Abstract
BACKGROUND/OBJECTIVES:
Care-partner support affects outcomes among assisted living (AL) residents. Yet, little is known about care-partner support and its effects on hospitalization during post-acute care transitions. This study examined the variation in care-partner support and its impact on hospitalizations among AL residents receiving Medicare home health (HH) services.
DESIGN:
Analysis of national data from the Outcome and Assessment Information Set, Medicare claims, Area Health Resources File and the Social Deprivation Index File.
SETTING:
AL facilities and Medicare HH agencies in the U.S.
PARTICIPANTS:
741,926 Medicare HH admissions of AL residents in 2017.
MEASUREMENTS:
Care-partner support during the HH admission was measured based on the type and frequency of assistance from AL staff in seven domains (i.e., activities of daily living [ADL], instrumental ADLs [IADL], medication administration, treatment, medical equipment, home safety, and transportation). Care-partner support in each domain was measured as “assistance not needed” (reference group), “Care-partner currently provides assistance”, “care-partner need additional training / support to provide assistance” (i.e., inadequate care-partner support), and “care-partner unavailable / unlikely to provide assistance” (i.e., unavailable care-partner support). Outcome was time-to-hospitalization during the HH admission.
RESULTS:
Among the 741,926 Medicare HH admissions of AL residents, inadequate care-partner support was identified for all 7 domains that ranged from 13.1% (for transportation) to 49.8% (for treatment), and care-partner support was unavailable from 0.9% (for transportation) to 11.0% (for treatment). In Cox proportional hazard models adjusted for patient covariates and geography, compared with “assistance not needed”, having inadequate and unavailable care-partner support was related to increased risk of hospitalization by 8.9% (treatment [Hazard Ratio / HR =1.089, p<0.001]) to 41.3% (medication administration [HR =1.413, p<0.001]).
CONCLUSION:
For AL residents receiving HH services, having less care-partner support was related to increased risk of hospitalization, particularly regarding medication administration, medical equipment, and transportation/advocacy.
Keywords: Assisted Living Facilities, Care Partner, Home Health Care, Hospitalization, Medicare
BACKGROUND
Assisted living (AL) facilities represent one of the fastest growing residential care options that provides housing, personal care, social and some non-skilled health-related services to older adults who need supportive care.1 Many of the AL residents are older than 85 years (52%) and have limitations in activities of daily living (ADL; 64%), multiple chronic conditions (74%), cognitive impairment such as Alzheimer’s disease and related dementias (ADRD; 42%), and depressive symptoms (28%).2,3 Therefore, AL residents often need additional care support to age in place.
The need for care support is likely more pronounced when AL residents have significant health status changes, such as during post-acute care transitions. Home health (HH) care is the largest provider of Medicare-certified post-acute care in the patient’s home.4 HH care includes skilled nursing (medication reconciliation, patient education, care coordination), physical/occupational therapy (home exercise and home safety training]), and social work (engagement with community-based services and insurance coverage), as well as non-skilled personal care aide assistance (house making, cooking, laundry)5; all are provided in the patient’s home or place of primary residency such as AL. HH care is effective at improving physical function,6 reducing hospitalizations,7,8 and delaying nursing home admissions.9 AL residents commonly use HH services during post-acute care transitions.10 However, HH care is only provided intermittently (e.g., 2-3 visits/week),8 and additional care-partner support may be important to AL residents.11,12
Substantial variation exists in the availability and sources of care-partner support among AL residents. Research has shown that AL facilities with more licensed staff have lower rates of hospitalization and nursing home placement.13,14 However, most (83.3%) of AL staff are unlicensed (e.g., certified nurse assistants and personal care aides) and only 16% are licensed personnel such as registered nurses (6.1%) and licensed practical nurses (9.9%).15 Furthermore, AL staffing requirements16 vary across states.17 AL residents primarily receive support from AL care-partners, though some may be provided by privately hired aides, family and friends. Lastly, an AL resident’s need for support can manifest in multiple domains, including domains related to everyday activities (e.g., ADLs and IADLs) and domains important to disease management and medical tasks (e.g., administering medications and managing treatment equipment). No study has examined such variation in care-partner support or its adequacy among AL residents during care transitions, such as during post-acute HH care.
This study evaluated 1) the degree of care-partner support among AL residents while receiving Medicare HH care, and 2) the impact of care-partner support on risk of hospitalization in these residents during the HH admission. We hypothesized that AL residents with more care-partner support were less likely to be hospitalized during Medicare HH services.
METHODS
Data Source
This study utilized several 2017 national datasets including the Outcome and Assessment Information Set (OASIS),18 the Master Beneficiary Summary File (MBSF), the Area Health Resource File (AHRF), and the Social Deprivation Index (SDI)File. These datasets and the study variables derived from each were summarized in Supplemental Table 1.
Study Sample
The study included Medicare HH admissions in 2017 of Medicare beneficiaries 65 years or older who were AL residents. We identified AL residence using a validated approach based on an OASIS item on living situation and availability of assistance (M1100), where AL residence was identified if the living situation was “congregate residential care or assisted living facilities” and the availability of assistance was “around the clock”.10 AL residents who died during HH care were excluded. One AL resident may have more than one HH admission in 2017, and each HH admission may contain one or more 60-day episodes. The final sample included 741,926 Medicare HH admissions of 509,424 unique AL residents.
Dependent Variable.
Hospitalization.
Hospitalization during the HH admission was identified using OASIS records. We measured hospitalization as a time-to-event variable, i.e., number of days from the start date of HH admission to hospitalization date. If more than one hospitalization occurred during the HH admission, only the first was used to define the outcome. The HH admission ranged from 0 to 364 days with an average of 39 days.
Independent Variable.
