Abstract
Community pharmacists are responsible for providing the appropriate information on the use of medications to patients, which may enhance their medication adherence. The extent of control that patients have on their health care preferences creates many challenges for community pharmacists. This study aimed to determine the impact of pharmacist interventions and patient decisions on health outcomes concerning medication adherence and the quality use of medicines among patients attending community pharmacies. Appropriate studies were identified in a systematic search using the databases of Medline, Scopus, Google Scholar, and PubMed. The search included literature published between 2004 and 2019. The database searches yielded 683 titles, of which 19 studies were included after the full-text analysis with a total of 9313 participants. Metaprop command in Stata software version 14 was used for the analysis. This study was undertaken based on the general principles of the Cochrane Handbook for Systematic Reviews of Interventions and subsequently reported according to the Preferred Reporting Items for Systematic Reviews (PRISMA) extension. The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach was directly used to rate the quality of evidence (high, moderate, low, or very low). The results revealed the effective interaction between patients and community pharmacists, the importance of pharmacist intervention on medication adherence and quality use of medicine, and the role of community pharmacists in counselling patients. Decision/choice of patients in self-care and self-medication is a factor contributing to health outcomes. Effective interaction of community pharmacists with patients in terms of medication adherence and quality use of medicines provided a better health outcome among patients. The community pharmacists influenced the decision/choice of patients in self-care and self-medications.
Keywords: pharmacist interventions, patient choice, patient decision, quality use of medicine, patient-centered care, patient autonomy
1. Introduction
The pharmacy profession plays an important role in the health care setting and pharmacists undertake a range of responsibilities in health care services [1]. The services provided in community pharmacy have undergone rapid expansion in recent years; these include public health advice on disease management and prevention, counselling on the rational use of medicines, and making appropriate referrals to other relevant health care professionals [2]. Community pharmacists are often the first point of contact for reliable information and advice for consumers and patients [3].
Patient-centered communication in community pharmacy facilitates patient empowerment and encourages patients to take an active part in the decision-making concerning their care. Patient empowerment is an essential prerequisite for effective autonomy [4] and involves the amount of control that patients have over their health outcomes [5]. On the other hand, autonomy, a crucial ethical and legal principle, allows individuals to make their own choices about their health behavior and the management of their illnesses [6]. This encompasses the individuals’ self-governance, the functional capacity to think, and to diligently decide and act based on the influence of independent thought [7]. In health care, patient autonomy refers to the patient’s personal right to consent or refuse a treatment [4].
Physical and mental competencies are necessary for patient empowerment, which creates dilemmas for health care providers in determining patient competencies [8]; in some instances, the patients’ personal ability to consent is questioned due to their lack of competencies [9]. As community pharmacists deal with patients while making health care decisions, the goal is to move toward optimal patient care [10]. In general, community pharmacists constantly face dilemmas in balancing the patients’ legal rights to autonomy against making interventions toward quality health outcomes [11]. However, in a health care intervention, the patient should have the capacity, be free from coercion or undue influence, and be informed appropriately about treatment goals [12]. This raises the question of whether the quality of patient health outcomes is due to the intervention of community pharmacists or the patients’ choices/decisions.
Pharmacists exert autonomy by placing patients’ rights before the regulations that govern pharmacy practice [13]. The amount of control that patients should have over their health care decisions/choices [14] is a cardinal question, which brings challenges to the community pharmacists.
In general, community pharmacists perceive that patients’ decision-making about their health care depends on their ideas and emotional state of social well-being [15]. This may put patients at higher risk if they are unaware of the medication dose regimen and the potential interactions with other medications [16]. Subsequently, this may lead to poor adherence to therapy and medication-related risks. A systematic review has already shown that community pharmacists play a major role in the health outcomes of patients by their interventions in medication adherence and quality use of medicines [17]. However, patient autonomy in health outcomes has not been analyzed among patients attending a community pharmacy. Therefore, there is a need for systematic information to measure the impact of pharmacists’ intervention and patients’ decisions on medication adherence and the quality use of medicines. Thus, the main goal of the present study was to determine the effect of patient autonomy on the health outcome of patients attending community pharmacies. This systematic review also aimed to summarize the evidence of pharmacists’ interventions and patients’ decisions on the health outcomes in terms of medication adherence and quality use of medicines among patients attending community pharmacies.
2. Materials and Methods
2.1. Ethics Approval
This study obtained ethical approval from the International Medical University (IMU) Joint Committee on Research and Ethics. Approval number: MPP1/202 (01).
2.2. Study Design
The impact of patient autonomy on medication adherence and quality use of medicine among patients attending community pharmacies was undertaken based on the general principles of the Cochrane Handbook for Systematic Reviews of Interventions and subsequently reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension. The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach was directly used to rate the quality of evidence (high, moderate, low, or very low) to determine if the authors provided a clearly defined research question and theoretical background.
2.3. Inclusion Criteria
Only peer-reviewed articles written in English and dealing with adult patients were considered. The studies were required to have an observational or experimental design and to address the potential relationship between the health outcomes and the patients’ decisions, with patients’ decisions being considered as an independent variable or as a mediator, and with health quality outcome being assessed directly as an outcome variable. The review was limited to the following in relation to medication adherence and quality use of medicine among patients attending community pharmacies:
Effect of patients’ decision on health outcome.
Effect of pharmacists’ intervention on health outcome.
Effect of patients’ decision over pharmacists’ intervention on health outcome.
2.4. Exclusion Criteria
The studies excluded from this review were papers that were not available in English, qualitative studies, essays, literature reviews, commentaries, study protocols, conceptual papers, and conference abstracts.
