Abstract
Since December 2019, the global burden of the COVID-19 pandemic has increased rapidly and has impacted nearly every country in the world, affecting those who are elderly or with underlying comorbidities or immunocompromised states. Aim of this systematic review is to summarize lung histopathological characteristics of COVID-19, not only for diagnostic purpose but also to evaluate changes that can reflect pathophysiological pathways that can inform clinicians of useful treatment strategies. We identified following histopathological changes among our patients:: hyaline membranes; endothelial cells/ interstitial cells involvement; alveolar cells, type I pneumocytes/ type II pneumocytes involvement; interstitial and/ or alveolar edema; evidence of hemorrhage, of inflammatory cells, evidence of microthrombi; evidence of fibrin deposition and of viral infection in the tissue samples.
The scenario with proliferative cell desquamation is typical of Acute Respiratory Distress Syndrome (ARDS) that can be classified as diffuse alveolar damage (DAD) and not DAD-ARDS. The proposed pathological mechanism concerns the role of both innate and adaptive components of the immune system. COVID-19 lethal cases present themselves as a heterogeneous disease, characterized by the different simultaneous presence of different histological findings, which reflect histological phases with corresponding different pathological pathways (epithelial, vascular and fibrotic changes), in the same patient.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13027-021-00369-0.
Keywords: COVID-19, Histopathology, Lung, Therapy, Systematic review
Introduction
Since December 2019, the global burden of COVID-19 pandemic has risen rapidly and impacted almost all countries worldwide. Among the wide number of infective diseases, Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-Cov2) emerged to be a global burden with 123,636,852 cases of infected and 2,721,891 deaths (https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases). Though majority recovery from this infection, those who are elderly or with underlying comorbidities, frail or immunocompromised states face severe outcomes including Acute Respiratory Distress Syndrome (ARDS), ICU (Intesive Care Unit) admissions, use of ventilator and deaths [1]. Although the majority of patients heal by itself, it is estimated that 13.8% of infected is at risk of severe disease and up to 6.1% can be involved by a critical form of COVID-19 disease, with respiratory failure, septic shock and multiple organ dysfunction or failure (https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf).
Immune system encompasses a wide range of cellular and chemical messages to deal with pathogens. Both immune system and pathogens characteristics, act in causing damage to the surrounding tissue [2]. In Europe, COVID-19 disease outbreak involved above all Spain and Italy with 182,816 and 168,941 cases respectively, while reporting a higher number of deaths (10.5%; 13.12%). In Italy, in the most affected regions, the lethality rate reached very high peaks with the maximum peak of 18.48% in Lombardy on 17/04/2020, (http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1) while the average case fatality rate of the same day was of 13,19% (http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1). Government actions, above all social distancing, decreased virus spread, improving the general situation in Europe, meanwhile in USA, India and Brazil the number of new cases is still exponentially growing, with 48,354; 161,736 and 37,017 new cases respectively (https://covid19.who.int/).
Reasons related to this discrepancy are still unclear. Multiple factors may lead to differences in rates of infection and mortality across regions. For e.g. it has been supposed that virus, while infecting Europe, may have mutated and become more aggressive [3–7], while mutation dynamics analysis showed a relative stable genetic sequence and a low rate mutation [8]. In addition, characteristics of populations have to be accounted [4]. Further underlying medical and healthcare system, access to health care facilities and ventilators as well as treatment protocols might have resulted into these differences. At last, different therapy protocols could modify the interaction between virus and host, changing the disease evolution [9–12]. For example, chloroquine and ribavirin were shown to decrease viral infection in vitro, although considering a wide range of adverse effects [13]. In vitro studies might suggest the use of higher doses considering a virus-based approach, with consequences on side effects without evaluating the host-based effect on inflammatory response. Many compounds have shown relevant virus-based efficacy in-vitro models but with several limitations on clinical reproducibly. For example, some of them requires high EC50/Cmax ratios at clinically relevant dosages, with consequences of side effects like immunosuppression [14]. Failing of some therapies furthermore, can be associated to a delay on drug administration in relation to symptoms occurrence or lack of availability to the masses or differences in efficacy and effectiveness in specialized subgroups of population [14, 15].
SARS-Cov2 belongs to the family of coronavirus together with Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS). Little is known of the impact of SARS-CoV2 on lung tissue damage. The aim of this work is to critically review histopathological findings of COVID-19, focusing on pathological mechanisms, in order to suggest a target therapy approach, virus or host-based.
Methods
Protocol and registration
This systematic review has been carried out following the “Preferred Reporting Items for Systematic Reviews and Meta Analyses” (PRISMA) guidelines [16]. Prospectively, the protocol for this systematic review has been registered on International prospective register of systematic reviews (PROSPERO) with the following registration code: CRD42020182279.
PICO question
PICO (Population, Intervention, Comparison and Outcome) question was relevant to assess: Population (such as patients diagnosed of COVID-19 disease), Intervention (undergoing histopathological examination), Control (not applicable) and Outcome (histopathological changes related to SARS-Cov-2 infection).
The formulation of the PICO question was as follows: what are the histopathological changes in lungs of patients affected by SARS-COV-2 infection during COVID-19 disease?
PICO highlighted limitation of the current study, since a comparison control group was missing in the included studies (case reports/case series).
Eligibility criteria
We took into consideration studies written and published in English language only. Only clinical studies were included, reporting, in both prospective and retrospective case reports, case-series and cohort studies, the histopathological findings in lungs of patients with confirmed death of COVID-19 disease because of SARS-Cov2 infection. Studies to be included had to report an accurate description of histopathological changes/images or reported through their autopsy reports.
At last, studies performed in vitro, in animal models or lacking evidence of SARS-Cov2 infection were excluded from this systematic review.
Information sources and search strategy
Two authors (I. S. D. S. and M. A. R.) independently carried out an online bibliographic search through PubMed and Web of Science. This search started on April 1st 2020 and was continued every day before the last search on 1st June 2020, because of the high number of articles published daily about COVID-19 disease. MeSH terms and free text words were combined using Boolean operators (AND, OR). The following search string was used and input in the search bars of the previous reported databases: (COVID-19 OR SARS-Cov2) AND (histopathological finding OR paraffin OR pathology OR histopathology OR autopsy).
Screening, study selection and data collection process
All searches from our databases were put in excel sheets designed for title and abstract screening. Screening of target studies was performed independently by two authors (I. S. D. S. and M. A. R.) through all the resulting research articles. We calculated Cohen’s kappa to calculate interrater reliability in screening process between two reviewers. A score of 0.71 represents good agreement between reviewers. In case of disagreement, during the screening and selection process, a third reviewer (A. A.) took the final decision through mutual consensus in a joint discussion Studies meeting the previous reported inclusion criteria, proceeded to full text review and data abstraction. M. M. and A. A. reviewed and completed the full text abstraction. Following information were retrieved from each article: Author’s first name, Year of publication, Country, number of patients, mean age, sex, comorbidities, hyaline membranes, comorbidities, evidence of endothelial cells / interstitial cells involvement, presence or absence alveolar cells, type I pneumocytes/ type II pneumocytes involvement, evidence of inflammatory cells, sampling methods for histopathological examination, detection methods, evidence of microthrombi, evidence of hemorrhage, fibrin deposition, interstitial/alveolar edema and viral detection method within the cells. A. A. and M. M performed the data extraction.
Risk of bias assessment
Included studies underwent quality check and risk of bias assessment. This qualitative analysis was performed according Murad’s quality checklist of case series and case report [17]. As reported, the scale consists of four parameters, to evaluate the a) patient selection; b) exposure ascertainment; c) causality and d) reporting. Each section contains one to four question to be addressed. As it is suggested we performed an overall judgement about methodological quality since questions 4, 5 and 6 are mostly relevant to cases of adverse drug events. Each requested field will be considered as adequate, inadequate or not evaluable. The table showing this tool for evaluating the methodological quality of case reports and case series, is reported in the original manuscript [17].
Results
Study selection
Last search was performed on 01/06/2020, reporting a total of 852 records on PubMed database and 356 on Web of Science. These records were screened only by title and abstract and a total number of 98 articles passed the first selection process. Resulting records underwent full-text reading to meet the inclusion criteria. After this last step, a total of 27 articles fulfilled the inclusion criteria and were included in the quality and synthesis. Prisma Flowchart summarizing the selection process is reported in Fig. 1, studies and reasons for exclusion are collected in supplemental Table 1. The level of agreement between reviewers in the selection process was good since the K-agreement statistic reported a value of 0.71.
Fig. 1.
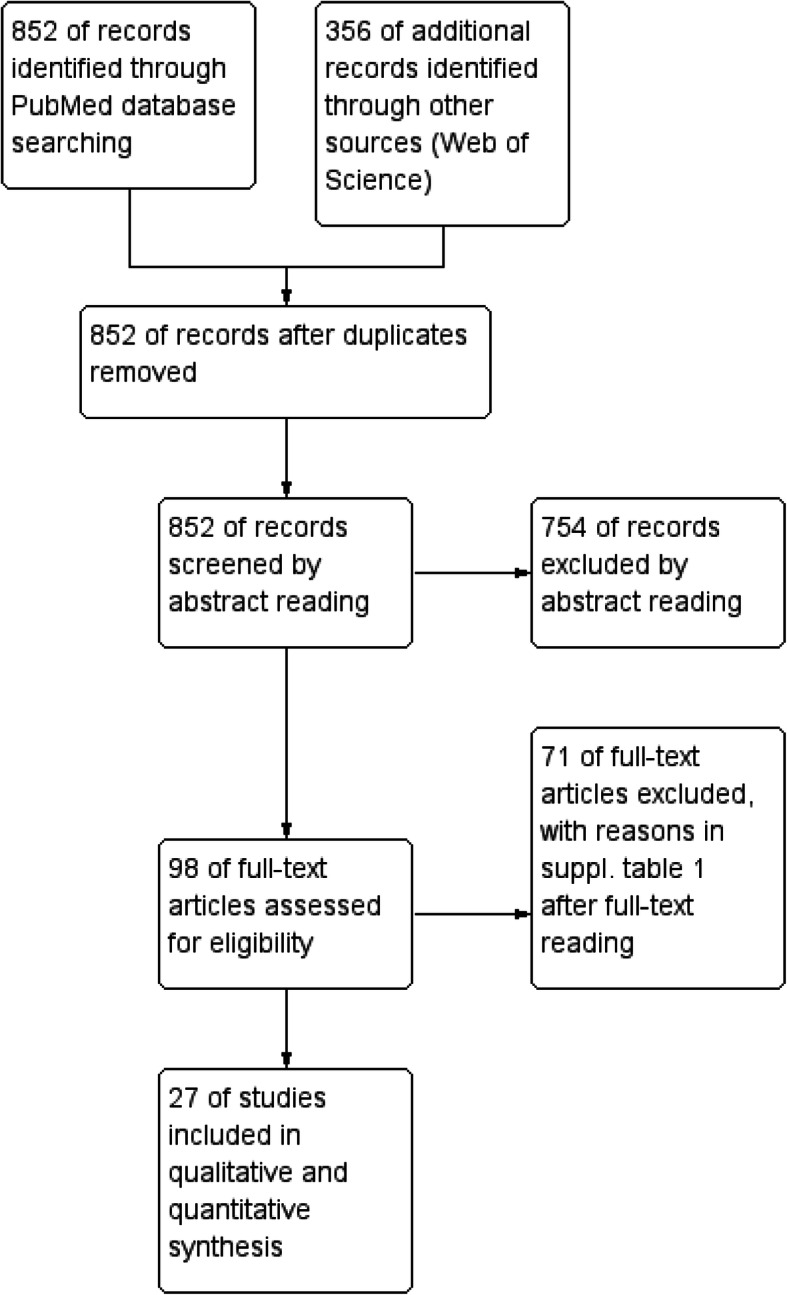
PRISMA Flowchart of selection process
Characteristics of included studies and methodological quality assessment
A total number of 196 patients, who died of COVID-19 disease, underwent surgical specimen resection through biopsy (Yao et al. [18]; Xu et al. [19]; Varga et al. [20]; Harkin et al. [21]; Li et al. [22]; Shao et al. [23]; Pernazza et al. [24]; Tian et al. [25]; Tian et al. [26]; Cai et al. [27] and Zeng et al. [28]) or post-mortem autopsy (Fox et al. [29]; Lacy et al. [30]; Menter et al. [31]; Barton et al. [32]; Karami et al. [33]; Magro et al. [34]; Lax et al. [35]; Adachi et al. [36]; Yan et al. [37]; Ackermann et al. [38]; Schaller et al. [39]; Martines et al. [40]; Buja et al. [41]; Sekulic et al. [42]; Aguiar et al. [43] and Konopka et al. [44]) to assess histopathological changes in lung parenchyma. Most of studies were performed in China [18, 19, 22, 23, 25–28, 30], together with USA [21, 29, 32, 34, 37, 40–42, 44]. Seven studies were performed in Europe [20, 24, 31, 35, 38, 39, 43], while remaining ones were performed in Japan [36] and Iran [33]. Of these 196 patients, 66 were females,. Comorbidities were reported in most of patients. Only one patient reported no comorbidities [23] meanwhile six studies did not reported [18, 19, 21, 33, 36, 38]. In general, most commonly reported systemic diseases were diabetes, obesity, hyperlipidemia, hypertension and cardiovascular disease. Some patients reported concomitant lung diseases, such as lung adenocarcinoma [24, 26, 27] or Chronic Obstructive Pulmonary Disease (COPD) [22, 27, 31]. Population characteristics are summarized in Table 1.
