Abstract
Patient: Female, 17-year-old
Final Diagnosis: Periorbital abscess • retinal artery and vein occlusion
Symptoms: Blindness • nasal congestion • pain the eye • proptosis
Medication: —
Clinical Procedure: Drainage • endoscopic sinus surgery
Specialty: Otolaryngology
Objective:
Unusual clinical course
Background:
Periorbital abscesses are uncommon complications of acute bacterial rhinosinusitis; with the evolution of diagnostic and therapeutic methods, it is rare that the patient progresses to irreversible blindness. Central retinal artery occlusion (CRAO) and central retinal vein occlusion (CRVO) rarely occur simultaneously and the factors that influence this occurrence are not well understood.
Case Report:
This is a case report of an immunocompetent healthy adolescent girl, who developed irreversible blindness caused by a periorbital abscess secondary to acute bacterial rhinosinusitis due to CRAO and CRVO. Despite 6 days of clinical treatment, including intravenous antibiotics (vancomycin-associated piperacillin with tazobactam), she had a large periorbital abscess and could not open her left eye. Therefore, she was transferred to a tertiary hospital; 1 day after her admission, she underwent surgical treatment to drain the abscess through external and endoscopic access. In addition, she received broad-spectrum antibiotics (meropenem with vancomycin) for 3 weeks. She was no longer able to perceive light with the left eye, despite her clinical improvement. This case report discusses the factors that could have contributed to this poor outcome, despite clinical and surgical treatment.
Conclusions:
We conclude that there are several mechanisms that can lead to the loss of vision and when the indicated surgical intervention is delayed, it can increase the risk of visual sequelae.
Keywords: Orbital Cellulitis, Sinusitis, Vision Disorders
Background
Periorbital cellulitis and abscesses are rare complications of acute bacterial rhinosinusitis (ABRS), which are more frequent in the pediatric age group. The current incidence of ABRS complications is 3 cases per 1 million people every year, with orbital infections being the most common (60% to 80%) [1]. Historically, the periorbital complications have been classified by Chandler as inflammatory edema (preseptal cellulitis), orbital cellulitis, subperiosteal abscess (SPA), orbital abscess, and cavernous sinus thrombosis (CST) [2]. CST can be classified in the group of intracranial complications [3].
Permanent visual loss occurred in about 20% of patients with postseptal inflammation in the pre-antibiotic era [4]. Despite a substantial reduction in the incidence of irreversible blindness in orbital complications of ABRS (5.5% to 10%), the factors that lead to permanent visual loss are not yet fully explained [3]. One of the mechanisms of this visual repercussion is ischemia of the retina due to occlusion of its central artery (first reported in 2003) [5]. Simultaneous occlusion of the central artery and vein is even rarer, with very few cases reported [6].
Here, we present a case of an immunocompetent adolescent girl with an SPA, who developed unilateral irreversible blindness and visible signs of central retinal artery occlusion (CRAO) and central retinal vein occlusion (CRVO), which are a rare complication with an unusual clinical course.
Case Report
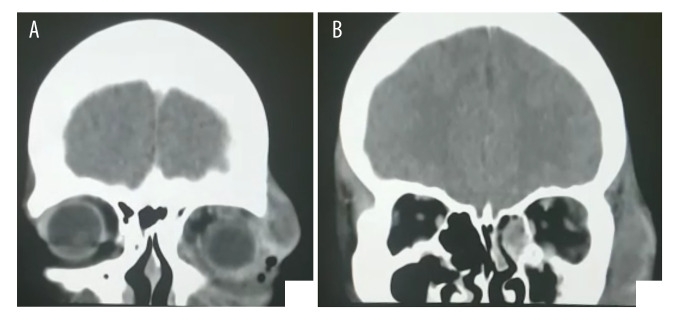
A 17-year-old, previously healthy female patient, with nothing remarkable in her family history, was transferred to a tertiary hospital from a General Emergency Unit. She reported having pain and periorbital edema in the left eye for 6 days, without any symptoms in her right eye. She referred nasal obstruction and discharge a couple of days prior to the orbital condition; however, her symptoms were very vague and unspecific. She had been admitted at a General Emergency Unit 3 days earlier, where a computed tomography (CT) scan had suggested orbital complication by acute pansinusitis (Figure 1A, 1B). While hospitalized in that unit, she was administered 2 treatments of intravenous antibiotic therapy. The first antibiotic therapy was not described; the second treatment was vancomycin (2 g/day) with piperacillin and tazobactam (12 g/day and 1.5 g/day) for 48 hours, with no signs of improvement. After admission in our hospital, upon examination, an intense bipalpebral edema with hyperemia was observed in the left eye, which extended to the zygomatic region. There was a hematic and purulent secretion through the spontaneous cutaneous holes above and below the left eye. She was incapable of spontaneous eye opening and denied any perception of external light in the left eye.
