Abstract
In patients with challenging femoral vein anatomy, transcatheter patent foramen ovale (PFO) closure can be safely and effectively be done through the jugular veins guided by ICE from the arm. This novel technique can potentially save resources (anesthesia and TEE) and provide an option for patients without a femoral option.
Keywords: ICE from the arm, IVC thrombus, PFO, RIJ PFO closure
In patients with challenging femoral vein anatomy, transcatheter patent foramen ovale (PFO) closure can be safely and effectively be done through the jugular veins guided by ICE from the arm. This novel technique can potentially save resources (anesthesia and TEE) and provide an option for patients without a femoral option.

1. INTRODUCTION
Transcatheter patent foramen ovale (PFO) closure is typically done utilizing femoral access for both intracardiac echocardiography (ICE) and device deployment. We hereby report the first two cases of PFO closure through the jugular veins guided by ICE from the arm in patients without any femoral options secondary to large burden of clot in the IVC. This novel technique can potentially save resources (anesthesia and TEE cardiologist), provide an option for patients without a femoral option, and avoid complications secondary to mechanical ventilation needed to perform TEE.
Transcatheter patent foramen ovale (PFO) closure is typically done utilizing femoral access, and it is increasingly being performed guided by intracardiac echocardiography (ICE) rather than transesophageal echocardiogram (TEE). The procedure is considerably more challenging when femoral access is not feasible secondary to congenital or acquired causes. Few case reports have reported the use of the internal jugular veins to perform the procedure in special circumstances. 1 , 2 , 3 These procedures have all utilized general anesthesia and transesophageal echocardiogram to guide the closure device deployment. We hereby report two cases of PFO closure through the internal jugular vein guided by intracardiac echocardiography (ICE) through a left basilic vein access and under conscious sedation.
2. CASE REPORT
Our first patient is a 28‐year‐old male with hypercoagulable state secondary to methylenetetrahydrofolate (MTHFR) mutation complicated by multiple deep venous thromboses (DVT) who had stopped taking anticoagulation for few years. He is admitted to the hospital for acute DVT and multiple bilateral pulmonary emboli (PE). His vital signs showed sinus tachycardia at 110 bpm and a normal blood pressure. Further imaging with CT scan and lower extremity venous Doppler scans revealed bilateral lower extremity DVTs in femoral veins that extends into the inferior vena cava (IVC) with near occlusion of the IVC (Figure 1). An echocardiogram showed a PFO with predominant right‐to‐left shunt and an enlarged right ventricle (RV). The left ventricular ejection fraction was normal, and there were no other abnormalities on echocardiogram.
FIGURE 1.
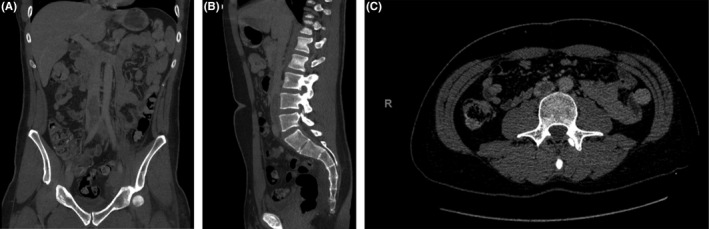
Extensive clot burden in the IVC prohibiting access from femoral veins
Our second patient is a 24‐year‐old female with history of recurrent DVTs and May‐Thurner syndrome with left common iliac vein stenting who has not been taking anticoagulation. She is admitted with acute multiple bilateral PEs with evidence of RV strain. Further imaging showed extensive thrombosis of her iliac venous system secondary to in‐stent thrombosis. An echocardiogram showed large PFO with bidirectional shunt.
For both cases, given the extensive clot burden in the ilio‐femoral and IVC system, PEs and RV strain on echo, the decision was made to perform transcatheter local thrombolysis using the EKOS catheter system. However, the presence of a large PFO with right‐to‐left shunting was concerning for paradoxical embolus, possible stroke, or systemic embolus during manipulation of equipment. Thus, after multidisciplinary team discussions, a PFO closure was planned prior to thrombolysis or any venous procedures for both patients.
3. DISCUSSION
For both of our patients, femoral access was not feasible secondary to large clot burden and fear of paradoxical embolus while inserting equipment in the femoral‐iliac venous system. Options for access for PFO closure device include (a) transjugular and (b) transhepatic. The procedure could be done with TEE guidance although ICE has been the predominant imaging modality for PFO closures in the United States. Options for access for ICE catheter include (a) transjugular, (b) transhepatic, or (c) left upper extremity venous access.
TEE requires general anesthesia and requires another operator to perform, thus we decided to perform the procedure with ICE guidance through the left upper extremity venous system utilizing the jugular vein for PFO closure.
Since transhepatic access can be complex, we elected to use the arm and the jugular veins to perform these procedures.
