Abstract
Purpose:
This study examined sexually assaulted women patients’ perspectives of the quality of care provided by Sexual Assault Nurse Examiners, orSANEs, including whether the patients’ perspectives varied by their demographic characteristics and health status prior to the assault.
Methods:
695 women patients who received care from SANEs at 13 US emergency care centers and community-based programs completed standardized surveys one week after receiving SANE care for sexual assault.
Results:
Most patients strongly agreed that SANEs provided high quality care, including taking patients’ needs/concerns seriously; not acting like the assault was the patient’s fault; showing care/compassion; explaining the sexual assault exam; and providing follow-up information. Perceptions did not vary by the patients’ demographic characteristics or pre-assault health status.
Conclusions:
Sexually assaulted women patients evaluated at 13 widely geographically distributed SANE programs consistently reported that SANEs provide high quality, compassionate care.
Keywords: Anxiety, Quality of Care, PTSD, Sexual Assault Nurse Examiners, Trauma Informed Care, Women
Introduction
Sexual assault is a major public health problem for US women, and is common across sociodemographic groups.1–2 Women who present for emergency care after sexual assault commonly experience high levels of pain and distress, and multiple negative health sequela after sexual assault are common.3–4 Sensitive provision of emergency nursing services is essential to appropriately address the needs of this diverse group of patients.5
The first sexual assault nurse examiner (SANE) programs developed in the 1970s, with programs becoming more widely available in the 1990s.6–7 SANEs are specially trained nursing specialists who offer sexually assaulted patients comprehensive acute care and collect evidence that can be used in assailant prosecutions.8–9 SANEs are trained to prioritize addressing patients’ needs and concerns, create a non-judgmental atmosphere, demonstrate care/compassion, provide clear explanations of the sexual assault exam, and provide important follow-up information.6 SANEs have been shown to effectively collect forensic evidence, provide needed clinical care, and foster collaborative relationships between professionals involved in sexual assault cases.10–14
In contrast, little research has gathered patients’ perspectives of the quality of their SANE care. Moreover, to our knowledge no studies have examined whether perspectives of SANE care differ according to women patients’ demographic characteristics and health status prior to the assault, important questions given the diversity of the SANE patient population. One of the few investigations that examined patients’ views of SANE care was a Canadian qualitative study of eight SANE patients. Patients felt that SANEs cared about them, made them feel safe, were not pushy, believed them, were emotionally supportive, and provided clear information.15 Another study found that 85% of 70 SANE patients in Minneapolis felt that SANEs listened to them.16 Another investigation of 52 patients from a Midwestern SANE program found that virtually all patients perceived that SANEs provided clear explanations about the exam, took patients’ needs/concerns seriously, listened to patients, showed care/compassion, and provided clear medication instructions.17 A qualitative investigation of 20 primarily white women rape patients of a Midwestern SANE program found that patients appreciated SANEs’ explanations of the exam process, being given choices during the exam, and being treated with care/compassion.18
This past pioneering research on patients’ perceptions of SANE care offers important insights. However, generalizability of these studies is limited by small samples, single SANE programs evaluated, and limited racial/ethnic diversity. To extend this research, in this study we investigated perceptions of a large, diverse group of women sexual assault patients who received care from SANEs working at 13 geographically distributed emergency care and community-based programs in the US. We address two questions. (1) To what extent did patients perceive that SANEs provided high quality care, including: taking patients’ needs/concerns seriously; not acting like the assault was the patient’s fault; showing care/compassion; explaining the sexual assault exam; and providing follow-up information? (2) Did patients’ perceptions of SANE care differ by patients’ demographic characteristics (including age, race, ethnicity, education level, employment status, income level, and marital status) and health status prior to the assault (including symptoms of anxiety, depression, posttraumatic stress, somatic, and pain symptoms)?
Materials and Methods
SETTINGS AND SAMPLES.
