Abstract
Climate change is negatively impacting the mental health of populations. This scoping review aims to assess the available literature related to climate change and mental health across the World Health Organisation’s (WHO) five global research priorities for protecting human health from climate change. We conducted a scoping review to identify original research studies related to mental health and climate change using online academic databases. We assessed the quality of studies where appropriate assessment tools were available. We identified 120 original studies published between 2001 and 2020. Most studies were quantitative (n = 67), cross-sectional (n = 42), conducted in high-income countries (n = 87), and concerned with the first of the WHO global research priorities—assessing the mental health risks associated with climate change (n = 101). Several climate-related exposures, including heat, humidity, rainfall, drought, wildfires, and floods were associated with psychological distress, worsened mental health, and higher mortality among people with pre-existing mental health conditions, increased psychiatric hospitalisations, and heightened suicide rates. Few studies (n = 19) addressed the other four global research priorities of protecting health from climate change (effective interventions (n = 8); mitigation and adaptation (n = 7); improving decision-support (n = 3); and cost estimations (n = 1)). While climate change and mental health represents a rapidly growing area of research, it needs to accelerate and broaden in scope to respond with evidence-based mitigation and adaptation strategies.
Keywords: global health, climate, mental disorders, environmental health
1. Introduction
In 2009, a Lancet Commission on Climate Change asserted that “climate change is the biggest global health threat of the 21st century” [1]. In response, the ‘Lancet Countdown on health and climate change’ has been established as an independent, global monitoring system dedicated to tracking the health dimensions of the impacts of, and the response to, climate change [2]. While the Lancet Countdown includes numerous health indicators, it currently lacks an indicator capable of capturing the impact of climate change on mental health globally. This lack of representation in global climate and health initiatives is of considerable concern, as mental disorders are a leading cause of burden of disease globally and contribute to increased rates of premature mortality [3].
Climate change is expected to impact mental health via a range of direct and indirect pathways [4]. Direct pathways include exposure to traumatic events, such as bushfires and other severe weather-related events. Indirect pathways largely operate through a range of social, political, and economic determinants of mental health such as poverty, unemployment, and housing. Vulnerable people and places, especially in low-income countries, are anticipated to be particularly badly impacted [4].
Three recent reviews have attempted to synthesise the existing literature on climate change and mental health. Middleton et al., have explored the mental health impacts of climate change among Indigenous Peoples, populations in which climate change impacts are anticipated to be amplified [5]. Hayes et al. conducted a scoping review to explore an important question of how mental health might be integrated into climate change and health vulnerability assessments [6]. Cianconi et al. examined the association between climate change-related events and mental health; however, the review did not assess the quality of these studies [7]. Yet, assessing the quality of studies in such a novel and growing area of research is critical, as it helps identify research gaps and methodological issues that will help formulate recommendations for future studies.
The World Health Organization (WHO) has proposed five global research priorities for protecting human health from climate change: assessing the risks; identifying the most effective interventions; guiding health-promoting mitigation and adaptation decisions in other sectors; improving decision-support; and estimating the costs of protecting health from climate change [8]. Currently, there has only been the assessment of the evidence base across the first of these five research priority areas (assessing the risks).
Building upon existing reviews, this scoping review aims to assess the available literature and explore the key literature gaps, related to climate change and mental health across WHO’s five global research priorities for protecting human health from climate change. This is essential in order to understand the current gaps in the literature and inform future research priorities.
2. Methods
2.1. Scoping Review
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines [9] in conjunction with the PRISMA Extension for Scoping Reviews (PRISMA-ScR) [10]. To identify original research studies related to mental health and climate change, the following online databases were searched from 1 January 2001, to 31 December 2020: PubMed, PsycINFO, EMBASE, CINAHL, Web of Science, and Scopus. The PubMed search string (Box 1) was adapted for each database (search strings for each database can be found in the Appendix A). Whilst acknowledging there are other relevant and broader constructs of mental health, such as ‘emotional wellbeing’, we elected to constrain our search terms to draw a boundary around an otherwise unmanageable number of references. Additional studies were identified by examining the reference lists of key review articles. Three authors (F.C., S.A., and M.P.) independently conducted title/abstract and full-text screening using Endnote X9, and two authors (SA, M.P.) independently extracted data from studies that met the inclusion criteria into a Microsoft Excel sheet. Consensus was sought among these authors throughout this process.
Box 1. PubMed search string.
Search ((((((((((((“Climate Change”[Mesh]) OR “Global Warming”[Mesh]) OR “Global Warming”[tiab]) OR “climate change”[tiab]) OR “Greenhouse Effect”[Mesh]) OR “Greenhouse Effect”[tiab]) OR “Climatic Processes”[Mesh]) OR “Hot Temperature”[Mesh]) OR “Climate”[Mesh]) OR “Weather”[Mesh]) OR “Weather”[tiab])) AND (((((((“Mental Disorders”[Mesh]) OR “Mental Disorders”[tiab]) OR “Mental Disorder”[tiab]) OR “Mental illness”[tiab]) OR “Mental illnesses”[tiab]) OR “Mental Health”[Mesh]) OR “mental health”[tiab])
The inclusion criteria were as follows:
Must relate to mental health and climate change across one or more of the domains defined by the Lancet Countdown for Health and Climate Change 2018 [11]: climate change impacts, exposures, and vulnerability; adaptation, planning, and resilience for health; mitigation actions and health co-benefits; finance and economics; and public and political engagement
Must be original research (e.g., cross-sectional or cohort studies)
Publication year must be from 2001 onwards
English language
Details of the protocol for this review were registered on PROSPERO (registration number CRD42020161076) and can be accessed at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020161076.
2.2. Quality Assessment
The same three authors (F.C., S.A., and M.P.) assessed all studies for which appropriate quality assessment tools were available (n = 93). We used the ‘Observational Cohort and Cross-Sectional Studies’ and ‘Case Series Studies’ Quality Assessment tools from the National Heart, Lung, and Blood Institute (NHLBI) [12]. The NHLBI tools were robustly developed and include individualised tools for a range of study designs (e.g., cohort, cross-sectional, case series). Qualitative studies were assessed using the Critical Appraisal Skills Programme (CASP) Qualitative Checklist [13]. Ecological studies were evaluated using a scale adapted from Cortes-Ramirez et al. [14], with the “sample size” and “validity of statistical inferences” criteria removed as their specificity was not deemed relevant to providing an overall quality assessment of the studies included in the review. We did not assess the quality of studies employing modelling, case report, time-series, case-crossover, panel, or other unique study designs due to the lack of appropriate quality assessment tools.
Studies were assessed as either ‘poor’, ‘fair, or ‘good’, guided by a series of questions set by the quality assessment tools. The findings of ‘poor’ quality studies were excluded from our synthesis of results but can be found listed in Table A1.
2.3. Research Framework
Studies were grouped by a member of the team under the five global research priorities for protecting health from climate change proposed by the World Health Organization: assessing the risks; identifying the most effective interventions; guiding health-promoting mitigation and adaptation decisions in other sectors; improving decision-support; and estimating the costs of protecting health from climate change [8]. Further information about the WHO framework can be found in Appendix A.
2.4. Figure Preparation
The PRISMA flow diagram was prepared using PRISMA2020: R package and ShinyApp for producing PRISMA 2020 compliant flow diagrams (Version 0.0.1) [15]. The world map was created using the rworldmap package (version 1.3-6) [16] in RStudio (version 1.3.1093) [17] with R 4.0.3 [18]. The graph of studies over time was also created in RStudio using ggplot2 (version 3.3.3) [19].
3. Results
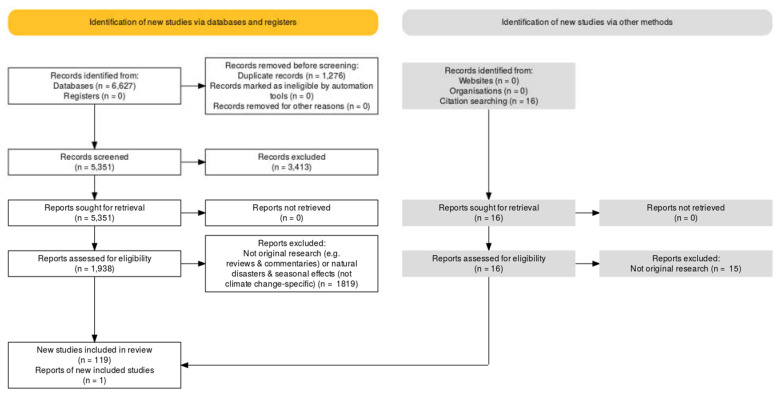
We identified 120 original research studies that examined mental health in the context of climate change-related exposures (Figure 1). Sixty-seven studies reported quantitative data, 34 reported qualitative data, and 19 reported a combination of qualitative and quantitative data. The most common study design was cross-sectional (n = 42), followed by case studies (n = 28), modelling studies (n = 12), ecological studies (n = 7) and cohort studies (n = 7). Table A1 provides a summary of the included studies.
Figure 1.
PRISMA flow diagram of study selection.
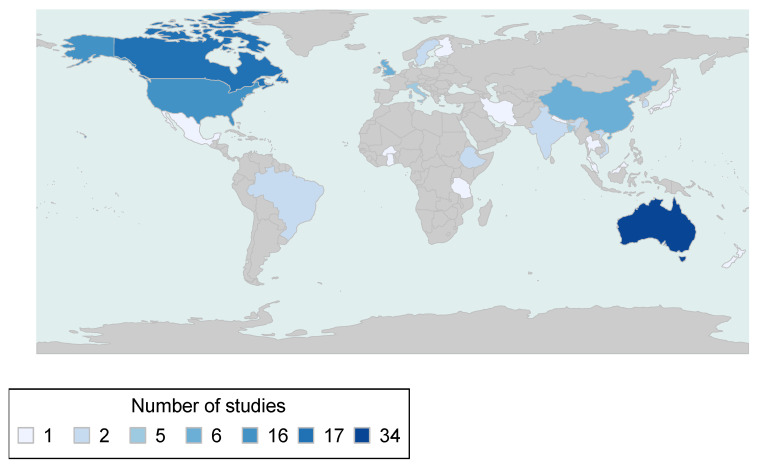
The geographies which represented the most original research studies were Australia (n = 34), Canada (n = 17), USA (n = 16), China (n = 6), United Kingdom (n = 6), Italy (n = 5), and Bangladesh (n = 5) (Figure 2). The majority of studies (77%) were carried out in high-income countries, with 12% from upper middle income, 12% from lower middle income and only 3% from low-income countries (as per World Bank classifications).
Figure 2.
Map of included studies.
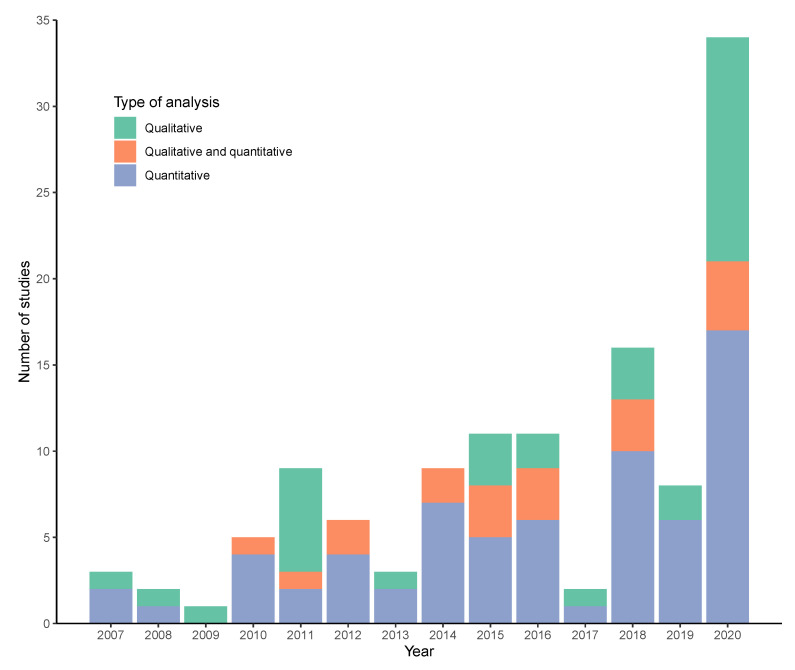
Although we searched for studies from 2001 onwards, we did not identify any published before 2007. There was an overall increasing trend in the number of studies between 2007 and 2020, with the highest number in 2020 (34 studies) (Figure 3).
Figure 3.
Number of studies published over time, by analysis type.
The following sections provide a narrative summary of the original research corresponding to the WHO framework.
3.1. Assessing the Risks
The majority of studies (n = 101 out of 120) examined the mental health risks posed by climate change. The literature linked mental health outcomes to several climate-related exposures—heat, humidity, rainfall, drought, wildfires, and floods. Other environmental exposures, such as tropical cyclones and storms, were not included as no studies were found that explicitly referred to climate change. This section will present studies according to the following three categories (which are not mutually exclusive): (1) environmental exposures; (2) mental health outcomes; and (3) specific sub-groups and contexts that might be particularly vulnerable to the impact of climate change on mental health.
3.2. Environmental Exposures
3.2.1. Temperature and Humidity
The most commonly examined environmental exposure in relation to health risk was temperature (n = 27), which was often measured alongside other meteorological variables such as humidity and rainfall. In most studies, an increase in temperature was positively correlated with poor mental health outcomes.
Three studies from Australia found associations between heat and mental health outcomes; however, the evidence was inconsistent. For example, Ding et al., report that an increase in temperature and humidity affects psychological distress, independently from pre-existing depression or anxiety [20]. Similarly, another study that looked at data from Adelaide, Australia, found that while there was a positive association between temperatures exceeding the maximum and minimum thresholds (32 °C and 16 °C) and psychiatric presentations to the emergency department, there was a significant decrease in this effect when temperatures were considered extreme [21]. A third study conducted on children in Australia showed a small effect of worsened childhood mental health with an increase in annual average daily maximum temperatures [22].
Several studies from Asia found that fluctuating temperatures influenced mental health and well-being, impacting productivity and livelihoods [23,24,25]. Long-term exposure to high and low temperatures in Taiwan resulted in a 7% increase of major depressive disorder incidence per 1 °C increment in regions with an average annual temperature above the median 23 °C. A higher incidence was found in the older age group (65+ years), with a slightly higher hazard ratio for males in this group, and females in the younger age group (20–64 years) [26].
