headings were extracted from the results of this query, and the search was repeated iteratively until no new articles or search terms were identified. The final list of search terms is shown in Supplemental Table 1. Additionally, major radiation oncology and medical education journals were searched for in-press articles (Supplemental Table 2). Articles that met inclusion criteria were identified and included. Three reviewers (J.A.M., D.M.R., and M.K.R.) independently determined article eligibility through unanimous consensus. Publications were initially screened by title and abstract alone; for cases in which inclusion status was unclear based on this information, the full-text article was downloaded and evaluated.
Articles were coded for predetermined parameters of interest including study year, country of publication by first author affiliation, type of journal (medical education or oncology research), study design (cohort, before/after, cross sectional), study size of experimental group, type of mentored participant (attendings, residents, or medical students), type of mentorship (Table 1), program components, and method of evaluation. Additionally, outcomes (both professional and personal) for any interventions were summarized, and limitations to each study were noted. PRISMA-ScR recommendations for assessing risk of bias were completed during analysis. Based on scoping review methodology meta-analysis was not conducted (15,16)Institutional review board approval was not required for this study.
Results
The initial search yielded 1443 articles of which 1432 did not meet inclusion criteria. Additionally, three in-press articles were identified in the journals searched. In all, thirteen publications from 2008–2019 were included (see Flow Diagram in Figure 1). No articles prior to 2008 met the inclusion criteria. Individual studies are summarized in Table 2 (10,18–30). Findings by data type are shown in Table 3. The most commonly described form of mentorship was the dyad (9 of 14, 64.3%), followed by team (2 of 14, 14.3%), and peer (1 of 14, 7.1%); two articles did not specify mentorship type (2 of 14, 14.3%). Publication country of origin by first author affiliation most commonly was the United States (11 of 14, 78.6%), and the remainder were from Canada (3 of 14, 21.4%). The majority of journal types were oncology research (12 of 14, 85.7%), while two were medical education (2 of 14, 14.3%).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) flow diagram of systematic review protocol
Table 2.
Publications meeting inclusion criteria
| Author(s) | Study Year | Country | Study Design | Study Size | Mentored Participant | Form of Mentorship | Program Components | Method of Evaluation | Outcomes | Limitations |
|---|---|---|---|---|---|---|---|---|---|---|
| Boyd et al. | 2019 | USA | Cross- sectional | 22 | Medical students | Dyad | This initiative pairs students with radiation oncology faculty for clinical or research mentorship | Survey | Seventeen (77.3%) participants reported that the mentorship program strongly affected their career choice. All respondents reported the mentorship program as effective or very effective. | Single institution, possibility of recall bias |
| Croke et al. | 2019 | Canada | Cross- sectional | 20 | Residents | Unspecified | Semi-structured interviews | Inductive thematic analysis | Four major themes emerged: (i) the perceived experiences of residents and faculty with mentorship, (ii) the evolution of mentorship needs during residency training, (iii) the mechanisms of creating mentorship relationships and (iv) peer mentorship | Possibility of selection bias, non-generalizable results |
| Lee et al. | 2019 | USA | Cohort | 532 | All groups | Dyad | 2014–2015 ASTRO meeting abstracts were evaluated for gender of presenting author and senior author | Multivariable logistic regression model evaluated factors associated with subsequent higher-impact publications | FM pairings (OR 2.48; 95% confidence interval, 1.32–4.66) and MF pairings (OR 2.38; 95% confidence interval, 1.19–4.77) had higher odds of high-impact publication than MM pairings. No significant difference in outcome between FF and MM pairings | Inability to control for confounders |
| Sayan et al. | 2019 | USA | Cross- sectional | 126 | Residents | Unspecified | Unspecified | MEMeQ survey | Participation in formal mentorship program led to higher satisfaction with mentoring (90% vs. 9%, p < 0.001). 38% of residents were either satisfied/very satisfied with their mentoring experience, while 49% of residents were unsatisfied/very unsatisfied | Small sample size, geographic restrictions |
