Introduction
Pustular psoriasis of pregnancy is a form of generalized pustular psoriasis commonly associated with severe hypocalcemia. In pustular psoriasis of pregnancy, hypocalcemia is viewed as the consequence of the dermatosis rather than being recognized as a trigger.1 In the other clinical presentations of psoriasis, hypocalcemia is not usually described, and the relationship between hypocalcemia and psoriasis flares is unclear.1,2 It has been suggested that calcium homeostasis could be involved in the development or exacerbation of psoriasis because hypocalcemia can damage cell adhesion molecules, such as cadherins, which are dependent on calcium.3 An interesting aspect of this relationship is the observation of the dynamics of hypocalcemia remediation on the clinical remission of psoriasis. We present a case of febrile pustular psoriasis associated with severe hypocalcemia, which improved with calcium supplementation alone.
Case report
A 28-year-old man was admitted with a febrile, diffuse, erythematous eruption. Symptoms began in October 2017 with psoriasis of the scalp. He had no past medical history of psoriasis or other relevant conditions. His psoriasis extended progressively in the form of plaques on the body over several weeks. He had been treated with topical calcipotriol and betamethasone dipropionate with no satisfactory improvement. In May 2018, the lesions were worsening, with a flare of multiple pustules, fever, and polyarthralgia, for which he received oral naproxene. Three weeks later, he was admitted to the emergency department for persistent fever, arthralgia, generalized edema, dyspnea, a 13-kg weight gain, cramps, and an exacerbation of the psoriasis.
Physical examination revealed significant leg edema, disseminated erythematous and squamous plaques, numerous sterile pustules on the legs, and onycholysis. The plaques were hyperkeratotic with inflammatory edges. He had numerous pustules on the legs and some plaques on the abdomen and the thighs associated with gross hyperkeratosis, as can be seen in rupioid psoriasis.4 The Psoriasis Area and Severity Index score was not calculated, because it was not suited to his partially pustular clinical presentation (Fig 1).
Fig 1.
Clinical presentation. A, Disseminated erythematous and squamous plaques. B, Scaly plaques with inflammatory edges on the legs. C, Scaling plaques on the thighs. D, Numerous sterile pustules on the legs.
Physical examination revealed sinus tachycardia and the Trousseau sign (sudden contraction of the fingers and hand into the so-called obstetrical position due to carpal spasms). Laboratory tests revealed significant leukocytosis (12.5 g/L) and elevated C-reactive protein (CRP) (346 mg/L). Albumin and renal function were normal. The remaining laboratory examinations showed severe hypocalcemia (0.96 mmol/L; normal range, 2.2-2.6 mmol/L) and hypomagnesemia (0.62 mmol/L; normal range, 0.7-1.1 mmol/L) and increased levels of creatine phosphokinase (1512 U/L; normal, <200 U/L) and phosphorus (1.52 mmol/L; normal range, 0.8-1.5 mmol/L). The parathyroid hormone level was low (6 pg/mL; normal range, 9.4-29.8 pg/mL), indicating a diagnosis of primary hypoparathyroidism.
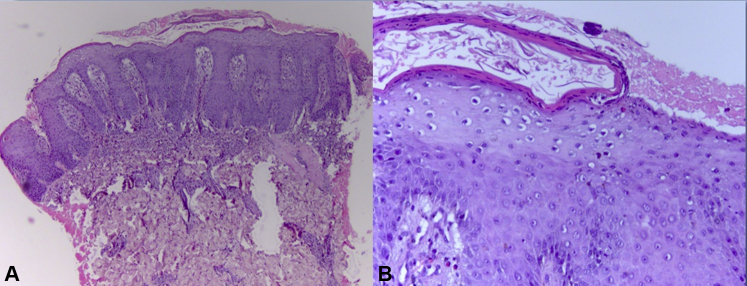
The skin biopsy was conclusive for a diagnosis of pustular psoriasis. Epidermal hyperplasia and parakeratotic hyperkeratosis associated with exocytosis of polynuclear cells were observed. The biopsy also revealed a subcorneal spongiform pustule. There was a superficial inflammatory infiltrate with lymphocytes and the presence of some polynuclear cells. Periodic acid Schiff staining was negative (Fig 2).
Fig 2.
Skin biopsy. A, The skin biopsy was conclusive for a diagnosis of pustular psoriasis. Histopathologic examination revealed epidermal hyperplasia with clubbed and branched rete ridges (Hematoxylin-eosin stain; original magnification, ×40). B, Accentuated epidermal hyperplasia, parakeratotic hyperkeratosis associated with exocytosis of polynuclear cells, and a subcorneal spongiform pustule were observed (Hematoxylin-eosin stain; original magnification, ×100).
First the patient received amoxicillin clavulanic acid (3 g/day) for a suspicion of infectious cellulitis. Blood culture and skin culture of an unroofed pustule, which were performed before antibiotherapy initiation, were negative, and amoxicillin-clavulanic acid was discontinued after 3 days.