2.5. Search Strategy
Given the importance of including evidence from observational studies in systematic reviews, relevant studies were identified through a systematic search of Medline and Scopus databases using subject headings and free-text terms. The PICO and Boolean search strategies were applied. The database search fields for titles, index terms, and abstracts were searched based on the following general research string: patient self-efficacy OR patient choice OR patient preference OR decision-making AND medication adherence AND quality use of medicines AND patient-centered care AND community pharmacist* AND pharmacist intervention. The search included all the literature published from 2004 to 2019. Subsequently, to supplement the main results of the online database searches (Medline and Scopus), the authors searched for articles that cited the potential identified studies using Google Scholar and PubMed MeSH and screened these articles for potential studies. Additionally, the authors directly screened the bibliographies of the potential identified studies. Two authors screened the titles and abstracts. Two authors selected and included full-text articles; these two authors read all the published full texts of the potential papers to confirm the inclusion criteria. All disagreements were resolved by consensus. In line with this, the data extraction process was performed by an author using a basic data-extraction instrument that encompassed the author, the year of the study, the setting, involvement of participants, possible interventions assessed, direct outcome measures, and all the main and essential findings of the studies.
2.6. Data Extraction and Synthesis
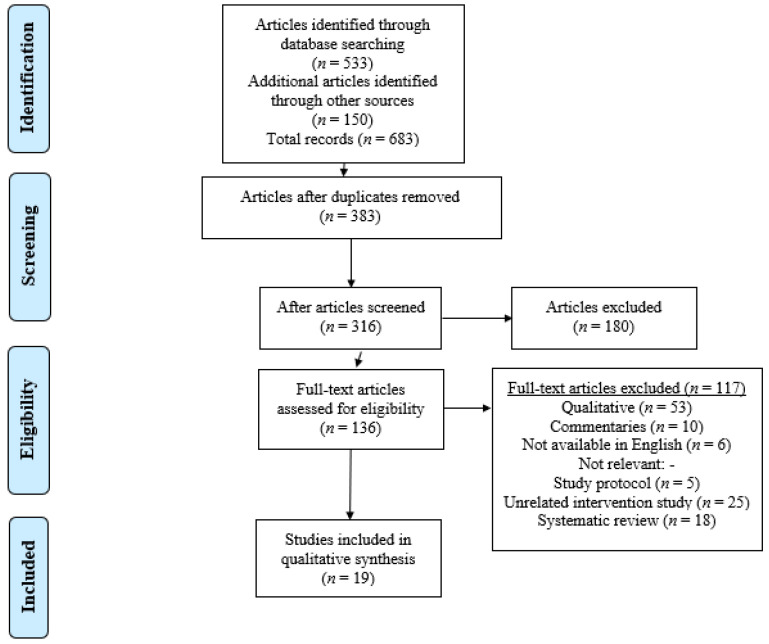
This systematic review was prepared following the PRISMA flow diagram (Figure 1) to assess the methodological quality of studies and sensitivity analysis of the GRADE approach. Cochrane’s Q and I2 statistics were used to evaluate the heterogeneity of the studies. Metaprop command in Stata software was used for the analysis (StataCorp. 2015, Stata Statistical Software: Release 14. College Station, TX, USA: StataCorp LP). Funnel plots by Egger and Begg tests were used to assess the publication bias. Forest plots showed high heterogeneity values, which resulted from variations in sample sizes and different populations. Hence, a meta-analysis was not used in the data synthesis as all the included studies directly demonstrated large heterogeneity in terms of the conceptualization and operationalization of quality health outcome in terms of medication adherence and quality use of medicine. Therefore, a descriptive synthesis was conducted and reported the impact of pharmacists’ interventions and patients’ decision on the health outcome. In this systematic review, effect sizes estimated the statistically significance studies, which were pooled and presented to obtain an overall effect size. The following four statements, which were common among published studies, were considered as outcomes for the systemic review:
Effective interaction between patients and community pharmacists.
Importance of pharmacists’ intervention on medication adherence and quality use of medicine.
Role of community pharmacists in counselling patients when dispensing medications.
Decision/choice of patients in self-care and self-medication.
Figure 1.
Flow diagram of the study selection process.
The first statement assessed the effect of patients’ decisions on health outcomes, while statements 2 and 3 assessed the effect of pharmacists’ interventions on health outcomes. The last statement assessed the effect of patients’ decisions over pharmacists’ interventions on health outcomes.
2.7. Risk of Bias
The risk of bias in the studies was assessed, based on nine standard criteria suggested by the Cochrane Effective Practice and Organization of Care (EPOC) [18]. An overall rating of risk of bias was determined based on scores obtained for each domain. The risk of bias assessment is presented in Table 1.
Table 1.
Risk of bias of included study categories is based on Effective Practice and Organization of Care (EPOC).
| Study Author, (Year) | Was the Allocation Sequence Adequately Generated? | Was Allocation Adequately Concealed? | Was the Study Adequately Protected Against Contamination? | Was Knowledge of the Allocated Interventions Adequately Prevented? | Were Incomplete Outcome Data Adequately Addressed? | Was Baseline Outcome Measurement Similar? | Was the Baseline Characteristic Similar? | Was the Study Free from Selective Outcome Reporting? | Overall Risk |
|---|---|---|---|---|---|---|---|---|---|
| 1. Rickles (2005) [19] | Low | Low | Unclear | Unclear | Low | Low | Low | Low | Unclear |
| 2. Vella (2015) [20] | Unclear | Unclear | Low | Unclear | Low | Low | Unclear | Low | Unclear |
| 3. Robinson (2010) [21] | Low | Low | Low | Low | Low | Low | Low | Low | Unclear |
| 4. Major (2010) [22] | Low | Low | Unclear | Unclear | Low | Unclear | Low | Low | Unclear |
| 5. El-Kohly (2017) [23] | Low | Unclear | Low | Unclear | Low | Low | Unclear | Low | Unclear |
| 6. Kayyali (2018) [24] | Low | Low | Low | High | Low | Low | Low | Low | High |
| 7. Al-Arifi (2012) [25] | Low | Low | Low | Low | Low | Low | Low | Low | Unclear |
| 8. Sookaneknun (2004) [26] | Low | Low | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| 9. Eussen (2010) [27] | Unclear | Low | Unclear | Unclear | Low | Unclear | Low | Low | Unclear |
| 10. Millar (2016) [28] | Low | Low | Low | High | Low | Low | Unclear | Low | Unclear |
| 11. Tinelli (2007) [29] | Low | Low | Low | Low | Low | Low | Unclear | Low | Unclear |
| 12. Gultekin (2019) [30] | Low | Low | Low | High | Low | Low | Low | Low | High |
| 13. Basheti (2008) [31] | Low | Unclear | Low | Unclear | Low | Unclear | Low | Low | Unclear |
| 14. Kelly (2014) [32] | Unclear | Low | Low | Low | Low | Unclear | Low | Low | Unclear |
| 15. Caltic (2013) [33] | Low | Low | Unclear | Low | Low | Low | Unclear | Low | Unclear |
| 16. Merks (2014) [34] | Low | Low | Low | Low | Low | Unclear | Low | Low | Unclear |
| 17. Awad (2017) [35] | Low | Low | Low | Unclear | Unclear | Low | Low | Low | Unclear |
| 18. Wirth (2010) [36] | Low | Low | Low | Low | Low | Low | Low | Low | Unclear |
| 19. Lau (2019) [37] | Low | Low | Low | Low | Low | Low | Low | Low | Unclear |
3. Results
The database searches yielded 683 titles, of which 19 studies were included after the full-text analysis. If any of the articles reported more than one direct outcome regarding the relationship between the patient’s decision and quality health outcome, each result was included separately. Figure 1 provides an overview of the selection process.
