Supplemental Digital Content is Available in the Text.
Key Words: SARS-CoV-2 infection, COVID-19, HIV infection, health services accessibility, public health administration, Japan
Background:
During the COVID-19 outbreak, facility capacity for HIV testing has been limited. Furthermore, people may have opted against HIV testing during this period to avoid COVID-19 exposure. We investigated the influence of the COVID-19 pandemic on HIV testing and the number of reported HIV cases in Japan.
Methods:
We analyzed quarterly HIV/AIDS-related data from 2015 to the second quarter of 2020 using an anomaly detection approach. The data included the number of consultations, the number of HIV tests performed by public health centers or municipalities, and the number of newly reported HIV cases with and without an AIDS diagnosis. We further performed the same analysis for 2 subgroups: men who have sex with men (MSM) and non-Japanese persons.
Results:
The number of HIV tests (9,584 vs. 35,908 in the year-before period) and consultations (11,689 vs. 32,565) performed by public health centers significantly declined in the second quarter of 2020, whereas the proportion of new HIV cases with an AIDS diagnosis (36.2% vs. 26.4%) significantly increased after removing the trend and seasonality effects. HIV cases without an AIDS diagnosis decreased (166 vs. 217), but the reduction was not significant. We confirmed similar trends for the men who have sex with men and non-Japanese subgroups.
Conclusions:
During the COVID-19 pandemic, the current HIV testing system in Japan seems to have missed more cases of HIV before developing AIDS. Continuously monitoring the situation and securing sufficient test resources by use of self-testing is essential to understand the clear epidemiological picture of HIV incidence during the COVID-19 pandemic.
INTRODUCTION
In Japan, the first case of COVID-19 with a travel history to Wuhan was identified on January 16, 2020. Entry restrictions for all foreign citizens with a travel history to Hubei province (China) were implemented on February 3, after which the restrictions were gradually expanded to other countries. Control measures to contain the epidemic based on contact tracing and a targeted testing strategy were implemented since late February 2020.1 However, the containment measures failed, and the number of cases continuously and gradually increased. As a response, a state of emergency was declared in 7 provinces on April 7, 2020, which was expanded to the whole country on April 16. After the declaration, the epidemic slowed down. The state of emergency was lifted by May 25, and processes to reopen businesses were initiated.2 By the end of June 2020, a total of 18,593 cases had been identified in Japan, and 972 among them had died.3
The ongoing COVID-19 pandemic has had broad influences on lifestyle and health issues beyond COVID-19. Especially, non–COVID-19 diseases have been at a lower priority for treatment because medical resources have been disproportionately allocated to treat COVID-19 patients in many health care facilities, and the capacity to care for non–COVID-19 disease has been limited. Moreover, health care facilities need to balance the benefits of providing care for noncritical conditions with minimizing the risk for COVID-19 infection among both health care professionals and patients.4
People living with HIV infections have better outcomes with early diagnosis and connection to antiretroviral treatment.5,6 Early diagnosis before the development of AIDS is also key to preventing onward transmission. This is because the acute phase of 3–4 weeks since infection before seroconversion,7 which is followed by the pre-AIDS stage with a relatively low viral load for about 10 years,8,9 is characterized by a high viral load. Furthermore, receiving an HIV diagnosis is expected to facilitate behavioral change.10 However, the COVID-19 pandemic may disrupt early diagnosis. For example, Lagat et al11 reported a decline in HIV test volume in Kenya because of many barriers related to COVID-19, such as lack of funds to visit clinics and fear of COVID-19 infection at clinics.
