Abstract
Owing to progressive population aging, elderly people (aged 65 and above) face challenges in carrying out activities of daily living, while placement of the elderly in a care facility is expensive and mentally taxing for them. Thus, there is a need to develop their own homes into smart homes using new technologies. However, this raises concerns of privacy and data security for users since it can be handled remotely. Hence, with advancing technologies it is important to overcome this challenge using privacy-preserving and non-intrusive models. For this review, 235 articles were scanned from databases, out of which 31 articles pertaining to in-home technologies that assist the elderly in living independently were shortlisted for inclusion. They described the adoption of various methodologies like different sensor-based mechanisms, wearables, camera-based techniques, robots, and machine learning strategies to provide a safe and comfortable environment to the elderly. Recent innovations have rendered these technologies more unobtrusive and privacy-preserving with increasing use of environmental sensors and less use of cameras and other devices that may compromise the privacy of individuals. There is a need to develop a comprehensive system for smart homes which ensures patient safety, privacy, and data security; in addition, robots should be integrated with the existing sensor-based platforms to assist in carrying out daily activities and therapies as required.
Keywords: elderly, independent living, privacy-preserving, smart homes, sensors, unobtrusive
1. Introduction
Progressive population aging is a global phenomenon. Improvements in public health, medicine, nutrition, and workplace safety standards have contributed to higher life expectancy. According to a United Nations report, the population aged ≥ 65 years is projected to be approximately 2 billion by 2050 [1]. This exponential increase in the aging population is liable to impose a significant burden on the socioeconomic well-being of many countries. Healthcare systems across the world will face the challenge of delivering efficient services to better educated, elderly population within strict budgetary constraints.
Elderly individuals tend to face difficulties in carrying out routine daily activities [2], which may make them dependent on caregivers or family members. In addition to the increased prevalence of comorbid conditions, elderly individuals tend to develop cognitive impairment with progression of age. Low physical strength [3], age-related dementia [4], depression [5], behavioral changes [6], and compromised communication skills [7] are some of the other issues that contribute to the increased dependency of elderly people.
Placement of the elderly in a nursing home or a care facility against their will has a detrimental effect on their well-being; it often leads to social isolation, depression, and greater dependency for completing self-care tasks [8]. Elderly people typically prefer to live in their homes rather than in a facility even when they require specialized care. In a survey, 30% of individuals over the age of 65 years were of the opinion that they would “rather die” than enter a nursing home [8]. The considerable costs involved in the care of an aging population and the perennial shortage of healthcare professionals [9] have prompted efforts by both industry and researchers to develop and test alternate models of care [10]. In particular, several studies have investigated the feasibility and effectiveness of systems for assistance and health monitoring of elderly in their home environment [11].
Remote health monitoring by leveraging technology is an efficient and cost-effective solution [12] to promote the well-being of the elderly by allowing them to age in place within the comfort of their own home; at the same time, they can be monitored and taken care of with use of technology that can predict any abnormal behavior and can alert the caregivers accordingly. This technology can allow an elderly person to live independently without the constant need for help from a family member or friend, boosting their moral and confidence. These remote monitoring systems do not intrude the daily lives and also allow real-time tracking of important functional parameters with few human resources and at reduced cost. The main objective of all smart solutions is to improve the quality of life (QoL) of the user [13]. The World Health Organization (WHO) defines QoL as the “individual’s perception of their position in life in the context of the culture and value systems and in relation to their goals, expectations, standards and concerns. It is a broad ranging concept affected in a complex way by the persons’ physical health, psychological state, level of independence, social relationships and their relationship to salient features of their environment” [14].
Artificial intelligence (AI), and machine learning algorithms are being widely used in smart technology applications. They may be applied in the entire network of sensors or just may be to as a part of the smart home. It can help in device management, energy conservation, health monitoring, intelligent communication, security and assistive personal robots by using data processing, prediction-making, voice recognition, decision-making and activity recognition [15]. Voice and image recognition via AI are being used in many smart home products, whereas prediction-making, activity recognition and data processing are being widely studied and enhanced.
Development of an effective and impactful smart home requires investigation of various susceptibility issues associated with the elderly people. These homes offer a safe and welcome space for elderly. Safety is the top priority for these concepts of smart care [16]. But there are chances of emergency events or incidents, which may occur due to the old age nature, like falls or urgent health issues. However, the current technology has incorporated methods to prevent and detect critical situations [17]. The advancement of technology allows the applied models to detect if a particular situation or event is an emergency or not. These methods can be used and provide immediate assistance when required.
Preserving the user privacy is another crucial aspect that needs due attention in smart home development technology. In Internet of Things (IoT) applications, users provide personal data to different devices and services, whereby privacy becomes extremely vulnerable [18,19,20].
In particular, location-based service (LBS), which uses personal data of users, is becoming increasingly popular [21]. Preservation of users’ identity (and hence the personal information) from the service providers (SPs) has attracted the attention of many researchers. The technology needs to be robust to protect the privacy and be non-intrusive, so that the users can trust their systems and take full advantage of it. Existing architecture needs to be more inclined towards security and privacy [22]. A less secure smart home can lead to exposure of the personal information of users to strangers or malicious entities. To the best of our knowledge, no standard definition for privacy-preserved age in place is available in the literature.
The usage of various technologies like sensors, cameras, robots, artificial intelligence, voice-based protocols, in a home or a building may improve the quality of life, well-being, energy conservation, safety and productivity [23,24,25,26,27]. The utilization of Internet of Things (IoT) has increased, creating a network of different objects, like sensors, actuators, mobile devices, tablets, etc. [28].
These remote monitoring technologies use sensors [29,30,31,32] and cameras [33] to monitor the elderly, detect falls or for emergency situations. Developments in technology have led to usage of wireless sensor networks placed all over the house at designated points, which collects the data and is usually processed and analyzed by controlled thru a suitable algorithm to give report to the caretaker or healthcare provider. Various types of sensors, have been used, be it environmental sensors, water sensors, temperature sensors, wearable sensors to keep track to numerous activities like, water usage, sleeping patterns, walking patterns, eating patterns, etc.
Several reviews have assessed the requirements of older adults in the context of home-based health care or telecare [34,35]; however, two systematic reviews specifically examined the facets of aging in place, i.e., a systematic review on cost effectiveness of aging in place [36] and a systematic review of acceptance of technology for aging in place [37]. The authors of the first review [36] found that the existing technologies were of low quality; in addition, the authors were not able to draw any definitive conclusions owing to lack of standardization of measurement indices in various studies. The technology acceptance review identified issues pertaining to discretion and affordability, control and freedom, and anxiety of stigmatization and institutionalization [37]. These two reviews have contributed significantly to the understanding of the concept of aging-in-place; however, each review was focused on a single aspect of the lived experience. Another review [38] synthesized and evaluated the existing qualitative evidence pertaining to aging in place in the US. The value of aging in place is determined and affected by various factors such as culture and differences in economic and social structure [39]. This review [38] was based on experiences in the US and the findings may not be entirely generalizable to other countries.
Few reviews talk about the application of AI technology to smart homes. One review [40] evaluated the intelligent surveillance systems in smart home environments, another review [41] investigated philosophical keystones and how they assist healthcare workers, scientist to collaborate with engineers to develop intelligent health-assistive smart homes. Kumar et al. [42] discussed the different variety of home automation systems and how they use AI tools. These systems were mostly applied as comfort ability, remote control, optimal resource utilization, and security.
It was noted that there were very few reviews which target the protection of privacy in the smart homes designed for the elderly. Given the availability of literature there is a need to review the current strategies and how they can be further enhanced. The current status of the research needs to be analyzed and evaluated for the various features that constitute in development of smart home, how each of these features can be further advanced in terms of technology and usability, how they can be made secure and unobtrusive, so that the users do not feel that they are under surveillance. The objective of this systematic literature review was to identify the different types of smart-home solutions or technology-based strategies available to assist the elderly to live independently in their homes and assess the current state of privacy preserving technologies incorporated into these homes.
2. Methods
A systematic literature review (SLR) condenses existing proof, identifying holes and identifies directions for future research.
Search Strategy
An extensive literature research was performed in the PubMed, SCOPUS and IEEE Xplorer databases. The keywords used were “smart homes”, “elderly”, “aging in place”, “non-intrusive”, “privacy preserving”, and “independent living”. They were used in combinations like the following:
Smart Home AND (Elderly OR Aging in place) OR (Non-Intrusive OR Privacy)
Smart Home AND (Elderly OR Aging in place) AND Non-Intrusive
Smart Home AND Elderly AND Privacy
Using advanced search techniques, the databases were searched, in combinations of these terms appearing in all metadata (title, abstract, keywords, full text) and were later screen according to various criteria mentioned in the next section.
