Abstract
The health of smallholder farmers is crucial for ensuring food and nutritional security for two billion people. However, their health is in jeopardy for several reasons including challenges from climate change impacts. Using a narrative literature review supported by field observations and informal interviews with key informants in India, Bangladesh and Malawi, this paper identifies and discusses the health impacts of climate change under four categories: (i) communicable diseases, (ii) non-communicable diseases, (iii) mental health, and (iv) occupational health, safety and other health issues. The health impacts of climate change on smallholder farmers will hamper the realization of many of the United Nations' Sustainable Development Goals, and a series of recommendations are made to regional and country governments to address the increasing health impacts of accelerating climate change among smallholder farmers.
Keywords: Climate change, Smallholder farmers, Health impacts, SDGs
1. Introduction
The food and nutritional security of two billion people around the world depend largely on smallholder farmers [1], defined as those who hold less than 2 ha [ha] of agricultural land [[1], [2], [3], [4]]. The estimated 500 million smallholder farming households worldwide, comprise a large proportion of the world's poor, often living on less than $2 a day [5]. Smallholder farms account for about 84% of the world's farms and cover 12% of global agricultural land [1], while providing 70% of kilocalories to the people of Asia and sub-Saharan Africa [6]. Despite their crucial roles in producing food and contributing to agricultural sustainability [7], smallholder farmers are subject to a vicious cycle of poverty caused by limited financial resources, environmental stresses and poor social support, as well as health and education challenges. With limited access to human, social, economic, technological resources and capital, the poverty cycle often deepens over generations [[8], [9], [10]].
In addition to existing challenges, the impacts of climate change are making smallholder farmers and their agricultural systems more vulnerable [11,12]. While smallholder farmers are struggling to adapt their agricultural systems to climate change impacts, their health is also impacted by climate change. Safe working conditions and good health are crucial preconditions needed to sustain agriculture practices and ensure the productivity of smallholder farms. Climate change further threatens these conditions through more frequent natural disasters and the increasing occurrence of malnutrition and communicable and non-communicable diseases. This review paper examines how and why the health of smallholder farmers is affected by climate change and what potential interventions may address these issues.
2. Methodology
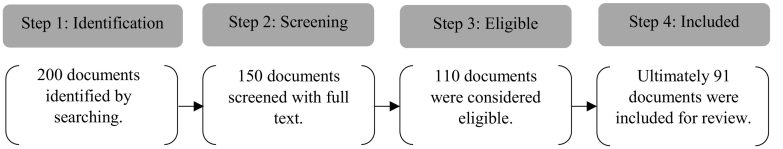
The authors have directly observed and experienced various socio-ecological and health impacts of climate change on smallholder farmers in Bangladesh, India, and Malawi over the last 20 years. We developed a topical approach to a narrative literature review. This was informed by open-ended informal discussions with key informants in Malawi and in Bangladesh that were carried out over multiple field visits during 2018–20 to understand the health impacts due to increased average temperatures and increase in extreme weather events resulting from climate change. Key informants included knowledgeable small-holder farmers as well as professionals and experts from government departments (i.e., health, agriculture, environment, and disaster management) and NGOs working directly with farmers and in the fields. We conducted a narrative literature review of both peer-reviewed and grey literature using a topical approach with the following keyword search terms: “smallholder farmers”, “food security”, “climate change and smallholder farmers”, “climate change and health impacts”, “climate change and agriculture”, “extreme weather events distribution”, and “infectious diseases distribution”. Using both (i) Boolean search methods applied to key word combinations and (ii) identification of pivotal papers known to the authors, we applied the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) strategic review process ([13], see Fig. 1) to identify 200 documents that address how the impacts of climate change are making smallholder farmers and their agricultural systems more vulnerable. Of these, 150 were selected for screening based on a refined focus on how and why the health of smallholder farmers is or may be affected by climate change. All 150 paper abstracts were reviewed, and 110 documents were selected as eligible, and 91 documents were included for full review for this narrative literature review. Our findings are presented and discussed in Section 3.0, followed by a conclusion and recommendations in Section 4.0.
Fig. 1.
PRISMA flow diagram of narrative literature review.
3. Results and discussion
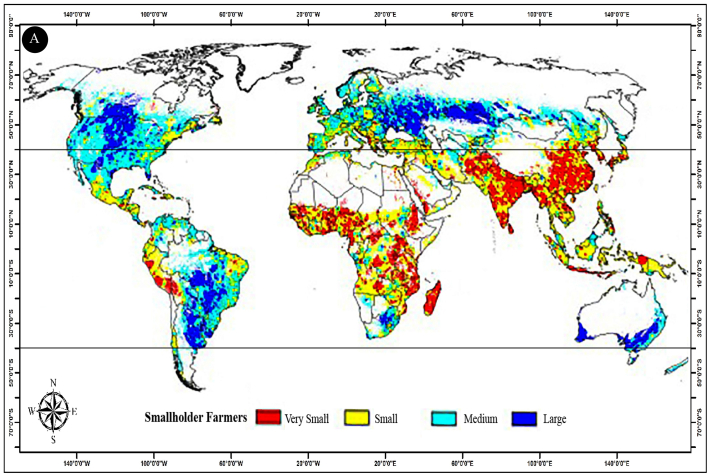
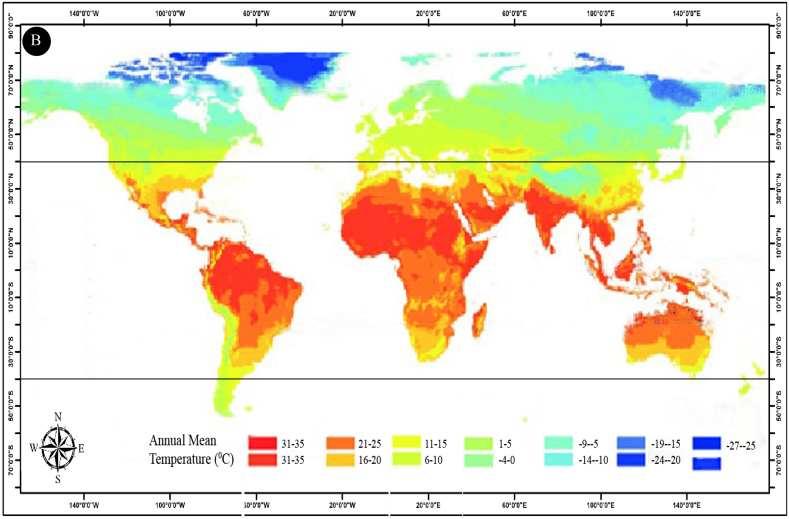
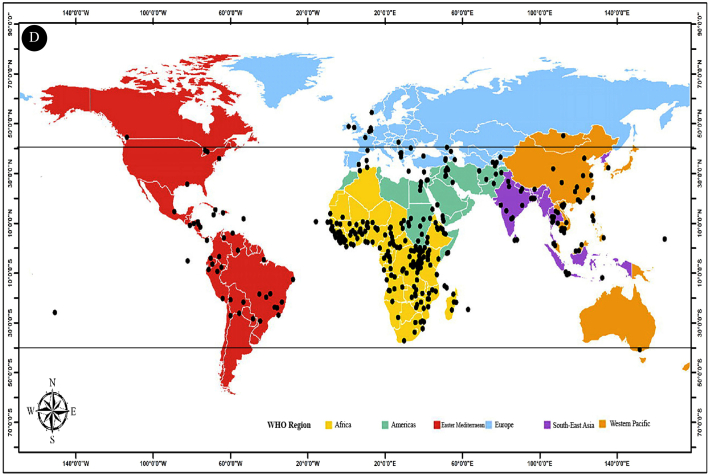
Most smallholder farms are located mainly in the tropical and subtropical regions of Asia and Africa, and to a lesser extent, in Latin America. A much smaller number are in temperate zones up to about 40°N and S latitudes, including areas in Europe and North America (Fig. 2A & B). As reflected in the rankings of the 2014 Climate Change Vulnerability Index (CCVI), the regions having the greatest numbers of small farmers are experiencing and will experience the highest frequency of extreme weather events. The top ten CCVI highly vulnerable countries are: Bangladesh, Guinea-Bissau, Sierra Leone, Haiti, South Sudan, Nigeria, DR Congo, Cambodia, Philippines, and Ethiopia. The CCVI Index assesses the vulnerability of human populations to extreme climate events and changes over the last 30 years by combining (i) exposure to climate extremes, (ii) current human sensitivity to climate stressors, and the (iii) capacity of the country to adapt to the impacts of climate change [14]. Climate models show that climate variability will be especially strong in tropical and subtropical regions (between 50°N and S), which will be hotspots for more frequent extreme weather events [15,16] (see Fig. 2C). In addition, most emerging infectious diseases (both vector-borne and direct pathogen) are distributed within these tropical, subtropical, and temperate regions (see Fig. 2D).