To increase HIV testing opportunities, in the United States, the Centers for Disease Control and Prevention is recommending self-testing of HIV or home specimen collection (eg, dried blood spot or oral fluid test) to avoid COVID-19 infection risk associated with face-to-face testing services.12 In Japan, the number of self-collection–based HIV tests has increased (from 26,000 tests in 2005 to 91,000 tests in 201613); however, self-testing is not yet approved by health authorities owing to technical issues. Thus, the majority of tests are still conducted at public health centers (118,000 tests in 201614) and clinics (number unknown) (ie, facility-based testing). During the COVID-19 pandemic, however, public health centers and clinics have been overwhelmed by COVID-19 polymerase chain reaction testing and administrative work, and many have temporarily suspended or limited HIV testing.15–17 Note that public health centers in Japan are local governmental facilities under the Ministry of Health, Labour and Welfare of Japan and are responsible for various public health issues, including infectious diseases and chronic diseases.18 The role of the public health centers is like that of state or county departments of health in the United States. In the context of infectious disease, the public health centers provide relevant information to the public (ie, awareness programs), collect data on designated infectious diseases, including HIV and COVID-19 following Infectious Diseases Control Law,19 and organize HIV testing sites and events.
Given the limited availability of HIV testing in Japan during the COVID-19 pandemic, we expected that the number of HIV diagnoses would be affected during this period. However, the direction and magnitude of the effect would likely be dependent on the stage of infection and whether they come with AIDS diagnoses. We hypothesized that the number of HIV cases without an AIDS diagnosis would decrease because those without symptoms may have delayed or skipped routine testing, or their test would not be prioritized by health care providers. In contrast, we hypothesized that the number of HIV cases with an AIDS diagnosis would remain stable because testing for these later-stage infections is usually prompted by specific symptoms, and the testing would be prioritized by health care providers.
We compared the following HIV-related data during the first 2 quarters of 2020 with earlier data: (1) the number of HIV consultations received by public health centers, (2) the number of tests performed at public health centers and municipalities, (3) the number of newly reported HIV cases without an AIDS diagnosis, and (4) the number of newly reported HIV cases with an AIDS diagnosis. Furthermore, we assessed whether the proportion of new HIV cases with an AIDS diagnosis increased during the first 2 quarters of 2020.
METHODS
Data
HIV/AIDS-related data were extracted from the quarterly report from the National AIDS Surveillance Committee from the first quarter of 2015 to the second quarter of 2020 (accessed: September 16, 2020).14 The data included (1) the number of HIV/AIDS-related consultations at public health centers, (2) the number of HIV antibody tests performed at public health centers or by municipalities, and (3) the number of reported HIV cases with and without an AIDS diagnosis in Japan.
Note that the number of tests performed by public health centers, which was the measure used in this study, accounts for less than half of the total number of tests in Japan. By contrast, the number of HIV cases with or without an AIDS diagnosis covers all reported cases (including those tested at clinics and hospitals as well as public health centers) because medical doctors are mandated to report HIV cases following the Infectious Diseases Control Law.19
AIDS was defined by any of 23 AIDS-defining diseases.20 The reported information included AIDS diagnosis, transmission route (homosexual intercourse, heterosexual intercourse, injection drug use, mother-to-child transmission, or others), demographic information (age, sex, nationality [Japanese or non-Japanese], area of living [prefecture]). The number of quarterly HIV cases with some breakdowns were available (ie, individual data were not publicly accessible).
The data for HIV tests and consultation only count those performed in public health centers (ie, data for HIV tests performed at clinics or hospitals or by self-testing were not available). Public health centers offer free and anonymous HIV testing and consultation services. The consultation service is designated for all individuals for any telephone inquiries relevant to HIV and AIDS, including prevention, testing, and treatment. The current HIV screening test performed in the public health centers mostly uses the fourth-generation enzyme-linked immunosorbent assay, which is the test for HIV-1 p24 antigen and anti-HIV-1/2 antibodies.21 Furthermore, Western blot analysis and nucleic acid amplification testing are performed on positive assays for confirmation. Only quarterly data were available.