The retrieved articles were shortlisted, and duplicate publications were removed. Subsequently, the titles and abstracts of the remaining studies were screened against the following criteria.
The inclusion criteria were:
Studies published in English.
Studies that used technology in the home, both technologies embedded in the home or independent technology (such as a robot).
Addressed the needs of older adults living independently both healthy and elderly with health issues (monitoring of activities of daily living or health).
Studies that entailed implementation or deployment of technology, even if in a pilot form, or proposed studies, to assess the feasibility and outcomes.
Studies that were published within the last decade, so that the latest researched were included.
The exclusion criteria were:
Studies published as academic theses.
Studies which were reviews, book chapters.
Studies which were not health-related and focused on other aspects such as energy-conservation or security surveillance systems
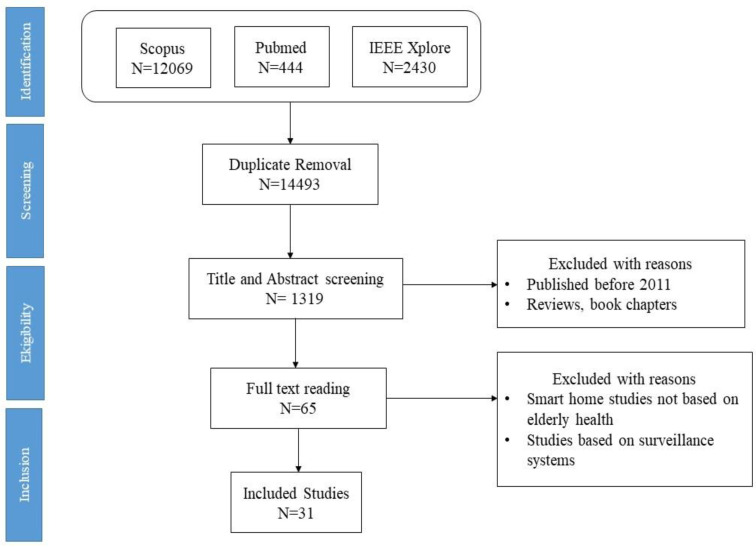
Figure 1, shows the selection strategy using PRISMA flowchart.
Figure 1.
Schematic illustration of the literature search.
3. Results
A total of 1319 studies were identified after title and abstract screening, out of which 65 were accessed for full text reading and as a result 31 were finally included in the review. The features available for smart home systems that were found in the shortlisted studies can broadly categorized into the following categories:
3.1. Application of Environmental Sensors, Wearables and Cameras
Twenty-nine studies [43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71] included in this review entailed the use of various types of sensors; mostly environmental sensors, as the key elements involved in the functioning of a smart home. These studies entailed deployment of entire sensor-based network systems or placement of various sensors all over the home for monitoring the ADL and the overall well-being of subjects.
3.2. Security and Privacy of Data
Eleven studies [43,44,47,49,51,55,58,59,60,65,67] have been more focused in developing smart homes with protection of user privacy being the utmost priority.
3.3. AI Machine Learning and Robots in Smart Homes
Twenty-seven [43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,65,67,72,73] out of the 31 studies used AI, machine learning, or robots in their smart home techniques.
3.4. Usage Safety, Emergency Services and Fall Detection
Four studies [45,60,63,71] out of 31 studies had incorporated some linkage with emergency services. Nine studies [44,45,46,53,58,60,61,66,67] out of 31 studies investigated technologies with in-built fall detection capability
3.5. User Feedback, Satisfaction and Effects of Smart Homes
Eight [43,44,58,60,63,66] of the 31 studies included in this review, the systems deployed were aimed at providing some sort of medical support by health monitoring and taking appropriate action. Fourteen [43,45,47,48,49,51,52,53,55,60,64,65,69,72] of the 31 studies were aimed at monitoring the environment for any abnormalities and detecting falls, which allowed the elderly to stay alone in their homes.
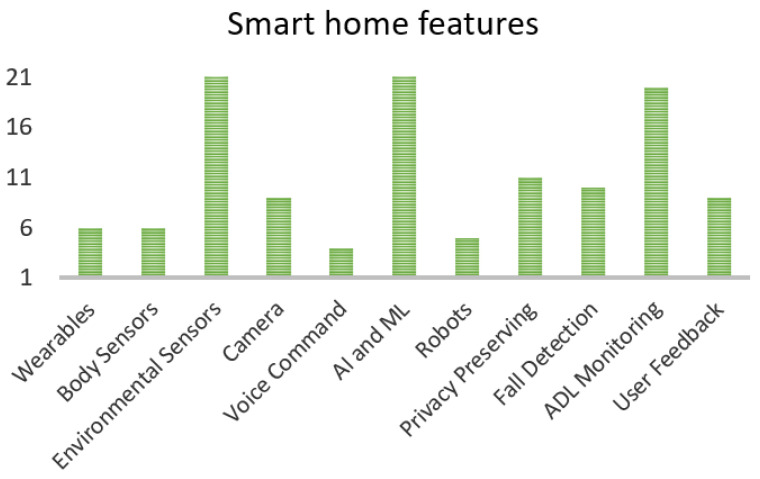
Figure 2 shows the numbers of studies with different features of smart home. This figure enlists in detail features like wearable, body sensors, environmental sensors, cameras, voice command feature, Al or ML capabilities, robots, privacy preservation, fall detection and monitoring of daily activities. Each bar represents the number of studies out of 31 which have included the mentioned feature.
Figure 2.
Smart home features in selected studies.
Table 1 below summarizes the key characteristics of these studies. Table 2 enlists the different features and tools used in the shortlisted studies, such as wearable devices, environmental sensors, cameras, robots, voice commands; in addition, we assessed whether these systems had safeguards to protect user privacy.
Table 1.
Summary of the studies included in the review.
| No. | Reference | Subjects | Method Used | Features | Results |
|---|---|---|---|---|---|
| 1 | Kim et al. 2017 [43] | 20 Elderly with depression |
|
|
|
| 2 | Deen 2015 [44] | Healthy Elderly Sample size: Not mentioned |
|
|
|
| 3 | Sprint et al. 2016 [45] | 3 females aged ≥ 80 years |
|
|
|
| 4 | Wilson et al. 2019 [46] | 26 subjects |
|
|
|
| 5 | Alberdi et al. 2018 [47] | 29 older adults | Unobtrusive collection of behavioral data of elderly living alone in Smart-Homes.
|
|
|
| 6 | Dawadi et al. 2013 [48] | 179 participants |
|
|
|
| 7 | Aramendi et al. 2018 [49] | 29 elderly |
|
|
|
| 8 | Kshirsagar et al. 2020 [50] | Proposed study, No subjects |
|
|
|
| 9 | Yu et al. 2019 [51] | 1 female elderly |
|
|
|
| 10 | Jekel et al. 2016 [52] | 65-80 year old patients with MCI and healthy elderly |
|
|
|
| 11 | Gnanavel et al. 2016 [53] | Proposed system, no subjects |
|
|
|
| 12 | Rizvi et al. 2018 [54] | Proposed system for elderly/blind//handicapped people |
|
|
|
| 13 | Lotfi et al. 2012 [55] | Elderly people with dementia Sample size: Not mentioned |
|
|
|
| 14 | Nisar et al. 2016 [56] | Proposed system, no subjects |
|
|
|
| 15 | Saunders et al. 2016 [57] | T&L component 20 subjects Interaction component 3 subjects |
|
|
|
| 16 | Do et al. 2018 [58] | Graduate students Sample Size: 10 |
|
|
|
| 17 | Bennaser et al. 2019 [59] | Elderly people Sample size: Not mentioned |
|
|
|
| 18 | Taramasco et al. 2019 [60] | Proposed system No subjects |
|
|
|
| 19 | Iakovakis et al. 2016 [61] | 15 Elderly (10 Parkinson’s disease and 5 healthy) |
|
|
|
| 20 | Yu et al. 2015 [62] | 5 Healthy elderly |
|
|
|
| 21 | Tsukiyama 2015 [63] | 1 Healthy elderly |
|
|
|
| 22 | Suryadevara et al. 2013 [64] | Healthy elderly Sample Size not mentioned |
|
|
|
| 23 | Grguric et al. 2019 [65] | Elderly people Sample size: Not mentioned |
|
|
|
| 24 | Yu et al. 2012 [66] | 15 Healthy Elderly |
|
|
|
| 25 | Portet et al. 2013 [67] | Healthy elderly people Sample size: 8 |
|
|
|
| 26 | Hattink et al. 2016 [68] | 42 elderly with MCI or dementia and 32 informal caregivers |
|
|
|
| 27 | Lupiani et al. 2015 [69] | 25 Healthy elderly |
|
|
|
| 28 | Rudzicz et al. 2015 [70] | 10 Elderly with Alzheimer’s disease |
|
|
|
| 29 | Hu et al. 2020 [71] | Proposed system, no subjects |
|
|
|
| 30 | Bianchi et al. 2019 [72] | Proposed system for the elderly |
|
|
|
| 31 | Fischinger et al. 2016 [73] | 49 Healthy elderly |
|
|
|
Table 2.
