Abstract
Objectives
Rapid review to determine the magnitude of association between potential risk factors and severity of COVID-19, to inform vaccine prioritisation in Canada.
Setting
Ovid MEDLINE(R) ALL, Epistemonikos COVID-19 in L·OVE Platform, McMaster COVID-19 Evidence Alerts and websites were searched to 15 June 2020. Eligible studies were conducted in high-income countries and used multivariate analyses.
Participants
After piloting, screening, data extraction and quality appraisal were performed by a single experienced reviewer. Of 3740 unique records identified, 34 were included that reported on median 596 (range 44–418 794) participants, aged 42–84 years. 19/34 (56%) were good quality.
Outcomes
Hospitalisation, intensive care unit admission, length of stay in hospital or intensive care unit, mechanical ventilation, severe disease, mortality.
Results
Authors synthesised findings narratively and appraised the certainty of the evidence for each risk factor–outcome association. There was low or moderate certainty evidence for a large (≥2-fold) magnitude of association between hospitalisation in people with COVID-19, and: obesity class III, heart failure, diabetes, chronic kidney disease, dementia, age >45 years, male gender, black race/ethnicity (vs non-Hispanic white), homelessness and low income. Age >60 and >70 years may be associated with large increases in mechanical ventilation and severe disease, respectively. For mortality, a large magnitude of association may exist with liver disease, Bangladeshi ethnicity (vs British white), age >45 years, age >80 years (vs 65–69 years) and male gender among 20–64 years (but not older). Associations with hospitalisation and mortality may be very large (≥5-fold) for those aged ≥60 years.
Conclusions
Increasing age (especially >60 years) may be the most important risk factor for severe outcomes. High-quality primary research accounting for multiple confounders is needed to better understand the magnitude of associations for severity of COVID-19 with several other factors.
PROSPERO registration number
CRD42020198001.
Keywords: COVID-19, epidemiology, public health, intensive & critical care
Strengths and limitations of this study.
This rapid review captured a broad range of risk factors and outcomes associated with COVID-19 severity.
Eligible studies reported independent associations through statistical adjustment and were applicable to high-income countries.
The certainty of evidence was assessed for each risk factor-outcome-population association.
The rapid approach involved pilot testing each review step with multiple reviewers until a high level of agreement was achieved; then a single experienced reviewer completed study selection, data extraction and risk of bias assessments.
The review includes studies published up to June 2020; guidance on vaccine prioritisation should also consider emerging evidence.
Introduction
COVID-19 is an infectious respiratory disease caused by the newly identified SARS-CoV-2,1 which reached worldwide pandemic status in early March 2020.2 As of 7 December, there were over 65.8 million confirmed cases worldwide and 1.5 million deaths attributed to the virus.3 Most people who develop COVID-19 will experience mild-to-moderate illness primarily affecting the respiratory system and recover at home.4 In more severe cases, patients may require specialised care (eg, admission to hospital and/or intensive care unit (ICU), assisted ventilation)5 as the disease can progress to respiratory failure and/or affect multiple organ systems.4
Given the rapid spread of COVID-19 since its first emergence in late 2019, and potential for severe illness (including death), the development of a preventive vaccine has become a global priority.6 Vaccine development has been progressing at an unprecedented pace7–10; however, the initial vaccine supply is not expected to be sufficient to cover the entire population right away. Therefore, it is of high priority to policymakers to plan for the efficient, effective and equitable allocation of vaccines when limited supply will necessitate recommendations for the vaccination of certain groups earlier than others. Due to the novel nature of COVID-19, these groups for early vaccination have not yet been established.11
The National Advisory Committee on Immunisation (NACI) is an expert advisory body that provides advice on the use of vaccines in Canada.12 At the time of writing, NACI is developing guidance on priority pandemic immunisation strategies for COVID-19 vaccination when initial vaccine supply is limited.11 To inform this guidance, NACI is using its recently published Ethics, Equity, Feasibility and Acceptability (EEFA) Framework13 to ensure these factors are systematically and comprehensively considered. One of the evidence informed tools that make up this framework is the ‘Equity Matrix’ which has adapted the PROGRESS-Plus model of health determinants and outcomes14 to ensure important vaccine-specific equity factors are explicitly included. The resulting ‘P2ROGRESS And Other Factors’ framework includes a range of biological and social factors that likely contribute to inequities in health outcomes across population groups (eg, pre-existing disease/condition, place/state of residence, race/ethnicity/culture/language, occupation, gender identity/sex), but it is not yet clear how each factor might apply to COVID-19 outcomes. A discussion on the use of this Equity Matrix, with evidence from this rapid review, as a critical tool to guide the ethically just allocation of scarce resources is published elsewhere.15
With the aim of providing timely, evidence-informed guidance on pandemic vaccine prioritisation, NACI required a rigorous and expedited synthesis of the available evidence on population groups that are at increased risk of severe illness and mortality as a result of COVID-19. Responding to this need, we conducted a rapid review to determine the magnitude of association between ‘P2ROGRESS And Other Factors’ and risk of severe outcomes of COVID-19.
Methods
Review approach
Rapid reviews are a form of knowledge synthesis that accelerate the process of conducting a traditional systematic review through streamlining or omitting some steps to produce evidence in a resource-efficient manner.16 Methods for streamlining one or more stages of the review process are highly dependent on context such as the organisational capacity of the review producer (eg, trained and experienced personnel), and needs of policy-makers for decision making17 18; one or more of the systematic review dimensions (ie, scope, comprehensiveness, rigour/quality control, approach to synthesis, conclusions) may be modified for a rapid review.17
The need for empiric evidence to inform the prioritisation of pandemic immunisation strategies in Canada necessitated a rapid but rigorous approach to synthesising the currently available data. Therefore, we performed a rapid review informed by traditional systematic review methodology,19 with several modifications to allow for the evidence to be synthesised on an expedited timeline. We sought stakeholder input on the review question, eligibility criteria and outcomes, to inform the protocol for applicability and feasibility. We used a single experienced reviewer to select studies, extract data and assess risk of bias, whereas in traditional systematic reviews these steps typically involve two reviewers to some degree. To ensure methodological rigour, we conducted pilot testing with more than one reviewer at each step; once a high level of agreement was achieved, a single reviewer proceeded with completing the step. In addition, we focused the scope of the review to include only higher quality studies (ie, using adjusted analysis), and those having high applicability to Canada (eg, high-income countries with universal-like healthcare systems).
