Abstract
The World Health Organization (WHO) announced that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may spread through aerosols, so-called airborne transmission, especially in a poorly ventilated indoor environment. Ventilation protects the occupants against airborne transmission. Various studies have been performed on the importance of sufficient ventilation for diluting the concentration of virus and lowering any subsequent dose inhaled by the occupants. However, the ventilation situation can be problematic in public buildings and other shared spaces, such as shops, offices, schools, and restaurants. If ventilation is provided by opening windows, the outdoor airflow rate depends strongly on the specific local conditions (opening sizes, relative positions, climatic and weather conditions).
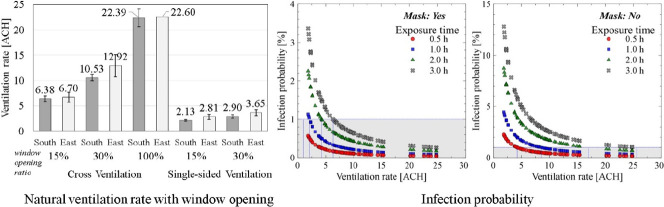
This study uses field measurements to analyze the natural ventilation performance in a school building according to the window opening rates, positions, and weather conditions. The ventilation rates were calculated by the tracer gas decay method, and the infection risk was assessed using the Wells-Riley equation. Under cross-ventilation conditions, the average ventilation rates were measured at 6.51 h−1 for 15% window opening, and 11.20 h−1 for 30% window opening. For single-sided ventilation, the ventilation rates were reduced to about 30% of the values from the cross-ventilation cases. The infection probability is less than 1% in all cases when a mask is worn and more than 15% of the windows are open with cross-ventilation. With single-sided ventilation, if the exposure time is less than 1 h, the infection probability can be kept less than 1% with a mask. However, the infection probability exceeds 1% in all cases where exposure time is greater than 2 h, regardless of whether or not a mask is worn. Also, when the air conditioner was operated with a window opening ratio of 15%, power consumption increased by 10.2%.
Keywords: Coronavirus disease 2019 (COVID-19), Airborne transmission, Natural ventilation, Air changes per hour (ACH), Infection probability, Classroom
Graphical abstract
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is thought to spread primarily from human to human, by close and direct contact transmission, as well as through larger respiratory droplets of >5–10 μm in diameter (WHO, 2020a). However, viral transmission via small airborne micro-droplets and particles (referred to as ‘aerosols’, ≤1 μm) has received considerable attention (Domingo et al., 2020; Hadei et al., 2020; Klompas et al., 2020; Morawska and Cao, 2020). Smaller virus-containing respiratory droplets and particles can remain suspended in the air over long distances and time periods. Airborne transmission of SARS-CoV-2 can occur under special circumstances such as enclosed spaces, prolonged exposure to respiratory particles and inadequate ventilation or air handling. Transmission of Coronavirus Disease 2019 (COVID-19) in a confined space was 18.7 times greater compared to an open-air environment (Nishiura et al., 2020). Ten persons from three families who had eaten at the same air-conditioned restaurant X in Guangzhou, China, were infected by the inadequate inner circulated airflow of the air conditioner (Lu et al., 2020). However, the staff who served food to the infected person in restaurant X were not infected, which suggests that exposure time influences the infection risk.
The evidence for airborne transmission of COVID-19 is currently incomplete, and some hospital-based studies have carried out air sampling for SARS-CoV-2. SARS-CoV-2 genomic RNA has been detected in airborne material collected by air samplers positioned distal to COVID-19 patients (Chia et al., 2020; Guo et al., 2020; Liu et al., 2020; Santarpia et al., 2020). Respiratory virus can survive aerosolization and poses an inhalation biohazard risk. Doremalen et al. experimentally generated aerosol particles with SARS-CoV-2 and found that the virus remained viable during a three-hour testing period (Van Doremalen et al., 2020). Fears et al. reported that the virus retained infectivity and integrity for up to 16 h in laboratory-created respirable-sized aerosols (Fears et al., 2020).
Increased rates of transmission occur in buildings where people are likely to be in the presence of an infected person in a crowded indoor space for relatively long periods of time and, therefore, exposed to airborne particles (Hu et al., 2020). There is also clear evidence that poor ventilation contributes to the spread of other airborne diseases, such as tuberculosis and SARS (Li et al., 2007). Ventilation that already exists can be enhanced easily at a relatively low cost to reduce the number of infections and consequently to save lives. Ventilation is the process of providing outdoor air to a space or building by natural or mechanical means (ISO, 2017b). Appropriate distribution of outdoor clean air ensures that adequate dilution is achieved where and when needed, avoiding the build-up of viral contamination (Melikov, 2011; Thatiparti et al., 2016; Thatiparti et al., 2017).
Klompas et al. stressed the importance of well-ventilated space, arguing that exposure to an infected person in a poorly ventilated space allows otherwise insignificant amounts of virus-laden aerosols to accumulate (Klompas et al., 2020). Also, Morawska and Milton emphasize the importance of sufficient and effective ventilation for supplying clean outdoor air in public spaces to slow the spread of the virus (Morawska and Milton, 2020). In particular, natural ventilation (NV) has been widely suggested and successfully implemented in handling various epidemic diseases historically, and NV can be an effective solution in preventing viral spread where costly mechanical ventilation (MV) systems are not installed (Zhai, 2020). The American Society of Heating, Ventilating, and Air-Conditioning Engineers (ASHRAE) and the Federation of European Heating, Ventilation and Air Conditioning Associations (REHVA) have recognized potential airborne hazards indoors and recommended ventilation control measures accordingly (ASHRAE, 2020; REHVA, 2020). The design, operation and maintenance of naturally ventilated facilities is not straightforward, and comprehensive guidance is available (Chartier and Pessoa-Silva, 2009). For instance, in March the WHO specified that in a COVID-19 infective ward at least 160 L/s/patient have to be provided if natural ventilation is used (WHO, 2020b).