Features of smart home technology.
| Study | Wearable | Body Sensors | Environmental Sensors | Camera | Voice Command | AI and ML | Robots | Privacy Preserving | Fall Detection | ADL Monitorirng | Feedback Provided by User |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kim et al. 2017 [43] | No | No | Yes | No | No | Yes | No | Yes | No | Yes | No |
| Deen 2015 [44] | Yes | Yes | Yes | No | No | Yes | No | Yes | Yes | Yes | No |
| Sprint et al. 2016 [45] | No | No | Yes | No | No | Yes | No | No | Yes | Yes | No |
| Wilson et al. 2019 [46] | No | No | Yes | Yes | No | Yes | Yes | Not mentioned | Yes | Yes | Yes |
| Alberdi et al. 2018 [47] | No | No | Yes | No | No | Yes | No | Yes | No | Yes | No |
| Dawadi et al. 2013 [48] | No | No | Yes | No | No | Yes | No | Not mentioned | No | Yes | No |
| Aramendi et al. 2018 [49] | No | No | Yes | No | No | Yes | No | Yes | No | Yes | No |
| Kshirsagar et al. 2020 [50] | Yes | Yes | Yes | No | No | Yes | No | Not mentioned | No | No | Yes |
| Yu et al. 2019 [51] | No | No | Yes | No | No | No | No | Yes | No | yes | Yes |
| Jekel et al. 2016 [52] | No | No | Yes | Yes | No | No | No | No | No | Yea | Yes |
| Gnanavel et al. 2016 [53] | No | Yes | Yes | No | No | No | No | Not mentioned | Yes | Yes | No |
| Rizvi et al. 2018 [54] | No | No | Yes | No | No | No | No | No | No | No | No |
| Lotfi et al. 2012 [55] | No | No | Yes | No | No | Yes | No | Yes | No | Yes | No |
| Nisar et al. 2016 [56] | No | No | Yes | No | No | No | No | No | No | Yes | No |
| Saunders et al. 2016 [57] | No | No | Yes | No | Yes | Yes | Yes | Not mentioned | No | No | Yes |
| Do et al. 2018 [58] | Yes | No | Yes | Yes (on robot) | No | Yes | Yes | Yes | Yes | Yes | No |
| Bennaser et al. 2019 [59] | Yes | Yes | Yes | No | No | Yes | No | Yes | No | Yes | No |
| Taramasco et al. 2019 [60] | No | No | Yes | Yes | No | Yes | No | Yes | Yes | No | No |
| Iakovakis et al. 2016 [61] | Yes | Yes | Yes | No | No | Yes | No | Not Mentioned | Yes | Yes | No |
| Yu et al. 2015 [62] | No | No | Yes | No | No | Yes | No | No | No | No | No |
| Tsukiyama 2015 [63] | No | No | Yes | No | No | Yes | No | Not mentioned | No | Yes | No |
| Suryadevara et al. 2013 [64] | No | No | Yes | No | No | No | No | No | No | Yes | No |
| Grguric et al. 2019 [65] | No | No | Yes | No | No | Yes | No | Yes | No | No | Yes |
| Yu et al. 2012 [66] | No | No | No | Yes | No | Yes | No | Not Mentioned | Yes | Yes | No |
| Portet et al. 2013 [67] | No | No | Yes | Yes (video conference) | Yes | No | No | Yes | Yes | Yes | Yes |
| Hattink et al. 2016 [68] | No | No | Yes | Yes | No | No | No | No | No | No | NO |
| Lupiani et al. 2015 [69] | No | No | Yes | No | No | Yes | NO | Not mentioned | No | Yes | No |
| Rudzicz et al. 2015 [70] | No | No | No | Yes (on robot) | Yes | Yes | Yes | Not mentioned | No | No | Yes |
| Rudzicz et al. 2015 [70] | No | No | No | Yes (on robot) | Yes | Yes | Yes | Not mentioned | No | No | Yes |
| Hu et al. 2020 [71] | No | No | Yes | Yes | No | No | No | No | No | no | No |
| Bianchi et al. 2019 [72] | Yes | Yes | No | No | No | Yes | No | Not mentioned | No | No | No |
| Fischinger et al. 2016 [73] | No | No | No | No | Yes | Yes | Yes | Not mentioned | No | No | Yes |
4. Discussion
This systematic review was conducted to showcase the range of currently available smart-home technologies that improve the quality of life of the elderly, while maintaining their privacy and comfort. Thirty-one studies conducted during the period 2010–2020 were included in the review. The topic of smart homes is very broad and can be looked at through many different perspectives: security [74], safety [75], health monitoring [76], social interaction [77], general well-being [43], support for carrying out activities of daily living, timely reminders for certain tasks or intake of medications. This review mainly focused on the aspects of health monitoring and environmental monitoring with use of technology involving the use of sensors, wearables, and robots. In addition, we assessed any potential concerns pertaining to the privacy of users.
4.1. Application of Environmental Sensors, Wearables, and Cameras
The smart-home technologies are now becoming increasingly non-intrusive as more people are becoming aware of the dangers of privacy breach; at the same time, these entail continuous monitoring of the well-being of the user. Most of the technologies are for monitoring the health of elderly people through use of sensor-based platforms, wearable devices, robots, or by simply monitoring the environment to notice any unusual activity or anomaly. These systems generate reports or inform the caregiver in case of any anomaly.
Kim et al. [43] used sensors to monitor the mental health of the subject; these sensors helped detect normal behavior or mild depression with 90% accuracy. Deen [44] used sensing technology to monitor the walking patterns, which helped in early detection of muscle weakness, fall, and improper sleeping patterns. Lotfi et al. [55] employed wireless sensors and a computerized base station to monitor patients with dementia who were living independently. The information from the sensors was transmitted to care givers through a centralized portal and helped predict any anomalies. Do et al. [58] used a system which included home-based robot, sensor network, body-based sensor network, a mobile device, cloud-based servers, and remotely accessible caregivers. Grguric et al. [65] developed a sensor-based system with AI capability to learn the subject’s behavior over time and detect any abnormal behavior. Yu et al. [66] medication adherence in the subjects. Tsukiyama [63] used water-flow sensors, IR-based motion sensors and radio-frequency identification (RFID) receivers to screen the daily activities of an elderly and sense any atypical conditions. The water flow sensors monitored the usage of water during urination, kitchen activities, and self-hygiene to maintain a check on any deviation from a healthy lifestyle.
Environments and platforms using several types of sensors (such as motion sensors, water sensors, light sensors placed at designated spots in various parts of the home) help in carrying out ADL, fall detection, and other activities. The usage of camera and wearables was very limited. In the 31 studies reviewed, only five studies [46,66,67,68,71] entailed the use of a camera. Wilson et al. [46] used to monitor the elderly with their permission. Portet et al. [67] used camera only for social communication between the elderly and their families and friends. Yu et al. [66] used a fall detection system based on computer vision, while. Hattink et al. [68] used camera as a part of their surveillance system to monitor falls and emergencies. Hu et al. [71] used a camera array to detect falls and alert the caregivers.
Wearables do not pose any threat to privacy, however, it is not feasible or practical to constantly wear one. Moreover, wearables typically have a relatively short battery life, require maintenance, and cause discomfort over long usage if required to wear consistently throughout the day., may lead to allergic reactions, rashes [78]. Six studies [44,50,58,59,61,71] out of 31 used wearables in the form of body sensors, smartwatch, and monitors. Kshirsagar et al. [50] proposed a wearable glove-based system, with embedded flexural sensors, microcontrollers and Bluetooth features. The gesture generated signals which controlled various home appliances through a mobile application. Jekel et al. [52] included subjects with MCI along with healthy older adults, they carried out their study by setting up a two-room furnished flat with sensors on the items in the house and the subjects were asked to carry out simple tasks, sensor data was monitored and helped in the prediction of MCI or deteriorating cognitive functions. Hattink et al. [68] developed a system called Rosetta for their MCI and dementia diagnosed subjects. The system consisted of three subsystems, one supported in carrying out all the daily activities, another system recorded the data for analysis, third system detected any anomalies, emergency situation like fall or medical assistance. However, certain challenges have not been addressed. These include use of sensors in the washroom or during bathing, sensors to detect falls, and sensors which can distinguish between the elderly and their pets (animal companions to cater to the loneliness) or visitors and residents.
