Abstract
Background: A previous 2-year cohort study has shown that isolated high home systolic blood pressure (IH-HSBP) may increase the risk of diabetic nephropathy, using normal HBP as a reference. However, this association has not been previously assessed in the medium to long term. Methods: This prospective 5-year cohort study of 424 patients, with normal or mildly increased albuminuria, investigated the effect of IH-HSBP on the risk of diabetic nephropathy in patients with type 2 diabetes mellitus. Diabetic nephropathy was defined as an advancement from normal or mildly increased albuminuira to moderate or severely increased albuminuria. Results: Among 424 patients, 75 developed diabetic nephropathy during the study period. The adjusted odds ratio for developing diabetic nephropathy given IH-HSBP was 2.39 (95% confidence interval, 1.15–4.96, p = 0.02). The odds ratio for developing nephropathy in patients with IH-HSBP younger than 65 years was higher than that in patients with IH-HSBP older than 65 years. Conclusion: IH-HSBP was associated with an increased risk of diabetic nephropathy among type 2 diabetes mellitus patients with normal or mildly increased albuminuria in the medium to long term. The results support and strengthen previous reports. These findings suggest that IH-HSBP might be a useful marker in disease prognostication.
Keywords: albuminuria, diabetes mellitus, isolated high home systolic blood pressure, diabetic nephropathy
1. Introduction
Home blood pressure (HBP) control is paramount to diabetic nephropathy prevention [1]. Several important factors of HBP, including day-to-day variability [2] or pulse pressure [3], have been reported as relevant to the risk of diabetic nephropathy.
Isolated systolic hypertension (ISH) is diagnosed when systolic blood pressure (SBP) is hypertensive, while diastolic blood pressure (DBP) is normotensive [4]. ISH has been shown to increase the risk of premature mortality in patients with cardiovascular disease; it is a common form of hypertension [5,6,7].
ISH expressed as HBP (home ISH) has also been shown to affect the risk of diabetic nephropathy. In fact, our group has previously shown that isolated high home systolic blood pressure (IH-HSBP) might be a useful marker in the prognostication of diabetic nephropathy, based on data from a 2-year cohort study [8]. Nevertheless, the follow-up period in that study was relatively short, likely limiting its statistical power. To address this limitation, we performed a follow-up study with patients diagnosed with type 2 diabetes mellitus (DM), aiming to provide a valid assessment of the impact of ISH on the risk of diabetic nephropathy in this patient group over the medium to long term.
2. Design and Methods
We used the same resources in our previous study, which is based on data from the HBP cohort of patients with type 2 diabetes mellitus who had regularly attended the diabetes outpatient clinic at the Kyoto Prefectural University of Medicine Hospital or other general hospitals located in Japan (KAMOGAWA-HBP study) [1].
The present study included patients with type 2 DM; the impact of HBP on the risk of diabetic nephropathy was evaluated. Nephropathy was graded as follows: normal or mild albuminuria, defined as urinary albumin/creatinine ratio (UACR) < 30 mg per gram of creatinine (mg/g Cr); moderately increased albuminuria (microalbuminuria), defined as UACR 30–300 mg/g Cr; or severely increased albuminuria (macroalbuminuria), defined as UACR >300 mg/g Cr [9,10,11,12,13,14]. The development of diabetic nephropathy was defined as an advancement from normal or mild albuminuira to moderately or severely increased albuminuria within 5 years. The study protocol was approved by the local Research Ethics Committee, RBMR-E-349; the study adhered to the principles of the Declaration of Helsinki, and informed consent was obtained from all patients prior to enrollment.
2.1. Data Collection
Blood samples for biochemical measurements were taken in the morning. Serum lipid profile (including levels of triglycerides, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol) and levels of creatinine and hemoglobin A1C (HbA1c), and of other biochemical markers, were assessed by standard laboratory methods. The data collection of urinary samples was performed simultaneously with the beginning of HBP measurements. An immunoturbidimetric assay was used to measure UACR; the mean value of three consecutive urinary measurements was equivalent to UACR. Levels of HbA1c were classified and reported according to the National Glycohemoglobin Standardization Program guidelines, as recommended by the Japan Diabetes Society [15]. Data on patient demographic and clinical characteristics, including sex, age, duration of DM, smoking status, and those who consumed alcohol or antihypertensive medication were collected at the same time as HBP measurements began. To measure brachial–ankle pulse wave velocity (baPWV), the volume plethysmographic method was used, which was also the method utilized in our previous cohort study [16]. Diagnosis of diabetic nephropathy was based on the Diagnostic Nephropathy Study Group criteria [17]. Alcohol drinking status (never, social, or everyday) and smoking status (never, past, or current) were checked by interview. Type 2 DM was diagnosed when a fasting plasma glucose level was more than 126 mg/dl (7.0 mmol/L), or a random plasma glucose was more than 200 mg/dl (11.1 mmol/L), based on the American Diabetes Association criteria [18].
2.2. HBP Measurements
Patients were instructed to measure their BP 3 times each morning and evening for 14 consecutive days, and the 14-day average of the 3 morning and 3 evening mean values were calculated for each. Patients were instructed to measure their morning BP within 1 h of waking up, before breakfast, before taking medication, having sat, and having rested for at least 5 min [19]. Similar instructions applied to evening BP measurements, which were obtained before bedtime. Eating was prohibited for over one hour before measurement before going to bed. Moreover, patients were instructed that the cuff of the measuring device should be placed around the contralateral side of the dominant arm, with its position maintained at the level of the heart. HBP measurements were performed with an automated device—HEM-70801C (Omron Healthcare Co. Ltd., Kyoto, Japan)—which used a digital display to present values of SBP/DBP and heart rate, measured using the cuff-oscillometric method. HEM-70801C uses the same components and BP-determining algorithm as those of another device, HEM-705IT, which was previously validated and satisfied the criteria of the British Hypertension Society protocol [20].
