Abstract
Dentinogenesis imperfecta (DGI) type II affects both primary and permanent dentitions and has the autosomal mode of inheritance. The affected teeth may appear as amber or gray because of chipping of enamel shortly after their eruption. Correct diagnosis and management are highly needed to restore the quality of oral health and to improve esthetics and masticatory functions. We present here a case of systematic and conservative dental approach in the management of a 7-year-old child having Dentinogenesis Imperfecta Type II (DGI Type II) with 1 ½ follow-up.
Keywords: Dental management, dentinogenesis imperfecta, mixed dentition
INTRODUCTION
The genetic mutations during the formation of dentine organic matrix result in hereditary dentin disorders, namely dentinogenesis imperfect (DGI) and dentin dysplasia.[1] Robert and Schour in 1939 used the terminology, “DGI,” to describe the opalescent teeth that usually known as Capdepont's teeth and tulip teeth. Shields in 1973[2] further categorized DGI into three types: DGI Type I associated with osteogenesis imperfecta occurs due to genetic mutations in collagen type 1, COL1A1 and COL1A2 and is usually associated with osteogenesis imperfecta. DGI Type II and DGI Type III are caused by a mutation in genes encoding for dentin sialophosphoprotein gene.[3]
Shield's DGI Type I: intraorally, it is presented as amber and translucent teeth with significant attrition. Radiographically, constricted short roots are seen along obliterated pulp because of dentin hypertrophy.[2] Shield's DGI Type II: clinically, it has similar features of DGI Type I with presence of bulbous crowns and marked constriction at cementoenamel junction with the absence of osteogenesis imperfecta.[2] Shield's DGI Type III: Also known as Brandywine isolate, firstly seen in the tri-racial population from Maryland and Washington DC. The clinical features are similar to those of DGI Type I and II. Radiographically, they are described as shell teeth because of the hollow appearance created by wide pulp chambers.
Histologically, coarse and less number of dentinal tubules is seen in circumferential dentin with nonscalloped dentinoenamel junction.[4] Mantle dentin is usually unaffected. The area of void dentinal tubules also seen in dentin with less number of odontoblasts.
The teeth affected with DGI, primarily the posterior teeth undergoes severe and rapid attrition because of defective dentin formation leading to the loss of occlusal vertical dimension.[1] Multiple teeth with pulpal exposures occur as a result of rapid attrition which may also be associated with dental abscesses. Treatment in mixed dentition is quite challenging and requires frequent follow-ups to monitor the eruption sequence and status of permanent teeth.
CASE REPORT
A 7-year-old male child reported to the department of pediatric and preventive dentistry with a chief complaint of brownish discoloration in all teeth since eruption along with multiple missing teeth for 2 years. The patient also gave a history of delayed eruption of deciduous teeth, difficulty in chewing food due to increased sensitivity to hot and cold. Child also had a medical history of undergoing heart surgery in which cardiac pacemaker was placed for the correction of atrial septal in defect 5 years ago. There was no systemic association of any bone abnormality.
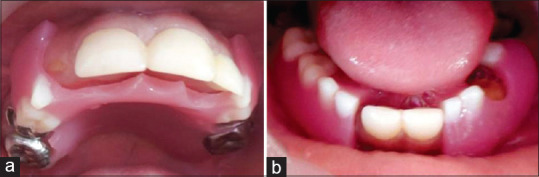
Clinical examination revealed mixed dentition with tulip shaped, opalescent brown-colored teeth with marked cervical constriction at cementoenamel junction in both primary and permanent dentition. Furthermore, multiple missing teeth and deep caries with pulpal involvement were observed in all the primary teeth. Over retained and grossly decayed primary maxillary right central incisor was present along with permanent maxillary right central incisor erupting palatally [Figure 1a]. Primary maxillary left and right canines were grossly decayed with the presence of only root stumps [Figure 1a]. Primary mandibular left second molar and right first molars had deep caries along with Grade III mobility [Figure 1b]. Permanent mandibular right first molar was already restored 6 months ago in some private dental clinic.
