Abstract
Based on the abundance of scientific publications, the polymodal sensor TRPV1 is known as one of the most studied proteins within the TRP channel family. This receptor has been found in numerous cell types from different species as well as in spermatozoa. The present review is focused on analyzing the role played by this important channel in the post-ejaculatory life of spermatozoa, where it has been described to be involved in events such as capacitation, acrosome reaction, calcium trafficking, sperm migration, and fertilization. By performing an exhaustive bibliographic search, this review gathers, for the first time, all the modulators of the TRPV1 function that, to our knowledge, were described to date in different species and cell types. Moreover, all those modulators with a relationship with the reproductive process, either found in the female tract, seminal plasma, or spermatozoa, are presented here. Since the sperm migration through the female reproductive tract is one of the most intriguing and less understood events of the fertilization process, in the present work, chemotaxis, thermotaxis, and rheotaxis guiding mechanisms and their relationship with TRPV1 receptor are deeply analyzed, hypothesizing its (in)direct participation during the sperm migration. Last, TRPV1 is presented as a pharmacological target, with a special focus on humans and some pathologies in mammals strictly related to the male reproductive system.
Keywords: TRPV1, spermatozoa, thermotaxis, chemotaxis, endocannabinoid system, mammals, human, sperm signaling, ion channel
1. Introduction
Transient receptor potential vanilloid 1 (TRPV1) is one of the most studied members within the big family of transient receptor potential (TRP) channels. The structure and function of this protein have been widely studied by numerous researchers in order to decipher its exact mechanism of action, although some aspects remain unknown. TRPV1 has been found in multiple cell types, organs, and tissues from different species, and a great number of articles and reviews have investigated and discussed this polymodal channel [1,2,3,4]. TRPV1 acts as a multimodal sensor for numerous physical, chemical, and mechanical studies by being a key player in signal transduction in multiple processes.
In the present review, we focused on the role of TRPV1 on spermatozoa physiology after ejaculation. This receptor has been shown to participate in multiple events of the sperm functions, such as the acrosome reaction, calcium trafficking, and fertilization. Here, based on exhaustive bibliographic research of international peer-reviewed literature (literature found in the database Scopus), TRPV1, its subfamily vanilloid TRP, and the big TRP family are presented and discussed. The protein structure and its multiple modulators found in different cell types and species are reviewed as well. After examining the modulators of TRPV1 previously described, only the ones found in the reproductive tract, seminal plasma, or spermatozoa with a potential role in sperm physiology were considered for further investigation in this review.
One of the most intriguing events of the post-ejaculatory life of the spermatozoa in the migration through the female tract and toward the fertilization site. During this trip, which may last from hours to days (depending on the species) [5,6], spermatozoa reside within the oviduct, where they remain bound to the oviductal epithelium [7] or are guided by various stimuli, such as rheotaxis (caused by the peristaltic movements of the oviduct smooth muscle and the fluid production), chemotaxis (promoted by the response to chemical factors) and thermotaxis (induced by the gradient of temperature). These guiding mechanisms and their relationship with the TRPV1 receptor are also examined thoroughly in this review. For instance, this channel protein has been recently recognized as a heat-sensing receptor during thermotaxis in humans [8]. Finally, the use of TRPV1 as a pharmacological target in humans and the incidence of pathologies related to the male reproductive system in mammals are explored.
2. TRPV1: Family and Subfamily
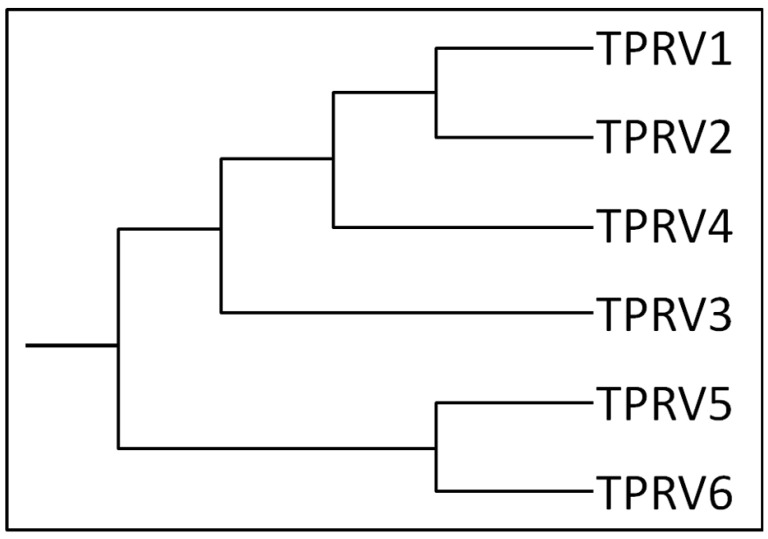
TRPV1 has been shown to be present in numerous tissues and cells of different species, from the urinary bladder [9], corneal fibroblasts [10], brain [11], and breast cancer cells [12], to the reproductive system, as female organs and placenta [13,14]. TRPV1 belongs to the vanilloid TRP subfamily, which also comprises TRPV2, TRPV3, TRPV4, TRPV5, and TRPV6. Figure 1 shows a graphical phylogenetic reconstruction of the TRPV subfamily, while Supplementary Figure S1 shows the alignment and phylogenetic reconstruction, performed using the function “build” of ETE3 v3.1.1 [15] as implemented on the GenomeNet (https://www.genome.jp/tools/ete/; accessed on 20 April 2021). Fasta sequences were obtained from UniProtKB (https://www.uniprot.org/; accessed on 20 April 2021). The tree was constructed using fasttree with slow NNI and MLACC=3 (to make the maximum-likelihood NNIs more exhaustive) [16]. Values at nodes are SH-like local support.
Figure 1.
Human TRPV channel subfamily dendrogram. The schema shows a graphical phylogenetic reconstruction of the TRPV subfamily, created from the alignment and phylogenetic reconstruction obtained after using ClustalW.
In addition to TRPV, six more subfamilies are included within the big TRP family, differentiated by their amino acid sequence and structural homology [17]: canonical TRP channels (TRPC); melastatin TRP channels (TRPM); polycystin TRP channels (TRPP); mucolipin TRP channels; ankyrin TRP channels; and no mechanoreceptor potential C (nompC) TRP (TRPN) channels.
TRPs constitute a group of ion channels that serve as cellular sensors for multiple physical and chemical stimuli and are considered the most diversified group of ion channels [18]. They are related to signal transduction and sensitivity to different mechanical, physical, and chemical (exogenous and endogenous) stimuli. Moreover, these receptors are known to be very versatile and diverse in their regulatory mechanism, gating, and selectivity, being generally characterized as non-selective to cations and thus conferring them the ability to influx several monovalent and divalent cations upon activation, including Ca2+ ions [19], K+, and Na+, as well as cyclic nucleotides [20].
TRPV channels are the best-studied TRP subfamily, probably due to the role played in the pain pathway [21]. While TRPV1 to TRPV4 are Ca2+ permeable, non-selective cationic channels, thermosensitive and sensitive to endogenous and exogenous ligands TRPV5 and TRPV6 are relatively more selective for Ca2+ ion and not thermosensitive [18,22].
TRPV1 was the first mammalian TRP channel to be cloned in 1997 [21]. Since then, many researchers around the globe have focused their efforts on deciphering the protein structure and the mechanisms regulating its function.
3. TRPV1: Protein Structure
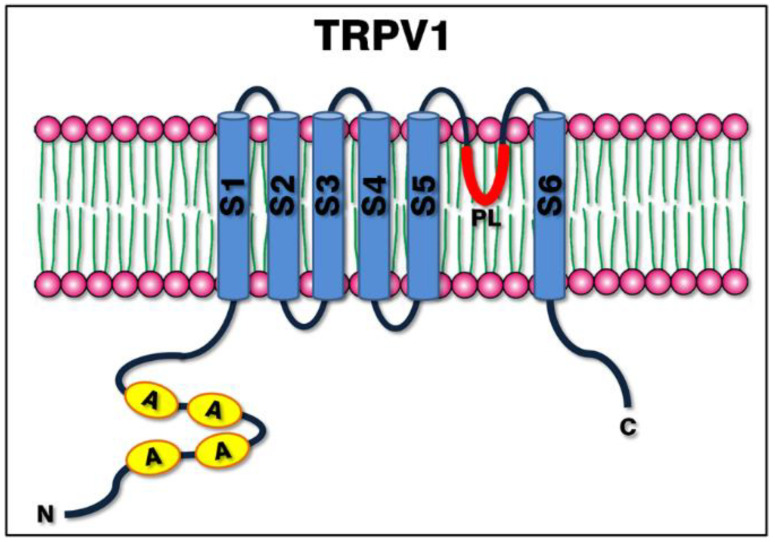
The structure of the TRPV1 channel was first solved in 2008 by Moiseenkova-Bell et al. [23]. Similar to other voltage-gated channels, TRPV1 is a six-pass transmembrane protein (S1–S6) exhibiting a four-fold symmetry around a central ion pathway, with a reentrant pore loop (PL) (hydrophobic handle) between the 5th and 6th transmembrane helices (S5 and S6, respectively), an intracellular N-terminus rich in ankyrin repeats [24] and a relative short C-terminal region [1,25,26]. The basic structure is shared with the other members of the TRP channels family, and the variability in the amino acid sequence in the 4th transmembrane helix is responsible for the voltage-dependent activation [1,20]. A representative image of the channel can be observed in Figure 2.
Figure 2.
Structure of the TRPV1 channel. The image shows a simplified schema of the protein structure within the plasma membrane, consisting of six transmembrane helices (S1 to S6), a hydrophobic pore loop (PL) between S5 and S6, the N-terminal domain rich in ankyrin repeats and the C-terminal domain.
One of the most interesting features of the TRPV1 structure is the existence of intracellular domains (e.g., the N-terminal domain) key for the interaction with other proteins, as well as the presence of binding sites for different molecules able to modulate the protein function. For example, calmodulin (CaM) protein has been found to bind to the first ankyrin repeat of the N-terminal domain [27]. Ankyrin repeats consist of approximately 33 residues repeating motif containing 24 copies of these repeats and linked to the S1 by a 77-amino-acid segment [28]. These domains are known to be present in over 400 proteins with numerous functions, mainly protein-protein interaction, and may also serve as a binding site for molecules such as ATP.
The structure of the C-terminal domain, except for two isolated fragments, is unavailable. However, through experiments of single-particle cryo-electron microscopy, the TRP box placed in this region was shown to be oriented toward the S4–S5 linker and the pre-helix-S1, suggesting its essential role in the allosteric modulation of the protein [26].
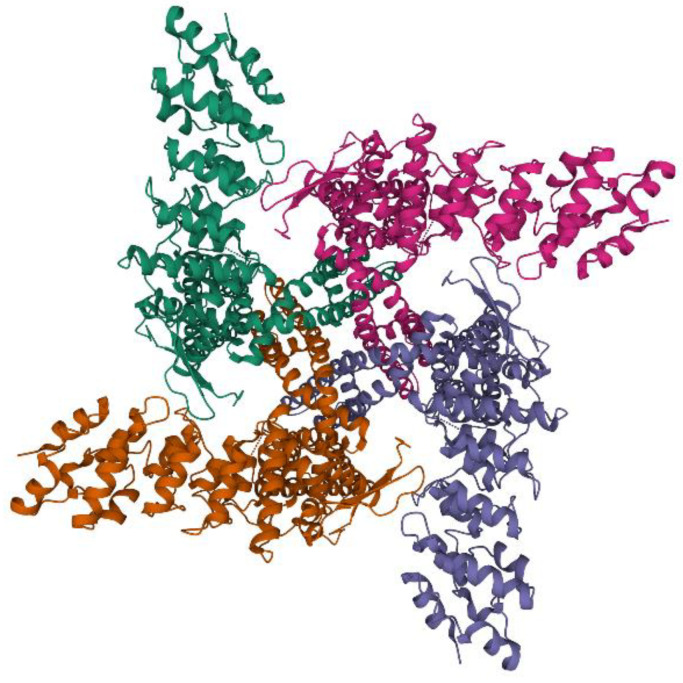
Aimed to provide a general vision of the protein structure, Figure 3 shows a three-dimensional image of the TRPV1 structure determined using single-particle electron cryo-microscopy by Liao et coll. [26]. The 3D structure can be viewed at https://www.rcsb.org/structure/3J5P (assessed on 20 April 2021), PDB ID 3J5P [29,30].
Figure 3.