Table 1.
List of included studies and data extraction
| Author (year) | Country | Patients (n) | Mean age (years) | Sex (M/F) | Comorbidities | Hyaline membranes | Endothelial cells alteration (ECA), interstitial cells involvement (ICI) | Alveolar cells: Type I pneumocytes/ Type II pneumocytes involvement | Hemorrhage | Sampling methods | Detection methods | (Micro)thrombi | Inflammatory cells | Fibrin deposits | Interstitial/ alveolar edema | Viral detection methods |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Li et al. (2020) [22] | China | 69 | 51 | M/F 40/29 | Diabetes (8), hypertension (17), coronary disease (4), chronic liver disease (7), chronic respiratory system disease (7), malignancy (1) | Reported (2) | ICI | DAD, pneumocyte hyperplasia, desquamation of pneumocytes | NA | Biopsy | H&E, Masson’s trichrome stain, IHC, EM | NA | CD68+ macrophages, neutrophils, CD4 + and CD8+ T cells | NA | Focal exudative edema | Yes, EM, ISH |
| Buja et al. (2020) [41] | USA | 23 | 55 | M/F 12/7 | Obesity, hypertension, myotonic dystrophy, type II diabetes | Absent | ICI | Type I,II pneumocytes hyperplasia | Reported | Autopsy | RT-PCR | Formation of microthrombi in arterioles | Neutrophils, lymphocytes, macrophages | Intra-vascular and intra-vascular edema | Reported | Yes, EM |
| Menter et al. (2020) [45] | Switzerland | 21 | 76 | M/F 17/4 | Hypertension (21), cardiovascular disease (15), diabetes mellitus (7), COPD (3), chronic neurological conditions (5), malignancy (3), chronic liver disease (2), chronic kidney disease (4), acquired immunosuppression (1) | Reported | Capillary congestion (21), vasculitis (1) | Syncytial cells of pneumocytes II origin (11), DAD (8) | Reported (3) | Autopsy | IHC for fibrin, 360x, H&E, IHC | Microthrombi of alveolar capillaries (5) | Prominent lymphoid infiltrate (3) | NA | Interstitial edema | Yes, SARS-CoV-2 specific RT–qPCR, viral genome detected with the TaqMan 2019-nCoV Assay Kit v1 (Thermo Fisher Scientific) targeting three different viral genomic regions (ORFab1,S Protein, N Protein) |
| Lax et al. (2020) [35] | Austria | 11 | 81 | M/F 8/3 | Diabetes mellitus, cardiovascular disease | Reported (11) | ICI, fibroblast proliferation (9) | Pneumocytes proliferation (9) | Reported (8) | Resection | H&E | Reported (11) | Macrophages, lymphocytes, plasma cells, neutrophils | Reported | Reported (10) | Yes, RT-PCR results positive in the right and left bronchus ´10/10) |
| Fox et al. (2020) [29] | USA | 10 | 61 | NA | At least one comorbidity, the most common: hypertension, type II diabetes, obesity | Reported (2) | ICI, CD61+ megakaryocytes with nuclear hypercromasia and atypia | DAD (10), desquamation | Foci of hemorrhage (9) | Autopsy | H&E | Reported (11) | CD4+ and CD8+ lymphocytes | Reported | Reported (2) | DRAQS and SYTO RNASelect fluorescent staining |
| Schaller et al. (2020) [39] | Germany | 10 | 79 | M/F 7/3 | Hypertension, hypothyroidism, diabetes | Reported | ICI, fibroblastic cells | Pneumocytes hyperplasia | NA | Autopsy | IHC | Microthrombireported | Lymphocytes | Reported | Alveolar edema | Yes, RT-PCR, IHC |
| Martines et al. (2020) [40] | USA | 8 | 74 | M/F 4/4 | Hypertension, chronic kidney disease, diabetes, obesity | NA | NA | Type II pneumocytes hyperplasia | Reported | Autopsy | IHC, H&E | Microthrombi observed | Macrophages, neutrophils, leukocytes | Reported | Alveolar edema | Yes, IHC (rabbit polyclonal antibody), RT-PCR |
| Ackermann et al. (2020) [46] | Germany | 7 | 73 | M/F 5/2 | NA | NA | ECA | Type II pneumocytes hyperplasia | Reported | Autopsy | IHC, scanner election microscopy | Fibrin thrombi | T lymphocytes | Intra-alveolar fibrin | Mild interstitial edema | No |
| Cai et al. (2020) [27] | China | 7 | 60 | M/F 5/2 | Interstitial lung disease (1), coronary atherosclerosis (3), chronic obstructive pulmonary disease (2), hyperlipidemia | Absent (1) | ICI, fibrous connective tissue proliferation | No evident pneumocytes hyperplasia (1) | NA | Biopsy | H&E | NA | Plasma cells and macrophages (1) | NA | NA | No |
| Magro et al. (2020) [34] | USA | 5 | 55 | M/F 3/2 | Coronary heart disease, diabetes, hepatitis C | Reported | ICI | Type II | Reported | Biopsy | IHC,RT-PCR | Reported | AP and LP of complement | Reported | Reported | Yes, using NUANCE software |
| Tian et al. (2020) [47] | China | 4 | 73 | M/F 3/1 | Chronic lymphocytic leukemia, cirrhosis, variceal rupture bleeding, diabetes, hypertension, status post renal transplantation for 3 months | Reported (3) | ICI, fibrinoid necrosis of the small vessels | DAD, type II hyperplasia, syncytial giant cells formation pneumocytes | Reported | Biopsy | H&E, IHC | NA | scanty inflammatory cells | Reported | NA | Yes, RT-PCR positive only in case 2 |
| Varga et al. (2020) [20] | Switzerland | 3 | 66 | M7F 2/1 | Coronary heart disease, hypertension, diabetes, obesity | NA | ECA | NA | NA | Biopsy | IHC | NA | Mononuclear cells, apoptotic bodies | NA | Reported | Yes, EM in kidney and small bowel tissue but no obvious viral particles in the lung tissue |
| Barton et al. (2020) [48] | USA | 2 | 60 | M/F 2/0 | Hypertension, remote deep veins thrombosis, myotonic dystrophy | Reported | Congestion of septal capillaries | DAD in the acute stage (only in one case) | NA | Autopsy | IHC, H&E | Microthrombi reported | CD3+ T lymphocytes, rare CD20+ lymphocytes, CD8+ T lymphocytes, macrophages, non appreciated neutrophils oreosinophils | NA | Reported | Bilateral lung parenchymal swabs positive only in one case |
| Tian et al. (2020) [26] | China | 2 | 79 | M/F 1/1 | Lung adenocarcinoma | Not prominent | ICI, proliferating fibroblasts 1 case) | NA, type II pneumocytes hyperplasia (1 case) | NA | Autopsy | H&E | NA | Mononuclear inflammatory cells | Focal fibrin exudates | Alveolar edema | No |
| Sekulic et al. (2020) [42] | USA | 2 | 68 | M/F 2/0 | Diabetes mellitus relates renal disease … left ventricular hypertrophy, atherosclerotic coronary artery disease, hypertension, congestive splenomegaly, sinusoidal congestion of the liver | Reported (2) | fibroblastic proliferation | DAD, scattered multinucleated giant cells, squamous metaplasia features of type II pneumocytes viral infection | NA | Autopsy | H&E, EM | NA | Relative paucity of chronic inflammatory cells | Intra-alveolar fibrin deposition | Interstitial edema | Yes, PCR (2) |
| Yao et al. (2020) [18] | China | 1 | 78 | M/F 0/1 | NA | Reported | ICI | Type II; DAD with desquamation or proliferative type II cells | NA | Biopsy | PCR(X3), IHC, H&E | Hyaline thrombi in micro vessels | Macrophages, CD8+ and CD4+ T cells, CD20+ cells | Reported | No pulmonary edema | Yes, EM, IHC with monoclonal anti-nucleoprotein antibody |
| Lacy et al. (2020) [49] | China | 1 | 58 | M/F 0/1 | Type II diabetes, obesity, hypertension | Reported | ICI, no fibroblastic foci | NA, pneumocyte hyperplasia, no viral inclusion or specific cytopathic changes,focal multinucleated cells | Reported | Autopsy | RT-PCR | NA | Macrophages | Reported | Diffuse proteinaceous edema | No viral inclusion or cytopathic changes identified |
| Xu et al. (2020) [19] | China | 1 | 50 | M/F 1/0 | NA | Reported | NA | Desquamation, early ARDS, atypical enlarges pneumocytes with large nuclei, amphophilic granular cytoplasm and prominent nucleoli. No obvious intranuclear or intracytoplasmic viral inclusion identified | NA | Biopsy | NA | NA | Lymphocytes | NA | Reported | No obvious viral inclusion identified |
| Karami et al. (2020) [33] | Iran | 1 | 27 | M/F 0/1 | NA | Reported | NA | Pneumocyte proliferation, multinucleation and nuclear atypia, metaplastic changes | NA | Autopsy | NA | NA | Lymphocytes and macrophages | NA | NA | Yes, RT-PCR confirmed SARS-CoV-2 infection in the lungs |
| Harkin et al. (2020) [21] | USA | 1 | 34 | M/F 1/0 | NA | Absent | NA | Type II pneumocytes hyperplasia | NA | Autopsy | RT-PCR | NA | Lymphocytes, hystiocytes | Intra-alveolar fibrin deposits | NA | Yes, RT-PCR positive in BAL |
| Shao et al. (2020) [50] | China | 1 | 65 | M/F 1/0 | Absent | Reported | ICI, proliferating fibroblasts, dilated pulmonary capillaries | DAD, type II pneumocyte multinucleation, hyperplasia and increased nuclear size, hypercromasia, hyperplasia of alveolarepithelial cells | NA | Biopsy | IHC, GMS | Reported (11) | Lymphocytes, neutrophils, macrophages | Intra-alveolar fibrin exudate | NA | No, IHC staining for anti-SARS-Cov-2 N Protein was negative |
| Adachi et al. (2020) [36] | Japan | 1 | 84 | M/F 0/1 | NA | Reported | ICI, vascularcongestion | Type II pneumocytes hyperplasia, squamous metaplasia, desquamation | Intra-alveolar hemorrhage | Autopsy | H&E, IHC | NA | Plasma cells | NA | NA | Yes, rabbit polyclonal antibodies |
| Yan et al. (2020) [37] | USA | 1 | 44 | M/F 0/1 | Obesity | Reported | Non necrotizing lymphocytic vasculitis | DAD, desquamation, pneumocytes with ample cytoplasm and enlarged nuclei | NA | Autopsy | EM | Not identified | Lymphocytes | Fibrin aggregates within blood vessels | NA | No |
| Pernazza et al. (2020) [51] | Italy | 1 | 61 | M/F 1/0 | Lung adenocarcinoma | Absent | ICI | Pneumocytes desquamation, reactive hyperplasia with focal nuclear inclusion | Diffuse hemorrhage | Biopsy | H&E, IHC | NA | inflammatory infiltrate mainly composed by cytotoxic (CD8+) T lymphocytes, neutrophilic vascular margination, macrophages | Scanty fibrin deposited on the alveolar surface | Interstitial edema | No |
| Aguiar et al. (2020) [43] | Switzerland | 1 | 31 | M/F 0/1 | Obesity, hypertension, myotonic dystrophy, type II diabetes | Reported | Vascular stasis, reported megakaryocytes | DAD, type II pneumocytes hyperplasia neither viral inclusion nor giant multinucleated giant cells | Hemorrhagic edema, alveolar hemorrhage | Autopsy | H&E, IHC | Absence of hyaline thrombi in microvessels | intra-alveolar macrophages, PMN, T (CD3+) lymphocytes | Intra-alveolar fibrin deposition | Reported | Yes, rRT-PCR in the lower respiratory tract |
