Abstract
The advancement of technology remained an immersive interest for humankind throughout the past decades. Tech enterprises offered a stream of innovation to address the universal healthcare concerns. The novel coronavirus holds a substantial foothold of planet earth which is combatted by digital interventions across afflicted geographical boundaries and territories. This study aims to explore the trends of modern healthcare technologies and Artificial Intelligence (AI) during COVID-19 crisis, define the concepts and clinical role of AI in the mitigation of COVID-19, investigate and correlate the efficacy of AI-enabled technology in medical imaging during COVID-19 and determine advantages, drawbacks, and challenges of artificial intelligence during COVID-19 pandemic.
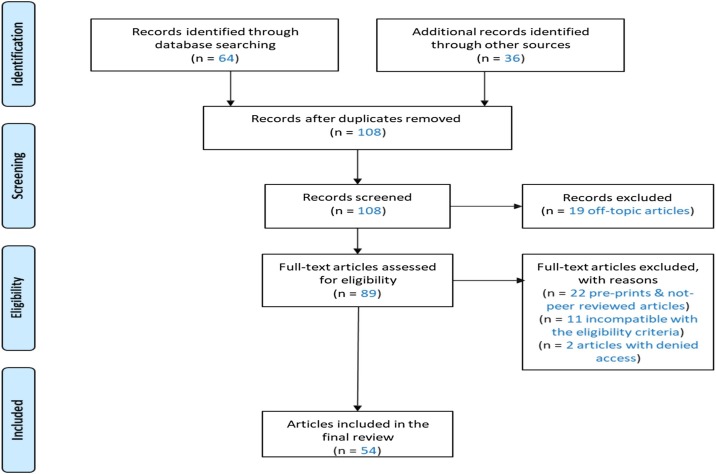
The paper applied systematic review approach using a deliberated research protocol and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart.
Digital technologies can coordinate COVID-19 responses in a cascade fashion that extends from the clinical care facility to the exterior of the pending viral epicenter. With cases of healthcare robotics, aerial drones, and the internet of things as evidentiary examples. PCR tests and medical imaging are the frontier diagnostics of COVID-19. Computed tomography helped to correct the accuracy variation of PCR tests at a clinical sensitivity of 98 %. Artificial intelligence can enable autonomous COVID-19 responses using techniques like machine learning.
Technology could be an endless system of innovation and opportunities when sourced effectively. Scientists can utilize technology to resolve global concerns challenging the history of tangible possibility. Digital interventions have enhanced the responses to COVID-19, magnified the role of medical imaging amid the COVID-19 crisis and have exposed healthcare professionals to the opportunity of contactless care.
Keywords: Healthcare, Digital technologies, Artificial intelligence, Machine learning, COVID-19, Medical imaging
1. Introduction
Humanity had endured the difficulty of pandemics since time immemorial. Historians chronicle the cohabitation between pathological infestations and humankind. Specifically, the viral pathogens that transformed infectious plagues into a cosmopolitan cause throughout the past two decades. These transmissible plagues paralleled the continuity of human civilization, from the walls of ancient settlements to the high-rise skyscrapers of modern times (Bansal et al., 2020).
Early eruptions of global pandemics happened during the 14th century, an era of the incidence of the Bubonic Plague or the Black Death. Ancient anecdotes narrate the discovery of the Black Death in maiden trade ships arriving at European ports. The ships labelled as the “plague ships’’ launched the rapidly communicable plague through medieval Europe (Yue et al., 2017). Studies perceived the Black Death as an evolutionary hallmark in the lineage of global pandemics; depicted through the cultural revolution of medieval art and science. The artisan collections expressed the macabre of the Black Death that claimed 50 million lives in 5 years (Allam, 2020; Getz, 1991). Following the First World War, the year of 1918 marked the succession of the Black Death in the form of the Spanish flu. Medical anthropologists attributed the ecology of the Spanish flu to the H1N1 influenza virus. Follow up research speculated the city of Étaples, France as the source of the outbreak. Epidemiological statistics documented the Spanish flu morbidity at an estimated 500 million infections and 50 million casualties (Killingray, 1994). Subsequently, the cycle of novel pandemics resumed in 1957 with the onset of the Asian flu. This strain of flu was reported in China at a mortality rate of 1.1 million deaths by the time of containment.
A decade later, the world succumbed to the Influenza (A) virus (H3N2) that accounted for around one million deaths since the first reports in Hong Kong. The Chinese public witnessed the original Severe Acute Respiratory Syndrome (SARS) in 2002. SARS caused a total of 774 deaths during the onset of the virus. Several infectious contagions followed the SARS outbreak inclusive of the Swine flu in 2009, the Zaire Ebola Virus in the Democratic Republic of Congo, the Zika Virus in 2015, and COVID-19 in 2019 (Allam, 2020). The novel coronavirus (COVID-19) is a viral infection caused by the eighth strain of coronaviruses or (SARS-CoV-2). COVID-19 commenced in the Chinese city of Wuhan in the Hubei province (Bragazzi et al., 2020; Ko et al., 2020). The world health organization (WHO) maintained the unprecedented communicability of COVID-19 through the WHO coronavirus dashboard. A public web platform was designed to extrapolate the circulation and reported cases of COVID-19. During the inception of this paper, the WHO coronavirus dashboard recorded 37,888,384 confirmed infections and 1,081,868 deaths in 235 countries (World Health Organization, 2020).
SARS-CoV-2 and Black Death airborne pathogens surrounded the world rapidly during their respective periods of discovery and early case accounts. Frontline responders reincarnated the endeavor of centennial plague doctors combating the onslaught of the Black Death (Shamekh et al., 2020). Plague doctors resorted to a protective ensemble of long black coats, black top hats, and beaked masks that concealed fragrant herbs to mask the odor of decomposing corpses scattered around afflicted areas (Glatter and Finkelman, 2020). Flash forward to present times, virologists embarked on the journey of decoding the pathophysiology of COVID-19. The perturbations of the virus included the inconspicuous etiology of COVID-19. Genetic layer classifies SARS- CoV-2 as a single-stranded RNA, beta coronavirus comprised of four principal proteinaceous components: a spike, a membrane, an envelope, and nucleo-capsid proteins (Bragazzi et al., 2020). Spike proteins are surface glycoproteins that facilitate the viral invasion of SARS-CoV-2 in the host cell. Virion penetration is motivated by the interaction between spike protein and the ACE2 (Angiotensin-converting enzyme 2) enzymes. ACE2 is a taxonomy of surface proteins identified in pulmonary tissue, namely, type II alveolar pneumocytes. Viral biosynthesis, replication, and transcription happen in the host cells before the maturation and viral RNA discharge. During cultivation, the assembled virions proceed to congregate and multiply in the cellular cytoplasm (Yuki et al., 2020). The biological reproduction stimulates an immune response that damages the lungs and finalizes the evolution of COVID-19. This unique molecular composition attributes the signature biological transmutation of COVID-19 (Shaikh et al., 2020).
According to the WHO, the clinical presentation of COVID-19 represents a variety of respiratory sequelae. Common manifestations encompassed malaise, muscle aches, fever, dry cough, and shortness of breath. Reciprocally, Acute Respiratory Distress Syndrome (ARDS), pneumonia, multiple organ failure, and death signified the complications of COVID-19 (Xu et al., 2020). The infection comorbidities include obesity, chronic smoking, and chronic cardiac disease. Scientific research concluded a disparity in the chain of infection of COVID-19; COVID-19 showed a cross-species transmission pattern (Tsiknakis et al., 2020). Researchers ascertained this genetic activity during the outbreak’s initial stage in the Hunan Seafood Wholesale market in Wuhan. The virus spreads from bats and other intermediate hosts like pangolins and finally to humans. Thus, facilitating human to human transmission (Bragazzi et al., 2020). Human to human infections can occur through small respiratory droplets and aerosols. Asymptomatic transmissibility is feasible in COVID-19 patients with an appraised incubation period of 2–14 days. Hence, increasing the threat of the virus and the scope of contamination within the infected demographics (Shaikh et al., 2020).
Furthermore, the complex morphology of COVID-19 formed an additional level of difficulty for healthcare professionals worldwide. Primarily, the scarcity in clinical specificity of COVID 19 (Tsiknakis et al., 2020). The healthcare society expresses clinical specificity as a reproducible metric measuring the probability of a negative diagnostic result (Hussain et al., 2020). This scarcity stimulated the sharp spike and frequency in reported COVID-19 cases (O. S. Albahri, Zaidan, et al., 2020). Therefore, unearthing existing vulnerabilities within healthcare infrastructure systems (HIS) in international governments and territories. COVID-19 leveraged global HIS systems to the limit of collapse in a variety of clinical circumstances. For instance, the shortage of healthcare professionals with seniority, and disease’s experience, lack of testing supplies that rectify false positive and false negative diagnostic readings (Kim et al., 2020). Frontline responders are subjected to psychological anxiety and an unprecedented patient influx daily. Such phenomenon fosters human error consequent to the execution of traditional or manual protocols in the diagnosis, treatment, and interpretation of COVID-19 patient data. Hence, patient’s prognosis and survival can be compromised (Albahri et al., 2020a, 2020b, 2020c).
Fortunately, the advent of COVID-19 coincided with the fourth industrial revolution. The period that supplied the demand for innovative technologies in multiple multifaceted industries worldwide (Agbehadji et al., 2020). Mainstream academia describes technology as a paradigm of protocols, frameworks, and instruments generated by the causative effect of scientific information labored to achieve a particular purpose (Kim et al., 2020). Technology revolutionized the medical profession by providing a comprehensive spectrum of potentials in disease documentation, disease containment, facilitated clinical research, and the digitization of healthcare systems across established healthcare facilities (Allam, 2020; Kim et al., 2020). Regarding COVID-19, computer scientists strived to assist healthcare professionals in the war against COVID-19. Their contributions included developing contact tracing applications and home quarantine surveillance technologies via smartphones, wearables, and interactive maps. The interactive and publicly available global tracing map was mainly launched by the Center for Systems Science and Engineering at Johns Hopkins University on January 20th, 2020. Additional applications included thermal scanners, robotics, depth cameras were introduced to detect the respiratory pattern of COIVD-19 patients, and the development of artificial intelligence (AI) (Adly et al., 2020).
Labeled as the father of artificial intelligence (AI), Professor Marvin Minsky is amongst the scientists pool in artificial intelligence invented by John McCarthy in 1956 (Hussain et al., 2020). Computer scientists explained the principle of artificial intelligence as the ability of machines and programmed computer systems to mirror the human capacity to learn, interpret, and develop resolutions to a particular issue (Adly et al., 2020; Madurai Elavarasan and Pugazhendhi, 2020). Public health professionals received AI with great enthusiasm in 2018 due to the limitless capabilities provided by AI. Mixture of Numerous technology sought the chance to pioneer the movement of implementing AI in the mitigation of COVID-19; explicitly, BlueDot and Metabiota (Hussain et al., 2020).
BlueDot is a web-based startup venture established by Dr. Kamran Khan in the during the SARS outbreak in 2003. The company rose to the publicity during the Swine flu outbreak of 2009. The reputation was credited to the accurate prediction framework designed by the company to track the progression of the virus. The framework created an exact forecast of the infectious trends of the virus using global air data. BlueDot solidified its leadership further during the Ebola outbreak of 2014 by disseminating its copyright risk assessment modules that predicted the Ebola virus’s eventual spread in three Western African countries. The corporation continued its ambitious projects in the current catastrophe of COVID-19. Eventually, computing a detailed projection of possible COVID-19 targets nine days before the WHO’s initial announcement. Compared to BlueDot, Metabiota was confined to human and animal research during its early ventures, especially in the African continent. Metabiota projected a steady growth and captivated the US government’s attention that deployed the startup venture in the mitigation of the Ebola pandemic. Artificial intelligence techniques being machine learning, deep learning, and natural language processing algorithms sharpened the company’s studies in human behavioral analysis through social media. Metabiota implemented the findings to determine future COVID-19 targets a week before the official announcements in Japan, Thailand, and Hong Kong. Artificial intelligence evidence a significant advantage in the management of COVID-19 (Allam, 2020). It has delivered numerous applications in diagnostics, therapeutics, medical imaging, and reduction of the physical interactions between healthcare professionals and COVID-19 patients. Henceforth, diminishing the occupational exposure of healthcare workers to COVID-19 (Adly et al., 2020).
Currently, there are many commercial AI applications available for health care systems. For example, PATHAI (improving diagnostic pathology) helps pathologists for more accurate diagnosis of samples. PAGER (proactive healthcare management) is another application that improves patient treatment through making health care recommendations. For drug discovery, ATOMWISE application can identify chemical structures and compounds. Lastly, the Quibim platform uses medical imaging and AI for early detection of COVID-19 (Builtin, 2020; MDDI, 2020).
Clinical imaging has demonstrated a significant role in the early detection of COVID-19. Although the differentiation of other viral pneumonia from COVID-19 pneumonia is challenging and difficult on Computed tomography (CT) scan alone (Feng et al., 2020), it has reported a high sensitivity of 97 % specifically in patients with clinical suspicions of COVID-19 but with negative Reverse transcription polymerase chain reaction (RT-PCR) test results (Fechner et al., 2020). Additionally, to assess the lung changes while avoiding the patient’s movement suspected to have COVID-19, the American College of Radiology (ACR) suggested placing portable x-ray machines in the department. Therefore, portable chest x-ray (CXR) can be considered as a first-line imaging tool to evaluate the abnormalities present in symptomatic patient lungs (Cellina et al., 2020).
Moreover, diagnosing COVID -19 patients through images is a bit challenging as there are some limitations of some imaging modalities. A study of four cases was done in Italy to compare Chest x-ray to chest CT scan in diagnosing COVID-19. The chest x-ray images for the four patients came negative without any sign of abnormality. However, the chest CT scan showed some COVID-19 imaging features such as ground-glass opacity (GGO), crazy paving pattern and consolidation. The study shows a high probability of having a false negative chest x-ray for a positive COVID-19 patient. Although chest x-ray is the better option because it is a faster and extensively accessible tool for evaluating lung parenchyma, most COVID-19 imaging research papers are currently focusing on chest CT because of its higher sensitivity (Cellina et al., 2020).
Another study conducted on 234 patients addressed other CXR findings; they observed that 55 out of 234 patients had nodules and 156 had reticular–nodular opacities in their chest radiograph and reported that CXR has a sensitivity of 68.1 %, with variability between 69%–90% (Cozzi et al., 2020). Additionally, the sensitivity of CXR in the current literature ranges from 25 % to 69 % (Oterino Serrano et al., 2020).
COVID-19 has been linked to other features such as vascular enlargement and air Broncho-gram (Meiler et al., 2020). Another study addressed chest CT images showing additional signs of COVID-19 lesions, such as interlobular thickening of septa in a crazy-paving pattern, air trapping and reverse halo sign (Y. Li and Xia, 2020). Also, a study aimed to correlate the chest CT findings of COVID-19 patients with the course of the disease. The authors found that crazy paving, bronchus distortion, bronchiectasis, air trapping, and mediastinal and hilar lymph node enlargement were more profound in the Intensive Care Unit (ICU) patients compared to non-ICU and discharged patients (Erturk et al., 2020). One of the studies mentioned that in severe cases chest CT showed flaky or widespread lesions (Yu et al., 2020).
Chest CT has been used to identify the stage of the lung lesions. About 30 patients were found to be in early stage, 49.1 % of 110 cases in the progressive stage and 26 patients were in a severe category. For chest CT follow-up patients, 12 out of 16 patients (75 %) demonstrated disease progression, 25 % of 16 patients were of a mild degree and five moderate cases were seen on CT (Wang et al., 2020). Among those patients, CT findings showed disease extent as minimal in two patients, 4 patients had moderate progression, and two patients showed severe disease extent.
Furthermore, some of the reviewed articles discussed the significance of chest CT in identifying COVID-19 lung lesion distribution. In a study, an initial CT scan of the chest performed on 51 patients showed that the majority of the patients (74.5 %) had an infection in all five lobes of the lung while the remaining had an infection in other lobes individually or bilaterally (Y. Li and Xia, 2020). CT can detect peripheral lung lesions in 43.6 % of 110 patients and lesions in both central and peripheral zones in 56.4 % of cases. Additionally, Chest CT was used to image lesion distribution in different lung lobes. About 5.5 % of 110 patients displayed multiple lung lesions while 9.1 % showed individual lobe lung lesions. The Majority of patients (72.7 %) were seen to have lesions in multiple lobes of the right and left lung (Wang et al., 2020). The distribution of pulmonary lesions on CT of COVID-19 patients was mostly at all stages with the highest rate (66.6 %) at stage 2. A few patients have central lesions (2.1 %) (Ding et al., 2020).
Another study showed that a 38-year-old symptomatic patient did RT-PCR test four times. The results came negative four times. However, the CT chest images were susceptible as they showed patchy ground-glass opacities (GGO) as a typical imaging feature of COVID-19 (Feng et al., 2020). A review article stated that according to ACR, chest CT should not be used for screening as a first-line for the diagnosis of COVID-19 and should rather be used for symptomatic patients with clinical indications (Asefi and Safaie, 2020).