3.1. Study Characteristics
The studies included in this systematic review (n = 19) were from various countries: the United Kingdom (n = 4), the United States of America (n = 3), Australia (n = 2), Saudi Arabia (n = 2), and Malta (2). There was one study each from Hungary, Canada, Bosnia-Herzegovina, Thailand, North Cyprus, and Kuwait. The characteristics of the included studies are described in Table 2.
Table 2.
Characteristics of the included studies.
| z | Author | Setting (Country) | Publication Year | Sample Size | Targeted Care Type | Intervention | Outcome Measures | Outcome Assessment |
|---|---|---|---|---|---|---|---|---|
| 1. | Rickles [19] | USA | 2005 | 60 | Pharmacist & Patient | Pharmacist–Patient Collaboration | Patient adherence | Randomized controlled |
| 2. | Vella [20] | Malta | 2015 | 824 | Pharmacist & Patient | Pharmacist-led services | Consumer perception | Cross sectional |
| 3. | Robinson [21] | USA | 2010 | 376 | Patient | Pharmaceutical care intervention | Medication adherence | Comparison |
| 4. | Major [22] | Hungary | 2010 | 1486 | Patient | Habits & Interests | Nonprescription Medications | Cross sectional |
| 5. | El-Kohly [23] | Saudi Arabia | 2017 | 1000 | Patient | Patients’ Perception | Perception of Community Pharmacists & Services | Cross sectional |
| 6. | Kayyali [24] | UK | 2018 | 319 | Patients | Improving adherence | Shared decision making | Mixed method |
| 7. | Al-Arifi 25] | Saudi Arabia | 2012 | 125 | Community Pharmacist | Patient counselling | Pharmacist’s role | Cross sectional |
| 8. | Sookaneknun [26] | Thailand | 2004 | 235 | Pharmacist & Patient | Pharmaceutical care intervention | Health outcome | Randomized controlled |
| 9. | Eussen [27] | USA | 2010 | 899 | Patient | Community pharmacy-based interventions | Quality use of medicines | Randomized controlled |
| 10. | Millar [28] | UK | 2016 | 539 | Community Pharmacists | Intermediate care and medicines management | Pharmacists’ perceptions | Cross sectional |
| 11. | Tinelli [29] | UK | 2007 | 1232 | Pharmacists | Medications management service | Pharmacist intervention | Randomized controlled |
| 12. | Gultekin [30] | North Cyprus | 2019 | 110 | Patients | Assessment of the source of information | Satisfaction, Techniques and Perception of Information | Cross sectional |
| 13. | Basheti [31] | Australia | 2008 | 97 | Pharmacists & Patients | Pharmacist intervention | Quality use of medicines | Randomized controlled |
| 14. | Kelly [32] | Canada | 2014 | 384 | Patient | Patient Attitudes | Role & Services of Pharmacists | Cross sectional |
| 15. | Catic [33] | Bosnia-Herzegovina | 2013 | 182 | Patient | Patients Perception | Perception and Role of Community Pharmacists | Cross sectional |
| 16. | Merks [34] | UK | 2014 | 417 | Patient | Patients’ choice of Pharmacy | Factors that influence patients’ choice | Cross sectional |
| 17. | Awad [35] | Kuwait | 2017 | 433 | Patient | Patients Perception, Expectation and Views | Community Pharmacy Practice | Cross sectional |
| 18. | Wirth [36] | Malta | 2010 | 500 | Patient | Patients Perception | Perception of the Pharmacists & Services | Cross sectional |
| 19. | Lau [37] | Australia | 2019 | 95 | Patient-Pharmacists | Counselling Interactions | Counselling on Persistent Pain | Cross sectional |
3.2. Effective Interaction between Patients and the Community Pharmacists
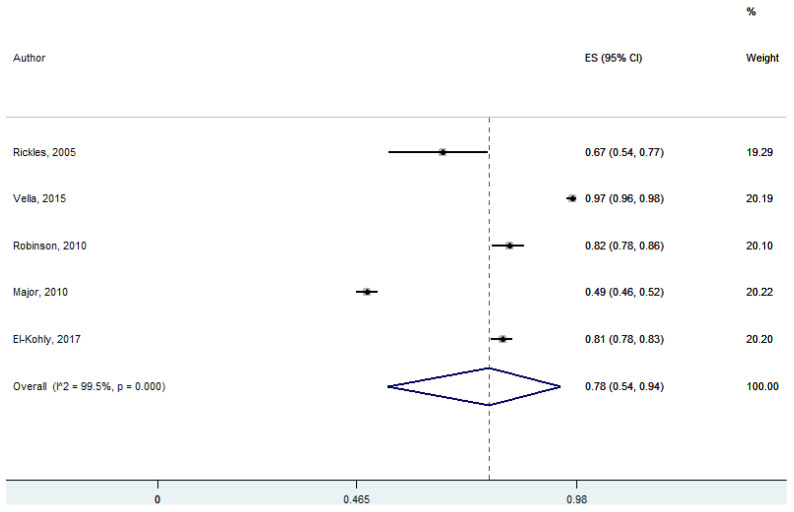
Five studies discussed the effect of patient–pharmacist interaction. Pharmacists respected the covenantal professional relationship with their patients and had an effective interaction with them to achieve the desired health outcome by shared decision-making. Pharmacists had an effective interaction with their patients, which was statistically significant at 95% CI 47–85; p = 0.00 (pooled effect size: 0.67) (Figure 2).
