Abstract
The whole world almost came to a standstill due to the COVID-19 pandemic. In response to this pandemic, most psychological responses have been at a higher prevalence such as stress, anxiety, depression, lower mental well-being, poor sleep quality, along with the fear of contracting the COVID-19 disease. Related to these psychological responses, previous studies have suggested an association between COVID-19 fear and stress as well as stress and sleep quality. The present study aimed to assess the association between COVID-19 fear and sleep quality and investigate the possible mediating effect of perceived stress during this pandemic. The data were collected, utilizing a self-report online questionnaire, from a sample of 521 Bangladeshi adults. Results showed significant gender differences in COVID-19 fear, stress, and sleep quality and also a significant association between these variables. Mediation results revealed that stress fully mediated the association between COVID-19 fear and sleep quality for males and partially mediated it for females. These results suggest that women are in a more vulnerable position in this pandemic. These findings would be helpful to mental health professionals and policy makers to address the psychological problems induced by the current pandemic.
Keywords: COVID-19 pandemic, COVID-19 fear, Stress, Sleep quality, Women
COVID-19 pandemic; COVID-19 fear; Stress; Sleep quality; Women.
Introduction
Since the end of 2019, the world has been experiencing the cruelty of SARS-CoV-2 and within only three months time, the virus had reached pandemic proportions. On a global scale, the mortality and morbidity count of the disease is rapidly changing. As of April 23, 2021, there were over 144,367,284 million confirmed cases of COVID-19 and more than 3,066,270 deaths reported globally (World Health Organization, 2021 April 23). Countries worldwide have been quick to take measures (i.e., social distancing, quarantine, partial and complete lockdown) to put off further transmission. In Bangladesh, the first COVID-19 positive case was reported on March 8, 2020, and the first death on March 18, 2020. Since then, the number of cases has escalated and subsequently multiplied. On April 23, 2021, there were a total of 736,074 COVID-19 positive cases reported, and 10,781 people who have died from COVID-19 (World Health Organization, 2021 April 23).
The pandemic has unsettled normal life. Apart from the emergency health concerns, the pandemic has also brought about momentous psychological, social, and economic challenges. Studies revealed the consequences of a stagnant situation as subsequent aberrations in cognitive functions, cardiovascular, and neuroendocrine systems that can lead to sleep disturbance and psychological problems, like depression (Bhatti and Haq, 2017; Cacioppo and Cacioppo, 2014). In addition, several empirical studies documented a higher prevalence of poor sleep quality and sleep disturbances during the current pandemic (Beck et al., 2021; Jahrami et al., 2021; Martinez-Lezaun et al., 2020; Voitsidis et al., 2020); although the impact of this pandemic on sleep quality is inconclusive. Gao and Scullin (2020) reported non-significant association between the pandemic and sleep. Moreover, a higher prevalence rate of fear of contagion by COVID-19, stress, anxiety, depression symptoms are also evident (Ahmed et al., 2020a, 2020b; Ahorsu et al., 2020a; Taylor et al., 2020; Wang et al., 2020a, 2020b).
Fear is known as one of the most primitive feelings that come up in the face of a real or perceived threat. Some physiological symptoms such as an increase in pulse, muscle stiffness, and acceleration of breathing as well as some psychological symptoms like attention deficit, resulted in a response of fear-producing events. Typical studies have suggested that females and younger people have higher fears of contagion (e.g., Andrade et al., 2020; Kassim et al., 2021; Rodríguez-Hidalgo et al., 2020). Exposure to unprecedented levels of fear, loss of control, and loneliness of social isolation have also been found to lead to stress and panic (Ahmed et al., 2020a; Rubin and Wessely, 2020). Additionally, an overflowing and overwhelming amount of information related to COVID-19 from social media has created unnecessary fear and confusion and subsequently led to the rise of stress (Usher et al., 2020).
Stress is known as any kind of negative emotional experience associated to further biochemical, physiological, cognitive, and behavioral responses. Stress usually occurs as an outcome of physical, environmental, interpersonal-social, or psychological causes (Beidel et al., 2014). Furthermore, any uncontrollable, unpredictable, uncertain, and significant events or phenomenon can increase the risk of stress (Taylor, 2006). Stress is not always undesirable, as an optimum level is required for adaptation. Lower stress makes it easier to cope, while higher stress levels can lead to physical and psychological problems. Besides the threat to physical health, the current pandemic increases the perceived stress level and subsequent psychological problems, such as, anxiety and depression (Harper et al., 2020; Pakpour and Griffiths, 2020; Taylor et al., 2020). A recent cross-cultural study has suggested that higher stress levels are more commonly found among young, female, single, and lower educated individuals (Kowal et al., 2020).
Studies suggested sleep (e.g., sleep quality, sleep latency, awakeness during the night, and sleep complaints) can be susceptible to alteration due to irrepressible or random stressors (Hefez et al., 1987; Mellman et al., 1995; Tempesta et al., 2013). It is also evident that perceived stress hinders sleep quality (Åkerstedt et al., 2012; Eliasson et al., 2010). The higher the perceived stress, the worse the sleep quality (Brand et al., 2011; Charles et al., 2011; Gerber et al., 2010; Murata et al., 2007; Sadeh et al., 2004; Xu et al., 2016), and the reduction in perceived stress predicted an improvement in sleep quality (Eliasson et al., 2010). Subsequently, dissatisfaction with sleep (duration and/or quality) impinge on social functioning (Li et al., 2006). Stress even plays an important role in the onset and development of sleep disorders (Dou et al., 2019; Redeker et al., 2020; Yan et al., 2010). Although the current pandemic does not affect all equally (Kocevska et al., 2020), females have been found to be more vulnerable in experiencing poor sleep quality and sleep problems (i.e., Beck et al., 2021; Martinez-Lezaun et al., 2020).