In the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019) [21], the target level of HBP control is under 125/75 mmHg in hypertensive patients with DM. Patients were classified into 4 groups based on HBP levels: normal HBP (morning SBP < 125 mmHg and morning DBP < 75 mmHg), isolated high IH-HSBP (morning SBP > 125 mmHg and morning DBP < 75 mmHg), isolated high home DBP (IH-HDBP) (morning SBP < 125 mmHg and morning DBP > 75 mmHg), and high HBP (morning SBP > 125 mmHg and morning DBP > 75 mmHg) [21,22].
2.3. Statistical Analysis
Participant baseline characteristics were reported as median, with interquartile range or count, as suitable. Logistic regression analysis was used to assess the relationship between IH-HSBP, IH-HDBP, and high HBP, and the risk of diabetic nephropathy, with “normal HBP” set as a reference. The following factors were included as covariates in the adjusted models: sex, body mass index (BMI), duration of diabetes, levels of HbA1c, of total cholesterol, of creatinine, and use of antihypertensive medication (Model 2). Separate adjustments were made for the use of renin–angiotensin–aldosterone system inhibitors instead of other antihypertensive medications (Model 3).
In addition, subgroup analyses were performed for age (≥65 years vs. <65 years) and SBP control (≥135 mmHg vs. <135 mmHg). JSH2019 [21] adopted 135/85 mmHg as the diagnostic criterion for hypertension based on HBP. p-values < 0.05 were considered indicative of statistically significant findings. Statistical analyses were performed using JMP version 13.2 software (SAS Institute Inc., Cary, NC, USA).
3. Results
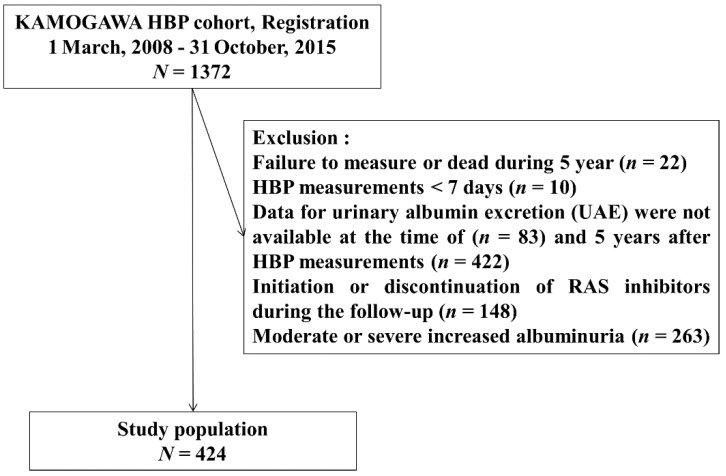
A total of 1372 consecutive patients with type 2 DM, aged 20–90 years, were recruited for this study. In all, 64 and 422 patients were excluded due to insufficient HBP and UACR data, respectively. In addition, there were 148 patients who were newly prescribed angiotensin II receptor blocker (ARB) or angiotensin-converting-enzyme inhibitor (ACE-I), or who stopped using them during follow-up. Another 263 patients who had moderately or severely increased albuminuria were also excluded.
The final sample included 424 patients with normal or mild albuminuria (Figure 1). Among them, during 5-year follow-up period, 74 patients developed moderately increased albuminuria and 1 patient developed severely increased albuminuria.
Figure 1.
Study flow diagram for the registration of patients.
Patient baseline demographic and clinical characteristics are presented in Table 1 and Table 2. Median (interquartile range) age, duration of diabetes, BMI, and levels of total cholesterol and those of HbA1C were 64.0 (59.0–70.0) years, 9.0 (4.8–15.0) years, 23.0 (21.4–25.3) kg/m2, 191 (170–212) mg/dL, and 6.6% (6.2%–7.3%), respectively. The patients in the IH-HSBP group were older than those in the high HBP group (69.6 vs. 60.6 years, p < 0.001). The unadjusted odds ratio (OR) with 95% confidence interval (CI) of developing diabetic nephropathy, given IH-HSBP, IH-HDBP, and high HBP, was 2.68 (1.36–5.30), 0.78 (0.21–2.81), and 1.63 (0.87–3.04), respectively (Table 3), using normal HBP as a reference. In multivariate analyses, adjusted OR (95% CI) of developing diabetic nephropathy, given IH-HSBP, was 2.36% (1.14%–4.89%, p = 0.02) in Model 2 and 2.39% (1.15%–4.96%, p = 0.02) in Model 3 (Table 3).
Table 1.
Characteristics of patients.
| Sex | |
|---|---|
| Male | 228 (53.8) |
| Female | 196 (46.2) |
| Age (y) | 64.0 (59.0–70.0) |
| Duration of diabetes (y) | 9.0 (4.8–15.0) |
| Body mass index (kg/m2) | 23.0 (21.4–25.3) |
| Mean morning systolic blood pressure (mmHg) | 128.1 (117.4–138.2) |
| Mean morning diastolic blood pressure (mmHg) | 73.2 (66.5–79.9) |
| Mean evening systolic blood pressure (mmHg) | 123.4 (115.0–133.1) |
| Mean evening diastolic blood pressure (mmHg) | 67.7 (61.9–74.2) |
| Clinic systolic blood pressure (mmHg) | 136.0 (123.0–146.0) |
| Clinic diastolic blood pressure (mmHg) | 76.7 (70.0–80.3) |
| Hemoglobin A1c (mmol/mol) | 52.0 (48.6–59.5) |
| Total cholesterol (mg/dL) | 191 (170–212) |
| Creatinine (mg/dL) | 0.70 (0.58–0.83) |
| eGFR (ml/min/1.732) | 75.0 (63.1–89.0) |
| baPWV | 1762 (1501–2002) |
| Smoking status | |
| Current smoker | 63 (18.1) |
| Past smoker | 109 (31.3) |
| Alcohol drinking | |
| everyday | 99 (28.6) |
| social | 71 (20.5) |
| Diabetic complications | |
| Retinopathy | 84 (23.5) |
| Neuropathy | 118 (31.8) |
| Neuropathy | 118 (31.8) |
| Macrovascular disease | 101 (27.0) |
| Use of antihypertensive medication | 192 (45.2) |
| RAS (−/+) | 267/156 |
For categorical variables, n (%) is presented. For continuous variables, median (interquartile range) is presented. eGFR, estimated glemerular filtration rate; baPWV, brachial–ankle pulse wave velocity; RAS, renin–angiotensin–aldosterone system.