4. PROCEDURAL TECHNIQUE
Left basilic vein and right internal jugular vein access was obtained using ultrasound guidance (Figure 2A). A regular J wire was advanced through the basilic vein to the right atrium and was exchanged to an Amplatz Extra stiff wire over which a 10 Fr × 40 cm Cook sheath was advanced to right atrium. A St Jude ICE catheter (Abbott Vascular) was advanced to the right atrium and was passively exposed (Figure 2B). ICE was used to take detailed images of the intra‐atrial septum and the PFO tunnel (Video S1). The treating team should understand that ICE images are inverted compared to when ICE is used from the femoral side.
FIGURE 2.
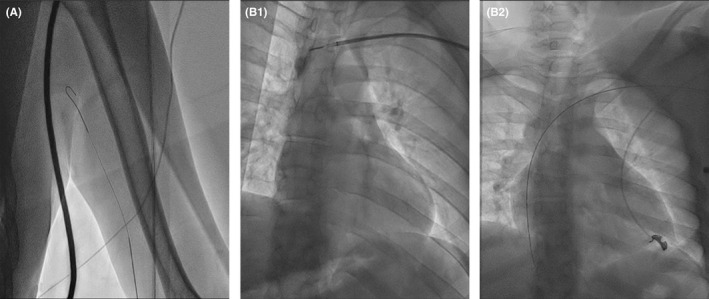
Access and sheath insertion. A, Left basilic vein access followed by inserting a 10 × 40 cm Cook sheath and ICE. B, Inserting a 10 x 40 cm Cook sheath and ICE
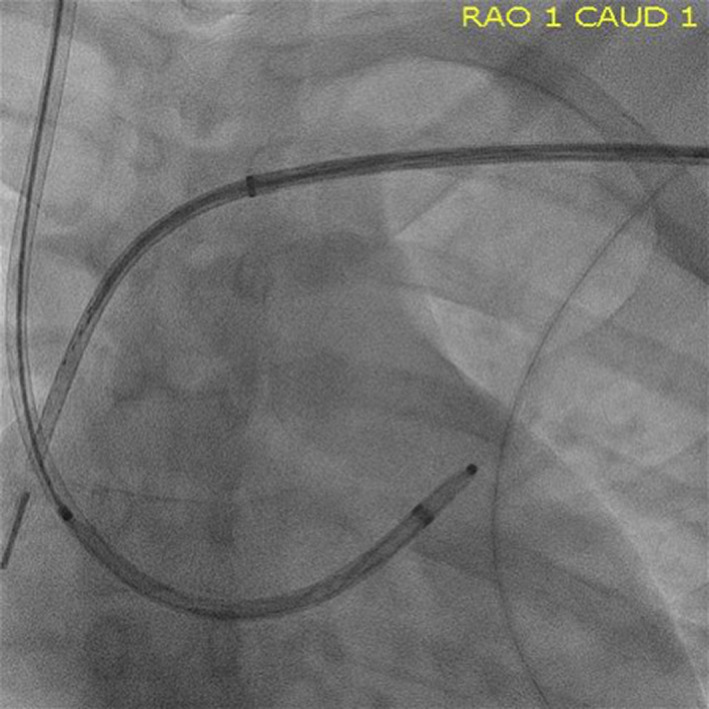
A short 9 Fr sheath was placed in the RIJ access. A small curl Agilis deflectable (Abbott Vascular, Santa Clara, CA) catheter and an angled glide wire were used to cross the septum (Video S2). In the first patient, the Agilis catheter was used to deploy the PFO closure device. In the second patient, the Agilis catheter was exchanged to TorqVue 120° sheath (Abbott Vascular, Santa Clara, CA) using an Amplatz Extra stiff wire in the pulmonary vein (Figure 3). A 35 mm PFO closure device (Abbott Vascular, Santa Clara, CA) is advanced to the left atrium through the TorqVue sheath (Figure 4) and deployed in the usual manner under ICE and fluoro guidance (Figure 5 and Video S3). ICE was used to study the intra‐atrial septum and once satisfied with the result, the device can be released (Video S4). ICE is used again to interrogate the PFO closure device (Figure 6).
FIGURE 3.
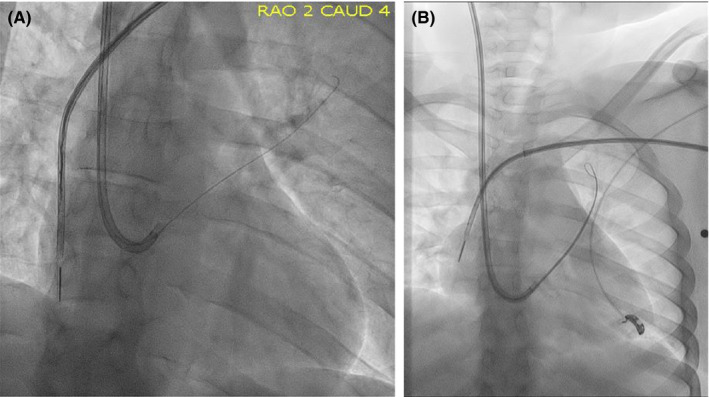
A wire is used to wire the pulmonary vein, and an MP diagnostic catheter is advanced over the wire to the pulmonary vein and exchanged for a Amplatz stiff wire, over which the TorqVue sheath is advanced across the PFO
FIGURE 4.