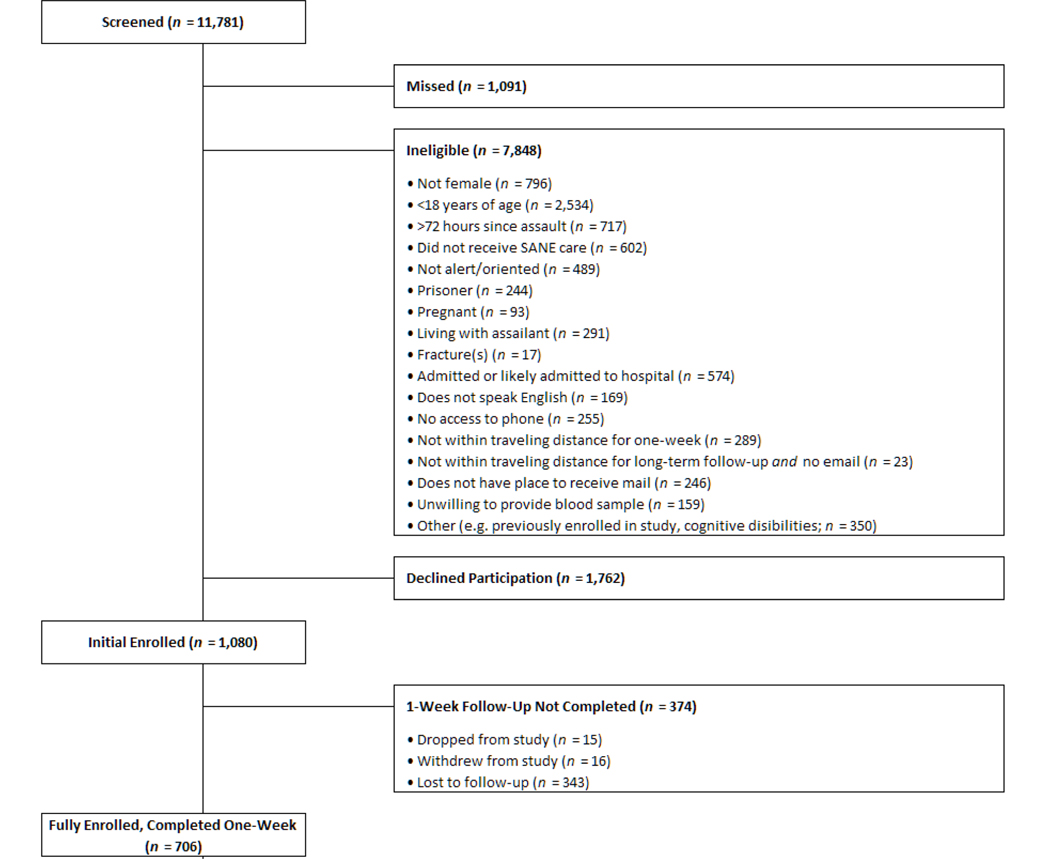
This research is part of the Women’s Health Study (WHS), the first large-scale, emergency care-based, multisite longitudinal cohort study of adult women sexual assault patients.19 The main purpose of the overall study is to better understand acute, persistent, and chronic pain development among women sexual assault survivors, and the current sub-analyses are designed to address how patients perceive SANE services. The current results have not been reported elsewhere. From 2015 through 2019, 706 study participants (Figure 1) were fully consented and enrolled at the one week from 13 geographically-distributed US emergency care and community-based SANE programs: Albuquerque SANE Collaborative (NM), UC Health Memorial Hospital (Colorado Springs, CO), Tulsa Forensic Nursing Services (OK), Austin Safe (Austin, TX), Denver Health (CO), Crisis Center of Birmingham (AL), Hennepin Healthcare (Minneapolis, MN), Christiana Care (Newark, DE), University of Louisville SANE Hospital (KY), Philadelphia SARC (PA), Cone Health (Greensboro, NC), Wayne State University Hospital and Wayne County SAFE (Detroit, MC), and DC SANE (Washington, DC).20 Full description of exclusion rates and reasons is available elsewhere. A power analysis for the sample size was based on proposed main outcomes for the overall study. 19 Women who were at least 18 years old and presented for SANE care within 72 hours of sexual assault were eligible to participate. Patients were not eligible if they could not provide informed consent; were pregnant; were living with the assailant; had an assault related fracture or required hospital admission; did not speak English; did not have a telephone/mailing address; were unwilling to provide blood samples; or were incarcerated. Research staff provided patients with informed consent information (for details, see Short et al).19
Figure 1.
Participant enrollment and study flow.
ASSESSMENT.
Participants completed self-administered survey assessments one week after receiving SANE care at a follow up visit. These surveys were completed on laptop computers in private rooms. Surveys asked about patients’ perceptions of SANE care, demographic characteristics, and health status prior to the assault. Perceptions of SANE care were evaluated using 5 survey questions, that assessed whether the SANE took the patient’s needs/concerns seriously; did not act like the assault was the patient’s fault; showed care/compassion; explained the sexual assault exam; and provided follow-up information. Patients responded to each survey question using a scale from 1 (strongly disagree) to 4 (strongly agree), with higher scores indicating a higher quality of care. In addition, for each patient, an overall Care Quality Score was created by computing the mean of the responses on the five survey items. The Care Quality Score could range from 1 to 4, with higher scores indicating a higher overall quality of care.