Three-dimensional structure of TRPV1. The image shows a caption of the protein structure obtained by Liao et coll. (2013) using single-particle electron cryo-microscopy [26]. Obtained from https://www.rcsb.org/structure/3J5P (accessed on 20 April 2021), PDB ID 3J5P [29,30].
4. TRPV1: Function, Modulators, and Mechanisms of Regulation
Due to its wide expression in the peripheral and central nervous system (including primary sensory neurons, spinal cord, and brain), the TRPV1 channel has been demonstrated to be involved in mediating the sensation of pain in inflammation, and it was shown during the intense burning sensation after a heat exposure above 42 °C. However, the widespread expression of TRPV1 not only within the nervous system but in numerous tissues and organs in humans and other mammals suggests its involvement in multiple important functions also in non-pain-related physiological and pathological conditions [3]. For instance, TRPV1 has been demonstrated to be an active player in the cell-environment crosstalk influencing cell behavior, such as in cancer and immunity. It has been found to be expressed in cells of the innate and adaptative immune system, although its exact role remains to be determined [31]. Moreover, the involvement of this ion channel in energy homeostasis was recently discovered, probably in the control of food intake and energy expenditure [32].
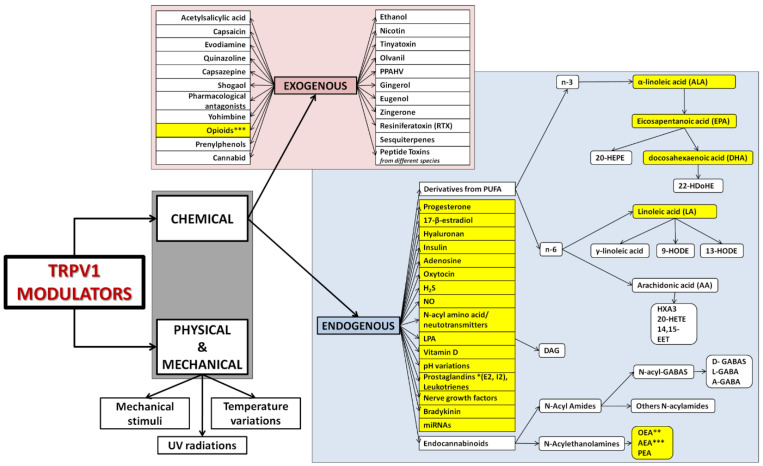
TRPV1 displays extraordinary flexibility of movement in response to different agonists [33]. Several agonists and modulators (exogenous and endogenous) of the TRPV1 function have been identified in the last 30 years. Figure 4 gathers the most common and well-known modulators of the protein. It is important to note that the classification in endogenous and exogenous depends on the source of the compounds referred to the cell, i.e., endogenous stimuli are substances produced by the cell (e.g., the spermatozoa), while exogenous source include compounds that can be found inside the organism (e.g., in the follicular fluid).
Figure 4.
Modulators of TRPV1 function. The schema shows most of the activators and modulators of TRPV1 function investigated to date, divided into two main groups: physical and physical stimuli; and chemical activators. Physical and mechanical modulators include temperature variations (heat or cold) [34], UV radiation [35,36], and mechanical stimuli [37]. The chemical activators group is divided in turn into two subgroups depending on the origin of the activator/modulator: exogenous and endogenous. Exogenous stimuli are capsaicin [38] and its antagonist capsazepine [39], resiniferatoxin (RTX) [37,40], bradykinin [41], yohimbine [42], ethanol [43], evodiamine [44], 17-β-estradiol [45], quinazoline [46], progesterone [47], numerous opioids [48], nicotine [49], hyaluronan [50], insulin [51], tinyatoxin [52], olvanil [53], acetylsalicylic acid [54], eugenol [55], sesquiterpenes [56,57,58], cannabidiol [59], prenylphenols [60], zingerone [61], shogaol [61], PPAHV [62], gingerol [63], numerous pharmacological antagonists [64,65,66,67], and peptide toxins from different species [4,68]. Endogenous activators comprise numerous compounds [1], such as the wide family derived from polyunsaturated fatty acids (PUFAs). According to the position of the first double bond present in their structures, this big family can be divided into n-3 (α-linolenic acid (ALA) and its products eicosapentanoic acid (EPA), docosahexaenoic acid (DHA), 20-hydroxyeicosapentaenoic acid (20-HEPE) and 22-hydroxyeicosapentaenoic acid (22-HDoHE)), and n-6 linoleic acid (LA) and its products γ-linoleic acid, arachidonic acid (AA) [69] (which produces hepoxylin, HXA-3, 14,15-epoxyeicosatrienoic acid, 14,15-EET, and 20-hydroxyeicosatetranoic acid, 20-HETE), 9- and 13-hydroxyoctadecadienoic acids (9-HODE and 13-HODE). Other agonists endogenously secreted are oxytocin [70], adenosine [71], nitric oxide [72], hydrogen sulfide (H2S) [73], lysophosphatidic acid (LPA) [74] and its derivative diacylglycerol [75], pH variations [76,77], vitamin D [78], N-acyl amino acids/neurotransmitters [79], miRNAs [80,81], prostaglandins, nerve growth factors and the endocannabinoids family, including N-Acyl amides [82] (N-acyl GABAS [83,84] derived then in D-GABAs, L-GABA and A-GABA) and N-acylethanolamines (NAEs) [85], such as anandamide (AEA) *** [86], oleylethanolamine (OEA) [87] and palmitoylethanolamine (PEA) [88]. * Product from arachidonic acid. ** Derived also from oleic acid, identified as a TRPV1 natural inhibitor [89]. *** Can be exogenous and endogenous. Compounds evidenced in yellow have been found to produce an effect also in spermatozoa, being synthesized by them or present in the oviductal fluid or female reproductive tract.
The two classical and widely studied agonists of TRPV1 are capsaicin and resiniferatoxin (this last considered an ultrapotent agonist) [37], although recent experiments have shown faster and longer-lasting analgesic effects by targeting some new compounds such as (not specified by the authors) [90]. The exact mechanism by which capsaicin induces the opening of TRPV1 and then its activation is not completely known yet. However, it has been demonstrated the ability of capsaicin (a lipophilic molecule) to permeate the cell plasma membrane, probably by penetrating the bilayer before flipping from the extracellular to the intracellular leaflet [91]. Then, capsaicin may bind TRPV1 at an unknown site, activating the channel and thus allowing the ATP binding to the ankyrin repeats, modulating the calcium-dependent channel desensitization [92,93].
Despite the efforts made by numerous researchers, to date, very little is known about the exact mechanisms of activation of TRPV1, giving rise to some hypotheses [94] and a consensus on the existence of various opening gates within the channel. Moreover, it is important to consider that, as discussed by Rosenbaum et coll. (2007) [95], binding sites are different from gating sites, which are also able to induce changes in the allosteric properties of the protein, thus sensitizing the channel to other agonists. As explained by the authors, capsaicin can sensitize TRPV1 to protons and heat even at low concentrations, unable to produce a direct activation [95].
What is well-known is the presence of TRPV1 in membrane microdomains (lipid rafts), i.e., cholesterol- and sphingolipid-enriched membrane domains characterized by their insolubility in Triton X-100 detergent (also known as detergent-resistant membranes, DRMs). These rafts play a pivotal role in cell signaling by being the residing site for many proteins embedded within the membrane or acting as a binding or interacting site. Even if TRPV1 concentrations are estimated to be low in normal conditions, Botto et coll. (2010) have demonstrated how bicarbonate exposure induces the protein increase within the lipid microdomains [96], thus exposing the ability of this receptor to translocate in response to certain stimuli and in certain biochemical contexts, hypothesizing an integrated functional dialogue between membrane microdomain architecture and the endocannabinoid system.
5. Role of TRPV1 on Spermatozoa
TRPV1 involvement in sperm cells maturation and function has been demonstrated by different researchers in the last years. It has been reported to be present in mature spermatozoa in many species (duck [18], fish [97], bull [98], boar [14], and human [8,99]). TRPV5 has also been detected in rats [100], while TRPV4 may be present in various vertebrates sperm cells. The last has been observed to be present as an N-glycosylated protein, which activation induces a Ca2+ influx, suggesting its involvement in sperm motility [101]. Table 1 gathers all the species where TRPV1 was found on spermatozoa, while Table 2 presents all the modulators from Figure 4 that have been found in the female reproductive tract or in the seminal plasma and on spermatozoa, and which relationship with the process of reproduction has been already described or exit enough evidence to be hypothesized.
Table 1.
Functional sperm TRPV1 channels described in different vertebrates.
Table 2.
Modulators of TRPV1 function found in the female reproductive tract, seminal plasma, or spermatozoa in different mammals.
| TRPV1 Modulator | Female Reproductive Tract | Seminal Plasma/Spermatozoa | Animal Group * | Reference |
|---|---|---|---|---|
| 17-β-estradiol | X | Bovine, swine, rabbit, equine | [103,104,105] | |
| Anandamide (AEA) | X | X | Bovine, human, swine, murine | [14,106,107,108] |
| Arachidonic acid (AA) ** | X | Human | [109,110] | |
| Bradykinin | X | Swine | [111] | |
| Docosahexaenoic acid (DHA) ** | X | Human | [109,110,112] | |
| Eicosapentanoic acid (EPA) ** | X | Human | [109,110] | |
| H2S | X | X | Human | [113,114,115] |
| Hyaluronan | X | All mammals | [116,117] | |
| Insulin | X | Human | [118] | |
| Leukotriene B4 | X | Bovine | [119] | |
| Linoleic acid (LA) ** | X | Human | [109,110] | |
| miRNAs | X | X | Murine, bovine, human | [120,121,122] |
| N-acyl amino acids | X | X | Human | [123] |
| Nerve growth factors | X | Rabbit, bovine | [124,125] | |
| NO | X | X | Bovine, human, swine, mouse, equine | [113,115,126] |
| Oleoylethanolamine (OEA) | X | Bovine | [106] | |
| Opioids | X | Human | [127] | |
| Oxytocin | X | Human | [128] | |
| Palmitoylethanolamine (PEA) | X | Bovine | [106] | |
| pH variations | X | Human | [129] | |
| Progesterone | X | Bovine, swine, rabbit, equine | [103,104,105] | |
| Prostaglandins | X | Bovine | [126] | |
| Vitamin D | X | X | Human | [130,131,132] |
| α-linolenic acid (ALA) ** | X | Human | [109,110] |
* Example (but not limited to) of the animal species where the modulator was found. ** Component of the sperm phospholipid membrane.
TRPV1 has been suggested to have an important physiological role in sperm capacitation and acrosome reaction (AR), thus contributing to the complex process of fertilization [133]. Indeed, in mammals, fertilization involves multiple events, initiating either with the sperm cells entrance into the cervix and the later headway of the healthiest spermatozoa [5,113] toward the uterus or the direct deposition within the uterus, depending on the species. Once the spermatozoa reach the oviduct [134], they bind to the oviductal epithelium for hours to days forming a functional sperm reservoir as demonstrated in several mammalian species [135]. After this indefinite period of time and by a still partially unknown mechanism [7], spermatozoa detach from the oviduct and continue their way toward the oocyte, interacting afterward with the proteins from the zona pellucida (ZP) of the egg and thus triggering the release of the acrosome content with the enzymes necessary to penetrate the ZP. Once the sperm cells adhere to the plasma membrane via its equatorial region, fuse, and incorporate the spermatozoon into the ooplasm until the fertilization is completed. Thus, the zygote can divide by successive mitosis to form an embryo [136].
One of the current challenges in regard to the fertilization process remains the understanding of the complex and still completely unknown communication between the spermatozoa and the female environment, which prevents premature capacitation and helps to preserve the sperm fertilizing potential until the encounter with the egg. To achieve a successful sperm-egg interaction, two conditions are mandatory: both capacitated spermatozoa and mature oocytes must be present at the same location in the oviduct. The first condition implies that spermatozoa should acquire the fertilizing ability through the process of capacitation in view of the meeting with the egg, experiencing a series of complex events that modify some of their biochemical, chemical, or physicochemical features. The second one requires the participation of the intricate neuroendocrine female axis, which by the active role of hormones such as progesterone and estradiol interacts not only with the female tract (for instance, the ovary and oviducts) but also directly with the spermatozoa, contributing to the successful encounter between the male and female gametes. However, numerous mechanisms involved in mammalian fertilization remain to be elucidated, such as the sperm/egg ratio (specifically at the fertilization site) that is somehow and highly regulated to avoid polyspermy.