NACI’s High Consequence Infectious Disease Vaccine Working Group was consulted to develop and refine the scope of the review (ie, priority population(s), risk condition(s)/factor(s), and outcomes of interest), but was not involved in the conduct of the review. The working group was not involved in selection of studies nor the synthesis of findings.
The review was conducted following an a-priori protocol (PROSPERO #CRD42020198001). Because there is not yet formal guidance on the reporting of rapid reviews, reporting adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.20
Literature search
A health sciences librarian searched Ovid MEDLINE(R) ALL on 15 June 2020 using concepts related to COVID-19, P2ROGRESS And Other Factors, and severe outcomes (online supplemental file 1). The search was limited to studies published in English or French in 2020. Additionally, the search was limited to populations in countries that are members of the Organisation for Economic Cooperation and Development (OECD),21 in an effort to include studies of highest relevance to the Canadian context. Editorials and letters were excluded. We supplemented the Medline search by handsearching Epistemonikos COVID-19 in L·OVE Platform (https://app.iloveevidence.com/topics) and McMaster COVID-19 Evidence Alerts (https://plus.mcmaster.ca/COVID-19/) for relevant prognosis or aetiology studies up to 12 June 2020. A handsearch of relevant websites recommended by the NACI working group was also undertaken, as well as continual surveillance for publication of relevant preprints located by the search. Searches were exported to an Endnote Library (X9, Clarivate Analytics, Philadelphia, Pennsylvania USA) and duplicates removed.
bmjopen-2020-044684supp001.pdf (1,017.8KB, pdf)
Eligibility criteria
We included studies published in English or French since 1 January 2020 that reported on the magnitude of association between potential P2ROGRESS And Other Factors and several outcomes of COVID-19 (online supplemental file 2). Eligible source populations, in order of priority, were people (1) from a general/community sample, (2) with COVID-19 confirmed (by laboratory testing or epidemiologic linkage) and (3) hospitalised with COVID-19. Although considered potentially of interest, studies only including people with a risk factor of interest were not included. We excluded studies where the entire study population had severe disease (eg, ICU settings). To ensure relevance to the Canadian context, studies had to be conducted in OECD countries21; we included OECD studies from countries that do not provide universal (or near universal) coverage for core medical services (ie, Chile, Greece, Mexico, Poland, the Slovak Republic and the USA)22 but considered these to be less applicable to the Canadian context when interpreting the findings. The infection must have been confirmed by laboratory testing or linked epidemiologically (eg, household contact). Studies including populations with other pandemic-related infections (eg, severe acute respiratory syndrome, Middle East respiratory syndrome) were excluded if data specific to COVID-19 cases could not be isolated.
The exposures of interest were any P2ROGRESS And Other Factors believed to be associated with differential outcomes across population groups (ie, pre-existing conditions, place or state of residence, race/ethnicity/culture/language, immigration, refugee status, occupation, gender identity or sex, religion or belief system, education or literacy level, socioeconomic status, social capital, age and other factors).23 24 We did not include as risk factors any signs or symptoms on presentation with COVID-19. Eligible comparators were those within the same source population (eg, all hospitalised, as described above) that did not have the P2ROGRESS And Other Factor, or experienced a P2ROGRESS And Other Factor to a different degree (eg, older vs younger). We excluded studies of interventions.
Any length of follow-up for outcomes of interest was acceptable. Eligible studies reported on at least one primary outcome (ie, rate of hospitalisation, hospital length of stay, severe disease (as defined by study authors; eg, composite outcome of ICU transfer or death), ICU admission and length of stay, need for mechanical ventilation (MV), and mortality (case fatality or all-cause). We refer to this range of outcomes as ‘severe COVID-19’ or ‘severity of COVID-19’ throughout the review, though distinct from the composite outcome of ‘severe disease’. Each of these outcomes are applicable to at least one of the above-mentioned eligible populations. In order to prioritise the most rigorous and applicable evidence, we included only prospective and retrospective cohort studies that employed a multivariate analysis and provided results of the independent contribution of P2ROGRESS And Other Factors to severe outcomes, while accounting for potential confounders (minimally age and sex). Preprints were included only if they were accepted by a peer-reviewed journal; preprints that were later published (between the date of the search and manuscript submission) were included. Government reports from handsearched websites were eligible.
Study selection
All records retrieved by the searches were exported to a Microsoft Office Excel (Microsoft, Redmond, Washington, USA) spreadsheet for screening. After piloting the eligibility criteria on a sample of 70 records, one reviewer independently screened records for inclusion by title/abstract, and those deemed to be potentially relevant were assessed by full text. Uncertainties about the inclusion of any full text study were resolved through consultation with a second reviewer.
Data extraction
Following a pilot round, one reviewer independently extracted data from each included study into an Excel workbook. We extracted data on (1) population size and demographics, (2) setting, (3) dates of data collection, (4) COVID-19 ascertainment method, (5) coinfections, (6) outcomes reported with definitions for composite outcomes (eg, severe disease), (7) number of participants analysed and (8) relevant outcome data related to P2ROGRESS factors of interest (using the most adjusted model, if more than one was reported). For both continuous and dichotomous outcomes, we extracted adjusted relative effect sizes (ie, OR, risk ratio (RR), HR) and measures of variability (95% CI). A second reviewer was consulted in the event of uncertainty about any of the extracted data. Given the expedited approach, we extracted only data that were reported within the included studies and made no attempt to contact authors for missing or unclear data.
Quality assessments
To expedite quality assessments, we did not use a formal tool; instead we focused on key variables that were considered to be most relevant to the topic, and that would allow for meaningful stratification of studies by quality. The key variables that we used to assess the quality of the included studies were (1) the extent of adjustment for relevant covariates (ie, basic adjustment for age and sex, vs more extensive adjustment for numerous potential confounders including comorbidities), (2) follow-up duration and extent of censorship for some outcomes (eg, ≥2 weeks for mortality) and (3) inappropriate or large exclusions from the study and/or analysis (eg, missing data on risk factor status or analytical variables). Following assessment of these key variables by a single reviewer, studies without concerns for all three criteria were rated good while others were rated fair. A second reviewer was consulted in the case of uncertainty about the assessment of any individual study.