| Efstathiou et al. | 2018 | USA | Cohort | 114 | Attendings | Dyad | Junior attendings were assigned mentor pairs, completed three formal training sessions, and had informal meetings | Survey before and after program completion. Long-term retention, promotion, and funding data | Mentees demonstrated an increase in satisfaction from baseline in five of seven domains. At long-term follow up mentees were more like than controls to hold senior faculty positions (47% vs 13%; p = 0.030) despite no initial difference | Mentees from two different specialties (radiation oncology and anesthesia); Possibility of control group response bias |
| Ko and Kimple | 2018 | USA | Before/ After | Unspecified | Residents | Dyad | Residents discussed completed individual development questionnaire with mentor | Survey before and after discussion | Completion was associated with an increase in confidence in knowing how to achieve career goals, develop strengths, and grow the mentor-mentee relationship | Small sample size resulted in no statistical analysis |
| Lalani et al. | 2018 | Canada | Cross- sectional | 221 | Attendings | Peer | Unspecified | Survey | 56% indicated difficulty in identifying role models. Only 51% reported having a primary mentor. 49% of respondents reported being very or somewhat satisfied with their mentorship experiences | Possibility of reporting/ recall bias, no longitudinal follow up |
| Engel et al. | 2017 | USA | Before/ After | 49 | Residents | Dyad | Residents and attendings were paired then met at a national conference | Post survey | Nearly all responders (97% of residents and 95% of attendings) rated the overall program as a 4 or 5 out of 5. 64% and 73% of residents and attendings preferred in-person meetings. 94% of residents and 77% of attendings planned on continuing a professional correspondence | |
| Sura et al. | 2017 | USA | Before/ After | 23 | Medical students | Team | Webinar on applying to radiation oncology | Pre/post webinar survey | Areas of medical student concern included minimum statistics to match, importance of research, how to match in specific location, and the importance of away rotations | Low response rate |
| Dhami et al. | 2016 | USA | Cross- sectional | 150 | Residents | Dyad | Unspecified | Survey | 87% felt mentorship was critical for successful training. 53% had a current mentor. 77% of those in a formal mentorship program found it to be helpful. Areas of benefit were career development (83%), work life balance (70%), and research (75%). In those without a mentor areas of disadvantage were research (47%), job search (45%), and networking (40%). | Low survey response rate (25%) |
| Hirsch et al. | 2015 | USA | Cohort | 76 | Medical students | Dyad | Mentees were organized by mentorship tracks, which included a clinical track and a research track | Survey | Of 58 alumni, 17 (29.3%) applied to and matched into radiation oncology residencies. Alumni of both the research and the clinical track were 5.76 (p< .01) times more likely to enter a radiation oncology residency program than the average single-track alumnus | Possibility of response bias |
| Holliday et al. | 2014 | USA | Cross- sectional | 158 | Attendings | Dyad | Surveyed academic radiation oncologists | Participants were surveyed on having a mentor, and research productivity metrics such as number of publications and h-index | 96/158 surveyed had a mentor and Faculty with a mentor had higher numbers of publications, citations, h- and m-indices | Low response rate with possibility of selection bias in more research productive individuals |
| DeNunzio et al. | 2010 | USA | n/a | n/a | Medical Students | Dyad | Mentorship in radiation oncology can be initiated in traditional classroom courses, and through other ways such as student interest groups and summer programs | |||
| Barrett et al. | 2008 | Canada | Cohort | 97 | Medical Students | Team | The Ivan H. Smith Memorial Studentship program connects medical students with clinical and research mentorship in oncology and radiation oncology | Survey | Between 1971 and 1981, 97 recipients 4 entered radiation oncology practice (4.12%) compared to 12 of 1683 (0.7%) post MD-trainees who went on to complete radiation oncology training in 1989. |
Table 3.
