Abstract
The new dumbbell‐shaped, covered self‐expanding metallic stent can efficiently remove the choledocholiths in cases with common bile duct (CBD) strictures; moreover, it may potentially prevent a positional displacement and contribute to the better improvement of the CBD stricture.
Keywords: benign biliary stricture, chronic pancreatitis, common bile duct stones
The new dumbbell‐shaped, covered self‐expanding metallic stent can efficiently remove the choledocholiths in cases with common bile duct (CBD) strictures; moreover, it may potentially prevent a positional displacement and contribute to the better improvement of the CBD stricture.

1. INTRODUCTION
Endoscopic removal of bile stones is challenging in cases with a distal stricture of the common bile duct. A new dumbbell‐shaped covered self‐expanding metallic stent can efficiently remove the common bile duct stones in cases with stricture of the common bile duct caused by chronic pancreatitis.
Common bile duct (CBD) stones are usually a risk factor for cholangitis; hence, their removal is recommended. Surgical or endoscopic lithotomy is the preferred treatment modality to remove the CBD stones. Endoscopic lithotomy has become the first choice of treatment as it is a minimally invasive procedure.
Removal of CBD stones by endoscopic lithotomy may be challenging in patients with a very large stone size, multiple stones packed closely, 1 , 2 , 3 , 4 , 5 a history of digestive tract reconstruction, 6 , 7 or a combination of these factors. In addition to these factors, the presence of a CBD stricture also increases the difficulty of endoscopic lithotomy. 8 , 9 , 10 If a distal CBD stricture is narrower than the diameter of the CBD stones, removing the stones becomes further complicated.
We report a case in which the removal of CBD stones was difficult due to a CBD stricture caused by chronic pancreatitis (CP); hence, endoscopic lithotripsy was also challenging. However, the stones were spontaneously removed following the insertion of a covered self‐expanding metallic stent (CSEMS).
2. CASE PRESENTATION
A 65‐year‐old man was admitted to our hospital for a periodic medical examination for CP. He also underwent periodic imaging examinations during follow‐up, for the last 10 years, for a benign biliary stricture caused by CP. Magnetic resonance cholangiopancreatography (MRCP) conducted as a part of these examinations revealed multiple CBD stones (Figure 1A). Contrast‐enhanced computed tomography performed 6 months before the MRCP had not revealed stones in the CBD; however, gallbladder stones were seen. It was presumed that the gallbladder stones had now progressively moved to the CBD. Therefore, we performed an endoscopic therapy for the CBD stones.
FIGURE 1.
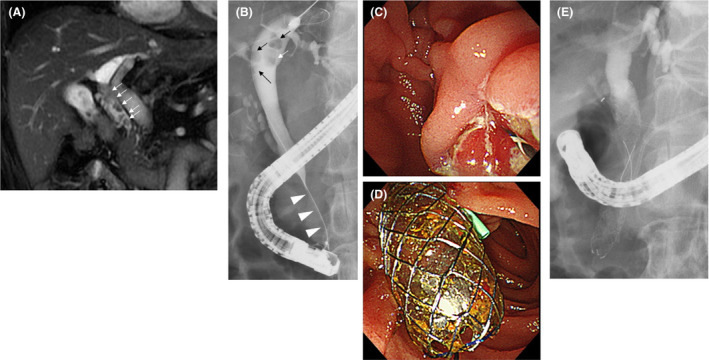
The clinical course until the first endoscopic retrograde cholangiopancreatography (ERCP). A, Common bile duct (CBD) stones (arrow) were detected on magnetic resonance cholangiopancreatography. B, In addition to the CBD stones (arrow), distal CBD stricture (arrowhead) was observed on endoscopic cholangiography. C, After cholangiography, endoscopic sphincterotomy was performed. D, E, A covered self‐expandable metallic stent was placed to dilate the distal CBD stricture after the pancreatic stent was inserted to prevent post‐ERCP pancreatitis
