Abstract
Background
The COVID-19 pandemic and ensuing national lockdowns have dramatically changed the healthcare landscape. The pandemic’s impact on people with chronic obstructive pulmonary disease (COPD) remains poorly understood. We hypothesised that the UK-wide lockdown restrictions were associated with reductions in severe COPD exacerbations. We provide the first national level analyses of the impact of the COVID-19 pandemic and first lockdown on severe COPD exacerbations resulting in emergency hospital admissions and/or leading to death as well as those recorded in primary care or emergency departments.
Methods
Using data from Public Health Scotland and the Secure Anonymised Information Linkage Databank in Wales, we accessed weekly counts of emergency hospital admissions and deaths due to COPD over the first 30 weeks of 2020 and compared these to the national averages over the preceding 5 years. For both Scotland and Wales, we undertook interrupted time-series analyses to model the impact of instigating lockdown on these outcomes. Using fixed-effect meta-analysis, we derived pooled estimates of the overall changes in trends across the two nations.
Results
Lockdown was associated with 48% pooled reduction in emergency admissions for COPD in both countries (incidence rate ratio, IRR 0.52, 95% CI 0.46 to 0.58), relative to the 5-year averages. There was no statistically significant change in deaths due to COPD (pooled IRR 1.08, 95% CI 0.87 to 1.33). In Wales, lockdown was associated with 39% reduction in primary care consultations for acute exacerbation of COPD (IRR 0.61, 95% CI 0.52 to 0.71) and 46% reduction in COPD-related emergency department attendances (IRR 0.54, 95% CI 0.36 to 0.81).
Conclusions
The UK-wide lockdown was associated with the most substantial reductions in COPD exacerbations ever seen across Scotland and Wales, with no corresponding increase in COPD deaths. This may have resulted from reduced transmission of respiratory infections, reduced exposure to outdoor air pollution and/or improved COPD self-management.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-021-02000-w.
Keywords: Acute exacerbation of chronic obstructive pulmonary disease, COVID-19 lockdown
Background
The COVID-19 pandemic and subsequent challenges to healthcare systems have led to unprecedented disruptions of routine care for people with chronic conditions. In response to a surge in COVID-19 cases, the UK and devolved governments announced the first nationwide lockdown on 23rd March 2020, thereby severely restricting movements and social contacts [1]. The accompanying messages to avoid overwhelming the National Health Service (NHS) and fear of contracting SARS-CoV-2 in healthcare settings had an impact on people’s willingness to seek emergency care [2].
There is evidence that the UK-wide lockdown was associated with poorer cardiovascular [3] and cancer [4] outcomes, but its impact on serious chronic obstructive pulmonary disease (COPD) outcomes remains unclear.
Despite the disruption to routine COPD care [5, 6], the societal changes associated with lockdown—in particular, improvements in air quality and reductions in other viruses responsible for acute respiratory tract infections [7, 8]—may have led to an overall improvement in COPD outcomes. The available body of evidence suggests that there may have been a reduction in acute exacerbations of COPD (AECOPD), but these data are difficult to interpret because of methodological limitations including studying selective populations and/or from a limited number of centres [9–26]. Despite the changes in healthcare-seeking behaviour during the lockdown, people with severe AECOPD were still likely to seek medical attention as the symptoms are intense such that they are difficult to tolerate at home [12].
We sought to investigate the impact of the UK-wide COVID-19 lockdown on the overall numbers of recorded severe AECOPDs leading to admission and/or death across the entire populations of Scotland and Wales. To contextualise the findings, we also investigate AECOPDs that were recorded in primary care and emergency departments (EDs) in Wales.
Methods
Data sources, populations and case definitions
The study was based on the entire populations of Scotland and Wales (the 2019 mid-year population estimates were 5,463,300 and 3,152,900, respectively). We accessed complete coverage person-level datasets from Public Health Scotland (PHS) [27] and the Secure Anonymised Information Linkage (SAIL) Databank [28] in Wales. PHS receives individual-level data from all general or acute specialties in NHS hospitals in Scotland. The SAIL Databank receives linkable, routinely collected data from all NHS hospitals in Wales and 80% of general practices as well as other healthcare and administrative data.
We defined two primary outcome measures relating to severe COPD exacerbations: COPD-related emergency hospital admission, and death due to COPD. Emergency admissions for COPD were defined as those with a primary diagnosis of COPD recorded using the J43 and J44 codes of the 10th revision of the International Statistical Classification of Diseases (ICD-10). These data were extracted from the Scottish Morbidity Record 01 (SMR01) and the Patient Episodes Database for Wales (PEDW), both of which undergo regular data quality checks [29, 30]. In Wales, we also extracted the average length of stay (LOS) of COPD admissions.
Deaths due to COPD were defined as those with COPD (ICD-10 codes of J43 and J44) as the underlying cause of death in the National Records of Scotland (NRS) deaths database or the Annual District Death Extract (ADDE) in SAIL. Mortality data were regularly checked and validated by the UK Office for National Statistics (ONS) [31–33].
In Wales, we also had access to primary care and ED data. We defined COPD-related ED attendances as those with a COPD code (14B) as the primary diagnosis in the Emergency Department Dataset (EDDS) in SAIL. We defined a general practitioner-recorded AECOPD from the Welsh Longitudinal General Practice (WLGP) dataset in SAIL as an AECOPD code preceded by a COPD diagnosis code. The code sets are included in the supplementary information.
Statistical analyses
We visualised the trends of the aforementioned outcomes for the first 30 calendar weeks in 2020 and corresponding national averages for the preceding 5 years. To investigate the impact of the UK lockdown on these outcomes, we undertook interrupted time series analyses with a single change point of the 23rd of March (week 13). We modelled the trends in the first 30 calendar weeks in 2020 and the corresponding 5-year averages (2015–2019) using Poisson generalised linear regression in R 4.0.3. The initial change point model in both the baseline period and 2020 had a pre-lockdown slope and intercept as well as an instantaneous change in intercept at the week of lockdown and a change in slope following lockdown. In the baseline period, we were anticipating no change in intercept and no change in slope at week 13. The final model was based upon the baseline and 2020 data and included a binary variable to differentiate the two periods, together with interaction terms for the slopes and instantaneous effects of lockdown. These interaction terms were used to compare the slopes prior to lockdown in the baseline period with 2020, to compare the instantaneous change in intercept at lockdown in baseline with 2020 and to compare the change in slope post-lockdown in baseline with 2020. Residual plots were used to check the linearity assumption, and the Breusch-Godfrey test [34] was used to assess autocorrelation. Separate models were used in Scotland and Wales, and z tests were used to compare the model coefficients between the two countries. We then used fixed-effect meta-analysis to derive pooled estimates from their weighted averages.