Care-partner support was measured based on the frequency of care-partner assistance in seven domains during the HH admission (OASIS M2102), which is primarily provided by care-partners in AL. The seven domains of care-partner support included: 1) ADL (e.g., ambulation, bathing, dressing, toileting, eating); 2) IADL (e.g., housekeeping, laundry, and meal preparation); 3) medication management; 4) treatment (e.g., wound care, home exercise, insertion/removal of catheters, vital signs and blood glucose measurement); 5) medical equipment (e.g., oxygen and intravenous / ventilator therapy); 6) home safety (e.g., fall prevention and removal of environmental hazards); and 7) transportation / advocacy (e.g., medical appointment). In each domain, care-partner support was assessed by HH clinicians (i.e., mostly registered nurses) in four levels, including “assistance not needed” (reference group), “care-partner currently provides assistance”, “care-partner needs additional training / support to provide assistance” (referred to as “inadequate care-partner support”), and “care-partner unavailable / unlikely to provide assistance” (referred to as “unavailable care-partner support”). This item (OASIS M2102) has satisfactory reliability (Cohen’s k=0.59, percent agreement=89.8%)19 and has been used in multiple previous studies to assess care support during transitional HH care.12,20,21
Patient Covariates
Patient covariates included demographics (age, sex, race/ethnicity, Medicare-Medicaid dual eligibility [full/partial/no Medicaid benefits22], Medicare insurance type [Medicare fee-for-service/Medicare Advantage]) and the following health status variables: 1) Charlson comorbidity index calculated, 3) body mass index (BMI), 4) severe pain, 5) unhealed pressure ulcer with open wound (≥ stage II) present, 6) depressive symptoms (Patient Health Questinnaire-2 score ≥3 / physician-prescribed depression intervention in care plan), and 7) composite ADL limitation, which was measured using the corrected Likert approach23–28 - based on nine OASIS items on ADLs (i.e., grooming, dressing, bathing, toilet transferring, toilet hygiene, transferring, ambulation, and eating), where a higher score (range 0-9) indicates more ADL limitations.25
Geographic Covariates
Given the geographic variation in HH29 and AL,3 we controlled for county fixed effects (dummy variables) and zip code-level SDI.
Statistical Analysis
Descriptive statistics were used to summarize sample characteristics as means (standard deviations [S.D.]) or median (interquartile range) for continuous variables and frequency (%, [N]) for categorical variables. We examined the relationship of care-partner support with hospitalization using survival analysis to account for censoring related to the duration of HH admission, because information on hospitalization was not available beyond the HH admission. To estimate the relationship between care-partner support and hospitalization across the seven domains, we fit separate multivariate Cox proportional hazard models for each domain as the independent variable. The proportional-hazards assumption was not violated, as shown in results of log-log plot of survival and Kaplan-Meier and predicted survival plot. Sensitivity analyses were conducted using only the initial HH admission of each AL resident in CY 2017. Statistical analyses were conducted using Stata 15.1 (College Station, TX).
Results
AL residents with unavailable care-partner support in at least one of the seven domains (13.6%) were more likely to be racial/ethnic minorities, dual eligible, to live in more socially deprived zip codes, to have higher Charlson comorbidity index, depressive symptoms, unhealed pressure ulcer with open wound, and longer HH admission. Table 1 provides a detailed breakdown of sample characteristics.
Table 1.
Sample Characteristics (N=741,926)
| Variable | Caregiver Support Cohorts | P-value* | |
|---|---|---|---|
| Having unavailable caregiver support in ≥ 1 of the 7 domains (n=641,077, 86.4%) | Not having unavailable caregiver support in any of the 7 domains (n=100,849, 13.6%) | ||
| Age, mean (S.D.) | 82.1 (12.03) | 82.8(11.02) | <0.001 |
| Female, %(N) | 64.5% (64,997) | 67.0% (429,539) | <0.001 |
| Race/ethnicity, N(%) | |||
| – Non-Hispanic White | 83.9 % (84,623) | 89.8% (575,817) | <0.001 |
| – Non-Hispanic Black | 4.8 % (4,791) | 4.8% (30,466) | |
| – Hispanics | 9.5% (9,588) | 3.2% (20,390) | |
| – Others (including Asians and other non-Hispanic, non-white groups) | 1.8% (1,847) | 2.2% (14,404) | |
| Medicare-Medicaid dual eligibility, %(N) | |||
| – Medicare Only | 66.9% (67,520) | 75.9 % (486,690) | <0.001 |
| – Full eligible | 2.3% (22,456) | 16.1% (103,079) | |
| – Partial eligible | 10.8% (10,873) | 8.0% (51,308) | |
| Medicare insurance type, %(N) | |||
| – Medicare fee-for-service | 76.3% (76,949) | 71.6% (458,931) | |
| – Medicare Advantage | 23.7% (23,900) | 28.4% (182,146) | |
| Body mass index, mean (S.D.) | 26.8 (5.53) | 26.5 (5.20) | <0.001 |
| Chronic conditions, %(N) | |||
| – Acute Myocardial Infarction | 9.3% (9,398) | 9.0% (57,424) | <0.001 |