Table 2.
Characteristics of patients according to the 4 groups based on HBP levels.
| Hypertension Status (n) | Normal HBP Group (152) | Isolated High HSBP Group (83) | Isolated High HDBP Group (30) | High HBP Group (159) |
|---|---|---|---|---|
| Male/female | 74/78 | 40/43 | 19/11 | 95/64 |
| Age (y) | 64 (58–70) | 69 (63–75) | 60 (45–65) | 63 (58–70) |
| Body mass index (kg/m2) | 22.1 (20.9–24.1) | 22.5 (21.2–24.7) | 23.8 (21.7–26.1) | 24.0 (21.8–26.4) |
| Mean morning systolic blood pressure (mmHg) | 115.5 (107.7–119.0 | 133.3 (128.8–139.6) | 120.0 (116.9–122.2) | 139.0 (132.2–146.1) |
| Mean morning diastolic blood pressure (mmHg) | 66.3 (62.6–69.0) | 69.4 (64.8–72.1) | 77.2 (76.4–81.6) | 81.6 (77.9–86.7) |
| Mean evening systolic blood pressure (mmHg) | 112.9 (107.6–119.3) | 129.6 (123.6–136.3) | 118.4 (114.7–123.5) | 131.1 (123.7–140.1) |
| Mean evening diastolic blood pressure (mmHg) | 62.9 (58.7–67.2) | 63.5 (60.0–67.6) | 74.3 (70.9–77.6) | 75.1 (70.4–80.6) |
| Clinic systolic blood pressure (mmHg) | 124.1 (114.5–134.8) | 141.3 (134.8–151.2) | 126.8 (119.0–143.3) | 140.7 (130.6–153.0) |
| Clinic diastolic blood pressure (mmHg) | 71.7 (65.8–76.0) | 71.7 (65.6–77.7) | 82.3 (78.3–92.0) | 83.0 (78.7–86.7) |
| Hemoglobin A1c (%) | 6.5 (6.2–7.1) | 6.8 (6.2–7.5) | 6.4 (6.0–6.8) | 6.7 (6.2–7.3) |
| Total cholesterol (mg/dL) | 188.5 (164.8–211.5) | 192 (170.5–206) | 189 (167–209) | 191 (175–216) |
| Creatinine (mg/dL) | 0.67 (0.55–0.80) | 0.69 (0.55–0.85) | 0.70 (0.62–0.78) | 0.70 (0.58–0.83) |
| eGFR (ml/min/1.732) | 77.8 (64.0–95.0) | 71.1 (58.0–85.0) | 84.5 (76.0–96.8) | 75.0 (64.3–86.0) |
| baPWV (cm/sec) | 1584 (1411–1858) | 1844 (1645–2059) | 1491 (1281–2150) | 1726 (1509–1995) |
| Smoking status (never/past/current) | 89/42/20 | 45/16/21 | 19/7/4 | 85/42/27 |
| Alcohol drinking (never/social/everyday) | 97/34/20 | 53/9/20 | 16/8/6 | 69/35/49 |
| Retinopathy (NDR/SDR/PDR) | 120/13/13 | 52/18/10 | 24/4/1 | 124/19/8 |
| Neuropathy (−/+) | 111/41 | 57/25 | 28/1 | 120/37 |
| Macrovascular complication (−/+) | 131/21 | 68/15 | 29/1 | 139/20 |
| Antihypertensive medication (−/+) | 103/49 | 39/44 | 22/8 | 68/91 |
| RAS (−/+) | 116/36 | 43/40 | 23/7 | 85/73 |
HBP, home blood pressure; HSBP, home systolic blood pressure; HDBP, home diastolic blood pressure; eGFR, estimated glemerular filtration rate; baPWV, brachial–ankle pulse wave velocity; NDR, no diabetic retinopathy; SDR, simple diabetic retinopathy; PDR, proliferative diabetic retinopathy; −, without; +, with. For categorical variables, n is presented. For continuous variables, median (interquartile range) is presented.
Table 3.
Unadjusted and adjusted odds ratios for the development of diabetic nephropathy.
| Hypertension Status (n) | Model 1 | * Model 2 | * Model 3 | |||
|---|---|---|---|---|---|---|
| Unadjusted OR (95%CI) | p Value | Adjusted OR (95%CI) | p Value | Adjusted OR (95%CI) | p Value | |
| Normal HBP group (152) | 1 | 1 | 1 | |||
| Isolated high HSBP group (83) | 2.68 (1.36–5.30) | 0.004 | 2.36 (1.14–4.89) | 0.020 | 2.39 (1.15–4.96) | 0.019 |
| Isolated high HDBP group (30) | 0.78 (0.21–2.81) | 0.701 | 0.54 (0.12–2.53) | 0.438 | 0.54 (0.12–52.5) | 0.434 |
| High HBP group (159) | 1.63 (0.87–3.04) | 0.126 | 1.57 (0.79–3.12) | 0.193 | 1.60 (0.81–3.17) | 0.173 |
HBP, home blood pressure; HSBP, home systolic blood pressure; normal HBP (morning SBP < 125 mmHg and morning DBP < 75 mmHg); isolated high HSBP (morning SBP > 125 mmHg and morning DBP < 75 mmHg); isolated high HDBP (morning SBP < 125 mmHg and morning DBP > 75 mmHg); and high HBP (morning SBP > 125 mmHg and morning DBP > 75 mmHg). * Model 2: Odds ratios were adjusted for sex, age, duration of diabetes mellitus, body mass index, hemoglobin A1C, total cholesterol, creatinine, and the use of antihypertensive medications. * Model 3: Odds ratios were adjusted for variables in Model 2 and additional adjustment for the use of renin–angiotensin system inhibitors instead of the use of antihypertensive medications.