| Konopka et al. (2020) [44] | USA | 1 | 37 | M/F 1/0 | Asthma, type II diabetes | Scattered hyaline membranes | ECA | DAD, mucous plugs, mucous glands, hyperplasia, type II pneumocytes hyperplasia | NA | Autopsy | H&E | Rare within small vessels | scattered neutrophils | Fibrin-airspace exudate | Reported | No |
| Zeng et al. (2020) [28] | China | 1 | 55 | M/F 0/1 | Pulmonary node | Not observed | ICI | Type II pneumocytes hyperplasia | NA | Lobectomy | H&E | NA | Monocytes, T (CD3+), B (CD20 + and PAX5+) lymphocytes, (MUM1+) plasma cells, CD4+ helper and CD8+ cytotoxic lymphocytes, natural killer (CD56+) macrophages, (CD163+) M2 macrophages | Not observed | Reported | Yes, PCR, in situ hybridization technology |
Main histopathological reported findings of Covid-19 related lung disease
Main histopathological changes of Covid-19 related lung disease were reported as presence of following histopathological changes:: hyaline membranes; endothelial cells / interstitial cells involvement; alveolar cells, type I pneumocytes/ type II pneumocytes involvement; interstitial and/or alveolar edema; evidence of hemorrhage; evidence of inflammatory cells; evidence of microthrombi; evidence of fibrin deposition and evidence of viral infection in the tissue sample.
Hyaline membranes
Hyaline membranes were reported in 19 (21, 22, 25, 26, 28, 32–40, 42, 45–47) out of 27 included studies representing a histological report in almost 80% of studies performed on lethal cases of COVID-19 disease. In one study, including two patients, hyaline membranes were reported to be not prominent [26] or scattered [44]. Therefore, while three studies did not report any information about this parameter [20, 38, 40], hyaline membranes were reported in 19/24 of included studies representing a histological report in almost 80% of studies performed on lethal cases of COVID-19 disease.
Interstitial cell involvement
Interstitial cell involvement was commonly reported in seven studies [18, 22, 28, 30, 34, 41, 42]. Interstitial cell involvement, associated with fibroblast proliferation, was reported in Tian et al. and Lax et al. studies [26, 35]. Schaller et al. also reported interstitial cell involvement with fibroblast proliferation [39], together with Sekulic et al. [42]. Cai et al. reported interstitial cell involvement and fibrous connective tissue proliferation [27]. Interstitial cell involvement together with CD61+ megakaryocytes with hyperchromatic nuclei and atypia was reported in Fox et al. study [29]. Endothelial cell alteration (ECA) was reported by Menter et al. as capillary congestion in all included patients (twenty-one), meanwhile only one patient reported vasculitis [31]. Congestion, specifically of septal capillaries, was reported in two patients in Barton et al. [32]. Ackermann et al., Varga et al. and Konopka et al. reported generic ECA [20, 38, 44], meanwhile Yan et al. reported non-necrotizing lymphocytic vasculitis. At last, Aguiar et al. reported vascular stasis with megakaryocytes [43].
Both, interstitial cell involvement and ECA, were reported in three studies [23, 25, 36]. In Xu et al., Karamy et al., Harkin et al. and Martines et al. studies, interstitial cell involvement and ECA were not investigated [21, 33, 40].
A wide spectrum of epithelial alterations was reported involving alveolar cells, above all type II pneumocytes. Specifically, some studies attributed hyperplasia to type II pneumocytes, describing DAD with desquamation of proliferative cells [18, 19, 22, 24, 28, 29, 36, 37, 43, 44] and syncytial cell formation [25, 31]. Karami et al., Adachi et al. and Sekulic et al. reported metaplastic changes associated to multinucleation and nuclear atypia [33, 36, 42]. Varga et al. did not report any information [20]; Cai et al. stated no evidence of pneumocyte hyperplasia [27]. In total 19 studies reported epithelial changes consistent with epithelial histological pattern of acute lung injury.
Alveolar edema
Another characteristic of lung tissue damage is the interstitial or alveolar edema. Well defined interstitial edema was reported in four studies [24, 31, 38, 42]. Lacy et al. described diffuse proteinaceous edema [30], meanwhile most of authors reported generic edema [19, 20, 22, 28, 29, 32, 34, 35, 41, 43, 44]. Alveolar edema was found in few reports [26, 39, 40]. In Yao et al. record there was no pulmonary edema [18]. These features were not evaluated in the remaining studies [21, 23, 25, 27, 33, 36, 37].
Hemorrhage
. Twelve studies reported events of hemorrhage [25, 30, 31, 34, 35, 38, 40, 41, 43], with different severity ranging from intra-alveolar hemorrhage [36], focal [29] to diffuse [24]. By evaluating studies that reported these events, almost 45% of studies with lethal cases of COVID-19 disease presented this histological finding.
Inflammatory cells
Macrophages were the most abundant cell-type, reported in 13 over 27 studies [18, 21, 23, 24, 27, 28, 30, 32, 33, 35, 40, 41, 43]. Lymphocytes were the second most abundant kind of inflammatory cell infiltration [19, 21, 23, 28, 29, 33, 35, 37, 39, 41, 43]. In Ackermann et al. report there was evidence of T-cell infiltration [38], while Yao et al. describe both T- and B-cell infiltration. Patients displayed also plasma cells [27, 35, 36] and neutrophil infiltration [23, 35, 40, 41, 44]. A nonspecific lymphoid infiltrate was indicated in four studies [20, 26, 31, 34]. Moreover, some studies reported a deeper analysis of inflammatory cell infiltration. Yao et al. highlight the presence of macrophages, CD8+ and CD4+ T cells and CD20+ B cells [18], meanwhile in Barton et al. samples there was evidence of CD3+ T lymphocytes, rare CD20+ B lymphocytes, CD8+ T lymphocytes and CD4+ T cells, macrophages, while neutrophils or eosinophils were not appreciated [32]. Li et al. also reported CD68+ macrophages, neutrophils, CD4+ and CD8+ T cells [22]. Inflammatory infiltrate mainly composed by cytotoxic (CD8+) T lymphocytes, neutrophilic vascular margination and macrophages were descripted by Pernazza et al. [24]. Zeng et al. performed a detailed analysis of lymphoid infiltrate, demonstrating evidence of monocytes, T (CD3+), B (CD20+ and PAX5+) lymphocytes, (MUM1+) plasmacells, CD4+ helper and CD8+ cytotoxic lymphocytes, natural killer (CD56+), (CD68+) macrophages and (CD163+) M2 macrophages.
At last, Tian et al. [25] and Sekulic et al. [42] were the only one reporting scanty inflammatory cells.
Microthrombi
Microthrombi were reported in twelve studies [18, 23, 29, 31, 32, 34, 35, 38–41, 44]. Yao et al. descripted hyaline thrombi in microvessels, while were found as fibrin thrombi in Ackermann et al. study [18, 38]. Menter et al. reported evidence of microthrombi of alveolar capillaries [31].
Fibrin deposits
Another important histopathological change was fibrin deposits. These were descripted mainly as intra-alveolar [21, 23, 37, 38, 42, 43], in addition Buja et al. reported the contemporary presence of extravascular deposits [41]. In one study, scanty fibrin deposits were reported on the alveolar surface [24].
Representation of main histological features of COVID-19 in lung tissue pathology are collected in Fig. 2.
Fig. 2.
Summary of histopathological features occurring in fatal cases of COVID-19 lung injury. Findings of epithelial, vascular and fibrotic pattern are represented. Note that epithelial damage like viral cytopathic changes, desquamation and reactive hyperplasia of type II pneumocytes, hyaline membrane formation and interstitial inflammatory response have been frequently observed together with findings of vascular damage like capillary congestion, intracapillary microthombosis, alveolar hemorrhage, interstitial and intra-alveolar edema. Furthermore, interstitial fibrous changes, occurring separately or in combination with epithelial and/or vascular injury in a subgroup of patients, are shown. For further details see descriptive text
SARS-Cov2 in lung tissue: Histopathological examination
Last evaluated parameter was the confirmation of SARS-Cov2 in the lung tissue. This exploration was performed through different techniques. Yao et al. carried out electronic microscope investigation together with IHC with monoclonal anti-nucleoprotein antibody [18]. In Xu et al. and Lacy et al. studies there were no viral inclusion or cytopathic changes [19, 30]. Menter et al. investigated through SARS-CoV2 specific qRT-PCR, viral genome detected with the TaqMan 2019-nCov Assay Kit v1 (Thermo Fisher Scientific) targeting three different viral genomic regions (ORFab1, S Protein, N Protein) [31]. Barton performed the inspection on bilateral lung parenchymal swab [32]. qRT-PCR analysis was the most common methodology [21, 25, 28, 33, 35, 39, 40, 42, 43], followed by IHC and FISH [18, 22, 23, 28, 29, 39, 40]. Buja et al. investigated through electronic microscope [41].
Risk of bias assessment
Results from quality and risk of bias assessment are summarized in Table 2. Briefly, only four studies fulfilled the quality checklist [22, 29, 34, 35]. Only one study [21] failed in “domains - leading explanatory questions” since the aim of the study was to report the delay in COVID-19 disease diagnosis. “Selection - Does the patient(s) represent(s) the whole experience of the investigator (center) or is the selection method unclear to the extent that other patients with similar presentation may not have been reported?” checklist resulted unclear in most of studies, because the patient selection method was unclear [18–21, 23, 26–28, 30–33, 36, 37, 40–44]. In general, overall quality was satisfactory in all included studies, but Varga et al. [20], where exposure to SARS-Cov2 was not ascertained, together with Ackermann et al. study [38]. Konopka et al. reported a positive test results for SARS-Cov2 without method and material details. A complete report of quality checklist is reported in Table 2.