Figure 1.
(A, B) Computed tomography: Coronal section showed rhinosinusitis with a periorbital abscess.
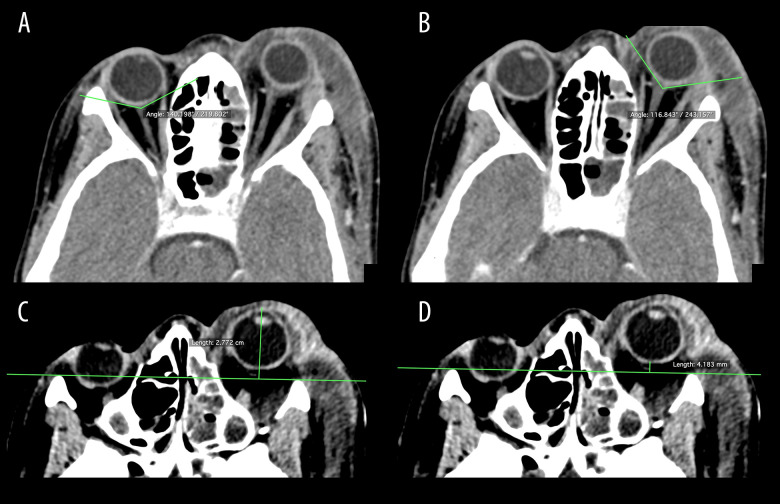
Since the hospital admission, she was administered a new antibiotic treatment (meropenem 6 g/day and vancomycin 2 g/day) and corticosteroid therapy (hydrocortisone 900 mg/day initially, with gradual dose reduction) for the first 7 days. After an otorhinolaryngologic evaluation, a new CT was performed. The imaging showed an extensive inflammation in the maxillary, zygomatic, and left eyelid regions and a collection of pus measuring 6.0×4.4×1.6 cm (about 21.9 ml in volume), with gaseous foci in between. In addition, there was a 4.77-mm protrusion of the homolateral eyeball and mucal thickening of the paranasal sinuses, with preserved intraconal fat, and without lamina papyracea dehiscence. The posterior angles of the eyeballs were approximately 140º on the right side and 117º on the left side (Figure 2A, 2B). The distance from the anterior sclera and the interzygomatic line on the left side was 27.7 mm (Figure 2C, 2D). The image was suggestive of pre- and postseptal cellulitis secondary to ABRS complicated with non-medial SPA.
Figure 2.
Computed tomography, axial sections: (A, B) Difference between the posterior angles of eyeballs (right: approx. 140º; left: approx. 117º). (C) Distance between the anterior sclera and the 27.7-mm interzygomatic line. (D) Ocular proptosis (4.2 mm).
During the day of the admission, she presented with toxemia and hypotension, reported dyspnea, and required supplemental oxygen by nasal catheter for a few hours. Laboratory tests showed leukocytosis (20 500 white blood cells/microliter of blood) with neutrophilia, a moderate increase in inflammatory markers, hypokalemia, and altered renal function (creati-nine 2.8 mg/dL and urea 71 mg/dL). Serological tests for HIV, syphilis, and hepatitis were non-reactive and her serum rheumatological tests (rheumatoid factor, antinuclear antibodies, and antineutrophil cytoplasmic antibody) were negative.