Figure 2.
Effective interaction between patients and the community pharmacists (five studies).
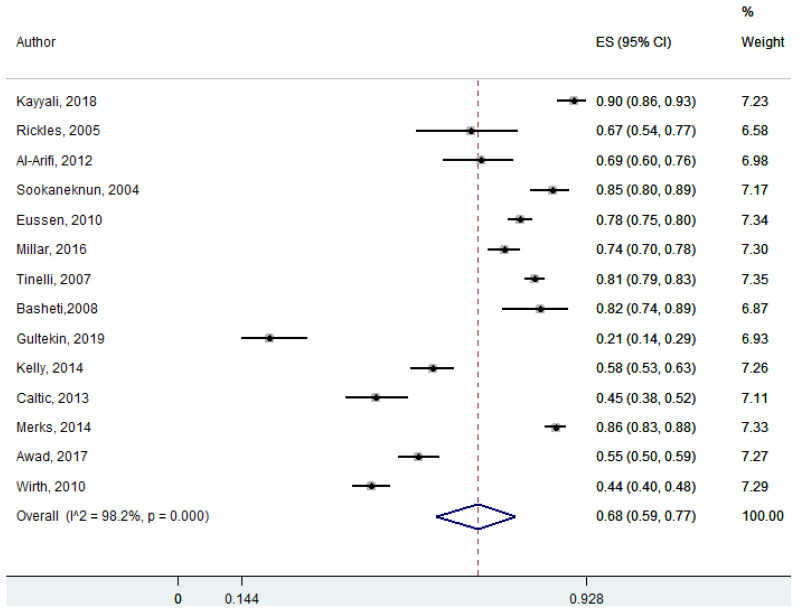
3.3. Importance of Pharmacists’ Intervention on Medication Adherence and Quality Use of Medicine
Eight studies looked at the importance of pharmacists’ intervention on medication adherence and quality use of medicine. These studies revealed that patients considered pharmacists as important health care providers as pharmacists’ interventions provided a better health outcome and helped in decision making in terms of medication use and adherence. Patients agreed on the importance of pharmacists’ intervention on medication use and adherence, which was statistically significant at 95% Cl 39–66; p = 0.00 (pooled effect size: 0.53) (Figure 3).
Figure 3.
Importance of pharmacists’ intervention on medication adherence and quality use of medicine (14 studies).
3.4. Role of Community Pharmacists in Counselling Patients When Dispensing Medications
Fourteen studies discussed the role of community pharmacists in dispensing prescription and non-prescription medications. The pharmacists had counselled the patients on medication adherence and quality use of medicines while dispensing medications for various ailments. Community pharmacists were involved in patient counselling in terms of medication adherence and quality use of medicines, which was statistically significant at 95% Cl 56–78; p = 0.00 (pooled effect size: 0.68) (Figure 4).
Figure 4.
Role of community pharmacists in counselling patients when dispensing medications (seven studies).
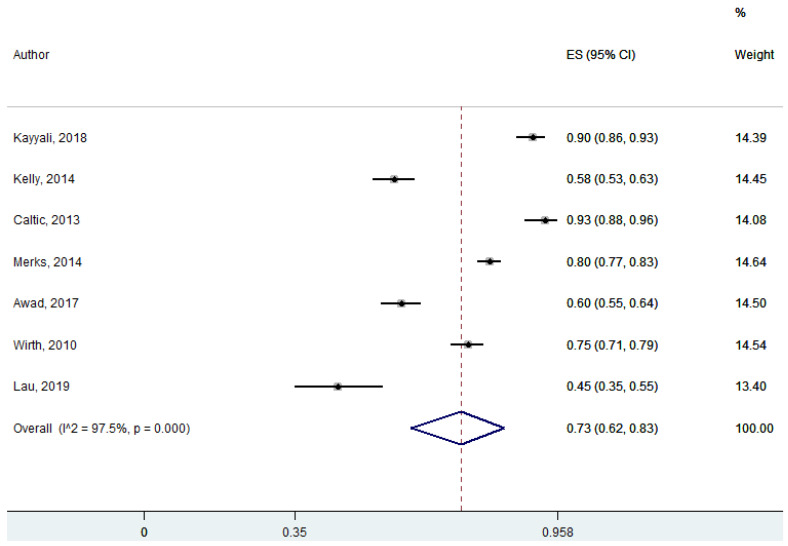
3.5. Decision/Choice of Patients in Self-Care and Self-Medication
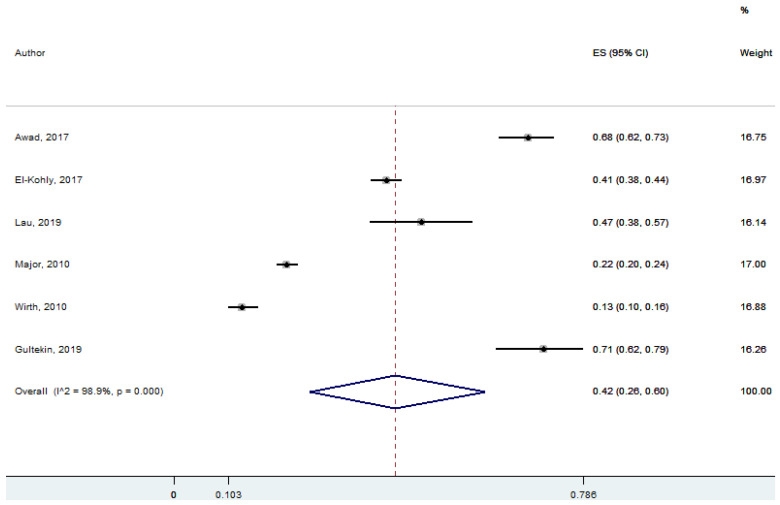
Six studies discussed the decisions/choices of patients in self-care and self-medication. Patients’ self-care directly related to their own decisions and the initiation of their actions by themselves. Patients’ preferences or choices sometimes depend on pharmacists’ recommendations while deciding on their medications for minor ailments. A vast number of minor ailments are self-limiting, requiring minimal or no medical interventions. Community pharmacists influenced the patients’ decision/choice in self-care and self-management, which was statistically significant at 95% Cl 26–60; p = 0.00 (pooled effect size: 0.42) (Figure 5).