Table 2.
Qualitative evaluation of included study to assess the risk of bias
| Author | Country | Domains | Selection | Ascertainment (1) (2) | Casuality | Reporting | |
|---|---|---|---|---|---|---|---|
| Yao et Al. | China | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Lacy et Al. | China | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Menter et al. | Switzerland | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Barton et Al | USA | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Xu et al. | China | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Karami et Al. | Iran | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Varga et al. | Switzerland | Ascertained | Unclear | Unclear | Ascertained | Unclear | Ascertained |
| Magro et al. | USA | Ascertained | Ascertained | Ascertained | Ascertained | Ascertained | Ascertained |
| Pernazza et al. | Italy | Ascertained | Ascertained | Ascertained | Ascertained | Unclear | Ascertained |
| Ackermann et al. | Belgium | Ascertained | Ascertained | Unclear | Ascertained | Ascertained | Ascertained |
| Harkin et al. | USA | Unclear | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Fox et al. | USA | Ascertained | Ascertained | Ascertained | Ascertained | Ascertained | Ascertained |
| Tian et al. | China | Ascertained | Ascertained | Ascertained | Ascertained | Unclear | Ascertained |
| Tian et al. | China | Ascertained | Unclear | Ascertained | Ascertained | Unclear | Ascertained |
| Shao et al. | China | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Buja et al. | USA | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Li et al. | China | Ascertained | Ascertained | Ascertained | Ascertained | Ascertained | Ascertained |
| Yan et al. | USA | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Adachi et al. | Japan | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Schaller et al. | Germany | Ascertained | Ascertained | Ascertained | Ascertained | Ascertained | Unclear |
| Martines et al. | USA | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Lax et al. | Austrai | Ascertained | Ascertained | Ascertained | Ascertained | Ascertained | Ascertained |
| Cai et al. | China | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Sekulic et al. | USA | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Aguiar et al. | Switzerland | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
| Konopka et al. | USA | Ascertained | Unclear | Unclear | Ascertained | Ascertained | Ascertained |
| Zeng et al. | China | Ascertained | Unclear | Ascertained | Ascertained | Ascertained | Ascertained |
Discussion
Despite the high lethality and mortality of SARS-CoV-2 infection, very limited research exists on histological aspects of COVID-19 disease in the literature. Some histological aspects have been described because there was no awareness of the infection and patients had been operated on for other reasons [21, 24]. In most of cases, autopsy procedures were not performed because of high standard security protocols needed, since, as reported by Zhou et al., viral shedding continues until death among people who passed away from COVID [52]. However, histopathology is still considered the gold standard procedure to assess for pathological changes across a broad range of diseases [53]. In this scenario, the aim of this systematic review is to provide summarizing lung histopathological characteristics of COVID-19 disease, not only for diagnostic purpose but also to evaluate changes that can reflect physio-pathological pathways that can inform clinicians of useful treatment strategies.
From this systematic review, lung injury itself reflects histopathological alterations including alveolar and interstitial alterations, type II pneumocyte hyperplasia and cytological atypia, with hyaline membrane formation, while only around 20% of studies with lethal cases of COVID-19 disease showed fibroblast proliferation. Generally, this scenario is typical of ARDS, with desquamation of proliferative cells and follows the clinical diagnostic criteria of the Berlin definition [54]. Histologically, ARDS can be classified as DAD and non-DAD-ARDS [55]. Both Guerin and Thille showed a mean association of clinical ARDS with DAD, respectively in 58 and 56% of patients, with an increase of this association up to 69% in patients with severe forms of ARDS [56, 57].
Although many studies shared histopathological evidence of DAD, only nine studies reported diagnostic clinical criteria of ARDS, for which patients died [19, 22, 29, 33, 34, 37, 38, 41, 44]. Different studies [19, 58, 59] suggest the use of corticosteroid to prevent ARDS evolution. Specifically in COVID-19 disease; Raju et al. in their systematic review and meta-analysis of registered trials reported promising results of corticosteroids in the treatment of severe form of COVID-19 disease, although highlighting limitations [60]. Sarma et al. performed a similar study by investigating the use of steroids in the management of diverse forms of severity of the disease. In this meta-analysis emerged that patients with severe disease benefitted of steroids therapy, reducing mortality and the need of assisted ventilation, while no improvements were observed in patients with mild forms of COVID-19 [61]. Moreover, in a meta-analysis of randomized study including 1703 patients, low-dosage corticosteroids improved survival in hospitalized patients needing respiratory assistance [62]. Xu et al. reported common histopathological alteration of ARDS, such as hyaline membranes and pneumocytes desquamation with cellular changes. Same alterations were reported by Li et al. [22] who also highlight how pro-inflammatory cytokines were higher during disease worsening and suggest the use of therapy targeting those cytokines.
Moreover, Magro et al. suggest that COVID-19 disease differs from typical ARDS at histopathological level. Patients included in their study reported changes to the alveolar capillaries, signs of thrombotic microvascular injury. This phenomenon leads to the activation of clotting pathway with consequent fibrin deposition [34]. Vascular changes were also found in Ackermann et al. study [38]. In this scenario, although COVID-19 disease seems to cause lung injury through an epithelial pattern, another study evaluating patient level data lung changes and symptoms, defined three different patterns of lung damage. In Polak et al. review of 129 patients, 110 reported lung epithelial damage, 76 patients vascular damage and 28 fibrotic changes. These patterns were mixed in 47 patients with 32 patients reporting overlapping epithelial and vascular damage. Furthermore, epithelial damage was consequence of host viral response in the early phase of the disease, followed by host inflammatory response and hypercoagulation leading to a vascular pattern, ending in a fibrosis of pulmonary tissue in the 22% of patients. Although these interesting results, patterns of damage can overlap in some patients and can be prominent in different stages of COVID-19 disease [63]. From our systematic review, vascular pattern of interstitial lung injury, mainly characterized by microthrombi and proteinaceous and fibrinous exudate associated to edema is often associated to the dominant epithelial damage, at the base of DAD. Therefore, ARDS in COVID-19 disease should not be intended as independent from DAD, but ARDS in these patients reflects the common denominator of DAD with the addition of vascular damage. This vascular damage is more common in COVID-19 lung disease, compared to other kinds of different origins ARDS.
The vascular endothelium is an active paracrine, endocrine and autocrine organ that is indispensable for the regulation of vascular tone and the maintenance of vascular homeostasis [64]. Endothelial dysfunction is the main cause of microcirculation alterations by moving the vascular balance more towards vasoconstriction with subsequent organ ischemia, inflammation with associated tissue edema and procoagulant state [65]. The SARS-CoV-2 coronavirus accesses host cells through the binding of its spike glycoprotein with the angiotensin 2 converting enzyme, sialic acid receptor, serine protease 2 transmembrane and extracellular matrix inducer metalloproteinase CD147; cathepsin B and L also participate in the entry of the virus. All these factors are expressed in endothelial cells [66]. COVID-19 patients show a broad spectrum of endothelial alterations, such as an increase in the activity of coagulation factor VIII and a high increase in von Willebrand factor [67] and angiotensin II level in the plasma, associated with viral load and lung damage [68]. Angiotensin II leads to microvascular permeability [69], to the transcription of tissue factor in endothelial cells [70] and to activation of platelets [71]. Angiotensin II can trigger the release of several components of the complement system from endothelial cells [72, 73]. These mechanisms support the key role of the endothelium in the pathogenesis of thrombosis in COVID-19 patients [74, 75]. When endothelial damage occurs, extracellular matrix is exposed to circulating blood, favoring platelet binding. Moreover, endothelial lung damage is considered the hallmark of ARDS [76]. In this scenario, the relationship between damaged endothelial cells and impaired platelet function gains impact in COVID-19 disease. In physiological conditions, at least five main mechanisms stabilize the lung endothelial basal barrier function, such as the release of soluble mediators that promote barrier integrity through endothelial signaling; the physical obstruction of the spaces in the endothelial barrier; the maintenance of the main structural characteristics of the endothelial cells necessary for the integrity of the barrier; stimulation or enhancement of endothelial cell growth and the neutralization or elimination of agents that increase endothelial permeability and compromise the integrity of the barrier [77]. Megakaryocytes were reported in samples from Fox et al. and Aguiar et al. [29, 43]. Therefore, megakaryocytes and platelets appear to be reprogrammed under certain disease conditions. In such contexts, the profile of platelet signaling factors that can influence the function and permeability of the endothelial barrier can change from a stabilizing state to a predominantly inflammatory one. Platelets and platelet products, including serotonin and TxA2, have been implicated in the pulmonary vascular blood pressure response to LPS infusion and other experimental models of ALI ARDS, but there are differences in results that may depend on species and other variables [78]. As in systemic circulation, pulmonary vascular reactivity responses to factors released by platelets depend on whether the endothelium is intact and capable of synthesizing vasodilators, including PGI2 and NO [79].
The endothelial cellular damage during COVID-19 is probably induced more by mechanisms of innate immunity with alternative cell death mechanisms to apoptosis that induce inflammation (necroptosis) [80] and immunothrombosis (netosis) [81]. Results from this study enforce evidence coming from other studies where inflammatory response seems to play an important role in lung damage and gravity of symptoms [82–84].
The proposed pathological mechanism, after infection, regards the role of both innate and adaptive components of the immune system. Lingeswaran at al. reviewed the immunological mechanisms undergoing in COVID-19 disease. They report a delayed type-1 INF response in the early phase of disease by innate immune cells, leading to an ineffective T-cell response. Subsequently, macrophages and recruited lymphocytes are responsible of pro-inflammatory mediators secretion. These mechanisms lead to a cytokine storm, contributing to the worsening of the disease [82].
Cross-talk between inflammatory cells and SARS-Cov-2 has been attributed to Toll-like receptors (TLRs). Among this, TLR4 acquired an important role in COVID-19 disease [85]. A key point is the activation of the TLRs both in platelets and in the endothelium, which can be induced both by direct binding of the SARS-CoV-2 and by indirect activation of cellular damage [86]. Choudhury et al. suggest that TLR4 is most likely to bind molecular patterns from SARS-CoV-2 promoting inflammatory pathways [85]. This molecular mechanism could be the crosstalk between the destruction of the vascular endothelial barrier in the pulmonary interstitium with the formation of proteinaceous edema and the activation of microthrombosis. Interestingly, TLR activation modulates the microvascular permeability and expression of coagulation mediators [87]. Both of these factors are important in COVID-19 leading to edematous lung damage and the formation of microthrombi, events that induce the activation of known mechanisms in sepsis and that induce multi-organ failure [88]. Moreover, TLR4 of EC, is able to activate mononuclear cells by the secretion of IL-6 [89]. Virus induced activation of TLR4 may be an important mechanism in COVID-19 disease. This consideration might explain the possible response to drugs modulating IL-6 levels [90]. IL-6 is a highly inducible pro-inflammatory cytokine secreted by several cell types including monocytes, lymphocytes, fibroblasts and endothelial cells; interleukin-1β (IL-1β) and TNF-α, viral infection and Angiotensin II are able to induce IL-6 [91, 92]. IL-6 plays an important role in the activation of endothelial cells during the initial phase of inflammation, inducing greater vascular permeability, the secretion of pro-inflammatory cytokines / chemokines by endothelial cells (IL-6, IL- 8, MCP-1 and complement activation C5a). In COVID-19 patients, IL-6 levels appear to be directly related to disease severity [93, 94]. Another important cytokine with increased serum levels observed in COVID-19 is soluble IL-2R, which is also related to the severity of the disease [95, 96]. Endothelial lung cells have also been shown to express IL-2R on their surface and that IL-2 could bind to endothelial cells and induce pulmonary edema in response to this link [97, 98]. Summarizing, IL-2R expression and IL-2 response may be implicated in the pathophysiology of COVID-19. Finally, pro-inflammatory cytokines, in particular IL-1β, IL-6 and TNFα, which are elevated in patients with COVID-19 induce the loss of normal antithrombotic and anti-inflammatory functions of endothelial cells, leading to dysregulation of coagulation, complement and platelet activation and leukocyte recruitment, explaining the wide range of immunological cells and the wide spectrum of histopathologic alterations. Recently two meta-analysis have been published investigating the administration of IL-6 inhibitors (Tocilizumab) in patients with COVID-19 disease. Improved overall survival resulted in severe patients after Tocilizumab administration [99, 100].