Temperature also affected mental health and well-being in several studies conducted in North America. Noelke et al. reported that temperatures above daily averages reduced positive emotions like happiness, increased negative emotions like anger and stress, and increased fatigue [27]. Another study found that monthly temperatures above 30 °C increased the probability of mental health difficulties by 0.5%, and ongoing exposure to increasing temperatures (1 °C over five years) was associated with a 2% increase in the prevalence of mental health issues [28]. High ambient temperatures were also found to increase help-seeking for mental health, such as crisis text line usage in young adults in several urban areas in the United States [29]. A study exploring protective factors in the context of extreme seasonal weather in Tennessee, USA found that social cohesion was associated with reduced mental health impacts among low- and moderate-income residents [30].
3.2.2. Drought and Rainfall
Drought was another frequently studied climate exposure (n = 16). All but one of the studies were from Australia and primarily focussed on rural communities. Almost half of these studies were based on large, longitudinal studies and utilised standard mental health measures such as the Kessler Psychological Distress Scale (K10). A nationally representative cross-sectional survey of Australian residents found that while drought was associated with elevated psychological distress (as measured by the K10) in rural communities, this was not the case for urban dwellers [31].
A longitudinal cohort study showed elevated drought-related stress and psychological distress (as measured by the K10) among farmers [32]. Drought-related stress, which captures worry about the impacts of drought on themselves and their families and communities, was influenced by socio-demographic and community factors (e.g., loss, government compliance pressures, and difficulties accessing mental health support or receiving inappropriate mental health services) that differed from the factors that influenced psychological distress [33]. Factors associated with higher psychological distress included being unemployed and exposure to other adverse life events, while protective factors included financial security, social support, and a sense of community [32,34]. The evidence for differential impacts on gender and age is conflicting [35,36,37].
One multi-country study has looked at rainfall as a climate-related exposure and has reported that the highest prevalence of mood disorders is observed in countries characterised by small variations across monthly rainfall and high levels of rainfall [38].
3.2.3. Wildfire
Two studies from North America examined the impacts of wildfires on mental health. Qualitative interviews of people purposively sampled to include a broad cross-section of backgrounds and experiences from a severe 2014 wildfire season in the North-West Territories of Canada, in the context of climate change, reported how experiences of evacuation and isolation, as well as feelings of fear, stress, and uncertainty, contributed to acute and long-term negative impacts on mental and emotional well-being [39]. Prolonged smoke events were linked to respiratory problems, extended time indoors, and disruptions to livelihood and land-based activities, which negatively affected mental well-being [39].
A household study conducted one year after the Wallow Fire in Arizona, United States, concluded higher solastalgia, a term used to indicate distress caused by environmental change (measured using a scale adapted from [40]), and an adverse financial impact of the fire was associated with clinically significant psychological distress (as measured by the K10). In contrast, a higher family functioning score was associated with less psychological distress [41]. Other countries that experience regular wildfires, such as Australia, referred to as bushfires, had no research exploring mental health impacts in the context of climate change.
3.2.4. Flood
Several studies examined the mental health impacts of flooding. An Australian study qualitatively explored individuals’ experiences from rural communities, concluding that the threat of drought and flood are intertwined and contributed to decreased well-being from stress, anxiety, loss, and fear [42]. A cohort study from the UK looking at the long-term impact of flooding found psychological morbidity persisted for at least three years after the flooding event [43].
In addition to the tangible mental health impacts related to exposure to specific climate change-related events, studies have reported psychological impacts of perceived risks associated with climate change [44,45].
3.3. Mental Health Outcomes
3.3.1. Symptom Scales and Screening Tools
Symptom scales were commonly used to examine mental health outcomes. Distress (n = 17) was one of the most investigated outcomes; primarily psychological distress measured using the K10. Some studies attempted to develop specific environmental distress measures, including a scale for solastalgia and a specific ‘climate change distress’ scale [41,46,47,48]. Four studies used validated screening tools for mental disorders [39,41,45,46]. Only one study used a structured diagnostic instrument to determine mental disorder diagnoses [49].
3.3.2. Hospital Admissions
Alternatively, many studies utilised routinely collected administrative data. Psychiatric hospital admissions associated with temperature and heat waves were frequently studied (n = 15). These studies demonstrate a positive association, particularly with elevated temperatures, with susceptibility varying in terms of demographic variables (e.g., older people shown to be at higher risk) [50,51] and type of disorder (e.g., organic disorders such as dementia) [52]. The relationship between hospital admissions and heat has been examined for a range of mental and neurological disorders, including dementia, mood disorders, anxiety disorders, schizophrenia, bipolar disorder, somatoform disorders, and disorders of psychological development [52,53,54].
3.3.3. Mortality
Mortality has also been found to be influenced by high ambient temperatures for people living with mental illness and neurological conditions. A study of health outcome data from Adelaide, South Australia, for 1993–2006, has demonstrated that mortality attributed to mental and behavioural disorders increased during heat waves in the 65- to 74-years age group and in persons with psychosis [52,55]. Another European study supports this finding with increased mortality risk for people with psychiatric disorders during heat waves from 2000 to 2008 in Rome and Stockholm, particularly for older people (75+) and women. A study from England found that primary care patients with psychosis, dementia, and alcohol or substance misuse experienced significantly higher heat-related mortality above regionally defined temperature thresholds. This effect was more marked for younger patients and those with a primary diagnosis of alcohol or substance misuse [56,57]. Nitschke et al., found a small increase in mental health-related mortality in people aged 65–74 years during heat waves in metropolitan Adelaide [58]. Projections of mortality under different climate change scenarios in China also estimate increasing trends in heat-related excess mortality for mental disorders but a decreasing trend in cold-related excess mortality [59].
3.3.4. Self-Harm
Temperature has also been associated with self-harm and suicide rates [60,61,62,63,64]. Data from Finland found that temperature variability explained more than 60% of the total suicide variance over several decades [62]. Using data from the US and Mexico, suicide rates were found to increase by 0.7% and 3.1%, respectively, for a 1 °C increase in monthly average temperature, with unmitigated climate change projected to result in a combined 21,770 (95% CI 8950–39,260) additional suicides by 2050 [64].
3.3.5. Burden of Disease
Studies attempting to quantify the burden of mental disorders attributable to climate change are sparse. One study from South Korea has estimated the burden of disease related to climate change for a range of conditions and climate-related measures, including PTSD, as an outcome of disasters [65]. Unfortunately, this study was limited in several ways, including a lack of availability of input data.
3.4. Vulnerable Populations and Life Stages
3.4.1. Pre-existing Mental Illness
We identified a body of research related to populations and contexts that are anticipated to be more vulnerable to climate change and its mental health impacts. People taking certain psychotropic medications (including hypnotics, anxiolytics, and antipsychotics) are at increased risk of heatstroke and death as a result of high temperatures, possibly due to disruptions in thermoregulation triggered by some psychotropic medications [56,66]. One study from Australia showed that people living with obsessive-compulsive disorder (OCD) experience obsessions and compulsions directly aligned with climate change concerns [67].
3.4.2. Youth
According to the results of a national survey of Australian children aged 6–11, higher temperatures may impact children’s mental health [22]. Youth affected by drought may also experience cumulative mental health impacts [68].
3.4.3. Indigenous People
Qualitative studies reporting the unique mental health impacts of climate change on Inuit communities in Canada have described a loss of place-based solace, land-based activities such as hunting, and cultural identity due to changing weather and local landscapes [69,70]. Changes in sea ice stability and surface area are of particular cultural concern for Inuit [71]. Studies among these communities report that climate and environmental changes increase family stress, enhance the possibility of increased drug and alcohol use, amplify previous traumas and mental health stressors, and may increase the risk of suicidal ideation [72]. Indigenous communities from Alaska have also expressed significant concern for climate change and its impacts on local sustenance resources, such as berries [73]. Mental health, physical health, traditional/western education, access to country food and store-bought foods, access to financial resources, social networks, and connection to Inuit identity emerged as key components of Inuit adaptive capacity in the face of climate change [74]. Studies conducted with Aboriginal and Torres Strait Islander peoples from Australia also highlight the environmental impacts of climate change on emotional wellbeing, including increased community distress from deteriorating the connection to country [75,76]. Heat also appeared to be associated with suicide incidence in Australia’s Indigenous populations; however, other socio-demographic factors may play a more critical role than meteorological factors [77].
3.4.4. Low- and Middle-Income Countries
A study from Ethiopia, a low-income country that has a high dependency on the local environment to meet basic human and animal needs, demonstrated that seasonal environmental changes related to water security expose populations to significant emotional distress [78]. Small island developing states in the Pacific Ocean have been deemed to be particularly at risk and vulnerable to the impacts of climate change. Low-lying villages in the Solomon Islands in the South Pacific report that sea-level rise causes fear and worry on a personal and community level [79]. Research from Tuvalu, another small Pacific Island experiencing the threat of sea-level rise, describes the individual experiences of distress in the face of climate change and underscores the necessity to provide access to culturally informed social and mental health services in the region [80]. Three studies from Bangladesh have reported negative effects on emotional well-being as a result of climate-induced immobility [81,82,83].
3.5. Identifying the Most Effective Interventions
There were eight studies related to interventions; however, these were primarily exploratory and qualitative and focused on health professionals and community settings, and did not provide clear support for any one specific intervention.
One study looked at the health and social service responses to the long-term mental health impacts of a flood event. It concluded that sustained recovery interventions rooted in local knowledge and interdisciplinary action were required and that there are unintended consequences related to psychosocial interventions that can incite complex emotions and impact psychosocial recovery [84].
A study from rural Australia has described how a community development model, incorporating elements of health promotion, education, and early intervention, was accepted and considered effective in helping communities build capacity and resilience in the face of chronic drought-related hardship [85]. Unfortunately, this study did not measure the intervention’s impact on the mental health status of participants. Another Australian study that focused on rural health service managers found that 90% of respondents perceived climate change as likely to impact mental health and highlighted the important role of rural health services in education and advocacy on climate change’s health impacts [86]. A case study of health promotion practices that address climate change in Victorian (Australia) healthcare settings found that community gardens improved social connectedness and mental and physical health [87]. Results of a study from Canada revealed the need for improved medical education on climate change and health, including mental health, suggesting that a 3-h education activity would be useful and would allow family physicians to use this knowledge in their daily practice, notably through prevention and counselling [88].
Two studies explored the relationship between pro-environmental behaviour and mental health in terms of awareness of health risks and potential health co-benefits. Results from a survey in China indicated that residents’ health-risk perception is positively affected by climate-change information. Additionally, perceiving climate change as detrimental to mental health was shown to influence a residents’ attitude and intention to take environmental action more than physical health-risk perception [89]. A study of UK households found that while individual-level pro-environmental attitudes were negatively associated with mental health, household pro-environmental behaviours and attitudes of other household members were associated with positive outcomes, pointing towards a role of social capital and the household level as an important target for interventions [90].
Finally, a study exploring health perceptions in climate-driven migrants found that emphasis was placed on the importance of mental health, indicating that mental health interventions could be effective in this population [91].
3.6. Guiding Health-Promoting Mitigation and Adaptation Decisions in Other Sectors
A small number of studies (n = 7) examined how sectors outside of health can mitigate and adapt to reduce climate change impacts on mental health. Three of these studies were from Inuit communities. Social and environmental factors that may protect mental health and wellbeing were highlighted, including being on the land and connecting to Inuit culture, as well as how Inuit-led monitoring of environmental conditions can guide climate change adaptation that considers intangible losses and damages to well-being and ways of living [92,93,94]. A study from Nepal revealed similar themes [95], while a 15-year prospective cohort study of Hurricane Katrina survivors (New Orleans, LA, USA) has concluded that mitigation efforts should prevent trauma exposure through investments in climate resilience and eliminating evacuation impediments [96].
Barriers to implementing strategies to adapt to combat the agricultural impacts of climate change have resulted in negative mental health outcomes among subsistence farmers in Burkina Faso [97]. Barriers comprised financial and time constraints, material and labour shortages, and inaccessible information; however, awareness of climate change was also reported to be limited.
Finally, an exploratory study surveying people affected by widespread public safety power shutoffs (PSPS) to reduce the risk of wildfires in California found that while people were mostly supportive of PSPS as an adaptation measure, it was associated with poorer physical and mental health [98].
3.7. Improving Decision-Support
Very few studies (n = 3) reported issues that could support improved decision-making around mental health and climate change. Between 2010 and 2012, the WHO Division of Pacific Technical Support led a regional climate change and health vulnerability assessment and adaptation planning project in collaboration with health sector partners in 13 Pacific Island countries. Mental health was identified as a high-priority climate-sensitive health risk in eight out of the 13 countries [99]. However, another study found that policy documents on climate change from 12 countries made little or no reference to nine vulnerable groups, including people with mental illness [100].
A study designed to develop and validate indices of adaptation to flooding found that people who perceived a risk of flooding in their home in the next five years adopted more preventative behaviours and adaptation behaviours than those who perceived little or no risk at all. Additionally, people who felt more adverse effects of flooding on their physical or mental health tended to adopt more adaptive behaviours than those who felt little or no adverse effects on their health [101].
3.8. Estimating the Costs of Protecting Health from Climate Change
We did not find any studies that assessed the costs associated with climate change impacts on mental health. However, one study from the United Kingdom found that a social prescribing service for mental health—a service model which supports people to access healthcare resources and psychosocial support, considered to hold potential for reduced cost and carbon-footprint—was associated with reduced financial costs but an increased carbon footprint per patient. However, none of the differences between groups reached statistical significance [102].
3.9. Quality of Studies
Overall, the studies identified in this review were of sound (fair to good) quality. Out of the 93 studies that were quality assessed, 75% were rated good, 23% fair and 2% poor. It is important to note that we found significant variability in how environmental exposures were measured. Among the quantitative studies, we identified two types of approaches to measure exposure to climate-sensitive environmental hazards: (i) self-reported exposures using questionnaires and interviews (note that all qualitative studies used self-reported exposures) and (ii) interpolated exposures using external sources of data.
Fifty-two studies relied on self-reported information to assign a climate change-related exposure to study participants. We found large variability across the survey questions used to capture self-reported exposures, as no standardised questionnaire exists (in contrast to self-reported mental health outcomes) to measure subjective experience regarding climate-sensitive environmental hazards. Specifically, each study in our selected sample used a different question or metric to capture the environmental exposure. Such variability makes the evaluation of the robustness of used tools and the comparison between studies difficult. To the best of our knowledge, we did not identify any self-reported tool regarding the exposures of interest that were validated beforehand.