The day after admission, the otorhinolaryngology team performed an SPA drainage through external and endoscopic access. For intraorbital pressure relief, an incision was made in the upper eyelid. Drainage of a large volume of the purulent secretion and the paranasal sinuses was achieved via a functional sinus endoscopic surgery, with endoscopic manipulation of the lamina papyracea. Most of the secretion was sent to the laboratory for analysis and cultures. She showed gradual improvement in her general condition, eyelid edema, and renal function without the need for dialysis. Eye movements, previously limited to adduction and abduction, readily normalized. Nonetheless, immediately after the surgical procedure, visual acuity on the left was limited to hand movement and in the subsequent days she no longer perceived light. Four days after surgery, in an ophthalmological evaluation, an altered consensual photomotor reflex, a pupil with medium fixed mydriasis, and 16 mmHg intraocular pressure (normal range 10 mmHg to 21 mmHg) were observed in the affected eye. There were no changes in the right eye. She was unable to spontaneously open the left eyelid. The fundus of the left eye contained extensive intraretinal hemorrhages in all quadrants, disc edema, serous retinal detachment, and an abnormal vascular sheath, suggesting a combined thrombosis of the CRAO and CRVO.
She was hospitalized in our unit for 21 days and treated with a previously administered antibiotic therapy regimen (vancomycin with piperacillin and tazobactam). The secretions and purulent liquid drained at surgery had shown no growth in the laboratory analysis and cultures. She was treated for hypokalemia and hypomagnesemia of difficult management, as she needed intravenous repletion for 11 days. A series of laboratory tests were performed (complete blood cell count, electrolytes, inflammatory markers, creatinine, and urea). Her white blood cell count normalized after 14 days and there was a rapid drop in the inflammatory markers. Magnetic resonance imaging of the head performed 9 days after the surgical procedure showed persistent inflammation without a specific finding that explained visual loss. She was discharged in general good condition, with a significant reduction in facial and eyelid edema, and normal blood parameters. She was prescribed oral antibiotics for a further 14 days (amoxicillin with clavulanate 2 g/day).
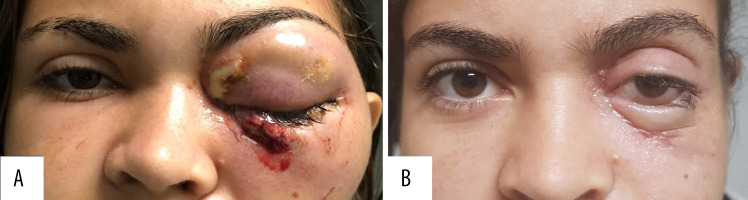
During the follow-up appointment on the 27th postoperative day, she presented with residual eyelid edema and normal ocular motricity, although she still had no perception of light or spontaneous opening of the left eye (Figure 3A, 3B). She exhibited the consensual photomotor reflex, but without reference to the left side. The conjunctiva had mild chemosis and punctate keratitis. She had no other concerns. Her last follow-up was 3 months after the surgery, when she reported no improvement in her left eye vision.
Figure 3.
(A) Patient on the first day of hospitalization. (B) Patient on the 27th postoperative day (already discharged).
We obtained informed consent from the patient and her legal guardian (mother) about this publication, as it is a rare case. We received approval from the Institutional Review Board for publication of this case report.
Discussion
We presented the case of an SPA secondary to ABRS, complicated with permanent vision loss. Despite the reduced visual acuity, which is a frequent patient concern (35% to 37%), only 4% of patients maintain it in the long-term [4], as seen in the present case. This complication is more frequent after post-septal cellulitis and with significant ocular proptosis; however, the exact mechanisms and factors that lead to blindness are still unconfirmed [6,7].
Reasons for this significant complication could be exposure keratopathy with ulcer formation, ischemia due to thrombophlebitis along the orbital veins without valves, and compression ischemia resulting in CRAO [4]. Other mechanisms include stretching of the vessels that nurture the optic nerve, ischemic optic neuropathy, and traction of the optic nerve [8,9].