Fig. 2.
(A) Global distribution of farm field size (smallholder farmers, adapted and modified from [18]); (B) Global distribution of annual mean temperature by latitude (adapted and modified from [19] with permission); (C) Climate change-induced extreme weather events related to meteorological, hydrological, and climatological phenomena in 2014 (adapted and modified from [20] with permission); (D) Geographical distribution of emerging infectious diseases reported by WHO from 1996 to 2009 (adapted and modified from [21] with permission). Note: All the maps from (A) to (D) have been reconstructed by using ArcGIS. (B), (C), and (D) represent data from 2009 to 2014. Due to lack of availability of more recent data, these maps are considered baseline maps.
In the tropics and subtropics, smallholder farmers live on homesteads near or on their farms and often carry out physically strenuous agricultural tasks in the open sun without proper protection, exposing them to variable and sometimes severe, climatic conditions. Most have limited or no financial ability or political support to plan for and counteract extreme weather events such as flooding, hurricanes or prolonged drought. In addition, smallholder farmers frequently suffer from food and nutritional insecurity and the consequences of exposure to animal and insect attacks as well as the negative health effects of pesticides, fertilizers, and biological pollution [17].
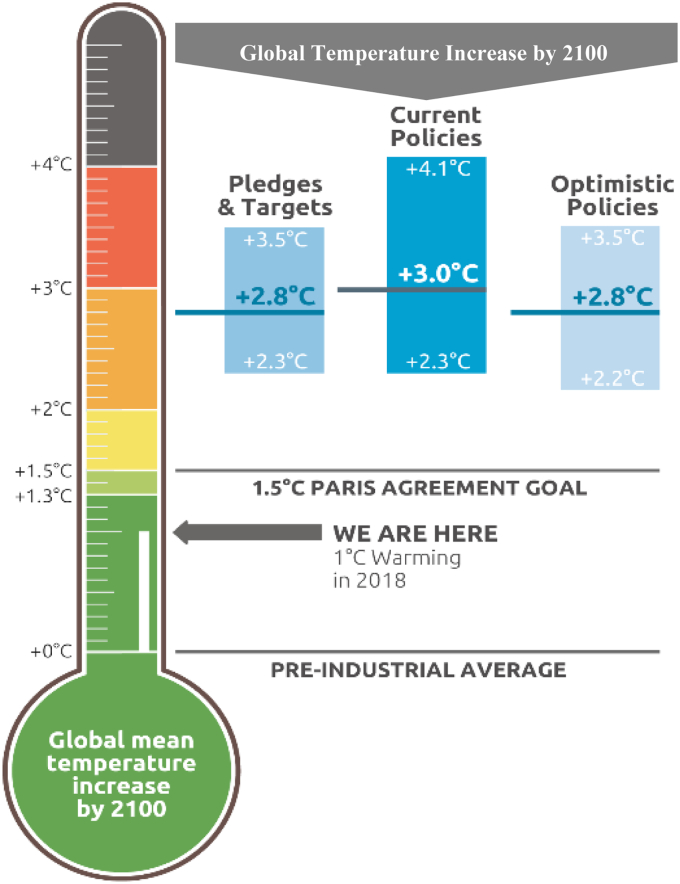
The world is experiencing increasing temperatures that will increase further, even if the Paris Agreement is fully implemented. While smallholder farmers already face the health issues outlined above, these will intensify due to growing climate change impacts. Without full implementation of the Paris Agreement, the global average temperature may increase by about 3 °C by 2100 [22], as shown in Fig. 3.
Fig. 3.
The world has already experienced a 1 °C temperature increase. By implementing the Paris Agreement, temperature will still increase, but may be kept to 1.5 °C. Without full implementation of the Paris Agreement, global temperature may increase an average of 3 °C by 2100 (adapted and modified from [22] with permission).
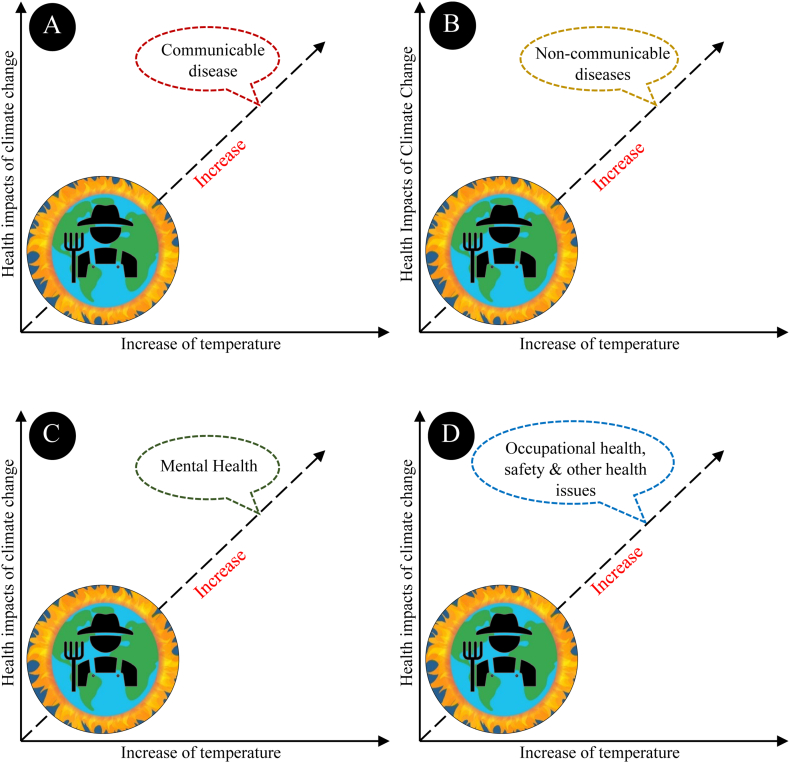
The health impacts of climate change on smallholder farmers can grouped in to four categories: (i) communicable diseases, (ii) non-communicable diseases, (iii) mental health, and (iv) occupational health, safety, and other health issues, as depicted in Fig. 4. These are discussed in 3.1, 3.2, 3.3, 3.4 below.