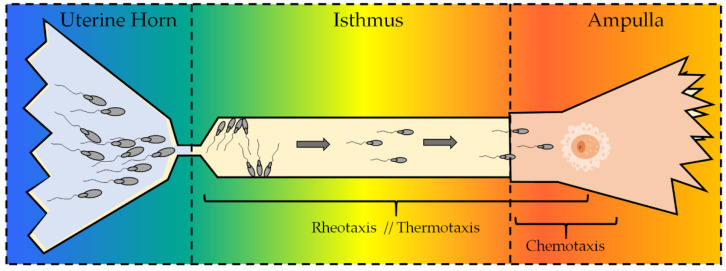
One of the fertilization events that still merits further investigation in the reproduction field is the sperm selection that is taking place in the female genital tract, from where the semen is deposited to the site of fertilization. This issue has attracted the attention of numerous researchers during the last decades (see the reviews by Suarez and Pacey 2006 [137] and Miller 2018 [138]). Along with the active peristaltic movements due to the contractions of the oviduct smooth muscle and the fluid production (rheotaxis) [139], chemotaxis and thermotaxis have been proposed as the mechanisms that help the spermatozoa to reach the fertilization site once in the oviducts [140]. It is thought that, in vivo, thermotaxis, rheotaxis, and chemotaxis are complementary, involving spermatozoa being first guided by thermotaxis and rheotaxis and then mainly by chemotaxis when they are proximal to the oocyte [141]. However, the most plausible explanation is that the three mechanisms could occur simultaneously in some regions of the oviduct, contributing together to the arrival of the sperm cell to the meeting with the oocyte. It is worthy to note that the oviduct should be intended as a 4D system in which every event occurs in a certain location and time, which could help to understand the variations in the hormone concentrations (e.g., progesterone or estradiol) in a precise location and period of time. Thus, rheotaxis and thermotaxis may act in a first moment, being then not replaced but supported by the chemical stimuli to complete the journey. Figure 5 shows a diagram of the oviduct of mammals, with the three sperm gradients in the tract where these mechanisms are supposed to exert their guidance. TRPV1 acts as a polymodal sensor, reacting in a graded manner to diverse physical, mechanical, and chemical stimuli and changing its response depending on the concentrations, agonists, modulators, and even the environment [142]. Its function within these migration processes is discussed below.
Figure 5.
Female oviduct and sperm migration. The diagram shows the female tract of mammals and the three sperm guidance mechanisms, depending on the site in which they have been described to act. While rheotaxis and thermotaxis have been suggested to act mostly in long-range distances, chemotaxis is supposed to take place only in the proximity of the female egg (considering that the exact fertilization site is species-dependent). The colors represent the thermal and chemical gradient (from left to right).
5.1. Sperm Chemotaxis, TRPV1, and the Endocannabinoid System (ECS)
As shown by numerous researchers [139,143,144,145,146,147], chemotaxis guides spermatozoa and helps them to find the oocyte due to the great sensitivity of the sperm cells to picomolar concentrations of progesterone (P4) [144] and other molecules from the follicular or oviductal fluid [141]. On this basis, hormones such as P4, secreted from the cumulus cells surrounding the oocyte, act as a sperm chemoattractant [144,148], demonstrated on different animal species as human [144], rabbit [149], equine [147], mouse [150] and swine [146]. P4 then induces the influx of Ca2+ by activating progesterone receptors as CatSper receptors [151], participating in the sperm migration. Since extracellular Ca2+ is a necessary condition for sperm chemotaxis, the inhibition of the calcium channels may block the process of sperm migration, as demonstrated in some species [152,153].
Interestingly, a multifunctional molecule has been shown to modify the function of numerous ion channels, probably by altering the thickness and elastic properties of the surrounding lipid bilayer [154] or interacting with protein channels [155]. This molecule is cholesterol, a major component of plasma membranes that confers them high mechanical strength and preventing from cell lysis. Their concentrations vary from cell to cell and from one species to another, while the distribution of this amphipathic molecule is confined to the membrane microdomains or lipid rafts. Some researchers have evaluated the role of cholesterol on TRPV1 function. For instance, Picazo-Juarez et coll. (2011) found a cholesterol-binding site in TRPV1, precisely in the S5 helix. The existence of this binding motif has been proposed as responsible for the cholesterol sensitivity of TRPV1 [156]. In addition to that, some researchers have demonstrated a depletion of the TRPV1 protein amount after cholesterol depletion in adult rat dorsal root ganglion neurons [157], suggesting that TRPV1 could be localized in the cholesterol-rich microdomains, while studies in the cell line HEK293 found TRPV1 in cholesterol-poor (non-rafts) microdomains but not in cholesterol-rich rafts [156]. Storti et coll. (2015) suggested a spatial-temporal regulation of TRPV1 dynamics, proposing three populations of TRPV1: the first able to bind caveolin-1 protein (present in the rafts); the second interacting with tubulin; and the third as a freely-fast diffusion fraction [158]. With this information, it is possible to suggest a species- and cell-specific role of cholesterol modulation of the TRPV1 function, with important participation of different proteins from the raft microdomains.
In addition to the physiological role exerted by TRPV1 in the transmembrane calcium trafficking [159], it was also demonstrated to be a molecular target for a great variety of molecules (evidenced in navy blue in Figure 4) that were found either within the oviductal fluid or directly synthesized by the sperm cells. This complex ensemble of molecules in which concentrations are spatial-temporal dependent influence in a coordinated manner the sperm migration through the oviduct.
Among these molecules (evidenced in navy blue in Figure 4), anandamide stands out as an example, a molecule from the endocannabinoid system. Some molecules and receptors from the endocannabinoid system have been demonstrated to be involved in the dialogue between the female oviductal fluid and the spermatozoa during the sperm migration along the reproductive tract. Anandamide (arachidonoylethanolamide, AEA) is synthesized, degraded, bound, and transported by the biochemical machinery present in mammalian spermatozoa [14]. This major endogenous endocannabinoid/endovanilloid ligand is present in the uterus and the implantation site [160,161], where AEA was found to stimulate the migration of endometrial stromal cells via type 1 cannabinoid receptor (CB1R) in a dose-dependent manner by activating the ERK1/2 and PI3K/Akt pathways [162]. It is also present in seminal plasma and uterine fluids [14], activating or inhibiting cannabinoid receptors depending on its concentration, producing a dual-stage effect that could be explained in a three-step process:
First, the high levels of AEA within the seminal plasma and the uterine fluid may prevent the sperm cells from premature capacitation by acting as an inhibitor. AEA interacts with CB1R, a Gi/o protein-coupled receptor in which activation, concurrently with the low levels of bicarbonate, prevents the increase in the membrane fluidity, known as a key feature of capacitated spermatozoa. In fact, during the normal process of capacitation, the plasma membrane (PM) and the outer acrosome membrane (OAM) become less stable and gradually acquire the ability to fuse (fusogenicity) [163,164]. This status is possible due to the high-stable asymmetrical organization of the membranes, in which the aminophospholipids phosphatidylserine (PS) and phosphatidylethanolamine (PE) are concentrated in the inner leaflet, and the choline phospholipids sphingomyelin (SM) and phosphatidylcholine (PC) in the outer leaflet of the sperm head. This asymmetry is established and maintained by the action of several translocating enzymes with various phospholipid specificities and modulated by PKA-dependent phosphorylation. Thus, if fusogenicity increases, AR could take place before the meeting with the ZP of the oocyte. If AR is not fully completed, the spermatozoa are unable to release the acrosome content, preventing precocious capacitation or death of the sperm cell.
In the second step, spermatozoa experience a variation in the AEA levels during their way toward the oocyte, moving from high concentrations of AEA to low concentrations (activating state) within the oviduct [165]. At the same time, the concentration of the ion bicarbonate increases, producing a migration of CB1R to the equatorial region of the sperm and thus attenuation of its activity. It then activates the soluble isoform of adenylyl cyclase (sAC), giving rise to an increase in the intracellular cAMP levels acting via a PKA-dependent pathway [14,99,166]. This increase in the intracellular AMP, along with many others, contributes to the sperm acquisition of their fertilizing ability within the oviduct in vivo or after incubation under capacitating conditions in vitro. The PM phospholipid redistribution and lipid scrambling take place, leading to an increase in the sperm membrane fluidity and disorder and the cholesterol efflux by soluble protein acceptors from the anterior sperm head. The calcium-dependent polymerization of G-actin provokes the formation of an F-actin network that forms a diaphragm between PM and OAM, a structure of great importance for signal transduction [167].
During the third step, an increase in the endogenous AEA concentrations (secreted by the sperm cells) is likely to play a role in stabilizing the acrosome membrane, thus preventing non-targeted AR by interacting this time with TRPV1.
Ref. [14,99], which acts as a controller of the F-actin network. TRPV1, located over the post-equatorial area of the sperm head, is inactive at early capacitation stages. As capacitation progresses, this protein translocates from the post-equatorial to the anterior region of the sperm head, becoming active. Its activation thus triggers a membrane depolarization wave, opening the voltage-operated calcium channels (VOCC), leading to an increase in the intracellular calcium concentration. This calcium gradient is able to activate some receptors, such as TRPV1, which may contribute to the modulation of the capacitation status. The increase in the intracellular calcium concentrations helps then in the F-actin depolymerization and the disappearance of the actin network, allowing the PM and OAM interaction.
Altogether, the information conveyed so far suggests an indirect role for TRPV1 in sperm chemotaxis, which may be controlled by molecules of the endocannabinoid system such as anandamide. Indeed, the concentrations of AEA and its differences of concentration within the female tract could influence sperm migration, as in other cell types. For example, Ca2+ influx upon activation of CB1R and TRPV1 by AEA has been demonstrated to induce the sperm release from the oviductal sperm reservoir in bovine [168]. Another study performed in sea urchins by Guerrero et coll. (2010) suggested the sperm’s ability to increase the concentration of Ca2+ in the flagellum. Moreover, they observed a curvature in the presence of a negative chemoattractant gradient, which could constitute a characteristic of chemotactic motility not only in sea urchin spermatozoa but in other species as well. This response could be adapted, promoting the sperm-egg interaction and the fusion of their membranes [169]. A detailed study of this effect would be necessary for mammal species, including the potential role that TRPV1 could exert in this sperm ability.
More recently, several studies examined the regulatory role played by microRNAs (miRNAs) in posttranscriptional regulation of TRPV1. For instance, it was demonstrated that miR-338-3p directly targets TRPV1, increasing mechanical allodynia and thermal hyperalgesia as well as the expression of inflammation-associated genes (COX-2, TNF-α, and IL-6) [80]. Regarding the spermatozoa, dysregulation of miRNAs has been correlated to male infertility [170], allowing to hypothesize a correlation between miRNAs and TRPV1 receptor also in spermatozoa. Furthermore, numerous researchers have correlated the up- or down-regulation of different miRNAs in asthenozoospermic, oligoasthenozoospermic and/or tetrazoospermic patients compared to normozoospermic men, showing a potentially interesting role in the diagnosis of male infertility [121,171,172,173]. However, further research is needed to decipher their exact correlation.
5.2. Thermotaxis and TRPV1: Role in Human Spermatozoa
In humans, the presence of the TRPV1 receptor has been demonstrated in both the spermatozoa and the testis [8,99]. In spermatozoa, the expression of this receptor is associated with the sperm’s ability to move toward a temperature gradient. While chemotaxis is considered to exert short-range guidance [174], thermotaxis is chemically defined as the movement toward or away from a thermal stimulus, and it has been studied in mammalian spermatozoa as long-range guidance. It is well accepted that during ovulation in mammals, a difference of temperature is established between the sperm reservoir and the fertilization site, reaching a gap of approximately 2 °C in some species as rabbit [175] or 0.7 °C in swine [176]. Moreover, it has been demonstrated the sperm has the capability to sense small temperature differences, responding even to changes as little as 0.0006 °C in humans [177]. Even if the exact molecular mechanisms for sperm migration by thermotaxis are completely unknown, TRPV1 has been identified as one of the receptors able to identify the temperature fluctuations and guide the spermatozoa across the oviduct toward the fertilization site. Furthermore, the involvement of the distal half of the C-terminal domain in the thermal sensitivity [178] was demonstrated, shedding some light into the function of this protein domain.
