INTRODUCTION
Road traffic injuries and drug overdoses are the two leading causes of injury death in the U.S.1 In 2017, these two mechanisms were responsible for more than 100,000 deaths. Perhaps more importantly, these two leading causes of injury are closely interconnected. Opioids and other drugs affect driving abilities (e.g., reaction time, alertness, concentration) and crash-related injuries often result in opioid prescribing,2,3 creating a potential feedback loop from crash to injury to pain to opioid use and back to crash. At any given time, about 20% of drivers have a potentially impairing drug in their system.4
Despite the magnitude of these public health problems, very little is known about the interactions between transportation and opioid use. Research has generally relied on isolated trend and risk factor analyses.5,6 As a result, our picture of connections between these two public health problems is incomplete. Studies to date have largely used fatal crash data to estimate relationships between opioids and other drugs and crash culpability. This work has been limited by toxicological data quality, little contextual information on road users’ health, and a narrow focus on fatal crashes only. Likewise, studies that have examined drug-involved crashes in traditional health care databases generally include little information about crash circumstances.7,8 These isolated or “siloed” perspectives limit an understanding of the connections between opioid and traffic crashes and limit abilities to develop solutions. This article examines the linkage potential of two rich population-based data systems, prescription drug monitoring programs (PDMP) and police-reported crash databases, and identifies knowledge gaps amenable to data linkage studies.
POPULATION-BASED SURVEILLANCE ON DRUG DISPENSING AND CRASHES
We first provide an overview of PDMP and crash data system attributes across the U.S. We then follow with a discussion of PDMP-crash data linkage feasibility, potentially transferable lessons from other linkage efforts, and knowledge gaps that could be addressed using PDMP-crash linked data.
Prescription Drug Monitoring Programs
PDMPs are state-level databases designed to facilitate the collection, monitoring, and analysis of data on dispensed controlled substances. By aggregating patient, pharmacy, prescriber, and prescription data entered by pharmacies, PDMPs are primarily used to enhance patient care and support development of prevention and treatment strategies for drug misuse. PDMPs currently exist in all 50 states and the District of Columbia (Missouri has a partial, not statewide, PDMP), among which 65% (n=33) were operational prior to 2010 (Table 1). Controlled substances tracked by PDMPs are classified by the Drug Enforcement Agency into “schedules” according to their potential harm, ranging from Schedule II (high misuse and addiction potential, e.g., methadone) to Schedule V (low misuse and addiction potential, e.g., cough medications with low codeine levels). Controlled substances classified as Schedules II-V are monitored by 76% (n=39) of PDMPs, while the remaining 24% (n=12) monitor Schedules II-IV. Several PDMPs also monitor other, non-scheduled drugs of concern (e.g., butalbital, pseudoephedrine). Schedule I controlled substances include illegal substances with no accepted medical use and are not tracked in PDMPs.
Table 1.
Select attributes of prescription drug monitoring programsa pertinent to crash report linkage, investigation, and analyses (n=51)b
| Attribute | N (%) |
|---|---|
| Year Prescription Drug Monitoring Program (PDMP) first operational | |
| <1990 | 9 (18) |
| 1990-1999 | 7 (14) |
| 2000-2009 | 17 (33) |
| 2010-2017 | 18 (35) |
| Agency responsible for PDMP administration | |
| Pharmacy Board | 20 (39) |
| Department of Health | 17 (33) |
| Professional Licensing Agency | 6 (12) |
| Law Enforcement Agency | 4 (8) |
| Substance Abuse Agency | 3 (6) |
| Consumer Protection Agency | 1 (2) |
| Authority to release PDMP data for research | |
| No authority to release | 3 (6) |
| Authorized to release | 48 (94) |
| Law enforcement access to data | |
| Access if active investigation | 36 (71) |
| Access if court process (e.g., court order, subpoena, search warrant) | 15 (29) |
| Types of data available to law enforcement | |
| Patient, prescriber, dispenser histories | 42 (82) |
| Patient and prescriber histories | 6 (12) |
| Patient history | 1 (2) |
| Unknown | 2 (4) |
| Controlled substances monitored c | |
| Schedules II-IV | 12 (24) |
| Schedules II-V | 39 (76) |
| Requirement that substance-related driving convictions be included in PDMP | |
| Yes | 1 (2) |
| No | 50 (98) |
Missouri’s PDMP does not span the entire state.