Figure 1.
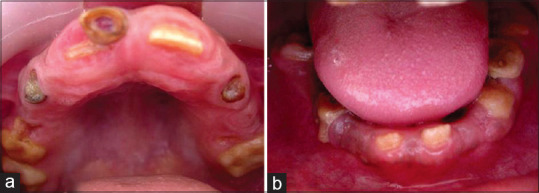
(a) Preoperative view of the maxillary arch. (b) Preoperative view of the mandibular arch
The panoramic radiograph revealed both the dentitions were affected having bulbous crowns with short roots. All the teeth had enlarged pulp chambers and a very little dentin giving them a characteristic shell tooth appearance [Figure 2]. Based on the clinical and radiographical findings, provisional diagnosis of DGI Type II was made.
Figure 2.
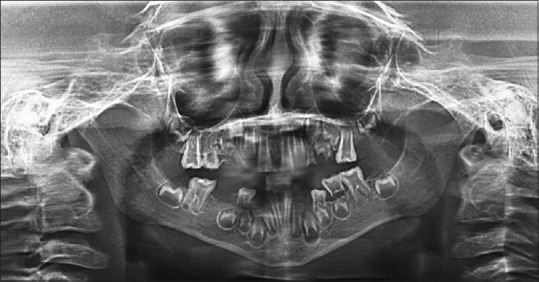
Orthopantomogram revealing enlarged pulp chambers giving characteristic Shell tooth appearance
Treatment plan was based on the clinical guidelines by American Academy of Pediatric Dentistry (AAPD)[5] that included extraction of nonrestorable teeth, preventive, functional, and esthetic rehabilitation. Diet counseling was done as child was on high cariogenic diet and oral hygiene instructions were given as a part of preventive measure to be taken at home. Behavior management was done by tell-show-do technique, distraction by showing him cartoons and making positive reassurances. The patient was treated on the dental chair under local anesthesia. Antibiotic prophylaxis regimen was followed before the extractions of primary maxillary right central incisor, primary maxillary left and right canines, primary mandibular left second molar, and primary mandibular right first molar.
Primary mandibular first molar was sectioned and histopathological examination was carried out to make the final diagnosis. Decalcified H&E stained section of dentin shows the presence of irregular fewer tubules with large areas of hypocalcified matrix. Area of void dentinal tubules is also seen [Figure 3a]. Ground section of the present case showed irregular and fewer dentinal tubules throughout the section [Figure 3b]. Final diagnosis of DGI Type II was made.
Figure 3.
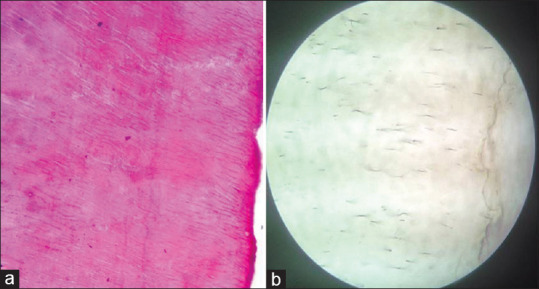
(a) Decalcified H&E-stained section of dentin. (b) Ground section showing irregular and fewer dentinal tubules
Stainless steel crown was placed on primary maxillary right second molar and permanent maxillary left and right first molars as a preventive measure to prevent their breakdown in future [Figure 4a]. Stainless crowns on permanent mandibular first molars were also the part of treatment plan, but parents insisted for the esthetic correction first including the management of the space visible due to multiple missing and extracted teeth. Maxillary and mandibular impressions were made with alginate impression material and resulting dental stone casts were mounted on a semi-adjustable articulator with the use of centric record. Maxillary and mandibular removable functional space maintainers were fabricated and delivered to improve masticatory functions and restore clinical vertical height [Figure 4b-d]. Esthetic rehabilitation was achieved by placing Pedoform Strip crowns to do minimal cutting and avoid pulpal exposures on all four permanent maxillary and mandibular central incisors [Figure 4b-d]. Once the esthetic correction was achieved and child's masticatory function was established, the patient did not turn up for the preventive measures planned for permanent mandibular first molars.