In pre-specified sensitivity analyses, we restricted the definition of the study outcomes in Wales to people aged at least 35 years with a smoking history (current or former smokers) documented in the Welsh Longitudinal General Practice (WLGP) dataset. Linkage to the WLGP dataset was available within the SAIL Databank through the Anonymised Linkage Field (ALF) [35]. We excluded records with missing ALF field or low-quality linkage.
For COPD admissions in Wales, we compared length of stay over the weeks 13 to 30 between 2020 and the 5-year average using a separate Poisson model controlled for week number. We used beta regression to model the relationship between the year of admission and the proportion of COPD admissions during which patients died due to COPD in every week, with week number as a covariate.
Data analysis was performed in R 4.0.2.
Reporting guidelines
We followed the Framework for Enhanced Reporting of Interrupted Time Series (FERITS) [36] and the REporting of studies Conducted using Observational Routinely collected Data (RECORD) statement [37] in the reporting of this study (see the Supplementary Materials).
Role of the funding source
The funders had no role in the study design, data collection and analysis, interpretation of findings, writing of the manuscript, or the decision to submit this manuscript for publication.
Results
Emergency admissions
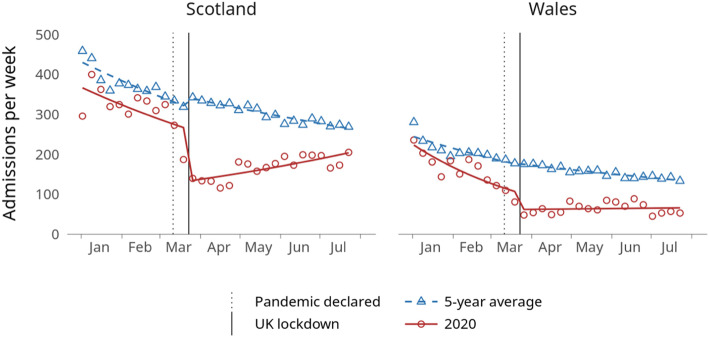
In the first 30 weeks of 2020, there were a total of 9847 emergency admissions for COPD in Scotland (6786) and Wales (3061). Those admissions were consistently lower than the averages of the corresponding periods in the preceding 5 years in both countries (Fig. 1).
Fig. 1.
Weekly count of emergency COPD admissions in Scotland and Wales in 2020 and the corresponding 5-year averages (2015–2019, points) in addition to modelled trend lines
In Scotland, the slope before lockdown in 2020 was decreasing (IRR 0.97, 95% CI 0.96 to 0.98), although there was no evidence that this slope differed from the 5-year average (IRR 1.00, 95% CI 0.98 to 1.01). Introducing lockdown in week 13 was associated with a reduction in admissions by 48% (IRR 0.52; 95% CI 0.47 to 0.58). This reduction was 52% greater than the average change at the same point in the preceding 5 years (IRR 0.48; 95% CI 0.42 to 0.55). The slope of admissions then gradually increased over the coming weeks (IRR 1.05, 95% CI 1.04 to 1.07), which was in contrast to the slope of the 5-year average which was decreasing (Fig. 1 and Table 1).
Table 1.
Poisson models of emergency COPD admissions in 2020 and the corresponding 5-year averages (2015-2019).
| Scotland | Wales | Pooled estimates | ||||
|---|---|---|---|---|---|---|
| IRR (95% CI) | p value | IRR (95% CI) | p value | IRR (95% CI) | p value | |
| Pre-lockdown intercept in 2020 compared to 5-year average | 0.83 (0.75, 0.91) | < 0.001 | 0.59 (0.51, 0.67) | < 0.001 | 0.74 (0.68, 0.80) | < 0.001 |
| Slope in weeks 1–12 | ||||||
| 5-year average | 0.97 (0.97, 0.98) | < 0.001 | 0.97 (0.96, 0.98) | < 0.001 | 0.97 (0.97, 0.98) | < 0.001 |
| 2020 | 0.97 (0.96, 0.98) | < 0.001 | 0.94 (0.92, 0.95) | < 0.001 | 0.96 (0.95, 0.97) | < 0.001 |
| 2020 relative to 5-year average | 1.00 (0.98, 1.01) | 0.686 | 0.96 (0.95, 0.98) | < 0.001 | 0.99 (0.98, 1.00) | 0.006 |
| Change in level at week 13 | ||||||
| 5-year average | 1.08 (1.00, 1.18) | 0.056 | 1.02 (0.92, 1.15) | 0.666 | 1.06 (0.99, 1.13) | 0.072 |
| 2020 | 0.52 (0.47, 0.58) | < 0.001 | 0.62 (0.53, 0.72) | < 0.001 | 0.55 (0.50, 0.60) | < 0.001 |
| 2020 relative to 5-year average | 0.48 (0.42, 0.55) | < 0.001 | 0.60 (0.50, 0.73) | < 0.001 | 0.52 (0.46, 0.58) | < 0.001 |
| Change in slope after week 13 | ||||||
| 5-year average | 1.01 (1.00, 1.02) | 0.023 | 1.01 (1.00, 1.03) | 0.034 | 1.01 (1.00, 1.02) | 0.002 |
| 2020 | 1.05 (1.04, 1.07) | < 0.001 | 1.07 (1.05, 1.09) | < 0.001 | 1.06 (1.05, 1.07) | < 0.001 |
| 2020 relative to 5-year average | 1.04 (1.03, 1.06) | < 0.001 | 1.06 (1.03, 1.08) | < 0.001 | 1.05 (1.03, 1.06) | < 0.001 |
In Wales, admissions in the first 12 weeks of 2020 were falling (IRR 0.94, 95% CI 0.92 to 0.95), slightly faster than the corresponding 5-year average (IRR 0.96, 95% CI 0.95 to 0.98). Introducing lockdown in week 13 was associated with a 38% reduction in admissions (IRR 0.62, 95% CI 0.53 to 0.72). This reduction was 40% greater than the average change at the same point in the preceding 5 years (IRR 0.60; 95% CI 0.50 to 0.73). Similar to the pattern seen in Scotland, there was a slight gradual increase in the slope of admissions over the ensuing weeks (IRR 1.07, 95% CI 1.05 to 1.09), which contrasted with the decreasing slope in the 5-year average (Fig. 1 and Table 1). Admissions for COPD were 22% shorter in 2020 during lockdown than in the corresponding periods in the preceding 5 years (IRR 0.78, 95% CI 0.78 to 0.79, p value < 0.001). However, there was no evidence that the proportion of COPD admissions during which patients died due to COPD in the weeks 13 to 30 was different in 2020 than the corresponding periods of the preceding 5 years (odds ratio 1.05, 95% CI 0.77 to 1.43, p value 0.756).