In public buildings and other shared spaces, such as shops, offices, schools, kindergartens, libraries, restaurants, elevators, conference rooms and public transport, ventilation systems range from purpose-designed mechanical systems to simply relying on open doors and windows. The ventilation rates of these facilities are significantly lower than in hospitals for various reasons, including limiting airflow for energy and cost savings.
Previous studies quantified the required ventilation rate to prevent the spread of viral infections using the infection probability index (Andrade et al., 2018; Noakes and Sleigh, 2008; Riley, 1982; Sun and Zhai, 2020). The Wells–Riley equation is a classic model for quantifying the risk associated with airborne transmission of respiratory diseases (Riley et al., 1978). The building factors, particularly the ventilation rate, are important removal mechanisms for airborne infectious agents (Escombe et al., 2007). Hui Dai and Bin Zhao reported that in order to keep the infection probability below 1% when staying in a school classroom for 2 h, the ventilation rate should be 2 ACH with a mask and 7 ACH without a mask (Dai and Zhao, 2020).
In this study, we examined the natural ventilation performance in a school building by field measurement, and the infection probability was estimated according to the natural ventilation rate. School classrooms often keep close due to draught and outside noise, and their occupancy density is very high, making them very vulnerable to virus infection. The universal goal is to prioritize the reopening of schools as safely and as quickly as possible. The United Nations Educational, Scientific and Cultural Organization (UNESCO), United Nations Children's Fund (UNICEF), World Food Programme (WFP) and World Bank issued guidelines on the safe reopening of schools amidst ongoing closures affecting nearly 1.3 billion students worldwide. Accordingly, the Korean government issued guidelines for natural ventilation of classrooms for school reopening. Classrooms are to be ventilated by opening more than 30% of the classroom windows during class. In a condition of high outdoor air temperature in summer, it is recommended that an air conditioner be used with the windows open. However, there is no quantitative basis for the 30% window opening criteria, and there is no specification of cross- or single-sided ventilation, which is an important issue in natural ventilation performance. In addition, there is a concern about additional power consumption due to an increase in the cooling load by opening the windows while the air conditioner is operating.
This study aims to quantify the natural ventilation performance according to the window opening conditions and infection probability to answer the question, “what is the sufficient natural ventilation rate in the recent COVID-19 situation” in a school classroom. The issues related to open-window ventilation, air conditioning, and infection probability were analyzed as follows: (1) quantify the natural ventilation rate according to the window opening rate and ventilation method (cross- and single-sided ventilation), (2) identify the probability of infection according to the natural ventilation rate, (3) analyze the amount of additional power consumed by operating air conditioners under natural ventilation.
2. Methods
2.1. Quantification of natural ventilation rate
The tracer gas decay method is used in a wide range of diagnostic techniques, including leak detection and ventilation rate measurements in buildings (Sherman, 1990). The tracer gas decay method is suitable because it requires the least amount of tracer gas, relatively simple equipment, and a minimal level of data analysis (Okuyama and Onishi, 2012). The tracer gas decay method using CO2 gas as tracer gas can be expressed by:
| (1) |
where C in, t and C in, 0 is the tracer gas concentration at any time point and the beginning of the record time period, respectively. C out is the outdoor gas concentration. N is the ventilation flow rate.
The ventilation rate due to window opening can fluctuate in real time depending on indoor and outdoor temperature difference and external wind velocity. In addition, the CO2 concentration sprayed indoors with window opening condition can be diluted in a very short time. In order to secure measurement reliability using short-time measurement data, the multipoint decay method was used to calculate the ventilation rate. The formula is as follows (Cui et al., 2015; ISO, 2017a).
| (2) |
2.2. Evaluation of the infection risk: Wells-Riley equation
The Wells-Riley model is a simple and quick evaluation method of the airborne infection risk, because it uses the concept of quantum to implicitly consider the infectivity, infectious source strength, biological decay of pathogens, etc. The Wells–Riley equation is as follows (Riley et al., 1978):
| (3) |
where P is the probability of infection risk; C is the number of cases that develop infection; and S is the number of susceptible people. I is the number of infectors; in this study, thus, we assumed I = 1. The variable p is the pulmonary ventilation rate of susceptible people (m3/h); p = 0.3 m3/h when people are sitting or participating in light activity indoors (Duan, 2013). Q is the room ventilation rate (m3/h); q is the quantum generation rate by an infected person (h−1); and t is the exposure time (h).
The unit “quantum” in Wells-Riley equation, can be defined as the required threshold number of infectious airborne particles that can infect susceptible people (Riley et al., 1978; Yan et al., 2017). When the exposure time and ventilation rate are known, quantum generation rate can be calculated from Eq. (3) epidemiologically from an outbreak case (Sze To and Chao, 2010).
The filtration efficiency of mask is defined as the percentage of a contaminant removed by the mask filter (Dbouk and Drikakis, 2020). The filtration effect of a mask can dilute the concentration of exhaled pathogens in infected person and inhaled pathogens in susceptible people. The filtration efficiency of general medical surgical masks, against aerosols containing viruses, can be set as 50% considering the influence of air leakage (Davies et al., 2013).
The modified Wells–Riley equation with mask filtration efficiency is as follows:
| (4) |
where η I , η S are mask efficiencies for the infected person and susceptible person, respectively. The quantum generation rate of COVID-19 (q) ranged from 10.5–48 h−1 (Buonanno et al., 2020; Dai and Zhao, 2020). Therefore, q is defined as 48, meaning a greater likelihood of being infected.