In addition, 48 studies relied on interpolated exposures using various types of available meteorological data sources. Some studies used meteorological data (mostly precipitation and temperature) from monitoring stations in the area of interest, often retrieved from the national or regional bureau of meteorology or data service centres. Other studies relied on remote sensing data from various satellite products with reanalysis, including the PRISM Climate Group [103] or the Berkeley Earth Surface Temperature Dataset [104]. While some studies used the meteorological variable directly in their analysis, such as daily maximum temperature, others further calculated indices or metrics to define weather events such as drought and heat waves. Most studies used the finest spatial resolution that was available while some used large-scale measurements when assigning exposure to meteorological variables, which may lead to important misclassification biases and impact effect estimates of interest. Indeed, assigning the same exposure to temperature, for example, on a given day to all individuals in a country or region is unlikely to accurately represent individuals’ exposure given well-documented local variations in microclimates [105,106]. We also found differences in the temporal scales that were used across studies. While most studies relied on daily estimates to capture acute effects on mental health outcomes, other studies used monthly or annual estimates to capture chronic impacts, describing various mechanisms such as economic insecurity or migration. Finally, some studies provided limited details regarding data sources and how indices were calculated, making it difficult to understand how exposures were estimated and hindering reproducibility efforts.
4. Discussion
This scoping review is the first to explore the existing original research literature that investigates climate change and mental health using WHO’s global research priorities as a framework [8]. We identified 120 original studies published between 2001 and 2020 that specifically referenced climate change impacts, adaptation, mitigation, and other interventions relevant to mental health. Most studies were quantitative, used a cross-sectional design, were conducted in high-income countries, and were concerned with assessing the mental health risks associated with climate change-related exposures.
The literature consistently points to the negative associations that climate change-related events have with individuals’ and communities’ mental health. Climate change-related events were shown to be associated with psychological distress, worsened mental health (particularly among people with pre-existing mental health conditions), increased psychiatric hospitalisations, higher mortality among people with mental illness, and heightened suicide rates. These results are largely in line with the detrimental impacts that climate change has been shown to have on many other aspects of health [2].
While the overwhelming focus on the mental health risks of climate change is understandable and has generated insight and traction for advocating the importance of considering mental health within climate change, only four studies have focused on protective factors or the coping mechanisms people and communities have used when responding to the detrimental mental health impacts of climate change [26,38,90,105]. An in-depth understanding of which factors constitute ‘resilience’ in the face of climate change would contribute to a more nuanced picture of the associations between climate change and mental health [107] and could be useful when devising programs and policies for those most heavily impacted by climate change.
Additionally, the focus on characterising and quantifying the linkages between climate change and mental health has not been matched by applied research on addressing and reducing these associated mental health risks [8]. Future work should investigate more systematically the possible effectiveness, scalability, and cost-effectiveness of interventions and policies aimed at safeguarding mental health in the face of climate change, including non-mental health interventions. Various health professionals, including nurses [108], emergency department clinicians [109,110], clinical psychologists, and psychiatrists [111,112], have already outlined ways to address mental health problems related to climate change within clinical practice and broader policy, highlighting the strong willingness to act in the medical community. There is also a growing movement of climate advocacy in the health sector, recognising the responsibility to protect the health of current and future generations and calling for meaningful government action [113].
The current review points to some important avenues for future research. As mentioned above, one key research priority is to dissect the association between mental health and climate change by investigating possible mediators and moderators as well as risk, vulnerability, and resilience factors in different populations. A systems-thinking approach, as advocated by Berry et al., might be particularly suitable for this endeavour [114]. This will be aided by more precise operationalization and conceptualization of environmental and mental health variables in the climate change space, another important research priority. Recent work to devise precise measurement instruments for constructs such as climate anxiety [115] represents an important step in this direction. Additionally, in order to move beyond the assessment of risk, other important research priorities relate to understanding how climate change adaptation and mitigation strategies might impact mental health and wellbeing [98] and how engagement in different types of pro-environmental behaviours such as climate activism might impact mental health [116]. A more comprehensive discussion of future directions in climate change and mental health research and practice will be covered in a separate paper by the authors.
The current review has a number of implications for policymakers and intergovernmental organizations such as the World Health Organization. While WHO is increasingly directing its attention to the health impacts of climate change, mental health has generally remained absent from these conversations. For example, as part of the Health and Climate Change Country Profile Project WHO 2019–2020 cycle, WHO reported that only three (i.e., Antigua and Barbuda, United Arab Emirates, and Solomon Islands) out of the 10 recently reviewed countries included mental health and well-being outcomes as part of their climate-sensitive health outcomes monitoring systems [117]. This is in stark contrast with other conditions such as vector-borne and waterborne disease, for which monitoring systems were in place for nine out of the 10 recently reviewed countries. The current review highlights the need for monitoring systems to systematically include mental health as part of their indicators in order to ensure precise monitoring and availability of data at the national level. Additionally, it indicates the importance of including climate change as an important determinant of mental health in policy documentation and action plans, such as in the future extension of the WHO Mental Health Action Plan 2013–2020 [118] to 2030. Importantly, future work might want to explore whether existing WHO documentation and intervention plans for humanitarian settings such as the mhGAP-HIG [119], the Building Back Better framework [120], and scalable psychological interventions [121] are applicable in the context of climate change or whether more specific adaptations are needed. Finally, WHO’s recent work on the integration of mental health and psychosocial support (MHPSS) within disaster risk reduction efforts [122] might represent an important opportunity to integrate climate change within MHPSS.
Palinkas et al. have reviewed the preparedness and response strategies from a mental health services perspective across three areas: (1) acute and extreme weather events; (2) sub-acute or long-term events; and (3) the prospect of long-term and permanent changes, such as an uninhabitable physical environment [122,123]. It is these long-term impacts, in particular, which may demand a shift in attention, as we found only one study which examined the mental health impacts of more general and permanent environmental degradation [124].
A substantial limitation in the surveyed literature concerns the under-representation of research from low- and middle-income countries. The majority of studies identified in this review were conducted in Australia, Canada, and the US. However, evidence indicates that low- and middle-income countries are more at risk of climate change-related events and have fewer resources to respond to these stressors due to pre-existing vulnerabilities [125,126]. For example, according to the Climate Change Vulnerability Index, the five most vulnerable countries in the face of climate change globally in 2016 were Central African Republic, Democratic Republic of Congo, Haiti, Liberia, and South Sudan, all low-income countries considered at “extreme risk” in the face of climate change [127]. These vulnerable regions and populations are among the least responsible for the greenhouse gases that are warming the planet. The concept of climate justice highlights this double inequality of climate change, where there is an inverse distribution between risk and responsibility [128].
A possible limitation of the current study is that the search strategy used means that studies were included only if the authors explicitly linked the climate-related stressor they were considering and climate change. Indeed, a large amount of literature exists concerning the association between disasters and mental health [129] (without explicitly linking an increase in frequency and severity to climate change) which is likely to add value to the field. The geographical origin of the literature reviewed in the current paper is skewed towards high-income countries and unrepresentative of many regions of the world. The reasons for the relative abundance of research in countries such as Australia is worth exploring. Perhaps one reason for an under-representation of research from certain regions is that we only assessed studies in English. The decision to not explore non-English studies was related to our limited resources and capacity combined with the anticipation this extended search would yield limited studies.
It is also important to acknowledge that existing quality assessment tools are largely subjective and not perfectly adapted to the designs of studies included in this review and we were not able to assess the quality of studies employing modelling, case report, time-series, case-crossover, panel, or other unique study designs. Overall, our quality assessments highlight a need for improvement in future research—notably concerning improved measures of environmental exposures and mental health outcomes. For example, assessing the sensitivity and specificity of self-reported tools, for a given context and a given environmental hazard exposure, would be beneficial for assessing the reliability of such tools and allowing comparison across populations and studies.
The increasing number of studies on climate change and mental health parallels the growing traction in the broader field of climate change and health. Since 2007, the academic literature on this topic has tripled and media reports have increased by 78% [130]. However, mental health remains in a secondary position to physical health concerns, reflecting the state of global mental health more generally—despite research advances, the substantial burden of disease attributable to mental disorders has not improved, the quality of mental health services is routinely worse than services for physical health and government investment remains extremely limited [131]. This neglect is apparent in our findings and results in a continued lack of progress in improving the mental health of populations. The inattention to climate change impacts on mental health found in our scoping review echoes that noted by the Lancet Countdown report in 2018 [130]. This report noted that of the 16 national health adaptation strategies reviewed, mental health was the least considered climate-sensitive health outcome (mentioned by five out of 16 national health adaptation strategies).
5. Conclusions
The current scoping review has shown that climate change and mental health represents a rapidly growing area of research; however, it is underdeveloped and will need to accelerate and broaden in scope to respond with evidence-based mitigation and adaptation strategies. Most of the research has been devoted to assessing the mental health risks due to climate change, with less applied research investigating practical issues such as identifying the most effective interventions and policies to safeguard mental health in the face of climate change. Most of the research conducted to date is quantitative, cross-sectional, and conducted in high-income countries—therefore somewhat limiting the interpretability and the generalisability of the findings. Despite these limitations, the existing evidence overwhelmingly points to a negative association between climate change and mental health. Future research should aim at producing more robust and methodologically sound evidence on the link between mental health and climate change while also bearing in mind the importance of investigating what interventions, policies, and decision-making mechanisms can be put in place to mitigate the mental health impacts of climate change. This should represent a key priority in mental health research as, just like with physical health, climate change represents the biggest global threat to mental health of the 21st century [1].
Appendix A
Appendix A.1. Protecting Health from Climate Change—Global Research Priorities from the World Health Organization (WHO 2009)
-
(I)Assessing the risks
- Improved evaluation of current climate-related health risks, rather than a primary focus on risks over very long timeframes
- Identification of vulnerable populations and life stages
- Quantification of the fraction of morbidity and mortality attributable to climate hazards, and to climate change
- Better assessment of neglected climate-mental health linkages
-
(II)Identifying the most effective interventions
- Systematic reviews of the evidence base for interventions
- Methodological research to improve analytical tools for cost-effectiveness analysis
-
(III)Guiding health-promoting mitigation and adaption decisions in other sectors
- Improved methods for assessment of the health implications of decisions in other sectors
- Health implications of climate change mitigation: energy and transport sectors
- Health implications of climate change adaptation: water, food and agriculture sectors
- Improved integration of climate change mitigation, adaptation, and health through “settings-based” research
-
(IV)Improving decision-support
- Research to improve vulnerability and adaptation assessments
- Improvement of operational predictions
- Improved understanding of decision-making processes
-
(V)Estimating the costs of protecting health from climate change
- Definition of harmonized methods to estimate costs and benefits
- Assessment of the health costs of inaction and the costs of adaptation
- Improved economic assessment of the health co-benefits of climate change mitigation
Appendix A.2. Search Strings by Online Database
PsycINFO: (((IndexTermsFilt: (“Atmospheric Conditions”) OR IndexTermsFilt: (“Climate Change”) OR IndexTermsFilt: (“Global Warming”)) OR (title: (“global warming”)) OR (abstract: (“global warming”)) OR (title: (“climate change”)) OR (abstract: (“climate change”)) OR (title: (“greenhouse effect”)) OR (abstract: (“greenhouse effect”)) OR (title: (weather)) OR (abstract: (weather))) AND ((Year: [2001 TO 2019]) AND PublicationTypeFilt: “Peer Reviewed Journal” AND ((PopulationGroupFilt: (“Human”))))) AND (((IndexTermsFilt: (“Mental Disorders”) OR IndexTermsFilt: (“Mental Health”)) OR (title: (“mental disorders”)) OR (abstract: (“mental disorders”)) OR (title: (“mental disorder”)) OR (abstract: (“mental disorder”)) OR (title: (“mental illness”)) OR (abstract: (“mental illness”)) OR (title: (“mental illnesses”)) OR (abstract: (“mental illnesses”)) OR (title: (“mental health”)) OR (abstract: (“mental health”))) AND ((Year: [2001 TO 2020]) AND PublicationTypeFilt: “Peer Reviewed Journal” AND ((PopulationGroupFilt: (“Human”)))))
EMBASE: (‘climate’/exp OR ‘greenhouse effect’/exp OR ‘weather’/exp OR ‘high temperature’/exp OR ‘climate change’:ab,ti OR ‘global warming’:ab,ti OR ‘greenhouse effect’:ab,ti OR ‘weather’:ab,ti) AND (‘mental disease’/exp OR ‘mental health’/exp OR ‘mental disorders’:ab,ti OR ‘mental disorder’:ab,ti OR ‘mental illness’:ab,ti OR ‘mental illnesses’:ab,ti OR ‘mental health’:ab,ti) AND [english]/lim AND [embase]/lim NOT [medline]/lim AND [2001–2020]/py
Web of Science: TS=(global warming OR climate change OR greenhouse effect OR weather) AND TS=(mental disorder OR mental disorders OR mental illness OR mental illnesses OR mental health) AND LANGUAGE: (English) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=2001–2020
Scopus: ((TITLE-ABS-KEY (“climate change”) OR TITLE-ABS-KEY (“global warming”) OR TITLE-ABS-KEY (“greenhouse effect”) OR TITLE-ABS-KEY (weather) AND (( TITLE-ABS-KEY (“mental disorder”) OR TITLE-ABS-KEY (“mental illness”) OR TITLE-ABS-KEY (“mental health”)) AND PUBYEAR > 2000 AND PUBYEAR < 2021)
CINAHL: (MH “Weather+”) OR (MH “Climate+”) OR TI(“climate change” or “global warming” or “greenhouse effect” or weather) OR AB(“climate change” or “global warming” or “greenhouse effect” or weather) AND (MM “Mental Health”) OR (MH “Behavioral and Mental Disorders+”) OR TI (“mental disorders” or “mental disorder” or “mental health” or “mental illness” OR “mental illnesses”) OR AB (“mental disorders” or “mental disorder” or “mental health” or “mental illness” OR “mental illnesses”) Limiters - Published Date: 20010101-20201231; English Language; Peer Reviewed; Exclude MEDLINE records
Table A1.
