Abstract
Virus-related liver carcinogenesis is one of the main contributors of cancer-related death worldwide mainly due to the impact of chronic hepatitis B and C infections. Three mechanisms have been proposed to explain the oncogenic properties of hepatitis B virus (HBV) infection: induction of chronic inflammation and cirrhosis, expression of HBV oncogenic proteins, and insertional mutagenesis into the genome of infected hepatocytes. Hepatitis B insertional mutagenesis modifies the function of cancer driver genes and could promote chromosomal instability. In contrast, hepatitis C virus promotes hepatocellular carcinoma (HCC) occurrence mainly through cirrhosis development whereas the direct oncogenic role of the virus in human remains debated. Finally, adeno associated virus type 2 (AAV2), a defective DNA virus, has been associated with occurrence of HCC harboring insertional mutagenesis of the virus. Since these tumors developed in a non-cirrhotic context and in the absence of a known etiological factor, AAV2 appears to be the direct cause of tumor development in these patients via a mechanism of insertional mutagenesis altering similar oncogenes and tumor suppressor genes targeted by HBV. A better understanding of virus-related oncogenesis will be helpful to develop new preventive strategies and therapies directed against specific alterations observed in virus-related HCC.
Keywords: hepatitis B, adeno associated virus type 2, genetic alterations, hepatitis delta
1. Introduction
Eliminating viral hepatitis has become a priority goal for the World Health Organization, which estimates that today, 325 million people are globally living with a viral hepatitis worldwide, with a vast majority being undiagnosed and/or untreated [1]. The viral cause of hepatitis was described for the first time in 1944 [2]. From 1965 to 1989, five hepatotropic viruses were identified—Hepatitis Viruses A, B, C, D, and E (Table 1) [3]. Several other risk factors such alcohol consumption or metabolic liver diseases can induce liver inflammation but viral infections remain so far the leading cause of chronic liver disease worldwide [4]. Hepatitis B, C, and D viruses can induce chronic infection; among people infected by Hepatitis B Virus (HBV), more than 90% of neonates develop chronic hepatitis but less than 10% in adulthood [5]. Due to the frequent progression of chronic hepatitis to cirrhosis and liver tumor development, chronic hepatitis B and C infections account for 1.3 million deaths each year [1].
Table 1.
Description of hepatitis viruses and their relationship with development of hepatocellular carcinoma.
| Virus | Genome | Number of Chronic Carriers | Development of Cirrhosis | Development of HCC | Oncogenic Mechanisms | Viral Oncoproteins |
|---|---|---|---|---|---|---|
| HAV | Single-stranded, positive-sense linear RNA virus | No chronic infection | No | No | -- | -- |
| HBV | Partially double-stranded, circular DNA virus | 257 millions | Yes | Yes | Chronic inflammation, oncoprotein, insertional mutagenesis | HBx, altered HBs or HBx |
| HCV | Single-stranded, positive-sense linear RNA virus | 71 millions | Yes | Yes | Chronic inflammation, oncoprotein | Core protein, NS3, NS4B, NS5A |
| HDV | Single-stranded, negative sense, closed circular RNA virus | 5% of HBV carriers | Yes | Yes | Chronic inflammation, oncoprotein | HDAg |
| HEV | Single-stranded, positive-sense linear RNA virus | Only in immuno compromized patient | Only in immuno compromized patient | Exceptionnal (immuno compromized patient) | -- | -- |
| AAV2 | Single-stranded DNA virus | 30–80% of positive serology in the general population 26% of AAV2 detected in liver |
No | Yes (rare event occurring in normal liver) | Insertional mutagenesis | -- |
Liver tumor is currently the fourth cause of death by cancer in the world with 782,000 deaths per year [6]. Hepatocellular carcinoma (HCC) represents 90% of all primary liver tumors and is related to HBV or Hepatitis C Virus (HCV) chronic infections in 85% of the cases [7]. In HBV- and HCV-infected patients, liver disease progression is explained by the constant and unsuccessful attempts of the immune system to clear the virus, leading to chronic liver damage [8]. Regardless of the cause (viral infection, chronic alcohol consumption, metabolic syndrome), chronic inflammation leading to liver cirrhosis plays a crucial role in carcinogenesis as up to 85% of HCC occurs on a background of cirrhosis [9]. Early oncogenic steps include WNT-β-catenin pathway activation, re-expression of fetal genes, deregulation of protein-folding machinery and the response to oxidative stress, replicative senescence bypassed by TERT promoter mutation [9]. However, apart from this common indirect mechanism, some studies showed that hepatitis viruses may have direct oncogenic properties, and especially HBV as 10 to 30% of HBV-associated HCC develop in a non-cirrhotic liver [10,11].
HCC are highly heterogenous tumors, and the knowledge of their genetic diversity has significantly increased in the recent years with advances in molecular classification and dissection of genetic drivers [11,12]. The main somatic genetic alterations observed in HCC were related to telomere maintenance (TERT promoter 40–60%, TERT amplification 5%), cell cycle control (TP53 15–40%, RB1 3–8%, CDKN2A 2–12%), Wnt-β catenin pathway (CTNNB1 10–35%, AXIN1 5–15%), epigenetic regulation (ARID1A 5–15%, ARID2 3–10%), oxidative stress pathway (NFE2L2 3–6%, KEAP1 2–8%) and AKT/mTOR and Ras/Raf MAP Kinase pathways (RPS6KA3 2–9%, PIK3CA 1%, TSC1 2%, TCS2 3%, FGF19 5%) with 2 to 6 driver genes altered per tumor among a total of 40 to 60 coding somatic mutations [13,14,15,16,17]. These genomic studies have highlighted specificities related to risk factors and helped to better understand the role played by viruses in hepatocarcinogenesis.
This review aims to give an overview about the genetics of viral hepatitis-associated liver tumors (Table 2) and the direct and indirect consequences of viral infections on HCC development.
Table 2.
Genomic profiles of virus-related HCC.
| Virus | HCC Features | Enriched Mutated Genes | Main Targeted Genes by Viral Integrations |
|---|---|---|---|
| Hepatitis B | Proliferative HCC, stem cell features, chromosomal instability |
TP53 (R249S), IRF2 | TERT, MLL4, CCNE1 |
| Hepatitis C | Less agressive, hepatocyte-like features differentiated, chromosomal stability |
TERT promoter, CTNNB1 | -- |
| Hepatitis D | Genetic instability | SPAT1 | -- |
| Adeno-Associated Virus type 2 | -- | PTEN, AXIN1 | CCNA2, CCNE1, GLI1 |
2. Genomics of Hepatitis B-Related HCC
More than 50% of HCC worldwide are associated with HBV infection and this percentage rises to 85% in some areas where the virus is endemic (China, Sub-Saharan Africa) [18]. Moreover, these numbers are probably underestimated because some HCC may develop as part of occult HBV infections that are usually not identified [19]. The risk of developing HCC is 15 to 20 times higher in people with chronic B infection than in the uninfected population [18]. This risk increases with the progression of liver disease: among cirrhotic patients, the incidence of developing HCC over 5 years is 15% in highly endemic regions such as Asia and Africa and 10% in the rest of the world [10]. However, regardless of the severity of the underlying liver disease, the risk of HCC in HBV-infected individuals is higher in endemic areas than in Western countries, possibly due to early acquisition of the virus at birth, longer duration of infection, or exposure to environmental genotoxic toxins such as aflatoxin B1 and aristolochic acid.
2.1. HBV Structure and Cell Cycle
Hepatitis B Virus (HBV) is a DNA virus of 3.2 kb. In an infectious viral particle, the HBV DNA is circular and partially double-stranded, in a form known as relaxed circular DNA (rcDNA). The HBV structure relies on an envelope composed of lipids and three types of surface proteins (HBsAg), containing a nucleocapsid composed of dimers (HBcAg), inside which the viral DNA genome is covalently linked with the viral polymerase [20].
Once entered in the cell via endocytosis, the surface proteins are cleaved, allowing the release of the nucleocapsid, which is transported to the nucleus [21]. The HBV rcDNA is then converted into a persistent covalently closed circular DNA (cccDNA) form compacted with cellular proteins (histones and non-histones) into a mini-chromosome [22]. Viral messenger RNAs (mRNA) are transcribed from HBV cccDNA and transported to the cytoplasm to be translated by the host cell in the different viral proteins, including HBx, a protein essential for cccDNA transcription [23]. HBV pregenomic RNA (pgRNA) is packaged by the capsid proteins and retrotranscribed by the viral polymerase into rcDNA (in 90% of cases) or into a double-strand linear DNA (dslDNA) form (in 10% of cases) [24]. Part of the nucleocapsid containing rcDNA or dslDNA returns to the host cell nucleus to be recycled and thus allows the maintenance of a pool of cccDNA in the nucleus. The other part is enveloped with the surface proteins and released outside the cell. Inside the nucleus, dslDNA may be integrated in the host genome. This illegitimate integration process is independent of the virus replication cycle and does not depend on the expression of viral proteins [25].