2.3. Field measurement
2.3.1. Overview of the field measurement
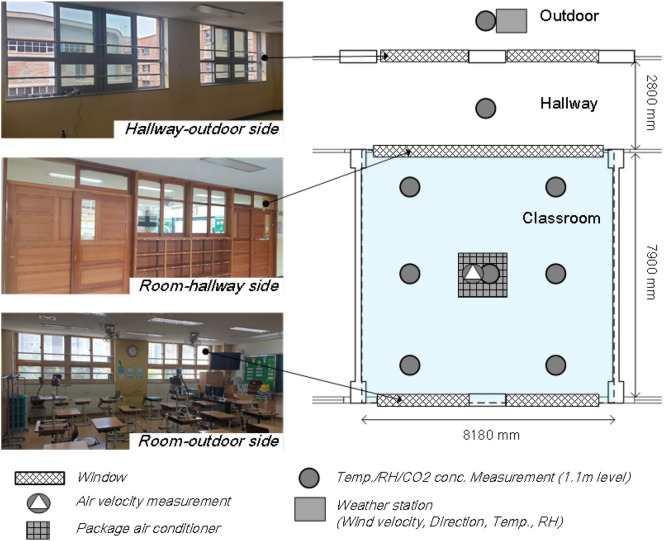
Three classrooms at an elementary school located in Suwon, Korea, were selected as the test spaces. The area of the rooms were 64.62 m2, their volumes were 168.0 m3, and all rooms were located on the 4th floor. Each test classroom was equipped with a package air conditioner. The measurements were performed during May 14–29, 2020. As shown in Fig. S1, to analyze the dependence of natural ventilation performance on wind speed and wind direction, classrooms facing south (Rooms 1 and 2) and a classroom facing east (Room 3) were analyzed simultaneously. The characteristics of the analyzed classroom are shown in Table S1.
As shown in Fig. 1 , the windows of the room-outdoor side and the hallway-outdoor side consist of a total of four pairs of upper and lower windows. On the room-hallway side, there are windows above the doors and between the doors. Detailed explanations of measurements and equipment installation locations are shown in Table S2 and Fig. 1. Outdoor environmental conditions including temperature, relative humidity, CO2 concentration, outdoor wind velocity, and wind direction were measured on the rooftop of the target school building, where there was no wind shielding effect. CO2 gas was injected at a high concentration in a room with all windows and doors closed, and tracer gas was diffused into the room with a mixing fan. Then the windows were opened to measure the indoor tracer gas concentration histories. Indoor temperature, relative humidity, and CO2 level were measured at seven points in the test room. The indoor air velocity was measured at the mid-point of the target classroom to identify draft perception. Thermal comfort research literature indicates that indoor air speed in hot climates should be set between 0.2 and 1.50 m/s, yet 0.2 m/s has been deemed in ASHRAE Standard 55 to be the threshold of draft perception inside air-conditioned buildings (ANSI/ASHRAE, 2017).
Fig. 1.
Field measurement configurations.
The air conditioner was operated with the window open, assuming that the indoor temperature can increase excessively due to the opening of windows in the summer season. The air conditioner set temperature was 25 °C, and the air volume was set to low wind volume to prevent excessive mixing of indoor air. The power consumption was measured for 2.5 h at window opening ratios of 0%, 15%, and 30% (cross-ventilation) with air conditioner operation.
2.3.2. Window opening conditions
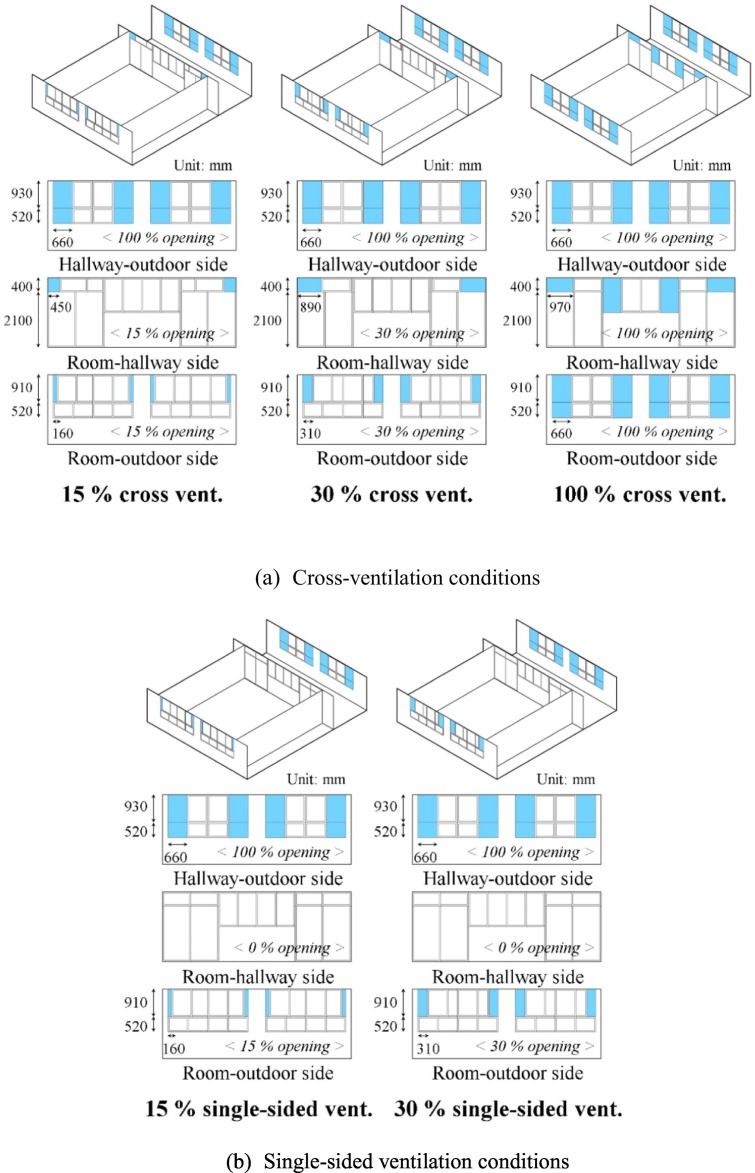
Fig. 2 is a schematic diagram of the window opening conditions analyzed in this study. In this study, cross-ventilation means opening both the room-outdoor side and the room-hallway side windows. Single-sided ventilation means that the windows on the room-hallway side are closed, and only the windows on the room-outdoor side are opened.