Summary of original research (N = 120).
| Assessing the Risks (n = 101) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Exposure | Quality Rating | |
| Acharibasam and Anuga 2018 | Ghana | NR | Cross-sectional | Farmers from three districts in Northern Ghana | 180 | Emotional regulation practices (given psychological distance i.e., geographical, social) | Self-reported exposure to excessive heat, declined rainfall, prolonged drought, excessive floods, and strong wind using questionnaires | Fair | |
| Aguglia, Serafini et al., 2020 | Italy | 2013–2015 | Cross-sectional | Psychiatric patients in Turin | 730 | Involuntary admissions | Interpolated exposure using daily meteorological data on wind, temperature, humidity, barometric pressure, solar radiation, rain, and hours of sunshine from Italian Meteorology’s Climate Data Service of Physics Department of the University of Turin | Good | |
| Albrecht, Sartore et al., 2007 | Australia | 2003–2006 | Cross-sectional | Residents of the Upper Hunter region of NSW and rural NSW | 60 | Solastalgia and environmental distress | Self-reported exposure to drought and mining using interviews, focus groups, and surveys | Fair | |
| Allen 2020 | USA | NR | Cross-sectional | Social workers in Alaska | 159 | Social workers’ attitudes about climate change and perceptions of the effects of climate change on their clients | Self-reported exposure to climate change using surveys | Poor | |
| Anderson 2009 | Australia | 2004–2007 | Phenomenological | Women health workers from Mallee, Victoria | 2 | How drought and climate change impact rural mental health, and how discourse of endurance and uncertainty can exacerbate problems in rural social work. | Self-reported exposure to drought using oral histories | Good | |
| Asugeni, MacLaren et al., 2015 | Solomon Islands | NR | Cross-sectional | Residents of six remote villages in East Malaita | 57 | Mental health | Self-reported exposure to sea-level rise using questionnaires | Good | |
| Austin, Handley et al., 2018 | Australia | 2007–2013 | Cohort | Farmers in NSW | 664 | Concerns about climate change | Self-reported exposure to climate change using surveys | Good | |
| Austin, Rich et al., 2020 | Australia | 2007–2013 | Cohort | Rural residents in NSW | 823 | Personal drought-related stress (PDS), community drought-related stress (CDS), and general psychological distress (K10) | Interpolated exposure using monthly meteorological data on rainfall to assess drought conditions | Good | |
| Ayeb-Karlsson, Kniveton et al., 2020 | Bangladesh | 2014–2015 | Mixed-method: Q-methodology and discourse analysis | Residents of Bhola Slum, Dhaka | 62 | Wellbeing and immobility | Self-reported exposure to climate-induced noneconomic losses using storytelling methodology | N/A | |
| Ayeb-Karlsson 2020 | Bangladesh | 2014–2016 | Case study | Residents of Bhola Slum, Dhaka | 140 | Immobility decision-making and wellbeing | Self-reported exposure to climate-induced immobility using Q-based discourse analysis | Fair | |
| Ayeb-Karlsson 2020 | Bangladesh | 2014–2016 | Case study | Residents of three coastal cyclone affected study sites of Bangladesh (Dalbanga South, Mazer Char and Gabtola). | 280 | Emotional fear and mental trauma | Self-reported exposure to climate-induced immobility using Q-based discourse analysis | Fair | |
| Berry and Peel 2015 | Australia | 2013 | Cross-sectional | Residents of regional and rural Australia (all states except Tasmania) | 6674 | Psychological distress (K10), emotional well-being (life satisfaction, happiness, and optimism), CC attitudes (belief, worry, distrust) | Self-reported exposure to climate change using surveys | Good | |
| Billiot 2018 | USA | NR | Cross-sectional | Indigenous community in South Louisiana | 160 | Health (physical, emotional, mental) | Self-reported exposure to environmental changes (including foul smelling air, noise, heavy vehicle movement, pollution, heritage destruction, soil erosion, loss of native fisheries) using surveys | Good | |
| Bryan, Ward et al., 2020 | United Kingdom | NR | Case study | Community members of seven different river catchments | 41 | Health and well-being | Self-reported exposure to drought using semi-structured and narrative interviews | Good | |
| Bunce 2016 | Canada | 2015 | Case study | Inuit women in Iqaluit, Nunavut | 42 | Vulnerability and adaptive capacity | Self-reported exposure to climate change using interviews and focus groups | Good | |
| Burke, González et al., 2018 | USA and Mexico | USA 1968–2004 Mexico1990–2010 |
Modelling | Populations of USA and Mexico | USA = 851,088; Mexico = 611,366 | Suicide rates and depressive language | Interpolated exposure using gridded (4 × 4 km) daily meteorological data, from <10,000 weather stations, on temperature and precipitation from PRISM for the US; gridded daily (Berkeley Earth Surface Temperature Dataset) and monthly (Temperature and Precipitation: 1900–2010 Gridded Monthly Time Series Version 3.02, University of Delaware) temperature and precipitation data for Mexico | N/A | |
| Carleton 2017 | India | 1967–2013 | Modelling | Population of India | 1472 deaths per 100,000 | Suicide rates | Interpolated exposure using gridded (1 × 1 degree) daily meteorological data on temperature from the National Center for Environmental Prediction and gridded (0.5 × 0.5 degree) monthly cumulative precipitation data from the University of Delaware | N/A | |
| Carlsen, Oudin et al., 2019 | Sweden | 2012–2017 | Case-crossover | Residents of Gothenburg | 84,230 | Daily psychiatric emergency visits | Interpolated exposure using daily meteorological data, from an urban background measuring station, on temperature from the Swedish Meteorological and Hydrological Institute data repository | N/A | |
| Carnie, Berry et al., 2011 | Australia | 2008–2009 | Case study | Young people, teachers, and service providers in rural drought-affected NSW | 96 | Mental health | Self-reported exposure to drought using consultative forums | Good | |
| Chan, Lam et al., 2018 | Hong Kong | 2002–2011 | Ecological | Public hospital admissions | N/A | Mental-disorder hospitalisation | Interpolated exposure using daily meteorological data, from a monitoring station near the centre of Hong Kong, on temperature and humidity from the Hong Kong Observatory and daily average level of air pollutants, from all general air quality monitoring stations except one rural location, from the Environmental Protection Department of Hong Kong | Good | |
| Chen, Lin et al., 2019 | Taiwan | 2003–2013 | Cohort | Taiwan health insurance beneficiaries | 945,171 | MDD diagnosis | Interpolated exposure using daily meteorological data, from the weather monitoring station nearest the residential township of subjects, on temperature, sunshine duration, and precipitation from the Taiwan Central Weather Bureau | Good | |
| Cooper, Hutchings et al., 2019 | Ethiopia | 2017–2018 | Cross-sectional | Members of three villages in Afar region: Eger, Tirtira, Adkonta | 36 | Emotional wellbeing | Self-reported exposure to water insecurity using focus groups and interviews | Good | |
| Cunsolo Willox, Harper et al., 2012 | Canada | 2009–2010 | Case study | Residents of the Inuit community of Rigolet, Nunatsiavut | 112 | Lived experiences of ecological grief and loss | Self-reported exposure to caribou decline using interviews | Good | |
| Cunsolo Willox, Harper et al., 2013 | Canada | 2010 | Case study | Residents of the Inuit community of Rigolet, Nunatsiavut, community-based health workers and Nunatsiavut Government health professionals | 67 | Sense of place, health, and well-being | Self-reported exposure to climate change using interviews | Good | |
| Cunsolo, Borish et al., 2020 | Canada | NR | Case study | Inuit from the Nunatsiavut and NunatuKavut regions | 105 | Mental health and well-being | Self-reported exposure to climate change using interviews | Good | |
| Dean and Stain 2010 | Australia | 2007 | Cross-sectional | Adolescents (aged 11–17) from five schools in rural NSW | 111 | Emotional well-being (Strengths and Difficulties Questionnaire) and perceived impacts of drought (Drought and Community Survey for Children) | Self-reported exposure to drought using focus groups and surveys | Fair | |
| Di Giorgi, Michielin et al., 2020 | Italy | NR | Cross-sectional | Migrants from African countries with extreme and high vulnerability to climate change in Northern Italy | 100 | Perception of climate change, loss of social capital, and mental health (depressive and anxiety symptoms) | Self-reported exposure to climate change using interviews | Fair | |
| Di Nicola, Mazza et al., 2020 | Italy | 2016–2019 | Cross-sectional | Euthymic bipolar patients in Rome | 704 (352 bipolar subjects, 352 healthy controls) | Weather sensitivity (assessed using METEO-Questionnaire) and its relationship to suicide attempts | Self-reported exposure to weather and climate variation using questionnaires | Good | |
| Ding, Berry et al., 2016 | Australia | 2006–2008 | Cross-sectional | Residents of NSW aged 45+ | 53,144 | Psychological distress (K10) and having been treated for depression or anxiety | Interpolated exposure using gridded (5 × 5 km) daily meteorological data, based on in situ observations and topography-resolving analysis, on temperature and vapour pressure (to approximate humidity) from the Australian Bureau of Meteorology | Good | |
| Dodd, Scott et al., 2018 | Canada | 2015 | Phenomenological | Residents of four Northwest Territories communities | 30 | Mental and emotional well-being, physical health, and livelihoods | Self-reported exposure to wildfires using interviews | Good | |
| du Bray 2018 | USA, Fiji, Cyprus, New Zealand, England | 2014 | Ethnography | Biophysically vulnerable communities in the US (Mobile, Alabama; Kodiak, Alaska; Phoenix, Arizona), Fiji (Viti Levu), Cyprus (Nicosia), New Zealand (Wellington), England (London | Total: 375 (USA: 103 Fiji: 68 Cyprus: 40 New Zealand: 86 London: 78) |
Emotional impacts | Self-reported exposure to climate change using interviews and surveys | Good | |
| Durkalec, Furgal et al., 2015 | Canada | 2010–2011 | Case study | Residents of the Inuit community of Nain, Nunatsiavut | 22 | Health | Self-reported exposure to sea ice using focus groups and interviews | Good | |
| Eisenman, McCaffrey et al., 2015 | USA | 2012 | Cross-sectional | Residents of five communities affected by the Wallow Fire in Arizona | 416 | Psychological distress (K10) and solastalgia | Self-reported exposure to wildfires using surveys | Good | |
| Ellis and Albrecht 2017 | Australia | 2013–2014 | Case study | Family farmers in Newdegate, WA | 22 | Place-related mental health and wellbeing | Self-reported exposure to climate change using interviews | Good | |
| Farrokhi, Khankeh et al., 2020 | Iran | 2018–2019 | Case study | Not specified | 33 | Self-reported emotional and mood effects | Self-reported climate change risk perception using interviews | Fair | |
| Fearnley, Magalhaes et al., 2014 | Australia | 2006–2008 | Cross-sectional | Women in south-west WA | 879 | Mental health component scores | Interpolated exposure using environmental data, based on proportional mapping, on dryland salinity from the Western Australian Department of Agriculture’s soil and landscape mapping database, and gridded (5 × 5 km) land surface temperature and normalised difference vegetation index (proxy for rainfall) from the National Oceanographic and Atmospheric Administration’s (NOAA) Advanced Very High Radiometer | Good | |
| Fischer and Van de Vliert 2011 | Global | N/A | Modelling | Nonclinical adult populations | N/A | Indicators of general health complaints, burnout, state and trait anxiety, and depression | Interpolated exposure; monthly temperature deviations calculated at the country level but data source not provided. | N/A | |
| Flint, Robinson et al., 2011 | USA | 2008–2010 | Participatory research | Residents of three remote Alaska Native communities | Interviews: 65 Surveys: 116 |
Perceived health status and impacts of berries, measured health benefits of berries, perceived environmental and community wellness | Self-reported exposure to environmental changes using interviews, focus groups, and surveys | Good | |
| Friel, Berry et al., 2014 | Australia | 2007–2008 | Cross-sectional | Nationally representative sample of Australian residents aged 15 years and over | 5012 | Psychological distress (K10) and three indicative measures of food insecurity | Interpolated exposure using gridded (0.25 degree) monthly meteorological data on rainfall (used to calculate Hutchinson Drought Indices) from the Australian Bureau of Meteorology | Good | |
| Fuentes, Asselin et al., 2020 | Canada | 2016 | Cross-sectional | Members of four Indigenous communities in the eastern Canadian boreal forest | 251 | Environmental distress (using questionnaire based on the Environmental Distress Scale (EDS) and the Connor–Davidson Resilience Scale (CD-RISC-10)) | Self-reported exposure to environmental changes using questionnaires | Good | |
| Gibson, Haslam et al., 2019 | Tuvalu | 2015 | Case study | Residents of Tuvalu and key informants | 39 | Psychological distress and associated impairment | Self-reported exposure to climate change using interviews | Good | |
| Gibson, Barnett et al., 2020 | Tuvalu | 2016 | Cross-sectional | Tuvaluan residents in Funafuti | 100 | Determinants and idioms of distress and culturally prescribed responses to coping with distress | Self-reported exposure to climate change using interviews | Fair | |
| Gu, Zhang et al., 2020 | China | 2009–2018 | Modelling | Residents in Ningo, China | 372,027 | Mortality | Interpolated exposure using daily meteorological data, from Yinzhou station (Lat. 29.79 N, Long. 121.55 E; the only national basic weather monitoring station in the central urban area of Ningbo) on temperature and humidity from the Ningbo Meteorological Bureau | N/A | |
| Hanigan, Schirmer et al., 2018 | Australia | 2015 | Cross-sectional | Adults living in rural areas in Victoria | 5312 | Psychological distress (K10) | Interpolated exposure using monthly meteorological data on rainfall (used to calculate Hutchinson Drought Indices) from the Australian Bureau of Meteorology | Good | |