The survey also asked about patients’ demographic characteristics. Characteristics assessed included: age; race (White, Black/African American, American Indian/Alaskan Native, or Other); Hispanic/Latina ethnicity (yes or no); education level (more than high school graduate, high school graduate, or less than high school graduate); employment status (working full-time, working part-time, unemployed, student, or receiving disability); annual income level (more than $100,000, $60,000 to $99,999, $20,000 to $59,000, less than $20,000, or did not know); and marital status (never married, married, or separated/divorced/widowed).
The survey also asked patients specific questions about their health prior to the assault. Anxiety symptoms during the week prior to the assault were assessed via the Patient-Reported Outcomes Measurement Information System (PROMIS) short form 8a.21 Scores of 60 or more indicating clinically relevant levels of anxiety symptoms. Depression symptoms during the week prior to the assault were assessed via the PROMIS short form 8b,21 with scores of 60 or more indicating clinically relevant levels of depression symptoms. Posttraumatic stress symptoms (PTSS) during the month prior to the assault were assessed using 10 items adapted from the PTSD Checklist.22 Endorsement of re-experiencing, avoidance, and hyperarousal symptoms at least two times per week along with distress or impairment at least two times a week considered clinically relevant symptoms. Somatic symptoms during the week prior to the assault were assessed using 21 items,23 with scores of 19 or more suggestive of clinically relevant symptoms. Overall pain severity one week prior to the assault was assessed using an item from the Pain Severity Numeric Rating Scale,24 with scores of 4 or more indicating moderate or severe pain.
DATA ANALYSES.
The analysis data set included 695 of 706 enrolled patients (98% of the enrolled sample) who had complete survey information available on the survey questions examining SANE care. Participants who did not complete any SANE care items (n=11) were excluded; otherwise, participants with missing data were dropped pairwise. Descriptive statistics examined patients’ demographic characteristics, health status prior to the assault, and perceptions of care provided by SANEs. Bivariate analyses and Kruskal-Wallis non-parametric one-way analysis of variance tests25 investigated whether patients’ overall Care Quality Scores varied by patients’ demographic characteristics and health status prior to the assault.
INSTITUTIONAL REVIEW BOARD (IRB) APPROVAL.
The study protocol was approved by IRBs at the University of North Carolina at Chapel Hill and each study site.
Results
Table 1 presents information on the patients’ demographic characteristics. Patients ranged from 18 to 68 years of age, with a mean age of 28. Sixty-five percent were White, 13% were Black/African American, 6% were American Indian/Alaskan Native, and 15% were another racial group. Twenty-six percent were Hispanic/Latina. The majority (67%) had more than a high school education, 24% were high school graduates, and 8% had not completed high school. Thirty-eight percent worked full-time, 21% worked part-time, 19% were unemployed, 11% were students, and 9% received disability. Incomes ranged from more than $100,000 (8%) to less than $20,000 (36%). Seventy-nine percent of patients had never married, 7% were married, and 15% were separated, divorced, or widowed.
TABLE 1.
Patients’ demographic characteristics (n=695)
| Demographic Characteristics | Range | Mean | SD |
|---|---|---|---|
| Age | 18–68 | 28.30 | 9.58 |
| n | % | ||
| Age Category (n=692) | |||
| 18–20 | 165 | 23.7 | |
| 21–30 | 328 | 47.2 | |
| 31–40 | 125 | 18.0 | |
| 41–50 | 39 | 5.6 | |
| 51 or older | 35 | 5.0 | |
| Race (n=682) | |||
| White | 450 | 64.7 | |
| Black/African American | 87 | 12.5 | |
| American Indian/Alaskan Native | 40 | 5.8 | |
| Other | 105 | 15.1 | |
| Hispanic/Latina Ethnicity (n=679) | |||
| Yes | 168 | 25.6 | |
| No | 501 | 72.1 | |
| Education level (n=689) | |||
| More than high school graduate | 465 | 66.9 | |
| High school graduate | 168 | 24.2 | |
| Less than high school graduate | 56 | 8.1 | |
| Employment status (n=681) | |||
| Work full-time | 262 | 37.7 | |
| Work part-time | 149 | 21.4 | |
| Unemployed | 135 | 19.4 | |
| Student | 74 | 10.6 | |
| Disability | 61 | 8.8 | |
| Annual income (n=645) | |||
| ≥ $100,000 | 53 | 7.6 | |
| $60,000 to $99,999 | 80 | 11.5 | |
| $20,000 to $59,999 | 264 | 38.0 | |
| <$20,000 | 248 | 35.7 | |
| Did not know | 42 | 6.0 | |
| Marital status (n=688) | |||
| Never married | 542 | 78.0 | |
| Married | 45 | 6.5 | |
| Separated/Divorced/Widowed | 101 | 14.5 | |
Table 2 presents information on the patients’ reported health prior to the sexual assault. Anxiety scores ranged from 37.10 to 83.10 (mean=52.66), with 27% of patients reporting clinically relevant anxiety symptoms. Depression scores ranged from 37.10 to 81.10 (mean=51.69), with 23% of patients reporting clinically relevant depressive symptoms. Posttraumatic stress scores ranged from 0 to 36 (mean=13.89), with 37% of patients reporting clinically relevant posttraumatic stress symptoms. Somatic scores ranged from 0 to 199 (mean=15.47), with 26% of patients reporting clinically relevant somatic symptoms. Pain severity scores ranged from 0 to 10 (mean=1.82), with 19% of patients reporting moderate or severe pain.