An endoscopic cholangiography revealed a stricture of the distal CBD and four CBD stones. The shortest diameter of each of the four stones (6, 5, 4, and 3 mm) was larger than the diameter of the distal CBD lumen (Figure 1B); therefore, endoscopic extraction of the stones was challenging. After endoscopic sphincterotomy (Figure 1C), we attempted to remove the CBD stones using a basket catheter, which is often used for the destruction of stones. However, the movement of the basket catheter was limited by the biliary stricture. Therefore, the basket catheter could only hold a small stone but could not extract them. The distal biliary duct was extremely narrow. Therefore, there was a possibility that the placement of multiple biliary plastic stents would be difficult, or they would not dilate the distal biliary stricture adequately to remove the CBD stones. Additionally, no pancreatic atrophy was observed during the imaging examinations. Due to the risk of injury to the pancreatic parenchyma, we did not perform dilatation with a balloon catheter. Considering all these factors, a CSEMS was placed to dilate the distal CBD stricture (Figure 1D–E). The CSEMS used in this case was BONASTENT M‐intraductal 8 mm 7 cm (Standard Sci Tech). The stent has a dumbbell shape, with an 8 mm diameter at both ends and a 6 mm diameter at the center (Figure 2). The distal tip of the stent was pushed out from the duodenum to prevent proximal migration of the stent. Due to the flared tips of the BONASTENT M‐intraductal, the risk of proximal migration of the stent is reduced. The diameter of the CSEMS (8 mm) was the same as the diameter of the CBD. The length of the distal biliary stricture was 3 cm. A 7 or 6 cm‐long stent had a midportion length of 2 cm, which is the longest BONASTENT M‐intraductal available commercially. In this case, the superior portion of the distal biliary stricture was slightly narrow. Therefore, we selected a longer stent of 7 cm. Before the CSEMS insertion, a 5‐Fr 12 cm straight pancreatic stent was placed in the main pancreatic duct to prevent postendoscopic retrograde cholangiopancreatography pancreatitis. 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19
FIGURE 2.
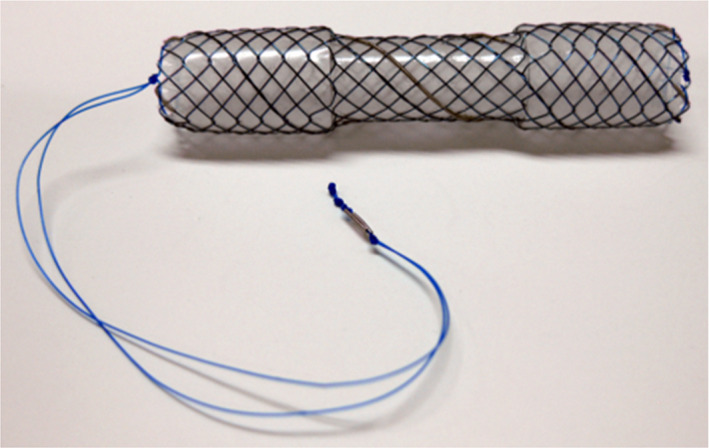
The covered self‐expandable metallic stent (CSEMS) used in this case was the BONASTENT M‐intraductal. The shape of the stent resembles a dumbbell. By pulling a string, the BONASTENT M‐intraductal becomes narrower. Therefore, the CSEMS is easy to remove
Endoscopic cholangiography was repeated a week after the first cholangiography. We observed that all the CBD stones detected in the initial cholangiography had disappeared spontaneously (Figure 3A). After the CSEMS removal, the biliary sludge was removed using a balloon catheter (Figure 3B). We confirmed that there were no stones in the CBD, and the stricture of the distal CBD showed slight improvement (Figure 3C). Finally, the pancreatic stent was removed.
FIGURE 3.
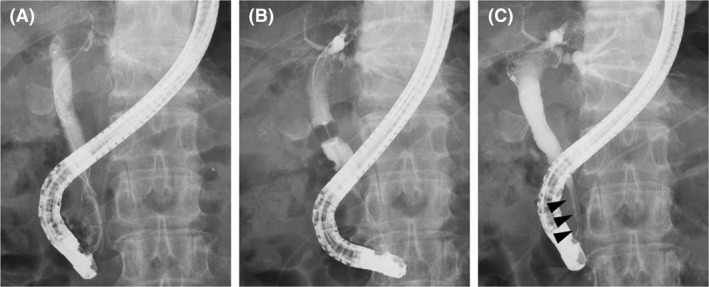
The findings of the second endoscopic cholangiography. A, No stones in the common bile duct (CBD) were observed. B, After the covered self‐expandable metallic stent was removed, the biliary sludge was removed by a balloon catheter. C, It was confirmed that the stricture of distal CBD was improved to some extent (arrowhead)
Approximately a year after the CBD stones were removed using the CSEMS, no recurrence of the CBD stones was observed on the follow‐up imaging at an outpatient clinic.