Recently, over the alterations in immunological response, complement and coagulation dysfunction have been associated to a worse outcome in patients with COVID-19 disease [101–103]. Results coming from this systematic review show evidence of microthrombi, hemorrhage and both interstitial and alveolar edema. These pathological processes have occurred in autopsy cases and it has been clinically proven that patients with alterations of coagulation-fibrinolysis parameters (D-dimers, PT, APTT, Fibrinogen, platelet count, FDP, AT, uPA, PAI-1), in particular if associated with parameters of inflammation, cytokine storm, activation of macrophages and endothelial cells (PCR, TNF-alpha, IL-1, IL-6, IL-8, IL-10, ferritin) reported a greater risk of developing severe pathology and to die from the disease [104]. As reported by Polak et al., fibro-proliferative processes were documented also in patients during the pre-symptomatic period and in the early phase of disease [63]. These processes have been already descripted during the early phase of ARDS [105] and an alteration of the balance between coagulation and fibrinolysis regulates pathological cell remodeling during the DAD [106]. Furthermore, coagulation is also part of the early-innate response to infections, in fact, coagulation system has evolved as an effector pathway of the immune response, by depositing fibrin around bacteria, trapping them, preventing their dissemination and favoring innate and specific defenses [107]. In COVID-19 disease, autopsy diagnostic findings demonstrate the presence of microthrombosis with associated perivascular inflammation, showing a possible role of endothelial inflammation in microvascular thrombosis. Although this hypothesis should be evaluated in future studies, there is emerging evidence that in COVID-19 disease, the damage of the endothelium could represent a cardinal event of the prothrombotic state and therefore microthrombosis may occur as primary event related to the SARS-CoV-2 virus infection and to the abnormal innate and adaptive immunity response, highlighting the role of host immunity in the development of COVID-19 disease. Villar et al. define the ability of corticosteroids to decrease the contemporary association between inflammation – coagulation and fibro-proliferation, with consequences on COVID-19 disease resolution [108].
These synergistic processes are histologically associated to DAD, in particular to hyaline membranes and inflammatory exudation [19, 108]. Inflammation, coagulation and fibro-proliferative processes may occur earlier, before the evidence of clinically relevant ARDS. While worsening of disease, the establishing of clinical ARDS, leads to a general status of hypoxia, which may induce an increase of Tissue factor, VIIa factor and Serpin 1, which in turn are primarily responsible for the development of a pro-coagulant and anti-fibrinolytic state [109, 110]. In previously reported animal models of SARS, alterations in coagulation and intra-alveolar deposition of fibrin proceed in parallel and occur in a particularly complex scenario in which pro-inflammatory factors participate (IL-1, TNF-alpha, IL-6), pro-fibrotic (TGF, CTGF, PDGF), together with the increase expression of the urokinetic pathway with activation of both pro-fibrinolytic and anti-fibrinolytic genes. Moreover, factors involved in plasminogen activation determine the activation of the plasminogen-plasmin system and are related to lethality; also the synergistic association between inflammatory factors and expression of fibrinolytic genes can explain the bleeding aspects observed in animal models [111]. This scenario is well described in Menter et al., and Yao et al. COVID-19 autopsy [18, 31], where necrotic-hemorrhagic aspects are observed together with endoalveolar and interstitial fibrosis associated with diffuse microthrombosis. Meanwhile, microthrombosis has not been identified in post-mortem biopsies in a study of Tian et al. [26]. Retrospective clinical evidence, have shown in Chinese patients that the use of low molecular weight heparins is related to a better clinical outcome only in cases with an increase in D-dimers and with alteration of the parameters of the coagulation. Administration of heparin is associated with adverse events when the patient does not present high D-Dimers and when there is no alteration of the coagulation parameters [112, 113]. Contrary to these reported clinical retrospective studies, the results of histopathological studies showed that D-dimers are elevated in almost all fatal cases of Covid-19 disease; furthermore, in a fair proportion of cases (29%) the D-dimers were ten times higher than the normal limits [34, 63]. It seems useful using anticoagulant treatment in severe conditions of COVID-19, in order to reduce mortality [114–116], while, using of prophylactic administration of low molecular weight heparin in early phase of COVID-19 disease has to be ascertained by randomized clinical trial (NCT04492254 – https://clinicaltrials.gov/ct2/show/NCT04492254 - NIH-clinicaltrials.gov) [117], considering also, the non-anticoagulant related effects of heparin [116].
Another histopathological alteration in COVID-19 disease is the evidence of pulmonary fibrosis. Generally, fibrosis can be result of chronic inflammation or can develop as primary fibro-proliferative process, genetically influenced and age-related, in idiopathic pulmonary fibrosis (IPF). Pulmonary fibrosis is a recognized sequel of ARDS. This is characterized by a diffuse alveolar pulmonary epithelial and endothelial damage, leading to an increase in pulmonary edema, permeability and alveolar filling [118]. Numerous epidemiological, viral and current clinical evidences support the possibility that pulmonary fibrosis may be one of the main complications in COVID-19 patients [119, 120]. Fibrosis is result of different mechanisms, which collaborate in promoting fibrin deposition. Damaged alveoli release different markers both in the blood and in the alveolar compartment; contemporary, vascular endothelial injury leads to an increase of microvascular permeability and alveolar edema. In some patients, the significant and persistent accumulation of macrophages, fibrocytes, fibroblasts and myofibroblasts in the alveolar compartment leads to excessive deposition of extracellular matrix components including fibronectin and type I and III collagen, among other proteins. An imbalance between profibrotic and antifibrotic mediators may subsequently determine this fibroproliferative response [121, 122]. The pathophysiological process of pulmonary fibrosis is believed to be an abnormal wound healing state. The abnormal proliferation of fibroblasts and the accumulation of ECM proteins (such as collagen) have become the center of recent research on pulmonary fibrosis [123]. Interestingly, circulating fibroblasts are positively correlated with the degree of fibrosis, indicating which patients with IPF may face an increased risk of unfavorable prognosis. CXCR4 is the main chemokine receptor expressed on circulating fibroblasts in humans and mice, and there is a direct correlation between the lung and plasma levels of CXCL12 and the number of circulating pulmonary fibrocytes in patients with pulmonary fibrosis [124].
The rationale for the use of antifibrotic therapy is based on the spectrum of fibrotic lung disease observed in COVID-19, which ranges from fibrosis associated with the organization of pneumonia to severe ALI, in which there is evolution to widespread fibrotic change [125]. However, these drugs do not address the immune dysregulation of SARS-CoV-2 infection, nor they are able to attenuate the prothrombotic aspects of this complex pathogenic process [119]. Although these considerations, an interesting target for antifibrotic therapies can be the TGF-β pathway. There are drugs in development that target various molecules in this pathway, including anti-integrin αvβ6, PLN-74809 and galectins. These are particularly interesting candidates because the SARS-CoV-2 spike protein contains an Arg-Gly-Asp integrin-binding domain and a number of coronaviruses contain an N-terminal galectin fold [126]. Strategies for blocking αvβ6 integrin have been evaluated in vivo models of ALI [127, 128]. Furthermore, IL-1, which has been identified as a key component of the cytokine storm in COVID-19 and other viruses, could mediate its effects through Arg-Gly-Asp binding integrin [129]. Other studies have identified mTOR as an emerging target in IPF [130, 131]. In addition, PRM-151 is an analogue of SAP (also known as PTX2), which is a member of the pentraxin family of proteins that includes C-reactive protein and PTX3 and has shown promise in a phase 2 study for IPF [132].
In conclusion, COVID-19 lethal cases appear as a heterogeneous disease, characterized by of contemporary presence of different histological findings, which reflect diverse pathological pathways. Epithelial, vascular and fibrotic changes may occur as separate alterations or together (Fig. 2). Histological evidence of edema, together with DAD and events of microthrombosis in major of deceased COVID-19 patients, suggest the use of combined and early administration of steroid-centered therapy, in association of targeted therapies. For example, promising results come from a single center observational study, in which the association of Tocilizumab and steroid was associated with better outcome [133]. Future studies should detect reliable biomarkers of lung tissue pathological status, in order to develop target therapies.
Supplementary Information
Additional file 1: Supplemental Table 1 List of excluded studies and reason of exclusion.
Acknowledgements
Not applicable.
Authors’ contributions
GP and VCAC contributed to conception, design, data analysis and interpretation and drafted the manuscript; ISDS, MAR, MM, AA, MCP contributed to conception, design and article searching and data acquisition and drafted the manuscript, GT, KZ and MEB contributed to data acquisition control and critically revised the manuscript; SA drafted and critically revised; SP and FMB critically revised the manuscript; LLM contributed to conception drafted and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Funding
Authors did not receive any funding.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Authors declare no interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Giuseppe Pannone and Vito Carlo Alberto Caponio contributed equally to this work.
References
- 1.Hajjar LA, Costa I, Rizk SI, Biselli B, Gomes BR, Bittar CS, de Oliveira GQ, de Almeida JP, de Oliveira Bello MV, Garzillo C, et al. Intensive care management of patients with COVID-19: a practical approach. Ann Intensive Care. 2021;11(1):36. doi: 10.1186/s13613-021-00820-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reis e Sousa C. Sensing infection and tissue damage. EMBO Mol Med. 2017;9(3):285–288. doi: 10.15252/emmm.201607227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pachetti M, Marini B, Benedetti F, Giudici F, Mauro E, Storici P, Masciovecchio C, Angeletti S, Ciccozzi M, Gallo RC, Zella D, Ippodrino R. Emerging SARS-CoV-2 mutation hot spots include a novel RNA-dependent-RNA polymerase variant. J Transl Med. 2020;18(1):179. doi: 10.1186/s12967-020-02344-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rudan I. A cascade of causes that led to the COVID-19 tragedy in Italy and in other European Union countries. J Glob Health. 2020;10(1):010335. doi: 10.7189/jogh.10.010335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, Hengartner N, Giorgi EE, Bhattacharya T, Foley B, Hastie KM, Parker MD, Partridge DG, Evans CM, Freeman TM, de Silva TI, McDanal C, Perez LG, Tang H, Moon-Walker A, Whelan SP, LaBranche CC, Saphire EO, Montefiori DC, Angyal A, Brown RL, Carrilero L, Green LR, Groves DC, Johnson KJ, Keeley AJ, Lindsey BB, Parsons PJ, Raza M, Rowland-Jones S, Smith N, Tucker RM, Wang D, Wyles MD. Tracking changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 virus. Cell. 2020;182(4):812–827. doi: 10.1016/j.cell.2020.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirby T. New variant of SARS-CoV-2 in UK causes surge of COVID-19. Lancet Respir Med. 2021;9(2):e20–e21. doi: 10.1016/S2213-2600(21)00005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tang JW, Toovey OTR, Harvey KN, Hui DDS. Introduction of the south African SARS-CoV-2 variant 501Y.V2 into the UK. J Inf Secur. 2021;82(4):e8–e10. doi: 10.1016/j.jinf.2021.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yong Jia, Gangxu Shen, Yujuan Zhang, Keng-Shiang Huang, Hsing-Ying Ho, Wei-Shio Hor, Chih-Hui Yang, Chengdao Li, Wei-Lung Wang. Analysis of the mutation dynamics of SARS-CoV-2 reveals the spread history and emergence of RBD mutant with lower ACE2 binding affinity. bioRxiv. 2020.04.09.034942. 10.1101/2020.04.09.034942.