Fig. 2.
Window opening conditions (blue shading indicates open windows). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
The window opening ratio is defined as the ratio of the opened window area to the maximum openable window area. The upper windows of the classroom are opened so that high-temperature outdoor air does not mix with the cold air of the lower part of the room and passes through the upper part of the room to discharge pollutants from the upper part of the room. The hallway-outdoor side windows are always 100% open for smooth movement of the airflow. The openable window area is 3.78 m2 for the room-outdoor side, 2.37 m2 for the room-hallway side, and 3.83 m2 for the outdoor-hallway side. In the case of cross-ventilation, the total opening areas for each opening ratio were 0.94, 1.84, and 6.15 m2 for 15, 30, and 100%, respectively; for single-sided ventilation, opening areas were 0.58 and 1.13 m2 for opening ratios of 15 and 30%, respectively. The basis for calculating the opening areas is shown in Table S3.
2.3.3. Case configuration
The measurement cases are shown in Table 1 . The analyzed cases were constructed according to the window opening ratio and cross- or single-sided ventilation. The asterisk mark (*) indicates an additional case with air conditioner activated. The ventilation rate and infection probability were compared between classrooms on the south side (Rooms 1 and 2) to analyze the dependence on the ventilation method (window opening ratio and cross- or single-sided ventilation). The ventilation rate and infection probability were compared between the east side classroom (Room 3) and the south side classrooms (Rooms 1 and 2) to analyze the dependence of natural ventilation performance on wind direction.
Table 1.
The analyzed cases.
| Case | Ventilation method |
|
|---|---|---|
| Cross- or single-sided ventilation | Opening ratio | |
| Base casea | – | 0% (closed) |
| Case 1–1a | Cross-ventilation | 15% |
| Case 1–2a | 30% | |
| Case 1–3 | 100% | |
| Case 2–1 | Single-sided ventilation | 15% |
| Case 2–2 | 30% | |
Additional case tested with air conditioner operation.
3. Results and discussion
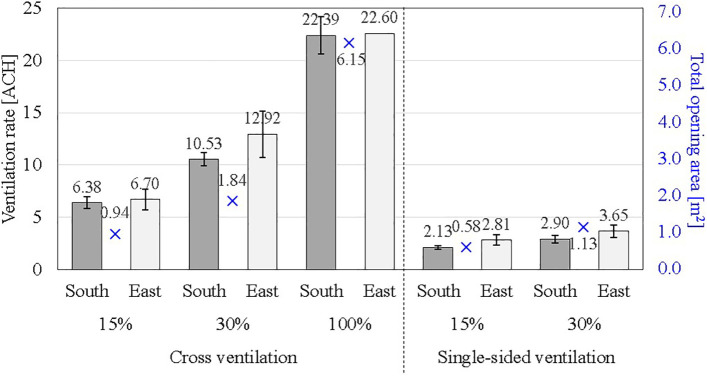
3.1. Natural ventilation rate with the window opening ratio
Infiltration rates of the analyzed classroom with both windows and doors closed were 0.30, 0.29, 0.32 h−1, which is very tight. Natural ventilation rates according to window opening ratio and ventilation methods (cross or single-sided) were quantified in the same outdoor conditions for three analyzed classrooms. The outdoor temperature during the field measurement periods was 25.82 ± 3.69° C, and the wind velocity was 0.96 ± 0.45 m/s, corresponding to typical summer conditions in Korea (Choi and Song, 2020). The results of the ventilation rate according to the window opening rates and ventilation strategy are shown in Table 2 and Fig. 3 .
Table 2.
Ventilation rates according to window opening ratio.
| Case | Ventilation strategy |
Measurement results |
Outdoor conditions |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cross- or Single-sided ventilation | Opening ratio | Ventilation rate [ACHb], indoor air velocity [m/s] | South side |
East side |
Wind velocity [m/s] | Wind direction [°] | Temp. difference [°C] | |||||
| Mean | SD | Na | Mean | SD | Na | |||||||
| Base case | – | 0% | ACH | 0.30 | 0.00 | 2 | 0.32 | – | 1 | 0.41 | 0 | 6.20 |
| Case 1–1 | Cross-ventilation | 15% | ACH, m/s |
6.38 0.08 |
1.85 0.03 |
11 – |
6.70 0.10 |
2.57 0.02 |
7 – |
0.70 | 292.5 – |
2.79 – |
| Case 1–2 | 30% | ACH, m/s |
10.53 0.12 |
2.61 0.03 |
18 – |
12.92 0.19 |
5.81 0.04 |
7 – |
1.05 | 0 – |
3.87 – |
|
| Case 1–3 | 100% | ACH, m/s |
22.39 0.24 |
3.98 0.07 |
5 – |
22.60 0.19 |
– – |
1 – |
1.06 | 0 – |
3.28 – |
|
| Case 2–1 | Single-sided ventilation | 15% | ACH, m/s |
2.13 0.05 |
0.23 0.01 |
2 – |
2.81 0.06 |
0.86 0.01 |
3 – |
0.84 | 292.5 – |
3.01 – |
| Case 2–2 | 30% | ACH, m/s |
2.90 0.05 |
0.74 0.02 |
4 – |
3.65 0.07 |
1.20 0.02 |
4 – |
1.12 | 0 – |
3.96 – |
|
Bold emphasizes ACH - the most important value in this table.
N: number of measurements.
ACH: air changes per hour.
Fig. 3.
Ventilation rate according to window opening method.
Under cross-ventilation conditions, the average ventilation rate in the south-side room was measured at 6.38 h−1 for 15% window opening, 10.53 h−1 for 30%, and 22.39 h−1 for 100%. Compared to the results for 15% opening, the ventilation rate increased 1.7 times with 30% opening and 3.5 times with 100% opening.