TABLE 2.
Patients’ health symptoms prior to the sexual assault
| Symptom Scores Prior to Sexual Assault | Clinically High Symptom Levels Prior to Sexual Assault | ||||
|---|---|---|---|---|---|
| Range | Mean | SD | n | % | |
| Anxiety symptoms (n=686) | 37.10–83.10 | 52.66 | 11.34 | 185 | 26.6 |
| Depression symptoms (n=687) | 37.10–81.10 | 51.69 | 10.69 | 157 | 22.6 |
| PTSS symptoms (n=686) | 0–36.00 | 13.89 | 11.17 | 260 | 37.4 |
| Somatic symptoms (n=691) | 0–198.00 | 15.47 | 26.91 | 179 | 25.8 |
| Pain severity (n=681) | 0–10.00 | 1.82 | 2.41 | 133 | 19.1 |
The majority of women sexual assault patients who participated in this survey reported receiving a high quality of care by the SANEs (Table 3). Most patients “strongly agreed” that SANEs took their needs/concerns seriously (90%), did not act as if the assault was their fault (89%), cared and showed compassion (88%), explained the exam (86%), and gave follow-up information (75%). Mean scores for each of the five survey items ranged from 3.67 to 3.85, showing that most patients reported that SANEs provided high quality care on each of the five domains assessed. Moreover, the mean Overall Care Quality Score (3.79) indicated that patients reported receiving an overall high quality of care from SANEs.
TABLE 3.
Number and percentage of patients with various perceptions of the quality of SANE care in five domains and the Overall Care Quality Score (n = 695)
| Strongly Agree (coded 4) | Agree (coded 3) | Disagree (coded 2) | Strongly Disagree (coded 1) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Survey Items | n | % | n | % | n | % | n | % | Mean | SD |
| Took needs/concerns seriously | 623 | 89.6 | 56 | 8.1 | 2 | 0.3 | 14 | 2.0 | 3.85 | 0.50 |
| Did not act like it was my fault | 621 | 89.4 | 40 | 5.8 | 8 | 1.2 | 26 | 3.7 | 3.81 | 0.64 |
| Cared and showed compassion | 608 | 87.5 | 68 | 9.5 | 4 | 0.6 | 15 | 2.2 | 3.83 | 0.53 |
| Explained the exam | 598 | 86.0 | 76 | 10.9 | 8 | 1.2 | 13 | 1.9 | 3.81 | 0.54 |
| Gave follow-up information | 519 | 74.7 | 141 | 20.3 | 16 | 2.3 | 19 | 2.7 | 3.67 | 0.66 |
| Overall Care Quality Score | ---- | ---- | ---- | ---- | ---- | ---- | ---- | ---- | 3.79 | 0.44 |
Table 4 shows that Overall Care Quality Scores did not differ significantly by patients’ demographic characteristics or health status prior to the assault. For each category of age, race, ethnicity, education, employment status, income and marital status, the mean Overall Care Quality scores were extremely high, ranging from 3.66 to 3.87. In addition, Overall Care Quality scores did not differ significantly between patients who had clinically high levels of depression, anxiety, PTSS, somatic pain symptoms prior to the assault and those who did not have clinically high levels of these symptoms prior to the assault. For each category with these groups, the mean Overall Care Quality scores were extremely high, ranging from 3.70 to 3.82.