- 9.Geleris J, Sun Y, Platt J, Zucker J, Baldwin M, Hripcsak G, Labella A, Manson D, Kubin C, Barr RG, et al. Observational study of Hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. 2020;382(25):2411–2418. doi: 10.1056/NEJMoa2012410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elhusseiny KM, Abd-Elhay FA, Kamel MG Possible therapeutic agents for COVID-19: a comprehensive review. Expert Rev Anti-Infect Ther. 2020;18(10):1005–20. 10.1080/14787210.2020.1782742. Epub 2020 June 30. [DOI] [PubMed]
- 11.Pardo J, Shukla AM, Chamarthi G, Gupte A. The journey of remdesivir: from Ebola to COVID-19. Drugs Context. 2020;9:1–9. doi: 10.7573/dic.2020-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu MY, Zheng B, Zhang Y, Li JP. Role and mechanism of angiotensin-converting enzyme 2 in acute lung injury in coronavirus disease 2019. Chronic Dis Transl Med. 2020;6(2):98-105. 10.1016/j.cdtm.2020.05.003. Epub 2020 May 19. [DOI] [PMC free article] [PubMed]
- 13.Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, Shi Z, Hu Z, Zhong W, Xiao G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zumla A, Chan JF, Azhar EI, Hui DS, Yuen KY. Coronaviruses - drug discovery and therapeutic options. Nat Rev Drug Discov. 2016;15(5):327–347. doi: 10.1038/nrd.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan JF, Chan KH, Kao RY, To KK, Zheng BJ, Li CP, Li PT, Dai J, Mok FK, Chen H, et al. Broad-spectrum antivirals for the emerging Middle East respiratory syndrome coronavirus. J Inf Secur. 2013;67(6):606–616. doi: 10.1016/j.jinf.2013.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 17.Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23(2):60–63. doi: 10.1136/bmjebm-2017-110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yao XH, He ZC, Li TY, Zhang HR, Wang Y, Mou H, Guo Q, Yu SC, Ding Y, Liu X, Ping YF, Bian XW. Pathological evidence for residual SARS-CoV-2 in pulmonary tissues of a ready-for-discharge patient. Cell Res. 2020;30(6):541–543. doi: 10.1038/s41422-020-0318-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harkin TJ, Rurak KM, Martins J, Eber C, Szporn AH, Beasley MB. Delayed diagnosis of COVID-19 in a 34-year-old man with atypical presentation. Lancet Respir Med. 2020;8(6):644–46. 10.1016/S2213-2600(20)30232-0. [DOI] [PMC free article] [PubMed]
- 22.Li S, Jiang L, Li X, Lin F, Wang Y, Li B, Jiang T, An W, Liu S, Liu H, Xu P, Zhao L, Zhang L, Mu J, Wang H, Kang J, Li Y, Huang L, Zhu C, Zhao S, Lu J, Ji J, Zhao J. Clinical and pathological investigation of patients with severe COVID-19. JCI Insight. 2020 Jun 18;5(12):e138070. 10.1172/jci.insight.138070. [DOI] [PMC free article] [PubMed]
- 23.Shao C, Liu H, Meng L, Sun L, Wang Y, Yue Z, Kong H, Li H, Weng H, Lv F, Jin R. Evolution of severe acute respiratory syndrome coronavirus 2 RNA test results in a patient with fatal coronavirus disease 2019: a case report. Hum Pathol. 2020;101:82–88. doi: 10.1016/j.humpath.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pernazza A, Mancini M, Rullo E, Bassi M, De Giacomo T, Rocca CD, d'Amati G. Early histologic findings of pulmonary SARS-CoV-2 infection detected in a surgical specimen. Virchows Arch. 2020;477(5):743–748. doi: 10.1007/s00428-020-02829-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tian S, Xiong Y, Liu H, Niu L, Guo J, Liao M, Xiao SY. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33(6):1007–1014. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung Cancer. J Thorac Oncol. 2020;15(5):700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cai Y, Hao Z, Gao Y, Ping W, Wang Q, Peng S, Zhao B, Sun W, Zhu M, Li K, Han Y, Kuang D, Chu Q, Fu X, Zhang N. Coronavirus disease 2019 in the perioperative period of lung resection: a brief report from a single thoracic surgery Department in Wuhan, People's Republic of China. J Thorac Oncol. 2020;15(6):1065–1072. doi: 10.1016/j.jtho.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zeng Z, Xu L, Xie XY, Yan HL, Xie BJ, Xu WZ, Liu XA, Kang GJ, Jiang WL, Yuan JP. Pulmonary pathology of early phase COVID-19 pneumonia in a patient with a benign lung lesion. Histopathology. 2020;77(5):823–831. doi: 10.1111/his.14138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8(7):681–6. 10.1016/S2213-2600(20)30243-5. Epub 2020 May 27. [DOI] [PMC free article] [PubMed]
- 30.Lacy JM, Brooks EG, Akers J, Armstrong D, Decker L, Gonzalez A, Humphrey W, Mayer R, Miller M, Perez C, Arango JAR, Sathyavagiswaran L, Stroh W, Utley S. Covid-19: postmortem diagnostic and biosafety considerations. Am J Forensic Med Pathol. 2020;41(3):143–151. doi: 10.1097/PAF.0000000000000567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, Frank S, Turek D, Willi N, Pargger H, Bassetti S, Leuppi JD, Cathomas G, Tolnay M, Mertz KD, Tzankov A. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction. Histopathology. 2020;77(2):198–209. doi: 10.1111/his.14134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barton LM, Duval EJ, Stroberg E, Ghosh S, Mukhopadhyay S. COVID-19 Autopsies, Oklahoma, USA. Am J Clin Pathol. 2020;153(6):725–733. doi: 10.1093/ajcp/aqaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karami P, Naghavi M, Feyzi A, Aghamohammadi M, Novin MS, Mobaien A, et al. WITHDRAWN: mortality of a pregnant patient diagnosed with COVID-19: a case report with clinical, radiological, and histopathological findings. Travel Med Infect Dis. 2020;101665. 10.1016/j.tmaid.2020.101665. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 34.Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, Baxter-Stoltzfus A, Laurence J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lax SF, Skok K, Zechner P, Kessler HH, Kaufmann N, Koelblinger C, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: results from a prospective, Single-Center, Clinicopathologic Case Series. Ann Intern Med. 2020;173(5):350–61.10.7326/M20-2566. Epub 2020 May 14. [DOI] [PMC free article] [PubMed]
- 36.Adachi T, Chong JM, Nakajima N, Sano M, Yamazaki J, Miyamoto I, et al. Clinicopathologic and Immunohistochemical Findings from Autopsy of Patient with COVID-19, Japan. Emerg Infect Dis. 2020;26(9):2157–61. 10.3201/eid2609.201353. [DOI] [PMC free article] [PubMed]
- 37.Yan L, Mir M, Sanchez P, Beg M, Peters J, Enriquez O, Gilbert A. COVID-19 in a Hispanic Woman. Arch Pathol Lab Med. 2020;144(9):1041–7. 10.5858/arpa.2020-0217-SA. [DOI] [PubMed]
- 38.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Jonigk D. Pulmonary vascular Endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schaller T, Hirschbühl K, Burkhardt K, et al. Postmortem Examination of Patients With COVID-19. JAMA. 2020;323(24):2518–20. 10.1001/jama.2020.8907. [DOI] [PMC free article] [PubMed]
- 40.Martines RB, Ritter JM, Matkovic E, Gary J, Bollweg BC, Bullock H, et al. Pathology and Pathogenesis of SARS-CoV-2 Associated with Fatal Coronavirus Disease, United States. Emerg Infect Dis. 2020;26(9):2005–15. 10.3201/eid2609.202095. [DOI] [PMC free article] [PubMed]
- 41.Buja LM, Wolf DA, Zhao B, Akkanti B, McDonald M, Lelenwa L, Reilly N, Ottaviani G, Elghetany MT, Trujillo DO, et al. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc Pathol. 2020;48:107233. doi: 10.1016/j.carpath.2020.107233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sekulic M, Harper H, Nezami BG, Shen DL, Sekulic SP, Koeth AT, Harding CV, Gilmore H, Sadri N. Molecular detection of SARS-CoV-2 infection in FFPE samples and Histopathologic findings in fatal SARS-CoV-2 cases. Am J Clin Pathol. 2020;154(2):190–200. doi: 10.1093/ajcp/aqaa091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aguiar D, Lobrinus JA, Schibler M, Fracasso T, Lardi C. Inside the lungs of COVID-19 disease. Int J Legal Med. 2020;134(4):1271–1274. doi: 10.1007/s00414-020-02318-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Konopka KE, Wilson A, Myers JL. Postmortem Lung Findings in a Patient With Asthma and Coronavirus Disease 2019. Chest. 2020;158(3):e99–e101. 10.1016/j.chest.2020.04.032. [DOI] [PMC free article] [PubMed]
- 45.Zynyuk L, Huxter J, Muller RU, Fox SE. The presence of a second rat has only subtle effects on the location-specific firing of hippocampal place cells. Hippocampus. 2012;22(6):1405–1416. doi: 10.1002/hipo.20977. [DOI] [PubMed] [Google Scholar]
- 46.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Jonigk D. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120–8. 10.1056/NEJMoa2015432. Epub 2020 May 21. [DOI] [PMC free article] [PubMed]
- 47.Tian J, Yuan X, Xiao J, Zhong Q, Yang C, Liu B, Cai Y, Lu Z, Wang J, Wang Y, et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21(7):893–903. doi: 10.1016/S1470-2045(20)30309-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Barton LM, Duval EJ, Stroberg E, Ghosh S, Mukhopadhyay S. COVID-19 Autopsies, Oklahoma. USA. Am J Clin Pathol. 2020;153(6):725–733. doi: 10.1093/ajcp/aqaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lacy JM, Brooks EG, Akers J, Armstrong D, Decker L, Gonzalez A, Humphrey W, Mayer R, Miller M, Perez C, Arango JAR, Sathyavagiswaran L, Stroh W, Utley S. COVID-19: Postmortem Diagnostic and Biosafety Considerations. Am J Forensic Med Pathol. 2020;41(3):143–51. 10.1097/PAF.0000000000000567. [DOI] [PMC free article] [PubMed]
- 50.Shao L, Li X, Zhou Y, Yu Y, Liu Y, Liu M, Zhang R, Zhang H, Wang X, Zhou F. Novel Insights Into Illness Progression and Risk Profiles for Mortality in Non-survivors of COVID-19. Front Med (Lausanne) 2020;7:246. doi: 10.3389/fmed.2020.00246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pernazza A, Mancini M, Rullo, E. et al. Early histologic findings of pulmonary SARS-CoV-2 infection detected in a surgical specimen. Virchows Arch. 2020;477:743–8. 10.1007/s00428-020-02829-1. [DOI] [PMC free article] [PubMed]
- 52.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.den Bakker MA. Is histopathology still the gold standard? Ned Tijdschr Geneeskd. 2017;160:D981. [PubMed] [Google Scholar]
- 54.Force ADT, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 55.Park J, Lee YJ, Lee J, Park SS, Cho YJ, Lee SM, Kim YW, Han SK, Yoo CG. Histopathologic heterogeneity of acute respiratory distress syndrome revealed by surgical lung biopsy and its clinical implications. Korean J Intern Med. 2018;33(3):532–540. doi: 10.3904/kjim.2016.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guerin C, Bayle F, Leray V, Debord S, Stoian A, Yonis H, Roudaut JB, Bourdin G, Devouassoux-Shisheboran M, Bucher E, et al. Open lung biopsy in nonresolving ARDS frequently identifies diffuse alveolar damage regardless of the severity stage and may have implications for patient management. Intensive Care Med. 2015;41(2):222–230. doi: 10.1007/s00134-014-3583-2. [DOI] [PubMed] [Google Scholar]