For single-sided ventilation, the ventilation rate was 2.13 h−1 for 15% window opening and 2.90 h−1 for 30%; these ventilation rates are about 33% and 28%, respectively, of the rates of the cross-ventilation cases. Even though the total window opening area of the 30% opening single-sided ventilation case (1.13 m2) was greater than that of the 15% opening cross-ventilation case (0.94 m2), the ventilation rate was higher under the cross-ventilation cases.
Even under the same ventilation method and outdoor conditions, the ventilation rate varies depending on the wind direction. The ventilation rate of Room 3, with east-facing windows, was slightly higher than those of Rooms 1 and 2, with south-facing windows. However, there was not much difference in ventilation rate depending on the wind direction because of the low outdoor wind velocity (≤1.5 m/s) during the measurement periods.
When there is a large amount of natural ventilation, the indoor airflow becomes strong, and there is a risk of contamination transmission or the spread of viruses by airflow. Fig. S2 indicate the results of indoor air-velocity according to the ventilation rates. In all cases analyzed in this study, the indoor air-velocity was less than 0.3 m/s. This means that people can barely feel air movement due to natural ventilation, and the local discomfort is minimal. This is because the outdoor wind speed was kept below 1 m/s during 63% of the experimental periods (summer season in Korea).
3.2. Infection probability
The exposure time used in calculating the infection probability ranged from 0.5 h (the unit class time of the elementary school) to 3 h (the maximum lecture time of the university). The reference ventilation rates are the measured values in this study.
Table 3 indicates the infection probability according to the ventilation rate, exposure time, and status of mask wearing. The red text indicates infection probabilities exceeding 1%. The base case with closed windows shows a high infection probability of more than 1% (3.46–57.20%) in all cases. However, if more than 15% of the windows are open under cross-ventilation conditions, a ventilation rate above 6 h−1 (air changes per hour, ACH) is secured, and the infection probability is less than 1% in all cases when a mask is worn.
Table 3.
Infection probability results.
| Case | Ventilation strategy |
Ventilation rate [ACH] | Ventilation volume [CMH] | Infection probability [%] |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.5 h |
1 h |
2 h |
3 h |
|||||||||
| Cross- or single-sided ventilation | Opening ratio | Mask: Y | Mask: N | Mask: Y | Mask: N | Mask: Y | Mask: N | Mask: Y | Mask: N | |||
| Base case | – | 0% | 0.30 | 50.4 | 3.47 | 13.19 | 6.83 | 24.64 | 13.19 | 43.21 | 19.12 | 57.20 |
| Case 1–1 | Cross-ventilation | 15% | 6.51 | 1093.7 | 0.16 | 0.66 | 0.33 | 1.31 | 0.66 | 2.59 | 0.98 | 3.87 |
| Case 1–2 | 30% | 11.20 | 1181.6 | 0.10 | 0.38 | 0.19 | 0.76 | 0.38 | 1.51 | 0.57 | 2.26 | |
| Case 1–3 | 100% | 22.43 | 3768.2 | 0.05 | 0.19 | 0.10 | 0.38 | 0.19 | 0.76 | 0.29 | 1.14 | |
| Case 2–1 | Single-sided ventilation | 15% | 2.54 | 426.7 | 0.42 | 1.67 | 0.84 | 3.32 | 1.67 | 6.52 | 2.50 | 9.62 |
| Case 2–2 | 30% | 3.28 | 551.0 | 0.33 | 1.30 | 0.65 | 2.57 | 1.30 | 5.08 | 1.94 | 7.53 | |
Under single-sided ventilation conditions, the ventilation rate decreases by more than 60% compared to cross-ventilation, but for exposure time conditions less than 1 h, the infection probability can be limited to less than 1% with a mask. However, the infection probability exceeds 1% in all cases, when exposure time is greater than 2 h, regardless of whether a mask is worn or not.
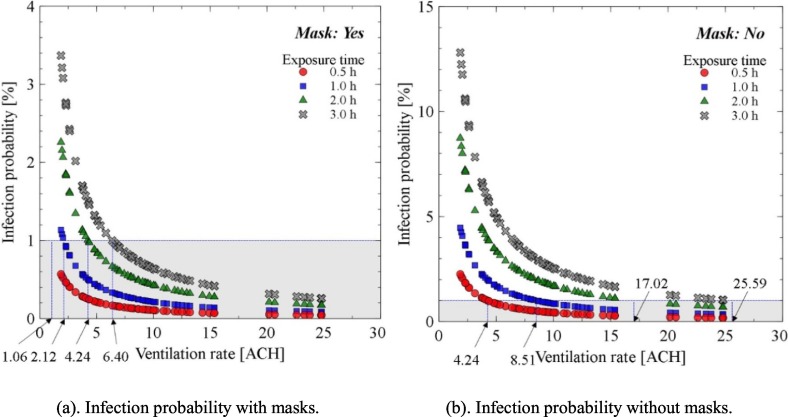
Fig. 4 indicates the infection probability according to the exposure time and the ventilation rate. When wearing a mask, the required ventilation rates to keep the infection probability below 1% should be about 1.06, 2.12, 4.24, and 6.40 h−1, respectively, for the exposure times of 0.5, 1, 2, and 3 h. However, if a mask is not worn, the required ventilation rate should be about 4.24, 8.51, 17.02, and 25.59 h−1, respectively, for exposure times of 0.5, 1, 2, and 3 h.
Fig. 4.
Infection probability according to ventilation rate by exposure time.
The lower the ventilation rate and the longer the exposure time, the higher the risk of infection. The infection probability increases arithmetically as the exposure time increases under the same ventilation rate conditions. In 0.5 h exposure time, the infection probability stays less than 1% with the ventilation rate of 1.87 h−1.