The hypocalcemia was immediately supplemented with intravenous calcium. Within 3 days, the calcium level rose from 0.9 mmol/L to 1.3 mmol/L. Without any other treatment for the psoriasis, a significant improvement was observed: remission of the pustules and fever, and regression of the plaques. Cholecalciferol was introduced to counter the hypoparathyroidism. Since the patient was clinically stable and the psoriasis began to improve, we decided not to introduce any psoriasis-specific treatment and to follow the clinical evolution and the rise in serum calcium values.
On the 6th day, the calcium level was 1.8 mmol/L, the psoriasis plaques kept improving, and the CRP level decreased to 270 mg/L. On the 7th day, he received 1 day of topical steroids, but this treatment was discontinued after 24 hours. On the 13th day, the calcium concentration had reached 1.9 mmol/L, the psoriasis plaques had flattened with a complete regression of the scaling, and the CRP level reached 73 mg/L (Fig 3).
Fig 3.
Clinical improvement. The pustules had disappeared completely, and most of the plaques had begun to flatten on day 6 (A, B), when the calcium level was at 1.8 mmol/L. Plaques had flattened completely without scaling on day 13 (C, D), when the calcium level reached 1.9 mmol/L. After 3 weeks, only post-inflammatory pigmentation was observed (not illustrated).
A few months after this flare, ultraviolet B phototherapy was started because the psoriasis relapsed in the form of a few plaques on the limbs.
Discussion
We report a case of pustular psoriasis responding to calcium supplementation and oral cholecalciferol. The patient had a form of psoriasis comprising both pustular areas and scaly plaques present for several weeks, and we consider it unlikely that the patient had a spontaneous improvement. Among the other treatments that he received, we believe that none was responsible for the clinical improvement. Our hypothesis is that calcium supplementation could have had a role in the induction of rapid clinical improvement.
Our patient received only intravenous calcium and cholecalciferol, a few days of antibiotics, and one day of topical steroids. The urgent need was to normalize blood calcium because of the potentially life-threatening situation. The correction was therefore rapid, and at the same time, the psoriasis rapidly improved even before the introduction of cholecalciferol. Thus, this clinical evolution suggests that normalization of calcium levels could have had a positive impact on the favorable clinical outcome.
The link between calcium supplementation and improvement of pustular psoriasis has been reported previously, and a display of published case reports is available in Table I.
Table I.
Literature review of psoriasis cases treated with calcium supplementation
| Cases report | Number of cases (Sex, age) | Clinical characteristics | Hypocalcemia before psoriasis | Etiology of hypocalcemia | Past history of psoriasis | Treatment prior to calcium supplementation | Concomitant treatment of calcium supplementation | Evolution |
|---|---|---|---|---|---|---|---|---|
| Vickers HR et Sneddon IB5 | F, 51 and M, 43 | Severe and extensive psoriasis | Yes | Post thyroidectomy | No | No | Calciferol | Improvement in 3 to 6 weeks, psoriasis relapsed whenever calcium levels fell |
| Montgomery PR6 | F, 63 | Extensive psoriasis | Yes | Post thyroidectomy | No | No | Calciferol | Great improvement |
| Wallace HJ et al7 | M, 51 | Generalized pustular psoriasis | Yes | Steatorrhoea | No | No | Local and systemic antibiotics, local corticosteroid, dapsone, vitamins, and calciferol | Calcium was initially low and returned normal when the skin improved |
| Risum G8 | M, 29 | Plantar pustular psoriasis and erythroderma | Yes | Primary hypoparathyroidism | Vulgaris psoriasis | Methotrexate >2 weeks, Antibiotics and systemic steroids for 1 week, topical treatment | Calciferol | Improvement within a few days after starting calcium treatment |
| Stewart et al9 | F | Generalized pustular psoriasis | Yes | Post thyroidectomy | Vulgaris psoriasis | Topical steroids | Dihydrotactysterol | Within 48 hours: normocalcemia, new pustules abruptly terminated and skin returned to normal within 1 to 3 weeks |
| Kawamura et al10 | F, 36 | Generalized pustular psoriasis | Yes | Primary hypoparathyroidism | No | No | Calcitriol | When the serum calcium level became normal, the pustules disappeared and erythroderma completely resolved |
| Ashkevari S et al3 | F, 17 | Rupioid and pustular psoriasis | Yes | Idiopathic hypoparathyroidism | No | No | Calcitriol | After 10 days the pustular lesions cleared completely, after 6 month no further lesions |
| LeeY et al11 | M, 70 | Generalized pustular psoriasis | Yes | Post thyroidectomy | No | Topical steroids | Calciferol | Within 1 week, the pustular skin lesions and erythroderma rapidly cleared as the calcium level rose; resolved completely the following week |
| Guerreiro de Moura CAG et al1 | F, 73 | Generalized pustular psoriasis | Yes | Post thyroidectomy | No | No | Cholecalciferol | Significant improvement |
| Knuever J et al12 | M, 39 | Generalized pustular psoriasis | No | Primary hypoparathyroidism | For 20 years | No | Calcitriol and hydrocortisol | Pustules vanished within 24 h after the first calcium infusion and plaques improved very quickly |
F, Female; M, male.