CRAO, as suggested by the present patient’s fundoscopy, is a well-known complication of orbital cellulitis. Although uncommon, CRAO can be confirmed by delayed arterial filling observed in the fluorescein angiography; this was not available in our unit. CRVO due to inflammatory orbital disease is less common and less severe than CRAO and has slightly better visual outcomes. Despite few reports in the literature, it is possible to have both conditions simultaneously due to inflammatory or infectious conditions [6].
The tension in the orbit is a condition in which severe proptosis by compression of the intraorbital space leads to an irreversible stretching of the optic nerve and results in the deterioration of vision [10]. Proptosis is significant when the anterior distance to the interzygomatic line is >21 mm, as seen in the present case (27.7 mm) [11,12]. It can be associated with orbital compartment syndrome, in which increased intraorbital pressure results in impaired perfusion of the optic nerve and the eyeball [13]. Consequently, this acute increase in pressure caused by the mass effect of an SPA can result in the disturbance of retinal circulation, compressive and/or ischemic optic neuropathy, and traction of the optic nerve [9].
A 1989 analytical study correlated the posterior angle of the eyeball with increased proptosis and optic nerve extension in acute and subacute orbital pictures. Those with an angle between 120º and 130º had mild visual dysfunction and a good response to treatment; however, those with an angle <120º had a worse visual outcome [14]. In the present case, the patient would be in the second group, with a posterior angle of 117º, which could indicate a worse outcome.
The age of the patient in the present case is an important factor. Patients aged <9 years tend to have simpler and more responsive infections, while older children and adults have more complex infections from multiple organisms [4]. In the study by Patt and Manning, 4 out of 159 people were permanently blinded by orbital complications of ABRS; they were all >15 years old and had SPA [15]. In another study, 3 out of the 25 patients with orbital complications of ABRS required surgical intervention and developed irreversible blindness; they were all >9 years old [3]. Conforming with reported literature, the patient in the present case was a teenager (>9 years old) with a very complex infection, and she developed blindness despite the surgical intervention.
The delay in surgical intervention is a factor that can lead to less-than-optimum results [4,9]. A sudden increase in the intraorbital pressure can require early surgical intervention if the antibiotic is not effective and if there is an SPA finding on the CT [6,9]. In the study by Ismi et al, those with irreversible blindness had a longer time interval between the onset of symptoms and the surgical procedure; they concluded that ophthalmic symptoms for >2.5 days are a risk for irreversible loss of vision [3].
The recommended indications for surgical intervention by the most recent systematic review about the pediatric age group are age >9 years, frontal sinusitis, a large or non-medial SPA, suspected subperiosteal infection by anerobic pathogens, recurrent abscess after drainage, evidence of chronic sinusitis, acute involvement of the optic nerve or retina, and/or dental infection [16]. The patient in the present case was 17 years old, had a large, non-medial abscess suggesting an anerobic infection, and visual loss, and required urgent surgery. She had arrived at the hospital 6 days after the onset of symptoms and there is a possibility that this delay interfered with her visual prognosis. Another predictor of visual sequelae is the presence of comorbidities (diabetes, chronic kidney disease, immunosuppression, pregnancy) as they can affect the immune response. They can potentially increase the risk of irreversible blindness by 68.3% [3]. The patient in the present case did not have these conditions, yet she did not progress well.
Nowadays, irreversible blindness from an SPA is rare. Several mechanisms for this complication have been proposed; however, the factors that lead to it need further studies. In this case report, after reviewing the literature about the subject, we reinforce the importance of rapid surgical intervention when indicated, especially for patients with orbital symptoms for ≥2.5 days and patients who are >9 years old, as they tend to have more complex conditions.
Conclusions
We presented a case report of a periorbital abscess, which was a complication of ABRS that resulted in CRAO and CRVO. The patient developed irreversible blindness, probably due to the combined CRAO and CRVO. Despite being a rare condition, poor visual outcomes still occur and it is crucial to know the involved mechanisms and criteria for urgent surgical drainage.
Acknowledgments
Ophthalmology Reference Center (CEROF) from Federal University of Goiás (UFG).