Synthesis
Given substantial clinical (eg, risk factors and/or comparators examined, outcome definitions) and methodological (varying covariates included in the adjusted analyses, different measures of association) heterogeneity, it was not thought appropriate to pool the studies statistically. Instead, we present a narrative summary of the results across studies for each risk factor. When making conclusions about the association between a P2ROGRESS And Other Factor and an outcome, we focused primarily on the magnitude of effect rather than statistical significance, which is heavily dependent on sample size. We categorised associations to be small/unimportant (OR or RR)≤1.70), moderate (1.71 to 1.99), large (≥2.00) or very large (≥5.00).25 When determining the magnitude, we compared findings across all relevant studies and often relied heavily on the findings of the largest and/or good-quality studies.
Certainty of evidence
The expedited approach to evidence synthesis did not allow for a formal appraisal of the certainty of evidence across studies for each P2ROGRESS And Other Factor-Outcome association. Instead, a single reviewer assessed the certainty of the evidence for each association considering relevant components of the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach26 27: (1) directness in terms of country (presence of universal healthcare) and source population (community sample vs hospitalised patients), (2) sample size (n<500 considered small) and magnitude of association, (3) study quality and (4) consistency of associations (in direction and magnitude) across studies. Bodies of evidence started at high certainty28 and were rated down for weaknesses in any of the aforementioned characteristics. The level of certainty in associations are referred to using the terms ‘uncertain’ (no or very low certainty), ‘may’ (low or some certainty) and ‘probably’ (moderate certainty).29 At least two other reviewers confirmed the certainty of evidence appraisals, with disagreements resolved by discussion.
Results
Characteristics of studies
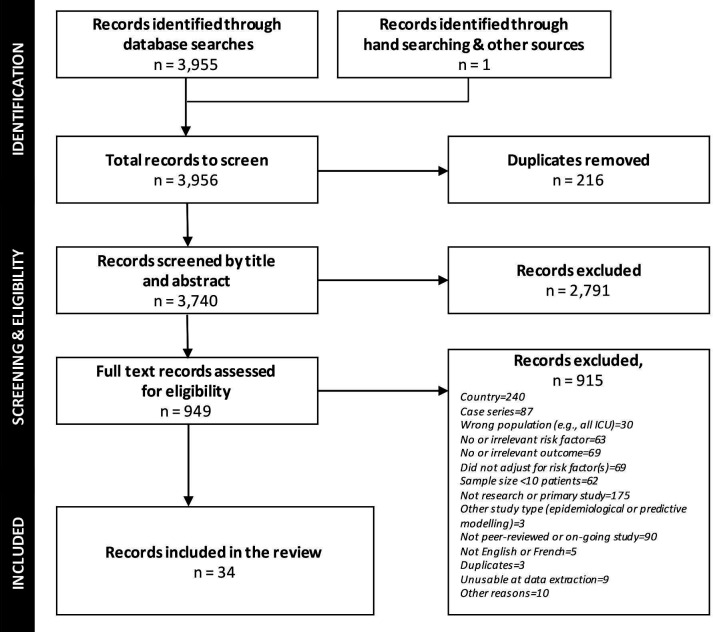
Of 3740 unique records identified by the searches, 949 were screened at full text, and 34 studies that reported on 32 unique populations were included in the review (figure 1, online supplemental file 3) shows studies excluded by full text, with reasons).30–63 Three studies conducted in the UK46 51 54 used overlapping cohorts from a single medical/research database and were considered as a single population in the analysis. Another large UK study63 is likely to also be overlapping with these populations, but the degree of overlap is not known.
Figure 1.
PRISMA flow of study selection. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1 shows the characteristics of the included studies (full details about individual studies in online supplemental file 4). The studies were published between 23 April and 6 July 2020, and half (17/34, 50%) reported on populations in the USA.30 31 38 39 43–45 47–50 52 53 56 58 60 61 The remaining countries represented (Italy,32 34–37 42 57 62 Spain,33 UK40 46 51 54 55 59 63) all have universal or universal-like healthcare (one study used data from 17 countries). All studies reported on adults, and the overall median was 596 participants (range 44–418 794). The mean or median age of the populations studied ranged from 42 to 84 years (in 32/34 (94%) mean age was 54 –71 years). Most studies (16/34, 47%) examined the association between risk factors and outcomes in a hospitalised population. Studies reported variable definitions of ‘severe disease’; we considered them sufficiently similar to be grouped under this outcome. Studies most commonly reported on the independent association of pre-existing conditions (n=27 studies), gender identity or sex (n=18) and race or ethnicity (n=12) with severe outcomes (most commonly hospitalisation, n=9). P2ROGRESS And Other Factors not examined in the included studies were immigration or refugee status, religion or belief system, social capital and substance abuse disorders. There were also no data specific to pregnant women, indigenous populations, people with disabilities, nor different ages in children.
Table 1.
Included studies overview (n=34)
| Study design and country (noof studies) |
P2ROGRESS risk factors (no of studies*) |
COVID-19 (no of studies) |
Primary outcomes (no of studies*) |
Risk of bias (no of studies) |
Study design:
Country:
|
|
Diagnosis:
|
|
Good (19) Fair (15) |
*A study may contribute to more than one risk group or outcome.
†Study of healthcare workers includes data from Australia, Canada, Chile, China, Germany, India, Ireland, Italy, Netherlands, New Zealand, Pakistan, Poland, Singapore, South Africa, Sweden, UK and USA.
‡Severe disease, defined by studies as (number of studies): requiring high-flow oxygen (1); ICU or MV (1); non-invasive ventilation or MV (1); MV (4); ICU or mortality (composite)(4); hospitalisation and/or 30-day mortality (composite)(1); MV or mortality (composite)(1); ICU, MV, discharge to hospice or death (composite)(1).
COPD, chronic obstructive pulmonary disease; ICD, International Classification of Diseases; ICU, intensive care unit; MV, mechanical ventilation; NR, not reported; RT-PCR, reverse transcription PCR.