Moreover, the Chinese critical care ultrasound study group and Italian academy of thoracic ultrasound recently suggested that ultrasound of the lung (LUS) is an accurate and appropriate tool to identify lung involvement in patients with COVID-19, specifically for pregnant women; it is the safest option and can be done several times during pregnancy due to radiation-free technique characteristic and the ability to detect pneumonia related to COVID-19 (Buonsenso et al., 2020).
Additionally, Ultrasound is one of the imaging modalities that has been used to scan positive COVID-19 patients. The sonographers have faced a unique challenge as their work requires close patient contact for a long period, which increases the risk of COVID-19 transmission. Therefore, the protocol for the scan was done by the radiologist to reduce the examination time. In addition, the use of the US scan was considered the last option for COVID-19 patients due to the increased infection risk for the sonographers (Eastgate et al., 2020). A study stated that LUS findings among 10 pediatric patients were mainly vertical B-lines, white lung signs, irregularities of pleura, and subpleural consolidation. LUS has been demonstrated to be an important imaging tool in assessing moderate and severe COVID-19 pneumonia (Sultan and Sehgal, 2020).
Furthermore, case studies reviewed from Canada and Turkey described lung US findings of a health care worker and pregnant patient. LUS, as a radiation free modality, could be safely used to image pregnant women. The pregnant patient displayed diffuse and thick B-lines on either side of the lungs and had basal posterior involvement, while the health care worker demonstrated multifocal B-lines, thickening of pleura, and subpleural consolidation (Sultan and Sehgal, 2020). Moreover, a research paper on 4 pregnant patients with COVID-19 was conducted to observe lung involvement by ultrasound. All four patients showed signs of COVID-19 pneumonia on LUS including irregular pleural line, white lung, large sub-pleural consolidations, and multiple vertical artifacts (Buonsenso et al., 2020).
Additionally, numerous studies reported that the appearance of air Broncho-gram sign in COVID-19 patients. Air Broncho-gram sign was mostly visible in the early and progressive stages (Sultan and Sehgal, 2020). Three other articles reported that LUS is superior to chest CT in detecting smaller peri-pulmonary lung lesion along with pleural and peri-pulmonary effusion (Bosso et al., 2020; Convissar et al., 2020; Sultan and Sehgal, 2020).
Although PCR test is routinely used, it has many limitations, including possible false negative results that require repeating the test, the result accessibility can take 2 days and the shortage of test kit. Additionally, CT scan alone can show normal images of COVID-19 patients. Therefore, integrating CT scan with AI using useful data such as clinical symptoms has improved the detection sensitivity similar to an expert radiologist level. Using this approach, COVID-19 cases were accurately detected compared to the wrong classification of the radiologist alone (Mei et al., 2020). Another study reported that using a trained deep learning algorithms scored 90.8 % accuracy, 84 % sensitivity, and 93 % specificity in classifying COVID-19 pneumonia (Harmon et al., 2020). Moreover, a study has compared the DeepCOVID-XR AI algorithm’s performance to five radiology experts on 300 images. The accuracy of DeepCOVID-XR’s accuracy was higher (82 %) than the consensus (81 %) of all five radiologists (Wehbe et al., 2020).
The current status of combining AI, digital techniques and clinical imaging technologies concentrates on three main areas; positive or negative COVID-19 classification, lung lesions quantity identification, and differentiating COVID-19 from other types of Pneumonia. Although many studies have reported an acceptable accuracy, sensitivity, and specificity of such techniques, it is difficult to identify COVID-19 patients with a negative PCR test. Therefore, the clinical decision cannot only rely on AI in the presence of valuable lab tests. In order to improve the current role of such technologies, more useful data regarding certain diseases like diabetes, liver and kidney lesions, and age can be incorporated to improve the overall diagnostic performance (Li et al., 2020a, b; Summers, 2020).
The resilience of modern digital technologies and artificial intelligence during COVID-19 created a great disagreement among healthcare professionals. Forming a divide of acceptance and rejection. Such debate motivated the foundation of this paper to answer a collection of research questions; (1) How did the pandemic help promoting the digital uprising of modern healthcare technologies and artificial intelligence? (2) What are the clinical applications of artificial intelligence during COVID-19? (3) What is the efficacy of AI-enabled technology in the disciplines of clinical imaging? (4) What are the pitfalls and challenges of artificial intelligence encountered during COVID-19?
The study targets to answer the previous questions by achieving the following aims: (1) Explore the trends of modern healthcare technologies and artificial intelligence during COVID-19 crisis (2) Define the concepts and clinical role of artificial intelligence in the mitigation of COVID-19 (3) Investigate and correlate the efficacy of AI-enabled technology in medical imaging during COVID-19 (4) Determine the advantages, limitations, and challenges of artificial intelligence during COVID-19 pandemic.
2. Materials and methods
This research paper was developed based on the principles of systematic literature reviews. Systematic literature reviews are distinguished publications that maintain a profound societal influence in scientific explorations and dedicated healthcare research (O. S. Albahri, Zaidan, et al., 2020). Such literary pieces designed the standard module of generalizing research literacy in the scientific community and the healthcare workforce; through guided collection and categorization of the current body of literature relevant to a particular research question. The compiled literature is eventually analyzed following rigorous eligibility criteria hypothesized around an expansive research protocol (Liberati et al., 2009). The research aims to collate the latest full-text and peer-reviewed publications covering the scope of modern digital technologies and artificial intelligence during COVID-19.
Correspondingly, the research methodology utilized an extensive literature search constituting four databases: Google Scholar, PubMed, IEEE Xplore, and Fatima College of Health Sciences (FCHS) learning center database (EBSCOhost); to inspect all original publications associated with the topic of interest. The database selection rationale articulated the abundance of scientific literature from multiple databases presented by Google Scholar. Google Scholar functions as an umbrella server for a range of databases as exemplified by Elsevier. PubMed and IEEE Xplore were synonymous in terms of diversity and validity of interdisciplinary publications on COVID-19. The FCHS learning center database was employed to provide a supplementary portal for additional articles associated with technology, artificial intelligence, and COVID-19. The candidacy of the extracted literature cohort was determined through specific eligibility criteria; (1) Articles written in the English language (2) Full-text and peer-reviewed articles published between March 2020 and September 2020 (3) Publications and studies conducted during the COVID-19 pandemic (4) Publications that include keywords connected to technology, artificial intelligence, and COVID-19. Further article stratification was concluded by a subsidiary exclusion criterion; (1) Pre-print publications and articles that await peer- review (2) Publications with denied access (3) Publications incompatible with the research scope (4) Articles that lack a revision timeline including submission, review, and publication dates (5) Articles that exhibit subjective opinion or bias about the proposed review topic.
This review adopted a four-phase research procedure. Phase one originated from the preliminary search on September 3rd, 2020 of the Google Scholar database. The search identified 53 articles that expressed a tendency of variety in the acquired search results. Thus, prompting the phase two initiation on the following day by conducting a secondary search using the Google Scholar database to validate the quality of the displayed results. The secondary search yielded 40 publications focusing on artificial intelligence contributions in the healthcare industry during COVID-19. Phase three commenced on September 5th, 2020, and marked the inspection of PubMed and IEEE Xplore. September 6th, 2020 dated the investigation of the FCHS learning database, namely, EBSCOhost. Statistically, the selected data incorporated 12 articles from PubMed, 3 articles from IEEE Xplore, and 2 articles from the FCHS learning center database. Table 1 and Fig. 1 stratify the database search protocol and acquired results. Congruently, the accumulated literature cohort tallied a total of 110 articles assessed for eligibility using the pre-determined eligibility criteria. Nineteen publications were eliminated on account of incompatibility with the research scope during the primary title and abstract inspections. Duplication was evident in two publications obtained from EBSCOhost. Eleven publications were removed due to ineligibility in terms of the requisite criteria. Eventually, the systematic literature review included a total of 54 that fulfilled the inclusion criteria.
Table 1.
Systematic research data and accumulated results.
| Search date | Selected database | Extracted results | Applied search terms |
|---|---|---|---|
| 3/9/2020 | Google Scholar | 53 | "modern technologies" COVID- 19 |
| 4/9/2020 | 40 | Artificial intelligence in healthcare during COVID-19 | |
| 5/9/2020 | PubMed | 12 | "artificial intelligence" COVID-19 |
| IEEE Xplore | 3 | (((("All Metadata”: artificial intelligence) AND "All Metadata":COVID-19) AND "All Metadata": COVID-19) AND "All Metadata”: AI) | |
| 6/9/2020 | FCHS learning database (EBSCOhost) | 2 | (((("All Metadata”: artificial intelligence) AND "All Metadata":COVID-19) AND "All Metadata”: technologies) AND "All Metadata": AI) |
| Total | 110 |
Fig. 1.
Systematic Search Process extrapolated using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart.
3. Results
3.1. Digital technologies and COVID-19
Digital technologies supported the world in addressing the tragic impact of the novel coronavirus pandemic (Kumar et al., 2020). COVID-19 painted a picture of resistance to the routineness of human life with weakened global economies and three billion people confined in compulsory public health lockdowns as the proprietary tones of COVID-19 (Lin and Hou, 2020). Digital health societies, symposiums, and contributors lead the international scene in the consumption of technological interventions to circumvent the ripple of COVID-19. Examples of such interventions entailed the management of case detection, socioeconomic impressions streamed by the circulation of the virus, and the institution of public health mandates to tackle the outbreak within the affected territories (Kapoor et al., 2020; Whitelaw et al., 2020). Researchers continue to interpret the interlinked combinations provided by digital technologies in response to COVID-19. This section of the systematic literature review discusses a variety of digital technologies associated with targeted COVID-19 responses from the perspective of the included literature; (1) Digital interventions within clinical facilities (2) Digital interventions outside clinical facilities (3) Digital interventions within the World Wide Web.
3.1.1. Digital interventions within clinical facilities
3.1.1.1. 3D-printing
The global invasion of COVID-19 triggered tragic deficiencies in medical supply chains of personal protective equipment (PPE). Frontline responders require protective facial masks, goggles, and protective shields to tend to COVID-19 patients. PPE reduces the inherent occupational exposure by inhibiting the user from absorbing the viral droplets containing COVID-19. Three- dimensional printing remedied the emerging shortages by efficiently producing crucial medical supplies at accelerated speed using readily available material. The printing process involves applying a 3D laser to generate accurate measurements of the facial features of the potential user leading to the fabrication of a personalized facial mask. Open-source data contributes to the cost efficiency of three-dimensional printing as it facilitates the circulation of biodegradable material in the production of protective face shields (Tsikala Vafea et al., 2020).
3.1.1.2. Robots
Healthcare robotics represents a specimen of the technological interventions promoted by the spread of COVID-19. Dedicated COVID-19 treatment facilities resorted to healthcare robotics to establish remote treatment protocols and viral infection control. Facilities stationed the robots in various central departments that housed COVID-19 patients analogous to isolation wards and intensive care units. Deployed units directed the autonomous completion of lab tests, vital signs acquisition, facility-based disinfection, and waste management. Logistical delivery of essential patient supplies to in-bound patient rooms was also attainable through the stationed robotic units within the hospital premises (Mastaneh and Mouseli, 2020). The Providence Regional Medical Centre in Washington exercised an assistant robot capable of remote vital signs acquisition through a built-in stethoscope. Nevertheless, the robot functioned as a communication channel between physicians and COVID-19 patients allowing the former to communicate with patients through live stream video conferences (HealthManagement.org, and Team, E., 2020).
3.1.1.3. Telemedicine
Telemedicine is witnessing a period of profound use due to the novel coronavirus pandemic. The prospect of remote healthcare services is one of the gold standards of telemedicine that increases accessibility to medical services through the Information and Communication Technology platform or ICT. ICT platforms authorized physicians to launch teleconsultations using telecommunication networks or video conferences to address patient complaints and presented cases. In terms of COVID-19, telemedicine can provide real-time patient observation of quarantined individuals through self – reported medical information using smartphones or other digital devices. Telemedicine systems can stream continuous notification to healthcare providers reporting the patient’s symptoms and disease progression. Such data can simplify the generalization of remote population management across the afflicted state (Fagherazzi et al., 2020; Kapoor et al., 2020; Mastaneh and Mouseli, 2020). Technology-enabled critical care services or tele-critical care (TCC) signifies an expanded perspective of traditional intensive care units’ conveniences. TCC can coordinate the transfer of critically ill patients in hospitals with limited occupancy or capabilities. The proper patient provision ensures the conservation of PPE reserves, and minimizes occupational exposure in paramedics and medical ambulances. Medical ICUs can witness significant advantages in the maximization of ICU efficacy in terms of early monitoring of possible respiratory complications associated with COVID-19 and conscious use of ICU resources like unit occupancy and available ventilators (Scott et al., 2020).
3.1.2. Digital interventions outside clinical facilities
3.1.2.1. Drones
Drones played a vital role in the technological response to COVID-19. The drones provided aerial case detection, diagnostics, and supervision of the mandated public health regulations in terms of efficiency and population compliance. Healthcare professionals can operate drones to execute frequent supply deliveries of patient laboratory samples and relevant essentials quickly and efficiently (Mastaneh and Mouseli, 2020). Drones can enforce population compliance through visual and audio prompts to the offenders for violating the public health mandates and omitting the use of a protective face mask. This practice was notable in China as drones patrolled rural localities with diagnosed cases and reported public health policies violations to the relevant authorities (HealthManagement.org, and Team, E., 2020). High-resolution cameras, specialized thermal scanners, and high-performance computer systems are among the repertoire of tools offered by drones to limit the spread of COVID-19 in airports and public transportation hubs. Thermal scanning of places of populated congregation and remote disinfection of COVID-19 hotspots are examples of drone capabilities adopted in multiple countries worldwide (HealthManagement.org, and Team, E., 2020; Kapoor et al., 2020).
3.1.3. Digital interventions within the World Wide Web
3.1.3.1. Geographic Information Systems (GIS)
Geographic information systems or GIS systems are mobile computer-based frameworks that compile, archive, and categorize spatial data related to planet earth’s surface. The embedded data cohorts could consist of street signs, geographical locations, population census, and characteristic vegetation within the system area coverage (Drew et al., 2020; Mbunge, 2020). GIS systems can guide technological interventions for COVID-19 diagnostics through data reports that entail the location of diagnosed cases, hospital occupancy, and patient compliance with public health regulations. The system proceeds to perform a complex spatial analysis of COVID-19 related data that assists the authorities in maintaining constant surveillance of the virus spread within the infected country and the world (Mastaneh and Mouseli, 2020).
3.1.3.2. Internet of things (IoT)
The internet of things is a composite system that resembles the taxonomy of the human organ system. IoT frameworks are an entity of subsidiary systems functioning as a central component in the system network. Computer scientists stimulated IoT systems capabilities to become a vault of accessible public data available to the general population with examples ranging from daily case statistics to global fatality rates around the world (Adly et al., 2020). Generalized internet of things frameworks can create communication channels between medical devices and the World Wide Web. Therefore, increasing the accessibility to vital information and medical services determines the disease progression and possible prognosis (Mastaneh and Mouseli, 2020).
3.1.4. Provisions and limitations
Technology-driven responses witnessed universal adaptation on a global scale to limit the spread of COVID-19. Researchers and stakeholders investigated the arguments reflecting the limitations of digital technologies in a variety of COVID-19 literature (Coombs, 2020). Table 2 highlights a collection of provisions and limitations encountered with the adaptation of digital technology interventions.
Table 2.
Provisions and limitations of technological interventions related to COVID-19.
| Provisions/ limitations | Description / illustrative example | References |
|---|---|---|
| Internet accessibility | Digital technologies rely on the availability of internet access which allows digital frameworks to reach full potential in terms of generalization and connectivity within the established server coverage. | (Budd et al., 2020) |
| Capital expenditure | Technological interventions require significant amounts of capital to invest in the development, maintenance, and adaptation of digital technologies in response to COVID-19. Such technologies encompass digital assistants like SIRI and ALEXA. | (Keesara et al., 2020) |
| Digital divide | The disparity in accessibility to digital technologies can limit the coverage of technological interventions in some population groups that lack access to digital technologies. | (Ramsetty and Adams, 2020) |
3.2. Artificial intelligence and COVID-19
3.2.1. Behind the ones and zeros: an AI glossary
Artificial intelligence is a discipline of many stratospheres and entwined intricacies. These intricacies mirror the coping mechanism of the human cerebral network with the fabrication of intelligent agents. Intelligent agents are the computerized counterpart of the human cerebral neurons as the artificial intelligence apparatus gradually develops an autonomous capacity to process the setting, the present data, and the parties involved to deduce the resolution of a particular scenario. Hence, reincarnating the architecture of human thought (Agbehadji et al., 2020). Table 3 summarizes some of the common terminologies associated with artificial intelligence.
Table 3.