Fig. 4.
Without controlling increasing temperature, the health impacts of [A] communicable diseases, [B] non-communicable diseases, [C] mental health, and [D] occupational health, safety, and other health issues of climate change on smallholder farmers will all worsen with time.
3.1. Communicable diseases
Climate change is altering temperature and humidity [23], and this is having effects on the patterns, frequency, and clusters of extreme weather events such as cyclones, floods, and drought in tropical and subtropical regions [24]. These extreme weather events disrupt social and environmental settings and can create favourable conditions for microbes, vectors, and reservoir animal hosts to transmit communicable diseases to humans [25].
Climate change has increased the intensity of Tropical Cyclones (TCs) [26]. TCs can raise the risk of transmission and outbreak of infectious diseases including leptospirosis, dengue, malaria, cholera, zika, diarrhea, dysentery, acute respiratory infections, and pulmonary tuberculosis. They can also create favourable conditions and sites for vector breeding while hindering sanitation management and good personal hygiene practices. Furthermore, TCs often cause population displacement and can inhibit healthcare access [27]. As a consequence, TCs can significantly affect the health of smallholder farmers who are located within TC-prone areas as can be seen in Fig. 2A and C. For instance, the incidence of diarrhea, dysentery, and acute respiratory infections rose after cyclone Nargis in the coastal areas of Bangladesh [28], and two subdivisions in coastal India where most of the settlers are smallholder farmers observed significantly higher [30%–60%) incidence of diarrhea in 2009 after cyclone Aila [29]. A questionnaire survey administered by the first author in 2010 among 25 smallholder farm households in the southwest coast of Bangladesh after Cyclone Sidr (2007) revealed that 96% of the households were affected by diarrhea due to lack of fresh water.
Climate change can worsen overall flooding risk, and the frequency of flooding is especially high in tropical and subtropical regions [30]. In particular, according to Marsooli et al. [31], coastal flooding in tropical regions will increase with more frequent TCs. Flooding disrupts and contaminates the freshwater supply and contributes to poor sanitation, damage to infrastructure, and failure in delivery of and access to medical and public health services [27], which in turn may increase the risk of many foodborne and waterborne infectious diseases in addition to those mentioned above, such as conjunctivitis, schistosomiasis, skin and soft tissue infection, and dermatitis [32]. The risks of these diseases are higher among smallholder farmers since most live in flood-prone regions as can be seen in Fig. 2A and C and usually do not have the resources needed to protect themselves adequately.
In contrast, due to climate change, in other parts of some tropical and subtropical countries the intensity of drought has increased [33]. Where there is decreased rainfall and drought, infectious diseases can become more significant through the contamination of ground- and surface-water by viruses, protozoa, and bacteria. In drought conditions, smallholder farmers who get their drinking water from private wells are at higher risk for these drought-related infectious diseases [34]. Further, in drought stressed areas, agricultural adaptation techniques such as mulching may shelter some pests and diseases [35], while rainwater harvesting may be the source of a variety of infectious diseases [36].
Higher temperatures and humidity combined with changing and increasingly variable precipitation can also lead to risks of vector-borne disease [37] because of prolonged transmission seasons, favourable breeding conditions and reduced effectiveness of vector-control interventions [25,38,39].
Worldwide and especially in tropical, subtropical, and temperate regions, climate change has been reported to be a driver for emerging food safety risks at various stages of the food chain, from primary production through to consumption [40,41]. Unseasonal rain at the time of harvest can result in agricultural products becoming contaminated with fungi and mycotoxins such as aflatoxins. Consumption of such contaminated products by smallholder farmers, who often have limited choices, may be responsible for disease outbreaks [42]. During transport and storage, higher temperatures also favor the growth of pathogenic agents in meat and fish, which can easily cause illness for the smallholder farmers who consume them.
3.2. Non-communicable diseases
Perhaps less obviously, climate change-induced extreme weather events such as heat waves, droughts, storms, and floods in tropical, subtropical, and temperate regions can exacerbate the incidence of some non-communicable diseases [43], including cardiovascular disease, cancers, respiratory issues, and malnutrition [44] among smallholder farmers. For example, heat-triggered chronic kidney disease associated with recurrent dehydration has been observed in Central America, North America, South America, the Middle East, Africa, and India [45], accounting for the highest rates of death from kidney disease in the world [46], and has been newly identified as a sentinel disease of climate change [47]. In addition, climate change-induced heat waves increase the risk of incidence of heat-related health impacts such as heat exhaustion and heat stroke as well as cardiovascular, respiratory, and other diseases [48,49]. As outdoor workers who labor in open fields under the sun, smallholder farmers in these regions of warm climates are especially exposed to climate change-intensified heat waves and disease.
Flooding and cyclones contribute to a wide range of health and safety consequences such as drowning, injury and disability [50] among farmers who stay at home or in the fields to protect their land and agricultural products during disasters.
Climate change may also increase smallholder farmers' risk of neurological disorders as they suffer from malnutrition or are exposed to biotoxins [algal and fungal] through agricultural practices and food consumption [51]. Warmer water associated with climate change favors harmful algal blooms in waterbodies which are often the source of water for irrigation and sometimes for human consumption [52]. Warmer temperatures can also increase the abundance of soil-based fungi which can attack and damage crops [53].
Climate change-induced natural disasters (e.g., flood and cyclone) have significant impacts on the agricultural sector by directly damaging crops, supply chains, and agriculture-supporting ecosystems which affect livelihoods, food security, and nutrition [54]. Smallholder farmers' health depends on access to adequate, affordable, good-quality, and nutritious food. Food insecurity among smallholder farmers can lead to undernutrition [55], with short-term consequences of mortality, morbidity, and disability and long-term effects on body growth, intellectual ability, reproductive performance, and metabolic and cardiovascular disease [56].
Sea level rise causes growing salinity in many regions where smallholder farmers work. As a result, they are subject to saline-related issues such as hypertension, cardiovascular disease, and miscarriage [[57], [58], [59], [60], [61]]. For example, while the millions of smallholder farmers in coastal Bangladesh are subject to the immediate health impacts of natural calamities such as cyclone and flood [62], their long-term health is also affected by the gradually increasing salinity [63].