| Hansen, Bi et al., 2008 | Australia | 1993–2006 | Ecological | Residents of Adelaide metropolitan area | 171,614 | Hospital admissions and mortality attributed to mental, behavioural, and cognitive disorders | Interpolated exposure using daily meteorological data, from a central city weather station, on temperature from the Australian Bureau of Meteorology | Good | |
| Helama, Holopainen et al., 2013 | Finland | 1751–2008 | Modelling | Finnish population | 94,356 | Suicide | Interpolated exposure using meteorological data on temperature from the Uppsala temperature record [Department of Meteorology, Uppsala University] | N/A | |
| Helm, Pollitt et al., 2018 | USA | NR | Cross-sectional | Adults who have at least one child | 342 | Depressive symptoms and pro-environmental behaviours | Self-reported exposure to environmental concern using surveys | Fair | |
| Hoffmann, Oliveira et al., 2016 | Brazil | 2014 | Case report | Individual patient with schizophrenia on clozapine treatment | 1 | Heat stroke | Not applicable | N/A | |
| Howard, Ahmed et al., 2020 | USA | 2017 | Cross-sectional | Farmers and ranchers in Montana | 125 | Climate risk perception and mental well-being, including climate-related anxiety | Self-reported exposure to climate change using surveys | Fair | |
| Jones, Wootton et al., 2012 | Australia | 2008–2009 | Cross-sectional | Patients with OCD checking subtype in Sydney | 50 | OCD symptoms | Self-reported exposure to climate change using clinical interviews | Fair | |
| Kabir 2018 | Bangladesh | 2015–2016 | Case study | Residents and health professionals in the Hill-Tracts region | 125 | Psychological health and well-being | Self-reported exposure to climate change using interviews | Fair | |
| Khalaj, Lloyd et al., 2010 | Australia | 1998–2006 | Case-only | Residents of Sydney East and West, Illawarra, Gosford-Wyong, and Newcastle | 1,497,655 | Emergency hospital admissions and underlying conditions | Interpolated exposure using daily meteorological data, from a monitoring station in each of the five regions of interest, on temperature (used to examine extreme heat) from the NSW Bureau of Meteorology | N/A | |
| Kim, Lim et al., 2015 | South Korea | 1992–2009 | Modelling | Residents of Seoul | 271,633 | Mortality (relative risks and attributable deaths) | Interpolated exposure using daily meteorological data, from the representative synoptic surface observation station in Seoul, on humidity, air pressure, and temperature from the Korea Meteorological Administration | N/A | |
| Li, Ferreira et al., 2020 | USA | 1993–2010 | Cross-sectional | USA adult population | 3,060,158 | Self-reported mental health | Interpolated exposure using gridded (4 × 4 km) daily meteorological data on temperature and precipitation from PRISM | Good | |
| Lindvall, Kinsman et al., 2020 | Somalia, Kenya and Ethiopia | 2018 | Case study | Stakeholders from different disciplines (climate, weather, environment, migration, and public health) and agencies (national, regional, and local; governmental, non-governmental, and UN) | 39 | Health and health care access | Self-reported exposure to drought-related migration using interviews | Good | |
| Liu, Liu et al., 2018 | China | 2010 | Case-crossover | Residents of Jinan | 19,569 | Daily hospital visits for mental illness | Interpolated exposure using daily meteorological data on temperature (used to define heatwave events), humidity, wind, and air pressure from the China Meteorological Data Sharing Service System | N/A | |
| Mason, Erwin et al., 2018 | USA | 2016 | Cross-sectional | Primarily low- and moderate-income residents of Knoxville, Tennessee | 424 | Self-reported mental health and potential mediating factors including feeling prepared for extreme weather, general health, income, social cohesion, and concern about climate change | Self-reported exposure to summer heat waves and extreme winter weather using surveys | Fair | |
| Mason, Sharma et al., 2020 | USA | 2016 | Cross-sectional | Low- to middle-income adults of different racial groups in Knoxville, Tennessee | 426 | Physical and mental health, associations with human, financial, physical, and social capital | Self-reported exposure to summer heat waves and extreme winter weather using surveys | Fair | |
| Mayner, Arbon et al., 2010 | Australia | 2009 | Cross-sectional | Emergency department patients in Adelaide | 9244 | ED patient presentations | Interpolated exposure using meteorological data in Adelaide was used to define two types of heat waves events (Australian Bureau of Meteorology criterion) | Good | |
| McNamara and Westoby 2011 | Australia | 2009–2010 | Case study | Aunties (respected older women) living on Erub Island, Torres Strait | 4 | Emotional, cultural, psycho-social impacts | Self-reported exposure to climate change using interviews | Good | |
| Middleton, Cunsolo et al., 2020 | Canada | 2012–2013 | Case study | Inuit community members and health professionals in Nunatsiavut | 116 | Mental health and wellness | Self-reported exposure to changing weather and seasonal patterns using interviews | Good | |
| Mulchandani, Armstrong et al., 2020 | England | 2015–2017 | Cohort | People living in neighbourhoods affected by flooding in the south of England between 1 December 2013, and 31 March 2014 | 819 | Depression, anxiety, and PTSD | Self-reported exposure to flooding using questionnaires | Good | |
| Ng, Wilson et al., 2015 | Australia | NR | Case study | Adults living in four rural communities in NSW | 46 | Wellbeing | Self-reported exposure to flood and drought using interviews and focus groups | Good | |
| Nitschke, Tucker et al., 2007 | Australia | 1993–2006 | Case-series | Residents of Adelaide metropolitan area | N/A | Ambulance transports, hospital admissions, and mortality | Interpolated exposure using daily meteorological data, from Kent Town station, on temperature (used to define heatwave events) from the Australian Bureau of Meteorology | Good | |
| Niu, Gao et al., 2020 | China | 2016–2018 | Time-series | Patients with mental disorders residing in Beijing | 16,606 | Daily emergency visits related to mental disorders | Interpolated exposure using daily meteorological data, from three fixed-site stations in Beijing, on temperature, humidity, duration of sunshine, barometric pressure, precipitation, and wind from the China Meteorological Data Service Center | N/A | |
| Noelke, McGovern et al., 2016 | USA | 2008–2013 | Cross-sectional | Population aged 18+ | 1,900,000 | Emotional well-being | Interpolated exposure using gridded (0.125 × 0.125 degree) daily meteorological data on temperature from the North American Land Data Assimilation System | Good | |
| Obradovich, Migliorini et al., 2018 | USA | 2002–2012 | Cross-sectional | USA residents | 1,961,743 | Mental health difficulties | Interpolated exposure using gridded (4 × 4 km) daily meteorological data on temperature and precipitation from PRISM, and average daily data on cloud cover, humidity, and wind from the National Centers for Environmental Prediction Reanalysis II project | Good | |
| OBrien, Berry et al., 2014 | Australia | 2007–2008 | Cross-sectional | Nationally representative sample of Australian residents aged 15 years and over | 5012 | Psychological distress (K10) | Interpolated exposure using daily meteorological data on rainfall (used to calculate Hutchinson Drought Indices) from the Australian Bureau of Meteorology | Good | |
| Ogunbode, Böhm et al., 2019 | United Kingdom | 2013–2014 | Cross-sectional | British sample (this study only used a sub-sample of a larger questionnaire. They only used individuals who indicated that they had been personally affected a little, a fair amount, or a great deal by the 2013/2014 UK winter flooding | 821 | Negative emotions and mitigation intention | Self-reported exposure to flooding using surveys | Good | |
| Oudin Astrom, Schifano et al., 2015 | Italy and Sweden | 2000–2008 | Cohort | Residents of Rome and Stockholm aged 50 years or older | 110,531 | Mortality | Interpolated exposure using daily meteorological data, from the airport station closest to the city in Rome and the station at Bromma City aiport in Stockholm, on temperature (used to define heatwave events) | Good | |
| Page, Hajat et al., 2012 | England | 1998–2007 | Cohort | Patients with primary diagnoses of psychosis, dementia, alcohol misuse, and other substance misuse | 22,562 | Mortality | Interpolated exposure using daily meteorological data, from all monitoring stations in England, on temperature from the British Atmospheric Data Centre | Good | |
| Pailler and Tsaneva 2018 | India | 2003 & 2007 | Cross-sectional | Sample of 8468 from World Health Survey (WHS) in 2003 and 7759 from 2007 Study on global AGEing and adult health (SAGE) | 16,227 | Depression; stress (cognitive and sleep difficulties, ability to cope); agency (control) | Interpolated exposure using gridded (0.5 × 0.5 degree) monthly meteorological data on temperature and precipitation (used to define weather extremes) from the Matsurra & Willmott ‘Terrestrial air temperature and precipitation: Monthly and annual time series (1950–1999)’ | Good | |
| Polain, Berry et al., 2011 | Australia | 2008 | Case study | Older farmers in NSW | 152 | Mental health | Self-reported exposure to drought using consultative forums | Good | |
| Powers, Dobson et al., 2015 | Australia | 1996–2008 | Cohort | Women living in rural Australia | 6664 | Mental Health Index scores (from the Medical Outcomes Study Short Form 36-SF36) | Interpolated exposure; the Hutchinson Drought Index was used but data source not provided. | Good | |
| Powers, Loxton et al., 2012 | Australia | 2004 | Cross-sectional | Women living outside major cities | 6584 | SF-36 General Health (GH) and Mental Health (MH) scores, and perceived stress | Interpolated exposure to Exceptional Circumstances declared area using the 2004 survey with latitude and longitude declared areas in the same year for each participant. | Good | |
| Preti, Lentini et al., 2007 | Italy | 1974–2003 | Modelling | Italians | 97,693 | Suicide | Interpolated exposure using monthly meteorological data on temperature anomalies from the Istituto di Scienze dell’Atmosfera e del Clima (Institute of Atmospheric Sciences and Climate) | N/A | |
| Proverbs, Lantz et al., 2020 | Canada | 2017 | Case study | Members of four Gwich’in First Nation communities in the Northwest Territories | 29 | Well-being | Self-reported exposure to access to fish using interviews | Good | |
| Qi, Hu et al., 2014 | Australia | 1986–2005 | Modelling | Population of Australia | 45,293 | Suicide rates | Interpolated exposure using monthly meteorological data, from monitoring stations in each Local Government Area, on rainfall, humidity, and temperature from the Australian Bureau of Meteorology | N/A | |
| Rahman, Mohamad et al., 2014 | Malaysia | 2012 | Cross-sectional | University students in Malaysia | 200 | Perceived awareness and perceived physical and psychological impact | Self-reported exposure to climate change using surveys | Good | |
| Rigby, Rosen et al., 2011 | Australia | 2008 | Case study | Aboriginal communities in NSW | 166 | Social and emotional well-being, and possible adaptive strategies | Self-reported exposure to drought using consultative forums | Good | |
| Rotge, Fossati et al., 2014 | Global | 2001–2005 | Ecological | Populations of 17 countries: Belgium, Colombia, France, Germany, Israel, Italy, Japan, Lebanon, Mexico, Netherlands, New Zealand, Nigeria, PR China, South Africa, Spain, Ukraine, United States | 85,052 | Lifetime prevalence of mood disorders | Interpolated exposure using monthly meteorological data on temperature and rainfall from the World Bank Group | Fair | |
| Sartore, Kelly et al., 2008 | Australia | NR | Case study | Two rural communities in NSW | 39 | Emotional and social wellbeing | Self-reported exposure to drought using focus groups | Good | |
| Searle and Gow 2010 | Australia | 2008 | Cross-sectional | University students and members of the general public in Queensland | 275 | Climate change distress; environmental beliefs (NEP); depression, anxiety, and stress (DASS-21); future anxiety (FAS3); intolerance of uncertainty (IUS-12); religiosity (SCSRFQ-SF) | Self-reported exposure to climate change using questionnaires | Good | |
| Sim, Kim et al., 2020 | Japan | 1972–2015 | Time-series | Population of Japan | 1,067,333 | Suicide | Interpolated exposure using daily meteorological data, from a weather station in the capital city of each prefecture, on temperature and humidity from the Japan Meteorology Agency | N/A | |
| Stain, Kelly et al., 2011 | Australia | 2006–2009 | Cross-sectional | Adults living in rural NSW | 302 | Psychological distress (K10) and an index of concern or worry about drought | Interpolated exposure using gridded (0.25 degree) monthly meteorological data on rainfall (used to calculate drought exposure) from the Australian Bureau of Meteorology | Good | |
| Sugg, Dixon et al., 2019 | USA | 2013–2017 | Time-series | Adolescents and young adults in Atlanta, Georgia; Chicago, Illinois; Los Angeles, California, and New York City; New York. | 59,000 | Crisis support-seeking behaviour | Interpolated exposure using daily meteorological data, from the following international airport weather stations: Atlanta Hartsfield, Chicago O’Hare, LaGuardia, and Los Angeles, on temperature from the Applied Climate Information System available from and maintained by the National Oceanic and Atmospheric Administration’s Regional Climate Centers | N/A | |
| Tasdik Hasan, Adhikary et al., 2020 | Bangladesh | 2015 | Case study | Key informants and cyclone-affected people in Koyra Sadar Upazila, Khulna district | 20 | Perceived need for mental health support and availability of such services | Self-reported exposure to cyclones using interviews | Good | |
| Tawatsupa, Lim et al., 2010 | Thailand | 2005 | Cross-sectional | Workers | 40,913 | Psychological distress (K10) and overall health (first question of SF8) | Self-reported exposure to heat stress using questionnaires | Fair | |
| Trang, Rocklov et al., 2016 | Vietnam | 2008–2012 | Time-series | Patients with mental disorders in the north of Vietnam | 21,443 | Hospital admissions for mental disorders | Interpolated exposure using daily meteorological data, from several monitoring stations in Hanoi, on temperature (used to define heatwave events) | N/A | |