For a better understanding of the data on HIV cases, we analyzed the data for the following 2 subgroups: men who have sex with men (MSM) and non-Japanese persons. MSM account for approximately 70% of the newly reported HIV cases,14 and foreigners are considered vulnerable during disasters owing to language barriers and discrimination.22 MSM in the data were defined as male cases infected through homosexual intercourse. The data on the number of tests and consultations were not separately reported for these subgroups. Note that HIV cases were separately reported according to AIDS diagnosis at the time of the test (ie, with or without an AIDS diagnosis). Because the data used in this study are publicly available without any restriction and deidentified summary data, neither an ethical statement nor consent was necessary.
Anomaly Detection
We applied an anomaly detection approach to those longitudinal data to identify the period when the number of HIV-related consultations, HIV antibody tests, and new HIV cases with and without an AIDS diagnosis were disrupted. Furthermore, we tested when the proportion of new HIV cases with an AIDS diagnosis was disrupted. First, each set of longitudinal data was decomposed into seasonal, trend, and remainder components by seasonal trend decomposition using LOESS, which is known as STL decomposition.23 The reason we adapted the STL decomposition method is that it guarantees preferable interpretability regarding the source of anomalies: it can explicitly model the periodic and linear components simultaneously in the model, and thus, we can focus on the remainder (or residual) component to detect anomalies after adjusting for the 2 components. In the STL, LOESS smoothing was iteratively used to determine the trend component. After removing the trend component, LOESS smoothing was again used to extract the seasonal component (1-year cycle). The trend component was tested for whether it had an increasing or decreasing trend using a nonparametric Spearman test.24 The remainder was analyzed with an anomaly detection method, the generalized extreme studentized deviate test (GESD), which identified outliers progressively using the deviation from mean as a test statistic.25 A statistical significance level was set at 0.05. All analyses were performed on the statistical computing software R 4.0.1 (R Development Core Team) with the library “anomalize.”
RESULTS
Table 1 summarizes the data on quarterly numbers of consultations, HIV tests, and HIV cases. Over the period studied (2015 to the second quarter of 2020), the quarterly numbers of consultations and HIV tests at public health centers were both approximately 30,000. Median quarterly numbers of HIV cases with and without an AIDS diagnosis were 240 (interquartile range, 218–252) and 100 (85–109), respectively. Thus, the proportion of new HIV cases with an AIDS diagnosis was 28.9% (interquartile range, 27.3%–30.9%). Approximately 70% and 55% of HIV cases with and without AIDS were explained by MSM during the period, whereas approximately 10% of them were from the non-Japanese population.
TABLE 1.
Quarterly Numbers of Consultations and HIV Tests at Public Health Centers and HIV Cases, 2015 to the Second Quarter of 2020*
| Consultations | Tests | HIV† | AIDS‡ | Prop. Of AIDS (%)§ | |
| Total‖ | 31,076 (29,755–32,735) | 31,009 (28,562–34,051) | 240 (218–252) | 100 (85–109) | 28.9 (27.3–30.9) |
| MSM | 174 (150–184) | 56 (48–61) | 24.8 (22.2–26.9) | ||
| Non-Japanese | 32 (28–38) | 9 (8–11) | 25.8 (20–27.3) |
Median quarterly numbers and 25% and 75% percentiles (in parentheses) are reported. The number of consultations and HIV tests at public health centers were not available for subpopulations (MSM and the non-Japanese population).
Quarterly number of HIV cases without an AIDS diagnosis.
Quarterly number of HIV cases with an AIDS diagnosis.
Proportion of new HIV cases with an AIDS diagnosis.
Total population includes MSM and the non-Japanese population.