The estimated effects in Wales did not change significantly after restricting the analysis to those aged ≥ 35 years at admission with a smoking history (Table B, Additional file 1).
There was a 48% pooled reduction in admissions during lockdown across Scotland and Wales (IRR 0.52, 95% CI 0.46 to 0.58).
Deaths
There were a total of 2554 deaths with COPD as the underlying cause in Scotland (1535) and Wales (1019) in the first 30 weeks of 2020.
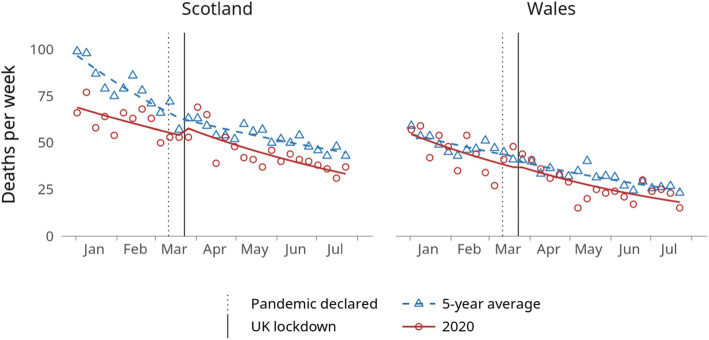
In 2020 before lockdown, the trend of deaths with COPD as the underlying cause was not significantly different from the 5-year average (Fig. 2). The slope of deaths during this period was falling slightly in both nations (Scotland: IRR 0.98, 95 %CI 0.96 to 1.00; Wales: IRR 0.97, 95% CI 0.94 to 0.99, Table 2), as it did in the corresponding 5-year average.
Fig. 2.
Weekly count of deaths with COPD as the underlying cause in Scotland and Wales in 2020 and the corresponding 5-year averages (2015–2019, points) in addition to modelled trend lines
Table 2.
Poisson models of deaths with COPD as the underlying cause in 2020 and the corresponding 5-year averages (2015–2019).
| Scotland | Wales | Pooled estimates | ||||
|---|---|---|---|---|---|---|
| IRR (95% CI) | p value | IRR (95% CI) | p value | IRR (95% CI) | p value | |
| Pre-lockdown intercept in 2020 compared to 5-year average | 0.87 (0.70, 1.08) | 0.206 | 0.85 (0.66, 1.11) | 0.234 | 0.86 (0.73, 1.02) | 0.083 |
| Slope in weeks 1–12 | ||||||
| 5-year average | 0.96 (0.94, 0.98) | < 0.001 | 0.98 (0.96, 1.00) | 0.063 | 0.97 (0.95, 0.98) | < 0.001 |
| 2020 | 0.98 (0.96, 1.00) | 0.042 | 0.97 (0.94, 0.99) | 0.004 | 0.97 (0.96, 0.99) | 0.001 |
| 2020 relative to 5-year average | 1.02 (0.99, 1.05) | 0.240 | 0.99 (0.95, 1.02) | 0.446 | 1.00 (0.98, 1.03) | 0.673 |
| Change in level at week 13 | ||||||
| 5-year average | 1.02 (0.84, 1.22) | 0.869 | 0.95 (0.75, 1.20) | 0.657 | 0.99 (0.86, 1.14) | 0.883 |
| 2020 | 1.09 (0.89, 1.33) | 0.417 | 1.03 (0.81, 1.32) | 0.803 | 1.06 (0.91, 1.24) | 0.432 |
| 2020 relative to 5-year average | 1.07 (0.81, 1.41) | 0.627 | 1.09 (0.78, 1.53) | 0.627 | 1.08 (0.87, 1.33) | 0.494 |
| Change in slope after week 13 | ||||||
| 5-year average | 1.02 (1.00, 1.04) | 0.084 | 0.99 (0.97, 1.02) | 0.687 | 1.01 (0.99, 1.03) | 0.266 |
| 2020 | 0.99 (0.97, 1.01) | 0.411 | 0.99 (0.96, 1.02) | 0.699 | 0.99 (0.97, 1.01) | 0.379 |
| 2020 relative to 5-year average | 0.97 (0.94, 1.00) | 0.078 | 1.00 (0.96, 1.04) | 0.997 | 0.98 (0.96, 1.01) | 0.169 |
There was no statistically significant change in deaths following the introduction of lockdown at week 13 of 2020 nor at the same point in the 5-year average in both nations (in Scotland, IRR in 2020 relative to 5-year average: 1.07, 95% CI 0.81 to 1.41; in Wales, IRR 1.09, 95% CI 0.78 to 1.53; pooled IRR: 1.08, 95% CI 0.87 to 1.33).
Deaths during the lockdown continued to fall, similar to the same period in the 5-year average (Fig. 2).
The estimated effects in Wales did not change after restricting the analysis to those with a smoking history who died at the age of ≥ 35 years (Table C, Additional file 1).
Primary care consultations
In Wales, there were 4575 primary care consultations for AECOPD in the first 30 weeks of 2020. Before lockdown, consultations were declining (IRR 0.93, 95% CI 0.92 to 0.94) in a steeper slope than the 5-year average (IRR 0.96, 95% CI 0.95 to 0.97, Table 3 and Fig. 3). Introducing lockdown was associated with a 39% instantaneous reduction in those consultations after adjusting for the 5-year averages (IRR 0.61, 95% CI 0.52 to 0.71). After week 13 of 2020, the slope continued to decline although it was less steep than the pre-lockdown slope (IRR for change in slope: 1.03, 95% CI 1.01 to 1.04). The estimated effects did not change after restricting the analysis to those with a smoking history who died at the age of ≥ 35 years (Table D, Additional file 1).
Table 3.