Figure 5.
Decision/choice of patients in self-care and self-medication (six studies).
4. Discussion
This systematic review was conducted to focus on health outcomes in terms of medication adherence and quality use of medicines in patients attending community pharmacies. The current evidence revealed that ‘Effective interaction between patients and the community pharmacists’, ‘Importance of pharmacists’ intervention on medication adherence and quality use of medicine’, ‘Role of community pharmacists in counselling patients when dispensing medications’, and ‘Decision/choice of patients in self-care and self-medication’ are factors that contributed to better health outcomes. Despite having different methodologies, most studies were consistent with the conclusion that the pharmacists’ interventions had an impact on patients’ decisions on the health outcome.
The results of this systematic review indicated an interesting aspect of ‘Patient–pharmacist interaction’. Patient–pharmacist interaction is about treating patients receiving health care with dignity and respect and involving them in all decisions about their health. It is an essential component in providing sufficient advice to patients on their medications. By establishing a rapport with patients, pharmacists provide advice on the rational use of medications [38]. This patient-centered approach and therapeutic relationship with patients has become the top priority for most health care professionals [39]. Building a good therapeutic relationship helps health care professionals to provide optimal care and quality health outcomes for patients [40]. The patient–pharmacist relationship enables patients to ask for advice and to share their decisions with their pharmacists and follow-up [41]. As the number of new medications available is increasing, and patients with long-term illness and comorbidity need to take more than one medication concurrently, it is challenging patients to comply with prescribed medication regimens [42]. Thus, pharmaceutical care is necessary for the quality use of medicine and adherence. Quality Use of Medicines is primarily a patient-oriented movement, with the documentation stressing the importance of patient–professional communication along with patient knowledge and understanding of their medicines. Studies have shown improved health outcomes when there is an effective interaction between pharmacists and patients [43,44]. Patients view their pharmacists’ competence as a key factor to sustain a therapeutic relationship with them. However, to have effective communication between patient and pharmacists, trust and patient satisfaction are necessary [45].
This systematic review highlighted the importance of pharmacists’ intervention on medication adherence and quality use of medicine in managing patients’ medication therapy. Medication therapy management helps pharmacists to identify patients at-risk and resolve their pharmaceutical care issues [46]. Community pharmacists educate their patients on the quality use of medicines by encouraging their patients to take correct dosages at the correct time; they advise patients on appropriate medication usage and other ways to manage their ailments [47]. There is a high prevalence of inappropriate prescribing and medication errors exist within health care systems [48]. This often leads to adverse events, which are usually preventable. Pharmacists have a significant impact on reducing and preventing medication errors and their related problems [49]. As pharmacists’ services and interventions are effective and contribute to the patients’ cost savings, they help to reduce health care expenses [50]. Pharmacists’ interventions increase patient adherence to medications, thereby reducing unnecessary hospital visits and hospitalizations [51].
The results from this systematic review also revealed that patient counselling by community pharmacists on medication adherence and quality use of medicines while dispensing medication influences the quality health outcome of the patients. The quality health outcome is associated with patient adherence to the treatment regimens. Moreover, non-adherence to treatment regimens may become a threat to health and an increased economic burden for the patients [52]. Using a patient-centered approach and effective communication, community pharmacists can help patients manage their condition appropriately, improve their health, and help them to minimize the disease burden. Nevertheless, community pharmacists also need to consider that any social and/or economic changes in a patient’s life may affect their medical management [53]. Hence, each encounter with patients must include an intervention comprising a review of medication and compliance problems; this may enhance the autonomy of patients in deciding/choosing their management therapy.
Despite the meaningful intention of promoting choice to patients, it is not always possible to do this, especially if we look at the implications of such choices from different perspectives. It is suggested that there is always a probable conflict between allowing a greater choice for consumers and changing health care policy that is directed more toward standardized health care provision. Pharmacists are expected to offer choice, simply because it will promote and enhance autonomy, but also it is the right thing to do. However, the choice itself comes with responsibility, that is, one that is accountable for their choice and decision-making, and arguably, one choice usually impacts on other people, particularly when resources are scarce. In the present review, patients’ decisions/choices in self-care and self-medication were found to affect their health outcome, especially for minor ailments. The availability of “over-the-counter” or “non-prescription” medications to the public may vary in different countries. Although these medications are approved by the regulatory agencies, their safety and effectiveness for individual consumers/patients often require supervision or intervention by health care professionals. While studies suggested that most consumers/patients read the information provided before taking medications [54], their decisions in selecting such medication may not be appropriate. Most non-prescription medications are purchased based on product information available on the packaging [22]. When consumers/patients seek help when purchasing, this is termed “facilitated self-medication” [55]. When medications are purchased through community pharmacies, pharmacists facilitate self-care decision making. As the use of over the counter or non-prescription medications is increasing, there is a need for specific counselling by pharmacists while facilitating self-medication [56].