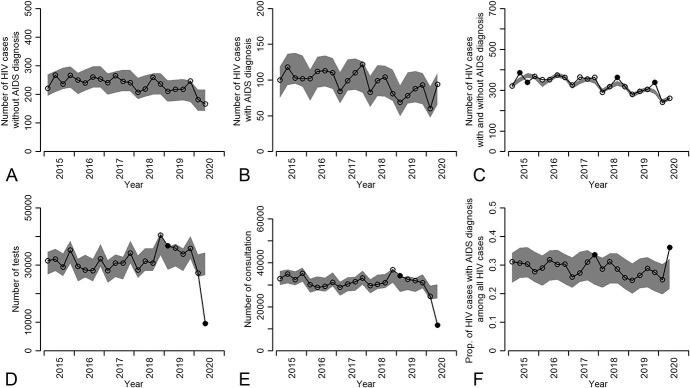
Figure 1 shows the observed data points and the computed normal range (the shaded area) for the number of HIV tests and consultations performed and the number of newly diagnosed HIV cases with and without an AIDS diagnosis. By the last quarter of 2019 (ie, before the COVID-19 pandemic), a few data points significantly deviated from the normal range. However, the magnitude of the deviation of those numbers was modest. Focusing on the data in 2020, we found significant and large deviation in the number of HIV tests (Fig. 1D) and consultations (Fig. 1E), and the proportion of new HIV cases with an AIDS diagnosis (Fig. 1F) in the second quarter of 2020 after removing the trend and seasonality effects. The numbers of HIV tests and consultations performed by public health centers decreased from 35,908 and 32,565 (2019) to 9,584 and 11,689 (2020) in the second quarter, respectively. The proportion of new HIV cases with an AIDS diagnosis increased from 26.4% (2019) to 36.2% (2020) in the second quarter. Note that the numbers of HIV and AIDS cases were not significantly deviated from the normal range; however, the number of HIV cases without an AIDS diagnosis numerically decreased (from 217 to 166 in the second quarter of 2019 and 2020), whereas the number with AIDS diagnosis increased (from 78 to 94 in the second quarter of 2019 and 2020). We did not observe deviation in any numbers in the first quarter of 2020.
FIGURE 1.
Number of HIV tests and consultations performed by public health centers and municipalities and number of newly diagnosed HIV cases with and without an AIDS diagnosis from 2015 to the first quarter of 2020: (A) Number of newly reported HIV cases without an AIDS diagnosis, (B) number of newly reported HIV cases with an AIDS diagnosis, (C) number of newly reported HIV cases with and without an AIDS diagnosis, (D) number of HIV tests performed by public health centers or municipals, (E) number of consultations received by public health centers, (F) proportion of new HIV cases with an AIDS diagnosis. The black circles are observed data, and the grey shaded areas correspond to the normal range. Observed data outside the normal range are considered abnormal and are filled with black.
As a sensitivity analysis, we examined the longitudinal data for HIV cases with and without an AIDS diagnosis in 2 subgroups: MSM and the non-Japanese population. We observed a similar trend in the number of HIV cases with and without an HIV diagnosis (the former increased and latter decreased) in the second quarter of 2020 compared with the same period of 2019; however, these trends were not significant (see Fig. S1AB and S2AB, Supplemental Digital Content, http://links.lww.com/QAI/B624). The proportion of new HIV cases with an AIDS diagnosis numerically increased in the second quarter of 2020 in these 2 subgroups, which significantly increased when all cases were analyzed (see Figs. S1D and S2D, Supplemental Digital Content, http://links.lww.com/QAI/B624); however, the proportion was in the normal range.
DISCUSSION
A significant anomaly was identified in the number of tests and consultations performed by public health centers and municipalities, and the proportion of new HIV cases with an AIDS diagnosis in the second quarter of 2020 after removing seasonality and trend, which corresponds to the period of the COVID-19 pandemic in Japan. Furthermore, the number of HIV cases without an AIDS diagnosis numerically decreased in the second quarter of 2020, although this change was not significant. We did not observe a significant anomaly in the first quarter of 2020, which was before the state of emergency was announced in Japan.2
It is worth noting that the number of HIV cases without an AIDS diagnosis did not decline as much as the number of tests (the former dropped 23.5%, whereas the latter dropped 73.3% compared with the year-before period). This might be because more HIV cases without AIDS symptoms visited clinics because of their recent unsafe risk behavior or acute HIV symptoms (they might have sought the COVID-19 test first as the symptoms are similar), assuming that most of those without an AIDS diagnosis were recently infected by HIV.