Includes 50 U.S. states and the District of Columbia
Several PDMPs also monitor other specific drugs of concern that might fall outside of these classes (e.g., pseudoephedrine); see Appendix for specific information by state.
All state PDMPs require detailed dispensing records, including prescription and fill dates, quantity dispensed, days supply, and dosage. Also required in all PDMP databases is the collection of personally identifiable information (PII), including first and last name, address, and date of birth, with some capturing other forms of identification (i.e., driver’s license number, social security number). Nearly all PDMPs (94%, n=48) are authorized to release data for research purposes, and law enforcement are often able to gain PDMP access either during an active investigation (71%, n=36) or during court proceedings (29%, n=15). In addition, Utah mandates that substance-related driving convictions (e.g., driving while impaired) be entered in the PDMP. State-level details regarding attributes and specific data elements collected by PDMPs are provided in Appendix Table 1.
Road traffic crash reports
Crash reports provide the primary data source for road safety research. Crash reports are completed by law enforcement officers at the crash scene and include individual, roadway, and vehicle information. Data generally follow a standard format, based on the Model Minimum Uniform Crash Criteria (MMUCC). PII often include first and last name, address, date of birth, and driver’s license number.
While many crash report data elements are consistent across states, including detailed information on vehicle characteristics, roadway design, environmental characteristics, and persons’ actions at the time of the crash (e.g., ran a red light) and injury status, specific documentation regarding drug involvement varies considerably by state. Sixty-two percent (n=30) of state crash report forms include a field for law enforcement to document whether they suspect a driver to be under the influence of drugs at the time of the crash (Table 2). Most state crash report forms (84%; n=43) provide an opportunity for the officer to document the type of drug test administrated (e.g., blood, urine, drug recognition expert evaluation). Results are most often captured as a positive or negative indication for drug involvement (55%, n=28 states). Additionally, 65% (n=33) of crash report forms provide a field for officers to indicate whether drugs involved were prescriptions or illicit drugs. Completion rates for these fields vary by state and time, and importantly, are germane only to the post-crash population. Scientific inference is severely limited in the absence of population-based based data on drug dispensing and use in the general population of all drivers (crash and non-crash). State-level details regarding specific drug-related data elements captured in crash reports is provided in Appendix Table 2.
Table 2.
Select attributes of crash report forms pertinent to linked analyses with prescription drug monitoring program data (n=51)a
| Attribute | N (%) |
|---|---|
| Year of last crash report form update | |
| 2005-2009 | 16 (31) |
| 2010-2014 | 23 (45) |
| 2015-2018 | 12 (24) |
| Field to document whether drugs were suspected b | |
| Yes | 30 (59) |
| Unknown or not mentioned | 21 (41) |
| Field to document type of drug test administered b | |
| Yes | 43 (84) |
| Unknown or not mentioned | 8 (16) |
| Detail of drug test result documentation b,c | |
| Positive or negative indication for drug involvement | 28 (55) |
| Drugs selected from a pre-defined list | 11 (22) |
| Narrative, supplemental document, or drug recognition expert report | 4 (8) |
| Unknown or not mentioned | 8 (16) |
| Field for whether prescription or illicit drugs involved b | |
| Yes | 33 (65) |
| Unknown or not mentioned | 18 (35) |
Includes 50 U.S. states and the District of Columbia
Documents whether a field is available on crash report form to capture these elements; completeness varies by state.
Generally captured in terms of broad categories; see Appendix for specific information by state.
Note: State laws and practices may vary with respect to release of data for linkage and research purposes and is an important state-specific consideration.