Rizvi et al. [54] developed an Android-based system, comprising of two modules—a GSM module and a Bluetooth module—which allowed users to control the home devices both remotely and locally through custom designed mobile application. The targeted subjects were elderly and handicapped people. Nisar et al. [56] also developed an android based smart home system where the application had three modules: the sensor module, the controller module and actuator module. Sensor-based devices could be accessed through smartphones both remotely and locally, thus making life efficient for the elderly while also reducing power consumption.
4.2. Security and Privacy of Data
Security and privacy are key concerns when designing a smart home. Users are generally apprehensive about their privacy as well as data security [79]. Proper ethical agreement must be obtained prior to the use of any video or IP cameras for observation purpose to allay these concerns. Since the end devices frequently transmit data to a central controller, simple eavesdropping attacks can lead to data leaks; the types of end devices can expose the identity of the user. Thus, potential attackers can infer when the house is vacant or identify who is present in the house so that they can break in or cause severe situations. However, none of the 31 studies had explicitly mentioned any such data security feature in their technologies.
A trend was discernible in the 31 studies, wherein studies carried out in recent years accorded due attention to make the technology as non-intrusive and privacy-preserving as possible. Security and privacy are major areas of concern as duly pointed out in several studies [80,81,82]. They have used non-intrusive techniques for achieving their target outcome with the help of different kinds of sensors, wearables and robots. We have developed several deep learning models [83,84,85,86,87] based on privacy-preserved activity and posture recognition tasks; however, three [85,86,87] of these studies were for eldercare ADL monitoring, these studies are not included in this review paper as they have employed an open dataset. Also, most of these techniques do not employ cameras in order to make the users more comfortable. Less usage of cameras and wearables is an added advantage.
4.3. AI Machine Learning and Robots In Smart Homes
AI and machine learning are two remarkable innovations that can help in the development of highly advanced and smart strategies. Utilization of AI, machine learning, and fuzzy logic can render the systems more efficient and help them produce more reliable and accurate results. Cutting-edge sensing techniques and machine learning strategies are being used in smart homes to autonomously respond to the needs of their users; however, they are rooted in the environment.
The RiSH [58] comprises a robot for home service, a sensor network deployed across the home, a sensor network for monitoring body activities, a mobile device, cloud-based servers, and remotely available caregivers. The robot embedded in RISH had the capability to recognize 37 distinct individual activities through sound actions and was able to identify falling sounds with 80% accuracy at the frame level. The study demonstrated the ability of RiSH and the home service robot in observing and supporting the resident. Grguric et al. [65] used artificial intelligence theories of decision making, reasoning, and pattern recognition based on the advances in ambient intelligence (AmI), sensor networks, and human-computer interaction (HCI). The system studies a person’s behavior patterns without invading their privacy and signals the caregiver(s) in case of detection of an abnormal situation. Iakovakis et al. [61] used a fuzzy logic-based assistive tool for prevention of falls in patients with Parkinson’s disease. The system gathered important signal information from smartwatch and other home-based motion sensors to monitor the risk of fall due to orthostatic hypotension. Rudzicz et al. [70] investigated the use of a mobile robot designed to assist in ADL of elderly people with Alzheimer’s disease by monitoring visuals and providing verbal prompts in difficult situations. Fischinger et al. [73] used a robot called ‘Hobbit’ that assisted the elderly living independently at home. The robotic system adequately performed its core tasks and the subjects were able to perform all tasks with support of the robot. Wilson et al. [46] developed a robot activity support system (RAS) comprised of a sensing network that interacted with the robot; the system detected activity errors in the everyday environment and provided appropriate assistance. For example, it provided physical assistance by locating the key objects required for ADL in the home. Dawadi et al. [48] developed a network of motion and temperature sensors, which scrutinized the daily activities; a machine learning algorithm processed the collected data to compute the task quality, task accuracy, and task sequencing scores. Bianchi et al. [72] proposed a wearable device integrated with deep learning techniques, which recognized most common daily living activities. Saunder et al. [57] used a commercially available robot for their study. They described the teaching and learning method, where the robot is first taught about all the requirements and logistics of a sensor-based house, and once the robot learns it can assist the subjects in their daily living activities. Due to this methodology the robot can easily be customized to meet individual needs, the subjects found this method to be very easy to use and helpful.
4.4. Usage Safety, Emergency Services and Fall Detection
Ample importance has been accorded to user safety during the development of smart technologies for home, especially those for monitoring the health of elderly patients with dementia, Alzheimer’s, or Parkinson’s disease. These patients are more comfortable in their own homes owing to their familiarity with the environment; use of these smart technologies can inculcate a sense of security and alleviate fear and anxiety. These technologies empower these elderly people to recollect their daily tasks (e.g., taking medicine, drinking water, etc.), make them more self-sufficient, reduce their social isolation, and enhance their sense of self-worth. Some studies investigated the use of systems that periodically send reports to caregivers pertaining to the activities carried out by elderly and also notifies in case of any anomaly; however, very few studies have emergency services embedded into the system.
Taramasco et al. [60] embedded an emergency button which can place a call to the caregivers and is also connected to emergency and fire-fighting departments. Tsukiyama [63] deployed a system that assesses the health condition of the elderly and forecasts any emergency situation to a local healthcare center without any explicit user interaction. Fischinger et al. [73] employed a robot which can detect emergency and handle the situation appropriately. Fall detection technology is an essential element of any smart home technology for elderly. Elderly people are more vulnerable to falls due to age-related conditions such as muscle weakness, arthritis, and muscle atrophy. Falls may lead to severe injuries that necessitate medical help.
Deen et al. [44] employed a system which can detect health issues, muscle weakness, and fall through a smart walking monitor and smart joint monitor. Portet et al. [68] used a system with the ability to detect fall and help subjects in calling for help. Do et al. [58] used a robot which was able to detect fall sounds with 80% accuracy. Taramasco et al. [60] incorporated special falling sensors in its tele monitoring ADL platform to detect falls. Iakovakis et al. [61] used a fuzzy logic based assistive tool for fall prevention. Yu et al. [66] used a computer vision-based fall detection system for monitoring an elderly person in home care. Fischinger et al. [73] used a care robot which was able to prevent and detect falls. Gnanavel et al. [53] also include a fall detection system, including a heartbeat sensor, pressure sensor and temperature sensor and alerted the caregivers via SMS in case of any anomaly. Hattink et al. [68] had a surveillance system, which was able to detect inactivity, and was able to predict and alert the caregivers of an emergency situation. Hu et al. [71] was a camera P2P based system which detected falls and alerted the caregivers.
4.5. User Feedback, Satisfaction and Effects of Smart Homes
The response of the people towards usage of these smart-systems also seems affirmative [50,51,52,57,71,72]. A study [62] showed improved medication adherence among subjects with use of used water sensors to monitor the usage of water to check maintenance of a healthy lifestyle. However, the positive effects cannot be generalized as these studies were performed with small sample sizes of less than 50; moreover, proxy subjects were used in some cases [58].
A trend observed in the 31 studies was that the deployed smart systems were able to achieve their targeted outcome; moreover, the users rated the systems as sensors to track the medicine intake. Others studied usability [65] and acceptability [88]. However, each of the studies had some limitations and none of the studies replicated a model of a complete smart home. The study by Do et al. [58] used a system that is closest to a complete smart home solution; it includes a home service robot, a home sensor network, a body sensor network, a mobile device, cloud servers, and remote caregivers. The system monitors the ADL, informs the caregivers in case of any anomaly, has a robot at hand to assist in ADL with the ability to recognize 37 daily activities and detect falls. The only limitation was that their technology required the use of a wearable device; as discussed above, wearables are not very comfortable for constant daily use. In addition, there was no fall detection technology used in the bathroom, which is a very high-risk area for falls.