Poisson models of primary care consultations for acute exacerbations of COPD in Wales in 2020 and the corresponding 5-year averages (2015–2019)
| IRR (95% CI) | p value | |
|---|---|---|
| Pre-lockdown intercept in 2020 compared to 5-year average | 0.76 (0.68, 0.86) | < 0.001 |
| Slope in weeks 1–12 | ||
| 5-year average | 0.97 (0.96, 0.98) | < 0.001 |
| 2020 | 0.93 (0.92, 0.94) | < 0.001 |
| 2020 relative to 5-year average | 0.96 (0.95, 0.97) | < 0.001 |
| Change in level at week 13 | ||
| 5-year average | 1.05 (0.95, 1.16) | 0.322 |
| 2020 | 0.64 (0.56, 0.72) | < 0.001 |
| 2020 relative to 5-year average | 0.61 (0.52, 0.71) | < 0.001 |
| Change in slope after week 13 | ||
| 5-year average | 1.01 (1.00, 1.02) | 0.043 |
| 2020 | 1.03 (1.01, 1.04) | < 0.001 |
| 2020 relative to 5-year average | 1.01 (1.00, 1.03) | 0.147 |
Fig. 3.
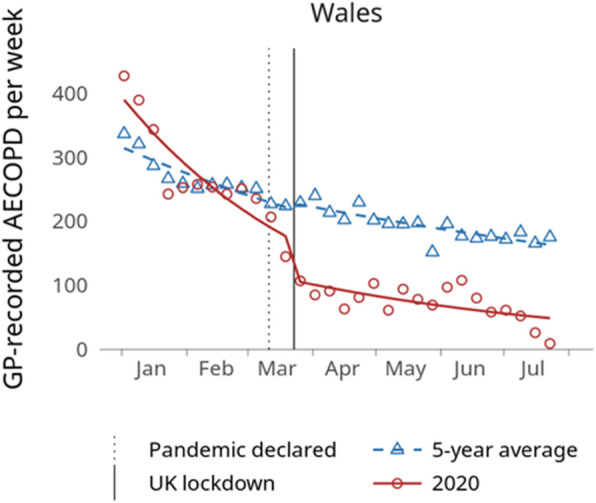
Weekly count of primary care consultations for acute exacerbation of COPD in Wales in 2020 and the corresponding 5-year averages (2015–2019, points) in addition to modelled trend lines
Emergency department attendances
In Wales, there were 625 COPD-related ED attendances in the first 30 weeks of 2020. These events were consistently lower in the weeks 1 to 30 in 2020 than in the same period of the preceding 5 years (Fig. 4). There was no clear trend before lockdown (IRR 0.97, 95% CI 0.94 to 1.01, Table 4), unlike the corresponding slope in the baseline period which was decreasing. Introducing lockdown was associated with a 46% fall in attendances compared with the 5-year averages (IRR 0.54, 95% CI 0.36 to 0.81). After week 13 of 2020, there was an upward slope (IRR for change in slope: 1.05, 95% CI 1.01 to 1.09), unlike the corresponding slope in the baseline period which continued to decrease. The estimated effects did not change after restricting the analysis to those with a smoking history who died at the age of ≥ 35 years (Table E, Additional file 1).
Fig. 4.
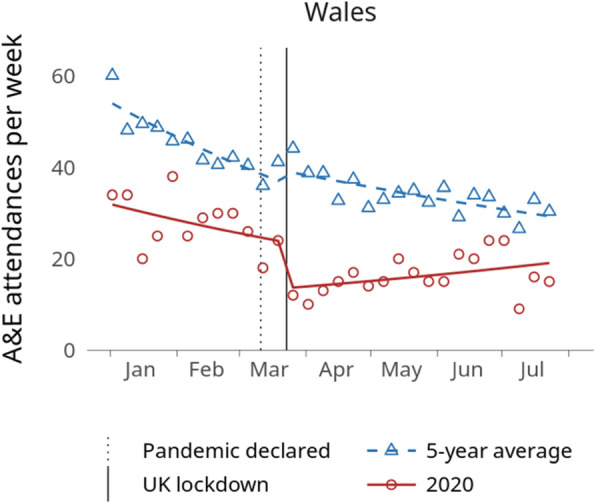
Weekly count of COPD-related emergency department attendances in Wales in 2020 and the corresponding 5-year averages (2015–2019, points) in addition to modelled trend lines
Table 4.
Poisson models of COPD-related emergency department attendances in Wales in 2020 and the corresponding 5-year averages (2015–2019)
| IRR (95% CI) | p value | |
|---|---|---|
| Pre-lockdown intercept in 2020 compared to 5-year average | 0.65 (0.48, 0.88) | 0.006 |
| Slope in weeks 1–12 | ||
| 5-year average | 0.97 (0.94, 0.99) | 0.006 |
| 2020 | 0.97 (0.94, 1.01) | 0.101 |
| 2020 relative to 5-year average | 1.01 (0.97, 1.05) | 0.686 |
| Change in level at week 13 | ||
| 5-year average | 1.08 (0.85, 1.38) | 0.508 |
| 2020 | 0.59 (0.42, 0.82) | 0.002 |
| 2020 relative to 5-year average | 0.54 (0.36, 0.81) | 0.003 |
| Change in slope after week 13 | ||
| 5-year average | 1.02 (0.99, 1.05) | 0.227 |
| 2020 | 1.05 (1.01, 1.09) | 0.019 |
| 2020 relative to 5-year average | 1.03 (0.98, 1.08) | 0.256 |
Discussion
Our national level interrupted time-series analyses of the impact of lockdown across Scotland and Wales found substantial reductions in severe AECOPD leading to ED attendance and/or hospital admission as well as the less severe AECOPD that are recorded in primary care. The levels remained well below the corresponding 5-year averages throughout the study period. The easing of strict lockdown restrictions announced at the end of May 2020 [38, 39] did not lead to a substantial rebound in these events, but there was a gradual rise in ED attendances and admissions. There was no evidence of an increase in deaths due to COPD during the lockdown.
These findings are especially significant given that COPD exacerbations are one of the commonest reasons for emergency admission to hospital [40]. Reduced incidence of AECOPDs therefore increases healthcare capacity and resources available for those with COVID-19, as well as conferring obvious benefits to people with COPD. A reduction in AECOPD admissions is also particularly advantageous given the specific challenges in the hospital management of AECOPD during the pandemic—components of care, such as non-invasive ventilation (NIV), are associated with increased risk of viral transmission due to aerosolization [41] and can therefore only be delivered in specified clinical areas.