Crash and drug-related surveillance data linkage
Prior examples
Several states have initiated or established data systems linking PDMP data to other sources of public health information, providing rich perspectives and information on the opioid epidemic.9,10 Notable examples include comprehensive data systems in Massachusetts and Tennessee. Massachusetts passed legislation in 2015 to facilitate data sharing across five government agencies and ten data sources related to the opioid crisis, providing an unprecedented look at opioid prescribing, addiction, treatment, and overdose impacts across the state.10 Similarly, legislation in Tennessee facilitated the development of a data warehouse that stores and links multiple sources of health and prescription data to improve understanding of drug-related issues.11 In addition to these comprehensive and ongoing data systems, other states have conducted one-time linkages between state PDMPs and emergency department data, hospital admissions, criminal justice data, health insurance claims data, vital statistics records, medical examiner data, or Veteran’s Health Administration data to answer novel questions and guide policy.(select examples:12–14)
From a road safety perspective, there have been efforts to take a more comprehensive look at contributors to and burden of crashes. In New Jersey, a comprehensive crash outcomes database was established and includes licensing, crash report, and citation data.15 The system is also currently expanding to include sources of health data (hospital discharge data, vital records), providing a unique view of causes and consequences of crashes.16 Multiple states have used probabilistic methods to link crash and injury outcome data (e.g., the Crash Outcome Data Evaluation System) to gain a more complete understanding of crash impacts and to support transportation policy.17 Finally, numerous one-time linkage efforts have combined crash data with other state databases to explore individual risk factors, subpopulations, or trends in road traffic crashes.(select examples: 18,19)
Potential for PDMP-crash data linkage and transferable linkage lessons
Our assessment of state PDMP and crash database attributes (Tables 1 and 2) indicates that linkage of these two sources is likely feasible in many states with respect to statutory requirements and identifiers available for potential linkage. Additionally, linkage efforts underway in states highlight both the readiness in many states, as well as transferable lessons to potential crash-PDMP data linkage, including: 1) many states have either a comprehensive data system to build from or technical or political experiences to draw from; 2) political will and legislation serve a critical role in fostering linkage processes and creating sustainable data system structures;10,11 and 3) coalitions of data owners and users can ensure accurate and highly useful research and continued linkage support.20 We discuss each of these aspects below.
First, linkage requires high-quality matching variables, thorough knowledge about sources to be linked (e.g., data quality considerations), and best practice linkage approaches. In addition to these technical issues, ongoing linkage necessitates trusted relationships between agencies involved. We found many states had a successful history of linkage with PDMP or crash records, suggesting potential foundations to leverage from both technical and political perspectives. Second, many sustainable linked data systems are backed by political will and/or policy, which can help ensure stable funding streams for linkage activities and active use of the data.10,11 While such opportunities can be difficult to create and foster, there is currently considerable political attention on PDMP data systems, including refining information collected, mandating their use, and bringing in other data sources to increase overall utility. Public health and road safety partners should explore these efforts as potential windows of opportunity to elevate calls for crash data linkage.
Sustainability of linked data systems often includes the establishment of an active coalition that includes data owners and other key stakeholders, providing a forum to regularly demonstrate the tangible benefits of linkage and discuss future analytic directions.20 In some states, a promising approach could involve integrating crash records experts and PDMP data owners into existing, active opioid or road safety coalitions. In other states, stakeholder integration may be more straightforward, e.g., in four states, law enforcement manages both PDMP and crash records (Table 1).
INSIGHTS TO INFORM PUBLIC HEALTH AND SAFETY PRACTICE
PDMP-crash data linkage provides an opportunity to address several research gaps and ultimately improve clinical, public health, and road safety practice (e.g., informing Drug Recognition Expert training and practice) (Figure 1). Linkage can increase understanding of risk factors and context surrounding crashes as well as provide insights regarding consequences of these events. For example, through a comprehensive understanding of drivers’ opioid and other controlled substance regimens prior to crash events, researchers can gain a sense of which substances are most often implicated in crashes and which individual drugs or drug combinations warrant further risk analyses to ultimately inform the evidence base on impairment. Historically, our understanding of substance-impaired driving has been hampered by availability and quality of data. While PDMP-crash data linkage does not solve all impaired driving research limitations (e.g., lack of personal exposure/miles traveled data), it provides a valuable opportunity to illuminate, at a population level, specific substances, combinations of substances, and dose and duration factors deserving more detailed consideration.
FIGURE 1.