3.3. Measurement of power consumption by air conditioner under natural ventilation conditions
There is a concern about an increase in cooling power consumption when an air conditioner is operated with natural ventilation. Experiments were conducted on the increase of the amount of natural ventilation and the cooling consumption of air conditioners according to the window opening rate in Rooms 1 and 2. The outdoor air temperature was 28.7–29.8 °C, and the set-point temperature of the air conditioner was 25 °C during measurements.
The ventilation rate was measured at 5.15 ± 0.48 ACH under 15% open conditions and 8.93 ± 0.90 ACH under 30% open conditions. The ventilation rate decreased by 19.3% and 15.2% for the 15% open and 30% open conditions, respectively, when the air conditioner was operated. This is because the airflow from the air conditioner pressurizes the room, reducing the differential pressure, which is the driving force of natural ventilation.
When the air conditioner was operating and the window opening rates were 0%, 15%, and 30%, the power consumption per hour was measured at 0.83, 0.92, and 1.02 kW, respectively (Fig. 5 ). In other words, the cooling energy consumption increased by 10.2% and 22.5% when the windows were opened by 15% and 30%, respectively, compared to the usage when the window was closed. Even with natural ventilation and operation of an air conditioner in the summer, the associated increase in cooling energy was not very high. This is because the temperature difference between indoors and outdoors is not large in summer.
Fig. 5.
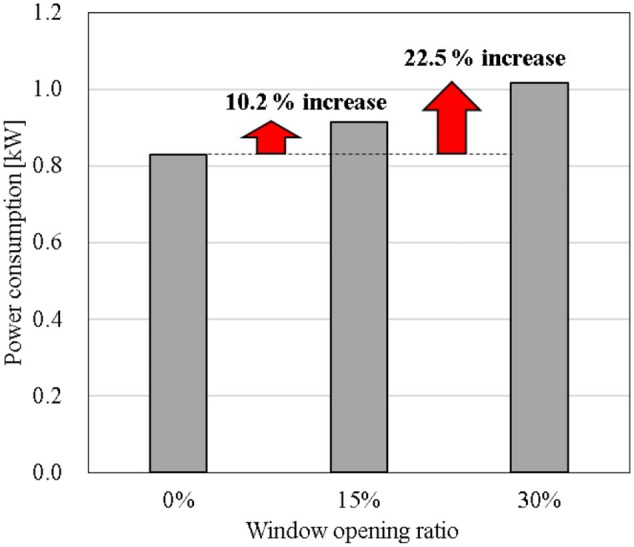
Power consumption according to air conditioner operation and window opening ratio.
3.4. Discussion
Various studies have been performed on the importance of sufficient ventilation for diluting the concentration of virus and lowering any subsequent dose inhaled by the occupants. Even if ventilation can be performed by opening a window, the ventilation rate varies depending on special local conditions such as window opening sizes and positions, single-sided or cross ventilation, and weather conditions.
On the other hand, the infection rate decreases as the ventilation rate increases, but it also varies depending on the exposure time and whether wearing a mask or not. Another issue is the increase in energy demand when the air-conditioner is operated with the window open for ventilation in cooling season, which is also a factor that hinders ventilation. In this regard, the results of this study suggest the following facts.
Even if windows were opened to only 15% of the maximum openable window area, the amount of natural ventilation was about 6 h−1. According to the most recent US guidelines, the ventilation rate should be at least 12 h−1 for newly constructed or renovated airborne infection isolation rooms (AIIRs) and 6 h−1 for existing rooms (ANSI/ASHRAE, 2017; Architects, 2006). This suggests that natural ventilation, where windows in the classroom are opened slightly, can meet the ventilation rate required for infection prevention facilities.
In cross-ventilation under the same opening conditions, the opening area of the window was 1.6 times greater than that of single-sided ventilation conditions, but the ventilation rate was more than 3 times higher. In other words, the ventilation rate per the total opening area was about twice as large for cross-ventilation compared to single-sided ventilation. Cross-ventilation is efficient in terms of air exchange rate compared to single-sided ventilation, and cross-ventilation is recommended to minimize the infection possibility in high-density public buildings. If cross-ventilation is not possible, it is advisable to use an auxiliary fan to achieve the same effect as cross-ventilation.
The infection risk decreases as the natural ventilation rate increases. However, natural ventilation rate by window opening can vary with changes in external environmental conditions. Fig. S3 (a) shows the infection probability according to ventilation rate under the condition of 3 h exposure time and wearing a mask. Even at the same window opening ratio, there is a large deviation in the ventilation rate, leading to a large variation in the risk of infection. At 15% window opening, the average ventilation rate of 6.51 h−1 achieves an average infection probability of less than 1% when wearing a mask, but the values ranged from 0.64 to 2.42%. In other words, a specific window opening ratio does not guarantee a certain ventilation rate and infection probability. To compensate for this, wearing a mask and minimizing exposure time can help prevent infection effectively.
The infection probability can be reduced by about four times when a mask was worn under the same ventilation rate conditions. Even if the ventilation rate is secured around 25 h−1 under conditions of 100% opening condition, as shown in Fig. S3 (b), the infection probability is greater than 1% if a mask is not worn. In contrast, if a ventilation rate of 6.38 h−1 is secured, even after 3 h of exposure time, the infection probability can be kept below 1% with a mask, confirming the importance of wearing a mask.
Natural ventilation as a countermeasure against airborne transmission of the virus is also limited to spring, summer, and fall in Korea when the outside temperature is favorable for indoor thermal environment control. Under conditions where sufficient ventilation is not secured through natural ventilation, it is desirable to reduce the exposure time. Cutting indoor exposure time in half can reduce the risk of infection to about 50%. Melikov et al. (Melikov et al., 2020) emphasized that short room occupation times with long breaks reduces the concentration in the room of aerosols exhaled by infected person. Continuous ventilation is recommended in multi-use facilities, such as offices, schools, libraries and restaurants, in order to promote air dilution around a source and the removal of respiratory viruses.