To the best of our knowledge, this is the first national level analysis of the impact of the COVID-19 lockdown on AECOPD incidence and mortality, using data across primary and secondary care as well as data on deaths. We used population-based data with high-to-complete geographical coverage across Scotland and Wales, which enabled comparison of findings between the two UK nations, which were broadly comparable.
Our study has some limitations. Firstly, there are no validated case definitions for COPD admissions or deaths in UK data, and so the case definitions used may have variable accuracy. We did not include deaths with COPD as a contributing cause because they would not have been specific enough for the purpose of this study. Data on AECOPD in primary care and ED data is under-recorded [42, 43]. However, our sensitivity analysis, limiting data to those aged ≥ 35 and ever-smokers, did not impact our overall results. Further, given that we were interested in trends over time rather than absolute numbers and that coding practices of these events are unlikely to have changed, this is unlikely to have significantly affected our findings.
The observed reduction in AECOPDs during lockdown does not necessarily imply direct causal effects of lockdown. Nonetheless, they are likely to have been mediated by reductions in the transmission of other respiratory pathogens and outdoor air pollution during lockdown [7, 8, 14], both of which have a major role in triggering AECOPD [44]. These factors could also have mediated the reductions in emergency admissions for asthma that have been reported following lockdowns [45–48].
A number of potential confounding factors such as changes in prescribing for COPD [49], behavioural changes related to improved self-management and smoking reduction/cessation [50], and possibly improved air quality [7] during the first wave of pandemic might have contributed to the observed reduction in AECOPDs. However, we were not in a position to adjust for these potential sources of bias. Care therefore needs to be taken when interpreting our findings. Furthermore, national messaging on the need to avoid overwhelming the NHS and the fear about the spread of SARS-CoV-2 might have contributed to the fall in AECOPD-related ED attendances and admissions during the first wave of the pandemic. However, this effect on healthcare-seeking behaviour is likely limited in those experiencing a severe AECOPD, which usually requires hospital assessment and treatment. In addition, the corresponding decline in AECOPD in primary care records suggests a true decline in incidence during lockdown. However, it is possible that the milder forms of AECOPDs have been self-managed by patients and were not presented to the health care system during lockdown.
The lifting of restrictions on travel and social contact was associated with a gradual rise in emergency admissions for AECOPD seen in our data for Scotland and Wales. This could be partly due to an increase in the circulation of respiratory viruses (mainly rhinoviruses initially) [8] and levels of outdoor air pollutants [51]. However, this could also be explained by an increasing threshold of hospital admission, since primary care consultations for AECOPD continued to fall towards summer in accordance with the typical seasonal trend of AECOPD in the UK [52].
Although there is extensive literature on COPD as a risk factor for COVID-19 severe outcomes and deaths [53–55], there is currently limited data examining how the pandemic, and specifically lockdowns, has affected COPD deaths more widely. Two studies from Hong Kong and England reported no difference in inpatient mortality during admissions for COPD exacerbation [13, 15]. Analysis of excess mortality from specific conditions is important in understanding whether reductions in emergency healthcare utilisation represent a true reduction in incidence or avoidance of healthcare settings, the latter of which could lead to increased mortality. Our study has shown no significant increase in non-COVID COPD deaths over the first 30 weeks of 2020. This is in contrast to a recent analysis of cardiovascular mortality in England and Wales [3], which demonstrated excess non-COVID acute cardiovascular deaths. The authors suggested that people with these diagnoses either did not seek help for their illness or were not referred to hospital, consistent with the greatest proportional increase in cardiovascular deaths occurring in community settings. Data from England from March to September 2020 from the Office for National Statistics shows that COVID-19 accounted for over 90% of excess deaths among those aged over 75 from both sexes, but the proportion of non-COVID excess deaths was higher across younger people [56]. The leading causes of these non-COVID excess deaths were dementia, ischaemic heart disease, cerebrovascular disease and other circulatory diseases. Deaths in England due to “chronic lower respiratory diseases” (ICD-10 codes J40-47) including COPD actually fell compared to expected levels when assessed cumulatively from March to September 2020 [56], consistent with our findings in Scotland and Wales.
There are several important areas for future investigation to understand underlying reasons for our findings. These include person-level analyses of how factors related to COPD, such as disease severity, control and health service utilisation and positive drivers such as reduced exposure to respiratory pathogens and pollutants, improved self-management, smoking cessation and other behavioural changes, might have affected the risk of AECOPD and related death during lockdown. If further work suggests that altered outdoor air pollution levels have played a significant role, findings should spur increased drive to improve air quality longer term [57]. Other interventions with the potential to produce lasting reductions in the rate of severe AECOPD include the facilitation of self-management of chronic conditions and the consolidation of public health messages to reduce the transmission of respiratory infections, including hand hygiene, use of facemasks and wider deployment of testing and isolation when viruses are most likely to be circulating.
Conclusions
We found significant declines in AECOPDs across primary and secondary care in Scotland and Wales during the initial UK-wide lockdown in 2020, with no associated increase in non-COVID deaths due to COPD. Our study strengthens the notion that outcomes relating to chronic respiratory disease improved during the lockdown period. It is crucial to assess the fuller impact of the pandemic on care and outcomes in chronic health conditions such as COPD, including non-COVID related morbidity and mortality. This will inform the targeting of public health strategy to minimise any adverse effects as well as capture any positive elements that could be harnessed to reduce hospital admissions in vulnerable groups over the longer term.
Supplementary Information
Additional file 1. Includes Read codes for COPD diagnosis, acute exacerbation of COPD, and smoking status used for sensitivity analysis, model diagnostics (Table A), the results of the sensitivity analysis (Tables B, C, D, and E), and the reporting checklists (FERITS, STROBE, RECORD).
Acknowledgements
This study made use of anonymised data held at PHS and the SAIL Databank. We would like to acknowledge all the data providers who make anonymised data available for research.