| Trinh, Feeny et al., 2020 | Vietnam | 2002–2013 | Modelling | Children | 2000 | Stunting and underweight in children, and parental mental health as a mediating factor | Interpolated exposure using gridded (0.5 × 0.5 degree) monthly meteorological data on rainfall from the National Oceanic and Atmospheric Administration | N/A | |
| Verplanken and Roy 2013 | Europe and USA | 2012 | Participatory research | Participants who took survey in USA and Europe | 132 | Habitual ecological worrying | Self-reported exposure to climate change using surveys | Fair | |
| Vida, Durocher et al., 2012 | Canada | 1995–2007 | Modelling | Patients aged 15 years and older in Quebec | 347,552 | Emergency department visits for mental and psychosocial problems | Interpolated exposure using daily meteorological data, from available weather stations, on temperature and humidity from Environment Canada and the Ministry of Sustainable Development, Environment, and Parks | N/A | |
| Wang, Lavigne et al., 2014 | Canada | 2002–2010 | Ecological | Residents of Toronto | 271,746 | Emergency room (ER) visits related to mental and behavioural diseases (MBD) | Interpolated exposure using hourly meteorological data, from the monitoring station at Toronto Pearson International Airport, on temperature and humidity from Environment Canada | Good | |
| Wei, Zhang et al., 2020 | China | 2005–2014 | Ecological | Patients of Anhui Mental Health Center in Hefei | 36,607 | Admissions for schizophrenia | Interpolated exposure to precipitation data for the region Hefei and flood events were defined based on established criteria. | Poor | |
| Williams, Hill et al., 2016 | New Zealand | 1993–2009 | Modelling | Population of New Zealand | 47,265 | Self-harm hospitalisations | Interpolated exposure using gridded (5 km) daily meteorological data, from a virtual climate network, on temperature from the National Institute of Water and Atmospheric Research | N/A | |
| Williams, Nitschke et al., 2012 | Australia | 1993–2009 | Ecological | Population of Adelaide | N/A | Mortality, ambulance call-outs, emergency department (ED) presentations and hospital admissions | Interpolated exposure using daily meteorological data, from Kent Town station, on temperature from the Australian Bureau of Meteorology | Good | |
| Xu, Wheeler et al., 2018 | Australia | 2008–2014 | Cross-sectional | Australian children | 6857 | Mental health | Interpolated exposure using gridded daily meteorological data on temperature from the Australian Bureau of Meteorology | Good | |
| Xu, Zhao et al., 2020 | Brazil | 2000–2015 | Case-crossover | Brazilian population | 49,145,997 | All-cause and cause-specific hospitalisations | Interpolated exposure using gridded (0.25 degree) daily meteorological data on temperature, from a Brazilian meteorological dataset, with the analyses restricted to the hottest four consecutive months (hot season) for each city each year during the study period | N/A | |
| Yazd, Wheeler et al., 2020 | Australia | 2001–2015 | Panel | Farmers in the Murray-Darling Basin | 235 | Mental health, assessed using the mental health inventory (MHI-5), a sub-scale of the SF-36 | Interpolated exposure using gridded monthly meteorological data on rainfall (used to define drought) from the Australian Bureau of Meteorology | N/A | |
| Yoon, Oh et al., 2014 | South Korea | 2008, 2100 | Modelling (burden of disease) | Population of South Korea | N/A | Burden of disease (DALYs) attributable to climate factors | Interpolated exposure using daily meteorological data, from 77 regional meteorological offices and observatories, on temperature from the Korea Meteorological Administration; ozone concentration data from the 2008 Annual Report of Ambient Air Quality in Korea; and the number of natural disasters was based on the Annual Report of Disasters in Korea | N/A | |
| Zhao, Zhang et al., 2016 | China | 2005–2014 | Ecological | Population of Hubei | 36,607 | Emergency hospital admissions for schizophrenia | Interpolated exposure using daily meteorological data on temperature and humidity from the Hefei Bureau of Meteorology | Good | |
| Identifying the Most Effective Interventions (n = 8) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Quality Rating | ||
| Hart, Berry et al., 2011 | Australia | 2007–2010 | Program development | All rural communities facing prolonged drought in NSW | 3000 | A community development model effective in helping communities build capacity and resilience in the face of chronic drought-related hardship. | N/A | ||
| Hayes, Poland et al., 2020 | Canada | 2018 | Case study | Key informant health and social services leaders, front-line health and social services workers and community members who experienced the 2013 Southern Alberta flood | 46 | Health and social service responses to the long-term mental health impacts of the flood | Good | ||
| Heaney and Winter 2016 | Tanzania | 2013 | Case study | Two demographically matched adult Maasai populations in Arusha: rural-to-urban migrants and permanent rural residents (i.e., non-migrants) | 14 | Health perceptions and help-seeking behaviours | Good | ||
| Netuveli and Watts 2020 | United Kingdom | 2009–2010 | Panel | UK households | 22,427 people in 9344 households | Life satisfaction, self-rated health, mental health (assessed using 12-item version of the General Health Questionnaire (GHQ-12)), physical quality of life and mental quality of life | N/A | ||
| Patrick and Capetola 2011 | Australia | 2010–2011 | Case study | Victorian health care agencies that explicitly identified climate change as a priority | 10 | Health promotion practice | Good | ||
| Purcell and McGirr 2018 | Australia | NR | Cross-sectional | Health service managers working in rural remote metropolitan areas in NSW |
43 | Perceptions and recommendations of rural HSMs on climate change and its impact on health in their local communities | Fair | ||
| Valois, Blouin et al., 2016 | Canada | NR | Cross-sectional | Family physicians in Quebec | 24 | Family physicians’ educational needs regarding the health impacts of climate change | Good | ||
| Wang, Jiang et al., 2019 | China | 2018 | Cross-sectional | Chinese residents | 1273 | Environmental complaint behaviour | Fair | ||
| Guiding Health-Promoting Mitigation and Adaption Decisions in Other Sectors (n = 7) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Quality Rating | ||
| Harper, Edge et al., 2015 | Canada | 2010 | Participatory research | Inuit community members and government employees in the Nunatsiavut region | 209 | Climate-sensitive health issues | Good | ||
| MacFarlane, Shakya et al., 2015 | Nepal | 2014 | Participatory research | Female subsistence farmers aged 27–49 years in the Jumla district |
10 | Mental health | Good | ||
| Petrasek MacDonald, Cunsolo Willox et al., 2015 | Canada | 2012–2013 | Case study | Inuit youth in Nunatsiavut | 17 | Youth-specific protective factors that enhance mental health and well-being | Good | ||
| Raker, Arcaya et al., 2020 | USA | 2003–2018 | Cross-sectional | Low-income primarily Black parents in New Orleans and Houston | 113 | Lessons learned from the RISK project, including planning priorities to mitigate the health consequences of disasters | Good | ||
| Sawatzky, Cunsolo et al., 2020 | Canada | 2015–2016 | Case study | Inuit community members, government representatives and health professionals in Rigolet | 31 | Conceptual framework for an Inuit-led integrated environment and health monitoring system | Good | ||
| Sorgho, Mank et al., 2020 | Burkina Faso | 2018 | Case study | Subsistence farmers | 32 | Perceptions of climate change and health; agricultural adaptation strategies including barriers and possibilities; dietary adaptation practices; sources of support (social and governmental) | Good | ||
| Wong-Parodi 2020 | USA | 2019 | Cross-sectional | Individuals living in one of 41 California counties in PG&E’s and SCE’s (utility companies) public safety power shutoffs (PSPS) zone | 328 | Physical and mental health; views on the PSPS decisions; response to those decisions; views on wildfire risk | Fair | ||
| Improving Decision-Support (n = 3) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Quality Rating | ||
| McIver, Kim et al., 2016 | Cook Islands, Federated States of Micronesia, Fiji, Kiribati, Marshall Islands, Nauru, Niue, Palau, Samoa, Solomon Islands, Tonga, Tuvalu, and Vanuatu |
2010–2012 | Vulnerability assessment | Pacific island countries | 13 Pacific island countries | Health risks and adaptation strategies | N/A | ||
| Seidel and Bell 2014 | Australia, Belgium, Wales, Finland, Denmark, Germany, United Kingdom, Russia, USA, Spain, Scotland, Netherlands | 2012 | ‘Critical computational linguistics’ | High-income countries | Exhaustive sample of national adaptation policy documents from Annex 1 (‘developed’) countries of the UNFCC |
Representation of climate-vulnerable groups in adaptation policy | N/A | ||
| Valois, Caron et al., 2019 | Canada | NR | Cross-sectional | Adults living in or near a designated flood-prone area in Quebec | 1951 | Behavioural indices of flood adaptation | Fair | ||
| Estimating the Costs of Protecting Health from Climate Change (n = 1) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Quality Rating | ||
| Maughan, Patel et al., 2016 | United Kingdom | 2011–2014 | Retrospective observational study | Patients with a common mental health condition attending the Connect service; control group of patients attending same primary care service not attending Connect | Connect group = 30, control group = 29 | Financial and environmental impacts of GP appointments, psychotropic medications and secondary-care referrals | Good | ||
Abbreviations—NR: not reported; NSW: New South Wales; USA: United States of America; WA: Western Australia.
Author Contributions
Conceptualization: F.C., T.B., M.P., and S.A.; methodology: F.C., S.A., and T.B.; validation: F.C. and S.A.; formal analysis: F.C., S.A., T.B., and M.P.; data curation: F.C., S.A., T.B., and M.P.; writing—original draft preparation: F.C., S.A., and T.B.; writing—review and editing: F.C., S.A., T.B., M.P., J.A., A.M., and J.G.S.; supervision: J.G.S. All authors have read and agreed to the published version of the manuscript.
Funding
F.C. is supported by an Australian National Health and Medical Research Council (NHMRC) Early Career Fellowship (APP1138488).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Costello A., Abbas M., Allen A., Ball S., Bell S., Bellamy R., Friel S., Groce N., Johnson A., Kett M. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693–1733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 2.Watts N., Amann M., Arnell N., Ayeb-Karlsson S., Beagley J., Belesova K., Boykoff M., Byass P., Cai W., Campbell-Lendrum D. The 2020 report of The Lancet Countdown on health and climate change: Responding to converging crises. Lancet. 2020;397:129–170. doi: 10.1016/S0140-6736(20)32290-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel V., Chisholm D., Parikh R., Charlson F.J., Degenhardt L., Dua T., Ferrari A.J., Hyman S., Laxminarayan R., Levin C., et al. Addressing the burden of mental, neurological, and substance use disorders: Key messages from Disease Control Priorities, 3rd edition. Lancet. 2015;387:1672–1685. doi: 10.1016/S0140-6736(15)00390-6. [DOI] [PubMed] [Google Scholar]
- 4.Berry H.L., Bowen K., Kjellstrom T. Climate change and mental health: A causal pathways framework. Int. J. Public Health. 2010;55:123–132. doi: 10.1007/s00038-009-0112-0. [DOI] [PubMed] [Google Scholar]
- 5.Middleton J., Cunsolo A., Jones-Bitton A., Wright C.J., Harper S.L. Indigenous mental health in a changing climate: A systematic scoping review of the global literature. Environ. Res. Lett. 2020;15:53001. doi: 10.1088/1748-9326/ab68a9. [DOI] [Google Scholar]
- 6.Hayes K., Poland B. Addressing Mental Health in a Changing Climate: Incorporating Mental Health Indicators into Climate Change and Health Vulnerability and Adaptation Assessments. Int. J. Environ. Res. Public Health. 2018;15:1806. doi: 10.3390/ijerph15091806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cianconi P., Betrò S., Janiri L. The Impact of Climate Change on Mental Health: A Systematic Descriptive Review. Front. Psychiatry. 2020;11:1–15. doi: 10.3389/fpsyt.2020.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO . Protecting Health from Climate Change: Global Research Priorities. World Health Organisation; Geneva, Switzerland: 2009. [Google Scholar]
- 9.Page M.J., McKenzie J., Bossuyt P., Boutron I., Hoffmann T., Mulrow C., Shamseer L. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. MetaArXiv. 2020 doi: 10.31222/osf.io/v7gm2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D., Horsley T., Weeks L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 11.Watts N., Amann M., Arnell N., Ayeb-Karlsson S., Belesova K., Berry H., Bouley T., Boykoff M., Byass P., Cai W., et al. The 2018 report of the Lancet Countdown on health and climate change: Shaping the health of nations for centuries to come. Lancet. 2018;392:2479–2514. doi: 10.1016/S0140-6736(18)32594-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute for Health Study Quality Assessment Tools. [(accessed on 8 February 2021)]; Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 13.CASP CASP Checklists. [(accessed on 8 February 2021)]; Available online: https://casp-uk.net/casp-tools-checklists/
- 14.Cortes-Ramirez J., Naish S., Sly P.D., Jagals P. Mortality and morbidity in populations in the vicinity of coal mining: A systematic review. BMC Public Health. 2018;18:721. doi: 10.1186/s12889-018-5505-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haddaway N.R., McGuinness L.A. PRISMA2020: R package and ShinyApp for producing PRISMA 2020 compliant flow diagrams (Version 0.0.1) Zenodo. 2020 doi: 10.5281/zenodo.4287835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.South A. rworldmap: A new R package for mapping global data. R J. 2011;3:43. doi: 10.32614/RJ-2011-006. [DOI] [Google Scholar]
- 17.Team R. RStudio: Integrated Development for R. RStudio. [(accessed on 23 April 2021)]; Available online: http://www.rstudio.com/
- 18.Team R.C. R: A language and environment for statistical computing. [(accessed on 23 April 2021)]; Available online: https://www.R-project.org/
- 19.Wickham H. ggplot2: Elegant Graphics for Data Analysis. [(accessed on 23 April 2021)]; Available online: https://ggplot2.tidyverse.org.