In subgroup analyses, an adjusted OR (95% CI) for developing nephropathy, given IH-HSBP, was 1.68 (0.66–4.27) among age > 65 years (Table 4); meanwhile, in age < 65 years, an adjusted OR (95% CI) was 3.06% (0.63%–15.0%) (Table 4), using normal HBP as a reference.
Table 4.
Unadjusted and adjusted odds ratios for the development of diabetic nephropathy in patients equal to or more than 65 years old and less than 65 years old.
| Hypertension Status | Model 1 | * Model 2 | * Model 3 | |||
|---|---|---|---|---|---|---|
| Unadjusted OR (95%CI) | p Value | Adjusted OR (95%CI) | p Value | Adjusted OR (95%CI) | p Value | |
| ≥65 years old | ||||||
| Normal HBP group | 1 | 1 | 1 | |||
| Isolated high HSBP group | 1.90 (0.85–4.23) | 0.116 | 1.70 (0.67–4.33) | 0.263 | 1.68 (0.66–4.27) | 0.275 |
| <65 years old | ||||||
| Normal HBP group | 1 | 1 | 1 | |||
| Isolated high HSBP group | 3.08 (0.76–12.5) | 0.116 | 3.07 (0.62–15.1) | 0.167 | 3.06 (0.63–15.0) | 0.167 |
HBP, home blood pressure; HSBP, home systolic blood pressure; * Model 2: Odds ratios were adjusted for sex, age, duration of diabetes mellitus, body mass index, hemoglobin A1C, total cholesterol, creatinine, and the use of antihypertensive medications. * Model 3: Odds ratios were adjusted for variables in Model 2 and additional adjustment for the use of renin–angiotensin system inhibitors instead of the use of antihypertensive medications.
In subgroup analysis of SBP control, in patients with equal to or more than 135 mmHg, the adjusted odds ratio (95% CI) of IH-HSBP, using normal HBP as a reference group for the development of diabetic nephropathy, was 5.39% (1.92–18.6%) (Table 5). In patients with <135 mmHg, the adjusted odds ratio (95% CI) of IH-HSBP was 0.71% (0.32–1.35%) (Table 5). The odds of each adjusting factor for the development of diabetic nephropathy are presented in Table 6.
Table 5.
Unadjusted and adjusted odds ratios for the development of diabetic nephropathy in patients according to systolic blood pressure.
| Hypertension Status | Model 1 | * Model 2 | * Model 3 | |||
|---|---|---|---|---|---|---|
| Unadjusted OR (95%CI) | p Value | Adjusted OR (95%CI) | p Value | Adjusted OR (95%CI) | p Value | |
| ≥135 mmHg | ||||||
| Normal HBP group | 1 | 1 | 1 | |||
| Isolated high HSBP group | 4.21 (1.73–12.6) | 0.0009 | 5.59 (2.02–19.1) | 0.0005 | 5.39 (1.92–18.6) | 0.0008 |
| <135 mmHg | ||||||
| Normal HBP group | 1 | 1 | 1 | |||
| Isolated high HSBP group | 1.31 (0.63–2.52) | 0.452 | 0.75 (0.33–1.57) | 0.449 | 0.71 (0.32–1.35) | 0.384 |
HBP, home blood pressure; HSBP, home systolic blood pressure; * Model 2: Odds ratios were adjusted for sex, age, duration of diabetes mellitus, body mass index, hemoglobin A1C, total cholesterol, creatinine, and the use of antihypertensive medications. * Model 3: Odds ratios were adjusted for variables in Model 2 and additional adjustment for the use of renin–angiotensin system inhibitors instead of use of antihypertensive medications.
Table 6.
The odds of each adjusting factor for the development of diabetic nephropathy according to systolic blood pressure.
| SBP Control ≥ 135 mmHg | SBP Control < 135 mmHg | |
|---|---|---|
| Sex | 0.86 (0.36–1.98) | 0.69 (0.36–1.29) |
| Duration of diabetes | 0.99 (0.95–1.04) | 0.98 (0.95–1.01) |
| Body mass index | 1.08 (0.97–1.22) | 0.93 (0.86–1.01) |
| Hemoglobin A1c | 1.12 (0.73–1.80) | 0.73 (0.52–1.03) |
| Total cholesterol | 1.00 (0.99–1.02) | 0.99 (0.98–1.003) |
| Creatinine | 1.13 (0.51–6.26) | 0.74 (0.13–4.56) |
| Use of antihypertensive medication | 0.90 (0.38–2.06) | 0.69 (0.37–1.32) |
| Use of RAS | 1.00 (0.43–2.29) | 0.78 (0.40–1.56) |
SBP, systolic blood pressure; RAS, renin–angiotensin–aldosterone system.
4. Discussion
In the present study, IH-HSBP was associated with an increased risk of transition to moderate or severe albuminuria in patients with type 2 DM during a 5-year follow-up period.
The results are in line with the previous 2-year cohort study [8]. The mechanism likely to account for the association between IH-HSBP and diabetic nephropathy risk has been described elsewhere [23,24,25,26,27,28,29]. Increased arterial stiffness has been associated with the development of ISH [30]. Further arterial aging might result in additional increase of IH-HSBP, which is a risk factor for target organ dysfunction [31] and diabetic nephropathy [32]. The association between proteinuria and high BP is strictly related to very high risk of cardiovascular disease in type 2 diabetes [33,34]. In advanced type 2 diabetic nephropathy, appropriate management is of great importance [35]. So, we should adequately man-age home SBP. In HBP management, especially, we should clarify the association be-tween albuminuria and isolated high HSBP.
In the present study, IH-HSBP was associated with an increased risk of diabetic nephropathy; however, high HBP was not. The patients in the IH-HSBP group were older than those in the high HBP group. When arterial stiffness was compared between the IH-HSBP and High-HBP groups using baPWV measurements, there appeared to be higher arterial stiffness among patients in the IH-HSBP group than in those in the High-HBP group (Table S1) [16,36]. Arterial aging in IH-HSBP may be associated with increased odds for the development of diabetic nephropathy. Similarly, the isolated high HDBP group was not associated with an increased risk of diabetic nephropathy development. Those in the isolated HDBP group were younger, had a short duration of diabetes, lower baPWV, and also lower HSBP than the isolated high HSBP group (Table S2). For these reasons, only the isolated HSBP was associated with an increased risk of diabetic nephropathy development in this study.