3.3. Mental health
Climate change may increase the risk of mental health impacts among smallholder farmers as they face the hardships of practicing agriculture along with the uncertainties associated with extreme weather events [64] as well as slow-onset events including sea level rise, increasing temperatures, ocean acidification, glacial retreat and its related impacts, salinization, land and forest degradation, loss of biodiversity, and desertification [65,66]. For instance, in India, climate change may have contributed to the suicides of nearly 60,000 Indian farmers and farm workers over the past three decades [67]. Suicides increase during India's agricultural growing season, when heat also reduces crop yields. The frequent cyclones, flooding and drought in tropical and subtropical regions make sustainable agriculture difficult, and the potential yields of crop production may fall [68]. Climate change threatens the provision of a safe and stable water supply and other vital provisional and regulatory ecosystem services [69,70], and thus endangers the agricultural practices that depend on them. All these can augment the concerns and create mental pressure on marginal farmers who are already facing uncertainties about their ability to thrive or even survive.
Crop loss, income loss, uncertainty about outcomes, inefficient disaster management to protect agriculture, destruction of infrastructure and homesteads, frequency of natural disasters, and limited resources and capacity to cope with shocks exacerbate mental pressure, depression, and anxiety among farmers and their families. Hasan et al. [71] found that the coastal inhabitants of cyclone-prone areas in Bangladesh, most of whom are smallholder farmers, suffered from various types of mental health pressure such as acute stress, sleep disorders, post-traumatic stress disorder [PTSD], anxiety, suicidal ideation, and depression after a cyclone. Nahar et al. [72] noted that a survey conducted in Bangladesh two months after Cyclone Sidr (2007) showed that 25%, 18%, 16%, and 15% of 750 survivors suffered from posttraumatic stress disorders, major depressive disorders, somatoform disorders, and mixed anxiety and depressive disorders, respectively. At the very least, climate change-related ecological grief and eco-anxiety [73] will create mental pressure among farmers apart from post-disaster mental health conditions.
3.4. Occupational health, safety and other health issues
In 2017, 153 billion hours of labour were lost globally owing to heat exposure, 80% of which occurred in the agricultural sector, and labour losses are likely to increase, especially in tropical and subtropical regions [74]. Temperature increases make heat stress more widespread, thus reducing the total number of work hours for smallholder farmers [75]. Climate change-related heat stress and humidity lead to risks for unprotected outdoor workers in unsafe conditions. The health effects of these conditions can lead to loss of work capacity, income, and livelihood opportunities and reduced productivity [76].
In extreme weather events like floods and cyclones, smallholder farmers are also more commonly victims of animal [most commonly snake] and insect bites [50]. In addition, smallholder farmers in many tropical and subtropical countries such as Bangladesh and India are affected by climate change-related frequent lightning [77,78], which often causes death, as they work in harsh weather in the field without any protection [79,80]. This has become a serious issue during the monsoon season for smallholder farmers in both Bangladesh and India [81,82].
Smallholder farmers also face health and safety risks associated with evacuation from disaster [83]. Climate change impacts on smallholder farmers' health and agriculture may increase the migration of smallholder farmers [84,85]. Migrant smallholder farmers will encounter migration-related health issues, such as psychological ill-health, exposure to environmental risk in the destination site, food insecurity, inadequate water and sanitation and infectious diseases [86].
Climate change will hamper the livelihoods of smallholder farmers [12,85]. Their already undermined livelihoods and socio-economic vulnerabilities will be further threatened as the impacts of climate change [86] reduce their low adaptive capacity [12,87] and hinder their access to healthcare facilities to address their health problems.
4. Conclusion and recommendations
In order to continue their livelihoods and produce food, smallholder farmers have learned how to cope, adapt, and develop resilient practices in the settings surrounding their homesteads and farms. As climate change is impacting the environment in which they live and farm, new challenges have been added. Climate change is increasing the incidents of extreme weather events and creating favourable conditions for the emergence and spread of communicable and non-communicable diseases, and smallholder farmers are most often the victims. Smallholder farmers will have to further adapt their agricultural systems as well as face climate change-related health impacts that can reduce work performance, income and productivity and perpetuate a downward spiral into ill health. While facing these challenges, they still have to produce food which is essential for their existence and to provide for the broader population.
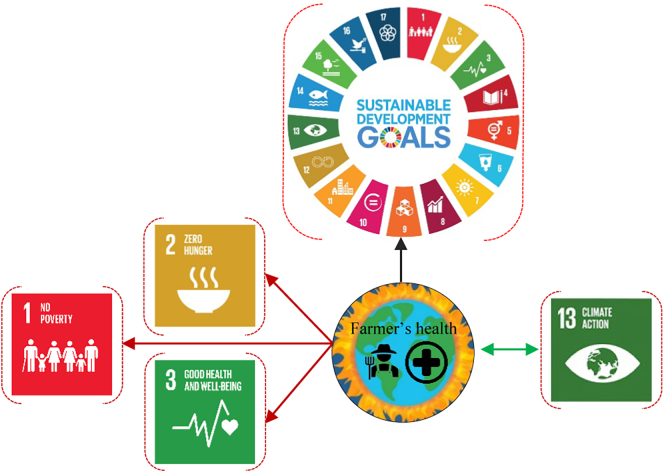
Smallholder farmers provide 70% of kilocalories to the people of Asia and sub-Saharan Africa [6], and are central actors involved in achieving the United Nations' Sustainable Development Goals (SDGs) in many developing countries [88]. They play an especially crucial role in SDG1: No Poverty, SDG 2: Zero Hunger, SGD 3: Good Health and Well-being [89], and SDG 3: Life on Land [88]. The intensifying health impacts of climate change will have profound impacts on their ability to contribute to meeting these goals (see Fig. 5). The COP21 agreement (the 2015 UN Conference of Parties on Climate Change) has emphasised the need to strengthen the adaptive capacity of smallholder farmers for the adaptation of agriculture under climate change scenarios [1].
Fig. 5.
Impacts of smallholder farmers' health on SDGs. Black arrow (→) indicates overall negative impacts on all 17 SDGs, and green arrow ( ) indicates reverse impacts, which means climate action [SDG:15] will reduce the health impacts of climate change on smallholder farmers. Red arrow (
) indicates reverse impacts, which means climate action [SDG:15] will reduce the health impacts of climate change on smallholder farmers. Red arrow ( ) indicates smallholder farmers' health impact of climate change will have serious negative impacts on achiving SDGs: 1, 2 & 3. Note: In the diagram SGD 1: No Poverty, SGD 2: Zero Hunger, SGD 3: Good Health and Well-being, SGD 4: Quality Education, SGD 5: Gender Equality, SGD 6: Clean Water and Sanitation, SGD 7: Affordable and Clean Energy, SGD 8: Decent Work and Economic Growth, SGD 9: Industry, Innovation and Infrastructure, SGD 10: Reducing Inequality, SGD 11: Sustainable Cities and Communities, SGD 12: Responsible Consumption and Production, SGD 13: Climate Action, SGD 14: Life Below Water, SGD 15: Life On Land, SGD 16: Peace, Justice, and Strong Institutions, SGD 17: Partnerships for the Goals. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
) indicates smallholder farmers' health impact of climate change will have serious negative impacts on achiving SDGs: 1, 2 & 3. Note: In the diagram SGD 1: No Poverty, SGD 2: Zero Hunger, SGD 3: Good Health and Well-being, SGD 4: Quality Education, SGD 5: Gender Equality, SGD 6: Clean Water and Sanitation, SGD 7: Affordable and Clean Energy, SGD 8: Decent Work and Economic Growth, SGD 9: Industry, Innovation and Infrastructure, SGD 10: Reducing Inequality, SGD 11: Sustainable Cities and Communities, SGD 12: Responsible Consumption and Production, SGD 13: Climate Action, SGD 14: Life Below Water, SGD 15: Life On Land, SGD 16: Peace, Justice, and Strong Institutions, SGD 17: Partnerships for the Goals. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
COVID-19 has shown how vital smallholder productivity and its contribution to the economy, food security, and sustained agricultural livelihoods are for local communities in a pandemic situation [90,91]. However, smallholder farmers' health has often been neglected in debates about the future of agriculture and left out of policymaking approaches such as climate-smart agriculture, sustainable agricultural intensification, transformation of global food systems, ensuring food and nutritional security, circular agriculture, regenerative agriculture, ecosystem health, poverty reduction, and agroecology-based adaptation.