The association between psoriasis and hypocalcemia is known, especially in pustular psoriasis of pregnancy, and it seems to be a secondary metabolic phenomenon. Hypocalcemia is secondary to the extensive cutaneous inflammation resulting from an extravasation of albumin and albumin-bound calcium into the interstitial space.13 Therefore, treatment should target the inflammation. It has been suggested that calcium homeostasis could be involved in the development or exacerbation of psoriasis, since hypocalcemia can damage cell adhesion molecules.3 Calcium has a role in keratinocyte differentiation and proliferation, and cell adhesion requires cadherins, which are calcium-dependent molecules.14 The mechanism operating between calcium and keratinocyte differentiation is not fully understood, but these elements of pathophysiology could explain in part why hypocalcemia triggered a flare-up of psoriasis in this patient and why the normalization of serum calcium values led to a large extent to the improvement of the psoriasis.
In our case, hypocalcemia was probably present before the psoriasis, because the patient had been reporting clinical signs of hypocalcemia, such as the Trousseau sign and paresthesia as lasting for several years. Here, hypocalcemia appears to be a relevant factor in inducing this psoriasis flare. More awareness is needed, both at the clinical and fundamental level, to gain a better understanding of the relationship between hypocalcemia and pustular psoriasis.
Conflicts of interest
None declared.
Footnotes
Funding sources: None.
References
- 1.Guerreiro de Moura C.A.G., de Assis L.H., Góes P. A case of acute generalized pustular psoriasis of von Zumbusch triggered by hypocalcemia. Case Rep Dermatol. 2015;7(3):345–351. doi: 10.1159/000442380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gueydan M., Folchetti G., Christofilis M.A., Valéro R., Grob J.J., Vialettes B. [Impetigo herpetiformis, a rare manifestation of severe hypocalcemia] Ann Endocrinol (Paris) 2002;63(6 Pt 1):502–504. [PubMed] [Google Scholar]
- 3.Ashkevari S.S., Maboodi A. Acute generalized pustular psoriasis and idiopathic hypoparathyroidism in an adolescent girl. Acta Med Iran. 2004;42(4):300–302. [Google Scholar]
- 4.Griffiths C., Barker J., Bleiker T., Chalmers R., Creamer D., editors. Rook's Textbook of Dermatology. 9th ed. Wiley-Blackwell; 2016. Pustular psoriasis; p. 4696. [Google Scholar]
- 5.Vickers H.R., Sneddon I.B. Psoriasis and hypoparathyroidism. Br J Dermatol. 1963;75:419–421. doi: 10.1111/j.1365-2133.1963.tb13536.x. [DOI] [PubMed] [Google Scholar]
- 6.Montgomery P.R. Psoriasis in association with hypocalcaemia. Proc R Soc Med. 1964;57(12):1128–1129. doi: 10.1177/003591576405701209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallace H.J. Generalized pustular psoriasis (von zumbush) with episodic hypocalcaemia. Proc R Soc Med. 1965;58(6):425–427. doi: 10.1177/003591576505800615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Risum G. Psoriasis exacerbated by hypoparathyroidism with hypocalcaemia. Br J Dermatol. 1973;89(3):309–312. doi: 10.1111/j.1365-2133.1973.tb02980.x. [DOI] [PubMed] [Google Scholar]
- 9.Stewart A.F., Battaglini-Sabetta J., Millstone L. Hypocalcemia-induced pustular psoriasis of von Zumbusch. New experience with an old syndrome. Ann Intern Med. 1984;100(5):677–680. doi: 10.7326/0003-4819-100-5-677. [DOI] [PubMed] [Google Scholar]
- 10.Kawamura A., Kinoshita M.T., Suzuki H. Generalized pustular psoriasis with hypoparathyroidism. Eur J Dermatol. 1999;9(7):574–576. [PubMed] [Google Scholar]
- 11.Lee Y., Nam Y.H., Lee J.H., Park J.K., Seo Y.J. Hypocalcaemia-induced pustular psoriasis-like skin eruption. Br J Dermatol. 2005;152(3):591–593. doi: 10.1111/j.1365-2133.2005.06460.x. [DOI] [PubMed] [Google Scholar]
- 12.Knuever J., Tantcheva-Poor I. Generalized pustular psoriasis: A possible association with severe hypocalcaemia due to primary hypoparathyroidism. J Dermatol. 2017;44(12):1416–1417. doi: 10.1111/1346-8138.13724. [DOI] [PubMed] [Google Scholar]
- 13.Thio H.B., Vermeer B.J. Hypocalcemia in impetigo herpetiformis: a secondary transient phenomenon? Arch Dermatol. 1991;127(10):1587–1588. [PubMed] [Google Scholar]
- 14.Popp T., Steinritz D., Breit A. Wnt5a/β-catenin signaling drives calcium-induced differentiation of human primary keratinocytes. J Invest Dermatol. 2014;134(8):2183–2191. doi: 10.1038/jid.2014.149. [DOI] [PubMed] [Google Scholar]