The effect of IH-HSBP on the development of diabetic nephropathy, defined using estimated glomerular filtration rate (eGFR), is very important. Then, we analyzed the association between IH-HSBP and the development of diabetic nephropathy, defined using eGFR, and found that there was no relationship between them. We examined the association between changes in eGFR and the factors which were associated with IH-HSBP, including duration of diabetes or baPWV, and found no association. We assume that development of diabetic nephropathy, defined using ACR but not eGFR, was associated with pathophysiology of IH-HSBP in this study, although the precise mechanism is not unclear. Moreover, in this study, the mean (standard deviation) change in eGFR over 5 years was −0.37 (7.92) mL/min/1.732, which might be too small to properly analyze the development of diabetic nephropathy.
Initiation or discontinuation of anti-diabetic medications such as sodium glucose co-transporter (SGLT2) inhibitors may affect intra-glomerular pressure and the progression of diabetic nephropathy. However, SGLT2 inhibitors were not used at the start or during the initial 2-year follow-up period of this study. Among 424 patients with type 2 DM in the present cohort, 24 patients were newly prescribed SGLT2 inhibitors during the study period. Nevertheless, use of SGLT2 inhibitors did not affect the risk of diabetic nephropathy associated with IH-HSBP. Most present study patients were prescribed these agents for less than one year, which might have reduced their impact on outcomes of interest. Further studies are needed to examine this effect.
ISH among young-to-middle-aged Japanese people is associated with premature mortality due to cardiovascular disease [37]. In the present study, age-stratified subgroup analysis revealed that the adjusted OR was higher among patients aged <65 years than in those aged ≥65 years. These findings were consistent with those of our previous study [8], in that the association between IH-HSBP and diabetic nephropathy was weakened in patients ≥ 65. Among the patients with IH-HSBP ≥ 65, the progression of diabetic nephropathy was observed in 9.4% (2-year) and 9.5% (5-year). The progression of diabetic nephropathy did not increase over 3 years among the patients with IH-HSBP ≥ 65. Therefore, the association between IH-HSBP and diabetic nephropathy was weakened in patients aged ≥65. Meanwhile, subgroup analyses stratified by SBP status revealed that IH-HSBP increased the risk of diabetic nephropathy only in patients with SBP ≥ 135 mmHg. Patients with IH-HSBP may be at a lower risk if their SBP measurements meet the hypertension diagnostic criteria of less than 135 mmHg [21]. It should be noted that patients in this group were older and more likely to take antihypertensive medications than patients with SBP < 135 mmHg (Table S3). Patients with SBP ≥ 135 mmHg had remarkable ISH, which would be associated with arterial damage and diabetic nephropathy.
To the best of our knowledge, this is the first study to evaluate the impact of IH-HSBP on the risk of diabetic nephropathy in patients with type 2 DM over the medium to long term. The results support and strengthen previous reports. In addition, the risk of younger patients with ISH was elucidated through the 5-year follow-up period.
Nevertheless, this study has several limitations, which should be considered when interpreting its findings. First, we did not have data on salt intake, protein intake, or levels of exercise, which would be associated with the development of diabetic nephropathy [27,38,39,40,41]. In this regard, we could not clearly identify the prognostic significance of HBP for the development of diabetic nephropathy, even in a longer study. Second, only Japanese men and women were included in the study population. Therefore, these findings might not be generalized to other ethnic groups. Third, only single baseline measurements of BP were performed. This may be potential bias. However, the association of target organ damage was confirmed by BP at baseline or during follow-up [21]. Single BP assessments would be reliable when the addition of subsequent values does not significantly alter the results. Fourth, another important issue is the ultrasound findings on kidneys in the baseline, particularly the size of kidneys, which should be hypertrophic or enlarged before a moderately increased albuminuria development. However, these were not the ultrasound findings on kidneys. Fifth, the risk of ISH, defined by home BP on developing albuminuria in diabetic patients, was similar after the follow-up period and was prolonged for 3 years. The results were essentially similar to previous findings, and thus could not add new information for clinical science. We should at least prolong the follow-up period up to 10 years or more. Finally, a non-albuminuric phenotype has for years been reported in diabetic kidney disease (DKD) of type 2 DM [42]. Therefore, many patients with type 2 DM, despite being normoalbuminuric if they have a GRF of <60 mil/min/1.73m2, still have DKD. In the present study, we did not include patients with a GFR of <60 mil/min/1.73m2. Thus, we were not able to evaluate the decline in renal function in the definition of DKD in this study. Further studies will be conducted in the future.
5. Conclusions
In conclusion, IH-HSBP in patients with type 2 diabetes mellitus was a prognostic factor for the development of diabetic nephropathy in a prospective 5-year cohort study.
Acknowledgments
We thank Naoko Higo R.N., Machiko Hasegawa R.N., and Terumi Kaneko R.N. of the Kyoto Prefectural University of Medicine for teaching patients how to measure their blood pressure, and Sayoko Horibe, Hiroko Kawamura, and Aiko Aida, also of the Kyoto Prefectural University of Medicine, for their secretarial assistance. We thank Editage for English language editing.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10091929/s1, Table S1: The comparison of arterial stiffness among patients with isolated high HSBP or High-HBP, Table S2: The comparison of the patients with isolated high HSBP or isolated high HDBP, Table S3: The comparison of patients according to systolic blood pressure.
Author Contributions
N.K. (Nobuko Kitagawa) or N.K. (Noriyuki Kitagawa) designed the study, performed data analyses, and reviewed/edited the manuscript; E.U. designed the study, contributed to the collection of research data, performed data analyses, drafted the manuscript, and was the main study physician responsible for the KAMOGAWA-HBP study in Kyoto Prefectural University of Medicine, Graduate School of Medical Science; H.U., N.N. and M.H. designed the study protocol, reviewed data reports, and reviewed the study manuscript; I.Y. supervised data analysis, contributed to manuscript preparation, contributed to discussion, and reviewed/edited the manuscript; M.A. and M.Y. designed the study protocol, reviewed data reports, and reviewed the study manuscript; M.F. designed the protocol, performed data analyses, drafted the manuscript, and was the principal investigator of the Kyoto Prefectural University of Medicine, Graduate School of Medical Science, and lead principal investigator for the study. All authors reviewed and provided edits and comments on manuscript drafts. E.U. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors have read and agreed to the published version of the manuscript.