| – Alzheimer’s Disease | 32.2% (32,433) | 30.9% (198,106) | <0.001 |
| – Alzheimer’s Disease and Related Disorders | 64.7% (65,266) | 62.3% (399,481) | <0.001 |
| – Atrial Fibrillation | 30.2% (30,447) | 28.9% (185,471) | <0.001 |
| – Cataract | 74.4% (75,006) | 73.9% (473,971) | 0.003 |
| – Chronic Kidney Disease | 58.3% (58,803) | 52.7% (337,806) | <0.001 |
| – Chronic Obstructive Pulmonary Disease | 47.5% (47,919) | 40.9% (262,352) | <0.001 |
| – Heart Failure | 55.3% (55,784) | 50.3% (322,171) | <0.001 |
| – Diabetes | 52.4% (52,811) | 45.0% (288,304) | <0.001 |
| – Glaucoma | 30.2% (30,438) | 27.6% (176,963) | <0.001 |
| – Hip/Pelvic Fracture | 16.0% (16,108) | 15.9% (101,977) | 0.598 |
| – Ischemic Heart Disease | 70.4% (70,968) | 63.9% (409,855) | <0.001 |
| – Depression | 68.5% (69,121) | 63.0% (404,134) | <0.001 |
| – Osteoporosis | 40.0% (40,378) | 39.0% (250,187) | <0.001 |
| – Rheumatoid Arthritis/Osteoarthritis | 77.1% (77,720) | 72.8% (466,454) | <0.001 |
| – Stroke/Transient Ischemic Attack | 33.5% (33,823) | 33.0% (211,255) | <0.001 |
| – Breast Cancer | 7.9% (8,008) | 7.9% (50,582) | 0.581 |
| – Colorectal Cancer | 4.4% (4,382) | 4.1% (26,490) | 0.002 |
| – Prostate Cancer | 5.9% (5,945) | 5.5% (35,057) | <0.001 |
| – Lung Cancer | 2.1% (2,078) | 1.9% (11,879) | <0.001 |
| – Endometrial Cancer | 1.5% (1,471) | 1.5% (9,277) | 0.776 |
| – Anemia | 81.1% (81,784) | 76.4% (489,727) | <0.001 |
| – Asthma | 22.3% (22,492) | 19.6% (125,451) | <0.001 |
| – Hyperlipidemia | 83.4% (84,074) | 80.3% (514,483) | <0.001 |
| – Benign Prostatic Hyperplasia | 22.5% (22,680) | 20.0% (128,395) | <0.001 |
| – Hypertension | 90.2% (90,973) | 86.9% (557,153) | <0.001 |
| – Acquired Hypothyroidism | 44.6% (45,014) | 41.5% (266,072) | <0.001 |
| Having present moderate to severe cognitive impairment, %(N) | 61.9% (62,463) | 62.5% (400,353) | 0.002 |
| Having present depressive symptoms, %(N) | 31.4% (31,685) | 29.2% (187,441) | <0.001 |
| Composite activities of daily living (ADL) limitation score, mean (S.D.) | 4.6 (1.69) | 4.7 (1.58) | <0.001 |
| Having present severe pain, %(N) | 20.7% (20,885) | 21.7% (139,366) | <0.001 |
| Having present unhealed pressure ulcer ≥ stage II, %(N) | 9.9% (9,979) | 5.6% (35,834) | <0.001 |
| Days of index home health admission (mean [median, Q1, Q3]) | 43.7 (37.6, 22.8, 50.6) | 42.0 (37.5, 22.5, 50.6) | <0.001 |
| Number of home health agencies per 1000 older adults age 65+ in the county of patient residence, mean (S.D.) | 0.3(0.27) | 0.2 (0.26) | <0.001 |
| Number of hospital beds per 1000 older adults age 65+ in the county of patient residence, mean (S.D.) | 15.5 (8.95) | 15.5 (10.22) | 0.979 |
| Number of skilled nursing facility beds per 1000 older adults age 65+ in the county of patient residence, mean (S.D.) | 29.6 (14.8) | 31.3 (14.8) | <0.001 |
| Social deprivation index | 49.5 (27.07) | 47.6 (26.53) | <0.001 |
p-value based on Chi Square (categorical variables) and T test (continuous variables) analyses
At the start of the HH admission, AL residents needed care-partner support in all the seven assessed domains, including IADL (99.6%), transportation (98.9%), ADL (98.5%), medication administration (97.2%), safety (93.2%), treatment (84.8%) and medical equipment (53.9%). Inadequate care-partner support was noted in treatment (49.8%), ADLs (41.4%), and medication administration (33.0%). In addition, unavailable care-partner support was noted in 0.9% (for transportation) to 11.0% (for treatment) of these HH admissions of AL residents (see Table 2 and Figure 1).
Table 2.
Levels of Caregiver Support in Seven Domains (N=741,926)
| Caregiver Support Categories | Activities of Daily Living+ | Instrumental Activities of Daily Living++ | Medication Administration | Treatment* | Equipment** | Safety | Transportation / Advocacy |
|---|---|---|---|---|---|---|---|
| no assistance needed, %(N) | 1.5% (11,399) | 0.4% (2,540) | 2.8% (20,485) | 15.2% (113,172) | 46.1% (341,923) | 6.8% (50,340) | 1.1% (7,097) |
| non-home health caregiver(s) currently provide assistance, %(N) | 54.8% (406,455) | 79.4% (589,073) | 61.8% (458,436) | 24.0% (177,947) | 28.1% (208,797) | 62.9% (466,412) | 84.9% (630,282) |
| non-home health caregiver(s) need training/supportive services to provide assistance, %(N) | 41.4% (307,018) | 19.2% (142,678) | 33.0% (244,820) | 49.8% (369,337) | 24.1% (178,405) | 29.2% (216,727) | 13.1% (96,981) |
| non-home health caregiver(s) are unavailable / unclear / unlikely to provide assistance in this area, %(N) | 2.3% (17,054) | 1.0% (7,635) | 2.4% (18,185) | 11.0% (81,470) | 1.7% (12,801) | 1.1% (8,447) | 0.9% (6,756) |
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
Activities of daily living include ambulation, bathing, dressing, toileting, eating;
Instrumental activities of daily living include housekeeping, laundry, and meal preparation;
Examples of caregiver support with treatment: changing wound dressings, home exercise, insertion/removal of catheters, measurement of vital signs and blood glucose, etc.;
Examples of caregiver support with equipment: oxygen, IV/infusion equipment, ventilator therapy, wheelchairs, etc.;
Figure 1.