The PFO occluder device is advanced like usual through the TorqVue sheath
FIGURE 5.
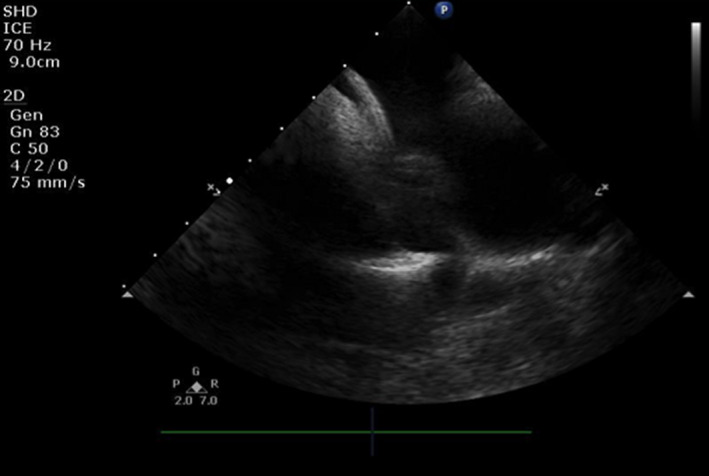
Deployment of the PFO occluder device using ICE and fluoro guidance
FIGURE 6.

After releasing the PFO occluder device, the device can be seen stable and in excellent position
5. ADVANTAGES AND LIMITATIONS
Many advantages exist to this novel technique. First, this can avoid mechanical ventilation in patients who can potentially be managed with conscious sedation that can save resources for the hospital. Moreover, these patients could potentially have issues with general anesthesia (side effects of medications and hemodynamic instability in the presence of large PEs and RV strain) and mechanical ventilation and perhaps would be better to avoid. Second, it does not require the presence of another cardiologist to perform TEE.
ICE from the arm could be challenging to interpret because it will be inverted. One way to go around that is to use the “invert” button on the echo machine. Operators familiar with ICE should have no problem with performing and correctly interpreting ICE from the arm. Closure of the 10 Fr basilic vein access could theoretically be an issue; however, we have closed both patients with pressure dressing and a coband without any complications.
6. CONCLUSION
We hereby report the first two cases of PFO closure through the jugular veins guided by ICE from the arm in patients without any femoral options secondary to large burden of clot in the IVC. This novel technique can potentially save resources (anesthesia and TEE cardiologist), provide an option for patients without a femoral option, and avoid complications secondary to mechanical ventilation needed to perform TEE.
CONFLICTS OF INTEREST
Marvin H. Eng is a clinical proctor for Edwards Lifesciences. Tiberio Frisoli is a clinical proctor for Edwards Lifesciences. William W. O’Neill is a consultant to Abiomed, Medtronic, and Boston Scientific. The remaining authors have no relevant relationships to disclose.
AUTHOR CONTRIBUTIONS
Mohammed Qintar MD MSc* and Marvin H Eng MD: performed the procedure and wrote the manuscript. Pedro Villablanca MD MSc, Tiberio Frisoli MD, Brian O’Neill MD, and William W O’Neill MD: wrote the manuscript, performed critical editing, and involved in data collection. James Lee MD and Dee Dee Wang MD: reviewed images and videos, and performed critical editing.
Supporting information
Video S1
Video S2
Video S3
Video S4
Qintar M, Villablanca P, Lee J, et al. Patent foramen ovale closure with vena cava thrombus: You need an arm and a neck!. Clin Case Rep. 2021;9:e03384. 10.1002/ccr3.3884
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, MQ, upon reasonable request.
REFERENCES
- 1. Hascoet S, Fraisse A, Elbaz M. Successful percutaneous transcatheter patent foramen ovale closure through the right internal jugular vein using a steerable catheter. Catheter Cardiovas Interv. 2013;82:E598‐602. [DOI] [PubMed] [Google Scholar]
- 2. Sader MA, De Moor M, Pomerantsev E, Palacios IF. Percutaneous transcatheter patent foramen ovale closure using the right internal jugular venous approach. Catheter Cardiovas Interv. 2003;60:536‐539. [DOI] [PubMed] [Google Scholar]
- 3. Fanari Z, Hammami S, Hopkins JT. Successful Percutaneous transcatheter patent foramen ovale closure through the right internal jugular vein using stiff amplatzer catheter with a reshaped tip. Delaware Med J. 2016;88:238‐241. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1
Video S2
Video S3
Video S4
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, MQ, upon reasonable request.