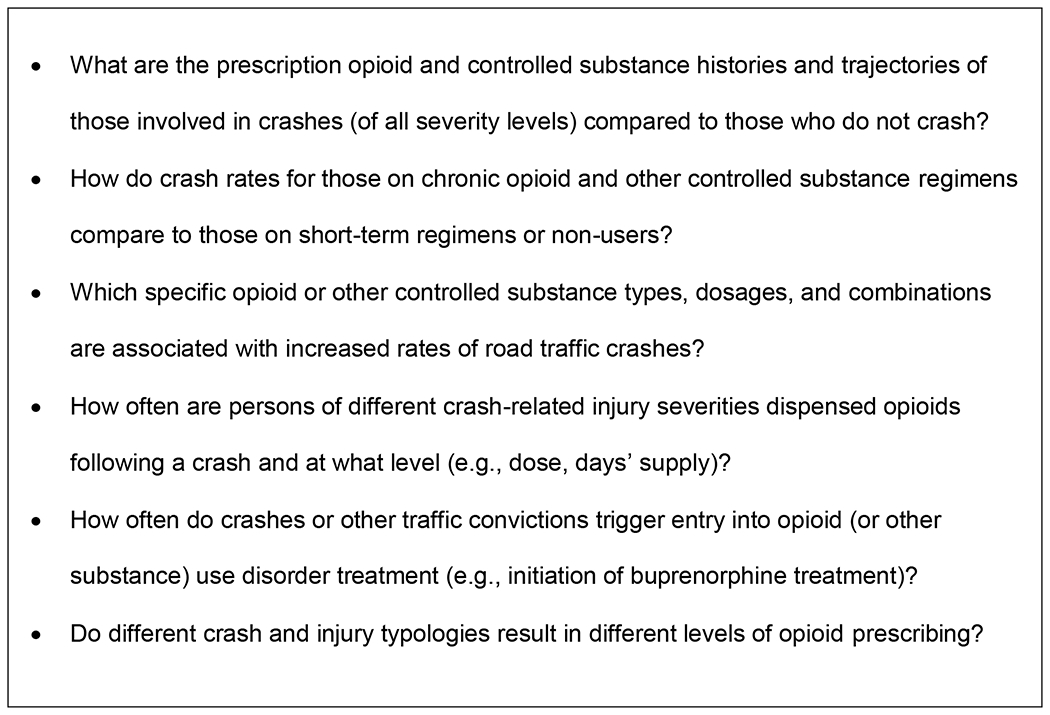
Pressing research questions best answered using linked crash reports and prescription drug monitoring program data
In addition to understanding drug-related trajectories leading up to crash events, PDMP-crash data linkage can provide a critical perspective on crash effects, with implications for tertiary prevention following a crash. For example, one could examine how often individuals experiencing crash-related injuries are dispensed opioids and other substances and the crash and substance-related risk factors for long-term drug utilization trajectories that progress from those injuries, as well as the impacts these trajectories might then have on future crash risk. Exploring prescription drug trajectories post-crash and provision of addiction treatment-related medications (e.g., buprenorphine for opioid addiction) can advance understanding of the extent and ways in which crashes alter drug use and connection to treatment (e.g., through drug courts or other channels). While preventing crashes (primary prevention) is of foremost importance, understanding how post-crash pathways might be beneficially altered and repeated injury minimized is critical (tertiary prevention). Ultimately, isolating the impacts of specific prescription drug regimens on crash risk can directly inform patient drug counseling and interventions, including consideration of alternate travel modes.
CONCLUSIONS
Crash and PDMP population-based data systems contain rich information on prescription drug histories and detailed crash circumstances, providing a valuable opportunity to advance understanding of prescription drug trajectories leading to crash events and effects of crashes on subsequent prescription drug patterns. Unfortunately, routine, on-going linkage of these data sources is lacking. However, many states have strong linkage foundations in opioid or road safety arenas, providing technical and political proficiencies to leverage. A complete and unbiased exploration of opioid-impaired driving and its consequences will require comprehensive health, substance, and travel exposure data. PDMP-crash data linkage can help fill one important piece of this puzzle and yield insights regarding the complex interplay between opioids and driving.