Study quality
The majority of studies (19/34, 56%) were rated as good quality30 31 36 38 40–43 47 49 52 53 55–60 62 because they adjusted for age, sex and pre-existing disease in their analysis, had adequate follow-up of outcomes and few or no missing data. The remaining studies had flaws in one or more of the three domains that we considered to be most important for this review.
Association between risk factors and outcomes
Table 2 shows a summary of findings for associations between each reported risk factor and outcomes of interest; detailed data are in online supplemental file 5.
Table 2.
Summary of evidence for associations between risk factors and severe outcomes of COVID-19
| Risk factor (at-risk vs reference population)* | Population† | Magnitude of association (confidence in association)‡, by outcome Magnitude of associations are shown as: uncertain (no/very low confidence), no important association (-; OR or RR ≤1.70), moderate association (+1.71–1.99), large/important association (++;≥2.00), or very large important association (+++;≥5.00) |
||||
| Hospitalisation | ICU admission | Mechanical ventilation | Severe disease | Mortality | ||
| Pre-existing conditions | ||||||
| Body mass index (BMI) (kg/m2)§ | ||||||
| Underweight (<18.5) vs normal (18.5–24.9) | Hospitalised | – (low) |
– (low) |
– (low) |
||
| Overweight (25.0–29.9) vs normal | Community sample or positive for COVID-19 | – (low) |
uncertain | uncertain | – (low) |
– (low) |
| Obesity class I and II (≥30.0) vs normal | Community sample or positive for COVID-19 | + (low) |
+ (low) |
+ (low) |
– (low) |
– (moderate) |
| Obesity class III (≥40.0) vs normal | Positive for COVID-19 | ++ (low) |
uncertain | + (low) |
- to + (low) |
|
| Respiratory conditions | ||||||
| Chronic, varied (eg, asthma, COPD) | Community sample or positive for COVID-19 | – (moderate) |
uncertain | uncertain | – (moderate) |
– (moderate) |
| Prior pneumonia | Community sample | – (low) |
||||
| Cardiovascular disease | ||||||
| Heart failure | Community sample | – (low) |
||||
| Positive for COVID-19 | ++ (low) |
+ (low) |
– (low) |
|||
| Coronary artery disease, hypertension, hyperlipidaemia, composite outcomes | Community sample or positive for COVID-19 | – (moderate) |
uncertain | uncertain | – (low) |
– (low) |
| Diabetes | Community sample | – (low) |
||||
| Positive for COVID-19 | ++ (low) |
uncertain | – (low) |
– (low) |
– (moderate) |
|
| Liver disease | Positive for COVID-19 | – (low) |
++ (low) |
|||
| Hospitalised | – (low) |
|||||
| Chronic kidney disease | Community sample or positive for COVID-19 | ++ (moderate) |
– (moderate) |
– (moderate) |
||
| Inflammatory bowel disease | Positive for COVID-19 | – (low) |
– (low) |
|||
| Dementia/chronic neurological disorders | ||||||
| Alzheimer’s disease or dementia | Community sample | ++ (low) |
– (low) |
|||
| Chronic neurological disorders | Hospitalised | – (low) |
||||
| Cancer | ||||||
| Any cancer | Positive for COVID-19 | – (moderate) |
– (moderate) |
– (moderate) |
||
| Haematological malignancy | Positive for COVID-19 | + (low) |
||||
| Immunocompromised | ||||||
| Rheumatic disease | Positive for COVID-19 | uncertain | uncertain | uncertain | ||
| HIV | Hospitalised | uncertain | ||||
| Mental health | ||||||
| Depression | Positive for COVID-19 | – (low) |
||||
| Ever visited a psychiatrist | Community sample | – (low) |
||||
| Other factors | ||||||
| Age§ | ||||||
| 45–54 vs ≤45 years old | Positive for COVID-19 | ++ (moderate) |
– (low) |
++ (low) |
||
| 50–64 vs ≤45 years old | Positive for COVID-19 | ++ (moderate) |
– (low) |
++ (moderate) |
||
| >60 vs ≤45 years old | Positive for COVID-19 | ++/+++ (moderate/low) |
++ (low) |
+ (low) |
++/+++ (moderate/low) |
|
| >70 or 75 vs ≤45 years old | Positive for COVID-19 | +++ (moderate) |
++ (low) |
+++ (moderate) |
||
| >80 vs ≤45 years old | Positive for COVID-19 | +++ (low) |
+++ (low) |
|||
| 70–79 vs 65–69 years old | Hospitalised | – (moderate) |
||||
| >80 vs 65–69 years old | Hospitalised | ++ (low) |
||||
| Increased age (continuous/incremental)¶ | Community sample or positive for COVID-19 | Approximately 2%–6% relative increase per year (moderate) | – (low) |
– (low) |
– (low) |
Approximately 5%–10% relative increase per year (moderate) |
| Gender or sex | ||||||
| Male vs female (all ages, mean 54–73) | Community sample | – (low) |
||||
| Positive for COVID-19 | ++ (moderate) |
uncertain | + (low) |
– (low) |
– (moderate) |
|
| Male vs female (20–64 years)** | Hospitalised | ++ (low) |
||||
| Race/ethnicity | ||||||
| Black vs non-Hispanic white | Community sample or positive for COVID-19 | ++ (low) |
– (moderate) |
– (moderate) |
– (moderate) |
– (moderate) |
| Hispanic vs non-Hispanic white | Positive for COVID-19 | – (low) |
uncertain | – (low) |
– (low) |
|
| Asian vs white | Community sample or positive for COVID-19 | – (moderate) |
– (low) |
– (low) |
– (low) |
– (moderate) |
| Asian (Bangladeshi) vs British white | Hospitalised | ++ (low) |
||||
| Culture/language/immigrant/refugee status | ||||||
| Place of residence/household size | ||||||
| Living in a low income area | Positive for COVID-19 | – (low) |
||||
| Homeless vs has a home | Positive for COVID-19 | ++ (low) |
||||
| Suburban vs urban hospital | Hospitalised | uncertain | ||||
| 1, 3 or 4 vs 2 household members | Community sample | – (low) |
||||
| Occupation | ||||||
| Laryngologist or intubator vs assistant | Healthcare workers for COVID-19 patients | – (low) |
||||
| Education level | ||||||
| Lower education vs university degree | Community sample | – (low) |
||||
| Socioeconomic status | ||||||
| Highest vs lowest quintile of social deprivation | Community sample | + (low) |
– (moderate) |
|||
| Income ≤25th vs >50th or 75th percentile | Positive for COVID-19 | ++ (low) |
||||
| ≥Average vs below average income | Community sample | – (low) |
||||
| Smoking | ||||||
| Current or former vs never | Community sample or positive for COVID-19 | – (moderate) |
uncertain | – (low) |
– (low) |
|
| Alcohol consumption | ||||||
| Above vs within guidelines | Community sample or positive for COVID-19 | – (low) |
||||
| Physical activity level | ||||||
| Below vs within guidelines | Community sample or positive for COVID-19 | – (low) |
||||
*When not listed, the reference group are those without the risk factor.