Glossary of common artificial intelligence terminology.
| Terminology | Definition | References |
|---|---|---|
| Deep learning | The computation of the human independent critical thinking, interpretation, and resolution through the categorization of random data. | (Salman et al., 2020) |
| Machine learning | The recognition of data through identified patterns. | (Bansal et al., 2020) |
| Convolutional neural network (CNN) | A deep learning algorithm that targets AI systems designated in the segregation of multimedia information (i.e. video, audio, and images) | (Salman et al., 2020) |
| Supervised learning | Data comprehension through the use of cataloged data. | (Hussain et al., 2020) |
| Unsupervised learning | Data comprehension through the use of uncatalogued data. | |
| Natural language processing (NLP) | The encoding of accumulated data obtained through natural linguistics and dialogue. | |
| Natural inspired computing (NICC) | The development of novel algorithms and hardware through the multidisciplinary integration of mathematics, computer science, theoretical physics, etc. | (Agbehadji et al., 2020) |
| Convolutional layers | A set of predetermined parameters that shape the AI learning process. | (Salman et al., 2020) |
| Pooling | The learning blocks of CNN. | |
| Fully connected layers | Interlinked sets of CNN neurons that transfer learning data. | |
| Reinforcement learning | The training of an AI platform through a specified set of rewards and penalties established by the human programmer. | (Hussain et al., 2020) |
| Big data | The total volume of heterogeneous computed data in the present databases. | (Agbehadji et al., 2020) |
3.2.2. AI applications against COVID-19
3.2.2.1. Remote detection and diagnostics
The signature communicability and lethality of COVID-19 represented a physiological fortress for the medical group and scientists alike. This challenge is founded on the rapidly mutative sequelae of COVID-19. Rapidly, the alteration of COVID-19 sequelae is governed by pre-existing lung conditions. Pulmonary atelectasis, hemorrhage, edema, and lung tissue neoplasia are illustrative examples capable of altering COVID-19 diagnosis and confusing the trained medical eye (Adly et al., 2020). Public health experts state the standard diagnostics of COVID-19 as a methodology of two folds consisting of nasopharyngeal PCR swabs and diagnostic radiology (Salman et al., 2020). PCR test analysis reported a characteristic disparity in the differential diagnosis yielding a percentage of 60–71% clinical sensitivity (Adly et al., 2020). Therefore, comprising the prospect of fast and definite acquisition of essential diagnostics relevant to patient survival (Naudé, 2020). Public health experts resorted to bio surveillance to rectify the disparity of present molecular testing kits and provide the basis for remote detection and prevention of COVID-19 (Bansal et al., 2020).
Contact tracing is a mainstay public health prevention regulation that detects the exposure of a particular sample of individuals to an infectious contagion through a reverse revision of each member’s activities and movements involved in the chain of transmission (Lalmuanawma et al., 2020). Public health epidemiology dates the application of contact tracing in instances of global pandemics like SARS, MERS, flu, Ebola, and COVID-19 (Agbehadji et al., 2020; Lin and Hou, 2020). This process is evident in COVID-19 prevention protocols that allow a stringent observation of infected cases during 14 days through cellular technologies like global positioning systems, Bluetooth, social activity maps, and network credit card transactions. In episodes of proper systematic deployment, contact tracing can provide means of real-time detection, identification, and prevention of severe COVID-19 epicenters (Lalmuanawma et al., 2020). Hence, reducing predicted causalities and augmenting the success of COVID-19 responses employed in individual localities and governments as solidified in South Korea (Lin and Hou, 2020). The antithesis of the beneficial role of contact tracing manifests in possible data security breaches, invasion of autonomous privacy, and mishandling of the heterogeneous data volume (Lalmuanawma et al., 2020).
Artificial intelligence devices assisted researchers and stakeholders to broaden the spectrum of contact tracing through the integration of artificial intelligence, big data, and Machine learning to enhance the scale of detection, identification, and parameter of contact tracing technologies (Bansal et al., 2020; Bragazzi et al., 2020). Big data systems enable the accumulation of structured and unstructured data computed in the global databases on the internet. Clinical data obtained through big data can encompass radiographic images, alternative diagnostics including, salivary testing kits, pharmacology, and digitized health care documentation (Agbehadji et al., 2020; Bragazzi et al., 2020). Machine learning and artificial intelligence encouraged researchers to discover key biological metrics associated with the treatment paradigm of COVID-19 counting on radiographic image history and hematology of the reported cases (Lalmuanawma et al., 2020).
Artificial intelligence introduced the concept of digital phenotyping. Digital phenotyping exploits cellular-based sampling of surveys, texts, multimedia, and screen patterns to generate a detailed phenotype of the user’s movements, behavioral trends, and digital signature (Bansal et al., 2020). The efficacy of AI-enabled contact tracing and digital phenotyping is determined by the subject’s commitment to provide the required data for contact tracing analysis. Several non-medical technology combinations like Google and Apple proposed a Bluetooth operated contact tracing application that configures the operator’s phone to a visual platform reporting proximity to a known COVID-19 case. Furthermore, Bluetooth powered contact tracing applications can breed the incidence of false positives and false negative diagnosis of COVID-19 due to mask-based socialization between the user and other mask-wearing individuals or personal inner circle (Lin and Hou, 2020). The tradeoffs of AI-integrated contact tracing contrast with cost-efficiency, higher clinical sensitivity, minimized occupational exposure, and minimal detection time compared to conventional human-operated screening protocols (Agbehadji et al., 2020).
Contact tracing applications were an adopted public health practice in the Arabian Peninsula with the Tabaud and TraceCovid as prominent instances. The Saudi Data and Artificial Intelligence Authority (SDAIA) designed the Tabaud or distancing standard Arabic dialect to establish a contact tracing network for all involved contacts. TraceCovid is a contact tracing application adopted in the United Arab Emirates as a part of the smart solutions platform in response to COVID-19 (Hassounah et al., 2020; Lalmuanawma et al., 2020).
3.2.2.2. Expediting COVID vaccine and therapeutics
Vaccines are synthetic pharmaceuticals that stimulate the body to produce antibodies to mitigate foreign viral bacteria invasion. The public health contributions of vaccines are emphasized in targeted disease prevention and elimination of infectious diseases through reproducible efficacy and long-term stability (Kim et al., 2020). COVID-19 genomics revealed an intricate physiological puzzle that compelled scientists to adopt a changed strategy to mitigate the spread of COVID-19. This strategy consisted of investigating the current repository of antiviral medications for potential repurposing, synthetic modification of present antivirals to accommodate COVID-19 biology, and the application of alternative interventions including, traditional Chinese medicine to expand the potential of drug synthesis and repurposing. Artificial intelligence assisted researchers in the knowledge of pharmacological therapeutics and immunizations of COVID-19 (Bragazzi et al., 2020). Natural language processing enabled clinicians to assume and identify COVID-19 related pharmaceuticals through the linguistic analysis of syntax found in dedicated pharmacology references (Adly et al., 2020).
Moreover, Machine learning provided accurate identification and suggestions of possible medications eligible for COVID-19 repurposing such as Atazanavir and Baricitinib (Naudé, 2020). Baricitinib is an immunosuppressant prescribed for patients with rheumatoid arthritis and myelofibrosis (Adly et al., 2020). The discovery of Baricitinib was the byproduct of the joint venture between numerous dedicated institutions like BenevolentAI, the Imperial College of London, and a university establishment (Bragazzi et al., 2020). Machine learning extrapolated a projected timeline for vaccine development in an estimated 18 months (Naudé, 2020). When paired with reverse vaccinology, machine learning determined six potential vaccinations that target the proteins of the COVID-19 molecule, as reported by the Hong Kong headquarters of Insilico Medicine (Bansal et al., 2020; Bragazzi et al., 2020). Reverse vaccinology is a discipline that applies computed technology to sequencing genome information (Del Tordello et al., 2017).
3.2.2.3. COVID-19 treatment
AI applications can be useful for COVID-19 treatment planning (Tayarani and M. H., 2020; van der Schaar et al., 2021). It was reported that an approach based on machine learning could analyze and differentiate between different types of treatment plans that can aid physicians in selecting an effective treatment plan (Pu et al., 2020). Additionally, the patient’s recovery prediction was evaluated using three machine learning techniques. The results showed that patients with fever and fatigue living in China did not recover (Ella Hassanien et al., 2020). Also, AI was found useful in COVID-19 disease progression and the need for oxygen treatment prediction using machine learning (Obinata et al., 2020). Another application is related to the ability of the AI to prioritizing patients based on their health conditions. This technique utilizes Multi-Biological Laboratory Examination Framework to classify patients into mild, moderate, and severe cases to receive the most effective treatment (Albahri et al., 2020a, 2020b, 2020c). Moreover, recovered COVID-19 patients can develop antibodies that can help the immune system of other severe cases. Therefore, AI was utilized using machine learning to identify the suitable donors and most critical patients (O. S. Albahri, Al-Obaidi, et al., 2020).
3.2.2.4. Redefining routine clinical tasks
COVID-19 patients have consumed emergency departments, intensive care units, and floor units to the maximum capacity worldwide (Debnath et al., 2020). According to reported metrics in global clinical facilities, the approximate COVID-19 death rate measures at 4.5 % amid confirmed infections as of March 26th, 2020. Notwithstanding the interval of 0.2–15% death rate calculated in infected demographics determined by age and history of pre-existing conditions (Salman et al., 2020). The Our World Data initiative is among the scientific publications aimed to deliver empirical statistics regarding COVID-19.
For instance, case fatality rate or CFR ratio is the death censuses divided by the total COVID-19 cases within an affected area. The case fatality rate pattern may fluctuate by the constant change in pandemics data trends comparable to daily case counts (Roser et al., 2020). Treatment paradigms and protocols differed in many hospitals and specialized medical institutions as some facilities resorted to manual data spreadsheets containing patient-centered information. Healthcare workers discard the manual spreadsheets following patient discharge. The practice of manual spreadsheets may lead to data mismanagement due to the constant surplus of COVID-19 patients with variable case characteristics and physiological phenotypes.
Artificial intelligence systems can facilitate the clinical workload imposed on healthcare professionals through digitized data collection, storage, and examination using state of the art portable devices and technology with installed electronic health records platforms (Adly et al., 2020; Debnath et al., 2020). Mobile tablets and personal digital assistance devices can provide significant convenience in facilitating data access for healthcare professionals regardless of their location, presided tasks, and rotation within the campus of the hospital or specialized institutions. Smartphones and smart bracelets can develop a third-party medium for physicians to consume AI-powered real-time case surveillance of isolated infections and private settings including the patient’s residence and social interactions (Adly et al., 2020). Machine learning can redefine the environment of clinical decision making in COVID-19 emergency departments by calculating risk trajectories, disease progression, prognostic outcome, and the effects of ventilation on the generalized case therapeutics and viral phenotype. Thus, mapping the proper prioritization and resource allocation of depleted supplies using empirical probabilities resembling respiratory failure incidence (Debnath et al., 2020).
3.2.2.5. Revolutionizing knowledge dissemination
The American dramatist Zora Neale Hurston describes research as a formalized curiosity and investigation with a purpose (Hoffman-Jeep, 2005). The vague nature of COVID-19 promoted widespread collaborations between researchers, technology stakeholders, computer scientists, virologists, and clinicians from all professions to organize a systematic application and stratification of COVID-19 research data. Data mined publications encompassed AI-focused and non-AI focused research. Hence, creating a preprint trend noted in several prominent databases. Artificial intelligence system developers sourced non-AI-focused articles to browse for characteristic COVID-19 information that may enrich the training of original AI platforms designated in the management of COVID-19 (Naudé, 2020).
The COVID-19 Open Research Dataset or CORD-19 is a prominent example of COVID-19 knowledge dissemination developed by the partnership of Google, Semantic Scholar, Chan Zuckerberg Initiative, Microsoft research group, National Library of Medicine–National Institutes of Health, and the Center for Security and Emerging Technology in Georgetown University under the supervision of the Office of Science and Technology Policy of the United States White House. CORD-19 data inventory consists of 59,000 full-text research topics ranging from SARS-Cov-2 to COVID-19 disease, and former coronaviruses as documented on May, 26th 2020. The database acts as a symposium for AI scientists to converge their exclusive insights and innovations to assemble AI devices to the remission of COVID-19. WellAI and SciSight are AI-powered databases abstracted with the goal of directed literature search through machine learning algorithms and visualization maps to define the editorials that suit the user’s scope and criteria (Kricka et al., 2020).
3.2.3. Challenges and future prospects
Artificial intelligence is perceived with lauded acceptance and opposition from all scientific aisles (Allam, 2020). Intelligent AI agents opened the scientific retrospective view in terms of COVID-19 and the prospects of artificial intelligence. The majority of artificial intelligence research associations praised digitized economies, supply chains, and exports as future AI landscapes following the reduction of COVID-19 (Naudé, 2020). Additional research findings project the construction of smart cities and the integration of robotics in human labor as anticipated artificial intelligence presentations post−COVID-19 (Bragazzi et al., 2020; Naudé, 2020). Table 4 collects some encountered challenges and tradeoffs of artificial intelligence in consideration of COVID-19.
Table 4.
Challenges and tradeoffs of artificial intelligence in terms of COVID-19.
| Challenge | Description / illustrative example | References |
|---|---|---|
| Logistical maintenance | Compulsory public health lockdowns can impede communication between machine learning data specialists, engineers, and healthcare personnel to ensure proper usage and maintenance of the AI algorithm. | (Debnath et al., 2020) |
| Existing AI technique limitations | The performance of deep learning is restricted by the provided human data, inherent computation of all case-related probabilities, and the volume of training data. | (Hussain et al., 2020) |
| Invasion of individual privacy | Public health COVID-19 responses and guidelines mandated the use of private user data (i.e. contact tracing) | (Naudé, 2020) |
| Training data shortage | Scarce training data can compromise the performance and efficiency of COVID-19 centered AI models. | |
| Heterogeneous data cohorts | The disparity in COVID-19 variables can influence the results of predictive AI models. Such variables include the incubation period, levels of dyspnea, and oxygen saturation. | (Adly et al., 2020; Debnath et al., 2020) |
| Chatbots | Chatbots are conversation simulators created to offer an alternative platform of human-AI communication. These systems require long term training and maintenance to minimize the incidence of deficient clinical diagnosis and false response inputs. | (Madurai Elavarasan and Pugazhendhi, 2020) |
3.3. Artificial intelligence and medical imaging during COVID-19
PCR swabs surfaced as abstract instrumentations in discrete COVID-19 diagnostics except for disparate detection accuracy depending on the sample quality, storage, and manual handling (Shi et al., 2020). Medical imaging rose to compensate for PCR tests discrepancies and impede the chain of transmission of COVID-19 (Shaikh et al., 2020). Radiographic imaging modalities contribute to the observation of disease progression (Greenspan et al., 2020) by using radiographic image evidence to support frontline responders in establishing a diagnostic strategy compatible with the presented patient data (Shi et al., 2020). The radiographic imaging modalities of COVID-19 were sorted into primary and secondary modalities in terms of rationale, relevant studies, and imaging characteristics of diagnosed COVID-19 cases.
3.3.1. Radiographic workup of COVID-19
3.3.1.1. Primary imaging modalities
3.3.1.1.1. Chest radiography
Chest radiographs (CXRs) are routine imaging procedures that map the anatomical chest patterns through means of attenuation of ionizing radiation generated from an X-ray machine tube. The representation of pulmonary pathology in routine CXRs assisted healthcare professionals in the expository investigation of COVID-19 sequelae, explicitly, early pathological infestations of COVID-19 (Shaikh et al., 2020). X-ray machines are everywhere in medical imaging departments due to their cost-effectiveness and staple reliability (Kundu et al., 2020). COVID-19 patients can present normal CXR findings in response to prompt acquisition times, absence of pathological signs in the pulmonary tissue, and elusive radiographic findings (Manna et al., 2020). In the medical imaging society, variations in test circumstances, symptomatology, virus incubation time, and false negatives started a paradox debating the merits of CXRs as diagnostic imaging tools to scan and diagnose COVID-19 (Kundu et al., 2020).
Positive CXR radiographs demonstrate COVID-19 as blurred patches on the lung’s bilateral surface with altered locations and severity depending on the infection stage. The lung opacifications intensify in texture, solidity, and severity with the continuation of COVID-19 inflammation in the afflicted lungs. Mild COVID-19 cases may contrast routine COVID-19 opacifications. The COVID-19 CXR findings are revealed in 10–12 days after the disease initial exposure (Manna et al., 2020). COVID-19 CXRs share significant commonalities with viral pneumonia. Therefore, challenging radiologists in the differential diagnosis of COVID-19 compared to viral pneumonia (Chowdhury et al., 2020). The radiographic technique of COVID-19 consists of bedside AP CXRs, PA, and lateral chest projections to evaluate the onset of COVID-19 in the respiratory system (Manna et al., 2020).
3.3.1.1.2. Computed tomography
Computed tomography defines the correlation between the rotatory imaging detectors and ionizing radiation to emulate cross-sectional slices of the chosen scan coverage. Thoracic computed tomography exceeded PCR tests’ diagnostic accuracy and the false-negative readings of CXRs with a clinical sensitivity of 98 %, in contrast to 71 % in PCR swabs (Kundu et al., 2020; Nagpal et al., 2020). Computed tomography operators begin the image acquisition by instructing the patient to maintain a fixed position on the gantry patient bed and adhere to a set of breathing instructions during scan acquisition. Radiologists undertake the image reading and interoperation processes using the comprehensive scan coverage of thoracic CT slices. Thoracic CT slices cover the pulmonary anatomy from the pulmonary apices to the costophrenic angles to evaluate thoracic pathologies depending on the patient’s body habitus. Computed tomography operators reconstruct the raw scan data and transfer the images to PACS servers following computer-based post-processing of the preliminary raw data (Nagpal et al., 2020).