- 57.Thille AW, Esteban A, Fernandez-Segoviano P, Rodriguez JM, Aramburu JA, Penuelas O, Cortes-Puch I, Cardinal-Fernandez P, Lorente JA, Frutos-Vivar F. Comparison of the Berlin definition for acute respiratory distress syndrome with autopsy. Am J Respir Crit Care Med. 2013;187(7):761–767. doi: 10.1164/rccm.201211-1981OC. [DOI] [PubMed] [Google Scholar]
- 58.Meduri GU, Annane D, Chrousos GP, Marik PE, Sinclair SE. Activation and regulation of systemic inflammation in ARDS: rationale for prolonged glucocorticoid therapy. Chest. 2009;136(6):1631–1643. doi: 10.1378/chest.08-2408. [DOI] [PubMed] [Google Scholar]
- 59.Meduri GU, Bridges L, Siemieniuk RAC, Kocak M. An exploratory reanalysis of the randomized trial on efficacy of corticosteroids as rescue therapy for the late phase of acute respiratory distress syndrome. Crit Care Med. 2018;46(6):884–891. doi: 10.1097/CCM.0000000000003021. [DOI] [PubMed] [Google Scholar]
- 60.Raju R. V P, Biatris PS, J S: therapeutic role of corticosteroids in COVID-19: a systematic review of registered clinical trials. Futur J Pharm Sci. 2021;7(1):67. doi: 10.1186/s43094-021-00217-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sarma P, Bhattacharyya A, Kaur H, Prajapat M, Prakash A, Kumar S, Bansal S, Kirubakaran R, Reddy DH, Muktesh G, Kaushal K, Sharma S, Shekhar N, Avti P, Thota P, Medhi B. Efficacy and safety of steroid therapy in COVID-19: a rapid systematic review and Meta-analysis. Indian J Pharmacol. 2020;52(6):535–550. doi: 10.4103/ijp.ijp_1146_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li SS, Hohl CM. CJEM journal club: corticosteroids use for critically ill COVID-19 patients. CJEM. 2021;23(2):162–163. doi: 10.1007/s43678-020-00056-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Polak SB, Van Gool IC, Cohen D, von der Thusen JH, van Paassen J. A systematic review of pathological findings in COVID-19: a pathophysiological timeline and possible mechanisms of disease progression. Mod Pathol. 2020;33(11):2128–2138. doi: 10.1038/s41379-020-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Flammer AJ, Anderson T, Celermajer DS, Creager MA, Deanfield J, Ganz P, Hamburg NM, Luscher TF, Shechter M, Taddei S, et al. The assessment of endothelial function: from research into clinical practice. Circulation. 2012;126(6):753–767. doi: 10.1161/CIRCULATIONAHA.112.093245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bonetti PO, Lerman LO, Lerman A. Endothelial dysfunction: a marker of atherosclerotic risk. Arterioscler Thromb Vasc Biol. 2003;23(2):168–175. doi: 10.1161/01.ATV.0000051384.43104.FC. [DOI] [PubMed] [Google Scholar]
- 66.Sardu C, Gambardella J, Morelli MB, Wang X, Marfella R, Santulli G. Hypertension, Thrombosis, Kidney Failure, and Diabetes: Is COVID-19 an Endothelial Disease? A Comprehensive Evaluation of Clinical and Basic Evidence. J Clin Med. 2020;9(5):1417. 10.3390/jcm9051417. [DOI] [PMC free article] [PubMed]
- 67.Escher R, Breakey N, Lammle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res. 2020;190:62. doi: 10.1016/j.thromres.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, Wang Z, Li J, Li J, Feng C, Zhang Z, Wang L, Peng L, Chen L, Qin Y, Zhao D, Tan S, Yin L, Xu J, Zhou C, Jiang C, Liu L. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63(3):364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Williams B, Baker AQ, Gallacher B, Lodwick D. Angiotensin II increases vascular permeability factor gene expression by human vascular smooth muscle cells. Hypertension. 1995;25(5):913–917. doi: 10.1161/01.HYP.25.5.913. [DOI] [PubMed] [Google Scholar]
- 70.Dielis AW, Smid M, Spronk HM, Hamulyak K, Kroon AA, ten Cate H, de Leeuw PW. The prothrombotic paradox of hypertension: role of the renin-angiotensin and kallikrein-kinin systems. Hypertension. 2005;46(6):1236–1242. doi: 10.1161/01.HYP.0000193538.20705.23. [DOI] [PubMed] [Google Scholar]
- 71.Jagroop IA, Mikhailidis DP. Angiotensin II can induce and potentiate shape change in human platelets: effect of losartan. J Hum Hypertens. 2000;14(9):581–585. doi: 10.1038/sj.jhh.1001102. [DOI] [PubMed] [Google Scholar]
- 72.Langeggen H, Berge KE, Macor P, Fischetti F, Tedesco F, Hetland G, Berg K, Johnson E. Detection of mRNA for the terminal complement components C5, C6, C8 and C9 in human umbilical vein endothelial cells in vitro. APMIS. 2001;109(1):73–78. doi: 10.1111/j.1600-0463.2001.tb00016.x. [DOI] [PubMed] [Google Scholar]
- 73.Langeggen H, Pausa M, Johnson E, Casarsa C, Tedesco F. The endothelium is an extrahepatic site of synthesis of the seventh component of the complement system. Clin Exp Immunol. 2000;121(1):69–76. doi: 10.1046/j.1365-2249.2000.01238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fischetti F, Tedesco F. Cross-talk between the complement system and endothelial cells in physiologic conditions and in vascular diseases. Autoimmunity. 2006;39(5):417–428. doi: 10.1080/08916930600739712. [DOI] [PubMed] [Google Scholar]
- 75.Risitano AM, Mastellos DC, Huber-Lang M, Yancopoulou D, Garlanda C, Ciceri F, Lambris JD. Complement as a target in COVID-19? Nat Rev Immunol. 2020;20(6):343–344. doi: 10.1038/s41577-020-0320-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Maniatis NA, Orfanos SE. The endothelium in acute lung injury/acute respiratory distress syndrome. Curr Opin Crit Care. 2008;14(1):22–30. doi: 10.1097/MCC.0b013e3282f269b9. [DOI] [PubMed] [Google Scholar]
- 77.Ho-Tin-Noe B, Demers M, Wagner DD. How platelets safeguard vascular integrity. J Thromb Haemost. 2011;9(Suppl 1):56–65. doi: 10.1111/j.1538-7836.2011.04317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kroll MH, Afshar-Kharghan V. Platelets in pulmonary vascular physiology and pathology. Pulm Circ. 2012;2(3):291–308. doi: 10.4103/2045-8932.101398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sandoo A, van Zanten JJ, Metsios GS, Carroll D, Kitas GD. The endothelium and its role in regulating vascular tone. Open Cardiovasc Med J. 2010;4:302–312. doi: 10.2174/1874192401004010302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Badagliacca R, Sciomer S, Petrosillo N. Endothelin receptor antagonists for pulmonary arterial hypertension and COVID-19: friend or foe? J Heart Lung Transplant. 2020;39(7):729–730. doi: 10.1016/j.healun.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mozzini C, Girelli D. The role of neutrophil extracellular traps in Covid-19: only an hypothesis or a potential new field of research? Thromb Res. 2020;191:26–27. doi: 10.1016/j.thromres.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lingeswaran M, Goyal T, Ghosh R, Suri S, Mitra P, Misra S, Sharma P. Inflammation, immunity and Immunogenetics in COVID-19: a narrative review. Indian J Clin Biochem. 2020;35(3):260–273. doi: 10.1007/s12291-020-00897-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Merad M, Martin JC. Author correction: pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20(7):448. doi: 10.1038/s41577-020-0353-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tay MZ, Poh CM, Renia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20(6):363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Choudhury A, Mukherjee S. In silico studies on the comparative characterization of the interactions of SARS-CoV-2 spike glycoprotein with ACE-2 receptor homologs and human TLRs. J Med Virol. 2020;92(10):2105–2113. doi: 10.1002/jmv.25987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Olejnik J, Hume AJ, Muhlberger E. Toll-like receptor 4 in acute viral infection: too much of a good thing. PLoS Pathog. 2018;14(12):e1007390. doi: 10.1371/journal.ppat.1007390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Vallance TM, Zeuner MT, Williams HF, Widera D, Vaiyapuri S. Toll-like receptor 4 Signalling and its impact on platelet function, thrombosis, and Haemostasis. Mediat Inflamm. 2017;2017:9605894. doi: 10.1155/2017/9605894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Khakpour S, Wilhelmsen K, Hellman J. Vascular endothelial cell toll-like receptor pathways in sepsis. Innate Immun. 2015;21(8):827–846. doi: 10.1177/1753425915606525. [DOI] [PubMed] [Google Scholar]
- 89.Lu Z, Li Y, Jin J, Zhang X, Lopes-Virella MF, Huang Y. Toll-like receptor 4 activation in microvascular endothelial cells triggers a robust inflammatory response and cross talk with mononuclear cells via interleukin-6. Arterioscler Thromb Vasc Biol. 2012;32(7):1696–1706. doi: 10.1161/ATVBAHA.112.251181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Atal S, Fatima Z. IL-6 inhibitors in the treatment of serious COVID-19: a promising therapy? Pharmaceut Med. 2020;34(4):223–31.10.1007/s40290-020-00342-z. [DOI] [PMC free article] [PubMed]
- 91.Luther JM, Gainer JV, Murphey LJ, Yu C, Vaughan DE, Morrow JD, Brown NJ. Angiotensin II induces interleukin-6 in humans through a mineralocorticoid receptor-dependent mechanism. Hypertension. 2006;48(6):1050–1057. doi: 10.1161/01.HYP.0000248135.97380.76. [DOI] [PubMed] [Google Scholar]
- 92.Wassmann S, Stumpf M, Strehlow K, Schmid A, Schieffer B, Bohm M, Nickenig G. Interleukin-6 induces oxidative stress and endothelial dysfunction by overexpression of the angiotensin II type 1 receptor. Circ Res. 2004;94(4):534–541. doi: 10.1161/01.RES.0000115557.25127.8D. [DOI] [PubMed] [Google Scholar]
- 93.Chen X, Zhao B, Qu Y, et al. Detectable serum severe acute respiratory syndrome coronavirus 2 viral load (RNAemia) is closely correlated with drastically elevated interleukin 6 level in critically Ill patients with coronavirus disease 2019. Clin Infect Dis. 2020;71(8):1937-42. 10.1093/cid/ciaa449. [DOI] [PMC free article] [PubMed]
- 94.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang F, Hou H, Luo Y, Tang G, Wu S, Huang M, et al. The laboratory tests and host immunity of COVID-19 patients with different severity of illness. JCI Insight. 2020;5(10):e137799. Published 2020 May 21. 10.1172/jci.insight.137799. [DOI] [PMC free article] [PubMed]