Supplementary Material
Appendix Table 1. Attributes of prescription drug monitoring programs pertinent to crash report linkage, investigation, and analyses by state and the District of Columbia (n=51)
Appendix Table 2. Attributes of crash report databases pertinent to linked analyses with prescription drug monitoring program data by state and the District of Columbia (n=51)
ACKNOWLEDGEMENTS
This project was directly supported by the Collaborative Sciences Center for Road Safety (www.roadsafety.unc.edu), a United States Department of Transportation National University Transportation Center (award # 69A3551747113). The UNC Injury Prevention Research Center is partly supported by an award (R49/CE0042479) from the Centers for Disease Control and Prevention. Study sponsors had no role in study design, data collection, data analysis, and interpretation of data; in writing the report; or in the decision to submit the report for peer-reviewed publication. RBN, KS, AMH, SWM, CRC designed the study and created the data acquisition plan; RBN, KS, and AMH collected the data and drafted the manuscript; SWM and CRC provided critical revisions of the manuscript for important intellectual content. All authors approved the final version of the submitted manuscript. No financial disclosures were reported by the authors of this paper.
CONFLICT OF INTEREST STATEMENT:
The authors have no conflicts of interest to report. This project was directly supported by the Collaborative Sciences Center for Road Safety (www.roadsafety.unc.edu), a United States Department of Transportation National University Transportation Center (award # 69A3551747113). The UNC Injury Prevention Research Center is partly supported by an award (R49/CE0042479) from the Centers for Disease Control and Prevention. Study sponsors had no role in study design, data collection, data analysis, and interpretation of data; in writing the report; or in the decision to submit the report for peer-reviewed publication.
APPENDIX
Details on PDMP-related data abstraction, crash record-related data abstraction, and Appendix Tables 1 and 2 can be found in the attached Appendix files.
Footnotes
FINANCIAL DISCLOSURE: No financial disclosures were reported by the authors of this paper.
Contributor Information
Rebecca B. Naumann, Department of Epidemiology and Injury Prevention Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Kristin Shiue, Department of Epidemiology and Injury Prevention Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Amin Mohamadi Hezaveh, Department of Civil and Environmental Engineering, University of Tennessee, Knoxville, TN.
Stephen W. Marshall, Department of Epidemiology and Injury Prevention Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Christopher R. Cherry, Department of Civil and Environmental Engineering, University of Tennessee, Knoxville, TN.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC). Wide-ranging Online Data for Epidemiologic Research: National Vital Statistics System Mortality Data. Atlanta, GA: CDC. https://wonder.cdc.gov/. Accessed 2019. Accessed February 22, 2019. [Google Scholar]
- 2.Pergolizzi JV Jr., Taylor R Jr., LeQuang JA, et al. Driving under the influence of opioids: what prescribers should know. J Opioid Manag. 2018;14(6):415–427. [DOI] [PubMed] [Google Scholar]
- 3.Berecki-Gisolf J, Hassani-Mahmooei B, Collie A, McClure R. Prescription opioid and benzodiazepine use after road traffic injury. Pain Med. 2016;17(2):304–313. [DOI] [PubMed] [Google Scholar]
- 4.Berning A, Compton R, Wochinger K. Results of the 2013–2014 National Roadside Survey of alcohol and drug use by drivers. Traffic Safety Facts Research Note. Report No. DOT HS 812 118. Washington, DC: National Highway Traffic Safety Administration. Published February 2015. [PubMed] [Google Scholar]
- 5.Chihuri S, Li G. Use of prescription opioids and motor vehicle crashes: a meta analysis. Accid Anal Prev. 2017;109:123–131. [DOI] [PubMed] [Google Scholar]
- 6.Gjerde H, Strand MC, Morland J. Driving under the influence of non-alcohol drugs--an update Part I: epidemiological studies. Forensic Sci Rev. 2015;27(2):89–113. [PubMed] [Google Scholar]