The cognitive – mediational theory of emotions posits that the degree of stress created by a stressor determines by one's thinking and appraisal about it (Lazarus, 1991; Lazarus and Folkman, 1984). For this theory, there are two steps that help to determine the degree of threat or harm induced by a stressor and one's reaction to this stressor. First, one estimates the severity of a stressor and classifies it as either a threat or a challenge (primary appraisal). If one perceives the stressor as a threat, then secondary appraisal comes with bodily and emotional reactions. In this step (second), one assesses the resources available to deal with the stressor, such as time, money, physical ability, and so on (secondary appraisal). Insufficient resources to meet the environment demands can then induce stress that results in changes of one's emotional state and effects one's health (Epel et al., 2018; Folkman and Lazarus, 1985; Folkman et al., 1986; Lazarus et al., 1985). This theory provides an understanding of the impact of the current pandemic (stressor) on emotional reaction (perceived stress) and bodily responses (sleep quality).
Emerging evidence based on the COVID-19 pandemic suggests the possibility of immediate and lasting repercussions of perceived stress on impacting one's cognitive functioning along with emotional and physiological state. Whenever a person stresses over the virus and fears contracting COVID-19, their brain can become stimulated and excited, causing sleep disturbances and possibly lowering cognitive and physical performance. Therefore, considering the pandemic situation where people feel a heightened fear of contagion, there might be an association between COVID-19 fear and sleep quality. Based on existing empirical evidence and the cognitive – mediational theory, fear can lead to stress, leading to poorer sleep quality. Here, stress might mediate the possible association between COVID-19 fear and sleep quality. Therefore, the present study aimed to assess the association between COVID-19 fear and sleep quality with the possible mediating effect of stress. Based on the above discussion, the following hypotheses were tested–
Hypothesis 1
Females will have higher fear of the COVID-19 disease, perceived stress, and lower sleep quality compared to males; and
Hypothesis 2
There will be an association between fear of the COVID-19 disease and sleep quality, with perceived stress mediating this association.
Methods
Data and sample
The present study is part of the project titled ‘Personality Traits, Fear of COVID-19, Stress, and Sleep Quality’ (Ahmed et al., 2020c) approved by the Faculty Review Board for Human Participant of Biological Sciences, University of Dhaka, Bangladesh (103/biol.scs.2020-21). In this project, data were collected through an online survey utilizing a Google Form. Before taking part in the survey, participants provided informed consent. As this was an online survey, participants provided their consent by clicking “yes” if they agreed to participate. Participation was voluntary, and participants did not receive any compensation. Based on a priori power calculation (small-to-medium effect size, α = .05, 95% power), the minimum required sample was 319. The data of this study contained responses from a sample of 521 participants (49.7% female) that was higher than the required number of study participants. Participants' age ranged between 18 years to 80 years old (M = 24.78 years, SD = 7.00 years). In terms of educational levels that participants accomplished, 13.44% completed higher secondary level, 60.65% had an undergraduate degree, and 23.80% graduated. Among them, 14.97% were married and 84.64% were unmarried.
Measures
The data utilized in this study were collected through the Fear of COVID-19 Scale (Ahorsu et al., 2020a; Ahmed et al., 2021 [Bangla version]), the Perceived Stress Scale -10 items (Cohen and Williamson, 1988; Islam, 2020 [Bangla version]), and subjective sleep quality item of the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989).
Fear of COVID-19 scale (FCV-19S)
The Fear of COVID-19 Scale is a unidimensional valid assessment tool for assessing COVID-19 related fear. This scale is comprised of seven statements (e.g., “It makes me uncomfortable to think about Coronavirus-19”). The authors have reported good reliability and validity using the classical test theory and Rasch analysis of the modern theory approach. This scale has been used widely among researchers globally and has been validated in several languages. Ahmed et al. (2021) have reported this scale (Bangla version) as a psychometrically sound tool using the classical test theory approach and the graded response model (GRM) of the modern test theory approach. For this scale, participants expressed their agreement on each statement using a five-point Likert-type scale, ranging from strongly disagree (1) to strongly agree (5). Total scores ranged between 7 and 35. The higher scores suggest a higher level of COVID-19 related fear. In the present study, the FCV-19SB had good internal consistency reliabilities (α = .87, ω = .87) and good model fits in confirmatory factor analysis (χ2/df = 2.54, Comparative Fit Index [CFI] = 1.00, TLI = 1.00, Root Mean Square Error of Approximation [RMSEA] = .05, and Standardized Root Mean square Residual [SRMR] = .04).
Perceived stress scale-10 (PSS-10)
The Perceived Stress Scale (PSS-10) is one of the widely used scales for assessing perceived stress. This scale comprises ten questions (e.g., “how often have you felt nervous and ‘stressed’?”) that assess one's feelings and thoughts during the last month. Participants expressed their opinion regarding each question using a five-point Likert-type scale, ranging between never (0) and very often (4). The total scores ranged between 0 and 40. The higher scores suggest a higher stress perception during the last month. Like the original PSS-10, the PSS-10 Bangla had good reliability and validity to assess the perceived stress among Bangladeshi people. In this study, PSS-10 Bangla had good internal consistency reliabilities (α = .86, ω = .86) and good model fits in confirmatory factor analysis (χ2/df = 3.00, GFI = .96, CFI = .96, RMSEA = .06, and SRMR = .04).