- 20.Ding N., Berry H.L., Bennett C.M. The Importance of Humidity in the Relationship between Heat and Population Mental Health: Evidence from Australia. PLoS ONE. 2016;11:e0164190. doi: 10.1371/journal.pone.0164190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams S., Nitschke M., Sullivan T., Tucker G.R., Weinstein P., Pisaniello D.L., Parton K.A., Bi P. Heat and health in Adelaide, South Australia: Assessment of heat thresholds and temperature relationships. Sci. Total Environ. 2012;414:126–133. doi: 10.1016/j.scitotenv.2011.11.038. [DOI] [PubMed] [Google Scholar]
- 22.Xu Y., Wheeler S.A., Zuo A. Will boys’ mental health fare worse under a hotter climate in Australia? Popul. Environ. 2018;40:158–181. doi: 10.1007/s11111-018-0306-6. [DOI] [Google Scholar]
- 23.Kabir S.M.S. Psychological health challenges of the hill-tracts region for climate change in Bangladesh. Asian J. Psychiatry. 2018;34:74–77. doi: 10.1016/j.ajp.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 24.Pailler S., Tsaneva M. The effects of climate variability on psychological well-being in India. World Dev. 2018;106:15–26. doi: 10.1016/j.worlddev.2018.01.002. [DOI] [Google Scholar]
- 25.Tawatsupa B., Lim L.L., Kjellstrom T., Seubsman S.A., Sleigh A., The Thai Cohort Study T. The association between overall health, psychological distress, and occupational heat stress among a large national cohort of 40,913 Thai workers. Glob. Health Action. 2010;3:1–11. doi: 10.3402/gha.v3i0.5034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen N.T., Lin P.H., Guo Y.L. Long-term exposure to high temperature associated with the incidence of major depressive disorder. Sci. Total Environ. 2019;659:1016–1020. doi: 10.1016/j.scitotenv.2018.12.434. [DOI] [PubMed] [Google Scholar]
- 27.Noelke C., McGovern M., Corsi D.J., Jimenez M.P., Stern A., Wing I.S., Berkman L. Increasing ambient temperature reduces emotional well-being. Environ. Res. 2016;151:124–129. doi: 10.1016/j.envres.2016.06.045. [DOI] [PubMed] [Google Scholar]
- 28.Obradovich N., Migliorini R., Paulus M.P., Rahwan I. Empirical evidence of mental health risks posed by climate change. Proc. Natl. Acad. Sci. USA. 2018;115:10953–10958. doi: 10.1073/pnas.1801528115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sugg M.M., Dixon P.G., Runkle J.D. Crisis support-seeking behavior and temperature in the United States: Is there an association in young adults and adolescents? Sci. Total Environ. 2019;669:400–411. doi: 10.1016/j.scitotenv.2019.02.434. [DOI] [PubMed] [Google Scholar]
- 30.Mason L.R., Erwin J., Brown A., Ellis K.N., Hathaway J.M. Health Impacts of Extreme Weather Events: Exploring Protective Factors with a Capitals Framework. J. Evid. Inf. Soc. Work. 2018;15:579–593. doi: 10.1080/23761407.2018.1502115. [DOI] [PubMed] [Google Scholar]
- 31.OBrien L., Berry H.L., Coleman C., Hanigan I.C. Drought as a mental health exposure. Environ. Res. 2014;131:181–187. doi: 10.1016/j.envres.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 32.Austin E.K., Handley T., Kiem A.S., Rich J.L., Lewin T.J., Askland H.H., Askarimarnani S.S., Perkins D.A., Kelly B.J. Drought-related stress among farmers: Findings from the Australian Rural Mental Health Study. Med. J. Aust. 2018;209:159–165. doi: 10.5694/mja17.01200. [DOI] [PubMed] [Google Scholar]
- 33.Polain J.D., Berry H.L., Hoskin J.O. Rapid change, climate adversity and the next ‘big dry’: Older farmers’ mental health. Aust. J. Rural Health. 2011;19:239–243. doi: 10.1111/j.1440-1584.2011.01219.x. [DOI] [PubMed] [Google Scholar]
- 34.Stain H.J., Kelly B., Carr V.J., Lewin T.J., Fitzgerald M., Fragar L. The psychological impact of chronic environmental adversity: Responding to prolonged drought. Soc. Sci. Med. 2011;73:1593–1599. doi: 10.1016/j.socscimed.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 35.Hanigan I.C., Schirmer J., Niyonsenga T. Drought and Distress in Southeastern Australia. EcoHealth. 2018;15:642–655. doi: 10.1007/s10393-018-1339-0. [DOI] [PubMed] [Google Scholar]
- 36.Powers J.R., Dobson A.J., Berry H.L., Graves A.M., Hanigan I.C., Loxton D. Lack of association between drought and mental health in a cohort of 45-61 year old rural Australian women. Aust. N. Z. J. Public Health. 2015;39:518–523. doi: 10.1111/1753-6405.12369. [DOI] [PubMed] [Google Scholar]
- 37.Powers J.R., Loxton D., Baker J., Rich J.L., Dobson A.J. Empirical evidence suggests adverse climate events have not affected Australian women’s health and well-being. Aust. N. Z. J. Public Health. 2012;36:452–457. doi: 10.1111/j.1753-6405.2012.00848.x. [DOI] [PubMed] [Google Scholar]
- 38.Rotge J.Y., Fossati P., Lemogne C. Climate and prevalence of mood disorders: A cross-national correlation study. J. Clin. Psychiatry. 2014;75:408. doi: 10.4088/JCP.13l08810. [DOI] [PubMed] [Google Scholar]
- 39.Dodd W., Scott P., Howard C., Scott C., Rose C., Cunsolo A., Orbinski J. Lived experience of a record wildfire season in the Northwest Territories, Canada. Can. J. Public Health Rev. Can. De Sante Publique. 2018;109:327–337. doi: 10.17269/s41997-018-0070-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Higginbotham N., Connor L., Albrecht G., Freeman S., Agho K. Validation of an Environmental Distress Scale. EcoHealth. 2006;3:245–254. doi: 10.1007/s10393-006-0069-x. [DOI] [Google Scholar]
- 41.Eisenman D., McCaffrey S., Donatello I., Marshal G. An Ecosystems and Vulnerable Populations Perspective on Solastalgia and Psychological Distress After a Wildfire. EcoHealth. 2015;12:602–610. doi: 10.1007/s10393-015-1052-1. [DOI] [PubMed] [Google Scholar]
- 42.Ng F.Y., Wilson L.A., Veitch C. Climate adversity and resilience: The voice of rural Australia. Rural Remote Health. 2015;15:3071. [PubMed] [Google Scholar]
- 43.Mulchandani R., Armstrong B., Beck C.R., Waite T.D., Amlôt R., Kovats S., Leonardi G., Rubin G.J., Oliver I. The English National Cohort Study of Flooding & Health: Psychological morbidity at three years of follow up. BMC Public Health. 2020;20:321. doi: 10.1186/s12889-020-8424-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Farrokhi M., Khankeh H.R., Amanat N., Kamali M., Fathi M. Psychological aspects of climate change risk perception: A content analysis in Iranian context. J. Educ. Health Promot. 2020;9:346. doi: 10.4103/jehp.jehp_415_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Howard M., Ahmed S., Lachapelle P., Schure M.B. Farmer and rancher perceptions of climate change and their relationships with mental health. J. Rural Ment. Health. 2020;44:87–95. doi: 10.1037/rmh0000131. [DOI] [Google Scholar]
- 46.Albrecht G., Sartore G.M., Connor L., Higginbotham N., Freeman S., Kelly B., Stain H., Tonna A., Pollard G. Solastalgia: The distress caused by environmental change. Australas. Psychiatry Bull. R. Aust. N. Z. Coll. Psychiatr. 2007;15(Suppl. 1):S95–S98. doi: 10.1080/10398560701701288. [DOI] [PubMed] [Google Scholar]
- 47.Fuentes L., Asselin H., Bélisle A.C., Labra O. Impacts of Environmental Changes on Well-Being in Indigenous Communities in Eastern Canada. Int. J. Environ. Res. Public Health. 2020;17:637. doi: 10.3390/ijerph17020637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Searle K., Gow K. Do concerns about climate change lead to distress? Int. J. Clim. Chang. Strat. Manag. 2010;2:362–379. doi: 10.1108/17568691011089891. [DOI] [Google Scholar]
- 49.Billiot S.M. Ph.D. Thesis. Washington University; St Louis, MO, USA: 2018. How Do Environmental Changes and Shared Cultural Experiences Impact the Health of Indigenous Peoples in South Louisiana? [Google Scholar]
- 50.Chan E.Y.Y., Lam H.C.Y., So S.H.W., Goggins W.B., Ho J.Y., Liu S., Chung P.P.W. Association between Ambient Temperatures and Mental Disorder Hospitalizations in a Subtropical City: A Time-Series Study of Hong Kong Special Administrative Region. Int. J. Environ. Res. Public Health. 2018;15:754. doi: 10.3390/ijerph15040754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xu R., Zhao Q., Coelho M.S., Saldiva P.H., Abramson M.J., Li S., Guo Y.J.P.M. Socioeconomic level and associations between heat exposure and all-cause and cause-specific hospitalization in 1,814 Brazilian cities: A nationwide case-crossover study. PLoS Med. 2020;17:e1003369. doi: 10.1371/journal.pmed.1003369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hansen A., Bi P., Nitschke M., Ryan P., Pisaniello D., Tucker G. The effect of heat waves on mental health in a temperate Australian city. Environ. Health Perspect. 2008;116:1369–1375. doi: 10.1289/ehp.11339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang X., Lavigne E., Ouellette-kuntz H., Chen B.E. Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in Toronto, Canada. J. Affect. Disord. 2014;155:154–161. doi: 10.1016/j.jad.2013.10.042. [DOI] [PubMed] [Google Scholar]
- 54.Trang P.M., Rocklov J., Giang K.B., Kullgren G., Nilsson M. Heatwaves and Hospital Admissions for Mental Disorders in Northern Vietnam. PLoS ONE. 2016;11:e0155609. doi: 10.1371/journal.pone.0155609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu X., Liu H., Fan H., Liu Y., Ding G. Influence of Heat Waves on Daily Hospital Visits for Mental Illness in Jinan, China—A Case-Crossover Study. Int. J. Environ. Res. Public Health. 2018;16:87. doi: 10.3390/ijerph16010087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Page L.A., Hajat S., Kovats R.S., Howard L.M. Temperature-related deaths in people with psychosis, dementia and substance misuse. Br. J. Psychiatry J. Ment. Sci. 2012;200:485–490. doi: 10.1192/bjp.bp.111.100404. [DOI] [PubMed] [Google Scholar]
- 57.Oudin Astrom D., Schifano P., Asta F., Lallo A., Michelozzi P., Rocklov J., Forsberg B. The effect of heat waves on mortality in susceptible groups: A cohort study of a mediterranean and a northern European City. Environ. Health A Glob. Access Sci. Source. 2015;14:30. doi: 10.1186/s12940-015-0012-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nitschke M., Tucker G.R., Bi P. Morbidity and mortality during heatwaves in metropolitan Adelaide. Med. J. Aust. 2007;187:662–665. doi: 10.5694/j.1326-5377.2007.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 59.Gu S., Zhang L., Sun S., Wang X., Lu B., Han H., Yang J., Wang A.J.E.I. Projections of temperature-related cause-specific mortality under climate change scenarios in a coastal city of China. Environ. Int. 2020;143:105889. doi: 10.1016/j.envint.2020.105889. [DOI] [PubMed] [Google Scholar]
- 60.Williams M.N., Hill S.R., Spicer J. Do hotter temperatures increase the incidence of self-harm hospitalisations? Psychol. Health Med. 2016;21:226–235. doi: 10.1080/13548506.2015.1028945. [DOI] [PubMed] [Google Scholar]
- 61.Carleton T.A. Crop-damaging temperatures increase suicide rates in India. Proc. Natl. Acad. Sci. USA. 2017;114:8746–8751. doi: 10.1073/pnas.1701354114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Helama S., Holopainen J., Partonen T. Temperature-associated suicide mortality: Contrasting roles of climatic warming and the suicide prevention program in Finland. Environ. Health Prev. Med. 2013;18:349–355. doi: 10.1007/s12199-013-0329-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Preti A., Lentini G., Maugeri M. Global warming possibly linked to an enhanced risk of suicide: Data from Italy, 1974–2003. J. Affect. Disord. 2007;102:19–25. doi: 10.1016/j.jad.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 64.Burke M., González F., Baylis P., Heft-Neal S., Baysan C., Basu S., Hsiang S. Higher temperatures increase suicide rates in the United States and Mexico. Nat. Clim. Chang. 2018;8:723–729. doi: 10.1038/s41558-018-0222-x. [DOI] [Google Scholar]
- 65.Yoon S.J., Oh I.H., Seo H.Y., Kim E.J. Measuring the burden of disease due to climate change and developing a forecast model in South Korea. Public Health. 2014;128:725–733. doi: 10.1016/j.puhe.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 66.Hoffmann M.S., Oliveira L.M., Lobato M.I., Belmonte-de-Abreu P. Heat stroke during long-term clozapine treatment: Should we be concerned about hot weather? Trends Psychiatry Psychother. 2016;38:56–59. doi: 10.1590/2237-6089-2015-0066. [DOI] [PubMed] [Google Scholar]
- 67.Jones M.K., Wootton B.M., Vaccaro L.D., Menzies R.G. The impact of climate change on obsessive compulsive checking concerns. Aust. N. Z. J. Psychiatry. 2012;46:265–270. doi: 10.1177/0004867411433951. [DOI] [PubMed] [Google Scholar]
- 68.Dean J.G., Stain H.J. Mental health impact for adolescents living with prolonged drought. Aust. J. Rural Health. 2010;18:32–37. doi: 10.1111/j.1440-1584.2009.01107.x. [DOI] [PubMed] [Google Scholar]
- 69.Cunsolo Willox A., Harper S.L., Ford J.D., Landman K., Houle K., Edge V.L. “From this place and of this place:” climate change, sense of place, and health in Nunatsiavut, Canada. Soc. Sci. Med. 2012;75:538–547. doi: 10.1016/j.socscimed.2012.03.043. [DOI] [PubMed] [Google Scholar]
- 70.Carnie T.L., Berry H.L., Blinkhorn S.A., Hart C.R. In their own words: Young people’s mental health in drought-affected rural and remote NSW. AJRH. 2011;19:244–248. doi: 10.1111/j.1440-1584.2011.01224.x. [DOI] [PubMed] [Google Scholar]
- 71.Durkalec A., Furgal C., Skinner M.W., Sheldon T. Climate change influences on environment as a determinant of Indigenous health: Relationships to place, sea ice, and health in an Inuit community. Soc. Sci. Med. 2015;136–137:17–26. doi: 10.1016/j.socscimed.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 72.Cunsolo Willox A., Harper S.L., Ford J.D., Edge V.L., Landman K., Houle K., Blake S., Wolfrey C. Climate change and mental health: An exploratory case study from Rigolet, Nunatsiavut, Canada. Clim. Chang. 2013;121:255–270. doi: 10.1007/s10584-013-0875-4. [DOI] [Google Scholar]
- 73.Flint C.G., Robinson E.S., Kellogg J., Ferguson G., Boufajreldin L., Dolan M., Raskin I., Lila M.A. Promoting wellness in Alaskan villages: Integrating traditional knowledge and science of wild berries. EcoHealth. 2011;8:199–209. doi: 10.1007/s10393-011-0707-9. [DOI] [PubMed] [Google Scholar]
- 74.Bunce A., Ford J., Harper S., Edge V. Ihacc Research Team. Vulnerability and adaptive capacity of Inuit women to climate change: A case study from Iqaluit, Nunavut. Nat. Hazards. 2016;83:1419–1441. doi: 10.1007/s11069-016-2398-6. [DOI] [Google Scholar]