Article characteristics.
| number of articles n (%) | |
|---|---|
| Total Articles | 14 (100) |
| Type of Mentorship | |
| Dyad | 9 (64.3) |
| Team | 2 (14.3) |
| Peer | 1 (7.1) |
| Unspecified | 2 ) |
| Mentored participant | |
| Residents | 5 (35.7) |
| Medical students | 5 (35.7) |
| Attendings | 3 (21.4) |
| All levels | 1 (7.1) |
| Method of Evaluation | |
| Survey | 9 (64.3) |
| Productivity metrics | 2 (14.3) |
| Survey and productivity metrics | 1 (7.1) |
| Interviews | 1 (7.1) |
| None | 1 (7.1) |
| Outcomes | |
| Objective | 4 (28.6) |
| Subjective | 8 (57.1) |
| Both | 1 (7.1) |
| None | 1 (7.1) |
Thirteen studies (92.9%) targeted a specific training level for the mentee. The most commonly mentored participants were residents (5 of 14, 35.7%), and medical students (5 of 14, 35.7%) followed by attendings (3 of 14, 21.4%). In one study (7.1%) of the mentored participants included members from all the above groups (first author abstract presenters at a national conference) (21).
Thirteen of fourteen studies (92.9%) described the experimental study design. Mentorship program components varied widely and are reported in Table 2. Methods of program evaluation most commonly included surveys (10 of 13, 76.9%), mentee productivity metrics (2 of 13, 15.4%), and semi-structured interviews (1 of 13, 7.7%). Most study designs were cross-sectional (6 of 13, 46.2%), followed by cohort (4 of 13, 30.8%), and before/after (3 of 13, 23.1%). Median sample size, reported in 12 of 13 experimental studies, was 132(coefficient of variation 1.06).
Outcomes were described in all thirteen experimental studies. Subjective outcomes alone were most frequently reported (8 of 13, 57.1%), followed by objective outcomes only (4 of 13, 28.6%) and both subjective and objective outcomes (1 of 13, 7.1%). Subjective outcomes broadly were reported by satisfaction ratings on Likert-type scales. Mentee satisfaction was reported by six of the studies, of which all found that most mentees were either “satisfied” or “very satisfied” with their mentorship experiences (10,18,19,22,23,26). The objective outcomes reported were increased research productivity (measured by number of publications, citations, h- and m-indices, higher odds of publication in a high impact journal (measured by journal impact factor), greater likelihood to hold a senior faculty position, and greater likelihood that a medical student mentee would enter radiation oncology residency.
Four of the studies compared individuals enrolled in a formal mentorship program as a “mentee” to individuals either not enrolled in a formal program or without a current mentor (10,19,22,26). Mentorship satisfaction was higher among those participating in formal mentorship activities compared to those participating in informal mentorship activities (three studies report p<0.05) (10,22,26). Areas of perceived benefit among those in formal mentorship activities included increased confidence in achieving career goals, and improved research productivity. Greater satisfaction with work/life balance was reported by three of the studies (10,19,26). While these studies did not specify what areas of work/life balance mentees were more satisfied in, an additional study identified areas of work/life improvement mentees desired from their mentorship experience, citing balancing work/life responsibilities specifically mentioning family planning as a challenge for many resident mentees (20). Several studies of formal mentorship programs also spoke of common themes that emerged through mentee feedback, including elevating mentee enthusiasm, increasing academic productivity, promoting program satisfaction, and furthering career goals (10,18–20,22,23). Despite this apparent efficacy, however, five studies (35.7%) described mentee dissatisfaction with their mentorship experiences (19,20,22,24,26). Four of the studies described residents as the mentored participant while one described attendings, both groups showing similar levels of dissatisfaction with mentorship experiences, around 50% of those surveyed. Common explanations for mentee dissatisfaction included difficulty of finding a mentor, lack of suitability of mentor, inadequate interest or commitment from a mentor, inexperienced mentors, insufficient time for mentorship activities, and lack of formal mentorship interactions (20,22,24,26).
Discussion
This study is the first scoping review of mentorship initiatives in radiation oncology, identifying fourteen publications that meet predefined search criteria and elucidate successes and barriers to mentorship within the field. The majority of identified studies highlight that mentorship initiatives increase mentee enthusiasm, research productivity, and overall program satisfaction. This is consistent with the literature on mentorship initiatives in other fields of medicine (8–13). Many (35.7%) cite barriers such as difficulty with finding a mentor, inadequate interest from mentor, lack of mentor experience, and time constraints as barriers to effective mentorship. Participation in a formal mentorship program was associated with higher rates of satisfaction, potentially due to removal of these barriers by, for example, facilitating mentee-mentor connections, providing dedicated time for mentorship activities, and formal departmental training for new mentors. Some areas of increased satisfaction lacked specifics, such as increased work/life balance. Further studies could help identify specific areas of work/life balance improvement. Shortcomings in formalized mentorship programs were appreciated when one party was perceived as being disinterested or insufficiently committed to the program (20,26).