3. DISCUSSION
There are three reports in the literature about cases of CBD stones with distal CBD strictures that were treated using CSEMS (Table 1). However, two case series did not mention the details of the cases with CBD stones and distal CBD strictures. A case series by Cerefice et al 8 comprised cases in which the CBD stones were difficult to remove using conventional endoscopic methods. Another case series by García‐Cano et al 10 comprised older patients who had difficulty in tolerating the endoscopic lithotripsy due to the long duration of the procedure.
TABLE 1.
Previous reports of CBD stones with distant CBD stricture treated using CSEMS
| First author, y | Number of cases with CBD stricture | Reason for CBD stricture | CSEMS | Duration of CSEMS insertion | All stone removal |
|---|---|---|---|---|---|
| Cerefice et al, 2011 8 | 5 | NA | Wallstent or Viabil | NA in patients with distant CBD stricture | |
| Okabe et al, 2012 9 | 1 | CP | Wall Flex | 2 wk | Achieved by lithotripsy |
| García‐Cano et al, 2013 10 | 11 | NA | Wall Flex | 90‐389 d | 7/11 |
| This case | 1 | CP | BONASTENT M‐intraductal | 7 d | Spontaneously disappeared |
Abbreviations: CBD, common bile duct; CP, chronic pancreatitis; CSEMS, covered self‐expandable metallic stent; NA, not available.
A case report by Okabe et al 9 described a case of CBD stones and distal CBD stricture due to CP. The CBD stones remained in the biliary duct and the upper portion of the CSEMS, and the distal biliary stricture did not improve despite CSEMS placement for 14 days. In contrast, the CBD stones spontaneously disappeared in our case, and the distal biliary stricture also improved slightly after the placement of the CSEMS for only 7 days. This indicates that the new CSEMS BONASTENT M‐intraductal (Standard Sci Tech) can lead to good dilatation. The stent's dumbbell shape was thought to slightly prevent stent migration and transmit a dilation force to the CBD stricture.
The CSEMS should be placed for a longer duration to avoid recurrence of the CBD stones. Although CSEMS dilated the distal CBD stricture, the distal CBD remained thin (Figure 3C). In the previous reports, the duration and effectiveness of the CSEMS placement for CBD strictures secondary to CP were variable. Cahen et al 20 reported six cases that received CSEMS for CBD stricture with CP. They reported the CSEMS removal time to be 3‐6 months and that 66% of the CBD strictures showed improvement. Lalezari et al 21 reported a case with CP in which the CBD was dilated by CSEMS. In this report, the CSEMS was placed for 63 days, and the CBD stricture had improved. Haapamäki et al 22 conducted a randomized controlled study on the effectiveness of multiple plastic stents vs the CSEMS in treating biliary stricture with CP. In this study, CSEMS was removed 6 months after randomization, and the 2‐year stricture‐free success rate was 92% (24/26). Although the targets were not CP patients alone, Park et al 23 increased the duration of CSEMS placement to ≥120 days for resolution of the CBD stricture.
However, complications such as migration and embedment have been reported when the CSEMS was left in place for a longer duration. 10 , 20 , 23 , 24 , 25 A new dumbbell‐shaped CSEMS is thought to be useful in preventing migration. The duodenal tip of the dumbbell shape can prevent the embedment and migration into the biliary tract superiorly, while the hilar tip can prevent duodenal migration. If the new dumbbell‐shaped CSEMS migrates into the biliary tract superiorly, removal of the stent is thought to be easier than removing other types of the CSEMSs, primarily because the dumbbell‐shaped CSEMS becomes narrower by pulling a string that is attached at the duodenal tip (Figure 2). Park et al 23 described that migration of the CSEMS is a risk factor that prevents the resolution of benign CBD strictures. The dumbbell shape is expected to prevent migration and dilate the CBD stricture effectively. In fact, in this case, the CBD stricture was slightly dilated after CSEMS placement for only 7 days.