Under the COVID-19 pandemic situation, public health centers temporarily suspended HIV tests.17 Furthermore, people might have skipped the testing at public health centers because of fear of COVID-19 infection or because of the state of emergency. The temporal change we observed may reflect such temporal changes in the HIV testing system in the public health centers and municipalities. We need to interpret the results carefully. First, we only analyzed the number of tests performed by public health centers and municipalities. For example, self-collection–based tests (mostly using dried blood spots) are increasing (from 26,000 tests in 2005 to 91,000 tests in 201613), and tests are available in clinics and hospitals; however, the count of those tests was not available. Given that, the number of tests performed by public health centers (118,000 tests in 201614) is considered to account for at most half of the tests performed in Japan. It is probable that the number of those types of HIV tests also increased during the same period as compensation for the reduction in the number of tests performed by public health centers and municipalities. Second, we do not know the full picture of the impact of the COVID-19 pandemic on HIV epidemiology. We used the number of reported HIV cases; however, there is likely a substantial proportion of undiagnosed cases (approximately 20%26), and it is uncertain whether the number and the proportion of undiagnosed cases changed during the COVID-19 pandemic. It is possible that the incidence increased (or decreased) during the COVID-19 pandemic. Therefore, even though the number of new HIV cases did not change dramatically, this does not indicate that the number of tests is sufficient to identify all patients with HIV. Indeed, the number of reported HIV-positive cases without progression to AIDS in the second quarter of 2020 was the lowest in the past 5 years and the proportion of new HIV cases with an AIDS diagnosis significantly increased. This raises the concern that testing opportunities might not be sufficient to fully capture the epidemiological situation of HIV/AIDS during the COVID-19 pandemic in Japan. Because most of the HIV cases with an AIDS diagnosis are identified in clinics or hospitals because of specific symptoms, HIV cases with an AIDS diagnosis are less prone to being affected by health care avoidance even under the COVID-19 pandemic. We need to keep monitoring the situation and adapting testing strategies to work in these unusual circumstances.
As the COVID-19 pandemic continues, we do not know how long the HIV testing opportunities provided by public health centers could be disrupted and how this disruption could affect HIV spread. Given that early detection and treatment initiation for HIV is lifesaving, providing sufficient HIV testing opportunities is important. If the COVID-19 pandemic continuously disrupts testing opportunities, diagnosing 90% of people living with HIV, which is a target proposed by UNAIDS,27 might be difficult to achieve. Self-testing and home specimen collection could be a key to fill the gap between the need for HIV testing and the constraints related to the COVID-19 outbreak.
The strength of this study is that we used the quarterly HIV/AIDS reports in Japan, which include all diagnosed cases, because physicians are required to report all diagnosed cases under the Infectious Diseases Control Law.19 Furthermore, the cases reported as HIV cases with an AIDS diagnosis include only the cases of newly diagnosed HIV infection cooccurring with AIDS. Therefore, we could quantify the proportion of patients presenting with AIDS at the time of diagnosis, which captures late presentation for diagnosis and is more likely if testing resources are not accessible.
A limitation of this study is that we were not able to account for the heterogeneous epidemiology of HIV between different regions. The incidence of HIV has been observed to be higher in urban areas, such as Tokyo and Osaka, than in rural areas. Thus, public health centers in urban areas have allocated budgetary resources toward HIV testing, whereas this has not been prioritized in rural areas. During the COVID-19 pandemic, the testing opportunities in rural areas may have declined even further than those in urban areas. Our study mainly focused on HIV cases with and without an AIDS diagnosis and testing regardless of the patient's characteristics. One of the concerns in this pandemic is that more vulnerable populations, such as sex workers, low-income populations, the younger population, and foreigners, may have experienced disproportionate harms. Further studies should focus on these populations and identify barriers to testing. We did not observe an anomaly in the subgroup analyses. This could be because the number of cases was originally reported on a quarterly basis, which might have resulted in low power. Data with more granularity (ie, monthly or weekly basis) need to be analyzed for a better understanding of the situation. We used only the number of tests performed by public health centers and municipalities; thus, self-tests and home specimen collection, which are increasingly popular, and tests performed in clinics and hospitals, were not counted. Further investigation is necessary to focus on these types of tests to fully understand the response of the HIV testing system to the COVID-19 pandemic in Japan.