Pittsburgh sleep quality index
The Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989) is the most used assessment tool for assessing sleep quality. This scale comprises 18 individual items that assess seven sleep quality components (e.g., subjective sleep quality, sleep latency, habitual sleep efficiency, etc.). In this study, data collected using the item for assessing subjective sleep quality were utilized. Participants rated their sleep quality during the last 14 days using a four-point scale, ranged between very good (0) and very bad (3).
Statistical analysis
In the current study, IBM SPSS v26 was utilized for data management and analysis (descriptive statistics [frequencies, percentages, mean, standard deviation, skewness, and kurtosis], two-independent sample t-test, Pearson product-moment correlation, and mediation analysis using process macros v3.4 [Hayes, 2013]). Frequency and percentages were performed to assess the distribution of demographic characteristics. The data normality was examined through study variables’ skewness and kurtosis values (≤2 for skewness and ≤7 for kurtosis; recommended by Kim, 2013). Gender differences in study variables were estimated using the two independent sample t-test. Pearson correlation was utilized to assess the association between study variables. Finally, process macros (model 4) was utilized to estimate mediating effect of stress on the association COVID-19 fear and sleep quality.
Results
Descriptive statistics (mean, SD, skewness, and kurtosis) of study variables are presented in Table 1. Skewness (ranged between -.17 and .83) and kurtosis (ranged between -.64 and .42) values were between the recommended range (>2 for skewness and >7 for kurtosis; Kim, 2013). These values suggested the normality of the data.
Table 1.
Descriptive statistics of fear of the COVID-19 disease, stress, and sleep quality.
| Variables | Mean | SD | Skewness | Kurtosis | Correlations |
|
|---|---|---|---|---|---|---|
| Stress | Sleep quality | |||||
| Fear of COVID-19 disease | 18.97 | 6.74 | .16 | -.64 | .51∗∗∗ [.42, .60] .43∗∗∗ [.32, .52] |
.22∗∗∗ [.10, .33] .28∗∗∗ [.16, .39] |
| Stress | 18.94 | 7.36 | -.17 | -.22 | .46∗∗∗ [.36, .55] .33∗∗∗ [.22, .44] |
|
| Sleep Quality | .96 | .83 | .83 | .42 | ||
∗∗∗p < .001.
Values in the parenthesis are 95% CI; Bold values are correlation coefficients between study variables for female sample.
Results regarding gender differences in Table 2 confirmed Hypothesis 1. Table 2 demonstrated that females had significantly higher COVID-19 fear (t (518) = -4.90, p < .001, 95% CI [ -3.97, -1.70], Cohen's d = -.43), perceived stress (t (518) = -6.10, p < .001, 95% CI [ -5.03, -2.58], Cohen's d = -.54), and lower sleep quality (t (518) = -2.92, p = .004, 95% CI [ -.35, -.07], Cohen's d = -.27). As there were significant mean differences in all study variables, further analyses were done separately for males and females.
Table 2.
Mean differences in fear of the COVID-19 disease, stress, and sleep quality by gender.
| Variables | Groups | M | SD | t-value (518) | p-value | Effect size | 95% CI |
|
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Fear of COVID-19 disease | Male (261) | 17.54 | 6.16 | -4.90 | <.001 | -.43 | -3.97 | -1.70 |
| Female (259) | 20.37 | 6.99 | ||||||
| Stress | Male (261) | 17.03 | 6.87 | -6.10 | <.001 | -.54 | -5.03 | -2.58 |
| Female (259) | 20.84 | 7.36 | ||||||
| Sleep quality | Male (261) | .85 | .81 | -2.92 | .004 | -.27 | -.35 | -.07 |
| Female (259) | 1.07 | .84 | ||||||
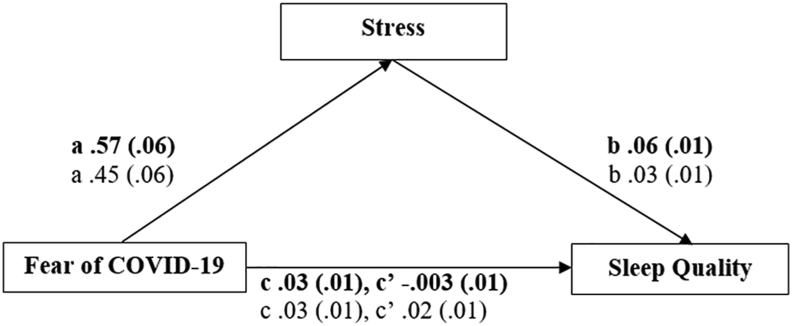
Correlation coefficient results, displayed in Table 1, and mediation analyses results, in Table 3, confirmed Hypothesis 2. Results regarding the correlation coefficients in Table 1 showed significant correlations (low to moderate) between study variables for both males (ranging between .22 and .51) and females (ranging between .26 and .28). In Table 3, a mediation analysis for males was presented as model 1 and model 2 for the female sample. In model 1, results showed a significant total effect of COVID-19 fear (B = .03, SE = .01, p < .001, R2 = .05) on sleep quality. COVID-19 fear was also a strong predictor of stress (B = .57, SE = .06, p < .001, R2 = .26). In the final step, the mediator (stress) was the significant predictor of sleep quality (B = .06, SE = .01, p < .001), but COVID-19 fear was a non-significant predictor (B = -.003, SE = .01, p > .05). Both variables contributed 21% variability of sleep quality. These results in model 1 suggest that stress fully mediated the association between fear of the COVID-19 disease and sleep quality for males.
Table 3.