2.2. Genomic Landscape of HBV-Related HCC
Genomic alterations as well as transcriptomic dysregulation observed in HCC are strongly associated with risk factors. A recent study compared the mutation and transcriptomic profiles (reviewed in [26]) of HBV-related HCC with HCC related to other etiologies. HBV-related HCC were enriched in proliferative subclasses (G1-G3 transcriptomic subgroups) and specially in HCC with stem cell features (G1 transcriptomic subgroup). Moreover, the cell cycle pathway was more frequently altered in HBV-related HCC, mainly via inactivating mutations of TP53 (41% in HBV versus 16% in other etiologies) and IRF2, these two mutations being mutually exclusive [27]. In contrast, mutations of NFE2L2 or CTNNB1 genes were less frequent in HBV-related HCC [12]. In these HBV-related tumors, the mutational spectrum of TP53 has the particularity to have a high frequency of mutations on codon 249 (R249S) caused by exposure to Aflatoxin B1, as discussed below. Furthermore, TP53 mutations are associated with lower survival among patients with HBV-related HCC but not among those with HCC related to another etiology, suggesting a prognostic value of these mutations only in this specific group of particularly aggressive HCC [27].
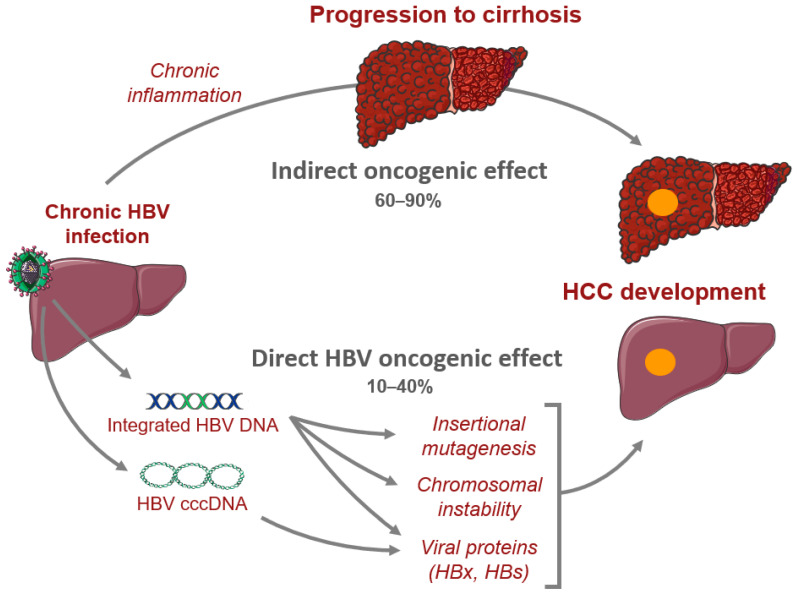
Moreover, one of the genomic feature of HBV-related HCC is the presence of frequent viral integrations in genes involved in carcinogenesis such as TERT, MLL4, and CCNE1 [11]. Finally, a higher rate of chromosomal instability is observed in HBV-related HCC [28]. This can probably be explained by the ability of HBV to induce genomic instability via viral integrations and HBx activity as well as by the frequency of mutations observed in TP53 and IRF2, two genes involved in the maintenance of chromosome stability (Figure 1) [11].
Figure 1.
Oncogenic mechanisms related to hepatitis B virus. We figured the direct and indirect mechanisms leading to HCC development in patients with chronic hepatitis B infection.
2.3. HBV Oncogenic Proteins
The HBx protein contains 154 amino acids and is encoded by the smallest open reading frame (ORF) of the HBV viral genome. This protein has been studied extensively and the results obtained vary considerably depending on the cell models and experimental conditions used. As experiments have been performed with a strong overexpression of the HBx protein or in the absence of other viral proteins, they do not necessarily reflect the infectious context [29]. The functions of this protein are still controversial but can be broadly divided into two groups: the role of HBx in viral replication through degradation of the host factors and transcriptional modulation and its involvement in hepato-carcinogenesis.
HBx could foster tumor development through the following mechanisms (reviewed in [11,30,31]): (1) transcription dysregulation due to its interaction with transcription factors, chromatin-modifying enzymes, or components of the cellular transcriptional machinery, (2) regulation of senescence through TERT overexpression, inhibition of p53 or Rb proteins, and p53 sequestration in the cytoplasm [31], (3) regulation of apoptosis through both pro- and anti-apoptotic properties, depending on the level of HBx expression and the cellular context, (4) impairment of DNA repair through interaction with DDB1 or p53 proteins, (5) dysregulation of the cell cycle and the mitotic process through activation of MAP-Kinase, JNK, or Src kinase pathways.
In contrast, a recent study reported a higher frequency of inactivating mutations of the HBx gene in HCC compared to non-tumor tissues, suggesting a role of tumor suppressor gene of HBx and the existence of a selection pressure during carcinogenesis that could promote proliferation of cells in which HBx is inactive [27].
2.4. HBV Integrations
The identification of an HBV sequence integrated into the DNA of a human HCC was first described in 1980 [32] and it is now admitted that HBV integration events are observed in almost all tumors (80–90%) [33]. However, since integrations occur within a few days after infection [34], decades may elapse between viral insertion and HCC development. So far, three mechanisms have been proposed to explain the oncogenic consequences of integrations: insertional mutagenesis nearby a cancer-related gene, expression of abnormal viral proteins from integrated HBV DNA, and induction of chromosomal instability [24,35].
First, viral integrations may induce changes in gene expression via activation of transcription through integration in promoters, exons or introns, and, to a lesser extent, in intergenic regions [36,37,38]. Three genes have been identified as recurrent integration sites (40% of HBV-related HCC): TERT, MLL4, and CCNE1 [39,40]. TERT is the gene the most frequently altered by HBV integrations that are mainly located in the promoter and mutually exclusive of other TERT alterations such as promoter mutations [14,41,42]. Moreover, the closer the integration site is to the transcription initiation site, the higher is TERT expression, suggesting that the viral sequence acts as an enhancer [38]. Two recent studies using cellular models have shown that the “Enhancer I” region can induce TERT activation via the recruitment of transcription factors [40,42]. MLL4 integrations are located between exons 2 and 6 and induce the synthesis of fusion HBV-MLL4 transcripts. HBV integrations generally modify the open-reading frame, resulting in a loss of function [39,43,44,45]. Finally, viral insertions in CCNE1 induce an overexpression of the gene and a deregulation of the cell cycle fostering replicative stress responsible of a specific signature of rearrangements in the tumor genome [46]. The same genomic pattern is observed in HCC with HBV integrations in CCNA2 leading to a protein truncated at its N-terminal end, lacking of its regulatory domain. All HCC harboring an alteration in CCNA2 or CCNE1 (due to viral integration or structural rearrangements) belong to a homogeneous subgroup of large and aggressive tumors with a poor prognostic mostly developed in the absence of cirrhosis. A recent study showed that tumors with a high number of HBV integrations were associated with poor prognosis [47].
Moreover, the HBV sequence integrated in the hepatocyte genome could contain the full preS/S ORF region and its promoter and could be responsible of the expression of viral proteins. Several studies showed that HBsAg can derive from HBV integrated DNA [48,49] and remain functional as the formation of infectious HDV virions was observed [50,51]. Interestingly, HCC replicating the virus and expressing pgRNA were associated with a specific transcriptomic profile and have a good prognosis [49]. However, deletions of the preS region are frequently identified in HCC, removing the C-terminal part of preS1 domain or the N-terminal part of preS2 domain. In vitro, the expression of altered envelope proteins induces endoplasmic reticulum stress, oxidative stress, and DNA damage, leading to cell cycle progression and malignant transformation [52,53]. In addition, given the structure of dslDNA, the ORF X is truncated at its C-terminal end in integrated sequences, as observed in at least half of the HCC for which this viral gene was detectable [42]. This leads to the synthesis of a truncated or fusion transcript. The overexpression of a truncated HBx protein has been associated in in vitro and in vivo models with progenitor cell properties, malignant transformation, inhibition of apoptosis, and tumor invasion [42,54,55]. However, these phenotypes may be due to a HBx overexpression at a level much higher than its expression under the activity of its native promoter. Overall, as mentioned above, since the role played by the wild-type HBx protein in carcinogenesis is not well established, it is difficult to conclude on the oncogenic potential of the truncated HBx protein without alternative models of infection [56].
Finally, HBV integrations are enriched near fragile sites, repeated regions, CpG islands and telomeres in tumors but not in non-tumor tissues, suggesting that hepatocytes with alterations in these regions are selected during carcinogenesis and that such integrations promote HCC development by inducing genomic instability [57]. In addition, a significant proportion of the viral integration sites occurred in the vicinity of DNA copy number alterations [14,37,39]. We recently described frequent chromosome rearrangements at HBV integration sites leading to cancer-driver genes (TERT, TP53, MYC) alterations [47]. The number of integrations is also associated with the number of structural variants [41], and two hypotheses have been proposed to explain this association. Chromosomal instability induced by an external factor may promote the integration mechanism of the virus as HBV insertions occur preferentially at double-stranded break sites [41]. At the other side, viral integration can be a driver inducing genomic instability and structural variants, as discussed above for integrations in CCNA2 or CCNE1 genes [46].