- 96.Hou H, Zhang B, Huang H, Luo Y, Wu S, Tang G, Liu W, Mao L, Mao L, Wang F, et al. Using IL-2R/lymphocytes for predicting the clinical progression of patients with COVID-19. Clin Exp Immunol. 2020;201(1):76–84. doi: 10.1111/cei.13450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Krieg C, Letourneau S, Pantaleo G, Boyman O. Improved IL-2 immunotherapy by selective stimulation of IL-2 receptors on lymphocytes and endothelial cells. Proc Natl Acad Sci U S A. 2010;107(26):11906–11911. doi: 10.1073/pnas.1002569107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pons S, Fodil S, Azoulay E, Zafrani L. The vascular endothelium: the cornerstone of organ dysfunction in severe SARS-CoV-2 infection. Crit Care. 2020;24(1):353. doi: 10.1186/s13054-020-03062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nugroho CW, Suryantoro SD, Yuliasih Y, Rosyid AN, Asmarawati TP, Andrianto L, Setiawan HW, Mahdi BA, Windradi C, Agustin ED, et al. Optimal use of tocilizumab for severe and critical COVID-19: a systematic review and meta-analysis. F1000Res. 2021;10:73. doi: 10.12688/f1000research.45046.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sarfraz A, Sarfraz Z, Sarfraz M, Aftab H, Pervaiz Z. Tocilizumab and COVID-19: a Meta-analysis of 2120 patients with severe disease and implications for clinical trial methodologies. Turk J Med Sci. 2020. 10.3906/sag-2010-131. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 101.Ramlall V, Thangaraj PM, Meydan C, Foox J, Butler D, Kim J, May B, De Freitas JK, Glicksberg BS, Mason CE, et al. Immune complement and coagulation dysfunction in adverse outcomes of SARS-CoV-2 infection. Nat Med. 2020;26(10):1609–1615. doi: 10.1038/s41591-020-1021-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Martin-Rojas RM, Perez-Rus G, Delgado-Pinos VE, Domingo-Gonzalez A, Regalado-Artamendi I, Alba-Urdiales N, Demelo-Rodriguez P, Monsalvo S, Rodriguez-Macias G, Ballesteros M, et al. COVID-19 coagulopathy: an in-depth analysis of the coagulation system. Eur J Haematol. 2020;105(6):741–750. doi: 10.1111/ejh.13501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Coccheri S. COVID-19: the crucial role of blood coagulation and fibrinolysis. Intern Emerg Med. 2020;15(8):1369–1373. doi: 10.1007/s11739-020-02443-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lippi G. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Marshall RP, Bellingan G, Webb S, Puddicombe A, Goldsack N, McAnulty RJ, Laurent GJ. Fibroproliferation occurs early in the acute respiratory distress syndrome and impacts on outcome. Am J Respir Crit Care Med. 2000;162(5):1783–1788. doi: 10.1164/ajrccm.162.5.2001061. [DOI] [PubMed] [Google Scholar]
- 106.Gralinski LE, Ferris MT, Aylor DL, Whitmore AC, Green R, Frieman MB, Deming D, Menachery VD, Miller DR, Buus RJ, et al. Genome wide identification of SARS-CoV susceptibility loci using the collaborative cross. PLoS Genet. 2015;11(10):e1005504. doi: 10.1371/journal.pgen.1005504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Antoniak S. The coagulation system in host defense. Res Pract Thromb Haemost. 2018;2(3):549–557. doi: 10.1002/rth2.12109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Villar J, Confalonieri M, Pastores SM, Meduri GU. Rationale for prolonged corticosteroid treatment in the acute respiratory distress syndrome caused by coronavirus disease 2019. Crit Care Explor. 2020;2(4):e0111. doi: 10.1097/CCE.0000000000000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Idell S, James KK, Levin EG, Schwartz BS, Manchanda N, Maunder RJ, Martin TR, McLarty J, Fair DS. Local abnormalities in coagulation and fibrinolytic pathways predispose to alveolar fibrin deposition in the adult respiratory distress syndrome. J Clin Invest. 1989;84(2):695–705. doi: 10.1172/JCI114217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wygrecka M, Jablonska E, Guenther A, Preissner KT, Markart P. Current view on alveolar coagulation and fibrinolysis in acute inflammatory and chronic interstitial lung diseases. Thromb Haemost. 2008;99(3):494–501. doi: 10.1160/TH07-11-0666. [DOI] [PubMed] [Google Scholar]
- 111.Gralinski LE, Bankhead A 3rd, Jeng S, Menachery VD, Proll S, Belisle SE, Matzke M, Webb-Robertson BJ, Luna ML, Shukla AK, Ferris MT, Bolles M, Chang J, Aicher L, Waters KM, Smith RD, Metz TO, Law GL, Katze MG, McWeeney S, Baric RS. Mechanisms of severe acute respiratory syndrome coronavirus-induced acute lung injury. mBio. 2013;4(4):e00271–13. 10.1128/mBio.00271-13. [DOI] [PMC free article] [PubMed]
- 112.Porfidia A, Pola R. Venous thromboembolism and heparin use in COVID-19 patients: juggling between pragmatic choices, suggestions of medical societies and the lack of guidelines. J Thromb Thrombolysis. 2020;50(1):68–71. doi: 10.1007/s11239-020-02125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kow CS, Hasan SS. Use of low-molecular-weight heparin in COVID-19 patients. J Vasc Surg Venous Lymphat Disord. 2020 ;8(5):900–1. 10.1016/j.jvsv.2020.06.006. Epub 2020 June 17. [DOI] [PMC free article] [PubMed]
- 114.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Paranjpe I, Fuster V, Lala A, Russak AJ, Glicksberg BS, Levin MA, Charney AW, Narula J, Fayad ZA, Bagiella E, Zhao S, Nadkarni GN. Association of Treatment Dose Anticoagulation with in-Hospital Survival among Hospitalized Patients with COVID-19. J Am Coll Cardiol. 2020;76(1):122–124. doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Buijsers B, Yanginlar C, Maciej-Hulme ML, de Mast Q, van der Vlag J. Beneficial non-anticoagulant mechanisms underlying heparin treatment of COVID-19 patients. EBioMedicine. 2020;59:102969. doi: 10.1016/j.ebiom.2020.102969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hippensteel JA, LaRiviere WB, Colbert JF, Langouet-Astrie CJ, Schmidt EP. Heparin as a therapy for COVID-19: current evidence and future possibilities. Am J Physiol Lung Cell Mol Physiol. 2020;319(2):L211–L217. doi: 10.1152/ajplung.00199.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1334–1349. doi: 10.1056/NEJM200005043421806. [DOI] [PubMed] [Google Scholar]
- 119.George PM, Wells AU, Jenkins RG. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir Med. 2020;8(8):807–815. doi: 10.1016/S2213-2600(20)30225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang J, Wang BJ, Yang JC, Wang MY, Chen C, Luo GX, He WF. Advances in the research of mechanism of pulmonary fibrosis induced by Corona virus disease 2019 and the corresponding therapeutic measures. Zhonghua Shao Shang Za Zhi. 2020;36(0):E006. doi: 10.3760/cma.j.cn501120-20200307-00132. [DOI] [PubMed] [Google Scholar]
- 121.Burnham EL, Janssen WJ, Riches DW, Moss M, Downey GP. The fibroproliferative response in acute respiratory distress syndrome: mechanisms and clinical significance. Eur Respir J. 2014;43(1):276–285. doi: 10.1183/09031936.00196412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lucas R, Verin AD, Black SM, Catravas JD. Regulators of endothelial and epithelial barrier integrity and function in acute lung injury. Biochem Pharmacol. 2009;77(12):1763–1772. doi: 10.1016/j.bcp.2009.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Epstein Shochet G, Wollin L, Shitrit D. Fibroblast-matrix interplay: Nintedanib and pirfenidone modulate the effect of IPF fibroblast-conditioned matrix on normal fibroblast phenotype. Respirology. 2018;23(8):756–763. doi: 10.1111/resp.13287. [DOI] [PubMed] [Google Scholar]
- 124.Chow LN, Schreiner P, Ng BY, Lo B, Hughes MR, Scott RW, Gusti V, Lecour S, Simonson E, Manisali I, et al. Impact of a CXCL12/CXCR4 antagonist in Bleomycin (BLM) induced pulmonary fibrosis and carbon tetrachloride (CCl4) induced hepatic fibrosis in mice. PLoS One. 2016;11(3):e0151765. doi: 10.1371/journal.pone.0151765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Li F. Receptor recognition mechanisms of coronaviruses: a decade of structural studies. J Virol. 2015;89(4):1954–1964. doi: 10.1128/JVI.02615-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Pittet JF, Griffiths MJ, Geiser T, Kaminski N, Dalton SL, Huang X, Brown LA, Gotwals PJ, Koteliansky VE, Matthay MA, et al. TGF-beta is a critical mediator of acute lung injury. J Clin Invest. 2001;107(12):1537–1544. doi: 10.1172/JCI11963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Jenkins RG, Su X, Su G, Scotton CJ, Camerer E, Laurent GJ, Davis GE, Chambers RC, Matthay MA, Sheppard D. Ligation of protease-activated receptor 1 enhances alpha(v)beta6 integrin-dependent TGF-beta activation and promotes acute lung injury. J Clin Invest. 2006;116(6):1606–1614. doi: 10.1172/JCI27183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ganter MT, Roux J, Miyazawa B, Howard M, Frank JA, Su G, Sheppard D, Violette SM, Weinreb PH, Horan GS, et al. Interleukin-1beta causes acute lung injury via alphavbeta5 and alphavbeta6 integrin-dependent mechanisms. Circ Res. 2008;102(7):804–812. doi: 10.1161/CIRCRESAHA.107.161067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Allen RJ, Guillen-Guio B, Oldham JM, Ma SF, Dressen A, Paynton ML, Kraven LM, Obeidat M, Li X, Ng M, et al. Genome-wide association study of susceptibility to idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2020;201(5):564–574. doi: 10.1164/rccm.201905-1017OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lukey PT, Harrison SA, Yang S, Man Y, Holman BF, Rashidnasab A, et al. A randomised, placebo-controlled study of omipalisib (PI3K/mTOR) in idiopathic pulmonary fibrosis. Eur Respir J. 2019;53(3):1801992. 10.1183/13993003.01992-2018. [DOI] [PubMed]
- 132.Raghu G, van den Blink B, Hamblin MJ, Brown AW, Golden JA, Ho LA, Wijsenbeek MS, Vasakova M, Pesci A, Antin-Ozerkis DE, et al. Effect of recombinant human Pentraxin 2 vs placebo on change in forced vital capacity in patients with idiopathic pulmonary fibrosis: a randomized clinical trial. JAMA. 2018;319(22):2299–2307. doi: 10.1001/jama.2018.6129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Mikulska M, Nicolini LA, Signori A, Di Biagio A, Sepulcri C, Russo C, Dettori S, Berruti M, Sormani MP, Giacobbe DR, et al. Tocilizumab and steroid treatment in patients with COVID-19 pneumonia. PLoS One. 2020;15(8):e0237831. doi: 10.1371/journal.pone.0237831. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplemental Table 1 List of excluded studies and reason of exclusion.
Data Availability Statement
Not applicable.