Medical imaging stakeholders have reported a plethora of COVID-19 findings in thoracic computed scans including ground-glass opacities (GGOs), crazy paving patterns, lobular consolidations, and the reverse halo sign as radiographic findings of COVID-19 (Kundu et al., 2020). GGOs are at the most encountered computed tomography findings at a predominance of 60–70 % as stated in epidemiological studies from Wuhan city (Nagpal et al., 2020). GGOs are round morphological developments that occur in response to extra levels of radiographic attenuation in the thorax without any caused pathological mutations to the respiratory systems’ normal bronchial and vascular habitus (Manna et al., 2020). The lower right lobe is the primary site of GGOs in COVID-19 patients. GGO lesions may diffuse in the periphery of the lungs with increased thickness and infiltration according to the stage of infection (Nagpal et al., 2020).
Crazy paving patterns are a subtype of GGOs with notable septal line thickening in the lobular pulmonary borders that may accompany GGOs or lung consolidations. Therefore, modeling a shape analogous to irregular paved cobblestones (Nagpal et al., 2020). Lobular lung consolidations are solid obstructive opacities located in the airway borders and vascular margins of the lungs. The lobular lung consolidations may lead to lower pulmonary lobes involvement in the posterior and inferior directions (Manna et al., 2020). COVID-19 consolidations may express air bronchograms and lung cavitation in the infected tissue depending on disease stage at the time of image acquisition. The reverse halo sign or the atoll sign is a GGO enclosed by profuse marginal consolidations. Reverse halo findings subsidize the alveolar damage in the interstitium and airway of COVID-19 patients (Nagpal et al., 2020).
Hematological laboratory tests can demonstrate the vascular pathophysiology of COVID-19. D-dimer tests and vascular thrombogenicity are diagnostic assessments of vascular pathophysiology (Shaikh et al., 2020). Medical imaging uses halo sign to show COVID-19-induced vascular injury. Halo sign refer to masses or nodules superimposed by GGOs. The halo sign commonly arises in angiographic disorders like vasculitis and vascular hemorrhage (Nagpal et al., 2020). Radiographers use pulmonary CT angiography or duplex venous sonography to investigate the vascular appearance of COVID-19. The computed tomography findings of COVID-19 mature within 6–13 days of the official disease cycle (Manna et al., 2020).
3.3.1.2. Secondary imaging modalities
3.3.1.2.1. Magnetic resonance imaging
Magnetic resonance imaging applies magnetic and radio waves oscillation principles to produce sharp resolution images of the organs and soft tissue fascia within the region of interest. Pulmonary MRI scan findings revealed episodes of increased signal intensity on T1 and T2 weighted COVID-19 pneumonia images congruous to GGOs and peripheral lung involvement on thoracic CTs and CXR scans. Supplementary magnetic resonance imaging series revealed subtle cardiac damage in COVID-19 patients with signs of cardiomyopathy and myocarditis. Cine cardiac MRIs can deliver real-time motion images showing COVID-19 myocarditis registered by cardiac wall motion anomalies and delayed contrast enhancement within the scanned myocardium (Manna et al., 2020). Progressive viral research confirmed the neurological pathology stimulated by COVID-19 with recorded brain damage, great vessel occlusion, and pediatric encephalitis (Shaikh et al., 2020).
3.3.1.2.2. Point of care ultrasound
Mobile chest sonography is a staple imaging investigation occurring at the patient's bedside during an emergency or intensive care setting. Sonography is popular in medical imaging due to the convenience, omission of ionizing radiation, affordability, and consistency in scan replication and diagnostic findings. Point of care sonograms cited interrupted brightness mode lines, pulmonary consolidations, and pleural line thickness as signs of COVID-19 pneumonia. Follow-up sonograms of recovered COVID-19 patients displayed horizontal amplitude lines determining the remission of COVID-19 from the lung parenchyma (Manna et al., 2020).
3.3.1.2.3. Positron emission tomography
Positron emission tomography is a nuclear imaging procedure that traces inflammatory and oncological processes within the body through radiographic compounds denoted as tracers. Fluorodeoxyglucose is the leading radiotracer in positron emission tomography (Shaikh et al., 2020). COVID-19 inflammation can lead to residual FDG uptake conforming themes of GGOs and variable attenuation levels within the anatomy of interest (Manna et al., 2020). Positron emission tomography scans with excess radiation dosage and prolonged scan time can identify the radiotracer motion and uptake within the whole body (Shaikh et al., 2020).
3.3.2. AI-integrated Medical imaging in the period of COVID-19
The ambiguity of COVID-19 aggravated the concern of occupational exposure to vulnerable frontline responders attending to patients with high viral shedding levels, leading to hospital personnel’s consequent infection. Artificial intelligence accelerated the expansion of healthcare technologies to challenge the transmissibility of COVID-19 (Shi et al., 2020). Medical imaging departments sustained significant impairments in patient management, department occupancy, and capitalization of existing resources indigenousness to the clinical facilities and the administrative health boards in the country of interest (Manna et al., 2020).
Artificial intelligence agents automated medical imaging workflows in global imaging procedures during the COVID-19 pandemic with the example of patient monitoring. Modern imaging equipment utilized AI-enabled high-resolution cameras in mobile CT units using visual detection technologies to compute the patient habitus and parameters allied with image acquisition. Forward-looking infrared cameras and time of flight imaging are visual sense technologies that use artificial intelligence to outline the patient's anthropometry in terms of medical imaging. Artificial intelligence visual sensors execute autonomous computation of radiographic scan coverage and radiographic isocenters. Radiographic isocenters are the intersection between the center of the scan target and the scanner (Shi et al., 2020).
COVID-19 affiliated studies incorporated a pool of experimental conditions to establish the linkage between AI technologies and COVID-19 mitigation. Researchers designed the collection of scientific studies using various imaging modalities, artificial intelligence platforms, hospitalization settings, and patient demographics (Kundu et al., 2020). Table 5A, Table 5B reflect on the assortment of included AI-experiments conducted during the COVID-19 pandemic.
Table 5A.
Experimental conditions of the included medical imaging experiments of artificial intelligence and COVID-19.
| Experimental study | Setting | Duration | Imaging modality | Study population |
|---|---|---|---|---|
| (Zhang et al., 2020a, 2020b) | Huoshenshan Hospital in Wuhan | 35 days [February 11th - March 16th, 2020] | Chest CT | 2460 COVID-19 patients [1250 males and 1210 females in the age bracket of 11−93 years of age] |
| (Chowdhury et al., 2020) | Not disclosed | Not disclosed | Digital CXR | 3487 digital CXR collected from relevant COVID-19 literature [1485 viral pneumonia, 1579 normal CXRs, and 423 COVID-19 CXRs) |
| (Zhu et al., 2020) | Not disclosed | Not disclosed | Mobile CXR | 131 bedside CXRs collected from 84 COVID-19 patients [51males, 29 females, and 4 anonymous patients] |
| (Ozturk et al., 2020) | Not disclosed | Not disclosed | Raw CXR | 127 CXRs acquired from two separate databases (1) GitHub: (https://github.com/muhammedtalo/COVID-19) and (2) ChestX-ray8. [500 normal, 500 pneumonia, 82 males, and 43 females suffering from COVID-19] |
| (Hwang et al., 2020) | Seoul National University Hospital. | 40 days[January 31st -March 10th, 2020] | CXR | 332 COVID-19 patients [173 males and 159 females] |
| (Bai HX, et al., 2020) | 10 hospitals from China and the United States | 3 months [January 2020-April 2020] | Chest CT | 1186 patients [521 patients with positive PCR tests and 665 patients with pneumonia] |
| (Apostolopoulos et al., 2020) | Not disclosed | Not disclosed | CXR | 3905 CXRs attributable to various pulmonary disorders. The images were retrieved from several medical imaging databases (i.e. Radiopedia and the Radiological Society of North America (RSNA). |
| (Tsiknakis et al., 2020) | Not disclosed | April 11th, 2020 | CXR | The study encompassed 572 CXRs retrieved from (1) QUIBIM imagingcovid19 platform and (2) GitHub: (https://github.com/tsikup/COVID-19-xray-cnn) [150 bacterial pneumonia, 150 viral pneumonia. 122 COVID-19 CXRs, and 150 normal images |
| (Ko et al., 2020) | Wonkwang University Hospital, Chonnam National University Hospital in South Korea, and the Italian Society of Medical and Interventional Radiology [SIRM] public repository | Not disclosed | 2D Chest CT | 3993 Chest CTs of COVID-19 patients compiled from the participating institutions |
| (Song et al., 2020) | The Lu’an affiliated hospital of Anhui Medical University and the First Affiliated Hospital of University of Science and Technology of China | 35 days [January 18th - February 23rd, 2020] | Chest CT | 201 COVID-19 patients. [118 males and 83 females] |
| (Ni et al., 2020) | Seven hospitals in China. | Not disclosed | Chest CT | 14,435 patients [2154 COVID-19 patients and 5874 patients presenting other respiratory pneumonia] |
| (Ran et al., 2020) | Henry Ford Health system [5 hospitals and 30 clinics] | Not disclosed | CXR | 5805 CXRs with RT-PCR confirmed COVID-19 pneumonia from 2060 patients and 5300 CXRs with non-COVID-19 pneumonia from 3148 patients. |
Table 5B.
Objectives, results, advantages and disadvantages of the included novel COVID-19-AI imaging studies.
| Experimental study | Research direction & AI technology | Results | Advantages | Disadvantages |
|---|---|---|---|---|
| (Zhang et al., 2020a, 2020b) | Triage of COVID-19 pneumonia using the deep learning software uAI. | The uAI Intelligent Assistant Analysis System detected COVID-19 Pneumonia in addition to COVID-19 CT findings (i.e. GGOs and lobular lesions) | Useful for localization and quantification of lung lesions | Requires manual human modification to rollout negative lesions |
| Useful for treatment planning based on the affected lung regions | ||||
| Not applicable for critical cases (CT) | ||||
| (Chowdhury et al., 2020) | Autonomous detection of COVID-19 pneumonia using transfer learning. | The transfer learning system managed to train CNNs to achieve readings of 99.7 %, 99.7 %, 99.7 %, 99.55 %,97.9 %, 97.95 %, 97.9 %, and 98.8 % in taxonomical accuracy, pathological sensitivity, and specificity to COVID-19. | Useful for normal and abnormal classification Image augmentation can slightly enhance the overall performance | Large data set is required to improve the accuracy |
| (Zhu et al., 2020) | Classification of COVID-19 severity on portable CXRs using deep learning CNNs and an expert radiologist panel. | The deep learning CNNs accomplished a comparable staging accuracy to the three-member radiologist panel at a mean absolute error of 8.5 %. | Incorporating AI with portable X-ray images provide more accessible diagnosis than CT scan | Small data set was used |
| No Correlation with radiographic score system | ||||
| No correlation with clinical non imaging information | ||||
| Useful for disease severity identification | ||||
| Transfer learning is superior to traditional learning techniques in terms of shorter training time | ||||
| (Ozturk et al., 2020) | Autonomous detection of COVID-19 using deep learning CNNs and an expert radiologist panel to compare normal Vs. COVID-19 and COVID-19 Vs. pneumonia. | The proposed obtained an accuracy of 98.08 % in binary classification and 87.02 % in multi-class classification. | No manual extraction is needed | Small data set was used |
| Incorporating AI with X-ray images provide more accessible diagnosis than CT scan Heat-maps images are useful for localization | ||||
| (Hwang et al., 2020) | Evaluation of deep learning CAD (computer-aided detection) system performance in image interpretation of suspected COVID-19 CXRs. | AI CAD system generated a 68.8% sensitivity and 66.7% specificity to COVID-19. COVID-19 pneumonia was also detected at a 72.3% specificity and 81.5% sensitivity. | CAD technique provides shorter diagnostic time than PCR result | Lack of trained data on COVID-19 images |
| (Bai et al., 2020) | Evaluation of AI integrated image interpretation workflow in the differentiation of COVID-19 and other pulmonary findings on chest CTs. | Deep learning apparatus assisted radiologists in improving the diagnostic performance in terms of COVID-19 at a 90% accuracy, 91% specificity, and 88% sensitivity. | AI augmentation is useful for differentiating COVID-19 from other pneumonia on CT images | Small data set was used |
| Lack of homogenous pneumonia cases | ||||
| (Apostolopoulos et al., 2020) | Autonomous detection of COVID-19 using transfer learning, deep learning, and CNNs. | The proposed study method delivered 99.42 % specificity, 99.18 % accuracy, and 97.36 % sensitivity in the identification of biological markers of COVID-19. | Useful to identify new pulmonary abnormalities as new biomarkers | Small data set was used |
| Lack of suspected COVID-19 patients data | ||||
| (Tsiknakis et al., 2020) | Development of a feasible AI model in terms of image interpretation of COVID-19 CXRs using transfer learning techniques and the evaluation of an expert radiologist panel. | The transfer learning model was capable of undertaking binary, ternary, and quaternary at the area under curve of 1 during the management of a 5 stage dataset. | Attention maps can improve the final clinical decision | limited data set |
| (Ko et al., 2020) | Rapid triage, investigation, and differentiation of the pulmonology of COVID-19, pneumonia, and non-pneumonia disorders of the lungs using transfer learning. | The ResNet-50 model outperformed the transfer learning models at a 99.87 % accuracy, 100 % specificity, and a 99.58 % sensitivity. Hence, providing a reliable diagnostic detection of COVID-19 pneumonia. | Useful for differentiating COVID-19 from other pneumonia on CT images | Small data set was used Lack of data for validation |
| (Song et al., 2020) | Autonomous differentiation of viral pneumonia from COVID-19 computed tomography findings using bi-directional generative adversarial network data architecture to enhance unsupervised learning of the presented data. | The novel AI platform generated a maximum specificity of 91 % and a sensitivity of 92 % during the training, testing, and validation stages of the study. | Useful for differentiating COVID-19 from other pneumonia on CT images | Small data set was used Variation in CT image acquisition parameters Lack of data of severe COVID-19 cases |
| (Ni et al., 2020) | Autonomous recognition of CXR COVID-19 findings using deep learning. | The deep learning platform maintained a consistent diagnostic performance in comparison to the expert radiologists at a maximum accuracy of 0.85 Vs. 0.93 of expert medical imaging residents. | Useful for quantitative detection of abnormalities | Small data set was used |
| Lack of specificity in comparison to radiologists | ||||
| (Ran et al., 2020) | Autonomous differentiation of COVID-19 pneumonia from other causes of CXR abnormalities and test the system performance against thoracic radiologists using deep neural networks. | CV19-Net was able to differentiate COVID-19 related pneumonia from other types of pneumonia with performance paralleling that of experienced thoracic radiologists at a confidence interval of 95%. The combination of chest radiography with the proposed CV19-Net deep learning algorithm has the potential as an accurate method to improve the accuracy and the estimated times of the radiological interpretation process of COVID-19 pneumonia. | Useful for differentiating COVID-19 from other pneumonia on CT images | Lack of pneumonia types classification |
| Lack of COVID-19 representative data |
3.3.3. Interpretation of AI-integrated medical imaging
The successive waves of COVID-19 reiterated the paradox of artificial intelligence in the discipline of medical imaging (O. S. Albahri, Zaidan, et al., 2020). Artificial intelligence is a topic of avidity in the medical imaging society. Medical imaging experts welcomed AI features in routine medical imaging tasks that may encompass oncological staging, radiographic image reconstruction, disease triage, and radiographic segmentation (Reyes et al., 2020).
Radiographic image segmentation composites a computed deconstruction of fundamental features of COVID-19 findings. AI-driven segmentation extracts individual structural components of the human lung corresponding to the pulmonary lobes, bronchial systems, and incidental lung infection or present neoplasia. Thus, radiologists are fostering suitable conditions to utilize computer-based quantification and evaluation of COVID-19 (Shi et al., 2020). The limitations of artificial intelligence are the large number of metadata and diverse platforms that require clinical facilities to apply reliable protocols in AI technique selection, integration, and interpretation of the computed medical imaging results in terms of COVID-19 (Albahri et al., 2020a, 2020b, 2020c).
4. Discussion
The fourth industrial revolution established technology at the helm of the fight against COVID-19. Technology directed the scene of smart interventions in several technology-driven countries across the seven continents counting South Korea, Japan, Germany, Iran, Italy, China, Turkey, Thailand, Canada, and many more (Fields et al., 2020). The adopted smart solutions diversified in concept, target, and technique ranging from social media repurposing to applying artificial intelligence platforms to maximize the scope of contactless responses to COVID-19 (Budd et al., 2020). This paper aimed to undertake the literary expedition in the pool of intercontinental literature discussing and deciphering the significance of technology in the battle of the novel coronavirus pandemic.
The method of this review adopted the principles of systematic literature reviews using a selective research protocol of four leading web-based databases to mine for literature about technology, medical imaging, and artificial intelligence during the present times of COVID-19. Thus, yielding 54 articles for targeted inclusion associated with the research direction and objectives in terms of keywords, research scope, and publication results. The included articles were tabulated into three letter-coded batches (A) digital technologies and COVID-19 (B) Artificial intelligence and COVID-19 (C) Artificial intelligence and medical imaging during COVID-19, and summarized in terms of aims, strengths, limitations and conclusion (Appendix A–D).