In conclusion, the new dumbbell‐shaped CSEMS is efficient in removing the CBD stones with CBD strictures that occur due to CP. The stent might have the potential to prevent positional displacement and contribute to the dilation of the CBD stricture.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTION
YI, MS, and TT: wrote the paper. RS, NK, HA, YS, HI, YO, JN, MT, MH, TK, RK, and TH: provided clinical advice. HO: reviewed and wrote the paper.
ETHICAL APPROVAL
Informed consent was obtained from the patient for inclusion in the study. All procedures were approved by the Institutional Review Board of Fukushima Medical University (approved number: 2453).
ACKNOWLEDGMENTS
We thank all the staff at the Department of Gastroenterology of Fukushima Medical University, the Department of Endoscopy of Fukushima Medical University Hospital, and the gastroenterology ward of Fukushima Medical University Hospital. We also thank editage for providing English language revision.
Ishizaki Y, Sugimoto M, Takagi T, et al. Spontaneous disappearance of common bile duct stones following the insertion of a new dumbbell‐shaped, covered self‐expandable metallic stent in a patient with benign biliary stricture. Clin Case Rep. 2021;9:e04093. 10.1002/ccr3.4093
Funding information
Department of Gastroenterology, Fukushima Medical University.
DATA AVAILABILITY STATEMENT
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57(2):156‐159. [DOI] [PubMed] [Google Scholar]
- 2. Meine GC, Baron TH. Endoscopic papillary large‐balloon dilation combined with endoscopic biliary sphincterotomy for the removal of bile duct stones (with video). Gastrointest Endosc. 2011;74(5):1119‐1126; quiz 1115 e1111‐1115. [DOI] [PubMed] [Google Scholar]
- 3. Garcia‐Cano J, Arana LT, Ayllon CJ, et al. Biliary sphincterotomy dilation for the extraction of difficult common bile duct stones. Rev Esp Enferm Dig. 2009;101(8):541‐545. [DOI] [PubMed] [Google Scholar]
- 4. Itoi T, Itokawa F, Sofuni A, et al. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104(3):560‐565. [DOI] [PubMed] [Google Scholar]
- 5. Kim HG, Cheon YK, Cho YD, et al. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J Gastroenterol. 2009;15(34):4298‐4304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Park TY, Bang CS, Choi SH, et al. Forward‐viewing endoscope for ERCP in patients with Billroth II gastrectomy: a systematic review and meta‐analysis. Surg Endosc. 2018;32(11):4598‐4613. [DOI] [PubMed] [Google Scholar]
- 7. Itoi T, Ishii K, Sofuni A, et al. Single‐balloon enteroscopy‐assisted ERCP in patients with Billroth II gastrectomy or Roux‐en‐Y anastomosis (with video). Am J Gastroenterol. 2010;105(1):93‐99. [DOI] [PubMed] [Google Scholar]
- 8. Cerefice M, Sauer B, Javaid M, et al. Complex biliary stones: treatment with removable self‐expandable metal stents: a new approach (with videos). Gastrointest Endosc. 2011;74(3):520‐526. [DOI] [PubMed] [Google Scholar]
- 9. Okabe Y, Ishida Y, Sasaki Y, Ushijima T, Sugiyama G, Tsuruta O. Use of a partially covered self‐expandable metallic stent to treat a biliary stricture secondary to chronic pancreatitis complicated by recurrent cholangitis: a case report. Dig Endosc. 2012;24(Suppl 1):55‐58. [DOI] [PubMed] [Google Scholar]
- 10. García‐Cano J, Reyes‐Guevara AK, Martínez‐Pérez T, et al. Fully covered self‐expanding metal stents in the management of difficult common bile duct stones. Rev Esp Enferm Dig. 2013;105(1):7‐12. [DOI] [PubMed] [Google Scholar]