†Outcomes of severe disease (as defined by authors), ICU admission, mechanical ventilation and mortality are all in a hospitalised population, except for liver disease, where findings differed depending on the population denominator used.
‡A formal assessment of the quality/confidence of the evidence was not performed but was informed by the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach. We determined our confidence in the magnitude of the associations by considering primarily study limitations (risk of bias), consistency in findings across studies and precision (sample size). Very low confidence indicates that were have no/very low confidence about possible associations; low means that the evidence indicates that there may be an association; moderate means that the evidence indicates that there probably is an association. High certainty evidence was not found for any association.
§For categorical data for age, and BMI, the reference group differed slightly across studies.
¶For continuous or incremental data for age, the rate of hospitalisation and mortality outcomes, approximately half of the studies analysed data on a continuum (with the remainder reporting in incremental categories, for example, 5 years units).
**Subgroup data from one study that analysed the younger population separately.
COPD, chronic obstructive pulmonary disease; ICU, intensive care unit; RR, risk ratio.
There was low or moderate certainty of evidence for important/large associations with increased hospitalisation in people having confirmed COVID-19, for the following risk factors: obesity class III (body mass index ≥40 kg/m2; one study, n=5297),56 heart failure (two studies, n=6331),30 56 diabetes (two studies, n=6331),30 56 chronic kidney disease (confirmed COVID-19 or community sample; two studies, n=4 24 073),54 56 dementia (one study, n=4 18 794),54 age over 45 years (vs 45 or younger; two studies, n=6331),30 56 male gender (three studies, n=3812),30 56 58 black race/ethnicity (vs non-Hispanic white; confirmed COVID-19 and community samples, 5 studies in four populations, n=428 606),30 51 54 56 58 homelessness (one study, n=1052)30 and low income (<25th vs >50th percentile; one study, n=1052).30 Age over 60 and over 70 years may be associated with important increases in the rate of MV (one study, n=486)47 and severe disease (one study, n=2725),56 respectively.
There may be important associations for increased mortality with liver disease (two studies, n=20 597),40 60 Bangladeshi ethnicity (vs British white; one study, n=130 091),63 and age over 45 years (vs <45 years; three studies, n=87 819).40 56 63 The data were somewhat inconsistent for gender, with most studies showing moderate certainty of no important effect, but one large fair quality study (n=1 30 091)63 from the UK that stratified its analysis by age showed that hospitalised males aged 20–64 years (but not older) may be at about twofold increased risk of mortality compared with females.
Associations with hospitalisation and mortality may be very large for those aged over 60 years (two studies, n=6331 for hospitalisation30 56; three studies, n=24 163 for mortality40 48 56) and are probably very large for those over 70 years (two studies, n=6331 for hospitalisation30 56; two studies, n=22 858 for mortality40 56). One study (n=63 094)63 directly compared subgroups of older hospitalised adults, showing that compared with those aged 65–69 years, there may be no important association with mortality among adults aged 70–79 years, but the strength of associations may increase about a magnitude of twofold for those 80 years and older. Studies treating age on a continuum or across small increments consistently found that the magnitude of association for hospitalisation and mortality increased with increasing age (eg, approximately 2%–6% and 5%–10% relative increase per year) (three studies in two populations, n=422 275 for hospitalisation51 54 58; 11 studies, n=6877 for mortality).32–34 38 42 45 52 53 55 58 62
A moderate magnitude of association may exist between MV (four studies, n=1559),45 47 49 53 ICU admission (two studies, n=873),45 49 and severe disease (one study, n=2725)56 and obesity (body mass index ≥30 or 40 kg/m2); severe disease and heart failure (one study, n=2725)56; mortality and haematological malignancy (one study, n=1183)59; MV and male gender (four studies, n=881)34 47 49 53; and hospitalisation and social deprivation (highest vs lowest quintile; one study, n=340 996).51
There was moderate certainty evidence for no important increase in hospitalisation with chronic respiratory conditions (four studies in three populations, n=425 125),30 51 54 56 cardiovascular disease apart from heart failure (ie, coronary artery disease, hypertension, hyperlipidaemia; four studies in three populations, n=425 125),30 51 54 56 non-specific cancer (two studies, n=6331),30 56 Asian race/ethnicity other than Bangladeshi (vs non-Hispanic white; 3 studies in two populations, n=424 073),51 54 56 and current or former smoking (five studies in three populations, n=425 125).30 46 51 54 56 Additionally, there was moderate certainty evidence for no important increase in severe disease with chronic respiratory conditions (one study, n=2725),56 chronic kidney disease (two studies, n=2922),31 56 non-specific cancer (two studies, n=2769),36 56 and black race/ethnicity (vs non-Hispanic white; two studies, n=3030)43 56 and no important increase in mortality with obesity (body mass index ≥30 kg/m2; six studies, n=8716),42 45 50 53 56 58 chronic respiratory conditions (four studies, n=23 315),38 40 53 56 diabetes (four studies, n=23 315),38 40 53 56 chronic kidney disease (three studies, n=23 058), nonspecific cancer (three studies, n=24 041),40 56 59 male gender (nine studies, n=27 875),32–34 38 40 42 53 56 58 Black (five studies, n=135 418)45 55 56 58 63 or Asian race/ethnicity (vs non-Hispanic white; three studies, n=4015)45 55 56 and social deprivation (lowest vs highest quintile; one study, n=130 091).63 Overall, there were few data for the ICU and MV outcomes.