Batch (A) articles entailed 18 publications about digital technologies’ notions in the mitigation of COVID-19. The findings of the discussed articles lead to the exploration of home quarantine, technology researchers, and stakeholders undertaking the precedence of COVID-19 (Kapoor et al., 2020; Whitelaw et al., 2020). Further reflection on the articles in question allowed to deliberate on categorizing of technological interventions in the included literature. The eventual conclusions classified the technological interventions as digital interventions within clinical facilities, digital interventions outside clinical facilities, and digital interventions within the World Wide Web. The category of digital interventions within clinical facilities reflected on the ability of 3D printing to compensate for depleted PPE supplies, the multipurpose field of healthcare robotics to protect frontline responders, and the applications of telemedicine addressing the redefined conveniences of healthcare consultations, ICU units, and ER departments (Mastaneh and Mouseli, 2020; Scott et al., 2020; Tsikala Vafea et al., 2020). Aerial drones were the prime focus of digital interventions outside clinical facilities due to the reiterated applications of autonomous supply deliveries to clinical facilities charged with the care of COVID-19 patients (HealthManagement.org, and Team, E., 2020; Kapoor et al., 2020; Mastaneh and Mouseli, 2020). Batch (A) was finalized with digital interventions within the World Wide Web discussing Geographic Information Systems and the internet of things to secure the databases of COVID-19 data (Adly et al., 2020; Mastaneh and Mouseli, 2020). The provisions of digital technologies are capital expenditure, Internet accessibility, and the digital divide among the compromised demographics to COVID-19 (Budd et al., 2020; Keesara et al., 2020; Ramsetty and Adams, 2020).
Artificial intelligence was the exclusive focus in batches (B) and (C). Batch B focused on the definitions of AI concepts, COVID-19 applications, ending at the investigation of challenges and prospects of artificial intelligence using 15 included articles from the systematic search protocol results. In terms of COVID-19 applications, artificial intelligence offers remote detection and diagnostics, expedited COVID-19 vaccine and therapeutics, redefined clinical workflow and revolutionized knowledge dissemination in a continuous apparatus to systematically address the novelty of COVID-19 (Bansal et al., 2020; Kim et al., 2020; Naudé, 2020). Batch (C) convened 21 articles based on artificial intelligence and medical imaging interactions during the novel coronavirus pandemic. Batch (c) articles continued exploring artificial intelligence and medical imaging by assessing the radiographic workup of COVID-19 to conclude chest radiography and computed tomography as the primary imaging modalities (Shaikh et al., 2020). Ahead of magnetic resonance imaging, point of care sonography, and positron emission tomography as secondary imaging modalities of COVID-19 (Manna et al., 2020). The topic of novel AI-driven medical imaging experiments was the research direction of 12 research publications targeting the use of artificial intelligence technologies to facilitate the imaging workload of COVID-19 patients. For instance, convolutional neural networks can identify the patterns within medical radiographs to simplify the differentiation of COVID-19 from pneumonia-affiliated disorders (Salman et al., 2020).
5. Conclusion
COVID-19 is the latest addition to a pedigree of infectious pandemics that spanned the last two decades. A lethal virus that paralyzed the cycle of life and captured the modern world within the walls of a residence and the World Wide Web. Scientists of the present millennia are equipped with the innovation and resourcefulness of the ever-expanding tech industry. Technology is a universe of algorithms, platforms, and contexts that redefine the lane of possibility for humanity.
Healthcare technologies aided frontline responders to strategize the response against the elusive virus leading to the advanced sequencing of the viral genome at a record speed and discovering innovative diagnostics to detect, quarantine, and treat confirmed cases worldwide. Reverse transcriptase-polymerase chain reaction swabs offered a means of direct diagnosis of COVID cases but a compromised accuracy depending on the conditions of the collected samples. The successful use of medical imaging, digital technologies, and artificial intelligence compensated for PCR tests disparate accuracy.
Medical imaging modalities screen and detect COVID-19 using chest radiography and computed tomography as gold standards in diagnosing suspected cases. Radiologists can repurpose magnetic resonance imaging, point of care sonography, and positron emission tomography as supportive modalities to visualize the disease’s subtle and long term features. Artificial intelligence is a debate of elation and opposition among medical imaging professionals.
The intelligent agents proved to deliver a consistent diversity of applications within healthcare facilities and beyond. Artificial intelligence technologies exposed healthcare professionals to the opportunity of contactless care. Contactless care allows frontline responders to tend to fragile COVID-19 patients and minimizes the likelihood of inherent occupational exposure to the depleting disease.
The opposition of artificial intelligence stems from the requirements and early research that qualify novel AI platforms for generalization and public use. Artificial intelligence agents require vigorous programming, investment, training, and research process to validate the platform’s efficacy, application rationale, without the exception of the limits of predictability in terms of the platform’s direction and future use.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to thank the Radiography and Medical Imaging senior students (Aisha Yunuis Mohamed Hasan Al Hammadi, Emtithal Yousif Mohamed Osman, Fatimah Mirza Mohamed Saleh and Sarah Ahmed Khameis Almotawa) for providing help during the research.
Appendix A. Batch (A) articles related to Digital technologies and COVID-19
| Article # | Article title | Publication URL |
|---|---|---|
| 1. | Digital technologies in the public-health response to COVID-19 | https://www.nature.com/articles/s41591-020-1011-4 |
| 2. | Covid-19 and Health Care’s Digital Revolution | https://www.nejm.org/doi/full/10.1056/NEJMp2005835 |
| 3. | Applications of digital technology in COVID-19 pandemic planning and response | https://www.thelancet.com/journals/landig/article/PIIS2589-7500(20)30142-4/fulltext |
| 4. | COVID-19: What Can Healthcare Learn? | https://healthmanagement.org/c/healthmanagement/issuearticle/covid-19-what-can-healthcare-learn |
| 5. | Rapid implementation of mobile technology for real-time epidemiology of COVID-19 | https://science.sciencemag.org/content/368/6497/1362 |
| 6. | Digital healthcare: The only solution for better healthcare during COVID-19 pandemic? | https://www.sciencedirect.com/science/article/pii/S0019483220300584 |
| 7. | Digital Health Strategies to Fight COVID-19 Worldwide: Challenges, Recommendations, and a Call for Papers | https://www.jmir.org/2020/6/e19284/ |
| 8. | A review of modern technologies for tackling COVID-19 pandemic | https://www.sciencedirect.com/science/article/pii/S1871402120301272 |
| 9. | Restructured society and environment: A review on potential technological strategies to control the COVID-19 pandemic | https://www.sciencedirect.com/science/article/pii/S0048969720323755 |
| 10. | Integrating emerging technologies into COVID-19 contact tracing: Opportunities, challenges and pitfalls | https://www.sciencedirect.com/science/article/pii/S1871402120303325 |
| 11. | Digital technology applications for contact tracing: the new promise for COVID-19 and beyond? | https://link.springer.com/article/10.1186/s41256-020-00164-1 |
| 12. | Technology and its Solutions in the Era of COVID-19 Crisis: A Review of Literature | http://jebhpme.ssu.ac.ir/article-1-279-en.html |
| 13. | A Study on Fight Against COVID-19 from Latest Technological Intervention | https://link.springer.com/article/10.1007/s42979-020-00301-0 |
| 14. | Emerging Technologies for Use in the Study, Diagnosis, and Treatment of Patients with COVID-19 | https://link.springer.com/article/10.1007/s12195-020-00629-w |
| 15. | Advanced Digital Health Technologies for COVID-19 and Future Emergencies | https://www.researchgate.net/publication/341674785_Advanced_Digital_Health_Technologies_for_COVID-19_and_Future_Emergencies |
| 16. | Will COVID-19 be the tipping point for the Intelligent Automation of work? A review of the debate and implications for research | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7365646/ |
| 17. | Digital Response During the COVID-19 Pandemic in Saudi Arabia | https://www.jmir.org/2020/9/e19338/ |
| 18. | Impact of the digital divide in the age of COVID-19 | https://academic.oup.com/jamia/article/27/7/1147/5826352 |
Appendix B. Batch (B) articles related to Artificial intelligence and COVID-19
| Article # | Article title | Publication URL |
|---|---|---|
| 1. | AI Techniques for COVID-19 | https://ieeexplore.ieee.org/document/9136710 |
| 2. | The Rise of Machine Intelligence in the COVID-19 Pandemic and Its Impact on Health Policy | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7378493/ |
| 3. | Review of Big Data Analytics, Artificial Intelligence and Nature-Inspired Computing Models towards Accurate Detection of COVID-19 Pandemic Cases and Contact Tracing | https://www.mdpi.com/1660-4601/17/15/5330 |
| 4. | Approaches Based on Artificial Intelligence and the Internet of Intelligent Things to Prevent the Spread of COVID-19: Scoping Review | https://www.jmir.org/2020/8/e19104/ |
| 5. | A Review for Artificial Intelligence Proving to Fight against COVID-19 Pandemic and Prefatory Health Policy | http://216.10.241.171/jmbas.in/index.php/jmbas/article/view/247 |
| 6. | A Deep Learning System to Screen Novel Coronavirus Disease 2019 Pneumonia | https://www.sciencedirect.com/science/article/pii/S2095809920301636 |
| 7. | Artificial intelligence vs COVID-19: limitations, constraints and pitfalls | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7186767/ |
| 8. | COVID-19 Detection using Artificial Intelligence | http://dstore.alazhar.edu.ps/xmlui/handle/123456789/587 |
| 9. | How Big Data and Artificial Intelligence Can Help Better Manage the COVID-19 Pandemic | https://www.mdpi.com/1660-4601/17/9/3176/htm |
| 10. | Combat COVID-19 with artificial intelligence and big data | https://academic.oup.com/jtm/article/27/5/taaa080/5841603 |
| 11. | Machine learning to assist clinical decision-making during the COVID-19 pandemic | https://link.springer.com/article/10.1186/s42234-020-00050-8 |
| 12. | Utility of Artificial Intelligence Amidst the COVID 19 Pandemic: A Review | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7395799/ |
| 13. | Applications of machine learning and artificial intelligence for Covid-19 (SARS-CoV-2) pandemic: A review | https://www.sciencedirect.com/science/article/pii/S0960077920304562 |
| 14. | How artificial intelligence and machine learning can help healthcare systems respond to COVID-19 | https://www.vanderschaar-lab.com/NewWebsite/covid-19/post1/paper.pdf |
| 15. | Artificial Intelligence-Powered Search Tools and Resources in the Fight Against COVID-19 | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7294813// |
Appendix C. Batch (C) articles related to Artificial Intelligence and Medical Imaging during COVID-19
| Article # | Article title | Publication URL |
|---|---|---|
| 1. | Can AI Help in Screening Viral and COVID-19 Pneumonia? | https://ieeexplore.ieee.org/document/9144185 |
| 2. | Deep transfer learning artificial intelligence accurately stages COVID-19 lung disease severity on portable chest radiographs | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386587/ |
| 3. | Imaging of COVID-19 pneumonia: Patterns, pathogenesis, and advances | https://www.birpublications.org/doi/10.1259/bjr.20200538?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed |
| 4. | Implementation of a Deep Learning-Based Computer-Aided Detection System for the Interpretation of Chest Radiographs in Patients Suspected for COVID-19 | https://www.kjronline.org/DOIx.php?id=10.3348/kjr.2020.0536 |
| 5. | Automated detection of COVID-19 cases using deep neural networks with X-ray images | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7187882/ |
| 6. | AI Augmentation of Radiologist Performance in Distinguishing COVID-19 from Pneumonia of Other Etiology on Chest CT | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7233483/ |
| 7. | Extracting Possibly Representative COVID-19 Biomarkers from X-ray Images with Deep Learning Approach and Image Data Related to Pulmonary Diseases | https://link.springer.com/article/10.1007%2Fs40846-020-00529-4 |
| 8. | Systematic review of artificial intelligence techniques in the detection and classification of COVID-19 medical images in terms of evaluation and benchmarking: Taxonomy analysis, challenges, future solutions and methodological aspects | https://www.sciencedirect.com/science/article/pii/S187603412030558X |
| 9. | Automated detection and quantification of COVID-19 pneumonia: CT imaging analysis by a deep learning-based software | https://link.springer.com/article/10.1007/s00259-020-04953-1 |
| 10. | End-to-end automatic differentiation of the coronavirus disease 2019 (COVID-19) from viral pneumonia based on chest CT | https://link.springer.com/article/10.1007/s00259-020-04929-1 |
| 11. | Review of Artificial Intelligence Techniques in Imaging Data Acquisition, Segmentation and Diagnosis for COVID-19 | https://ieeexplore.ieee.org/document/9069255 |
| 12. | A deep learning approach to characterize 2019 coronavirus disease (COVID-19) pneumonia in chest CT images | https://link.springer.com/article/10.1007/s00330-020-07044-9 |
| 13. | Coronavirus Disease 2019 (COVID-19) diagnostic technologies: A country-based retrospective analysis of screening and containment procedures during the first wave of the pandemic | https://www.sciencedirect.com/science/article/pii/S0899707120303193 |
| 14. | Position paper on COVID-19 imaging and AI: From the clinical needs and technological challenges to initial AI solutions at the lab and national level towards a new era for AI in healthcare | https://www.sciencedirect.com/science/article/pii/S136184152030164X |
| 15. | Interpretable artificial intelligence framework for COVID-19 screening on chest X-rays/ | https://www.spandidos-publications.com/10.3892/etm.2020.8797 |
| 16. | Current Landscape of Imaging and the Potential Role for Artificial Intelligence in the Management of COVID-19 | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7320858/ |
| 17. | COVID-19 Pneumonia Diagnosis Using a Simple 2D Deep Learning Framework with a Single Chest CT Image: Model Development and Validation | https://www.jmir.org/2020/6/e19569/ |
| 18. | On the Interpretability of Artificial Intelligence in Radiology: Challenges and Opportunities | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7259808/#__ffn_sectitle |
| 19. | COVID-19: A Multimodality Review of Radiologic Techniques, Clinical Utility, and Imaging Features | https://pubs.rsna.org/doi/full/10.1148/ryct.2020200210 |
| 20. | How Might AI and Chest Imaging Help Unravel COVID-19’s Mysteries? | https://pubs.rsna.org/doi/10.1148/ryai.2020200053 |
| 21. | Diagnosis of COVID-19 Pneumonia Using Chest Radiography: Value of Artificial Intelligence | https://pubs.rsna.org/doi/10.1148/radiol.2020202944 |
Appendix D. Summary of the included studies
| Title | Aims | Strengths | Limitations | Conclusion |
|---|---|---|---|---|
| Approaches Based on artificial intelligence and the internet of intelligent things to prevent the spread of COVID-19: Scoping review | To analyze the current literature, discuss the applicability of reported ideas for using AI to prevent and control COVID-19, and build a comprehensive view of how current systems may be useful in particular areas (i.e. health care administrators, computer scientists, and policy makers worldwide) | The article describes the multidisciplinary applications of AI and real time efficacy in the mitigation of COVID-19. | Lacks other studies that might provide some additional perspective in the scope of AI and COVID-19. | The field of medical AI applications remains at early stages which was evident in the lack of literature pertaining to medical AI applications (i.e. resource allocation and experimental therapeutics). |
| Review of big data analytics, artificial intelligence and nature-inspired computing models towards accurate detection of COVID-19 pandemic cases and contact tracing | To compare the characteristics of big data, AI, nature-inspired computing models in terms of accuracy of COVID-19 contact tracing. | The article describes the role of technologies in the mitigation of COVID-19, clearly illustrates the addressed concepts in a simple and applicable language. | Lacks graphic representations through charts and figures that could display the efficacy of the proposed techniques in the mitigation of COVID-19. | AI models can help to address the gap in COVID-19 diagnostics but with a limited capacity that requires further programming and subject compliance. |
| Systematic review of artificial intelligence techniques in the detection and classification of COVID-19 medical images in terms of evaluation and benchmarking: Taxonomy analysis, challenges, future solutions and methodological aspects | To present AI techniques used in COVID-19 diagnostics with the notions of medical imaging benchmarking and evaluation. | Highlights a clear scope and compares other relevant studies that discuss the addressed topic, provides a proposed solution to address the lack in AI literature, and demonstrates the findings in an assortment of summarization tables that highlight the points of interest. | Lacks the input of experienced radiologists’ and real-world applications of the proposed solution being MCDA to ascertain the platform’s efficacy in addressing the shortcomings of AI. | The diversity of AI technologies can pose a challenge in terms of usage rationale during the suitable situation. |
| The Rise of Machine Intelligence in the COVID-19 Pandemic and Its Impact on Health Policy. In Surveying the Covid-19 Pandemic and its Implications | To emphasize the need of targeted use of technology to address future pandemics. | Provides clear details regarding the role of AI in the mitigation of COVID-19, highlights the chain of events related to the emergence and spread of COVID-19, and explains the background of AI and digital technologies to help curb COVID-19. | Lacks definitions of AI related concepts and real-time evaluation of the AI techniques. | Successful use of technology can mitigate the risks of future pandemics following COVID-19. |