TABLE 4.
Patients’ Overall Care Quality scores, stratified by patients’ demographic characteristics and clinically relevant health symptoms prior to sexual assault (n=695)
| Demographic Characteristic | Mean | SD | Kruskal-Wallis Nonparametric One Way Anova p-value |
|---|---|---|---|
| Age | .136 | ||
| 18–20 | 3.73 | 0.54 | |
| 21–30 | 3.82 | 0.41 | |
| 31–40 | 3.83 | 0.36 | |
| 41–50 | 3.79 | 0.37 | |
| 51 and older | 3.66 | 0.58 | |
| Race | .615 | ||
| White | 3.82 | 0.37 | |
| American Indian/Alaskan Native |
3.67 | 0.64 | |
| Black/African American | 3.81 | 0.30 | |
| Other | 3.75 | 0.58 | |
| Hispanic/Latina ethnicity | .351 | ||
| No | 3.76 | 0.51 | |
| Yes | 3.81 | 0.41 | |
| Education level | .096 | ||
| More than high school graduate | 3.82 | 0.41 | |
| High school graduate | 3.72 | 0.51 | |
| Less than high school graduate | 3.87 | 0.24 | |
| Employment status | .139 | ||
| Full-time employment | 3.84 | 0.35 | |
| Student | 3.83 | 0.36 | |
| Part-time employment | 3.73 | 0.58 | |
| Disability | 3.74 | 0.41 | |
| Unemployed | 3.76 | 0.50 | |
| Annual income | .403 | ||
| > $100,000 | 3.85 | 0.27 | |
| $60,000 to $99,999 | 3.85 | 0.39 | |
| $20,000 to $59,999 | 3.80 | 0.43 | |
| < $20,000 | 3.76 | 0.49 | |
| Marital status | .510 | ||
| Married | 3.85 | 0.30 | |
| Never married | 3.79 | 0.45 | |
| Separated/divorced/widowed | 3.75 | 0.47 | |
| Clinically Relevant Levels of Health Symptoms Prior to Sexual Assault | Mean | SD | Kruskal-Wallis Nonparametric One Way Anova p-value |
| Depression symptoms | .506 | ||
| No | 3.82 | 0.40 | |
| Yes | 3.70 | 0.61 | |
| Anxiety symptoms | .842 | ||
| No | 3.81 | 0.37 | |
| Yes | 3.74 | 0.58 | |
| Posttraumatic stress symptoms | .673 | ||
| No | 3.81 | 0.43 | |
| Yes | 3.77 | 0.47 | |
| Somatic symptoms | .921 | ||
| No | 3.79 | 0.44 | |
| Yes | 3.79 | 0.45 | |
| Pain severity | .903 | ||
| No | 3.82 | 0.41 | |
| Yes | 3.79 | 0.44 | |
Discussion
To our knowledge this study is the first to examine assessments of SANE care by a large group of women sexual assault patients presenting to diverse SANE programs in the US. Our results are consistent with smaller studies in showing that the vast majority of patients who participate view SANEs as providing high quality care.15–18 Our results extend this past research by showing that this is true for each of the five care domains examined in this study, including taking patients’ needs/concerns seriously, not acting as if the assault was the fault of the patient, showing care and compassion, explaining the exam, and providing follow-up information. In addition, our results also extend previous findings by demonstrating that the majority of women sexual assault patients willing to participate in research view their SANE care as high quality, across geographically, demographically, and administratively (i.e., emergency care-based, community-based) diverse SANE programs, diverse sexual assault patient demographic groups, and women sexual assault patients with diverse mental and physical health status.
These quantitative findings are consistent with participants’ qualitative reports. For example, one women sexual assault patient wrote, “The SANE nurse that I experienced was PHENOMENAL…her general attitude and humor greatly affected me in positive ways after the assault”. Another sexual assault patient wrote, “Everything was really good…I didn’t even know they had that SANE organization…You guys are doing everything right.”
This research also has clinical and policy implications. Unfortunately, SANE programs are not available in all locations across the US. Indeed, one reported noted a shortage of SANE programs in every US state evaluated.26 Specifically, it may be particularly difficult for women in rural areas to access SANE care.27 The lack of availability of SANE programs in all areas may be in part attributable to difficulties with funding. SANE programs are typically funded through a combination governmental funds, hospital donations, fundraising, and money from nongovernment agencies and other grants, as well as funding from the Violence Against Women Act (VAWA) and Victims of Crime Act (VOCA). However, SANE programs often face budget cuts28 and operate at a loss given that SANE programs (including equipment and training) can be expensive to maintain.29 Indeed, empirical studies have indicated that lack of funding is a “major problem” for more than half of SANE programs. 30 When SANE care is not available, other resources (e.g., non-clinical forensic evaluations or other interdisciplinary clinician teams) may provide services. Such teams may not have the advanced multidisciplinary training and breadth of experiences SANEs have in providing health care, collecting forensic evidence, and fulfilling these needs in a trauma-informed and compassionate manner.