Funding
EU received grant support from the Japanese Study Group for Physiology and Management of Blood Pressure, and the Astellas Foundation for Research on Metabolic Disorders (grant number: 4024).
Institutional Review Board Statement
The study design was approved by the appropriate ethics review board. The ethics committee of Kyoto Prefectural University of Medicine approved the study, and the study was conducted in accordance with Declaration of Helsinki.
Informed Consent Statement
All study participants provided informed consent.
Data Availability Statement
Data are available upon reasonable request to the corresponding author.
Conflicts of Interest
N.K., N.K., E.U., H.U., N.N., M.H., M.A., M.Y., and M.F. have received grant and research support from AstraZeneca plc, Astellas Pharma Inc., Bristol-Myers Squibb K.K., Daiichi Sankyo Co., Ltd., Eli Lilly Japan K.K., Kyowa Hakko Kirin Company Ltd., Kowa Pharmaceutical Co., Ltd., Kissei Pharmaceutical Co., Ltd., MSD K.K., Mitsubishi Tanabe Pharma Corp., Novo Nordisk Pharma Ltd., Nippon Chemiphar Company Ltd., Sanwa Kagaku Kenkyusho Co., Ltd., Sanofi K.K., Taisho Toyama Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., and TERUMO Co. I.Y. has received grants from Japan Society for the Promotion of Science KAKENHI, and Health, Labour and Welfare Policy Research Grants, speaker fees from Chugai Pharmaceutical Co, AstraZeneca plt, Japan Tabacco Pharamaceutical Division, and Nippon Shinyaku Co. The remaining authors have nothing to declare. The sponsors were not involved in the study design; in the collection, analysis, interpretation of data; nor in the writing of this manuscript; nor in the decision to submit the article for publication. The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article. The authors declare that, although they are affiliated with a department that is supported financially by a pharmaceutical company, the authors received no current funding for this study, and department affiliation does not alter their adherence to all journal policies on sharing data and materials.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ushigome E., Oyabu C., Tanaka T., Hasegawa G., Ohnishi M., Tsunoda S., Ushigome H., Yokota I., Nakamura N., Oda Y., et al. Impact of masked hypertension on diabetic nephropathy in patients with type II diabetes: A KAMOGAWA-HBP study. J. Am. Soc. Hypertens. 2018;12:364–371. doi: 10.1016/j.jash.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Ushigome E., Matsumoto S., Oyabu C., Kitagawa N., Tanaka T., Hasegawa G., Ohnishi M., Tsunoda S., Ushigome H., Yokota I., et al. Prognostic significance of day-by-day variability of home blood pressure on progression to macroalbuminuria in patients with diabetes. J. Hypertens. 2018;36:1068–1075. doi: 10.1097/HJH.0000000000001657. [DOI] [PubMed] [Google Scholar]
- 3.Kitagawa N., Ushigome E., Matsumoto S., Oyabu C., Ushigome H., Yokota I., Asano M., Tanaka M., Yamazaki M., Fukui M. Prognostic significance of home pulse pressure for progression of diabetic nephropathy: KAMOGAWA-HBP Study. Hypertens. Res. 2018;41:363–371. doi: 10.1038/s41440-018-0024-6. [DOI] [PubMed] [Google Scholar]
- 4.Bulpitt C.J., Fletcher A.E., Thijs L., Steassen J.A., Antikainen R., Davidson C., Fagard R., Gil-Extremera B., Jääskivi M., O’Brien E., et al. Symptoms reported by elderly patients with isolated systolic hypertension: Baseline data from the SYST-EUR trial. Systolic Hypertension in Europe. Age Ageing. 1999;28:15–22. doi: 10.1093/ageing/28.1.15. [DOI] [PubMed] [Google Scholar]
- 5.Lakatta E.G. Mechanism of hypertension in the elderly. J. Am. Geriatr. Soc. 1989;37:780–790. doi: 10.1111/j.1532-5415.1989.tb02243.x. [DOI] [PubMed] [Google Scholar]
- 6.Messerli F.H., Ventura H., Aristimuno G.G., Suarez D.H., Dreslinski G.R., Frohlich E.D. Arterial compliance in systolic hypertension. Clin. Exp. Hypertens. 1982;4:1037–1044. doi: 10.3109/10641968209060772. [DOI] [PubMed] [Google Scholar]
- 7.Hozawa A., Ohkubo T., Nagai K., Kikuya M., Matubara M., Tsuji I., Ito S., Satoh H., Hisamichi S., Imai Y. Prognosis of isolatedsystolic and isolated diastolic hypertension as assessed by self-measurement of blood pressure at home: The Ohasamastudy. Arch. Intern. Med. 2000;160:3301–3306. doi: 10.1001/archinte.160.21.3301. [DOI] [PubMed] [Google Scholar]
- 8.Kitagawa N., Ushigome E., Tanaka T., Hasegawa G., Nakamura N., Ohnishi M., Tsunoda S., Ushigome H., Yokota I., Kitagawa N., et al. Isolated high home systolic blood pressure in patients with type 2 diabetes is a prognostic factor for the development of diabetic nephropathy: KAMOGAWA-HBP Study. Diabetes Res. Clin. Pract. 2019;158:107920. doi: 10.1016/j.diabres.2019.107920. [DOI] [PubMed] [Google Scholar]
- 9.Gerstein H.C., Mann J., Yi Q., Zinman B., Dinneen S.F., Hoogwerf B., Hallé J.P., Young J., Rashkow A., Joyce C., et al. Hope Study Investigators. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001;286:421–426. doi: 10.1001/jama.286.4.421. [DOI] [PubMed] [Google Scholar]