Most smallholder farmers live in least developed countries [LDCs] in tropical and subtropical regions and fragile conditions. The health impacts of climate change on these farmers exacerbate the poverty cycle, with cascading impacts on global food security. Climate change-related health impacts are a major concern for their coping capacity. Therefore, to minimize the risks of the health impacts of climate change, the following recommendations should be considered at regional and country levels:
-
■
Climate change-related health impacts on smallholder farmers should be given special consideration in public health policy and disaster management.
-
■
Easily understandable digital information systems to explain the climate change-related health impacts on and to smallholder farmers should be created in order to identify the risks as well as to provide more effective and efficient medical services and warning systems.
-
■
Smallholder farmers' welfare and health have to be resilient in facing the effects of extreme weather in order to continue their agricultural activities and ensure local and regional food and nutritional security. Therefore, regional-scale management and protection infrastructures to cope with extreme weather events such as cyclones, flooding, and drought are needed.
-
■
Agricultural extension work should be conducted to introduce climate smart agricultural practices for relevant climate change scenarios.
-
■
Awareness campaigns about the health impacts of climate change directed at small-holder farmers should be developed.
-
■
Health services specific to the health impacts of climate change and targeted for delivery to small holder farmers should be developed.
-
■
Farmers should get access to food aid and nutritional support, as needed.
-
■
Facilities should be created to store their agricultural products during the extreme events.
-
■
Guidance and financial assistance/loans should be provided in order to purchase new equipment needed to adapt and to adopt new management practices to cope with climate change impacts to protect agriculture as well as health. Smallholder farmers will also need market support to keep their livelihoods alive and ensure food security.
-
■
A good understanding of health impacts is essential for better health policy for smallholder farmers, health impact modelling, and forecasting. The health impacts of climate change on smallholder farmers are the outcome of non-linearly connected multidimensional factors, so a complex adaptive system-based framework will be useful in developing a complete, validated, and integrated model of these heath impacts.
-
■
It is essential to increase outreach and strengthen health systems so that they are climate-resilient and responsive and accessible to smallholder farmers.
Declaration of Competing Interest
The authors declare no conflict of interest.
Contributor Information
Byomkesh Talukder, Email: byomkesh.talukder@gmail.com.
James Orbinski, Email: orbinski@yorku.ca.
References
- 1.Ricciardi V., Ramankutty N., Mehrabi Z., Jarvis L., Chookolingo B. How much of the world's food do smallholders produce? Glob. Food Security. 2018;17:64–72. doi: 10.1016/j.gfs.2018.05.002. [DOI] [Google Scholar]
- 2.Khalil C.A., Conforti P., Ergin I., Gennari P. Food Agric. Org. United Nations; 2017. Defining Small-scale Food Producers to Monitor Target 2.3. Of the 2030 Agenda for Sustainable Development; p. 17.http://www.fao.org/3/i6858e/i6858e.pdf [Google Scholar]
- 3.Herrero M., Thornton P.K., Power B., Bogard J.R., Remans R., Fritz S.…Havlík P. Farming and the geography of nutrient production for human use: a transdisciplinary analysis. Lancet Planet. Health. 2017;1(1):e33–e42. doi: 10.1016/S2542-5196(17)30007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lowder S.K., Skoet J., Raney T. The number, size, and distribution of farms, smallholder farms, and family farms worldwide. World Dev. 2016;87:16–29. doi: 10.1016/j.worlddev.2015.10.041. [DOI] [Google Scholar]
- 5.WB . World Bank; 2016. A Year in the Lives of Smallholder Farmers.https://www.worldbank.org/en/news/feature/2016/02/25/a-year-in-the-lives-of-smallholder-farming-families [Google Scholar]
- 6.Fanzo J. From big to small: the significance of smallholder farms in the global food system. Lancet Planet. Health. 2017;1:e15–e16. doi: 10.1016/S2542-5196(17)30011-6. [DOI] [PubMed] [Google Scholar]
- 7.Andrade J. IISD; 2016. Smallholder Farmers and Enabling Their Access to Sustainable Markets Commentary Report. 2016 State of Sustainability Initiatives.https://www.iisd.org/ssi/wp-content/uploads/2019/09/Smallholders_publication.pdf [Google Scholar]
- 8.IFAD aand UNEP . International Fund for Agricultural Development; Rome: 2013. Smallholders, Food Security and the Environment.https://www.ifad.org/documents/38714170/39135645/smallholders_report.pdf/133e8903-0204-4e7d-a780-bca847933f2e [Google Scholar]
- 9.Lowder S.K., Sánchez M.V., Bertini R. Farms, Family Farms, Farmland Distribution and Farm Labour: What Do We Know Today? 2019. http://www.fao.org/3/ca7036en/ca7036en.pdf 854-2020-093.