4.5.1. Statistical Analysis
If we observe quantitatively 80% of the studies used some form of sensor embedded in their systems, be they environmental sensors, body sensors, motions sensors, etc. These sensors are the crux of a smart home system as they can monitor and record every move, without hampering inhabitants’ daily life, invading their privacy, and also through these sensors, the daily activities can be made efficient and easy to be carried out by subjects with minimum effort. Nearly a fifth (19.3%) of studies used wearables, it was seen that incorporation of wearables in the studies has decreased with time, in recent years, studies are now more focused on sensors and robots to enable a good functional smart home for elderly. Over a third (35.4%) of studies declared usage unobtrusive or privacy-preserving techniques in their methodology, few didn’t mention privacy or their unobtrusiveness, even though this is a very low percentage considering this is an important feature, more focus needs to be put in to include privacy and security feature of a smart home, as with advancing technology, there are new ways to breach security and theft of data can be dangerous. Moreover, it puts the subject at ease if they know that the system is secure and protected and their personal data is safe. Nearly 90% (87.09%) of studies have incorporated AI, ML or robots in their smart home research, as these strategies are proving to be more efficient and beneficial, though they are still in their infancy, more research should be put in to incorporate more features and make it more easy to use for the elderly
The studies were reviewed were RCTs, pilot studies, experimental studies and also proposed studies. Nearly a fifth (19.3%) were proposed studies, which catered to different subjects like MCI, handicapped and dementia patients or healthy elderly. These studies show a great potential in their research but needs to be validated by including subjects and conducting trials to verify their claim. Few studies open a new window in regard to care of MCI and dementia diagnosed elderly via a smart home strategy. These studies have potential to benefit them immensely in their daily activities, help them live independently, while keeping the caregiver at ease, with emergency and fall detection alert techniques.
To summarize the main features of the smart home technology in the included literature: 80% of the smart home systems reviewed used sensor-based platforms, 29.1% used cameras, 19.3% used wearables, 35.4% used unobtrusive methods, 16.1% used robots, 70.9% used AI and machine learning and 32.2% had fall detection capabilities.
4.5.2. Recommendations for Future Research
There is an inevitable compromise between utility and feasibility. Multiple hardwired installation may be needed at all positions where support could be required (e.g., bathroom, kitchen, and bedroom), which may not be very cost effective. Conversely, installation of too few units may introduce gaps where activity will not be noticed. Integration of robots with smart homes can help with some of these tradeoffs. Moreover, a physically embodied entity like a robot will have greater chances of acceptance than an embedded system [88,89].
Also, robots along with the sensor technology could be a better strategy, as robots can be programmed to assist in ADL (bringing the medicine, reminding of tasks, keeping company, aiding in physical needs like sitting as standing [90], calling the caregivers, etc.), while sensors can be used to monitor the environment. Moreover, there are other determinants of QoL apart from health. Most of the studies employed systems aimed at providing some sort of healthcare.
Satisfaction with and acceptability of any smart home systems is culture-dependent and thus varies in different societies. Age and gender seem to influence people’s idea of space [88], which can also affect the acceptability of a system, in particular where behavior is continuously monitored. Identification of the level of user acceptance is a major challenge for system developers [91].
However, as seen the technology readiness for these systems was rated as low. These systems need to incorporate more mechanisms to protect user privacy and data security in order to gain the trust of their users. Apart from monitoring the health status, these systems should incorporate means of entertainment and companionship to ward off loneliness and anxiety. None of the 31 included studies can be considered a complete smart home system, which is unobtrusive, monitors health, has emergency features, helps in ADL together with keeping them motivated and less lonely and less anxious. These measures would provide a happy and positive place to age in place. In addition, more robust safety features should be incorporated in such technologies to achieve a complete smart home solution. Inclusion of entertainment and gaming [91], social companionship [92], and constant support and assurance can help improve the usability and acceptability of the systems, especially among the elderly, especially for those who live independently, as they will be able to keep themselves busy through these features and not feel depressed.
There is a paucity of research on this aspect. None of the 31 studies reviewed had incorporated entertainment as an add-on option in their system, although one study [72] did have the option of video conferencing with friends and family members. Four studies [48,59,71,72] included robots which could provide some sense of companionship to the user. Future research should focus on these aspects along with monitoring the activities and providing healthcare linkage.
To summarize the main features of the smart home technology, out of 31 chosen literature references 27 used environmental sensors, 22 studies used AI or ML techniques in their strategies, 20 systems could monitor activities of daily living, 11 systems used privacy-preserving methods, 10 used fall detection techniques, 9 studies collected feedback from the user, 9 used cameras in their systems, 6 used wearables, 6 used body sensors, 5 involved robot-based methods and 4 used voice commands. Figure 2 depicts this f information in the form of bar graph.
To conclude, a complete smart home should include a strategically designed sensor-based platform which can function with multiple residents in the house; in addition, non-intrusive fall detection sensors should be installed in washrooms. Emergency buttons should be easily accessible to provide ready access to emergency services. Use of cameras and wearables should be minimized. Integration of robot with the system can assist in ADL, provide medication reminders, and inculcate a sense of companionship [83] to alleviate depression and anxiety. Data security and privacy should be accorded highest priority in the development of smart home solutions.
5. Conclusions
Use of smart-home technology for improving the QoL of older adults has received a generally positive response. The studies included in this review for the most part achieved their target outcomes. However, 50% of the studies pertained to monitoring the ADLs of the subjects and informing their caregivers in case of any abnormalities or discrepancies; the other studies deployed systems to achieve very specific tasks such as checking the medication adherence, monitoring the water flow, and analyzing the walking and sleep patterns.
While most of the studies achieved their objectives, none of the studies can claim to have achieved the objective of implementing a complete smart home. Future studies should incorporate all the key features required in a smart home: individual privacy, monitoring via sensor-based technology, assistance in daily activities via a home robot, provision for connecting to caregivers, access to emergency assistance, and predicting depression.
Abbreviations
| SVM | Support Vector Machine |
| RiSH | A robot-integrated smart home |
| STRETCH | Socio-Technical Resilience for Enhancing Targeted Community Healthcare |
| ADL | Activities of Daily Living |
| LSTM | Long-Short Term Memory |
| GRU | Gated Recurrent Units |
| BLSTM | Bidirectional Long Short-Term Memory |
| CASAS-AR | Center for Advanced Studies in Adaptive Systems-Activity Recognition |
| ML | Machine Learning |
| GSM | Global System for Mobile Communications |
| HMM | Hidden Markov Model |
| MQTT | Message Queuing Telemetry Transport |
Author Contributions
Conceptualization, M.G., F.A., and S.K.; methodology, M.G. and S.K.; resources, F.A., S.K.; writing—original draft preparation, M.G. and S.K.; writing—review and editing F.A., M.G. and T.-H.T., supervision, T.-H.T.; funding acquisition, M.G. All authors have read and agreed to the published version of the manuscript.
Funding
This study is supported by the research grant (No. 31T136) which was funded by the College of Information Technology, United Arab Emirates University (UAEU).
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Not Applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations . World Population Ageing 2019. United Nations; New York, NY, USA: 2019. [Google Scholar]
- 2.McColl D., Louie W.Y.G., Nejat G. Brian 2.1: A Socially assistive robot for the elderly and cognitively impaired. IEEE Robot. Autom. Mag. 2013 doi: 10.1109/MRA.2012.2229939. [DOI] [Google Scholar]
- 3.Grimby G. Physical Activity and Muscle Training in the Elderly. Acta Med. Scand. 1986;711:233–237. doi: 10.1111/j.0954-6820.1986.tb08956.x. [DOI] [PubMed] [Google Scholar]
- 4.Alnajjar F., Khalid S., Vogan A.A., Shimoda S., Nouchi R., Kawashima R. Emerging Cognitive Intervention Technologies to Meet the Needs of an Aging Population: A Systematic Review. Front. Aging Neurosci. 2019 doi: 10.3389/fnagi.2019.00291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cole M.G., Dendukuri N. Risk factors for depression among elderly community subjects: A systematic review and meta-analysis. Am. J. Psychiatry. 2003;160:1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 6.Mainetti L., Patrono L., Rametta P. Capturing Behavioral Changes of Elderly People through UNOBTRUISIVE Sensing Technologies; Proceedings of the 24th International Conference on Software, Telecommunications and Computer Networks (SoftCOM); Split, Croatia. 22–24 September 2016; pp. 1–3. [DOI] [Google Scholar]
- 7.Yorkston K.M., Bourgeois M.S., Baylor C.R. Communication and Aging. Phys. Med. Rehabil. Clin. 2011;21:309–319. doi: 10.1016/j.pmr.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mattimore T.J., Wenger N.S., Desbiens N.A., Teno J.M., Hamel M.B., Liu H., Califf R., Connors A.F., Lynn J., Oye R.K. Surrogate and physician understanding of patients’ preferences for living permanently in a nursing home. J. Am. Geriatr. Soc. 1997;45:818–824. doi: 10.1111/j.1532-5415.1997.tb01508.x. [DOI] [PubMed] [Google Scholar]
- 9.Bemelmans R., Jan G., Jonker P., de Witte L. Socially Assistive Robots in Elderly Care: A Systematic Review into Effects and Effectiveness. JMDA. 2020;13:114–120.e1. doi: 10.1016/j.jamda.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Majumder S., Aghayi E., Noferesti M., Memarzadeh-Tehran H., Mondal T., Pang Z., Deen M.J. Smart homes for elderly healthcare—Recent advances and research challenges. Sensors. 2017;17:2496. doi: 10.3390/s17112496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cook D.J. Health monitoring and assistance to support aging in place. J. Univers. Comput. Sci. 2006;12:15–19. [Google Scholar]
- 12.The Benefits of Remote Patient Monitoring Technologies. [(accessed on 21 April 2021)]; Available online: https://www.itij.com/latest/long-read/benefits-remote-patient-monitoring-technologies.