- 10.Kramer H., Jacobs D.R., Bild D., Post W., Saad M.F., Detrano R., Tracy R., Cooper R., Liu K. Urine albumin excretion and subclinical cardiovascular disease: The multi-ethnic study of atherosclerosis. Hypertension. 2005;46:38–43. doi: 10.1161/01.HYP.0000171189.48911.18. [DOI] [PubMed] [Google Scholar]
- 11.Krolewski A.S., Niewczas M.A., Skupien J., Gohda T., Smiles A., Eckfeldt J.H., Doria A., Warram J.H. Early progressive renal decline precedes the onset of microalbuminuria and its progression to macroalbuminuria. Diabetes Care. 2014;37:226–234. doi: 10.2337/dc13-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ushigome E., Fukui M., Sakabe K., Tanaka M., Inada S., Omoto A., Tanaka T., Fukuda W., Atsuta H., Ohnishi M., et al. Uncontrolled home blood pressure in the morning is associated with nephropathy in Japanese type 2 diabetes. Heart Vessels. 2011;26:609–615. doi: 10.1007/s00380-010-0107-z. [DOI] [PubMed] [Google Scholar]
- 13.Nakade Y., Toyama T., Furuichi K., Kitajima S., Miyajima Y., Fukamachi M., Sagara A., Shinozaki Y., Hara A., Shimizu M., et al. Impact of kidney function and urinary protein excretion on intima–media thickness in Japanese patients with type 2 diabetes. Clin. Exp. Nephrol. 2015;19:909–917. doi: 10.1007/s10157-015-1088-0. [DOI] [PubMed] [Google Scholar]
- 14.Levey A.S., Eckardt K.U., Dorman N.M., Christiansen S.L., Cheung M., Jadoul M., Winkelmayer W.C. Nomenclature for kidney function and disease-executive summary and glossary from a Kidney Disease: Improving Global Outcomes (KDIGO) consensus conference. Eur. Heart J. 2020;41:4592–4598. doi: 10.1093/eurheartj/ehaa650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kashiwagi A., Kasuga M., Araki E., Oka Y., Hanafusa T., Ito H., Tominaga M., Oikawa S., Noda M., Kawamura T., et al. Committee on the Standardization of Diabetes Mellitus-Related Laboratory Testing of Japan Diabetes Society. International clinical harmonization of glycated hemoglobin in Japan: From Japan Diabetes Society to National Glycohemoglobin Standardization Program values. J. Diabetes Investig. 2012;3:39–40. doi: 10.1111/j.2040-1124.2012.00207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kitagawa N., Ushigome E., Matsumoto S., Oyabu C., Ushigome H., Yokota I., Asano M., Tanaka M., Yamazaki M., Fukui M. Threshold value of home pulse pressure predicting arterial stiffness in patients with type 2 diabetes: KAMOGAWA-HBP study. J. Clin. Hypertens. 2018;20:472–477. doi: 10.1111/jch.13209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wada T., Haneda M., Furuichi K., Babazono T., Yokoyama H., Iseki K., Araki S., Ninomiya T., Hara S., Suzuki Y., et al. Research Group of Diabetic Nephropathy, Ministry of Health, Labour, and Welfare of Japan. Clinical impact of albuminuria and glomerular filtration rate on renal and cardiovascular events, and all-cause mortality in Japanese patients with type 2 diabetes. Clin. Exp. Nephrol. 2014;18:621–622. doi: 10.1007/s10157-013-0931-4. [DOI] [PubMed] [Google Scholar]
- 18.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2002;25:S5–S20. doi: 10.2337/diacare.25.2007.S5. [DOI] [PubMed] [Google Scholar]
- 19.Imai Y., Otsuka K., Kawano Y., Shimada K., Hayashi H., Tochikubo O., Miyakawa M., Fukiyama K., Japan Society of Hypertension Japanese Society of Hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens. Res. 2003;26:771–782. doi: 10.1291/hypres.26.771. [DOI] [PubMed] [Google Scholar]
- 20.Coleman A., Fraaman P., Steel S., Shennan A. Validation of the Omron 705IT (HEM-759-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Press. Monit. 2006;11:27–32. doi: 10.1097/01.mbp.0000189788.05736.5f. [DOI] [PubMed] [Google Scholar]
- 21.Umemura S., Arima H., Arima S., Asayama K., Dohi Y., Hirooka Y., Horio T., Hoshide S., Ikeda S., Ishimitsu T., et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019) Hypertens. Res. 2019;42:1235–1481. doi: 10.1038/s41440-019-0284-9. [DOI] [PubMed] [Google Scholar]
- 22.Kai H. Blood pressure management in patients with type 2 diabetes mellitus. Hypertens. Res. 2017;40:721–729. doi: 10.1038/hr.2017.55. [DOI] [PubMed] [Google Scholar]
- 23.Franklin S.S., Gustin W., Ⅳ., Wong N.D., Larson M.G., Weber M.A., Kannel W.B., Levy D. Hemodynamic patterns of age-related changes in blood pressure. Framingham Heart Study. Circulation. 1997;96:308–315. doi: 10.1161/01.CIR.96.1.308. [DOI] [PubMed] [Google Scholar]
- 24.Safar M.E. Arterial aging-hemodynamic changes and therapeutic options. Nat. Rev. Cardiol. 2010;7:442–449. doi: 10.1038/nrcardio.2010.96. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell G.F., Conlin P.R., Dunlap M.E., Lacourrvciere Y., Arnold J.M.O., Ogilvie R.I., Neutel J., Izzo J.L., Jr., Pfeffer M.A. Aortic diameter, wall stiffness, and wave reflection in systolic hypertension. Hypertension. 2008;51:105–111. doi: 10.1161/HYPERTENSIONAHA.107.099721. [DOI] [PubMed] [Google Scholar]
- 26.Messerli F.H., Frohlich E.D., Suarez D.H., Dreslinski G.R., Dunn F.G., Cole F.E. Borderline hypertension: Relationship between age, hemodynamics, and circulating catecholamines. Circulation. 1981;64:760–764. doi: 10.1161/01.CIR.64.4.760. [DOI] [PubMed] [Google Scholar]