While the majority of identified studies based their mentorship initiatives on the dyad model, this review highlights the potential for employment of diverse mentorship types to achieve different goals. In one study in which dyad pairs were formed at a national conference, the number of interested mentees exceeded the number of available mentors leading to some mentors taking on multiple mentees, and some potential mentees being unable to participate (24). With increasing limitations on administrative or academic time for physicians, there has been increased reliance on facilitated peer group mentorship to potentially circumvent limitations of mentor time and experience (21,31). Peer Mentorship is another form of mentorship that circumvents these limitations. Lalani et al. reported Peer Mentorship among 63% of surveyed early career attendings; it is unclear how prevalent it is among other levels of trainees (19). Peer mentorship may be an underutilized technique that could be relatively easily employed by academic institutions.
Development of multi-institutional collaborative mentorship programs might enhance the ability of individuals to identify potential mentors and provide a framework for mentor-mentee introduction. Such initiatives would be particularly valuable in smaller programs in which mentorship opportunities with in-house faculty as well as exposure to outside faculty may be more limited. For a list of mentorship opportunities see Supplementary Table 3. In the era of the coronavirus there have been many additional multi-institutional mentorship initiatives, particularly focusing on Distance Mentorship. One such initiative is the Virtual Visiting Professor Network seeking to connect radiation oncology residents and the rest of the radiation oncology community with medical education. The platform features a “visiting professor” giving a talk each month (32). Other initiatives are aimed at medical students such as virtual away rotations where students can learn about the field. To give added didactics for medical students, there is the Radiation Oncology Virtual Education Rotation (ROVER): Multi-Institutional Teaching Sessions (33). This series of case-based sessions is aimed to review disease sites and treatment. These virtual experiences provide additional avenues of mentorship engagement in a time when in person meetings are not possible. Additional initiatives are currently underway at Institutions across the country including additional virtual options that have arisen due to the COVID pandemic. The authors believe that this is a topic that will continue to be of interest to the radiation oncology community and we look forward to continued investigation in this area.
One area the current literature does not address is mentorship for radiation oncologists in private practice or employed at a nonacademic hospital. Evidence from the general medical literature suggests that clinical faculty struggle more with identifying mentorship than research faculty which coincides with the observed lack of clinical mentorship in the radiation oncology literature (34). Radiation oncologists in these settings account for approximately 60% of the workforce, and many private practice settings are small, resulting in challenges to traditional (dyad) forms of mentorship (35). Anecdotal evidence suggests that other mentorship models such as peer mentoring and distance mentoring might already be in use informally, presenting potential opportunities to better support faculty through formalizing opportunities outside the traditional academic environment.
Another gap identified in this review is formal mentorship programs for individuals traditionally underrepresented in radiation oncology. It is well documented that radiation oncology suffers from a lack of diversity in underrepresented minorities and a gender disparity (35–40). In other fields, mentorship has been used as a tool to increase diversity (41,42). These articles report that mentorship can target underrepresented students at multiple points along the pipeline to the medical specialty. For premedical students, mentorship programs such as informal meetings at career fairs and associations with pre-medical minority student groups can increase the number of competitive medical school applicants (41). For medical students mentors connect students early on with exposure to the field and opportunities to build a competitive residency application. They also have the added benefit to provide a conductive outlet for students to speak up, and ask questions (41). In radiation oncology the benefits of mentorship on medical students are clear. Students who had multiple mentors (research and clinical) were more likely to match into radiation oncology than those without multiple mentors, possibly due to increased research opportunities, and exposure to the field (18). The lack of gender and racial diversity in radiation oncology can be best addressed by increasing diversity in the pipeline, and mentorship is one of many ways to connect students to a rewarding field.