Mediating effects of stress on the association between fear of the COVID-19 disease and sleep quality.
| Model | Antecedent | Consequent |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total effect on Sleep quality (Y) |
Stress (M) |
Sleep quality (Y) |
|||||||||||
| B | SE | LLCI | ULCI | B | SE | LLCI | ULCI | B | SE | LLCI | ULCI | ||
| 1 | FoC (X) | .03∗∗∗ | .01 | .01 | .05 | .57∗∗∗ | .06 | .46 | .70 | -.003 | .01 | -.02 | .01 |
| Stress (M) | .06∗∗∗ | .01 | . 04 | .07 | |||||||||
| Indirect effect | .03∗∗∗ | .01 | .02 | .04 | |||||||||
| Constant | .34∗ | .15 | .05 | .64 | 6.99∗∗∗ | 1.12 | 4.81 | 9.16 | -.04 | .15 | -.33 | .24 | |
| R2 = .05, F(1, 259) = 13.29, p < .001, f2 = .05 | R2 = .26, F(1, 259) = 92.90, p < .001, f2 = .36 | R2 = .21, F(2, 258) = 34.12, p < .001, f2 = .26 | |||||||||||
| 2 | FoC (X) | .03∗∗∗ | .01 | .02 | .05 | .45∗∗∗ | .06 | .33 | .57 | .02∗∗ | .01 | .01 | .04 |
| Stress (M) | .03∗∗∗ | .01 | .02 | .04 | |||||||||
| Indirect effect | .01∗∗∗ | .004 | .01 | .02 | |||||||||
| Constant | .39∗ | .15 | .09 | .70 | 11.71∗∗∗ | 1.28 | 9.19 | 14.23 | .05 | .17 | -.29 | .39 | |
| R2 = .08, F(1, 257) = 21.38, p < .001, f2 = .08 | R2 = .18, F(1, 257) = 57.01, p < .001, f2 = .22 | R2 = .13, F(2, 256) = 19.26, p < .001, f2 = .15 | |||||||||||
Model 1: mediation model for males.
Model 2: mediation model for females.
∗p < .05, ∗∗p < .01, ∗∗∗p < .001, X = independent variable, M = mediator variable, Y = dependent variable, SE = standard error, LLCI = lower limit of 95% confidence interval, UCLI = upper limit of 95% confidence interval, FoC = Fear of COVID-19 disease, f2 = effect size.
In model 2, results show that COVID-19 fear's total effect on sleep quality was significant (B = .03, SE = .01, p < .001, R2 = .08). COVID-19 fear also significantly associated with the mediator variable, stress (B = .45, SE = .06, p < .001, R2 = .18). In the final step, both COVID-19 fear (B = .02, SE = .01, p < .01) and stress (B = .03, SE = .01, p < .001) were significant predictors of sleep quality. Both variables contributed 13% variability of sleep quality. Overall, the mediation results in model 2 suggest that stress partially mediates the association between fear of the COVID-19 disease and sleep quality for females. Figure 1 demonstrates the mediation results for both males and females.
Figure 1.
Mediating role of stress in COVID-19 fear predicting sleep quality for both males and females. Bolded values are beta coefficients for males.
Discussion
The COVID-19 pandemic is a global health emergency that could potentially have a severe impact on public health. Fear of the COVID-19 disease is one of the most frequent psychological reactions among people during the current pandemic. The present study investigated the influence of fear of the COVID-19 disease on sleep quality and examined whether perceived stress mediates this association. Thus, two hypotheses were formulated to assess the association between study variables, and the results confirmed both hypotheses. Results suggested significantly higher COVID-19 fear, perceived stress, and poorer subjective sleep quality among females than males. These findings indicated that women are psychologically more vulnerable during the current pandemic. Results regarding these differences are consistent with previous findings (Ahmed et al., 2020b; Bitan et al., 2020; Caci et al., 2020; Fatima et al., 2016; Fitzpatrick et al., 2020; Guadagni et al., 2020; Madrid-Valero et al., 2017; Matud, 2004; Reznik et al., 2020; Rodríguez-Hidalgo et al., 2020; Russo et al., 1985; Tang et al., 2017). Females generally show greater stress responsiveness than males (Hasler, 2010), and they have higher levels of fear of death and death anxiety than men (Dattel and Neimeyer, 1990). The higher prevalence of the fear of death and death anxiety might be important reasons for higher COVID-19 fear among females. Biological and psychological factors have also been shown to contribute to these differences; as women were reported to be more sensitive to stress hormones and threats, less likely to use adaptive coping strategies, and more likely to provide negative appraisals to emergencies than men (Verma et al., 2011). Women are also at higher risk of developing stress-related symptoms as they have more caregiving responsibilities and are expected to balance work and household tasks in all types of situations (Cleary, 1987, p. 39; Li and Graham, 2017; Li et al., 2020; Liu et al., 2021). These differences might lead women to report greater subjective sleep disturbances than men. Guadagni et al. (2020) have suggested depression, anxiety, and trauma as significant predictors of sleep quality and insomnia among women. Women, young adults, and those who are uncertain about the possibility of being infected with COVID-19 are more likely to develop sleep problems (Casagrande et al., 2020).