5. Strengths and Limitations
This study produced evidence of patient–pharmacist interactions, the role of pharmacists and the importance of community pharmacists’ interventions. Evidence was also provided on patient autonomy in community pharmacies. This is important, as it provides information to enhance the role of community pharmacists in terms of medication adherence and quality use of medicines for quality health outcome. Some of the observational studies in this systematic review reported the outcomes of patients who chose treatments based on their preferences and the advice of their provider. However, pharmacist intervention is a factor that influenced treatment choices/decisions of patients, which was also a factor for better health outcome. However, this study had some limitations. First, there was substantial heterogeneity across the included studies; this was likely due to the differences in the adjusted variables across studies and the assessment methods utilized, as some of the studies employed an open-ended questionnaire while others used a closed-ended questionnaire. As a result, a meta-analysis was not performed. Second, although the search strategy was comprehensive, only studies published in English were included.
6. Implication for Practice
This review indicates that although patients’ decisions/choices have an impact on the health outcome in terms of medication adherence and quality use of medicines, community pharmacists’ intervention influenced or facilitated the health outcome of patients. Hence, community pharmacists should continue to interact and provide interventions by applying their knowledge, experience, and skills to the best of their ability to assure optimal outcomes for their patients.
7. Conclusions
One of the key roles of community pharmacists is to enhance the autonomy of patients to decide/choose their medication management and therapies. Patient–pharmacist interactions contributed to the shared decision-making related to medication management. Patients considered community pharmacists as important health care providers as they provide interventions and help to decide medication adherence and quality use of medicine. The community pharmacists influenced the decision/choice of patients in self-care and self-medication.
Acknowledgments
All of the authors acknowledge Brian Furman, University of Strathclyde, for his help in improving the use of English in the manuscript.
Author Contributions
Conceptualization, K.R. and M.K.M.; Methodology, K.R.; Software, K.R. and S.S.; Validation, K.R., S.S. and M.K.M.; Formal analysis, S.S.; Investigation, K.R.; Resources, M.K.M.; Data curation, S.S.; Writing—original draft preparation, S.S.; Writing—review and editing, K.R.; Visualization, M.K.M.; Supervision, K.R. and M.K.M.; Project administration, S.S.; Funding acquisition, K.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Institute for Research, Development, and Innovation of International Medical University, grant number MPP1/2020 (01).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Joint Committee for Research and Ethics of International Medical University (protocol code MPP 2020/(1) and 11 March 2020).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the nature of the study (i.e., systematic review).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kehrer J.P., Eberhart G., Wing M., Horon K. Pharmacy’s role in a modern health continuum. Can. Pharm. J. Rev. Pharm. Can. 2013;146:321–324. doi: 10.1177/1715163513506370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kho B.P., Hassali M.A.A., Lim C.J., Saleem F. Challenges in the management of community pharmacies in Malaysia. Pharm. Pract. 2017;15:933. doi: 10.18549/PharmPract.2017.02.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agomo C.O. The role of community pharmacists in public health: A scoping review of the literature. J. Pharm. Health Serv. Res. 2012;3:25–33. doi: 10.1111/j.1759-8893.2011.00074.x. [DOI] [Google Scholar]
- 4.Entwistle V.A., Carter S.M., Cribb A., McCaffery K. Supporting Patient Autonomy: The Importance of Clinician-patient Relationships. J. Gen. Intern. Med. 2010;25:741–745. doi: 10.1007/s11606-010-1292-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McAllister M., Dunn G., Payne K., Davies L., Todd C. Patient empowerment: The need to consider it as a measurable patient-reported outcome for chronic conditions. BMC Health Serv. Res. 2012;12:157. doi: 10.1186/1472-6963-12-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen J., Mullins C.D., Novak P., Thomas S.B. Personalized Strategies to Activate and Empower Patients in Health Care and Reduce Health Disparities. Health Educ. Behav. 2016;43:25–34. doi: 10.1177/1090198115579415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roche C., Kelliher F. Exploring the Patient Consent Process in Community Pharmacy Practice. J. Bus. Ethics. 2008;86:91–99. doi: 10.1007/s10551-008-9836-7. [DOI] [Google Scholar]
- 8.Wakefield D., Bayly J., Selman L.E., Firth A.M., Higginson I.J., Murtagh F.E. Patient empowerment, what does it mean for adults in the advanced stages of a life-limiting illness: A systematic review using critical interpretive synthesis. Palliat. Med. 2018;32:1288–1304. doi: 10.1177/0269216318783919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leo R.J. Competency and the Capacity to Make Treatment Decisions: A primer for primary care physicians. Prim. Care Companion J. Clin. Psychiatry. 1999;1:131–141. doi: 10.4088/PCC.v01n0501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ilardo M.L., Speciale A. The Community Pharmacist: Perceived Barriers and Patient-Centered Care Communication. Int. J. Environ. Res. Public Health. 2020;17:536. doi: 10.3390/ijerph17020536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kruijtbosch M., Göttgens-Jansen W., Floor-Schreudering A., Van Leeuwen E., Bouvy M.L. Moral dilemmas of community pharmacists: A narrative study. Int. J. Clin. Pharm. 2018;40:74–83. doi: 10.1007/s11096-017-0561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coggon J., Miola J. Autonomy, Liberty, and Medical Decision-Making. Camb. Law J. 2011;70:523–547. doi: 10.1017/S0008197311000845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Delpasand K., Afshar L., Tavakkoli S.N. The Ethical Principles in Pharmacist-Patient Relationship. J. Clin. Diagn. Res. 2019;13:FE01–FE03. doi: 10.7860/JCDR/2019/39812.12692. [DOI] [Google Scholar]
- 14.Auerbach S.M. Should patients have control over their own health care?: Empirical evidence and research issues. Ann. Behav. Med. 2000;22:246–259. doi: 10.1007/BF02895120. [DOI] [PubMed] [Google Scholar]
- 15.Goundrey-Smith S. The Connected Community Pharmacy: Benefits for Healthcare and Implications for Health Policy. Front. Pharm. 2018;9:1352. doi: 10.3389/fphar.2018.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Phipps D., Noyce P., Parker D., Ashcroft D. Medication safety in community pharmacy: A qualitative study of the so-ciotechnical context. BMC Health Serv. Res. 2009;9:158. doi: 10.1186/1472-6963-9-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Milosavljevic A., Aspden T., Harrison J. Community pharmacist-led interventions and their impact on patients’ medica-tion adherence and other health outcomes: A systematic review. Int. J. Pharm. Pract. 2018;26:387–397. doi: 10.1111/ijpp.12462. [DOI] [PubMed] [Google Scholar]
- 18.Cochrane Effective Practice and Organization of Care Suggested Risk of Bias Criteria for EPOC Reviews. [(accessed on 26 November 2020)]; Available online: https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-forauthors2017/suggested_risk_of_bias_criteria_for_epoc_reviews.pdf.