The exposure of spermatozoa to a higher temperature in some tracts of the female oviduct (specifically, in the fertilization site) has been shown to influence the membrane structure and fluidity as well [163]. Studies performed in humans showed that non-capacitated spermatozoa are able to migrate toward a gradient of 31–37 °C, demonstrating an amplified response in capacitated spermatozoa. De Toni and coll. (2016) demonstrated thus the role of TRPV1 as a mediator of sperm thermotaxis in humans, related to the calcium-mobilizing properties of TRPV1 and the calcium-dependent increase in motility observed during sperm migration by thermotaxis [8]. Indeed, sperm cells that preferentially move toward a higher temperature gradient have an increased expression of the TRPV1 channel when compared to non-migrating cells. Despite these important results, it is yet to be clarified the exact distribution and localization of TRPV1 in human spermatozoa [179]. From a molecular point of view, the study of TRPV1 function could be of great importance to decipher if the protein is directly involved in thermotaxis or in concomitant processes (i.e., capacitation or acrosome reaction [179]). This will surely bring new insights regarding the role of TRPV1 in sperm function and also contribute to the discovering of new therapeutic strategies to treat male infertility.
5.3. Sperm Rheotaxis
Sperm rheotaxis has been suggested as a major guidance and selection force during the sperm migration toward the egg; however, the exact mechanism of action remains unknown, and some of the results obtained over the last few years are contradictory. Earlier experiments performed by Miki and Clapham suggested that this form of guidance may be due to the spiral rotation of the sperm tail caused by the increase in the intracellular Ca2+ concentrations, which increases the amplitude of the distal tail excursion and thus the tangential force, producing an effect of sperm hyperactivation. This condition, characterized by asymmetric and larger amplitude flagellar waveform, helps the sperm cells to swim in viscous solutions [139]. Additionally, mechanical forces have been studied on mammalian sperm in relation to the sperm detachment from the oviductal epithelial cells, which may be assisted by a form of mechanical hyperactivation [180,181]. Other than TRPV4, TRPV1 is also recognized as a sensor for hyperosmolarity in some cell types [182], playing a pivotal role in cell homeostasis and ion balance. This faculty to act as an osmolarity sensor is supposed to help in the sperm journey along the oviduct.
Regarding the rheotactic movements induced by the intracellular calcium, later experiments were realized in human sperm by Zhang et coll. (20016) aimed to classify rheotaxis as a passive or active process revealed the absence of differences in flagellar beating and intracellular Ca2+ between freely swimming spermatozoa and sperm guided by rheotaxis. While the authors maintain that rheotaxis is a passive process with no flow sensing involved, they hypothesize as well that weak or not perceptible signaling derived from the Ca2+ entry into the cell may occur [183], something supported as well by other researchers [139,184] and that may count on CatSper as the channel for the calcium entry [139]. Very recently, Schiffer and collaborators suggested through their experiments in humans and mice that sperm rheotaxis was enabled by passive biomechanical and hydrodynamic processes rather than calcium signaling mediated by CatSper [185]. Even if a role for TRPV1 could be easy to hypothesize due to the potential participation of calcium signaling and their multiple well-known modulators met along the sperm journey, what it is clear here is that further experiments would be necessary to establish the exact mechanism by which this migration force occurs, the participation levels for TRPV1 and the commitment with chemo- and thermotaxis.
6. TRPV1 as a Pharmacological Target and Future Perspectives
Studying mice mutants is a useful tool to study numerous pathologies in human and other animal species. Numerous researchers have used the homozygous mutant for TRPV1 in mouse species to carry out their research activity. Trpv1 KO (trpv−/−) are viable and with no gene product in dorsal root ganglia and low or absent response to vanilloid compounds, heat, or pH variations. Moreover, they are characterized by a lack of response after capsaicin subcutaneous injection and deficits in thermally evoked pain behavior. Interestingly, TRPV1 KO mice live longer than wild-types, displaying a youthful metabolic profile, a higher tolerance to glucose, better motor coordination, and reduced aging. It was recently demonstrated that TRPV1 is crucial to maintain a constant body temperature, being necessary for thermal homeostasis [186]. Additionally, TRPV1 KO mice are fertile, thus complicating the enlightenment of the relationship between TRPV1 expression and male infertility. However, it is easily explained due to the coexistence of redundant mechanisms as a safety strategy, by which the failure of one of them does not affect the efficiency of the whole process [187]. Thus, to date, it is clear that TRPV1 plays a role in sperm function and capacitation in a mechanism related to the endocannabinoid system [188]. Lewis and collaborators demonstrated a decrease in the TRPV1 binding to CB receptors translated into a loss of function in infertile patients. However, the mRNA and protein levels remained stable, complicating the clarification of these decreases and thus the effect on capacitation and the sperm function [107].
Regarding the pharmacological spectrum, the aim of the TRPV1 study has been focused mainly on the area of analgesics and pain relief by exploiting the agonists/antagonists properties of the great number of these protein modulators. Many compounds have been developed to either activate or inhibit this receptor, but to date, none of them are included in routine clinical practice. However, further experiments are needed with the scope of deciphering the TRPV1 ligands and the interaction and binding sites, as well as the complete structure of the protein within the membrane. Furthermore, the data gathered here bring to light the role of TRPV1 in the process of sperm migration-related specifically to chemo- and thermotaxis guidance mechanisms, which could constitute a new therapeutical tool to be applied for sperm selection in human as in other animal species.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijms22094306/s1, Figure S1: Dendrogram of human TRPV1. Supplementary Figure S1 shows the alignment and phylogenetic reconstruction, performed using the function “build” of ETE3 v3.1.1 [15] as implemented on the GenomeNet (https://www.genome.jp/tools/ete/; accessed on 20 April 2021). Fasta sequences were obtained from UniProtKB (https://www.uniprot.org/; accessed on 20 April 2021). The tree was constructed using fasttree with slow NNI and MLACC=3 (to make the maximum-likelihood NNIs more exhaustive) [16]. Values at nodes are SH-like local support.
Author Contributions
Conceptualization, M.R.-S. and N.B.; methodology, N.B.; software, L.V.; validation, M.R.-S., N.B., and B.B.; formal analysis, M.R.-S., N.B., L.V., C.C., A.T., G.C., J.M.-S. and B.B.; investigation, M.R.-S., N.B., L.V., C.C., A.T., G.C., J.M.-S. and B.B.; resources, N.B. and B.B.; data curation, M.R.-S., L.V., and N.B.; writing—original draft preparation, M.R.-S. and N.B.; writing—review and editing, M.R.-S., N.B., L.V., C.C., A.T., G.C., J.M.-S. and B.B.; visualization, M.R.-S., L.V., and N.B.; supervision, N.B. and B.B.; project administration, N.B. and B.B.; funding acquisition, N.B. and B.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Benítez-Angeles M., Morales-Lázaro S.L., Juárez-González E., Rosenbaum T. TRPV1: Structure, Endogenous Agonists, and Mechanisms. Int. J. Mol. Sci. 2020;21:3421. doi: 10.3390/ijms21103421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jara-Oseguera A., Simon S., Rosenbaum T. TRPV1: On the Road to Pain Relief. Curr. Mol. Pharmacol. 2010;1:255–269. doi: 10.2174/1874467210801030255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White J.P.M., Urban L., Nagy I. TRPV1 Function in Health and Disease. Curr. Pharm. Biotechnol. 2010;12:130–144. doi: 10.2174/138920111793937844. [DOI] [PubMed] [Google Scholar]
- 4.Geron M., Hazan A., Priel A. Animal toxins providing insights into TRPV1 activation mechanism. Toxins. 2017;9:326. doi: 10.3390/toxins9100326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suarez S.S. Mammalian sperm interactions with the female reproductive tract. Cell Tissue Res. 2016;363:185–194. doi: 10.1007/s00441-015-2244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ardon F., Markello R.D., Hu L., Deutsch Z.I., Tung C.-K., Wu M., Suarez S.S. Dynamics of Bovine Sperm Interaction with Epithelium Differ Between Oviductal Isthmus and Ampulla. Biol. Reprod. 2016;95:90. doi: 10.1095/biolreprod.116.140632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramal-Sanchez M., Bernabo N., Tsikis G., Blache M.C., Labas V., Druart X., Mermillod P., Saint-Dizier M. Progesterone induces sperm release from oviductal epithelial cells by modifying sperm proteomics, lipidomics and membrane fluidity. Mol. Cell. Endocrinol. 2020;504 doi: 10.1016/j.mce.2020.110723. [DOI] [PubMed] [Google Scholar]
- 8.De Toni L., Garolla A., Menegazzo M., Magagna S., Di Nisio A., Šabović I., Rocca M.S., Scattolini V., Filippi A., Foresta C. Heat sensing receptor TRPV1 is a mediator of thermotaxis in human spermatozoa. PLoS ONE. 2016;11:e0167622. doi: 10.1371/journal.pone.0167622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Szallasi A., Conte B., Goso C., Blumberg P.M., Manzini S. Characterization of a peripheral vanilloid (capsaicin) receptor in the urinary bladder of the rat. Life Sci. 1993;52 doi: 10.1016/0024-3205(93)90051-4. [DOI] [PubMed] [Google Scholar]
- 10.Yang Y., Yang H., Wang Z., Mergler S., Wolosin J.M., Reinach P.S. Functional TRPV1 expression in human corneal fibroblasts. Exp. Eye Res. 2013;107:121–129. doi: 10.1016/j.exer.2012.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marrone M.C., Morabito A., Giustizieri M., Chiurchiù V., Leuti A., Mattioli M., Marinelli S., Riganti L., Lombardi M., Murana E., et al. TRPV1 channels are critical brain inflammation detectors and neuropathic pain biomarkers in mice. Nat. Commun. 2017;8:15292. doi: 10.1038/ncomms15292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weber L.V., Al-Refae K., Wölk G., Bonatz G., Altmüller J., Becker C., Gisselmann G., Hatt H. Expression and functionality of TRPV1 in breast cancer cells. Breast Cancer Targets Ther. 2016;8:243–252. doi: 10.2147/BCTT.S121610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dörr J., Fecher-Trost C. Advances in Experimental Medicine and Biology. Volume 704. Springer; Berlin/Heidelberg, Germany: 2011. TRP channels in female reproductive organs and placenta; pp. 909–928. [DOI] [PubMed] [Google Scholar]
- 14.Maccarrone M., Barboni B., Paradisi A., Bernabò N., Gasperi V., Pistilli M.G., Fezza F., Lucidi P., Mattioli M. Characterization of the endocannabinoid system in boar spermatozoa and implications for sperm capacitation and acrosome reaction. J. Cell Sci. 2005;118:4393–4404. doi: 10.1242/jcs.02536. [DOI] [PubMed] [Google Scholar]