When an air conditioner is running, if the windows are opened 15%, the power consumption increases by only about 10%. Active natural ventilation is recommended because the cost does not increase significantly, even if an air conditioner is operated with natural ventilation in summer. However, ventilation is essential to prevent infection even in winter, but heating costs increase if you open a window and perform natural ventilation. Heat recovery ventilation is required for continuous ventilation under conditions with large indoor and outdoor temperature differences, such as in winter in Korea.
The limitation of the current study is the Wells–Riley equation assumes well-mixed room air and a steady-state infectious particle concentration which varies with the ventilation rate (Riley et al., 1978). Typically, well-defined airflow pattern exists in practice in a room with natural ventilation. Also, indoor directional airflow might play a role in increasing or reducing the spreading of the infection in indoor environments. In the case of natural ventilation in winter, thermal discomfort and heating energy increase issues should be analyzed. In addition, this measurement was conducted under non-occupancy conditions, but it is also necessary to analyze the case where a person occupies the room. However, the main focus of this study is to analyze the natural ventilation performance as a whole in a school building according to the window opening rates and to examine the possibility of reducing the infection rate through natural ventilation. So we reserved the related issues for further study.
4. Conclusions
Field measurements were used to analyze natural ventilation strategies using window opening in a school building to cope with the current COVID-19 situation. The infection rate was calculated according to the natural ventilation performance, exposure time, and whether a mask was worn. This study suggests an appropriate window opening area to prevent viral air infection that can be applied in real-world conditions. The main results of this study are as follows:
-
(1)
The ventilation rates according to window opening ratios of 15, 30, and 100% under cross-ventilation were measured at 6.51, 11.20, and 22.43 ACH, respectively, in the summer season in Korea.
-
(2)
The infection possibility can be maintained at less than 1% by securing 6.51 ACH (1093.7 CMH), restricting exposure time to less than 3 h and wearing a mask. The Korean government's guidelines for opening windows 30% were found to provide a sufficient natural ventilation rate to prevent airborne virus infection in public buildings.
-
(3)
Wearing a mask can reduce the infection probability by four times compared to not wearing it, and the infection probability increased arithmetically as the exposure time increased. In situations where sufficient ventilation is not available, it is important to wear a mask or minimize exposure time.
-
(4)
Power consumption by an air conditioner increased by 10.2% and 22.5% under opening ratios of 15% and 30%, respectively compared to conditions where all windows were closed and there was no natural ventilation. Even when air conditioning and natural ventilation occur at the same time, the additional cost is not high in the summer in Korea.
-
(5)
Cross-ventilation is efficient in terms of air exchange rate compared to single-sided ventilation, and cross-ventilation is recommended to minimize the infection possibility in high-density public buildings. If cross-ventilation is not possible, it is advisable to use an auxiliary fan to achieve the same effect as cross-ventilation.
CRediT authorship contribution statement
Sowoo Park: Data curation, Investigation, Writing – original draft. Younhee Choi: Investigation, Visualization. Doosam Song: Writing – review & editing. Eun Kyung Kim: Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This work was supported by a National Research Foundation of Korea (NRF) grant (2019M3E7A1113080) funded by the Korean government (MSIT, MOE).
Editor: Pavlos Kassomenos
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2021.147764.
Appendix A. Supplementary data
Supplementary material
References
- Andrade A., Dominski F.H., Pereira M.L., de Liz C.M., Buonanno G. Infection risk in gyms during physical exercise. Environ. Sci. Pollut. Res. 2018;25:19675–19686. doi: 10.1007/s11356-018-1822-8. [DOI] [PubMed] [Google Scholar]
- ANSI/ASHRAE . American Society of Heating, Refrigerating and Air-Conditioning Engineers; Atlanta, GA: 2017. Standard 55–2017: Thermal Environmental Conditions for Human Occupancy. [Google Scholar]
- Architects AIo . AIA Washington; 2006. Guidelines for Design and Construction of Health Care Facilities. [Google Scholar]
- ASHRAE . American Society of Heating, Ventilating, and Air-Conditioning Engineers; 2020. COVID-19 (coronavirus) preparedness resources. [Google Scholar]
- Buonanno G., Stabile L., Morawska L. Estimation of airborne viral emission: quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020;141 doi: 10.1016/j.envint.2020.105794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartier Y., Pessoa-Silva C. World Health Organization; 2009. Natural Ventilation for Infection Control in Health-Care Settings. [PubMed] [Google Scholar]
- Chia P.Y., Coleman K.K., Tan Y.K., Ong S.W.X., Gum M., Lau S.K., et al. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat. Commun. 2020;11:1–7. doi: 10.1038/s41467-020-16670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi Y., Song D. How to quantify natural ventilation rate of single-sided ventilation with trickle ventilator? Build. Environ. 2020;181 [Google Scholar]
- Cui S., Cohen M., Stabat P., Marchio D. CO2 tracer gas concentration decay method for measuring air change rate. Build. Environ. 2015;84:162–169. [Google Scholar]
- Dai H., Zhao B. Building Simulation. vol. 13. Springer; 2020. Association of the infection probability of COVID-19 with ventilation rates in confined spaces; pp. 1321–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies A., Thompson K.-A., Giri K., Kafatos G., Walker J., Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Dis. Med. Public Health Prep. 2013;7:413–418. doi: 10.1017/dmp.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dbouk T., Drikakis D. On respiratory droplets and face masks. Phys. Fluids. 2020;32 doi: 10.1063/5.0015044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domingo J.L., Marquès M., Rovira J. Influence of airborne transmission of SARS-CoV-2 on COVID-19 pandemic. A review. Environ. Res. 2020;414:109861. doi: 10.1016/j.envres.2020.109861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan X. China Environmental Press; Beijing: 2013. Exposure Factors Handbook of Chinese Population. [Google Scholar]
- Escombe A.R., Oeser C.C., Gilman R.H., Navincopa M., Ticona E., Pan W., et al. Natural ventilation for the prevention of airborne contagion. PLoS Med. 2007;4 doi: 10.1371/journal.pmed.0040068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fears A.C., Klimstra W.B., Duprex P., Hartman A., Weaver S.C., Plante K.S., et al. Persistence of severe acute respiratory syndrome coronavirus 2 in aerosol suspensions. Emerg. Infect. Dis. 2020;26:2168. doi: 10.3201/eid2609.201806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Z.-D., Wang Z.-Y., Zhang S.-F., Li X., Li L., Li C., et al. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg. Infect. Dis. 2020;26 doi: 10.3201/eid2607.200885. 10.3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadei M., Hopke P.K., Jonidi A., Shahsavani A. A letter about the airborne transmission of SARS-CoV-2 based on the current evidence. Aerosol Air Qual. Res. 2020;20:911–914. [Google Scholar]
- Hu M., Lin H., Wang J., Xu C., Tatem A.J., Meng B., et al. The risk of COVID-19 transmission in train passengers: an epidemiological and modelling study. Clin. Infect. Dis. 2020;72(4):604–610. doi: 10.1093/cid/ciaa1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISO . International Organization for Standardization (ISO); 2017. B. 12569: 2017. Thermal Performance of Buildings and Materials-Determination of Specific Airflow Rate in Buildings-Tracer Gas Dilution Method. [Google Scholar]
- ISO. B. 17772-1: 2017. Energy performance of buildings. Indoor environmental quality. Indoor environmental input parameters for the design and assessment of energy performance of buildings 2017b.