- 75.McNamara K.E., Westoby R. Solastalgia and the gendered nature of climate change: An example from Erub Island, Torres Strait. EcoHealth. 2011;8:233–236. doi: 10.1007/s10393-011-0698-6. [DOI] [PubMed] [Google Scholar]
- 76.Rigby C.W., Rosen A., Berry H.L., Hart C.R. If the land’s sick, we’re sick:* the impact of prolonged drought on the social and emotional well-being of Aboriginal communities in rural New South Wales. Aust J. Rural Health. 2011;19:249–254. doi: 10.1111/j.1440-1584.2011.01223.x. [DOI] [PubMed] [Google Scholar]
- 77.Qi X., Hu W., Mengersen K., Tong S. Socio-environmental drivers and suicide in Australia: Bayesian spatial analysis. BMC Public Health. 2014;14:681. doi: 10.1186/1471-2458-14-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cooper S., Hutchings P., Butterworth J., Joseph S., Kebede A., Parker A., Terefe B., Van Koppen B. Environmental associated emotional distress and the dangers of climate change for pastoralist mental health. Glob. Environ. Chang. 2019;59:1–15. doi: 10.1016/j.gloenvcha.2019.101994. [DOI] [Google Scholar]
- 79.Asugeni J., MacLaren D., Massey P.D., Speare R. Mental health issues from rising sea level in a remote coastal region of the Solomon Islands: Current and future. Australas. Psychiatry Bull. R. Aust. N. Z. Coll. Psychiatr. 2015;23:22–25. doi: 10.1177/1039856215609767. [DOI] [PubMed] [Google Scholar]
- 80.Gibson K.E., Barnett J., Haslam N., Kaplan I. The mental health impacts of climate change: Findings from a Pacific Island atoll nation. J. Anxiety Disord. 2020;73:102237. doi: 10.1016/j.janxdis.2020.102237. [DOI] [PubMed] [Google Scholar]
- 81.Ayeb-Karlsson S. ‘When we were children we had dreams, then we came to Dhaka to survive’: Urban stories connecting loss of wellbeing, displacement and (im)mobility. Clim. Dev. 2020:1–12. doi: 10.1080/17565529.2020.1777078. [DOI] [Google Scholar]
- 82.Ayeb-Karlsson S. ‘I do not like her going to the shelter’: Stories on gendered disaster (im) mobility and wellbeing loss in coastal Bangladesh. J. Int. J. Disaster Risk Reduct. 2020;50:101904. doi: 10.1016/j.ijdrr.2020.101904. [DOI] [Google Scholar]
- 83.Ayeb-Karlsson S., Kniveton D., Cannon T. Trapped in the prison of the mind: Notions of climate-induced (im)mobility decision-making and wellbeing from an urban informal settlement in Bangladesh. Palgrave Commun. 2020;6 doi: 10.1057/s41599-020-0443-2. [DOI] [Google Scholar]
- 84.Hayes K., Poland B., Cole D.C., Agic B. Psychosocial adaptation to climate change in High River, Alberta: Implications for policy and practice. Can. J. Public Health Rev. Can. De Sante Publique. 2020;111:880–889. doi: 10.17269/s41997-020-00380-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hart C.R., Berry H.L., Tonna A.M. Improving the mental health of rural New South Wales communities facing drought and other adversities. Aust. J. Rural Health. 2011;19:231–238. doi: 10.1111/j.1440-1584.2011.01225.x. [DOI] [PubMed] [Google Scholar]
- 86.Purcell R., McGirr J. Rural health service managers’ perspectives on preparing rural health services for climate change. Aust. J. Rural Health. 2018;26:20–25. doi: 10.1111/ajr.12374. [DOI] [PubMed] [Google Scholar]
- 87.Patrick R., Capetola T. It’s here! Are we ready? Five case studies of health promotion practices that address climate change from within Victorian health care settings. Health Promot. J. Aust. 2011;22:S61–S67. doi: 10.1071/HE11461. [DOI] [PubMed] [Google Scholar]
- 88.Valois P., Blouin P., Ouellet C., Renaud J.S., Belanger D., Gosselin P. The Health Impacts of Climate Change: A Continuing Medical Education Needs Assessment Framework. J. Contin. Educ. Health Prof. 2016;36:218–225. doi: 10.1097/CEH.0000000000000084. [DOI] [PubMed] [Google Scholar]
- 89.Wang S., Jiang J., Zhou Y., Li J., Zhao D., Lin S. Climate-change information, health-risk perception and residents’ environmental complaint behavior: An empirical study in China. Environ. Geochem. Health. 2019;42:719–732. doi: 10.1007/s10653-018-0235-4. [DOI] [PubMed] [Google Scholar]
- 90.Netuveli G., Watts P. Pro-environmental behaviours and attitudes are associated with health, wellbeing and life satisfaction in multiple occupancy households in the UK Household Longitudinal Study. Popul. Environ. 2020;41:347–371. doi: 10.1007/s11111-020-00337-7. [DOI] [Google Scholar]
- 91.Heaney A.K., Winter S.J. Climate-driven migration: An exploratory case study of Maasai health perceptions and help-seeking behaviors. Int. J. Public Health. 2016;61:641–649. doi: 10.1007/s00038-015-0759-7. [DOI] [PubMed] [Google Scholar]
- 92.Petrasek MacDonald J., Cunsolo Willox A., Ford J.D., Shiwak I., Wood M. Protective factors for mental health and well-being in a changing climate: Perspectives from Inuit youth in Nunatsiavut, Labrador. Soc. Sci. Med. 2015;141:133–141. doi: 10.1016/j.socscimed.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 93.Sawatzky A., Cunsolo A., Jones-Bitton A., Gillis D., Wood M., Flowers C., Shiwak I., Harper S.L., Rigolet Inuit Community G. “The best scientists are the people that’s out there”: Inuit-led integrated environment and health monitoring to respond to climate change in the Circumpolar North. Clim. Chang. 2020;160:45–66. doi: 10.1007/s10584-019-02647-8. [DOI] [Google Scholar]
- 94.Harper S.L., Edge V.L., Ford J., Willox A.C., Wood M., McEwen S.A. Climate-sensitive health priorities in Nunatsiavut, Canada. BMC Public Health. 2015;15:605. doi: 10.1186/s12889-015-1874-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.MacFarlane E.K., Shakya R., Berry H.L., Kohrt B.A. Implications of participatory methods to address mental health needs associated with climate change: ‘Photovoice’ in Nepal. BJPsych. Int. 2015;12:33–35. doi: 10.1192/S2056474000000246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Raker E.J., Arcaya M.C., Lowe S.R., Zacher M., Rhodes J., Waters M.C. Mitigating Health Disparities After Natural Disasters: Lessons From The RISK Project: Study examines mitigating health disparities after natural disasters. Health Aff. 2020;39:2128–2135. doi: 10.1377/hlthaff.2020.01161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sorgho R., Mank I., Kagoné M., Souares A., Danquah I., Sauerborn R.J.I.J.o.E.R., Health P. “We Will Always Ask Ourselves the Question of How to Feed the Family”: Subsistence Farmers’ Perceptions on Adaptation to Climate Change in Burkina Faso. Int. J. Environ. Res. Public Health. 2020;17:7200. doi: 10.3390/ijerph17197200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wong-Parodi G. When climate change adaptation becomes a “looming threat” to society: Exploring views and responses to California wildfires and public safety power shutoffs. Energy Res. Soc. Sci. 2020;70 doi: 10.1016/j.erss.2020.101757. [DOI] [Google Scholar]
- 99.McIver L., Kim R., Woodward A., Hales S., Spickett J., Katscherian D., Hashizume M., Honda Y., Kim H., Iddings S., et al. Health Impacts of Climate Change in Pacific Island Countries: A Regional Assessment of Vulnerabilities and Adaptation Priorities. Environ. Health Perspect. 2016;124:1707–1714. doi: 10.1289/ehp.1509756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Seidel B.M., Bell E. Health adaptation policy for climate vulnerable groups: A ‘critical computational linguistics’ analysis. BMC Public Health. 2014;14:1235. doi: 10.1186/1471-2458-14-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Valois P., Caron M., Gousse-Lessard A.S., Talbot D., Renaud J.S. Development and validation of five behavioral indices of flood adaptation. BMC Public Health. 2019;19:245. doi: 10.1186/s12889-019-6564-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Maughan D.L., Patel A., Parveen T., Braithwaite I., Cook J., Lillywhite R., Cooke M. Primary-care-based social prescribing for mental health: An analysis of financial and environmental sustainability. Prim. Health Care Res. Dev. 2016;17:114–121. doi: 10.1017/S1463423615000328. [DOI] [PubMed] [Google Scholar]
- 103.PRISM Climate Group PRISM Climate Data. [(accessed on 8 February 2021)]; Available online: https://prism.oregonstate.edu/
- 104.Berkeley Earth Data Overview. [(accessed on 8 February 2021)]; Available online: http://berkeleyearth.org/data/
- 105.Schinasi L.H., Benmarhnia T., De Roos A.J. Modification of the association between high ambient temperature and health by urban microclimate indicators: A systematic review and meta-analysis. Environ. Res. 2018;161:168–180. doi: 10.1016/j.envres.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 106.Tsoka S., Tsikaloudaki K., Theodosiou T., Bikas D. Urban Warming and Cities’ Microclimates: Investigation Methods and Mitigation Strategies—A Review. Energies. 2020;13:1414. doi: 10.3390/en13061414. [DOI] [Google Scholar]
- 107.Weissbecker I. Climate Change and Human Well-Being Global Challenges and Opportunities. Springer; New York, NY, USA: 2011. [Google Scholar]
- 108.Kameg B.N. Climate Change and Mental Health: Implications for Nurses. J. Psychosoc. Nurs. Ment. Health Serv. 2020;58:25–30. doi: 10.3928/02793695-20200624-05. [DOI] [PubMed] [Google Scholar]
- 109.Nicholas P.K., Breakey S., White B.P., Brown M.J., Fanuele J., Starodub R., Ros A.V. Mental Health Impacts of Climate Change: Perspectives for the ED Clinician. J. Emerg. Nurs. 2020;46:590–599. doi: 10.1016/j.jen.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Liu J., Potter T., Zahner S. Policy brief on climate change and mental health/well-being. Nurs. Outlook. 2020;68:517–522. doi: 10.1016/j.outlook.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Pinsky E., Guerrero A.P.S., Livingston R. Our House Is on Fire: Child and Adolescent Psychiatrists in the Era of the Climate Crisis. J. Am. Acad. Child. Adolesc. Psychiatry. 2020;59:580–582. doi: 10.1016/j.jaac.2020.01.016. [DOI] [PubMed] [Google Scholar]
- 112.Seritan A.L., Seritan I. The Time Is Now: Climate Change and Mental Health. Acad. Psychiatry. 2020;44:373–374. doi: 10.1007/s40596-020-01212-1. [DOI] [PubMed] [Google Scholar]
- 113.Arabena K., Armstrong F., Berry H., Brooks P., Capon T., Crabb B., Demaio A., Doherty P., Lewin S., Lo S., et al. Australian health professionals’ statement on climate change and health. Lancet. 2018;392:2169–2170. doi: 10.1016/S0140-6736(18)32610-2. [DOI] [PubMed] [Google Scholar]
- 114.Berry H.L., Waite T.D., Dear K.B., Capon A.G., Murray V. The case for systems thinking about climate change and mental health. Nat. Clim. Chang. 2018;8:282–290. doi: 10.1038/s41558-018-0102-4. [DOI] [Google Scholar]
- 115.Clayton S., Karazsia B.T. Development and validation of a measure of climate change anxiety. J. Environ. Psychol. 2020;69 doi: 10.1016/j.jenvp.2020.101434. [DOI] [Google Scholar]
- 116.Hope E.C., Velez G., Offidani-Bertrand C., Keels M., Durkee M.I. Political activism and mental health among Black and Latinx college students. Cult. Divers. Ethn. Minor. Psychol. 2018;24:26–39. doi: 10.1037/cdp0000144. [DOI] [PubMed] [Google Scholar]
- 117.World Health Organization Health and Climate Change Country Profiles. [(accessed on 10 March 2021)]; Available online: https://www.who.int/activities/monitoring-health-impacts-of-climate-change-and-national-progress.
- 118.World Health Organization . Mental Health Action Plan 2013–2020. World Health Organization; Geneva, Switzerland: 2013. [Google Scholar]
- 119.World Health Organization mhGAP Humanitarian Intervention Guide (mhGAP-HIG): Clinical Management of Mental, Neurological and Substance Use Conditions in Humanitarian Emergencies. [(accessed on 10 March 2021)]; Available online: http://www.who.int/mental_health/publications/mhgap_hig/en/
- 120.World Health Organization Building Back Better: Sustainable Mental Health Care after Emergencies. [(accessed on 10 March 2021)]; Available online: https://www.who.int/mental_health/emergencies/building_back_better/en/
- 121.World Health Organization Scalable Psychological Interventions for People in Communities Affected by Adversity: A New Area of Mental Health and Psychosocial Work at WHO. [(accessed on 10 March 2021)]; Available online: https://apps.who.int/iris/handle/10665/254581.
- 122.Palinkas L.A., O’Donnell M.L., Lau W., Wong M.J.I.J.O.E.R., Health P. Strategies for Delivering Mental Health Services in Response to Global Climate Change: A Narrative Review. Int. J. Environ. Res. Public Health. 2020;17:8562. doi: 10.3390/ijerph17228562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Climate and Health Alliance Climate and Health Alliance. [(accessed on 2 November 2020)]; Available online: https://www.caha.org.au/
- 124.Fearnley E.J., Magalhaes R.J., Speldewinde P., Weinstein P., Dobson A. Environmental correlates of mental health measures for women in Western Australia. EcoHealth. 2014;11:502–511. doi: 10.1007/s10393-014-0966-3. [DOI] [PubMed] [Google Scholar]
- 125.Smith K.R., Woodward A., Campbell-Lendrum D.D., Chadee D., Honda Y., Liu Q., Olwoch J.M., Revich B., Sauerborn R. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Cambridge University Press; Cambridge, UK: 2014. Human health: Impacts, adaptation, and co-benefits; pp. 709–754. [Google Scholar]
- 126.Hayes K., Blashki G., Wiseman J., Burke S., Reifels L. Climate change and mental health: Risks, impacts and priority actions. Int. J. Ment. Health Syst. 2018;12:28. doi: 10.1186/s13033-018-0210-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Maplecroft V. Climate Change Vulnerabillity Index 2017. [(accessed on 10 March 2021)]; Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/verisk%20index.pdf.
- 128.Ingle H.E., Mikulewicz M. Mental health and climate change: Tackling invisible injustice. Lancet Planet. Health. 2020;4:e128–e130. doi: 10.1016/S2542-5196(20)30081-4. [DOI] [PubMed] [Google Scholar]
- 129.Goldmann E., Galea S. Mental health consequences of disasters. Annu. Rev. Public Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- 130.Watts N., Amann M., Ayeb-Karlsson S., Belesova K., Bouley T., Boykoff M., Byass P., Cai W., Campbell-Lendrum D., Chambers J., et al. The Lancet Countdown on health and climate change: From 25 years of inaction to a global transformation for public health. Lancet. 2018;391:581–630. doi: 10.1016/S0140-6736(17)32464-9. [DOI] [PubMed] [Google Scholar]
- 131.Patel V., Saxena S., Lund C., Thornicroft G., Baingana F., Bolton P., Chisholm D., Collins P.Y., Cooper J.L., Eaton J., et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392:1553–1598. doi: 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]