Discussion
Responding to a need for empiric evidence to inform decision making on Canada’s immunisation strategies,11 in this rapid review, we synthesised studies employing multivariate analysis to ascertain potential independent associations between ‘P2ROGRESS And Other Factors’ and severe outcomes of COVID-19. Among 22 potential risk factors examined across the included studies, the most important risk factors (ie, those associated with large/important increased risk or odds; RR or OR ≥2.0) for hospitalisation among those with confirmed COVID-19 were several pre-existing chronic health conditions (obesity class III, heart failure, diabetes, chronic kidney disease [community sample or with COVID-19], dementia [community sample]), older age (>45 years vs younger), male gender, black race/ethnicity (community sample or with COVID-19), homelessness and low income (≤25th vs >50th percentile). Liver disease may be have a large magnitude of association with increased mortality among people with COVID-19; advancing age (>45 years vs younger) and Bangladeshi ethnicity (vs British white) are likely to have large magnitude of associations with increased mortality among hospitalised patients. There is evidence to suggest that male gender may be associated with increased mortality among younger (20–64 years), but not older men.
Among the factors that increase the chance of severe outcomes, age seemed to be the most influential; adults older than 60 years may have at least five times the magnitude of association with hospitalisation and mortality from COVID-19 compared with those aged less than 45 years. This association with increased hospitalisation and mortality appears to magnify at least to some degree even for those older than 60 years, with those aged over 80 years possibly having double the magnitude of association for mortality of those aged 65–69 years.
The findings of this rapid review will be used to populate the Equity Matrix of NACI’s EEFA Framework,13 which will be a part of a suite of considerations for informing the development of NACI recommendations on priority pandemic immunisation strategies when initial COVID-19 vaccine supply is limited. NACI will be using the results of this rapid review and their current understanding of the epidemiology of COVID-19 in Canada to identify distinct inequities associated with COVID-19, potential reasons for these inequities and suggested interventions to reduce inequities and improve access to vaccine when it becomes available. The Equity Matrix applied to COVID-19 with evidence to date can be found elsewhere.15
Limitations of the evidence
There are several limitations to the evidence base. Though we focused the review on better quality studies that minimally controlled for age and sex, the strength of certain associations should be interpreted cautiously because there are likely to be multiple unmeasured confounders that have not been accounted for. For example, studies reporting on associations between outcomes and age did not adjust for nursing home residency and studies examining race did not account for occupation which may be an important confounder influencing susceptibility to the infection.63 In addition, it is important to be aware that criteria for COVID-19 testing and hospitalisation may differ by place and time, but it is difficult to predict how this may have impacted the findings. In general, many studies conducted testing based on symptoms and the evidence is likely most applicable to these populations. The evidence for MV, ICU admission and severe disease outcomes was relatively sparse. As we located no evidence meeting our publication date and inclusion criteria to inform the impact of immigration or refugee status, religion or belief system, social capital, substance abuse disorders, pregnancy, Indigenous identity, living with a disability, nor differing levels of risk among children in various age groups, there is a need for high quality primary research (accounting for multiple confounders) to better understand the magnitude of association with these risk factors. Given the rapid emergence of new evidence on the topic, potential associations (or lack of association) for which only low or very low certainty of evidence is available should continue to be reviewed as new primary research is published.
Strengths and limitations of the review
Our analysis across a large range of risk factors by detailed outcomes along the continuum of the natural history of COVID-19 disease highlights the methodological rigour and comprehensiveness of the present work. Whereas many rapid reviews omit all assessment of study quality and certainty of the evidence, we felt this was critical for rigour of interpretation and undertook these steps. Given our rapid approach, it is possible that studies were missed and that undetected errors in data exist. We mitigated this by piloting the screening and data extraction process and using experienced reviewers, and it is unlikely that any important studies were missed that would have altered the findings of the review.64 We conducted risk of bias assessments at the study level, rather than at the outcome level, and incorporated these into our GRADE assessments at the risk factor-outcome-population level. Given that our eligibility criteria narrowed inclusion to higher quality studies that were most applicable to the review objective, it is unlikely that our appraisals of the certainty of evidence would be substantially impacted. Nevertheless, an in-depth evaluation of the study quality at the outcome level may be worth undertaking if feasible in future work.
The evidence presented in this review should be interpreted as most applicable to people with COVID-19 symptoms or in general populations, but not necessarily to those with severe infections because studies focused solely on patients with severe COVID-19 (ie, in ICU settings) were excluded. Most studies of patients in the ICU setting that we located were relatively small and descriptive in nature, such that many would have been otherwise excluded, due to lack of adjustment, or only have been able to provide low or very low certainty evidence due to their lack of precision. Additionally, generalisations to other countries should be made with caution, as high-risk groups in these populations may differ.
Supplementary Material
Acknowledgments
We would like to thank the National Advisory Committee on Immunisation (NACI) High Consequence Infectious Disease Vaccine Working Group (Caroline Quach, Shelley Deeks, Yen Bui, Kathleen Dooling, Robyn Harrison, Kyla Hildebrand, Michelle Murti, Jesse Papenburg, Robert Pless, Nathan Stall, and Stephen Vaughan) for their contributions to the project. We also thank Liz Dennett (MLIS) for conducting the Medline search, and Karyn Crawford for assisting with article retrieval.
Footnotes
Contributors: AW, JP, AB, BV and LH contributed to the conception and design of the study. AW, JP, SG, SR, AB and BV contributed to the screening of eligible studies. AW, SG, SR and AB contributed to the acquisition of data. AW, JP, MG, BV and LH contributed to the synthesis and interpretation of data. AW, JP and MG drafted the manuscript. AW, JP, MG, SG, SR, AB, BV and LH revised the manuscript for important intellectual content. All authors approved the manuscript for submission.
Funding: National Advisory Committee on Immunisation (Canada); contract No. 4600001536.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: grants from the National Advisory Committee for Immunisation during the conduct of the study; no other relationships or activities that could appear to have influenced the submitted work. LH is supported by a Canada Research Chair in Knowledge Synthesis and Translation.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information. No additional data available; all data used in this review are available within the manuscript and accompanying online supplemental files.
References
- 1.World Health Organization . Naming the coronavirus disease (COVID-19) and the virus that causes it, 2020. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it [Accessed 31 Jul 2020].