- 27.Julius S., Pascual A.V., London R. Role of parasympathetic inhibition in the hyperkinetic type borderline hypertension. Circulation. 1971;44:413–418. doi: 10.1161/01.CIR.44.3.413. [DOI] [PubMed] [Google Scholar]
- 28.Ekundayo O.J., Allman R.M., Sanders P.W., Aban I., Love T.E., Arnett D., Ahmed A. Isolated systolic hypertension and incident heart failure in older adults: A propensity-matched study. Hypertension. 2009;53:458–465. doi: 10.1161/HYPERTENSIONAHA.108.119792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.D’Sell D.R., Monnier V.M. Molecular basis of arterial stiffening: Role of glycation—A mini-review. Gerontology. 2012;58:227–237. doi: 10.1159/000334668. [DOI] [PubMed] [Google Scholar]
- 30.Kamoi K., Miyakoshi M., Soda S., Kaneko S., Nakagawa O. Usefulness of home blood pressure measurement in the morning in type 2 diabetic patients. Diabetes Care. 2002;25:2218–2223. doi: 10.2337/diacare.25.12.2218. [DOI] [PubMed] [Google Scholar]
- 31.Tomiyama H., Shiina K., Nakano H., Iwasaki Y., Matsumoto C., Fujii M., Chikamori T., Yamashina A. Arterial stiffness and pressure wave reflection in the development of isolated diastolic hypertension. J. Hypertens. 2020;38:2000–2007. doi: 10.1097/HJH.0000000000002519. [DOI] [PubMed] [Google Scholar]
- 32.Ushigome E., Hamaguchi M., Matsumoto S., Oyabu C., Omoto A., Tanaka T., Fukuda W., Hasegawa G., Mogami S., Ohnishi M., et al. Optimal home SBP targets for preventing the progression of diabetic nephropathy in patients with type 2 diabetes mellitus. J. Hypertens. 2015;33:1853–1859. doi: 10.1097/HJH.0000000000000636. discussion 1859. [DOI] [PubMed] [Google Scholar]
- 33.Minutolo R., Gabbai F.B., Provenzano M., Chiodini P., Borrelli S., Garofalo C., Sasso F.C., Santoro D., Bellizzi V., Conte G., et al. Cardiorenal prognosis by residual proteinuria level in diabetic chronic kidney disease: Pooled analysis of four cohort studies. Nephrol. Dial. Transplant. 2018;33:1942–1949. doi: 10.1093/ndt/gfy032. [DOI] [PubMed] [Google Scholar]
- 34.Sasso F.C., Nicola L.D., Carbonara O., Nasti R., Minutolo R., Salvatore T., Conte G., Torella R. Cardiovascular risk factors and disease management in type 2 diabetic patients with diabetic nephropathy. Diabetes Care. 2006;29:498–503. doi: 10.2337/diacare.29.03.06.dc05-1776. [DOI] [PubMed] [Google Scholar]
- 35.Minutolo R., Sasso F.C., Chiodini P., Cianciaruso B., Carbonara O., Zamboli P., Tirino G., Pota A., Torella R., Conte G., et al. Management of cardiovascular risk factors in advanced type 2 diabetic nephropathy: A comparative analysis in nephrology, diabetology and primary care settings. J. Hypertens. 2006;24:1655–1661. doi: 10.1097/01.hjh.0000239303.93872.31. [DOI] [PubMed] [Google Scholar]
- 36.Ninomiya T., Kojima I., Doi Y., Fukuhara M., Hirakawa Y., Hata J., Kitazono T., Kiyohara Y. Brachial-ankle pulse wave velocity predicts the development of cardiovascular disease in a general Japanese population: The Hisayama study. J. Hypertens. 2013;31:477–483. doi: 10.1097/HJH.0b013e32835c5c23. [DOI] [PubMed] [Google Scholar]
- 37.Hiramatsu T., Miura K., Ohkubo T., Kadota A., Kondo K., Kita Y., Hayakawa T., Kanda H., Okamura T., Okayama A., et al. NIPPON DATA80 Research Group. Isolated systolic hypertension and 29-year cardiovascular mortality risk in Japanese adults aged 30–49 years. J. Hypertens. 2020;38:2230–2236. doi: 10.1097/HJH.0000000000002533. [DOI] [PubMed] [Google Scholar]
- 38.Ha S.K. Dietary salt intake and hypertension Electrolyte. Blood Press. 2014;12:7–18. doi: 10.5049/EBP.2014.12.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Machnik A., Neuhofer W., Jantsch J., Dahlmann A., Tammela T., Machura K., Park J.K., Beck F.X., Müller D.N., Derer W., et al. Macrophages regulate salt-dependent volume and blood pressure through a vascular endothelial growth factor-C-dependent buffering mechanism. Nat. Med. 2009;15:545–552. doi: 10.1038/nm.1960. [DOI] [PubMed] [Google Scholar]
- 40.Zhu H.G., Jiang Z.S., Gong P.Y., Zhang D.M., Zou Z.W., Zhang Q., Ma H.M., Guo Z.G., Zhao J.Y., Dong J.J., et al. Efficacy of low-protein diet for diabetic nephropathy: A systematic review of randomized controlled trials. Lipids Health Dis. 2018;17:141. doi: 10.1186/s12944-018-0791-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao W., Katzmarzyk P.T., Horswell R., Wang Y., Li W., Johnson J., Heymsfield S.B., Cefalu W.T., Ryan D.H., Hu G. Aggressive blood pressure control increases coronary heart disease risk among diabetic patients. Diabetes Care. 2013;36:3287–3296. doi: 10.2337/dc13-0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Penno G., Solini A., Orsi E., Bonora E., Fondelli C., Trevisan R., Vedovato M., Cavalot F., Lamacchia O., Scardapane M., et al. Non-albuminuric renal impairment is a strong predictor of mortality in individuals with type 2 diabetes: The Renal In-sufficiency And Cardiovascular Events (RIACE) Italian multicentre study. Diabetologia. 2018;61:2277–2289. doi: 10.1007/s00125-018-4691-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request to the corresponding author.