| Extracting Possibly Representative COVID-19 Biomarkers from X-ray Images with Deep Learning Approach and Image Data Related to Pulmonary Diseases | Autonomous detection of COVID-19 using transfer learning, deep learning, and CNNs. | The article is critically organized with a detailed purpose, methods and results. | The pneumonia incidence samples are older recorded samples and do not represent pneumonia images from patients with suspected Coronavirus symptoms. | The proposed study method delivered 99.42 % specificity, 99.18 % accuracy, and 97.36 % sensitivity identifying biological markers of COVID-19. |
| A Study on Fight Against COVID-19 from Latest Technological Intervention | To study the efficacy of technological interventions against COVID-19 in aspects of home quarantine and AI-assisted diagnostics. | Provides a clear overview of the article with a detailed description of the diagnosis and therapeutics. | Lack of clear definition of AI and background or details about COVID-19. | AI offers the prospect of the full functional capability to mitigate COVID-19. |
| Utility of Artificial Intelligence Amidst the COVID 19 Pandemic: A Review | To describe the history and utility of machine learning in mitigating infectious pandemics and in retrospect to COVID-19. | Employs a consistent progression of ideas starting from the definition of machine learning and ending with machine learning’s clinical utility against COVID-19. | Lacks images and real-time incident involving the application of ML in a COVID-19 related setting. | Machine learning is a flexible AI technology manipulated in various medical circumstances, namely, mitigation of infectious pandemics. |
| How Big Data and Artificial Intelligence Can Help Against COVID-19 | To highlight and summarize the applications of AI and big data in the global efforts against COVID-19. | Explains the potential of AI and big data in the mitigation of COVID-19 using a hierarchal approach that includes short, mid, and long term application. | Lacks real-time applications that might provide additional illustration and understanding of AI and big data implementation in the COVID-19 response. | Big data and artificial intelligence can provide short, mid, and long term applications that may influence COVID-19 and future development concepts. |
| Digital technologies in the public-health response to COVID-19 | To capture the breadth of digital innovations for the public-health response to COVID-19 worldwide and their limitations, and barriers to their implementation, including legal, ethical and privacy barriers, as well as organizational and workforce barriers. | Offers a comprehensive background on COVID-19 and a wide explanation of the epidemiological aspects of COVID-19 using graphs and tables. | No notable limitations were mentioned. | COVID-19 inherently promoted digital technologies and allowed the exploration of the possibility of digitized healthcare. |
| Can AI Help in Screening Viral and COVID-19 Pneumonia? | Autonomous detection of COVID-19 pneumonia using transfer learning. | The publication displayed an organized outline, abstract, sampling method, and research methodology. | The publication fails to mention the participants’ awareness about the nature of the research. | The transfer learning system managed to train CNNs to achieve readings of 99.7 %, 99.7 %, 99.7 %, 99.55 %,97.9 %, 97.95 %, 97.9 %, and 98.8 % in taxonomical accuracy, pathological sensitivity, and specificity to COVID-19. |
| Will COVID-19 be the tipping point for the Intelligent Automation of work? A review of the debate and implications for research | To review the arguments in favor and opposition of increasing the level of AI adoption stimulated by COVID-19 with reflection on the influence of this argument in healthcare research. | Clearly explained the key arguments in favor of increased AI adoption include consumer preferences, increasing familiarity with AI technologies, and increased business confidence in AI. | Short conclusion and evident lack of in-text citations. | Information systems and management will become a topic of interest following the recovery after COVID-19. |
| Machine learning to assist clinical decision-making during the COVID-19 pandemic | To depict the importance and incidence of the emergency ML phenomena to help aid healthcare professional exercises evidence based practice and clinical decision making. | Portrays the multifaceted role of ML/AI in the mitigation of COVID-19 through many clinical scenarios and ethical-legal issues from healthcare professionals and patients alike. | Lacks statistical information on ML/AI’s actual implementation during COVID-19 including healthcare professionals and the perspective of healthcare professionals on ML/AI modals. | Medical machine learning is a prospect raised by COVID-19 and can offer a vast utility of applications to help facilitate the workflow undertaken in clinical healthcare facilities worldwide. |
| Rapid implementation of mobile technology for real-time epidemiology of COVID-19 | The goal was to establish the Coronavirus Pandemic Epidemiology (COPE) group to invite international scientists with expertise in big data research and epidemiology to develop a COVID-19 Symptom Tracker mobile application. | The publication offered full disclosure of the study participants being the Welsh Government, NHS Wales, the Scottish Government, and NHS Scotland. The approach has the benefit of allowing rapid deployment across a large cross-section of the population during an unprecedented health crisis. | Smartphone application does not represent a random sampling of the population. | The proposed approach offers early stages regarding the discussed concepts and novel consortium. The app was first launched in the UK on March 24th 2020, as opposed to March 29th in the USA, in which the app managed to garner more than 2.8 million users as of May 2, 2020. |
| Coronavirus Disease 2019 (COVID-19) diagnostic technologies: A country-based retrospective analysis of screening and containment procedures during the first wave of the pandemic | To illustrate country-based retrospective analysis of screening and containment procedures during the first wave of the pandemic. | Well organized article with clear details of the presented information. | Screening protocols must consider subspecialist expertise and time to diagnosis, in addition to diagnostic accuracy. National and institutional protocols must consider local availability of resources. | Diagnosis of COVID-19 is challenging due to a prolonged asymptomatic phase. RT-PCR has been considered the gold standard. However, suboptimal sensitivity in early disease and regional shortages of testing kits have limited its use. |
| Digital Response During the COVID-19 Pandemic in Saudi Arabia | The aim is to highlight how Saudi Arabia has used digital technology during the COVID-19 pandemic in the domains of public health, health care services, education, telecommunication, commerce, and risk communication. | All digital solutions and tools used to encompass during the COVID-19 outbreak in Saudi Arabia up to manuscript revision. | This paper lists apps but does not evaluate them or check for user experiences. Moreover, the criteria for inclusion in this paper were subjective. The authors attempted to decrease the effect of this subjectivity using discussion and consensus. | The Saudi Vision 2030 framework, released in 2017, has paved the path for digital transformation. COVID-19 enabled the promotion and testing of this transition. In Saudi Arabia, artificial intelligence in integrating different data sources during future outbreaks could be further explored. Also, decreasing the number of mobile apps and merging their functions could increase and facilitate their use. |
| COVID-19: What Can Healthcare Learn? | To demonstrate facts related to COVID-19 and to highlight on the role of healthcare workers during this pandemic. | The article has valuable recommendations related to COVID-19. | Lack of abstract, background, and conclusion. | The safety and protection of healthcare workers should be a top priority. Protective gear should be provided to healthcare workers immediately because, in the end, these are the people who will play an essential role in minimizing the level of illness and the number of deaths. |
| AI Techniques for COVID-19 | The aim of this study is to summarize the current state of AI applications in clinical administrations while battling COVID-19 and also to highlight various intelligence techniques and methods that can be applied to various types of medical information-based pandemic. | There was an attempt to benefit medical practitioners and medical researchers in overpowering their difficulties while handling COVID-19 big data. This survey study has also ended up with a detailed discussion about how AI implementation can be a massive advantage in combating various similar viruses. | Lacks some background information regarding AI (i.e. Definition and history of development). | The artificial intelligence tool is arriving at the clinical field in present times. AI techniques help in speeding up researches and assisting in the current COVID-19 crisis. Computer-based intelligence is not just useful in treating COVID-19 contaminated patients yet also for their proper medical check-ups. It can follow the emergency of COVID-19 at various scales, for example, clinical and epidemiological applications. |
| Implementation of a deep learning-based computer aided detection system for the interpretation of chest radiographs in patients suspected for covid-19 | The aim of this study is ‘to describe the experience of implementing a deep learning-based computer-aided detection (CAD) system for the interpretation of chest X-ray radiographs (CXR) of suspected coronavirus disease (COVID-19) patients and investigate the diagnostic performance of CXR interpretation with CAD assistance. | The results were clear and well explained in details | Small sample size | Radiologists with CAD assistance could identify patients with PCR-positive COVID-19 or pneumonia on CXR with an acceptable performance. In patients suspected of COVID-19, CXR had much faster TATs than PCRs. |
| Digital healthcare: The only solution for better healthcare during COVID-19 pandemic? | The paper focuses on ‘how digital solutions can impact healthcare during this pandemic’. | The information is clear and well organized. | Brief abstract and lack of detailed introduction. | Digital health systems are well suited to provide novel solutions to the public health emergency. These include the development of robust surveillance systems, telehealth, novel diagnostic and clinical decision-making tools. |
| Covid-19 and health care’s digital revolution | To demonstrate the importance of digital technology during COVID-19 and to show some important services that should be considered during this pandemic. | Information is clear and well organized. | Lack of clear abstract and conclusion. | Digital and technological revolution have transformed the world over the past century. As health care systems nationwide brace for a surge of COVID-19 cases, urgent action is required to transform health care delivery and scale up our systems by unleashing digital technologies power. |
| A Review for Artificial Intelligence Proving to Fight Against COVID-19 Pandemic and Prefatory Health Policy | The aim of the study is to discuss the various aspects of modern technology used to fight against COVID-19 outbreak crisis at different scales, including medical image processing, disease tracking, prediction, outcomes, computational biology and medicines. | The study uses various data sources, including MEDLINE, Global Health, PsycINFO, and Scopus databases. | No notable limitations were mentioned. | Emerging technologies are set to play an essential role in our response to the COVID-19 pandemic. There is an interest for future work on building up a benchmark framework to assess and look at the current techniques. The present models acquired extraordinary accuracy in recognizing COVID-19 symptoms with different kinds of viral pneumonia utilizing radiology imaging. |
| COVID-19 pneumonia diagnosis using a simple 2d deep learning framework with a single chest CT image: Model development and validation | The study aimed to rapidly develop an AI technique to diagnose COVID-19 pneumonia in CT images and differentiate it from non–COVID-19 pneumonia and non-pneumonia diseases. | The study specifics a precise research method as well as a validation process. | Lack of a COVID-19 CT database that allows additional training of the platform | FCONet, a simple 2D deep learning framework based on a single chest CT image, provides excellent diagnostic performance in detecting COVID-19 pneumonia. |
| The paper clearly describes the implications and testing parameters of each measured category under uniform scientific testing conditions. | Small sample size was used | |||
| The findings were illustrated through several means including tables and graphic heat signatures which provided additional convenience and understanding of the paper. The study included a performance comparison between the proposed platform and radiologist. | ||||
| Artificial intelligence-powered search tools and resources in the fight against covid-19 | This paper explores three prominent initiatives: COVID-19 focused datasets (e.g., CORD-19); Artificial intelligence-powered search tools (e.g., WellAI, SciSight); and contact tracing based on mobile communication technology. | The article was organized critically including the tables and diagrams. | No notable limitations were mentioned. | The new AI-powered search tools will accelerate research and development in COVID-19 as the world strives to develop efficient and timely testing and effective therapies to combat this pandemic. |
| How Might AI and Chest Imaging Help Unravel COVID-19′s Mysteries? | The study aims to explore the role of AI-chest image in detecting COVID-19. | Information was well organized in details. | The Summary and abstract were short and not specific. Lack of conclusion. |
Artificial intelligence (AI) can expand the role of chest imaging in COVID-19 beyond diagnosis to enable risk stratification, treatment monitoring, and the discovery of novel therapeutic targets. |
| Applications of machine learning and artificial intelligence for Covid-19 (SARS-CoV-2) pandemic: A review | The article aims to comprehensively review the role of AI and ML as one significant method in the arena of screening, predicting, forecasting, contact tracing, and drug development for SARS-CoV-2 and its related epidemic. | The publication employs summarization tables enabling full comprehension and illustration of the presented information. | The study lacks information about the integration of AI in COVID-19 related medical imaging. | The ongoing development in AI and ML has significantly improved treatment, medication, screening, prediction, forecasting, contact tracing, and the drug/vaccine development process for COVID-19. |
| Combat COVID-19 with artificial intelligence and big data. | To demonstrate the role of AI and big data in the mitigation of COVID-19 in Asian countries. | Information was well organized in details. | Minimal information on additional healthcare applications of AI during COVID-19 and lack of definitions of technology associated terminologies. | Researchers and technology companies are exploring ways to improve contact-tracing systems without mass surveillance to achieve the benefits of location-tracking while protecting individual privacy. |
| Restructured society and environment: A review on potential technological strategies to control the COVID-19 pandemic | The intention of this study is to uncover the hidden roles of technologies that ultimately help for controlling the pandemic. | Information was well organized in details. | No notable limitations were mentioned. | The strategies utilizing potential technologies would yield better benefits during the pandemic which in turn aids in controlling the spreading of infection. |
| COVID-19: A Multimodality Review of Radiologic Techniques, Clinical Utility, and Imaging Features | To review the radiological utility of COVID-19 being CT, CXR, US, NM, and echocardiography. | The article provides a clear and detailed investigation of each radiographic modality’s associated characteristics implemented in the screening process of COVID-19. | The study discusses AI with minimal details and lacks definition associated with the discipline of AI. | CXR and CT observations have been concluded to be the most effective diagnostic modalities. US works well with CT. A comprehensive description of MRI and PET is needed. |
| Technology and its Solutions in the Era of COVID-19 Crisis: A Review of Literature. | The study aims to investigate the technologies that have been applied to solve the COVID-19 crisis. | The review is logically organized and offers a balanced critical analysis of the literature. | Short conclusion | Technologies with the ability to reduce human contacts through teleservices and those that quickly enable decision-making via in-depth analysis received more attention among the health authorities and organizations. |
| Integrating emerging technologies into COVID-19 contact tracing: Opportunities, challenges and pitfalls. | The paper focuses on contact tracing apps by using GPS, Wi-Fi, Bluetooth, Social graph and Card transaction data to track users as well as AI. | Information was well organized in details. | Technical limitation Dealing with asymptomatic individuals. |
Integrating emerging technologies into COVID-19 contact tracing is seen as a viable option in mitigating coronavirus spread. |
| Imaging of COVID-19 pneumonia: Patterns, pathogenesis, and advances | To highlight common imaging findings using illustrative examples, describe the evolution of disease over time, discuss differences in imaging appearance of adult and pediatric patients and review the available literature on quantitative CT for COVID-19. | The article is critically organized. Clear and detailed background. The role of CT imaging in detecting the infection was clearly stated. |
Lack of a clear definition of artificial intelligence. | Medical imaging is an integral tool in the fight against COVID-19 using a collection of modalities (i.e. CXR, CT, MRI, and US) |
| Artificial intelligence vs COVID-19: limitations, constraints and pitfalls | Aims to tackle the topic of AI, namely, its shortages and limitation in terms of COVID-19 response. | Provides comparisons of relevant studies | Lack of visual data analysis to provide additional comprehension and illustration of the proposed findings. | AI measures are at early stages to be applicable. |