- 13.Pal D., Triyason T., Funikul S. Smart Homes and Quality of Life for the Elderly: A Systematic Review; Proceedings of the 2017 IEEE International Symposium on Multimedia (ISM); Taichung, Taiwan. 11–13 December 2017; pp. 413–419. [Google Scholar]
- 14.World Health Organization . WHOQOL Measuring Quality of Life. Division of Mental Health and Prevention of Substance Abuse of the WHO; Geneva, Switzerland: 1997. [Google Scholar]
- 15.Guo X., Shen Z., Zhang Y., Wu T. Review on the Application of Artificial Intelligence in Smart Homes. Smart Cities. 2019;2:402–420. doi: 10.3390/smartcities2030025. [DOI] [Google Scholar]
- 16.Giffinger R., Fertner C., Kramar H., Kalasek R., Pichler N., Meijers E. Smart Cities-Ranking of European Medium-Sized Cities, Centre of Regional Science. [(accessed on 21 April 2021)];2007 Available online: http://www.smart-cities.eu/download/smart_cities_final_report.pdf.
- 17.Guillemin P., Friess P. The Cluster of European Research Projects. River Publishers; Aalborg, Denmark: 2009. Internet of things strategic research roadmap. In Tech. Report. [Google Scholar]
- 18.Kochovski P., Gec S., Stankovski V., Bajec M., Drobintsev P.D. Trust management in a blockchain based fog computing platform with trustless smart oracles. Futur. Gener. Comput. Syst. 2019;101:747–759. doi: 10.1016/j.future.2019.07.030. [DOI] [Google Scholar]
- 19.Lou W., Ren K. Security, Privacy, And Accountability in Wireless Access Networks. IEEE Wirel. Commun. 2009;16:80–87. doi: 10.1109/MWC.2009.5281259. [DOI] [Google Scholar]
- 20.Bertino E. Data Privacy for IoT Systems; Proceedings of the 2016 IEEE International Conference on Big Data (Big Data); Washington, DC, USA. 5–8 December 2016; pp. 3645–3647. [Google Scholar]
- 21.Ou L., Yin H., Qin Z., Xiao S., Yang G., Hu Y. An Efficient and Privacy-Preserving Multiuser Cloud-Based LBS Query Scheme. Cyberspace Secur. Future Internet. 2018;2018 doi: 10.1155/2018/4724815. [DOI] [Google Scholar]
- 22.Chakravorty A., Wlodarczyk T., Rong C. Privacy preserving data analytics for smart homes; Proceedings of the 2013 IEEE Security and Privacy Workshops; San Francisco, CA, USA. 23–24 May 2013; pp. 23–27. [Google Scholar]
- 23.Marikyan D., Papagiannidis S., Alamanos E. A systematic review of the smart home literature: A user perspective. Technol. Forecast. Soc. Change. 2018;138:139–154. doi: 10.1016/j.techfore.2018.08.015. [DOI] [Google Scholar]
- 24.Balta-Ozkan N., Amerighi O., Boteler B. Technology Analysis & Strategic Management A comparison of consumer perceptions towards smart homes in the UK, Germany and Italy: Reflections for policy and future research. Technol. Anal. Strateg. Manag. 2014;26:37–41. [Google Scholar]
- 25.Mazorra M.L., Oliveira M., Souza A., Silva W.B., dos Santos G.M., da Silva L.R.A., da Silva M.G., Bartoli C.G., de Oliveira J.G. Involvement of brassinosteroids and ethylene in the control of mitochondrial electron transport chain in postharvest papaya fruit. Theor. Exp. Plant Physiol. 2013;25:203–212. doi: 10.1590/S2197-00252013005000003. [DOI] [Google Scholar]
- 26.Hong D., Shin J., Lee J. Strategic management of next-generation connected life: Focusing on smart key and car–home connectivity. Technol. Forecast. Soc. Chang. 2016;103:11–20. doi: 10.1016/j.techfore.2015.10.006. [DOI] [Google Scholar]
- 27.Sepasgozar S., Hawken S., Sargolzaei S., Foroozanfa M. Implementing citizen centric technology in developing smart cities: A model for predicting the acceptance of urban technologies. Technol. Forecast. Soc. Chang. 2019;142:105–116. doi: 10.1016/j.techfore.2018.09.012. [DOI] [Google Scholar]
- 28.Silverio-Fernández M., Renukappa S., Suresh S. What is a smart device?—A conceptualisation within the paradigm of the internet of things. Vis. Eng. 2018 doi: 10.1186/s40327-018-0063-8. [DOI] [Google Scholar]
- 29.Ransing R.S., Rajput M. Smart home for elderly care, based on wireless sensor network; Proceedings of the 2015 International Conference on Nascent Technologies in the Engineering Field (ICNTE); Navi Mumbai, India. 9–10 January 2015. [Google Scholar]
- 30.Byun J., Jeon B., Noh J., Kim Y., Park S. An Intelligent Self-Adjusting Sensor for Smart Home Services based on ZigBee Communications. IEEE Trans. Consum. Electron. 2012;58:794–802. doi: 10.1109/TCE.2012.6311320. [DOI] [Google Scholar]
- 31.Ghayvat H., Liu J., Mukhopadhyay S.C., Gui X. Wellness Sensor Networks: A Proposal and Implementation for Smart Home for Assisted Living. IEEE Sens. J. 2015 doi: 10.1109/JSEN.2015.2475626. [DOI] [Google Scholar]
- 32.Zimmermann L., Member S., Weigel R., Fischer G. Fusion of Non-Intrusive Environmental Sensors for Occupancy Detection in Smart Homes. IEEE Internet Things J. 2017 doi: 10.1109/JIOT.2017.2752134. [DOI] [Google Scholar]
- 33.Hu C.-L., Bamrung C., Kamintra W., Ruengittinun S., Mongkolwat P., Hui L., Lo S.-H. Proceedings of the 2019 8th International Conference on Innovation, Communication and Engineering (ICICE), Zhengzhou, China, 25–30 October 2019. IEEE; Piscataway, NJ, USA: 2020. Using Camera Array to Detect Elderly Falling and Distribute Alerting Media for Smart Home Care; pp. 98–101. [Google Scholar]
- 34.Gregory A., Mackintosh S., Kumar S., Grech C. Experiences of health care for older people who need support to live at home: A systematic review of the qualitative literature. Geriatr. Nurs. 2017 doi: 10.1016/j.gerinurse.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 35.Karlsen C., Ludvigsen M.S., Moe C.E., Haraldstad K., Thygesen E. Experiences of community-dwelling older adults with the use of telecare in home care services: A qualitative systematic review. JBI Database Syst. Rev. Implement. Rep. 2017 doi: 10.11124/JBISRIR-2017-003345. [DOI] [PubMed] [Google Scholar]