- 15.Huerta-Cepas J., Serra F., Bork P. ETE 3: Reconstruction, Analysis, and Visualization of Phylogenomic Data. Mol. Biol. Evol. 2016;33:1635–1638. doi: 10.1093/molbev/msw046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Price M.N., Dehal P.S., Arkin A.P. Fasttree: Computing large minimum evolution trees with profiles instead of a distance matrix. Mol. Biol. Evol. 2009;26:1641–1650. doi: 10.1093/molbev/msp077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu L.J., Sweet T.B., Clapham D.E. International Union of Basic and Clinical Pharmacology. LXXVI. Current progress in the Mammalian TRP ion channel family. Pharmacol. Rev. 2010;62:381–404. doi: 10.1124/pr.110.002725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Majhi R.K., Kumar A., Giri S., Goswami C. Differential expression and localization of thermosensitive Transient Receptor Potential Vanilloid (TRPV) channels in the mature sperm of white pekin duck (Anas platyrhynchos) bioRxiv. 2020 doi: 10.1101/2020.02.10.941732. [DOI] [PubMed] [Google Scholar]
- 19.Nilius B., Owsianik G. The transient receptor potential family of ion channels. Genome Biol. 2011;12:1–11. doi: 10.1186/gb-2011-12-3-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhu M.X. TRP Channels. CRC Press; Boca Raton, FL, USA: 2016. [Google Scholar]
- 21.Caterina M.J., Schumacher M.A., Tominaga M., Rosen T.A., Levine J.D., Julius D. The capsaicin receptor: A heat-activated ion channel in the pain pathway. Nature. 1997;389:816–824. doi: 10.1038/39807. [DOI] [PubMed] [Google Scholar]
- 22.Kumar A., Mishra A.K., Swain D.K., Singh V., Yadav S., Saxena A. Role of transient receptor potential channels in regulating spermatozoa functions: A mini-review. Vet. World. 2018;11:1618–1623. doi: 10.14202/vetworld.2018.1618-1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moiseenkova-Bell V.Y., Stanciu L.A., Serysheva I.I., Tobe B.J., Wensel T.G. Structure of TRPV1 channel revealed by electron cryomicroscopy. Proc. Natl. Acad. Sci. USA. 2008;105:7451–7455. doi: 10.1073/pnas.0711835105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lishko P.V., Procko E., Jin X., Phelps C.B., Gaudet R. The Ankyrin Repeats of TRPV1 Bind Multiple Ligands and Modulate Channel Sensitivity. Neuron. 2007;54:905–918. doi: 10.1016/j.neuron.2007.05.027. [DOI] [PubMed] [Google Scholar]
- 25.Tominaga M., Tominaga T. Structure and function of TRPV1. Pflugers Arch. Eur. J. Physiol. 2005;451:143–150. doi: 10.1007/s00424-005-1457-8. [DOI] [PubMed] [Google Scholar]
- 26.Liao M., Cao E., Julius D., Cheng Y. Structure of the TRPV1 ion channel determined by electron cryo-microscopy. Nature. 2013;504:107–112. doi: 10.1038/nature12822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenbaum T., Gordon-Shaag A., Munari M., Gordon S.E. Ca2+/Calmodulin Modulates TRPV1 Activation by Capsaicin. J. Gen. Physiol. 2004;123:53–62. doi: 10.1085/jgp.200308906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ma L., Yang F., Vu S., Zheng J. Exploring functional roles of TRPV1 intracellular domains with unstructured peptide-insertion screening. Sci. Rep. 2016;6:33827. doi: 10.1038/srep33827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.RCSB PDB: Homepage. [(accessed on 26 January 2021)]; Available online: https://www.rcsb.org/
- 30.Sehnal D., Rose A.S., Koča J., Burley S.K., Velankar S. Mol*: Towards a common library and tools for web molecular graphics. MolVA; Proceedings of the Conference of Visualization, EuroVis; Brno, Czech Republic. 4–8 June 2018; [DOI] [Google Scholar]
- 31.Bujak J.K., Kosmala D., Szopa I.M., Majchrzak K., Bednarczyk P. Inflammation, Cancer and Immunity—Implication of TRPV1 Channel. Front. Oncol. 2019;9:1087. doi: 10.3389/fonc.2019.01087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Christie S., Wittert G.A., Li H., Page A.J. Involvement of TRPV1 Channels in Energy Homeostasis. Front. Endocrinol. 2018;9:420. doi: 10.3389/fendo.2018.00420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.López-Romero A.E., Hernández-Araiza I., Torres-Quiroz F., Tovar-Y-Romo L.B., Islas L.D., Rosenbaum T. TRP ion channels: Proteins with conformational flexibility. Channels. 2019;13:207–226. doi: 10.1080/19336950.2019.1626793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zheng W., Wen H. Heat activation mechanism of TRPV1: New insights from molecular dynamics simulation. Temperature. 2019;6:120–131. doi: 10.1080/23328940.2019.1578634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Caterina M., Pang Z. TRP Channels in Skin Biology and Pathophysiology. Pharmaceuticals. 2016;9:77. doi: 10.3390/ph9040077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee Y.M., Kang S.M., Lee S.R., Kong K.H., Lee J.Y., Kim E.J., Chung J.H. Inhibitory effects of TRPV1 blocker on UV-induced responses in the hairless mice. Arch. Dermatol. Res. 2011;303:727–736. doi: 10.1007/s00403-011-1153-9. [DOI] [PubMed] [Google Scholar]
- 37.Caterina M.J., Julius D. The vanilloid receptor: A molecular gateway to the pain pathway. Annu. Rev. Neurosci. 2001;24:487–517. doi: 10.1146/annurev.neuro.24.1.487. [DOI] [PubMed] [Google Scholar]
- 38.Szolcsányi J. Forty years in capsaicin research for sensory pharmacology and physiology. Neuropeptides. 2004;38:377–384. doi: 10.1016/j.npep.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen T.L., Nam Y.S., Lee S.Y., Kim H.C., Jang C.G. Effects of capsazepine, a transient receptor potential vanilloid type 1 antagonist, on morphine-induced antinociception, tolerance, and dependence in mice. Br. J. Anaesth. 2010;105:668–674. doi: 10.1093/bja/aeq212. [DOI] [PubMed] [Google Scholar]
- 40.Raisinghani M., Pabbidi R.M., Premkumar L.S. Activation of transient receptor potential vanilloid 1 (TRPV1) by resiniferatoxin. J. Physiol. 2005;567:771–786. doi: 10.1113/jphysiol.2005.087874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mathivanan S., Devesa I., Changeux J.P., Ferrer-Montiel A. Bradykinin induces TRPV1 exocytotic recruitment in peptidergic nociceptors. Front. Pharmacol. 2016;7 doi: 10.3389/fphar.2016.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dessaint J., Yu W., Krause J.E., Yue L. Yohimbine inhibits firing activities of rat dorsal root ganglion neurons by blocking Na+ channels and vanilloid VR1 receptors. Eur. J. Pharmacol. 2004;485:11–20. doi: 10.1016/j.ejphar.2003.11.039. [DOI] [PubMed] [Google Scholar]
- 43.Nicoletti P., Trevisani M., Manconi M., Gatti R., De Siena G., Zagli G., Benemei S., Capone J.A., Geppetti P., Pini L.A. Ethanol causes neurogenic vasodilation by TRPV1 activation and CGRP release in the trigeminovascular system of the guinea pig. Cephalalgia. 2008;28:9–17. doi: 10.1111/j.1468-2982.2007.01448.x. [DOI] [PubMed] [Google Scholar]
- 44.Pearce L.V., Petukhov P.A., Szabo T., Kedei N., Bizik F., Kozikowski A.P., Blumberg P.M. Evodiamine functions as an agonist for the vanilloid receptor TRPV1. Org. Biomol. Chem. 2004;2:2281–2286. doi: 10.1039/b404506h. [DOI] [PubMed] [Google Scholar]
- 45.Payrits M., Sághy É., Csekő K., Pohóczky K., Bölcskei K., Ernszt D., Barabás K., Szolcsányi J., Ábrahám I.M., Helyes Z., et al. Estradiol Sensitizes the Transient Receptor Potential Vanilloid 1 Receptor in Pain Responses. Endocrinology. 2017;158:3249–3258. doi: 10.1210/en.2017-00101. [DOI] [PubMed] [Google Scholar]
- 46.Zheng X., Hodgetts K.J., Brielmann H., Hutchison A., Burkamp F., Brian Jones A., Blurton P., Clarkson R., Chandrasekhar J., Bakthavatchalam R., et al. From arylureas to biarylamides to aminoquinazolines: Discovery of a novel, potent TRPV1 antagonist. Bioorganic Med. Chem. Lett. 2006;16:5217–5221. doi: 10.1016/j.bmcl.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 47.Ortíz-Rentería M., Juárez-Contreras R., González-Ramírez R., Islas L.D., Sierra-Ramírez F., Llorente I., Simon S.A., Hiriart M., Rosenbaum T., Morales-Lázaro S.L. TRPV1 channels and the progesterone receptor Sig-1R interact to regulate pain. Proc. Natl. Acad. Sci. USA. 2018;115:E1657–E1666. doi: 10.1073/pnas.1715972115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roohbakhsh A., Shamsizadeh A. Neuropathology of Drug Addictions and Substance Misuse. Volume 3. Elsevier Inc.; Amsterdam, The Netherlands: 2016. Opioids and TRPV1 Receptors; pp. 433–442. [Google Scholar]
- 49.Kanezaki M., Ebihara S., Gui P., Ebihara T., Kohzuki M. Effect of cigarette smoking on cough reflex induced by TRPV1 and TRPA1 stimulations. Respir. Med. 2012;106:406–412. doi: 10.1016/j.rmed.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 50.Caires R., Luis E., Taberner F.J., Fernandez-Ballester G., Ferrer-Montiel A., Balazs E.A., Gomis A., Belmonte C., De La Peña E. Hyaluronan modulates TRPV1 channel opening, reducing peripheral nociceptor activity and pain. Nat. Commun. 2015;6:8095. doi: 10.1038/ncomms9095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Van Buren J.J., Bhat S., Rotello R., Pauza M.E., Premkumar L.S. Sensitization and translocation of TRPVI by insulin and IGF-I. Mol. Pain. 2005;1:17. doi: 10.1186/1744-8069-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Witte D.G., Cassar S.C., Masters J.N., Esbenshade T., Hancock A.A. Use of a fluorescent imaging plate reader-based calcium assay to assess pharmacological differences between the human and rat vanilloid receptor. J. Biomol. Screen. 2002;7:466–475. doi: 10.1177/108705702237679. [DOI] [PubMed] [Google Scholar]
- 53.Hoffmann J., Supronsinchai W., Andreou A.P., Summ O., Akerman S., Goadsby P.J. Olvanil acts on transient receptor potential vanilloid channel 1 and cannabinoid receptors to modulate neuronal transmission in the trigeminovascular system. Pain. 2012;153:2226–2232. doi: 10.1016/j.pain.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 54.Maurer K., Binzen U., Mörz H., Bugert P., Schedel A., Treede R.D., Greffrath W. Acetylsalicylic acid enhances tachyphylaxis of repetitive capsaicin responses in TRPV1-GFP expressing HEK293 cells. Neurosci. Lett. 2014;563:101–106. doi: 10.1016/j.neulet.2014.01.050. [DOI] [PubMed] [Google Scholar]
- 55.Park C.K., Kim K., Jung S.J., Kim M.J., Ahn D.K., Hong S.D., Kim J.S., Oh S.B. Molecular mechanism for local anesthetic action of eugenol in the rat trigeminal system. Pain. 2009;144:84–94. doi: 10.1016/j.pain.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 56.André E., Campi B., Trevisani M., Ferreira J., Malheiros Â., Yunes R.A., Calixto J.B., Geppetti P. Pharmacological characterisation of the plant sesquiterpenes polygodial and drimanial as vanilloid receptor agonists. Biochem. Pharmacol. 2006;71:1248–1254. doi: 10.1016/j.bcp.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 57.Kalsi M., Walter A., Lee B., DeLaat A., Trigueros R.R., Happel K., Sepesy R., Nguyen B., Manwill P.K., Rakotondraibe L.H., et al. Stop the crop: Insights into the insecticidal mode of action of cinnamodial against mosquitoes. Pestic. Biochem. Physiol. 2021;171:104743. doi: 10.1016/j.pestbp.2020.104743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bessac B.F., Jordt S.E. Breathtaking TRP channels: TRPA1 and TRPV1 in airway chemosensation and reflex control. Physiology. 2008;23:360–370. doi: 10.1152/physiol.00026.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Starkus J., Jansen C., Shimoda L.M.N., Stokes A.J., Small-Howard A.L., Turner H. Diverse TRPV1 responses to cannabinoids. Channels. 2019;13:172–191. doi: 10.1080/19336950.2019.1619436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vriens J., Nilius B., Vennekens R. Herbal Compounds and Toxins Modulating TRP Channels. Curr. Neuropharmacol. 2008;6:79–96. doi: 10.2174/157015908783769644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim Y.S., Hong C., Lee S.W., Nam J.H., Kim B.J. Effects of ginger and its pungent constituents on transient receptor potential channels. Int. J. Mol. Med. 2016;38:1905–1914. doi: 10.3892/ijmm.2016.2791. [DOI] [PubMed] [Google Scholar]