- 7.Gibson JE, Hubbard RB, Smith CJP, Tata LJ, Britton JR, Fogarty AW. Use of self-controlled analytical techniques to assess the association between use of prescription medications and the risk of motor vehicle crashes. Am J Epidemiol. 2009;169(6):761–768. [DOI] [PubMed] [Google Scholar]
- 8.Quinn PD, Hur K, Chang Z, et al. Incident and long-term opioid therapy among patients with psychiatric conditions and medications: a national study of commercial health care claims. Pain. 2017;158(1):140–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slavova S, Bunn TL, Hargrove SL, Corey T, Ingram V. Linking death certificates, postmortem toxicology, and prescription history data for better identification of populations at increased risk for drug intoxication deaths. Pharmaceut Med. 2017;31(3):155–165. [Google Scholar]
- 10.Massachusetts Department of Public Health. Legislative report: Chapter 55 opioid overdose study. Boston, MA: Massachusetts Department of Public Health. https://www.mass.gov/files/documents/2017/08/31/legislative-report-chapter-55-aug-2017.pdf. Published August 2017. Accessed July 19, 2019. [Google Scholar]
- 11.Office of Informatics and Analytics, Tennessee Department of Health. Tennessee’s annual overdose report: understanding and responding to the opioid epidemic in Tennessee using mortality, morbidity, and prescription data. Nashville, TN: Tennessee Department of Health. https://www.tn.gov/content/dam/tn/health/documents/pdo/2019_Report.pdf. Published February 2019. Accessed July 19,2019. [Google Scholar]
- 12.Naumann RB, Marshall SW, Lund JL, Gottfredson NC, Ringwalt C, Skinner AC. Evaluating short- and long-term impacts of a Medicaid “lock-in” program on opioid and benzodiazepine prescriptions dispensed to beneficiaries. Drug Alcohol Depend. 2018;182:112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dasgupta N, Funk MJ, Proescholdbell S, Hirsch A, Ribisl KM, Marshall S. Cohort study of the impact of high-dose opioid analgesics on overdose mortality. Pain Med. 2016;17(1):85–98. [DOI] [PubMed] [Google Scholar]
- 14.Carlson KF, Gilbert TA, Morasco BJ, et al. Linkage of VA and state prescription drug monitoring program data to examine concurrent opioid and sedative-hypnotic prescriptions among veterans. Health Serv Res. 2018;53 Suppl 3:5285–5308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curry AE, Metzger KB, Pfeiffer MR, Elliott MR, Winston FK, Power TJ. Motor vehicle crash risk among adolescents and young adults with attention-deficit/hyperactivity disorder. JAMA Pediatr. 2017;171(8):756–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curry AE. Catalyzing young driver research via data linkage: development of a comprehensive traffic safety data warehouse. NIH grant 5R21HD092850-02. 2017.
- 17.National Highway Traffic Safety Administration (NHTSA). The Crash Outcome Data Evaluation System (CODES) and applications to improve traffic safety decision-making. Report No. DOT HS 811 181. Washington, DC: NHTSA. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/811181. Published April 2010. Accessed July 19, 2019. [Google Scholar]
- 18.Bunn T, Singleton M, Nicholson V, Slavova S. Concordance of motor vehicle crash, emergency department, and inpatient hospitalization data sets in the identification of drugs in injured drivers. Traffic Inj Prev. 2013;14(7):680–689. [DOI] [PubMed] [Google Scholar]
- 19.Conderino S, Fung L, Sedlar S, Norton JM. Linkage of traffic crash and hospitalization records with limited identifiers for enhanced public health surveillance. Accid Anal Prev. 2017;101:117–123. [DOI] [PubMed] [Google Scholar]
- 20.Milani J, Kindelberger J, Bergen G, et al. Assessment of characteristics of state data linkage systems. Report No. DOT HS 812 180. Washington, DC: National Highway Traffic Safety Administration, and Atlanta: Centers for Disease Control and Prevention. https://www.cdc.gov/motorvehiclesafety/pdf/linkage/assessment_of_characteristics_of_state_data_linkage_systems-a.pdf. Published August 2015. Accessed July 19, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Table 1. Attributes of prescription drug monitoring programs pertinent to crash report linkage, investigation, and analyses by state and the District of Columbia (n=51)
Appendix Table 2. Attributes of crash report databases pertinent to linked analyses with prescription drug monitoring program data by state and the District of Columbia (n=51)