SANE’s training and experience in cultural competency may play a role in the high ratings for SANEs across various demographic groups. Although it is critical to strive for continuous improvement in cultural competency, SANE training emphasizes the need to be aware of and respect cultural differences. 31 Nationally representative surveys have found conflicting results regarding whether demographic characteristics play a role in who seeks SANE care. Resnick et al32 found women who were not white were more likely to receive post-assault care, while the more recent findings by Amstadter33 indicated white race and income <$20k predicted being more likely to seek post-assault care (not specific to SANE care). Thus, more research is needed to determine whether there are health disparities in access to SANE care, but our research indicates that when women do receive such care, they are typically satisfied regardless of their demographic characteristics.
Limitations
As with all research, this study has strengths and limitations. Strengths include the large sample of patients seen by SANEs in diverse SANE programs, and the use of standardized assessment procedures. However, the emergency centers/programs participating in the study were not specifically selected to be nationally representative of all SANE programs, thus our results cannot be viewed as providing specific estimates of experiences with SANEs at all programs across the US. In addition, only women patients 18 years of age or older were studied, so the findings may not be generalizable to male or teen patients. The results are not generalizable to patients who were ineligible to participant in our study, including those who presented for care >72 hours since assault, not alert/oriented, incarcerated, pregnant, living with the assailant, admitted for acute care, fracture(s), and other reasons listed in Figure 1. Future research should include children, men, and LGBTQ sexual assault patients as they may face unique challenges and have different perspectives on SANE services. Moreover, the pre-assault health concerns examined were limited to emotional health and pain symptoms; therefore, these findings may not be generalizable to sexually assaulted patients with other types of pre-assault health conditions. The majority of our sites were in urban/suburban areas, so future research should examine SANE care satisfaction among patients living in rural areas. Finally, considering the majority of patients’ responses were at the upper end of our scale, it is possible that ceiling effects existed in our measurement of perceptions of SANE care or a social desirability bias affected the results. Future research should consider more nuanced measures, such as utilizing Likert-scales with 7–10 possible response options.
Implications for Emergency Clinical Care
The results of this research strongly reinforce the importance of including SANEs whenever possible in treating women sexual assault patients. SANEs provide an emotionally supportive and respectful environment for patients while performing evidence collection and/or providing health-related services in the immediate aftermath of assault, and these services are critical in helping to begin the emotional and physical healing process. Leaders of hospitals and community health centers should develop and support their SANE programs, to ensure that sexual assault patients can receive the high quality of care that they deserve.
Conclusions
The majority of adult women sexual assault patients seen by SANEs at 13 geographically and demographically diverse emergency care- and community-based SANE programs in the US, and who were willing to participate in our follow up study, reported that SANEs provide a high quality of care. Adult women sexual assault patients consistently reported that SANEs took their needs/concerns seriously, did not act like the assault was their fault, showed care and compassion, explained the exam, and provided follow-up information. These perceptions were consistent among patients with varied demographic characteristics and pre-assault health status. We encourage all health services and facilities that treat sexually assaulted patients to include SANE care as part of their routine response to these trauma patients.
Contribution to Emergency Nursing Practice.
Few studies have examined women patients’ perspectives of SANE care, and none have examined whether perspectives differ according to sexual assault patients demographic characteristics or pre-assault health status.
Nearly 700 women sexual assault patients evaluated at 13 widely geographically distributed SANE programs reported receiving high quality SANE care, including taking their needs/concerns seriously, not acting like the assault was their fault, showing care/compassion, explaining the sexual assault exam, and providing follow-up information. There were no significant differences in perceptions of care according to demographic or pre-assault health characteristics.
SANEs provide critical services greatly valued by women sexual assault patients. SANEs should be used whenever possible in emergency nursing settings to treat sexually assaulted women.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Megan Lechner, Forensic Nurse Examiner Clinical Manager, Colorado SANE/SAFE Project Director, Memorial Hospital UCHealth, Colorado Springs, Colorado.
Kathy Bell, Forensic Nursing Administrator, Tulsa Police Department, Tulsa Oklahoma.