- 62.Phillips E., Reeve A., Bevan S., McIntyre P. Identification of Species-specific Determinants of the Action of the Antagonist Capsazepine and the Agonist PPAHV on TRPV1. J. Biol. Chem. 2004;279:17165–17172. doi: 10.1074/jbc.M313328200. [DOI] [PubMed] [Google Scholar]
- 63.Geng S., Zheng Y., Meng M., Guo Z., Cao N., Ma X., Du Z., Li J., Duan Y., Du G. Gingerol Reverses the Cancer-Promoting Effect of Capsaicin by Increased TRPV1 Level in a Urethane-Induced Lung Carcinogenic Model. J. Agric. Food Chem. 2016;64:6203–6211. doi: 10.1021/acs.jafc.6b02480. [DOI] [PubMed] [Google Scholar]
- 64.Gavva N.R., Tamir R., Klionsky L., Norman M.H., Louis J.C., Wild K.D., Treanor J.J.S. Proton activation does not alter antagonist interaction with the capsaicin-binding pocket of TRPV1. Mol. Pharmacol. 2005;68:1524–1533. doi: 10.1124/mol.105.015727. [DOI] [PubMed] [Google Scholar]
- 65.Garami A., Pakai E., McDonald H.A., Reilly R.M., Gomtsyan A., Corrigan J.J., Pinter E., Zhu D.X.D., Lehto S.G., Gavva N.R., et al. TRPV1 antagonists that cause hypothermia, instead of hyperthermia, in rodents: Compounds’ pharmacological profiles, in vivo targets, thermoeffectors recruited and implications for drug development. Acta Physiol. 2018;223:e13038. doi: 10.1111/apha.13038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kym P.R., Kort M.E., Hutchins C.W. Analgesic potential of TRPV1 antagonists. Biochem. Pharmacol. 2009;78:211–216. doi: 10.1016/j.bcp.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 67.Brederson J.D., Kym P.R., Szallasi A. Targeting TRP channels for pain relief. Eur. J. Pharmacol. 2013;716:61–76. doi: 10.1016/j.ejphar.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 68.Bohlen C.J., Priel A., Zhou S., King D., Siemens J., Julius D. A bivalent tarantula toxin activates the capsaicin receptor, TRPV1, by targeting the outer pore domain. Cell. 2010;141:834–845. doi: 10.1016/j.cell.2010.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hamers A.J.P., Ahluwalia A. Arachidonic acid metabolites induce TRPV1-mediated inflammation. FASEB J. 2017;31 doi: 10.1096/FASEBJ.31.1_SUPPLEMENT.825.5. [DOI] [Google Scholar]
- 70.Nersesyan Y., Demirkhanyan L., Cabezas-Bratesco D., Oakes V., Kusuda R., Dawson T., Sun X., Cao C., Cohen A.M., Chelluboina B., et al. Oxytocin Modulates Nociception as an Agonist of Pain-Sensing TRPV1. Cell Rep. 2017;21:1681–1691. doi: 10.1016/j.celrep.2017.10.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Puntambekar P., Van Buren J., Raisinghani M., Premkumar L.S., Ramkumar V. Direct Interaction of Adenosine with the TRPV1 Channel Protein. J. Neurosci. 2004;24:3663–3671. doi: 10.1523/JNEUROSCI.4773-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhao J.F., Shyue S.K., Lee T.S. Excess nitric oxide activates TRPV1-Ca2+-calpain signaling and promotes PEST-dependent degradation of liver X receptor α. Int. J. Biol. Sci. 2016;12:18–29. doi: 10.7150/ijbs.13549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Koroleva K., Mustafina A., Yakovlev A., Hermann A., Giniatullin R., Sitdikova G. Receptor Mechanisms Mediating the Pro-Nociceptive Action of Hydrogen Sulfide in Rat Trigeminal Neurons and Meningeal Afferents. Front. Cell. Neurosci. 2017;11:226. doi: 10.3389/fncel.2017.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nieto-Posadas A., Picazo-Juárez G., Llorente I., Jara-Oseguera A., Morales-Lázaro S., Escalante-Alcalde D., Islas L.D., Rosenbaum T. Lysophosphatidic acid directly activates TRPV1 through a C-terminal binding site. Nat. Chem. Biol. 2012;8:78–85. doi: 10.1038/nchembio.712. [DOI] [PubMed] [Google Scholar]
- 75.Woo D.H., Jung S.J., Zhu M.H., Park C.K., Kim Y.H., Oh S.B., Lee C.J. Direct activation of Transient Receptor Potential Vanilloid 1(TRPV1) by Diacylglycerol (DAG) Mol. Pain. 2008;4 doi: 10.1186/1744-8069-4-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dhaka A., Uzzell V., Dubin A.E., Mathur J., Petrus M., Bandell M., Patapoutian A. TRPV1 is activated by both acidic and basic pH. J. Neurosci. 2009;29:153–158. doi: 10.1523/JNEUROSCI.4901-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bianchi B.R., Lee C.H., Jarvis M.F., El Kouhen R., Moreland R.B., Faltynek C.R., Puttfarcken P.S. Modulation of human TRPV1 receptor activity by extracellular protons and host cell expression system. Eur. J. Pharmacol. 2006;537:20–30. doi: 10.1016/j.ejphar.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 78.Long W., Fatehi M., Soni S., Panigrahi R., Philippaert K., Yu Y., Kelly R., Boonen B., Barr A., Golec D., et al. Vitamin D is an endogenous partial agonist of the transient receptor potential vanilloid 1 channel. J. Physiol. 2020;598:4321–4338. doi: 10.1113/JP279961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Connor M., Vaughan C.W., Vandenberg R.J. N-Acyl amino acids and N-acyl neurotransmitter conjugates: Neuromodulators and probes for new drug targets. Br. J. Pharmacol. 2010;160:1857–1871. doi: 10.1111/j.1476-5381.2010.00862.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ma Y., Deng Q., Li S., Chen M., Jin B., Wang M. TRPV1, Targeted by miR-338-3p, Induces Neuropathic Pain by Interacting with NECAB2. J. Mol. Neurosci. 2021;71:55–65. doi: 10.1007/s12031-020-01626-4. [DOI] [PubMed] [Google Scholar]
- 81.Zhang J., Zhou Z., Zhang N., Jin W., Ren Y., Chen C. Establishment of preliminary regulatory network of TRPV1 and related cytokines. Saudi J. Biol. Sci. 2017;24:582–588. doi: 10.1016/j.sjbs.2017.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Raboune S., Stuart J.M., Leishman E., Takacs S.M., Rhodes B., Basnet A., Jameyfield E., McHugh D., Widlanski T., Bradshaw H.B. Novel endogenous N-acyl amides activate TRPV1-4 receptors, BV-2 microglia, and are regulated in brain in an acute model of inflammation. Front. Cell. Neurosci. 2014;8 doi: 10.3389/fncel.2014.00195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hanack C., Moroni M., Lima W.C., Wende H., Kirchner M., Adelfinger L., Schrenk-Siemens K., Tappe-Theodor A., Wetzel C., Kuich P.H., et al. GABA blocks pathological but not acute TRPV1 pain signals. Cell. 2015;160:759–770. doi: 10.1016/j.cell.2015.01.022. [DOI] [PubMed] [Google Scholar]
- 84.Gonzalez-Hernandez A., Charlet A. Oxytocin, GABA, and TRPV1, the Analgesic Triad? Front. Mol. Neurosci. 2018;11:398. doi: 10.3389/fnmol.2018.00398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Movahed P., Jönsson B.A.G., Birnir B., Wingstrand J.A., Jørgensen T.D., Ermund A., Sterner O., Zygmunt P.M., Högestätt E.D. Endogenous unsaturated C18 N-acylethanolamines are vanilloid receptor (TRPV1) agonists. J. Biol. Chem. 2005;280:38496–38504. doi: 10.1074/jbc.M507429200. [DOI] [PubMed] [Google Scholar]
- 86.Van der Stelt M., Trevisani M., Vellani V., De Petrocellis L., Schiano Moriello A., Campi B., McNaughton P., Geppetti P., Di Marzo V. Anandamide acts as an intracellular messenger amplifying Ca2+ influx via TRPV1 channels. EMBO J. 2005;24:3026–3037. doi: 10.1038/sj.emboj.7600784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ahern G.P. Activation of TRPV1 by the satiety factor oleoylethanolamide. J. Biol. Chem. 2003;278:30429–30434. doi: 10.1074/jbc.M305051200. [DOI] [PubMed] [Google Scholar]
- 88.Karwad M.A., Macpherson T., Wang B., Theophilidou E., Sarmad S., Barrett D.A., Larvin M., Wright K.L., Lund J.N., O’Sullivan S.E. Oleoylethanolamine and palmitoylethanolamine modulate intestinal permeability in vitro via TRPV1 and PPARα. FASEB J. 2017;31:469–481. doi: 10.1096/fj.201500132. [DOI] [PubMed] [Google Scholar]
- 89.Morales-Lázaro S.L., Llorente I., Sierra-Ramírez F., López-Romero A.E., Ortíz-Rentería M., Serrano-Flores B., Simon S.A., Islas L.D., Rosenbaum T. Inhibition of TRPV1 channels by a naturally occurring omega-9 fatty acid reduces pain and itch. Nat. Commun. 2016;7:13092. doi: 10.1038/ncomms13092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Duarte Y., Cáceres J., Sepúlveda R.V., Arriagada D., Olivares P., Díaz-Franulic I., Stehberg J., González-Nilo F. Novel TRPV1 Channel Agonists With Faster and More Potent Analgesic Properties Than Capsaicin. Front. Pharmacol. 2020;11:1040. doi: 10.3389/fphar.2020.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hanson S.M., Newstead S., Swartz K.J., Sansom M.S.P. Capsaicin interaction with TRPV1 channels in a lipid bilayer: Molecular dynamics simulation. Biophys. J. 2015;108:1425–1434. doi: 10.1016/j.bpj.2015.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jung J., Hwang S.W., Kwak J., Lee S.Y., Kang C.J., Kim W.B., Kim D., Oh U. Capsaicin binds to the intracellular domain of the capsaicin-activated ion channel. J. Neurosci. 1999;19:529–538. doi: 10.1523/JNEUROSCI.19-02-00529.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chu Y., Cohen B.E., Chuang H.H. A single TRPV1 amino acid controls species sensitivity to capsaicin. Sci. Rep. 2020;10:1–12. doi: 10.1038/s41598-020-64584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kasimova M.A., Yazici A.T., Yudin Y., Granata D., Klein M.L., Rohacs T., Carnevale V. A hypothetical molecular mechanism for TRPV1 activation that invokes rotation of an S6 asparagine. J. Gen. Physiol. 2018;150:1554–1566. doi: 10.1085/jgp.201812124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rosenbaum T., Simon S.A. TRPV1 Receptors and Signal Transduction. CRC Press; Boca Raton, FL, USA: Taylor & Francis; Abingdon, UK: 2007. [PubMed] [Google Scholar]
- 96.Botto L., Bernabò N., Palestini P., Barboni B. Bicarbonate Induces Membrane Reorganization and CBR1 and TRPV1 Endocannabinoid Receptor Migration in Lipid Microdomains in Capacitating Boar Spermatozoa. J. Membr. Biol. 2010;238:33–41. doi: 10.1007/s00232-010-9316-8. [DOI] [PubMed] [Google Scholar]
- 97.Majhi R.K., Kumar A., Yadav M., Swain N., Kumari S., Saha A., Pradhan A., Goswami L., Saha S., Samanta L., et al. Thermosensitive ion channel TRPV1 is endogenously expressed in the sperm of a fresh water teleost fish (Labeo rohita) and regulates sperm motility. Channels. 2013;7 doi: 10.4161/chan.25793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gervasi M.G., Osycka-Salut C., Caballero J., Vazquez-Levin M., Pereyra E., Billi S., Franchi A., Perez-Martinez S. Anandamide capacitates bull spermatozoa through CB1 and TRPV1 activation. PLoS ONE. 2011;6:e16993. doi: 10.1371/journal.pone.0016993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Francavilla F., Battista N., Barbonetti A., Vassallo M.R.C., Rapino C., Antonangelo C., Pasquariello N., Catanzaro G., Barboni B., Maccarrone M. Characterization of the endocannabinoid system in human spermatozoa and involvement of transient receptor potential vanilloid 1 receptor in their fertilizing ability. Endocrinology. 2009;150:4692–4700. doi: 10.1210/en.2009-0057. [DOI] [PubMed] [Google Scholar]
- 100.Li S., Wang X., Ye H., Gao W., Pu X., Yang Z. Distribution profiles of transient receptor potential melastatin-and vanilloid-related channels in rat spermatogenic cells and sperm. Mol. Biol. Rep. 2010;37:1287–1293. doi: 10.1007/s11033-009-9503-9. [DOI] [PubMed] [Google Scholar]