3. Genomics of Hepatitis C-Related HCC
Hepatitis C Virus (HCV) is one of the main etiology of HCC in low incidence areas (Western Europe, North America, Japan, Middle-East) [7,18]. The risk of developing HCC in patients with chronic hepatitis C increases with the severity of fibrosis stage. Overall, the rate of HCC occurrence is 1–5% per year in cirrhotic patients [18] modulated by numerous factors related to host (older age, male sex, severity of liver disease, presence of comorbidities) or virus (HCV genotype, HCV viral load, coinfections with HBV or HIV, viral eradication) [10].
3.1. HCV Structure and Cell Cycle
HCV is a single-stranded, positive-sense linear RNA virus of 9.6 kb that includes a 5’ non-coding region, an open reading frame, and a 3’ non-coding region [58]. Viral particles are composed of a lipidic envelope with two viral envelope glycoproteins anchored (E1 and E2), containing an icosahedral capsid formed by Core proteins, inside which is the viral genome [59].
When the virion enters the cell, the fusion of the viral envelope to the endosome membrane and the dissociation of the viral core allow the release of the HCV genome in the cytoplasm [60]. The viral RNA is recognized as a mRNA and translated by the host cellular machinery to form a precursor polyprotein of about 3000 amino acids [61]. This polyprotein is then cleaved by cellular and viral enzymes into ten viral proteins: the structural proteins (Core protein, E1 and E2), the non-structural proteins (NS2, NS3, NS4A, NS4B, NS5A et NS5B), and the protein p7, which is the result of an incomplete cleavage from the E2 protein [62]. Replication complexes are then formed with non-structural proteins and viral RNA to catalyze the transcription of a negative-sense RNA intermediate from which the positive-sense RNA is finally generated. Capsid proteins assemble and recruit HCV genome, before being enveloped, and mature virions are released outside the cell via the secretory pathway [61].
3.2. Genomic Landscape of HCV-Related HCC
Compared to HBV-related HCC, HCV-related HCC are less aggressive, with chromosomal stability, more differentiated and they tend to retain hepatocyte-like features [63,64]. A study comparing patients with these two etiologies highlighted a significantly higher frequency of TERT and CTNNB1 mutations in HCV-related HCC (53.6% and 26.4%, respectively) than in HBV-related (41.7% and 16.7%, respectively) [65]. However, mutations in cancer-related genes are very similar between HCV- and alcohol-related HCC suggesting that the difference observed in the literature between HCV- and HBV-induced HCC is mainly explained by the specific genomic profile of HBV-related HCC [13].
Mutations observed in HCV-related HCC are mainly triggered by an indirect effect of immune-mediated chronic inflammation and by liver damage. Moreover, since HCV has a lifecycle exclusively cytoplasmic, pro-oncogenic events are more likely to be indirect [66]. However, several observations suggest a potential direct role of HCV in the carcinogenic process. Clinical evidence showed that HCC can occur in HCV-infected patients in the absence of cirrhosis, although at a lower frequencies than in cirrhotic patients [67,68]. Furthermore, in vivo studies demonstrated that HCC develop in HCV transgenic mice in the absence of inflammation or fibrosis [69,70]. Overall, these results suggested that the persistence of HCV infection and of the expression of viral proteins could play a role in HCC promotion.
3.3. HCV Oncogenic Proteins
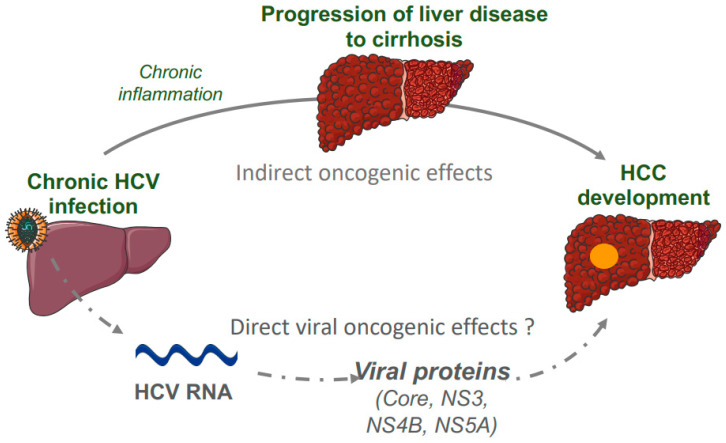
The core protein is highly conserved and plays a role in viral assembly and in the modulation of cellular transformation, transcription, apoptosis, lipid metabolism, and oxidative stress (reviewed in [71]) (Figure 2). Mice with liver-specific expression of the core gene developed histological features of chronic hepatitis C infection and HCC, without enhanced liver inflammation [69]. Possible oncogenic mechanisms relies on the properties of the HCV core protein to deregulate the cell cycle and promote cell proliferation by interacting with the proteins p53, p73 and Rb, by activating the Raf1/MAPK and Wnt/β-catenin pathways, by modulating the TGFβ signaling or by increasing telomerase activity [29]. This protein may also induce transformational changes in hepatocytes by upregulating several cellular proteins regulating inflammation such as IL-6, gp130, leptin receptor, and STAT3 [29].
Figure 2.
Oncogenic mechanisms related to hepatitis C virus. Direct and indirect oncogenic mechanisms leading to HCC development in patients with chronic hepatitis C infection were represented.
In addition, three non-structural HCV proteins (NS3, NS4B, NS5A) activate different mechanisms that inhibit apoptosis, accelerate proliferation, and induce genomic instability [8]. In vitro experiments highlighted that HCV NS3 can induce cellular transformation directly via its serine protease activity [72,73]. HCV NS4B may play a direct role in cellular transformation in cooperation with the HA-ras oncogene [74,75], or may have an indirect contribution to carcinogenesis by inducing endoplasmic reticulum (ER) stress and modulating lipid metabolism [76]. HCV NS5A is part of the HCV RNA replication complex and may promote the establishment of chronic HCV infection and then HCC development via its antiapoptotic activity (Figure 2) [77,78].
However, as all these studies analyzing the potential oncogenic properties of HCV proteins are based on overexpression experiments, they do not reflect the expression levels in HCV-infected cells, and do not take into account the inflammatory environment [8].
4. Genomics of Hepatitis D-Related HCC
Around 5% of people infected with HBV worldwide are diagnosed as co-infected with hepatitis D virus (HDV), but this percentage is likely underestimated as HDV diagnosis is not systematically assessed in the majority of developing countries [1]. HDV is a defective virus that requires HBsAg to be pathogenic. Therefore, HDV infection can occur through simultaneous coinfection with HBV or through HDV superinfection of chronic HBV-infected patients [79].
4.1. HDV Structure and Natural History of Infection
HDV is a small RNA virus (1.7 kb) with a single-stranded genome contained in a nucleocapsid formed by proteins termed HD antigens (HDAg) [80] and surrounded by a lipid envelope with the three types of HBV surface proteins [81,82]. Once entered in hepatocytes, the HDV genome is released, it translocates to the nucleus, and uses RNA polymerase II to replicate [83]. This replication is based on a Rolling-circle mechanism. A first step generates an anti-genome complementary to the HDV genome and a second step uses this anti-genome to reform the initial genome that will be enveloped in the new virions [83]. An anti-genomic RNA is also the template for the synthesis of two forms of HDAg: the S-HDAg proteins necessary for viral replication and the L-HDAg proteins that allow the assembly of virions by binding to the HBsAg proteins [84].
HDV infection generally results in decreased HBV viral replication, although viral dominance appears to fluctuate over time in patients [85,86]. The mechanism proposed to explain this HDV dominance (reviewed in [79]) are based on HDAg, which induce epigenetic regulation of HBV cccDNA reducing pgRNA transcription, repressing HBV enhancer sequences and decreasing the stability of HBV viral RNAs. Moreover, another hypothesis suggests that HDV virion assembly is favored in hepatocytes where HBV does not replicate but when HBsAg are produced from the integrated forms of the virus [51]. Finally, HDV induces a strong immune response producing interferons that could have an antiviral effect on HBV [87].
HDV infection is considered as the most severe form of chronic viral hepatitis, although it relies on the presence of HBV infection [88]. Progression to cirrhosis is observed in 10–15% of these patients after 2 years and in more than 80% of patients after 30 years [89]. Recent clinical observations suggest that co-infection also increases the risk of HCC compared to HBV infection alone [90,91,92]. As HDV requires the presence of HBV to propagate, it is unlikely that HDV has direct oncogenic properties. However, several events occurring during HDV infection may promote HCC development such as induction of oxidative stress by HDV-related inflammation or interference with DNA methylation by HDV proteins [93].
4.2. Genomic Landscape of HDV-Related HCC
Few data are currently available to understand the genomic landscape of HDV-related HCC [92]. The analysis of 5 HDV-HCC has revealed a strong activation of pathways involved in cell-cycle, DNA replication, DNA damage, and DNA repair, and suggested a key role of genetic instability in HDV-related carcinogenesis [94]. Comparison of HDV-HCC with HBV-HCC and HCV-HCC underlined that the molecular mechanisms involved are distinct for each hepatitis virus. A genomic analysis on 76 HCC from Mongolian patients included a high proportion of HDV-HCC (n = 28) [95,96] and showed an enrichment of mutations in SPAT1, a gene encoding for α-spectrin, in HDV-related HCC [96]. However, SPAT1 had never been reported as a HCC driver gene in other studies and the impact of HDV in liver carcinogenesis remains to be better elucidated. Interestingly, HBV/HDV related HCC harbored less frequent HBV insertion in cancer drivers gene such as the TERT promoter compared to HBV alone related HCC [47].