We demonstrated that the uptake of HIV testing provided by public health centers and municipalities declined; furthermore, HIV cases without an AIDS diagnosis during the COVID-19 pandemic numerically decreased and the proportion of new HIV cases with an AIDS diagnosis increased. Thus, it will be critical to provide sufficient HIV testing opportunities and keep sustained attention on the unpredictable and previously unobserved public health consequences of the interactions between the dual COVID-19 and HIV epidemics.
ACKNOWLEDGMENTS
Conceived and designed the study: K.E., S.I., Analyzed the data: K.E. initially analyzed the data, and N.Y. and D.Y. verified the analyses. Wrote the paper: K.E., Y.K., N.Y., M.R., C.L., A.I.B., D.Y., S. Ichikawa, D.M., S. Iwami. All authors read and approved the final manuscript.
Footnotes
S.I. received the following funding: Grants-in-Aid for JSPS Scientific Research (KAKENHI) Scientific Research B 18KT0018, 18H01139, 16H04845, Scientific Research in Innovative Areas 20H05042, 19H04839, 18H05103; AMED J-PRIDE 19fm0208006s0103, 19fm0208014h0003, 19fm0208019h0103; AMED Research Program on HIV/AIDS 19fk0410023s0101; Research Program on Emerging and Re-emerging Infectious Diseases 19fk0108050h0003; 19fk0210036h0502; JST MIRAI; Moonshot R&D Grant Number JPMJMS2021 and JPMJMS2025; Daiwa Securities Health Foundation. M.R. received funding from the NIH National Institute on Aging through Grant number 1R01AG069128. D.Y. received funding from Daiwa Securities Health Foundation. The remaining authors have no funding or conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
Contributor Information
Yoshiki Koizumi, Email: koizumi.yoshi@gmail.com.
Nao Yamamoto, Email: nao.m.yamamoto@gmail.com.
Molly Rosenberg, Email: rosenmol@indiana.edu.
Christina Ludema, Email: cludema@indiana.edu.
Ana I. Bento, Email: abento@iu.edu.
Daisuke Yoneoka, Email: daisuke.yoneoka@slcn.ac.jp.
Seiichi Ichikawa, Email: s-ichikawa@kinjo-u.ac.jp.
Daisuke Mizushima, Email: dmizushi@acc.ncgm.go.jp.
Shingo Iwami, Email: siwami@kyushu-u.org.