- 101.Kumar A., Majhi R.K., Swain N., Giri S.C., Kar S., Samanta L., Goswami C. TRPV4 is endogenously expressed in vertebrate spermatozoa and regulates intracellular calcium in human sperm. Biochem. Biophys. Res. Commun. 2016;473:781–788. doi: 10.1016/j.bbrc.2016.03.071. [DOI] [PubMed] [Google Scholar]
- 102.Grimaldi P., Orlando P., Di Siena S., Lolicato F., Petrosino S., Bisogno T., Geremia R., De Petrocellis L., Di Marzo V. The endocannabinoid system and pivotal role of the CB2 receptor in mouse spermatogenesis. Proc. Natl. Acad. Sci. USA. 2009;106:11131–11136. doi: 10.1073/pnas.0812789106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lamy J., Liere P., Pianos A., Aprahamian F., Mermillod P., Saint-Dizier M. Steroid hormones in bovine oviductal fluid during the estrous cycle. Theriogenology. 2016;86:1409–1420. doi: 10.1016/j.theriogenology.2016.04.086. [DOI] [PubMed] [Google Scholar]
- 104.Ballester L., Romero-Aguirregomezcorta J., Soriano-Úbeda C., Matás C., Romar R., Coy P. Timing of oviductal fluid collection, steroid concentrations, and sperm preservation method affect porcine in vitro fertilization efficiency. Fertil. Steril. 2014;102:1762–1768. doi: 10.1016/j.fertnstert.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 105.Saint-Dizier M., Schoen J., Chen S., Banliat C., Mermillod P. Composing the early embryonic microenvironment: Physiology and regulation of oviductal secretions. Int. J. Mol. Sci. 2020;21:223. doi: 10.3390/ijms21010223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gervasi M.G., Marczylo T.H., Lam P.M., Rana S., Franchi A.M., Konje J.C., Perez-Martinez S. Anandamide Levels Fluctuate in the Bovine Oviduct during the Oestrous Cycle. PLoS ONE. 2013;8:e72521. doi: 10.1371/journal.pone.0072521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lewis S.E.M., Rapino C., Di Tommaso M., Pucci M., Battista N., Paro R., Simon L., Lutton D., Maccarrone M. Differences in the Endocannabinoid System of Sperm from Fertile and Infertile Men. PLoS ONE. 2012;7:e47704. doi: 10.1371/journal.pone.0047704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Catanzaro G., Battista N., Rossi G., Di Tommaso M., Pucci M., Pirazzi V., Cecconi S., Maccarrone M. Effect of capacitation on the endocannabinoid system of mouse sperm. Mol. Cell. Endocrinol. 2011;343:88–92. doi: 10.1016/j.mce.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 109.Safarinejad M.R., Hosseini S.Y., Dadkhah F., Asgari M.A. Relationship of omega-3 and omega-6 fatty acids with semen characteristics, and anti-oxidant status of seminal plasma: A comparison between fertile and infertile men. Clin. Nutr. 2010;29:100–105. doi: 10.1016/j.clnu.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 110.Collodel G., Castellini C., Lee J.C.Y., Signorini C. Relevance of Fatty Acids to Sperm Maturation and Quality. Oxid. Med. Cell. Longev. 2020;2020 doi: 10.1155/2020/7038124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Allen M.R., Zhang B.R., Hettinger A.M., Goad D.W., Malayer J.R., Geisert R.D. Detection of bradykinin and bradykinin-β2 receptors in the porcine endometrium during the estrous cycle and early pregnancy. Biol. Reprod. 2002;66:574–579. doi: 10.1095/biolreprod66.3.574. [DOI] [PubMed] [Google Scholar]
- 112.Martínez-Soto J.C., Landeras J., Gadea J. Spermatozoa and seminal plasma fatty acids as predictors of cryopreservation success. Andrology. 2013;1:365–375. doi: 10.1111/j.2047-2927.2012.00040.x. [DOI] [PubMed] [Google Scholar]
- 113.Li S., Winuthayanon W. Oviduct: Roles in fertilization and early embryo development. J. Endocrinol. 2017;232:R1–R26. doi: 10.1530/JOE-16-0302. [DOI] [PubMed] [Google Scholar]
- 114.Ning N., Zhu J., Du Y., Gao X., Liu C., Li J. Dysregulation of hydrogen sulphide metabolism impairs oviductal transport of embryos. Nat. Commun. 2014;5:1–8. doi: 10.1038/ncomms5107. [DOI] [PubMed] [Google Scholar]
- 115.Kadlec M., Ros-Santaella J.L., Pintus E. The roles of no and h2s in sperm biology: Recent advances and new perspectives. Int. J. Mol. Sci. 2020;21:2174. doi: 10.3390/ijms21062174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rodriguez-Martinez H., Tienthai P., Atikuzzaman M., Vicente-Carrillo A., Rubér M., Alvarez-Rodriguez M. The ubiquitous hyaluronan: Functionally implicated in the oviduct? Theriogenology. 2016;86:182–186. doi: 10.1016/j.theriogenology.2015.11.025. [DOI] [PubMed] [Google Scholar]
- 117.Fouladi-Nashta A.A., Raheem K.A., Marei W.F., Ghafari F., Hartshorne G.M. Regulation and roles of the hyaluronan system in mammalian reproduction. Reproduction. 2017;153:R43–R58. doi: 10.1530/REP-16-0240. [DOI] [PubMed] [Google Scholar]
- 118.Leisegang K., Bouic P.J.D., Menkveld R., Henkel R.R. Obesity is associated with increased seminal insulin and leptin alongside reduced fertility parameters in a controlled male cohort. Reprod. Biol. Endocrinol. 2014;12 doi: 10.1186/1477-7827-12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Korzekwa A.J., Bah M.M., Kurzynowski A., Lukasik K., Groblewska A., Skarzynski D.J. Leukotrienes modulate secretion of progesterone and prostaglandins during the estrous cycle and early pregnancy in cattle: An in vivo study. Reproduction. 2010;140:767–776. doi: 10.1530/REP-10-0202. [DOI] [PubMed] [Google Scholar]
- 120.De Mateo S., Sassone-Corsi P. Regulation of spermatogenesis by small non-coding RNAs: Role of the germ granule. Semin. Cell Dev. Biol. 2014;29:84–92. doi: 10.1016/j.semcdb.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fereshteh Z., Schmidt S.A., Al-Dossary A.A., Accerbi M., Arighi C., Cowart J., Song J.L., Green P.J., Choi K., Yoo S., et al. Murine Oviductosomes (OVS) microRNA profiling during the estrous cycle: Delivery of OVS-borne microRNAs to sperm where miR-34c-5p localizes at the centrosome. Sci. Rep. 2018;8:16094. doi: 10.1038/s41598-018-34409-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Almiñana C., Tsikis G., Labas V., Uzbekov R., da Silveira J.C., Bauersachs S., Mermillod P. Deciphering the oviductal extracellular vesicles content across the estrous cycle: Implications for the gametes-oviduct interactions and the environment of the potential embryo. BMC Genom. 2018;19 doi: 10.1186/s12864-018-4982-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Engel K.M., Baumann S., Rolle-Kampczyk U., Schiller J., von Bergen M., Grunewald S. Metabolomic profiling reveals correlations between spermiogram parameters and the metabolites present in human spermatozoa and seminal plasma. PLoS ONE. 2019;14:e0211679. doi: 10.1371/journal.pone.0211679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Castellini C., Mattioli S., Dal Bosco A., Collodel G., Pistilli A., Stabile A.M., MacChioni L., Mancuso F., Luca G., Rende M. In vitro effect of nerve growth factor on the main traits of rabbit sperm. Reprod. Biol. Endocrinol. 2019;17 doi: 10.1186/s12958-019-0533-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Tribulo P., Bogle O., Mapletoft R.J., Adams G.P. Bioactivity of ovulation inducing factor (or nerve growth factor) in bovine seminal plasma and its effects on ovarian function in cattle. Theriogenology. 2015;83:1394–1401. doi: 10.1016/j.theriogenology.2014.12.014. [DOI] [PubMed] [Google Scholar]
- 126.Kobayashi Y., Yamamoto Y., Kageyama S., Hirayama H., Kimura K., Okuda K. Regulation of bovine oviductal NO synthesis by follicular steroids and prostaglandins. Reproduction. 2016;151:577–587. doi: 10.1530/REP-15-0254. [DOI] [PubMed] [Google Scholar]
- 127.Agirregoitia E., Valdivia A., Carracedo A., Casis L., Gil J., Subiran N., Ochoa C., Irazusta J. Expression and Localization of δ-, κ-, and μ-Opioid Receptors in Human Spermatozoa and Implications for Sperm Motility. J. Clin. Endocrinol. Metab. 2006;91:4969–4975. doi: 10.1210/jc.2006-0599. [DOI] [PubMed] [Google Scholar]
- 128.Mostafa T., Rashed L.A., Osman I., Marawan M. Seminal plasma oxytocin and oxidative stress levels in infertile men with varicocele. Andrologia. 2015;47:209–213. doi: 10.1111/and.12248. [DOI] [PubMed] [Google Scholar]
- 129.Ng K.Y.B., Mingels R., Morgan H., Macklon N., Cheong Y. In vivo oxygen, temperature and pH dynamics in the female reproductive tract and their importance in human conception: A systematic review. Hum. Reprod. Update. 2018;24:15–34. doi: 10.1093/humupd/dmx028. [DOI] [PubMed] [Google Scholar]
- 130.Firouzabadi R.D., Rahmani E., Rahsepar M., Firouzabadi M.M. Value of follicular fluid vitamin D in predicting the pregnancy rate in an IVF program. Arch. Gynecol. Obstet. 2014;289:201–206. doi: 10.1007/s00404-013-2959-9. [DOI] [PubMed] [Google Scholar]
- 131.Anifandis G.M., Dafopoulos K., Messini C.I., Chalvatzas N., Liakos N., Pournaras S., Messinis I.E. Prognostic value of follicular fluid 25-OH vitamin D and glucose levels in the IVF outcome. Reprod. Biol. Endocrinol. 2010;8 doi: 10.1186/1477-7827-8-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Jueraitetibaike K., Ding Z., Wang D.D., Peng L.P., Jing J., Chen L., Ge X., Qiu X.H., Yao B. The effect of Vitamin D on sperm motility and the underlying mechanism. Asian J. Androl. 2019;21:400–407. doi: 10.4103/aja.aja_105_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Shukla K.K., Mahdi A.A., Rajender S. Ion Channels in Sperm Physiology and Male Fertility and Infertility. J. Androl. 2012;33:777–788. doi: 10.2164/jandrol.111.015552. [DOI] [PubMed] [Google Scholar]
- 134.Gadella B.M. Reproductive tract modifications of the boar sperm surface. Mol. Reprod. Dev. 2017;84:822–831. doi: 10.1002/mrd.22821. [DOI] [PubMed] [Google Scholar]
- 135.Suarez S.S. The Oviductal Sperm Reservoir in Mammals: Mechanisms of Formation. Biol. Reprod. 1998;58:1105–1107. doi: 10.1095/biolreprod58.5.1105. [DOI] [PubMed] [Google Scholar]
- 136.Georgadaki K., Khoury N., Spandidos D.A., Zoumpourlis V. The molecular basis of fertilization (Review) Int. J. Mol. Med. 2016;38:979–986. doi: 10.3892/ijmm.2016.2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Suarez S.S., Pacey A.A. Sperm transport in the female reproductive tract. Hum. Reprod. Update. 2006;12:23–37. doi: 10.1093/humupd/dmi047. [DOI] [PubMed] [Google Scholar]
- 138.Miller D.J. Review: The epic journey of sperm through the female reproductive tract. Animal. 2018;12:s110–s120. doi: 10.1017/S1751731118000526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Miki K., Clapham D.E. Rheotaxis guides mammalian sperm. Curr. Biol. 2013;23:443–452. doi: 10.1016/j.cub.2013.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hino T., Yanagimachi R. Active peristaltic movements and fluid production of the mouse oviduct: Their roles in fluid and sperm transport and fertilization. Biol. Reprod. 2019;101:240–249. doi: 10.1093/biolre/ioz061. [DOI] [PubMed] [Google Scholar]
- 141.Eisenbach M., Giojalas L.C. Sperm guidance in mammals—An unpaved road to the egg. Nat. Rev. Mol. Cell Biol. 2006;7:276–285. doi: 10.1038/nrm1893. [DOI] [PubMed] [Google Scholar]
- 142.Caterina M.J., Park U. Chapter 4 TRPV1: A Polymodal Sensor in the Nociceptor Terminal. Curr. Top. Membr. 2006;57:113–150. [Google Scholar]
- 143.Teves M.E., Barbano F., Guidobaldi H.A., Sanchez R., Miska W., Giojalas L.C. Progesterone at the picomolar range is a chemoattractant for mammalian spermatozoa. Fertil. Steril. 2006;86:745–749. doi: 10.1016/j.fertnstert.2006.02.080. [DOI] [PubMed] [Google Scholar]
- 144.Oren-Benaroya R., Orvieto R., Gakamsky A., Pinchasov M., Eisenbach M. The sperm chemoattractant secreted from human cumulus cells is progesterone. Hum. Reprod. 2008;23:2339–2345. doi: 10.1093/humrep/den265. [DOI] [PubMed] [Google Scholar]