5. Interactions with Exposures to Genotoxic Agents
Exposure to genotoxic agents is responsible of mutational processes that can be identified using new generation sequencing through the analysis of mutational signatures. In particular, Aflatoxin B1 (AFB1) and Aristolochic Acid are associated with two specific mutational signatures observed in HCC [97].
5.1. HBV Infection and Aflatoxin B1 Exposure
Aflatoxin B1 (AFB1) is a carcinogenic mycotoxin produced by a fungus called Aspergillus flavus that can contaminate cereals and peanuts. Whereas it is almost non-existent in Western countries, 90% of the population of sub-Saharan West Africa is exposed to this toxin [98]. AFB1 is an independent risk factor of HCC development when exposure is high but requires HBV as a cofactor when exposure is low or moderate (reviewed in [99]).
From a molecular point of view, AFB1 is oxidized in cells by CYP450 enzymes to form an unstable metabolite that reacts with DNA and produces adducts on guanine residues. The majority of these adducts are repaired by the nucleotide excision mechanism but the remaining DNA lesions can generate mutations, mostly G-T transversions [100]. The G > T substitution on the TP53 gene induces the R249S mutation frequently identified in HCC and considered as pathognomonic of AFB1 exposure [98]. Several mechanisms have been suggested to explain how HBV could increase the mutagenic effect of AFB1 (reviewed in [98]): the chronic viral infection may directly increase the activity of CYP450 enzymes and generate oxidative stress, the selection pressure may favor clonal proliferation of cells containing these mutations, and finally the HBx protein deregulating DNA repair by nucleotide excision may impair the repair of DNA adducts. We recently showed that patients with HBV related HCC and AFB1 exposure where younger with more frequent HCC harboring stem cell features compared to HBV related HCC without AFB1 exposure [47]. Furthermore, a genomic characterization of HCC related to AFB1 exposure identified frequent mutations in the ADGRB1 gene in addition to those described in TP53. These HCC contained more neo-antigens and harbored high lymphocyte infiltration and high PD-L1 expression [101].
5.2. HBV Infection and Aristolochic Acid Exposure
Aristolochic acid is a highly mutagenic compound contained in plants called Aristolochia or Asarum [102]. These plants have been used in traditional Chinese medicine for several centuries. The interaction between metabolites of aristolochic acid and DNA generates the formation of adducts on adenine residues and thus leads to the appearance of A-T transversions [103,104]. A recent epidemiological study conducted in Taiwan demonstrated that, since aristolochic acid was prescribed as a treatment for chronic hepatitis B until 2003, 59.4% of patients infected with HBV were exposed to the genotoxic agent [105]. This work also demonstrated a dose-dependent association between aristolochic acid exposure and the development of HCC in HBV-infected patients. This suggests a cooperation between HBV and aristolochic acid promoting carcinogenesis [106].
5.3. HDV Infection and Genotoxic Exposures
A recent genomic study on Mongolian HDV-HCC identified an association between HDV infection and mutational signatures suggestive of exposition to alkylating agents, tobacco chewing, 1,8-Dinitropyrene and furan [96].
6. AAV as a New Player in Viral-Associated Liver Tumors
The Adeno-associated virus (AAV) is a defective DNA virus responsible of non-pathogenic and frequent infections in the general population (30–80%). However, recurrent clonal integrations of AAV2 have been identified in a subgroup of HCC in 2015, suggesting that this virus could be pathogenic in rare circumstances [107].
6.1. AAV Structure and Natural History of Infection in the Liver
AAV is a small, single-stranded DNA virus with an unwrapped capsid [108]. It is a defective virus as it requires the presence of another virus to replicate (an adenovirus or a herpes simplex virus) and otherwise establishes a latent infection [109,110]. Twelve distinct serotypes have been described and AAV2 is the most common in humans [111]. They are considered as non-pathogenic to humans and are widely used in gene therapy as the transfection of recombinant AAV vectors shows a high efficacy and low immunogenicity [112].
Although it has been shown a few years ago that the liver is the main site of infection of AAV viruses [113], little information was available on the natural history of infection until recently. The analysis of non-tumor tissues and liver tumors from a cohort of 1319 patients revealed the presence of AAV DNA in 21% of patients, more frequently in non-tumor tissues than in tumors and mainly in young female patients without cirrhosis. Two main AAV genotypes were identified: AAV2 and a recombined sequence of AAV2/AAV13. Moreover, the study assessed the presence of episomal AAV DNA in 26% of non-tumor tissues, strongly associated with viral RNA expression, suggesting that the virus is transcriptionally active in the liver of these patients. Human Herpes Virus 6 (HHV-6) was suggested to be the main helper virus co-infecting liver tissues during active AAV infection.
6.2. AAV-Related Liver Carcinogenesis
Only 8% of the tumors analyzed contained AAV DNA and the proportion was identical between malignant and benign tumors, but the malignant tumors harbored a higher number of copies per cell due to clonal viral integrations. A total of 19 clonal integrations were identified in 2% of the HCC cohort and almost no episomal form of the virus. All HCC were developed on non-cirrhotic liver and without other viral etiologies. Within all published studies, the genes described as altered by somatic AAV insertional mutagenesis were CCNA2, CCNE2, TERT, TNFSF10, MLL4, and GLI1/INHBE [107,114,115,116]. Two mechanisms were described to explain the oncogenic consequences of AAV clonal integrations. First, the integrated AAV sequence frequently contains viral enhancers and transcription factor binding sites [117], leading to the strong overexpression of the oncogene at vicinity (CCNE1 or TERT) [46,107]. Second, viral integrated sequences may induce the synthesis of truncated transcripts due to the use of an alternative Transcription Start Site (TSS) or of the viral poly-A site (for integrations in CCNA2 and TNFSF10, respectively). Although rare, viral integration of AAV in specific regions of the human genome can promote hepatocarcinogenesis in a non-cirrhotic liver, confirming that AAV is associated with HCC occurrence via an insertional mutagenesis mechanism.
Interestingly, a region present in all inserted AAV sequences was recently described as a liver-specific enhancer-promoter element [117]. Although this region is absent in most AAV vectors currently in use, different animal models showed that integrated AAV vectors can induce clonal expansion [118] and play a role in carcinogenesis [119,120]. To date, no liver tumor has been reported in patients treated using AAV vectors, but they should be followed longitudinally to monitor long-term effects and assess the potential risk of HCC development [107,121].
7. Conclusions & Perspective
Major advances have been performed on the knowledge of the direct and indirect roles of hepatic viruses during liver carcinogenesis as well as on the description of the specific genomic profiles present in HBV- and HCV-related HCC. However, there is still unmet needs in the field of pathophysiology of virus-related carcinogenesis and in translation in clinical practices. First, few data are available in HDV-related liver carcinogenesis. Moreover, the impact of viral suppression of hepatitis B and viral eradication of hepatitis C on HCC pathogenesis remains to be studied in the future, in order to better understand why malignant transformation still occurs even after control of the etiology. The translation in clinical practice is still limited in terms of prediction of HCC occurrence or early detection of HCC in patients with HBV and HCV infection. New biomarkers based on our knowledge of early events of viral liver carcinogenesis should be developed. Finally, future clinical trials of targeted therapies and immunotherapies need to be adapted on the specificity of each virus-induced carcinogenesis, such as enrichment in specific genetic alterations or expression of viral neoantigens.