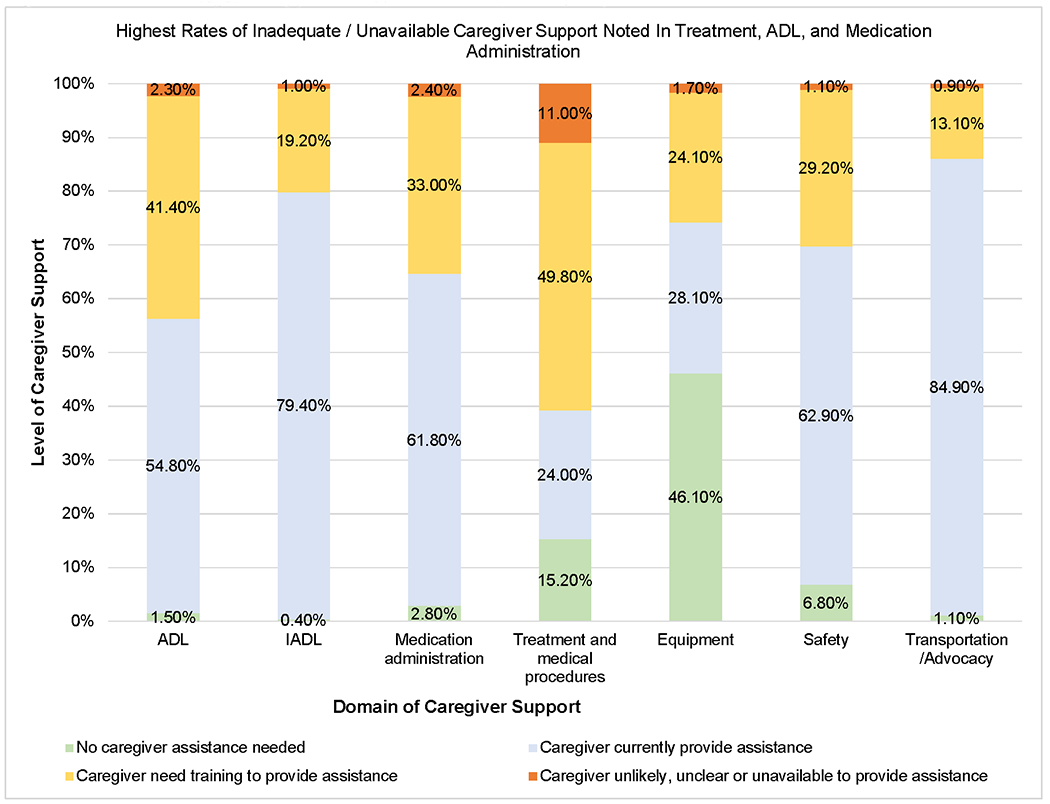
Levels of Care-Partner Support In Seven Domains (N=741,926)
In Cox proportional hazard models of time-to-hospitalization that adjusted for patient and geographic covariates, care-partner support of different levels and domains were significantly related to the risk of hospitalization (Figure 2, Table 3). Specifically, having unavailable care-partner support was related to increased risk of hospitalization, particularly for domains of medication administration (Hazard Ratio [HR] = 1.413, 95% confidence interval [CI]: 1.352, 1.478; p<0.001), transportation / advocacy (e.g., for medical appointments; HR=1.204, 95% CI: 1.123, 1.291; p<0.001), and home safety (HR=1.158, 95% CI: 1.103, 1.215, p<0.001), as compared to AL residents who did not need care-partner support in these domains, respectively.
Figure 2.
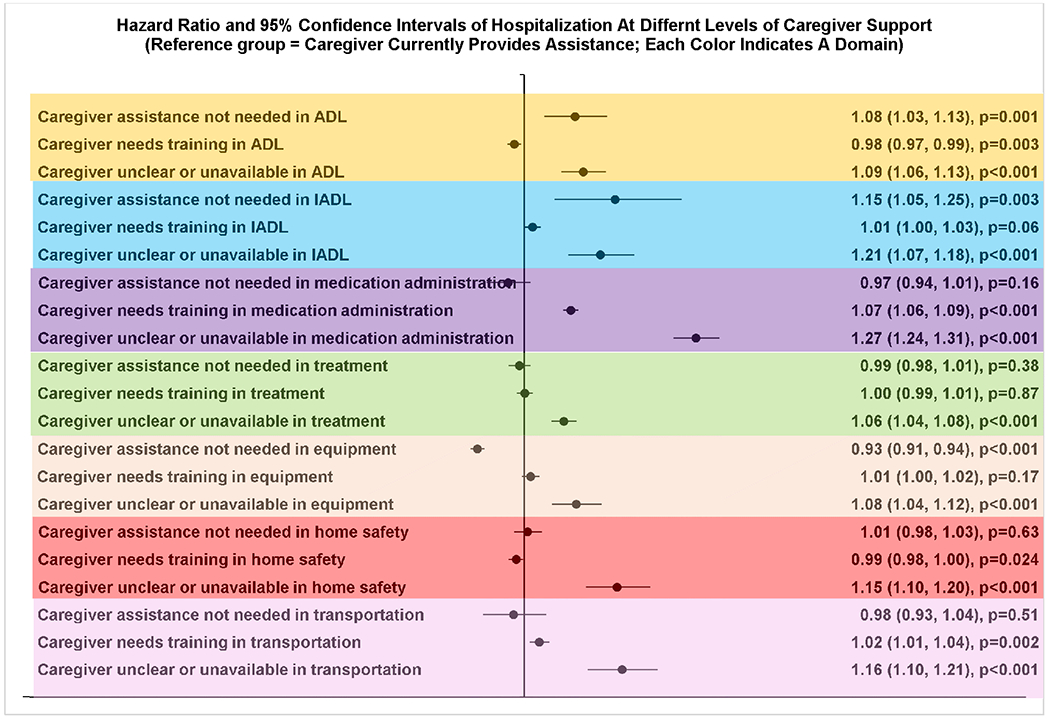
Relationship Between Care-Partner Support and Hospitalization (N=741,926).
Table 3.