| A deep learning approach to characterize 2019 coronavirus disease (COVID-19) pneumonia in chest CT images | Study focuses on utilizing a deep learning model for automatic detection of abnormalities in chest CT images from COVID-19 patients. | Information was well organized in details. | Short study duration which may affect the results and the proposed model efficacy | The algorithm showed excellent performance in detecting COVID-19 pneumonia on chest CT images compared with resident radiologists. |
| Digital technology applications for contact tracing: the new promise for COVID-19 and beyond? | Discusses the digital technology applications that are used for the rapid tracing and notification of potentially infected people. | Included a table that illustrates the worldwide implementation of digital health technology for COVID-19 contact tracing. | There was no clear definition of Artificial intelligence (AI). | Digital technology can complement or in some cases amplify the traditional approach to global health program implementation. |
| Automated detection of COVID-19 cases using deep neural networks with X-ray images | Aims to explore a new model for automatic COVID-19 detection using raw chest X-ray images. | Images and graphs provided extra clarification to the reader. | Small sample size of X-ray images | This system can be used from remote places in COVID-19 affected countries to overcome a shortage of radiologists. |
| Impact of the digital divide in the age of COVID-19 | Show the impact of Digital Divide. | Information was well organized in details. | Insufficient references to support the conclusion. | The diminished accessibility to technology based on various social factors, sometimes referred to as the digital gap or digital divide, was being exposed at a critical time in a public health crisis. |
| Diagnosis of COVID-19 Pneumonia Using Chest Radiography: Value of Artificial Intelligence | To develop an artificial intelligence algorithm to differentiate COVID-19 pneumonia from other causes of CXR abnormalities. | The use of flowcharts, diagrams, tables, X-ray images clearly demonstrated the data. | The collected data may not reflect the true prevalence of the disease. | An artificial intelligence algorithm differentiated between COVID-19 pneumonia and non-COVID-19 pneumonia in chest x-ray radiographs with high sensitivity and specificity. |
| On the Interpretability of Artificial Intelligence in Radiology: Challenges and Opportunities | This review discusses radiologists’ opinions and suggestion trends and challenges that need to be addressed to effectively streamline interpretability methods in clinical practice. | Provides clear insights on each discussed modal including illustrative examples, charts, definitions, and operational work scenarios. | The study fails to discuss the implementation of presented methods in COVID-19. | Interpretability methods can improve understanding, trust, and verification of radiology artificial intelligence systems. |
| COVID-19 Detection using Artificial Intelligence | To develop a novel AI screening platform for usage and dissemination of COVID-19 x-rays. | The findings are confirmed with adjunct charts and tables and defines common AI concepts including deep learning, CNN, pooling, and convolutional layers. | The sample size is relatively small to promote generalization and validation of the proposed framework | The proposed model achieved sensitivity of 100 %, specificity of 100 %, accuracy of 100 %, PPV of 100%, and NPV of 100% in the dataset. |
| Advanced Digital Health Technologies for COVID-19 and Future Emergencies. | This article describes how digital health technologies are being or could be used for COVID-19 mitigation. | The article is well structured and critically organized | Lack of detailed discussion of the proposed technologies. | Digital technologies are capable of mitigating COVID-19 using a diverse range of applications to address the virus novelty. |
| Current Landscape of Imaging and the Potential Role for Artificial Intelligence in the Management of COVID-19 | To review the current landscape of imaging modalities and artificial intelligence approaches as applied in COVID-19 management. | Clearly states significant information of the current imaging paradigm on COVID-19 in addition to AI modals. | Lack of some additional radiographic modalities (i.e. MRI and US). | Artificial intelligence can enhance the predictive power and the utilization of these imaging approaches. |
| Review of Artificial Intelligence Techniques in Imaging Data Acquisition, Segmentation and Diagnosis for COVID-19 | To cover the scope of AI-assisted diagnostics and relevant clinical tests aimed to screen, study, detect, and diagnose in terms of COVID-19. | The review article provides a simplified outline of AI associated data inclusive of applications and future research prospects. | The paper lacks an explanation of the methodology applied in article selection and inclusion in the study findings. | This paper talks about how AI gives protected, exact and productive imaging arrangements in COVID-19 applications. Two modalities X-ray and CT are utilized to shows the adequacy of AI engaged clinical imaging for COVID-19. |
| End-to-end automatic differentiation of the coronavirus disease 2019 (COVID-19) from viral pneumonia based on chest CT | Autonomous differentiation of viral pneumonia from COVID-19 computed tomography findings. | The usage of figures and tables clarify the scope of the paper | The sampling population is relatively small which may impede the generalization of the proposed modal. | The novel AI platform generated a maximum specificity of 91 % and a sensitivity of 92% during the study’s training, testing, and validation stages. |
| Emerging Technologies for Use in the Study, Diagnosis, and Treatment of Patients with COVID-19 | The purpose of this review is to summarize emerging technologies being implemented in the study, diagnosis, and treatment of COVID-19’. | Clear explanation of emerging technologies including artificial Intelligence Well and detailed information about the treatments and type of medication and vaccination. |
Lack of detailed discussion of the proposed technologies’ limitations. | The advent of COVID-19 helped motivate researchers to investigate the scope and evidence related to technology’s efficacy against COVID-19. |
| Interpretable artificial intelligence framework for COVID‑19 screening on chest X‑rays | Development of a feasible AI model in terms of image interpretation of COVID-19 CXRs using transfer learning techniques and the evaluation of an expert radiologist panel. | The study utilized several quantitative metrics including sensitivity, specificity, accuracy, and area under curve. | Lack of training the AI module using larger sample size and additional input from experienced radiologists. | The transfer learning model was capable of undertaking binary, ternary, and quaternary at the area under curve of 1 during the management of a 5 stage dataset. |
| Applications of digital technology in COVID-19 pandemic planning and response | To provide a framework for the application of digital technologies in pandemic management and response. | Well summarized table of digital technology initiatives used in pandemic preparedness and response identifying every country that used that type of initiative. | No notable limitations were mentioned. | Successful repurposing of technology allowed several countries to flatten the curve of COVID-19 in their respective localities. |
| A Deep Learning System to Screen Novel Coronavirus Disease 2019 Pneumonia | This study aimed to establish an early screening model to distinguish COVID-19 from healthy cases through pulmonary CT images using deep learning techniques. | Information was well organized in details. | The study is limited to only one district in in China. | The proposed model achieved an overall accuracy rate of 86.7%, and would be a promising supplementary diagnostic method for frontline clinical doctors. |
| Automated detection and quantification of COVID-19 pneumonia: CT imaging analysis by a deep learning-based software | Triage of COVID-19 pneumonia using the deep learning software uAI. | A well-organized study was conducted using CT and uAI. | The sampling population is relatively small which may impede the proposed modal generalization. | The uAI Intelligent Assistant Analysis System detected COVID-19 pneumonia in addition to COVID-19 CT findings (i.e. GGOs and lobular lesions) |
| AI Augmentation of Radiologist Performance in Distinguishing COVID-19 from Pneumonia of Other Etiology on Chest CT | Evaluation of AI integrated image interpretation workflow in the differentiation of COVID-19 and other pulmonary findings on chest CTs. | The study is relevant and novel for demonstrating the effect of AI augmentation on radiologist performance in distinguishing COVID-19 from pneumonia of other etiology on chest CT. | There was a significant difference in baseline characteristics between COVID-19 and non-COVID-19 pneumonia patients which could have introduced bias. | Deep learning apparatus helped radiologists to improve the diagnostic performance in terms of COVID-19 at a 90% accuracy, 91% specificity, and 88% sensitivity. |
| Deep transfer learning artificial intelligence accurately stages COVID-19 lung disease severity on portable chest radiographs | Classification of COVID-19 severity on portable CXRs using deep learning CNNs and an expert radiologist panel. | Information was well organized in details. | Lack of detailed discussion of the proposed approach’s limitations. | The deep learning CNNs accomplished a comparable staging accuracy to the three-member radiologist panel at a mean absolute error of 8.5%. |
| How Might AI and Chest Imaging Help Unravel COVID-19′s Mysteries? | This article describes how AI has the potential to expand the role of chest imaging beyond the debatable realm of diagnosis to risk stratification, treatment monitoring, and potential discovery of novel therapeutic targets. | Information was well organized in details. | Summary/abstract was very short and not specific. | AI technologies can help to address multiple aspects of medical imaging during COVID-19 and beyond. |
| Applications of machine learning and artificial intelligence for Covid-19 (SARS-CoV-2) pandemic: A review | To discusses the application of machine learning and AI during COVID-19 using multiple encounters reported worldwide. | Employs summarization tables enabling complete comprehension and illustration of the presented information. | Lack of information about the integration of AI in COVID-19 related medical imaging. | COVID-19 allowed machine learning to surface in the medical community. Thus, exposing healthcare professional to contactless care. |
| Combat COVID-19 with artificial intelligence and big data. | To discuss the role of AI and big data in the mitigation of COVID 19, namely, Asian countries. | The article includes a summarization table that ensures additional comprehension of the presented information and offers background information on COVID-19 and the history of contact tracing apps in global epidemiological responses to infectious pandemics. | minimal information on the additional healthcare applications of AI during COVID-19. No other global contact tracing apps used in the mitigation of COVID-19 were discussed. | Effective COVID-19 responses are governed by the successful use of technology and public compliance to the digital interventions. |
References
- Adly A.S., Adly A.S., Adly M.S. Approaches based on artificial intelligence and the internet of intelligent things to prevent the spread of COVID-19: scoping review. J. Med. Internet Res. 2020 doi: 10.2196/19104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agbehadji I.E., Awuzie B.O., Ngowi A.B., Millham R.C. Review of big data analytics, artificial intelligence and nature-inspired computing models towards accurate detection of COVID-19 pandemic cases and contact tracing. Int. J. Environ. Res. Public Health. 2020;17(15):1–16. doi: 10.3390/ijerph17155330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albahri A.S., Al-Obaidi J.R., Zaidan A.A., Albahri O.S., Hamid R.A., Zaidan B.B., Alamoodi A.H., Hashim M. Multi-biological laboratory examination framework for the prioritization of patients with COVID-19 based on integrated AHP and group VIKOR methods. Int. J. Inf. Technol. Decis. Mak. 2020;19(5):1247–1269. doi: 10.1142/S0219622020500285. [DOI] [Google Scholar]
- Albahri O.S., Al-Obaidi J.R., Zaidan A.A., Albahri A.S., Zaidan B.B., Salih M.M., Qays A., Dawood K.A., Mohammed R.T., Abdulkareem K.H., Aleesa A.M., Alamoodi A.H., Chyad M.A., Zulkifli C.Z. Helping doctors hasten COVID-19 treatment: towards a rescue framework for the transfusion of best convalescent plasma to the most critical patients based on biological requirements via ml and novel MCDM methods. Comput. Methods Programs Biomed. 2020;196 doi: 10.1016/j.cmpb.2020.105617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albahri O.S., Zaidan A.A., Albahri A.S., Zaidan B.B., Abdulkareem K.H., Al-qaysi Z.T., Alamoodi A.H., Aleesa A.M., Chyad M.A., Alesa R.M., Kem L.C., Lakulu M.M., Ibrahim A.B., Rashid N.A. Systematic review of artificial intelligence techniques in the detection and classification of COVID-19 medical images in terms of evaluation and benchmarking: Taxonomy analysis, challenges, future solutions and methodological aspects. J. Infect. Public Health. 2020;13(10):1381–1396. doi: 10.1016/j.jiph.2020.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allam Z. Surveying the Covid-19 Pandemic and Its Implications. Elsevier; 2020. The rise of machine intelligence in the COVID-19 pandemic and its impact on health policy; pp. 89–96. 2020. [DOI] [Google Scholar]
- Apostolopoulos I.D., Aznaouridis S.I., Tzani M.A. Extracting possibly representative COVID-19 biomarkers from X-ray images with deep learning approach and image data related to pulmonary diseases. J. Med. Biol. Eng. 2020;40(3):462–469. doi: 10.1007/s40846-020-00529-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asefi H., Safaie A. The role of chest CT scan in diagnosis of COVID-19. Adv. J. Emergency Med. 2020;4(11):1–5. doi: 10.22114/ajem.v4i2s.451. [DOI] [Google Scholar]
- Bai H.X., Wang R., Xiong Z., Hsieh B., Chang K., Halsey K., Tran T.M.L., Choi J.W., Wang D.C., Shi L.B., Mei J., Jiang X.L., Pan I., Zeng Q.H., Hu P.F., Li Y.H., Fu F.X., Huang R.Y., Sebro R., Yu Q.Z., Atalay M.K., L. W AI Augmentation of Radiologist Performance in Distinguishing COVID-19 from Pneumonia of Other Etiology. Radiology. 2020;296(3):1–29. doi: 10.1148/radiol.2020201491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bansal A., Padappayil R.P., Garg C., Singal A., Gupta M., Klein A. Utility of artificial intelligence amidst the COVID 19 pandemic: a review. J. Med. Syst. 2020;44(9):19–24. doi: 10.1007/s10916-020-01617-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosso G., Allegorico E., Pagano A., Porta G., Serra C., Minerva V., Mercurio V., Russo T., Altruda C., Arbo P., De Sio C., Dello Vicario F., Numis F.G. Lung ultrasound as diagnostic tool for SARS-CoV-2 infection. Intern. Emerg. Med. 2020:0123456789. doi: 10.1007/s11739-020-02512-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bragazzi N.L., Dai Haijiang, Giovanni Damiani M.B., Martini M., Wu, J How big data and artificial intelligence can help against COVID-19. Int. J. Environ. Res. Public Health. 2020;17(9):1–8. doi: 10.3390/ijerph17093176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budd J., Miller B.S., Manning E.M., Lampos V., Zhuang M., Edelstein M., Rees G., Emery V.C., Stevens M.M., Keegan N., Short M.J., Pillay D., Manley E., Cox I.J., Heymann D., Johnson A.M., McKendry R.A. Digital technologies in the public-health response to COVID-19. Nat. Med. 2020;26(1):1183–1192. doi: 10.1038/s41591-020-1011-4. [DOI] [PubMed] [Google Scholar]
- Builtin . 2020. 19 Artificial Intelligence Examples You Should Know | Built In.https://builtin.com/artificial-intelligence/examples-ai-in-industry Retrieved January 26, 2021, from. [Google Scholar]
- Buonsenso D., Raffaelli F., Tamburrini E., Biasucci D.G., Salvi S., Smargiassi A., Inchingolo R., Scambia G., Lanzone A., Testa A.C., Moro F. Clinical role of lung ultrasound for diagnosis and monitoring of COVID-19 pneumonia in pregnant women. Ultrasound Obstet. Gynecol. 2020;56(1):106–109. doi: 10.1002/uog.22055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellina M., Orsi M., Toluian T., Valenti Pittino C., Oliva G. False negative chest X-Rays in patients affected by COVID-19 pneumonia and corresponding chest CT findings. Radiography. 2020;26(3):e189–e194. doi: 10.1016/j.radi.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury M.E.H., Rahman T., Khandakar A., Mazhar R., Kadir M.A., Mahbub Z., Bin, Islam K.R., Khan M.S., Iqbal A., Emadi N., Al, Reaz M.B.I., Islam M.T. Can AI Help in Screening Viral and COVID-19 Pneumonia? IEEE Access. 2020;8:132665–132676. doi: 10.1109/ACCESS.2020.3010287. [DOI] [Google Scholar]
- Convissar D.L., Gibson L.E., Berra L., Bittner E.A., Chang M.G. Application of lung ultrasound during the COVID-19 pandemic: a narrative review. Anesth. Analg. 2020;131(2):345–350. doi: 10.1213/ANE.0000000000004929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coombs C. Will COVID-19 be the tipping point for the Intelligent Automation of work? A review of the debate and implications for research. Int. J. Inf. Manage. 2020;55(1):1–5. doi: 10.1016/j.ijinfomgt.2020.102182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cozzi D., Albanesi M., Cavigli E., Moroni C., Bindi A., Luvarà S., Lucarini S., Busoni S., Mazzoni L.N., Miele V. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome. Radiologia Medica. 2020;125(8):730–737. doi: 10.1007/s11547-020-01232-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debnath S., Barnaby D.P., Coppa K., Makhnevich A., Kim E.J., Chatterjee S., Tóth V., Levy T.J., Paradis M.D., Cohen S.L., Hirsch J.S., Zanos T.P., Northwell COVID-19 Research Consortium Machine learning to assist clinical decision-making during the COVID-19 pandemic. Bioelectron. Med. 2020;6(14):1–8. doi: 10.1186/s42234-020-00050-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Tordello E., Rappuoli R., Delany I. Human Vaccines: Emerging Technologies in Design and Development. Academic Press; 2017. Reverse vaccinology: exploiting genomes for vaccine design; pp. 65–86. 2016. [DOI] [Google Scholar]