- 2.World Health Organization . Coronavirus disease 2019 (COVID-19): situation report - 51. Geneva, Switzerland: World Health Organization, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf [Google Scholar]
- 3.World Health Organization . Coronavirus disease 2019 (COVID-19): weekly epidemiological update 17. Geneva, Switzerland: World Health Organization, 2020. https://www.who.int/publications/m/item/weekly-epidemiological-update-8-december-2020 [Google Scholar]
- 4.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis 2020;34:101623. 10.1016/j.tmaid.2020.101623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Government of Canada . Coronavirus disease 2019 (COVID-19): epidemiology update. Ottawa, Canada: Government of Canada, 2020. https://health-infobase.canada.ca/src/data/covidLive/Epidemiological-summary-of-COVID-19-cases-in-Canada-Canada.ca.pdf [Google Scholar]
- 6.World Health Organization . Accelerating a safe and effective COVID-19 vaccine. Geneva, Switzerland: World Health Organization, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/accelerating-a-safe-and-effective-covid-19-vaccine [Google Scholar]
- 7.Health Canada . Statement on UK’s authorization of its first COVID-19 vaccine, manufactured by Pfizer/BioNTech. Ottawa, Canada: Health Canada, 2020. https://www.canada.ca/en/health-canada/news/2020/12/statement-on-uks-authorization-of-its-first-covid-19-vaccine-manufactured-by-pfizerbiontech.html [Google Scholar]
- 8.Health Canada . Vaccines and treatments for COVID-19: progress. Ottawa, Canada: Health Canada, 2020. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks/covid-19-vaccine-treatment.html [Google Scholar]
- 9.World Health Organization . Draft landscape of COVID-19 candidate vaccines. Geneva, Switzerland: World Health Organization, 2020. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines [Google Scholar]
- 10.Thanh Le T, Andreadakis Z, Kumar A, et al. The COVID-19 vaccine development landscape. Nat Rev Drug Discov 2020;19:305–6. 10.1038/d41573-020-00073-5 [DOI] [PubMed] [Google Scholar]
- 11.Government of Canada . Research priorities for COVID-19 vaccines to support public health decisions. Ottawa, Canada: Government of Canada, 2020. https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/research-priorities-covid-19-vaccines.html [Google Scholar]
- 12.Government of Canada . National Advisory Committee on immunization (NACI): membership and representation. Ottawa, Canada: Government of Canada, 2020. https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/naci-membership-representation.html [Google Scholar]
- 13.Ismail SJ, Hardy K, Tunis MC, et al. A framework for the systematic consideration of ethics, equity, feasibility, and acceptability in vaccine program recommendations. Vaccine 2020;38:5861–76. 10.1016/j.vaccine.2020.05.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Evans T, Brown H. Road traffic crashes: operationalizing equity in the context of health sector reform. Inj Control Saf Promot 2003;10:11–12. 10.1076/icsp.10.1.11.14117 [DOI] [PubMed] [Google Scholar]
- 15.Ismail SJ, Tunis MC, Zhao L. Navigating inequities: a roadmap out of the pandemic. BMJ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamel C, Michaud A, Thuku M, et al. Defining rapid reviews: a systematic scoping review and thematic analysis of definitions and defining characteristics of rapid reviews. J Clin Epidemiol 2021;129:74–85. 10.1016/j.jclinepi.2020.09.041 [DOI] [PubMed] [Google Scholar]
- 17.Hartling L, Guise J-M, Kato E, et al. A taxonomy of rapid reviews links report types and methods to specific decision-making contexts. J Clin Epidemiol 2015;68:1451–62. 10.1016/j.jclinepi.2015.05.036 [DOI] [PubMed] [Google Scholar]
- 18.Tricco AC, Langlois EV, Straus SE, . Rapid reviews to strengthen health policy and systems: a practical guide. Geneva, Switzerland: World Health Organization, 2017. [Google Scholar]
- 19.Higgins J, Thomas J, Chandler J. Cochrane handbook for systematic reviews of interventions. 2nd Edition. Chinchester, UK: John Wiley & Sons, 2019. [Google Scholar]
- 20.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Organisation for Economic Cooperation and Development . Member countries, 2020. Available: https://www.oecd.org/about/members-and-partners/ [Accessed 24 Aug 2020].
- 22.Fraser Institute . Comparing performance of universal health care countries, 2019. Available: https://www.fraserinstitute.org/studies/comparing-performance-of-universal-health-care-countries-2019 [Accessed 24 Aug 2020].