As there were significant differences in study variables, the hypothesized mediational model was tested separately for males and females. Results revealed a significant association between fear of the COVID-19 disease, stress, and sleep quality for both males and females. A mediation analysis’ results showed COVID-19 fear as a significant predictor of sleep quality, and this association was fully mediated by perceived stress for males and partially mediated by perceived stress for females. This result, regarding the association between COVID-19 fear and stress, was consistent with previous studies (Bitan et al., 2020; Islam et al., 2020; Jakovljevic et al., 2020; Restubog et al., 2020). Bitan et al. (2020) also suggested a stronger association of COVID-19 fear with anxiety and stress than with depression. Moreover, in terms of other psychological COVID-19 impacts, several studies have suggested the association between COVID-19 fear and mental health (e.g., Ahorsu et al., 2020a, b; Bitan et al., 2020, Khattak et al., 2020; Salehi et al., 2020). Xiao et al. (2020) have suggested that both anxiety and stress are associated with poor sleep quality in this pandemic, as both anxiety and stress reduce the social capital of sleep quality. Additionally, association between increased stress and lower sleep quality depicted in the present study were found to be consistent with previous studies (Brand et al., 2011; Charles et al., 2011; Gerber et al., 2010; Murata et al., 2007; Sadeh et al., 2004; Xu et al., 2016). In research higher stress levels have also been associated with worse self-reported health, deterioration of sleep quality, decreased well-being, higher levels of depression, increased disability, and cognitive impairment (De Beurs et al., 1999; Hossain et al., 2019; Lynch, 2000; Richardson et al., 2010; Wilson et al., 2011; Wolitzky-Taylor et al., 2010; Zhang et al., 2020).
The present study presented a novel finding to explain the underlying mechanism for poor sleep quality during the current pandemic. Mediational results also demonstrated that COVID-19 fear and perceived stress did not equally contribute to sleep quality of both males (21% variability) and females (13% variability). Differences in psychological responses (i.e., anxiety, stress, etc.) in this challenging time might be a factor that contributes to this gender difference in sleep quality.
In summary, our results indicated a greater vulnerability in women to be affected by many psychological distresses during the COVID-19 pandemic. Therefore, the present study's findings will help the authorities better understand how the fear of the COVID-19 disease is impacting the general Bangladeshi population. These findings can also be used to help inform effective policies implemented to control the transmission rate of COVID-19, without increasing psychological distress. These results also point to the need to design interventions and psychosocial support to reduce the negative impacts of the COVID-19 outbreak on people's mental health.
Limitations
Some limitations of the current study need to be acknowledged. First, the data were collected through an online survey using self-reported scales. Data collected using a self-reported questionnaire might be subjected to social desirability bias. Second, the present study sample was selected through a non-probability sampling technique. Due to the method of sample selection, the generalizability of the findings might be limited, and potential users should use cautiously. Third, sleep quality was assessed by one question of the PSQI (subjective sleep quality). This single item assessment might induce measurement error. Finally, our study did not control which participants were in quarantine zones and which were not. The quarantine can amplify adverse psychological reactions to COVID-19 (Rossi et al., 2020). Future studies should aim to address the limitations of the present study mentioned above. Moreover, future research should explore longitudinal studies to assess the changes in the perceived stress, fear of the COVID-19 disease, and sleep quality. Additionally, future studies should consider other the variables like personality, COVID-19 infection, and mental health outcomes (depression, PTSD symptoms, and OCD symptoms).
Conclusion
COVID-19 is adding vigorously to the incidence of psychological concerns. The present study exhibited that stress significantly mediated the relationship between perceived fear of the COVID-19 disease and sleep quality. It urges for the implications of some statutory mental health support services to reduce the negative impact of the COVID-19 outbreak on people's mental health. Considering the present circumstances, tele-counseling would be effective for rendering psychological support to reduce the perceived stress and improve sleep quality. Although some private mental health support centres provide tele-counseling support, these are insufficient to meet the vast demand due to the current pandemic. The government should come forward with a guideline for rendering mental health support in this pandemic and take the initiative to provide mental health support (e.g., tele-counseling, psychological first aid, etc.). As women are more vulnerable in terms of higher stress and fear of the COVID-19 disease and poorer sleep quality than males, mental health policy and support programs should pay special attention to females' psychological needs.
Declarations
Author contribution statement
Rumana Ferdousi Siddique: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Oli Ahmed: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Kazi Nur Hossain: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We sincerely acknowledge language editing support from Mary C. Jobe of The George Washington University.