- Ding X., Xu J., Zhou J., Long Q. Chest CT findings of COVID-19 pneumonia by duration of symptoms. Eur. J. Radiol. 2020;127(April):109009. doi: 10.1016/j.ejrad.2020.109009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drew D.A., Nguyen L.H., Steves C.J., Menni C., Freydin M., Varsavsky T., Sudre C.H., Jorge Cardoso M., Ourselin S., Wolf J., Spector T.D., Chan A.T. Rapid implementation of mobile technology for real-time epidemiology of COVID-19. Science. 2020;6497(368):1362–1367. doi: 10.1126/science.abc0473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eastgate P., Neep M.J., Steffens T., Westerink A. COVID-19 Pandemic – considerations and challenges for the management of medical imaging departments in Queensland. J. Med. Radiat. Sci. 2020;(February):1–7. doi: 10.1002/jmrs.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ella Hassanien A., Salam A., Darwish A., Salam A.A., Darwsih A. 2020. EasyChair Preprint № 3223 Artificial Intelligence Approach to Predict the COVID-19 Patient’s Recovery Artificial Intelligence Approach to Predict the COVID-19 Patient’s Recovery. EasyChair.www.egyptscience.net [Google Scholar]
- Erturk S.M., Durak G., Ayyildiz H., Comert R.G., Medetalibeyoglu A., Senkal N., Uysal E., Tunaci A. Covid-19: correlation of early chest computed tomography findings with the course of disease. J. Comput. Assist. Tomogr. 2020;44(5):633–639. doi: 10.1097/RCT.0000000000001073. [DOI] [PubMed] [Google Scholar]
- Fagherazzi G., Goetzinger C., Rashid M.A., Aguayo G.A., Huiart L. Digital health strategies to fight COVID-19 worldwide: Challenges, recommendations, and a call for papers. J. Med. Internet Res. 2020;22(6):e19284. doi: 10.2196/19284. JMIR Publications Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fechner C., Strobel K., Treumann T., Sonderegger B., Azzola A., Fornaro J., Schrading S., Roos J.E. COVID-19 and the role of imaging: early experiences in Central Switzerland. Swiss Med. 2020;150(25–26):1–10. doi: 10.4414/smw.2020.20304. [DOI] [PubMed] [Google Scholar]
- Feng H., Liu Y., Lv M., Zhong J. A case report of COVID-19 with false negative RT-PCR test: necessity of chest CT. J. Radiol. 2020;38(5):409–410. doi: 10.1007/s11604-020-00967-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields B.K.K., Demirjian N.L., Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19) diagnostic technologies: a country-based retrospective analysis of screening and containment procedures during the first wave of the pandemic. Clin. Imaging. 2020;67(June):219–225. doi: 10.1016/j.clinimag.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getz F.M. Black Death and the silver lining: meaning, continuity, and revolutionary change in histories of medieval plague. J. Hist. Biol. 1991;24(2):265–289. doi: 10.1007/BF00209432. [DOI] [PubMed] [Google Scholar]
- Glatter K., Finkelman P. History of the plague: an ancient pandemic for the age of Covid-19. Am. J. Med. 2020;000(000):1–6. doi: 10.1016/j.amjmed.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenspan H., San José Estépar R., Niessen W.J., Siegel E., Nielsen M. Position paper on COVID-19 imaging and AI: from the clinical needs and technological challenges to initial AI solutions at the lab and national level towards a new era for AI in healthcare. Med. Image Anal. 2020;66 doi: 10.1016/j.media.2020.101800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon S.A., Sanford T.H., Xu S., Turkbey E.B., Roth H., Xu Z., Yang D., Myronenko A., Anderson V., Amalou A., Blain M., Kassin M., Long D., Varble N., Walker S.M., Bagci U., Ierardi A.M., Stellato E., Plensich G.G., Turkbey B. Artificial intelligence for the detection of COVID-19 pneumonia on chest CT using multinational datasets. Nat. Commun. 2020;11(1):1–7. doi: 10.1038/s41467-020-17971-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassounah M., Raheel H., Alhefzi M. Digital response during the COVID-19 pandemic in Saudi Arabia. J. Med. Internet Res. 2020;22(9):e19338. doi: 10.2196/19338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HealthManagement.org, & Team, E COVID-19: What Can Healthcare Learn? Health Manag. Org. J. 2020;20(2):126–129. doi: 10.3366/E135555020800009X. [DOI] [Google Scholar]
- Hoffman-Jeep L. Creating ethnography: zora neale Hurston and Lydia Cabrera. Afr. Am. Rev. 2005;39(3):337–353. doi: 10.2307/40033668. [DOI] [Google Scholar]
- Hussain A.A., Bouachir O., Al-Turjman F., Aloqaily M. AI techniques for COVID-19. IEEE Access. 2020;8:128776–128795. doi: 10.1109/ACCESS.2020.3007939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang E.J., Kim H., Yoon S.H., Goo J.M., Park C.M. Implementation of a deep learning-based computeraided detection system for the interpretation of chest radiographs in patients suspected for covid-19. Korean J. Radiol. 2020;21(10):1150–1160. doi: 10.3348/kjr.2020.0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapoor A., Guha S., Kanti Das M., Goswami K.C., Yadav R. Digital healthcare: The only solution for better healthcare during COVID-19 pandemic? Indian Heart J. 2020;72(2):61–64. doi: 10.1016/j.ihj.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keesara S., Jonas A., Schulman K. Covid-19 and health care’s digital revolution. N. Engl. J. Med. 2020:1–3. doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- Killingray D. The influenza pandemic of 1918-1919 in the British caribbean. Soc. Hist. Med. 1994;7(1):59–87. doi: 10.1093/shm/7.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H., Han Gyoonhee, Song Jae-Hoon. A review for artificial intelligence proving to fight against COVID-19 pandemic and prefatory health policy. J. Med. Biomed. Appl. Sci. 2020;8(8):494–506. doi: 10.15520/jmbas.v8i8.247. [DOI] [Google Scholar]
- Ko H., Chung H., Kang W.S., Kim K.W., Shin Y., Kang S.J., Lee J.H., Kim Y.J., Kim N.Y., Jung H., Lee J. COVID-19 pneumonia diagnosis using a simple 2d deep learning framework with a single chest CT image: model development and validation. J. Med. Internet Res. 2020;22(6):1–13. doi: 10.2196/19569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kricka L.J., Polevikov S., Park J.Y., Fortina P., Bernardini S., Satchkov D., Kolesov V., Grishkov M. Artificial intelligence-powered search tools and resources in the fight against covid-19. Electron. J. Int. Fed. Clin. Chem. Laboratory Med. 2020;31(2):106–116. [PMC free article] [PubMed] [Google Scholar]
- Kumar A., Gupta P.K., Srivastava A. A review of modern technologies for tackling COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14(4):569–573. doi: 10.1016/j.dsx.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kundu S., Elhalawani H., Gichoya J.W., Kahn C.E. How Might AI and Chest Imaging Help Unravel COVID-19’s Mysteries? Radiology: Artificial Intelligence. 2020;2(3):1–17. doi: 10.1148/ryai.2020200053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalmuanawma S., Hussain J., Chhakchhuak L. Applications of machine learning and artificial intelligence for Covid-19 (SARS-CoV-2) pandemic: a review. Chaos Solitons Fractals. 2020;139:1–6. doi: 10.1016/j.chaos.2020.110059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. Am. J. Roentgenol. 2020;214(6):1280–1286. doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- Li L., Qin L., Xu Z., Yin Y., Wang X., Kong B., Bai J., Lu Y., Fang Z., Song Q., Cao K., Liu D., Wang G., Xu Q., Fang X., Zhang S., Xia J., Xia J. Using artificial intelligence to detect COVID-19 and community-acquired pneumonia based on pulmonary CT: evaluation of the diagnostic accuracy. Radiology. 2020;296(2):E65–E71. doi: 10.1148/radiol.2020200905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Zhong Z., Li Y., Zhang T., Gao L., Jin D., Sun Y., Ye X., Yu L., Hu Z., Xiao J., Huang L., Tang Y. From community-acquired pneumonia to COVID-19: a deep learning–based method for quantitative analysis of COVID-19 on thick-section CT scans. Eur. Radiol. 2020;30(12):6828–6837. doi: 10.1007/s00330-020-07042-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62(10) doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Lin L., Hou Z. Combat COVID-19 with artificial intelligence and big data. J. Travel Med. 2020;27(5):1–4. doi: 10.1093/jtm/taaa080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madurai Elavarasan R., Pugazhendhi R. Restructured society and environment: a review on potential technological strategies to control the COVID-19 pandemic. Sci. Total Environ. 2020;725:1–18. doi: 10.1016/j.scitotenv.2020.138858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manna S., Wruble J., Maron S.Z., Toussie D., Voutsinas N., Finkelstein M., Cedillo M.A., Diamond J., Eber C., Jacobi A., Chung M., Bernheim A. COVID-19: a multimodality review of radiologic techniques, clinical utility, and imaging features. Radiology: Cardiothoracic Imaging. 2020;2(3):1–28. doi: 10.1148/ryct.2020200210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastaneh Z., Mouseli A. Technology and its solutions in the era of COVID-19 crisis: a review of literature. Evid. Based Health Policy, Manag. Econ. 2020;4(2):138–149. doi: 10.18502/jebhpme.v4i2.3438. [DOI] [Google Scholar]
- Mbunge E. Integrating emerging technologies into COVID-19 contact tracing: opportunities, challenges and pitfalls. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14(6):1631–1636. doi: 10.1016/j.dsx.2020.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MDDI . 2020. Quibim Combines AI and Imaging to Detect COVID-19.https://www.mddionline.com/artificial-intelligence/quibim-combines-ai-and-imaging-detect-covid-19 Retrieved January 26, 2021, from. [Google Scholar]
- Mei X., Lee H.C., Diao K., Huang M., Lin B., Liu C., Xie Z., Ma Y., Robson P.M., Chung M., Bernheim A., Mani V., Calcagno C., Li K., Li S., Shan H., Lv J., Zhao T., Xia J., Yang Y. Artificial intelligence-enabled rapid diagnosis of COVID-19 patients. medRxiv. medRxiv. 2020 doi: 10.1101/2020.04.12.20062661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiler S., Schaible J., Poschenrieder F., Scharf G., Zeman F., Rennert J., Pregler B., Kleine H., Stroszczynski C., Zorger N., Hamer O.W. Can CT performed in the early disease phase predict outcome of patients with COVID 19 pneumonia? Analysis of a cohort of 64 patients from Germany. Eur. J. Radiol. 2020;131(August):109256. doi: 10.1016/j.ejrad.2020.109256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagpal P., Narayanasamy S., Vidholia A., Guo J., Shin K.M., Lee C.H., Hoffman E.A. Imaging of COVID-19 pneumonia: patterns, pathogenesis, and advances. Br. J. Radiol. 2020;93(1113):20200538. doi: 10.1259/bjr.20200538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naudé W. Artificial intelligence vs COVID-19: limitations, constraints and pitfalls. AI Soc. 2020;35(3):761–765. doi: 10.1007/s00146-020-00978-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni Q., Sun Z.Y., Qi L., Chen W., Yang Y., Wang L., Zhang X., Yang L., Fang Y., Xing Z., Zhou Z., Yu Y., Lu G.M., Zhang L.J. A deep learning approach to characterize 2019 coronavirus disease (COVID-19) pneumonia in chest CT images. Eur. Radiol. 2020:1–11. doi: 10.1007/s00330-020-07044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obinata H., Ruan P., Mori H., Zhu W., Sasaki H., Tatsuya K., Wakana M., Tanaka M., Hsu P.-L., Yang D., Xu Z., Xu D., Tamura K., Yokobori S. 2020. Can Artificial Intelligence Predict the Need for Oxygen Therapy in Early Stage COVID-19 Pneumonia? [DOI] [Google Scholar]
- Oterino Serrano C., Alonso E., Andrés M., Buitrago N.M., Pérez Vigara A., Parrón Pajares M., Cuesta López E., Garzón Moll G., Martin Espin I., Bueno Barriocanal M., De Ceano-Vivas la Calle M., Calvo Rey C., Bret-Zurita M. Pediatric chest x-ray in covid-19 infection. Eur. J. Radiol. 2020;131(August) doi: 10.1016/j.ejrad.2020.109236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozturk T., Talo M., Yildirim E.A., Baloglu U.B., Yildirim O., Rajendra Acharya U. Automated detection of COVID-19 cases using deep neural networks with X-ray images. Comput. Biol. Med. 2020;121(1):1–12. doi: 10.1016/j.compbiomed.2020.103792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pu X., Chen K., Liu J., Wen J., Zhneng S., Li H. Machine learning-based method for interpreting the guidelines of the diagnosis and treatment of COVID-19. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi. 2020;37(3):365–372. doi: 10.7507/1001-5515.202003045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsetty A., Adams C. Impact of the digital divide in the age of COVID-19. J. Am. Med. Inf. Assoc.: JAMIA. 2020;27(7):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes M., Meier R., Pereira S., Silva C.A., Dahlweid F.-M., Tengg-Kobligk Hvon, Summers R.M., Wiest R. On the interpretability of artificial intelligence in radiology: challenges and opportunities. Radiology: Artificial Intelligence. 2020;2(3):1–12. doi: 10.1148/ryai.2020190043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roser M., Ritchie H., Ortiz-Ospina E., Hasell J. 2020. Coronavirus (COVID-19) Cases - Statistics and Research - Our World in Data. Our World in Data. [Google Scholar]
- Salman F.M., Abu-Naser S.S., Alajrami E., Abu-Nasser B.S., Ashqar B.A.M. COVID-19 detection using artificial intelligence. Int. J. Acad. Eng. Res. 2020;4(3):18–25. [Google Scholar]
- Scott B.K., Miller G.T., Fonda S.J., Yeaw R.E., Gaudaen J.C., Pavliscsak H.H., Quinn M.T., Pamplin J.C. Advanced digital health technologies for COVID-19 and future emergencies. Telemed. E-health. 2020;26(10):1–6. doi: 10.1089/tmj.2020.0140. [DOI] [PubMed] [Google Scholar]
- Shaikh F., Anderson M.B., Sohail M.R., Mulero F., Awan O., Dupont-Roettger D., Kubassova O., Dehmeshki J., Bisdas S. Current landscape of imaging and the potential role for artificial intelligence in the management of COVID-19. Curr. Probl. Diagn. Radiol. 2020;0(0):1–6. doi: 10.1067/j.cpradiol.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamekh A., Mahmoodpoor A., Sanaie S. COVID-19: is it the black death of the 21st century? Health Promot. Perspect. 2020;10(3):166–167. doi: 10.34172/hpp.2020.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi F., Wang J., Shi J., Wu Z., Wang Q., Tang Z., He K., Shi Y., Shen D. Review of artificial intelligence techniques in imaging data acquisition, segmentation and diagnosis for COVID-19. IEEE Rev. Biomed. Eng. 2020:1–13. doi: 10.1109/RBME.2020.2987975. [DOI] [PubMed] [Google Scholar]
- Song J., Wang H., Liu Y., Wu W., Dai G., Wu Z., Zhu P., Zhang W., Yeom K.W., Deng K. End-to-end automatic differentiation of the coronavirus disease 2019 (COVID-19) from viral pneumonia based on chest CT. Eur. J. Nucl. Med. Mol. Imaging. 2020;47(11):2516–2524. doi: 10.1007/s00259-020-04929-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultan L.R., Sehgal C.M. A review of early experience in lung ultrasound in the diagnosis and management of COVID-19. Ultrasound Med. Biol. 2020;46(9):2530–2545. doi: 10.1016/j.ultrasmedbio.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summers R.M. Artificial intelligence of COVID-19 imaging: a hammer in search of a nail. Radiology. 2020:204226. doi: 10.1148/radiol.2020204226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tayarani N., M. H Applications of artificial intelligence in battling against covid-19: a literature review. Chaos Solitons Fractals. 2020;142:110338. doi: 10.1016/j.chaos.2020.110338. Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsikala Vafea M., Atalla E., Georgakas J., Shehadeh F., Mylona E.K., Kalligeros M., Mylonakis E. Emerging Technologies for Use in the Study, Diagnosis, and Treatment of Patients with COVID-19. Cell. Mol. Bioeng. 2020;13(4):249–257. doi: 10.1007/s12195-020-00629-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsiknakis N., Trivizakis E., Vassalou E., Papadakis G., Spandidos D., Tsatsakis A., Sánchez‑García J., López‑González R., Papanikolaou N., Karantanas A., Marias K. Interpretable artificial intelligence framework for COVID‑19 screening on chest X‑rays. Exp. Ther. Med. 2020;20(2):727–735. doi: 10.3892/etm.2020.8797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Schaar M., Alaa A.M., Floto A., Gimson A., Scholtes S., Wood A., McKinney E., Jarrett D., Lio P., Ercole A. How artificial intelligence and machine learning can help healthcare systems respond to COVID-19. Mach. Learn. 2021;110(1):1–14. doi: 10.1007/s10994-020-05928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K., Kang S., Tian R., Zhang X., Wang Y. Imaging manifestations and diagnostic value of chest CT of coronavirus disease 2019 (COVID-19) in the Xiaogan area. Clin. Radiol. 2020;75(5):341–347. doi: 10.1016/j.crad.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehbe R.M., Sheng J., Dutta S., Chai S., Dravid A., Barutcu S., Wu Y., Cantrell D.R., Xiao N., Allen B.D., MacNealy G.A., Savas H., Agrawal R., Parekh N., Katsaggelos A.K. DeepCOVID-XR: an artificial intelligence algorithm to detect COVID-19 on chest radiographs trained and tested on a large US clinical dataset. Radiology. 2020:203511. doi: 10.1148/radiol.2020203511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitelaw S., Mamas M.A., Topol E., Van Spall H.G.C. Applications of digital technology in COVID-19 pandemic planning and response. The Lancet Digital Health. 2020;2(8):e435–e440. doi: 10.1016/S2589-7500(20)30142-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2020. WHO Coronavirus Disease (COVID-19) Dashboard. [Google Scholar]
- Xu X., Jiang X., Ma C., Du P., Li X., Lv S., Yu L., Ni Q., Chen Y., Su J., Lang G., Li Y., Zhao H., Liu J., Xu K., Ruan L., Sheng J., Qiu Y., Wu W., Li L. A deep learning system to screen novel coronavirus disease 2019 pneumonia. Engineering. 2020;xxxx(xxxx):0–7. doi: 10.1016/j.eng.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Z., Li X., Sun H., Wang J., Zhao T., Chen H., Ma Y., Zhu S., Xie Z. Rapid identification of COVID-19 severity in CT scans through classification of deep features. Biomed. Eng. Online. 2020;19(1):1–13. doi: 10.1186/s12938-020-00807-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue R.P.H., Lee H.F., Wu C.Y.H. Trade routes and plague transmission in pre-industrial Europe. Sci. Rep. 2017;7(1):1–10. doi: 10.1038/s41598-017-13481-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin. Immunol. 2020;215(1):1–8. doi: 10.1016/j.clim.2020.108427. https://doi.org/https://dx.doi.org/10.1016%2Fj.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Ran, Tie Xin, Qi Zhihua, Bevins Nicholas B., Zhang Chengzhu, Griner Dalton, Song Thomas K., Nadig Jeffrey D., Schiebler Mark L., Garrett John W., Ke Li, Reeder Scott B., G.-H. C Diagnosis of COVID-19 pneumonia using chest radiography: value of artificial intelligence. Radiology. 2020;0(0):1–42. doi: 10.1148/radiol.2020202944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Htao, Zhang Jsong, Zhang Hhua, Nan Ydong, Zhao Y., Fu Eqing, Xie Yhong, Liu W., Li Wping, Zhang Hjun, Jiang H., Li Cmei, Li Yyan, Ma Rna, Dang Skang, Gao Bbo, Zhang Xjing, Zhang T. Automated detection and quantification of COVID-19 pneumonia: CT imaging analysis by a deep learning-based software. Eur. J. Nucl. Med. Mol. Imaging. 2020;47(11):2525–2532. doi: 10.1007/s00259-020-04953-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Shen B., Abbasi A., Hoshmand-Kochi M., Li H., Duong T.Q. Deep transfer learning artificial intelligence accurately stages COVID-19 lung disease severity on portable chest radiographs. PLoS One. 2020;15(7 July):1–11. doi: 10.1371/journal.pone.0236621. [DOI] [PMC free article] [PubMed] [Google Scholar]