Nicole A. Short, Institute for Trauma Recovery, University of North Carolina, Chapel Hill, NC.
Sandra L. Martin, Department of Maternal and Child Health, University of North Carolina, Chapel Hill, NC.
Jenny Black, Austin SAFE, Austin, TX.
Jennie A. Buchanan, Department of Emergency Medicine, Denver Health, Denver, CO.
Rhiannon Reese, Crisis Center of Birmingham, Birmingham, AL.
Jeffrey D. Ho, Hennepin Assault Response Team.
Gordon D. Reed, Department of Emergency Medicine, Christiana Care, Newark, DE.
Melissa Platt, SAFE Service, University of Louisville Hospital, Louisville, KY.
Ralph Riviello, University of Texas Health, San Antonio, TX.
Catherine Rossi, Cone Health, Greensboro, NC.
Patricia Nouhan, Department of Emergency Medicine, Wayne State University, Detroit, MI.
Carolyn Phillips, DC SANE, Washington, DC.
Kenneth A. Bollen, University of North Carolina, Chapel Hill, NC.
Samuel A. McLean, Institute for Trauma Recovery, University of North Carolina, Chapel Hill, NC.
References
- 1.Smith SG, Zhang X, Basile KC, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data Brief – Updated Release. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. 2018. https://www.cdc.gov/violenceprevention/pdf/2015data-brief508.pdf. Accessed 23 June 2020. [Google Scholar]
- 2.Ullman SE, Najdowski CJ. Vulnerability and Protective Factors for sexual assault. In: Koss MP, White JW, Kazdin AE, eds. Violence Against Women and Children: Volume 1, Mapping the Terrain. Washington DC: American Psychological Association; 2011:151–172. [Google Scholar]
- 3.Dworkin ER, Menon SV, Bystrynski J, et al. Sexual assault victimization and psychopathology: A review and meta-analysis. Clin Psychol Rev. 2017;56:65–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martin SL, Macy R, Young S. Health and economic consequences of sexual violence. In: Koss MP, White JW, Kazdin AE, eds. Violence Against Women and Children: Volume 1, Mapping the Terrain. Washington DC: American Psychological Association; 2011:173–195. [Google Scholar]
- 5.Campbell R, Patterson DA. Services for victims of sexual violence. In: Koss MP, White JW, Kazdin AE, eds. Violence Against Women and Children: Volume 2, Navigating Solutions. Washington DC: American Psychological Association; 2011:95–114. [Google Scholar]
- 6.Ledray LE. Sexual Assault Nurse Examiner (SANE) Development and Operation Guide. Office for Victims of Crime, Washington DC;1999. https://www.ncjrs.gov/ovc_archives/reports/saneguide.pdf. Accessed 23 June 2020. [Google Scholar]
- 7.Ledray LE, Arndt S. Examining the sexual assault victim: A new model for nursing care. J Psychosoc Nurs Men. 1994;32(2):7–11. [DOI] [PubMed] [Google Scholar]
- 8.International Association of Forensic Nurses. Sexual Assault Nurse Examiners, 2020. https://www.forensicnurses.org/page/aboutSANE; Accessed 23 June 2020.
- 9.National Institute of Justice. National Best Practices for sexual assault kits: A multidisciplinary approach. U.S. Department of Justice, Office of Justice Programs, 2017. https://nij.ojp.gov/topics/articles/national-best-practices-sexual-assault-kits-multidisciplinary-approach. Accessed 21 February 2020. [Google Scholar]
- 10.Campbell R, Bybee D, Townsend SM, Shaw J, et al. The impact of sexual assault nurse examiner programs on criminal justice case outcomes: a multisite replication study. Violence Against Women. 2014;20(5):607–625. [DOI] [PubMed] [Google Scholar]
- 11.Campbell R, Patterson D, Bybee D. Prosecution of adult sexual assault cases: a longitudinal analysis of the impact of a sexual assault nurse examiner program. Violence Against Women. 2012;18(2):223–44. doi: 10.1177/1077801212440158. [DOI] [PubMed] [Google Scholar]
- 12.Campbell R, Patterson D, Fehler-Cabral G. Using ecological theory to evaluate the effectiveness of an indigenous community intervention: A study of sexual assault nurse examiner (SANE) programs. Am J Community Psychol.2010;46:263–276. doi: 10.1007/s10464-010-9339-4. [DOI] [PubMed] [Google Scholar]
- 13.Campbell R, Patterson D, Lichty LF. The effectiveness of sexual assault nurse examiner (SANE) programs: A review of psychological, medical, legal, and community outcomes. Trauma Violence Abuse. 2005;6(4):313–329. [DOI] [PubMed] [Google Scholar]