- 36.Graybill E.M., McMeekin P., Wildman J. Can aging in place be cost effective? A systematic review. PLoS ONE. 2014;9:e102705. doi: 10.1371/journal.pone.0102705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peek S.T.M., Wouters E.J.M., van Hoof J., Luijkx K.G., Boeije H.R., Vrijhoef H.J.M. Factors influencing acceptance of technology for aging in place: A systematic review. Int. J. Med. Inform. 2014;83:235–248. doi: 10.1016/j.ijmedinf.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 38.Rosenwohl-Mack A., Schumacher K., Fang M.L., Fukuoka Y. Experiences of aging in place in the United States: Protocol for a systematic review and meta-ethnography of qualitative studies 11 Medical and Health Sciences 1117 Public Health and Health Services. Syst. Rev. 2018;7:1–7. doi: 10.1186/s13643-018-0820-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Golant S.M. Commentary: Irrational exuberance for the aging in place of vulnerable low-income older homeowners. J. Aging Soc. Policy. 2008 doi: 10.1080/08959420802131437. [DOI] [PubMed] [Google Scholar]
- 40.Rho S., Min G., Chen W. Engineering Applications of Artificial Intelligence Advanced issues in artificial intelligence and pattern recognition for intelligent surveillance system in smart home environment. Eng. Appl. Artif. Intell. 2012;25:1299–1300. doi: 10.1016/j.engappai.2012.07.007. [DOI] [Google Scholar]
- 41.Dermody G., Fritz R. A conceptual framework for clinicians working with artificial intelligence and health-assistive Smart Homes. Nurs. Inq. 2019;26:1–8. doi: 10.1111/nin.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kumar S., Qadeer M.A. Application of AI in Home Automation. IACSIT Int. J. Eng. Technol. 2012;4:4–8. doi: 10.7763/IJET.2012.V4.488. [DOI] [Google Scholar]
- 43.Kim J.Y., Liu N., Tan H.X., Chu C.H. Unobtrusive Monitoring to Detect Depression for Elderly with Chronic Illnesses. IEEE Sens. J. 2017;17:5694–5704. doi: 10.1109/JSEN.2017.2729594. [DOI] [Google Scholar]
- 44.Deen M.J. Information and communications technologies for elderly ubiquitous healthcare in a smart home. Pers. Ubiquitous Comput. 2015;19:573–599. doi: 10.1007/s00779-015-0856-x. [DOI] [Google Scholar]
- 45.Sprint G., Cook D.J., Fritz R., Schmitter-Edgecombe M. Using Smart Homes to Detect and Analyze Health Events. Computer. 2016;49:29–37. doi: 10.1109/MC.2016.338. [DOI] [Google Scholar]
- 46.Wilson G., Pereyda C., Raghunath N., de la Cruz G.V., Goel S., Nesaei S., Minor B., Schmitter-Edgecombe M., Taylor M.E., Cook D.J. Robot-enabled support of daily activities in smart home environments. Cogn. Syst. Res. 2019;54:258–272. doi: 10.1016/j.cogsys.2018.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alberdi A., Weakley A., Schmitter-Edgecombe M., Cook D.J., Goenaga A.A., Basarab A., Barrenechea Carrasco M. Smart Homes Predicting the Multi-Domain Symptoms of Alzheimer’s Disease. IEEE J. Biomed. Health Inform. 2018:1–8. doi: 10.1109/JBHI.2018.2798062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dawadi P.N., Member S., Cook D.J., Fellow I., Schmitter-Edgecombe M. Smart Home Monitoring of Complex Tasks. IEEE Trans Syst. Man Cybern. Part C Appl. Rev. 2013;43:1302–1313. doi: 10.1109/TSMC.2013.2252338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Aramendi A.A., Weakley A., Goenaga A.A., Schmitter-Edgecombe M., Cook D.J. Automatic assessment of functional health decline in older adults based on smart home data. J. Biomed. Inform. 2018;81:119–130. doi: 10.1016/j.jbi.2018.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kshirsagar S., Sachdev S., Singh N., Tiwari A., Sahu S. IoT Enabled Gesture-Controlled Home Automation for Disabled and Elderly; Proceedings of the 2020 4th International Conference on Computing Methodologies and Communication (ICCMC); Erode, India. 11–13 March 2020; pp. 821–826. [Google Scholar]
- 51.Yu J., An N., Hassan T., Kong Q. A Pilot Study on a Smart Home for Elders Based on Continuous In-Home Unobtrusive Monitoring Technology. Health Environ. Res. Des. J. 2019;12:206–219. doi: 10.1177/1937586719826059. [DOI] [PubMed] [Google Scholar]
- 52.Jekel K., Damian M., Storf H., Hausner L., Frölich L. Development of a Proxy-Free Objective Assessment Tool of Instrumental Activities of Daily Living in Mild Cognitive Impairment Using Smart Home Technologies. J. Alzheimer’s Dis. 2016;52:509–517. doi: 10.3233/JAD-151054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gnanavel R., Anjana P., Nappinnai K.S., Sahari N.P. Smart home system using a Wireless Sensor Network for elderly care; Proceedings of the 2016 2nd International Conference on Science Technology Engineering and Management (ICONSTEM); Chennai, India. 30–31 March 2016; pp. 51–55. [Google Scholar]
- 54.Rizvi S., Sohail I., Saleem M.M., Irtaza A., Zafar M., Syed M. A Smart Home Appliances Power Management System for Handicapped, Elder and Blind People; Proceedings of the 2018 4th International Conference on Computer and Information Sciences (ICCOINS); Kuala Lumpur, Malaysia. 13–14 August 2018; pp. 2018–2021. [Google Scholar]
- 55.Lotfi A., Langensiepen C., Mahmoud S.M., Akhlaghinia M.J. Smart homes for the elderly dementia sufferers: Identification and prediction of abnormal behaviour. J. Ambient Intell. Humaniz. Comput. 2012;3:205–218. doi: 10.1007/s12652-010-0043-x. [DOI] [Google Scholar]
- 56.Nisar K., Ibrahim A.A.A., Wu L., Adamov A., Deen M.J. Smart home for elderly living using Wireless Sensor Networks and an Android application; Proceedings of the 2016 IEEE 10th International Conference on Application of Information and Communication Technologies (AICT); Baku, Azerbaijan. 12–14 October 2016. [Google Scholar]
- 57.Saunders J., Syrdal D.S., Koay K.L., Burke N., Dautenhahn K. Teach Me-Show Me’-End-User Personalization of a Smart Home and Companion Robot. IEEE Trans. Hum. Mach. Syst. 2016;46:27–40. doi: 10.1109/THMS.2015.2445105. [DOI] [Google Scholar]
- 58.Do H.M., Pham M., Sheng W., Yang D., Liu M. RiSH: A robot-integrated smart home for elderly care. Rob. Auton. Syst. 2018;101:74–92. doi: 10.1016/j.robot.2017.12.008. [DOI] [Google Scholar]
- 59.Bennasar M., McCormick C., Price B., Gooch B., Stuart A., Mehta V., Clare L., Bennaceur A., Cohen J., Bandara A., et al. A Sensor Platform for Non-invasive Remote Monitoring of Older Adults in Real Time. Innov. Med. Healthc. Syst. Multimed. 2019:125–135. doi: 10.1007/978-981-13-8566-7_12. [DOI] [Google Scholar]
- 60.Taramasco C., Espinoza C., Riquelme F. Telemonitoring ADL Platform Based on Non-Intrusive and Privacy-friendly Sensors for the Care of the Elderly in Smart Homes. [(accessed on 21 April 2021)];Journées d’Etudesur sur la TéléSanté. 2019 Available online: https://hal.archives-ouvertes.fr/hal-02161094.