Most of the identified articles described study limitations. A majority of publications were cross-sectional studies and relied on self-report, with potential for selection and response bias given lower rates of overall response. Of the other study designs (cohort and before/after studies), most did not have a control group, and one was not able to include any statistical analysis due to its small sample size. Longitudinal follow-up was also limited in most studies. There is a need for future studies to prospectively implement and evaluate mentorship programs to ascertain the long-term benefits such as the one being conducted by Efstathiou et al. at Massachusetts General Hospital, where junior faculty mentees and their senior mentors participated in a formal mentorship program consisting of regular meetings and training sessions, after which long term outcomes (retention, promotion, and funding data) are tracked for mentorship program graduates after which long term outcomes (retention, promotion, and funding data) are tracked for mentorship program graduates (10). Furthermore, multi-institutional collaboration could increase sample size for statistical analyses and bolster the generalizability of findings.
This current study itself may be limited due to the review process and study design. It is possible that some applicable studies were not included, as the search was limited to PubMed, even though broad search criteria were used. This could be due to incomplete search terms or reviewer bias. The search was defined for formal mentorship initiatives, and mentorship can occur in many situations that are not explicitly intended to foster mentorship. Any study that was not identified as a mentorship initiative would not have been included. The search was limited to English language publications and could have missed any non-English language publications in the search. The identified body of literature was limited in number, and may also be subject to publication bias, as interventions are more likely to be published if they depict successful outcomes.
Conclusions
The goal of this study was to perform a scoping review of mentorship initiatives in radiation oncology to develop, evaluate, and disseminate radiation oncology mentorship initiatives. The identified interventions overwhelmingly focused on the dyad mentorship model. As such, further research is warranted to investigate the utility of other forms of mentorship to overcome identified barriers to mentorship, including time and experience. Many of the identified studies were hampered by small sample size; this limitation could be mitigated through the development of multi-institutional collaborative projects. Overall, mentorship appears to be exceptionally valuable in the field of radiation oncology, but remains understudied. This review provides a foundation for future scholarship into this important topic.
Supplementary Material
Acknowledgements:
This work was supported in part by the University of Wisconsin Carbone Cancer Center Support Grant NIH (P30 CA014520).
Dr. Golden reports funding from the National Institutes of Health, Radiation Oncology Institute, and Bucksbaum Institute for Clinical Excellence. He has a financial interest in RadOncQuestions LLC and HemOncReview LLC. Dr. Gillespie reports receiving grant funding from eCountour.org. Dr. Kimple was supported in part by the University of Wisconsin Carbone Cancer Center Support Grant NIH (P30 CA014520).
Footnotes
Conflicts of interest: No other authors report potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Scandura TA. Mentorship and career mobility: An empirical investigation. J Organ Behav. 1992;13(2):169–74. [Google Scholar]
- 2.Healy CC, Welchert AJ. Mentoring relations: A definition to advance research and practice. Educ Res. 1990;19(9):17–21. [Google Scholar]
- 3.Chopra V, Arora VM, Saint S. Will you be my mentor?—Four archetypes to help mentees succeed in academic medicine. JAMA Intern Med. 2018;178(2):175–6. [DOI] [PubMed] [Google Scholar]
- 4.Thorndyke LE, Gusic ME, Milner RJ. Functional mentoring: a practical approach with multilevel outcomes. J Contin Educ Health Prof. 2008;28(3):157–64. [DOI] [PubMed] [Google Scholar]