- 14.Campbell R, Townsend SM, Long SM, et al. Responding to sexual assault victims’ medical and emotional needs: A national study of the services provided by SANE programs. Research in Nursing & Health. 2006;29(5):384–398. 10.1002/nur.20137; Accessed June 2020. [DOI] [PubMed] [Google Scholar]
- 15.Ericksen J, Dudley C, McIntosh G, et al. Clients’ experiences with a specialized sexual assault service. J Emerg Nurs. 2002;28:86–90. [DOI] [PubMed] [Google Scholar]
- 16.Malloy M. Relationship of nurse identified therapeutic techniques to client satisfaction reports in a crisis program. Unpublished thesis, University of Minnesota, Minneapolis, 1991. [Google Scholar]
- 17.Campbell R, Patterson D, Adams AE, Diegel R, Coats S. A participatory evaluation project to measure SANE nursing practice and adult sexual assault patients’ psychological well-being. J Forensic Nurs. 2008;4(1):19–28. doi: 10.1111/j.1939-3938.2008.00003.x [DOI] [PubMed] [Google Scholar]
- 18.Fehler-Cabral G, Campbell R, Patterson D. Adult sexual assault survivors’ experiences with sexual assault nurse examiners (SANEs). J Interpers Violence. December 2011;26(18):3618–39. doi: 10.1177/0886260511403761. [DOI] [PubMed] [Google Scholar]
- 19.Short NA, Sullivan J, Soward A, et al. Protocol for the first large-scale emergency care-based longitudinal cohort study of recovery after sexual assault: the Women’s Health Study. BMJ Open. 2019;9:e031087. doi: 10.1136/bmjopen-2019-031087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.UNC Institute for Recovery. Better Tomorrow Network, 2020. https://www.med.unc.edu/itr/better-tomorrow-network/. Accessed 28 February 2020.
- 21.Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005– 2008. J Clin Epidemiol. 2010;63:1179–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blevins CA, Weathers FW, Davis MT, et al. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J Trauma Stress. 2015;28:489–498. doi: 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- 23.Auvergne L, Bortsov AV, Ulirsch JC, et al. Association of epidemiologic factors and genetic variants influencing hypothalamic-pituitary-adrenocortical axis function with Postconcussive symptoms after minor motor vehicle collision. Psychosom Med. 2016;78(1), 68–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10:390–392. [DOI] [PubMed] [Google Scholar]
- 25.Daniel WW. Kruskal-Wallis one-way analysis of variance by ranks. In Applied Nonparametric Statistics (2nd ed.), 1990. Boston: PWS-Kent. pp. 226–234. ISBN 0–534-91976–6 [Google Scholar]
- 26.United States Government Accountability Office. Sexual assault: information on availability of forensic examiners, 2018. Available at: https://www.gao.gov/assets/700/695914.pdf
- 27.Annan S. “‘We desperately need some help here’-The experience of legal experts with sexual assault and evidence collection in rural communities. 2014. [PubMed] [Google Scholar]
- 28.Campbell R, Patterson D, Lichty LF. The effectiveness of sexual assault nurse examiner(SANE) programs: A review of psychological, medical, legal, and community outcomes. Trauma, Violence, & Abuse. 2005:6:4:313–329. [DOI] [PubMed] [Google Scholar]
- 29.Maier SL. Sexual assault nurse examiners’ perceptions of funding challenges faced by SANE programs: “it stinks”. J Forens Nurs. 2012:8:2:81–93. [DOI] [PubMed] [Google Scholar]
- 30.Logan TK, Cole J, Capillo A. Sexual assault nurse examiner program characteristics, barriers, and lessons learned. J Forens Nurs. 2007:3:1:24–34. [DOI] [PubMed] [Google Scholar]
- 31.National Institute of Justice. National Best Practices for Sexual Assault Kits: A Multidisciplinary Approach. 2017. [Google Scholar]
- 32.Resnick HS, Holmes MM, Kilpatrick DG, Clum G, Acierno R, Best CL, Saunders BE. Predictors of post-rape medical care in a national sample of women. Am J Prev Med. 2000:19:4:214–219. [DOI] [PubMed] [Google Scholar]
- 33.Amstadter AB, McCauley JL, Ruggiero KJ, Resnick HS, Kilpatrick DG. Service utilization and help seeking in a national sample of female rape victims. Psych serv. 2008:59:12:1450–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]