Author Contributions
Writing—original draft preparation, C.P. and J.-C.N.; writing—review and editing, C.P., J.Z.-R. and J.-C.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
Jean-Charles Nault received a research grant from Bayer for Inserm UMR1138.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Global Hepatitis Report, 2017. WHO; Geneva, Switzerland: 2017. [Google Scholar]
- 2.Block T.M., Alter H.J., London W.T., Bray M. A historical perspective on the discovery and elucidation of the hepatitis B virus. Antivir. Res. 2016;131:109–123. doi: 10.1016/j.antiviral.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 3.Blum H.E. History and Global Burden of Viral Hepatitis. Dig. Dis. 2016;34:293–302. doi: 10.1159/000444466. [DOI] [PubMed] [Google Scholar]
- 4.Razavi H. Global Epidemiology of Viral Hepatitis. Gastroenterol. Clin. N. Am. 2020;49:179–189. doi: 10.1016/j.gtc.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 5.Trépo C., Chan H.L.Y., Lok A. Hepatitis B virus infection. Lancet. 2014;384:2053–2063. doi: 10.1016/S0140-6736(14)60220-8. [DOI] [PubMed] [Google Scholar]
- 6.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 7.Yang J.D., Hainaut P., Gores G.J., Amadou A., Plymoth A., Roberts L.R. A global view of hepatocellular carcinoma: Trends, risk, prevention and management. Nat. Rev. Gastroenterol. Hepatol. 2019;16:589–604. doi: 10.1038/s41575-019-0186-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shirvani-Dastgerdi E., Schwartz R.E., Ploss A. Hepatocarcinogenesis associated with hepatitis B, delta and C viruses. Curr. Opin. Virol. 2016;20:1–10. doi: 10.1016/j.coviro.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Llovet J.M., Zucman-Rossi J., Pikarsky E., Sangro B., Schwartz M., Sherman M., Gores G. Hepatocellular carcinoma. Nat. Rev. Dis. Prim. 2016;2:16018. doi: 10.1038/nrdp.2016.18. [DOI] [PubMed] [Google Scholar]
- 10.Fattovich G., Stroffolini T., Zagni I., Donato F. Hepatocellular carcinoma in cirrhosis: Incidence and risk factors. Gastroenterology. 2004;127:S35–S50. doi: 10.1053/j.gastro.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 11.Levrero M., Zucman-Rossi J. Mechanisms of HBV-induced hepatocellular carcinoma. J. Hepatol. 2016;64:S84–S101. doi: 10.1016/j.jhep.2016.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Schulze K., Nault J.-C., Villanueva A. Genetic profiling of hepatocellular carcinoma using next-generation sequencing. J. Hepatol. 2016;65:1031–1042. doi: 10.1016/j.jhep.2016.05.035. [DOI] [PubMed] [Google Scholar]
- 13.Schulze K., Imbeaud S., Letouzé E., Alexandrov L.B., Calderaro J., Rebouissou S., Couchy G., Meiller C., Shinde J., Soysouvanh F., et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nat. Genet. 2015;47:505–511. doi: 10.1038/ng.3252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Totoki Y., Tatsuno K., Covington K.R., Ueda H., Creighton C.J., Kato M., Tsuji S., Donehower L.A., Slagle B.L., Nakamura H., et al. Trans-ancestry mutational landscape of hepatocellular carcinoma genomes. Nat. Genet. 2014;46:1267–1273. doi: 10.1038/ng.3126. [DOI] [PubMed] [Google Scholar]
- 15.Dhanasekaran R., Nault J.-C., Roberts L.R., Zucman-Rossi J. Genomic Medicine and Implications for Hepatocellular Carcinoma Prevention and Therapy. Gastroenterology. 2019;156:492–509. doi: 10.1053/j.gastro.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ningarhari M., Caruso S., Hirsch T.Z., Bayard Q., Franconi A., Védie A.-L., Noblet B., Blanc J.-F., Amaddeo G., Ganne N., et al. Telomere length is key to hepatocellular carcinoma diversity and telomerase addiction is an actionable therapeutic target. J. Hepatol. 2021;74:1155–1166. doi: 10.1016/j.jhep.2020.11.052. [DOI] [PubMed] [Google Scholar]
- 17.Hirsch T.Z., Negulescu A., Gupta B., Caruso S., Noblet B., Couchy G., Bayard Q., Meunier L., Morcrette G., Scoazec J.-Y., et al. BAP1 mutations define a homogeneous subgroup of hepatocellular carcinoma with fibrolamellar-like features and activated PKA. J. Hepatol. 2020;72:924–936. doi: 10.1016/j.jhep.2019.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Petruzziello A. Epidemiology of Hepatitis B Virus (HBV) and Hepatitis C Virus (HCV) Related Hepatocellular Carcinoma. TOVJ. 2018;12:26–32. doi: 10.2174/1874357901812010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morales-Romero J., Vargas G., García-Román R. Occult HBV Infection: A Faceless Enemy in Liver Cancer Development. Viruses. 2014;6:1590–1611. doi: 10.3390/v6041590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lamontagne R.J., Bagga S., Bouchard M.J. Hepatitis B virus molecular biology and pathogenesis. Hepatoma Res. 2016;2:163. doi: 10.20517/2394-5079.2016.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Valaydon Z.S., Locarnini S.A. The virological aspects of hepatitis B. Best Pract. Res. Clin. Gastroenterol. 2017;31:257–264. doi: 10.1016/j.bpg.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 22.Nassal M. HBV cccDNA: Viral persistence reservoir and key obstacle for a cure of chronic hepatitis B. Gut. 2015;64:1972–1984. doi: 10.1136/gutjnl-2015-309809. [DOI] [PubMed] [Google Scholar]
- 23.Lucifora J., Arzberger S., Durantel D., Belloni L., Strubin M., Levrero M., Zoulim F., Hantz O., Protzer U. Hepatitis B virus X protein is essential to initiate and maintain virus replication after infection. J. Hepatol. 2011;55:996–1003. doi: 10.1016/j.jhep.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 24.Tu T., Budzinska M., Shackel N., Urban S. HBV DNA Integration: Molecular Mechanisms and Clinical Implications. Viruses. 2017;9:75. doi: 10.3390/v9040075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seeger C., Mason W.S. Molecular biology of hepatitis B virus infection. Virology. 2015;479–480:672–686. doi: 10.1016/j.virol.2015.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zucman-Rossi J., Villanueva A., Nault J.-C., Llovet J.M. Genetic Landscape and Biomarkers of Hepatocellular Carcinoma. Gastroenterology. 2015;149:1226–1239.e4. doi: 10.1053/j.gastro.2015.05.061. [DOI] [PubMed] [Google Scholar]
- 27.Amaddeo G., Cao Q., Ladeiro Y., Imbeaud S., Nault J.-C., Jaoui D., Gaston Mathe Y., Laurent C., Laurent A., Bioulac-Sage P., et al. Integration of tumour and viral genomic characterisations in HBV-related hepatocellular carcinomas. Gut. 2015;64:820–829. doi: 10.1136/gutjnl-2013-306228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guichard C., Amaddeo G., Imbeaud S., Ladeiro Y., Pelletier L., Maad I.B., Calderaro J., Bioulac-Sage P., Letexier M., Degos F., et al. Integrated analysis of somatic mutations and focal copy-number changes identifies key genes and pathways in hepatocellular carcinoma. Nat. Genet. 2012;44:694–698. doi: 10.1038/ng.2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bouchard M.J., Navas-Martin S. Hepatitis B and C virus hepatocarcinogenesis: Lessons learned and future challenges. Cancer Lett. 2011;305:123–143. doi: 10.1016/j.canlet.2010.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Benhenda S., Cougot D., Buendia M.-A., Neuveut C. Advances in Cancer Research. Volume 103. Elsevier; Amsterdam, The Netherlands: 2009. Chapter 4 Hepatitis B Virus X Protein; pp. 75–109. [DOI] [PubMed] [Google Scholar]
- 31.Kew M.C. Hepatitis B virus x protein in the pathogenesis of hepatitis B virus-induced hepatocellular carcinoma: HBX and HCC. J. Gastroenterol. Hepatol. 2011;26:144–152. doi: 10.1111/j.1440-1746.2010.06546.x. [DOI] [PubMed] [Google Scholar]
- 32.Brechot C., Pourcel C., Louise A., Rain B., Tiollais P. Presence of integrated hepatitis B virus DNA sequences in cellular DNA of human hepatocellular carcinoma. Nature. 1980;286:533–535. doi: 10.1038/286533a0. [DOI] [PubMed] [Google Scholar]
- 33.Bréchot C., Gozuacik D., Murakami Y., Paterlini-Bréchot P. Molecular bases for the development of hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC) Semin. Cancer Biol. 2000;10:211–231. doi: 10.1006/scbi.2000.0321. [DOI] [PubMed] [Google Scholar]