- 61.Iakovakis D.E., Papadopoulou F.A., Hadjileontiadis L.J. Fuzzy logic-based risk of fall estimation using smartwatch data as a means to form an assistive feedback mechanism in everyday living activities. Healthc. Technol. Lett. 2016 doi: 10.1049/htl.2016.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yu Z., Liang Y., Guo B., Zhou X., Ni H. Facilitating medication adherence in elderly care using ubiquitous sensors and mobile social networks. Comput. Commun. 2015 doi: 10.1016/j.comcom.2015.04.001. [DOI] [Google Scholar]
- 63.Tsukiyama T. In-home health monitoring system for solitary elderly. Procedia Comput. Sci. 2015 doi: 10.1016/j.procs.2015.08.338. [DOI] [Google Scholar]
- 64.Suryadevara N.K., Mukhopadhyay S.C., Wang R., Rayudu R.K. Forecasting the behavior of an elderly using wireless sensors data in a smart home. Eng. Appl. Artif. Intell. 2013;26:2641–2652. doi: 10.1016/j.engappai.2013.08.004. [DOI] [Google Scholar]
- 65.Grgurić A., Mošmondor M., Huljenić D. The smarthabits: An intelligent privacy-aware home care assistance system. Sensors. 2019;19:907. doi: 10.3390/s19040907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yu M., Rhuma A., Naqvi S.M., Wang L., Chambers J. A posture recognition-based fall detection system for monitoring an elderly person in a smart home environment. IEEE Trans. Inf. Technol. Biomed. 2012 doi: 10.1109/TITB.2012.2214786. [DOI] [PubMed] [Google Scholar]
- 67.Portet F., Vacher M., Golanski C., Roux C., Meillon B. Design and evaluation of a smart home voice interface for the elderly: Acceptability and objection aspects. Pers. Ubiquitous Comput. 2013;17:127–144. doi: 10.1007/s00779-011-0470-5. [DOI] [Google Scholar]
- 68.Hattink B.J.J., Meiland F.J.M., Overmars-Marx T., de Boer M., Ebben P.W.G., van Blanken M., Verhaeghe S., Stalpers-Croeze I., Jedlitschka A., Flick S.E., et al. The electronic, personalizable Rosetta system for dementia care: Exploring the user-friendliness, usefulness and impact. Disabil. Rehabil. Assist. Technol. 2016;11:61–71. doi: 10.3109/17483107.2014.932022. [DOI] [PubMed] [Google Scholar]
- 69.Lupiani E., Juarez J.M., Palma J., Marin R. Monitoring elderly people at home with temporal Case-Based Reasoning. Knowl. Based Syst. 2017;134:116–134. doi: 10.1016/j.knosys.2017.07.025. [DOI] [Google Scholar]
- 70.Rudzicz F., Wang R., Begum M., Mihailidis A. Speech interaction with personal assistive robots supporting aging at home for individuals with Alzheimer’s disease. ACM Trans. Access. Comput. 2015 doi: 10.1145/2744206. [DOI] [Google Scholar]
- 71.Hu R., Kabouteh A., Pawlitza K., Güttler J., Linner T., Bock T. Developing personalized intelligent interior units to promote activity and customized healthcare for aging society; Proceedings of the 36th International Symposium on Automation and Robotics in Construction (ISARC 2019); Banff, AB, Canada. 21–24 May 2019; pp. 234–241. [Google Scholar]
- 72.Bianchi V., Bassoli M., Lombardo G., Fornacciari P., Mordonini M., de Munari I. IoT Wearable Sensor and Deep Learning: An Integrated Approach for Personalized Human Activity Recognition in a Smart Home Environment. IEEE Internet Things J. 2019;6:8553–8562. doi: 10.1109/JIOT.2019.2920283. [DOI] [Google Scholar]
- 73.Fischinger D., Einramhof P., Papoutsakis K., Wohlkinger W., Mayer P., Panek P., Hofmann S., Körtner T., Weiss A., Argyros A.A., et al. Hobbit, a care robot supporting independent living at home: First prototype and lessons learned. Rob. Auton. Syst. 2016 doi: 10.1016/j.robot.2014.09.029. [DOI] [Google Scholar]
- 74.Jose A.C., Malekian R. Smart Home Automation Security: A Literature Review. Smart Comput. Rev. :2015. doi: 10.6029/smartcr.2015.04.004. [DOI] [Google Scholar]
- 75.Kim S., Jeong Y., Park S.O. RFID-based indoor location tracking to ensure the safety of the elderly in smart home environments. Pers. Ubiquitous Comput. 2012;17:1699–1707. doi: 10.1007/s00779-012-0604-4. [DOI] [Google Scholar]
- 76.Chatrati S.P., Hossain G., Goyal A., Bhan A., Bhattacharya S., Gaurav D., Tiwari S.M. Smart home health monitoring system for predicting type 2 diabetes and hypertension. J. King Saud Univ. Comput. Inf. Sci. 2020 doi: 10.1016/j.jksuci.2020.01.010. [DOI] [Google Scholar]
- 77.Lee J.K.B., Kwon O., Lee I. Companionship with smart home devices: The impact of social connectedness and interaction types on perceived social support and companionship in smart homes. Comput. Human Behav. 2017;75:922–934. doi: 10.1016/j.chb.2017.06.031. [DOI] [Google Scholar]
- 78.The Health Impacts of Wearable Technology. [(accessed on 21 April 2021)]; Available online: https://wp.nyu.edu/dispatch/2018/12/17/the-health-impacts-of-wearable-technology.
- 79.Here Are Five Reasons Consumers Won’t Buy Your Smart Home Device. [(accessed on 21 April 2021)]; Available online: https://www.hkstrategies.com/en/here-are-five-reasons-consumers-wont-buy-your-smart-home-device/
- 80.Klemmer S.R., Hartmann B., Takayama L. How bodies matter: Five themes for interaction design; Proceedings of the Conference on Designing Interactive Systems: Processes, Practices, Methods, and Techniques, DIS; University Park, PA, USA. 26–28 June 2006. [Google Scholar]
- 81.Demiris G., Hensel B.K., Skubic M., Rantz M. Senior residents’ perceived need of and preferences for ‘smart home’ sensor technologies. Int. J. Technol. Assess. Health Care. 2008;24:120–124. doi: 10.1017/S0266462307080154. [DOI] [PubMed] [Google Scholar]
- 82.Van Hoof J., Kort H.S.M., Rutten P.G.S., Duijnstee M.S.H. Ageing-in-place with the use of ambient intelligence technology: Perspectives of older users. Int. J. Med. Inform. 2011;80:310–331. doi: 10.1016/j.ijmedinf.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 83.Gochoo M., Tan T.-H., Huang S.-C., Alnajjar F., Yung-Fu C., Tsedevdorj B. Novel IoT-Based Privacy-Preserving Yoga Posture Recognition System Using Low-Resolution Infrared Sensors and Deep Learning. IEEE Internet Things J. 2019;6:7192–7200. doi: 10.1109/JIOT.2019.2915095. [DOI] [Google Scholar]
- 84.Gochoo M., Tan T.H., Alnajjar F., Hsieh J.W., Chen P.Y. Lownet: Privacy Preserved Ultra-Low Resolution Posture Image Classification; Proceedings of the 2020 IEEE International Conference on Image Processing (ICIP); Abu Dhabi, UAE. 25–28 October 2020; pp. 663–667. [Google Scholar]
- 85.Gochoo M., Tan T.-H., Liu S.-H., Jean F.-R., Alnajjar F., Huang S.-C. Unobtrusive Activity Recognition of Elderly People Living Alone Using Anonymous Binary Sensors and DCNN. IEEE J. Biomed. Health Inform. 2018 doi: 10.1109/JBHI.2018.2833618. [DOI] [PubMed] [Google Scholar]
- 86.Tan T.H., Gochoo M., Huang S.C., Liu Y.H., Liu S.H., Huang Y.F. Multi-resident activity recognition in a smart home using RGB activity image and DCNN. IEEE Sens. J. 2018;18:9718–9727. doi: 10.1109/JSEN.2018.2866806. [DOI] [Google Scholar]
- 87.Gochoo M., Tan T.H., Velusamy V., Liu S.H., Bayanduuren D., Huang S.C. Device-free non-privacy invasive classification of elderly travel patterns in a smart house using PIR sensors and DCNN. IEEE Sens. J. 2017;18:390–400. doi: 10.1109/JSEN.2017.2771287. [DOI] [Google Scholar]
- 88.Mourshed M., Zhao Y. Healthcare providers’ perception of design factors related to physical environments in hospitals. J. Environ. Psychol. 2012;32:362–370. doi: 10.1016/j.jenvp.2012.06.004. [DOI] [Google Scholar]
- 89.Alsinglawi B., Alnajjar F., Mubin O., Novoa M. A Framework for Home-Based Stroke Rehabilitation Using Interactive Games and Augmented Reality Feedback. Biosyst. Biorobot. 2018:252–255. doi: 10.1007/978-3-030-01845-0_50. [DOI] [Google Scholar]
- 90.Yang N., An Q., Yamakawa H., Tamura Y., Yamashita A., Takahashi K., Kinomoto M., Yamasaki H., Itkonen M., Alnaj-jar F.S., et al. Clarification of muscle synergy structure during standing-up motion of healthy young, elderly and post-stroke patients; Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR); London, UK. 17–20 July 2017; [DOI] [PubMed] [Google Scholar]
- 91.Al-Shaqi R., Mourshed M., Rezgui Y. Progress in ambient assisted systems for independent living by the elderly. SpringerPlus. 2016;5:1–20. doi: 10.1186/s40064-016-2272-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Vogan A.A., Alnajjar F., Gochoo M., Khalid S. Robots, AI, and Cognitive Training in an Era of Mass Age-Related Cog-nitive Decline: A Systematic Review. IEEE Access. 2020;8:18284–18304. doi: 10.1109/ACCESS.2020.2966819. [DOI] [Google Scholar]