Footnotes
Department and Institution Where Work Was Done
Head and Neck Unit, Department of Surgery, Federal University of Goiás, Goiânia, Brazil.
Conflicts of Interest
None.
References:
- 1.Fokkens WJ, Lund VJ, Hopkins C, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology. 2020;29:1–464. doi: 10.4193/Rhin20.600. [DOI] [PubMed] [Google Scholar]
- 2.Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80:1414–28. doi: 10.1288/00005537-197009000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Ismi O, Vayisog˘lu Y, Bal KK, et al. Surgical treatment of rhinosinusitis-related orbital complications: Factors affecting irreversible blindness. J Craniofac Surg. 2018;29(5):1294–99. doi: 10.1097/SCS.0000000000004531. [DOI] [PubMed] [Google Scholar]
- 4.Chaudhry IA, Al-Rashed W, Arat YO. The hot orbit: Orbital cellulitis. Middle East Afr J Ophthalmol. 2012;19(1):34–42. doi: 10.4103/0974-9233.92114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhola RM, Dhingra S, McCormick AG, et al. Central retinal artery occlusion following staphylococcal orbital cellulitis. Eye (Lond) 2003;17(1):109–11. doi: 10.1038/sj.eye.6700250. [DOI] [PubMed] [Google Scholar]
- 6.Keorochana N, Vongkulsiri S, Choontanom R. Combined central retinal vein, central retinal artery and cilioretinal artery occlusion with ischemic macular hole secondary to severe orbital cellulitis after black fly bite. Int Med Case Rep J. 2019;12:125–34. doi: 10.2147/IMCRJ.S189082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ozkurt FE, Ozkurt ZG, Gul A, et al. Managment of orbital complications of sinusitis. Arq Bras Oftalmol. 2014;77(5):293–96. doi: 10.5935/0004-2749.20140074. [DOI] [PubMed] [Google Scholar]
- 8.Dolman PJ, Glazer LC, Harris GJ, et al. Mechanisms of visual loss in severe proptosis. Ophthalmic Plast Reconstr Surg. 1991;7(4):256–60. doi: 10.1097/00002341-199112000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Okamoto Y, Hiraoka T, Okamoto F, et al. A case of subperiosteal abscess of the orbit with central retinal artery occlusion. Eur J Ophthalmol. 2009;19(2):288–91. doi: 10.1177/112067210901900219. [DOI] [PubMed] [Google Scholar]
- 10.Park CH, Jee DH, La TY. A case of odontogenic orbital cellulitis causing blindness by severe tension orbit. J Korean Med Sci. 2013;28(2):340–43. doi: 10.3346/jkms.2013.28.2.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sabharwal KK, Chouhan AL, Jain S. CT evaluation of proptosis. Indian J Radiol Imaging. 2006;16(4):683–88. [Google Scholar]
- 12.Sambasivarao K, Ushalatha B. Diagnostic Role of CT in the evaluation of proptosis. IOSR Journal of Dental and Medical Sciences. 2015;14(4):25–31. [Google Scholar]
- 13.Vohra V, Chawla H, Gupta M. Venous occlusion in a case of orbital cellulitis. Korean J Ophtalmol. 2016;30(6):483–84. doi: 10.3341/kjo.2016.30.6.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dalley RW, Robertson WD, Rootman J. Globe tenting: A sign of increased orbital tension. Am J Neuroradiol. 1989;10(1):181–86. [PMC free article] [PubMed] [Google Scholar]
- 15.Patt BS, Manning SC. Blindness resulting from orbital complications of sinusitis. Otolaryngol Head Neck Surg. 1991;104(6):789–95. doi: 10.1177/019459989110400604. [DOI] [PubMed] [Google Scholar]
- 16.Zhao EE, Koochakzadeh S, Nguyen AS, et al. Orbital complications of acute bacterial rhinosinusitis in the pediatric population: A systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol. 2020;135:110078. doi: 10.1016/j.ijporl.2020.110078. [DOI] [PubMed] [Google Scholar]