- 34.Tu T., Budzinska M.A., Vondran F.W.R., Shackel N.A., Urban S. Hepatitis B Virus DNA Integration Occurs Early in the Viral Life Cycle in an In Vitro Infection Model via Sodium Taurocholate Cotransporting Polypeptide-Dependent Uptake of Enveloped Virus Particles. J. Virol. 2018;92:e02007-17. doi: 10.1128/JVI.02007-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Budzinska M.A., Shackel N.A., Urban S., Tu T. Cellular Genomic Sites of Hepatitis B Virus DNA Integration. Genes. 2018;9:365. doi: 10.3390/genes9070365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ally A., Balasundaram M., Carlsen R., Chuah E., Clarke A., Dhalla N., Holt R.A., Jones S.J.M., Lee D., Ma Y., et al. Comprehensive and Integrative Genomic Characterization of Hepatocellular Carcinoma. Cell. 2017;169:1327–1341.e23. doi: 10.1016/j.cell.2017.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jiang Z., Jhunjhunwala S., Liu J., Haverty P.M., Kennemer M.I., Guan Y., Lee W., Carnevali P., Stinson J., Johnson S., et al. The effects of hepatitis B virus integration into the genomes of hepatocellular carcinoma patients. Genome Res. 2012;22:593–601. doi: 10.1101/gr.133926.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Toh S.T., Jin Y., Liu L., Wang J., Babrzadeh F., Gharizadeh B., Ronaghi M., Toh H.C., Chow P.K.-H., Chung A.Y.-F., et al. Deep sequencing of the hepatitis B virus in hepatocellular carcinoma patients reveals enriched integration events, structural alterations and sequence variations. Carcinogenesis. 2013;34:787–798. doi: 10.1093/carcin/bgs406. [DOI] [PubMed] [Google Scholar]
- 39.Sung W.-K., Zheng H., Li S., Chen R., Liu X., Li Y., Lee N.P., Lee W.H., Ariyaratne P.N., Tennakoon C., et al. Genome-wide survey of recurrent HBV integration in hepatocellular carcinoma. Nat. Genet. 2012;44:765–769. doi: 10.1038/ng.2295. [DOI] [PubMed] [Google Scholar]
- 40.Li C., Li C., Lin Y., Ho M., Chen D., Chen P., Yeh S. Androgen Receptor Enhances Hepatic Telomerase Reverse Transcriptase Gene Transcription After Hepatitis B Virus Integration or Point Mutation in Promoter Region. Hepatology. 2019;69:498–512. doi: 10.1002/hep.30201. [DOI] [PubMed] [Google Scholar]
- 41.Fujimoto A., Furuta M., Totoki Y., Tsunoda T., Kato M., Shiraishi Y., Tanaka H., Taniguchi H., Kawakami Y., Ueno M., et al. Whole-genome mutational landscape and characterization of noncoding and structural mutations in liver cancer. Nat. Genet. 2016;48:500–509. doi: 10.1038/ng.3547. [DOI] [PubMed] [Google Scholar]
- 42.Sze K.M., Ho D.W., Chiu Y., Tsui Y., Chan L., Lee J.M., Chok K.S., Chan A.C., Tang C., Tang V.W., et al. HBV-TERT Promoter Integration Harnesses Host ELF4 Resulting in TERT Gene Transcription in Hepatocellular Carcinoma. Hepatology. 2021;73:23–40. doi: 10.1002/hep.31231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dong H., Zhang L., Qian Z., Zhu X., Zhu G., Chen Y., Xie X., Ye Q., Zang J., Ren Z., et al. Identification of HBV-MLL4 Integration and Its Molecular Basis in Chinese Hepatocellular Carcinoma. PLoS ONE. 2015;10:e0123175. doi: 10.1371/journal.pone.0123175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Furuta M., Tanaka H., Shiraishi Y., Uchida T., Imamura M., Fujimoto A., Fujita M., Sasaki-Oku A., Maejima K., Nakano K., et al. Characterization of HBV integration patterns and timing in liver cancer and HBV-infected livers. Oncotarget. 2018;9:25075–25088. doi: 10.18632/oncotarget.25308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shiraishi Y., Fujimoto A., Furuta M., Tanaka H., Chiba K., Boroevich K.A., Abe T., Kawakami Y., Ueno M., Gotoh K., et al. Integrated Analysis of Whole Genome and Transcriptome Sequencing Reveals Diverse Transcriptomic Aberrations Driven by Somatic Genomic Changes in Liver Cancers. PLoS ONE. 2014;9:e114263. doi: 10.1371/journal.pone.0114263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bayard Q., Meunier L., Peneau C., Renault V., Shinde J., Nault J.-C., Mami I., Couchy G., Amaddeo G., Tubacher E., et al. Cyclin A2/E1 activation defines a hepatocellular carcinoma subclass with a rearrangement signature of replication stress. Nat. Commun. 2018;9:5235. doi: 10.1038/s41467-018-07552-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Péneau C., Imbeaud S., La Bella T., Hirsch T.Z., Caruso S., Calderaro J., Paradis V., Blanc J.-F., Letouzé E., Nault J.-C., et al. Hepatitis B virus integrations promote local and distant oncogenic driver alterations in hepatocellular carcinoma. Gut. 2021:gutjnl-2020-323153. doi: 10.1136/gutjnl-2020-323153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yoo S., Wang W., Wang Q., Fiel M.I., Lee E., Hiotis S.P., Zhu J. A pilot systematic genomic comparison of recurrence risks of hepatitis B virus-associated hepatocellular carcinoma with low- and high-degree liver fibrosis. BMC Med. 2017;15:214. doi: 10.1186/s12916-017-0973-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Halgand B., Desterke C., Rivière L., Fallot G., Sebagh M., Calderaro J., Bioulac-Sage P., Neuveut C., Buendia M.-A., Samuel D., et al. Hepatitis B Virus Pregenomic RNA in Hepatocellular Carcinoma: A Nosological and Prognostic Determinant. Hepatology. 2018;67:86–96. doi: 10.1002/hep.29463. [DOI] [PubMed] [Google Scholar]
- 50.Wooddell C.I., Yuen M.-F., Chan H.L.-Y., Gish R.G., Locarnini S.A., Chavez D., Ferrari C., Given B.D., Hamilton J., Kanner S.B., et al. RNAi-based treatment of chronically infected patients and chimpanzees reveals that integrated hepatitis B virus DNA is a source of HBsAg. Sci. Transl. Med. 2017;9:eaan0241. doi: 10.1126/scitranslmed.aan0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Freitas N., Cunha C., Menne S., Gudima S.O. Envelope Proteins Derived from Naturally Integrated Hepatitis B Virus DNA Support Assembly and Release of Infectious Hepatitis Delta Virus Particles. J. Virol. 2014;88:5742–5754. doi: 10.1128/JVI.00430-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Su I.-J., Wang L.H.-C., Hsieh W.-C., Wu H.-C., Teng C.-F., Tsai H.-W., Huang W. The emerging role of hepatitis B virus Pre-S2 deletion mutant proteins in HBV tumorigenesis. J. Biomed. Sci. 2014;21:98. doi: 10.1186/s12929-014-0098-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tong S., Revill P. Overview of hepatitis B viral replication and genetic variability. J. Hepatol. 2016;64:S4–S16. doi: 10.1016/j.jhep.2016.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ma N.-F., Lau S.H., Hu L., Xie D., Wu J., Yang J., Wang Y., Wu M.-C., Fung J., Bai X., et al. COOH-Terminal Truncated HBV X Protein Plays Key Role in Hepatocarcinogenesis. Clin. Cancer Res. 2008;14:5061–5068. doi: 10.1158/1078-0432.CCR-07-5082. [DOI] [PubMed] [Google Scholar]
- 55.Sze K.M.F., Chu G.K.Y., Lee J.M.F., Ng I.O.L. C-terminal truncated hepatitis B virus x protein is associated with metastasis and enhances invasiveness by c-jun/matrix metalloproteinase protein 10 activation in hepatocellular carcinoma. Hepatology. 2013;57:131–139. doi: 10.1002/hep.25979. [DOI] [PubMed] [Google Scholar]
- 56.Slagle B.L., Andrisani O.M., Bouchard M.J., Lee C.G.L., Ou J.-H.J., Siddiqui A. Technical standards for hepatitis B virus X protein (HBx) research. Hepatology. 2015;61:1416–1424. doi: 10.1002/hep.27360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhao L.-H., Liu X., Yan H.-X., Li W.-Y., Zeng X., Yang Y., Zhao J., Liu S.-P., Zhuang X.-H., Lin C., et al. Genomic and oncogenic preference of HBV integration in hepatocellular carcinoma. Nat. Commun. 2016;7:12992. doi: 10.1038/ncomms12992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lindenbach B.D., Rice C.M. Unravelling hepatitis C virus replication from genome to function. Nature. 2005;436:933–938. doi: 10.1038/nature04077. [DOI] [PubMed] [Google Scholar]
- 59.Penin F., Dubuisson J., Rey F.A., Moradpour D., Pawlotsky J.-M. Structural biology of hepatitis C virus. Hepatology. 2004;39:5–19. doi: 10.1002/hep.20032. [DOI] [PubMed] [Google Scholar]
- 60.Ding Q., von Schaewen M., Ploss A. The Impact of Hepatitis C Virus Entry on Viral Tropism. Cell Host Microbe. 2014;16:562–568. doi: 10.1016/j.chom.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rehermann B. Hepatitis C virus versus innate and adaptive immune responses: A tale of coevolution and coexistence. J. Clin. Investig. 2009;119:1745–1754. doi: 10.1172/JCI39133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Atoom A.M., Taylor N.G.A., Russell R.S. The elusive function of the hepatitis C virus p7 protein. Virology. 2014;462–463:377–387. doi: 10.1016/j.virol.2014.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rebouissou S., Nault J.-C. Advances in molecular classification and precision oncology in hepatocellular carcinoma. J. Hepatol. 2020;72:215–229. doi: 10.1016/j.jhep.2019.08.017. [DOI] [PubMed] [Google Scholar]