- 5.Geraci SA, Thigpen SC. A review of mentoring in academic medicine. Am J Med Sci. 2017;353(2):151–7. [DOI] [PubMed] [Google Scholar]
- 6.Sambunjak D, Straus SE, Marušić A. Mentoring in academic medicine: a systematic review. Jama. 2006;296(9):1103–15. [DOI] [PubMed] [Google Scholar]
- 7.Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: a systematic review. Acad Med. 2013;88(7):1029–37. [DOI] [PubMed] [Google Scholar]
- 8.Kostrubiak DE, Kwon M, Lee J, Flug JA, Hoffmann JC, Moshiri M, et al. Mentorship in Radiology. Curr Probl Diagn Radiol. 2017. October;46(5):385–90. [DOI] [PubMed] [Google Scholar]
- 9.Entezami P, Franzblau LE, Chung KC. Mentorship in surgical training: a systematic review. Hand. 2012;7(1):30–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Efstathiou JA, Drumm MR, Paly JP, Lawton DM, O’Neill RM, Niemierko A, et al. Long-term impact of a faculty mentoring program in academic medicine. PloS One. 2018;13(11):e0207634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morrison LJ, Lorens E, Bandiera G, Liles WC, Lee L, Hyland R, et al. Impact of a formal mentoring program on academic promotion of Department of Medicine faculty: a comparative study. Med Teach. 2014;36(7):608–14. [DOI] [PubMed] [Google Scholar]
- 12.Tracy EE, Jagsi R, Starr R, Tarbell NJ. Outcomes of a pilot faculty mentoring program. Am J Obstet Gynecol. 2004;191(6):1846–50. [DOI] [PubMed] [Google Scholar]
- 13.Wingard DL, Garman KA, Reznik V. Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine. Acad Med. 2004;79(10):S9–11. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018. October 2;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 16.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005. February 1;8(1):19–32. [Google Scholar]
- 17.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018. November 19;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyd GH, Rand AE, DeNunzio NJ, Agarwal A, Hirsch AE. The radiation oncology mentorship initiative: analysis of a formal mentoring initiative for medical students interested in radiation oncology . J Cancer Educ. 2019;1–4. [DOI] [PubMed] [Google Scholar]
- 19.Lalani N, Griffith KA, Jones RD, Spratt DE, Croke J, Jagsi R. Mentorship experiences of early-career academic radiation oncologists in North America. Int J Radiat Oncol Biol Phys. 2018;101(3):732–40. [DOI] [PubMed] [Google Scholar]
- 20.Croke J, Milne E, Bezjak A, Millar BA, Giuliani M, Heeneman S. Mentorship Needs for Radiation Oncology Residents: Implications for Programme Design. Clin Oncol R Coll Radiol G B. 2020. April;32(4):e119–25. [DOI] [PubMed] [Google Scholar]
- 21.Lee A, Albert A, Griffith K, Evans S, Rahimy E, Park HS, et al. Mentorship in Radiation Oncology: Role of Gender Diversity in Abstract Presenting and Senior Author Dyads on Subsequent High-Impact Publications. Adv Radiat Oncol. 2020. March 1;5(2):292–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sayan M, Ohri N, Lee A, Abou Yehia Z, Gupta A, Byun J, et al. The Impact of Formal Mentorship Programs on Mentorship Experience Among Radiation Oncology Residents From the Northeast. Front Oncol. 2019;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ko HC, Kimple RJ. The resident individual development plan as a guide for radiation oncology mentorship. Int J Radiat Oncol Biol Phys. 2018;101(4):786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Engel S, Lischalk JW, Barry P, Hopkins S, Welsh JS, Fernandez E, et al. Radiation Oncology Resident Mentorship: Results of a Resident-Coordinated Mentorship Program. J Am Coll Radiol JACR. 2017;14(12):1607–10. [DOI] [PubMed] [Google Scholar]
- 25.Sura K, Lischalk JW, Leckie J, Grills IS, Vapiwala N. Applying for radiation oncology residency: webinar-based medical student mentorship outreach. Int J Radiat Oncol Biol Phys. 2017;97(1):11–2. [DOI] [PubMed] [Google Scholar]
- 26.Dhami G, Gao W, Gensheimer MF, Trister AD, Kane G, Zeng J. Mentorship programs in radiation oncology residency training programs: a critical unmet need. Int J Radiat Oncol Biol Phys. 2016;94(1):27–30. [DOI] [PubMed] [Google Scholar]