- 23.O’Neill J, Tabish H, Welch V, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol 2014;67:56–64. 10.1016/j.jclinepi.2013.08.005 [DOI] [PubMed] [Google Scholar]
- 24.Oliver S, Kavanagh J, Caird J. Health promotion, inequalities and young people’s health: a systematic review of research. London, UK: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London, 2008. [Google Scholar]
- 25.Guyatt GH, Oxman AD, Sultan S, et al. GRADE guidelines: 9. Rating up the quality of evidence. J Clin Epidemiol 2011;64:1311–6. 10.1016/j.jclinepi.2011.06.004 [DOI] [PubMed] [Google Scholar]
- 26.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–94. 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 27.Murad MH, Mustafa RA, Schünemann HJ, et al. Rating the certainty in evidence in the absence of a single estimate of effect. Evid Based Med 2017;22:85–7. 10.1136/ebmed-2017-110668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iorio A, Spencer FA, Falavigna M, et al. Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. BMJ 2015;350:h870. 10.1136/bmj.h870 [DOI] [PubMed] [Google Scholar]
- 29.Santesso N, Glenton C, Dahm P, et al. GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. J Clin Epidemiol 2020;119:126–35. 10.1016/j.jclinepi.2019.10.014 [DOI] [PubMed] [Google Scholar]
- 30.Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff 2020;39:1253–62. 10.1377/hlthaff.2020.00598 [DOI] [PubMed] [Google Scholar]
- 31.Bhargava A, Fukushima EA, Levine M. Predictors for severe COVID-19 infection. Clin Infect Dis 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bianchetti A, Rozzini R, Guerini F, et al. Clinical presentation of COVID19 in dementia patients. J Nutr Health Aging 2020;24:560–2. 10.1007/s12603-020-1389-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borobia A, Carcas A, Arnalich F, et al. A cohort of patients with COVID-19 in a major teaching hospital in Europe. J Clin Med 2020;9:1733. 10.3390/jcm9061733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Busetto L, Bettini S, Fabris R, et al. Obesity and COVID-19: an Italian snapshot. Obesity 2020;28:1600–5. 10.1002/oby.22918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cecconi M, Piovani D, Brunetta E, et al. Early predictors of clinical deterioration in a cohort of 239 patients hospitalized for COVID-19 infection in Lombardy, Italy. J Clin Med 2020;9:1548. 10.3390/jcm9051548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colaneri M, Sacchi P, Zuccaro V, et al. Clinical characteristics of coronavirus disease (COVID-19) early findings from a teaching hospital in Pavia, North Italy, 21 to 28 February 2020. Euro Surveill 2020;25. 10.2807/1560-7917.ES.2020.25.16.2000460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Covino M, De Matteis G, Santoro M. Clinical characteristics and prognostic factors in COVID-19 patients aged >=80 years. Geriat Gerontol Int 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cummings MJ, Baldwin MR, Abrams D. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.D'Silva KM, Serling-Boyd N, Wallwork R, et al. Clinical characteristics and outcomes of patients with coronavirus disease 2019 (COVID-19) and rheumatic disease: a comparative cohort study from a US ‘hot spot’. Ann Rheum Dis 2020;79:1156–62. 10.1136/annrheumdis-2020-217888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 2020;369:m1985. 10.1136/bmj.m1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.El‐Boghdadly K, Wong DJN, Owen R, et al. Risks to healthcare workers following tracheal intubation of patients with COVID‐19: a prospective international multicentre cohort study. Anaesthesia 2020;75:1437–47. 10.1111/anae.15170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Giacomelli A, Ridolfo AL, Milazzo L, et al. 30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: a prospective cohort study. Pharmacol Res 2020;158:104931. 10.1016/j.phrs.2020.104931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gold JAW, Wong KK, Szablewski CM, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 - Georgia, March 2020. MMWR Morb Mortal Wkly Rep 2020;69:545–50. 10.15585/mmwr.mm6918e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hajifathalian K, Krisko T, Mehta A. Gastrointestinal and hepatic manifestations of 2019 novel coronavirus disease in a large cohort of infected patients from New York: clinical implications. Gastroenterol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hajifathalian K, Kumar S, Newberry C, et al. Obesity is associated with worse outcomes in COVID-19: analysis of early data from New York City. Obesity 2020;28:1606–12. 10.1002/oby.22923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hamer M, Kivimäki M, Gale CR, et al. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK. Brain Behav Immun 2020;87:184–7. 10.1016/j.bbi.2020.05.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hur K, Price CPE, Gray EL. Factors associated with intubation and prolonged intubation in hospitalized patients with COVID-19. JAMA Otolaryngol Head Neck Surg 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Imam Z, Odish F, Gill I, et al. Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States. J Intern Med 2020;288:469–76. 10.1111/joim.13119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kalligeros M, Shehadeh F, Mylona EK, et al. Association of obesity with disease severity among patients with coronavirus disease 2019. Obesity 2020;28:1200–4. 10.1002/oby.22859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Klang E, Kassim G, Soffer S, et al. Severe obesity as an independent risk factor for COVID-19 mortality in hospitalized patients younger than 50. Obesity 2020;28:1595–9. 10.1002/oby.22913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lassale C, Gaye B, Hamer M. Ethnic disparities in hospitalisation for COVID-19 in England: the role of socioeconomic factors, mental health, and inflammatory and pro-inflammatory factors in a community-based cohort study. Brain Behav Immun 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Okoh AK, Sossou C, Dangayach NS, et al. Coronavirus disease 19 in minority populations of Newark, New Jersey. Int J Equity Health 2020;19:93. 10.1186/s12939-020-01208-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Palaiodimos L, Kokkinidis DG, Li W, et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism 2020;108:154262. 10.1016/j.metabol.2020.154262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Patel AP, Paranjpe MD, Kathiresan NP, et al. Race, socioeconomic deprivation, and hospitalization for COVID-19 in English participants of a national Biobank. Int J Equity Health 2020;19. 10.1186/s12939-020-01227-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Perez-Guzman PN, Daunt A, Mukherjee S. Report 17: clinical characteristics and predictors of outcomes of hospitalized patients with COVID-19 in a London NHS trust: a retrospective cohort study. London: Imperial College, 2020. [Google Scholar]
- 56.Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 2020;369:m1966. 10.1136/bmj.m1966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Piano S, Dalbeni A, Vettore E, et al. Abnormal liver function tests predict transfer to intensive care unit and death in COVID-19. Liver Int 2020;40:2394–406. 10.1111/liv.14565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Price-Haywood EG, Burton J, Fort D, et al. Hospitalization and mortality among black patients and white patients with COVID-19. NEJM 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shah V, Ko Ko T, Zuckerman M, et al. Poor outcome and prolonged persistence of SARS‐CoV‐2 RNA in COVID‐19 patients with haematological malignancies; King’s College Hospital experience. Br J Haematol 2020;190. 10.1111/bjh.16935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Singh S, Khan A. Clinical characteristics and outcomes of COVID-19 among patients with pre-existing liver disease in United States: a multi-center research network study. Gastroenterol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Singh S, Khan A, Chowdhry M, et al. Risk of severe coronavirus disease 2019 in patients with inflammatory bowel disease in the United States: a multicenter research network study. Gastroenterology 2020;159:1575–8. 10.1053/j.gastro.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Violi F, Cangemi R, Romiti GF, et al. Is albumin predictor of mortality in COVID-19? Antioxid Redox Signal 2020. 10.1089/ars.2020.8142 [DOI] [PubMed] [Google Scholar]
- 63.England PH. Disparities in the risk and outcomes of COVID-19. London, UK: Public Health England, 2020. [Google Scholar]
- 64.Waffenschmidt S, Knelangen M, Sieben W, et al. Single screening versus conventional double screening for study selection in systematic reviews: a methodological systematic review. BMC Med Res Methodol 2019;19:132. 10.1186/s12874-019-0782-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-044684supp001.pdf (1,017.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. No additional data available; all data used in this review are available within the manuscript and accompanying online supplemental files.