Relationship Between Caregiving Support and Hospitalization (N=741,926)
| Domain of caregiver support | Level of caregiving support (reference group = caregiver provides assistance) | Hospitalization | |||
|---|---|---|---|---|---|
| Hazard Ratio | 95% Confidence Interval | p-value | |||
| ADL | Caregiver assistance not needed | 1.081 | 1.032 | 1.132 | 0.001 |
| Caregiver needs training | 0.984 | 0.973 | 0.995 | 0.003 | |
| Caregiver unclear or unavailable | 1.094 | 1.059 | 1.130 | <0.001 | |
| IADL | Caregiver assistance not needed | 1.145 | 1.048 | 1.251 | 0.003 |
| Caregiver needs training | 1.013 | 1.000 | 1.026 | 0.057 | |
| Caregiver unclear or unavailable | 1.121 | 1.070 | 1.175 | <0.001 | |
| Medication administration | Caregiver assistance not needed | 0.974 | 0.940 | 1.010 | 0.155 |
| Caregiver needs training | 1.074 | 1.062 | 1.086 | <0.001 | |
| Caregiver unclear or unavailable | 1.274 | 1.238 | 1.311 | <0.001 | |
| Treatment | Caregiver assistance not needed | 0.992 | 0.975 | 1.010 | 0.381 |
| Caregiver needs training | 1.001 | 0.988 | 1.014 | 0.865 | |
| Caregiver unclear or unavailable | 1.063 | 1.043 | 1.083 | <0.001 | |
| Medical Equipment | Caregiver assistance not needed | 0.925 | 0.914 | 0.937 | <0.001 |
| Caregiver needs training | 1.010 | 0.996 | 1.024 | 0.166 | |
| Caregiver unclear or unavailable | 1.083 | 1.044 | 1.123 | <0.001 | |
| Home Safety | Caregiver assistance not needed | 1.005 | 0.984 | 1.028 | 0.631 |
| Caregiver needs training | 0.987 | 0.975 | 0.998 | 0.024 | |
| Caregiver unclear or unavailable | 1.148 | 1.098 | 1.201 | <0.001 | |
| Transportation | Caregiver assistance not needed | 0.983 | 0.934 | 1.035 | 0.508 |
| Caregiver needs training | 1.024 | 1.009 | 1.040 | 0.002 | |
| Caregiver unclear or unavailable | 1.156 | 1.101 | 1.213 | <0.001 | |
Having inadequate care-partner support (i.e., care-partner needs training) was not consistently related to increase or decrease in the risk of hospitalization. Specifically, compared to AL residents who did not need care-partner support in a specific domain, having inadequate care-partner support was related to increased risk of hospitalization for medication administration (HR=1.158, 95% CI: 1.117, 1.201; p<0.001), transportation / advocacy (HR=1.047, 95% CI:0.993 1.104; p=0.091), equipment (HR=1.130, 95% CI 1.115, 1.145, p<0.001), treatment (HR=1.014, 95% CI: 0.998, 1.030; p=0.081), related to decreased risk of hospitalization for ADL (HR=0.992, 95% CI: 0.880, 0.967, p=0.001), home safety (HR=0.978, 95% CI: 0.955, 1.001, p=0.058), and IADL (HR=0.899, 95%CI 0.822, 0.983, p=0.019) (Figure 2, Table 3). Full models specific to each domain were shown in Supplementary Tables S2–S8. Sensitivity analysis conducted using only the initial HH admissions in CY2017 showed consistent results (Supplementary Table S9).
Discussion
This study was the first to examine care-partner support among AL residents who received Medicare HH services using national HH data. The two principal findings supported our hypotheses. First, the degree of care-partner support among AL residents while receiving Medicare HH care varied across the seven domains. Of note, 13.6% of the AL residents had unavailable care-partner support in at least one domain and they were more likely to be socially disadvantaged individuals (i.e., racial/ethnic minorities, dual eligible persons, and those living in communities of higher SDI index) who had depressive symptoms and spent more days in HH. Second, in domains that required procedural skilled care, particularly medication administration, treatment, transportation /advocacy for medical appointments, and equipment, having inadequate or unavailable care-partner support was associated with increased risk of hospitalization in AL residents. Such finding highlights the need for more intensive post-acute care of AL residents from skilled care providers, preferably before the patients return to AL facilities.
Findings in this study are consistent with prior data on inadequate care-partner support (32%) in AL facilities,30 especially for medication administration, treatment monitoring and assistance with adherence, and management of equipment that may be related to the lack of licensed staff in AL facilities. Data from the National Survey of Residential Care Facilities and the National Study of Long-Term Care Providers have shown that fewer than half of the AL facilities had licensed staff (registered and licensed practical nurses)17 and that within each AL, on average, only 6.1% of staff were licensed professionals such as registered nurses and licensed practical nurses.15,31 Our study, along with previous studies, found that even though AL facilities often provide non-skilled care support such as ADL and IADL assistance,3,31 AL residents may still have unmet needs for care-partner support in these domains during post-acute transitional care period.
There is a lack of federal regulations on the quality of AL care or on appropriate staffing in AL, and substantial variation exist in state regulatory stringency of AL regarding staffing and training, admission and retention criteria, provision of services such as medication administration, and specialized dementia care units.3,16,32–34 It is therefore unclear if the gap in care-partner support we noted in this study was transient due to worsened health status and post-acute care transition, or that AL residents, over the years since AL admission, have developed substantial functional impairments whose needs for support may have exceeded the level of support available at AL and may be better cared for with intensive support at a skilled nursing facility. It is important that potentially unmet needs in skilled care among AL residents be screened and met, particularly during care transitions such as after an acute hospitalization.
Previous studies with Medicare HH recipients have shown that persons with more caregiver support showed greater functional improvement21 with better discharge readiness35 at HH discharge, whereas those with inadequate caregiver support were more prone to risks of hospitalization,12,36,37 ED visit,38 and nursing home admission.39 The present study extends prior findings and highlighted domains that exert significant impacts on patient outcomes and domains where additional care-partner support is particularly inadequate, which are likely related to tasks that care-partners find to be challenging and need the most training with. Recent reports from the American Association of Retired Persons and National Alliance for Caregiving highlighted that there are 53 million Americans providing care to a family member or a friend in 2020, among whom 61% are working, 45% report financial strain, and 26% have recent health decline of themselves.40,41 In addition, family caregivers report much strain, burden and fear while conducting complicated and often medically related tasks with little to no training or support from health professionals, and while the care recipients develop increasingly complex needs for medical or care support.40,41 Findings in this study provide clear implications and priorities for future programs that aim at enhancing patient outcomes in the AL community, such as by improving support for care-partners with regard to medication administration, treatment adherence, and access to as well as follow-up with medical appointments.