References
- Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiat. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed O., Ahmed M.Z., Alim S.M.A.H.M., Khan M.D.A.U., Jobe M.C. COVID-19 outbreak in Bangladesh and associated psychological problems: an online survey. Death Stud. 2020;1–10 doi: 10.1080/07481187.2020.1818884. [DOI] [PubMed] [Google Scholar]
- Ahmed O., Hossain K.N., Siddique R.M., Jobe M.C. 2020. Personality Traits, Fear of COVID-19, Stress, and Sleep Quality.https://osf.io/qut94/ Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed O., Hossain K.N., Siddique R.M., Jobe M.C. COVID-19 fear, stress, sleep quality and coping activities during lockdown, and personality traits: a person-centered approach analysis. Pers. Indiv. Differ. 2021;178:110873. doi: 10.1016/j.paid.2021.110873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addiction. 2020 doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu D.K., Imani V., Lin C.Y., Timpka T., Broström A., Updegraff J.A., Arestedt K., Griffiths M.D., Pakpour A.H. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: an actor-partner interdependence modelling. Int. J. Ment. Health Addiction. 2020 doi: 10.1007/s11469-020-00340-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Åkerstedt T., Orsini N., Petersen H., Axelsson J., Lekander M., Kecklund G. Predicting sleep quality from stress and prior sleep – a study of day-to-day covariation across six weeks. Sleep Med. 2012;13(6):674–679. doi: 10.1016/j.sleep.2011.12.013. [DOI] [PubMed] [Google Scholar]
- Andrade E.F., Pereira L.J., Oliveira A.P.L., Orlando D.R., Alves D.A.G., Guilarducci J.S., Castelo P.M. Perceived fear of COVID-19 infection according to sex, age and occupational risk using the Brazilian version of the Fear of COVID-19 Scale. Death Stud. 2020:1–10. doi: 10.1080/07481187.2020.1809786. [DOI] [PubMed] [Google Scholar]
- Beck F., Leger D., Fressard L., Peretti-Watel P., Verger P., Coconel G. Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. J. Sleep Res. 2021;30(1):e13119. doi: 10.1111/jsr.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beidel D.C., Alfano C.A., Kofler M.J., Rao P.A., Scharfstein L., Wong Sarver N. The impact of social skills training for social anxiety disorder: a randomized controlled trial. J. Anxiety Disord. 2014;28(8):908–918. doi: 10.1016/j.janxdis.2014.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatti A., Haq A. The pathophysiology of perceived social isolation: effects on health and mortality. Cureus. 2017;9(1):994. doi: 10.7759/cureus.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitan D.T., Grossman-Giron A., Bloch Y., Mayer Y., Shiffman N., Mendlovic S. Fear of COVID-19 Scale: psychometric characteristics, reliability and validity in the Israeli population. Psychiatr. Res. 2020;289:113100. doi: 10.1016/j.psychres.2020.113100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand S., Beck J., Kalak N., Gerber M., Kirov R., Pühes U., Hatzinger M., Holsboer E. Dream recall and its relationship to sleep, perceived stress, and creativity among adolescents. J. Adolesc. Health. 2011;49(5):525–531. doi: 10.1016/j.jadohealth.2011.04.004. [DOI] [PubMed] [Google Scholar]
- Buysse D.J., Reynolds C.F., III, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. J. Psychiatr. Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Caci B., Miceli S., Scrima F., Cardaci M. Neuroticism and fear of COVID-19. The interplay between boredom, fantasy engagement, and perceived control over time. Front. Psychol. 2020;11:574393. doi: 10.3389/fpsyg.2020.574393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Cacioppo S. Social relationships and health: the toxic effects of perceived social isolation. Soc. Personal. Psychol. Compass. 2014;8(2):58–72. doi: 10.1111/spc3.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles L.E., Slaven J.E., Mnatsakanova A., Ma C., Violanti J.M., Fekedulegn D., Andrew M.E., Vila B.J., Burchfiel C.M. Association of perceived stress with sleep duration and sleep quality in police officers. Int. J. Emerg. Ment. Health. 2011;13(4):229–241. [PMC free article] [PubMed] [Google Scholar]
- Cleary P.D. Gender differences in stress-related disorders. In: Barnett R.C., Biener L., Baruch G.K., editors. Gender and Stress. Free Press; 1987. pp. 39–72. [Google Scholar]
- Cohen S., Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S., Oskamp S., editors. The Social Psychology of Health. Sage Publishers; 1988. [Google Scholar]
- Dattel A.R., Neimeyer R.A. Sex differences in death anxiety: testing the emotional expressiveness hypothesis. Death Stud. 1990;14(1):1–11. [Google Scholar]
- De Beurs E., Beekman A.T.F., van Balkom A.J.L.M., Deeg D.J.H., van Dyck R., van Tilburg W. Consequences of anxiety in older persons: its effect on disability, well-being and use of health services. Psychol. Med. 1999;29(3):583–593. doi: 10.1017/s0033291799008351. [DOI] [PubMed] [Google Scholar]
- Dou F., Wang M.H., Gao X. Effect of study pressure on sleep quality of senior three students: a moderated mediating model. Chin. J. Clin. Psychol. 2019;27(6):1275–1278+1282. [Google Scholar]
- Eliasson A.H., Kashani M., Mayhew M. Reducing perceived stress improves sleep quality: a longitudinal outcomes study. Chest. 2010;138(4):913A. [Google Scholar]
- Epel E.S., Crosswell A.D., Mayer S.E., Prather A.A., Slavich G.M., Puterman E., Mendes W.B. More than a feeling: a unified view of stress measurement for population science. Front. Neuroendocrinol. 2018;49:146–169. doi: 10.1016/j.yfrne.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatima Y., Doi S.A.R., Najman J.M., Mamun A.A. Exploring gender difference in sleep quality of young adults: findings from a large population study. Clin. Med. Res. 2016;14(3-4):138–144. doi: 10.3121/cmr.2016.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychol. Trauma: Theo. Res. Pract. Pol. 2020;12(S1):S17–S21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Folkman S., Lazarus R.S. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J. Pers. Soc. Psychol. 1985;48(1):150–170. doi: 10.1037//0022-3514.48.1.150. [DOI] [PubMed] [Google Scholar]