Figure 4.

(a) Postoperative view showing stainless steel crown placed. (b) Pedoform strip crowns placed on permanent maxillary and mandibular central incisors. (c and d) Restored vertical heights by placing maxillary and mandibular removable functional space maintainers
The patient came back after 1 year with a chief complaint of intermittent pain in the lower left and right back tooth region for 2 months. Intraoral examination revealed deep caries with positive tender on percussion in permanent mandibular first molars of the left and right side. Furthermore, permanent maxillary left lateral incisor and maxillary left first premolar were erupting in the oral cavity. Panoramic radiograph revealed deep caries involving pulp in permanent mandibular first molars with the presence of dental abscess in permanent mandibular left first molar [Figure 5]. The child continued to wear the space maintainers, but Pedoform strip crowns on permanent maxillary and mandibular central incisors were missing. Functional space maintainer was modified to allow the eruption of permanent maxillary left lateral incisor and maxillary left first premolar [Figure 6a and b]. Calcium hydroxide apexification was carried out in permanent mandibular first molars. Laboratory-fabricated heat cured acrylic crowns using the indirect technique were placed on permanent maxillary central incisors, permanent maxillary left lateral incisor and permanent mandibular central incisors to achieve better retention [Figure 6c].
Figure 5.
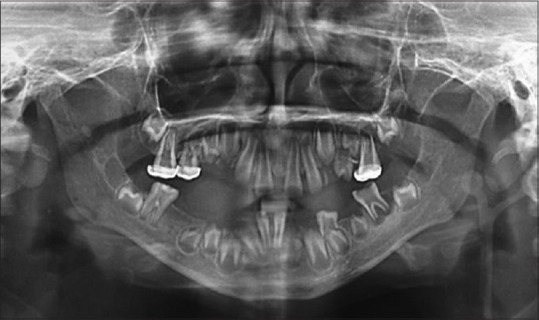
OPG revealing deep caries involving pulp in permanent mandibular first molars
Figure 6.
(a and b) Functional space maintainer modification done. (c) Laboratory fabricated heat-cured acrylic crowns placed
The patient was again recalled after 3 months to monitor the eruption status of permanent teeth. Intraoral examination revealed erupting permanent maxillary right lateral incisor. Modification in the design of functional space maintainer to allow the eruption of permanent maxillary right lateral incisor [Figure 7a and b]. Heat-cured acrylic crowns and stainless steel crowns were intact. Every 3 months follow-up was scheduled for them.
Figure 7.
(a and b) Functional space maintainer modification done
DISCUSSION
Patients with DGI present with unesthetic appearance due to the presence of opalescent brown colored teeth, compromised masticatory functions because severe attrition leading to pain shortly after the eruption of teeth. Initially, in DGI Type I and II pulp chambers may also be abnormally wide giving shell teeth appearance radiogroaphically that obliterate later on due to hypertrophied dentine.[2] This explains the shell tooth appearance in our presented case of DGI Type II.
As DGI Type II affects both the dentitions, therefore, treatment requires long follow-ups with the management of every single tooth erupting into the oral cavity leading to increase in cost of treatment. Frequent visits, socioeconomic status of the parents, understanding the psychology and managing the child accordingly are some of the major challenges in treating the young child that should not be overlooked. The esthetic concerns of the patient has to be considered as it impacts on their psychosocial behavior.[6]
Enamel chips off soon after the eruption because of underlying defective dentin, thus necessitating the preventive approach at earlier stage including full coverage of posterior teeth with stainless steel crowns and on anterior teeth with esthetic crowns such as celluloid strip crowns, indirect resin crowns or polycarbonate crowns.[5,7,8] In the presented case, all teeth were short and fragile, therefore, Pedoform strip crowns were first attempted to avoid further weakening of the tooth structure. But DGI was of severe type that may have resulted in poor adhesion to composite restoration explaining the poor retention of strip crowns.[9,10] Laboratory fabricated heat cured-acrylic crowns using indirect technique in the presented case proved more beneficial in terms of durability and function. Preserving the arch length in mixed dentition phase allows the eruption of permanent teeth in correct position, thus avoiding impacted teeth or orthodontic treatment in future. The functional space maintainers helped in maintenance of arch length along with restoring clinical vertical dimension and masticatory functions. The abnormal eruption sequence of permanent teeth made it important to design the appliances which were easily modifiable and also economic for the patient. Therefore, removable maxillary and mandibular functional space maintainers were preferred over fixed appliances to allow the eruption of permanent teeth along with maintaining the masticatory function and esthetics in the presented case.