- 10.CFS . Committee on World Food Security, Food and Agriculture Organization of the United Nations; 2020. Connecting Smallholders to Markets.http://www.fao.org/cfs/home/activities/smallholders/en/ [Google Scholar]
- 11.Fan S., Brzeska J., Keyzer M., Halsema A. Intl Food Policy Res Inst.; 2013. From Subsistence to Profit: Transforming smallholder Farms (Vol. 26) [Google Scholar]
- 12.Harvey C.A., Saborio-Rodríguez M., Martinez-Rodríguez M.R., Viguera B., Chain-Guadarrama A., Vignola R., Alpizar F. Climate change impacts and adaptation among smallholder farmers in Central America. Agricult. Food Security. 2018;7(1):1–20. doi: 10.1186/s40066-018-0209-x. [DOI] [Google Scholar]
- 13.Moher D., Liberati A., Tetzlaff J., Altman D.G., Prisma Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maplecroft World: Climate Change Vulnerability Index 2014. 2014. https://reliefweb.int/sites/reliefweb.int/files/resources/Climate_Change_Vulnerability_Index_%202014_Map_0.pdf
- 15.Mann M.E., Rahmstorf S., Kornhuber K., Steinman B.A., Miller S.K., Coumou D. Influence of anthropogenic climate change on planetary wave resonance and extreme weather events. Sci. Rep. 2017;7:45242. doi: 10.1038/srep45242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bathiany S., Dakos V., Scheffer M., Lenton T.M. Climate models predict increasing temperature variability in poor countries. Sci. Adv. 2018;4(5) doi: 10.1126/sciadv.aar5809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.ILO . SafeWork, Programme on Safety, Health and the Environment. Labour Protection Department International Labour Office; 2000. Safety and health in agriculture.https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---safework/documents/publication/wcms_110193.pdf [Google Scholar]
- 18.EU . European Joint Research Centre; 2019. World Atlas of Desertification. Feeding a Growing Global Population. Smallholder Agriculture.https://wad.jrc.ec.europa.eu/smallholderagriculture [Google Scholar]
- 19.Saikkonen K., Taulavuori K., Hyvönen T., Gundel P.E., Hamilton C.E., Vänninen I.…Helander M. Climate change-driven species' range shifts filtered by photoperiodism. Nat. Clim. Chang. 2012;2(4):239–242. doi: 10.1038/NCLIMATE1430. [DOI] [Google Scholar]
- 20.Munich R.E. Loss Events Worldwide 2014. Geographical overview. 2014. https://reliefweb.int/sites/reliefweb.int/files/resources/Munich-Re-World-map-Natural-catastrophes-2014.pdf
- 21.Chan E.H., Brewer T.F., Madoff L.C., Pollack M.P., Sonricker A.L., Keller M.…Brownstein J.S. Global capacity for emerging infectious disease detection. Proc. Natl. Acad. Sci. 2010;107(50):21701–21706. doi: 10.1073/pnas.1006219107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.CAT The CAT Thermometer. Climate Action Tracker (CAT) 2019. https://climateactiontracker.org/global/cat-thermometer/
- 23.Byrne M.P., O’Gorman P.A. Trends in continental temperature and humidity directly linked to ocean warming. Proc. Natl. Acad. Sci. 2018;115(19):4863–4868. doi: 10.1073/pnas.1722312115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seneviratne S.I., Nicholls N., Easterling D., Goodess C.M., Kanae S., Kossin J., Luo Y., Marengo J., McInnes K., Rahimi M., Reichstein M., Sorteberg A., Vera C., Zhang X. Changes in climate extremes and their impacts on the natural physical environment. In: Field C.B., Barros V., Stocker T.F., Qin D., Dokken D.J., Ebi K.L., …Midgley P.M., editors. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. Cambridge University Press; Cambridge, UK, and New York, NY, USA: 2012. pp. 109–230.https://www.ipcc.ch/site/assets/uploads/2018/03/SREX-Chap3_FINAL-1.pdf (A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change (IPCC)). [Google Scholar]
- 25.McMichael A.J. Extreme weather events and infectious disease outbreaks. Virulence. 2015;6(6):543–547. doi: 10.4161/21505594.2014.975022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mendelsohn R., Emanuel K., Chonabayashi S., Bakkensen L. The impact of climate change on global tropical cyclone damage. Nat. Clim. Chang. 2012;2(3):205–209. doi: 10.1038/NCLIMATE1357. [DOI] [Google Scholar]
- 27.Zheng J., Han W., Jiang B., Ma W., Zhang Y. Infectious diseases and tropical cyclones in Southeast China. Int. J. Environ. Res. Public Health. 2017;14(5):494. doi: 10.3390/ijerph14050494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Myint N.W., Kaewkungwal J., Singhasivanon P., Chaisiri K., Panjapiyakul P., Siriwan P.…Mu T.T. Are there any changes in burden and management of communicable diseases in areas affected by cyclone Nargis? Confl. Heal. 2011;5(1):9. doi: 10.1186/1752-1505-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang R., Xun H., Zhang Y., Wang W., Wang X., Jiang B., Ma W. Impacts of different grades of tropical cyclones on infectious diarrhea in Guangdong, 2005-2011. PLoS One. 2015;10(6) doi: 10.1371/journal.pone.0131423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hirabayashi Y., Mahendran R., Koirala S., Konoshima L., Yamazaki D., Watanabe S.…Kanae S. Global flood risk under climate change. Nat. Clim. Chang. 2013;3(9):816–821. doi: 10.1038/NCLIMATE1911. [DOI] [Google Scholar]
- 31.Marsooli R., Lin N., Emanuel K., Feng K. Climate change exacerbates hurricane flood hazards along US Atlantic and Gulf Coasts in spatially varying patterns. Nat. Commun. 2019;10(1):1–9. doi: 10.1038/s41467-019-11755-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown L., Murray V. Examining the relationship between infectious diseases and flooding in Europe: a systematic literature review and summary of possible public health interventions. Disaster Health. 2013;1(2):117–127. doi: 10.4161/dish.25216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carrão H., Naumann G., Barbosa P. Mapping global patterns of drought risk: an empirical framework based on sub-national estimates of hazard, exposure and vulnerability. Glob. Environ. Chang. 2016;39:108–124. doi: 10.1016/j.gloenvcha.2016.04.012. [DOI] [Google Scholar]
- 34.CDC . Centres for Diseases Control and Preventions; 2020. Health Implications of Drought.https://www.cdc.gov/nceh/drought/implications.htm [Google Scholar]
- 35.Shi M., Sun Y., Wang Z., He G., Quan H., He H. Plastic film mulching increased the accumulation and human health risks of phthalate esters in wheat grains. Environ. Pollut. 2019;250:1–7. doi: 10.1016/j.envpol.2019.03.064. [DOI] [PubMed] [Google Scholar]
- 36.Lye D.J. Health risks associated with consumption of untreated water from household roof catchment systems 1. JAWRA J. Am. Water Resour. Assoc. 2002;38(5):1301–1306. doi: 10.1111/j.1752-1688.2002.tb04349.x. [DOI] [Google Scholar]
- 37.Campbell-Lendrum D., Manga L., Bagayoko M., Sommerfeld J. Climate change and vector-borne diseases: what are the implications for public health research and policy? Philos. Trans. R. Soc. B: Biol. Sci. 2015;370(1665):20130552. doi: 10.1098/rstb.2013.0552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watts Health and climate change: policy responses to protect public health. Lancet. 2015;386(10006):1861–1914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 39.Paz S., Semenza J.C. El Niño and climate change—contributing factors in the dispersal of Zika virus in the Americas? Lancet. 2016;387(10020):745. doi: 10.1016/S0140-6736(16)00256-7. [DOI] [PubMed] [Google Scholar]