EAVE II Collaborators
Colin R Simpson, Wellington School of Health, Faculty of Health, Victoria University of Wellington, Wellington, New Zealand and Usher Institute, The University of Edinburgh, Edinburgh, UK
Jim McMenamin, Public Health Scotland, Glasgow, UK
Lewis D Ritchie, Centre of Academic Primary Care, University of Aberdeen, Aberdeen, UK
Mark Woolhouse, Usher Institute, The University of Edinburgh, Edinburgh, UK
Helen R Stagg, Usher Institute, The University of Edinburgh, Edinburgh, UK
Diogo Marques, Public Health Scotland, Glasgow, UK
Josie Murray, Public Health Scotland, Glasgow, UK
Sarah Stock, Usher Institute, The University of Edinburgh, Edinburgh, UK
Rachael Wood, Public Health Scotland and University of Edinburgh, UK
Colin McCowan, School of Medicine, University of St Andrews, St Andrews, UK
Utkarsh Agrawal, School of Medicine, University of St Andrews, St Andrews, UK
Annemarie B. Docherty, Usher Institute, The University of Edinburgh, Edinburgh, UK
Rachel H. Mulholland, Usher Institute, The University of Edinburgh, Edinburgh, UK
Emily Moore, Public Health Scotland, Glasgow, UK
James Marple, Royal Infirmary of Edinburgh, Edinburgh, UK
Vicky Hammersley, Usher Institute, The University of Edinburgh, Edinburgh, UK
Abbreviations
- ADDE
Annual District Death Extract
- AECOPD
Acute exacerbation of chronic obstructive pulmonary disease
- ALF
Anonymous Linking Field
- CI
Confidence interval
- COPD
Chronic obstructive pulmonary disease
- COVID-19
Coronavirus disease 2019
- ED
Emergency department
- EDDS
Emergency Department Dataset
- FERITS
Framework for Enhanced Reporting of Interrupted Time Series
- ICD
International Statistical Classification of Diseases
- IRR
Incidence rate ratio
- LOS
Length of stay
- NHS
National Health Service
- NIV
Non-invasive ventilation
- NRS
National Records of Scotland
- ONS
Office for National Statistics
- PEDW
Patient Episode Database for Wales
- PHS
Public Health Scotland
- RECORD
REporting of studies Conducted using Observational Routinely-collected Data
- SAIL
Secure Anonymised Information Linkage
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- SMR
Scottish Morbidity Records
- UK
United Kingdom
- WLGP
Welsh Longitudinal General Practice
Authors’ contributions
AS conceived this analysis, oversaw the work, and critically commented on the draft manuscript. MA analysed the data from Wales, prepared the tables and figures, and drafted the manuscript with SS. SK analysed the data from Scotland and commented on the draft analysis. CR oversaw the statistical analysis and commented on the draft manuscript. EV supported the analyses and critically reviewed the manuscript. RAL critically commented on the study design as it developed and the draft manuscript. GAD oversaw the work and critically commented on the draft manuscript. All authors critically reviewed and approved the final version of the manuscript.
Funding
This study was funded by the Medical Research Council (MR/R008345/1) with the support of BREATHE – The Health Data Research Hub for Respiratory Health [MC_PC_19004], which is funded through the UK Research and Innovation Industrial Strategy Challenge Fund and delivered through Health Data Research UK. The funders had no role in the design of the study, collection, analysis, and interpretation of data, or in writing the manuscript.
Availability of data and materials
The anonymised person-level data supporting the conclusions of this article are held by Public Health Scotland (https://publichealthscotland.scot/) and the SAIL Databank (https://saildatabank.com/) and are restricted and not publicly available but can be accessed upon reasonable requests and with permission from PHS and SAIL. All proposals to use SAIL are carefully reviewed by an independent Information Governance Review Panel (IGRP) to ensure proper and appropriate use of data (https://www.saildatabank.com/application-process). When approved, access is then provided through the SAIL Gateway, a privacy-protecting safe haven and a secure remote access system.
Declarations
Ethics approval and consent to participate
We were granted permissions from the Public Benefit and Privacy Panel for Health and Social Care (HSC-PBPP) of Public Health Scotland and SAIL’s independent Information Governance Review Panel to conduct this study. Ethical review was not required as only anonymised data were used.
Consent for publication
Not applicable.
Competing interests
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: funding from UK Research and Innovation (AS), Medical Research Council (CR), Health Data Research UK (RAL), and Public Health Scotland (CR) during the conduct of the study; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities that could appear to have influenced the submitted work.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mohammad A. Alsallakh and Shanya Sivakumaran contributed equally as first authors.
Contributor Information
Mohammad A. Alsallakh, Email: m.a.alsallakh@swansea.ac.uk
on behalf of the EAVE II Collaborators:
Colin R. Simpson, Jim McMenamin, Lewis D. Ritchie, Mark Woolhouse, Helen R. Stagg, Diogo Marques, Josie Murray, Sarah Stock, Rachael Wood, Colin McCowan, Utkarsh Agrawal, Annemarie B. Docherty, Rachel H. Mulholland, Emily Moore, James Marple, and Vicky Hammersley
References
- 1.Prime Minister’s statement on coronavirus (COVID-19): 23 March 2020 - GOV.UK. https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020. Accessed 20 Nov 2020.
- 2.Mulholland RH, Wood R, Stagg HR, Fischbacher C, Villacampa J, Simpson CR, Vasileiou E, McCowan C, Stock SJ, Docherty AB, Ritchie LD, Agrawal U, Robertson C, Murray JLK, MacKenzie F, Sheikh A. Impact of COVID-19 on accident and emergency attendances and emergency and planned hospital admissions in Scotland: an interrupted time-series analysis. J R Soc Med. 2020;113(11):444–453. doi: 10.1177/0141076820962447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu J, Mamas MA, Mohamed MO, Kwok CS, Roebuck C, Humberstone B, et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2020;107:heartjnl-2020-317912. 10.1136/heartjnl-2020-317912. [DOI] [PubMed]
- 4.Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, Rachet B, Aggarwal A. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Houchen-Wolloff L, Steiner MC. Pulmonary rehabilitation at a time of social distancing: Prime time for tele-rehabilitation? Thorax. 2020;75(6):446–447. doi: 10.1136/thoraxjnl-2020-214788. [DOI] [PubMed] [Google Scholar]
- 6.Philip K, Cumella A, Farrington-Douglas J, Laffan M, Hopkinson N. Respiratory patient experience of measures to reduce risk of COVID-19: Findings from a descriptive cross-sectional UK wide survey. BMJ Open. 2020;10(9):40951. doi: 10.1136/bmjopen-2020-040951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higham JE, Ramírez CA, Green MA, Morse AP. UK COVID-19 lockdown: 100 days of air pollution reduction? Air Qual Atmos Heal. 2020;1:8. doi: 10.1007/s11869-020-00937-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Public Health England National Influenza Report, 17 September 2020 - Week 38 report. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/918708/National_influence_report_17_September_2020_week_38.pdf. Accessed 4 Nov 2020.