The link between care-partner support and patient outcomes may be related to the complexity and intensity of support needed by AL residents during transitional care, when inadequate support can lead to medication errors, falls42 and healthcare-related infection20 – all are common causes of hospitalization. Given that AL residents have an average of 10 chronic conditions, take multiple medications, and have prevalent ADRD - all suggesting increased need for skilled care from trained professionals (e.g., nurses and care managers), it is likely that medically related support to them that is provided by unlicensed care-partners or family members is inadequate.
Care support for AL residents during transitional care may resemble two ends of a bridge that are not connected. On the one end, caregivers, such as AL care-partners, spend considerable amount of time with the residents, yet they lack the training and skills to undertake complex and often medically related tasks. In the U.S., family caregivers of community-dwelling older adults, including those with ADRD, reported providing complex medical care tasks such as skin/wound care43 and medication management44 without adequate training, yet with much stress and fear of making mistakes that will harm the patient.41 Although AL staff (mostly unlicensed) may have more training than family caregivers, it is important that enough training and resources be provided to AL staff to ensure safety of care. On the other end, trained health care professionals, such as HH clinicians, albeit having the skills to provide complex skilled care, often visit the patients intermittently, thus not being able to provide continuous support for the patient. This suggests that targeted collaboration between HH clinicians and caregivers such as AL care-partners on these complicated, medically related tasks (e.g., medication administration and medical equipment management) may be the missing piece to bridge the gap.
It is unclear why AL residents with inadequate care-partner support in ADL, IADL, and home safety had slightly lower risk of hospitalization than those who did not need support in these domains, respectively. A possible explanation is that care-partner support assessment at the start of HH admission may have resulted in increased attentiveness of AL care-partners to resident ADL and home safety needs, such as in fall prevention, during the HH episode, thus lowering their risk of hospitalization. In contrast, because ALs often do not provide skilled care services that HH does,31 inadequate care-partner support for more skilled care domains, such as medication administration and management of medical equipment, may not be easily corrected during an HH admission even when they are identified in an initial HH visit, due to the lack of licensed and skilled staff in AL.
This study has several limitations. First, due to lack of data on AL characteristics in this national study, differences in staffing and structural variables across ALs were not controlled for in multivariate models, thus residual confounding may be present in the estimated associations. Second, care-partner support measured in OASIS only reflected the need and supply of care-partner support during the HH admission, which was assessed by HH clinicians given the information that was available at the start of HH care. Future research is needed to employ comprehensive measures to assess all types of care support among AL residents not only during HH admission but also in other time periods, such as after the HH admission is complete and no HH oversight is provided.
CONCLUSION
During the period when AL residents were receiving Medicare HH services, having more care-partner support reduced their risk of hospitalization by up to 27%, highlighting the need for more intensive, skilled post-acute care support among AL residents. Care-partner support involves multiple domains and should be assessed to meet specific patient needs, which vary from person to person. Among the seven assessed domains of care-partner support, those that led to the most pronounced changes in the risk of hospitalization were related to procedural skills, such as medication administration, transportation for medical appointments, and medical equipment; these domains should be prioritized in future programs that aimed to improve care-partner support and prevent hospitalizations of AL residents. Dedicated and specific efforts should be made to bridge the support from AL care-partners that from skilled care HH clinicians to ensure that AL resident needs are met during post-acute care transitions.
Supplementary Material
Supplementary Table S1. Overview of Data and Variables
Supplementary Table S2. Care-Partner Support in Activities of Daily Living (ADL) and Hospitalization
Supplementary Table S3. Care-Partner Support in Instrumental Activities of Daily Living (IADL) and Hospitalization
Supplementary Table S4. Care-Partner Support in Medication Administration And Hospitalization
Supplementary Table S5. Care-Partner Support in Treatment And Hospitalization
Supplementary Table S6. Relationship Between Care-Partner Support in Equipment* on Hospitalization And Assisted Living Residents
Supplementary Table S7. Care-Partner Support in Home Safety And Hospitalization
Supplementary Table S8. Care-Partner Support in Transportation And Hospitalization
Supplementary Table S9. Sensitivity analysis with each patient’s initial HH admission in CY 2017 (N=443,956)
Key Points:
Care-partner support is critical for outcomes of assisted living (AL) residents during care transitions.
Assisted living (AL) residents had inadequate / unavailable care-partner support from AL staff, family, or privately hired aides in skilled care domains, particularly medication administration, assistance with treatment, and management of medical equipment.
The most pronounced increase in the risk of hospitalization during care transition was related to unavailable care-partner support for medication administration (by 41%.).
Why does this paper matter?
This study, among the first to examine care-partner support in AL residents during care transitions, showed that dedicated efforts should be made to bridge the support from AL care-partners and that from short-term home health clinicians, to fully meet AL resident needs in post-acute care transitions.
ACKNOWLEDGMENTS
Funding Statement: This study was conducted with the support of the following funders: Elaine C. Hubbard Center for Nursing Research on Aging Research Endowed Award (JW), Terry Family Research Endowed Award (JW), Valerie and Frank Furth Fund Award (JW) and the Agency for Health Care Research and Quality (AHRQ; R01HS026893 [HTG, YL]). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflict of Interest
The authors declare no conflicts of interest, financial, personal, or other related to this manuscript.