- 40.Tirado M.C., Clarke R., Jaykus L.A., McQuatters-Gollop A., Frank J.M. Climate change and food safety: a review. Food Res. Int. 2010;43(7):1745–1765. doi: 10.1016/j.foodres.2010.07.003. [DOI] [Google Scholar]
- 41.Battilani P., Toscano P., Van der Fels-Klerx H.J., Moretti A., Leggieri M.C., Brera C.…Robinson T. Aflatoxin B 1 contamination in maize in Europe increases due to climate change. Sci. Rep. 2016;6 doi: 10.1038/srep24328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Greenough G., McGeehin M., Bernard S.M., Trtanj J., Riad J., Engelberg D. The potential impacts of climate variability and change on health impacts of extreme weather events in the United States. Environ. Health Perspect. 2001;109(Suppl. 2):191–198. doi: 10.1289/ehp.109-1240666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.PAHO and WHO . Pan American Health Organization; Washington, DC: 2017. Epidemic of Chronic Kidney Disease in Agricultural Communities in Central America: Case Definitions, Methodological Basis and Approaches for Public Health Surveillance.https://iris.paho.org/handle/10665.2/34132 [Google Scholar]
- 44.Friel S., Bowen K., Campbell-Lendrum D., Frumkin H., McMichael A.J., Rasanathan K. Climate change, noncommunicable diseases, and development: the relationships and common policy opportunities. Annu. Rev. Public Health. 2011;32:133–147. doi: 10.1146/annurev-publhealth-071910-140612. [DOI] [PubMed] [Google Scholar]
- 45.Johnson R.J., Wesseling C., Newman L.S. Chronic kidney disease of unknown cause in agricultural communities. N. Engl. J. Med. 2019;380(19):1843–1852. doi: 10.1056/NEJMra1813869. [DOI] [PubMed] [Google Scholar]
- 46.PAHO and WHO . Pan American Health Organization and World Health organization; 2020. Climate Change for Health Professionals, a Pocketbook.https://iris.paho.org/bitstream/handle/10665.2/52930/9789275122839_eng.pdf?sequence=5 [Google Scholar]
- 47.Sorensen C., Garcia-Trabanino R. A new era of climate medicine — Addressing heat-triggered renal disease. N. Engl. J. Med. 2019;381(8):693–696. doi: 10.1056/NEJMp1907859. [DOI] [PubMed] [Google Scholar]
- 48.WHO . WHO Regional Office for Europe; 2011. Public Health Advice on Preventing Health Effects of Heat, New and Updated Information for Different Audiences.https://www.euro.who.int/__data/assets/pdf_file/0007/147265/Heat_information_sheet.pdf?ua=1 [Google Scholar]
- 49.Guo Y., Gasparrini A., Li S., Sera F., Vicedo-Cabrera A.M., de Sousa Zanotti Stagliorio Coelho M.…Overcenco A. Quantifying excess deaths related to heatwaves under climate change scenarios: a multicountry time series modelling study. PLoS Med. 2018;15(7) doi: 10.1371/journal.pmed.1002629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Okaka F.O., Odhiambo B. Relationship between flooding and outbreak of infectious diseases in Kenya: a review of the literature. J. Environ. Public Health. 2018;2018 doi: 10.1155/2018/5452938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.IWGCCH . Environmental Health perspectives and National Institute of Environmental Health Sciences; Research Triangle Park, NC: 2010. A Human Health Perspective on Climate Change. A Report Outlining the Research Needs on the Human Health Effects of Climate Change.https://factor.niehs.nih.gov/2014/6/science-climate/file692195_508.pdf [Google Scholar]
- 52.Wells M.L., Trainer V.L., Smayda T.J., Karlson B.S., Trick C.G., Kudela R.M.…Cochlan W.P. Harmful algal blooms and climate change: learning from the past and present to forecast the future. Harmful Algae. 2015;49:68–93. doi: 10.1016/j.hal.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bidartondo M.I., Ellis C., Kauserud H., Kennedy P.G., Lilleskov E., Suz L., Andrew C. Climate change: Fungal responses and effects. In: Willis Katherine J., editor. State of the World’s Fungi 2018. Royal Botanical Gardens, Kew, UK. 2018. pp. 62–69.https://www.fs.fed.us/nrs/pubs/jrnl/2018/nrs_2018_bidartondo_001.pdf [Google Scholar]
- 54.FAO . FAO; Rome, Italy: 2015. The Impact of Disasters on Agriculture and Food Security.http://www.fao.org/3/a-i5128e.pdf [Google Scholar]
- 55.Myers S.S., Smith M.R., Guth S., Golden C.D., Vaitla B., Mueller N.D.…Huybers P. Climate change and global food systems: potential impacts on food security and undernutrition. Annu. Rev. Public Health. 2017;38:259–277. doi: 10.1146/annurev-publhealth-031816-044356. [DOI] [PubMed] [Google Scholar]
- 56.Black R.E., Allen L.H., Bhutta Z.A., Caulfield L.E., De Onis M., Ezzati M.…Maternal and Child Undernutrition Study Group Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–260. doi: 10.1016/S01406736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 57.Scheelbeek P.F., Chowdhury M.A., Haines A., Alam D.S., Hoque M.A., Butler A.P.…Vineis P. Drinking water salinity and raised blood pressure: evidence from a cohort study in coastal Bangladesh. Environ. Health Perspect. 2017;125(5) doi: 10.1289/EHP659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khan A.E., Scheelbeek P.F.D., Shilpi A.B., Chan Q., Mojumder S.K., Rahman A.…Vineis P. Salinity in drinking water and the risk of (pre) eclampsia and gestational hypertension in coastal Bangladesh: a case-control study. PLoS One. 2014;9(9) doi: 10.1371/journal.pone.0108715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nahian M.A., Ahmed A., Lázár A.N., Hutton C.W., Salehin M., Streatfield P.K.…Renaud F. Elementa: Science of the Anthropocene. 2018. Drinking water salinity associated health crisis in coastal Bangladesh; p. 6. [DOI] [Google Scholar]
- 60.Stocher D.P., Klein C.P., Saccomori A.B., August P.M., Martins N.C., Couto P.R.…Matté C. Maternal high-salt diet alters redox state and mitochondrial function in newborn rat offspring's brain. Br. J. Nutr. 2018;119(9):1003–1011. doi: 10.1017/S0007114518000235. [DOI] [PubMed] [Google Scholar]
- 61.Talukder M.R.R., Rutherford S., Chu C., Hieu Nguyen T., Phung D. Association between salinity and hospital admission for hypertension: an ecological case–control study in the Mekong Delta region in Vietnam. J. Public Health. 2018;40(1):75–81. doi: 10.1093/pubmed/fdx041. [DOI] [PubMed] [Google Scholar]
- 62.Aryal J.P., Sapkota T.B., Rahut D.B., Krupnik T.J., Shahrin S., Jat M.L., Stirling C.M. Major climate risks and adaptation strategies of smallholder farmers in coastal Bangladesh. Environ. Manag. 2020;66:105–120. doi: 10.1007/s00267-020-01291-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khan J.R., Awan N., Archie R.J., Sultana N., Muurlink O. The association between drinking water salinity and hypertension in coastal Bangladesh. Glob. Health J. 2020;4(4):153–158. doi: 10.1016/j.glohj.2020.11.001. [DOI] [Google Scholar]
- 64.Graham H., White P., Cotton J., McManus S. Flood-and weather-damaged homes and mental health: an analysis using England’s mental health survey. Int. J. Environ. Res. Public Health. 2019;16(18):3256. doi: 10.3390/ijerph16183256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.UNFCCC Slow Onset Events. 2012. https://unfccc.int/resource/docs/2012/tp/07.pdf Technical paper. United nations Framework Convention on Climate Change. UN.
- 66.HRC The Slow Onset Effects of Climate Change and Human Rights Protection for Cross-Border Migrants. 2018. https://reliefweb.int/sites/reliefweb.int/files/resources/A_HRC_37_CRP.pdf Annual report of the United Nations High Commissioner for Human Rights and reports of the Office of the High Commissioner and the Secretary-General.