- 145.Eisenbach M. Mammalian sperm chemotaxis and its association with capacitation. Dev. Genet. 1999;25:87–94. doi: 10.1002/(SICI)1520-6408(1999)25:2<87::AID-DVG2>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 146.Berendsen J.T.W., Kruit S.A., Atak N., Willink E., Segerink L.I. Flow-Free Microfluidic Device for Quantifying Chemotaxis in Spermatozoa. Anal. Chem. 2020;92:3302–3306. doi: 10.1021/acs.analchem.9b05183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Dominguez E.M., Moreno-Irusta A., Bragulat A.F., Castex H.R., Losinno L., Giojalas L.C. Equine Spermatozoa at Optimum Physiological State Are Selected by Chemotaxis Toward Progesterone. J. Equine Vet. Sci. 2018;66:21. doi: 10.1016/j.jevs.2018.05.003. [DOI] [Google Scholar]
- 148.Sun F., Bahat A., Gakamsky A., Girsh E., Katz N., Giojalas L.C., Tur-Kaspa I., Eisenbach M. Human sperm chemotaxis: Both the oocyte and its surrounding cumulus cells secrete sperm chemoattractants. Hum. Reprod. 2005;20:761–767. doi: 10.1093/humrep/deh657. [DOI] [PubMed] [Google Scholar]
- 149.Guidobaldi H.A., Teves M.E., Uñates D.R., Anastasía A., Giojalas L.C. Progesterone from the cumulus cells is the sperm chemoattractant secreted by the rabbit oocyte cumulus complex. PLoS ONE. 2008;3:e3040. doi: 10.1371/journal.pone.0003040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Guidobaldi H.A., Hirohashi N., Cubilla M., Buffone M.G., Giojalas L.C. An intact acrosome is required for the chemotactic response to progesterone in mouse spermatozoa. Mol. Reprod. Dev. 2017;84:310–315. doi: 10.1002/mrd.22782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lishko P.V., Botchkina I.L., Kirichok Y. Progesterone activates the principal Ca2+ channel of human sperm. Nature. 2011;471:387–391. doi: 10.1038/nature09767. [DOI] [PubMed] [Google Scholar]
- 152.Kaupp U.B., Solzin J., Hildebrand E., Brown J.E., Helbig A., Hagen V., Beyermann M., Pampaloni F., Weyand I. The signal flow and motor response controling chemotaxis of sea urchin sperm. Nat. Cell Biol. 2003;5:109–117. doi: 10.1038/ncb915. [DOI] [PubMed] [Google Scholar]
- 153.Yoshida M., Murata M., Inaba K., Morisawa M. A chemoattractant for ascidian spermatozoa is a sulfated steroid. Proc. Natl. Acad. Sci. USA. 2002;99:14831–14836. doi: 10.1073/pnas.242470599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Levitan I., Christian A.E., Tulenko T.N., Rothblat G.H. Membrane cholesterol content modulates activation of volume-regulated anion current in bovine endothelial cells. J. Gen. Physiol. 2000;115:405–416. doi: 10.1085/jgp.115.4.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Levitan I., Fang Y., Rosenhouse-Dantsker A., Romanenko V. Cholesterol and ion channels. Subcell. Biochem. 2010;51:509–549. doi: 10.1007/978-90-481-8622-8_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Picazo-Juárez G., Romero-Suárez S., Nieto-Posadas A.S., Llorente I., Jara-Oseguera A.S., Briggs M., McIntosh T.J., Simon S.A., Ladrón-de-Guevara E., Islas L.D., et al. Identification of a binding motif in the S5 helix that confers cholesterol sensitivity to the TRPV1 ion channel. J. Biol. Chem. 2011;286:24966–24976. doi: 10.1074/jbc.M111.237537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Liu M., Huang W., Wu D., Priestley J.V. TRPV1, but not P2X3, requires cholesterol for its function and membrane expression in rat nociceptors. Eur. J. Neurosci. 2006;24:1–6. doi: 10.1111/j.1460-9568.2006.04889.x. [DOI] [PubMed] [Google Scholar]
- 158.Storti B., Di Rienzo C., Cardarelli F., Bizzarri R., Beltram F. Unveiling TRPV1 Spatio-Temporal Organization in Live Cell Membranes. PLoS ONE. 2015;10:e0116900. doi: 10.1371/journal.pone.0116900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Bernabò N., Pistilli M.G., Mattioli M., Barboni B. Role of TRPV1 channels in boar spermatozoa acquisition of fertilizing ability. Mol. Cell. Endocrinol. 2010;323:224–231. doi: 10.1016/j.mce.2010.02.025. [DOI] [PubMed] [Google Scholar]
- 160.Schmid P.C., Paria B.C., Krebsbach R.J., Schmid H.H.O., Dey S.K. Changes in anandamide levels in mouse uterus are associated with uterine receptivity for embryo implantation. Proc. Natl. Acad. Sci. USA. 1997;94:4188–4192. doi: 10.1073/pnas.94.8.4188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Das S.K., Paria B.C., Chakraborty I., Dey S.K. Cannabinoid ligand-receptor signaling in the mouse uterus. Proc. Natl. Acad. Sci. USA. 1995;92:4332–4336. doi: 10.1073/pnas.92.10.4332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Gentilini D., Besana A., Vigano P., Dalino P., Vignali M., Melandri M., Busacca M., Di Blasio A.M. Endocannabinoid system regulates migration of endometrial stromal cells via cannabinoid receptor 1 through the activation of PI3K and ERK1/2 pathways. Fertil. Steril. 2010;93:2588–2593. doi: 10.1016/j.fertnstert.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 163.Flesch F.M., Gadella B.M. Dynamics of the mammalian sperm plasma membrane in the process of fertilization. Biochim. Biophys. Acta -Rev. Biomembr. 2000;1469:197–235. doi: 10.1016/S0304-4157(00)00018-6. [DOI] [PubMed] [Google Scholar]
- 164.Leahy T., Gadella B.M. New insights into the regulation of cholesterol efflux from the sperm membrane. Asian J. Androl. 2015;17:561–567. doi: 10.4103/1008-682X.153309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Schuel H., Burkman L.J., Lippes J., Crickard K., Forester E., Piomelli D., Giuffrida A. N-Acylethanolamines in human reproductive fluids. Chem. Phys. Lipids. 2002;121:211–227. doi: 10.1016/S0009-3084(02)00158-5. [DOI] [PubMed] [Google Scholar]
- 166.Bernabò N., Palestini P., Chiarini M., Maccarrone M., Mattioli M., Barboni B. Endocannabinoid-binding CB1 and TRPV1 receptors as modulators of sperm capacitation. Commun. Integr. Biol. 2012;5:68–70. doi: 10.4161/cib.18118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Bernabò N., Berardinelli P., Mauro A., Russo V., Lucidi P., Mattioli M., Barboni B., Knoll A., Javaux E., Hewitt D., et al. The role of actin in capacitation-related signaling: An in silico and in vitro study. BMC Syst. Biol. 2011;5:47. doi: 10.1186/1752-0509-5-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Gervasi M.G., Osycka-Salut C., Sanchez T., Alonso C.A.I., Llados C., Castellano L., Franchi A.M., Villalõn M., Perez-Martinez S. Sperm Release from the Oviductal Epithelium Depends on Ca2+ Influx Upon Activation of CB1 and TRPV1 by Anandamide. J. Cell. Biochem. 2016;117:320–333. doi: 10.1002/jcb.25273. [DOI] [PubMed] [Google Scholar]
- 169.Guerrero A., Nishigaki T., Carneiro J., Tatsu Y., Wood C.D., Darszon A. Tuning sperm chemotaxis by calcium burst timing. Dev. Biol. 2010;344:52–65. doi: 10.1016/j.ydbio.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 170.MicroRNA Signature Targeting Transient Receptor Potential Channels in the Prognosis and Therapy of Cancer. J. Cell. Immunol. 2020;2 doi: 10.33696/immunology.2.023. [DOI] [Google Scholar]
- 171.Zhuang X., Li Z., Lin H., Gu L., Lin Q., Lu Z., Tzeng C.M. Integrated miRNA and mRNA expression profiling to identify mRNA targets of dysregulated miRNAs in non-obstructive azoospermia. Sci. Rep. 2015;5:7922. doi: 10.1038/srep07922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Heidary Z., Zaki-Dizaji M., Saliminejad K., Khorram Khorshid H.R. MicroRNA profiling in spermatozoa of men with unexplained asthenozoospermia. Andrologia. 2019;51:e13284. doi: 10.1111/and.13284. [DOI] [PubMed] [Google Scholar]
- 173.Khawar M.B., Mehmood R., Roohi N. Micrornas: Recent insights towards their role in male infertility and reproductive cancers. Bosn. J. Basic Med. Sci. 2019;19:31–42. doi: 10.17305/bjbms.2018.3477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Eisenbach M. Sperm chemotaxis. Rev. Reprod. 1999;4:56–66. doi: 10.1530/ror.0.0040056. [DOI] [PubMed] [Google Scholar]
- 175.David A., Vilensky A., Nathan H. Temperature Changes in the Different Parts of the Rabbit’s Oviduct. Int. J. Gynecol. Obstet. 1972;10:52–56. doi: 10.1002/j.1879-3479.1972.tb00818.x. [DOI] [Google Scholar]
- 176.Hunter R.H.F., Nichol R. A preovulatory temperature gradient between the isthmus and ampulla of pig oviducts during the phase of sperm storage. J. Reprod. Fertil. 1986;77:599–606. doi: 10.1530/jrf.0.0770599. [DOI] [PubMed] [Google Scholar]
- 177.Bahat A., Caplan S.R., Eisenbach M. Thermotaxis of human sperm cells in extraordinarily shallow temperature gradients over a wide range. PLoS ONE. 2012;7:e41915. doi: 10.1371/journal.pone.0041915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Brauchi S., Orta G., Salazar M., Rosenmann E., Latorre R. A hot-sensing cold receptor: C-terminal domain determines thermosensation in transient receptor potential channels. J. Neurosci. 2006;26:4835–4840. doi: 10.1523/JNEUROSCI.5080-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Pérez-Cerezales S., Bermejo-Álvarez P. TRPV1: A channel for mammalian sperm thermotaxis? Transl. Cancer Res. 2017;6 doi: 10.21037/tcr.2017.03.17. [DOI] [Google Scholar]
- 180.Curtis M.P., Kirkman-Brown J.C., Connolly T.J., Gaffney E.A. Modelling a tethered mammalian sperm cell undergoing hyperactivation. J. Theor. Biol. 2012;309:1–10. doi: 10.1016/j.jtbi.2012.05.035. [DOI] [PubMed] [Google Scholar]
- 181.Simons J., Olson S., Cortez R., Fauci L. The dynamics of sperm detachment from epithelium in a coupled fluid-biochemical model of hyperactivated motility. J. Theor. Biol. 2014;354:81–94. doi: 10.1016/j.jtbi.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 182.Hsu C.C., Chien K.H., Yarmishyn A.A., Buddhakosai W., Wu W.J., Lin T.C., Chiou S.H., Chen J.T., Peng C.H., Hwang D.K., et al. Modulation of osmotic stress-induced TRPV1 expression rescues human iPSC-derived retinal ganglion cells through PKA. Stem Cell Res. Ther. 2019;10 doi: 10.1186/s13287-019-1363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Zhang Z., Liu J., Meriano J., Ru C., Xie S., Luo J., Sun Y. Human sperm rheotaxis: A passive physical process. Sci. Rep. 2016;6:23553. doi: 10.1038/srep23553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Miller M.R., Kenny S.J., Mannowetz N., Mansell S.A., Wojcik M., Mendoza S., Zucker R.S., Xu K., Lishko P.V. Asymmetrically Positioned Flagellar Control Units Regulate Human Sperm Rotation. Cell Rep. 2018;24:2606–2613. doi: 10.1016/j.celrep.2018.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Schiffer C., Rieger S., Brenker C., Young S., Hamzeh H., Wachten D., Tüttelmann F., Röpke A., Kaupp U.B., Wang T., et al. Rotational motion and rheotaxis of human sperm do not require functional CatSper channels and transmembrane Ca2+ signaling. EMBO J. 2020;39 doi: 10.15252/embj.2019102363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Yonghak P., Miyata S., Kurganov E. TRPV1 is crucial for thermal homeostasis in the mouse by heat loss behaviors under warm ambient temperature. Sci. Rep. 2020;10:8799. doi: 10.1038/s41598-020-65703-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Bernabò N., Ordinelli A., Di Agostino R., Mattioli M., Barboni B. Network analyses of sperm-egg recognition and binding: Ready to rethink fertility mechanisms? Omi. A J. Integr. Biol. 2014;18:740–753. doi: 10.1089/omi.2014.0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Martínez-León E., Osycka-Salut C., Signorelli J., Kong M., Morales P., Pérez-Martínez S., Díaz E.S. Fibronectin modulates the endocannabinoid system through the cAMP/PKA pathway during human sperm capacitation. Mol. Reprod. Dev. 2019;86:224–238. doi: 10.1002/mrd.23097. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.