References
- 1.Zimmerman S, Gruber-Baldini AL, Sloane PD, et al. Assisted Living and Nursing Homes: Apples and Oranges? Gerontologist. 2003;43(suppl_2):107–117. [DOI] [PubMed] [Google Scholar]
- 2.Wang J, Kearney JA, Jia H, Shang J. Mental Health Disorders in Elderly People Receiving Home Care: Prevalence and Correlates in the National U.S. Population. Nurs Res. 2016;65(2):107–116. [DOI] [PubMed] [Google Scholar]
- 3.Caffrey C, Sengupta M, Park-Lee E, Moss A, Rosenoff E, Harris-Kojetin L. Residents Living in Residential Care Facilities: United States, 2010. NCHS Data Brief. 2012(91):1. [PubMed] [Google Scholar]
- 4.Medicare Payment Advisory Commission. A Data Book: Health Care Spending and the Medicare Program. Washington, DC; 2020. June. Available at: http://www.medpac.gov/-documents-/data-book. Accessed August 21, 2020. [Google Scholar]
- 5.Centers for Medicare & Medicaid Services (CMS). What’s Home Health Care? 2020. Available at: http://www.medicare.gov/what-medicare-covers/home-health-care/home-health-care-what-is-it-what-to-expect.html. Accessed August 21, 2020.
- 6.Wang J, Yu F, Cai X, Caprio TV, Li Y. Functional Outcome in Home Health: Do Racial and Ethnic Minority Patients With Dementia Fare Worse? PLoS One. 2020;15(5):e0233650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang J, Caprio TV, Simning A, et al. Association Between Home Health Services and Facility Admission in Older Adults With and Without Alzheimer’s Disease. J Am Med Dir Assoc. 2020;21(5):627–633.e9. doi: 10.1016/j.jamda.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Wang J, Liebel DV, Yu F, Caprio TV, Shang J. Inverse Dose-Response Relationship Between Home Health Care Services and Rehospitalization in Older Adults. J Am Med Dir Assoc. 2019;20(6):736–742. doi: 10.1016/j.jamda.2018.10.021. [DOI] [PubMed] [Google Scholar]
- 9.Young Y, Kalamaras J, Kelly L, Hornick D, Yucel R. Is Aging in Place Delaying Nursing Home Admission? J Am Med Dir Assoc. 2015;16(10):900.e901–900.e906. [DOI] [PubMed] [Google Scholar]
- 10.Nazareno J, Zhang W, Silver B, Dosa D, Gozalo P, Thomas K. Home Health Utilization in Assisted Living Settings. Med Care Res Rev. 2019:1077558719835049. doi: 10.1177/1077558719835049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang J, Simmons S, Maxwell CA, Schlundt DG, Mion L Home Health Nurses’ Perspectives and Care Processes Related to Older Persons with Frailty and Depression: A Mixed Method Pilot Study. J Community Health Nurs. 2018;35(3):118–136. doi: 10.1080/07370016.2018.1475799. [DOI] [PubMed] [Google Scholar]
- 12.Knox S, Downer B, Haas A, Middleton A, Ottenbacher KJ. Function and Caregiver Support Associated With Readmissions During Home Health for Individuals With Dementia. Arch Phys Med Rehabil. 2020;101(6):1009–1016. doi: 10.1016/j.apmr.2019.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stearns SC, Park J, Zimmerman S, Gruber-Baldini AL, Konrad TR, Sloane PD. Determinants and Effects of Nurse Staffing Intensity and Skill Mix In Residential Care/Assisted Living Settings. Gerontologist. 2007;47(5):662–671. doi: 10.1093/geront/47.5.662. [DOI] [PubMed] [Google Scholar]
- 14.Maxwell CJ, Soo A, Hogan DB, et al. Predictors of Nursing Home Placement from Assisted Living Settings in Canada. Can J Aging. 2013;32(4):333–348. doi: 10.1017/S0714980813000469. [DOI] [PubMed] [Google Scholar]
- 15.Harris-Kojetin L SM, Lendon JP, Rome V, Valverde R, Caffrey C. Long-term Care Providers and Services Users in the United States, 2015–2016. National Center for Health Statistics. Vital Health Stat 3(43). 2019. [PubMed] [Google Scholar]
- 16.Rome V, Harris-Kojetin L, Carder P. Variation in Licensed Nurse Staffing Characteristics by State Requirements in Residential Care. Res Gerontol Nurs. 2019;12(1):27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han K, Trinkoff AM, Storr CL, Lerner N, Yang BK. Variation Across U.S. Assisted Living Facilities: Admissions, Resident Care Needs, and Staffing. J Nurs Scholarsh. 2017;49(1):24–32. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services [CMS]. OASIS Data Sets, 2020; Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/OASIS-Data-Sets. Accessed August 21, 2020.