- 27.Hirsch AE, Agarwal A, Rand AE, DeNunzio NJ, Patel KR, Truong MT, et al. Medical student mentorship in radiation oncology at a single academic institution: a 10-year analysis. Pract Radiat Oncol. 2015;5(3):e163–8. [DOI] [PubMed] [Google Scholar]
- 28.Holliday E, Jagsi R, Thomas C, Wilson L, Fuller C. Standing on the Shoulders of Giants: Results From the Radiation Oncology Academic Development and Mentorship Assessment Project (ROADMAP). Int J Radiat Oncol Biol Phys. 2013. November 7;88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeNunzio N, Parekh A, Hirsch AE. Mentoring medical students in radiation oncology. J Am Coll Radiol. 2010;7(9):722–8. [DOI] [PubMed] [Google Scholar]
- 30.Barrett K, Mistry N, Hayter C, Poldre P, Henry M, Gardner S. The effectiveness of the Ivan H. Smith Memorial Studentships program on encouraging medical students to pursue a career in radiation oncology. J Cancer Educ. 2008. December 1;23(4):226. [DOI] [PubMed] [Google Scholar]
- 31.Fleming GM, Simmons JH, Xu M, Gesell SB, Brown RF, Cutrer WB, et al. A Facilitated Peer Mentoring Program for Junior Faculty to Promote Professional Development and Peer Networking. Vol. 90, Academic Medicine. 2015. p. 819–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Virtual Visiting Professor Network, University of Colorado Department of Radiation Oncology. Rad Onc Virtual Visiting Professor Network [Internet]. Available from: http://twitter.com/radoncvvpn?lang=en
- 33.Virtual Radiation Oncology for Medical Students [Internet]. Virtual Radiation Oncology for Medical Students. [cited 2020 Jul 4]. Available from: https://www.radoncvirtual.com
- 34.GARMAN KA, WINGARD DL, REZNIK V. Development of Junior Faculty’s Self-efficacy: Outcomes of a National Center of Leadership in Academic Medicine. Acad Med. 2001;76(10):S74–6. [DOI] [PubMed] [Google Scholar]
- 35.Fung CY, Chen E, Vapiwala N, Pohar S, Trifiletti D, Truong M-T, et al. The American Society for Radiation Oncology 2017 Radiation Oncologist Workforce Study. Int J Radiat Oncol • Biol • Phys. 2019. March 1;103(3):547–56. [DOI] [PubMed] [Google Scholar]
- 36.McClelland S, Woodhouse KD, Jaboin JJ, Zellars RC. Analysis of Pre-Residency Research Productivity, Dual Degree Status, and Gender Distribution of Underrepresented Minorities Among a Current United States Radiation Oncology Junior Resident Class. Int J Radiat Oncol Biol Phys. 2019. September 1;105(1):E151–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lightfoote JB, Fielding JR, Deville C, Gunderman RB, Morgan GN, Pandharipande PV, et al. Improving diversity, inclusion, and representation in radiology and radiation oncology part 1: why these matter. J Am Coll Radiol JACR. 2014. July;11(7):673–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones RD, Chapman CH, Holliday EB, Lalani N, Wilson E, Bonner JA, et al. Qualitative Assessment of Academic Radiation Oncology Department Chairs’ Insights on Diversity, Equity, and Inclusion: Progress, Challenges, and Future Aspirations. Int J Radiat Oncol Biol Phys. 2018. January;101(1):30–45. [DOI] [PubMed] [Google Scholar]
- 39.Beeler WH, Griffith KA, Jones RD, Chapman CH, Holliday EB, Lalani N, et al. Gender, Professional Experiences, and Personal Characteristics of Academic Radiation Oncology Chairs: Data to Inform the Pipeline for the 21st Century. Int J Radiat Oncol Biol Phys. 2019. January;104(5):979–86. [DOI] [PubMed] [Google Scholar]
- 40.Holliday EB, Siker M, Chapman CH, Jagsi R, Bitterman DS, Ahmed AA, et al. Achieving gender equity in the radiation oncology physician workforce. Adv Radiat Oncol. 2018. October 1;3(4):478–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pritchett EN, Pandya AG, Ferguson NN, Hu S, Ortega-Loayza AG, Lim HW. Diversity in dermatology: Roadmap for improvement. J Am Acad Dermatol. 2018. August;79(2):337–41. [DOI] [PubMed] [Google Scholar]
- 42.Dai JC, Agochukwu-Mmonu N, Hittelman AB. Strategies for Attracting Women and Underrepresented Minorities in Urology. Curr Urol Rep. 2019. September 2;20(10):61. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.