- Klompas M., Baker M.A., Rhee C. Airborne transmission of SARS-CoV-2: theoretical considerations and available evidence. Jama. 2020;324:441–442. doi: 10.1001/jama.2020.12458. [DOI] [PubMed] [Google Scholar]
- Li Y., Leung G.M., Tang J., Yang X., Chao C., Lin J.Z., et al. Role of ventilation in airborne transmission of infectious agents in the built environment-a multidisciplinary systematic review. Indoor Air. 2007;17:2–18. doi: 10.1111/j.1600-0668.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- Liu Y., Ning Z., Chen Y., Guo M., Liu Y., Gali N.K., et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–560. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Lu J., Gu J., Li K., Xu C., Su W., Lai Z., et al. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China. Emerg. Infect. Dis. 2020;26:1628. doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melikov A.K. Advanced air distribution. ASHRAE J. 2011;53:73–77. [Google Scholar]
- Melikov A.K., Ai Z., Markov D. Intermittent occupancy combined with ventilation: an efficient strategy for the reduction of airborne transmission indoors. Sci. Total Environ. 2020;744 doi: 10.1016/j.scitotenv.2020.140908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Milton D.K. It is time to address airborne transmission of COVID-19. Clin. Infect. Dis. 2020;6 doi: 10.1093/cid/ciaa939. (ciaa939) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishiura H., Oshitani H., Kobayashi T., Saito T., Sunagawa T., Matsui T., et al. Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19) MedRxiv. 2020 doi: 10.1101/2020.02.28.20029272. [DOI] [Google Scholar]
- Noakes C.J., Sleigh P.A. Indoor Air 2008: The 11th International Conference on Indoor Air Quality and Cl. Leeds; 2008. Applying the Wells-Riley equation to the risk of airborne infection in hospital environments: the importance of stochastic and proximity effects. [Google Scholar]
- Okuyama H., Onishi Y. Uncertainty analysis and optimum concentration decay term for air exchange rate measurements: estimation methods for effective volume and infiltration rate. Build. Environ. 2012;49:182–192. [Google Scholar]
- REHVA. COVID-19 guidance. 2020.
- Riley R. Indoor airborne infection. Environ. Int. 1982;8:317–320. [Google Scholar]
- Riley E., Murphy G., Riley R. Airborne spread of measles in a suburban elementary school. Am. J. Epidemiol. 1978;107:421–432. doi: 10.1093/oxfordjournals.aje.a112560. [DOI] [PubMed] [Google Scholar]
- Santarpia J.L., Rivera D.N., Herrera V.L., Morwitzer M.J., Creager H.M., Santarpia G.W., et al. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci. Rep. 2020;10:1–8. doi: 10.1038/s41598-020-69286-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman M.H. Tracer-gas techniques for measuring ventilation in a single zone. Build. Environ. 1990;25:365–374. [Google Scholar]
- Sun C., Zhai Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain. Cities Soc. 2020;62 doi: 10.1016/j.scs.2020.102390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sze To G.N., Chao C.Y.H. Review and comparison between the Wells–Riley and dose-response approaches to risk assessment of infectious respiratory diseases. Indoor Air. 2010;20:2–16. doi: 10.1111/j.1600-0668.2009.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thatiparti D.S., Ghia U., Mead K.R. Assessing effectiveness of ceiling-ventilated mock airborne infection isolation room in preventing hospital-acquired influenza transmission to health care workers. ASHRAE Trans. 2016;122:35. [PMC free article] [PubMed] [Google Scholar]
- Thatiparti D.S., Ghia U., Mead K.R. Computational fluid dynamics study on the influence of an alternate ventilation configuration on the possible flow path of infectious cough aerosols in a mock airborne infection isolation room. Sci. Technol. Built Environ. 2017;23:355–366. doi: 10.1080/23744731.2016.1222212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2020. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations: Scientific Brief, 27 March 2020. [Google Scholar]
- WHO . World Health Organization; 2020. Infection Prevention and Control during Health Care when COVID-19 Is Suspected: Interim Guidance, 19 March 2020. [Google Scholar]
- Yan Y., Li X., Shang Y., Tu J. Evaluation of airborne disease infection risks in an airliner cabin using the Lagrangian-based Wells-Riley approach. Build. Environ. 2017;121:79–92. doi: 10.1016/j.buildenv.2017.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai J. Facial mask: a necessity to beat COVID-19. Build. Environ. 2020;175:106827. doi: 10.1016/j.buildenv.2020.106827. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material