- 9.Berghaus TM, Karschnia P, Haberl S, Schwaiblmair M. Disproportionate decline in admissions for exacerbated COPD during the COVID-19 pandemic. Respir Med. 2020:106120. 10.1016/j.rmed.2020.106120. [DOI] [PMC free article] [PubMed]
- 10.Slagman A, Behringer W, Greiner F, Klein M, Weismann D, Erdmann B, Pigorsch M, Möckel M. Medical emergencies during the COVID-19 pandemic—an analysis of emergency department data in Germany. Dtsch Aerztebl Online. 2020;117:545–552. doi: 10.3238/arztebl.2020.0545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giamello JD, Abram S, Bernardi S, Lauria G. The emergency department in the COVID-19 era. Who are we missing? Eur J Emergency Med. 2020:305–6. 10.1097/MEJ.0000000000000718. [DOI] [PMC free article] [PubMed]
- 12.Baeza-Martínez C, Zamora-Molina L, Olea-Soto J, Soler-Sempere MJ, García-Pachón E. Reduction in hospital admissions for COPD exacerbation during the Covid-19 pandemic. Open Respir Arch. 2020;2(3):201–202. doi: 10.1016/j.opresp.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan KPF, Ma TF, Kwok WC, Leung JKC, Chiang KY, Ho JCM, Lam DCL, Tam TCC, Ip MSM, Ho PL. Significant reduction in hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in Hong Kong during coronavirus disease 2019 pandemic. Respir Med. 2020;171:106085. doi: 10.1016/j.rmed.2020.106085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tan JY, Conceicao EP, Wee LE, Sim XYJ, Venkatachalam I. COVID-19 public health measures: a reduction in hospital admissions for COPD exacerbations. Thorax. 2021;76:512–3. [DOI] [PubMed]
- 15.Sykes DL, Faruqi S, Holdsworth L, Crooks MG. Impact of COVID-19 on COPD and asthma admissions, and the pandemic from a patient’s perspective. ERJ Open Res. 2021;7(1):00822–02020. doi: 10.1183/23120541.00822-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu W, Dong M, Xiong M, Zhao D, Zhao Y, Wang M, Wang T, Liu Z, Lu L, Hu K. Clinical courses and outcomes of patients with chronic obstructive pulmonary disease during the COVID-19 epidemic in Hubei, China. Int J Chron Obstruct Pulmon Dis. 2020;15:2237–2248. doi: 10.2147/COPD.S265004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pleguezuelos E, Del Carmen A, Moreno E, Ortega P, Vila X, Ovejero L, et al. The experience of COPD patients in lockdown due to the COVID-19 pandemic. Int J Chron Obstruct Pulmon Dis. 2020;15:2621–2627. doi: 10.2147/COPD.S268421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baum A, Schwartz MD. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324(1):96–99. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff. 2020;39(11):2010–2017. doi: 10.1377/hlthaff.2020.00980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang Y, Chang C, Chen Y, Dong F, Zhang L, Sun Y. Symptoms, management and healthcare utilization of COPD patients during the COVID-19 epidemic in Beijing. Int J Chron Obstruct Pulmon Dis. 2020;15:2487–2494. doi: 10.2147/COPD.S270448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helgeland J, Telle KE, Grøsland M, Huseby BM, Håberg S, Lindman ASE. Admissions to Norwegian hospitals during the COVID-19 pandemic. Scand J Public Health. 2021:140349482110008. 10.1177/14034948211000813. [DOI] [PubMed]
- 22.Faria N, Costa MI, Gomes J, Sucena M. Reduction of severe exacerbations of COPD during COVID-19 pandemic in Portugal: a protective role of face masks? J Chronic Obstr Pulm Dis. 2021;1:9. doi: 10.1080/15412555.2021.1904387. [DOI] [PubMed] [Google Scholar]
- 23.Kyriakopoulos C, Gogali A, Exarchos K, Potonos D, Tatsis K, Apollonatou V, et al. Reduction in hospitalizations for respiratory diseases during the first COVID-19 wave in Greece. Respiration. 2021:1–6. 10.1159/000515323. [DOI] [PMC free article] [PubMed]
- 24.Jaehn P, Holmberg C, Uhlenbrock G, Pohl A, Finkenzeller T, Pawlik MT, Quack I, Ernstberger A, Rockmann F, Schreyer AG. Differential trends of admissions in accident and emergency departments during the COVID-19 pandemic in Germany. BMC Emerg Med. 2021;21(1):42. doi: 10.1186/s12873-021-00436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huh K, Kim Y-E, Ji W, Kim DW, Lee E-J, Kim J-H, et al. Decrease in hospital admissions for respiratory diseases during the COVID-19 pandemic: a nationwide claims study. Thorax. 2021:thoraxjnl-2020-216526. 10.1136/thoraxjnl-2020-216526. [DOI] [PubMed]
- 26.González J, Moncusí-Moix A, Benitez ID, Santisteve S, Monge A, Fontiveros MA, et al. Clinical consequences of COVID-19 lockdown in patients with COPD. Chest. 2021. 10.1016/j.chest.2020.12.057. [DOI] [PMC free article] [PubMed]
- 27.Public Health Scotland. Data and intelligence. https://www.isdscotland.org/. Accessed 9 Nov 2020.
- 28.Jones KH, Ford DV, Thompson S, Lyons RA. A profile of the SAIL databank on the UK secure research platform. Int J Popul Data Sci. 2019;4. [DOI] [PMC free article] [PubMed]
- 29.Data quality status report - Admitted Patient Care Data Set . NHS Wales Informatics Service. 2020. [Google Scholar]
- 30.Data Support and Monitoring: SMR Completeness. Public Health Scotland. 2021. https://www.isdscotland.org/products-and-Services/Data-Support-and-Monitoring/SMR-Completeness/. Accessed 6 Mar 2021.
- 31.User guide to mortality statistics - Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/methodologies/userguidetomortalitystatisticsjuly2017. Accessed 21 Nov 2020.
- 32.Quality of National Records of Scotland (NRS) Data on vital events. National Records of Scotland. https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/general-background-information/quality-of-national-records-of-scotland-nrs-data-on-vital-events. Accessed 6 Mar 2021.