- 64.Hoshida Y., Nijman S.M.B., Kobayashi M., Chan J.A., Brunet J.-P., Chiang D.Y., Villanueva A., Newell P., Ikeda K., Hashimoto M., et al. Integrative Transcriptome Analysis Reveals Common Molecular Subclasses of Human Hepatocellular Carcinoma. Cancer Res. 2009;69:7385–7392. doi: 10.1158/0008-5472.CAN-09-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pezzuto F., Izzo F., Buonaguro L., Annunziata C., Tatangelo F., Botti G., Buonaguro F.M., Tornesello M.L. Tumor specific mutations in TERT promoter and CTNNB1 gene in hepatitis B and hepatitis C related hepatocellular carcinoma. Oncotarget. 2016;7:54253–54262. doi: 10.18632/oncotarget.9801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bartosch B., Thimme R., Blum H.E., Zoulim F. Hepatitis C virus-induced hepatocarcinogenesis. J. Hepatol. 2009;51:810–820. doi: 10.1016/j.jhep.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 67.Lok A.S., Seeff L.B., Morgan T.R., di Bisceglie A.M., Sterling R.K., Curto T.M., Everson G.T., Lindsay K.L., Lee W.M., Bonkovsky H.L., et al. Incidence of Hepatocellular Carcinoma and Associated Risk Factors in Hepatitis C-Related Advanced Liver Disease. Gastroenterology. 2009;136:138–148. doi: 10.1053/j.gastro.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yeh M.M., Daniel H.D.-J., Torbenson M. Hepatitis C-associated hepatocellular carcinomas in non-cirrhotic livers. Mod. Pathol. 2010;23:276–283. doi: 10.1038/modpathol.2009.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moriya K., Fujie H., Shintani Y., Yotsuyanagi H., Tsutsumi T., Ishibashi K., Matsuura Y., Kimura S., Miyamura T., Koike K. The core protein of hepatitis C virus induces hepatocellular carcinoma in transgenic mice. Nat. Med. 1998;4:1065–1067. doi: 10.1038/2053. [DOI] [PubMed] [Google Scholar]
- 70.Moriishi K., Mochizuki R., Moriya K., Miyamoto H., Mori Y., Abe T., Murata S., Tanaka K., Miyamura T., Suzuki T., et al. Critical role of PA28 in hepatitis C virus-associated steatogenesis and hepatocarcinogenesis. Proc. Natl. Acad. Sci. USA. 2007;104:1661–1666. doi: 10.1073/pnas.0607312104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Roingeard P., Hourioux C. Hepatitis C virus core protein, lipid droplets and steatosis: HCV core, lipid droplets and steatosis. J. Viral Hepat. 2007;15:157–164. doi: 10.1111/j.1365-2893.2007.00953.x. [DOI] [PubMed] [Google Scholar]
- 72.Zemel R., Gerechet S., Greif H., Bachmatove L., Birk Y., Golan-Goldhirsh A., Kunin M., Berdichevsky Y., Benhar I., Tur-Kaspa R. Cell transformation induced by hepatitis C virus NS3 serine protease. J. Viral Hepat. 2001;8:96–102. doi: 10.1046/j.1365-2893.2001.00283.x. [DOI] [PubMed] [Google Scholar]
- 73.Smirnova I., Aksenov N., Vonsky M., Isaguliants M. Different transformation pathways of murine fibroblast NIH 3T3 cells by hepatitis C virus core and NS3 proteins. Cell Biol. Int. 2006;30:915–919. doi: 10.1016/j.cellbi.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 74.Park J.-S., Yang J.M., Min M.-K. Hepatitis C Virus Nonstructural Protein NS4B Transforms NIH3T3 Cells in Cooperation with the Ha-ras Oncogene. Biochem. Biophys. Res. Commun. 2000;267:7. doi: 10.1006/bbrc.1999.1999. [DOI] [PubMed] [Google Scholar]
- 75.Einav S., Sklan E.H., Moon H.M., Gehrig E., Liu P., Hao Y., Lowe A.W., Glenn J.S. The nucleotide binding motif of hepatitis C virus NS4B can mediate cellular transformation and tumor formation without Ha-ras co-transfection. Hepatology. 2008;47:827–835. doi: 10.1002/hep.22108. [DOI] [PubMed] [Google Scholar]
- 76.Park C.-Y., Jun H.-J., Wakita T., Cheong J.H., Hwang S.B. Hepatitis C Virus Nonstructural 4B Protein Modulates Sterol Regulatory Element-binding Protein Signaling via the AKT Pathway. J. Biol. Chem. 2009;284:9237–9246. doi: 10.1074/jbc.M808773200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chung Y.-L., Sheu M.-L., Yen S.-H. Hepatitis C virus NS5A as a potential viral Bcl-2 homologue interacts with Bax and inhibits apoptosis in hepatocellular carcinoma. Int. J. Cancer. 2003;107:65–73. doi: 10.1002/ijc.11303. [DOI] [PubMed] [Google Scholar]
- 78.Mankouri J., Dallas M.L., Hughes M.E., Griffin S.D.C., Macdonald A., Peers C., Harris M. Suppression of a pro-apoptotic K + channel as a mechanism for hepatitis C virus persistence. Proc. Natl. Acad. Sci. USA. 2009;106:15903–15908. doi: 10.1073/pnas.0906798106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mentha N., Clément S., Negro F., Alfaiate D. A review on hepatitis D: From virology to new therapies. J. Adv. Res. 2019;17:3–15. doi: 10.1016/j.jare.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang K.S., Choo Q.L., Weiner A.J., Ou J.H., Najarian R.C., Thayer R.M., Mullenbach G.T., Denniston K.J., Gerin J.L., Houghton M. Structure, sequence and expression of the hepatitis delta (delta) viral genome. Nature. 1986;323:508–514. doi: 10.1038/323508a0. [DOI] [PubMed] [Google Scholar]
- 81.Sureau C., Guerra B., Lanford R.E. Role of the large hepatitis B virus envelope protein in infectivity of the hepatitis delta virion. J. Virol. 1993;67:366–372. doi: 10.1128/JVI.67.1.366-372.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bonino F., Heermann K.H., Rizzetto M., Gerlich W.H. Hepatitis delta virus: Protein composition of delta antigen and its hepatitis B virus-derived envelope. J. Virol. 1986;58:945–950. doi: 10.1128/JVI.58.3.945-950.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lai M.M.C. The Molecular Biology of Hepatitis Delta Virus. Annu. Rev. Biochem. 1995;64:259–286. doi: 10.1146/annurev.bi.64.070195.001355. [DOI] [PubMed] [Google Scholar]
- 84.Weiner A.J., Choo Q.-L., Wang K.-S., Govindarajan S., Houghton’ M. A Single Antigenomic Open Reading Frame of the Hepatitis Delta Virus Encodes the Epitope(s) of Both Hepatitis Delta Antigen Polypeptides p248 and p278. J. Virol. 1988;62:6. doi: 10.1128/JVI.62.2.594-599.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Schaper M., Rodriguez-Frias F., Jardi R., Tabernero D., Homs M., Ruiz G., Quer J., Esteban R., Buti M. Quantitative longitudinal evaluations of hepatitis delta virus RNA and hepatitis B virus DNA shows a dynamic, complex replicative profile in chronic hepatitis B and D. J. Hepatol. 2010;52:7. doi: 10.1016/j.jhep.2009.10.036. [DOI] [PubMed] [Google Scholar]
- 86.Pollicino T., Raffa G., Santantonio T., Gaeta G.B., Iannello G., Alibrandi A., Squadrito G., Cacciola I., Calvi C., Colucci G., et al. Replicative and Transcriptional Activities of Hepatitis B Virus in Patients Coinfected with Hepatitis B and Hepatitis Delta Viruses. J. Virol. 2011;85:8. doi: 10.1128/JVI.01609-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Alfaiate D. HDV RNA replication is associated with HBV repression and interferon-stimulated genes induction in super-infected hepatocytes. Antivir. Res. 2016;136:19–31. doi: 10.1016/j.antiviral.2016.10.006. [DOI] [PubMed] [Google Scholar]
- 88.Fattovich G., Giustina G., Christensen E., Pantalena M., Zagni I., Realdi G., Schalm S.W. Influence of hepatitis delta virus infection on morbidity and mortality in compensated cirrhosis type B. Gut. 2000;46:420–426. doi: 10.1136/gut.46.3.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fattovich G., Boscaro S., Noventa F., Pornaro E., Stenico D., Alberti A., Ruol A., Realdi G. Influence of Hepatitis Delta Virus Infection on Progression to Cirrhosis in Chronic Hepatitis Type B. J. Infect. Dis. 1987;155:931–935. doi: 10.1093/infdis/155.5.931. [DOI] [PubMed] [Google Scholar]
- 90.Romeo R., Ninno E.D., Rumi M., Russo A., Sangiovanni A., Franchis R.D., Ronchi G., Colombo M. A 28-Year Study of the Course of Hepatitis Δ Infection: A Risk Factor for Cirrhosis and Hepatocellular Carcinoma. Gastroenterology. 2009;136:1629–1638. doi: 10.1053/j.gastro.2009.01.052. [DOI] [PubMed] [Google Scholar]