- Folkman S., Lazarus R.S., Dunkel-Schetter C., DeLongis A., Gruen R.J. Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. J. Pers. Soc. Psychol. 1986;50(5):992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- Gao C., Scullin M.K. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020;73:1–10. doi: 10.1016/j.sleep.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber M., Hartmann T., Brand S., Holsboer-Trachsler E., Pühse U. The relationship between shift work, perceived stress, sleep and health in Swiss police officers. J. Crim. Justice. 2010;38(6):1167–1175. [Google Scholar]
- Guadagni V., Umilta’ A., Iaria G. Sleep quality, empathy, and mood during the isolation period of the COVID-19 pandemic in the Canadian population: females and women suffered the most. Front. Glob. Wom. Health. 2020;1:585938. doi: 10.3389/fgwh.2020.585938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addiction. 2020:1–14. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler G. Pathophysiology of depression: Do we have any solid evidence of interest to clinicians? World Psych. 2010;9(3):155–161. doi: 10.1002/j.2051-5545.2010.tb00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. Guilford Press; 2013. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. [Google Scholar]
- Hefez A., Metz L., Lavie P. Long-term effects of extreme situational stress on sleep and dreaming. Am. J. Psychiatr. 1987;144(3):344–347. doi: 10.1176/ajp.144.3.344. [DOI] [PubMed] [Google Scholar]
- Hossain S., Anjum A., Hasan M.T., Uddin M.E., Hossain M.S., Sikder M.T. Self-perception of physical health conditions and its association with depression and anxiety among Bangladeshi university students. J. Affect. Disord. 2019;263:282–288. doi: 10.1016/j.jad.2019.11.153. [DOI] [PubMed] [Google Scholar]
- Islam M.N. Psychometric properties of the Bangla version of PSS-10: is it a single factor measure or not. Hellenic J. Psychol. 2020;17(1):15–34. [Google Scholar]
- Islam S.M.D.-U., Bodrud-Doza M., Khan R.M., Haque M.A., Mamun M.A. Exploring COVID-19 stress and its factors in Bangladesh: a perception-based study. Heliyon. 2020;6(7) doi: 10.1016/j.heliyon.2020.e04399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrami H., BaHammam A.S., Bragazzi N.L., Saif Z., Faris M., Vitiello M.V. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J. Clin. Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakovljevic M., Bjedov S., Jaksic N., Jakovljevic I. COVID-19 Pandemia and public and global mental health from the perspective of global health security. Psychiatr. Danub. 2020;32(1):6–14. doi: 10.24869/psyd.2020.6. [DOI] [PubMed] [Google Scholar]
- Kassim M.A.M., Pang N.T.P., Mohamed N.H., Kamu A., Ho C.M., Ayu F., Rahim S., Omar A., Jeffree M.S. Relationship between fear of COVID-19, psychopathology and sociodemographic variables in Malaysian population. Int. J. Ment. Health Addiction. 2021:1–8. doi: 10.1007/s11469-020-00444-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khattak S.R., Saeed I., Rehman S.U., Fayaz M. Impact of fear of COVID-19 pandemic on the mental health of nurses in Pakistan. J. Loss Trauma. 2020 [Google Scholar]
- Kim H.-Y. Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor. Dent. Endo. 2013;38:52–54. doi: 10.5395/rde.2013.38.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocevska D., Blanken T.F., Van Someren E.J.W., Rosler L. Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep Med. 2020;76:86–88. doi: 10.1016/j.sleep.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowal M., Coll-Martin T., Ikizer G., Rasmussen J., Eichel K., Studzinska A., Koszalkowska K., Karwowski M., Najmussaqib A., Pankowski D., Lieberoth A., Ahmed O. Who is the most stressed during the COVID-19 pandemic? Data from 26 countries and areas. Appl. Psychol. Health Well Being. 2020;12(4):946–966. doi: 10.1111/aphw.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R.S. Oxford University Press; 1991. Emotion and Adaptation. [Google Scholar]
- Lazarus R.S., Folkman S. Springer; 1984. Stress, Appraisal and Coping. [Google Scholar]
- Lazarus R.S., DeLongis A., Folkman S., Gruen R. Stress and adaptational outcomes: the problem of confounded measures. Am. Psychol. 1985;40(7):770–779. [PubMed] [Google Scholar]
- Li S.H., Graham B.M. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiat. 2017;4(1):73–82. doi: 10.1016/S2215-0366(16)30358-3. [DOI] [PubMed] [Google Scholar]
- Li S.W., Zhao Z.X., Pan J.Y. Consensus on definition, diagnosis and medication therapy of insomnia. Chin. J. Neurol. 2006;39:141–143. [Google Scholar]
- Li G., Miao J., Wang H., Xu S., Sun W., Fan Y., Zhang C., Zhu S., Zhu Z., Wang W. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J. Neurol. Neurosurg. Psychiatr. 2020;91(8):895–897. doi: 10.1136/jnnp-2020-323134. [DOI] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xu Y., Cai L., Ma S., Wang Y., Cai Z., Du H., Li R., Kang L., Zheng H., Liu Z., Zhang B. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J. Psychiatr. Res. 2021;137:393–400. doi: 10.1016/j.jpsychires.2021.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch S.M. Measurement and prediction of aging anxiety. Res. Aging. 2000;22(5):533–558. [Google Scholar]
- Madrid-Valero J.J., Martínez-Selva J.M., do Couto B.R., Sánchez-Romera J.F., Ordoñana J.R. Age and gender effects on the prevalence of poor sleep quality in the adult population. Gac. Sanit. 2017;31(1):18–22. doi: 10.1016/j.gaceta.2016.05.013. [DOI] [PubMed] [Google Scholar]
- Martinez-Lezaun I., Santamaria-Vazquez M., Del Libano M. Influence of confinement by COVID-19 on the quality of sleep and the interests of university students. Nat. Sci. Sleep. 2020;12:1075–1081. doi: 10.2147/NSS.S280892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matud M.P. Gender differences in stress and coping styles. Pers. Indiv. Differ. 2004;37(7):1401–1415. [Google Scholar]