- 33.Quality of mortality data during the coronavirus pandemic, England and Wales: 2020 - Office for National Statistics. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/qualityofmortalitydataduringthecoronaviruspandemicenglandandwales/2020.
- 34.Hothorn T, Zeileis A, Farebrother RW, Cummins C. lmtest: testing linear regression models. 2020. https://cran.r-project.org/package=lmtest.
- 35.Lyons RA, Jones KH, John G, Brooks CJ, Verplancke JP, Ford DV, et al. The SAIL databank: linking multiple health and social care datasets. BMC Med Inform Decis Mak. 2009;9. [DOI] [PMC free article] [PubMed]
- 36.Lopez-Bernal J. Framework for Enhanced Reporting of Interrupted Time Series (FERITS) [Reporting guidelines under development for observational studies]. https://www.equator-network.org/library/reporting-guidelines-under-development/reporting-guidelines-under-development-for-observational-studies/#92.
- 37.Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Peteresen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scottish Government . Coronavirus (COVID-19) update: First Minister’s speech 28 May 2020 - Scottish Government. 2020. [Google Scholar]
- 39.Welsh Government . Written statement: review of lockdown measures and the health protection (Coronavirus Restrictions) (Wales) Regulations 2020 | GOV.WALES. 2020. [Google Scholar]
- 40.National Institute for Health and Care Excellence . Quality standard and indicators briefing paper: Chronic obstructive pulmonary disease (COPD) update. 2015. [Google Scholar]
- 41.NHS National Services Scotland . Assessing the evidence base for medical procedures which create a higher risk of respiratory infection transmission from patient to healthcare worker. 2020. [Google Scholar]
- 42.Rothnie KJ, Müllerová H, Hurst JR, Smeeth L, Davis K, Thomas SL, et al. Validation of the recording of acute exacerbations of COPD in UK primary care electronic healthcare records. PLoS One. 2016;11(3):e0151357. [DOI] [PMC free article] [PubMed]
- 43.EDDS Data Validity. NHS Wales Informatics Service. https://nwis.nhs.wales/information-services/information-standards/data-quality/data-quality-standards/edds-data-validity/. Accessed 6 Mar 2021.
- 44.Wedzicha JA. Exacerbations: etiology and pathophysiologic mechanisms. Chest. 2002;121(5):136S–141S. doi: 10.1378/chest.121.5_suppl.136S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oreskovic NM, Kinane TB, Aryee E, Kuhlthau KA, Perrin JM. The unexpected risks of COVID-19 on asthma control in children. J Allergy Clin Immunol Pract. 2020;8(8):2489–2491. doi: 10.1016/j.jaip.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chavasse RJ. Covid-19: reduced asthma presentations in children. The BMJ. 2020;370. 10.1136/bmj.m2806. [DOI] [PubMed]
- 47.Krivec U, Kofol Seliger A, Tursic J. COVID-19 lockdown dropped the rate of paediatric asthma admissions. Arch Dis Child. 2020;105(8):809–810. doi: 10.1136/archdischild-2020-319522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Davies GA, Alsallakh MA, Sivakumaran S, Vasileiou E, Lyons RA, Robertson C, et al. Impact of COVID-19 lockdown on emergency asthma admissions and deaths: national interrupted time series analyses for Scotland and Wales. Thorax. 2021. https://thorax.bmj.com/content/early/2021/02/11/thoraxjnl-2020-216380.citation-tools. [DOI] [PubMed]
- 49.Chalitsios CV, McKeever TM, Langley TE, Shaw DE. Impact of COVID-19 on corticosteroids and antibiotics prescribing in England: an interrupted time series analysis. J Public Health (Bangkok). 2021. 10.1093/pubmed/fdab017. [DOI] [PMC free article] [PubMed]
- 50.McAuley H, Hadley K, Elneima O, Brightling CE, Evans RA, Steiner MC, Greening NJ. COPD in the time of COVID-19: an analysis of acute exacerbations and reported behavioural changes in patients with COPD. ERJ Open Res. 2021;7(1):00718–02020. doi: 10.1183/23120541.00718-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thieriot H, Myllyvirta L. Air pollution returns to European capitals: Paris faces largest rebound. 2020. https://energyandcleanair.org/wp/wp-content/uploads/2020/06/202006-Europe-Rebound-4.pdf. Accessed 4 Nov 2020.
- 52.Williams NP, Coombs NA, Johnson MJ, Josephs LK, Rigge LA, Staples KJ, Thomas M, Wilkinson TMA. Seasonality, risk factors and burden of community-acquired pneumonia in COPD patients: a population database study using linked health care records. Int J COPD. 2017;Volume 12:313–322. doi: 10.2147/COPD.S121389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P, Cockburn J, McDonald HI, MacKenna B, Tomlinson L, Douglas IJ, Rentsch CT, Mathur R, Wong AYS, Grieve R, Harrison D, Forbes H, Schultze A, Croker R, Parry J, Hester F, Harper S, Perera R, Evans SJW, Smeeth L, Goldacre B. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ. 2020;369. 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed]
- 55.Clift AK, Coupland CAC, Keogh RH, Diaz-Ordaz K, Williamson E, Harrison EM, et al. Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. BMJ. 2020. 10.1136/bmj.m3731. [DOI] [PMC free article] [PubMed]
- 56.Public Health England . Excess mortality in England, week ending 16 October 2020. 2020. [Google Scholar]
- 57.Sheikh A. Improving air quality needs to be a policy priority for governments globally. PLoS Med. 2020;17(2):e1003041. doi: 10.1371/journal.pmed.1003041. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Includes Read codes for COPD diagnosis, acute exacerbation of COPD, and smoking status used for sensitivity analysis, model diagnostics (Table A), the results of the sensitivity analysis (Tables B, C, D, and E), and the reporting checklists (FERITS, STROBE, RECORD).
Data Availability Statement
The anonymised person-level data supporting the conclusions of this article are held by Public Health Scotland (https://publichealthscotland.scot/) and the SAIL Databank (https://saildatabank.com/) and are restricted and not publicly available but can be accessed upon reasonable requests and with permission from PHS and SAIL. All proposals to use SAIL are carefully reviewed by an independent Information Governance Review Panel (IGRP) to ensure proper and appropriate use of data (https://www.saildatabank.com/application-process). When approved, access is then provided through the SAIL Gateway, a privacy-protecting safe haven and a secure remote access system.