- 19.Rickles N.M., Svarstad B.L., Statz-Paynter J.L., Taylor L.V., Kobak K.A. Pharmacist Telemonitoring of Antidepressant Use: Effects on Pharmacist–Patient Collaboration. J. Am. Pharm. Assoc. 2005;45:344–353. doi: 10.1331/1544345054003732. [DOI] [PubMed] [Google Scholar]
- 20.Vella M., Grima M., Wirth F., Pizzuto M.A., Bartolo N.S., Vella J., Azzopardi L.M. Consumer perception of community pharmacist extended professional services. J. Pharm. Health Serv. Res. 2015;6:91–96. doi: 10.1111/jphs.12094. [DOI] [Google Scholar]
- 21.Robinson J.D., Segal R., Lopez L.M., Doty R.E. Impact of a Pharmaceutical Care Intervention on Blood Pressure Control in a Chain Pharmacy Practice. Ann. Pharm. 2010;44:88–96. doi: 10.1345/aph.1L289. [DOI] [PubMed] [Google Scholar]
- 22.Major C., Vincze Z. Consumer habits and interests regarding non-prescription medications in Hungary. Fam. Pract. 2010;27:333–338. doi: 10.1093/fampra/cmp105. [DOI] [PubMed] [Google Scholar]
- 23.El-Kholy A.A., Abdel-Latif M.M. Publics’ perceptions of community pharmacists and satisfaction with pharmacy services in Saudi Arabia. Eur. J. Pharm. Med. Res. 2017;4:165–175. doi: 10.3390/medicina58030432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kayyali R., Gebara S.N., Hesso I., Funnell G., Naik M., Mason T., Uddin M.A., Al-Yaseri N., Khayyam U., Al-Haddad T., et al. Shared decision making and experiences of patients with long-term conditions: Has anything changed? BMC Health Serv. Res. 2018;18:763. doi: 10.1186/s12913-018-3575-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Arifi M.N. Patients’ perception, views and satisfaction with pharmacists’ role as health care provider in community pharmacy setting at Riyadh, Saudi Arabia. Saudi Pharm. J. 2012;20:323–330. doi: 10.1016/j.jsps.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sookaneknun P., Richards R.M., Sanguansermsri J., Teerasut C. Pharmacist Involvement in Primary Care Improves Hypertensive Patient Clinical Outcomes. Ann. Pharm. 2004;38:2023–2028. doi: 10.1345/aph.1D605. [DOI] [PubMed] [Google Scholar]
- 27.Eussen S.R., Van Der Elst M.E., Klungel O.H., Rompelberg C.J., Garssen J., Oosterveld M.H., De Boer A., De Gier J.J., Bouvy M.L. A Pharmaceutical Care Program to Improve Adherence to Statin Therapy: A Randomized Controlled Trial. Ann. Pharm. 2010;44:1905–1913. doi: 10.1345/aph.1P281. [DOI] [PubMed] [Google Scholar]
- 28.Millar A., Hughes C., Devlin M., Ryan C. A cross-sectional evaluation of community pharmacists’ perceptions of intermediate care and medicines management across the healthcare interface. Int. J. Clin. Pharm. 2016;38:1380–1389. doi: 10.1007/s11096-016-0377-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tinelli M., Bond C., Blenkinsopp A., Jaffray M., Watson M., Hannaford P. Patient Evaluation of a Community Pharmacy Medications Management Service. Ann. Pharm. 2007;41:1962–1970. doi: 10.1345/aph.1K242. [DOI] [PubMed] [Google Scholar]
- 30.Gültekin O., Abdi A.M., Al-Baghdadi H., Akansoy M., Rasmussen F., Başgut B. Counseling of inhalation medicine perceived by patients and their healthcare providers: Insights from North Cyprus. Int. J. Clin. Pharm. 2019;41:1272–1281. doi: 10.1007/s11096-019-00882-8. [DOI] [PubMed] [Google Scholar]
- 31.Basheti I.A., Armour C.L., Bosnic-Anticevich S.Z., Reddel H.K. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Educ. Couns. 2008;72:26–33. doi: 10.1016/j.pec.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 32.Kelly D.V., Young S., Phillips L., Clark D. Patient attitudes regarding the role of the pharmacist and interest in expanded pharmacist services. Can. Pharm. J. Rev. Pharm. Can. 2014;147:239–247. doi: 10.1177/1715163514535731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Catic T., Jusufovic F.I., Tabakovic V. Patients Perception of Community Pharmacist in Bosnia and Herzegovina. Mater. Socio Med. 2013;25:206–209. doi: 10.5455/msm.2013.25.206-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Merks P., Kaźmierczak J., Olszewska A.E., Kołtowska-Häggström M. Comparison of factors influencing patient choice of community pharmacy in Poland and in the UK, and identification of components of pharmaceutical care. Patient Prefer. Adherence. 2014;8:715–726. doi: 10.2147/PPA.S53829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Awad A.I., Al-Rasheedi A., Lemay J. Public Perceptions, Expectations, and Views of Community Pharmacy Practice in Kuwait. Med. Princ. Pract. 2017;26:438–446. doi: 10.1159/000481662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wirth F., Tabone F., Azzopardi L.M., Gauci M., Zarb-Adami M., Serracino-Inglott A. Consumer perception of the community pharmacist and community pharmacy services in Malta. J. Pharm. Health Serv. Res. 2010;1:189–194. doi: 10.1111/j.1759-8893.2010.00034.x. [DOI] [Google Scholar]