- 11. Singh P, Das A, Isenberg G, et al. Does prophylactic pancreatic stent placement reduce the risk of post‐ERCP acute pancreatitis? A meta‐analysis of controlled trials. Gastrointest Endosc. 2004;60(4):544‐550. [DOI] [PubMed] [Google Scholar]
- 12. Mazaki T, Masuda H, Takayama T. Prophylactic pancreatic stent placement and post‐ERCP pancreatitis: a systematic review and meta‐analysis. Endoscopy. 2010;42(10):842‐853. [DOI] [PubMed] [Google Scholar]
- 13. Choudhary A, Bechtold ML, Arif M, et al. Pancreatic stents for prophylaxis against post‐ERCP pancreatitis: a meta‐analysis and systematic review. Gastrointest Endosc. 2011;73(2):275‐282. [DOI] [PubMed] [Google Scholar]
- 14. Mazaki T, Mado K, Masuda H, Shiono M. Prophylactic pancreatic stent placement and post‐ERCP pancreatitis: an updated meta‐analysis. J Gastroenterol. 2014;49(2):343‐355. [DOI] [PubMed] [Google Scholar]
- 15. Shi QQ, Ning XY, Zhan LL, Tang GD, Lv XP. Placement of prophylactic pancreatic stents to prevent post‐endoscopic retrograde cholangiopancreatography pancreatitis in high‐risk patients: a meta‐analysis. World J Gastroenterol. 2014;20(22):7040‐7048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fan JH, Qian JB, Wang YM, Shi RH, Zhao CJ. Updated meta‐analysis of pancreatic stent placement in preventing post‐endoscopic retrograde cholangiopancreatography pancreatitis. World J Gastroenterol. 2015;21(24):7577‐7583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sugimoto M, Takagi T, Suzuki R, et al. Pancreatic stents to prevent post‐endoscopic retrograde cholangiopancreatography pancreatitis: a meta‐analysis. World J Metaanal. 2019;7(5):249‐258. [Google Scholar]
- 18. Sugimoto M, Takagi T, Suzuki R, et al. Pancreatic stents for the prevention of post‐endoscopic retrograde cholangiopancreatography pancreatitis should be inserted up to the pancreatic body or tail. World J Gastroenterol. 2018;24(22):2392‐2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sugimoto M, Takagi T, Suzuki R, et al. Prevention of post‐endoscopic retrograde cholangiopancreatography pancreatitis using pancreatic stents: a review of efficacy, diameter and length. World J Metaanal. 2019;7(6):259‐268. [Google Scholar]
- 20. Cahen DL, Rauws EA, Gouma DJ, Fockens P, Bruno MJ. Removable fully covered self‐expandable metal stents in the treatment of common bile duct strictures due to chronic pancreatitis: a case series. Endoscopy. 2008;40(8):697‐700. [DOI] [PubMed] [Google Scholar]
- 21. Lalezari D, Singh I, Reicher S, Eysselein VE. Evaluation of fully covered self‐expanding metal stents in benign biliary strictures and bile leaks. World J Gastrointest Endosc. 2013;5(7):332‐339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Haapamäki C, Kylänpää L, Udd M, et al. Randomized multicenter study of multiple plastic stents vs. covered self‐expandable metallic stent in the treatment of biliary stricture in chronic pancreatitis. Endoscopy. 2015;47(7):605‐610. [DOI] [PubMed] [Google Scholar]
- 23. Park JS, Lee SS, Song TJ, et al. Long‐term outcomes of covered self‐expandable metal stents for treating benign biliary strictures. Endoscopy. 2016;48(5):440‐447. [DOI] [PubMed] [Google Scholar]
- 24. Ryu CH, Kim MH, Lee SS, Park DH, Seo DW, Lee SK. Temporary placement of fully covered self‐expandable metal stents in benign biliary strictures. Korean J Gastroenterol. 2013;62(1):49‐54. [DOI] [PubMed] [Google Scholar]
- 25. Cantù P, Hookey LC, Morales A, Le Moine O, Devière J. The treatment of patients with symptomatic common bile duct stenosis secondary to chronic pancreatitis using partially covered metal stents: a pilot study. Endoscopy. 2005;37(8):735‐739. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.