- 19.O’Connor M, Davitt JK. The Outcome and Assessment Information Set (OASIS): A Review of Validity and Reliability. Home Health Care Serv Q. 2012;31(4):267–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osakwe ZT, Larson E, Shang J. Urinary Tract Infection-Related Hospitalization Among Older Adults Receiving Home Health Aare. Am J Infect Control. 2019;47(7):786–792.e781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho E, Kim EY, Lee NJ. Effects of Informal Caregivers on Function of Older Adults in Home Health Care. West J Nurs Res. 2013;35(1):57–75. [DOI] [PubMed] [Google Scholar]
- 22.Riley GF, Zhao L, Tilahun N. Understanding Factors Associated With Loss of Medicaid Coverage Among Dual Eligibles Can Help Identify Vulnerable Enrollees. Health Aff (Millwood). 2014;33(1):147–152. [DOI] [PubMed] [Google Scholar]
- 23.Scharpf TP, Madigan EA. Functional Status Outcome Measures In Home Health Care Patients With Heart Failure. Home Health Care Serv Q. 2010;29(4):155–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fortinsky RH, Garcia RI, Joseph Sheehan T, Madigan EA, Tullai-McGuinness S. Measuring Disability in Medicare Home Care Patients: Application of Rasch Modeling to the Outcome and Assessment Information Set. Med Care. 2003;41(5):601–15. doi: 10.1097/01.MLR.0000062553.63745.7A. [DOI] [PubMed] [Google Scholar]
- 25.Madigan EA, Gordon N, Fortinsky RH, Koroukian SM, Piña I, Riggs JS. Predictors of Functional Capacity Changes in a U.S. Population of Medicare Home Health Care Patients with Heart Failure. Arch Gerontol Geriatr. 2012;54(3):e300–e306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Osakwe ZT, Larson E, Andrews H, Shang J. Activities of Daily Living of Home Healthcare Patients. Home Healthc Now. 2019;37(3):165–173. doi: 10.1097/NHH.0000000000000736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Asiri FY, Marchetti GF, Ellis JL, et al. Predictors Of Functional And Gait Outcomes For Persons Poststroke Undergoing Home-based Rehabilitation. J Stroke Cerebrovasc Dis. 2014;23(7):1856–1864. [DOI] [PubMed] [Google Scholar]
- 28.Russell D, Rosati RJ, Peng TR, Barrón Y, Andreopoulos E. Continuity In The Provider Of Home Health Aide Services And The Likelihood Of Patient Improvement In Activities Of Daily Living. Home Health Care Management & Practice. 2013;25(1):6–12. [Google Scholar]
- 29.Reschovsky JD, Ghosh A, Stewart KA, Chollet DJ. Durable Medical Equipment And Home Health Among The Largest Contributors To Area Variations In Use Of Medicare Services. Health Aff (Millwood). 2012;31(5):956–964. [DOI] [PubMed] [Google Scholar]
- 30.Freedman VA, Spillman BC. The Residential Continuum From Home To Nursing Home: Size, Characteristics And Unmet Needs Of Older Adults. J Gerontol B Psychol Sci Soc Sci. 2014;69(Suppl 1):S42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khatutsky G, Ormond C, Wiener JM, Greene AM, Johnson R, Jessup EA, Vreeland E, Sengupta M, Caffrey C, HarrisKojetin L. Residential Care Communities And Their Residents In 2010: A National Portrait. DHHS Publication No. 2016-1041. Hyattsville, MD: National Center for Health Statistics. 2016. [Google Scholar]
- 32.Thomas KS, Zhang W, Cornell PY, Smith L, Kaskie B, Carder PC. State Variability in the Prevalence and Healthcare Utilization of Assisted Living Residents with Dementia. J Am Geriatr Soc. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carder PC. State Regulatory Approaches for Dementia Care in Residential Care and Assisted Living. Gerontologist. 2017;57(4):776–786. [DOI] [PubMed] [Google Scholar]
- 34.Kisling-Rundgren A, Paul DP III, Coustasse A. Costs, staffing, and services of assisted living in the United States: A Literature Review. Health Care Manag. 2016;35(2):156–163. [DOI] [PubMed] [Google Scholar]
- 35.O’Connor M, Moriarty H, Madden-Baer R, Bowles KH. Identifying Critical Factors in Determining Discharge Readiness from Skilled Home Health: An Interprofessional Perspective. Res Gerontol Nurs. 2016;9(6):269–277. [DOI] [PubMed] [Google Scholar]
- 36.Rosati RJ, Huang L, Navaie-Waliser M, Feldman PH. Risk Factors for Repeated Hospitalizations Among Home Healthcare Recipients. J Healthc Qual. 2003;25(2):4–11. [DOI] [PubMed] [Google Scholar]
- 37.Ma C, Shang J, Miner S, Lennox L, Squires A. The Prevalence, Reasons, and Risk Factors for Hospital Readmissions Among Home Health Care Patients: A Systematic Review. Home Health Care Management & Practice. 2017:1084822317741622. [Google Scholar]
- 38.Burgdorf J, Mulcahy J, Amjad H, Kasper JD, Covinsky K, Wolff JL. Family Caregiver Factors Associated With Emergency Department Utilization Among Community-Living Older Adults With Disabilities. J Prim Care Community Health. 2019;10:2150132719875636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blackburn J, Albright KC, Haley WE, et al. Men Lacking a Caregiver Have Greater Risk of Long-Term Nursing Home Placement After Stroke. J Am Geriatr Soc. 2018;66(1):133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.AARP and National Alliance for Caregiving. Caregiving in the United States 2020. Washington, DC: AARP. May 2020. 10.26419/ppi.00103.001 [DOI] [Google Scholar]
- 41.Reinhard S Home Alone Revisited: Family Caregivers Providing Complex Care. Washington, DC: AARP Public Policy Institute, 2019. Available at: https://www.aarp.org/content/dam/aarp/ppi/2019/04/home-alone-revisited-family-caregivers-providing-complex-care.pdf. Accessed August 21, 2020. [Google Scholar]
- 42.Irani E, Hirschman KB, Cacchione PZ, Bowles KH. The Role of Social, Economic, and Physical Environmental Factors in Care Planning for Home Health Care Recipients. Res Gerontol Nurs. 2020;13(3):130–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beach SR, Schulz R. Family Caregiver Factors Associated with Unmet Needs for Care of Older Adults. J Am Geriatr Soc. 2017;65(3):560–566. [DOI] [PubMed] [Google Scholar]
- 44.Polenick CA, Stanz SD, Leggett AN, Maust DT, Hodgson NA, Kales HC. Stressors and Resources Related to Medication Management: Associations With Spousal Caregivers’ Role Overload. Gerontologist. 2020;60(1):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. Overview of Data and Variables
Supplementary Table S2. Care-Partner Support in Activities of Daily Living (ADL) and Hospitalization
Supplementary Table S3. Care-Partner Support in Instrumental Activities of Daily Living (IADL) and Hospitalization
Supplementary Table S4. Care-Partner Support in Medication Administration And Hospitalization
Supplementary Table S5. Care-Partner Support in Treatment And Hospitalization
Supplementary Table S6. Relationship Between Care-Partner Support in Equipment* on Hospitalization And Assisted Living Residents
Supplementary Table S7. Care-Partner Support in Home Safety And Hospitalization
Supplementary Table S8. Care-Partner Support in Transportation And Hospitalization
Supplementary Table S9. Sensitivity analysis with each patient’s initial HH admission in CY 2017 (N=443,956)