- 37.Lau E.T.L., Tan S.H., Antwertinger Y.J., Hall A., Nissen L.M. Counseling interactions between patients living with persistent pain and pharmacists in Australia: Are we on the same page? J. Pain Res. 2019;12:2441–2455. doi: 10.2147/JPR.S199017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McDonough R.P., Bennett M.S. Improving Communication Skills of Pharmacy Students through Effective Precepting. Am. J. Pharm. Educ. 2006;70:58. doi: 10.5688/aj700358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hermansen C.J., Wiederholt J.B. Pharmacist-patient partnership development in an ambulatory clinical setting. Health Commun. 2001;13:307–325. doi: 10.1207/S15327027HC1303_5. [DOI] [PubMed] [Google Scholar]
- 40.Molassiotis A., Morris K., Trueman I. The importance of the patient–clinician relationship in adherence to antiretroviral medication. Int. J. Nurs. Pract. 2007;13:370–376. doi: 10.1111/j.1440-172X.2007.00652.x. [DOI] [PubMed] [Google Scholar]
- 41.Worley M.M., Schommer J.C., Brown L.M., Hadsall R.S., Ranelli P.L., Stratton T.P., Uden D.L. Pharmacists’ and patients’ roles in the pharmacist-patient relationship: Are pharmacists and patients reading from the same relationship script? Res. Soc. Adm. Pharm. 2007;3:47–69. doi: 10.1016/j.sapharm.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 42.Tarn D.M., Hertigae J., Paterniti D.A., Hays R.D., Kravitz R.L., Wenger N.S. Physician communication when prescribing new medications. Arch. Intern. Med. 2006;166:1855–1862. doi: 10.1001/archinte.166.17.1855. [DOI] [PubMed] [Google Scholar]
- 43.Pringle J., Melczak M., Aldridge A., Snyder M., Smith R. Medication adherence and its relationship to the therapeutic alliance: Results from an innovative pilot study within a community pharmacy MTM practice. Innov. Pharm. 2011;2:1–16. doi: 10.24926/iip.v2i1.216. [DOI] [Google Scholar]
- 44.Kerr A., Strawbridge J., Kelleher C., Mertens F., Pype P., Deveugele M., Pawlikowska T. How can pharmacists develop patient-pharmacist communication skills? A realist review protocol. Syst. Rev. 2017;6:14. doi: 10.1186/s13643-016-0396-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guirguis L.M., AlGhurair S.A., Simpson S.H. What elements of the patient–pharmacist relationship are associated with patient satisfaction? Patient Prefer. Adherence. 2012;6:663–676. doi: 10.2147/PPA.S35688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.American Pharmacists Association Medication Therapy Management Services. [(accessed on 26 November 2020)]; Available online: https://www.pharmacist.com/medication-therapy-management-services.
- 47.Moore A. Community pharmacists are well placed to encourage patients to take their medicines, study finds. Pharm. J. 2017;299:7903. doi: 10.1211/pj.2017.20203020. [DOI] [Google Scholar]
- 48.Assiri G.A., Shebl N.A., Mahmoud M.A., Aloudah N., Grant E., Aljadhey H., Sheikh A. What is the epidemiology of medication errors, error-related adverse events and risk factors for errors in adults managed in community care contexts? A systematic review of the international literature. BMJ Open. 2018;8:e019101. doi: 10.1136/bmjopen-2017-019101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Knudsen P., Herborg H., Mortensen A.R., Knudsen M., Hellebek A. Preventing medication errors in community pharmacy: Frequency and seriousness of medication errors. Qual. Saf. Health Care. 2007;16:291–296. doi: 10.1136/qshc.2006.018770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dalton K., Byrne S. Role of the pharmacist in reducing healthcare costs: Current insights. Integr. Pharm. Res. Pract. 2017;6:37–46. doi: 10.2147/IPRP.S108047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mossialos E., Courtin E., Naci H., Benrimoj S., Bouvy M., Farris K., Noyce P., Sketris I. From “retailers” to health care providers: Transforming the role of community pharmacists in chronic disease management. Health Policy. 2015;119:628–639. doi: 10.1016/j.healthpol.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 52.Martin L.R., Williams S.L., Haskard K.B., DiMatteo M.R. The challenge of patient adherence. Ther. Clin. Risk Manag. 2005;1:189–199. [PMC free article] [PubMed] [Google Scholar]
- 53.Laven A., Arnet I. How pharmacists can encourage patient adherence to medicines. Pharm. J. 2018;301:7916. doi: 10.1211/pj.2018.20205153. [DOI] [Google Scholar]
- 54.World Self-Medication Industry Responsible Self-Care and Self-Medication: A Worldwide Review of Consumer Surveys. Ferney-Voltaire. [(accessed on 26 November 2020)]; Available online: http://www.wsmi.org/wp-content/data/pdf/wsmibro3.pdf.
- 55.Rutter P. Role of community pharmacists in patients’ self-care and self-medication. Integr. Pharm. Res. Pract. 2015;4:57–65. doi: 10.2147/IPRP.S70403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ylä-Rautio H., Siissalo S., Leikola S. Drug-related problems and pharmacy interventions in non-prescription medication, with a focus on high-risk over-the-counter medications. Int. J. Clin. Pharm. 2020;42:786–795. doi: 10.1007/s11096-020-00984-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the nature of the study (i.e., systematic review).