- Mellman T.A., David D., Kulick-Bell R., Hebding J., Nolan B. Sleep disturbance and its relationship to psychiatric morbidity after Hurricane Andrew. Am. J. Psychiatr. 1995;152(11):1659–1663. doi: 10.1176/ajp.152.11.1659. [DOI] [PubMed] [Google Scholar]
- Murata C., Yatsuya H., Tamakoshi K., Otsuka R., Wada K., Toyoshima H. Psychological factors and insomnia among male civil servants in Japan. Sleep Med. 2007;8(3):209–214. doi: 10.1016/j.sleep.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Pakpour A.H., Griffiths M.D. The fear of COVID-19 and its role in preventive behaviors. J. Concurr. Disord. 2020;2(1):58–63. [Google Scholar]
- Redeker N.S., Conley S., Anderson G., Cline J., Andrews L., Mohsenin V., Jacoby D., Jeon S. Effects of cognitive behavioral therapy for insomnia on sleep, symptoms, stress, and autonomic function among patients with heart failure. Behav. Sleep Med. 2020;18(2):190–202. doi: 10.1080/15402002.2018.1546709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restubog S.L.D., Ocampo A.C.G., Wang L. Taking control amidst the chaos: emotion regulation during the COVID-19 pandemic. J. Vocat. Behav. 2020;119:103440. doi: 10.1016/j.jvb.2020.103440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reznik A., Gritsenko V., Konstantinov V., Khamenka N., Isralowitz R. COVID-19 fear in eastern Europe: validation of the fear of COVID-19 scale. Int. J. Ment. Health Addiction. 2020 doi: 10.1007/s11469-020-00283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson T.M., Simning A., He H., Conwell Y. Anxiety and its correlates among older adults accessing aging services. Int. J. Geriatr. Psychiatr. 2010;26(1):31–38. doi: 10.1002/gps.2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Hidalgo A.J., Pantaleón Y., Dios I., Falla D. Fear of COVID-19, stress, and anxiety in university undergraduate students: a predictive model for depression. Front. Psychol. 2020;11:591797. doi: 10.3389/fpsyg.2020.591797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Di Marco A., Rossi A., Siracusano A., Di Lorenzo G. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front. Psych. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin G.J., Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- Russo J., Miller D., Vitaliano P.P. The relationship of gender to perceived stress and distress in medical school. J. Psychosom. Obstet. Gynecol. 1985;4(2):117–124. [Google Scholar]
- Sadeh A., Keinan G., Daon K. Effects of stress on sleep: the moderating role of coping style. Health Psychol. 2004;23(5):542–545. doi: 10.1037/0278-6133.23.5.542. [DOI] [PubMed] [Google Scholar]
- Salehi L., Rahimzadeh M., Molaei E., Zaheri H., Esmaelzadeh-Saeieh S. The relationship among fear and anxiety of COVID-19, pregnancy experience, and mental health disorder in pregnant women: a structural equation model. Brain Behav. 2020;10 doi: 10.1002/brb3.1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang J., Liao Y., Kelly B.C., Xie L., Xiang Y.-T., Qi C., Pan C., Hao W., Liu T., Zhang F., Chen X. Gender and regional differences in sleep quality and insomnia: a general population-based study in Hunan Province of China. Sci. Rep. 2017;7:43690. doi: 10.1038/srep43690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S.E. sixth ed. McGraw-Hill; 2006. Health Psychology. [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Development and initial validation of the COVID stress scales. J. Anxiety Disord. 2020;72:102232. doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempesta D., Curcio G., De Gennaro L., Ferrara M. Long-Term impact of earthquakes on sleep quality. PloS One. 2013;8(2) doi: 10.1371/journal.pone.0055936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher K., Durkin J., Bhullar N. The COVID-19 pandemic and mental health impacts. Int. J. Ment. Health Nurs. 2020;29:315–318. doi: 10.1111/inm.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma R., Balhar Y.P.S., Gupta C.S. Gender differences in stress response: role of developmental and biological determinants. Indian Psychiatr. J. 2011;20(1):4–10. doi: 10.4103/0972-6748.98407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voitsidis P., Gliatas I., Bairachtari V., Papadopoulou K., Papageorgiou G., Parlapani E., Syngelakis M., Holeva V., Diakogiannis I. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatr. Res. 2020;289 doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. J. Am. Med. Assoc. 2020;323(14):1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson R.S., Begeny C.T., Boyle P.A., Schneider J.A., Bennett D.A. Vulnerability to stress, anxiety, and development of dementia in old age. Am. J. Geriatr. Psychiatr. 2011;19(4):327–334. doi: 10.1097/JGP.0b013e31820119da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor K.B., Castriotta N., Lenze E.J., Stanley M.A., Craske M.G. Anxiety disorders in older adults: a comprehensive review. Depress. Anxiety. 2010;27(2):190–211. doi: 10.1002/da.20653. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2021. WHO Coronavirus (COVID-19) Dashboard.https://covid19.who.int/ Retrieved from. [Google Scholar]
- Xiao H., Zhang Y., Kong D. Social capital and sleep quality in individuals who self-Isolated for 14 days during the Coronavirus Disease 2019 (COVID-19) outbreak in January 2020 in China. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. 2020;26:e923921-1–e923921-8. doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q., Zhao Y., Chen H., Jing J. Exploring sleep quality and related factors in Chinese midlife women. Health Care Women Int. 2016;37(6):620–635. doi: 10.1080/07399332.2015.1037443. [DOI] [PubMed] [Google Scholar]
- Yan Y.W., Liu M.Y., Tang X.D., Lin R.M. On the relationship among stress response, coping and sleep quality. Adv. Psychol. Sci. 2010;18(11):1734–1746. [Google Scholar]
- Zhang K., Zhang W., Wu B., Liu S. Anxiety about aging, resilience and health status among Chinese older adults: findings from Honolulu and Wuhan. Arch. Gerontol. Geriatr. 2020;88:104015. doi: 10.1016/j.archger.2020.104015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.