- 67.Carleton T.A. Crop-damaging temperatures increase suicide rates in India. Proc. Natl. Acad. Sci. 2017;114(33):8746–8751. doi: 10.1073/pnas.1701354114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hoegh-Guldberg O., Jacob D., Taylor M., Bindi M., Brown S., Camilloni I., Diedhiou A., Djalante R., Ebi K.L., Engelbrecht F., Guiot J., Hijioka Y., Mehrotra S., Payne A., Seneviratne S.I., Thomas A., Warren R., Zhou G. Impacts of 1.5°C Global Warming on Natural and Human Systems. In: Masson-Delmotte V., Zhai P., Pörtner H.-O., Roberts D., Skea J., Shukla P.R., …Waterfield T., editors. Global Warming of 1.5°C. An IPCC Special Report on the Impacts of Global Warming of 1.5°C Above Pre-industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty. 2018. https://www.ipcc.ch/site/assets/uploads/sites/2/2019/06/SR15_Chapter3_Low_Res.pdf In Press. [Google Scholar]
- 69.IUCN . International Union for Conservation of Nature; 2015. Water and Climate Change.https://www.iucn.org/sites/dev/files/import/downloads/water_and_climate_change_issues_brief.pdf Building climate change resilience through water management and ecosystems. Issues Brief. [Google Scholar]
- 70.FAO . FAO; 2011. Climate Change, Water and Food Security.http://www.fao.org/3/i2096e/i2096e.pdf FAO Water Reports 36. [Google Scholar]
- 71.Hasan M.T., Adhikary G., Mahmood S., Papri N., Shihab H.M., Kasujja R.…Nasreen M. Exploring mental health needs and services among affected population in a cyclone affected area in costal Bangladesh: a qualitative case study. Int. J. Ment. Heal. Syst. 2020;14(1):1–9. doi: 10.1186/s13033-020-00351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nahar N., Blomstedt Y., Wu B., Kandarina I., Trisnantoro L., Kinsman J. Increasing the provision of mental health care for vulnerable, disaster-affected people in Bangladesh. BMC Public Health. 2014;14(1):708. doi: 10.1186/1471-2458-14-708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cunsolo A., Harper S.L., Minor K., Hayes K., Williams K.G., Howard C. Ecological grief and anxiety: the start of a healthy response to climate change? Lancet Planet. Health. 2020;4(7):e261–e263. doi: 10.1016/S2542-5196(20)30144-3. https://www.thelancet.com/pdfs/journals/lanplh/PIIS2542-5196(20)30144-3.pdf [DOI] [PubMed] [Google Scholar]
- 74.Haines A., Ebi K. The imperative for climate action to protect health. N. Engl. J. Med. 2019;380(3):263–273. doi: 10.1056/NEJMra1807873. [DOI] [PubMed] [Google Scholar]
- 75.ILO . International Labour Organization; Geneva: 2019. Working on a Warmer Planet: The Impact of Heat Stress on Labour Productivity and Decent Work.https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/---publ/documents/publication/wcms_711919.pdf [Google Scholar]
- 76.Moda H.M., Minhas A. Impacts of climate change on outdoor workers and their safety: some research priorities. Int. J. Environ. Res. Public Health. 2019;16(18):3458. doi: 10.3390/ijerph16183458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Singh M.S., Kuang Z., Maloney E.D., Hannah W.M., Wolding B.O. Increasing potential for intense tropical and subtropical thunderstorms under global warming. Proc. Natl. Acad. Sci. 2017;114(44):11657–11662. doi: 10.1073/pnas.1707603114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.FAO . FAO; 2018. The Impact of Disasters and Crises on Agriculture and Food Security.http://www.fao.org/3/I8656EN/i8656en.pdf Report. [Google Scholar]
- 79.Biswas, A., Dalal, K., Hossain, J., Baset, K. U., Rahman, F., & Mashreky, S. R. (2016). Lightning injury is a disaster in Bangladesh?-Exploring its magnitude and public health needs. F1000Research, 5. doi:10.12688/f1000research.9537.1. [DOI] [PMC free article] [PubMed]
- 80.Holle R.L. International Conference on Lightning Protection (ICLP 2016) 2016. Lightning-caused deaths and injuries related to agriculture; pp. 1–6.https://my.vaisala.net/Vaisala%20Documents/Scientific%20papers/2016%20ILDC%20ILMC/Ron%20Holle.%20Lightning-caused%20Deaths%20and%20Injuries.pdf [Google Scholar]
- 81.Singh O., Singh J. Lightning fatalities over India: 1979–2011. Meteorol. Appl. 2015;22(4):770–778. doi: 10.1002/met.1520. [DOI] [Google Scholar]
- 82.Holle R.L., Dewan A., Said R., Brooks W.A., Hossain M.F., Rafiuddin M. Fatalities related to lightning occurrence and agriculture in Bangladesh. Int. J. Disaster Risk Reduct. 2019;41:101264. doi: 10.1016/j.ijdrr.2019.101264. [DOI] [Google Scholar]
- 83.Chapagain T., Raizada M.N. Impacts of natural disasters on smallholder farmers: gaps and recommendations. Agricult. Food Security. 2017;6(1):1–16. doi: 10.1186/s40066-017-0116-6. [DOI] [Google Scholar]
- 84.CTA and IFPRI . A Series of Meetings on ACP-EU Development Issues: Brussels Rural Development Briefings. 2013. Agricultural resilience in the face of crisis and shocks.https://brusselsbriefings.files.wordpress.com/2009/02/cta-reader-30_agricultural-resilience-eng-rev-2.pdf [Google Scholar]
- 85.Cohn A.S., Newton P., Gil J.D., Kuhl L., Samberg L., Ricciardi V.…Northrop S. Smallholder agriculture and climate change. Annu. Rev. Environ. Resour. 2017;42:347–375. doi: 10.1146/annurev-environ-102016-060946. [DOI] [Google Scholar]
- 86.Schwerdtle P., Bowen K., McMichael C. The health impacts of climate-related migration. BMC Med. 2018;16(1):1–7. doi: 10.1186/s12916-017-0981-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Holland M.B., Shamer S.Z., Imbach P., Zamora J.C., Moreno C.M., Hidalgo E.J.L.…Harvey C.A. Mapping adaptive capacity and smallholder agriculture: applying expert knowledge at the landscape scale. Clim. Chang. 2017;141(1):139–153. doi: 10.1007/s10584-016-1810-2. [DOI] [Google Scholar]
- 88.FAO and IFAD . FAO and IFAD; 2019. Putting Family Farmers at the Centre to Achieve the SDGs.http://www.fao.org/3/ca4532en/ca4532en.pdf [Google Scholar]
- 89.FAO Enabling Smallholders and Family Farmers to Access Appropriate Innovation, Information and Advisory Services for Sustainable Agrifood Systems. 2020. http://www.fao.org/3/nd410en/nd410en.pdf Executive Summary. Committee on Agriculture. 28 September - 2 October 2020.
- 90.Bhavani R.V., Gopinath R. The COVID19 pandemic crisis and the relevance of a farm-system-for-nutrition approach. Food Security. 2020;12(4):881–884. doi: 10.1007/s12571-020-01071-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.FAO . FAO; 2020. COVID-19 and the Role of Local Food Production in Building more Resilient Local Food Systems.http://www.fao.org/3/cb1020en/CB1020EN.pdf [Google Scholar]