- 91.Niro G.A. Outcome of chronic delta hepatitis in Italy: A long-term cohort study. J. Hepatol. 2010;53:7. doi: 10.1016/j.jhep.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 92.Puigvehí M., Moctezuma-Velázquez C., Villanueva A., Llovet J.M. The oncogenic role of hepatitis delta virus in hepatocellular carcinoma. JHEP Rep. 2019;1:120–130. doi: 10.1016/j.jhepr.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Romeo R., Petruzziello A., Pecheur E.I., Facchetti F., Perbellini R., Galmozzi E., Khan N.U., Di Capua L., Sabatino R., Botti G., et al. Hepatitis delta virus and hepatocellular carcinoma: An update. Epidemiol. Infect. 2018;146:1612–1618. doi: 10.1017/S0950268818001942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Diaz G., Engle R.E., Tice A., Melis M., Montenegro S., Rodriguez-Canales J., Hanson J., Emmert-Buck M.R., Bock K.W., Moore I.N., et al. Molecular Signature and Mechanisms of Hepatitis D Virus–Associated Hepatocellular Carcinoma. Mol. Cancer Res. 2018;16:1406–1419. doi: 10.1158/1541-7786.MCR-18-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chen X., Oidovsambuu O., Liu P., Grosely R., Elazar M., Winn V.D., Fram B., Boa Z., Dai H., Dashtseren B., et al. A novel quantitative microarray antibody capture (Q-MAC) assay identifies an extremely high HDV prevalence amongst HBV infected Mongolians. Hepatology. 2017;66:1739–1749. doi: 10.1002/hep.28957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Candia J., Bayarsaikhan E., Tandon M., Budhu A., Forgues M., Tovuu L.-O., Tudev U., Lack J., Chao A., Chinburen J., et al. The genomic landscape of Mongolian hepatocellular carcinoma. Nat. Commun. 2020;11:4383. doi: 10.1038/s41467-020-18186-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Letouzé E., Shinde J., Renault V., Couchy G., Blanc J.-F., Tubacher E., Bayard Q., Bacq D., Meyer V., Semhoun J., et al. Mutational signatures reveal the dynamic interplay of risk factors and cellular processes during liver tumorigenesis. Nat. Commun. 2017;8:1315. doi: 10.1038/s41467-017-01358-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gouas D., Shi H., Hainaut P. The aflatoxin-induced TP53 mutation at codon 249 (R249S): Biomarker of exposure, early detection and target for therapy. Cancer Lett. 2009;286:29–37. doi: 10.1016/j.canlet.2009.02.057. [DOI] [PubMed] [Google Scholar]
- 99.Kew M.C. Synergistic interaction between aflatoxin B1 and hepatitis B virus in hepatocarcinogenesis. Liver Int. 2003;23:405–409. doi: 10.1111/j.1478-3231.2003.00869.x. [DOI] [PubMed] [Google Scholar]
- 100.Smela M.E., Currier S.S., Bailey E.A., Essigmann J.M. The chemistry and biology of aflatoxin B1: From mutational spectrometry to carcinogenesis. Carcinogenesis. 2001;22:535–545. doi: 10.1093/carcin/22.4.535. [DOI] [PubMed] [Google Scholar]
- 101.Zhang W., He H., Zang M., Wu Q., Zhao H., Lu L., Ma P., Zheng H., Wang N., Zhang Y., et al. Genetic Features of Aflatoxin-Associated Hepatocellular Carcinoma. Gastroenterology. 2017;153:249–262.e2. doi: 10.1053/j.gastro.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 102.Arlt V.M. Aristolochic acid as a probable human cancer hazard in herbal remedies: A review. Mutagenesis. 2002;17:265–277. doi: 10.1093/mutage/17.4.265. [DOI] [PubMed] [Google Scholar]
- 103.Mei N., Arlt V.M., Phillips D.H., Heflich R.H., Chen T. DNA adduct formation and mutation induction by aristolochic acid in rat kidney and liver. Mutat. Res. Fundam. Mol. Mech. Mutagen. 2006;602:83–91. doi: 10.1016/j.mrfmmm.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Poon S.L., Pang S.-T., McPherson J.R., Yu W., Huang K.K., Guan P., Weng W.-H., Siew E.Y., Liu Y., Heng H.L., et al. Genome-Wide Mutational Signatures of Aristolochic Acid and Its Application as a Screening Tool. Sci. Transl. Med. 2013;5:197ra101. doi: 10.1126/scitranslmed.3006086. [DOI] [PubMed] [Google Scholar]
- 105.Chen C., Yang Y., Lin M., Lee C., Tsan Y., Lai M., Yang H., Ho W., Chen P., The Health Data Analysis in Taiwan (hDATa) Research Group Herbal medicine containing aristolochic acid and the risk of hepatocellular carcinoma in patients with hepatitis B virus infection. Int. J. Cancer. 2018;143:1578–1587. doi: 10.1002/ijc.31544. [DOI] [PubMed] [Google Scholar]
- 106.Nault J.-C., Letouzé E. Mutational Processes in Hepatocellular Carcinoma: The Story of Aristolochic Acid. Semin. Liver Dis. 2019;39:334–340. doi: 10.1055/s-0039-1685516. [DOI] [PubMed] [Google Scholar]
- 107.Nault J.-C., Datta S., Imbeaud S., Franconi A., Mallet M., Couchy G., Letouzé E., Pilati C., Verret B., Blanc J.-F., et al. Recurrent AAV2-related insertional mutagenesis in human hepatocellular carcinomas. Nat. Genet. 2015;47:1187–1193. doi: 10.1038/ng.3389. [DOI] [PubMed] [Google Scholar]
- 108.Gonçalves M.A. Adeno-associated virus: From defective virus to effective vector. Virol. J. 2005;2:43. doi: 10.1186/1743-422X-2-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Schultz B.R., Chamberlain J.S. Recombinant Adeno-associated Virus Transduction and Integration. Mol. Ther. 2008;16:1189–1199. doi: 10.1038/mt.2008.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Smith R.H. Adeno-associated virus integration: Virus versus vector. Gene Ther. 2008;15:817–822. doi: 10.1038/gt.2008.55. [DOI] [PubMed] [Google Scholar]
- 111.Boutin S., Monteilhet V., Veron P., Leborgne C., Benveniste O., Montus M.F., Masurier C. Prevalence of Serum IgG and Neutralizing Factors Against Adeno-Associated Virus (AAV) Types 1, 2, 5, 6, 8, and 9 in the Healthy Population: Implications for Gene Therapy Using AAV Vectors. Hum. Gene Ther. 2010;21:704–712. doi: 10.1089/hum.2009.182. [DOI] [PubMed] [Google Scholar]
- 112.Kotterman M.A., Schaffer D.V. Engineering adeno-associated viruses for clinical gene therapy. Nat. Rev. Genet. 2014;15:445–451. doi: 10.1038/nrg3742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gao G., Vandenberghe L.H., Alvira M.R., Lu Y., Calcedo R., Zhou X., Wilson J.M. Clades of Adeno-Associated Viruses Are Widely Disseminated in Human Tissues. JVI. 2004;78:6381–6388. doi: 10.1128/JVI.78.12.6381-6388.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zapatka M., Borozan I., Brewer D.S., Iskar M., Grundhoff A., Alawi M., Desai N., Sültmann H., Moch H., Cooper C.S., et al. The landscape of viral associations in human cancers. Nat. Genet. 2020;52:320–330. doi: 10.1038/s41588-019-0558-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tatsuno K., Midorikawa Y., Takayama T., Yamamoto S., Nagae G., Moriyama M., Nakagawa H., Koike K., Moriya K., Aburatani H. Impact of AAV2 and Hepatitis B Virus Integration Into Genome on Development of Hepatocellular Carcinoma in Patients with Prior Hepatitis B Virus Infection. Clin. Cancer Res. 2019;25:6217–6227. doi: 10.1158/1078-0432.CCR-18-4041. [DOI] [PubMed] [Google Scholar]
- 116.La Bella T., Imbeaud S., Peneau C., Mami I., Datta S., Bayard Q., Caruso S., Hirsch T.Z., Calderaro J., Morcrette G., et al. Adeno-associated virus in the liver: Natural history and consequences in tumour development. Gut. 2020;69:737–747. doi: 10.1136/gutjnl-2019-318281. [DOI] [PubMed] [Google Scholar]
- 117.Logan G.J., Dane A.P., Hallwirth C.V., Smyth C.M., Wilkie E.E., Amaya A.K., Zhu E., Khandekar N., Ginn S.L., Liao S.H.Y., et al. Identification of liver-specific enhancer–promoter activity in the 3′ untranslated region of the wild-type AAV2 genome. Nat. Genet. 2017;49:1267–1273. doi: 10.1038/ng.3893. [DOI] [PubMed] [Google Scholar]
- 118.Nguyen G.N. A long-term study of AAV gene therapy in dogs with hemophilia A identifies clonal expansions of transduced liver cells. Nat. Biotechnol. 2021;39:47–55. doi: 10.1038/s41587-020-0741-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chandler R.J., LaFave M.C., Varshney G.K., Trivedi N.S., Carrillo-Carrasco N., Senac J.S., Wu W., Hoffmann V., Elkahloun A.G., Burgess S.M., et al. Vector design influences hepatic genotoxicity after adeno-associated virus gene therapy. J. Clin. Investig. 2015;125:11. doi: 10.1172/JCI79213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Donsante A., Miller D.G., Li Y., Vogler C., Brunt E.M., Russell D.W., Sands M.S. AAV Vector Integration Sites in Mouse Hepatocellular Carcinoma. Science. 2007;317:477. doi: 10.1126/science.1142658. [DOI] [PubMed] [Google Scholar]
- 121.Nault J.-C. Wild-type AAV Insertions in Hepatocellular Carcinoma Do Not Inform Debate Over Genotoxicity Risk of Vectorized AAV. Mol. Ther. 2016;24:660–661. doi: 10.1038/mt.2016.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.