REFERENCES
- 1.Furuse Y, K Ko Y, Saito M, et al. Epidemiology of COVID-19 outbreak in Japan, January–March 2020. Jpn J Infect Dis. 2020;73:391–393. [DOI] [PubMed] [Google Scholar]
- 2.Han E, Tan MMJ, Turk E, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. 2020;396:1525–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Framework for Healthcare Systems Providing Non-COVID-19 Clinical Care during the COVID-19 Pandemic; 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html. Accessed July 27, 2020. [Google Scholar]
- 5.Lundgren JD, Babiker AG, Gordin F, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373:795–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Croxford S, Kitching A, Desai S, et al. Mortality and causes of death in people diagnosed with HIV in the era of highly active antiretroviral therapy compared with the general population: an analysis of a national observational cohort. Lancet Public Health. 2017;2:e35–e46. [DOI] [PubMed] [Google Scholar]
- 7.Pilcher CD, Eron JJ, Jr, Galvin S, et al. Acute HIV revisited: new opportunities for treatment and prevention. J Clin Invest. 2004;113:937–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bacchetti P, Moss AR. Incubation period of AIDS in san francisco. Nature. 1989;338:251–253. [DOI] [PubMed] [Google Scholar]
- 9.Muñoz A, Sabin CA, Phillips AN. The incubation period of AIDS. AIDS. 1997;11(Suppl A):S69–S76. [PubMed] [Google Scholar]
- 10.Rucinski KB, Rutstein SE, Powers KA, et al. Sustained sexual behavior change after acute HIV diagnosis in Malawi. Sex Transm Dis. 2018;45:741–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lagat H, Sharma M, Kariithi E, et al. Impact of the COVID-19 pandemic on HIV testing and assisted partner notification services, Western Kenya. AIDS Behav. 2020;24:3010–3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. HIV Self Testing Guidance; 2020. Available at: https://www.cdc.gov/nchhstp/dear_colleague/2020/dcl-042820-HIV-self-testing-guidance.html. Accessed July 29, 2020. [Google Scholar]
- 13.Takano M, Iwahashi K, Satoh I, et al. Assessment of HIV prevalence among MSM in Tokyo using self-collected dried blood spots delivered through the postal service. BMC Infect Dis. 2018;18:627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National AIDS Surveillance Committee. Quarterly report. 2020; Available at: https://api-net.jfap.or.jp/status/japan/index.html. Accessed September 16, 2020.
- 15.Tokyo Shimbun Nov 26, 2020, Available at: https://www.tokyo-np.co.jp/article/70598. Accessed December 31, 2020. [Google Scholar]
- 16.Shimizu K, Negita M. Lessons learned from Japan's response to the first Wave of COVID-19: a content analysis. Healthcare. 2020;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shimizu K, Wharton G, Sakamoto H, et al. Resurgence of covid-19 in Japan. BMJ. 2020;370:m3221. [DOI] [PubMed] [Google Scholar]
- 18.Katsuda N, Hinohara Y, Tomita K, et al. Structure and roles of public health centers (hokenjo) in Japan. Nagoya J Med Sci. 2011;73:59–68. [PMC free article] [PubMed] [Google Scholar]
- 19.Taniguchi K, Hashimoto S, Kawado M, et al. Overview of infectious disease surveillance system in Japan, 1999-2005. J Epidemiol. 2007;17(Suppl):S3–S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kimura S. Diagnostic criteria for HIV/AIDS in Japan. Nihon rinsho Jpn J Clin Med. 2002;60:688–693. [PubMed] [Google Scholar]
- 21.Stefic K, Guinard J, Peytavin G, et al. Screening for human immunodeficiency virus infection by use of a fourth-generation antigen/antibody assay and dried blood spots: in-depth analysis of sensitivity and performance assessment in a cross-sectional study. J Clin Microbiol. 2019;58:e01645–e01719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ye M, Aldrich DP. How natural hazards impact the social environment for vulnerable groups: an empirical investigation in Japan. Nat Hazards. 2021;105:67–81. [Google Scholar]
- 23.Cleveland RB, Cleveland WS, Terpenning I. STL: a seasonal-trend decomposition procedure based on loess. J Official Stat. 1990;6:3. [Google Scholar]
- 24.Siegel S, Castellan N. Non Parametric Statistics for the Behavioral Sciences. New-York: Mc Graw-Mill international edition; 1988. [Google Scholar]
- 25.Rosner B. Percentage points for a generalized ESD many-outlier procedure. Technometrics. 1983;25:165–172. [Google Scholar]
- 26.Nishiura H. Estimating the incidence and diagnosed proportion of HIV infections in Japan: a statistical modeling study. PeerJ. 2019;7:e6275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The Joint United Nations Programme on HIV/AIDS (UNAIDS). 90-90-90: Treatment for All. 2020; Available at: https://www.unaids.org/en/resources/909090. Accessed August 1, 2020. [Google Scholar]