CONCLUSION
Early management of teeth with DGI is imperative that includes behavior management, comprehensive, functional and esthetic correction. Composite restorations including Pedoform strip crowns may not give long-lasting results due to the biochemical changes in tooth structure affected with severe type of DGI. Frequent and long-term follow-ups are needed to prevent and intercept the future dental anomalies.
Why this paper is important for pediatric dentists?
DGI is not a common occurring dental anomaly. Its correct diagnosis is very crucial to improve the prognosis of the planned treatment. The anatomy and structure of affected teeth makes it highly difficult to achieve the desired results of the procedures that are routinely carried out with high success in patients not having DGI. This article also highlights the problems associated in managing a young fearful child having mixed dentition with abnormal eruption sequence and to provide the dental care accordingly by using multidisciplinary approach to minimize the need of future orthodontic treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Butler WT. Dentin matrix problems. Eur J Oral Sci. 1998;106:204–10. doi: 10.1111/j.1600-0722.1998.tb02177.x. [DOI] [PubMed] [Google Scholar]
- 2.Shields ED, Bixler D, el-Kafrawy AM. A proposed classification for heritable human dentine defects with a description of a new entity. Arch Oral Biol. 1973;18:543–53. doi: 10.1016/0003-9969(73)90075-7. [DOI] [PubMed] [Google Scholar]
- 3.Dong J, Gu T, Jeffords L, MacDougall M. Dentin phosphoprotein compound mutation in dentin sialophosphoprotein causes dentinogenesis imperfecta type III. Am J Med Genet A. 2005;132A:305–9. doi: 10.1002/ajmg.a.30460. [DOI] [PubMed] [Google Scholar]
- 4.Waltimo J, Ranta H, Lukinmaa PL. Ultrastructure of dentin matrix in heritable dentin defects. Scanning Microsc. 1995;9:185–97. [PubMed] [Google Scholar]
- 5.American Academy of Pediatric Dentistry. Guideline on Dental Management of Heritable Dental Developmental Anomalies. Pediatr Dent. 2016;38:302–7. [PubMed] [Google Scholar]
- 6.Davis LG, Ashworth PD, Spriggs LS. Psychological effects of anesthetic dental treatment. J Dent. 1998;26:547–54. doi: 10.1016/s0300-5712(97)00031-6. [DOI] [PubMed] [Google Scholar]
- 7.Sapir S, Shapira J. Dentinogenesis imperfecta: An early treatment strategy. Pediatr Dent. 2001;23:232–7. [PubMed] [Google Scholar]
- 8.Stewart RE, Luke LS, Pike AR. Preformed polycarbonate crowns for the restoration of anterior teeth. J Am Dent Assoc. 1974;88:103–7. doi: 10.14219/jada.archive.1974.0018. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki S, Nakata M, Eto K. Clinical and histological observations of opalescent dentin associated with enamel defects. Oral Surg Oral Med Oral Pathol. 1977;44:767–74. doi: 10.1016/0030-4220(77)90386-3. [DOI] [PubMed] [Google Scholar]
- 10.Sapir S, Shapira J. Clinical solutions for developmental defects of enamel and dentin in children. Pediatr Dent. 2007;29:330–6. [PubMed] [Google Scholar]



